Abstract
Background
Acute anterior shoulder dislocation, which is the most common type of dislocation, usually results from an injury. Subsequently, the shoulder is less stable and is more susceptible to re‐dislocation or recurrent instability (e.g. subluxation), especially in active young adults. After closed reduction, most of these injuries are treated with immobilisation of the injured arm in a sling or brace for a few weeks, followed by exercises. This is an update of a Cochrane Review first published in 2006 and last updated in 2014.
Objectives
To assess the effects (benefits and harms) of conservative interventions after closed reduction of traumatic anterior dislocation of the shoulder. These might include immobilisation, rehabilitative interventions or both.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register, the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL, PEDro and trial registries. We also searched conference proceedings and reference lists of included studies. Date of last search: May 2018.
Selection criteria
We included randomised or quasi‐randomised controlled trials comparing conservative interventions with no treatment, a different intervention or a variant of the intervention (e.g. a different duration) for treating people after closed reduction of a primary traumatic anterior shoulder dislocation. Inclusion was regardless of age, sex or mechanism of injury. Primary outcomes were re‐dislocation, patient‐reported shoulder instability measures and return to pre‐injury activities. Secondary outcomes included participant satisfaction, health‐related quality of life, any instability and adverse events.
Data collection and analysis
Both review authors independently selected studies, assessed risk of bias and extracted data. We contacted study authors for additional information. We pooled results of comparable groups of studies. We assessed risk of bias with the Cochrane 'Risk of bias' tool and the quality of the evidence with the GRADE approach.
Main results
We included seven trials (six randomised controlled trials and one quasi‐randomised controlled trial) with 704 participants; three of these trials (234 participants) are new to this update. The mean age across the trials was 29 years (range 12 to 90 years), and 82% of the participants were male. All trials compared immobilisation in external rotation (with or without an additional abduction component) versus internal rotation (the traditional method) following closed reduction. No trial evaluated any other interventions or comparisons, such as rehabilitation. All trials provided data for a follow‐up of one year or longer; the commonest length was two years or longer.
All trials were at some risk of bias, commonly performance and detection biases given the lack of blinding. Two trials were at high risk of selection bias and some trials were affected by attrition bias for some outcomes. We rated the certainty of the evidence as very low for all outcomes.
We are uncertain whether immobilisation in external rotation makes a difference to the risk of re‐dislocation after 12 months' or longer follow‐up compared with immobilisation in internal rotation (55/245 versus 73/243; risk ratio (RR) 0.67, 95% confidence interval (CI) 0.38 to 1.19; 488 participants; 6 studies; I² = 61%; very low certainty evidence). In a moderate‐risk population with an illustrative risk of 312 per 1000 people experiencing a dislocation in the internal rotation group, this equates to 103 fewer (95% CI 194 fewer to 60 more) re‐dislocations after immobilisation in external rotation. Thus this result covers the possibility of a benefit for each intervention.
Individually, the four studies (380 participants) reporting on validated patient‐reported outcome measures for shoulder instability at a minimum of 12 months' follow‐up found no evidence of a clinically important difference between the two interventions.
We are uncertain of the relative effects of the two methods of immobilisation on resumption of pre‐injury activities or sports. One study (169 participants) found no evidence of a difference between interventions in the return to pre‐injury activity of the affected arm. Two studies (135 participants) found greater return to sports in the external rotation group in a subgroup of participants who had sustained their injury during sports activities.
None of the trials reported on participant satisfaction or health‐related quality of life.
We are uncertain whether there is a difference between the two interventions in the number of participants experiencing instability, defined as either re‐dislocation or subluxation (RR 0.84, 95% CI 0.62 to 1.14; 395 participants, 3 studies; very low certainty evidence).
Data on adverse events were collected only in an ad hoc way in the seven studies. Reported "transient and resolved adverse events" were nine cases of shoulder stiffness or rigidity in the external rotation group and two cases of axillary rash in the internal rotation group. There were three "important" adverse events: hyperaesthesia and moderate hand pain; eighth cervical dermatome paraesthesia; and major movement restriction between 6 and 12 months. It was unclear to what extent these three events could be attributed to the treatment.
Authors' conclusions
The available evidence from randomised trials is limited to that comparing immobilisation in external versus internal rotation. Overall, the evidence is insufficient to draw firm conclusions about whether immobilisation in external rotation confers any benefit over immobilisation in internal rotation.
Considering that there are several unpublished and ongoing trials evaluating immobilisation in external versus internal rotation, the main priority for research on this question consists of the publication of completed trials and the completion and publication of ongoing trials. Meanwhile, evaluation of other interventions, including rehabilitation, is warranted. There is a need for sufficiently large, good‐quality, well‐reported randomised controlled trials with long‐term follow‐up. Future research should aim to determine the optimal immobilisation duration, precise indications for immobilisation, optimal rehabilitation interventions, and the acceptability of these different interventions.
Keywords: Adult, Female, Humans, Male, Conservative Treatment, Immobilization, Immobilization/adverse effects, Immobilization/methods, Joint Instability, Joint Instability/etiology, Randomized Controlled Trials as Topic, Shoulder Dislocation, Shoulder Dislocation/complications, Shoulder Dislocation/therapy
Plain language summary
Non‐surgical management after non‐surgical repositioning of traumatic anterior dislocation of the shoulder
Background
Acute anterior shoulder dislocation is an injury in which the top end of the upper arm bone is pushed out of the joint socket in a forward direction. Afterwards, the shoulder is less stable, and prone to either partial or complete re‐dislocation, especially in active young adults. Initial treatment involves putting the joint back in place. This is called ‘closed reduction’ when it is done without surgery. Subsequent treatment is often conservative (non‐surgical) and usually involves a period of immobilisation of the injured arm in a sling or brace, followed by exercises.
Review question
What are the benefits and harms of different conservative interventions for treating people after closed reduction of a primary traumatic anterior shoulder dislocation?
This is an update of a review that was first published in 2006 and last updated in 2014. We reviewed the evidence from clinical studies comparing any conservative intervention (e.g. immobilisation, rehabilitation) versus no treatment or a different intervention, or comparing different variants of an intervention (e.g. different duration). The primary outcomes of interest were re‐dislocation, patient‐reported shoulder instability measures (usually questionnaires) and return to pre‐injury activities. Further outcomes of interest included patients’ satisfaction with the intervention, health‐related quality of life and adverse events.
Search date
We conducted the searches of healthcare literature for this review in May 2018.
Study characteristics
We identified three new relevant studies in this update. In total, this review now includes seven studies with 704 participants. Most of the participants (82%) were male; the average age across the studies was 29 years (range 12 to 90 years). All of the studies investigated just one comparison: immobilisation in external rotation (when the arm is orientated outwards with the forearm away from the chest) versus immobilisation in internal rotation (the usual sling position, where the arm rests against the chest) following closed reduction. Participants were followed over different lengths of time; the most common duration was two years or longer.
Key results
We are uncertain whether immobilisation in external rotation makes a difference to the risk of re‐dislocation at one‐year or more follow‐up compared with immobilisation in internal rotation.
None of the four studies reporting on patient‐reported outcome measures for shoulder instability at a minimum of one‐year follow‐up found evidence of any important difference between the two interventions.
We are uncertain of the relative effects of the two methods of immobilisation on resumption of pre‐injury activities or sports. One study found no evidence of a difference between interventions in the return to pre‐injury activity of the affected arm. Two other studies found greater return to sports in the external rotation group in a small group of participants who had sustained their injury during sports activities.
None of the trials reported on participant satisfaction or health‐related quality of life. We are uncertain whether there is a difference between the two interventions in the number of participants experiencing instability, defined as either re‐dislocation or subluxation (a partial dislocation).
The reporting of adverse events (complications) was unsatisfactory. There were reports of nine cases of short‐term shoulder stiffness in the external rotation group and two cases of under‐arm rash in the internal fixation group. There were three more serious adverse events: abnormal sensitivity and hand pain; abnormal sensation such as tingling in the little finger and along to the elbow; and major movement restriction. It was unclear to what extent these three adverse events could be attributed to the treatment.
Certainty of the evidence
We rated the certainty of the evidence as very low for all outcomes. This was mainly because there were not enough data and we were unsure how reliable the results were from the individual studies. Thus we are uncertain about the estimates of effect.
Conclusions
Overall, the current evidence is insufficient to inform the choice of immobilisation in external versus internal rotation. There is no evidence to inform on any other conservative interventions following closed reduction of traumatic anterior dislocation of the shoulder.
Summary of findings
Summary of findings for the main comparison. Immobilisation in external rotation versus immobilisation in internal rotation following closed reduction of traumatic anterior dislocation of the shoulder.
| Immobilisation in external rotation versus immobilisation in internal rotation following closed reduction of traumatic anterior dislocation of the shoulder | ||||||
| Patient or population: patients undergoing conservative management after closed reduction of traumatic anterior dislocation of the shoulder Setting: splints or slings applied in emergency departments or clinics Intervention: immobilisation of arm in external rotation Comparison: immobilisation of arm in internal rotation | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Immobilisation in internal rotation | Immobilisation in external rotation | |||||
| Re‐dislocation Follow‐up: at 12 months or longer | Low riska | RR 0.67 (0.38 to 1.19) | 488 (6 RCTs) | ⊕⊝⊝⊝ VERY LOWd,e | ||
| 248 per 1000 | 167 per 1000 (95 to 296) | |||||
| Moderate riskb | ||||||
| 312 per 1000 | 209 per 1000 (119 to 372) | |||||
| High riskc | ||||||
| 417 per 1000 | 280 per 1000 (159 to 497) | |||||
| Validated patient‐reported outcome measures for shoulder disabilityf Follow‐up more than 24 months | See comments | See comments | ‐ | 380 (4 RCTs) | ⊕⊝⊝⊝ VERY LOWe,g | 3 of the 4 trials reported no or little difference in scores. 1 trial (97 participants) reported a difference favouring external rotation in the WOSI scoref: MD −43.20, 95% CI −72.38; −14.02. This, however, is unlikely to be clinically important. |
| Resumption of pre‐injury activities | See comments | See comments | ‐ | 347 (3 RCTs) | ⊕⊝⊝⊝ VERY LOWe,h | 1 study (169 participants) found no evidence of a difference between interventions in the return to pre‐injury activity of the affected arm (RR 1.02, 95% CI 0.80 to 1.29). 2 studies (178 participants) reported on return to sports for the subgroup of participants who had been sports active; both results were in favour of external rotation. |
| Participant satisfaction with the intervention | See comments | See comments | ‐ | ‐ | ‐ | Outcome not reported |
| Quality of life | See comments | See comments | ‐ | ‐ | ‐ | Outcome not reported |
| Any instability: re‐dislocation or subluxation, composite outcome Follow‐up at 12 months or longer | 419 per 1000i | 352 per 1000 (260 to 478) | RR 0.84 (0.62 to 1.14) | 395 (3 RCTs) | ⊕⊝⊝⊝ VERY LOWe,j | 2 other studies (135 participants) provided very low certainty evidence on instability defined as re‐dislocation and/or a positive apprehension test. Although favouring external fixation (RR 0.28, 95% CI 0.14 to 0.57), we judged the evidence at very low certaintyk (downgraded for risk of bias, imprecision and indirectness reflecting the suboptimal nature of this outcome). |
| Adverse events | See comments | See comments | ‐ | 645 (7 RCTs) | ⊕⊝⊝⊝ VERY LOWl | Adverse events were mostly not prespecified as an outcome, i.e. reported ad hoc. We split these into 'transient and resolved adverse events' and 'important' (serious) adverse events. In the first category, there were 9 cases of shoulder stiffness or rigidity in the external rotation group versus 2 cases of axillary rash in the internal fixation group. There were 3 'important' adverse events: hyperaesthesia and moderate hand pain; eighth cervical dermatome paraesthesia; and major movement restriction between 6 and 12 months. It was not clear to what extent the adverse events could be attributed to the treatment. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RR: risk ratio; WOSI: Western Ontario Shoulder Instability Index | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
a Assumed low risk based on the lowest control group (internal rotation group) risk out of the 6 contributing studies b Assumed moderate risk based on the median control risk of the 6 contributing studies c Assumed high risk based on the highest control group risk out of the 6 contributing studies d Downgraded by 1 level for risk of bias (mainly performance, detection and selection biases), 1 level for inconsistency (substantial heterogeneity: I² = 61%, Chi² = 0.002) and 1 level for imprecision (low number of events, CI overlapping no effect) e Publication bias was graded as undetected for all outcomes. We identified 5 studies evaluating immobilisation in external versus internal rotation that have been completed but that have yet not been published. While this suggests a risk of publication bias, we judged that the information available to us was insufficient for downgrading f 3 trials reported results based on the WOSI (range from 0 (least disability) to 2100 (worst disability)). 1 trial used the OSI (range from 0 (worst impairment) to 48 (least impairment)) g Downgraded by 1 level for risk of bias (mainly performance, detection and selection biases), 1 level for inconsistency (marked unexplainable difference of the effect of 1 study to that of the other studies) and 1 level for imprecision (low number of participants; 3 of the 4 studies found either no or only a small effect that was either reportedly non‐significant or had a CI including overlapping no effect) h Downgraded by 1 level for risk of bias (mainly performance, detection, selection biases), 1 level for inconsistency (difference in effect of the 3 studies ranging from a large effect favouring immobilisation in external rotation to no effect) and 1 level for imprecision (low number of outcome events; CIs of 3 of the 4 estimates overlapping no effect) i Assumed risk based on the median control risk of the 3 contributing studies j Downgraded by 2 levels for risk of bias (mainly performance, detection, selection and attrition biases) and 1 level for imprecision (low number of events; CIs for 2 of the 3 estimates overlapping no effect) k Downgraded by 2 levels for risk of bias (mainly performance, detection, selection and attrition biases), 1 level for imprecision (very low number of events) and 1 level for indirectness (suboptimal outcome measure) l Downgraded by 2 levels for risk of bias (mainly performance, detection, selection and attrition biases), 1 level for imprecision (very low number of outcome events and small study sample sizes; no CIs were reported) and 1 level for indirectness (poor definition and reporting of most adverse events)
Background
Description of the condition
Dislocation of the shoulder occurs when the head of the humerus (the top of the upper arm bone that forms the ball of the shoulder joint) is displaced out of the glenohumeral (shoulder) joint. The extent of dislocation varies from subluxation (partial dislocation) to full dislocation (where the joint surfaces completely lose contact). It is usually diagnosed by a combination of history, physical examination findings and imaging — most often radiography (x‐ray), but more rarely some other imaging modality such as magnetic resonance imaging (MRI). The direction of dislocation varies, but in most primary (first‐time) dislocations, the head of the humerus is displaced anteriorly (forwards) in relation to the glenoid fossa (the socket of the shoulder joint). The cause is usually trauma, typically during contact sports in adolescents and younger adults. In older adults, dislocation may result from a fall from standing height.
The nature and extent of damage to the soft tissue surrounding the shoulder joint from a traumatic anterior dislocation vary, and may involve bony, cartilaginous, ligamentous as well as tendinous or muscular structures (Demehri 2017; Forsythe 2015). Common presentations include the Bankart lesion, characterised by damage to the anteroinferior part of the glenoid labrum (the fibrocartilage rim that deepens the joint socket) and the capsule surrounding the joint (Bankart 1938); and the Hill‐Sachs lesion, which involves a compression fracture of the humeral head, as well as damage to its overlying cartilage (Hill 1940).
Estimates of the incidence of traumatic anterior shoulder dislocation vary across the literature. A recent epidemiological overview of estimates of the incidence of shoulder dislocation in various countries reported incidences per 100,000 person years of 12.3 cases in Denmark, 23.1 cases in Canada, 23.9 cases in the USA, 27.5 cases in Sweden and 56.3 cases in Norway (Cameron 2017). Cameron 2017 reported the incidence is highest during the second and third decade of life, with a peak in the late teens and early twenties, and that it decreases with increasing age. Furthermore, the incidence is higher in males and in athletes. The proportion of males was 71.8% in a large US‐based epidemiological study including a total of 8940 shoulder dislocations (Zacchilli 2010).
Once dislocation has occurred, the shoulder is less stable and is more susceptible to re‐dislocation. Estimates of the rate of re‐dislocation vary considerably across the literature. Two recent systematic reviews, with different inclusion criteria and numbers of studies, of prognostic studies investigating risk factors in people after conservative management of a traumatic first‐time anterior shoulder dislocation reported an overall proportion of recurrent instability (re‐dislocation or recurrent subluxation) of 39% (range 4% to 74%) after a minimum follow‐up of one year (Olds 2015); and of 21% (range 19% to 88%) after a minimum follow‐up of two years (in Wasserstein 2016). Olds 2015 reported proportions of recurrent instability of 51% in people aged 15 to 20 years; 36% in people aged 21 to 40 years; 11% in people aged 41 to 60 years; and 10% in people aged 61 or older. Re‐dislocation mainly occurs within the first year; Wasserstein 2016 reported a mean (SD) of 10.8 (0.42) months for the first episode.
Both Olds 2015 and Wasserstein 2016 found sex, age and concomitant fractures of the greater tuberosity to be key prognostic factors for recurrent instability after a primary traumatic anterior shoulder dislocation. The risk of recurrent instability was reported to be 3.18 times (95% CI 1.28 to 7.89) more likely in males than females in Olds 2015; and 2.68 times (95% CI 1.66 to 4.31) more likely in males in Wasserstein 2016. Olds 2015 found people aged 40 years or under were 13.46 times (95% CI 5.25 to 34.49) more likely to suffer recurrent instability than those older than 40 years. In Wasserstein 2016, people under 40 years were 20 times (95% CI 10.0 to 33.3) more likely to suffer recurrent instability than those who were 40 or over. Conversely, people with a concomitant fracture of the greater humeral tuberosity were found to be 7.69 times (95% CI 3.33 to 16.67) less likely to have a recurrent instability in Olds 2015; and 3.85 times (95% CI 3.33 to 10.00) less likely in Wasserstein 2016. There was poorer quality and often inconsistent evidence for other factors across the studies in the reviews and also across the two reviews.
Description of the intervention
Traditionally, a non‐surgical (conservative) approach, comprising closed reduction, three to six weeks' immobilisation in a sling (i.e. in internal rotation) and a subsequent physiotherapy or physical therapy programme has been used for first time dislocations (O'Brien 1987). However, we note recent trends to earlier mobilisation and thus a shorter duration of immobilisation (e.g. Berendes 2015). Moreover, a period of up to one week of immobilisation is proposed in a recent British (BESS/BOA) patient care pathway, which refers to evidence suggesting that the risk of re‐dislocation is not decreased with longer immobilisation (e.g. Paterson 2010).
Regarding the immobilisation position, recent years have seen much interest in an alternative to the traditional (internal rotation) immobilisation method, whereby the shoulder is immobilised in external (outward) rotation using a custom‐made (Itoi 2003) or commercially manufactured (Sullivan 2007) brace. The interest in immobilisation of the arm in external rotation traces back to work by Itoi and colleagues (Itoi 1999; Itoi 2001; Itoi 2003; Itoi 2007), who found that the separation of the labrum from the glenoid (as present with a Bankart lesion) was significantly reduced when the shoulder was positioned in external rotation compared with the traditional internal rotation (sling) position. Itoi postulated that this may enhance the healing of the Bankart lesion and reduce the risk of recurrent instability. He later suggested that the addition of an abduction component may further improve outcomes (Itoi 2015). Limited published data are available on the use of immobilisation in external rotation in clinical practice. However, the findings of two published surveys, conducted among orthopaedic surgeons in the Netherlands and Germany (Berendes 2015 and Balke 2016 respectively), indicate considerable variability. Berendes 2015 found that only 3% of the participating surgeons immobilised the shoulder in external rotation, whereas 97% immobilised it in internal rotation. Balke 2016 found that 15% of the participating surgeons always immobilised the shoulder in external rotation, whereas 46% did not use this position at all and 39% advised on immobilisation in external or internal rotation individually.
Physiotherapy or rehabilitation, typically started after the immobilisation period, usually entails advice, education and an exercise‐based regimen (typically addressing stability, coordination and strength of the shoulder, shoulder girdle, upper spinal muscles, or combinations of these) aimed at restoring normal shoulder function. This may be supplemented by manual therapy, soft tissue mobilisations and physical modalities.
Surgical intervention has generally been reserved for cases of chronic recurrence or instability. However, a Cochrane Review (Handoll 2004; updated in 2009) comparing surgical with non‐surgical treatment found some limited evidence supporting primary surgery for young adults, usually male, engaged in highly demanding physical activities who have sustained their first acute traumatic shoulder dislocation.
Our review considers the various approaches to post‐reduction conservative treatment, such as the duration and position of sling immobilisation, the modalities used, and the timing and extent of physiotherapy and rehabilitation interventions.
How the intervention might work
The aim of treatment for anterior dislocation is to restore a functional, painless and stable shoulder. The choice of treatment approach will be influenced by patient age and previous history of dislocation, occupation, level of activity, general health and ligamentous laxity and by expectations of patient adherence to a prescribed therapeutic regimen.
The aim of immobilisation is to allow healing. In this connection, some MRI and cadaveric studies of Bankart lesions have shown better and firmer repositioning of the peeled‐away capsule when the shoulder is externally rotated than when it is internally (inwardly) rotated — the position naturally imposed by a sling (Dymond 2011; Itoi 2001; Kitamura 2005; Liavaag 2009; Miller 2004; Moxon 2010; Pennekamp 2006; Seybold 2009; Siegler 2010). This has kindled and sustained interest in the possibility that immobilisation in external rotation may improve healing, and consequently outcomes, in comparison with the traditional approach. However any immobilisation has potential disadvantages, and there is an argument for shortening its duration (Paterson 2010) or forgoing it altogether (Hovelius 2008) to allow early restoration of movement, especially in the middle‐aged to elderly, who are susceptible to stiffness and frozen shoulder as a result of immobilisation (Robinson 2012) but are less prone to re‐dislocation than the young (Wasserstein 2016).
Finally, various exercise interventions might theoretically increase functional stability by restoring proprioception (spatial awareness) in the shoulder joint and by retraining muscles to help maintain joint congruency (Karatsolis 2006); while motion‐limiting braces might prevent re‐dislocation by restricting shoulder movement in vulnerable directions (Murray 2013).
Why it is important to do this review
This is an update of a Cochrane Review last updated in 2014 (Hanchard 2014); this included only four trials, all of which compared the immobilisation positions of external and internal rotation. It concluded that "the evidence is insufficient to demonstrate whether immobilisation in external rotation confers any benefit over immobilisation in internal rotation". Moreover, Hanchard 2014 pointed to a number of unpublished and ongoing trials that could inform this comparison, and to the continuing need for evidence to inform other aspects of conservative management for this injury. Since then, further trials evaluating immobilisation in external versus internal rotation have been published and there are also several registered studies. Questions still surround other aspects of immobilisation (including the timing of application and duration, position and whether any immobilisation is better than none at all, and rehabilitation (its general effectiveness, its relative effectiveness across different settings and the relative effectiveness of different packages and modes of delivery) and motion‐limiting braces. These considerations illustrated the need for an updated review.
Objectives
To assess the effects (benefits and harms) of conservative interventions after closed reduction of traumatic anterior dislocation of the shoulder. These might include immobilisation, rehabilitative interventions or both.
Methods
Criteria for considering studies for this review
Types of studies
We considered any randomised or quasi‐randomised controlled trials (the allocation of the latter by, for example, hospital record number or date of birth) evaluating conservative treatment after anterior dislocation of the shoulder.
Types of participants
Individuals who have undergone closed reduction for traumatic anterior dislocation of the shoulder. Ideally, the acute anterior shoulder dislocation should have been confirmed by physical examination and radiography or another imaging modality such as MRI. We intended to consider the potential for misdiagnosis, such as a missed proximal humeral fracture, in trials in which the method of diagnosis was unspecified or in which diagnosis was based on physical examination alone. We included trials including participants with concomitant injuries that are often associated with anterior shoulder dislocation, such as a fracture of the greater tuberosity of the humerus or a Bankart lesion, as long as treatment focused on the dislocation rather than on the concomitant injury.
Although we stated that we would include individuals of any age, we correctly anticipated finding no trials focused specifically on the management of traumatic anterior dislocation in children.
We excluded trials focusing on the treatment of participants with non‐traumatic or habitual dislocations, or concomitant fractures such as proximal humeral fractures involving the surgical neck, or multiple trauma; and those focusing on management of neurovascular complications or postsurgical management. We stipulated that trials with mixed populations involving any one indication of the above would be considered for inclusion if the proportion of the latter (e.g. atraumatic dislocation) was clearly defined for each treatment group and was clearly small (< 10%), or if separate data for acute traumatic anterior dislocation were provided.
Types of interventions
We planned the following.
To assess whether a difference exists between outcomes of different methods (including arm position) and durations (including none or intermittent) of postreduction immobilisation. However, we planned to exclude trials comparing variants (e.g. duration, position) or supplements to particular immobilisation techniques unless the general effectiveness of the method had been established.
To assess whether a difference exists between outcomes of the provision of rehabilitation intervention (of any kind) versus no intervention. Examples of rehabilitation interventions include advice and education, active and passive mobilisation, proprioception and stabilisation exercises, scapular setting and trunk stability exercises. These may be used in combination or individually and may be applied in various ways and settings. Although these interventions are potentially available to all patients allocated the rehabilitation intervention, their actual application may vary according to the perceived needs of individual patients. We aimed to assess this separately for the provision of any rehabilitation (a) during immobilisation, and (b) after immobilisation.
To assess whether a difference exists between outcomes of different types of rehabilitation interventions. Comparisons would have included different single modalities or different combinations of rehabilitation modalities. However, we planned to exclude trials comparing different techniques, timing (duration, frequency) and intensity of single rehabilitation modalities until the effectiveness of the modality itself had been established. We also would have excluded trials evaluating pharmacological interventions and trials testing interventions aimed solely at pain relief.
To assess whether a difference exists between outcomes of different methods of delivering/providing various rehabilitation interventions. Comparisons would have included supervised therapy versus home exercises, different methods of supervised therapy (e.g. individual versus group instruction) and differences in the frequency and duration of rehabilitation. In the first instance, we did not plan to include comparisons of rehabilitation intervention delivered by individual professionals (e.g. doctors, physiotherapists, occupational therapists) with different levels or backgrounds of expertise or training.
For this review update we selected the following four key comparisons that we considered to reflect priority questions.
Arm position during immobilisation: immobilisation in external rotation versus immobilisation in internal rotation (comparison already established in Hanchard 2014).
Use and duration of immobilisation: no or limited‐duration immobilisation (≤ 1 week) versus ‘standard’ duration (typically 3 weeks) (comparison proposed in Hanchard 2014). The underlying rationale for the comparison is likely to vary according to the participant group and extent of injury. Thus, we considered other comparisons of duration depending on the underlying rationale.
Provision of formal rehabilitation, typically post immobilisation: no formal rehabilitation (e.g. advice, education, home exercise sheet only) versus formal rehabilitation. We defined ‘formal rehabilitation’ as a therapeutic intervention typically provided by a health professional (e.g. a physiotherapist) other than the treating medical doctor, that typically includes demonstration and provision of supervised home exercises with or without adjunctive passive modalities over a certain period of time.
Preferable timing of provision of formal rehabilitation: during and following immobilisation versus following immobilisation only. We defined 'formal rehabilitation' as a therapeutic intervention provided by a health professional other than the treating medical doctor, i.e. typically by a physiotherapist, and typically including supervised exercises with or without adjunctive passive modalities.
Types of outcome measures
We sought the following outcome measures.
Primary outcomes
Re‐dislocation: separation of the joint requiring reduction and, ideally, verified.
Validated patient‐reported outcome measures (PROMs) for shoulder instability (e.g. Oxford Shoulder Instability Score (Dawson 1999), Western Ontario Shoulder Instability Index (WOSI) (Kirkley 1998)).
Resumption of pre‐injury activities (work, sport, recreational activities) (yes or no).
Secondary outcomes
Participant satisfaction with the intervention
Validated health‐related quality of life outcome measures (e.g. EQ‐5D (standardised measure of health outcome), Short Form‐36 (SF‐36)).
Any instability: subluxation (separation of the joint not requiring reduction) or subjective instability, either individually or grouped with dislocation as a composite outcome.
Important adverse events (not including re‐dislocation or instability) that were plausibly attributable to post‐reduction management (e.g. persistent pain, frozen shoulder). Other adverse events were to be reported narratively.
In addition, we intended to take note of any reports of service utilisation or resource use, for instance length of hospital stay, outpatient attendance and the provision and nature of physiotherapy; and participants' adherence to their allocated interventions.
We excluded studies that did not report on patient‐relevant clinical outcomes but instead reported solely on non‐clinical outcomes (e.g. radiological outcomes) as their link with clinical outcomes is largely unclear; i.e. not sufficiently established.
Timing of outcome measurement
Approximately one‐third of re‐dislocations occur within three months of the initial dislocation, and a further third between three and 12 months (Rhee 2009). We therefore proposed organising outcomes into the following time frames, with greatest importance attached to long‐term reporting.
Short‐term: up to and including three months following dislocation
Medium‐term: greater than three months and up to and including 12 months following dislocation
Long‐term: greater than 12 months following dislocation
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (May 2018), the Cochrane Central Register of Controlled Trials (CENTRAL; 2018, Issue 4) in the Cochrane Library (searched 21 May 2018), MEDLINE including Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE and Versions(R) (1946 to 16 May 2018), Embase (1974 to 2018 Week 21), CINAHL (1982 to 21 May 2018), PEDro (Physiotherapy Evidence Database) (1929 to May 2018) and OTseeker (Occupational Therapy Systematic Evaluation of Evidence Database) (inception to November 2012). We also searched the WHO International Clinical Trials Registry Platform (22 May 2018), ClinicalTrials.gov (22 May 2018) and the UK National Research Register (2005, Issue 3, now archived) for ongoing and recently completed trials. For this update, the searches were limited to 2013 onwards. We applied no language restrictions.
In MEDLINE (Ovid Web), the subject‐specific strategy was combined with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials, and this was modified for use in other databases (Lefebvre 2011). Search strategies for CENTRAL, MEDLINE, Embase, CINAHL and PEDro can be found in Appendix 1. Details of the search strategies used previously are published in Hanchard 2014 and Handoll 2006.
Searching other resources
We checked reference lists of articles. We searched the conference proceedings of the British Elbow and Shoulder Society (BESS), published in Shoulder & Elbow (2013 to 2017). We handsearched conference proceedings published in Orthopaedic Proceedings, a supplement to The Bone and Joint Journal (January 2013 to May 2018). We also checked the lists of ongoing studies and studies awaiting classification in Hanchard 2014 for any publications of these studies.
Data collection and analysis
Selection of studies
Both review authors (CB, CMR) independently assessed potentially eligible trials for inclusion; we resolved all disagreements through discussion. Titles of journals, names of authors and names of supporting institutions were not masked at any stage.
Data extraction and management
Both review authors independently extracted data. We piloted the date‐extraction form on an excluded study. We resolved any disagreement through discussion.
Assessment of risk of bias in included studies
We assessed risk of bias independently, without masking the source and authorship of trial reports. We piloted the assessment form on one trial. Between‐rater consistency in assessment was checked by one review author (CB) at data entry; and we resolved all disagreements by discussion. We used the Cochrane 'Risk of bias' tool (Higgins 2011): this tool incorporates assessment of randomisation (sequence generation and allocation concealment), blinding (of participants and of treatment providers), blinding of outcome assessment, completeness of outcome data, selection of outcomes reported and other sources of bias. Among these other sources we considered discrepancies in the level of skill or care with which compared interventions were applied (performance bias) and commercial sponsorship (because of the potential for reporting bias). In this update, in line with the stated intention in Hanchard 2014, we initially intended to assess risk of bias for objective outcomes (e.g. re‐dislocation) and subjective outcomes (e.g. PROMs) separately in our assessment of blinding of outcome assessment and completeness of outcome data. However, we changed this approach and assessed these two domains separately for each reported outcome instead.
Measures of treatment effect
When available and appropriate, we present quantitative data for outcomes listed in the inclusion criteria graphically. We calculated risk ratios (RRs) and 95% confidence intervals (CIs) for dichotomous outcomes. We calculated mean differences (MDs) and 95% CIs for continuous outcomes.
Unit of analysis issues
We were alert to the remote possibility of unit of analysis issues in the included studies but in the event we identified none. One participant in Chan 2018 was included twice: they experienced two shoulder dislocations, one in each shoulder, at an interval of three years (additional information provided by contact author). We considered the potential impact of this single case on the results was negligible.
Dealing with missing data
We approached study authors for missing data by email. If we requested answers to more than a few questions, we provided a pro forma to ensure clarity and to minimise the burden on trial authors. We did not impute missing data.
Assessment of heterogeneity
We tested heterogeneity between comparable trials using a standard Chi² test; this we considered statistically significant at a P value of less than 0.1. When we noted some indication of heterogeneity, from visual inspection of the results or based on results of the Chi² test, we also quantified heterogeneity/inconsistency using the I² statistic (Higgins 2003). We interpreted this as follows, according to guidance in Section 9.5.2, Higgins 2011.
0% to 40%: might not be important
30% to 60%: may represent moderate heterogeneity
50% to 90%: may represent substantial heterogeneity
75% to 100%: represents considerable heterogeneity
Assessment of reporting biases
If a meta‐analysis of a key outcome had included more than 10 studies, we would have considered exploring the potential for publication bias by generating a funnel plot. We considered the presence and number of completed but yet unpublished trials as an additional potential source of publication bias, but judged that the available information was too limited to allow for a clear judgement.
Data synthesis
Where appropriate, we pooled results of comparable studies using both fixed‐effect and random‐effects models. We decided the choice of the model by careful consideration of the extent of heterogeneity and whether it could be explained, in addition to other factors, such as the number and size of included studies. We used 95% CIs throughout. We considered not pooling data where there was considerable heterogeneity (I² statistic value ≥ 75%) that could not be explained by the diversity of methodological or clinical features among trials. Where it was inappropriate to pool data, we present trial data in the analyses or tables for illustrative purposes and report these in the text.
Subgroup analysis and investigation of heterogeneity
We proposed, where possible, to undertake subgroup analyses by sex, as males are at much greater risk of re‐dislocation (Olds 2015; Wasserstein 2016). We also proposed to subgroup by age, using two thresholds: 20 years or younger versus 21 years or older; and 39 years or younger versus 40 years or older. We chose the former threshold because patients aged 21 years or younger are at much greater risk of re‐dislocation (Wasserstein 2016), and the latter because of the markedly increased susceptibility of patients older than 40 years to post‐immobilisation stiffness and secondary frozen shoulder (Robinson 2012). We further proposed to subgroup by presence (versus absence) of a concomitant fracture of the greater tuberosity of the humerus, as there is evidence of an association between the presence of a greater tuberosity fracture and a decreased risk of instability or recurrent re‐dislocation (Olds 2015; Wasserstein 2016); or of presence (versus absence) of another specific lesion resulting from the dislocation (e.g. a Bankart lesion). However, there were insufficient data to conduct most of these subgroup analyses. We also planned but did not carry out separate outcome analyses of (1) participants who were physically active compared with those who were more sedentary; (2) physically active young adults engaged in highly demanding physical activities who have sustained primary anterior dislocation compared with others; and (3) participants with a primary dislocation compared with those with a recurrent dislocation. We anticipated that any subgroup differences would be in terms of size of effect (quantitative interaction) rather than direction of effect (qualitative interaction).
We also considered conducting an exploratory subgroup analysis of trials in which immobilisation in external rotation had an abduction component versus those without (external rotation only).
To test for differences between subgroups, we planned to inspect the overlap of confidence intervals and to perform the test for subgroup differences available in Review Manager 5 software.
Sensitivity analysis
We intended to perform sensitivity analyses, when appropriate, to investigate various aspects of trial and review methodology. We intended to include, when data were available, examinations of the effects of (1) removing trials at high risk of selection bias from inadequate allocation concealment or at high risk of detection bias from lack of blinded outcome assessment; (2) conducting worst‐case analyses for trials with missing data; and (3) using fixed‐effect versus random‐effects models for pooling.
'Summary of findings' table and assessment of the certainty of the evidence
Where data were available, we proposed to produce a 'Summary of findings' table for each of the prespecified priority comparisons (see types of interventions) and all primary and secondary outcomes. We applied the GRADE approach to assess the certainty of the evidence related to each of the key outcomes listed in the Types of outcome measures (see Section 12.2; Schunemann 2011). We used the GRADE approach following guidance from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). However, as the outcome data for most outcomes could only be pooled to a very limited extent, we further considered recent guidance on the application of the approach to evidence when data have been summarised narratively rather than by meta‐analysis (Murad 2017).
Results
Description of studies
Results of the search
We carried out searches were carried out in May 2018 and covered the period between September 2013 and May 2018 (see Appendix 1). We screened a total of 918 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (1); CENTRAL (155), MEDLINE (146), Embase (275), CINAHL (221), PEDro (18), the WHO ICTRP (53) and ClinicalTrials.gov (49). We further found three potentially eligible studies from other sources (one through the searches for conference proceedings, one through handsearching for further information on an ongoing trial and one incidentally through a different search).
After removing duplicates, we reduced 918 records to 665. We examined the titles and abstracts of these records and discarded 650, leaving a total of 15 new records (including trial registrations) to examine in more detail. Where possible, we obtained full‐text copies of these potentially relevant records.
We attempted to contact the investigators of the unpublished trials, either listed as ongoing or awaiting classification in Hanchard 2014 or newly identified, for information on their current status (ACTRN12611001183976; ACTRN12616001241426; Chan 2018 (formerly Kelly 2011); Eshoj 2017; ISRCTN41070054; ISRCTN48254181; Miller 2007; Murray 2016 (formerly NCT01111500); NCT02197819; NCT00707018). We received responses in relation to four studies (ACTRN12611001183976; ACTRN12616001241426; Chan 2018; Murray 2016).
At this stage, we excluded seven records. We also excluded one formerly ongoing study that had been abandoned (ACTRN12611001183976). New reports or information resulted in the inclusion of three more trials (Chan 2018: formerly Kelly 2011, a study awaiting classification; Heidari 2014; and Whelan 2014: formerly Whelan 2008, a study awaiting classification). Two registered studies (ACTRN12616001241426; NCT02197819), one study reported in a published protocol (Eshoj 2017), and ARTISAN, a study reported in the UK National Institute for Health Research Health Technology Assessment Database (NIHR‐HTA), were added as ongoing studies. One previously ongoing study was moved to studies awaiting classification (Murray 2016, formerly NCT01111500). We linked any references pertaining to the same study under a single study ID.
There are now seven included trials (Chan 2018; Finestone 2009; Heidari 2014; Itoi 2007; Liavaag 2011; Taskoparan 2010; Whelan 2014); 17 excluded studies (including nine from the previous searches); five ongoing trials; and six studies awaiting classification.
A flow diagram summarising the study selection process for this update is shown in Figure 1.
1.

Study flow diagram for this update (2019)
Included studies
Full details of the individual studies are given in the Characteristics of included studies tables. These also include information about funding sources and declarations of interests. We attempted to contact the corresponding authors of the three newly included trials for additional information on specific aspects including outcome data (Chan 2018; Heidari 2014; Whelan 2014). We received responses from one of the authors of Chan 2018 (Dr Kieran Bentick, personal communication 1 September 2018). We did not receive responses from the authors of Heidari 2014 and Whelan 2014.
Study design
Of the seven parallel, two‐group included clinical trials, six were RCTs (Chan 2018; Finestone 2009; Heidari 2014; Itoi 2007; Liavaag 2011; Whelan 2014), and one was a quasi‐randomised trial (Taskoparan 2010).
Study setting
The seven trials were conducted in seven different countries. Chan 2018 was conducted in six NHS hospitals across England; Finestone 2009 in the Accident and Emergency Department of an Israeli university hospital; Heidari 2014 in the emergency department of a university‐affiliated hospital in Iran; Itoi 2007 in 12 hospitals across Japan; Liavaag 2011 in 13 hospital emergency departments in Norway; Taskoparan 2010 in an emergency department in Turkey; and Whelan 2014 in three university clinics in Canada.
Study size
The trials included 704 participants. Study size ranged from 33 participants in Taskoparan 2010 to 198 in Itoi 2007. Of note: Chan 2018 had aimed to recruit 160 participants, but stopped at 72 participants as the trial was discontinued early.
Participants
All participants had experienced a primary traumatic anterior dislocation of the shoulder reduced by various closed methods. Regarding the prevalence of concomitant injuries, all but one of the trials specified 'associated fractures of the shoulder' as an exclusion criterion; Taskoparan 2010 did not provide any information. Liavaag 2011 and Whelan 2014 specified the type of fractures and other injuries, including labral lesions, that were excluded (see Characteristics of included studies). None of the trials provided information about the prevalence and characteristics of concurrent injuries for their actual study samples.
Five studies evaluated mixed, general populations, without restrictions of age and sex. In Finestone 2009, all 51 participants were male, and 40 of these were soldiers. Liavaag 2011 limited inclusion to patients aged 16 to 40 years, and Heidari 2014 limited inclusion to patients aged 15 to 55 years. Of the 704 participants, 578 (82%) were male. The mean age of the participants across the trials was 29 years: these ranged from 20 years in Finestone 2009 to 37 years in Itoi 2007. Participant age ranged from 12 to 90 years; both extremes were reported in Itoi 2007.
Interventions
All seven included trials compared post‐reduction immobilisation of the affected arm in external rotation (the arm oriented outwards and the forearm away from the chest) versus immobilisation in internal rotation (the traditional sling arrangement, with the forearm rested across the abdomen). In Table 2, the key characteristics of the immobilisation treatment are summarised for each trial.
1. Key characteristics of the immobilisation treatment.
| Study | Start of immobilisation (post‐dislocation) | Duration of immobilisation | External rotation position | Type of braces and slings | Providers |
| Chan 2018 | within 5 days | 4 weeks | 30° + 30° abduction | external rotation brace: Smartsling, Ossur, Reykjavik, Iceland); internal rotation sling: Polysling, Mölnlycke Health Care, Gothenburg, Sweden) |
appropriately trained members of staff (surgeons, nurses or healthcare assistants) |
| Finestone 2009 | no information | 4 weeks | 15° to 20° | external rotation brace: (manufacturer unspecified); internal rotation sling: traditional internal rotation sling |
unclear |
| Heidari 2014 | presumably on the same day (patients presented within 6 hours) | 3 weeks | 10° + 15° abduction | external rotation brace: stabiliser brace with adjustable angle of abduction (body: hard polyethylene); presumably commercially manufactured but purpose‐designed; internal rotation sling: sling and swathe bandage |
unclear |
| Itoi 2007 | within 2 days (termed day 1 to 3) |
3 weeks | 10° | external rotation brace: a) wire‐mesh splint covered with sponge and a stockinette (until October 2003); b) prototype brace, Alcare, Tokyo, Japan (from November 2003); internal rotation sling: sling and swathe |
the treating surgeons |
| Liavaag 2011 | within 24 hours | 3 weeks | 15° | external rotation brace: 15° UltraSling ER; DonJoy, Vista, California); internal rotation sling: normal collar and cuff device or sling and swathe |
unclear |
| Taskoparan 2010 | on the same day | 3 weeks | 10° | external rotation brace: "specific splint fixated in 10 degrees external rotation and adduction" (polyethylene/thermoplastic); internal rotation sling: 1st day: "valpaeu bandaging"; from 2nd day: "waist‐assisted sling" |
unclear |
| Whelan 2014 | presumably within 7 days (patients were assessed within 7 days) |
4 weeks | 0° to 5° | external rotation brace: DonJoy (Vista, California) external rotation shoulder brace; internal rotation sling: traditional internal rotation sling |
certified orthopaedic technicians |
Timing of immobilisation
There was some variation in the commencement of immobilisation. In Liavaag 2011 and Taskoparan 2010 immobilisation commenced on the day of the dislocation; in Itoi 2007 within two days after dislocation; and in Whelan 2014 within five days after dislocation. Heidari 2014 and Whelan 2014 did not specify when treatment commenced, but presumably treatment commenced shortly after the assessment in these trials, which was within six hours after dislocation in Heidari 2014 and within seven days after dislocation in Whelan 2014.
Duration of immobilisation
The duration of immobilisation, whether internal or external rotation, was three weeks in Heidari 2014, Itoi 2007, Taskoparan 2010 and Liavaag 2011; and four weeks in Chan 2018, Finestone 2009 and Whelan 2014. Participants were mostly instructed to remove their brace or sling only for showering.
Types or brands of braces and slings
The trials used a variety of external rotation braces. Chan 2018,Liavaag 2011 and Whelan 2014 reported using commercial off‐the‐shelf braces and specified the specific brand or manufacturer, or both. Immobilisation in internal rotation was mostly done with a traditional sling or sling and swathe bandage.
Position of immobilisation
The degree of external rotation used varied from 0° to 5° in Whelan 2014; 10° in Heidari 2014, Itoi 2007 and Taskoparan 2010; 15° in Liavaag 2011; 15° to 20° in Finestone 2009; to 30° in Chan 2018. In two trials, the arm was additionally immobilised in abduction: 30° in Chan 2018 and 15° in Heidari 2014.
Provision of immobilisation
The providers of the braces and slings, and of the accompanying instructions, were unclear in four studies (Finestone 2009; Heidari 2014; Liavaag 2011; Taskoparan 2010). In Chan 2018, the braces and slings were provided "by appropriately trained members of staff" (i.e. usually by surgeons, nurses or healthcare assistants; additional information provided by the contact author); in Itoi 2007, by the treating surgeons; and in Whelan 2014 by certified orthopaedic technicians.
Post‐immobilisation treatment
In six of the seven included trials, treatment with immobilisation was followed by some form of rehabilitation for both groups. In Liavaag 2011, there was no mention of rehabilitation. Most of the trials provided only limited information about the post‐immobilisation treatment, and most did not specify parameters such as duration or frequency. Whelan 2014 was alone in reporting an overall duration of 16 weeks. Chan 2018 was alone in providing the physiotherapy protocol for their study as a supplement to their report, in which a staged approach to rehabilitation was outlined, which ranged from an initial four‐week "quiet time" to "late rehabilitation" after six weeks. In all trials reporting post‐immobilisation treatment, exercises were the key component. These were supervised by physiotherapists in four trials (Chan 2018; Finestone 2009; Heidari 2014; Whelan 2014), with no information available for Itoi 2007 and Taskoparan 2010).
Outcomes
Primary outcomes
Only Itoi 2007 did not report on re‐dislocation as a discrete outcome. It was not always clear how this outcome was assessed and confirmed in the other six trials: in two trials, Chan 2018 and Heidari 2014, the assessment was either completely or partly patient‐reported; with either no, or no mention of, verification through reference to medical records or further evaluation.
Four studies reported on one or more validated patient‐reported outcome measures for shoulder instability. Three trials used the Western Ontario Shoulder Instability Index (WOSI) (Heidari 2014; Liavaag 2011 ; Whelan 2014) and Chan 2018 used the Oxford Shoulder Instability Index (OSI).
Three studies reported on return to pre‐injury sport or activities (Heidari 2014; Itoi 2007; Liavaag 2011).
Secondary outcomes
None of the included studies reported on participant satisfaction or on generic health‐related quality of life measures (e.g. EQ‐5D or SF‐36).
Any instability, including subluxation or subjective instability, either individually or grouped with dislocation as a composite outcome, was reported in several ways. Itoi 2007 and Liavaag 2011 prespecified re‐dislocation or subluxation as a composite outcome; Liavaag 2011 also prespecified subluxation as a stand‐alone outcome. Whelan 2014 prespecified 'recurrent instability' as the primary outcome; results were reported separately for 'recurrent dislocation', 'recurrent instability' (recurrent dislocation or subluxation) and 'recurrent instability requiring surgical stabilization'. Both Heidari 2014 and Taskoparan 2010 reported the rate of patients with a positive apprehension test.
Although adverse events were mentioned in all of the reports, the trials did not appear to have a priori strategies for defining or collecting these data.
Other outcomes
Adherence was the only other outcome collected by the included studies. Definitions and measurements of adherence varied across the six trials reporting this outcome.
We made the post‐hoc decision to document two further outcomes with the 'other outcomes', because we considered these as of potential interest both to clinicians and researchers: 'difficulties with wearing the braces or slings' and 'surgery'. Although these outcomes may arguably be viewed as 'adverse events', we considered it more appropriate to document them separately. Chan 2018 provided a detailed account of difficulties with wearing the braces and slings. Four studies reported the rate of patients who underwent surgery during the study period (Chan 2018; Finestone 2009; Heidari 2014; Liavaag 2011) .
Follow‐up time points
Follow‐ups were conducted at various time points, and were mostly defined as post‐dislocation (Table 3). However, not all outcomes were reported for all pre‐specified follow‐up time points in all trials, and some trials reported outcomes across a wide period of time that extended considerably beyond their last set follow‐up time. Notably, Taskoparan 2010 provided a table that listed the results of individual participants at individual follow‐ups, ranging from 6 to 41 months and also did not specify when data were collected on re‐dislocation or on adverse events. For Whelan 2014, results are presented for "minimum 12 months' follow‐up", but not for the different follow‐up points.
2. Lengths of follow‐up in the included studies.
| Study | Final follow‐up | Comments on follow‐up |
| Chan 2018 | 24 months | Set follow‐up times: 3 months; 1 & 2 years post‐dislocation |
| Finestone 2009 | mean 33.4 months (range 24 to 48) | Set follow‐up times: 2 & 6 weeks; 3 & 6 months; 1, 2, 3 & 4 years post‐injury |
| Heidari 2014 | 24 months and 33 months | Set follow‐up times; 3 weeks post‐intervention; 24 months post‐dislocation (re‐dislocation); 33 months post‐dislocation (WOSI only) |
| Itoi 2007 | mean 25.6 months (range 24 to 30) | Set follow‐up times: 6 months; 1 & 2 years (presumably post‐initiation of immobilisation) |
| Liavaag 2011 | mean 29.1 months (range 24 to 54) | Set follow‐up times: 3 weeks (adherence data); 2 years post‐dislocation. |
| Taskoparan 2010 | mean 21 months (range 6 to 41) | Set follow‐up times: 6 months (function scores); 1 & 2 years (radiographs and MRI) Not specified for re‐dislocation and adverse events Individual patient data presented with follow‐up ranging from 6 to 41 months |
| Whelan 2014 | mean 25 months (range 12 to 43) | Set follow‐up times: 4 weeks and 3, 6, 12, 18 & 24 months post‐dislocation. However, results were presented for a minimum of 12 months |
Funding and conflicts of interest
Five trials reported their sources of funding (Chan 2018; Finestone 2009; Heidari 2014; Itoi 2007; Whelan 2014); one stated that no funding was received (Liavaag 2011); and one did not provide any information about funding (Taskoparan 2010).
None of the trials explicitly declared any conflicts of interest. Six studies declared that there were no or at least no financial conflicts of interest while Taskoparan 2010 did not provide any information about conflicts of interest.
Further details about the funding and conflicts of interest are given in the Characteristics of included studies table.
Excluded studies
Fifteen of the 17 excluded studies or articles were excluded mainly as the result of insufficient information and lack of response from study authors (Harper 2000; Kiviluoto 1980; Staply 2002; Wakefield 2001) or failure to meet our selection criteria (Blanchard 2015; Chutkan 2012; Hovelius 1983; Hutchinson 2013; Itoi 2015; Königshausen 2014; Lacy 2015; McCarty 2014; Momenzadeh 2015; Whelan 2010; Xu 2003). Momenzadeh 2015 was excluded because it did not include any of the pre‐specified outcomes of interest for this review; this study focused exclusively on radiological outcomes at three weeks.
As reported in Hanchard 2014, the relationship between Itoi 2003, which was reported as a preliminary study, and Itoi 2007 was unclear. Furthermore, in light of contradictory information received from the trial investigator, we could not rule out the possibility that there were trial participants in common; therefore we excluded Itoi 2003.
Finally, we excluded one previously ongoing study after the principal investigator informed us that the trial had been abandoned (ACTRN12611001183976).
Further details of these studies are given in the Characteristics of excluded studies tables.
Studies awaiting classification
Six RCTs await classification; see Characteristics of studies awaiting classification. Five are parallel, two‐group RCTs comparing immobilisation in external rotation versus immobilisation in internal rotation (ISRCTN41070054; ISRCTN48254181; Miller 2007; Murray 2016; NCT00707018). We have identified no published full reports related to any of these, and our efforts to contact the corresponding authors for information about the current status of their study and the actual or anticipated availability of a published full report were mostly unsuccessful. ISRCTN41070054 (with an initial target sample size of 50, revised down to 38), ISRCTN48254181 with a target sample size of 150 and NCT00707018 with a target sample size of 50 are all completed, according to the WHO International Clinical Trials Registry Platform; and long intervals have passed since the respective anticipated or actual end dates (between 2008 and 2012). Miller 2007 and Murray 2016 are published abstracts, but neither provides sufficient information to stand alone. Miller 2007 reported interim results for 30 participants, but the total sample aimed for or achieved is unknown. Murray 2016 reported results for 50 participants. Dr Murray informed us that publication of this trial is pending (personal communication, 31 May 2018).
Outcomes of these five studies include re‐dislocation at two years (Murray 2016) or at unspecified time points (ISRCTN41070054; ISRCTN48254181); patient‐reported outcome measures for shoulder instability at one year (Miller 2007; NCT00707018); time taken to resume pre‐injury sport or other activities (NCT00707018); and any instability at two years (NCT00707018).
Also still awaiting classification is Itoi 2013. This parallel, three‐group RCT, which was already included as a study awaiting classification in Hanchard 2014, is published as a full report, but compares supplements to a yet unproven method (treatment with or without a shoulder motion restriction band following immobilisation in external rotation). As such, this trial is still not eligible for inclusion at this time.
Ongoing studies
All five ongoing studies are parallel, two‐group RCTs; see Characteristics of ongoing studies. Of these, two compare immobilisation in external rotation versus immobilisation in internal rotation (NCT01648335; NCT02197819). The recruitment status of NCT01648335, with an unspecified target sample size, is 'unknown' (ClinicalTrials.gov, last update posted in March 2013). NCT02197819, with a target sample size of 75, is still recruiting according to the registration record (accessed at ClinicalTrials.gov; last update posted August 2017); the estimated primary study completion date is specified as February 2018. Our attempts to obtain more information on these two trials were unsuccessful. Outcomes of these two studies included re‐dislocation.
The three other ongoing studies compare different aspects of rehabilitation after shoulder dislocation (ACTRN12616001241426; ARTISAN; Eshoj 2017). Recruitment of a target sample of 48 participants has been delayed until 2019 for ACTRN12616001241426, which is intended to test a purpose‐designed smartphone application (including information and an exercise‐based rehabilitation programme) as an adjunct to a supervised rehabilitation programme provided to all participants. The ARTISAN trial is a multicentre, NIHR‐funded study with a target sample size of 478 participants. It aims to compare two different rehabilitation strategies starting after two weeks of immobilisation: a single session of "advice to aid self‐management" versus the same session followed by a course of individually tailored physiotherapy over four months. Eshoj 2017, which has a published protocol, compared a 12‐week specific neuromuscular exercise programme (the 'SINEX' programme) versus 12 weeks of 'standard care'; i.e. a self‐managed shoulder exercise programme with a single introductory supervised physiotherapy session in 56 patients. According to the trial registration record (NCT02371928), data collection for this study was completed in June 2017. We were unsuccessful in our attempt to obtain information on the current status of this study. The primary outcome measures of these three studies are the OSI (ACTRN12616001241426; ARTISAN 2018) and the WOSI (Eshoj 2017).
Risk of bias in included studies
Risk of bias for the seven domains varied across the included studies and across outcomes (see Figure 2; Figure 3). All studies were at some, either high or unclear, risk for one or more outcomes, and we judged none to be at low risk.
2.
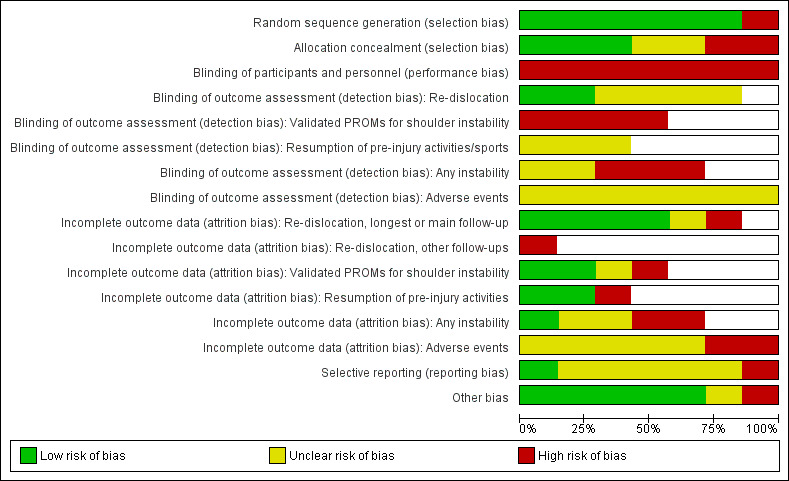
Risk of bias graph: authors' judgements about each risk of bias item presented as percentages across all included studies
3.
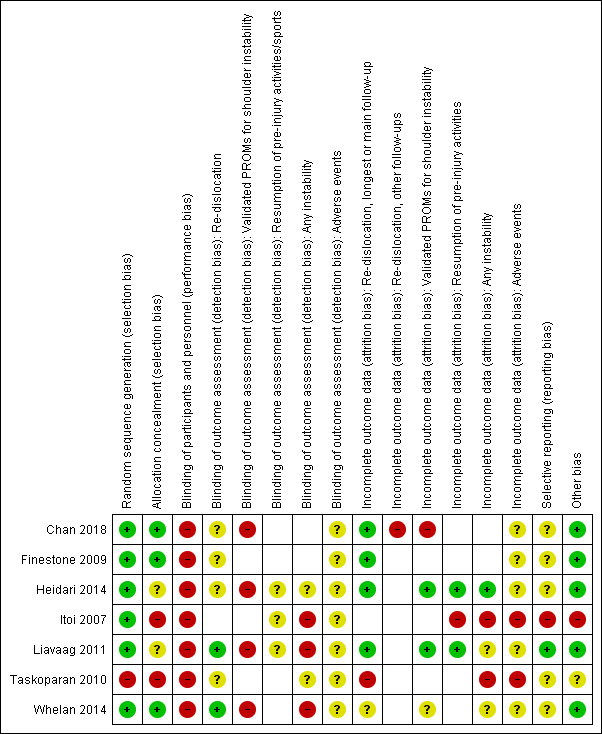
Risk of bias summary: authors' judgements about each risk of bias item for each included study
Allocation
We judged three of the seven trials to be at low risk of selection bias (Chan 2018; Finestone 2009; Whelan 2010). We judged two at high risk: Itoi 2007, which probably lacked allocation concealment; and Taskoparan 2010, as the result of quasi‐random sequence generation and lack of allocation concealment. We judged the remaining two trials at unclear risk of selection bias as both used sealed envelopes but provided insufficient details to confirm allocation concealment (Heidari 2014; Liavaag 2011).
Blinding
Blinding of participants and personnel
Due to the nature of the studied interventions, participants could not be blinded. We judged the risk of performance bias as 'high' for all seven trials. Regarding the blinding of the care providers, some trials did not provide any information about who applied the braces or slings and gave the initial instructions (Finestone 2009; Heidari 2014; Taskoparan 2010); and in two trials it was unclear whether those who applied the braces and slings and gave the instructions were otherwise independent of the trial (Chan 2018; Whelan 2014). In Itoi 2007, the participants were instructed by the treating surgeons, and the authors themselves stated that "we and the other surgeons might have made a stronger effort to ensure adherence to the external rotation immobilization". In Liavaag 2011, participants were informed of the preliminary results of Itoi 2007, which had favoured immobilisation in external rotation.
Blinding of outcome assessment
Re‐dislocation
We judged two trials that assessed re‐dislocation to be at low risk of detection bias because it was confirmed either by reference to medical records (Liavaag 2011) or radiography and/or record of manipulative reduction in a controlled hospital or healthcare setting (Whelan 2014). We rated another four studies at unclear risk of detection bias, reflecting either a lack of information how re‐dislocation was assessed and/or verified (Finestone 2009; Taskoparan 2010) or that re‐dislocation was (at least partly) patient‐reported, without further verification (Chan 2018; Heidari 2014). We considered that patients' reports of re‐dislocation, a distinct and clear‐cut event, are less vulnerable to subjectivity than other patient‐reported outcomes.
Validated patient‐reported outcome measures for shoulder instability
We judged all four trials that assessed this outcome to be at high risk of detection bias (Chan 2018; Heidari 2014; Liavaag 2011; Whelan 2014); the reason being that these patient‐reported outcome measures are inherently subjective.
Resumption of pre‐injury activities
We judged all three trials that assessed this outcome at unclear risk of bias (Heidari 2014; Itoi 2007; Liavaag 2011). Although this assessment is subjective we considered this outcome, assessed by a simple statement about whether or not the participants had resumed pre‐injury activities or sports, as less susceptible to bias than other subjective outcomes.
Any instability
We judged the three trials that assessed a composite outcome comprising re‐dislocation or subluxation at high risk of detection bias (Itoi 2007; Liavaag 2011; Whelan 2014). This is because subluxation is inevitably subjective and generally much less amenable than re‐dislocation to a clear‐cut definition. There was no mention of blinding for the two trials assessing instability via a clinician‐reported positive anterior apprehension test; hence we rated the risk of detection bias as unclear for these (Heidari 2014; Taskoparan 2010).
Adverse events
We rated all seven trials at unclear risk of detection bias for this outcome given the lack of information to allow a judgement.
Incomplete outcome data
Re‐dislocation
We judged the risk of attrition bias for re‐dislocation at final follow‐up was low for four trials as there were either no or small losses to follow‐up (Chan 2018; Finestone 2009; Heidari 2014; Liavaag 2011). We judged the risk as unclear for Whelan 2014, where no reason was given for the losses to follow‐up but these were similar in the two groups (13% versus 14%). We rated Taskoparan 2010 at high risk of attrition bias because the flow of participants throughout the study was unclear and there appeared to have been a large unexplained (and also unbalanced) number of losses to the 2‐year follow‐up (63% in the external rotation group and 35.3% in the external rotation group).
We judged the risk of bias was high for the interim scheduled follow‐ups at 3 and 12 months for Chan 2018 because the losses were unbalanced between the groups, with high proportions of losses in the internal rotation group: 22% versus 8% at 3‐month follow‐up; and 33% versus 14% at 12‐month follow‐up).
Validated patient‐reported outcome measures for shoulder instability
We rated two of the four trials that assessed this outcome at low risk of attrition bias because the losses were small (Heidari 2014; Liavaag 2011). We judged the risk as unclear for Whelan 2014, for the same reasons as above for re‐dislocation. We judged Chan 2018 at high risk because the losses to follow‐up were unbalanced at both the final 24‐month follow‐up (31% versus 17%) and 12‐month follow‐up (33% versus 17%). The reason for all losses to follow‐up was the inability to contact these participants. No missing data were replaced.
Resumption of pre‐injury activities
In two of the three studies who assessed this outcome, the reported outcome data related to a subgroup of participants who had sustained their injury during sports (Heidari 2014; Itoi 2007). We judged Heidari 2014 at low risk given the small loss to follow‐up and, conversely, Itoi 2007 at high risk because of the high loss to follow‐up. We judged Liavaag 2011 at unclear risk because the losses to follow‐up were reasonably low and balanced between the two groups (11% versus 10%).
Any instability
We judged Heidari 2014 was at low risk of bias for this outcome in view of the small loss to follow‐up; and Liavaag 2011 and Whelan 2014 at unclear risk, given the fairly modest loss to follow‐up was balanced in the two groups (13% versus 14% in both trials). We judged the other two trials reporting this outcome at high risk of attrition bias for any instability: in Itoi 2007, this was due to the high and unexplained attrition in both groups (18.3% versus 21.3%); and in Taskoparan 2010, there were very considerable unexplained losses to follow‐up, particularly at two years (62.5% versus 35.5%).
Adverse events
We judged five trials at unclear risk of attrition bias because of a lack of information (Chan 2018; Finestone 2009; Heidari 2014; Liavaag 2011; Whelan 2014); and two trials at high risk given their high loss to follow‐up (Itoi 2007; Taskoparan 2010).
Selective reporting
We judged the risk of reporting bias as low in one trial (Liavaag 2011), the only study for which a separately published a priori protocol was available. We judged the risk of reporting bias as unclear in five studies (Chan 2018; Finestone 2009; Heidari 2014; Taskoparan 2010; Whelan 2014), mainly because of insufficient information due to lack of a protocol, registration record or other publications. Additionally, in Whelan 2014 results were reported for a follow‐up of "at minimum 12 months" (mean 25, range 12 to 43 months), but not for each of the prespecified follow‐up points; it is unclear whether this may have introduced reporting bias. We judged Itoi 2007 at high risk of reporting bias because the start point and selection criteria varied across the available reports and may not have been determined prospectively, with related concerns regarding outcome assessment.
Other potential sources of bias
As per protocol we considered discrepancies in the level of skill or care with which the compared interventions were applied and commercial sponsorship (involvement). We also considered if there were any other sources of bias that were additional to those assessed in the other domains. We rated the risk of other bias based on whether we judged there was a risk of bias relating to the individual items. We judged the risk of other bias was low for five trials (Chan 2018; Finestone 2009; Heidari 2014; Liavaag 2011; Whelan 2014); unclear for Taskoparan 2010; and high for Itoi 2007.
Discrepancies in the level of skill or care with which the compared interventions were applied
Only Whelan 2014 identified the involvement of a certified orthopaedic technician for application of the interventions. The other trials provided no or minimal information on this aspect. Care programmes other than immobilisation and related advice, although mostly poorly described, appeared to have been comparable for both groups in all trials. Although we were unable to assess whether there were different skill levels in the provision of the two interventions, we did not consider any trial was at additional risk of performance bias.
Commercial sponsorship
Four trials were at low risk of bias related to commercial interests, either by explicit confirmation of receiving no benefits from a commercial company (Finestone 2009; Heidari 2014; Liavaag 2011) or an absence of commercial sources among the listed funders (Whelan 2014). In Chan 2018, the external rotation braces were provided by the manufacturer. However, the trial report notes that the manufacturer "[was] not involved in the design, data analysis or preparation of this data", which we consider indicates that the trial was conducted and reported independently of the commercial interests. Taskoparan 2010 did not provide any information about funding and was thus rated at unclear risk of other bias. We judged Itoi 2007 at high risk of bias relating to this aspect as they disclosed potentially substantial disbursements by the manufacturer of their immobilisers.
Other bias
Itoi 2007 reported switching from a locally made wire‐mesh splint covered with sponge and stockinette to a commercially manufactured external rotation prototype brace part way through the trial. We are unsure whether this change is a source of bias but unexplained change to protocol is of concern. Hence we rated this trial at unclear risk of bias for this aspect.
Effects of interventions
See: Table 1
All seven trials compared immobilisation of the affected arm in external rotation versus internal rotation. We could not organise outcomes within our planned framework of short term (up to and including three months following dislocation), medium term (greater than three months and up to and including 12 months) and long term (longer than 12 months) because the available data did not allow this. The most common follow‐up was '24 months or longer', which is when over 85% of re‐dislocations would be expected to have occurred (within two years after the initial dislocation; Robinson 2006).
We undertook some meta‐analyses. However, given the limitations of the data, a cautious approach is needed in the interpretation of these, which is reflected in our GRADE assessments of either low or very low certainty.
There were no or insufficient data to carry out our proposed subgroup analyses detailed in Subgroup analysis and investigation of heterogeneity. We present the available data for different age groups for re‐dislocation and 'any instability'. Possibilities for sensitivity analyses were also very limited.
The effects of interventions are reported below; see also Table 1.
Primary outcomes
Re‐dislocation
Six of the seven included studies contributed data from 488 participants (69% of the 704 randomised participants) to the results for this outcome; Itoi 2007 reported only on instability as a composite outcome of re‐dislocation or subluxation.
There is very low certainty evidence that external rotation may make little difference to the risk of re‐dislocation after 12 or more months' follow‐up (55/245 versus 73/243; RR 0.67, 95% CI 0.38 to 1.19; 488 participants; 6 studies; I² = 61%; see Analysis 1.1; Figure 4). We rated the quality of this evidence as very low after downgrading by one level for risk of bias, one level for inconsistency and one level for imprecision. We provide further data for re‐dislocation in Analysis 1.2. The mean proportion of participants with re‐dislocation across the six trials that investigated this outcome was 22% (range 4% to 37%) in the external rotation groups and 30% (range 25% to 42%) in the internal rotation groups. Sensitivity analysis shows that the removal of the only quasi‐RCT (Taskoparan 2010), which was at high risk of selection and attrition biases, resulted in little change to the results (RR 0.73, 95% CI 0.41 to 1.29; 455 participants, I² = 63%; analysis not shown). Sensitivity analysis confirmed the visual impression that Heidari 2014, the only trial that found a statistically significant result in favour of external rotation, was the source of the significant heterogeneity. The results after the removal of Heidari 2014 did not show a difference between the two groups (53/194 versus 56/192; RR 0.95, 95% CI 0.69 to 1.32; 386 participants; I² = 1%; analysis not shown).
1.1. Analysis.
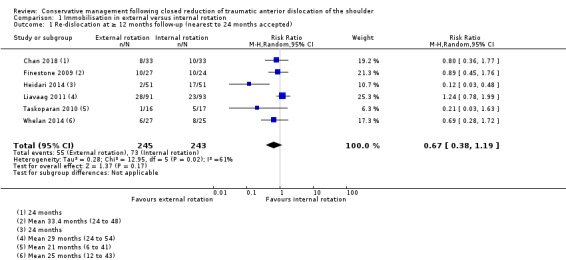
Comparison 1 Immobilisation in external versus internal rotation, Outcome 1 Re‐dislocation at ≥ 12 months follow‐up (nearest to 24 months accepted).
4.
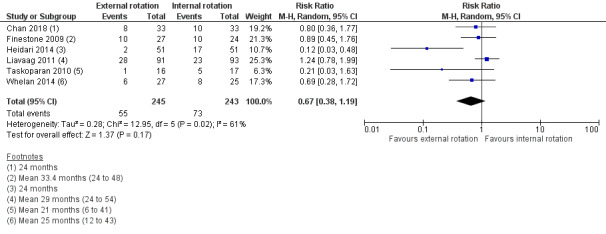
Forest plot of Re‐dislocation at ≥ 12 months follow‐up (nearest to 24 months accepted)
1.2. Analysis.
Comparison 1 Immobilisation in external versus internal rotation, Outcome 2 Re‐dislocation data at last follow‐up.
| Re‐dislocation data at last follow‐up | |||
|---|---|---|---|
| Study | Follow‐up | External rotation, n events/n group (%) | Internal rotation,n events/n group (%) |
| Chan 2018 | 24 months ("full period") | 8/33 (24%) | 10/33 (30%) |
| Finestone 2009 | Mean 33.4 (range 24 to 48) months | 10/27 (37%) | 10/24 (42%) |
| Heidari 2014 | 24 months | 2/51 (4%) | |
| Liavaag 2011 | Minimum 2 years, mean 29.1 (range 24‐54) months | 28/91 (31%) | 23/93 (25%) |
| Taskoparan 2010 | Mean 21 (range 6 to 41) months | 1/16 (6%) | 5/17 (29%) |
| Whelan 2014 | Minimum 12 months, mean 25 (range 12‐43) months | 6/27 (22%) | |
Chan 2018 provided additional data for prespecified follow‐ups at three months, when only one participant had experienced a re‐dislocation; and 12 months, when there was no evidence of a difference between the two groups (RR 0.88, 95% CI 0.37 to 2.10; 55 participants); Analysis 1.3.
1.3. Analysis.
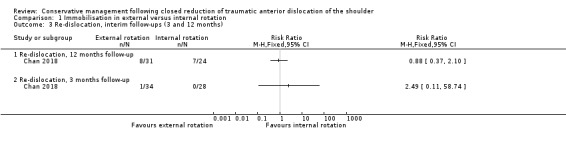
Comparison 1 Immobilisation in external versus internal rotation, Outcome 3 Re‐dislocation, interim follow‐ups (3 and 12 months).
Subgroup analyses
There were insufficient data to conduct subgroup analyses. Moreover, consideration was further complicated by the findings that the removal of Heidari 2014 alone resolved the finding of significant heterogeneity; and moreover resulted in evidence of little or no difference between the two groups. Data that could have contributed to subgroup analysis by age are presented in Table 4; as well as illustrating the insufficiency of the available data, the results for the 39 years or younger versus 40 years or older category are dominated by Heidari 2014.
3. Re‐dislocation: data for different age categories.
| Subgroup | Study | Age category | External rotation group | Internal rotation group |
| Data available for planned subgroup analysis age ≤ 20 years versus age ≥ 21 years | ||||
| age ≤ 20 years | Heidari 2014 | ≤ 20 years | 0/0 (0%) | 0/0 (0%) |
| Taskoparan 2010 | ≤ 20 years | 0/0 (0%) | 0/1 (0%) | |
| age ≥ 21 years | Heidari 2014 | ≥ 21 years | 2/51 (4%) | 17/51 (33%) |
| Taskoparan 2010 | ≥ 21 years | 1/16 (6%) | 5/16 (31%) | |
| Data available for planned subgroup analysis age ≤ 39 years versus age ≥ 40 years | ||||
| age ≤ 39 years | Heidari 2014 | ≤ 40 years | 2/42 (5%) | 16/47 (34%) |
| Liavaag 2011 | ≤ 40 years | 28/91 (31%) | 23/93 (25%) | |
| Taskoparan 2010 | ≤ 40 years | 1/12 (8%) | 5/14 (36%) | |
| Whelan 2014 | ≤ 35 years | 6/27 (22%) | 8/25 (32%) | |
| age ≥ 40 years | Heidari 2014 | ≥ 41 years | 0/9 (0%) | 1/4 (25%) |
| Taskoparan 2010 | ≤ 40 years | 0/4 (0%) | 0/3 (0%) | |
| Other data, including subgroups | ||||
| Other | Chan 2018 | 16 to 44 years | 8/33 (24%) | 10/33 (30%) |
| Finestone 2009 | 17 to 27 years | 19/27 (37%) | 10/24 (42%) | |
| Heidari 2014 | 21 to 30 years | 1/16 (6%) | 3/18 (17%) | |
| Heidari 2014 | 31 to 40 years | 1/26 4%) | 13/29 (45%) | |
| Liavaag 2011 | 16 to 22 years | 19/33 (58%) | 13/30 (43%) | |
| Liavaag 2011 | 23 to 29 years | 6/24 (25%) | 7/27 (26%) | |
| Liavaag 2011 | 30 to 40 years | 3/34 (9%) | 3/36 (8%) | |
| Taskoparan 2010 | 15 to 75 years | individual participant data in study report | ||
The table shows age‐related subgroup data for the predefined categories of interest (≤ 20 years versus ≥ 21 years; ≤ 39 years versus ≥ 40 years), as well as other subgroups or age ranges as reported in the trials. Actual thresholds varied as shown.
We considered conducting an exploratory subgroup analysis of trials in which immobilisation in external rotation had an abduction component versus those without (external rotation only). However, as well as there being only a few trials available in each subgroup, the heterogeneity between the two trials for the external rotation with abduction groups was considerable (I² = 84%); these results are presented for illustrative purposes only in Analysis 1.4.
1.4. Analysis.
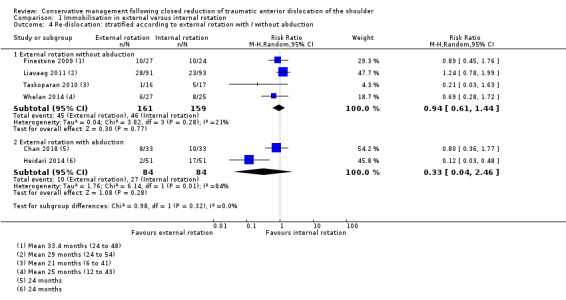
Comparison 1 Immobilisation in external versus internal rotation, Outcome 4 Re‐dislocation: stratified according to external rotation with / without abduction.
Time to re‐dislocation
The majority of re‐dislocations appeared to have occurred within the first year after the initial dislocation. Heidari 2014 and Itoi 2007 reported that most re‐dislocations occurred during the first year after the initial dislocation; however, Itoi 2007 did not provide separate data for this outcome. In Finestone 2009, the mean time to re‐dislocation was 12.4 months (range 4 to 36 months); and in Liavaag 2011, the mean time to re‐dislocation was 11.6 months (range 2 to 24 months). The data provided for the different lengths of follow‐up in Chan 2018 suggest that most dislocations occurred within the first year in this study. Taskoparan 2010 and Whelan 2014 did not provide any data.
Validated patient‐reported outcome measures for shoulder instability
Four of the seven included trials contributed data from 380 participants (54% of 704 randomised participants) to the results for this outcome (Chan 2018; Heidari 2014; Liavaag 2011; Whelan 2014). Three trials reported results based on the WOSI; this score, which comprises 21 items, each of which is scored on a 100 mm visual analogue scale, ranges from 0 (least disability) to 2100 (worst disability) (Angst 2011; Kirkley 1998). Chan 2018 reported results of the OSI; this score, which comprises 12 items (each of which has five response options, scoring 0 to 4), ranges from 0 (worst impairment) to 48 (least impairment) (Dawson 1999; van der Linde 2015). Although Taskoparan 2010 used the Rowe Score, another validated instrument for assessing instability, it was not clear whether this was patient‐assessed. Moreover, the data were not usable since they applied to a large range of follow‐up times (6 to 41 months) and the distribution was very skewed with 22 of the 33 at the top end (95 or 100) of the scale). We did not pool the very limited data that were potentially available for pooling for this outcome. We rated the certainty of the evidence for this outcome as very low after downgrading for risk of bias, imprecision and inconsistency (each by one level).
Heidari 2014 found lower WOSI scores, indicating less disability, at the 33‐months follow‐up in the external rotation group (MD −43.20, 95% CI −72.38 to −14.02; 97 participants; Analysis 1.5). Whelan 2014, which expressed the WOSI result in % of the total (reversed) score (0% = worst outcome, 100% = best outcome), found only a minimal difference between the groups in the WOSI at a mean follow‐up of 25 months: −3.00, 95% CI −12.78 to 6.78; 52 participants; Analysis 1.5). Reporting non‐parametric data, Chan 2018 reported no statistically significant differences between the groups in the OSI at either 24‐month (57 participants) or 12‐month (54 participants) follow‐ups, as did Liavaag 2011 (174 participants) based on WOSI results at a mean of 29 months' follow‐up; see Analysis 1.6.
1.5. Analysis.
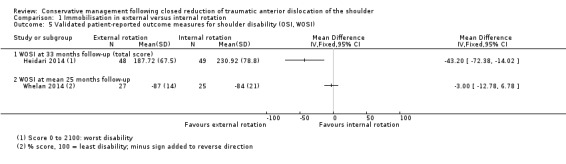
Comparison 1 Immobilisation in external versus internal rotation, Outcome 5 Validated patient‐reported outcome measures for shoulder disability (OSI, WOSI).
1.6. Analysis.
Comparison 1 Immobilisation in external versus internal rotation, Outcome 6 Validated PROMS: non‐parametric results.
| Validated PROMS: non‐parametric results | |||||
|---|---|---|---|---|---|
| Study | Follow‐up | Measure | External rotation | Internal rotation | Reported P |
| Final follow‐up | |||||
| Chan 2018 | 24 months | OSI (0 to 48: least impairment) | median 43.5 (range 12 to 48); n = 30 | median 43.5 (range 13 to 48); n = 27 | P = 0.50 |
| Liavaag 2011 | mean 29 months (24 to 54) | WOSI (0 to 2100: worst disability) | median 238 (interquartile range 101 to 707); n = 86 | median 375 (interquartile range 135 to 719); n = 88 | P = 0.32 |
| Interim follow‐up | |||||
| Chan 2018 | 12 months | OSI (0 to 48: least impairment) | median 43 (range 6 to 48); n = 30 | median 42.5 (range 5 to 48); n = 24 | P = 0.35 |
None of the trials provided estimates of the minimal important difference (MID) to guide interpretation of results for the OSI or WOSI. Also, only very limited MID estimates are yet available from the literature. Based on a cohort study of 105 participants with shoulder instability (primary dislocation or recurrent instability) and using an anchor‐based analysis approach, van der Linde 2017 suggested an estimate of around 6 points for the OSI and an estimate of around 14% for the WOSI (which corresponds to 294 points). These estimates provide some preliminary indication that the results of the trials, including that for Heidari 2014 where the larger 95% confidence limit (72.38) was much smaller than the MID of 294 points, for both the OSI and the WOSI are unlikely to be clinically important.
Resumption of pre‐injury activities
Three of the seven included trials contributed data from 347 participants (49% of 704 randomised participants) to the results for this outcome (Heidari 2014; Itoi 2007; Liavaag 2011). This outcome was poorly defined in each trial, and we considered the information provided was insufficient to justify pooling. We rated the certainty of the evidence for this outcome as very low after downgrading for risk of bias, imprecision and inconsistency (each by one level).
The available results are shown in Analysis 1.7. Both Heidari 2014 and Itoi 2007 reported the return to sports for the subgroup of participants who had sustained their initial injury during sport. Heidari 2014 found a large difference in favour of external rotation in return to pre‐injury sportive activities at 24 months: 26/31 versus 12/38; RR 2.66, 95% CI 1.62 to 4.35; 69 participants). Itoi 2007 found a greater return in the external rotation group at 24 months to any level of sport (43/60 versus 31/49, RR 1.13, 95% CI 0.87 to 1.48; 109 participants) and to pre‐injury sport activity (22/60 versus 10/49; RR 1.80, 95% CI 0.94 to 3.43; 109 participants). However, both 95% CIs for Itoi 2007 included the possibility of a result in favour of internal rotation. Liavaag 2011 found no difference between the two groups in the return to the pre‐injury level of activity with the affected arm at a mean 29 months' follow‐up: 51/83 versus 52/86; RR 1.02, 95% CI 0.80 to 1.29, 169 participants).
1.7. Analysis.
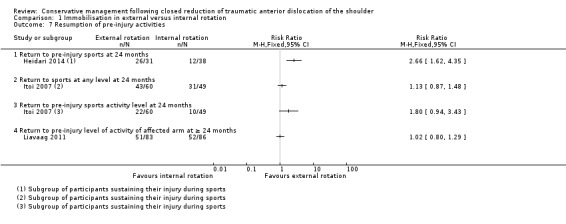
Comparison 1 Immobilisation in external versus internal rotation, Outcome 7 Resumption of pre‐injury activities.
Secondary outcomes
Participant satisfaction with the intervention
No studies considered this outcome.
Validated quality of life outcome measures
No studies considered generic health‐related quality of life outcome data (using e.g. EQ‐5D, SF‐36).
Any instability: subluxation or subjective instability (either individually or grouped with dislocation as a composite outcome)
Five of the seven included trials contributing data from 530 participants (75% of 704 randomised participants) reported this outcome in two distinct ways. In three trials, the outcome was defined in terms of subluxation or re‐dislocation (Itoi 2007; Liavaag 2011; Whelan 2014). In the other two trials, we defined it as a positive apprehension text or re‐dislocation (Heidari 2014; Taskoparan 2010). Although we pooled the data for each of these two categories, it was in the knowledge of serious limitations of the available data especially reflecting loss to follow‐up in Itoi 2007 (data available for 159 (80%) of 198 participants); Liavaag 2011 (subluxation data were only available for 163 (89%) of participants but 'recurrent instability' was reported for 184 participants in the trial report); and Taskoparan 2010 (25 (76% of 33) followed up for one year).
There is insufficient evidence of little or no between‐group difference in the number of participants with instability (subluxation or re‐dislocation, or potentially both): 77/205 versus 86/190; RR 0.84, 95% CI 0.62 to 1.14; 395 participants, 3 studies; I² = 31%; very low certainty evidence downgraded two levels for very serious risk of bias and one level for imprecision; Analysis 1.8). The data for our other measure of instability (positive apprehension or re‐dislocation) favoured the external rotation group but were dominated by the re‐dislocation data from Heidari 2014: 8/67 versus 29/68; RR 0.28, 95% CI 0.14 to 0.57; 135 participants, 2 studies; I² = 0%). We rated the certainty of this evidence as very low after downgrading by two levels for risk of bias, one level for imprecision and one level for indirectness (reflecting the suboptimal measurement of the outcome).
1.8. Analysis.
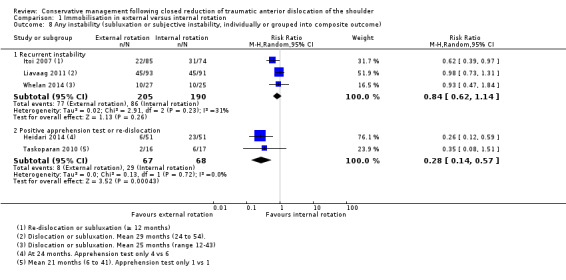
Comparison 1 Immobilisation in external versus internal rotation, Outcome 8 Any instability (subluxation or subjective instability, individually or grouped into composite outcome).
Itoi 2007 presented subgroup data related to different age groups for recurrent dislocation or reluxation at a follow‐up of two years or longer, with categories that were similar to our pre‐defined age categories: ≤ 20 years versus ≥ 21 years; ≤ 40 years, ≥ 40. The data are presented in Table 5.
4. Any instability: data for different age categories from Itoi 2007.
| Subgroup (age) | External rotation group | Internal rotation group |
| ≤ 20 years | 11/27 (41%) | 13/19 (68%) |
| ≥ 21 years | 11/58 (19%) | 18/55 (33%) |
| ≤ 40 years | 19/62 (31%) | 27/50 (52%) |
| ≤ 41 years | 3/23 (13%) | 4/24 (17%) |
The table shows age‐related subgroup data for the predefined categories of interest (≤ 20 years, ≥ 21 years, ≤ 39 years, ≥ 40 years)
Adverse events
With the exception of Chan 2018, trials reported specifically on adverse events, but usually in an ad hoc and incomplete way. It was sometimes unclear whether the reported 'adverse events' were exclusively treatment‐related and we found it hard to judge whether some events merited being considered 'important'. Thus, for example, Heidari 2014 reported three cases in the external fixation group of "transient shoulder rigidity that resolved by the time of the follow‐up at 24 months", without giving an indication of the severity, duration or treatment of the shoulder stiffness. We decided this was probably not an important adverse event and pooled this result with data from Itoi 2007 for six cases of temporary stiffness resolved via the "use of self‐directed range‐of‐motion exercises" and two cases of axillary rash in the internal rotation group in Finestone 2009.
Liavaag 2011 reported two "complications" at unspecified time points: one participant in the external rotation group had hyperaesthesia and moderate hand pain, and one in the internal rotation group had eighth cervical dermatome paraesthesia. Taskoparan 2010 reported that one participant in the internal rotation group had "30° limitation in abduction and 10 degrees in internal rotation in the 6th and 12th months. This patient was 75 years old and had additional rotator cuff problems". Taskoparan 2010 did not clarify whether these limitations were active (as with rotator cuff tear) or active and passive (as with frozen shoulder). We judged the complications from these two trials to be important adverse events. Whelan 2014 reported there had been no treatment‐related complications.
These data, stratified by the two categories of severity, are presented for illustrative purposes in Analysis 1.9: transient and resolved adverse events (9/196 versus 2/181; RR 2.73, 95% CI 0.83 to 9.02; 377 participants, 4 studies; I² = 56%); important adverse events (1/134 versus 2/134; RR 0.61, 95% CI 0.08 to 4.46; 268 participants, 3 studies; I² = 0%). We rated the certainty of the evidence for adverse events as very low after downgrading by two levels for risk of bias, one level for imprecision (very few events) and one level for indirectness reflecting the poor definition and reporting of adverse events.
1.9. Analysis.
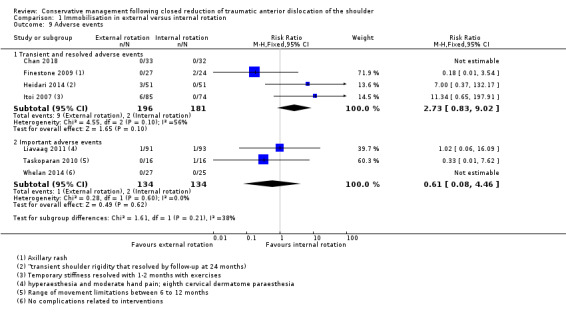
Comparison 1 Immobilisation in external versus internal rotation, Outcome 9 Adverse events.
Other outcomes
We intended to document any reports of service utilisation or resource use (e.g. length of hospital stay), outpatient attendance and the provision and nature of physiotherapy; and participants' adherence to their allocated interventions. Of these, only adherence was addressed in the included studies. We made the post hoc decision to report two further outcomes with the 'other outcomes', as we considered these data of interest to both clinicians and researchers: one was 'difficulties with wearing the braces or slings'; the other one 'surgery'. We did not consider these outcomes as 'adverse events'.
Adherence
Six studies reported on adherence, although using different measures and definitions. The data for complete or top‐level adherence to treatment interventions for six trials are shown in Analysis 1.10, with definitions of the measures used in individual trials provided in the footnotes. The differences in the measures used, the significant statistical heterogeneity (I² = 82%) together with differences in effect direction, meant that we did not pool these data. The extent of 'complete' adherence varied between trials, with almost full adherence reported for Finestone 2009; indeed the only omitted participant had removed his splint two days early. In contrast, only 47% of participants of the internal fixation group used their splints for at least 16 hours for at least 20 days in Liavaag 2011. As reported above, Itoi 2007 admitted the possibility that stronger encouragement to ensure adherence had been given to the external mobilisation group.
1.10. Analysis.

Comparison 1 Immobilisation in external versus internal rotation, Outcome 10 Adherence to treatment.
Difficulties with wearing the braces or slings
Chan 2018 alone provided a detailed description of reported difficulties with wearing the braces or slings. Overall, 27 of 34 participants (79%) in the external rotation group reported difficulties compared with 13 (46%) of 28 participants in the internal rotation group. The majority of the participants (21/34 (62%)) in the external rotation group complained about difficulties with wearing their braces during the night. Reasons included pain, difficulties with sleeping and loosening of straps. Other complaints included "feeling that the brace did not support the arm (21%), functionally awkward in the daytime (18%), difficulty in application of the sling (15%) and pain when in external rotation (12%)". In the conventional sling group, reported difficulties with wearing the slings included "night symptoms (25%), difficulty in application/loosening of the straps (14%), feeling hot/itchy (11%) and pain around the neck strap (7%)". The "level of comfort", which was assessed on a 4‐point ordinal scale (1 = very uncomfortable; 2 = moderately uncomfortable; 3 = slightly uncomfortable; 4 = comfortable), was reported as significantly higher in the conventional sling group; the median was 3.0 (range 1 to 4) in the external rotation group and 3.5 (range 3 to 4) in the internal rotation group (nonparametric analysis; reported P = 0.02).
Taskoparan 2010 noted that "all patients adapted quite well to the fixation methods".
Surgery
Four trials reported the rates of participants who underwent or were scheduled for surgery (Chan 2018; Finestone 2009; Itoi 2007; Whelan 2014). However, only very limited information was provided regarding the precise indications for surgery, and how the decision for surgery was arrived at. Pooled data showed evidence of little or no difference between the two groups (20/172 versus 24/155; RR 0.76, 95% CI 0.44 to 1.30; 327 participants, 4 studies; I² = 0%; very low certainty data downgraded one level for risk of bias and two levels for imprecision; Analysis 1.11).
1.11. Analysis.
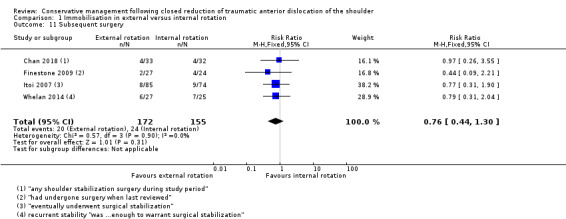
Comparison 1 Immobilisation in external versus internal rotation, Outcome 11 Subsequent surgery.
Economic outcomes
No data on aspects of service utilisation or resource use (e.g. length of hospital stay), outpatient attendance and the provision and nature of physiotherapy were reported.
Discussion
Summary of main results
This updated review of conservative management following closed reduction of traumatic, anterior shoulder dislocation now includes seven trials, which recruited 704 participants in total. In line with previous versions of this review, all trials made just one comparison: that of immobilisation in external versus internal rotation. The evidence for this comparison is presented in Table 1 and summarised below for the seven outcomes.
There is very low certainty evidence that there may be little or no difference between the two interventions in the numbers of participants experiencing a re‐dislocation at 12 months' or longer follow‐up. In Table 1, we identify the lowest, median and highest control group rates of re‐dislocation from the included trials to represent illustrative low‐, medium‐ and high‐risk populations and present the anticipated absolute effects for these three populations. We illustrate these results here for a moderate risk population: based on an illustrative risk of 312 people experiencing a dislocation in the internal rotation group, the pooled results from six studies (RR 0.67, 95% CI 0.38 to 1.19) equates to 103 fewer (95% CI 194 fewer to 60 more) re‐dislocations after immobilisation in external rotation.
There is no evidence of a clinically relevant difference between the two interventions in validated patient‐reported outcome measures for shoulder instability. Individually, the four studies reporting on validated patient‐reported outcome measures for shoulder instability at a minimum of 12 months' follow‐up found no evidence of a clinically important difference between the two interventions (very low certainty evidence).
We are uncertain of the relative effects of the two methods of immobilisation on resumption of pre‐injury activities or sports. One study (169 participants) found no evidence of a difference between interventions in the return to pre‐injury activity of the affected arm (very low certainty evidence). Two studies (135 participants) found greater return to sports in the external rotation group but this finding was limited to subgroups of participants who had sustained their injury during sports activities (very low certainty evidence).
No data were available for participant satisfaction with the intervention or for validated health‐related quality of life outcome measures (e.g. EQ‐5D and SF‐36).
There is no evidence of a difference between the two interventions in the number of participants experiencing instability, defined as either re‐dislocation of subluxation (very low certainty evidence).
There was very low certainty evidence available for adverse events, which were reported on an ad hoc basis in the seven trials. Reported 'transient and resolved adverse events' were nine cases of shoulder stiffness or rigidity in the external rotation group and two cases of axillary rash in the internal fixation group. There were three 'important' adverse events: hyperaesthesia and moderate hand pain; eighth cervical dermatome paraesthesia; and major movement restriction between 6 and 12 months. It was unclear to what extent these three adverse events could be attributed to the treatment.
The main results of this updated review confirm the results of the previous version by Hanchard 2014, and are twofold. Firstly, robust evidence for superiority of immobilisation in external rotation over immobilisation in internal rotation is still lacking, which implies that there is no justification for recommending any change in current clinical practice. Secondly, we found no includable evidence related to our other objectives.
Overall completeness and applicability of evidence
The available evidence from clinical trials on conservative management after closed reduction of traumatic primary anterior shoulder dislocation as yet relates exclusively to the comparison of immobilisation in external versus internal rotation. None of the included studies compared different durations of immobilisation or immobilisation versus no immobilisation. The latter may be of particular interest for older people who are at a much reduced risk of recurrence (Olds 2015; Wasserstein 2016) — but at greater risk of shoulder stiffness (de Boer 2005). Furthermore, none of the included studies addressed interventions following immobilisation, including comparisons of rehabilitation versus no rehabilitation or of different variants of rehabilitation. The lack of evidence on post‐immobilisation interventions is a remarkable finding considering that immobilisation represents only the initial short‐term treatment post dislocation. However, we identified three ongoing trials that were designed to compare different aspects of rehabilitation after traumatic primary shoulder dislocation, with target sample sizes of 48 (ACTRN12616001241426), 80 (Eshoj 2017) and 478 (Kearney 2018). This finding may indicate a timely shift of the focus of interest from initial treatment (with immobilisation) to other interventions (following initial immobilisation).
Overall completeness
Our search for this update led to the inclusion of only three new studies, so the current body of evidence consists of seven studies including 704 participants that compared immobilisation in external versus internal rotation. Pooled data for the main outcomes were available from 488 participants (69% of 704) for re‐dislocation and 395 (56% of 704) for any instability. No data are available for patient satisfaction or quality of life.
This should also be considered in the context of unpublished evidence. There are five completed studies that tested the same comparison, that are awaiting assessment and that may have recruited 318 participants (ISRCTN41070054; ISRCTN48254181; Miller 2007; Murray 2016; NCT00707018). Furthermore, there are two ongoing studies, one of which aims to recruit 75 participants (NCT02197819); the status of the other trial is unknown (NCT01648335). Thus the evidence for this comparison is far from being complete.
Applicability
Population
All participants had experienced a traumatic anterior dislocation of the shoulder that had been reduced by a closed method. All studies except Taskoparan 2010 explicitly excluded patients with associated fractures of the shoulder, and two studies also excluded patients with specific labral injuries (Liavaag 2011; Whelan 2014). However, as none of the trials specified the prevalence and/or characteristics of concurrent injuries within their actual samples, the applicability of the findings to patients with, or without, or with different types of concomitant injuries is unclear.
The evidence from the included studies represents the young and active as well as the relatively sedentary. Four studies evaluated mixed, general populations, with no restrictions on sex or age (Chan 2018; Finestone 2009; Itoi 2007; Whelan 2014). In contrast, all 51 participants were male of which 40 were soldiers in Finestone 2009. The greater proportion of males (82% of 704) in the studies is consistent with the epidemiology for this injury. Although there was insufficient information on the distribution of ages, an assessment of the mean ages and inclusion criteria of the seven studies suggests that the majority of participants were above 20 years and below 40 years old. These indicate that review findings are applicable to the majority of people who sustain this injury.
Interventions
The evidence included in this review relates exclusively to the comparison of immobilisation in external versus internal rotation. Some aspects of these interventions, such as the duration of immobilisation (3 or 4 weeks), were similar across the trials. However, given recent trends to promote immobilisation for shorter periods, such as up to a week (see Background), the longer duration used in the included studies may not reflect current practice or trends. Other aspects differed to some extent across the studies, such as the commencement of the immobilisation (ranging from within a couple of hours until seven days post injury) and the position of immobilisation in external rotation (which ranged from 0° to 5° external rotation in Whelan 2010 to 30° in Chan 2018; and was complemented by an abduction component in Chan 2018 and Heidari 2014 (30° and 15°, respectively)). It is unclear whether these differences could have affected estimates of effects and the applicability of the results. However, the fact that the precise position of the shoulder was mostly neither accurately measured nor monitored, and that the position is likely to have varied to some extent through the handling of the braces by the participants, tends to minimise the differences. The different external rotation angles appeared to be mostly justified by a trade‐off between findings from previous clinical trials or studies investigating structural aspects and the (documented or anticipated) tolerability of maximum external rotation angles. Our exploratory subgroup analysis of data for re‐dislocation related to external rotation with versus without an abduction component does not allow for any firm conclusions. It was not clear who provided the braces and slings as well as the accompanying instructions in four studies (Finestone 2009; Heidari 2014; Liavaag 2011; Taskoparan 2010). Differences in the level of experience and skills may have affected the way the braces and slings were applied, as well as the quality of the instructions that the participants received, and may thereby have affected outcome. Although all studies reported that the immobilisation period was followed by some sort of rehabilitation for both groups, most of the studies provided insufficient information regarding the precise duration, amount and content of rehabilitation treatment.
Outcomes and outcome assessment
Although definitions and reports of follow‐up periods varied across the trials, all trials included participants who were followed up for at least one year and generally two years (Table 3). Chan 2018 was the only study reporting data for interim time points (3 and 12 months). The literature on time to re‐dislocation suggests an average time to re‐dislocation of around 12 months: a recent systematic review by Wasserstein 2016 pooled data from four studies and reported a mean time of 10.8 months (SD 0.42). Regarding the studies included in our review, Finestone 2009 and Liavaag 2011 reported a mean time of 12.4 (range 4 to 36 months) and 11.6 months (2 to 24 months), respectively. Moreover Heidari 2014 and Itoi 2007 reported that the majority of re‐dislocations within their study samples occurred within the first year after the initial dislocation (the rate in Itoi 2007 was 83%). These data show that length of follow‐up was generally acceptable in the included trials. Nonetheless, considering that rates of re‐dislocation can still be expected to vary between follow‐ups of one year and two or more years, assessment at different time points (e.g. one year, two years) would have been helpful to ensure consistency across studies as well as to facilitate judgements about applicability.
All of our primary outcomes were addressed by at least some of the included studies. However, of our secondary outcomes there were no data for patient satisfaction or for quality of life using a validated generic health‐related quality of life outcome measure such as EQ‐5 or SF‐36. Interestingly, the term 'quality of life measure' is also commonly applied for disease specific PROMs, such as the WOSI and ASES (Heidari 2014; Whelan 2014). These outcome measures, though, are disease‐specific and were therefore considered with the validated PROMs for shoulder instability.
All studies included some documentation of adverse events; however, most did not specify adverse events as an a priori outcome, but reported them ad hoc. It was mostly unclear whether or not the reported events were systematically assessed in all participants, and no definitions were provided. Moreover the information provided was insufficient to judge whether the events were, or could be, related to the treatment, or whether they were (part of) distinct medical conditions that occurred sometime during the study periods. This was partly due to a lack of information on when the reported events occurred, but also the severity of the observed events was not sufficiently described. It is notable that all nine cases of short‐term shoulder stiffness occurred in the external rotation group; the possibility of this complication seems something that could be considered when treating people with the more rigid position used for external immobilisation. The a priori definition and specification of adverse events, and the systematic collection of data on adverse events, would have been helpful to determine the type and frequency of adverse events associated with immobilisation in external and internal rotation.
No data on aspects of service utilisation or resource use (e.g. length of hospital stay), outpatient attendance and the provision and nature of physiotherapy were reported.
Although patient satisfaction was not reported, adherence assessed in all seven trials and reported difficulties and complaints relating to brace or sling use measured in Chan 2018 may give some indirect guide to patient satisfaction during treatment. There may, however, be other factors. The high adherence rate in Finestone 2009 may be at least partly due to the fact that most participants were soldiers who, as the authors state, "had a high degree of self‐discipline and were treated within a military framework". Itoi 2007 pointed to the possibility that there had been stronger encouragement to ensure adherence given to the external mobilisation group. Liavaag 2011, whose authors also found higher adherence in the external rotation group, conjectured that participants in this group may have had confidence in the benefit of treatment. In contrast, Heidari 2014 reported greater adherence in the internal rotation group, and itemised in their discussion additional limitations associated with external rotation, such as walking safely through doorways, difficulties finding a comfortable sleeping position and risk of trauma in crowded locations. Data supporting this was presented in Chan 2018, who found a greater proportion of participants in the external rotation group reported difficulties, including with sleeping and feeling functionally awkward in the daytime. This finding is unsurprising, as intuitively one might expect maintenance of external rotation at the shoulder during normal day‐to‐day functioning to be cumbersome.
We introduced a new secondary outcome — 'subsequent surgery' — that helps to give a better picture of what happened to some of the people with recurrent instability. There is no evidence of a difference between the two groups.
Certainty of the evidence
We judged the certainty of the evidence included in this review as very low for all outcomes shown in Table 1. The grading of the quality of evidence means that we are uncertain about the estimates of effect.
We downgraded the certainty of the evidence for all outcomes at least by one level for risk of bias. In aggregate, concerns about risk of bias relate, to some extent, to all risk of bias domains, to all outcomes, and to all trials (Figure 2; Figure 3). Notable aspects were that we judged two of seven trials at high risk of selection bias and, reflecting that blinding to the interventions was not possible for either the participants or personnel, that all studies were at high risk of performance bias. This is demonstrated indirectly in Itoi 2007, where the trial authors raised the possibility that stronger encouragement to ensure adherence had been given to the external mobilisation group. The effect of lack of blinding on the risk of detection bias is likely to be outcome‐dependent, as reflected in our assessments for the different outcomes. The risk of attrition bias also varied with outcome: the presentation of the amount of losses to follow‐up was insufficient and often misleading, even when presented in flow diagrams, as they were not specified for each outcome. There was a high risk of selective reporting bias in Itoi 2007. The key domains that led to our downgrading for risk of bias by one level were selection bias, performance bias and detection bias. The key domain that led to our further downgrading by one level was attrition bias.
We downgraded the certainty of the evidence for several outcomes for inconsistency. For re‐dislocation, we noted that the substantial heterogeneity disappeared on the removal of Heidari 2014, which markedly differed from the other studies with regard to the positive findings in favour of immobilisation in external rotation for other outcomes. There are insufficient data to explore the underlying sources of heterogeneity and, in particular, to identify plausible reasons for the more positive findings in favour of external fixation of Heidari 2014.
We downgraded the certainty of the evidence for all outcomes for imprecision. This reflected wide 95% CIs, often including the possibility of benefit favouring either one of the interventions to various degrees, or no effect; as well as too few events and small sample sizes.
Indirectness was graded as not serious for most outcomes except 'any instability', which reflects the suboptimal measurement of the outcome; and 'adverse events', which reflects the ad hoc approach to collecting data on these and suboptimal reporting. Overall, however, the trials provided direct evidence to the review question despite some variation in the populations, interventions and outcomes.
Publication bias was graded as undetected for all outcomes. We identified five studies evaluating immobilisation in external versus internal rotation that have been completed but that have yet not been published. While this is of concern, as it suggests a risk of publication bias, we judged that the information available to us was insufficient for a clear judgement and thus did not downgrade for this item.
Potential biases in the review process
We strove throughout the development and execution of this updated review to minimise any potential for biases. Thus, when feasible, we adhered throughout to the detailed a priori protocol, which detailed every aspect of the review's aims, objectives and methods, and documented any changes that we considered necessary in Differences between protocol and review. We conducted a reasonably comprehensive search without language restriction, and involving various sources, and the key processes of study selection, data extraction and risk of bias assessment were each independently performed by the two review authors.
We contacted investigators and authors of ongoing studies and studies classified as awaiting classification for clarification of questions related to the status of their studies, and corresponding authors of the included studies for clarification of methodological aspects, missing details or data. Unfortunately we were unsuccessful in obtaining responses in the majority of cases. Regarding the three newly included studies, we received a response only from the authors of Chan 2018. Therefore, we had to mostly rely on the information provided in the study reports for the presentation of the study characteristics and results, and for our judgements of risk of bias, which means that our findings and judgements are affected by the completeness and quality of reporting.
As previously indicated (see Overall completeness and applicability of evidence), we recognise the number of studies awaiting classification as an unavoidable limitation of the review.
Although we did not conduct a formal update of the search after May 2018, we maintained regular checks via Medline (PubMed) auto‐alerts up to December 2018. These yielded Murray 2018, the full‐trial report of Murray 2016, another trial that compared immobilisation in external versus internal rotation; see Characteristics of studies awaiting classification). A brief investigation of the effects of adding the results for re‐dislocation from Murray 2018, which included 50 participants, did not indicate that its inclusion would lead to an important change to the review findings. The study will be included in a future update of this review.
Agreements and disagreements with other studies or reviews
We identified five systematic reviews that evaluated clinical outcomes of conservative care following primary anterior shoulder dislocation and that have been published since 2014 (when the previous version of this review, Hanchard 2014, was completed) (Kavaja 2018; Liu 2014; Longo 2014; Vavken 2014; Whelan 2016 ). Of these, three were limited to the comparison of immobilisation in external versus internal rotation (Liu 2014; Vavken 2014; Whelan 2016); whereas Longo 2014 and Kavaja 2018 had a broader scope. Longo 2014 was designed to compare surgical versus conservative interventions, but included the comparison of immobilisation in external versus internal rotation after closed reduction. Kavaja 2018 included any interventions for treating patients after a traumatic shoulder dislocation or with chronic post‐traumatic shoulder instability. The reviews differed in the numbers of included studies, which is mostly attributable to their publication date. None of the reviews included Chan 2018. Kavaja 2018, the most recently published review, did not include Taskoparan 2010, the reason being that quasi‐randomised trials were not included in this review.
The most commonly assessed outcome in the reviews was re‐dislocation or recurrence, which was assessed by all. Four of the reviews agreed with our findings of no evidence of a difference in the rate of re‐dislocation between immobilisation in external versus internal rotation following closed reduction (Kavaja 2018; Liu 2014; Vavken 2014; Whelan 2016). All four reviews pooled data on re‐dislocation or recurrence, with overall similar estimates despite some variability in the approaches to meta‐analysis. For example, some reviews — Liu 2014,Longo 2014 and Vavken 2014 — included data from Itoi 2007 in their meta‐analysis, hence synthesizing recurrence (re‐dislocation or subluxation) rather than re‐dislocation alone. In contrast to the findings from our review and the four other reviews, Longo 2014 was alone in reporting finding that immobilisation in external rotation resulted in a lower rate of re‐dislocation compared with internal rotation. This may be because Longo 2014 pooled data from just four studies (Finestone 2009; Itoi 2003;Itoi 2007;Taskoparan 2010). Of note: we excluded Itoi 2003 in favour of the reportedly definitive Itoi 2007 to avoid the potential risk of including data from duplicate populations.
Four of the reviews conducted subgroup analyses related to the participants' age, based on subgroups of under 30 years and over 30 years (Kavaja 2018; Liu 2014; Longo 2014; Vavken 2014; Whelan 2016). While we have presented the available data for different age categories, we consider there are insufficient data to justify conducting subgroup analysis. The findings of the other reviews were in agreement with our findings in relation to other outcomes, as far as these were addressed.
All five reviews considered that results were affected by methodological limitations and risk of bias in the included studies. The two reviews using GRADE assessed the evidence for re‐dislocation or recurrence as low quality (Kavaja 2018; Liu 2014); these assessments were based on a different set of trials than those included in our review.
Authors' conclusions
Implications for practice.
All currently available evidence from randomised controlled trials on conservative management following closed reduction of traumatic anterior dislocation of the shoulder relates to the comparison of immobilisation of the shoulder in external rotation versus internal rotation. Overall, there is insufficient evidence to determine whether immobilisation in external rotation confers any benefit over immobilisation in internal rotation. While there is some evidence in favour of immobilisation in external rotation, the findings are overall uncertain and therefore do not allow for the conclusion that immobilisation in external rotation is more effective than immobilisation in internal rotation. Moreover, there is insufficient evidence on adverse events to enable proper assessment of potential harms. The low certainty of the evidence for re‐dislocation means that further research is very likely to have an important impact on our confidence in the estimate of effect. The very low certainty of the evidence for all other outcomes means that any estimate of effect is very uncertain. The effects of the interventions in different subgroups of patients, such as patients in a specific age group or patients with or without concomitant injuries, is unclear. Thus, there remains a lack of evidence to inform the optimal choice of interventions in clinical practice.
Implications for research.
There remains a need for sufficiently powered, high‐quality and well‐reported (i.e. CONSORT‐compliant) randomised controlled trials of key conservative interventions following closed reduction after traumatic anterior shoulder dislocation. While some methodological aspects, such as blinding of participants and personnel, may not always be feasible, others, such as concealed allocation and blinded outcome assessment, are generally feasible and should therefore always be done as they would improve the quality and validity of future results.
Of the four key comparisons that we prespecified as reflecting priority questions (see Types of interventions), only one was addressed by the included trials. Regarding treatment with immobilisation, there is a need for evaluations of further aspects of the use and duration of immobilisation, such as, for example, immobilisation versus no immobilisation, immobilisation for one week versus three weeks, or a strict immobilisation regimen versus a regimen regulated by the patient, and the timing for resumption of activities that may provoke re‐dislocation or recurrent symptoms. Future investigations should carefully attend to the evaluation of different subgroups of participants to allow for the differentiation of effects between patients who are at different risks for re‐dislocation. It would be helpful if investigators consider the research on literature on risk factors for re‐dislocation. Two recent evidence syntheses suggests that patients' age, presence or absence of greater humeral tuberosity fractures, and patients' sex may be key factors to consider (Olds 2015; Wasserstein 2016). There is a clear need for trials evaluating other conservative interventions, such as physiotherapy.
Future trials should give careful attention to the choice and definition of outcome measures. Investigators should use well‐defined and validated functional outcome measures, and should include measures of health‐related quality of life and satisfaction with treatment, as these have not yet been evaluated. There is a need for more data on adverse events. The collection of adverse events data ad hoc, in the absence of pre‐defined definitions or strategies for data collection, is a serious flaw that casts doubt on the completeness of data and hampers comparison of beneficial and harmful effects. In future studies, key categories of potential adverse events should be established prospectively, and an active strategy should be put in place for collecting these data. Categories should be reported on even if they contain no events. Attention should further be given to the appropriate handling (and reporting) of missing data to minimise the risk of attrition bias.
There is a need for more consistency and homogeneity across trials regarding relevant aspects including, in particular, follow‐up points to enhance comparability across trials. Considering that most re‐dislocations appear to occur within the first year after the initial dislocation, a primary follow‐up of one year or longer seems reasonable, which could be supplemented by shorter or longer follow‐ups to allow for more differentiated judgements regarding short‐term, medium‐term and long‐term effects. The availability of individual participant data would be helpful to allow for differential subgroup analyses related to aspects such as age.
Future studies should also include economic data and consider conducting economic (i.e. cost‐effectiveness) analyses.
To ensure that efforts are not duplicated, researchers should consult trial registries before planning further research in this area. This particularly relates to the comparison between immobilisation in external versus internal rotation, along with research that is complementary to these; in these areas, pressing priorities include completion of ongoing work and publication of completed work.
What's new
| Date | Event | Description |
|---|---|---|
| 26 April 2018 | New search has been performed | For this version of the review, published in 2019, the following changes were made. 1. The search was updated to May 2018. 2. Some additional subject headings were added to the database search strategy. 3. Four main comparisons covering priority questions were listed prospectively. 4. The risk of bias assessment was expanded to include separate consideration of single or categories of outcomes in relation to blinding of outcome assessment and completeness of outcome data. 5. One adjusted and one new subgroup analysis was added prior to the search update. |
| 26 April 2018 | New citation required and conclusions have changed | New authorship. Although the implications for practice are essentially unchanged, those for research have been expanded, particularly in relation to patient subgroups and risk factors for re‐dislocation, and timing of follow‐up. |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 1, 2006
| Date | Event | Description |
|---|---|---|
| 1 March 2014 | New search has been performed | For this version of the review, published in 2014, Issue 4, the following changes were made. 1. The search was updated to September 2013. 2. Four new trials (Finestone 2009; Itoi 2007; Liavaag 2011; Taskoparan 2010) were included, and one previously included trial (Itoi 2003) was excluded. 3. In accordance with the policy of The Cochrane Collaboration, the review was updated to include new methodology, including assessment of risk of bias. 4. A 'Summary of findings' table was added. |
| 1 March 2014 | New citation required and conclusions have changed | Although the review conclusions still point to an overall lack of evidence to inform practice, the inclusion of four new trials, all of which compared immobilisation in external rotation versus immobilisation in the traditional position of internal rotation, brought a specific focus to the conclusions. Changes were made to the byline, with one new review author and removal of two previous review authors. |
| 5 September 2008 | Amended | Converted to new review format. |
Acknowledgements
We are very grateful to Nigel Hanchard, Lorna Goodchild and Lucksy Kottam for their contributions as authors to the previous version of this review. We thank Joanne Elliott and Maria Clarke for updating the searches, for conducting the updated searches, and for providing help during the screening process. We are very grateful to Helen Handoll and Joanne Elliott for providing editorial support. We are very grateful to external referees David Annison and Andrew Cuff for their helpful feedback and insights.
We thank Kieran Bentick, Cormac Kelly, Nicholas Noye, Jean‐Christophe Pelet, Stéphane Pelet and Timothy Walker for providing us information on their trials.
Appendices
Appendix 1. Search strategies (2013 to present)
Cochrane CENTRAL (CRS Online)
1 MESH DESCRIPTOR Shoulder Dislocation EXPLODE ALL AND CENTRAL: TARGET 2 (shoulder* AND (dislocat* or sublux* or instability or unstable)):TI,AB,KY AND CENTRAL: TARGET 3 (glenohumeral AND (joint or instability or unstable)):TI,AB,KY AND CENTRAL: TARGET 4 (lesion* AND (Hill Sachs or Bankart)):TI,AB,KY AND CENTRAL: TARGET 5 1 or 2 or 3 or 4 6 (immobilis* or immobiliz* or sling* or conservativ* or therap* or physiother* or rehabilitat* or mobilis* or mobiliz* or train* or exercis* or (physical AND therap*)): AB,KW.TI AND CENTRAL: TARGET 7 MESH DESCRIPTOR Exercise AND CENTRAL: TARGET 8 MESH DESCRIPTOR Exercise Therapy EXPLODE ALL AND CENTRAL: TARGET 9 MESH DESCRIPTOR REHABILITATION EXPLODE ALL AND CENTRAL: TARGET 10 MESH DESCRIPTOR Physical Therapy Modalities AND CENTRAL: TARGET 11 MESH DESCRIPTOR IMMOBILIZATION EXPLODE ALL AND CENTRAL: TARGET 12 6 or 7 or 8 or 9 or 10 or 11 13 5 and 12 14 01/09/2013_TO_21/05/2018: CRSCREATED AND CENTRAL: TARGET 15 13 AND 14
MEDLINE (Ovid Web)
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R)
1 Shoulder Dislocation/ 2 (shoulder$ adj3 (dislocat$ or sublux$ or instability or unstable)).tw. 3 (glenohumeral adj (joint or instability or unstable)).tw. 4 (lesion$1 adj (Hill Sachs or Bankart)).tw. 5 1 or 2 or 3 or 4 6 (immobilis$ or immobiliz$ or sling$ or conservativ$ or therap$ or physiother$ or rehabilitat$ or mobilis$ or mobiliz$ or train$ or exercis$ or physical therap$).tw. 7 Exercise/ or exp Exercise Therapy/ or exp REHABILITATION/ or Physical Therapy Modalities/ or exp IMMOBILIZATION/ 8 (rh or th).fs. 9 6 or 7 or 8 10 5 and 9 11 randomized controlled trial.pt. 12 controlled clinical trial.pt. 13 randomized.ab. 14 placebo.ab. 15 drug therapy.fs. 16 randomly.ab. 17 trial.ab. 18 groups.ab. 19 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 20 exp Animals/ not Humans.sh. 21 19 not 20 22 10 and 21 23 (201309* or 201310* or 201311* or 201312* or 2014* or 2015* or 2016* or 2017* or 2018*).ed,dt. 24 22 and 23
Embase (Ovid Web)
1 Shoulder Dislocation/ or Bankart Lesion/ 2 (shoulder$ adj3 (dislocat$ or sublux$ or instability or unstable)).tw. 3 (glenohumeral adj (joint or instability or unstable)).tw. 4 (lesion$1 adj (Hill Sachs or Bankart)).tw. 5 1 or 2 or 3 or 4 6 (immobilis$ or immobiliz$ or sling$ or conservativ$ or therap$ or physiother$ or rehabilitat$ or mobilis$ or mobiliz$ or train$ or exercis$ or physical therap$).tw. 7 (rh or th).fs. 8 Conservative Treatment/ or Physiotherapy/ or exp Exercise/ or Rehabilitation/ or exp immobilization/ 9 6 or 7 or 8 10 5 and 9 11 exp Randomized Controlled Trial/ 12 exp Double Blind Procedure/ 13 exp Single Blind Procedure/ 14 exp Crossover Procedure/ 15 Controlled Study/ 16 11 or 12 or 13 or 14 or 15 17 ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. 18 (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 19 ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 20 (cross?over$ or (cross adj1 over$)).tw. 21 ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 22 17 or 18 or 19 or 20 or 21 23 16 or 22 24 limit 23 to human 25 10 and 24 26 (201309* or 201310* or 201311* or 201312* or 2014* or 2015* or 2016* or 2017* or 2018*).dc. 27 25 and 26
CINAHL (EBSCO)
S1 (MH "Shoulder Dislocation") S2 TI ( (shoulder N3 dislocat*) or (shoulder N3 sublux*) or (shoulder N3 instability) or (shoulder N3 unstable) ) OR AB ( (glenohumeral N3 joint) or (glenohumeral N3 instability) or (glenohumeral N3 unstable) ) S3 TI ( (glenohumeral N3 joint) or (glenohumeral N3 instability) or (glenohumeral N3 unstable) ) OR AB ( (glenohumeral N3 joint) or (glenohumeral N3 instability) or (glenohumeral N3 unstable) ) S4 TI ( (lesion* N3 Hill Sachs) or (lesion* N3 Bankart) ) OR AB ( (lesion* N3 Hill Sachs) or (lesion* N3 Bankart) ) S5 S1 or S2 or S3 or S4 S6 TI ( (immobilis* or immobiliz* or sling* or conservativ* or therap* or physiother* or rehabilitat* or mobilis* or mobiliz* or train* or exercis* or physical therap*) ) OR AB ( (immobilis* or immobiliz* or sling* or conservativ* or therap* or physiother* or rehabilitat* or mobilis* or mobiliz* or train* or exercis* or physical therap*) ) S7 (MH "Rehabilitation+") or (MH immobilization or immobilisation) or (MH “physical therapy”) S8 MW rh OR MW th S9 S6 or S7 or S8 S10 S5 and S9 S11 (MH "Clinical Trials+") S12 (MH "Evaluation Research+") S13 (MH "Comparative Studies") S14 (MH "Crossover Design") S15 PT Clinical Trial S16 (MH "Random Assignment") S17 S11 or S12 or S13 or S14 or S15 or S16 S18 TX ((clinical or controlled or comparative or placebo or prospective or randomi?ed) and (trial or study)) S19 TX (random* and (allocat* or allot* or assign* or basis* or divid* or order*)) S20 TX ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) S21 TX ( crossover* or 'cross over' ) or TX cross n1 over S22 TX ((allocat* or allot* or assign* or divid*) and (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)) S23 S18 or S19 or S20 or S21 or S22 S24 S17 or S23 S25 S10 and S24 S26 EM 2013 OR EM 2014 OR EM 2015 OR EM 2016 OR EM 2017 OR EM 2018 S27S25 and S26
PEDro
1. Abstract & Title: dislocate* Body Part: upper arm, shoulder or shoulder girdle Method: clinical trial New records added since 01/09/2013 Match all search terms (AND)
2. Abstract & Title: sublux* Body Part: upper arm, shoulder or shoulder girdle Method: clinical trial New records added since 01/09/2013 Match all search terms (AND)
3. Abstract & Title: instability Body Part: upper arm, shoulder or shoulder girdle Method: clinical trial New records added since 01/09/2013 Match all search terms (AND)
WHO ICTRP
1. shoulder dislocation AND Immobiliz* OR shoulder dislocation AND immobilis* OR shoulder dislocation AND sling* OR shoulder dislocation AND conservativ* OR shoulder dislocation AND therap* OR shoulder dislocation AND exercis* OR shoulder dislocation AND rehabilitat* OR shoulder dislocation AND physiother* OR shoulder dislocation AND train* OR shoulder dislocation AND mobiliz* OR shoulder dislocation AND mobilis* OR shoulder dislocation AND external rotation OR shoulder dislocation AND brace*
2. shoulder instability AND Immobiliz* OR shoulder instability AND immobilis* OR shoulder instability AND sling* OR shoulder instability AND conservativ* OR shoulder instability AND therap* OR shoulder instability AND exercis* OR shoulder instability AND rehabilitat* OR shoulder instability AND physiother* OR shoulder instability AND train* OR shoulder instability AND mobiliz* OR shoulder instability AND mobilis* OR shoulder instability AND external rotation OR shoulder instability AND brace*
3. glenohumeral AND Immobiliz* OR glenohumeral AND immobilis* OR glenohumeral AND sling* OR glenohumeral AND conservativ* OR glenohumeral AND therap* OR glenohumeral AND exercis* OR glenohumeral AND rehabilitat* OR glenohumeral AND physiother* OR glenohumeral AND train* OR glenohumeral AND mobiliz* OR glenohumeral AND mobilis* OR glenohumeral AND external rotation OR glenohumeral AND brace*
4. bankart lesion AND Immobiliz* OR bankart lesion AND immobilis* OR bankart lesion AND sling* OR bankart lesion AND conservativ* OR bankart lesion AND therap* OR bankart lesion AND exercis* bankart lesion AND rehabilitat* OR bankart lesion AND physiother* OR bankart lesion AND train* OR bankart lesion AND mobiliz* OR bankart lesion AND external rotation OR bankart lesion AND brace*
5. Hill Sachs AND Immobiliz* OR Hill Sachs AND immobilis* OR Hill Sachs AND sling* OR Hill Sachs AND conservativ* OR Hill Sachs AND therap* OR Hill Sachs AND exercis* Hill Sachs AND rehabilitat* OR Hill Sachs AND physiother* OR Hill Sachs AND train* OR Hill Sachs AND mobiliz* OR Hill Sachs AND mobilis* OR Hill Sachs AND external rotation OR Hill Sachs AND brace*
ClinicalTrials.gov
1. shoulder dislocation AND (Immobilization OR immobilisation OR sling OR conservative OR therapy OR exercise OR rehabilitation OR physiotherapy OR training OR mobilization OR mobilisation) | First posted from 09/01/2013 to 05/22/2018
2. bankart lesion AND (Immobilization OR immobilisation OR sling OR conservative OR therapy OR exercise OR rehabilitation OR physiotherapy OR training OR mobilization OR mobilisation) | First posted from 09/01/2013 to 05/22/2018
3. glenohumeral subluxation AND (Immobilization OR immobilisation OR sling OR conservative OR therapy OR exercise OR rehabilitation OR physiotherapy OR training OR mobilization OR mobilisation) First posted from 09/01/2013 to 05/22/2018
Data and analyses
Comparison 1. Immobilisation in external versus internal rotation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Re‐dislocation at ≥ 12 months follow‐up (nearest to 24 months accepted) | 6 | 488 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.38, 1.19] |
| 2 Re‐dislocation data at last follow‐up | Other data | No numeric data | ||
| 3 Re‐dislocation, interim follow‐ups (3 and 12 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Re‐dislocation, 12 months follow‐up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Re‐dislocation, 3 months follow‐up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Re‐dislocation: stratified according to external rotation with / without abduction | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 External rotation without abduction | 4 | 320 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.61, 1.44] |
| 4.2 External rotation with abduction | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 2.46] |
| 5 Validated patient‐reported outcome measures for shoulder disability (OSI, WOSI) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 WOSI at 33 months follow‐up (total score) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 WOSI at mean 25 months follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Validated PROMS: non‐parametric results | Other data | No numeric data | ||
| 6.1 Final follow‐up | Other data | No numeric data | ||
| 6.2 Interim follow‐up | Other data | No numeric data | ||
| 7 Resumption of pre‐injury activities | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Return to pre‐injury sports at 24 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Return to sports at any level at 24 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Return to pre‐injury sports activity level at 24 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 Return to pre‐injury level of activity of affected arm at ≥ 24 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Any instability (subluxation or subjective instability, individually or grouped into composite outcome) | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Recurrent instability | 3 | 395 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.62, 1.14] |
| 8.2 Positive apprehension test or re‐dislocation | 2 | 135 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.14, 0.57] |
| 9 Adverse events | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Transient and resolved adverse events | 4 | 377 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.73 [0.83, 9.02] |
| 9.2 Important adverse events | 3 | 268 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.08, 4.46] |
| 10 Adherence to treatment | 6 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11 Subsequent surgery | 4 | 327 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.44, 1.30] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chan 2018.
| Methods |
Aim: "...to find out if an ‘off the shelf’ ER [external rotation] brace (Smartsling, Ossur, Reykjavik, Iceland) providing 30°of external rotation would reduce re‐dislocation rates and improve functional outcome in patients presenting with a shoulder dislocation, compared to a conventional sling." Method of randomisation: independently by telephone Assessor blinding: unclear Intention‐to‐treat analysis: yes Loss to follow‐up: there were discrepancies within the report (see notes). In the flow diagram, losses to follow‐up were reported as 18 (25%), comprising 6/36 (17%) in Group A and 12/36 (33%) in Group B at 12 months; and 15 (21%) comprising 6/36 (17%) in Group A and 9/36 (25%) in Group B at 24 months. These numbers relate to the secondary outcome; for the primary outcome, data were missing from only 3 participants (8%) in each group |
|
| Participants |
Setting: 6 (NHS) hospitals in England, UK Period of data collection: September 2006 to February 2011 Participants: 72 (the initial aim was to recruit 160 participants; however, the trial was discontinued early due to slow recruitment) Inclusion criteria: first‐time traumatic anterior shoulder dislocation; confirmation of diagnosis by radiography Exclusion criteria: associated fractures; indication for surgery (as determined by the recruiting surgeon); inability to provide informed consent; learning difficulties; mental illness; dementia; significant comorbidities; unwillingness to participate Sex: 61 (85%) male Age: median age Group A 25 years (range 17 to 44) years; Group B 23.8 (range 16 to 43) years Pre‐injury status: no information Assigned: 36/36 (Group A/B) Assessed: 30/27 (at final follow‐up) |
|
| Interventions |
Group A: immobilisation in an external rotation brace (Smartsling, Ossur, Reykjavik, Iceland) "which held the arm in 30° of external rotation and 30° of abduction" (p.3) Group B: immobilisation in internal rotation in a conventional sling (Polysling, Mölnlnlycke Health Care, Gothenburg, Sweden) Both groups: the braces and slings were provided in the clinic by "an appropriately trained member of staff (usually a surgeon, nurse or healthcare assistant)", and all participants were immobilised within 5 days after dislocation (additional information provided by contact author). Patients were instructed to wear the brace or sling for 4 weeks, both day and night, except when showering or bathing. It is not clear who applied the brace or sling or gave the accompanying instructions. Patients were instructed (by a physiotherapist) on a course of shoulder exercises and were provided with written information and advice for exercising at home. Compliance with exercising was reinforced through a telephone call by the trial coordinator a few days after the brace or sling had been applied |
|
| Outcomes | Clinical reviews were conducted at 3, 12 and 24 months post dislocation Prespecified as primary outcome Re‐dislocation (within 24 months): no information is provided on how re‐dislocation was assessed/confirmed. Data were collected by telephone interview if patients did not attend follow‐up appointments Prespecified as secondary outcomes Recurrent instability: measured with the Oxford Shoulder Instability questionnaire (OSI) (at 12 and 24 months) Surgery: "Any shoulder stabilization surgery during the study period was noted." (p.3) Difficulties with wearing the slings and braces: assessed with a questionnaire |
|
| Notes | Additional details of this study, including data for re‐dislocation at the 3 months' follow‐up, were provided by 1 of the study authors, Dr Kieran Bentick (personal communication 1 September 2018) The precise method used for the reduction of the shoulder dislocation is not specified ("All trial participants received standard manipulation under local or general anaesthetic to reduce the dislocation in the acute setting..." [p.3]) Unit of analysis: in this study, there were 72 cases of dislocation in 71 patients. 1 patient experienced a dislocation of the right shoulder 3 years after the dislocating the left, and was randomised twice (additional information provided by contact author) Loss to follow‐up: discrepant numbers were reported in the flow diagram, text and outcome table, and different numbers of participants were reported for the outcomes. The discrepancies were explained by the contact author as follows (personal communication, 1 September 2018): "At the conclusion of the trial once the data had been collected patients were contacted and further information was gained from records held at the hospitals randomising the patients. This was achieved by reviewing clinic letters from additional appointments. Between the two sufficient information was acquired to ascertain when and whether further dislocations had occurred in most cases (33 in each group). The consort flow diagram was however not altered." Recurrent instability/OSI (at 24 months): this was specified both as a primary and a secondary outcome in the Methods section of the report, but was reported only with the secondary outcomes in the Results section; hence, it was considered a secondary outcome in this review Relationship between this and previous reports: in the conference abstract by Kelly 2011 (included as study awaiting classification in Hanchard 2014), preliminary results of this study relating to outcomes after 1 year were reported Funding sources and declarations of interest: Funding: "This work was supported by: The British Elbow and Shoulder Society; Institute of Orthopaedics, Robert Jones and Agnes Hunt Hospital, Oswestry Shropshire; Ossur UK provided the ER braces and were not involved in the design, data analysis or preparation of this paper." Declaration of Conflicting Interests: "The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Randomisation was carried out independently by the York Trials Unit by telephone, with participants assigned to receive a conventional sling ... or an ER brace...” (p.3). |
| Allocation concealment (selection bias) | Low risk | Comment: allocation was done centrally (York Trials Unit, by telephone). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Due to the nature of the intervention, blinding of the patient or index surgeon was not possible.” (p.3). Comment: the care providers could also not be blinded. |
| Blinding of outcome assessment (detection bias) Re‐dislocation | Unclear risk | Quote: “Clinical and functional evaluations […] were conducted by site coordinators." (p.3). "All outcomes were [...] collected by a research co‐ordinator.” (p.3). Comment: it is not clear whether these coordinators were blinded. It is unclear how re‐dislocation was diagnosed and verified; outcome data were collected by telephone interview if patients failed to attend follow‐up appointments. It seems that the outcome was at least partly patient‐reported, hence involving subjective assessment. |
| Blinding of outcome assessment (detection bias) Validated PROMs for shoulder instability | High risk | Comment: this outcome (OSI) was patient‐assessed and hence inherently unblinded. The review authors judge that it is likely that the subjective outcome measurement may have been influenced by lack of blinding (considering also that the participants were unblinded to their treatment allocation). |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | Comment: there was insufficient information about how adverse events were assessed to make a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Re‐dislocation, longest or main follow‐up | Low risk | Comment: the amount of attrition for re‐dislocation was 8% and identical in both groups. The review authors considered it unlikely that this amount of losses to follow‐up would have affected the results for re‐dislocation. No missing data were replaced. |
| Incomplete outcome data (attrition bias) Re‐dislocation, other follow‐ups | High risk | Comment: attrition was unbalanced between both groups at the 12 months' and 3 months' follow‐up, and high in the internal rotation group (33% versus 14% at 12 months; 22% versus 8% at 3 months. The reported reason for all losses to follow‐up was the inability to contact these participants. No missing data were replaced. |
| Incomplete outcome data (attrition bias) Validated PROMs for shoulder instability | High risk | Comment: attrition for the OSI was unbalanced between both groups at the 24 months' and 12 months' follow‐up, and high in the internal rotation group (31% versus 17% at 24 months; 33% versus 17% at 12 months. The reported reason for all losses to follow‐up was the inability to contact these participants. No missing data were replaced. |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: there was insufficient information to make a judgement of 'low risk' or 'high risk' of bias. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no registration record or published protocol is available for this study. Kelly 2011, a conference abstract that was included as study awaiting classification in the previous version of the review, provided insufficient information for a judgement. Hence, there is insufficient information available to permit a judgement of ‘low risk’ or ‘high risk’. |
| Other bias | Low risk | Comment: none identified. |
Finestone 2009.
| Methods |
Aim: "To ascertain whether immobilisation after primary traumatic anterior dislocation of the shoulder in external rotation was more effective than immobilisation in internal rotation in preventing recurrent dislocation in a physically active population" Method of randomisation: computer‐generated randomised list Assessor blinding: no Intention‐to‐treat analysis: no information Loss to follow‐up: none |
|
| Participants |
Setting: Accident and Emergency Department of a University hospital, Israel Period of data collection: 1 January 2004 to 31 December 2006 (additional information provided by contact author) Participants: 51 Inclusion criteria: primary anterior dislocation of the shoulder; informed consent. It is unclear whether the exclusive recruitment of males was by chance or by intention Exclusion criteria: injury sustained in a motor vehicle accident; concurrent fracture of the greater tuberosity Sex: 51 male Age: mean 20 years, range 17 to 27 years Pre‐injury status: 22/27 (81.5%) in Group A and 18/24 (75%) in Group B were soldiers (additional information provided by contact author) Assigned: 27/24 (Group A/B) Assessed: 27/24 (at final follow‐up) |
|
| Interventions |
Group A: immobilisation in 15° to 20° of shoulder external rotation in a manufactured device (manufacturer's details not given), except when showering or changing clothes. No information was given on who applied the splint or gave the accompanying instructions Group B: immobilisation in an internal rotation brace with a component encircling the lower arm to maintain elbow adduction, except when showering or changing clothes. No information was given on who applied the splint or gave the accompanying instructions Both groups: after 4 weeks' immobilisation, participants began a standard regimen of physiotherapy (no further details were given). Participants with clinically stable shoulders on the basis of a negative supine apprehension test returned to full activity after 3 months |
|
| Outcomes | Reviews were conducted at 2 and 6 weeks, 3 and 6 months, and 1, 2, 3 and 4 years post‐injury None of the outcomes was prespecified with the methods Re‐dislocation: not further defined; it is unclear whether this was verified by reference to the medical notes, but this is likely to have been so, given the population in question. Identified re‐dislocators were further evaluated: "Those who sustained re‐dislocations were evaluated by either CT or MRI arthrography" (p.919) Adverse events: undefined Adherence: compliance with treatment; undefined (the reported results relate to whether the braces or slings were worn over the full immobilisation period) Surgical intervention: rate of participants with re‐dislocation who had undergone surgery when last reviewed (all were soldiers) |
|
| Notes | At injury, 5/27 (18.5%) in Group A and 5/24 (20.8%) in Group B had sustained axillary nerve neuropraxia. This resolved within 10 weeks in all cases. There were no fractures of the glenoid rim Closed reduction was performed in the Accident and Emergency Department by the Milch technique (n = 41) or the Hippocratic method (n = 10; 7/27 = 25.9% in Group A and 3/24 = 12.5% in Group B (additional information provided by contact author)) Re‐dislocations: these occurred at a mean of 13.8 months (range 4 to 43 months) after the first in Group A, and 12.4 months (range 4 to 46 months) after the first in Group B. Re‐dislocators were evaluated by CT or MRI arthrography. 19/20 (95%) were found to have a Bankart lesion, 1 of which was bony Funding sources and declarations of interest: "This study has been supported by a research grant of the IDF Medical Corporation and Israeli Ministry of Defence. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We aimed to have 55% of the patients in the external rotation brace ... we made up prior to the study 100 patient booklets numbered 001 to 100. Each booklet had a sealed envelope which contained either a slip for external or internal rotation bracing. The slips were placed into their respective envelopes according to a computer generated randomised list based on the file number" (additional information provided by contact author). |
| Allocation concealment (selection bias) | Low risk | Comment: see above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding of participants and personnel (care providers) was not possible. |
| Blinding of outcome assessment (detection bias) Re‐dislocation | Unclear risk | Comment: there is no mention of blinding, and the outcome of "recurrent dislocation" is not sufficiently defined to allow for a clear judgement of 'low risk' or 'high risk' of bias. |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | Comment: there is insufficient information about how adverse events were assessed to allow for a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Re‐dislocation, longest or main follow‐up | Low risk | Comment: outcome data for re‐dislocation is provided for all 51 participants. Participants appear to have been followed up to 4 years or the point of re‐dislocation, whichever was sooner. "No patient was lost to follow up" (additional information provided by contact author). |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: there is insufficient information on how (including from how many participants) data on adverse events and adherence were collected to allow for a judgement of 'low risk' or 'high risk' of bias. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol is available, but most key outcomes were reported. The numbers with clinical instability at 3 months, based on the supine instability test, were not reported. Group data on the numbers of participants requiring surgery were not given in the paper but were provided on request by the contact author. |
| Other bias | Low risk | Comment: none identified. |
Heidari 2014.
| Methods |
Aim: to compare "the effectiveness of the nonsurgical treatments of immobilization in abduction and external rotation vs immobilization in adduction and internal rotation after the primary anterior shoulder dislocation. We aimed to compare functional outcome and stability results between these two positions of shoulder stabilization." Method of randomisation: computer‐generated randomisation scheme Assessor blinding: unclear Intention‐to‐treat analysis: yes (unclear wording in the Methods section of the report; however, all participants received the intervention they were allocated to) Loss to follow‐up: 5 (5%) comprising 3/51 (6%) in Group A and 2/51 (4%) in Group B |
|
| Participants |
Setting: emergency department of a university‐affiliated hospital, Iran Period of data collection: October 2011 to March 2013 Participants: 102 Inclusion criteria: primary unilateral anterior dislocation of the shoulder (all patients were initially assessed by radiography); presentation to the emergency department within 6 hours post‐injury; age 15 to 55 years; willingness to be followed up Exclusion criteria: previous shoulder problems; surgical joint repair; multidirectional instability; shoulder injuries requiring surgical intervention; associated fractures of the shoulder according to results of routine radiographic examination; unwillingness to be followed up for 24 months. Sex: 91 (89%) male Age: 35.8 years, SD 8.9 years Subgroups: by age < 20 years; 21 to 30 years; 31 to 40 years; ≥ 41 years Pre‐injury status: 31/51 in Group A and 38/51 sustained their injury in sport activities. 20/51 in Group A and 13/51 in Group B sustained their injury in a trauma Assigned: 51/51 (Group A/B) Assessed: 48/49 (at final follow‐up) |
|
| Interventions |
Group A: immobilisation for 3 weeks in 15° of abduction and 10° of external rotation in a "stabilizer brace with an adjustable angle of abduction" (picture provided in study report). Part of the (fixation of the) brace came from Velcro (Velcro USA Inc, Manchester, NH, USA) Group B: immobilisation for 3 weeks in internal rotation in a "sling and swathe bandage" (not further described) Both groups: presumably, immobilisation started very soon after dislocation (all included presented to the emergency department within 6 hours). It is not clear who applied the brace or sling or gave the accompanying instructions. Patients were instructed to remove their brace or sling only during showering and were advised "to be cautious about hyperextension of the joint". They were further asked not "to change the position of the brace and to use the contralateral upper extremity to perform activities.” Following the immobilisation period, all participants underwent an identical exercise‐based rehabilitation program, which was supervised by a physiotherapist. No information is provided on the duration, frequency and intensity of rehabilitation. The participants were advised not to initiate sportive activities for at least 3 months post‐intervention |
|
| Outcomes | Follow‐up assessments were conducted at 3 weeks post‐intervention, at 24 months post‐dislocation and 33 months (WOSI only) post‐dislocation Prepecified as primary outcome Re‐dislocation: "defined as the humeral head being completely or partially out of the glenoid socket that reduced spontaneously or by manual maneuver." At the 3‐week follow‐up patients were asked whether they had experienced any further dislocations. It seems that outcomes at 24 and 33 months were mostly collected by telephone interviews (in cases where the patient could not be contacted, efforts were made to arrange for a direct examination at a clinic or at the patient's home) Prespecified as secondary outcomes Instability ‒anterior apprehension test (at the 3‐week follow‐up), tested in supine position, with the arm being placed in 90° of shoulder abduction and 90° of elbow flexion; stress on the glenohumeral joint was applied by an external rotation force "until the patient became apprehensive". The feeling that the shoulder would "come out of joint" was considered a positive test result Return to pre‐injury sports: not further specified Adherence: "proportion of non‐cooperative patients", assessed by the question: "Please indicate how many hours a day and for how long you wore the immobilizer." Participants who took off the brace or sling during the immobilisation period, except when taking a shower, were defined as non‐cooperative participants Western Ontario Shoulder Instability Index (WOSI) Adverse events:not prespecified as an outcome, undefined Surgical intervention:not prespecified as an outcome."Patients in both groups who experienced recurrent symptomatic instability at any time during the study underwent surgical intervention according to the orthopedic surgeon’s discretion." (p.761). This is not further addressed; it is unclear whether patients who underwent surgery were excluded from the study |
|
| Notes | The methods used for reduction of the shoulder dislocation were the traction‐countertraction manoeuvre in 79 patients (77.4%) and Kocher’s method in 23 (22.6%) Not all outcomes were assessed at all follow‐up time points. At the 33‐month follow‐up, only the WOSI was assessed. Results for the WOSI are only reported for the 33‐month follow‐up. No results are reported for the follow‐up at 3 weeks post‐intervention. The presented results for re‐dislocation, apprehension and return to sports relate to the 24‐month follow‐up, same as for adverse events Funding and declarations of interest: "The investigation was financially supported by a grant from Shahid Beheshti University of Medical Sciences, Iran (No. 16X‐03B‐76349). The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomly assigned (in a 1:1 ratio) … according to a computer‐generated randomization scheme." (p.760). |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Each … physician was provided with a set of opaque envelopes containing group assignment.” (p.760). Comment: it remains unclear whether envelopes were sequentially numbered, and sealed. Hence, the information was considered insufficient to permit a definitive judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding of participants and personnel (care providers) was not possible. |
| Blinding of outcome assessment (detection bias) Re‐dislocation | Unclear risk | Comment: there was no mention of blinding. It seems that re‐dislocation at 24 months was mostly assessed by telephone interview, i.e. subjectively. |
| Blinding of outcome assessment (detection bias) Validated PROMs for shoulder instability | High risk | Comment: the WOSI was patient‐assessed and hence inherently unblinded. The review authors judge that it is likely that estimates may have been influenced by lack of blinding (considering also that the participants were unblinded to their treatment allocation). |
| Blinding of outcome assessment (detection bias) Resumption of pre‐injury activities/sports | Unclear risk | Comment: return to sportive activities was patient‐assessed and was hence inherently unblinded. The review authors judged that it is possible that the outcome measurement may have been influenced by lack of blinding. However, this outcome was judged to be less prone to bias than other patient‐reported outcomes and risk of bias was therefore rated as unclear. |
| Blinding of outcome assessment (detection bias) Any instability | Unclear risk | Comment: the positive apprehension test was conducted by an examiner. However, as there was no mention of blinded outcome assessors, a judgement of ‘low risk’ or ‘high risk’ was not possible. |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | Comment: there was insufficient information about how adverse events were assessed to make a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Re‐dislocation, longest or main follow‐up | Low risk | Comment: there were reportedly no losses up to the 24‐month follow‐up; hence, this is not considered a potential source of bias. No information is provided about the planned or applied approach to missing outcome data; however, it seems that no missing data were replaced. |
| Incomplete outcome data (attrition bias) Validated PROMs for shoulder instability | Low risk | Comment: the amount of losses to the 33‐month follow‐up was small and similar across the groups (3/51 (6%) in Group A and 2/51 (4%) in Group B). |
| Incomplete outcome data (attrition bias) Resumption of pre‐injury activities | Low risk | Comment: the numbers of participants for whom resumption of pre‐injury activities is reported relate to a subgroup of participants. In view of the small number or losses to follow‐up, risk of attrition bias for this outcome was rated as low. |
| Incomplete outcome data (attrition bias) Any instability | Low risk | See above. |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: there was insufficient information to make a judgement of 'low risk' or 'high risk' of bias. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no registration record or published protocol is available for this study. There is insufficient information available to permit a judgement of ‘low risk’ or ‘high risk’. 2 outcomes (adverse effects and surgical intervention) were not prespecified with the methods but were reported with the results. |
| Other bias | Low risk | Comment: none identified. |
Itoi 2007.
| Methods |
Aim: "To report the two‐year results of a study testing the hypothesis that immobilization in external rotation versus internal rotation would reduce the recurrence rate after initial traumatic anterior dislocation of the shoulder" Method of randomisation: random number table Assessor blinding: no Intention‐to‐treat analysis: yes Loss to follow‐up: 39/198 (19.7%), comprising 19/104 (18.3%) in Group A and 20/94 (21.3%) in Group B |
|
| Participants |
Setting: Akita Hospital and 11 other institutes across Japan Period of data collection: October 2000 to March 2004 Participants: 198 Inclusion criteria: initial anterior dislocation caused by a substantial traumatic event; presentation within 3 days (including the day of dislocation); no associated fracture visible on routine radiographic examination; informed consent Exclusion criteria: no information was given Sex: 136 male (67%) Age: mean 37 years, range 12 to 90 years Subgroups: By age ≤ 20 years; 21 to 30 years; ≤ 30 years; 31 to 40 years; ≥ 41 years By interval between dislocation and immobilisation: 0 days; 1 day; 2 days By age and interval between dislocation and immobilisation: age ≤ 30 years and interval 0 days; age ≤ 30 years and interval 1 day; age ≤ 30 years and interval 2 days Pre‐injury status: 71/104 (68.3%) in Group A and 64/94 (68.1%) in Group B sustained their injury in sport. Among participants aged < 30 years, 53/56 (94.6%) in Group A and 39/42 (92.3%) in Group B sustained their injury in sport Assigned: 104/94 (Group A/B) Assessed: 85/74 (at final follow‐up) |
|
| Interventions |
Group A: immobilisation in 10° of external rotation, except when showering. Until November 2003, this was achieved using a wire‐mesh splint covered with sponge and stockinette (see Itoi 2003 for details). Starting in November 2003, a prototype manufactured brace was used (Alcare, Tokyo, Japan). Both methods appeared to limit wrist mobility. The treating surgeons (possibly authors of the report) applied the splintage and gave the accompanying instructions Group B: immobilisation in a sling and swathe except when showering. The treating surgeons (possibly authors of the report) applied the splintage and gave the accompanying instructions Both groups: immobilisation commenced between zero and 2 days post dislocation (day 1 to 3) and was continued for 3 weeks. Afterwards, rehabilitation comprised self‐directed active and passive range‐of‐motion exercises. Avoidance of vigorous sports activities for at least 3 months was advised |
|
| Outcomes | Follow‐up reviews were conducted at 6, 12 and 24 months (presumably after initiation of immobilisation), face‐to‐face or by telephone Prespecified as the primary outcome Self‐reported re‐dislocation or subluxation: dislocation was defined as "the humeral head being completely out of the glenoid socket until a reduction maneuver was performed, and subluxation was defined as the humeral head being completely or partially out of the glenoid socket but reducing spontaneously." (p.2127). The participants were asked whether they had experienced any further dislocation or subluxation after the immobilization Implicitly secondary outcomes Return to pre‐injury sport: at any level (subgroup who sustained injury in sport); at pre‐injury level (subgroup who sustained injury in sport); at any level (subgroup aged ≤ 30 years who sustained injury in sport); at pre‐injury level (subgroup aged ≤ 30 years who sustained injury in sport) Adherence: use of splint full‐ or part‐time for full 3 weeks; use of splint full‐time for full 3 weeks Adverse events:not prespecified as an outcome, undefined Surgical intervention: participants with recurrent dislocations or subluxations who "eventually underwent surgical stabilization" (p.2128) |
|
| Notes |
Relationship between this and previous reports: the full trial report of Itoi 2003 indicated that this was a preliminary study. A subsequent (2004) abstract stated that it was an interim report of an ongoing trial, referred to the random assignment of 96 participants and reported results for 80 participants. The selection criteria had changed in that participants with recurrent dislocations were now included, but humeral fractures were explicitly excluded, as were shoulders not immobilised within 3 days of injury. The mean follow‐up time in the 2004 abstract was 12.4 months Correspondence with Prof Itoi (July 2005) revealed that the trial was still ongoing. Results for 131 participants, all with initial dislocations, were reported at an Instructional Course Lecture (Principles and procedures for shoulder instability: an international perspective: non‐operative management of anterior instability) at the meeting of the American Academy of Orthopaedic Surgeons in 2005 (handout provided to authors by Prof Itoi) Itoi 2007 reports results for 198 participants with initial dislocation, recruited from October 2000, and correspondence with Prof Itoi (8 April 2011) indicates that this study sample does not incorporate that of Itoi 2003. However, the start point and selection criteria of Itoi 2007 may not have been determined prospectively, contributing to the grading of “unclear” in the “selection bias” section of the risk of bias table Method of reduction: manual reduction was by the elevation method (101 shoulders, 57 in Group A), the Hippocratic method (22 shoulders, 13 in Group A), the external rotation method (17 shoulders, 8 in Group A), the Kocher method (16 shoulders, 6 in Group A), the Stimson method (14 shoulders, 8 in Group A) and other methods (28 shoulders) (additional information provided by contact author) External rotation brace: adoption of the Alcare brace, which was easier to do on and off than the wire‐mesh splint, may have influenced adherence, as well as positioning and standardisation, part way through the study Re‐dislocations: mostly occurred during the first year (82% of those in Group A and 84% of those in Group B) Funding and declarations of interest: "In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants of less than $10,000 from Alcare, Tokyo, Japan. One or more of the authors, or a member of his or her immediate family, received, in any one year, payments or other benefits of less than $10,000 or a commitment or agreement to provide such benefits from a commercial entity (Al‐ care, Tokyo, Japan). No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed with the use of a random‐number table created by the principal investigator. Co‐investigators allocated the patients at their institutes with the use of this random number table." (p.2125). |
| Allocation concealment (selection bias) | High risk | Comment: the random‐number table was probably open: see above. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding of participants and personnel (care providers) was not possible. The instructions on the immobilisation protocol were given by the treating surgeons. Quote: "We and the other treating surgeons might have made a stronger effort to ensure adherence to the external rotation immobilization". |
| Blinding of outcome assessment (detection bias) Resumption of pre‐injury activities/sports | Unclear risk | Comment: return to sports was patient‐assessed and was hence inherently unblinded. The review authors judged that it is possible that the outcome measurement may have been influenced by lack of blinding. However, this outcome was judged to be less prone to bias than other patient‐reported outcomes and risk of bias was therefore rated as unclear. |
| Blinding of outcome assessment (detection bias) Any instability | High risk | Comment: there is no mention of blinding. Recurrence, which comprised self‐reported re‐dislocation or subluxation, was clearly defined, but subluxation is inevitably subjective. |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | There was insufficient information about how adverse events were assessed to make a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Resumption of pre‐injury activities | High risk | The numbers of participants for whom resumption of pre‐injury sports activities is reported relate to a subgroup of participants. It is likely that the high number of losses to follow‐up attrition may have affected the results of this outcome. |
| Incomplete outcome data (attrition bias) Any instability | High risk | Comment: attrition for recurrent instability was high in both groups (18.3% in Group A and 21.3% in Group B), and no reasons were provided. No information is provided about the planned or applied approach to missing outcome data; however, it seems that no missing data were replaced. |
| Incomplete outcome data (attrition bias) Adverse events | High risk | There was insufficient information. However, in view of the high number of losses to follow‐up, risk of attrition bias was judged as high for this outcome, too. |
| Selective reporting (reporting bias) | High risk | Comment: no protocol is available. Key outcomes were reported, but the start point and selection criteria are inconsistent across reports and may not have been determined prospectively. |
| Other bias | High risk | Comment: there is disclosure of funding or grants of < $10,000 by Alcare to 1 or more of the authors in support of preparation for the research. There is disclosure of payments or benefits of < $10,000 by Alcare to 1 or more of the authors or their immediate families. |
Liavaag 2011.
| Methods |
Aim: "To compare immobilization in internal rotation and external rotation after anterior shoulder dislocation" Method of randomisation: block randomisation Assessor blinding: no Intention‐to‐treat analysis: yes Loss to follow‐up: 4/188 (2.1%) comprising 2/93 (2.2%) in Group A and 2/95 (2.1%) in Group B as shown in the flow diagram. The reported numbers of participants with outcome data differed across outcomes. For subluxation, the loss to follow‐up was 25/188 (13%), comprising 12/93 (13%) in Group A and 13/95 (14%) in Group B; for return to pre‐injury level of physical activity with the affected shoulder it was 19/188 (10%), comprising 10/93 (11%) in Group A, and 9/95 (9%) in Group B |
|
| Participants |
Setting: Emergency Department of 13 hospitals in Norway Period of data collection: January 2005 to February 2008 Participants: 188 Inclusion criteria: age 16 to 40 years; successful reduction of primary traumatic anterior dislocation documented on conventional radiographs Exclusion criteria: fractured glenoid with a large bony defect (including > 20% of the glenoid rim) or a bony defect involving > 1/3 of the diameter of the glenoid fossa at the same level; fractured greater tuberosity with malalignment after repositioning; neuropathy related to dislocation or reduction; unwillingness or inability to participate Sex: 153 male (81%) Age: mean 26.8 years, SD 7.1 years Subgroups: age 16 to 24 years; age 25 to 40 years Pre‐injury status: 44/93 (47.3%) in Group A and 39/95 (41.1%) in Group B sustained their injury in sport. The ratio of minor to major trauma was 52:41 in Group A and 48:47 in Group B. 2 participants in each group had positive sulcus signs. 6 participants in Group A and 8 in Group B had other signs associated with generalised ligamentous laxity Assigned: 93/95 (Group A/B) Assessed: 91/93 (at final follow‐up) |
|
| Interventions |
Group A: immobilisation in an appropriately sized, manufactured shoulder immobiliser (15‐degree Ultrasling ER, DonJoy, Vista, California) in 15° of external rotation, except when showering. A line at the top of the immobiliser was parallel to the frontal plane when the arm was correctly positioned. The immobiliser incorporated the wrist. No information was given on who applied the immobilisation or gave the accompanying instructions Group B: immobilisation in a collar and cuff or a sling and swathe, except when showering. No information was given on who applied the immobilisation or gave the accompanying instructions Both groups: immobilisation commenced immediately after reduction (within 24 hours after dislocation) and continued for 3 weeks. No information was given on rehabilitation. |
|
| Outcomes | A standardised questionnaire was sent to participants 2 years post‐dislocation. Adherence data were gathered at 3‐week follow‐up Prespecified as the primary outcome Self‐reported (and verified) re‐dislocation: dislocation was defined as the humeral head being completely out of the glenoid until a reduction manoeuvre was performed. Participants recorded the date of the first recurrent dislocation on the questionnaire and this was confirmed by reference to medical records Prespecified as secondary outcomes Self‐reported subluxation: subluxation was defined as the humeral head being partially out of the glenoid Self‐reported recurrent instability: recurrent dislocation or subluxation Resumption of pre‐dislocation level of physical activity Adverse events: assessed with a questionnaire asking whether there were any persistent complaints caused by the shoulder dislocation (additional information provided by contact author) Surgical intervention: "surgical treatment of instability" (p.899) Western Ontario Shoulder Instability Index (WOSI) Adherence: daily immobilisation was recorded as "not at all," "up to 8 hours," "between 8 and 16 hours" and "more than 16 hours". The number of days on which immobilisation was used was also recorded. Participants who used immobilisation for > 16 hours daily for at least 20 days were labelled compliant |
|
| Notes | "There was no difference between the randomised groups in terms of demographic characteristics" at baseline Physicians were allowed to choose the method of reduction according to personal preference. Details were not reported 5 deviations from protocol were analysed as randomised in the intention‐to‐treat analysis, as follows: 2 participants in Group A were enrolled despite being ineligible (they were recurrent dislocators); 1 participant in Group B was enrolled despite being ineligible (this participant was a recurrent dislocator); 2 participants in Group A were incorrectly immobilised in internal rotation Re‐dislocations: mean time to re‐dislocation was 10.5 months (range 1 week to 2 years) in Group A and 11.6 months (range 2 months to 2 years) in Group B Self‐reported recurrent instability: a discrepancy was noted. Participants with recurrent instability (re‐dislocation or subluxation) are reported as a percentage of the full sample (N = 184), and yet "only 163 patients answered the question as to whether they had experienced subluxation". There appears to have been an assumption that non‐responders had not experienced subluxation. Because the distribution of responses across the 2 groups is unknown, the data are not usable in a meta‐analysis WOSI data: were reported to be not normally distributed. The individual data were unavailable to us, precluding analysis Funding sources and declarations of interest: "The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotation: "Block randomization was conducted for each hospital" (p.898). Comment: it is unclear how the sequences were generated. |
| Allocation concealment (selection bias) | Unclear risk | Quotation: "Concealed randomization was performed according to the method described by Altman, and sealed envelopes were used," (p.898). Comment: specific details were not given. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding of participants and personnel (care providers) was not possible. Participants were informed of the preliminary results of Itoi 2007 (favouring immobilisation in external rotation), which may have influenced adherence. |
| Blinding of outcome assessment (detection bias) Re‐dislocation | Low risk | Comment: there is no mention of blinding, but the primary outcome measure, re‐dislocation, was clearly defined, and participant reports were verified by reference to their medical records. |
| Blinding of outcome assessment (detection bias) Validated PROMs for shoulder instability | High risk | Comment: the WOSI was patient‐assessed and hence inherently unblinded. The review authors judge that it is likely that estimates may have been influenced by lack of blinding (considering also that the participants were unblinded to their treatment allocation). |
| Blinding of outcome assessment (detection bias) Resumption of pre‐injury activities/sports | Unclear risk | Comment: return to sportive activities was patient‐assessed and was hence inherently unblinded. The review authors judged that it is possible that the outcome measurement may have been influenced by lack of blinding. However, this outcome was judged to be less prone to bias than other patient‐reported outcomes and risk of bias was therefore rated as unclear. |
| Blinding of outcome assessment (detection bias) Any instability | High risk | Comment: subluxation was patient‐reported and was hence inevitably subjective. |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | Comment: there was insufficient information about how adverse events were assessed to make a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Re‐dislocation, longest or main follow‐up | Low risk | Comment: the proportion of losses to follow‐up for re‐dislocation was very small (2/95 (2%) for Group A and 2/93 (2%) for Group B, and was insufficient to have a clinically relevant impact on estimates of effect. No information is provided about the planned or applied approach to missing outcome data; however, it seems that no missing data were replaced. |
| Incomplete outcome data (attrition bias) Validated PROMs for shoulder instability | Low risk | Attrition was low for this outcome (5% in each group). |
| Incomplete outcome data (attrition bias) Resumption of pre‐injury activities | Low risk | Comment: attrition for this outcome was 11% in the external rotation group and 10% in the internal rotation group. The review authors judged that it is unclear whether this may have had an effect on the result. |
| Incomplete outcome data (attrition bias) Any instability | Unclear risk | Comment: attrition for subluxation was 13%, but was similar in both groups (13% in Group A and 14% in Group B). The review authors judged that it is unclear whether this may have had an effect on the result. |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: there was insufficient information to allow for a judgement of 'low risk' or 'high risk' of bias. |
| Selective reporting (reporting bias) | Low risk | Comment: a protocol was published (ClinicalTrials.gov Identifier: NCT00202735), and the study's prespecified primary outcome was reported. |
| Other bias | Low risk | Comment: none identified. |
Taskoparan 2010.
| Methods |
Aim: "To compare the functional and stability outcomes of the patients with acute anterior shoulder dislocation, who were stabilised at external versus internal rotation" Method of randomisation: alternation based on Emergency Department numbers Assessor blinding: no Intention‐to‐treat analysis: no Loss to follow‐up: Rowe and Constant‐Murley scoring was planned at 6 months, and control examinations (radiography and MRI) at 6, 12 and 24 months, thus a 2‐year follow‐up. Presumably the intent was to follow up re‐dislocations for the same period. However, individual data in Table 1 indicate that only 12/16 (75%) participants in Group A and 13/17 (76.5%) in Group B were followed up to 1 year (or were already accounted for as re‐dislocators). Only 6/16 (37.5%) participants in Group A and 11/17 (64.7%) in Group B were followed up to 2 years (or were already accounted for as re‐dislocators). Thus, while there was no loss to follow‐up at the short‐term (6‐month time point), there was potentially important loss at 1 year (25% in Group A, 23.5% in Group B) and especially at 2 years (62.5% in Group A, 35.3% in Group B) |
|
| Participants |
Setting: Emergency Department in Turkey Period of data collection: 2004 to 2008 Participants: 33 Inclusion criteria: acute primary traumatic anterior dislocation; admission on the first day of reduction Exclusion criteria: hyperlaxity; [implicitly] neural damage Sex: 31 male (94%) Age: mean 34.9 years (SD 17.9 years) in Group A, 28.9 years (14.8 years) in Group B (range 15 to 75) Subgroups: age < 20 years, n = 1; age 21 to 30 years, n = 21; age 31 to 40 years, n = 4; age > 40 years, n = 7 Pre‐injury status: 7/16 (43.8%) in Group A and 9/17 (52.9%) in Group B sustained their injury in sport Assigned: 16/17 (Group A/B) Assessed: 16/17 (at 6 months); 12/13 (at 1 year); 6/11 (final follow‐up at 2 years) |
|
| Interventions |
Group A: immobilisation in 10° of external rotation in a locally‐manufactured, hard polyethylene splint, removed only for showering. The immobiliser incorporated the wrist. No information was given on who applied the immobilisation or gave the accompanying instructions Group B: immobilisation in Velpeau bandaging on the first day, switching to a "waist‐assisted sling on the second day", removed only for showering. No information was given on who applied the immobilisation or gave the accompanying instructions Both groups: immobilisation commenced on the first day after reduction and continued for 3 weeks. Immediately afterwards, rehabilitation commenced, initially with isometric and pendular exercises. When isometric exercises were painless, isotonic exercises were commenced. Avoidance of sporting activities for 3 months was recommended |
|
| Outcomes | Follow‐up points were 6 months (Constant‐Murley score, Rowe score), 1 year and 2 years (radiographs and MRI) and unspecified (re‐dislocation, adverse events, apprehension test) (Outcomes were not prespecified as primary or secondary) Re‐dislocation: was not specified as an outcome with the methods but was reported in the results. The mechanism for gathering these data was not reported Constant‐Murley score (not used in review) Rowe score (not used in review) Adverse events: were not prespecified as an outcome, but severe functional limitation was reported in 1 participant 'Intimidation test': this was presumably meant to be the apprehension test, but no further information was given Difficulties with wearing the slings and braces:observation only |
|
| Notes | "Both groups were similar in basic clinical parameters" Method of reduction: reduction was by the Hippocratic method in 20 participants (11 in Group A), the Kocher manoeuvre in 12 participants (5 in Group A) and the Stimson manoeuvre in 1 participant (Group B) Funding sources and declarations of interest: no information. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients with odd emergency department administration numbers received stabilization at internal rotation ... and patients with even numbers received stabilization at external rotation." |
| Allocation concealment (selection bias) | High risk | Comment: allocation was based on case record number (see above). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding of participants and personnel (care providers) was not possible. |
| Blinding of outcome assessment (detection bias) Re‐dislocation | Unclear risk | Comment: there is no mention of blinding and there was insufficient information about how re‐dislocation was assessed and verified. Hence, there is insufficient information to allow for a judgement of 'low' or 'high' risk of bias. |
| Blinding of outcome assessment (detection bias) Any instability | Unclear risk | Comment: there is no mention of blinding and there was insufficient information about how the 'intimidation' test was assessed. Hence, there is insufficient information to allow for a judgement of 'low' or 'high' risk of bias. |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | Comment: there is insufficient information about how adverse events were assessed to allow for a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Re‐dislocation, longest or main follow‐up | High risk | Comment: 33 participants were included in this study, and results are reported for all. However, the presented individual follow‐up periods for the participants show that beyond 6 months there were considerable, unexplained losses to follow‐up, particularly at 2 years (62.5% in Group A and 35.3% in Group B). No information is provided about the planned or applied approach to missing outcome data; however, it seems that no missing data were replaced. |
| Incomplete outcome data (attrition bias) Any instability | High risk | Comment: see above. |
| Incomplete outcome data (attrition bias) Adverse events | High risk | There was insufficient information. However, in view of the high number of losses to follow‐up, risk of attrition bias was judged as high for this outcome, too. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no study protocol is available. 2 of the key outcomes reported (re‐dislocation and the apprehension test) were not specified as outcomes in the Methods section, and it is unclear how data on re‐dislocation and the 'intimidation' (apprehension) test were obtained. No specific data on adherence are presented. No usable outcome data was reported for the Rowe Score, and it was not clear whether this outcome measure was patient‐assessed, i.e. of relevance to the review. |
| Other bias | Unclear risk | Comment: no information about funding was provided. |
Whelan 2014.
| Methods |
Aim: "...to compare the (1) frequency of recurrent instability and (2) disease‐specific quality‐of‐life scores after treatment of first‐time shoulder dislocation using either immobilization in external rotation or immobilization in internal rotation in a group of young, North American patients." (p.2381) Method of randomisation: computer‐generated permuted block algorithm (stratified to study centre) Assessor blinding: yes Intention‐to‐treat analysis: no information Loss to follow‐up: 10 (17%), comprising 5/31 (16%) in Group A and group 5/29 (17%) in Group B |
|
| Participants |
Setting: Emergency departments and outpatient orthopaedic and primary care clinics at 3 university centres, Canada Period of data collection: September 2003 to March 2008 Participants: 60 Inclusion criteria: skeletally mature patients younger than 35 years with a primary anterior glenohumeral dislocation diagnosed by radiography. Exclusion criteria: history of previous instability in the affected shoulder; significant associated fractures of the proximal humerus, glenoid or scapula (exceptions: Hill‐Sachs lesions and/or small bony Bankart lesions); patients unwilling or unable to participate Sex: 55 male (92%) Age: mean 23 years, range 14 to 35 years Pre‐injury status: 6/31 (19%) in Group A and 9/29 (31%) in Group B had signs of positive ligamentous hypermobility Assigned: 31/29 (Group A/B) Assessed: 27/25 (at final follow‐up) for re‐dislocation and surgery (data for 2 participants who were lost to follow‐up was obtained from the next of kin); 26/24 for the other outcomes |
|
| Interventions |
Group A: immobilisation for 4 weeks with an external rotation shoulder brace, in 90° of elbow flexion, 0° of shoulder abduction and flexion and 0° to 5° of shoulder external rotation. All patients received an identical brace (DonJoy; DJO, LLC, Vista, CA, USA), which was adjusted by a certified orthopaedic technician
Group B: immobilisation for 4 weeks with a traditional internal rotation sling, in 90° of elbow flexion, 0° of shoulder abduction and flexion and 70° to 80° of shoulder internal rotation. All patients received an identical sling (DonJoy; DJO, LLC), which was adjusted by a certified orthopaedic technician Both groups: presumably, immobilisation started within 7 days after dislocation (patients were assessed for eligibility within 7 days after dislocation). Patients were instructed to wear the braces or slings at all times, except for brief periods of removal for showering and therapy. They were also provided with detailed written instructions including information about the appropriate use of the brace/sling, and with contact details of the study coordinators. Patients' compliance with wearing their brace or sling was encouraged through weekly telephone calls by the study coordinator After the immobilisation period, all patients began a 16‐week physical therapy programme which was provided by outpatient or private practice therapists |
|
| Outcomes | Follow‐up assessments were reportedly conducted at 4 weeks and 3, 6, 12, 18 and 24 months post‐dislocation Prespecified as primary outcome Recurrent instability (primary outcome), "defined by a documented episode of anterior shoulder dislocation ... with radiographic evidence of the same and/or requiring manipulative reduction in a controlled hospital or healthcare setting or multiple episodes of shoulder subluxation, which, in the patient’s opinion, was disabling or symptomatic enough to warrant surgical stabilization. An assessment by an orthopaedic surgeon was mandatory in the case of the recurrent subluxation before categorizing these patients as having had an adverse event." (pp.2382‐3). The results for this outcome are presented subdivided into the following outcomes: recurrent dislocation;recurrent instability (comprising recurrent dislocations and subluxations); and recurrent instability requiring surgical stabilization Prespecified as secondary outcomes Western Ontario Shoulder Instability Index (WOSI) American Shoulder and Elbow Surgeons evaluation form (ASES) (not used in review) Adherence: patients were asked to keep a diary of brace or sling wear (in which physical therapy attendance was also recorded). Compliance was further formally assessed with a questionnaire (not further specified) after the immobilisation period Adverse events: complications; not further specified Surgical intervention: surgery was considered based on the patient's opinion that the recurrent instability "was disabling or symptomatic enough to warrant surgical stabilisation" (p. 2383) |
|
| Notes | The methods used for the reduction of the shoulder dislocation are not specified Results are presented for "minimum 12 months' follow‐up", but not for the different follow‐up points Relationship between this and previous reports: Whelan 2008 was a conference abstract reporting preliminary results. There are discrepancies between the study report and the registration record (Litchfield; NCT00196560) relating to the outcomes: namely, time (weeks) to return to work and to return to sport is specified as an outcome in the registration file, but is not mentioned in the study report Funding and declarations of interest: "This trial was funded by the Physicians Services Incorporated Foundation and the American Shoulder and Elbow Surgeons Grant." Declarations of interests were not reported ("all ICMJE Conflict of Interest Forms for authors [...] can be viewed on request [...]." (p.2380). This study was conducted at the Fowler Kennedy Sport Medicine Clinic in London, Ontario, Canada, in conjunction with JOINTS Canada (Joint Orthopaedic Initiative for National Trials on the Shoulder Canada)." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “… patients … were randomly assigned (by computer‐generated, permuted block algorithm) to one of two immobilization groups…” (p.2382). Randomisation was stratified by study centre. |
| Allocation concealment (selection bias) | Low risk | Quote: “The randomization sequence was kept concealed by the use of sealed opaque, sequentially numbered envelopes, which were opened only after inclusion criteria were satisfied and informed consent had been obtained.” (p.2382). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding of participants and personnel (care providers) was not possible. |
| Blinding of outcome assessment (detection bias) Re‐dislocation | Low risk | Quote: "It [the trial] was single‐blinded in that all evaluations were performed by independent evaluators who were unaware of treatment allocation.” (p.2381). "...all [outcome] data were collected by a research coordinator who was blinded to the patient’s intervention assignment." (p.2382). |
| Blinding of outcome assessment (detection bias) Validated PROMs for shoulder instability | High risk | Comment: this outcome (WOSI) was subjective, i.e. patient‐assessed, and thus inevitably unblinded. The review authors judge that it is likely that results may have been influenced by lack of blinding (considering also that the participants were unblinded to their treatment allocation). |
| Blinding of outcome assessment (detection bias) Any instability | High risk | Comment: subluxation was patient‐assessed, and was hence inevitably unblinded. The review authors judge that it is likely that results may have been influenced by lack of blinding (considering also that the participants were unblinded to their treatment allocation). |
| Blinding of outcome assessment (detection bias) Adverse events | Unclear risk | Comment: there is insufficient information about how adverse events were assessed to allow for a judgement of 'low risk' or 'high risk' of bias. |
| Incomplete outcome data (attrition bias) Re‐dislocation, longest or main follow‐up | Unclear risk | Comment: the flow of participants through the study is insufficiently reported and unclear. There is no information about whether all participants received the treatment they were allocated to. However, all outcomes were reportedly analysed on an intention‐to‐treat basis. There is no information about the numbers of losses to follow‐up at each specific follow‐up time point. The proportion of losses reported for the "results at minimum 12 months' follow‐up" were fairly high, but were similar between the groups (13% in Group A, 14% in Group B). No reasons are provided for the losses to follow‐up. No information is provided about the planned or applied approach to missing outcome data; however, it seems that no missing data were replaced. The review authors judge that there is insufficient information to permit a clear judgement of ‘low’ or ‘high risk’. The fact that data on recurrent dislocation was obtained in a different way (from the next of kin) for 2 participants who were lost to follow‐up is not considered as likely to have influenced the outcome. |
| Incomplete outcome data (attrition bias) Validated PROMs for shoulder instability | Unclear risk | Comment: see above. |
| Incomplete outcome data (attrition bias) Any instability | Unclear risk | Comment: see above. |
| Incomplete outcome data (attrition bias) Adverse events | Unclear risk | Comment: there is insufficient information to allow for a judgement of 'low risk' or 'high risk' of bias. |
| Selective reporting (reporting bias) | Unclear risk | Comment: the presentation of the results in relation to the different follow‐up periods ("minimum 12 months' follow‐up") is unexplained and unclear (were participants excluded when they experienced re‐dislocation?) and is judged to raise the possibility of reporting bias as results may have differed across the different follow‐up time points. There are some discrepancies between the study report and the registration record which, though, relate to outcomes that were not of interest to this review (time (weeks) to return to work and to return to sport; ROM, strength). |
| Other bias | Low risk | Comment: none identified. |
CT: Computed tomography MRI: Magnetic resonance imaging SD: Standard deviation WOSI: Western Ontario Shoulder Instability Index
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12611001183976 | This trial was abandoned: “Unfortunately due to the low participation rate and high drop out rate we are no longer recruiting to the study. We do not intend to publish this research.” (personal communication with the principal investigator, Timothy Walker, 4 June 2018) |
| Blanchard 2015 | Not a trial: a summary of Hanchard 2014 |
| Chutkan 2012 | Not a trial: a commentary on Liavaag 2011 |
| Harper 2000 | No response was received to requests for information on this trial, which is listed in the National Research Register UK. We found no other reports of this trial |
| Hovelius 1983 | This trial involved 27 centres. At 6 centres, allocation to 2 different durations of immobilisation was based on date of shoulder dislocation. At the other 21 centres, treatment was given according to customary practice. Hence, overall this study was neither randomised nor quasi‐randomised |
| Hutchinson 2013 | Not a trial: a book review |
| Itoi 2003 | We have received contradictory information on the status of this preliminary quasi‐randomised study in relation to Itoi 2007. Excluded to remove the risk of duplicate populations |
| Itoi 2015 | Not an RCT or quasi‐RCT; no interventions or outcomes of relevance to the review question. In this study, which is labelled a “controlled laboratory study”, patients were assessed by MRI immediately after they consented to participate (after presenting with an initial traumatic anterior shoulder dislocation), and 4 different shoulder positions were assessed by MRI to investigate the (immediate) effect of these positions on the reduction of a Bankart lesion. |
| Kiviluoto 1980 | Of 99 people younger than 50 years in this study, 53 were immobilised for 1 week and 46 for 3 weeks. However, no indication reveals the method of allocation to the 2 groups, nor are results presented for these participants. We received no response from the study authors |
| Königshausen 2014 | Not an RCT or quasi‐RCT: a prospective cohort study of 28 patients with primary traumatic anterior shoulder dislocation, "to investigate the recurrence and instability rates of patients 5 years after primary traumatic anterior shoulder dislocation treated with an external rotation brace..." |
| Lacy 2015 | Not an RCT or quasi‐RCT: a study reporting on the development of a “low‐cost” shoulder brace. |
| McCarty 2014 | Not a trial: a commentary on Whelan 2014 |
| Momenzadeh 2015 | An RCT, in which none of our pre‐specified outcomes of interest for the review question were assessed. 20 patients with primary anterior shoulder dislocation were randomised to immobilisation in external or internal rotation. After 3 weeks, various radiographic parameters (displacement, separation and opening angle) were assessed by magnetic resonance arthrography to determine the effect of the shoulder immobilisation position on the coaptation of a Bankart lesion. |
| Staply 2002 | A contact person at the institution given for this trial as listed in the National Research Register UK indicated that this trial did not appear to have been started. We found no other reports of this trial |
| Wakefield 2001 | A draft report of this pilot study of 23 participants, comparing Intensive physiotherapy plus home exercises versus home exercises alone, was shared with review authors in June 2005. At that time, a report was expected to be submitted shortly for publication. We are unable to find a published version of the report, and the contact author is no longer available at the postal or email address given in the trial registry |
| Whelan 2010 | Not a trial: a commentary on Finestone 2009 |
| Xu 2003 | This was not a randomised controlled trial but a comparison, with a historical control group, of systematic rehabilitation therapy versus supporting bandage in 43 people with acute shoulder dislocation |
ASES: American Shoulder and Elbow Surgeons HRQoL: Health‐related quality of life ISRCTN: International Standard Randomised Controlled Trial Number Register MRI: Magnetic Resonance Imaging WOSI: Western Ontario Shoulder Instability Index
Characteristics of studies awaiting assessment [ordered by study ID]
ISRCTN41070054.
| Methods | Reportedly a randomised controlled trial |
| Participants | 38 people with anterior shoulder dislocation |
| Interventions | 1. External rotation splint 2. Sling |
| Outcomes | Follow‐up: not stated Incidence of recurrent dislocation |
| Notes | The anticipated end date of this UK‐based study, which is listed as completed on the ISRCTN registry, was 1 November 2010. We are unable to find a published report, and we received no response to our email and postal correspondence to the contact author, Mr N Nicolaou |
ISRCTN48254181.
| Methods | Stated to be a randomised controlled trial |
| Participants | 150 people with primary anterior shoulder dislocation |
| Interventions | 1. Arm immobilised in external rotation 2. Arm immobilised in internal rotation |
| Outcomes | Follow‐up: not stated Recurrence |
| Notes | The anticipated end date of this UK‐based study, which is listed as completed on the ISRCTN registry, was 1 May 2008. We are unable to find a published report, and we received no response to our email and postal correspondence to the contact author, Mr A Pimpalnerkar |
Itoi 2013.
| Methods | Randomised controlled trial |
| Participants | 109 people with primary traumatic shoulder dislocation. Study conducted in Japan |
| Interventions | 3 weeks' immobilisation in external rotation followed by: 1. no shoulder motion restriction band; 2. a shoulder motion restriction band for 3 weeks; or 3. a shoulder motion restriction band for 6 weeks. |
| Outcomes | Recurrent dislocation and return to sports, assessed at 2‐year follow‐up |
| Notes | No difference in recurrence rate was reported 'Awaiting classification' as evaluating a supplement to an immobilisation technique whose general effectiveness is not established |
Miller 2007.
| Methods | Method of randomisation: randomised multi‐centre ‒ no details |
| Participants | 30 people (to date) 18 to 30 years of age with acute, first‐time anterior dislocation of the shoulder. Study conducted in USA |
| Interventions | 3 weeks' immobilisation in: 1. a 15° external rotation brace; or 2. a sling. This was followed by an identical short course of physiotherapy |
| Outcomes | Follow‐up: 1 year WOSI, subjective portion of ASES shoulder assessment form and a study‐specific questionnaire |
| Notes | Interim results reported in a 2007 poster presentation. We received no response to our attempt to contact Dr BS Miller |
Murray 2016.
| Methods | Randomised controlled trial |
| Participants | 50 people with primary traumatic anterior dislocation of the shoulder. Study conducted in Canada. |
| Interventions | 3 weeks' immobilisation in: 1. external rotation; or 2. internal rotation No further information is provided. |
| Outcomes | Follow‐up: 2 years Primary: recurrent dislocation Secondary: healing rate of labral lesion, if present (diagnosed by MRI) |
| Notes | This study is as yet only reported in a conference abstract. We received the following response to our enquiry on the availability of a full report of this study from the corresponding author of the abstract, Dr Murray (personal communication by email, 31 May 2018): "We are actively trying to publish the manuscript but so far unsuccessfully. So it’s only a conference abstract for now." |
NCT00707018.
| Methods | Method of randomisation: initially quasi‐randomised using alternation (10 cases), then use of random numbers chart Assessor blinding: no Intention‐to‐treat analysis: no information Loss to follow‐up: not known |
| Participants | 50 people 14 to 30 years of age with acute, first‐time, traumatic, isolated anterior dislocation of the shoulder (no significant fractures) |
| Interventions | 1. External rotation shoulder sling 2. Internal rotation shoulder sling |
| Outcomes | Follow‐up: 2 years Primary: recurrent instability consisting of a documented episode of anterior shoulder dislocation or multiple episodes of shoulder subluxation Secondary: participant self‐reported outcome measures, time to return to work or sport |
| Notes | This USA‐based study is listed as completed on the ISRCTN registry, with an end date of 1 February 2012. We are unable to find a published report, and we received no response to our attempt to contact Prof EC McCarty |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12616001241426.
| Trial name or title | An RCT assessing the efficacy of smart phone apps in the conservative management of shoulder rehabilitation post dislocation in the male and female population between 15 to 60 years of age (registered scientific title) |
| Methods | Randomised controlled trial; Australia and New Zealand |
| Participants | Males and females (age 15 to 60 years) with radiologically or clinically diagnosed anterior dislocation of a shoulder (target sample size = 48) |
| Interventions | 1. Access to a smartphone application including information (related to the injury, management and prognosis) and a staged exercise‐based rehabilitation programme as an adjunct to a supervised (physiotherapy) rehabilitation programme 2. Supervised rehabilitation (same as for the intervention group) without access to the smartphone application. |
| Outcomes | Follow‐up: 18 months (final follow‐up) Outcomes: Oxford Shoulder Instability Score (OSIS); need for surgery; compliance with rehabilitation, "helpfulness" of the smartphone application |
| Starting date | See notes |
| Contact information | Principal investigator: Dr Nicholas Noye; nicholasnoye@gmail.com |
| Notes | The trial registration record was last updated in October 2017 (last accessed 2 August 2018). Recruitment for this study has not yet started ‒ we received the following response from the principal investigator, Dr Nicholas Noye, on our enquiry about the current status of the study: "... the study has been delayed. I now plan to start the trial here in Waikato NZ beginning next year and will not be commencing the Australian study until at least 2019..." (personal communication, by email, 25 May 2018). Dr Noye also sent us the (unpublished) protocol for the study. The information provided here is largely based on information provided in the protocol. |
ARTISAN.
| Trial name or title | Acute Rehabilitation following Traumatic anterior shoulder dISlocAtioN (ARTISAN) ‐ A Multi Centre RCT |
| Methods | Randomised controlled trial, multi‐centre; target sample size 478 (main study, proceeded by an internal pilot on a target sample of 50 participants); UK |
| Participants | People (≥ 18) with first‐time traumatic anterior shoulder dislocation |
| Interventions | Treatment includes up to 2 weeks of immobilisation (with intervention within 6 weeks post‐injury) 1. Single session (up to 1 hour) of "advice to aid self‐management" (including education on the injury, on complications and how to prevent pain; discussion exercises; use of different media) 2. Same session as 1., followed by a course of individually tailored physiotherapy (minimum of 2 sessions offered) for up to 30 minutes, over 4 months. |
| Outcomes | Follow‐up: 12 months (final follow‐up) Primary: Oxford Shoulder Instability Score (OSIS) (after 6 months) Secondary: functional outcome (Quick‐DASH), quality of life (EQ‐5D‐5L), complications, resource use |
| Starting date | Duration of study specified as from 1 June 2018 to 30 November 2021 |
| Contact information | Chief Investigator: Ass Prof Rebecca Kearney Warwick Clinical Trials The University of Warwick Gibbet Hill Road Coventry, CV4 7AL Tel: 02476573156 Email: r.s.kearney@warwick.ac.uk |
| Notes | An NIHR‐funded HTA project, which was incidentally found during other searches. The project has obviously only just been started. |
Eshoj 2017.
| Trial name or title | A neuromuscular exercise programme versus standard care for patients with traumatic anterior shoulder instability (the SINEX study) |
| Methods | Randomised controlled trial; target sample size 80 but number of actually enrolled participants was 56; Denmark |
| Participants | Patients (male or female, age 18 to 39 years) with primary or recurrent anterior shoulder dislocation |
| Interventions | 1. "SINEX programme": individual physiotherapist‐supervised neuromuscular shoulder exercise programme (12 weeks) 2. Self‐managed shoulder exercise programme with 1 introductory supervised physiotherapy session (12 weeks) |
| Outcomes | 104 weeks (final follow‐up) Primary: change in WOSI (after 12 weeks) Secondary: WOSI subdomains, kinesiophobia (Tampa Scale of Kinesiophobia), quality of life (EQ‐5D‐5L), pain, self‐reported shoulder function (Patient‐Specific Functioning Scale (PSFS), CMS), clinical shoulder instability (e.g. apprehension test), shoulder proprioception (e.g. joint repositioning), re‐dislocation/subluxation, medication use, satisfaction with treatment, adverse events. |
| Starting date | February 2015 |
| Contact information | Principal investigator: Henrik Eshoj: heshoj@health.sdu.dk |
| Notes | According to the trial registration record (NCT02371928; most recent update posted: March 2018; (last accessed 2 August 2018)), recruitment is completed (actual study completion date: June 2017). We tried to contact the principal investigator, Mr Henrik Eshoj, in May 2018 to enquire about the current status of the study and its anticipated publication, but have not received a response. The information presented here was mainly taken from the published protocol. |
NCT01648335.
| Trial name or title | A prospective study of the effect of treatment of first‐time traumatic shoulder anterior dislocation by immobilization in external rotation on the incidence of recurrent dislocation |
| Methods | Parallel assignment; intended sample size not reported |
| Participants | Males 18 to 29 years of age with first‐time dislocation of the shoulder |
| Interventions | 1. Immobilisation in internal rotation in a universal shoulder immobiliser 2. Immobilisation in external rotation in a universal shoulder immobiliser |
| Outcomes | Follow‐up: 6 months after dislocation Primary: number of recurrent dislocations Secondary: range of motion; supine apprehension test |
| Starting date | June 2012 |
| Contact information | None given |
| Notes | The recruitment status of this study is 'unknown' (ClinicalTrials.gov, last update posted in March 2013) and it may have been abandoned. No corresponding author details were available for this study. We attempted to make contact through the responsible organisation (Hadassah Medical Organization, Israel), but did not receive a response. |
NCT02197819.
| Trial name or title | A Randomized Evaluation of Emergent Immobilization in External Rotation in the Management of Acute Anterior Dislocations of the Shoulder (EERAADS) |
| Methods | Randomised controlled trial; target sample size 75; Canada |
| Participants | Patients (age 18 to 35 years) following reduction of a first‐time traumatic anterior shoulder dislocation |
| Interventions | 1. Immobilisation in an external rotation brace for 4 weeks (start < 4 hours post‐reduction) 2. Immobilisation in a traditional internal rotation sling (start < 4 hours post‐reduction) |
| Outcomes | Follow‐ups: 12 months (no further follow‐up points specified) Primary: re‐dislocation (within 12 months) Secondary: none specified |
| Starting date | February 2013 (study start date) |
| Contact information | contact: Dr Ryan M Khan; khanry@smh.ca (principal investigator: Dr Daniel B Welan) |
| Notes | According to the registration record (most recent update posted: August 2017 (last accessed 2 August 2018)), the trial is still recruiting. The estimated primary completion date specified as February 2018; the estimated study completion date as February 2019. We tried to contact Dr Khan in May 2018 to enquire about the current status of the study but have not received a response. 3 different age ranges for eligibility are provided within the registration record: 16 to 30; 18 to 40; 18 to 35 years. |
ACTRN: Australian New Zealand Clinical Trials Registry CMS: Constant‐Murley Score DASH: Disabilities of the Arm, Shoulder, and Hand EQ (‐5D‐5L): EuroQual (‐5D‐5L) NCT: National Clinical Trial WOSI: Western Ontario Shoulder Instability Index
Differences between protocol and review
Differences in the review update published in 2019
Prior to updating the search, the authors submitted a revised protocol section for the review that detailed the following.
Clarification in Types of participants of acceptable concomitant injuries that are often associated with anterior shoulder dislocation.
Listing of four main comparisons covering priority questions in Types of interventions.
As planned in Hanchard 2014, the risk of bias assessment was expanded to include separate consideration of subjective and objective outcomes in relation to blinding of outcome assessment and completeness of outcome data (Assessment of risk of bias in included studies). However, grouping of outcomes in this way proved unsatisfactory and we thus assessed these domains separately for each reported outcome.
We changed the lower of two age thresholds for subgroup analysis from 25 to 20 based on recent evidence (Wasserstein 2016), and added an additional subgroup analysis based on the presence or not of a greater tuberosity fracture (Olds 2015; Wasserstein 2016).
During the conduct of the review update, we made the following additional changes.
We added a post hoc explanatory statement in Types of outcome measures on the exclusion of studies that solely addressed non‐clinical outcomes.
We conducted an exploratory post hoc subgroup analysis of trials in which immobilisation in external rotation had an additional abduction component versus those without (external rotation only).
We made the post hoc decision to stratify 'adverse events' into 'transient and resolved' and 'important' as we considered this to more appropriately reflect the available data.
Differences in the review update published in 2014
In line with Cochrane recommendations, the review now assesses risk of bias.
For this version of the review, outcomes were revised and, to comply with current Cochrane guidance, the number of primary outcomes was reduced. We used GRADE to judge the quality of the evidence and have incorporated a 'Summary of findings' table: Table 1.
As indicated in the Results, we anticipated organising outcomes within a framework of short term (up to and including three months following dislocation), medium term (greater than three months and up to and including 12 months) and long term (longer than 12 months). Imposition of this framework was not necessary because all included studies reported outcomes in a mutually compatible framework: during or shortly after immobilisation (some adverse events) or up to or beyond two years post dislocation.
Contributions of authors
The review update was developed by Cordula Braun (CB) and Cliona McRobert (CMR). CB contacted authors of eligible trials to inform choices for study inclusion and to ask for extra information. Both review authors performed trial selection, quality assessment and data extraction. CB compiled the first draft of the review and received critical feedback from CMR. Cordula Braun is the guarantor of the review.
Contributions of the editorial base
Helen Handoll (Co‐ordinating Editor): edited the review; advised on methodology and review content; and approved the final version for publication. Joanne Elliott (Managing Editor): coordinated the editorial process; advised on content; and edited the review. Maria Clarke (Information Specialist): updated the search and edited the search methods section.
Sources of support
Internal sources
Cochrane Germany, Germany.
External sources
National Institute for Health Research (NIHR) via Cochrane Infrastructure funding to the Cochrane Bone, Joint and Muscle Trauma Group, UK.
Declarations of interest
Cordula Braun: none known Cliona McRobert: none known
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Chan 2018 {published data only}
- Bentick K. Response to request for additional data [personal communication]. Email to: C Braun 1 September 2018.
- Chan SK, Bentick KR, Kuiper JH, Kelly CP. External rotation bracing for first‐time anterior dislocation of the shoulder: a discontinued randomised controlled trial comparing external rotation bracing with conventional sling. Shoulder & Elbow 2018 April 26 [Epub ahead of print]. [DOI: ] [DOI] [PMC free article] [PubMed]
- Kelly CP, Smith HJ, Kuiper JH. External rotation bracing compared to conventional sling in first time anterior shoulder dislocation (abstract). Abstracts for the 22nd Annual Scientific Meeting, BESS,22–24 June 2011, Newcastle, UK; Shoulder & Elbow (on behalf of the British Shoulder and Elbow Society). 2011; Vol. 3, issue 4:273. [DOI: ]
- Kuiper JH, Smith HJ, Wales J, Kelly CP. External rotation bracing compared to conventional sling in first time anterior shoulder dislocation – The Shoulder Orthosis Study (SOS). Institute of Orthopaedics; Annual Report 2010/2011; www.orthopaedic‐institute.org/images/user/Institute%20Report%202011_Web.pdf (accessed 14 June 2013).
Finestone 2009 {published data only}
- Finestone A, Milgrom C, Radeva‐Petrova DR, Rath E, Barchilon V, Beyth S, et al. Bracing in external rotation for traumatic anterior dislocation of the shoulder. Journal of Bone and Joint Surgery. British Volume 2009;91(7):918‐21. [DOI] [PubMed] [Google Scholar]
- Milgrom C. Personal communication 5 October 2009.
Heidari 2014 {published data only}
- Heidari K, Asadollahi S, Vafaee R, Barfehei A, Kamalifar H, Chaboksavar ZA, et al. Immobilization in external rotation combined with abduction reduces the risk of recurrence after primary anterior shoulder dislocation. Journal of Shoulder and Elbow Surgery 2014;23(6):759‐66. [DOI] [PubMed] [Google Scholar]
Itoi 2007 {published data only}
- Itoi E. Personal communication 8 April 2011.
- Itoi E. Personal communication July 2005.
- Itoi E, Hatakeyama Y, Sato T, Kido T, Minagawa H, Yamamoto N, et al. Immobilization in external rotation after dislocation of the shoulder reduces the risk of recurrence [platform presentation]. American Academy of Orthopaedic Surgeons Annual Meeting; 2007 Feb 14‐18; San Diego (CA). 2007.
- Itoi E, Hatakeyama Y, Sato T, Kido T, Minagawa H, Yamamoto N, et al. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence: a randomized controlled trial. Journal of Bone and Joint Surgery. American Volume 2007;89(10):2124‐31. [DOI] [PubMed] [Google Scholar]
Liavaag 2011 {published data only}
- Liavaag S. Personal communication 21 April 2013.
- Liavaag S, Brox JI, Pripp AH, Enger M, Soldal LA, Svenningsen S. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomized controlled trial. Journal of Bone and Joint Surgery. American Volume 2011;93(10):897‐904. [DOI] [PubMed] [Google Scholar]
- Liavaag S, Stiris MG, Lindland ES, Enger M, Svenningsen S, Brox JI. Do Bankart lesions heal better in shoulders immobilized in external rotation? A randomized single‐blind study of 55 patients examined with MRI. Acta Orthopaedica 2009;80(5):579‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svenningsen S. Does immobilization of the shoulder in external rotation reduce the recurrence rate of shoulder dislocation?. clinicaltrials.gov/show/NCT00202735 (accessed 12 November 2012).
Taskoparan 2010 {published data only}
- Taskoparan H, Kilincoglu V, Tunay S, Bilgic S, Yurttas Y, Komurcu M. Immobilization of the shoulder in external rotation for prevention of recurrence in acute anterior dislocation. Acta Orthopaedica et Traumatologica Turcica 2010;44(4):278‐84. [DOI] [PubMed] [Google Scholar]
Whelan 2014 {published data only}
- Litchfield RB. A randomized evaluation of immobilization in external rotation in the management of acute anterior dislocations of the shoulder. clinicaltrials.gov/show/NCT00196560 (accessed 12 November 2012).
- Whelan D, Litchfield RB, Boorman RS, Dainty K, Wambolt E, Chan DS, et al. A randomized evaluation of immobilization in external rotation after primary shoulder dislocation [abstract]. American Academy of Orthopaedic Surgeons 75th Annual Meeting; 2008 Mar 5‐9; San Francisco (CA). 2008.
- Whelan DB, Litchfield R, Wambolt E, Dainty KN, Joint Orthopaedic Initiative for National Trials of the Shoulder (JOINTS). External rotation immobilization for primary shoulder dislocation: a randomized controlled trial. Clinical Orthopaedics and Related Research 2014;472(8):2380‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12611001183976 {unpublished data only}
- Walker T. Personal communication 13 November 2012.
- Walker T. A randomised controlled trial on the effect of physiotherapy and an external rotation brace on redislocation rate and shoulder function in patients aged 15‐40 years with a first time anterior shoulder dislocation. who.int/trialsearch/Trial.aspx?TrialID=ACTRN12611001183976 (accessed 12 November 2012).
- Walker T. Status of ACTRN12611001183976 "A randomised controlled trial on the effect of physiotherapy and an external rotation brace in the management of first time anterior shoulder dislocations in patients aged 15‐40 years." [personal communication]. Email to: C Braun 4 June 2018.
Blanchard 2015 {published data only}
- Blanchard D, Bourgeois S. Conservative management following closed reduction of a traumatic anterior dislocation of the shoulder. Orthopedic Nursing 2015;34(4):243‐4. [DOI] [PubMed] [Google Scholar]
Chutkan 2012 {published data only}
- Chutkan NB. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomized controlled trial. Orthopedics 2012;35(7):610‐1. [DOI] [PubMed] [Google Scholar]
Harper 2000 {unpublished data only}
- Harper W. Anterior shoulder dislocations in the over 45 years of age. a prospective randomised study. In: National Resarch Register, Issue 1, 2005. Oxford: Update Software. www.nrr.nhs.uk/ViewDocument.asp?ID=N0122017162 (accessed 12 May 2005).
Hovelius 1983 {published data only}
- Arciero RA, Taylor DC. Primary anterior dislocation of the shoulder in young patients. A ten‐year prospective study [letter]. Journal of Bone and Joint Surgery. American Volume 1998;80(2):299‐300. [PubMed] [Google Scholar]
- Hovelius L. Anterior dislocation of the shoulder in teenagers and young adults. Five year prognosis. Journal of Bone and Joint Surgery. American Volume 1987;69(3):393‐9. [PubMed] [Google Scholar]
- Hovelius L. The natural history of primary anterior dislocation of the shoulder in the young. Journal of Orthopaedic Science 1999;4(4):307‐17. [DOI] [PubMed] [Google Scholar]
- Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten‐year prospective study. Journal of Bone and Joint Surgery. American Volume 1996;78(11):1677‐84. [DOI] [PubMed] [Google Scholar]
- Hovelius L, Eriksson K, Fredin H, Hagberg G, Hussenius A, Lind B, et al. Recurrences after initial dislocation of the shoulder. Results of a prospective study of treatment. Journal of Bone and Joint Surgery. American Volume 1983;65(3):343‐9. [PubMed] [Google Scholar]
- Hovelius L, Lind B, Thorling J. Primary dislocation of the shoulder. Factors affecting the two‐year prognosis. Clinical Orthopaedics and Related Research 1982;(176):181‐5. [PubMed] [Google Scholar]
- Kirkley S. Primary anterior dislocation of the shoulder in young patients. A ten‐year prospective study [letter]. Journal of Bone and Joint Surgery. American Volume 1998;80(2):300‐1. [PubMed] [Google Scholar]
Hutchinson 2013 {published data only}
- Hutchinson M. Shoulder Instability: A Comprehensive Approach. Medicine & Science in Sports & Exercise 2013;45(1):216. [Google Scholar]
Itoi 2003 {published data only}
- Itoi E. Personal communication 10 July 2005.
- Itoi E, Hatakeyama Y, Kido T, Sato T, Minagawa H, Wakabayashi I, et al. A new method of immobilization after traumatic anterior dislocation of the shoulder: a preliminary study. Journal of Shoulder and Elbow Surgery 2003;12(5):413‐5. [DOI] [PubMed] [Google Scholar]
- Itoi E, Hatakeyama Y, Kido T, Sato T, Minagawa H, Wakabayashi I, et al. A new method of immobilization in dislocation of the shoulder: a prospective randomized study [abstract]. Annual Meeting of the American Academy of Orthopaedic Surgeons; 2003 February 5‐9; New Orleans [LA]. www.aaos.org/wordhtml/anmt2003/sciprog/200.htm (accessed 01 October 2003).
- Itoi E, Hatakeyama Y, Sato T, Kido T, Minagawa H, Wakabayashi I, et al. Immobilization in external rotation after shoulder dislocation: an interim report of an ongoing trial [abstract]. Annual Meeting of the American Academy of Orthopaedic Surgeons; 2004 March 10‐14; San Francisco (CA). www.aaos.org/wordhtml/anmt2004/sciprog/071.htm (accessed 07 April 2004).
Itoi 2015 {published data only}
- Itoi E, Kitamura T, Hitachi S, Hatta T, Yamamoto N, Sano H. Arm abduction provides a better reduction of the Bankart lesion during immobilization in external rotation after an initial shoulder dislocation. American Journal of Sports Medicine 2015;43(7):1731‐6. [DOI] [PubMed] [Google Scholar]
Kiviluoto 1980 {published data only}
- Kiviluoto O, Pasila M, Jaroma H, Sundholm A. Immobilization after primary dislocation of the shoulder. Acta Orthopaedica Scandinavica 1980;51(6):915‐9. [DOI] [PubMed] [Google Scholar]
Königshausen 2014 {published data only}
- Königshausen M, Schliemann B, Schildhauer TA, Seybold D. Evaluation of immobilization in external rotation after primary traumatic anterior shoulder dislocation: 5‐year results. Musculoskeletal Surgery 2014;98(2):143‐51. [DOI] [PubMed] [Google Scholar]
Lacy 2015 {published data only}
- Lacy K, Cooke C, Cooke P, Schupbach J, Vaidya R. Low‐cost alternative external rotation shoulder brace and review of treatment in acute shoulder dislocations. Western Journal of Emergency Medicine 2015;16(1):114‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCarty 2014 {published data only}
- McCarty EC. Immobilization with an external rotation brace was similar to an internal rotation sling for shoulder dislocation. Journal of Bone and Joint Surgery. American Volume 2014;96(16):1398. [DOI] [PubMed] [Google Scholar]
Momenzadeh 2015 {published data only}
- Momenzadeh OR, Pourmokhtari M, Sefidbakht S, Vosoughi AR. Does the position of shoulder immobilization after reduced anterior glenohumeral dislocation affect coaptation of a Bankart lesion? An arthrographic comparison. Journal of Orthopaedics and Traumatology 2015;16(4):317‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Staply 2002 {unpublished data only}
- Luya M. Personal communication 6 June 2005.
- Staply S. Anterior shoulder trial dislocation external rotation trial. In: National Resarch Register, Issue 1, 2005. Oxford: Update Software. www.nrr.nhs.uk/ViewDocument.asp?ID=N0284109750 (accessed 12 May 2005).
Wakefield 2001 {unpublished data only}
- Wakefield A. Personal communication 24 June 2005.
- Wakefield A. The role of physiotherapy in the prevention of recurrence of anterior shoulder dislocation. In: National Research Register, Issue 1, 2005. Oxford: Update Software. www.nrr.nhs.uk/ViewDocument.asp?ID=N0519070803 (accessed 12 May 2005).
Whelan 2010 {published data only}
- Whelan D. Immobilization in an external or internal rotation brace did not differ in preventing recurrent shoulder dislocation. Journal of Bone and Joint Surgery. American Volume 2010;92(5):1262. [DOI] [PubMed] [Google Scholar]
Xu 2003 {published data only}
- Xu Q, Gong Y, Lan Z, Xue C. Effects of systematic rehabilitation treatment on the stability of shoulder in young patients with shoulder dislocation. Zhongguo Linchuang Kangfu [Chinese Journal of Clinical Rehabilitation] 2003;14(7):2050‐1. [Google Scholar]
References to studies awaiting assessment
ISRCTN41070054 {unpublished data only}
- Nicolaou N. Splintage in external rotation for anterior glenohumeral dislocation: a prospective randomised and controlled study. apps.who.int/trialsearch/Trial.aspx?TrialID=ISRCTN41070054 (accessed 12 November 2012).
ISRCTN48254181 {unpublished data only}
- Pimpalnerker A. A comparison study of internal versus external rotation immobilisation for primary anterior shoulder dislocation. apps.who.int/trialsearch/Trial.aspx?TrialID=ISRCTN48254181 (accessed 12 November 2012).
Itoi 2013 {published data only}
- Itoi E, Hatakeyama Y, Itoigawa Y, Omi R, Shinozaki N, Yamamoto N, et al. Is protecting the healing ligament beneficial after immobilization in external rotation for an initial shoulder dislocation?. American Journal of Sports Medicine 2013;41(5):1126‐32. [DOI] [PubMed] [Google Scholar]
Miller 2007 {published data only}
- Miller BS, Cole EM, Sonnabend D, Kaar SG. Sling vs external rotation brace for shoulder dislocations: preliminary results of a randomized trial [poster presentation]. American Academy of Orthopaedic Surgeons Annual Meeting; 2007 Feb 14‐18; San Diego (CA) 2007.
Murray 2016 {published data only}
- Murray JC. Re: Enquiry on the availability of a full study report [personal communication]. Email to: C Braun 31 May 2018.
- Murray JC, Leclerc A, Pelet S. Immobilisation in external rotation after primary shoulder dislocation reduces the risk of recurrence in young patients: a randomised controlled trial. Bone & Joint Journal Orthopaedic Proceedings 2016;98_B(Supp 20):77. [DOI] [PubMed] [Google Scholar]
- Pelet S. Personal communication 21 January 2013.
- Pelet S, Cote H. First time anterior glenohumeral joint dislocation with a Bankart lesion in young patients: which type of immobilization should be chosen? A prospective randomized study. apps.who.int/trialsearch/Trial.aspx?TrialID=NCT01111500 (accessed 12 November 2012).
NCT00707018 {unpublished data only}
- McCarty E. Immobilization in external rotation after first time anterior shoulder dislocation: a prospective randomized study. apps.who.int/trialsearch/Trial.aspx?TrialID=NCT00707018 (accessed 12 November 2012).
References to ongoing studies
ACTRN12616001241426 {published data only}
- ACTRN12616001241426. An RCT assessing the efficacy of smart phone apps in the conservative management of shoulder rehabilitation post dislocation in the male and female population between 15‐60 years of age. apps.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12616001241426 (accessed 07 November 2018).
- Noye N. Re: Enquiry on your registered trial ACTRN12616001241426 [personal communication]. Email to: C. Braun 25 May 2018.
ARTISAN {published data only}
- ARTISAN Trial. Acute rehabilitation following traumatic anterior shoulder dISlocAtioN (ARTISAN) ‐ A Multi Centre RCT. Health Technology Assessment Research Projects: journalslibrary.nihr.ac.uk/programmes/hta/1616756/#/ (accessed 07 November 2018) 2018. [ISRCTN 63184243]
- Shah A. Acute rehabilitation following traumatic anterior shoulder dislocation. www.isrctn.com/ISRCTN63184243 (first received 3 September 2018).
Eshoj 2017 {published data only}
- Eshoj H. A neuromuscular exercise program for patients with anterior shoulder instability (SINEX). clinicaltrials.gov/ct2/show/NCT02371928 (first received 26 February 2015).
- Eshoj H, Rasmussen S, Frich LH, Hvass I, Christensen R, Jensen SL, et al. A neuromuscular exercise programme versus standard care for patients with traumatic anterior shoulder instability: study protocol for a randomised controlled trial (the SINEX study). Trials 2017;18(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01648335 {published data only}
- NCT01648335. A prospective study of the effect of treatment of first time traumatic shoulder anterior dislocation by immobilization in external rotation on the incidence of recurrent dislocation. apps.who.int/trialsearch/Trial.aspx?TrialID=NCT01648335 (accessed 1 November 2012).
NCT02197819 {published data only}
- NCT02197819. A randomized evaluation of emergent immobilization in External Rotation in the Management of Acute Anterior Dislocations of the Shoulder (EERAADS). apps.who.int/trialsearch/Trial2.aspx?TrialID=NCT02197819 (accessed 07 November 2018).
Additional references
Angst 2011
- Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J. Measures of adult shoulder function disabilities. Arthritis Care & Research 2011;63(S11):S174‐88. [DOI: ] [DOI] [PubMed] [Google Scholar]
Balke 2016
- Balke M, Shafizadeh S, Bouillon B, Banerjee M. Management of shoulder instability: the current state of treatment among German orthopaedic surgeons. Archives of Orthopaedic and Trauma Surgery 2016;136(12):1717‐21. [DOI] [PubMed] [Google Scholar]
Bankart 1938
- Bankart AS. The pathology and treatment of recurrent dislocation of the shoulder joint. British Journal of Surgery 1938;26(101):23‐9. [Google Scholar]
Berendes 2015
- Berendes TD, Pilot P, Nagels J, Vochteloo AJ, Nelissen RG. Survey on the management of acute first‐time anterior shoulder dislocation amongst Dutch public hospitals. Archives of Orthopaedic and Trauma Surgery 2015;135(4):447‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cameron 2017
- Cameron KL, Mauntel TC, Owens BD. The epidemiology of glenohumeral joint instability: incidence, burden, and long‐term consequences. Sports Medicine and Arthroscopy Review 2017;25(3):144‐9. [DOI] [PubMed] [Google Scholar]
Dawson 1999
- Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. Journal of Bone and Joint Surgery. British Volume 1999;81(3):420–6. [DOI] [PubMed] [Google Scholar]
de Boer 2005
- Boer P. Personal communication 21 October 2005.
Demehri 2017
- Demehri S, Hafezi‐Nejad N, Fishman EK. Advanced imaging of glenohumeral instability: the role of MRI and MDCT in providing what clinicians need to know. Emergency Radiology 2017;24(1):95‐103. [DOI] [PubMed] [Google Scholar]
Dymond 2011
- Dymond C, Stone R, Furyk J, Seymour J. Conservative management for traumatic shoulder dislocations: is external rotation clinically effective?. EMA ‐ Emergency Medicine Australasia. Conference: 27th Annual Scientific Meeting of the Australasian College for Emergency Medicine Canberra, ACT Australia 2011;23:28. [Google Scholar]
Forsythe 2015
- Forsythe B, Frank RM, Ahmed M, Verma NN, Cole BJ, Romeo AA, et al. Identification and treatment of existing copathology in anterior shoulder instability repair. Arthroscopy 2015;31(1):154‐66. [DOI] [PubMed] [Google Scholar]
Handoll 2004
- Handoll HHG, Almaiyah MA. Surgical versus non‐surgical treatment for acute anterior shoulder dislocation. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD004325.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hill 1940
- Hill HA, Sachs MD. The grooved defect of the humeral head: a frequently unrecognised complication of dislocations of the shoulder joint. Radiology 1940;35:690‐700. [Google Scholar]
Hovelius 2008
- Hovelius L, Olofsson A, Sandstrom B, Augustini BG, Krantz L, Fredin H, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty‐five‐year follow‐up. Journal of Bone and Joint Surgery. American Volume 2008;90:945‐52. [DOI] [PubMed] [Google Scholar]
Itoi 1999
- Itoi E, Hatakeyama Y, Urayama M, Pradhan R L, Kido T, Sato K. Position of immobilization after dislocation of the shoulder. A cadaveric study. Journal of Bone and Joint Surgery. American Volume 1999;81(3):385‐90. [PubMed] [Google Scholar]
Itoi 2001
- Itoi E, Sashi R, Minagawa H, Shinizu T, Wakabayashi I, Sato K. Position of immobilization after dislocation of the glenohumeral joint. A study with use of magnetic resonance imaging. Journal of Bone and Joint Surgery. American Volume 2001;83(5):661‐7. [DOI] [PubMed] [Google Scholar]
Karatsolis 2006
- Karatsolis K, Athanasopoulos S. The role of exercise in the conservative treatment of the anterior shoulder dislocation. Journal of Bodywork and Movement Therapies 2006;10(3):211‐9. [Google Scholar]
Kavaja 2018
- Kavaja L, Lähdeoja T, Malmivaara A, Paavola M. Treatment after traumatic shoulder dislocation: A systematic review with a network meta‐analysis. British Journal of Sports Medicine 2018;52:1498‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirkley 1998
- Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease‐specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). American Journal of Sports Medicine 1998;6:764–72. [DOI] [PubMed] [Google Scholar]
Kitamura 2005
- Kitamura T, Ikuta T. Immobilization with external rotation position after labrum injuries in young patients: repositioning of labrums observed by MRA. Shoulder Joint 2005;29(3):519‐22. [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Liavaag 2009
- Liavaag S, Stiris MG, Lindland ES, Enger M, Svenningsen S, Brox JI. Do Bankart lesions heal better in shoulders immobilized in external rotation? A randomized single‐blind study of 55 patients examined with MRI. Acta Orthopaedica 2009;80(5):579‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2014
- Liu A, Xue X, Chen Y, Bi F, Yan S. The external rotation immobilisation does not reduce recurrence rates or improve quality of life after primary anterior shoulder dislocation: a systematic review and meta‐analysis. Injury 2014;45(12):1842‐7. [DOI] [PubMed] [Google Scholar]
Longo 2014
- Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy ‐ Journal of Arthroscopic and Related Surgery 2014;30(4):506‐22. [DOI] [PubMed] [Google Scholar]
Miller 2004
- Miller BS, Sonnabend DH, Hatrick C, O'Leary S, Goldberg J, Harper W, et al. Should acute anterior dislocations of the shoulder be immobilized in external rotation? A cadaveric study. Journal of Shoulder and Elbow Surgery 2004;13:589‐92. [DOI] [PubMed] [Google Scholar]
Moxon 2010
- Moxon AP, Walker T, Rando A. External rotation brace combined with a physiotherapy program for first time anterior shoulder dislocators: a 2 year follow‐up. Australasian Medical Journal 2010;1(4):253‐8. [Google Scholar]
Murad 2017
- Murad MH, Mustafa RA, Schünemann HJ, Sultan S, Santesso N. Rating the certainty in evidence in the absence of a single estimate of effect. BMJ Evidence‐Based Medicine 2017;22(3):85‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 2013
- Murray IR, Ahmed I, White NJ, Robinson CM. Traumatic anterior shoulder instability in the athlete. Scandinavian Journal of Medicine & Science in Sports 2013;23(4):387‐405. [DOI] [PubMed] [Google Scholar]
Murray 2018
- Murray JC, Leclerc A, Balatri A, Pelet S. Immobilization in external rotation after primary shoulder dislocation reduces the risk of recurrence in young patients. A randomized controlled trial. Orthopaedics & Traumatology: Surgery & Research 2018 Nov 27 [Epub ahead of print]. [doi: 10.1016/j.otsr.2018.10.007] [DOI] [PubMed]
O'Brien 1987
- O'Brien SJ, Warren RF, Schwartz EA. Anterior shoulder instability. Orthopedic Clinics of North America 1987;18(3):395‐408. [PubMed] [Google Scholar]
Olds 2015
- Olds M, Ellis R, Donaldson K, Parmar P, Kersten P. Risk factors which predispose first‐time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta‐analysis. British Journal of Sports Medicine 2015;49(14):913‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paterson 2010
- Paterson WH, Throckmorton TW, Koester M, Azar FM, Kuhn JE. Position and duration of immobilization after primary anterior shoulder dislocation: a systematic review and meta‐analysis of the literature. Journal of Bone and Joint Surgery. American Volume 2010;92(18):2924‐33. [DOI] [PubMed] [Google Scholar]
Pennekamp 2006
- Pennekamp W, Gekle C, Nicolas V, Seybold D. Initial results of shoulder MRI in external rotation after primary shoulder dislocation and after immobilization in external rotation [Initiale ergebnisse der schulter‐MRT in ausenrotation bei primarer schulterluxation und nach ruhigstellung in ausenrotation]. RoFo Fortschritte auf dem Gebiet der Rontgenstrahlen und der Bildgebenden Verfahren 2006;178(4):410‐5. [DOI] [PubMed] [Google Scholar]
Rhee 2009
- Rhee YG, Cho NS, Cho SH. Traumatic anterior dislocation of the shoulder: factors affecting the progress of the traumatic anterior dislocation. Clinics in Orthopedic Surgery 2009;1(4):188‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robinson 2006
- Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. Journal of Bone and Joint Surgery. American Volume 2006;88(11):2326‐36. [DOI] [PubMed] [Google Scholar]
Robinson 2012
- Robinson CM, Seah KTM, Chee YH, Hindle P, Murray IR. Frozen shoulder. Journal of Bone and Joint Surgery. British Volume 2012;94(1):1‐9. [DOI] [PubMed] [Google Scholar]
Schunemann 2011
- Schunemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glaziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Seybold 2009
- Seybold D, Schliemann B, Heyer CM, Muhr G, Gekle C. Which labral lesion can be best reduced with external rotation of the shoulder after a first‐time traumatic anterior shoulder dislocation?. Archives of Orthopaedic and Trauma Surgery 2009;129(3):299‐304. [DOI] [PubMed] [Google Scholar]
Siegler 2010
- Siegler J, Proust J, Marcheix PSM, Charissoux JL, Mabit C, Arnaud JP. Is external rotation the correct immobilisation for acute shoulder dislocation? An MRI study. Orthopaedics and Traumatology: Surgery and Research 2010;96(4):329‐33. [DOI] [PubMed] [Google Scholar]
Sullivan 2007
- Sullivan LG, Bailie R, Weiss N, Miller BS. An evaluation of shoulder external rotation braces. Arthroscopy 2007;23(2):129‐34. [DOI] [PubMed] [Google Scholar]
van der Linde 2015
- Linde JA, Kampen DA, Beers LW, Deurzen DF, Terwee CB, Willems WJ. The Oxford Shoulder Instability Score; validation in Dutch and first‐time assessment of its smallest detectable change. Journal of Orthopaedic Surgery and Research 2015;10(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Linde 2017
- Linde JA, Kampen DA, Beers LW, Deurzen DF, Saris DB, Terwee CB. The responsiveness and minimal important change of the Western Ontario Shoulder Instability Index and Oxford Shoulder Instability Score. Journal of Orthopaedic and Sports Physical Therapy 2017;47(6):402‐10. [DOI] [PubMed] [Google Scholar]
Vavken 2014
- Vavken P, Sadoghi P, Quidde J, Lucas R, Delaney R, Mueller AM, et al. Immobilization in internal or external rotation does not change recurrence rates after traumatic anterior shoulder dislocation. Journal of Shoulder and Elbow Surgery 2014;23(1):13‐9. [DOI] [PubMed] [Google Scholar]
Wasserstein 2016
- Wasserstein DN, Sheth U, Colbenson K, Henry PD, Chahal J, Dwyer T, Kuhn JE. The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy 2016;32(12):2616‐25. [DOI: 10.1016/j.arthro.2016.05.039] [DOI] [PubMed] [Google Scholar]
Whelan 2016
- Whelan DB, Kletke SN, Schemitsch G, Chahal J. Immobilization in external rotation versus internal rotation after primary anterior shoulder dislocation. American Journal of Sports Medicine 2016;44(2):521‐32. [DOI] [PubMed] [Google Scholar]
Zacchilli 2010
- Zacchilli MA, Owens Brett D. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. Journal of Bone and Joint Surgery ‐ American Volume 2010;92(3):542‐9. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Hanchard 2014
- Hanchard NC, Goodchild LM, Kottam L. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database of Systematic Reviews 2014, Issue 4. [DOI: 10.1002/14651858.CD004962.pub3] [DOI] [PubMed] [Google Scholar]
Handoll 2006
- Handoll HHG, Hanchard NCA, Goodchild LM, Feary J. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD004962.pub2] [DOI] [PubMed] [Google Scholar]


