Abstract
Umbilical vein varices are rare fetal anomalies typically found intra-abdominally and identified on ultrasound prior to birth. Intra-abdominal umbilical vein varices account for approximately 4% of umbilical cord abnormalities and are thought to be a developmental abnormality rather than a congenital malformation. The umbilical vein varix anomaly been shown to be associated with a higher incidence of adverse perinatal outcomes and there is evidence of a relationship between this and chromosomal abnormalities. There have been few case reports of extra-abdominal varices. This case reviews a multiparous Hispanic female who delivered a baby with an extra-abdominal umbilical vein varix who was admitted to the neonatal intensive care unit but had an uncomplicated hospital course. The report reviews strategies for antenatal testing and surveillance of identified varices.
Keywords: pregnancy, materno-fetal medicine, ultrasonography
Background
This is a rare condition that neither the resident, family medicine attending nor neonatal intensive care unit (ICU) attending had seen in the past. In researching umbilical vein varices, this finding is associated with adverse perinatal outcomes and chromosomal abnormalities. Furthermore, this patient could have received more adequate antenatal testing had the varix been correctly identified on a prior ultrasound.
Case presentation
A G5P4004 Hispanic female, aged 34 years, at 36 weeks and 2 days by an 8-week dating ultrasound was referred for an urgent ultrasound evaluation following a non-reactive non-stress test (NST) during a routine 36-week prenatal visit.
The pregnancy was naturally conceived without artificial or in vitro assistance. Her past obstetrical history was significant for four prior spontaneous vaginal deliveries, all without antenatal or postpartum complications and all occurring outside of the current hospital system. Medications included a prenatal vitamin once daily. She had no allergies and denied tobacco, alcohol and illicit drug use. She had no family history of pregnancy-related diseases. Her blood type was O positive, antibody negative; rubella immune; HIV negative; rapid plasma reagin (RPR) non-reactive; hepatitis B surface antigen (HBSAg) negative; gonorrhoea/chlamydia negative. Her pregnancy was complicated by limited prenatal care, size measuring larger than dates, unknown group B streptococcus status and an elevated glucola (1 hour, 50 g dose) of 146 without a 3-hour glucose test.
The urgent ultrasound revealed a single intrauterine pregnancy at 36 weeks and 2 days and fetal growth at >90th percentile (estimated fetal weight 3732 g) and an abdominal circumference of >97th percentile. The amniotic fluid index was normal at 14.88 cm. There was a thickened area of umbilical cord with heterogeneous and hyperechoic areas seen around the vessels without a filling defect noted in the vessels or flow in the echogenic areas (figure 1). Umbilical artery Doppler studies were normal without absent or reverse flow seen (figure 2). There was positive fetal breathing during the exam. Routine ultrasound 1 month prior reported an umbilical cord cyst adjacent to the abdominal cord insertion and recommended follow-up ultrasound for interval growth in 1 month. The clinical significance of this umbilical cord finding was unknown, so in the setting of a non-reactive NST, induction of labour was recommended.
Figure 1.

Fetal ultrasound image, sagittal view.
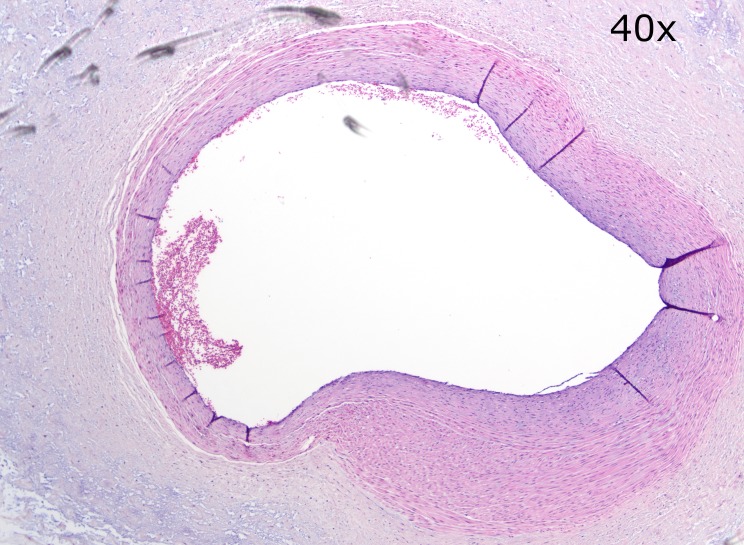
Figure 2.
Fetal ultrasound image, colour flow Doppler, arterial.
The initial fetal monitoring strip revealed a baseline rate of 150 bpm, minimal variability, absent accelerations, absent decelerations, with a final interpretation of non-reactive. After a dose of antibiotic (ampicillin 2 g intravenous then 1 g intravenous every 4 hours) was administered because of the gestational age below 37 weeks, our team proceeded with artificial rupture of membranes. The first stage of labour was 11 hours, 35 min. Second and third stages were 26 and 17 min, respectively. A male fetus was delivered by spontaneous vaginal delivery without complication. Apgar scores were 8 and 9 at 1 and 5 min, respectively, with a birth weight of 3647 g. Estimated maternal blood loss was 300 cc.
An abnormality of the extra-abdominal umbilical cord between the attachment of the cord and the placenta was noted (figure 3). The placenta was sent to pathology for immediate evaluation.
Figure 3.
Photo of extra-abdominal vein varix.
The gross pathological description of the placenta showed a singleton placenta with attached fetal membranes and portion of umbilical cord. The placental disc measured 22.7×17.5×3.5 cm and weighed 922.1 g (trimmed of umbilical cord and fetal membranes). The fetal surface was blue-grey, smooth and glistening. The fetal membranes were tan-pink, smooth, wrinkled and slightly thickened and opacified with a normal insertion. The segment of attached umbilical cord measured 29.8 cm in length by 1.5 cm in diameter (average) and demonstrated three umbilical vessels. It inserted in an eccentric fashion approximately 4.9 cm from the placental periphery and twisted to the right. A 19.5 cm in length by 4.9 cm in diameter portion of severely edematous umbilical cord was present freely floating in the specimen container. The umbilical cord additionally displayed multifocal areas of haemorrhage. The maternal surface was red-brown, slightly torn but appeared to be complete, and lobulated. On sectioning, parenchymal findings include red-brown, spongy, grossly unremarkable placental parenchyma.
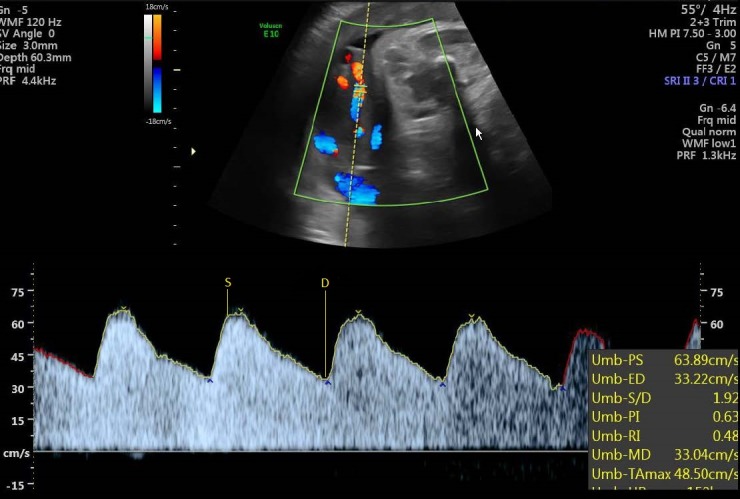
The final pathological diagnosis concluded this was a near-term, large-for-gestational age placenta (expected 372–542 g), with chorangiosis and a three-vessel umbilical cord with marked oedema, vascular dilatation (figure 4) and haemorrhage, consistent with varix.
Figure 4.
Image of dilated umbilical vessel within edematous umbilical cord (H&E, 40x).
Outcome and follow-up
The final pathology tissue specimen results showed a near-term, but large-for-gestational age placenta. There was a three-vessel umbilical cord with marked oedema, vascular dilatation and haemorrhage, consistent with an extra-abdominal umbilical vein varix.
The near-term male newborn patient was admitted to the neonatal ICU after delivery for close monitoring and was then discharged home with his mother on day 2 of admission after an uncomplicated hospital course.
Discussion
Umbilical vein varices are rare fetal anomalies typically found intra-abdominally and identified on ultrasound prior to birth. Intra-abdominal umbilical vein varices account for approximately 4% of umbilical cord abnormalities and are thought to be a developmental abnormality rather than a congenital malformation.1 There have been few case reports of extra-abdominal varices, which are typically identified as a postnatal diagnosis, and most of which are diagnosed retrospectively during autopsy.2 An extra-abdominal umbilical varix is difficult to diagnose prenatally as it can appear like a cyst on ultrasound prior to birth. Confirmation of the diagnosis requires pathology.1 Classification of an intra-abdominal umbilical vein varix includes measurement of an umbilical vein diameter ≥9 mm or wider than 50% the diameter of the intrahepatic umbilical vein.3 There is not clear data on classifying measurements of an extra-abdominal varix.
The umbilical vein varix anomaly has been shown to be associated with a higher incidence of adverse perinatal outcomes including intrauterine fetal death, fetal heart failure, hydrops fetalis, thrombosis, umbilical cord twisting with subsequent ulceration and blood loss.2 Other fetal anomalies include cryptorchidism and cerebral ventriculomegaly.4 There is also evidence of a relationship between the varix anomaly and chromosomal abnormalities including trisomy 21, trisomy 18 and mosaics like Turner’s syndrome.2 Because of the increased morbidity and mortality, chromosomal testing, fetal echocardiogram and antenatal surveillance are recommended.5 An expedited delivery may also be appropriate.5 In one study, 23 cases of intra-abdominal umbilical vein varix revealed 48% fetuses with normal outcomes and 35% with a structural anomaly present.6 It has been recommended that ultrasonography of the newborn be ordered to look for an anastomosis of the umbilical vein into the extrahepatic portal system that can lead to a life-threatening thrombosis of the portal system.7
The clinical significance of an extra-abdominal umbilical vein varix is unknown, but continued surveillance of growth and development during the perinatal period is warranted given the high rates of anomalies.
Learning points.
An umbilical vein varix is a rare fetal anomaly associated with high rates of adverse perinatal outcomes and fetal death.
Typically, intra-abdominal umbilical vein varices are in the prenatal period, but extra-abdominal umbilical vein varices are difficult to diagnose via ultrasound.
The clinical significance of an extra-abdominal umbilical vein varix is unknown; however, the majority of cases documented are identified after fetal death.
Generally accepted recommendations for fetuses with umbilical vein varices include chromosomal testing, fetal echocardiogram and antenatal surveillance with timely delivery.
Footnotes
Contributors: NC and LC-V both made substantial contributions to the conception and design of the work. SC drafted the work and LC-V revised it critically for important intellectual content. NC contributed in the pathological and histopathological assessment/specimen. NC, SC and LC-V give final approval of the version published. NC, SC and LC-V agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Parental/guardian consent obtained.
References
- 1. Bouzid A, Karmous N, Trabelsi H, Mkaouar L, Mourali M. Fetal Intra-abdominal Umbilical Vein Varix: A Case Report and Literature Review. Gynecology & Obstetrics 2016;06:2161–932. 10.4172/2161-0932.1000379 [DOI] [Google Scholar]
- 2. Al-Maghrabi HA, Contreras LHC, Martinez S. Extra abdominal Umbilical Vein Varix Causing Stillbirth: a Case Report. Annals of Pathology and Laboratory Medicine 2017;4:C94–C97. 10.21276/APALM.1265 [DOI] [Google Scholar]
- 3. Lallar M, Phadke SR. Fetal intra abdominal umbilical vein varix: Case series and review of literature. Indian J Radiol Imaging 2017;27:59 10.4103/0971-3026.202964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee SW, Kim MY, Kim JE, et al. Clinical characteristics and outcomes of antenatal fetal intra-abdominal umbilical vein varix detection. Obstet Gynecol Sci 2014;57:181–6. 10.5468/ogs.2014.57.3.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ozek MA, Calis P, Bayram M, et al. Fetal intraabdominal umbilical vein varix: antenatal diagnosis and management. J Matern Fetal Neonatal Med 2018;31:245–50. 10.1080/14767058.2016.1278208 [DOI] [PubMed] [Google Scholar]
- 6. Rahemtullah A, Lieberman E, Benson C, et al. Outcome of pregnancy after prenatal diagnosis of umbilical vein varix. J Ultrasound Med 2001;20:135–9. 10.7863/jum.2001.20.2.135 [DOI] [PubMed] [Google Scholar]
- 7. Beraud E, Rozel C, Milon J, et al. Umbilical vein varix: Importance of ante- and post-natal monitoring by ultrasound. 2015;96:21–6. [DOI] [PubMed] [Google Scholar]