Abstract
Background:
Laminitis is a common but critical disease that causes severe pain and disability in horses. The etiology and pathogenesis of laminitis remain inconclusive and a multimodal therapeutic approach is generally indicated. Acupuncture has been used as a treatment option; however, the required number of treatments is still controversial due to the lack of objective scientific evidence.
Aims:
The objective of this study was to determine if the response to a second acupuncture treatment differed from the response to the first
acupuncture treatment in horses with chronic laminitis.
Methods:
Fourteen horses with chronic laminitis were identified. Acupuncture points were determined based on the results of a diagnostic acupuncture palpation examination. The second acupuncture treatment and lameness examination were conducted one week after the first treatment. Ten minutes after each acupuncture treatment, a lameness examination was performed and included an objective examination using a body-mounted inertial sensor system called “Lameness Locator” and a routine lameness examination following the “American Association of Equine Practitioners” (AAEP) lameness scale. The level of lameness was statistically analyzed using paired t-test and Wilcoxon signed rank test with p-values <0.05 considered significant.
Results:
Both objective (P=0.042) and routine lameness examinations (P=0.027) showed that the level of lameness significantly decreased after the second acupuncture treatment compared to the response to the first treatment.
Conclusion:
The results of this study suggest that continued acupuncture treatments will result in increasing levels of pain relief, showing the advantage of performing more than one acupuncture treatment in horses with chronic laminitis.
Key Words: Acupuncture, Horse, Laminitis, Objective lameness examination
Introduction
Laminitis is a severely debilitating disease in horses caused by inflammatory and pathologic changes of the laminar junction which provide the link between the hoof wall and distal phalanx through the laminar junction (Mitchell et al., 2015 ▶). Several structures including dermo-epidermal junction, basement membrane, connective tissue of the laminar dermis, and the distal phalanx are associated with the laminar architecture (Faramarzi, 2014 ▶). When the laminar junction is disrupted and damaged, the hoof-distal phalanx bond fails and laminitis occurs (Faramarzi, 2014 ▶). Impaired attachment between the hoof wall and distal phalanx cannot withstand the weight of the horse and ground reaction forces, leading to shearing and damaging the laminae and associated vasculature, sinking and/or rotation of the distal phalanx; crushing the corium of the sole and coronet; and resulting in excruciating pain and lameness (Pollitt, 2004 ▶). The progression of pathological changes can include uncontrollable pain and foot deformation, may be career-ending, and ultimately result in the horse’s demise. Although the etiology and pathogenesis of laminitis has not been completely elucidated, various mechanisms including metabolic, mechanical and nutritional theories have been presented (Heymering, 2010 ▶). Thus, the treatment options are multifaceted and directed at different components of the known pathophysiologic processes for achieving desired outcomes (Mitchell et al., 2015 ▶; Parks and O’Grady, 2015 ▶).
Relief of pain, resolution of lameness, return to function and the overall welfare of the horse are major concerns for owners and veterinarians, and hence should be included in the treatment plan. If current treatment options are limited, associated with significant side-effects, and fail to manage pain and suffering, euthanasia of the animal could be inevitable (Hunt, 1993 ▶; Hood, 2011 ▶; Lancaster and Bowker, 2012 ▶). Acupuncture has been commonly used in veterinary medicine as a complementary and alternative treatment to address chronic pain, inflammation and systemic disorders including laminitis in horses (Kim et al., 2006 ▶; Cantwell, 2010 ▶). However, existing knowledge is often experiential and evidence-based clinical research is scarce (Habacher et al., 2006 ▶; Tangjitjaroen et al., 2009 ▶). While more than one acupuncture treatment is often recommended, the required number of treatments is still controversial due to the lack of objective scientific evidence (Habacher et al., 2006 ▶). The objective of this study was to determine if the response to a second acupuncture treatment differed from the response to the first acupuncture treatment in horses with chronic laminitis.
Materials and Methods
Animals
Fourteen client-owned horses were selected from one geographical area (Southern California; United States). The mean age ± standard deviation was 16.6 ± 5.4 years and included 8 mares and 6 geldings. Each patient had a history of chronic laminitis for a minimum of one month. Laminitis was diagnosed by referring veterinarians, via radiography and clinical signs, prior to any acupuncture treatment being performed. During the experimental period, alterations in trimming/shoeing, medications, supplements or nutrition were not allowed. This study was approved by the Institutional Animal Care and Use Committee (IACUC) and owners’ consent was obtained.
Acupuncture treatments
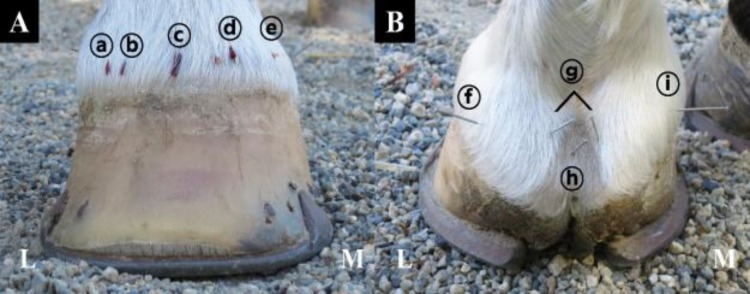
For consistency, specific acupoints were used as a basic treatment formula for all the horses and included: Small Intestine-1 (SI-1), Triple Heater-1 (TH-1), Large Intestine-1 (LI-1), (QIAN-TI-TOU), and QIAN-TI-TOU mirror point for hemo-acupuncture in dorsal region of the front foot and Heart-9 (HT-9), Pericardium-9 (PC-9), Lung-11 (LU-11), and (QIAN-TI-MEN) for dry needling in palmar region of the front foot (Fig. 1). Jing-Well points (HT-9, SI-1, TH-1, LI-1, LU-11, and PC-9) are recommended in Traditional Chinese Veterinary Medicine (TCVM) as local points for foot pain and/or inflammation. The QIAN-TI-MEN, QIAN-TI-TOU and Mirror points are also recommended as local points for any foot pain and/or inflammation. Those points are recommended for the treatment of the laminitis in horses. A diagnostic acupuncture palpation examination was performed before each treatment, and based on the results, additional acupoints were selected for each horse. The treatment plan included hemo-acupuncture, dry needling, and aqua-acupuncture; for consistency, dry needles were left in 20 min. All treatments were performed by a certified veterinary acupuncturist.
Fig. 1.
Basic treatment formula for all horses. (A) Hemo-acupuncture in dorsal region. From lateral (L) to medial (M), ⓐ Small Intestine-1, ⓑ QIAN-TI-TOU, ⓒ Triple Heater-1, ⓓ QIAN-TI-TOU mirror point, and ⓔ Large Intestine-1. (B) Dry needling in palmar region. From lateral (L) to medial (M), ⓕ Heart-9, ⓖ QIAN-TI-MEN, ⓗ Pericardium-9, and ⓘ Lung-11
Lameness examination
Two independent lameness examinations were performed following each acupuncture treatment. Those lameness examinations consisted of an objective lameness evaluation using a wireless body-mounted inertial gyroscope and accelerometer system called the “Lameness Locator” (Equinosis LLC, St. Louis, MO, USA) and a visual lameness examination based on the “American Association of Equine Practitioners” (AAEP) lameness grading scale (Swanson, 1984). For the objective lameness evaluation, three small (approximately 3 × 3 cm) wireless sensors were attached to the horses’ body. These included two single-axis acceleration sensors on the dorsal midline at the most dorsal aspect of the head bumper (poll area between the base of the ears) and at the level of the tuber sacrale (most dorsal aspect of the lumbosacral area), and one single-axis piezoelectric gyroscope sensor on the dorsal aspect of the right front pastern following manufacturer’s recommendation. The lameness score was reported as “Vector Sum” (Keegan et al., 2011 ▶; McCracken et al., 2012 ▶). In addition to objective lameness examination, a visual lameness examination was performed by experienced equine clinicians. All horses were evaluated for lameness 10 min after each acupuncture treatment and again one week after the first acupuncture treatment in a similar fashion.
Statistical analysis
The lameness severity data obtained from objective and visual lameness examinations after the first and second acupuncture treatments were statistically analyzed. Normal distribution of data was examined and consequently paired t-test and Wilcoxon signed rank were used to compare objective and visual lameness examinations, respectively. All statistical analyses were performed using SPSS Statistics for Windows version 18.0 (IBM Corp., Armonk, NY, USA) and p-values <0.05 were considered statistically significant.
Results
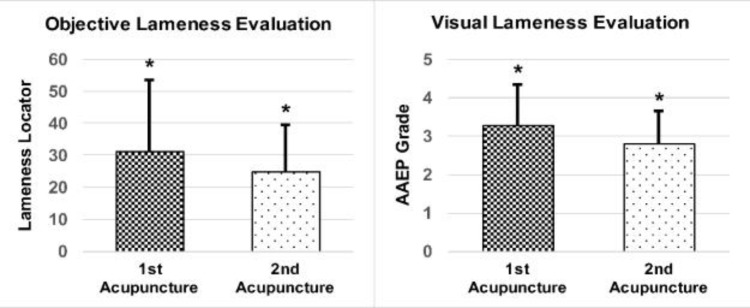
The lameness levels after the first and second acupuncture treatments were evaluated. After the first acupuncture treatment, both objective (Lameness Locator) and visual (following AAEP lameness grading) lameness examinations showed a slight increase of the lameness severity; although, it was not statistically significant. However, objective lameness examination after the second acupuncture treatment, showed 20.41% reduction in lameness severity which was statistically significant (P=0.042). Consistent with the objective examination, the results from the visual lameness examinations showed a significant reduction in lameness severity as well (P=0.027). The changes in lameness severity are shown in Fig. 2.
Fig. 2.
Comparison of the lameness level difference between first and second acupuncture treatment by objective (lameness locator) lameness evaluation (left) and visual (AAEP grading) lameness evaluation (right). P-values <0.05 were considered statistically significant. * P<0.05
Discussion
This study compared the response to acupuncture treatment after two initial acupuncture treatments; the results showed that adding a second acupuncture treatment further decreased the severity of lameness in horses with chronic laminitis. Interestingly, we found that after the first acupuncture treatment, the lameness became slightly worse. It is likely that the horses were not familiar with the temporary pain of acupuncture needles, especially hemo-acupuncture which might have a psychological effect causing nervousness. A previous study reported and described this deteriorating symptom after the acupuncture treatment as “dizziness reaction” or “healing crisis” (Jeong et al., 2009 ▶; Yoon, 2009 ▶). It is suggested that such dizziness reaction is a temporary expression diverging from acupuncture treatment (Yoon, 2009 ▶). We also found that such reaction was temporary, and the lameness of the horses significantly improved after the second acupuncture treatment.
The management of lameness through pain control in horses with chronic laminitis is a key element for determining prognosis and rehabilitation. Available treatments for chronic laminitis are very limited, mainly because of limited existing knowledge of the etiology and pathophysiology of the disease (Laskoski et al., 2016 ▶). Although several treatment options have been suggested to manage laminitis, they are limited by the time and effort needed for application, and by side-effects (Mitchell et al., 2015 ▶). A previous study reported that 19% of laminitic horses referred to veterinary teaching hospitals suffered from permanent lameness, while 48% were eventually euthanized (Hunt, 1993 ▶). While it is recognized that the horses presented to the teaching hospitals were generally more severe cases, the statistics reflect the limitations and poor outcomes of current laminitis treatment options.
Acupuncture is a minimally invasive and drug-free treatment modality; it exerts its therapeutic effects via a wide range of mechanisms to manage inflammation and chronic pain (Fry et al., 2014 ▶; Robinson and Manning, 2015 ▶). The neurophysiological mechanisms of acupuncture analgesia have been documented and include: opiate and non-opiate pain modulation, hippocampal nitric oxide synthase activity, and the expression of various mediators of neurologic inflammation, have been documented (le Jeune et al., 2016 ▶). Local effects of acupuncture, including pain relief, alteration in local circulation, and mediation of inflammation, are associated with the increase of calcitonin gene-related peptide and nitric oxide synthase activity (Tsuchiya et al., 2007 ▶; Fry et al., 2014 ▶). Moreover, earlier studies described that acupuncture inhibits expression and activation of metalloproteinases (MMPs) 2 and 9 that are associated with chronic laminitis (Dong et al., 2009 ▶; Loftus et al., 2009 ▶; Cayir et al., 2014 ▶). Therefore, it is probable that acupuncture treatment improves lameness through modulation of pain and local circulation, as well as preventing the exacerbation and relapse of laminitis.
Acupoints are focal areas of reduced electrical resistance that are attributed to specific anatomic locations; those points are associated with high concentrations of autonomic innervation, vasculature, and lymphatic drainage/vessels within the fascia and muscles (Petermann, 2011 ▶). Many of the acupoints that were used in this study, including HT-9, SI-1, TH-1, LI-1, LU-11, PC-9, and QIAN-TI-MEN, have been used and recommended by previous studies (Hackett et al., 1997 ▶; Thoresen, 2001 ▶; Shmalberg and Xie, 2009 ▶). Another study suggested the use of QIAN-TI-TOU and its mirror point in the treatment of hoof pain (Hackett et al., 1997 ▶). The addition of QIAN-TI-TOU and its mirror point were deemed beneficial as local toe points for the treatment of pain in chronic laminitic patients. For the sake of consistency, specific acupoints were designated as treatment formula and used for all patients.
Together these data support the likelihood that a second acupuncture treatment is beneficial; however, they do not provide insight or support conclusions regarding the frequency or the number of acupuncture treatments that are desirable for horses suffering from chronic laminitis.
Because of the nature and perspective of traditional oriental medicine, which treats each patient as a unique individual, acupuncture has remained a controversial subject (Robinson and Manning, 2015 ▶). Discrepancies exist in previous human studies as well, for example: one reference for addressing chronic pain recommended 10 acupuncture treatment sessions while other reports suggested 6 or 12 sessions (Ezzo et al., 2000 ▶; Irnich et al., 2001 ▶; MacPherson et al., 2015 ▶). These inconsistencies might be related to other factors such as the age, gender, disease status, and body condition of the patients. In addition, according to traditional oriental medicine, other factors, such as the patient’s personality and cumulative effect of acupuncture, may influence the response to acupuncture treatments (Ezzo et al., 2000 ▶). The treatment of chronic laminitis is multifaceted and challenging due to the complexity of laminitis and its pain. The goal of treatment is to manage the pain and prevent recurrence. Based on the results of this study, and the influence of acupuncture on multiple body systems through complex physiologic pathways, acupuncture is a valuable complimentary treatment for horses with chronic laminitis. Traditionally, more than one acupuncture treatment is required for a maximal therapeutic response in chronic conditions including laminitis. These results indicate that more than a single acupuncture treatment should be beneficial. We found further improvement after second acupuncture treatment in horses with chronic laminitis, compared to a single treatment. Nonetheless, further research utilizing randomized controlled trials with larger sample sizes and long-term follow up is warranted to determine the optimal number of acupuncture treatments and the duration of such treatments for the effective treatment of chronic laminitis in horses.
Acknowledgements
This study was supported by the American Holistic Veterinary Medicine Foundation, the National Research Foundation of Korea (NRF), Ministry of Education (2015R1A6A3A03016859), and Western University of Health Sciences, College of Veterinary Medicine.
Conflict of interest
The authors declare no conflicts of interest.
References
- Cantwell, SL Traditional Chinese veterinary medicine: the mechanism and management of acupuncture for chronic pain. Top. Companion Anim. Med. 2010;25:53–58. doi: 10.1053/j.tcam.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Cayir, Y , Ozdemir, G , Celik, M , Aksoy, H , Akturk, Z , Laloglu, E , Akcay, F Acupuncture decreases matrix metalloproteinase-2 activity in patients with migraine. Acupunct. Med. 2014;32:376–380. doi: 10.1136/acupmed-2014-010612. [DOI] [PubMed] [Google Scholar]
- Dong, H , Fan, YH , Zhang, W , Wang, Q , Yang, QZ , Xiong, LZ Repeated electroacupuncture preconditioning attenuates matrix metalloproteinase-9 expression and activity after focal cerebral ischemia in rats. Neurol. Res. 2009;31:853–858. doi: 10.1179/174313209X393960. [DOI] [PubMed] [Google Scholar]
- Ezzo, J , Berman, B , Hadhazy, VA , Jadad, AR , Lao, L , Singh, BB Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain. 2000;86:217–225. doi: 10.1016/S0304-3959(99)00304-8. [DOI] [PubMed] [Google Scholar]
- Faramarzi, B Morphological and biomechanical properties of equine laminar junction. J. Equine Vet. Sci. 2014;34:589–592. [Google Scholar]
- Fry, LM , Neary, SM , Sharrock, J , Rychel, JK Acupuncture for analgesia in veterinary medicine. Top. Companion Anim. Med. 2014;29:35–42. doi: 10.1053/j.tcam.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Habacher, G , Pittler, MH , Ernst, E Effectiveness of acupuncture in veterinary medicine: systematic review. J. Vet. Intern. Med. 2006;20:480–488. doi: 10.1892/0891-6640(2006)20[480:eoaivm]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Hackett, GE , Spitzfaden, DM , May, KJ , Savoldi, M , Dodd, M Acupuncture: is it effective for alleviation pain in the horse? Proc. Am. Assoc. Equine Pract. 1997;43:333–335. [Google Scholar]
- Heymering, HW 80 causes, predispositions, and pathways of laminitis. Vet. Clin. N. Am. Equine. 2010;26:13–19. doi: 10.1016/j.cveq.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Hood, DM Practical-laminitis: treatment by design. J. Equine Vet. Sci. 2011;31:592–594. [Google Scholar]
- Hunt, RJ A retrospective evaluation of laminitis in horses. Equine Vet. J. 1993;25:61–64. doi: 10.1111/j.2042-3306.1993.tb02903.x. [DOI] [PubMed] [Google Scholar]
- Irnich, D , Cummings, M , Behrens, N , Molzen, H , König, A , Gleditsch, J , Krauss, M , Natalis, M , Senn, E , Beyer, A Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ. 2001;322:1–6. doi: 10.1136/bmj.322.7302.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong, YJ , Lee, JH , Lee, SK , Kim, DR , Koh, BH A Sasang constitutional study on the Myunghyun symptom. J. Sasang Constitutional Med. 2009;21:20–27. [Google Scholar]
- Keegan, KG , Kramer, J , Yonezawa, Y , Maki, H , Pai, PF , Dent, EV , Kellerman, TE , Wilson, DA , Reed, SK Assessment of repeatability of a wireless, inertial sensor-based lameness evaluation system for horses. Am. J. Vet. Res. 2011;72:1156–1163. doi: 10.2460/ajvr.72.9.1156. [DOI] [PubMed] [Google Scholar]
- Kim, DH , Liu, J , Choi, SH , Macmanus, P , Jennings, P , Darcy, K , Burke, F , Leorald, N , Rogers, PA Acupuncture treatment in a case with equine laminitis. J. Vet. Clin. 2006;23:6–8. [Google Scholar]
- Lancaster, LS , Bowker, RM Acupuncture points of the horse’s distal thoracic limb: a neuroanatomic approach to the transposition of traditional points. Animals. 2012;2:455–471. doi: 10.3390/ani2030455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laskoski, LM , Valadão, CAA , Dittrich, RL , Deconto, I , Faleiros, RR An update on equine laminitis. Ciência Rural. 2016;46:547–553. [Google Scholar]
- Le Jeune, S , Henneman, K , May, K Acupuncture and equine rehabilitation. Vet. Clin. N. Am. Equine. 2016;32:73–85. doi: 10.1016/j.cveq.2015.12.004. [DOI] [PubMed] [Google Scholar]
- Loftus, JP , Johnson, PJ , Belknap, JK , Pettigrew, A , Black, SJ Leukocyte-derived and endogenous matrix metalloproteinases in the lamellae of horses with naturally acquired and experimentally induced laminitis. Vet. Immunol. Immunopathol. 2009;129:221–230. doi: 10.1016/j.vetimm.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Macpherson, H , Tilbrook, H , Richmond, S , Woodman, J , Ballard, K , Atkin, K , Bland, M , Eldred, J , Essex, H , Hewitt, C Alexander technique lessons or acupuncture sessions for persons with chronic neck pain: a randomized trial. Ann. Intern. Med. 2015;163:653–662. doi: 10.7326/M15-0667. [DOI] [PubMed] [Google Scholar]
- Mccracken, MJ , Kramer, J , Keegan, KG , Lopes, M , Wilson, DA , Reed, SK , Lacarrubba, A , Rasch, M Comparison of an inertial sensor system of lameness quantification with subjective lameness evaluation. Equine Vet. J. 2012;44:652–656. doi: 10.1111/j.2042-3306.2012.00571.x. [DOI] [PubMed] [Google Scholar]
- Mitchell, CF , Fugler, LA , Eades, SC The management of equine acute laminitis. Vet. Med. Res. Rep. 2015;6:39–47. doi: 10.2147/VMRR.S39967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks, AH , O’grady, SE . Chronic laminits. In: Sprayberry, KA , Robinson, NE , editors. Robinson’s current therapy in equine medicine. 7th Edn. Elsevier: St. Louis, Missouri; pp. 869–878. [Google Scholar]
- Petermann, U Comparison of pre-and post-treatment pain scores of twenty one horses with laminitis treated with acupoint and topical low level impulse laser therapy. Am. J. Tradit. Chinese Vet. Med. 2011;6:13–25. [Google Scholar]
- Pollitt, CC Equine laminitis. Clin. Tech. Equine P. 2004;3:34–44. [Google Scholar]
- Robinson, KA , Manning, ST Efficacy of a single-formula acupuncture treatment for horses with palmar heel pain. Can. Vet. J. 2015;56:1257–1260. [PMC free article] [PubMed] [Google Scholar]
- Shmalberg, J , Xie, H The clinical application of equine acupuncture. J. Equine Vet. Sci. 2009;29:645–652. [Google Scholar]
- Swanson, TD . Guide for veterinary service and judging of equestrian events. 3rd Edn. Golden, Colorado: American Association of Equine Practitioners; 1984. p. 24. [Google Scholar]
- Tangjitjaroen, W , Shmalberg, J , Colahan, PT , Xie, H Equine acupuncture research: an update. J. Equine Vet. Sci. 2009;29:698–709. [Google Scholar]
- Thoresen, AS . Equine ting-point therapy and Thoresen’s coronary band therapy. In: Schoen, AM , editor. Veterinary acupuncture. 2nd Edn. St. Louis: Mosby; 2001. pp. 489–501. [Google Scholar]
- Tsuchiya, M , Sato, EF , Inoue, M , Asada, A Acupuncture enhances generation of nitric oxide and increases local circulation. Anesth. Analg. 2007;104:301–307. doi: 10.1213/01.ane.0000230622.16367.fb. [DOI] [PubMed] [Google Scholar]
- Yoon, CH A study of reports about dizziness reaction - focus on the China academic journal. J. Korean Oriental Med. 2009;30:1–15. [Google Scholar]