Abstract
Home smoking bans may be an effective way to promote tobacco cessation among treatment seeking smokers. Few studies have examined this relationship in a quitline setting. Data were obtained from 14,296 adults who were enrolled in a state quitline between January 2011 and July 2016. This study investigated whether cessation rates varied by changes in home smoking ban implementation between enrollment and 7-month follow-up. The impact of changes in home smoking bans on cessation at follow-up was significantly modified by having other smokers living in the home at follow-up (P < 0.0001). Among callers who did not live with other smokers in the home, the highest odds ratio of 30-day cessation was for callers who reported bans at follow-up only (OR = 10.50, 95%CI: 8.00, 13.70), followed by callers who reported bans at both enrollment and follow-up (OR = 8.02, 95%CI: 6.27, 10.30) and callers who reported bans at enrollment only (OR = 2.06, 95% CI: 1.47, 2.89) compared with callers with no home smoking bans. When callers reported that they lived with other smokers in the home, the effect of home smoking bans on cessation was much smaller. Quitlines should support the implementation of home smoking bans as a part of callers’ goal setting activities to achieve tobacco cessation.
Introduction
Tobacco objectives in Healthy People 2020 include increasing the proportion of smoke-free homes [1]. Home smoking bans are a well-recognized strategy for protecting the health of children [2]. One study found that implementing complete home smoking bans substantially reduced cotinine levels in infants by upwards of 85% [3]. Home smoking bans are also beneficial for youth living in the home. For example, one study found that youth who lived in households with a complete home smoking ban were less likely to perceive a high prevalence of adult smoking in their town and were less likely to consider adult smoking to be socially acceptable compared with youths who lived in households without complete home smoking bans [4]. The associations existed regardless of whether there was a smoker in the home. Home smoking bans are also associated with reduced adolescent smoking; however, the association is stronger among homes with non-smoking parents compared with those with at least one smoking parent or other adult [5].
A growing number of observational studies have provided evidence that home smoking bans can also increase the likelihood of tobacco cessation. A prospective study found that complete smoking bans were associated with increased odds of a subsequent quit attempt and lower relapse rate among smokers who were preparing to quit [6]. Another observational study indicated that home smoking bans were the only significant predictor of quit attempts and cessation compared with workplace smoking bans and local tobacco control regulations [7]. A review of cross-sectional and longitudinal studies documented that a smoke-free home was related to increased smoking cessation and decreased cigarette use among adults [8].
Additional support comes from clinical trials that have documented positive effects of smoke-free home and tobacco smoke exposure reduction interventions on adult smoking behavior. A recent study which pooled data from three randomized controlled trials showed that low income smokers who adopted a smoke-free home were more likely to report quitting smoking than those who did not adopt a smoke-free home at 3- and 6-month follow-ups [9]. Another example is a behavioral counseling trial for underserved maternal smokers that focused on promoting efforts to reduce children’s exposure to tobacco smoke (not maternal cessation) [10]. The counseling intervention not only significantly reduced child cotinine levels, but also increased biochemically verified quit rates among maternal smokers compared with a usual care control group. Secondary analysis of the maternal smoking study demonstrated that home smoking ban restrictions partially mediated the association between the counseling intervention and maternal smokers’ bioverified quit status [11]. Additional evidence comes from a study that compared a behavioral intervention integrating pediatrician advice with telephone-based skills training and support from a health counselor compared with standard care in pediatrician primary care [12].
Quitlines have emerged as a standard care intervention for smoking cessation. Although burgeoning evidence exists on the impact of home smoking bans on cessation among clinical trials, there is little known about whether this association exists in large scale intervention settings, such as quitlines. In addition, few studies have identified factors that may affect the magnitude of the association between home smoking bans and cessation in those settings. Of particular interest is the impact of having other smokers living in the home. Research has shown that multimember households with smokers are less likely to consistently report strict home bans [13], which may weaken the effects of home smoking bans on cessation. The purpose of this study was to examine the effects of home smoking bans on 30-day tobacco cessation among callers to the Arizona Smokers’ Helpline (ASHLine), which provides smoking cessation services to ∼7700 individuals annually. Specifically, we aimed to: (i) determine if cessation rates varied by changes in the implementation of home smoking bans between enrollment and the 7-month follow-up period; and (ii) to examine whether the effect of home smoking bans was modified by the presence of other smokers living in the home.
Materials and methods
Participants and quitline services
This study was based on data obtained from adults who enrolled in ASHLine (https://ashline.org/) between 1 January 2011 and 26 July 2016. The ASHLine provides tobacco cessation services to Arizona residents who are self-referred (e.g. proactively call the quitline through media ads, or word of mouth) or are referred by healthcare providers. After completing an enrollment survey, callers are assigned to a tobacco cessation coach who conducts weekly calls for up to three months. Coaches provide information and support regarding identification of triggers, stimulus- and urge-management strategies, smoking cessation tips, preparation for setting a quit day, and relapse prevention. Callers who meet the eligibility criteria may receive up to 4 weeks of free nicotine replacement therapy, consisting of patches, gum, or lozenges. All callers who consent for a follow-up receive a 7-month telephone survey conducted by trained ASHLine staff to assess cessation outcomes. Because of the use of de-identified data, the study was granted exempt status by the University Institutional Review Board.
For most of the time period covered by this study (1 January 2011–1 January 2016), ASHLine did not have a standardized coaching protocol that included advice to implement home smoking bans. Coaches are trained to tailor advice and use problem solving strategies that promote cessation in a person-centered approach unique in the context of each caller. Thus, coaches and callers decide together whether setting goals to establish a home smoking ban would facilitate a caller’s cessation process. After 1 January 2016, ASHLine implemented a protocol to reduce tobacco smoke exposure protocol among children. The protocol targeted smokers who had a child under the age of 18 living at home. For those callers, coaches provided information about second- and third-hand smoke and engaged in discussions about environmental triggers and home smoking habits.
Measures
Tobacco cessation
Smoking cessation at 7-month follow-up was the primary outcome measure. Callers were asked, ‘Have you used tobacco in the last 30 days?’ Response options were yes or no.
Home smoking bans
At enrollment and 7-month follow-up, implementation of home smoking bans was assessed. At enrollment, callers were asked ‘Is smoking allowed in your home?’ Response options were: smoking not allowed; smoking allowed in some places; or smoking allowed anywhere.
At the 7-month follow-up, callers were asked ‘Is smoking/chewing/dipping allowed in your home?’ Response options were: yes; no, not at all; only in certain places; or outdoors only. Responses from both time points were categorized as complete home smoking ban, partial home smoking ban, or no home smoking ban. A complete home smoking ban was defined as no smoking allowed inside the home. The response options at enrollment, ‘smoking not allowed’ and at follow-up, ‘no, not at all’ and ‘outdoors only’ were categorized as complete home smoking ban. A partial home smoking ban was defined as smoking allowed in some places inside the home. The response options at enrollment, ‘allowed in some places,’ and at follow-up, ‘only in certain places,’ were categorized as partial home smoking ban. No home smoking ban was defined as smoking allowed anywhere in the home. The response options at enrollment, ‘smoking allowed anywhere,’ and at follow-up, ‘yes,’ were categorized as no home smoking ban.
Tobacco use behaviors
At enrollment, callers were asked about several tobacco use behaviors including age of smoking initiation, nicotine dependence, confidence in quitting, intention to quit smoking and living with other smokers. Age of smoking initiation was assessed by asking callers what age they started smoking cigarettes regularly. Nicotine dependence was determined by administering the Fagerstr�m Test for Nicotine Dependence [14]. Total scores were calculated from 5 items and ranged from 1 to 10 with higher scores indicating greater dependence. Confidence in quitting was measured using a single item. Callers were asked, ‘On a scale of 1–5, how sure are you that you will be able to quit using tobacco for at least 24 h?’ Response options ranged from 1 = not confident to 5 = extremely confident. Responses were dichotomized with confident = ‘confident’, ‘very confident’, or ‘extremely confident’ or not confident = ‘somewhat confident’ or ‘not confident.’ Intention to quit was assessed by asking callers, ‘Are you planning to quit smoking cigarettes within the next 30 days?’ Response options were: I have already quit; yes; no; or don’t know. Responses were dichotomized as yes = ‘yes’ or ‘I have already quit’ or no = ‘no’ or ‘I don’t know.’ Callers were also asked, ‘Do others smoke at home?’ Based on the question that preceded it, ‘others’ referred to other people in the household. Response options were: no; yes-inside; yes-outside. Responses were dichotomized as yes = ‘yes-inside’ or ‘yes-outside’or no = ‘no’. During the 7-month follow-up, other smokers living in the home was measured with the question, ‘Who else in your household uses tobacco?’ Response options were: significant other, no one, and other. Responses were dichotomized as no = ‘no one’ or yes = ‘significant other’ or ‘other’.
Cessation strategies
At the 7-month follow-up, callers were asked if they had used any tobacco cessation medication. Medication options were nicotine replacement therapies (i.e. patch, gum, lozenge), Chantix, and Zyban/Wellbutrin. Responses were dichotomized as yes or no. Data on number of completed coaching sessions were obtained from ASHLine call records. Coaching sessions were analysed as a binary variable, consisting of zero to four coaching sessions or five or more coaching sessions. This decision was based on the North American Quitline Consortium best practice protocols of five or more coaching sessions [15].
Demographics and health history
At enrollment, callers reported on age, gender, race, ethnicity, education level, type of health insurance and number of children under age 18 living in the home. Race was categorized as white, black, or other. Missing responses for Hispanic/Latino ethnicity were imputed as no. Education level was dichotomized as no high school diploma or high school diploma. Type of health insurance was used as a proxy measurement for socioeconomic status and was dichotomized as private insurance or not insured/underinsured. Callers reported on whether they had ever been treated for any of the following health conditions separately: asthma, hypertension, cancer, chronic obstructive pulmonary disease, diabetes or heart disease. Callers were also asked if they had they had ever been treated for ‘mental health or emotional challenges, such as anxiety disorder, depression, bipolar disorder, alcohol or drug abuse or schizophrenia.’ Response options for all health questions were: yes; no; I don’t know. Refusals were considered missing data, and responses of ‘I don’t know’ were inferred to be no.
Statistical analyses
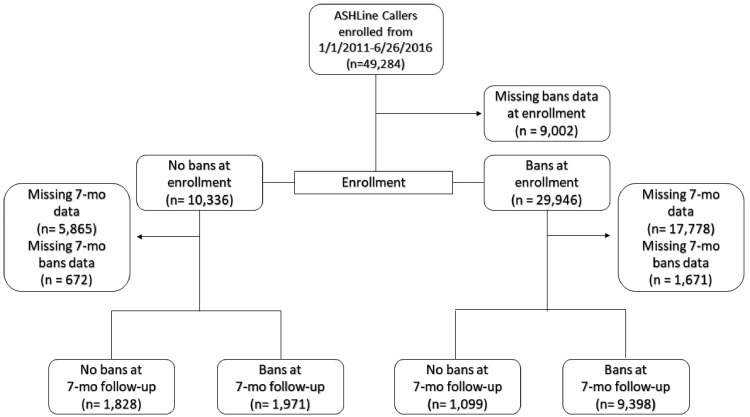
A total of 49 284 callers enrolled in ASHLine services between 1 January 2011 and 26 June 2016. Among the entire sample, 40 282 (81.7%) had data on home smoking bans at enrollment, and 14 296 (35.4%) had data on home smoking bans and tobacco cessation at the 7-month follow-up. Analyses were conducted with the sample of 14 296 callers who reported on home smoking bans at both time points and tobacco cessation at the 7-month follow-up. Figure 1 presents the caller flow diagram.
Fig. 1.
ASH Line caller flow diagram.
Descriptive statistics were computed and stratified by home smoking ban category, with differences tested using chi-square tests and analysis of variance (ANOVA). Home smoking ban categories were based on home smoking ban status at both assessment periods. Callers were categorized into: no home smoking bans, home smoking bans at enrollment only, home smoking bans at 7-month follow-up only, and home smoking bans at both enrollment and follow-up. Partial bans were combined with complete bans because of evidence that individuals with existing partial bans are more likely than those with no bans to implement complete bans over time [16].
We estimated unadjusted cessation rates for callers who reported implementing no home smoking bans at enrollment, by follow-up home smoking ban status and tested with a chi-square test for trend. Follow-up home smoking ban status included no home smoking ban, partial home smoking ban, and complete home smoking ban. Partial and complete home smoking bans were examined separately in order to determine if they had different effects on cessation.
Logistic regression was used to investigate the impact of changes in home smoking bans on 30-day cessation. Similar to the descriptive statistics, home smoking ban category was used in the analyses and partial bans were combined with complete home smoking bans. Adjusted models included the following pre-specified variables, which were chosen based on review of the literature: age, gender, education, chronic health condition, mental health condition, nicotine dependence, other smokers living in the home, use of tobacco cessation medication and number of coaching sessions. We included interaction terms of other smokers living in the home with home smoking bans to test whether the effects of home smoking bans were modified by having other smokers living in the home. Separate terms for other smokers living in the home at enrollment and follow-up were tested. Linearity in the logit for continuous variables was assessed using restricted cubic splines [17].
Sensitivity analyses
We carried out three sensitivity analyses for the logistic regression model. First, to assess the effect of missing data due to dropout for the outcome of 30-day cessation we used multiple imputation with chained equations [18]. Variables used in the primary analysis were used in the imputation and analysis model. Second, we investigated and allowed for nonlinearity in continuous variables (age, number of coaching calls) using restricted cubic splines [17]. Finally, our original analysis categorized partial home smoking bans into the complete home smoking bans group. We checked the sensitivity of our results to this assumption by classifying them into the no home smoking bans group. All analyses were performed in SAS version 9.4 [19]. Statistical significance was set at 0.05.
Results
Description of study participants
Table I presents the demographic characteristics, tobacco use behaviors and cessation strategies and outcomes among callers by home smoking bans category. Across the two time points, 12.8% callers reported implementing no home smoking bans, 7.7% callers reported implementing home smoking bans at enrollment only, 13.8% callers reported implementing home smoking bans at follow-up only, and 65.7% callers reported implementing home smoking bans at both enrollment and follow-up. When compared with callers who did not implement bans during both time points, those who implemented home smoking bans at enrollment and/or 7-month follow-up were younger, more likely to have children living in the home, and less likely to report having a chronic health condition. Callers who had implemented a home smoking ban at one or both time points were less likely to currently use tobacco every day, were less dependent on nicotine, smoked less, and were more confident in their ability to quit compared with callers who did not implement a home smoking ban at both time points.
Table I.
ASHLine caller characteristics at enrollment and 7-month follow-up (n = 14 296)
| Home smoking ban category | |||||
|---|---|---|---|---|---|
| Characteristics | None (n = 1828) | Enrollment only (n = 1099) | 7-month follow-up only (n = 1971) | Both enrollment and 7-month follow-up (n = 9398) | P-valuea |
| At enrollment | |||||
| Age, mean (SD) | 56.8 (11.8) | 52.3 (14.3) | 55.0 (12.2) | 50.3 (13.9) | <0.0001b,c,d |
| Female gender | 1072 (58.6) | 610 (55.5) | 1155 (58.6) | 5099 (54.3) | <0.0001d |
| Insurance | |||||
| State medicaid | 499 (27.3) | 287 (26.1) | 499 (25.3) | 1759 (18.7) | <0.0001b,c,d |
| Private | 995 (54.4) | 565 (51.4) | 1006 (51.0) | 5123 (54.5) | |
| Uninsured | 331 (18.1) | 242 (22.0) | 458 (23.2) | 2475 (26.3) | |
| Education | |||||
| High school or less | 293 (16.0) | 172 (15.7) | 318 (16.1) | 1342 (14.3) | 0.03d |
| More than high school | 1462 (80.0) | 885 (80.1) | 1575 (80.0) | 7804 (83.0) | |
| Children living in home | 176 (9.7) | 236 (21.5) | 264 (13.4) | 2958 (31.5) | <0.0001b,c,d |
| Chronic condition | |||||
| Asthma | 371 (20.3) | 264 (24.0) | 431 (21.9) | 1560 (16.6) | <0.0001b,d |
| COPD | 483 (26.4) | 242 (22.0) | 414 (21.0) | 1232 (13.1) | <0.0001b,c,d |
| Diabetes | 356 (19.5) | 165 (15.0) | 351 (17.8) | 1237 (13.2) | <0.0001b,d |
| Heart disease | 260 (14.2) | 131 (11.9) | 249 (12.6) | 838 (8.9) | <0.0001b,d |
| High blood pressure | 770 (42.1) | 376 (34.2) | 785 (39.8) | 2819 (30.0) | <0.0001b,d |
| Cancer | 185 (10.1) | 102 (9.3) | 189 (9.6) | 733 (7.8) | 0.0007d |
| Mental health condition | 830 (45.4) | 477 (43.4) | 763 (38.7) | 3193 (34.0) | <0.0001c,d |
| Any of the above | 1260 (68.9) | 701 (63.8) | 1286 (65.3) | 4981 (53.0) | <0.0001b,c,d |
| Other smokers living in the home | 978 (53.5) | 528 (48.0) | 911 (46.2) | 3949 (42.0) | <0.0001b,c,d |
| Smoking in the home | |||||
| Not allowed | 0 (0.0) | 0 (0.0) | 1908 (96.8) | 9299 (99.0) | <0.0001c,d |
| Allowed in some places | 0 (0.0) | 0 (0.0) | 63 (3.2) | 99 (1.0) | |
| Allowed anywhere | 1828 (100) | 1099 (100) | 0 (0.0) | 0 (0.0) | |
| Age of tobacco | |||||
| Initiation, mean (SD) | 17.4 (6.2) | 17.2 (5.7) | 17.6 (6.2) | 17.9 (6.2) | <0.0001d |
| Frequency of current tobacco use | <0.0001b,c,d | ||||
| Not at all | 79 (4.3) | 114 (10.4) | 112 (5.7) | 783 (8.3) | |
| Some days | 21 (1.2) | 18 (1.6) | 21 (1.1) | 185 (2.0) | |
| Every day | 1718 (94.0) | 950 (86.4) | 1820 (92.3) | 8354 (88.9) | |
| Number of cigarettes smoked per day, mean (SD) | 21.2 (11.3) | 19.0 (20.4) | 20.1 (11.7) | 15.4 (8.9) | <0.0001b,c,d |
| Nicotine dependence score (range 0–10), mean(SD) | 5.6 (2.3) | 4.9 (2.3) | 5.3 (2.2) | 4.3 (2.3) | <0.0001b,c,d |
| Number of quit attempts, mean (SD) | 3.0 (16.6) | 2.7 (13.3) | 3.1 (15.0) | 3.6 (23.3) | <0.0001d |
| Confidence in quitting | 1375 (75.2) | 918 (83.5) | 1637 (83.1) | 8047 (85.6) | <0.0001b,c,d |
| Intention to quit | 1655 (90.5) | 979 (89.1) | 1838 (93.3) | 8712 (92.7) | <0.0001c,d |
| At 7-month follow-up | |||||
| Other smokers living in the home | 747 (40.9) | 433 (39.4) | 544 (27.6) | 2537 (27.0) | <0.0001c,d |
| Use of tobacco cessation medication | 1144 (62.6) | 704 (64.1) | 1260 (63.9) | 6328 (67.3) | <0.0001c,d |
| Number of coaching sessions, mean (SD) | 4.6 (4.3) | 4.5 (4.8) | 5.3 (2.2) | 4.8 (4.2) | <0.0001c |
| 30-day cessation | 264 (14.4) | 234 (21.3) | 996 (50.3) | 4325 (46.0) | <0.0001b,c,d |
Mean (SD) shown for continuous variables, frequencies (%) shown for categorical variables. Partial bans were combined with complete home smoking bans. Missing data rates ranged from 0 to 5%, except for number of cigarettes per day (11%); nicotine dependence (9%); cessation medication (11%).
Overall Chi-square (categorical) and ANOVA tests for non-missing data.
Statistically significant between ‘None’ versus ‘Enrollment only’.
Statistically significant between ‘None’ versus ‘Follow-up only’.
Statistically significant between ‘None’ versus ‘Both’.
Impact of implementation of home smoking bans on tobacco cessation
Among the 3799 callers who reported no home smoking ban at enrollment, the highest rate of 30-day cessation at 7-month follow-up was reported by those who implemented complete home smoking bans at the follow-up (51.3%), followed by those who implemented partial home smoking bans (27.0%) and those who implemented no bans (14.4%; P < 0.0001, chi-square test of trend).
Impact of changes in home smoking ban implementation on tobacco cessation
The effect of changes in home smoking bans on cessation at the 7-month follow-up was significantly modified by the presence of other smokers living in the home at follow-up (P < 0.0001), but not by the presence of other smokers living in the home at enrollment (see Table II). The latter interaction term was removed from the model, and odds ratios for each of the home smoking bans categories were calculated with the reference category of no home smoking bans (at either enrollment or follow-up), stratified by whether there were other smokers living in the home at follow-up.
Table II.
Predictors of 30-day tobacco cessation at 7-month follow-up among ASHLine callersa
| Adjusted OR (95% CI) | P-value | |
|---|---|---|
| Home smoking bans, other smokers living in home (follow-up) | ||
| None | Ref | 0.37 |
| Enrollment only | 1.18 (0.82, 1.64) | <0.0001 |
| Follow-up only | 2.25 (1.65, 3.06) | <0.0001 |
| Both enrollment and follow-up | 1.63 (1.28, 2.07) | |
| Home smoking bans, no other smokers living in home (follow-up) | ||
| None | Ref | <0.0001 |
| Enrollment only | 2.06 (1.47, 2.89) | <0.0001 |
| Follow-up only | 10.5 (8.00, 13.70) | <0.0001 |
| Both enrollment and follow-up | 8.02 (6.27, 10.30) | |
| Other smokers living in home (enrollment) | 1.26 (1.14, 1.39) | <0.0001 |
| Male gender | 0.99 (0.91, 1.09) | 0.85 |
| Age | 1.04 (1.00, 1.08) | 0.06 |
| High school graduate or greater | 1.14 (1.01, 1.29) | 0.04 |
| Children living in home | 0.98 (0.88, 1.10) | 0.77 |
| Chronic health conditionb | 0.89 (0.81, 0.98) | 0.01 |
| Mental health condition | 0.74 (0.68, 0.82) | <0.0001 |
| Nicotine dependence score | 0.93 (0.91, 0.95) | <0.0001 |
| Use of tobacco cessation medication | 1.21 (1.09, 1.35) | 0.0003 |
| Intention to quit | 1.78 (1.38, 2.30) | <0.0001 |
| Number of coaching sessions | 1.10 (1.08, 1.11) | <0.0001 |
Partial bans were combined with complete home smoking bans. P values for interaction of bans and others smokers living in the home at follow-up <0.0001.
Model c-index = 0.73.
Chronic health condition included asthma, chronic obstructive pulmonary disease, diabetes, heart disease, high blood pressure, cancer and mental health condition.
Among callers with no other smokers living in the home at follow-up, the odds ratios of 30-day cessation at follow-up was 2.06 (95%CI: 1.47, 2.89) for callers with home smoking bans at enrollment only; 10.50 (95%CI: 8.00, 13.70) for callers with bans at follow-up only; and 8.02 (95%CI: 6.27, 10.30) for callers with home smoking bans at both enrollment and follow-up, as compared with callers with no home smoking bans. Among callers living with other smokers, the effect of home smoking bans on tobacco cessation was much smaller. Specifically, the odds ratios of 30-day cessation at follow-up was 1.18 (95%CI: 0.82, 1.64) for callers with home smoking bans at enrollment only; 2.25 (95%CI: 1.65, 3.06) for callers with bans at follow-up only, and 1.63 (95%CI: 1.28, 2.07) for callers with bans at both enrollment and follow-up compared with callers with no home smoking bans. Other variables that were associated with increased odds of 30-day tobacco cessation at 7-month follow-up were education, use of tobacco cessation medication, intention to quit, number of coaching sessions and other smokers living in the home at enrollment. Variables that were associated with decreased odds of cessation included reporting being treated for a chronic condition, reporting being treated for a mental health condition and higher nicotine dependence.
Sensitivity analyses
Table III shows the results of the sensitivity analyses. Each of the sensitivity analyses produced substantively similar results to the primary analysis, with the statistical significance of the interaction of other smokers living in the home and bans category remaining. The use of restrictive cubic splines to accommodate the non-linearity in coaching sessions and age yielded similar results to the primary analysis, although odds ratios were slightly larger. Including partial bans in the no bans category instead of the bans category also had little effect on odds ratio estimates. In the multiple imputation analysis, the effect of bans was still significantly modified by having other smokers living in the home at follow-up, but the estimated ORs were slightly larger for callers with other smokers living in the home at follow-up, and slightly smaller for callers without other smokers living in the home at follow-up.
Table III.
Sensitivity analysis results: adjusted odds ratios and 95% CIs for 20 multiply imputed datasets; a model that allowed for non-linearity in continuous variables (age and number of coaching sessions) using restricted cubic splines; and categorizing partial bans with no bans (instead of with complete bans)
| Primary results | Multiple imputation | Non-linearity | Categorizing partial bans with no bans | |
|---|---|---|---|---|
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Home bans, other smokers living in home | ||||
| None | Ref | Ref | Ref | Ref |
| Enrollment only | 1.18 (0.82, 1.64) | 1.29 (0.96, 1.62) | 1.20 (0.84, 1.72) | 1.38 (0.92, 2.06) |
| Follow-up only | 2.25 (1.65, 3.06) | 1.82 (1.49, 2.22) | 2.37 (1.74, 3.23) | 1.85 (1.44, 2.37) |
| Both enrollment and follow-up | 1.63 (1.27, 2.07) | 1.74 (1.39, 2.18) | 1.68 (1.32, 2.14) | 1.57 (1.25, 1.96) |
| Home bans, no other smokers living in home | ||||
| None | Ref | Ref | Ref | Ref |
| Enrollment only | 2.06 (1.40, 2.89) | 1.54 (1.20, 1.98) | 1.95(1.40, 2.72) | 2.70 (1.89, 3.86) |
| Follow-up only | 10.5 (8.0, 13.70) | 6.94 (5.70, 8.45) | 10.2 (7.86, 13.4) | 9.30 (7.46, 11.60) |
| Both enrollment and follow-up | 8.02 (6.27, 10.30) | 7.16 (5.78, 8.86) | 7.73 (6.09, 9.83) | 7.41 (5.98, 9.18) |
Note: Significance (P < 0.05) denoted by bold values.
Dropout before 7-month follow-up
Comparison of baseline characteristics of callers who dropped out with callers who had 7-month follow-up data is shown in the Supplementary Table AI. Although many of the comparisons were statistically significant, it was mostly due to the large sample size, with very small differences which are unlikely to be important. Dropping out of ASHLine services was associated with younger age (47.9 versus 51.9 years); female gender (59 versus 56%); children living in the home (30 versus 25%); not having a chronic medical condition (54 versus 58%); and being uninsured (31 versus 25%). Baseline behaviors and treatment experiences associated with dropout were other smokers living in the home (48 versus 45%); every day tobacco use (92 versus 88%); higher numbers of cigarettes smoked per day (17.6 versus 17.1); and higher nicotine dependence scores (4.8 versus 4.7). Callers who dropped out had significantly fewer coaching calls on average (2.8 versus 4.8 calls).
Discussion
This observational study provided insight on the use of home smoking bans among quitline callers, majority of whom received only general guidance on home smoking bans from the quitline. The results showed that implementing any type of home smoking ban, complete or partial, during the quitting process significantly increased the likelihood of cessation at 7-month follow-up. However, the rates of 30-day cessation were highest for the callers who implemented complete home smoking bans (51.3%) compared with those who implemented partial home smoking bans (27.0%) or no ban at all (14.4%). It was not surprising that the effects of home smoking bans on tobacco cessation were modified by the presence of other smokers living in the home. This provides further support that other smokers may create a social environment that is challenging to implement home smoking bans. A study found that multimember households with smokers were less likely to consistently report strict home bans [13]. Another study showed that households with three or more smokers experienced greater difficulties with enforcement of home smoking bans [16].
These findings suggest that callers may benefit from implementing home smoking bans as part of goal setting conducted with quitline coaches. Callers who implemented a complete or partial home smoking ban after enrolling in the quitline were more likely to report being quit compared with those who had already established home smoking bans at enrollment and maintained them at the 7-month follow-up. Among those with no ban at enrollment, perhaps making efforts to establish a home smoking ban enhances confidence in the smoking behavior change process that increases likelihood of cessation. Quitlines may use a variety of approaches to promote smoke-free homes among callers. At a minimum, quitlines may offer brief advice to all callers on how to implement home smoking bans as an integral part of the quitting and relapse prevention process, an effort that has the secondary benefit of protecting the health of children, non-smokers and pets living in the home. However, some research suggested that brief advice may not change parents’ likelihood of creating or maintaining home smoking bans [20]. Therefore, quitlines may need to provide more intensive home smoking ban interventions that are integrated within their standard cessation intervention protocol. They may want to adapt clinical interventions that have effectively reduced child tobacco smoke exposure and promoted parent tobacco cessation [12]. Alternatively, quitlines may want to consider the feasibility and impact of community-based interventions like the one created by Escoffery et al. [21] that promoted smoke-free homes using telephone coaching protocols. Quitlines should also consider practical, social, cultural and personal factors that may be involved in establishing a smoke-free home [22] when creating new protocols. For example, they may want to address the barriers faced by callers who live with other smokers. Quitlines may want to provide additional training on negotiation and communication skills, which may enable callers to implement and enforce home smoking bans without creating conflict and pressure for others to quit smoking if they are not ready. Such skills may help address and resolve acts of physical and verbal resistance that have been documented in the literature [23].
This study had some limitations. The study did not collect data on the processes of establishing and maintaining home smoking bans during the period between enrollment and the 7-month follow-up. It is possible that there may have been fluctuations and changes in implementation during the 7-month period, which may have impacted rates of tobacco cessation. In addition, the study did not assess the timing of home smoking ban implementation and cessation at the 7-month follow-up. The home smoking bans may have preceded or followed cessation. Another limitation was the use of different measures for home smoking bans and other smokers living in the home at enrollment and 7-month follow-up. This was a reflection of real-life practices in quitlines where survey items may be developed by different staff and implemented at different time points. It was possible, however, to categorize the response options into the same groups. This study also relied on self-report data on the use of home smoking bans. Research has shown some households, particularly those with smokers and children are less likely to consistently report strict home bans, raising concerns about analyses based solely on individual reports [13]. Another limitation was the use of self-report data on tobacco cessation, which may have been affected by recall and social desirability biases. Some intervention studies have documented significant group differences for self-reported abstinence but not for cotinine measures [24]. The quitline in this study does not obtain cotinine levels from callers. Collecting self-report data for tobacco cessation outcomes is standard practice among quitlines. There was also a significant amount of missing data at enrollment and 7-month follow-up. However, this limitation was offset by the large dataset. In addition, multiple imputation in the sensitivity analysis generally supported the results of the analysis.
This study identified several areas for future research on home smoking bans. More research is needed to understand the processes and patterns of implementing home smoking bans over time and related impacts on cessation. This study only measured home smoking bans at two separate time points. There were no data collected on home smoking ban implementation throughout the 7-month period. Another area for future research includes studies on the feasibility of conducting home smoking ban interventions in quitline settings. Feasibility studies may examine participant recruitment and retention, implementation and maintenance of home smoking bans, cessation behaviors and satisfaction with the intervention. Future studies should also consider the impact of financial and social contingencies to enforce home smoking bans. Subsequent investigations should include trials to examine the effectiveness of home smoking ban interventions in quitline settings, comparing brief and more comprehensive interventions with usual practice. In addition, researchers may want to consider administering objective measures of home smoking ban enforcement, such as biomarker tests with children or non-smokers living in the home or assessment of home air quality [2]. However, objective measurements may be difficult for quitlines to implement, and thus, feasibility studies may be needed.
Quitlines are an important and untapped resource for promoting smoke-free homes. The potential benefits of increasing the implementation of home smoking bans among the quitline population are significant at multiple levels. At the individual and interpersonal levels, encouraging home smoking bans among callers may increase rates of cessation and reduce tobacco smoke exposure to children and others living in the home. At the broader society level, reducing tobacco smoke exposure helps to create smoke-free norms and strengthen anti-tobacco culture [25]. Furthermore, disseminating smoke-free homes among low income households may help reduce income disparities in smoking cessation [26]. Thus, by promoting both cessation and smoke-free homes, quitlines may play a larger role in tobacco control efforts around the United States and globe.
Supplementary Material
Acknowledgements
The authors thank Benjamin R. Brady for his assistance with the ASHLine dataset and article revisions.
Funding
This work was supported by the Arizona Department of Health Services [grant numbers ADHS13-026130, ADHS11-007339 and HS160051-0/E1H37741] and the National Cancer Institute at the National Institutes of Health [grant number P30 CA023074]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies or the University of Arizona.
Conflict of interest statement
None declared.
References
- 1.Healthy People 2020. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Available at: https://www.healthypeople.gov/. Accessed: 20 March 2018.
- 2. Rosen LJ, Myers V, Hovell M. et al. Meta-analysis of parental protection of children from tobacco smoke exposure. Pediatrics 2014; 133: 698–714. [DOI] [PubMed] [Google Scholar]
- 3. Matt G, Quintana P, Hovell M. et al. Households contaminated by environmental tobacco smoke: sources of infant exposures. Tob Control 2004; 13: 29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Albers AB, Biener L, Siegel M. et al. Household smoking bans and adolescent antismoking attitudes and smoking initiation: findings from a longitudinal study of a Massachusetts youth cohort. Am J Public Health 2008; 98: 1886–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Emory K, Saquib N, Gilpin EA. et al. The association between home smoking restrictions and youth smoking behaviour: a review. Tob Control 2010; 19: 495–506. [DOI] [PubMed] [Google Scholar]
- 6. Pizacani BA, Martin D, Stark M. et al. A prospective study of household smoking bans and subsequent cessation related behaviour: the role of stage of change. Tob Control 2004; 13: 23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Biener L, Hamilton WL, Siegel M. et al. Individual, social-normative, and policy predictors of smoking cessation: a multilevel longitudinal analysis. Am J Public Health 2010; 100: 547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mills AL, Messer K, Gilpin EA. et al. The effect of smoke-free homes on adult smoking behavior: a review. Nicotine Tob Res 2009; 11: 1131–41. [DOI] [PubMed] [Google Scholar]
- 9. Haard�rfer R, Kreuter M, Berg CJ. et al. Cessation and reduction in smoking behavior: impact of creating a smoke-free home on smokers. Health Educ Res 2018; 33: 256–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Collins BN, Nair US, Hovell MF. et al. Reducing underserved children’s exposure to tobacco smoke: a randomized counseling trial with maternal smokers. Am J Prev Med 2015; 49: 534–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Collins BN, Nair US, Davis SM. et al. Increasing home smoking restrictions boosts underserved moms' bioverified quit success. Am J Health Behav 2019; 43: 50–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Collins BN, Lepore SJ, Winickoff JP. et al. An office-initiated multilevel intervention for tobacco smoke exposure: a randomized trial. Pediatr 2018; 141: S75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mumford EA, Levy DT, Romano EO.. Home smoking restrictions: problems in classification. Am J Prev Med 2004; 27: 126–31. [DOI] [PubMed] [Google Scholar]
- 14. Heatherton TF, Kozlowski LT, Frecker RC. et al. The Fagerstr�m Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict 1991; 86: 1119–27. [DOI] [PubMed] [Google Scholar]
- 15.North American Quitline Consortium. Quitline Services: Current Practice and Evidence Base, 2016. Phoenix, AZ, 2016.
- 16. Kegler MC, Haard�rfer R, Bundy LT. et al. Do partial home smoking bans signal progress toward a smoke-free home? Health Educ Res 2016; 31: 24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Desquilbet L, Mariotti F.. Dose‐response analyses using restricted cubic spline functions in public health research. Stat Med 2010; 29: 1037–57. [DOI] [PubMed] [Google Scholar]
- 18. Azur MJ, Stuart EA, Frangakis C. et al. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 2011; 20: 40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Institute S. SAS Version 9.4. Cary, NC: SAS Institute, 2013.
- 20. Wakefield M, Banham D, McCaul K. et al. Effect of feedback regarding urinary cotinine and brief tailored advice on home smoking restrictions among low-income parents of children with asthma: a controlled trial. Prev Med 2002; 34: 58–65. [DOI] [PubMed] [Google Scholar]
- 21. Escoffery C, Mullen P, Genkin B. et al. Coaching to create a smoke-free home in a brief secondhand smoke intervention. Health Educ Res 2017; 32: 555–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Passey ME, Longman JM, Robinson J. et al. Smoke-free homes: what are the barriers, motivators and enablers? A qualitative systematic review and thematic synthesis. BMJ Open 2016; 6: e010260.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kegler MC, Escoffery C, Groff A. et al. A qualitative study of how families decide to adopt household smoking restrictions. Fam Community Health 2007; 30: 328–41. [DOI] [PubMed] [Google Scholar]
- 24. Choi WS, Beebe LA, Nazir N. et al. All Nations Breath of Life: a randomized trial of smoking cessation for American Indians. Am J Prev Med 2016; 51: 743–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hovell MF, Hughes SC.. The behavioral ecology of secondhand smoke exposure: a pathway to complete tobacco control. Nicotine Tob Res 2009; 11: 1254–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vijayaraghavan M, Benmarnhia T, Pierce JP. et al. Income disparities in smoking cessation and the diffusion of smoke-free homes among U.S. smokers: results from two longitudinal surveys. PLoS One 2018; 13: e0201467. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.