Abstract
Background:
Breast cancer stands out among the most widely recognized forms of cancer among women. It has been observed that upper extremity lymphedema is one of the most risky and prevalent complication following breast cancer surgery that prompts functional impairment, psychological, and social problems.
Purpose:
To compare the effects of Kinesio taping and the application of the pressure garment on secondary lymphedema of the upper extremity.
Methods:
66 women were randomly allocated to the Kinesio taping (KT) group (n=33) and pressure garment (PG) group (n=33). The KT group received Kinesio taping application (2 times per week for 3 weeks), while the PG group received pressure garment (20- 60 mmHg) for at least 15-18 hours per day for 3 weeks. The outcome measures were limb circumference, Shoulder Pain and Disability Index questionnaire (SPADI), hand grip strength, and quality of life at the baseline and end of intervention.
Results:
The sum of limb circumferences, SPADI, hand grip strength, and quality of life significantly improved after treatment in the KT group (P<0.05). While the PG group showed no significant improvement in SPADI, hand grip strength, physical, role, pain, and fatigue score p>0.05, while the sum of limb circumferences significantly decreased (P<0.05). Significant differences were observed between the KT and PG groups at the end of the intervention (P<0.05).
Conclusion:
KT had significant changes in limb circumference, SPADI, hand grip strength and overall quality of life than PG in the treatment of subjects diagnosed with lymphedema after mastectomy.
Keywords: Kinesio taping, pressure garment, lymphedema, Mastectomy, Quality of life
Introduction
Breast cancer remains the most common form of cancer worldwide, and the number is increasing. Advances in breast cancer treatments may decrease breast cancer–related death rates, still sometimes it may lead to postsurgical lymphedema.1,2 Lymphedema is the collection of protein-rich fluid that causes constant swelling of the influenced body part and obstructs the stream of fluid.3 The most widely recognized reasons for lymphedema are radiotherapy and dissection of the lymph nodes in patients with breast cancer. Furthermore, the risk factors of lymphedema include broad axillary disease, obesity, and positive axillary lymph nodes.4-6
The incidence of upper extremity lymphedema is 17%, and the incidence is increased up to 2 years from diagnosis or surgery. Incidence in patients with dissection of axillary lymph node is 4 times more than that of sentinel lymph node biopsy.7 Women with cancer-related lymphedema feel heaviness and stiffness in their upper limbs, and dryness leads to infection and skin problems. They feel pain, discomfort, and difficulty in using their arms, affecting the psychological, functional, and physical status of many aspects of their life.8,9
Breast cancer–related lymphedema (BCRL) can be treated conservatively by pressure garments (PGs), manual lymphatic drainage, exercise, and laser therapy. Physiotherapy is important in the treatment of postsurgical breast lymphedema. Early physiotherapy intervention improves significantly the treatment outcomes. Physiotherapy management for at least 1 year significantly prevents the development of secondary lymphedema.10
The development of new techniques to relieve the symptoms of upper limb edema, pain, and sensory abnormalities has resulted in the discovery of new techniques. One important technique being used is Kinesio taping (KT) and was developed by Dr Kenzo Kase in 1973. The concept involves the application of tape that is attached to the skin. The applied tape is thinner and more elastic than the conventional tape by 120% to 140%.11 The material used was 100% acrylic, latex-free, and heat-activated. It is made of 100% cotton to allow quickening of the drying process. This allows the patient the freedom to wear it even when taking a shower without the need for replication and can be worn for approximately 3 to 4 days.12 Generally, the function of taping is essential to provide support during movement and prevent sports-related injuries. It has been used for several years and was initially identified with soft tissue injuries in sports-related activities.13
Kase et al reported that its effects were facilitating myofascial release and reabsorption of lymphatic fluid in the surrounding tissues. It enables the upper layers of the skin to be pulled, allowing space between the dermis and the muscle. Through this action, pressure exerted on the lymphatic vessels and channels is relieved, enhancing lymphatic flow, which cause better lymphatic drainage in the affected area.14 KT also has an effect on the reduction of pain15,16 and tissue swelling, which has been recognized by physical therapists in treating lymphedema. The following physiological effects are produced when KT is properly applied: decreases pain, correcting misalignment of joints, and removing accumulated lymphatic fluid. Other noted effects of KT include sensory stimulation, decrease in adhesions and contractures, skin softening, improvement of pliability, and reduction of scar formation.17
KT was effective in reducing postmastectomy lymphedema related to breast cancer; however, a recent meta-analysis showed that KT is not more efficient than other treatments.18
Previous studies showed that the compression effect of elastic PGs was documented to be efficient in controlling secondary lymphedema following breast cancer.19 In addition, one study showed that plain compression therapy for secondary lymphedema brought significant decrease in lymphedema of the upper limb in 34% of participants after 2 months and 39% of participants after 6 months.19 PG is considered as a part of compression therapy and can be used beneficially alone in the treatment of lymphedema.20
On the other hand, Singh et al reported that there was no difference in lymphedema status on L-Dex scores between pre-exercise and post-exercise or between the compression and non-compression conditions.21
Smile et al concluded that there was a lack of comparison between BCRL treatment techniques, which means that while conclusions and guidelines can be made, further studies are required for more clinically relevant data.22
Lymphedema is one of the fundamental issues arising after breast cancer surgery. It is critical to look for choices to reduce and control it. The effects of KT and PGs remain controversial in the application of postsurgical lymphedema after mastectomy. The aim of this study was to compare the effect of KT and PG primarily on limb circumference, Shoulder Pain and Disability Index (SPADI), handgrip strength, and quality of life in patients with BCRL.
Patients and Methods
The current study was approved by the Research Ethical Committee, Faculty of Physical Therapy, Cairo University (NO P.T. REC/012/001791) and registered in ClinicalTrial.gov with ID number NCT03401086 according to the Declaration of Helsinki principles, and an informed consent form was signed by each patient. A total of 66 women with unilateral BCRL (stages II and III) according to the International Society of Lymphology for at least 6 months and who completed phase I of complex decongestive therapy were invited. In the current study, the compression bandaging was replaced with either PG or KT; therefore, patients were included in the second phase of complex physical therapy, where the goal is to maintain limb volume. Arm circumference more than 2 cm or less than 8 cm in comparison with the other side was included. The exclusion criterion was any active disease leading to swelling, medications, especially diuretics, allergy, infection, pregnancy, heart and kidney diseases, bilateral lymphedema, skin diseases, and cellulitis.
Sample Size
Power analysis was initially done to calculate the sample size. Estimates of mean difference and standard deviation for the limb circumference were collected from a previous study3; the mean difference value and standard deviation were 5.0 and 6.6, respectively (2-tailed test; α = .05; 80% power). The current study required a sample size of 28 patients for each group. Thirty-three patients were recruited in each group to account for dropout rates of 20%.
Randomization
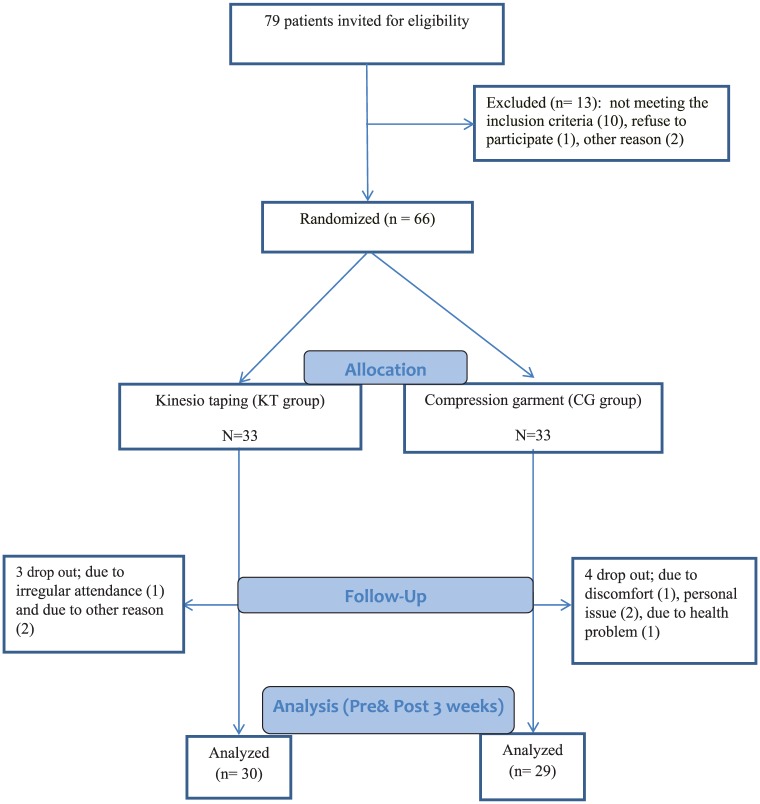
The participants were randomly assigned to 2 groups. The KT group included 33 patients, and the PG group included 33 patients. The subjects were instructed to draw an envelope from a concealed box; each envelope contained a yellow or blue card, and they were accordingly assigned to one of the 2 groups of the study. The person who had the concealed box and had access to it was a third party and not involved in the study. The individuals who drew yellow cards were assigned to the KT group, and those who drew blue cards were allotted to the PG group, as shown in Figure 1.
Figure 1.
Study flow chart.
Assessment
For all patients, we recorded the changes in the limb circumference, SPADI, handgrip strength, and quality of life pre and post 3 weeks of intervention. Measurement of arm circumference is the most commonly used technique for identifying lymphedema23 and is reliable for both surgical and nonsurgical upper limbs.24 It is measured using a tape with the patient in prone lying position, with elbows straight and arms relaxed at the sides. It was measured starting with 3 cm on the ulnar styloid process and proceeding with 45 cm proximal, and additionally at the metacarpal bones and mid-hand. The tape measure was put around the limb to prevent it from slacking and to ensure that there was no space in the tissue. The total circumference of the sound limb was ascertained similarly. The difference between the 2 measurements was identified using “circumference difference.”25,26
where CLAffected denotes the circumference of affected side at each 6 anatomical points; CLNormal denotes the circumference of normal limb at each 6 anatomical points; CD denotes the circumference difference of 2 limbs at each point; CDn denotes the circumference differences at each follow-up session; CD0 denotes the circumference difference at pretreatment session; and TRC denotes the total reduction in circumference.
SPADI was used to assess shoulder pain and disability. It incorporates 13 items assessing 2 domains: 5 items assess pain and 8 items evaluate disability. The reliability of its coefficients is ICC ≥0.8927 and has shown high internal consistency.28
Handgrip strength was evaluated using a dynamometer (78010, Lafayette Instrument Company, Loughboroug, Leics, England). The grip strength was measured with the patient in a standing position with adducted shoulder, elbow flexed at 90°, and forearm in mid position. The patient was instructed to do 3 trials with 15 seconds rest in between each, and the highest reading was reported.
The quality of life was assessed by cancer-specific questionnaire (EORTC QLQ-C30). It is composed of 30 questions, including functional scores (physical, social, emotional, and cognitive aspects). The functional scores ranged between 0 and 100, and higher scores indicated better condition. This questionnaire also included symptoms score (pain, dyspnea, fatigue, insomnia, nausea, loss of appetite, and financial problems). The symptom scores ranged from 100 to 0, and lower scores indicated better condition.29
Patient assessments were done in a different room (not treatment room) by an experienced collaborative blinded physiotherapist who was not part of the study. The participants were instructed not to describe their treatment during evaluation to ensure that blinding was successful.
Intervention
The KT group received Kinesio taping application twice per week, while the PG group received pressure garment (20-60 mm Hg) for at least 15 to 18 hours per day for 3 weeks. Both groups received a home exercise program in the form of a range of motion exercises involving shoulder flexion and extension, abduction, elevation up to 180°, external rotation/horizontal abduction, elbow flexion and extension, wall walking, and cane stretching. The printed exercise program was distributed among the women in both groups after showing them how to do these exercises.
All patients were instructed to perform the exercise program thrice daily with 10 repetitions each time. The patients were addressed about whether they were doing their exercises consistently and not during each visit to ensure that they were following the instructions.30
The KT was applied on cleaned and dried skin by an experienced physiotherapist twice per week for 3 weeks. The KT application consisted of 1 fan shape for the chest (5 straps), 2 fan shapes for the upper arm (4 straps), 2 for forearm (4 straps), and 1 fan shape for wrist (2 straps). The following techniques are according to Tantawy 2019.30
In the chest, the patient was positioned to stand upright, with the affected shoulder being externally rotated. The anchor was placed without tension in the anterior axilla on the sound side extended by 5 straps of a fan tape to the chest toward the affected axilla with 15% to 20% tension.
For the upper arm, the position of the patient was standing upright with extended and externally rotated shoulder; the first fan shape was applied by placing the anchor on the axilla without tension and extended by 5 tails with 15% to 25% tension to the anterior, lateral, and medial aspects of the upper arm. The second fan shape was applied with the patient in an upright standing position with extended shoulder and elbow, the anchor was applied without tension on the lateral end of the clavicle and extended by 5 tails to the posterior aspect of the arm.
For applying KT to the forearm, the patient was standing upright with extended elbow and wrist; the anchor of the first fan was applied on the medial epicondyle of the humerus without tension and ended by 5 tails straps on the anterior, medial, and lateral aspects of the forearm with 15% to 25% tension. From the same position, the second fan started from the lateral epicondyle of the humerus without tension and extended by 5 straps to the posterior aspect of the forearm with 15% to 25% tension.
For the hand, 2 fan shapes with 2 straps each were used. The first anchor was applied from the styloid process of the ulna while the other anchor of the styloid process of the radius without tension, then the wrist was flexed, and the trails were applied on the dorsal surface of the hand with 2 straps to the medial and lateral aspects of the proximal interphalangeal joints, respectively, with 15% to 25% tension.
The PG was applied on cleaned and dried skin. PGs were applied using Premium Lymphedema Gradient Garment (Jobskin, Long Eaton, England), which has a pressure gradient built into the garment by using a gram tension applied on gradient counter pressure to deliver between 20 and 60 mm Hg for at least 15 to 18 hours per day for 3 weeks.
Statistical Analysis
Descriptive statistics were used in the form of mean and standard deviation. The Kolmogorov-Smirnov test was used to assess the normality of the data. Inferential statistics analyzed all measurement changes using unpaired t test between KT and PG groups, and paired t test was used to measure changes within groups; analysis was conducted using SPSS version 20.0 (SPSS, Chicago, IL) with a significance level at P < .05 for all statistical measurements.
Results
Between February and November 2017, 66 women with upper extremity lymphedema secondary to breast cancer treatment participated in this study. Of the 66 patients who participated in this study, 59 completed the program of the study regularly, 30 from the KT group and 29 from the PG group. Three participants who were randomized to the KT group withdrew from the study because of irregular attendance (1) and without specific reason (2). Regarding the PG group, 4 patients dropped out due to discomfort (1), personal issue (2), and health problem (1), and their data were not accounted statistically as demonstrated in Figure 1 (study flow chart).
Before intervention, there were no significant differences between the KT and PG groups in their ages, heights, weights, body mass index, lymphedema duration, sum of limb circumference, SPADI, handgrip strength, and quality of life questionnaire (P > .05), as described in Table 1.
Table 1.
Demographic Data, Clinical Characteristics, and Quality of Life Questionnaire (QLQ-C30) Pre-Intervention in the KT and PG Groupsa.
| Variables | KT Group, Mean ± SD | PG Group, Mean ± SD | P |
|---|---|---|---|
| Demographic data | |||
| Number of patients | 30 | 29 | .85 |
| Age (years) | 54.3 ± 4.16 | 55.15 ± 3.27 | .38 |
| Height (cm) | 167 ± 7.1 | 165 ± 8.3 | .32 |
| Weight (kg) | 79.3 ± 7.4 | 78.5 ± 5.9 | .64 |
| BMI (kg/m2) | 28.4 ± 2.7 | 29.1 ± 2.5 | .30 |
| Clinical characteristics | |||
| Duration after mastectomy (months) | 7.6 ± 1.7 | 6.9 ± 1.4 | .09 |
| Sum of limb circumferences (cm) | 177.5 ± 15.4 | 172.2 ± 17.3 | .21 |
| Shoulder Pain and Disability Index (SPADI) | 75.8 ± 10.52 | 12.81 ± 73.4 | .43 |
| Handgrip strength (kg) | 18.91 ± 4.27 | 5.31 ± 17.42 | .24 |
| Type of surgery (breast and axillary), n (%) | |||
| Breast surgery | 5 (16.7%) | 4 (13.8%) | .80 |
| Breast surgery + axillary surgery | 25 (83.3%) | 25 (86.4%) | .89 |
| Types of treatment, n (%) | |||
| Chemotherapy | 17 (56.7%) | 15 (51.7%) | .88 |
| Chemotherapy + radiotherapy | 13 (43.3%) | 14 (48.3%) | .93 |
| Lymphedema stages, n (%) | |||
| Stage II | 21 (70.0%) | 18 (62.1%) | .26 |
| Stage III | 9 (30.0%) | 11 (37.9%) | .69 |
| Quality of life (QLQ-C30 [EORTC]) | |||
| Functional score | |||
| Physical score | 64.4 ± 17.3 | 62.1 ± 15.8 | .59 |
| Role score | 65.3 ± 21.7 | 64.7 ± 19.6 | .91 |
| Emotional score | 52.6 ± 18.6 | 53.2 ± 15.4 | .89 |
| Cognitive score | 61.5 ± 16.9 | 60.7 ± 17.5 | .85 |
| Social score | 73.7 ± 22.4 | 74.5 ± 25.2 | .89 |
| Symptoms scores | |||
| Pain score | 74.6 ± 27.5 | 71.2 ± 24.7 | .61 |
| Dyspnea score | 79.4 ± 31.4 | 78.6 ± 29.5 | .72 |
| Fatigue score | 72.8 ± 26.7 | 74.5 ± 28.7 | .81 |
| Appetite loss score | 84.7 ± 18.6 | 83.2 ± 21.5 | .77 |
| Nausea/vomiting score | 86.4 ± 16.2 | 84.9 ± 20.8 | .75 |
| Insomnia score | 78.5 ± 28.7 | 76.7 ± 35.4 | .74 |
| Financial problem score | 76.4 ± 26.8 | 74.7 ± 27.4 | .69 |
| Overall quality of life | 42.4 ± 16.7 | 45.7 ± 18.3 | .47 |
Abbreviations: KT, Kinesio taping; PG, pressure garment; EORTC, European Organization for Research and Treatment of Cancer.
Data are presented as mean ± standard deviation; significance at P ≤ .05.
The main findings of this study showed that all measures, including sum of limb circumference, SPADI, handgrip strength, and all domains of quality of life, improved significantly in the KT group at the end of the intervention (with P < .05), as demonstrated in Table 2. While the PG group showed no significant improvement in some measures such as clinical characteristics (handgrip strength), functional scores (physical and role scores), and symptom scores (pain and fatigue scores), with P > .05. The sum of limb circumferences and overall quality of life decreased significantly in the PG group as presented in Table 2.
Table 2.
Statistical Analysis of Mean Differences in the KT and PG Groups Pre- and Post-Interventiona.
| Variables | KT Group (n = 30) |
PG Group (n = 29) |
||||
|---|---|---|---|---|---|---|
| Pre-Intervention | Post-Intervention | P | Pre-Intervention | Post-Intervention | P | |
| Sum of limb circumferences (cm) | 177.5 ± 15.4 | 153.5 ± 9.24 | .01 | 172.2 ± 17.3 | 163.4 ± 14.6 | .04 |
| SPADI | 75.8 ± 10.52 | 48.4 ± 8.7 | .01 | 12.81 ± 73.4 | 67.6 ± 11.4 | .07 |
| Handgrip strength (kg) | 4.27 ± 18.91 | 27.7 ± 5.4 | .02 | 17.42 ± 5.31 | 19.6 ± 5.92 | .13 |
| QLQ-C30 (EORTC) | ||||||
| Functional scores | ||||||
| Physical score | 64.4 ± 17.3 | 73.28 ± 8.5 | .01 | 62.1 ± 15.8 | 67.3 ± 14.6 | .18 |
| Role score | 65.3 ± 21.7 | 77.7 ± 10.6 | .02 | 64.7 ± 19.6 | 70.1 ± 17.2 | .26 |
| Emotional score | 52.6 ± 18.6 | 65.4 ± 12.7 | .02 | 53.2 ± 15.4 | 61.2 ± 12.3 | .03 |
| Cognitive score | 61.5 ± 16.9 | 71.7 ± 12.4 | .01 | 60.7 ± 17.5 | 69.8 ± 13.4 | .02 |
| Social score | 73.7 ± 22.4 | 86.4 ± 17.2 | .01 | 74.5 ± 25.2 | 85.9 ± 17.8 | .04 |
| Symptom scores | ||||||
| Pain score | 74.6 ± 27.5 | 50.4 ± 18.6 | .002 | 71.2 ± 24.7 | 62.7 ± 22.4 | .16 |
| Dyspnea score | 79.4 ± 31.4 | 63.6 ± 22.3 | .03 | 78.6 ± 29.5 | 64.9 ± 22.2 | .04 |
| Fatigue score | 72.8 ± 26.7 | 52.3 ± 17.5 | .01 | 74.5 ± 28.7 | 63.8 ± 24.5 | .12 |
| Appetite loss score | 84.7 ± 18.6 | 69.3 ± 16.2 | .001 | 83.2 ± 21.5 | 72.8 ± 17.8 | .04 |
| Nausea/vomiting score | 86.4 ± 16.2 | 73.6 ± 13.4 | .01 | 84.9 ± 20.8 | 75.3 ± 15.6 | .04 |
| Insomnia score | 78.5 ± 28.7 | 59.3 ± 15.6 | .008 | 76.7 ± 35.4 | 62.1 ± 19.4 | .04 |
| Financial problem score | 76.4 ± 26.8 | 61.5 ± 13.7 | .02 | 74.7 ± 27.4 | 62.8 ± 17.1 | .04 |
| Overall quality of life | 42.4 ± 16.7 | 61.8 ± 12.4 | .001 | 45.7 ± 18.3 | 54.5 ± 15.4 | .04 |
Abbreviations: KT, Kinesio taping; PG, pressure garment; SPADI, Shoulder Pain and Disability Index; QLQ-C30, Quality of Life Questionnaire for Cancer; EORTC, European Organization for Research and Treatment of Cancer.
Data are presented as mean ± standard deviation; significance at P ≤ .05.
Limb circumference and SPADI decreased significantly in the 2 groups (P < .05), while the handgrip strength improved significantly only in the KT group (P < .05) and showed nonsignificant difference in the PG group (P > .05), as demonstrated in Table 2. When comparing the recipients of KT application with those of the PG application, recipients of KT application showed greater decreases in limb circumference and SPADI and significant improvement in handgrip strength as shown in Table 3.
Table 3.
Statistical Analysis of Mean Differences Between the KT and PG Groups Post-Interventiona.
| Variables | KT Group (n = 30) | PG Group (n = 29) | P |
|---|---|---|---|
| Sum of limb circumferences (cm) | 153.5 ± 9.24 | 163.4 ± 14.6 | .01 |
| SPADI | 48.4 ± 8.7 | 67.6 ± 11.4 | .01 |
| Handgrip strength (kg) | 27.7 ± 5.4 | 19.6 ± 5. 92 | .001 |
| QLQ-C30 (EORTC) | |||
| Functional scores | |||
| Physical score | 73.28 ± 8.5 | 67.3 ± 14.6 | .04 |
| Role score | 75.7 ± 10.6 | 70.1 ± 17.2 | .04 |
| Emotional score | 65.4 ± 1 2.7 | 61.2 ± 12.3 | .20 |
| Cognitive score | 71.7 ± 12.4 | 69.8 ± 13.4 | .57 |
| Social score | 86.4 ± 17.2 | 85.9 ± 17.8 | .91 |
| Symptom scores | |||
| Pain score | 50.4 ± 18.6 | 62.7 ± 22.4 | .02 |
| Dyspnea score | 63.6 ± 22.3 | 64.9 ± 22.2 | .82 |
| Fatigue score | 52.3 ± 17.5 | 63.8 ± 24.5 | .04 |
| Appetite loss score | 69.3 ± 16.2 | 72.8 ± 17.8 | .43 |
| Nausea/vomiting score | 73.6 ± 13.4 | 75.3 ± 15.6 | .65 |
| Insomnia score | 59.3 ± 15.6 | 62.1 ± 19.4 | .54 |
| Financial problem score | 61.5 ± 13.7 | 62.8 ± 17.1 | .74 |
| Overall quality of life | 61.8 ± 12.4 | 54.5 ± 15.4 | .04 |
Abbreviations: KT, Kinesio taping; PG, pressure garment; SPADI, Shoulder Pain and Disability Index; QLQ-C30, Quality of Life Questionnaire for Cancer; EORTC, European Organization for Research and Treatment of Cancer.
Data are presented as mean ± standard deviation; significance at P ≤ .05.
Regarding quality of life questionnaire (EORTC QLQ-C30), there was a significant statistical improvement in functional scores, including physical, role, emotional, cognitive, and social scores in the KT group (P < .05). While the PG group only showed a significant improvement in emotional, cognitive, and social scores and not in physical and role scores (P > .05), as described in Table 2. While comparing the 2 groups at the end of the study, the KT group improved significantly in functional scores than the PG group, as presented in Table 3.
There was also a significant statistical improvement in symptom scores, including pain, dyspnea, fatigue, appetite loss, nausea, insomnia, and financial problem scores, in the KT group (P < .05). But the PG group showed no significant improvement in pain and fatigue scores (P > .05), as described in Table 2. Compared with the recipients of PG application, recipients of KT improved significantly in symptom scores (Table 3). Also, the overall quality of life improved significantly in both groups, but there was a significant difference between both groups in favor of the KT group, as presented in Table 3.
Post intervention, there were statistical significant differences between the 2 groups in all clinical characteristics (sum of limb circumference, SPADI, and handgrip strength), 2 functional scores (physical and role), 2 symptom scores (pain and fatigue), and overall quality of life in favor of the KT group (P < .05), as described in Table 3.
Discussion
The reports of this study showed that the KT group had significant changes in limb circumference, SPADI, handgrip strength, and overall quality of life at the end of the intervention (P < .05) than PG group. The changes we observed may be attributable to the dynamics of lymph. Generally, lymph is a white milky fluid that can be influenced by all physical activities and also by the disturbance of lymphatic tissues. Studies on lymphedema subjects show that any method that can change the contour of extremities may increase the lymph flow.31 Subjects with lymphedema secondary to breast cancer treatment have reduced physical activity that may exacerbate the symptoms.32,33 Reduced physical activity leads to reduced muscle activity that leads to reduced lymph circulation; also post lymphedema reduces the normal physical activity and adversely affect the quality of life.34,35
These subjects commonly complained about pain, discomfort, reduced handgrip strength and joint movements in the related extremity, and also increase limb circumference.34 These features can occur at any time after the surgery, immediately or at any time after surgery.36 This affects the function of skin, fascia, muscle, and joints and reduces the overall quality of life.37 Hence, it is necessary to provide proper medical care and early physical therapy for these subjects. Recently, physical therapists adapted the latest concepts such as KT, PGs, and physical exercises for draining lymphatic fluid. The contribution of the above-mentioned techniques was unclear in lymphedema following mastectomy.
KT is a commonly used method of application for lymphedema subjects; still we do not have evidence for its mechanism of action.14,38 It is observed that it increases the gap between the connective tissues, such as skin and fascia, fascia and muscles, and skin and muscles, which enhances fluid movement.39,40 It has a property that the subjects can tolerate the application of tape for about 3 days or more and also has waterproof quality. The stage of lymphedema following mastectomy progresses slowly; hence, the ultimate effect of KT depends on the stage and the method of application.17 On the contrary, few studies on KT showed negative results on BCRL and should not be an alternative choice of treatment.41,42
In our study, the PG group did not show any improvement in SPADI, handgrip strength, functional scores (physical and role scores), and symptom scores (pain and fatigue scores), and this report has been supported by a systemic review conducted by Moseley et al.43 The lack of significant differences may be due to the procedure of application, and also the presence of lymph varies from quadrant to quadrant and subject to subject.44
The results of our study showed statistically significant difference in the KT group when compared with the PG group. The mechanism behind the difference in the KT group is that it continuously facilitates lymph circulation and enhances the lymph flow in lymph capillaries and is also helpful for tissue regeneration. An increase in the blood flow decreases pain and also improves the handgrip strength.45 Till now there are only a few studies that compare the effect of KT and PG in postmastectomy lymphedema subjects.14,46,47 In the PG group, physical exercise is required throughout the application, which does not permit the full range of movements.
In addition, PG has other side effects such as blistering, rashes, and discomfort, which lead to poor compliance,48,49 and this explains the poor quality of life that was observed in the PG group of the current study. The present study is in agreement with the results of Tsai et al, who reported significant reduction of lymphedema and lymph circumference in both groups receiving KT and PG, but a higher percentage of reduction was recorded in the KT group.50 Furthermore, the results of the current study was in accordance with that of Białoszewski et al, who found that KT application is more effective than massage in edema reduction after Ilizarov method.37
The results of the PG group were surprising; the lymph collection was decreased, which was maintained for 15 to 18 hours; these results were in accordance with that of Partsch et al.51 The reduction in edema was due to the pressure of the PG, which was more than the pressure of the veins. This could have also been induced by low or negative lymphatic pressures. These mechanisms lead to the opening of the lymph capillaries.52 Some parameters do not show a significant drop, which may be due to pressure changes in the PGs over time.
Limitations
The limitations of this study included small sample size and lack of regular follow-up period; also the study randomization was not standardized. Another limitation may be the pressure difference between the manufacturer prescription and actual delivery of PGs. Another limitation is initiation of KT and PG treatment after the first phase of lymphedema, which may bias the study. Also, there is absence of objective measurement of limb size in the outcome. Also, intention-to-treat statistical analysis was not performed.
Conclusion
Our study concluded that the KT group had more improvement in limb circumference, SPADI, handgrip strength, and overall quality of life than the PG group at the end of the intervention. Further study can be done with large sample sizes with better experimental design and investigate the long-term effect of KT application in postmastectomy subjects with lymphedema.
Acknowledgments
The authors thank all patients who participated in this study.
Footnotes
Author Contributions: SAT and WKA designed and conducted research. GN and DMK collected the data and made statistical analysis. SAT, WKA, GN, and DMK wrote the article. DMK revised and edited the manuscript. All authors read and approved the final draft.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Trial Registration: ClinicalTrial.gov (Identifier: NCT03401086).
ORCID iD: Sayed A. Tantawy  https://orcid.org/0000-0002-7676-7764
https://orcid.org/0000-0002-7676-7764
References
- 1. Didem K, Ufuk YS, Serdar S, Zümre A. The comparison of two different physiotherapy methods in treatment of lymphedema after breast surgery. Breast Cancer Res Treat. 2005;93:49-54. [DOI] [PubMed] [Google Scholar]
- 2. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225-249. [DOI] [PubMed] [Google Scholar]
- 3. Kazanoglu E, Basaran S, Paydas S, Sarpel T. Efficacy of pneumatic compression and low-level laser therapy in the treatment of postmastectomy lymphedema: a randomized controlled trial. Clin Rehabil. 2009;23:117-124. [DOI] [PubMed] [Google Scholar]
- 4. Pyszora A, Krajnik M. Is Kinesio taping useful for advanced cancer lymphedema treatment? A case report. Adv Palliat Med. 2010;9:141-144. [Google Scholar]
- 5. Bąk-Sosnowska M, Oleszko K, Skrzypulec-Plinta V. Psychological adaptation of mature women in the first days after mastectomy. Menopausal Rev. 2013;2:120-124. [Google Scholar]
- 6. Harris SR, Hugi MR, Olivotto IA, Levine M; Steering Committee for Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. Clinical practice guidelines for the care and treatment of breast cancer: 11. Lymphedema. CMAJ. 2001;164:191-199. [PMC free article] [PubMed] [Google Scholar]
- 7. Wetzig N, Gill PG, Espinoza D, et al. Sentinel-lymph-node-based management or routine axillary clearance? Five-year outcomes of the RACS Sentinel Node Biopsy Versus Axillary Clearance (SNAC) 1 Trial: assessment and incidence of true lymphedema. Ann Surg Oncol. 2017;24:1064-1070. [DOI] [PubMed] [Google Scholar]
- 8. Fu MR, Rosedale M. Breast cancer survivors’ experiences of lymphedema-related symptoms. J Pain Symptom Manage. 2009;38:849-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Towers A, Hodgson P, Shay C, Keeley V. Care of palliative patients with cancer-related lymphoedema. J Lymphoedema. 2010;5:72-80. [Google Scholar]
- 10. Lacomba MT, Sánchez MJY, Goñi AZ, et al. Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. BMJ. 2010;340:b5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Castro-Sánchez AM, Lara-Palomo IC, Matarán-Peñarrocha GA, Fernández-Sánchez M, Sánchez-Labraca N, Arroyo-Morales M. Kinesio taping reduces disability and pain slightly in chronic non-specific low back pain: a randomised trial. J Physiother. 2012;58:89-95. [DOI] [PubMed] [Google Scholar]
- 12. Thelen MD, Dauber JA, Stoneman PD. The clinical efficacy of Kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. J Orthop Sports Phys Ther. 2008;38:389-395. [DOI] [PubMed] [Google Scholar]
- 13. Halseth T, McChesney JW, Debeliso M, Vaughn R, Lien J. The effects of Kinesio taping on proprioception at the ankle. J Sports Sci Med. 2004;3:1-7. [PMC free article] [PubMed] [Google Scholar]
- 14. Kase K, Wallis J, Kase T. Clinical Therapeutic Applications of the Kinesio Taping Method. 2nd ed. Tokyo, Japan: Ken Ikai; 2003. [Google Scholar]
- 15. Tantawy SA, Kamel DM. The effect of Kinesio taping with exercise compared with exercise alone on pain, range of motion, and disability of the shoulder in postmastectomy females: a randomized control trial. J Phys Ther Sci. 2016;28:3300-3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tantawy SA, Kamel DM. Effect of Kinesio taping on pain post laparoscopic abdominal surgery: randomized controlled trial. IJTRR. 2015;4:250-255. [Google Scholar]
- 17. Pop TB, Karczmarek-Borowska B, Tymczak M, Hałas I, Banaś J. The influence of Kinesiology taping on the reduction of lymphoedema among women after mastectomy—preliminary study. Contemp Oncol (Pozn). 2014;18:124-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kasawara KT, Mapa JMR, Ferreira V, et al. Effects of Kinesio taping on breast cancer related lymphedema: a meta-analysis in clinical trials. Physiother Theory Pract. 2018;34:337-345. [DOI] [PubMed] [Google Scholar]
- 19. Bertelli G, Venturini M, Forno G, Macchiavello F, Dini D. Conservative treatment of postmastectomy lymphedema: a controlled, randomized trial. Ann Oncol. 1991;2:575-578. [DOI] [PubMed] [Google Scholar]
- 20. Gergich NLS, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer. 2008;112:2809-2819. [DOI] [PubMed] [Google Scholar]
- 21. Singh B, Newton RU, Cormie P, et al. Effects of compression on lymphedema during resistance exercise in women with breast cancer- related lymphedema: a randomized cross-over trial. Lymphology. 2015;48:80-92. [PubMed] [Google Scholar]
- 22. Smile TD, Tendulkar R, Schwarz G, et al. A review of treatment for breast cancer-related lymphedema: paradigms for clinical practice. Am J Clin Oncol. 2018;41:178-190. [DOI] [PubMed] [Google Scholar]
- 23. Czerniec SA, Ward LC, Lee MJ, Refshauge KM, Beith J, Kilbreath SL. Segmental measurement of breast cancer related arm lymphoedema using perometry and bioimpedance spectroscopy. Support Care Cancer. 2011;19:703-710. [DOI] [PubMed] [Google Scholar]
- 24. Karges JR. Assessing the Relationship Between Water Displacement and Circumferential Measurements in Determining Upper Extremity Volume in Women With Lymphedema [dissertation]. Indianapolis, IN: Krannert School of Physical Therapy, University of Indianapolis; 1996. [Google Scholar]
- 25. McKenzie DC, Kalda AL. Effect of upper extremity exercise on secondary lymphedema in breast cancer patients: a pilot study. J Clin Oncol. 2003;21:463-466. [DOI] [PubMed] [Google Scholar]
- 26. Kaviani A, Fateh M, Nooraie RY, Alinagi-Zadeh MR, Ataie-Fashtami L. Low-level laser therapy in management of postmastectomy lymphedema. Lasers Med Sci. 2006;21:90-94. [DOI] [PubMed] [Google Scholar]
- 27. Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009;61:623-632. [DOI] [PubMed] [Google Scholar]
- 28. Hill CL, Lester S, Taylor AW, Shanahan ME, Gill TK. Factor structure and validity of the shoulder pain and disability index in a population-based study of people with shoulder symptoms. BMC Musculoskelet Disord. 2011;12:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Montazeri A, Harirchi I, Vahdani M, et al. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTCQLQ-C30): translation and validation study of the Iranian version. Support Care Cancer. 1999;7:400-406. [DOI] [PubMed] [Google Scholar]
- 30. Tantawy SA. Secondary upper limb lymphedema following mastectomy responses to kinesio taping application: A pilot study. Bioscience Research. 2019; 16(2): 1174-1180. [Google Scholar]
- 31. Shim JY, Lee HR, Lee DC. The use of elastic adhesive tape to promote lymphatic flow in the rabbit hind leg. Yonsei Med J. 2003;44:1045-1052. [DOI] [PubMed] [Google Scholar]
- 32. Winters-Stone KM, Bennett J, Nail L, Schwartz A. Strength, physical activity and age predict fatigue in older breast cancer survivors. Oncol Nurs Forum. 2008;35:815-821. [DOI] [PubMed] [Google Scholar]
- 33. Fialka-Moser V, Crevenna R, Korpan M, Quittan M. Cancer rehabilitation: particularly with aspects on physical impairments. J Rehabil Med. 2003;35:153-162. [DOI] [PubMed] [Google Scholar]
- 34. Smoot B, Wong J, Cooper B, et al. Upper extremity impairments in women with or without lymphedema following breast cancer treatment. J Cancer Surviv. 2010;4:167-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chachaj A, Malyszczak K, Pyszel K, et al. Physical and psychological impairments of women with upper limb lymphedema following breast cancer treatment. Psychooncology. 2010;19:299-305. [DOI] [PubMed] [Google Scholar]
- 36. Wójcik A. Imaging methods in the diagnosis of lymphedema. Acta Balneologica. 2007;4:223-233. [Google Scholar]
- 37. Białoszewski D, Woźniak W, Zarek S. Clinical efficacy of Kinesiology taping in reducing edema of the lower limbs in patients treated with the Ilizarov method—preliminary report. Ortop Traumatol Rehabil. 2009;11:46-54. [PubMed] [Google Scholar]
- 38. Santambrogio F, Cappellino F, Cardone M, Merlino A, Michelini S. Therapeutic application of the Kinesio taping method in the management of breast cancer-related lymphedema. Eur J Lymphol Relat Problem. 2010;21:6-11. [Google Scholar]
- 39. Campolo M, Babu J, Dmochowska K, Scariah S, Varughese J. A comparison of two taping techniques (Kinesio and McConnell) and their effect on anterior knee pain during functional activities. Int J Sports Phys Ther. 2013;8:105-110. [PMC free article] [PubMed] [Google Scholar]
- 40. Kalron A, Bar-Sela S. A systematic review of the effectiveness of Kinesio Taping—fact or fashion? Eur J Phys Rehabil Med. 2013;49:699-709. [PubMed] [Google Scholar]
- 41. Smykla A, Walewicz K, Trybulski R, et al. Effect of Kinesiology taping on breast cancer-related lymphedema: a randomized single-blind controlled pilot study. Biomed Res Int. 2013;2013:767106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Taradaj J, Halski T, Rosinczuk J, Dymarek R, Laurowski A, Smykla A. The influence of Kinesiology taping on the volume of lymphedema and manual dexterity of the upper limb in women after breast cancer treatment. Eur J Cancer Care. 2016;25:647-660. [DOI] [PubMed] [Google Scholar]
- 43. Moseley AL, Carati CJ, Piller NB. A systematic review of common conservative therapies for arm lymphoedema secondary to breast cancer treatment. Ann Oncol. 2007;18:639-646. [DOI] [PubMed] [Google Scholar]
- 44. Földi M, Földi E. Textbook of Lymphology. Munich, Germany: Elsevier; 2006. [Google Scholar]
- 45. Zajt-Kwiatkowska J, Rajkowska-Labon E, Skrobol W, Bakula S. Kinesio taping as the auxillary method in the physiotherapy process the clinical application. Nowiny Lekarskie. 2005;74:190-194. [Google Scholar]
- 46. Lipińska A, Sliwiński Z, Kiebzak W, Kirenko J. The influence of Kinesio taping applications on lymphedema of an upper limb in women after mastectomy. Fizjoterapia Polska. 2007;3:258-269. [Google Scholar]
- 47. Szczegielniak J, Krajczy M, Bogacz K, et al. Kinesio taping in physiotherapy after abdominal surgery. Fizjoterapia Polska. 2007;3:299-307. [Google Scholar]
- 48. Chi CF, Lin CH, Yang HS. The causal analysis of requested alterations for pressure garments. J Burn Care Res. 2008;29:965-974. [DOI] [PubMed] [Google Scholar]
- 49. Ripper S, Renneberg B, Landmann C, Weigel G, Germann G. Adherence to pressure garment therapy in adult burn patients. Burns. 2009;35:657-664. [DOI] [PubMed] [Google Scholar]
- 50. Tsai HJ, Hung HC, Yang JL, Huang CS, Tsauo JY. Could Kinesio tape replace the bandage in decongestive lymphatic therapy for breast-cancer-related lymphedema? A pilot study. Support Care Cancer. 2009;17:1353-1360. [DOI] [PubMed] [Google Scholar]
- 51. Partsch H, Winiger J, Lun B. Compression stockings reduce occupational leg swelling. Dermatol Surg. 2004;30:737-743. [DOI] [PubMed] [Google Scholar]
- 52. Olszewski WL. Contractility patterns of human leg lymphatics in various stages of obstructive lymphedema. Ann N Y Acad Sci. 2008;1131:110-118. [DOI] [PubMed] [Google Scholar]