Abstract
Background
Many adults eligible for statin therapy for cardiovascular disease prevention are untreated. Our objective was to investigate patient‐reported reasons for statin underutilization, including noninitiation, refusal, and discontinuation.
Methods and Results
This study included the 5693 adults recommended for statin therapy in the PALM (Patient and Provider Assessment of Lipid Management) registry. Patient surveys evaluated statin experience, reasons for declining or discontinuing statins, and beliefs about statins and cardiovascular disease risk. Overall, 1511 of 5693 adults (26.5%) were not on treatment. Of those not on a statin, 894 (59.2%) reported never being offered a statin, 153 (10.1%) declined a statin, and 464 (30.7%) had discontinued therapy. Women (relative risk: 1.22), black adults (relative risk: 1.48), and those without insurance (relative risk: 1.38) were most likely to report never being offered a statin. Fear of side effects and perceived side effects were the most common reasons cited for declining or discontinuing a statin. Compared with statin users, those who declined or discontinued statins were less likely to believe statins are safe (70.4% of current users vs. 36.9% of those who declined and 37.4% of those who discontinued) or effective (86.3%, 67.4%, and 69.1%, respectively). Willingness to take a statin was high; 67.7% of those never offered and 59.7% of patients who discontinued a statin would consider initiating or retrying a statin.
Conclusions
More than half of patients eligible for statin therapy but not on treatment reported never being offered one by their doctor. Concern about side effects was the leading reason for statin refusal or discontinuation. Many patients were willing to reconsider statin therapy if offered.
Keywords: cardiovascular disease prevention, patient education/teaching, statin therapy
Subject Categories: Cardiovascular Disease, Primary Prevention
Short abstract
See Editorial by Braun
Clinical Perspective
What Is New?
More than half of patients eligible for but not on statin therapy report never being offered a statin by their doctor.
Fear of side effects and perceived side effects are the most common reasons for declining or discontinuing statin therapy.
Willingness to take a statin is high, among both patients who have declined statin therapy and those who have never been offered one.
What Are the Clinical Implications?
A significant opportunity exists to increase statin utilization by improving physician recognition of eligible patients.
Addressing patient perception of statin safety, especially among patients who decline or discontinue statin therapy, may improve statin utilization.
Patients who previously discontinued their statin may be receptive to retrying one if offered by their physician.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality in the United States, with nearly half of US adults projected to have some form of ASCVD by 2030.1 HMG‐CoA reductase (3‐hydroxy‐3‐methylglutaryl‐CoA reductase) inhibitors, or statins, are among the most effective medications for prevention of ASCVD.2 In 2013, the American College of Cardiology and the American Heart Association (ACC/AHA) released guidelines for statin use for ASCVD prevention, broadening statin recommendations to >12 million newly eligible high‐risk adults in the United States for primary prevention.3
Unfortunately, a large gap in statin use remains between guideline recommendations and actual clinical practice for both primary and secondary prevention. Even among the highest risk patients, those with established ASCVD, utilization is low.4, 5, 6 We recently reported that up to a quarter of those eligible for treatment were not on a statin in community practice.7 Statin underutilization results from failure of clinicians to identify and offer statins to eligible patients, patient refusal when offered, and discontinuation by some patients who are tried on the medication.8 Delineating the extent and causes of each of these aspects will help clinicians design appropriate interventions to improve both primary and secondary ASCVD prevention.
In this study, we analyzed data from the PALM (Patient and Provider Assessment of Lipid Management) registry to evaluate (1) patient‐reported reasons for lack of statin utilization, including lack of therapy being offered, patient refusal, and discontinuation of prior treatment, and (2) differences in beliefs regarding safety and efficacy of statin therapy and perceived risk of ASCVD between current statin users and those who were never offered, declined, or discontinued treatment.
Methods
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
Patient Population
The PALM registry was a cross‐sectional registry in the United States designed to evaluate lipid management practices and patient and provider beliefs about cholesterol, statin therapy, and heart disease. PALM enrolled 7938 patients from 140 cardiology, primary care, and endocrinology practices in the United States who were potentially eligible for statin therapy, including adults on statins, adults with risk factors for ASCVD, and adults with prior ASCVD. Patient surveys evaluated patient‐reported current statin utilization and prior statin experience as well as beliefs regarding statin efficacy and safety, risk of ASCVD, and trust in the healthcare provider.9 Surveys were collected on an iPad using a digital questionnaire that patients completed at enrollment. Core lab lipid panels were measured for all patients, and chart abstractions were completed to assess clinical characteristics. Enrollment was conducted between May 27, 2015, and November 12, 2015. All participants provided signed informed consent to participate, and each site obtained institutional review board approval for participation.
Among 7938 patients enrolled, 563 (7.1%) did not have either baseline chart review data (n=34, 0.4%) or lipid values (n=167, 2.1%) or did not complete a survey (n=347, 4.4%) and were ineligible for this analysis. Among those with survey data, we included 5693 participants who would have been recommended for statin therapy according to the 2013 ACC/AHA guideline10: (1) prior ASCVD (prior coronary artery disease or coronary revascularization, abdominal aortic aneurysm, carotid artery stenosis, peripheral arterial disease or peripheral revascularization, and prior stroke or transient ischemic attack), (2) LDL‐C (low‐density lipoprotein cholesterol) ≥190 mg/dL, (3) type 2 diabetes mellitus and age 40–75 years, or (4) estimated 10‐year ASCVD risk ≥7.5% by the pooled cohort equations and age 40 to 75 years.
At the time of enrollment, patients were asked whether they were currently on a statin or had previously been on any statin. Those never on a statin were asked whether they had ever been recommended a statin by a healthcare provider. Among those previously offered a statin and those who discontinued therapy, reasons for declining or discontinuing therapy were assessed. Patients were categorized into 4 groups: those currently on therapy, former statin users who had discontinued therapy, those who had been offered therapy by their doctor but declined, and those who reported they had never been offered statin therapy. Beliefs about statins and their own risk of heart disease were surveyed using 5‐point Likert scales and then categorized into binary variables for analysis. See Data S1 for the survey questions used in this analysis.
Analysis
Patient characteristics and beliefs were compared between current users and those who were never offered treatment, declined, or discontinued therapy. In descriptive analyses, categorical variables were summarized using percentages and compared using χ2 tests, continuous variables were presented using median (interquartile range), and these were compared using Wilcoxon rank sum tests. Reasons for lack of statin use were evaluated overall and stratified by indication.
To evaluate characteristics associated with never versus ever being offered a statin, which included those who declined or discontinued a statin, a multivariable model with Poisson regression was used to display the relative risks of the outcomes modeled.11 Clustering of patients within the same hospital was accounted for using the generalized estimating equation method.12 Variables considered and included in the model were age, race (white, black, or other), sex, Hispanic ethnicity, education (at least some college versus middle/high school), household income (nominal categorical variable), insurance (government, private, other, or none), type of site specialty (cardiology, primary/family care/internal medicine, endocrinology/other). The linearity of age in respect to the outcome “never being offered a statin” was checked and fitted as linear spline terms with 2 knots at 60 and 75, allowing different slopes. Except for the income variable, the percentage of missing for all variables above was <3%. The income value was missing for ≈7.0% of patients, and 26.9% of patients answered “I prefer not to answer this question.” We used multiple imputation with 20 imputations to impute all missing values of all variables. SAS procedure PROC MI was used for the imputation process, and SAS PROC MIANALYZE was used to combine the results of analysis carried out from 20 imputed data sets. The results of how factors associate with outcome were presented as relative risks with 95% CIs.
All statistical analyses were performed using SAS v9.4 (SAS Institute).
Results
Of the 5693 adults in the PALM registry who met ACC/AHA guidelines for statin therapy, 3184 (55.9%) had prior ASCVD and 2509 (44.1%) had an ACC/AHA indication for primary prevention statin use. The median ages of these primary and secondary prevention populations were 66 and 70 years, respectively; 51.9% and 36.3%, respectively, were female; and 17.7% and 10.1%, respectively, self‐identified as black race.
Overall, 26.5% (n=1511) of adults recommended for treatment were not on treatment, including 37.7% (n=945) of those recommended for primary prevention and 17.8% (n=566) of those recommended for secondary prevention. Of the 1511 adults recommended for but not on statin therapy, 894 (59.2%) reported never having been offered a statin, 464 (30.7%) reported having previously taken a statin but discontinuing therapy, and 153 (10.1%) had been offered statin therapy but declined (Figure 1).
Figure 1.
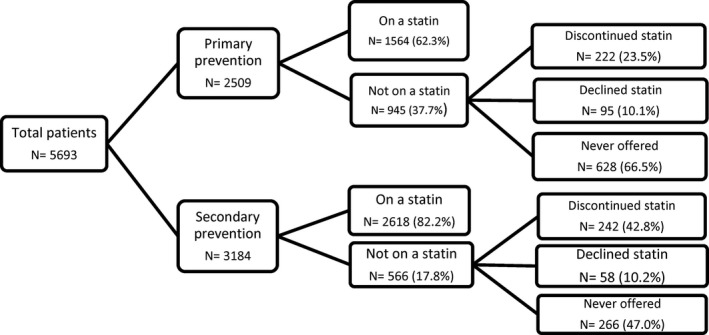
Statin utilization among adults recommended for treatment by indication.
Patient Characteristics
Table 1 shows characteristics of patients recommended for statins for either primary or secondary prevention stratified by statin use: current users, discontinued, declined, and never offered. Current statin users were more likely to be male (60.6%) than those who discontinued (42.5%) or declined (41.8%) statin therapy. Current statin users also had the highest rate of any atherosclerotic disease (62.6%), followed by those who discontinued statins (52.2%) and those who declined a statin (37.9%). Education levels were similar between current users and those who discontinued or declined statins (63.6% versus 66.4% and 58.3%, respectively, with at least some college; P=0.24 and P=0.18). There was no statistically significant difference in income levels among current users, those who discontinued, and those who declined statins. However, those who declined statins were more likely to have private insurance (67.3%) than current statin users (57.3%, P=0.02) or former statin users (55.3%, P=0.0002). There was no significant difference in use of nonstatin lipid‐lowering medications between current and former statin users (26.9% versus 28.6%, P=0.43), but those who declined statins were more likely than current users to use nonstatin therapy (35.8%, P=0.02). Total cholesterol and LDL‐C levels were highest in former statin users. Among the primary prevention population, estimated 10‐year ASCVD risk was similar for those on a statin and those who discontinued, declined, or reported never having been offered a statin (14.4–14.5% 10‐year ASCVD risk; Table 1).
Table 1.
Characteristics of Current, Former, and Never Statin Users
| Current Statin Therapy (n=4182) | Discontinued Statin Therapy (n=464) | P Value vs Current | Declined Statin Therapy (n=153) | P Value vs Current | Never Offered (n=894) | P Value vs Current | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Age, y | 68.0 (61.0–74.0) | 68.0 (61.0–75.0) | 0.56 | 67.0 (59.0–72.0) | 0.04 | 68.0 (60.0–72.0) | 0.02 |
| Sex (% male) | 2535 (60.6) | 197 (42.5) | <0.0001 | 64 (41.8) | <0.0001 | 437 (48.9) | <0.0001 |
| Race | |||||||
| White | 3581 (85.6) | 407 (87.7) | 0.56 | 128 (83.7) | 0.58 | 685 (76.6) | <0.0001 |
| Black | 504 (12.1) | 50 (10.8) | 23 (15.0) | 187 (20.9) | |||
| Asian | 86 (2.1) | 6 (1.3) | 2 (1.3) | 17 (1.9) | |||
| Other | 11 (0.3) | 1 (0.2) | 0 (0) | 5 (0.6) | |||
| Ethnicity: Hispanic | 419 (10.0) | 56 (11.2) | 0.43 | 30 (19.6) | 0.0001 | 125 (14.0) | 0.0005 |
| PALM practice type | |||||||
| Cardiology | 2102 (50.3) | 209 (45.0) | 0.18 | 56 (36.6) | 0.004 | 254 (28.4) | <0.0001 |
| Primary care/family practice/internal medicine | 1796 (43.0) | 217 (46.8) | 86 (56.2) | 570 (63.8) | |||
| Endocrinology | 146 (3.5) | 19 (4.1) | 8 (5.2) | 21 (2.4) | |||
| Other | 138 (3.3) | 19 (4.1) | 3 (2.0) | 49 (5.5) | |||
| Insurance status | |||||||
| Private | 2391 (57.3) | 256 (55.3) | 0.0002 | 103 (67.3) | 0.02 | 486 (54.4) | 0.0006 |
| Government | 1709 (41.0) | 186 (40.2) | 46 (30.1) | 374 (41.9) | |||
| Other/none | 72 (1.7) | 21 (4.5) | 4 (2.6) | 33 (3.7) | |||
| Education completed | |||||||
| At least some college | 2615 (63.6) | 306 (66.4) | 0.24 | 88 (58.3) | 0.18 | 502 (59.9) | 0.04 |
| Household income | |||||||
| ≤$35 000 | 957 (34.8) | 135 (40.8) | 0.07 | 35 (34.7) | 0.64 | 220 (41.4) | 0.02 |
| $35 000–$74 999 | 919 (33.4) | 112 (33.8) | 38 (37.6) | 162 (30.5) | |||
| $75 000–$99 999 | 319 (11.6) | 32 (9.7) | 8 (7.9) | 63 (11.8) | |||
| ≥$100 000 | 556 (20.2) | 52 (15.7) | 20 (19.8) | 87 (16.4) | |||
| Clinical characteristics | |||||||
| Any ASCVD | 2618 (62.6) | 222 (52.2) | <0.0001 | 58 (37.9) | <0.0001 | 266 (29.8) | <0.0001 |
| Prior MI | 801 (19.2) | 84 (18.1) | 0.58 | 9 (5.9) | <0.0001 | 35 (3.9) | <0.0001 |
| Prior stroke | 249 (6.0) | 39 (6.5) | 0.66 | 6 (3.9) | 0.29 | 29 (3.2) | 0.001 |
| Hypertension | 3518 (84.1) | 368 (79.3) | 0.01 | 115 (75.2) | 0.003 | 641 (71.7) | <0.0001 |
| Heart failure | 436 (10.5) | 59 (12.8) | 0.14 | 7 (4.6) | 0.02 | 55 (6.2) | <0.0001 |
| 10‐y risk (among primary prevention) | 14.5 (9.6–22.2) | 14.5 (9.6–21.7) | 0.60 | 14.4 (10.3–23.2) | 0.93 | 14.4 (9.7–21.0) | 0.81 |
| Lipids and therapy | |||||||
| Total cholesterol, mg/dL | 159.0 (137.0–185.0) | 215.0 (183.0–249.0) | <0.0001 | 205.0 (175.0–241.0) | <0.0001 | 194.0 (169.0–219.0) | <0.0001 |
| LDL‐C, mg/dL | 86.0 (68.0–107.0) | 134.0 (108.0–162.0) | <0.0001 | 125.0 (98.0–161.0) | <0.0001 | 117.0 (95.0–138.0) | <0.0001 |
| Currently on nonstatin lipid therapy | 1111 (26.9) | 132 (28.6) | 0.43 | 54 (35.8) | 0.02 | 198 (22.4) | 0.006 |
SI conversion factors: To convert cholesterol to mmol/L, multiply values by 0.0259. Data shown are median (interquartile range) or n (%). ASCVD indicates atherosclerotic cardiovascular disease; LDL‐C, low‐density lipoprotein cholesterol; MI, myocardial infarction; PALM, Patient and Provider Assessment of Lipid Management.
Patients Never Offered Statin Therapy
Compared with current statin users, PALM participants who were eligible for statin therapy but reported never being offered a statin by their provider were more likely to be female (51.1% vs 39.4%, P<0.001), of black race (20.9% versus 12.1%), and of Hispanic ethnicity (14.0% versus 10.1%, P=0.0005) and less likely to have prior ASCVD (29.8% versus 62.6%, P<0.001) and to see a cardiologist (28.4% versus 50.3%, P<0.001), and had lower rates of private insurance, college education, and lower household incomes (Table 1).
In multivariable analyses, black race compared with white race (relative risk: 1.48; 95% CI, 1.20–1.80; P=0.001), having “other” or no insurance compared with private insurance (relative risk: 1.38; 95% CI, 1.06–1.81; P=0.02), and female sex (relative risk: 1.22; 95% CI, 1.06–1.41; P=0.006) were all associated with increased likelihood of never being offered statin therapy (Table S1).
Reasons for Lack of Statin Utilization
Reasons for lack of statin utilization varied by indication. Among adults recommended for primary prevention but not on a statin (n=945), lack of statin utilization was largely due to participants reporting never being offered a statin (n=628, 66.5% of those not on a statin for primary prevention) rather than participants reporting discontinuing (n=222, 23.5%) or declining (n=95, 10.1%). In contrast, among those recommended for statins for secondary prevention not on therapy (n=566), similar numbers of adults reported discontinuing treatment (n=242, 42.8% of those not on a statin for secondary prevention) and never being offered therapy (n=266, 47.0%), whereas 58 (10.2%) reported being offered but declining therapy.
Among the 153 patients who declined statin therapy, fear of side effects was the most commonly cited reason (36.8% overall, 36.7% primary prevention, and 37.0% secondary prevention), followed by a preference to focus on diet or exercise (25.0%) and belief that statins were not necessary (19.4%; Figure 2). The primary prevention groups reported declining statin therapy more often than the secondary prevention cohort because of wanting to try diet and exercise (32.2% versus 13.0%, P=0.01), a dislike for taking medication (22.2% versus 7.4%, P=0.02), and preferring natural remedies (22.2% versus 5.6%, P=0.008).
Figure 2.
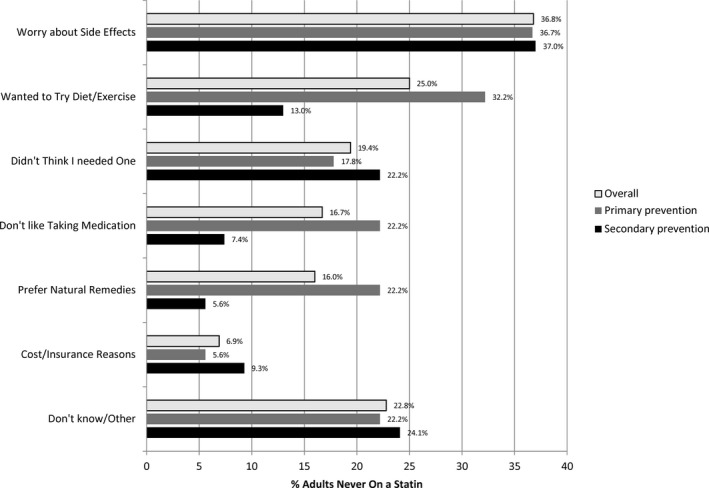
Patient‐reported reasons for declining statin therapy.
Among the 464 former statin users who reported discontinuing statin therapy, more than half (51.3%) were on a statin for ≥1 year, 29.4% between 1 month and 1 year, and 12.6% for <1 month. The most common reason patients reported for stopping statin therapy was perceived side effects (55.0%; Figure 3). Only 18.2% of adults who discontinued a statin felt they no longer needed one, with primary prevention patients more likely than secondary prevention patients to state that the statin was no longer needed (23.4% versus 13.5%, P=0.007).
Figure 3.
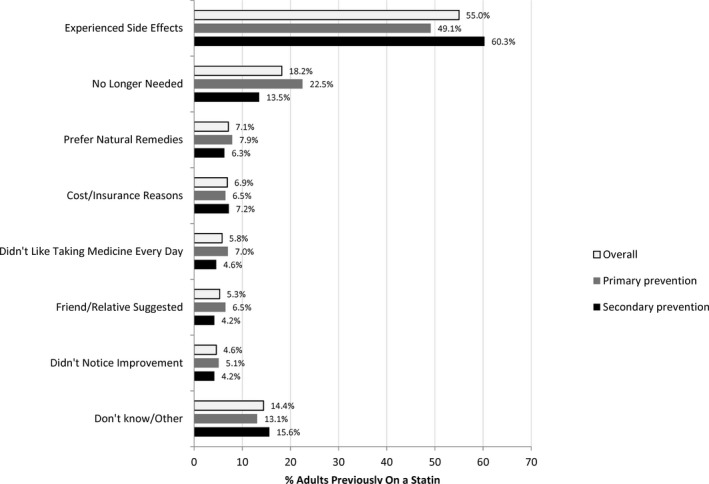
Patient‐reported reasons for statin discontinuation.
Patient Beliefs
Table 2 shows patient‐reported concerns about heart disease and beliefs in statin safety and risks. Compared with current statin users, those who discontinued statin therapy were more likely to report worrying about heart attack or stroke (50.7% versus 38.9%, P<0.0001) and less likely to agree that high cholesterol increases the risk of heart attack or stroke (78.8% versus 85.8%, P=0.0002). In contrast, there was no difference between worry about heart disease or believing that high cholesterol increases the risk for heart attack or stroke between those who declined a statin and current statin users.
Table 2.
Patient Beliefs About Statin Use and Safety by Statin Use Status
| Patient beliefs | Current Statin Therapy | Discontinued Statin Therapy | P Value vs Current | Declined Statin Therapy | P Value vs Current | Never Offered Statin Therapy | P Value vs Current |
|---|---|---|---|---|---|---|---|
| Cardiovascular risk | |||||||
| I worry that I may have a heart attack or stroke. | |||||||
| Occasionally or often | 1515 (38.9) | 221 (50.7) | <0.0001 | 53 (35.1) | 0.35 | 278 (35.5) | 0.08 |
| My risk of heart attack or stroke compared with others of my age/sex. | |||||||
| Slightly higher or much worse | 1520 (37.0) | 172 (37.7) | 0.77 | 49 (32.5) | 0.25 | 201 (24.3) | <0.0001 |
| People with high cholesterol are more likely to have heart attack or stroke. | |||||||
| Agree/strongly agree | 3147 (85.8) | 320 (78.8) | 0.0002 | 109 (82.0) | 0.22 | 607 (83.8) | 0.18 |
| Statin beliefs | |||||||
| Statins are effective. | |||||||
| Agree/strongly agree | 2957 (86.3) | 233 (69.1) | <0.0001 | 66 (67.4) | <0.0001 | 379 (74.9) | <0.0001 |
| Statins are safe. | |||||||
| Agree/strongly agree | 2221 (70.4) | 123 (37.4) | <0.0001 | 38 (36.9) | <0.0001 | 237 (53.4) | <0.0001 |
| Statin risks | |||||||
| Statins can cause diabetes mellitus. | |||||||
| Agree/strongly agree | 261 (13.0) | 39 (17.6) | 0.060 | 16 (24.6) | 0.007 | 43 (15.6) | 0.24 |
| Statins can cause muscle aches or pain. | |||||||
| Agree/strongly agree | 1638 (61.1) | 263 (76.0) | <0.0001 | 58 (64.4) | 0.52 | 162 (50.6) | 0.0003 |
| Statins can cause liver damage. | |||||||
| Agree/strongly agree | 1220 (54.7) | 162 (61.1) | 0.047 | 44 (56.4) | 0.77 | 145 (47.4) | 0.016 |
| Statins can cause memory loss. | |||||||
| Agree/strongly agree | 536 (27.1) | 65 (29.4) | 0.46 | 20 (29.4) | 0.67 | 45 (17.7) | 0.001 |
Missing data were more common for never statin users for all belief questions regarding statins (Table S2). Data are shown as n (%).
Compared with current statin users, those who discontinued or declined statins were less likely to report believing that statins are effective or safe: 70.4% of current statin users agreed with the statement that “statins are safe,” compared with only 37.4% of those who discontinued statins (P<0.0001) and 36.9% of those who declined therapy (P<0.0001). When queried about specific symptoms, differences in the beliefs in risk were attenuated. Those who discontinued statins were more likely than current users to believe that statins can cause liver damage (61.1% versus 54.7%, P<0.05) or muscle aches (76.0% versus 61.1%, P<0.0001) but not diabetes mellitus (17.6% discontinued versus 13.0% current, P=0.06). More than 1 in 4 former and current statin users reported believing that statins cause memory loss (29.4% versus 27.1%, respectively, P=0.46). Participants who declined statins were most likely to report that statins cause diabetes mellitus (24.6%, P=0.007 compared with current users) but otherwise had beliefs similar to those of current statin users.
There was a greater percentage of missing data for the questions regarding patient beliefs about statin therapy than on other parts of the survey. Participants who were never offered statin therapy were most likely to have missing data regarding their beliefs about the medication (Table S2).
Willingness to Take Statin Therapy
Among those who discontinued statin therapy, willingness to retry a statin was high. When asked if they would be willing to retry a statin if recommended by their doctor, 11.2% did not answer or did not know, and only 29.1% were unwilling to retry a statin (Figure S1). In contrast, 21.3% of those who had discontinued a statin were “possibly” willing and 38.4% were “very likely” or “almost certainly” willing to retry a statin.
Willingness to take a statin was also high among those who were never offered a statin. When asked if they were willing to try a statin if recommended by their doctor, 41.9% were “very likely” or “almost certainly” willing to take a statin, 25.8% were “possibly” willing to take a statin, and only 16.7% reported they were unwilling to take a statin (Figure S1).
Discussion
A large gap remains in use of statins between those patients recommended by national guidelines for statin therapy and those actually receiving one. In the PALM registry, a cross‐sectional evaluation of contemporary lipid management in clinical practice, 27% of adults recommended for statin therapy were not on a statin. The majority of patients (59.2%) who were not on a statin reported they did not recall ever being offered one by their doctor, which was the leading cause of patients not being on therapy, followed by patient discontinuation of treatment (30.7%) and patients declining therapy (10.1%). Among those who declined or discontinued therapy, fear of side effects and perceived side effects were the leading reported factors for lack of treatment. Worry about ASCVD risk was greater among those who discontinued statins, whereas current users were most likely to believe statins are safe or effective.
Among those recommended to take a statin but not currently on one, a majority reported never being offered a statin by their provider. In multivariable modeling, black adults, women, and those without insurance were least likely to report ever being offered a statin, raising concern about how differences in who is offered a statin may be contributing to disparities in care. Although it is impossible to know whether these patients were, in fact, never offered statin therapy or if they were but did not recall the conversation, these patients are likely to be open to a new conversation about statin therapy with their physician. Importantly, even among those who discontinued or who recalled having declined a statin, willingness to reconsider therapy was high. Thus, it appears that there is a large population of patients who are eligible for therapy but who have never been offered a statin or who do not recall being offered a statin but are willing to consider therapy.
Previous work evaluating statin utilization has examined clinical and demographic factors, such as age, sex, race, and comorbidities, but has not focused on how statin utilization may be affected by patient beliefs regarding statin therapy or concern about heart disease.13, 14, 15 In this study, among those who were offered therapy but declined, fear of side effects was by far the most commonly cited reason for not initiating therapy. Although the 2013 ACC/AHA guideline emphasizes the importance of a clinician–patient risk/benefit discussion, little guidance is provided on the best way to discuss real and perceived statin‐related side effects. Although statins are associated with certain risks, negative news stories about statins are common and have been associated with increased rates of statin discontinuation.16 Although we were unable to determine the degree to which patients’ decisions to decline statin therapy were related to factual versus incorrect beliefs about statin safety, misperceptions about statins are common; >1 in 4 adults in PALM believed that statins can cause memory loss, including 27.1% of those currently on statins. Efforts to improve statin uptake should include resources for clinicians to accurately describe the risks of statin therapy while combating misperceptions and addressing patient fears about medication.
Poor medication persistence with statin therapy has been previously documented, ranging from 40% to 70% at 1 year17, 18 and up to 50% of adults discontinuing statin therapy by 5 years.19 In the PALM registry, statin discontinuation accounted for about a third of lack of statin use overall, and nearly half of adults not on statin therapy for secondary prevention had previously tried but discontinued a statin, most often due to patient‐perceived side effects. Overall rates of perceived statin intolerance in the PALM registry were much higher than the rate expected from clinical trials, suggesting that many patients are falsely attributing other symptoms to their statin.20 This is consistent with other studies showing high rates of perceived side effects from statins.21, 22, 23, 24
Adults who discontinued their statins were more likely to worry about heart disease than those on statins. Those who discontinued or declined statins were less likely to believe that statins were effective or that high cholesterol caused heart attack and stroke and substantially less likely to believe statins are safe than those on therapy. Consequently, it appears that fear of statins, not a lack of fear of ASCVD, appears to be driving underutilization in adults who have discontinued or declined statin therapy. Focusing clinician–patient risk/benefit conversations on addressing concerns about statin side effects may be more effective than focusing on ASCVD risk alone.
Fortunately, in both former and “never” statin users, willingness to try or retry a statin was high, with more than half of former statin users reporting some degree of willingness to retry a statin. Many patients can be successfully rechallenged with a statin after experiencing perceived side effects. For example, in the GAUSS‐3 (Goal Achievement After Utilizing an Anti‐PCSK9 Antibody in Statin Intolerant Subjects 3) trial, 43.8% of patients who were statin intolerant were successfully rechallenged with atorvastatin 20 mg.25 Providers should maintain an ongoing dialogue with their patients about their willingness to retry a statin and discuss barriers to reinitiation.
Our study had several limitations. First, the PALM registry enrolled patients who were potentially eligible for statin therapy, including those already on statin therapy. This may have overestimated statin use in the study population. Second, patients self‐reported prior statin use and whether they had been offered a statin in the past. Self‐reported end points are subject to recall bias and may have led to underestimating the rate of discontinuing a statin, declining therapy, and being offered a statin. Third, although the overall survey response rate in PALM was high, participants were able to skip questions, and many never statin users chose to not answer questions regarding statin beliefs. This may represent an opportunity for education, as these patients appear to have few preconceived notions about statin therapy. Fourth, the subsample of patients who agreed to participate in PALM may not be representative of the nation. For example, adults who were more skeptical of medications or the healthcare system or who had less trust in their providers may have been less likely to enroll in PALM. Finally, our data come from a group of practices enrolling in the PALM registry and from enrolled patients at the time of a visit with a healthcare provider. Therefore, this sample represents patients who are actively seen in the healthcare system and cannot be used to explain reasons for underutilization in those without access to health care.
Conclusion
Significant opportunity for improvement in statin utilization remains among adults eligible for but not on statin therapy in the United States. The most commonly reported reason that patients recommended for statins were not on a statin was because they had never been offered one. Willingness to initiate or reinitiate statin therapy was high in both former and never statin users. Perceptions about statin safety, rather than perceptions about ASCVD risk or statin benefit, appear to be driving statin underutilization among those who decline or discontinue therapy.
Sources of Funding
The Patient and Provider Assessment of Lipid Management (PALM) registry received funding from Sanofi and Regeneron Pharmaceuticals. Dr Navar is supported by National Institutes of Health, National Heart, Lung, and Blood Institute grant K01HL133416. Sanofi and Regeneron Pharmaceuticals had no role in data collection or data analysis for this study. Apart from the employees listed as authors, the funder had no role in study design; data interpretation; preparation, review, or approval of the article; and decision to submit the article for publication. All analyses were done independently by the Duke Clinical Research Institute.
Disclosures
Dr Wang reports research grants (modest) from Pfizer, Bristol Myers Squibb; research grants (significant) from AstraZeneca, Boston Scientific, Daiichi Sankyo, Eli Lilly, Gilead Sciences, Regeneron Pharmaceuticals; honoraria (modest) from Merck, Gilead; honoraria (significant) from Sanofi. Dr Robinson reports research grants (significant) from Amarin, Amgen, Astra‐Zeneca, Eli Lilly, Esai, Glaxo‐Smith Kline, Merck, Pfizer, Regeneron/Sanofi, Takeda; consultant/advisory board (modest) for Amgen, Eli Lilly, Merck, Pfizer, Regeneron; consultant/advisory board (significant) for Sanofi, Dr Reddy Laboratories. Dr Goldberg reports research grants (modest) from Amarin, Amgen, Pfizer, Regeneron; research grants (significant) from Regeneron/Sanofi, IONIS; honoraria (modest) from Merck Manual; consultant/advisory board (modest) from Regeneron/Sanofi, Esperion, Akcea, and Novartis. Dr Virani reports research grants (significant) from the American Heart Association, the American Diabetes Association, and the US Department of Veterans Affairs; honoraria (significant) from American College of Cardiology, National Lipid Association; other (significant) steering committee for the Patient and Provider Assessment of Lipid Management (PALM) registry at Duke University (no financial remuneration). Dr Louie reports employment with Regeneron Pharmaceuticals, Inc.; ownership interest in Regeneron Pharmaceuticals, Inc. Ms Lee reports employment (significant) from Sanofi. Dr Peterson reports research grants (significant) from Amgen, Sanofi, Astrazeneca, Merck; consultant/advisory board (modest) from Amgen; consultant/advisory board (significant) from AstraZeneca, Merck, and Sanofi Aventis. Dr Navar reports research grants (significant) from Amgen, Sanofi, Amarin, Janssen, and Regeneron; consultant/advisory board (modest) for Amgen, Regeneron, NovoNordisk, AstraZeneca, and Sanofi. The remaining authors have no disclosures to report.
Supporting information
Data S1. Patient and Provider Assessment of Lipid Management (PALM) registry survey questions.
Table S1. Risk Factors Associated With Never Being Offered Statin Therapy
Table S2. Percentage of Missing Responses on Patient Belief Questionnaire by Statin Use Status
Figure S1. Patient‐reported willingness to retry or start statin therapy.
Acknowledgments
Peter Hoffmann of the Duke Clinical Research Institute provided editorial assistance.
(J Am Heart Assoc. 2019;8:e011765 DOI: 10.1161/JAHA.118.011765.)
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R; Cholesterol Treatment Trialists’ (CTT) Collaborators . Efficacy and safety of cholesterol‐lowering treatment: prospective meta‐analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. [DOI] [PubMed] [Google Scholar]
- 3. Pencina MJ, Navar‐Boggan AM, D'Agostino RB Sr, Williams K, Neely B, Sniderman AD, Peterson ED. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014;370:1422–1431. [DOI] [PubMed] [Google Scholar]
- 4. Maddox TM, Borden WB, Tang E, Virani SS, Oetgen WJ, Mullen JB, Chan PS, Casale PN, Douglas PS, Masoudi FA, Farmer SA, Rumsfeld J. Implications of the 2013 ACC/AHA cholesterol guidelines for adults in contemporary cardiovascular practice: insights from the NCDR PINNACLE registry. J Am Coll Cardiol. 2014;64:2183–2192. [DOI] [PubMed] [Google Scholar]
- 5. Pokharel Y, Tang F, Jones PG, Nambi V, Bittner VA, Hira RS, Nasir K, Chan PS, Maddox TM, Oetgen WJ, Heidenreich PA, Borden WB, Spertus JA, Petersen LA, Ballantyne CM, Virani SS. Adoption of the 2013 American College of Cardiology/American Heart Association Cholesterol Management Guideline in Cardiology Practices Nationwide. JAMA Cardiol. 2017;2:361–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pokharel Y, Gosch K, Nambi V, Chan PS, Kosiborod M, Oetgen WJ, Spertus JA, Ballantyne CM, Petersen LA, Virani SS. Practice‐level variation in statin use among patients with diabetes: insights from the PINNACLE registry. J Am Coll Cardiol. 2016;68:1368–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Navar AM, Wang TY, Li S, Robinson JG, Goldberg AC, Virani S, Roger VL, Wilson PWF, Elassal J, Lee LV, Peterson ED. Lipid management in contemporary community practice: results from the Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2017;193:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hirsh BJ, Smilowitz NR, Rosenson RS, Fuster V, Sperling LS. Utilization of and adherence to guideline‐recommended lipid‐lowering therapy after acute coronary syndrome: opportunities for improvement. J Am Coll Cardiol. 2015;66:184–192. [DOI] [PubMed] [Google Scholar]
- 9. Navar AM, Wang TY, Goldberg AC, Robinson JG, Roger VL, Wilson PF, Virani SS, Elassal J, Lee LV, Webb LE, Peterson E. Design and rationale for the patient and Provider Assessment of Lipid Management (PALM) Registry. Am Heart J. 2015;170:865–871. [DOI] [PubMed] [Google Scholar]
- 10. Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–S4. [DOI] [PubMed] [Google Scholar]
- 11. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 12. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 13. Mann DM, Woodard M, Muntner P, Falzon L, Kronish I. Predictors of non‐adherence to statins: a systemic review and meta‐analysis. Ann Pharmacother. 2010;44:1410–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mann DM, Allegrante JP, Natarajan S, Halm EA, Charlson M. Predictors of adherence to statins for primary prevention. Cardiovasc Drugs Ther. 2007;21:311–316. [DOI] [PubMed] [Google Scholar]
- 15. Ellis JJ, Erickson SR, Stevenson JG, Bernstein SJ, Stiles RA, Fendrick AM. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19:638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matthews A, Herrett E, Gasparrini A, Van Staa T, Goldacre B, Smeeth L, Bhaskaran K. Impact of statin related media coverage on use of statins: interrupted time series analysis with UK primary care data. BMJ. 2016;353:i3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Simons LA, Levis G, Simons J. Apparent discontinuation rates in patients prescribed lipid‐lowering drugs. Med J Aust. 1996;164:208–211. [DOI] [PubMed] [Google Scholar]
- 18. Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462–467. [DOI] [PubMed] [Google Scholar]
- 19. Avorn J, Monette J, Lacour A, Bohn RL, Monane M, Mogun H, LeLorier J. Persistence of use of lipid‐lowering medications: a cross‐national study. JAMA. 1998;279:1458–1462. [DOI] [PubMed] [Google Scholar]
- 20. Navar AM, Peterson ED, Li S, Robinson JG, Roger VL, Goldberg AC, Virani S, Wilson PWF, Nanna MG, Lee LV, Elassal J, Wang TY. Prevalence and management of symptoms associated with statin therapy in community practice: insights from the PALM (Patient and Provider Assessment of Lipid Management) registry. Circ Cardiovasc Qual Outcomes. 2018;11:e004249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kashani A, Phillips CO, Foody JM, Wang Y, Mangalmurti S, Ko DT, Krumholz HM. Risks associated with statin therapy. Circulation. 2006;114:2788–2797. [DOI] [PubMed] [Google Scholar]
- 22. Buettner C, Davis RB, Leveille SG, Mittleman MA, Mukamal KJ. Prevalence of musculoskeletal pain and statin use. J Gen Intern Med. 2008;23:1182–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wei MY, Ito MK, Cohen JD, Brinton EA, Jacobson TA. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7:472–483. [DOI] [PubMed] [Google Scholar]
- 24. Fernandez GE, Spatz ES, Jablecki CH, Phillips PS. Statin myopathy: a common dilemma not reflected in clinical trials. Cleve Clin J Med. 2011;78:393–403. [DOI] [PubMed] [Google Scholar]
- 25. Nissen SE, Stroes E, Dent‐Acosta SJ, Rosenson RS, Lehman SJ, Sattar N, Preiss D, Bruckert E, Ceška R, Lepor N, Ballantyne CM, Gouni‐Berthold I, Elliott M, Brennan DM, Wasserman SM, Somaratne R, Scott R, Stein EA; GAUSS‐3 Investigators . Efficacy and tolerability of evolocumab vs ezetimibe in patients with muscle‐related statin intolerance: the GAUSS‐3 randomized clinical trial. JAMA. 2016;315:1580–1590. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Patient and Provider Assessment of Lipid Management (PALM) registry survey questions.
Table S1. Risk Factors Associated With Never Being Offered Statin Therapy
Table S2. Percentage of Missing Responses on Patient Belief Questionnaire by Statin Use Status
Figure S1. Patient‐reported willingness to retry or start statin therapy.


