Abstract
Cryptococcal infection constitutes around 3% of opportunistic infections in solid organ transplant recipients. Most common organ affected in renal transplant recipients (RTRs) is central nervous system and usually presents with chronic meningoencephalitis (CME). Ischaemic stroke as a consequence of cryptococcal meningoencephalitisis rare and possibly due to the involvement of intracranial vessel by exudates causing vasculitis-related thrombosis. In this context, we describe an unusual case of asymptomatic cryptococcaemia in an RTR, progressing on to acute ischaemic stroke secondary to acute CME with near complete neurological recovery following timely diagnosis, early and appropriate antifungal treatment. The index case attempts to re-emphasise the significance of mandatory screening required to exclude the possibility of dissemination of cryptococcaemia in RTRs besides highlighting the requirement of prolonged induction phase with combination therapy, particularly in presence of stroke.
Keywords: cryptococcus, meningitis, vasculitis
Background
Cryptococcal infection is the third most common invasive fungal infection after Aspergillus and Candida in solid organ transplant recipients (SOTRs).1 The overall incidence of cryptococcosis in SOTRs is 2.8% (range, 0.3%–5%),2 with mortality rates reported between 33% and 42%.3 In an immunocompetent host, cryptococcal infection is subclinical and limited to lungs; however, in an immunocompromised state as in renal transplant recipient (RTR), central nervous system (CNS) is the most common site, followed by cutaneous, pulmonary, prostate and bone.4 Neurocryptococcosis usually present with focal neurological deficits like impaired cognition, seizures, cranial nerve deficits5 secondary to acute or chronic meningoencephalitis (CME) and cryptococcoma. Rarely, cerebral infarcts can occur secondary to cryptococcal vasculitis (incidence: 4%–8% of cryptococcal infections) and primarily affects basal ganglia, internal capsule, thalamus, frontal, temporal and parieto-occipital regions in the descending order.6 Sudden onset hemiparesis in an RTR in the absence of fever or a headache may masquerade as classic ischaemic stroke. However, lacunar infarcts secondary to small vessel vasculitis complicating CME due to opportunistic CNS infections (tubercular, fungal) although a rare entity, requires deliberation because of the entirely different approach to diagnosis, management and prognosis. We report an unusual case of CME presenting as an acute ischaemic stroke.
Case presentation
A 57-year-old man, who underwent a live emotionally related renal transplant 2 years ago (wife as a blood group compatible donor), with stable graft function (serum creatinine of 1.2 mg/dL) on triple immunosuppression therapy (tacrolimus, mycophenolate mofetil and steroids) presented with fever and graft-site pain for 2 days. Evaluation revealed raised serum creatinine of 2.8 mg/dL, with haemoglobin of 128 g/L, total leucocyte count of 8900×109/L. His chest X-ray, ultrasound abdomen and serum procalcitonin were normal and blood tacrolimus trough level was 6 ng/mL. Urine routine microscopy was normal with no pus cells, protein and red blood cells. Keeping the possibility of acute rejection, he underwent graft biopsy which revealed acute T cell-mediated rejection. He was treated with injection methylprednisolone 500 mg intravenous daily for 3 days, following which his symptoms resolved. However, a week later his blood culture (sent 3 days prior to pulse steroid) grew Cryptococcus neoformans. Although patient was asymptomatic despite cryptococcaemia, with no clinical evidence of cutaneous, pulmonary or neurological involvement, liposomal amphotericin (3 mg/kg/day, 150 mg/day) was commenced considering his immunocompromised state. Patient was advised for diagnostic lumbar puncture (cerebrospinal fluid [CSF] analysis) to rule out CNS cryptococcosis, however he did not consent for the same. One week later, patient presented to emergency room with sudden onset, progressive weakness of left half of body of 1 day duration. He denied history of fever, headache, vomiting, seizures, syncope, ear discharge or trauma. His neurological examination was remarkable for left spastic hemiparesis, left facial palsy, terminal neck stiffness and left extensor plantar. Rest of the physical examination was normal. CSF done now revealed raised protein (85.5 mg/dL), low sugar (38 mg/dL; with corresponding blood sugar of 130 mg/dL), raised cell count of 84 cells/mm3; (lymphocyte 80%), negative Gram stain and mycobacterial work-up (acid-fast bacilli stain, adenosine deaminase and PCR).Cytology for malignant cells as well as herpes simplex and toxoplasma PCR were negative; however, India ink showed rounded encapsulated yeast, sabouraud agar grew cream coloured colonies and cryptococcal antigen was positive (1:8). MRI with angiography revealed acute lacunar infarcts in the right basal ganglia and thalamus with multiple periventricular lacunar infarcts around the circle of Willis (figure 1). Work-up to search for possible alternative aetiology included Holter, echocardiography to rule out cardiac cause, anti-nuclear antibody (ANA), anti-neutrophil cytoplasmic antibody (ANCA) by ELISA, high sensitivity C-reactive protein (hsCRP) and erythrocyte sedimentation rate (ESR) to rule out vasculitis, antiphospholipid antibody (APLA) and procoagulant work-up to rule out hypercoagulable state was negative. Patient denied a medical history of diabetes (HbA1c—5.6%) and hypertension.
Figure 1.
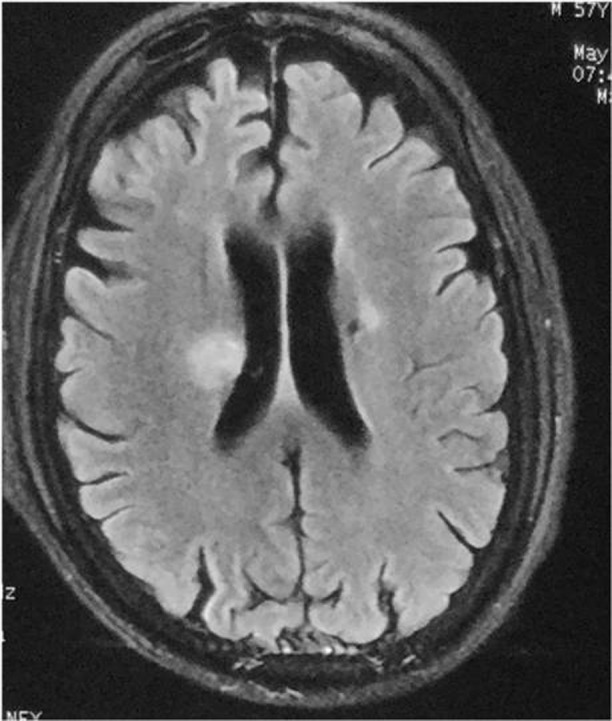
MRI brain showing hyper intense lesions in right thalamus, basal ganglia and periventricular area suggestive of acute infarct (T2/FLAIR image).
Treatment
Considering the possibility of cryptococcus-related CNS vasculitis, immunosuppression was curtailed (prednisolone tapered to 10 mg/day and mycophenolate mofetil and tacrolimus were withheld), and amphotericin was continued. Oral flucytosine was also added until CSF became sterile at 2 weeks. Patient recovered significantly with 3 weeks of amphotericin (cumulative dose −4.5 g) and he received consolidation phase with oral fluconazole (6 mg/kg/day for 8 weeks) and subsequently maintained on secondary suppressive fluconazole prophylaxis (4 mg/kg/day). Neurological reassessment following recovery from stroke did not reveal any evidence of hearing impairment, muscle weakness and cognitive deficits.
Outcome and follow-up
On follow-up, he continued to have persistent graft dysfunction with serum creatinine increasing to 3.5 mg/dL, repeat allograft biopsy was done, which revealed significant interstitial fibrosis and tubular atrophy (over 60%) with no evidence of rejection or simultaneous/consequent cryptococcal infection involving allograft. His graft function progressively worsened over the next 6 months, requiring initiation of haemodialysis. Now, he is doing fine on maintenance haemodialysis with minimal immunosuppression (prednisolone 5 mg/day).
Discussion
The index case is an RTR who was asymptomatic, when detected to have cryptococcaemia which later progressed on to acute ischaemic stroke secondary to acute meningoencephalitis, nevertheless had near complete neurological recovery following early and appropriate antifungal treatment. Neurocryptococcosis, a life-threatening infection, usually occurs in an immunocompromised patient. CME is traditionally detected by CSF demonstration of encapsulated yeast on India ink, mucicarmine or periodic acid Schiff stain in over 70% of patients with high specificity (97%) but poor sensitivity (73%).7 Confirmation is by culture on Saboraud’s medium with specific biochemical reactions (urease, phenoloxidase) and cryptococcal capsular polysaccharide antigen titre >1:8 in serum or CSF which has high sensitivity and specificity.8
Except for dimorphic fungi, most fungal pathogens are slow multipliers, thereby mandating at least 1–2 weeks of incubation time for blood cultures,9 as observed in the index case where cryptococcus was grown after 1 week. Cryptococcaemia results from lympho-haematogenous dissemination from an overt or subclinical pulmonary focus; however, search for the same was not rewarding in the index case.
Infarcts secondary to CME are mostly of lacunar type suggesting small vessel involvement; proposed aetiopathogenesis is enumerated in table 1. These lacunar infarcts tend to be acute, unilateral and multiple with predominant periventricular distribution attributable to the involvement of circle of Willis by basal exudates of chronic meningitis. Other uncommon10 neurovascular manifestations include cerebellar involvement,11 recurrent infarctions and progressive vascular dementia.
Table 1.
Lacunar infarcts in cryptococcal meningoencephalitis: aetiopathogenesis and work-up
| S no | Proposed etiopathogenesis | Work- up |
| 1 | Inflammation and strangulation of vessels leading to vasospasm |
MRI brain
Basal exudates meningeal enhancement hydrocephalus |
| 2 | Meningeal inflammation progressing to affect entire vessel wall causing thrombosis | |
| 3 | Stretching of inflamed vessels due to dilated ventricles | |
| 4 | Exaggerated inflammatory response |
Lab
Elevated ESR and hsCRP Anti-phospholipid antibody Anti-cardiolipin antibody Elevated factor VIII level Protein S deficiency |
| 5 | Acquired prothrombotic states |
Even when tangible-isolated organ involvement due to Cryptococcus is evident, as in index case, failure to screen for possible dissemination, and consequent delay in management with combination therapy (amphotericin and flucytosine) may contribute to poorer outcome as aptly evident in the largest ever series of 66 cases of CME from Indian subcontinent,12 where higher mortality and morbidity was observed in patients with infarct (n=20) when compared with patients who did not have infarct (n=46) with OR of 9.1 and 2.6, respectively.
Induction therapy in management of CME aims for rapid sterilisation of CSF, with atleast 2 weeks of amphotericin (1.0 mg/kg/day) in combination with flucytosine (100 mg/kg/day) as the first-line therapy to achieve early fungicidal activity (measured as the rate of yeast clearance/mL of CSF/day) and has been associated with a 40% lower hazard of mortality at 10 weeks. Slower rates of fungal clearance following amphotericin monotherapy have been shown to be associated with increased mortality at both 2 and 10 weeks.13 However, when flucytosine is unavailable, combination of amphotericin with fluconazole (800 mg/day) had better long-term outcomes than amphotericinand fluconazole (400 mg/day) or amphotericin alone.14
Learning points.
Cryptococcaemia in a renal transplant recipient (RTR) even when asymptomatic, should always be considered as a red herring for possible dissemination and warrants extensive evaluation and treatment.
Acute ischaemic stroke consequent to CME in an RTR is a rare entity, with higher mortality and morbidity; nevertheless, reversible if diagnosed early and adequately treated with prolonged induction phase comprising combination therapy with amphotericin and flucytosine, particularly in presence of stroke.
Footnotes
Contributors: VS and NP: writing, concept and image acquisition. RR and KLG: proof reading and corrections.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Pappas PG, Alexander BD, Andes DR, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis 2010;50:1101–11. 10.1086/651262 [DOI] [PubMed] [Google Scholar]
- 2. Singh N, Dromer F, Perfect JR, et al. Cryptococcosis in solid organ transplant recipients: current state of the science. Clin Infect Dis 2008;47:1321–7. 10.1086/592690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Abhilash KP, Mitra S, Arul JJ, et al. Changing paradigm of cryptococcal meningitis: an eight-year experience from a tertiary hospital in South India. Indian J Med Microbiol 2015;33:25–9. 10.4103/0255-0857.148372 [DOI] [PubMed] [Google Scholar]
- 4. Agrawal C, Sood V, Kumar A, et al. Cryptococcal infection in transplant kidney manifesting as chronic allograft dysfunction. Indian J Nephrol 2017;27:392–4. 10.4103/ijn.IJN_298_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kuriakose CK, Mishra AK, Vanjare HA, et al. Visual disturbance in patients with cryptococcal meningitis: The road ahead. J Neurosci Rural Pract 2017;8:151–2. 10.4103/0976-3147.193560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lan SH, Chang WN, Lu CH, et al. Cerebral infarction in chronic meningitis: a comparison of tuberculous meningitis and cryptococcal meningitis. QJM 2001;94:247–53. 10.1093/qjmed/94.5.247 [DOI] [PubMed] [Google Scholar]
- 7. Saha DC, Xess I, Biswas A, et al. Detection of Cryptococcus by conventional, serological and molecular methods. J Med Microbiol 2009;58(Pt 8):1098–105. 10.1099/jmm.0.007328-0 [DOI] [PubMed] [Google Scholar]
- 8. Agarwal V, Sachdev A, Agarwal G, et al. Disseminated cryptococcosis mimicking lymphoreticular malignancy in a HIV negative patient. JK Science 2004;6:93–5. [Google Scholar]
- 9. Bosshard PP. Incubation of fungal cultures: how long is long enough?. Mycoses 2011;54:e539–e545. 10.1111/j.1439-0507.2010.01977.x [DOI] [PubMed] [Google Scholar]
- 10. Eric Searls D, Sico JJ, Bulent Omay S, et al. Unusual presentations of nervous system infection by Cryptococcus neoformans. Clin Neurol Neurosurg 2009;111:638–42. 10.1016/j.clineuro.2009.05.007 [DOI] [PubMed] [Google Scholar]
- 11. Mishra AK, Vanjare HA, Raj PM. Cryptococcal meningitis presenting as acute onset bilateral cerebellar infarct. J Neurosci Rural Pract 2017;8:159–60. 10.4103/0976-3147.193537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mishra AK, Arvind VH, Muliyil D, et al. Cerebrovascular injury in cryptococcal meningitis. Int J Stroke 2018;13:57–65. 10.1177/1747493017706240 [DOI] [PubMed] [Google Scholar]
- 13. Bicanic T, Muzoora C, Brouwer AE, et al. Independent association between rate of clearance of infection and clinical outcome of HIV-associated cryptococcal meningitis: analysis of a combined cohort of 262 patients. Clin Infect Dis 2009;49:702–9. 10.1086/604716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pappas PG, Chetchotisakd P, Larsen RA, et al. A phase II randomized trial of amphotericin B alone or combined with fluconazole in the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis 2009;48:1775–83. 10.1086/599112 [DOI] [PubMed] [Google Scholar]


