Abstract
Hereditary segmental neurofibromatosis (SNF) is an extremely rare form of SNF with nine families reported till date. SNF is considered to be a result of mosaicism and hereditary transmission is possibly explained by increased susceptibility of mutations at neurofibromatosis gene loci. We report here three members of an Indian family with SNF. Our index case, a 20-year-old woman had multiple soft to firm papules and nodules over right shoulder associated with severe intermittent pain. Her father had three similar nodules over left upper arm and elder sister had two such nodules over right upper arm. The father and elder sister were incidentally diagnosed and they had never sought medical advice considering their lesions to be a familial trait. In the absence of symptoms, many familial cases of SNF are missed thus making any systematic analysis to ascertain its genetic basis difficult.
Keywords: dermatology, genetics
Background
Segmental neurofibromatosis (SNF) is a rare form of neurofibromatosis (NF) with a reported prevalence of 0.0014%–0.002%.1 It is included in the Riccardi’s classification as type V NF.2 Since its inception in 1931 by Gammel; its diagnostic criteria has changed significantly and so has its nomenclature.3 Crowe et al in 1956 termed it as sectoral NF presenting with dermatomal neurofibromas and café-au-lait spots.4 Riccardi’s initial diagnostic criteria were quite stringent and included unilateral involvement, absence of family history or systemic symptoms. However, with passage of time atypical manifestations of SNF were reported and in 1987 Roth et al reclassified SNF into four subtypes namely: true SNF, localised with deep involvement, hereditary SNF and bilateral SNF.1 Since then over 150 cases of SNF have been published in literature with varying manifestations. Least common among all is the hereditary SNF.1 Until there are nine reported families with SNF.5 We here report an Indian family where father and two daughters had SNF. Another interesting finding in the reported family is the variable severity of SNF.
Case presentation
Case 1 (index case)
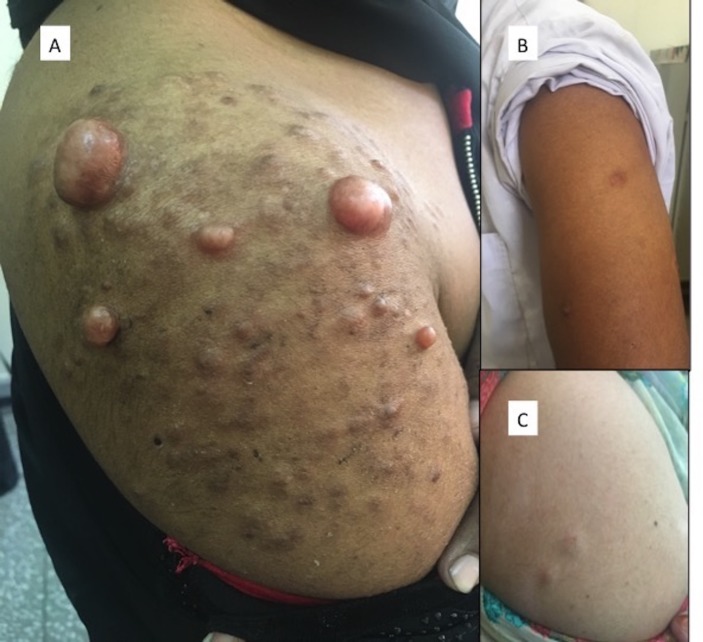
A 20-year-old Indian, woman presented with multiple nodules over right shoulder associated with severe pain extending till neck for the past 2 years. These were progressively increasing in size and number. There was no prior history of trauma or surgical intervention. On examination, there were multiple skin coloured to hyperpigmented papules and sessile nodules ranging in size from 0.5×0.5 to 4×3 cm over right shoulder (figure 1A). These were soft to firm in consistency and were slightly tender. Patient’s predominant concern was the excruciating intermittent pain apart from the cosmetic disfigurement. Her general physical examination including vitals as well as the systemic examination were normal. On the basis of clinical presentation with provisional diagnosis of SNF, family history was elicited and patient reported similar lesions in sister and father. She had total of seven siblings.
Figure 1.
(A) (Case 1) Multiple papules and nodules over right shoulder. (B) (Case 2) Three nodules over left upper arm. (C) (Case 3) Two nodules over right upper arm.
Case 2
A 54-year-old man (father of index case) had three soft, skin coloured, non-tender nodules of size 1×0.5 cm over left upper arm (figure 1B). He had never sought medical consultation for the same. He reported that he had a consanguineous marriage and his wife was his third degree relative.
Case 3
A 30-year-old woman (elder sister of index case) had two soft, non-tender, skin coloured nodules of size 1×0.5 cm over right upper arm (figure 1C). She also had never sought medical advice due to lack of symptoms considering it to be a familial trait. Patient had two offspring and none had similar lesions.
Investigations
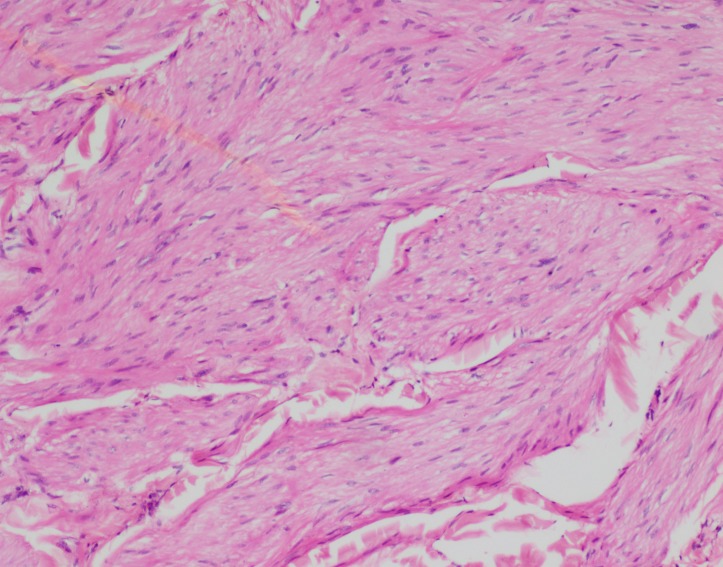
All the cases were thoroughly examined and none had other features of NF including café-au-lait macules, lisch nodules, axillary freckling, neurological deficit or cranial bone abnormalities. MRI of left shoulder was done for the index case which did not reveal involvement of deeper structures. Her biochemical investigations and blood counts were normal. A punch biopsy specimen (4 mm) was taken from all three for histopathological examination. Similar findings were reported in all the three specimens. It revealed a poorly encapsulated benign spindle cell tumor. The spindle cells had wavy nuclei without pleomorphism and were arranged in whorls with intersecting collagen bundles favouring a diagnosis of neurofibroma (figure 2). A gene mutation analysis for confirmation of diagnosis could not be performed due to financial constrains. A timeline representing the time of onset, progression and symptoms of the cases is depicted in table 1.
Figure 2.
(H&E x100) Benign spindle cell tumour forming whorls and intersecting fascicles.
Table 1.
Timeline of relevant findings in three reported cases
| Case no | Age (years) | Age at onset of lesions (years) | Progression | Symptoms |
| 1 (Index case) | 20 | 6 | Progressive | Pain |
| 2 (Sister) | 30 | 10 | Non-progressive | Asymptomatic |
| 3 (Father) | 54 | 15 | Non-progressive | Asymptomatic |
Treatment
Thus, a final diagnosis of hereditary SNF was established. Patient was counselled about the genetic nature of the disease emphasising the need for regular follow-up for early detection of malignancy. Index case was referred to neuromedicine for management of pain where she was started on pregabalin (75 mg two times per day).
Outcome and follow-up
She had partial relief after taking pregabalin for 4 weeks and is continuing it. Plastic surgery consultation for resection of lesion was sought but due to possibility of resultant deformity patient did not opt for it.
Discussion
SNF unlike NF-1 does not follow autosomal dominant mode of inheritance. It is considered to be a result of postzygotic somatic mutation in neural crest cells.6 If this mutation occurs prior to tissue differentiation; the resultant disease is generalised and indistinguishable from NF-1. But if it occurs later in development only localised disease develops. Thus, somatic mosaicism is considered to be the basis for SNF. Mosaicism in gonadal cell lines results in transmission of NF-1 in progeny.7 8
The basis of transmission of hereditary SNF is still unclear. Until nine families of hereditary SNF have been reported.5 With this small number genetic analysis to ascertain exact mode of transmission is difficult. Clinical presentation of SNF varies in different patients. Some present with localised neurofibromas and others with associated café-au-lait macules and axillary freckling. The largest case review done by Hager et al in 1997 reports thoracic dermatome (40%) to be the most common site involved followed by cervical (38%) and lumbar dermatome (24%). Facial involvement has been reported rarely.9 Pain is the most common symptom followed by neuritis and neurological deficit. Our patient also sought medical consultation for pain.
Limited number of cases of SNF has been reported with systemic involvement such as visceral neurofibromas, skeletal abnormalities and renal agenesis. Malignant nerve sheath tumours and malignant melanomas are the most common malignancies reported. Overall incidence of malignancies in SNF (5.3%) is slightly lower than that of NF-1 (7.0%).10
In the reported family, father had three lesions, one of the daughtesr had two lesions and the other had multiple lesions, progressive disease associated with episodes of pain. Thus, there was variable severity of SNF in all three of them. Pain and physical disfigurement prompted our index case to seek medical advice. Many asymptomatic cases are missed due to underreporting.
Hereditary transmission of SNF can possibly be explained by familial increased susceptibility of somatic mutations at NF-1 gene locus.11 Role of consanguinity also remains to be ascertained.
Patient’s perspective.
I (index case) did not take any medical consultation for my lesions initially as I thought it to be running in my family since my father as well as my sister had similar lesions. What is different in my case is the severe pain that I feel intermittently and also the incresing number of lesion. With the medicines my pain is better now but at the moment I am not considering surgery as an option as the resultant deformity could be more disfiguring.
Learning points.
Segmental neurofibromatosis (SNF) is considered to be a result of mosaicism.
Hereditary transmission is possibly explained by increased susceptibility of mutations at neurofibromatosis gene loci.
SNF can have hereditary transmission with variable severity in different family members.
All cases should be completely evaluated to find out obscure family members suffering from minimal disease to increase the database for genetic evaluation.
Footnotes
Contributors: This is to state that RJ contributed in planning and conception of this case series. NS was involved in conception and conduct of this case series. KR has contributed in patient care and management. RJ, NS and KR have contributed in drafting of the manuscript and revisions with intellectual inputs and have approved the final version to be submitted for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Maldonado Cid P, Sendagorta Cudós E, Noguera Morel L, et al. Bilateral segmental neurofibromatosis diagnosed during pregnancy. Dermatol Online J 2011;17:6. [PubMed] [Google Scholar]
- 2. Riccardi VM. Neurofibromatosis: clinical heterogeneity. Curr Probl Cancer 1982;7:1–34. 10.1016/S0147-0272(82)80016-0 [DOI] [PubMed] [Google Scholar]
- 3. Gammel JA. Localized neurofibromatosis. Arch Dermatol Syphiol 1931;24:712–3. [Google Scholar]
- 4. Crowe FW, Schull WJ, Neel JVA. Clinical, pathological and genetic study of multiple neurofibromatosis. Springfield, IL: Charles C. Thomas, 1956. [Google Scholar]
- 5. Jankovic I, Kovacevic P, Visnjic M, et al. A unique case of hereditary bilateral segmental neurofibromatosis on the face. An Bras Dermatol 2012;87:895–8. 10.1590/S0365-05962012000600012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tinschert S, Naumann I, Stegmann E, et al. Segmental neurofibromatosis is caused by somatic mutation of the neurofibromatosis type 1 (NF1) gene. Eur J Hum Genet 2000;8:455–9. 10.1038/sj.ejhg.5200493 [DOI] [PubMed] [Google Scholar]
- 7. McLimore H, McCaughey C, Vanness E. A case of late-onset segmental neurofibromatosis. WMJ 2014;113:72–3. [PubMed] [Google Scholar]
- 8. Oguzkan S, Cinbis M, Ayter S, et al. Familial segmental neurofibromatosis. J Child Neurol 2004;19:392–4. 10.1177/088307380401900515 [DOI] [PubMed] [Google Scholar]
- 9. Hager CM, Cohen PR, Tschen JA. Segmental neurofibromatosis: case reports and review. J Am Acad Dermatol 1997;37:864–9. 10.1016/S0190-9622(97)80013-8 [DOI] [PubMed] [Google Scholar]
- 10. Sloan JB, Fretzin DF, Bovenmyer DA. Genetic counseling in segmental neurofibromatosis. J Am Acad Dermatol 1990;22:461–7. 10.1016/0190-9622(90)70065-P [DOI] [PubMed] [Google Scholar]
- 11. Roth RR, Martines R, James WD. Segmental neurofibromatosis. Arch Dermatol 1987;123:917–20. 10.1001/archderm.1987.01660310085020 [DOI] [PubMed] [Google Scholar]