Abstract
Background
Patients with chronic total occlusion (CTO) may not participate in regular exercise because of refractory angina. Exercise participation after percutaneous coronary intervention (PCI) for CTO (CTO PCI) and the association of exercise with health status after CTO PCI is unknown.
Methods and Results
Overall, 1000 patients enrolled in the Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion OPEN CTO is a registry were asked about participation in regular exercise at baseline and 12 months after CTO PCI, and the frequency of exercise (<1, 1–2, ≥3 times/week) was collected among exercisers. Health status was assessed using the Seattle Angina Questionnaire (SAQ). Multivariable regression assessed 12‐month health status change across 4 groups defined by exercise frequency at baseline and 12 months after CTO PCI (no regular exercise at baseline and 12 months, reduced, increased, and consistent exercise at 12 months). Among 869 patients with complete exercise data, the proportion that exercised regularly increased from 33.5% at baseline to 56.6% 12 months after CTO PCI (P<0.01). Predictors of regular exercise at 12 months included baseline exercise, smoking, baseline and increase in SAQ scores for angina frequency, physical limitation, quality of life, and summary. After multivariable adjustment, consistent or increased exercise frequency was associated with significantly greater improvement in SAQ scores for angina frequency, physical limitation, quality of life, and summary (P<0.01).
Conclusions
Participation in regular exercise increased significantly 12 months after CTO PCI, and patients who had greater health status benefit after PCI were more likely to exercise regularly at 12 months. CTO PCI may enable coronary artery disease patients with limiting symptoms to engage in regular exercise and to support better long‐term outcomes.
Keywords: chronic total coronary occlusion, coronary artery disease, exercise, percutaneous coronary intervention
Subject Categories: Percutaneous Coronary Intervention
Clinical Perspective
What Is New?
Participation in regular exercise increased 1 year after percutaneous coronary intervention for chronic total occlusion.
Greater improvement in health status after percutaneous coronary intervention for chronic total occlusion was associated with participation in regular exercise.
What Are the Clinical Implications?
Percutaneous coronary intervention for chronic total occlusion provides patients who have limiting angina symptoms with an opportunity to benefit from regular exercise.
Introduction
Physical activity remains an important predictor of outcomes for patients with coronary artery disease (CAD),1 and improving functional status to allow patients to maintain an active lifestyle is a key goal of coronary revascularization.2 Recent studies have found that even small increases in physical activity are associated with lower cardiovascular mortality in patients with stable CAD.3 Unfortunately, patients with CAD often report lower levels of physical activity compared with those without CAD, and little is known about patterns of exercise following coronary revascularization.4 Chronic total occlusion (CTO) of coronary arteries is common in patients with CAD and is frequently associated with significant angina burden and physical limitation (PL) that may limit exercise capacity.4 Although successful percutaneous coronary intervention (PCI) for CTO (CTO PCI) has been shown to improve indexes of exercise performance,5, 6, 7 no studies have reported whether CTO PCI is associated with increased participation in regular exercise in long‐term follow‐up after the procedure. Moreover, the association of improvements in patients’ health status, a known benefit of CTO PCI,2, 8 with exercise patterns after revascularization has never been described. To address these gaps in knowledge, we studied patient‐reported participation in regular exercise at baseline and at 12 months after CTO PCI in a large multicenter study of consecutive patients undergoing CTO PCI. We also examined the association between change in health status 12 months after CTO PCI and exercise status at 12 months to understand whether improved health status was associated with greater exercise participation.
Methods
The data, analytical methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure. However, we encourage parties interested in collaboration and data sharing to contact the investigators.
Study Population
A complete description of the Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion (OPEN CTO) registry has been reported previously.9 Briefly, the OPEN CTO study is a prospective single‐arm study that enrolled consecutive patients with CTO who underwent attempted CTO PCI at 12 participating US sites between January 21, 2014, and July 22, 2015. Among eligible patients scheduled for CTO PCI by a designated operator, those who were ≥18 years of age, who were not pregnant, and who agreed to participate in telephone follow‐up were included. Exclusion criteria included barriers to participating in telephone follow‐up (deafness, dementia, English language, and incarceration). A CTO was defined as a lesion with Thrombolysis in Myocardial Infarction (TIMI) grade 0 antegrade flow that was thought to have been present for at least 3 months. Patients were treated according to the hybrid algorithm for CTO PCI.10 Enrollment of all consenting patients undergoing CTO PCI at each center was confirmed via linkage to each hospital's National Cardiovascular Data Registry CathPCI data to prevent bias related to failure to include all patients undergoing CTO PCI in the study. The results of this audit have been published previously and indicated no evidence of selection bias.9 All patients provided written informed consent, and the protocol was approved by the institutional review board of each participating site.
For this analysis, the study cohort was restricted to patients who completed the Seattle Angina Questionnaire (SAQ) at baseline and at 12‐month follow‐up (4 excluded for missing health status assessments), those with complete responses to questions assessing exercise participation at baseline and 12 months (22 excluded), and those with complete baseline and 12‐month follow‐up (105 excluded), yielding an analytic cohort of 869 patients (87% of potentially eligible patients). Excluded patients did not differ in most baseline characteristics but had slightly lower SAQ PL scores and higher prevalence of diabetes mellitus, heart failure, chronic kidney disease, and non–CTO‐PCI compared with the included patients (Table S1).
Exercise Assessment
At baseline and at protocol‐driven 12‐month follow‐up interviews, patients were asked about participation in regular exercise, with the question, “Have you been exercising on a regular basis (through a program or self‐initiated)?” and a response of either yes or no. Those who answered yes were then asked, “How often do you do this program?” with possible responses of <1, 1 to 2, 3, or >3 times/week. The final question related to exercise session duration was, “How long, on average, does a typical exercise session take?” with possible responses of <30, 30 to 45, or >45 minutes.
We then categorized participants into 4 groups according to their patterns of exercise at baseline and at 12 months. Patients were categorized as nonexercisers if they did not report regular exercise at baseline and at 12 months, as reduced exercisers if they reported regular exercise at baseline but no regular exercise at 12 months, as increased exercisers if they reported either no regular exercise at baseline and regular exercise at 12 months or if they reported a greater frequency of regular exercise at 12‐months than they did at baseline, and as consistent exercisers among regular exercisers who reported the same exercise frequency at baseline and 12‐month follow‐up.
Secondary prevention guidelines recommend at least moderate physical activity for at least 150 minutes/week for patients with CAD. To best approximate adherence to the guideline‐recommended physical activity level, we examined the proportion of patients who exercised for at least 30 minutes/session for at least 3 times/week at baseline and at 12 months.
Health Status Assessment
The SAQ was used to measure CAD‐specific health status.11 Trained study personnel administered the SAQ during the baseline interview when enrolling each patient in OPEN‐CTO. Follow‐up health status assessments were completed by telephone interview using trained, centralized study coordinators 12 months after CTO PCI. The SAQ is a valid and reliable 19‐item questionnaire with a 4‐week recall period that measures 5 domains of health in patients with CAD: angina frequency (AF), angina stability, quality of life (QoL), PL, and treatment satisfaction.11, 12 Domain scores range from 0 to 100, with higher scores indicating fewer symptoms and better QoL. The frequency of angina from the patients’ perspective was captured with the SAQ AF domain, which has been shown to correlate closely with daily angina diaries,13 and QoL was quantified using the SAQ QoL. Overall health status was summarized using the SAQ summary score (SS), which reflects the average of the SAQ PL, AF and QoL domains.14 For the SAQ SS and all domains, a mean change in score of at least 5 points among groups of patients is considered clinically meaningful.11 Long‐term health status change after CTO PCI was a focus of this study, defined as the change in score on each of these domains between baseline and 12‐month follow‐up interviews, stratified by exercise patterns.
Statistical Analyses
Univariate comparisons among the 4 exercise groups (no exercise, reduced, increased, consistent) at baseline were performed using 1‐way ANOVA for continuous variables and χ2 or Fisher exact test for categorical variables. We used the McNemar test to evaluate change from baseline to 12 months in (1) the proportion of patients participating in regular exercise and (2) the proportion of patients who adhered to an exercise frequency similar to guideline recommendations (≥30 minutes/session, ≥3 sessions/week).
To identify independent predictors of participation in regular exercise 12 months after CTO PCI, we used hierarchical multivariable logistic regression to assess predictors of patient‐reported participation in regular exercise at 12 months. Hierarchical modeling was used to account for clustering of patients within sites. We then analyzed each SAQ domain (AF, QoL, PL, and SS) using separate multivariable models to describe the association between exercise frequency and change in health status. To account for potential confounding of the association between change in exercise frequency and change in health status after CTO PCI using the SAQ AF, PL, QoL and SS scores, we used hierarchical multivariable linear regression models to account for clustering within sites and to adjust for potential confounding related to patient‐level variables. We adjusted for potential confounders identified a priori based on clinical experience, including baseline SAQ score in each respective domain, age, sex, number of antianginal medications, body mass index, history of peripheral artery disease, presence of physiologically complete revascularization at the conclusion of the procedure, technical success at 6 months, and current smoking.
We performed a sensitivity analysis to examine (1) the association of change in exercise and health status (SAQ SS) and (2) the predictors of regular exercise at 1 year among those who underwent successful CTO PCI. All statistical analyses were performed using SAS v9.4 (SAS Institute).
Results
The derivation of our analytic cohort is shown in Figure 1. The baseline characteristics of the study population, stratified by exercise participation category, are presented in Table 1. Patients who did not participate in regular exercise at baseline and at follow‐up were more likely to be female and had a greater burden of comorbidities including diabetes mellitus, peripheral arterial disease, and chronic lung disease. Baseline SAQ AF, PL, QoL, and SS were all lowest among those who did not participate in regular exercise at baseline (Table 2). All exercise groups achieved a clinically meaningful change of >5 points in all SAQ scores from baseline to 12 months. There was no difference in change in AF across the 4 exercise groups (P>0.05). The patients whose exercise increased had the largest change in QoL and SS, whereas those who did not participate in regular exercise at baseline and 12 months had the largest improvement in PL scores (Table 2).
Figure 1.
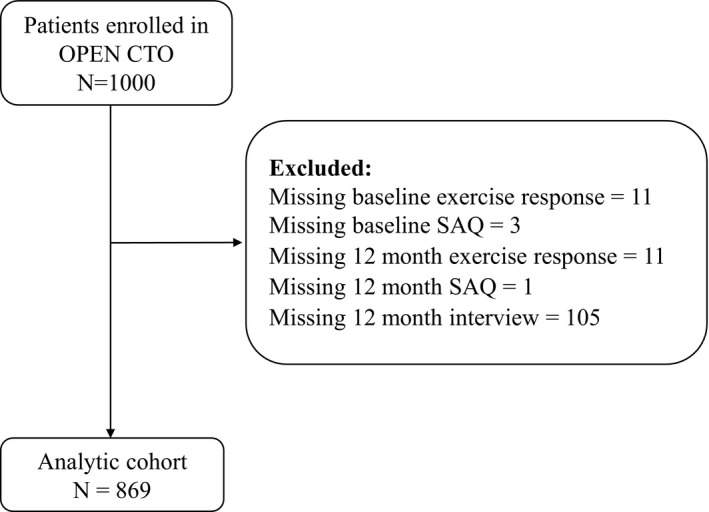
Flowchart of analytic population. OPEN CTO indicates Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion; SAQ, Seattle Angina Questionnaire.
Table 1.
Baseline Characteristics
| Exercise Groups | P Value | ||||
|---|---|---|---|---|---|
| None (n=310) | Reduced (n=94) | Increased (n=332) | Consistent (n=133) | ||
| Age, y | 65.3±10.5 | 65.9±10.6 | 64.6±9.6 | 67.4±9.4 | 0.05 |
| Male | 75.8 | 77.7 | 82.2 | 89.5 | 0.01 |
| White | 91.6 | 88.3 | 89.5 | 91.7 | 0.93 |
| Prior CABG | 39.7 | 33.0 | 35.8 | 36.1 | 0.61 |
| Prior PCI | 67.0 | 61.7 | 67.2 | 66.9 | 0.78 |
| BMI | 31.3±5.9 | 30.4±6.4 | 30.4±6.1 | 28.8±5.0 | <0.001 |
| Current smoker | 19.9 | 12.0 | 10.1 | 3.8 | <0.001 |
| Diabetes mellitus | 45.2 | 35.1 | 39.5 | 31.6 | 0.04 |
| Heart failure | 23.2 | 21.3 | 20.2 | 19.5 | 0.76 |
| Chronic kidney disease | 15.5 | 16.0 | 9.6 | 6.0 | 0.01 |
| Prior stroke/TIA | 6.1 | 8.5 | 6.6 | 10.5 | 0.37 |
| PAD | 22.6 | 13.8 | 15.7 | 12.8 | 0.03 |
| Lung disease | 18.7 | 16.0 | 11.4 | 8.3 | 0.01 |
| No. of antianginals | 1.8±0.9 | 1.4±0.8 | 1.5±0.8 | 1.6±0.8 | <0.001 |
| Any non‐CTO PCI | 10.0 | 16.0 | 14.8 | 12.0 | 0.24 |
| Primary CTO "vessel | 0.95 | ||||
| LAD | 18.7 | 21.3 | 21.4 | 21.8 | |
| LCX | 16.5 | 20.2 | 15.1 | 15.0 | |
| LM | 1.0 | 0.0 | 0.9 | 0.8 | |
| RCA | 63.9 | 58.5 | 62.7 | 62.4 | |
| Lesion length | 65.5 | 58.5 | 60.2 | 59.4 | 0.41 |
| Lesion no. 1: crossing successful | 0.08 | ||||
| Strategy | 37.2 | 38.6 | 39.5 | 49.6 | |
| AWE | 22.0 | 22.7 | 29.9 | 19.5 | |
| ADR | 13.4 | 13.6 | 8.4 | 8.9 | |
| RWE | 27.4 | 25.0 | 22.2 | 22.0 | |
| RD | |||||
| J‐CTO score | 2.4±1.2 | 2.4±1.3 | 2.3±1.3 | 2.3±1.2 | 0.64 |
| Technical success at 6 m | 90.0 | 90.4 | 90.1 | 89.5 | 0.10 |
Data presented as mean±SD for continuous variables or percentage for categorical variables. ADR indicates antegrade dissection and reentry; AWE, antegrade wire escalation; BMI, body mass index; CABG, coronary artery bypass grafting; CTO, chronic total occlusion; J‐CTO, Japanese multicenter CTO registry; LAD, left anterior descending artery; LCX, left circumference artery; LM, left main artery; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; RCA, right coronary artery; RD, retrograde dissection; RWE, retrograde wire escalation; TIA, transient ischemic attack.
Table 2.
Baseline, 1 Year, and Change in SAQ Scores
| Exercise Group | |||||
|---|---|---|---|---|---|
| None (n=310) | Reduced (n=94) | Increased (n=332) | Consistent (n=133) | P Value | |
| SAQ AF (BL) | 65.4±28.7 | 75.4±22.6 | 72.1±26.6 | 72.3±25.1 | 0.001 |
| SAQ AF (1 Y) | 89.7±19.8 | 93.8±16.5 | 95.2±15.6 | 95.6±13.3 | <0.001 |
| SAQ AF change (1 Y‐BL) | 24.3±27.2 | 18.4±24.2 | 23.1±26.1 | 23.3±25.7 | 0.30 |
| SAQ PL (BL) | 57.4±27.0 | 68.7±24.2 | 68.1±25.4 | 76.1±21.1 | <0.001 |
| SAQ PL (1 Y) | 92.0±16.3 | 95.7±11.5 | 96.5±11.0 | 97.7±6.3 | <0.001 |
| SAQ PL change (1 Y‐BL) | 30.1±23.9 | 21.5±19.7 | 26.6±26.0 | 19.7±18.2 | <0.001 |
| SAQ QoL (BL) | 44.4±27.2 | 49.3±25.8 | 49.5±27.0 | 60.2±25.3 | <0.001 |
| SAQ QoL (1 Y) | 72.9±24.5 | 70.8±24.4 | 83.8±17.1 | 86.6±16.3 | <0.001 |
| SAQ QoL change (1 Y‐BL) | 28.6±26.3 | 21.5±25.4 | 34.3±26.5 | 26.4±25.5 | <0.001 |
| SAQ SS (BL) | 55.9±23.2 | 64.3±19.2 | 63.2±22.4 | 69.4±19.2 | <0.001 |
| SAQ SS (1 Y) | 83.5±17.8 | 84.8±16.2 | 91.2±12.3 | 93.1±9.6 | <0.001 |
| SAQ SS change (1 Y‐BL) | 27.5±20.8 | 20.5±17.5 | 28.0±21.7 | 23.7±18.6 | 0.004 |
1 Y indicates 1 year after CTO‐PCI; AF, angina frequency; BL, baseline; SS, summary score; PL, physical limitation; QoL, quality of life; SAQ, Seattle Angina Questionnaire.
Change in Exercise Participation After CTO PCI
The proportion of patients who reported exercising regularly increased significantly from baseline to 12 months after CTO PCI (291 [33.5%] versus 492 [56.6%], P<0.01). Among 265 patients who did not report regular exercise at baseline but who participated in regular exercise at 12 months, 6 (2.2%) exercised <1 time/week, 46 (17.4%) exercised 1 to 2 times/week, 84 (31.7%) exercised 3 times/week, and 129 (48.7%) exercised >3 times/week at 12 months (Figure 2). A commonly recommended physical activity level for patients with CAD is participation in moderate physical activity for at least 150 minutes/week.15 We found that the proportion of those who reported exercising at least 3 times/week for at least 30 minutes/session increased from 20.8% (181/869) at baseline to 40.3% (350/869) at 12 months (P<0.0001).
Figure 2.
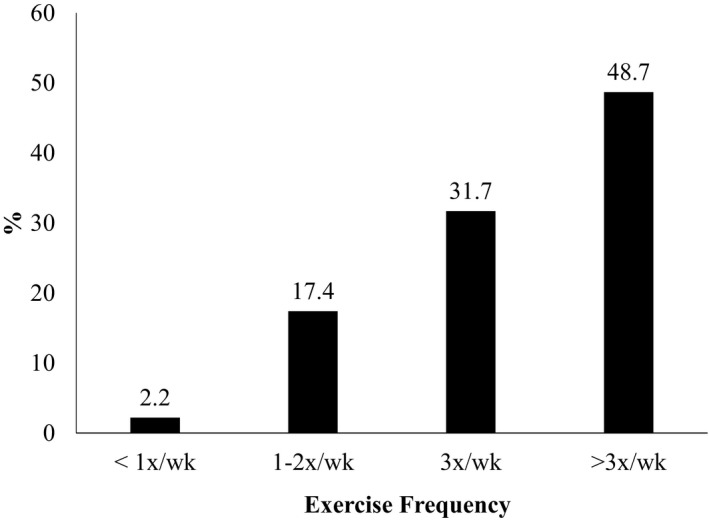
Distribution of exercise frequency at 1 year among patients who did not participate in regular exercise at baseline but did participate in regular exercise at 12 months after percutaneous coronary intervention for coronary chronic total occlusion (n=265).
Predictors of Regular Exercise at 12 Months
Significant predictors of regular exercise at 12 months are presented in Figure 3 and Figures S1 through S3. Current smoking was associated with a lower likelihood of regular exercise at 12 months (odds ratio [OR]: 0.4 [95% CI, 0.25–0.64]). Regular exercise at baseline was associated with greater likelihood of exercise at 12 months (OR: 3.55 [95% CI, 2.50–5.02]), as were higher baseline SAQ SS scores (OR: 1.20 per 5‐point increase [95% CI, 1.13–1.28]; Figure 3). SAQ scores for AF (OR: 1.08 per 5‐point change [95% CI, 1.02–1.13]), PL (OR: 1.15 per 5‐point change [95% CI, 1.07–1.24]), and QoL (OR: 1.14 per 5‐point change [95% CI, 1.09–1.19]) were also predictors of regular exercise at 12 months (Figures S1–S3). Interestingly, patients who reported greater health status increases between baseline and 12 months after CTO PCI were also more likely to exercise regularly (OR: 1.21 per 5‐point change in SS [95% CI, 1.14–1.29], Figure 3; OR: 1.07 per 5‐point change in AF [95% CI, 1.02–1.13], 1.12 per 5‐point change in PL [95% CI, 1.03–1.20], and 1.17 per 5‐point change in QoL [95% CI, 1.12–1.22]; Figures S1–S3).
Figure 3.
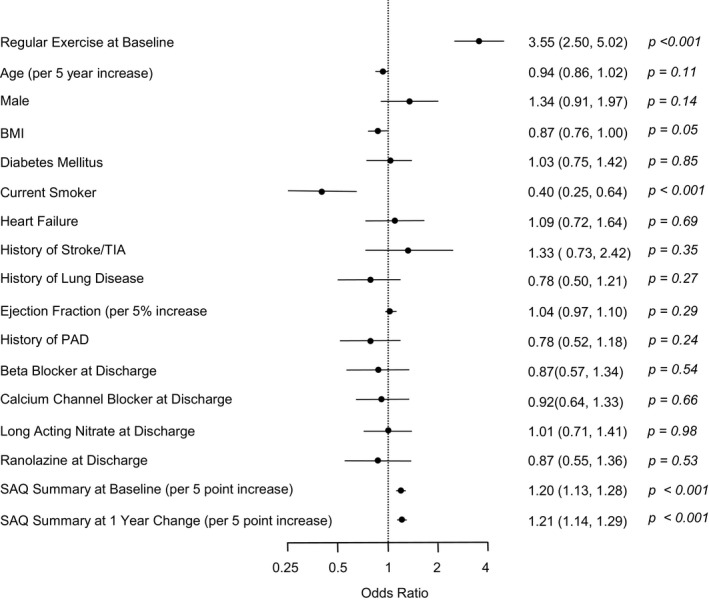
Predictors of participation in regular exercise at 1 year. BMI indicates body mass index; PAD, peripheral artery disease; SAQ, Seattle Angina Questionnaire; TIA, transient ischemic attack.
Association of Exercise and Health Status
Compared with patients who reported that they did not participate in regular exercise both at baseline and at 12‐month follow‐up, increases in both patient‐reported regular exercise and consistent exercise were associated with greater increase in SAQ AF, PL, QoL, and SS scores. This association remained significant after extensive multivariable adjustment (Figure 4). Both increased and consistent exercise were associated with clinically meaningful change (≥5‐point change) in SAQ scores for QoL (9.13 [95% CI, 6.14–12.12] and 7.36 [95% CI, 3.34–11.37], respectively) and SS (5.58 [95% CI, 3.49–7.67] and 5.28 [95% CI, 2.49–8.08], respectively). However, both increased and consistent exercise were associated with improved SAQ scores for AF (3.83 [95% CI, 1.28–6.37] and 4.26 [95% CI, 0.89–7.64], respectively) and PL (3.55 [95% CI, 1.42–5.69] and 3.52 [95% CI, 0.79–6.25], respectively) that were statistically significant (P<0.05 for all) but clinically small.
Figure 4.
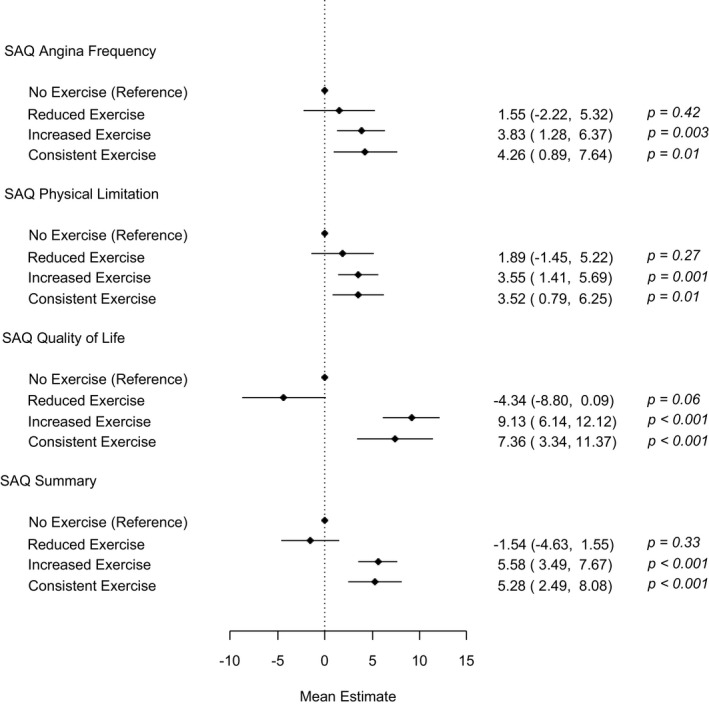
Association of change in exercise with change in Seattle Angina Questionnaire (SAQ) scores at 1 year after percutaneous coronary intervention for chronic total occlusion (CTO PCI).
Patients who reported less exercise at 12 months than they reported at baseline experienced similar change in health status, as assessed by each SAQ domain, compared with those who reported no regular exercise (Figure 4). Restricting the analysis to only those with technical success at 6 months produced similar results (Figures S4–S6).
Discussion
Successful treatment of CAD involves multiple interventions beyond pharmacologic therapy and coronary revascularization and should include lifestyle changes such as diet modification and exercise to maximize patients’ functional capacity and to reduce their risk of future cardiac events. In this study of patients undergoing CTO PCI, we found that only 1 in 3 patients reported any regular exercise, but this proportion increased to more than half of patients at 12 months after CTO PCI. Importantly, we found that exercise was independently associated with improved health status at 12 months after CTO PCI and that patients who reported improved health status after CTO PCI were more likely to participate in exercise 12 months after the procedure. Specifically, among those who increased or were consistent with their exercise frequency after CTO PCI, there were clinically meaningful improvements in QoL and overall health status and fewer but statistically significant improvements in their angina and disease‐specific physical function. In total, these findings underscore the potential impact of CTO PCI in enabling patients to pursue greater levels of regular physical activity for optimization of QoL and reduction of long‐term cardiac event rates.
Regular exercise is associated with reduced cardiovascular mortality and improved QoL,1, 3, 16 and as a result, guidelines strongly advise a minimum of 30 minutes of moderate physical activity at least 5 days a week (minimum 150 minutes/week) to reduce cardiovascular risk in patients with stable CAD.17 Patients with CTO commonly have refractory angina, which limits their participation in exercise. In accordance with data showing improvements in health status after CTO PCI,18 a principal indication for CTO PCI is to improve symptoms and functional capacity.19, 20 However, no prior studies have assessed whether the improvement in symptoms and health status associated with CTO PCI is associated with greater participation in regular exercise. In the present analysis, we show that among patients who did not participate in regular exercise at baseline, a majority increased participation in regular exercise by 12 months. In addition, the proportion of those who participated in exercise levels similar to guideline recommendations doubled from baseline to 12 months. With such increase in physical activity levels, these patients are likely to reap the benefits of regular exercise participation for overall health status and, potentially, cardiovascular events.3, 21
Our work supports and extends prior studies in the field. Few studies have examined the relationship between CTO PCI and exercise capacity. A study of 32 male patients with CTO and angina or congestive heart failure symptoms assessed change in peak oxygen uptake during cardiopulmonary exercise testing after CTO PCI. The authors found that successful CTO PCI was associated with an increase in peak V̇O2 from 17.7 mL/kg per minute at baseline to 19.1 mL/kg per minute at 5‐month follow‐up.5 In a separate prospective multicenter study, cardiopulmonary exercise testing was performed in 50 patients with CTO at baseline and at 7 months after CTO PCI. Peak V̇O2 significantly increased from 16.59 mL/kg per minute at baseline to 18.42 mL/kg per minute.6 Rossello et al demonstrated a significant improvement in exercise capacity measured by the 6‐minute walk test at 6 months after CTO PCI.7 Although these surrogate end points of exercise capacity may indicate greater ability to participate in regular exercise after CTO PCI, our study extends this work by documenting improvements with routine exercise in a large sample of unselected patients.
About a third of patients did not increase their exercise participation despite significant improvements in their symptoms and PL due to angina. The potential reasons for this finding are unclear but may involve a subset of patients who have other factors contributing to functional limitations beyond those attributable to their angina symptoms. Interestingly, patients who did not exercise at baseline or at 12‐month follow‐up reported the greatest improvements in functional capacity on the SAQ PL domain. The significance of this finding is unclear and may suggest that the possibility of engaging in exercise should be readdressed in follow‐up after PCI to identify patients who were previously unable to participate, given that functional status may improve enough to allow participation after CTO PCI. Further investigation is needed to better characterize those patients who are able to exercise and those who do not participate in regular exercise despite improvement in symptoms and functional capacity. This approach would allow for further exploration of novel strategies to engage these patients in cardiac rehabilitation or lifestyle counseling and help them adopt a healthy lifestyle.
We found that patients who had higher SAQ scores at baseline were more likely to exercise at follow‐up, potentially reflecting lower disease burden and better baseline functional capacity in comparison to patients who were more limited at baseline. However, we also found that patients who experienced greater improvements in health status, as assessed with the SAQ, were more likely to exercise regularly 12 months after the procedure. This finding may underscore the clinical impact of the procedure to achieve durable functional status improvements. Nevertheless, this observational study cannot determine whether exercise is a consequence of patients’ improved health status or if it is actually contributing to improved health status. Further studies will be needed to examine the impact of interventions to increase exercise after PCI and to determine how to maximize long‐term participation with regular exercise.
Our results should be interpreted in the context of the following potential limitations. First, OPEN CTO is a single‐arm study without a placebo control arm; therefore, residual and unmeasured confounding cannot be excluded, and a placebo effect from CTO PCI cannot be excluded. Second, we were unable to assess the potential impact of concurrent interventions, such as changes in antianginal medical regimens or participation in cardiac rehabilitation. Third, we cannot determine exactly which exercise regimens patients participated in, and further study is needed to determine whether some programs are associated with greater benefit than others. However, these results generalize to patient report of exercise participation, consistent with what patients typically report during office encounters with their physicians. Fourth, although the baseline characteristics of those with and without complete exercise data were largely similar, the presence of missing exercise data introduces the possibility of bias in our analysis. Finally, we relied on self‐reported participation in regular exercise for assessment of physical activity. Although these questions do not allow precise identification of exercise regions or duration of exercise,22 similar parsimonious questionnaires have been shown to possess prognostic value in patients with CAD.16
Conclusions
CTO PCI was associated with significantly increased participation in regular exercise at 12 months after PCI, and patients with greater health status improvement in follow‐up after the procedure were more likely to participate in regular exercise at 12 months. Because regular exercise was also an important predictor of better health status, as assessed by each SAQ domain, CTO PCI appears to be associated with important improvements in functional capacity that warrant further study.
Sources of Funding
The OPEN CTO (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures) study was supported by an investigator‐initiated grant from Boston Scientific. All data collection, data analyses, the preparation of the article, and the decision to submit the article for publication were done independently of the study sponsor. Dr Peri‐Okonny is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award no. T32HL110837. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
Grantham has received research grant support from and served on the advisory board for Boston Scientific, has received speaking fees and honoraria from Boston Scientific and Abbott Vascular, and is a part‐time employee of and owns equity in Corindus. Spertus received grant funding from the Patient‐Centered Outcomes Research Institute, Abbott Vascular, and Lilly and an equity interest in Health Outcomes Sciences (copyright to the Seattle Angina Questionnaire [SAQ]). Kirtane received institutional grants to Columbia University and/or Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, ReCor Medical, and Spectranetics. Lombardi owns equity in BridgePoint Medical. Salisbury received research grant support from Boston Scientific and Gilead and consulting or speaking fees from Abiomed, Boston Scientific, and Medtronic. The remaining authors have no disclosures to report.
Supporting information
Table S1. Baseline Characteristics of Excluded and Included Patients
Figure S1. Predictors of regular exercise at 1 year including Seattle Angina Questionnaire angina frequency.
Figure S2. Predictors of regular exercise at 1 year including Seattle Angina Questionnaire physical limitation.
Figure S3. Predictors of regular exercise at 1 year including Seattle Angina Questionnaire quality of life.
Figure S4. Association of change in exercise and health status change at 1 year among patients with successful percutaneous coronary intervention for chronic total occlusion at 6 months.
Figure S5. Predictors of exercise at 1 year among patients with successful percutaneous coronary intervention for chronic total occlusion at 6 months.
Figure S6. Distribution of exercise frequency at 12 months among patients who did not participate in regular exercise at baseline but did participate in regular exercise at 12 months among those with successful percutaneous coronary intervention for chronic total occlusion.
(J Am Heart Assoc. 2019;8:e011629 DOI: 10.1161/JAHA.118.011629.)
References
- 1. Alves AJ, Viana JL, Cavalcante SL, Oliveira NL, Duarte JA, Mota J, Oliveira J, Ribeiro F. Physical activity in primary and secondary prevention of cardiovascular disease: overview updated. World J Cardiol. 2016;8:575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Safley DM, Grantham JA, Hatch J, Jones PG, Spertus JA. Quality of life benefits of percutaneous coronary intervention for chronic occlusions. Catheter Cardiovasc Interv. 2014;84:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stewart RAH, Held C, Hadziosmanovic N, Armstrong PW, Cannon CP, Granger CB, Hagstrom E, Hochman JS, Koenig W, Lonn E, Nicolau JC, Steg PG, Vedin O, Wallentin L, White HD. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017;70:1689–1700. [DOI] [PubMed] [Google Scholar]
- 4. Jeroudi OM, Alomar ME, Michael TT, El Sabbagh A, Patel VG, Mogabgab O, Fuh E, Sherbet D, Lo N, Roesle M, Rangan BV, Abdullah SM, Hastings JL, Grodin J, Banerjee S, Brilakis ES. Prevalence and management of coronary chronic total occlusions in a tertiary Veterans Affairs hospital. Catheter Cardiovasc Interv. 2014;84:637–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abdullah SM, Hastings JL, Amsavelu S, Garcia‐Morales F, Hendrix F, Karatasakis A, Danek BA, Karacsonyi J, Rangan BV, Roesle M, Khalili H, Banerjee S, Brilakis ES. Percutaneous coronary intervention of coronary chronic total occlusions improves peak oxygen uptake during cardiopulmonary exercise testing. J Invasive Cardiol. 2017;29:83–91. [PubMed] [Google Scholar]
- 6. Mashayekhi K, Neuser H, Kraus A, Zimmer M, Dalibor J, Akin I, Werner G, Aurel T, Neumann FJ, Behnes M. Successful percutaneous coronary intervention improves cardiopulmonary exercise capacity in patients with chronic total occlusions. J Am Coll Cardiol. 2017;69:1095–1096. [DOI] [PubMed] [Google Scholar]
- 7. Rossello X, Pujadas S, Serra A, Bajo E, Carreras F, Barros A, Cinca J, Pons‐Llado G, Vaquerizo B. Assessment of inducible myocardial ischemia, quality of life, and functional status after successful percutaneous revascularization in patients with chronic total coronary occlusion. Am J Cardiol. 2016;117:720–726. [DOI] [PubMed] [Google Scholar]
- 8. Hirai T, Grantham JA, Sapontis J, Cohen DJ, Marso SP, Lombardi W, Karmpaliotis D, Moses J, Nicholson WJ, Pershad A, Wyman RM, Spaedy A, Cook S, Doshi P, Federici R, Nugent K, Gosch KL, Spertus JA, Salisbury AC. Impact of subintimal plaque modification procedures on health status after unsuccessful chronic total occlusion angioplasty. Catheter Cardiovasc Interv. 2018;91:1035–1042. [DOI] [PubMed] [Google Scholar]
- 9. Sapontis J, Marso SP, Cohen DJ, Lombardi W, Karmpaliotis D, Moses J, Nicholson WJ, Pershad A, Wyman RM, Spaedy A, Cook S, Doshi P, Federici R, Thompson CR, Nugent K, Gosch K, Spertus JA, Grantham JA. The outcomes, patient health status, and efficiency in chronic total occlusion hybrid procedures registry: rationale and design. Coron Artery Dis. 2017;28:110–119. [DOI] [PubMed] [Google Scholar]
- 10. Brilakis ES, Grantham JA, Rinfret S, Wyman RM, Burke MN, Karmpaliotis D, Lembo N, Pershad A, Kandzari DE, Buller CE, DeMartini T, Lombardi WL, Thompson CA. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012;5:367–379. [DOI] [PubMed] [Google Scholar]
- 11. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. [DOI] [PubMed] [Google Scholar]
- 12. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74:1240–1244. [DOI] [PubMed] [Google Scholar]
- 13. Arnold SV, Kosiborod M, Li Y, Jones PG, Yue P, Belardinelli L, Spertus JA. Comparison of the Seattle Angina Questionnaire with daily angina diary in the TERISA clinical trial. Circ Cardiovasc Qual Outcomes. 2014;7:844–850. [DOI] [PubMed] [Google Scholar]
- 14. Chan PS, Jones PG, Arnold SA, Spertus JA. Development and validation of a short version of the Seattle Angina Questionnaire. Circ Cardiovasc Qual Outcomes. 2014;7:640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd‐Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. [DOI] [PubMed] [Google Scholar]
- 16. Arnson Y, Rozanski A, Gransar H, Hayes SW, Friedman JD, Thomson LEJ, Berman DS. Impact of exercise on the relationship between CAC scores and all‐cause mortality. JACC Cardiovasc Imaging. 2017;10:1461–1468. [DOI] [PubMed] [Google Scholar]
- 17. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TA, Yanovski SZ. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960–2984. [DOI] [PubMed] [Google Scholar]
- 18. Grantham JA, Jones PG, Cannon L, Spertus JA. Quantifying the early health status benefits of successful chronic total occlusion recanalization: results from the Flowcardia's Approach to Chronic Total Occlusion Recanalization (FACTOR) trial. Circ Cardiovasc Qual Outcomes. 2010;3:284–290. [DOI] [PubMed] [Google Scholar]
- 19. Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Juni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio‐Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541–2619. [DOI] [PubMed] [Google Scholar]
- 20. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:2574–2609. [DOI] [PubMed] [Google Scholar]
- 21. Stewart R, Held C, Brown R, Vedin O, Hagstrom E, Lonn E, Armstrong P, Granger CB, Hochman J, Davies R, Soffer J, Wallentin L, White H. Physical activity in patients with stable coronary heart disease: an international perspective. Eur Heart J. 2013;34:3286–3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003;37:197–206; discussion 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline Characteristics of Excluded and Included Patients
Figure S1. Predictors of regular exercise at 1 year including Seattle Angina Questionnaire angina frequency.
Figure S2. Predictors of regular exercise at 1 year including Seattle Angina Questionnaire physical limitation.
Figure S3. Predictors of regular exercise at 1 year including Seattle Angina Questionnaire quality of life.
Figure S4. Association of change in exercise and health status change at 1 year among patients with successful percutaneous coronary intervention for chronic total occlusion at 6 months.
Figure S5. Predictors of exercise at 1 year among patients with successful percutaneous coronary intervention for chronic total occlusion at 6 months.
Figure S6. Distribution of exercise frequency at 12 months among patients who did not participate in regular exercise at baseline but did participate in regular exercise at 12 months among those with successful percutaneous coronary intervention for chronic total occlusion.


