Abstract
Background
Transpedicular screw insertion has become widely accepted for the correction of spinal deformity as well as degenerative and traumatic injury, but adoption of this technique has remained less widespread in the thoracic compared to the lumbar spine. This is thought to be associated with the relative technical difficulty of screw insertion into the narrower widths of the thoracic pedicles and the neurologic and mechanical risks associated with breach of the pedicle wall. The surgical decision making involves determining the appropriate sized screw for maximum fixation strength while simultaneously respecting the structural integrity of the vertebral pedicles to prevent a breach and provide better fixation. This paper presents a systematic review of criteria for thoracic pedicle screw diameter (SD) selection in order to orient inexperienced surgeons on the impact of this selection on pedicle breaching and fixation strength.
Methods
We performed a systematic literature review focused on studies reporting SD selection in relation to pedicle dimensions, measures of fixation strength, and breach rate.
Results
Twenty-nine articles that measured fixation strength, breach rate, and/or provided SD in relation to pedicle width were selected for inclusion.
Conclusions
A commonly accepted criteria for pedicle SD selection has not yet been proposed. Screw diameters approximately 80% of the pedicle width have been adopted, but this proportion is rarely reported in the midthoracic vertebrae for which smaller pedicles and inadequate hardware specificity result in higher breach rates. Depending upon the insertion technique adopted, greater specificity in diameter selection by vertebral level should be pursued in order to maximally target cortical bone purchase.
Clinical Relevance
Based on this review of the literature, we believe that proper selection of the SD for individual vertebral level directly affects the insertion technique and the potential breach.
Keywords: pedicle screws, bone fixation, fusion, thoracic spine, spine instrumentation
INTRODUCTION
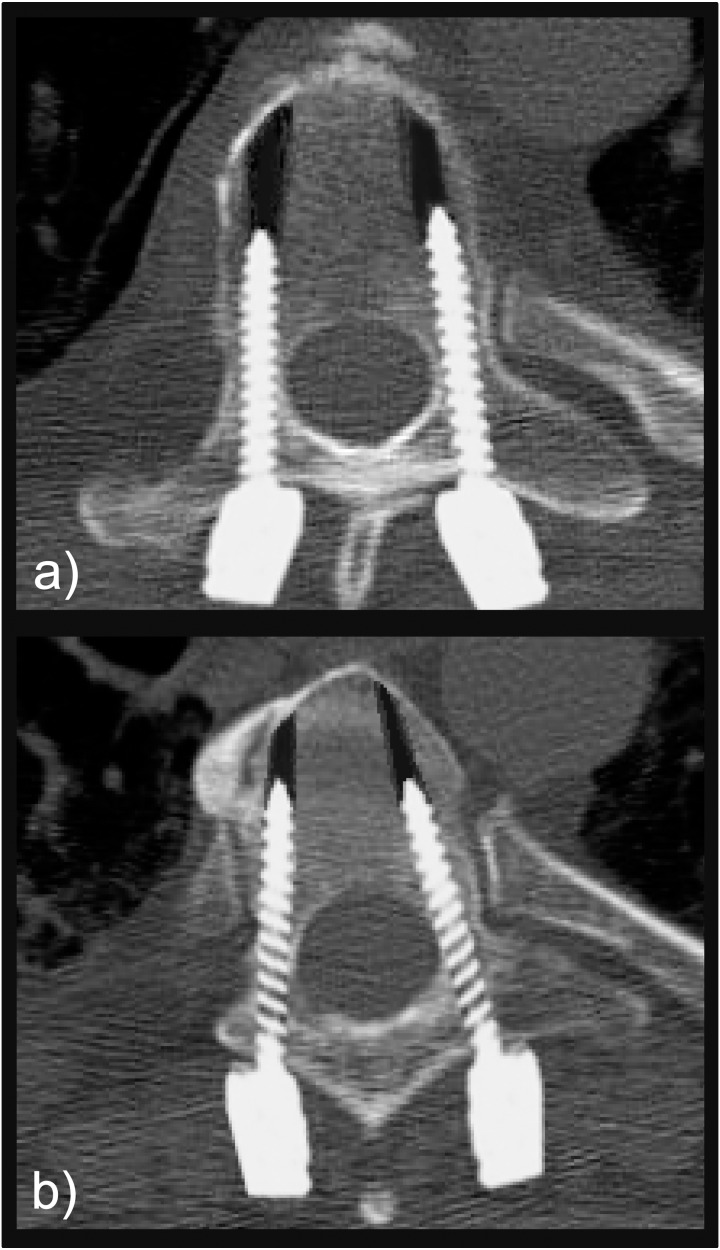
Transpedicular screw insertion has become the gold standard for spinal fixation used in the correction of spinal deformity1–3 and trauma.4–7 It is focused on achieving long-lasting fixation and strength and providing the scaffolding for a bony fusion. Despite the increased use of pedicle screw constructs, the insertion of pedicle screws in the thoracic spine represents unique challenges as compared to the earlier adopted instrumentation of lumbar segments. These challenges mainly stem from the increased technical difficulty in placing thoracic pedicle screws due to smaller sized pedicles and the proximity to neural, visceral, and vascular structures of the thorax.8,9 Screw misplacement (see Figure 1) can alter the pullout strength (POS)10 and can cause various complications such as intraoperative pedicle fracture, loosening, dural laceration, and transient neurologic injury.11 The accuracy of screw insertion has been analyzed extensively, and full containment within the cortical walls of the pedicle is achieved 69–94% of the time using the free-hand technique, with an increased range of 89–100% of attempts when utilizing computer tomography (CT) navigation across all vertebral levels.12 Additionally, a 2007 meta-analysis reporting on 130 studies representing 37 337 total screws reports an overall accuracy rate of 91.3% throughout the spine, with decreased accuracy at thoracic levels.13
Figure 1.
Pedicle screw insertion on computer generated images of (a) successfully placed screws and (b) misplaced screws: laterally for the right pedicle and medially for the left pedicle.
It has been shown that, when using currently accepted insertional techniques, malposition is strongly reduced with surgeon experience.14 Chen et al15 demonstrated that, using free-hand placement, an apprentice surgeon dangerously misplaced screws at a rate of 26.7%, in contrast to just 9.1% obtained by the chief surgeon. Furthermore, a minimum of 60 supervised screw placements were found to be necessary before the apprentice could accurately execute the free-hand technique independently. Additionally, in a 14-month period, Samdani et al16 reported a dangerous misplacement rate of 15.5% for a surgeon's first 181 implanted screws, which was reduced to 10.6% for the next 189 and 8.7% for the final 183 attempts. The selection of appropriate screw dimensions by vertebral level is key for successful insertion. As such, screw length is precisely pre-operatively and intraoperatively evaluated,17,18 but SD selection is left up to the experience of the surgeon.19 The tolerance for avoiding pedicle wall perforation has been theoretically proven to be reduced with increased SDs,20 while in actual placement, the screw is selected as the largest possible17,19 to achieve greater stability.21,22 These measures are reported, often in separate studies, as experiments measuring either pullout/fixation strength or breach rate of screws inserted in vitro or in cadaveric models. The resultant compromise between safety and stability that must be weighed for SD selection remains an important area of research which the current study will review.
This study aims to build a comprehensive systematic review of thoracic pedicle SD selection in order to summarize currently suggested selection criteria and demonstrate the impact that this decision can have on pedicle breaching and fixation strength. We hope these findings will be of particular interest to inexperienced surgeons for whom the breach rate in relation to SD has been shown to be significantly higher.
MATERIALS AND METHODS
Search Strategy
A systematic literature search was conducted in PubMed, Scopus, EMBASE and Biomed Central online databases using the syntax: (((thoracic) AND pedicle) AND screw) AND diameter. Of the 423 articles identified by this strategy, duplicates were removed, yielding 290 articles eligible for review. Following this initial search, we conducted 2 additional searches with the keywords “size” and “width” in place of “diameter.” After review, if articles were deemed worthy of inclusion, they were then checked against prior inclusions across all previous searches, and repeats were discarded. An additional 4 articles were also identified by hand search of the reference sections of articles identified by the review process.
Article Selection
Articles were selected for inclusion based on their contribution to 1 or more of 3 topics which we deemed relevant to our objective. These topics included (1) recommendations for appropriate SD selection including concurrent reporting of utilized SD and transverse pedicle dimension by vertebral level, (2) quantitative data on POS or insertional torque of pedicle screws of defined diameter, and (3) quantitative data on breach rate of inserted pedicle screws of defined diameter. Studies meeting inclusion criteria (2–3) are all linked by the reporting of SD across defined vertebral level(s), allowing for useful comparison between groups. Studies were excluded during the review process for meeting 1 or more of our 8 exclusion criteria: (1) full text article was unavailable, (2) article was not available in English, (3) morphometric study without actual screw placement or description of ideal screw dimension, (4) article contained no significant/sufficient discussion of 1 or more keywords, (5) article consisted of analysis irrelevant to the topic, (6) article discussed cervical or lumbar spinal segments rather than thoracic, (7) article detailed a nonhuman study, and/or (8) studies related to bicortical screw placements. Extraction of relevant data by 2 independent observers followed the review process, and any discrepancies were resolved by the lead author. Given the heterogeneity of the studies involved in this systematic review, we determined early on that it would not be feasible to combine data across studies for use in a quantitative meta-analysis. Instead, we set out to individually examine each study in order to extract the relevant information about the relationships between diameter, strength, and safety, while considering the unique strengths and limitations of each study.
Screw Diameter Selection in Relation to Pedicle Widths
In an attempt to uniform the reported diameters to the documented pedicle dimensions, since pedicles are mostly evaluated in CT axial slices through their transverse width, we calculated the ratios of SD to pedicle width (PW) in studies where both values were reported. In order to compute these ratios, the standard deviations were dropped from the reported values and are thus to be considered as approximations. Average ratios were computed with standard deviations, representing the average ratio of SD to PW by vertebral level across studies. Additionally, we calculated the average breach rate by level as documented in literature, and using 3 of the most referenced morphological studies on the pedicle dimensions, we correlated the breach rate to the PWs and to the adopted SD/PW ratio performing linear regression in Microsoft Excel software (Microsoft Corp., Redmond, Washington).
RESULTS
Search Results
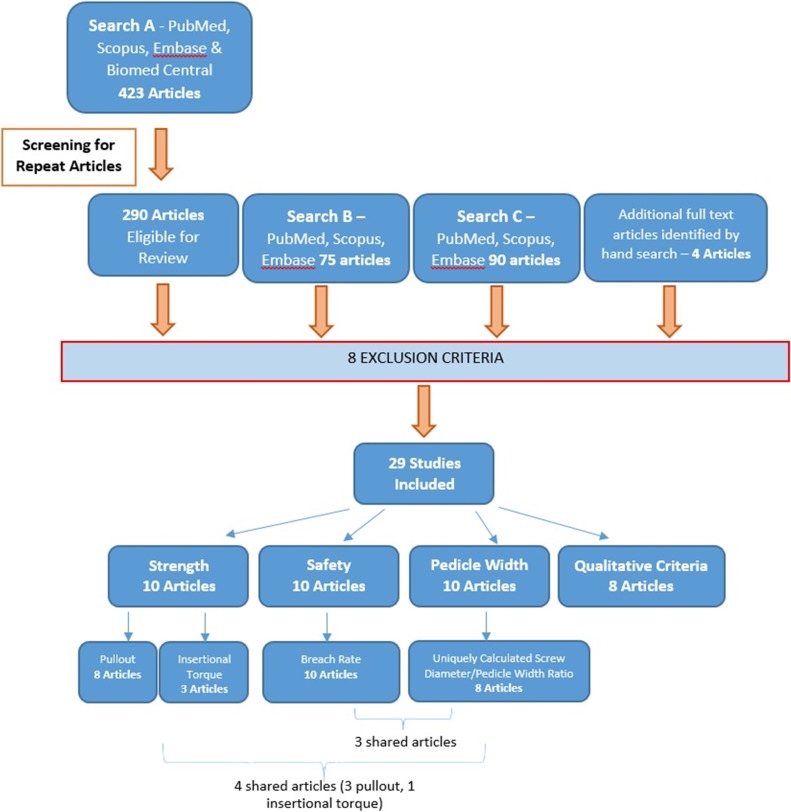
We identified 29 unique articles for inclusion in this review (see Figure 2). Among these studies, 18 provided information for SD selection in relationship to pedicle dimension, 10 reported quantifiable measures of fixation strength, and 10 reported values of breach rate. Studies providing recommendations for screw selection were often morphologic in nature and did not report data on safety/fixation strength of screw insertion. Of these, we reported the provided recommendations, and where possible, we calculated the SD to PW ratio, a measure that has been calculated in prior studies.23,24 Articles reporting fixation strength were further divided between those reporting POS of inserted screws and those reporting maximal insertional torque. Carmouche et al21 provided data on both of these measures of fixational strength and is thus listed twice in the summarizing table. There were 5 articles reporting measures of strength as well as PW22,25–28 and 4 articles reporting breach rate as well as PW.29–32
Figure 2.
Systematic review procedure: the exclusion criteria allowed the narrowing to a limited number of papers with detailed information on pedicle width, breach rate, and fixation strength.
Disclosed Criteria for Screw Diameter Selection
Articles which provided explicit recommendations for SD in relation to pedicle dimensions were highly variable (Table 1) and either consisted of a defined SD to PW ratio, a “pedicle fill” model,33 or discussed the clearance necessary between the diameters of the screw and pedicle.
Table 1.
Studies which offered recommendations for screw diameter (SD) in relation to pedicle width (PW): recommendations are reported with their relevant demographic to facilitate comparison across studies.
|
Study |
Recommendation |
Insertion Technique |
Subjects |
Average Age |
Range |
| Di Silvestre et al23 | SD should be 80% of PW. | Anatomical | Scoliosis patients | 33.4 | 12–54 |
| Suk et al37 | Ideal SD in adults is 80% of PW, but in children screws can be up to 115% of the PW. | Anatomical | Patients treated for spinal deformity | 18.5 | 2.7–70 |
| Takeshita et al24 | SD should not exceed 125% of PW. | Straightforward | Japanese scoliosis patients | 17.4 | 10–19 |
| Gstoettner et al36 | SD should not exceed 115% of PW. | Anatomical† | Scoliosis patients | 9–28 | |
| Lehman et al33 | SD chosen to achieve “70% pedicle fill.” | Not available | Generic cadaveric study | 62–93 | |
| Christodoulou et al35 | SD should closely match the internal trabecular PW and never exceed the external cortical PW. | Not available | Generic cadaveric study | 67.2 | 59–84 |
| Liau et al34 | SD should allow a 0.5 mm cortical margin on both the medial and lateral side to avoid fracture. | Anatomical† | Malaysian patients | 18–80 | |
| Kretzer et al16 | SD should allow a 0.5 mm cortical margin on both the medial and lateral side to avoid fracture. | Straightforward‡ | Random US patients | >18 | |
| Fujimoto et al32 | The size of the SD should be less than 0.5 mm smaller than the outer PW to be safely inserted in the pedicle cortex. | Not available | Japanese patients | 56 | 31–79 |
Measure taken considering the pedicle axis as reference.
Measures taken to best approximate the straightforward.
Suggested diameter values ranged from 80%23 to no more than 125% of PW.24 Two morphometric analyses of PW in different patient populations state that a 0.5 mm margin of cortical bone should be left on both the lateral and medial margins of the screw for safe fixation with both straightforward and anatomical insertion techniques.16,34
An additional study by Christodoulou et al,35 in which the insertion technique is not indicated, simply suggests that SD should be matched as closely as possible to the internal cortical diameter of the pedicle without ever exceeding the outer cortical width. Furthermore, when these studies are grouped by the age of their relevant patient population, only those dealing at least in part with a pediatric population offered recommendations for SD wider than the pedicle.24,36,37 These studies, based on both insertion techniques, define the upper limits for pediatric SD/PW between 1.15 and 1.25.
Of the 10 studies that concurrently reported PW and SD (Table 2), 5 also included measures of fixation strength, and 4 also include measures of breach rate. In an experimental study aimed at identifying criteria for safe diameter selection, Fujimoto et al,32 without specifying the insertion technique adopted, utilized SDs ranging from 4.0 to 6.5 mm and suggested that SDs should be 0.5 mm smaller than the PW. Helgeson et al25 defined the optimal screw size as the screw size equal to, or the first size smaller than, the PW but did not achieve this size in all the tested specimens that were instrumented with the straightforward technique.
Table 2.
Summary of data from studies concurrently reporting screw diameter and pedicle width.
|
Study |
Screw Diameter, mm (Vertebral Level) |
Pedicle Width, mm (Vertebral Level) |
Insertion Technique |
Screw Length (mm) |
Screw Type/Brand |
Average Age (Range) |
Sample Size |
| Chan et al29a | 5.0 (T1–6) | 5.2 (T1) | NA | NA | NA | NA | 240 |
| 6.0 (T7–12) | 4.9 (T2) | ||||||
| 4.3 (T3) | |||||||
| 4.2 (T4) | |||||||
| 4.1 (T5) | |||||||
| 4.4 (T6) | |||||||
| 5.0 (T7) | |||||||
| 4.9 (T8) | |||||||
| 5.3 (T9) | |||||||
| 6.3 (T10) | |||||||
| 6.9 (T11) | |||||||
| 6.6 (T12) | |||||||
| Holly et al30a | 4.0, 4.5, 5.5 (T1–12) | 4.4, 5.4, 7.9 (T1–12) | Anatomicalc | NA | NA | NA | 64 |
| Helgeson et al25b | 5.0 ± 0.80 and 5.70 ± 1.05 (T1–12) | 6.96 ± 1.89 (T1–12) | Straightforward | NA | Monoaxial, Medtronic, Sofamor-Danek, Memphis, Tenn | NA | 15 |
| Liljenqvist et al22b | 4.8 and 5.5 (T4–8) | 5.1± 1.1 (T4) | NA | T4–8: 35-40; T9–12: 45–50 | Munster System, Schorndorf, Germany | 74.3 (60–89) | 45 |
| 5.5, 6.5, and 7.2 (T9–12) | 5.0 ± 1.5 (T5) | ||||||
| 5.1 ± 1.2 (T6) | |||||||
| 5.4 ± 1.4 (T7) | |||||||
| 6.0 ± 1.3 (T8) | |||||||
| 6.6 ± 1.4 (T9) | |||||||
| 7.4 ± 1.3 (T10) | |||||||
| 8.8 ± 1.0 (T11) | |||||||
| 8.7 ± 1.3 (T12) | |||||||
| Hart et al31a | 4.0 (T1, T2) | 8.4± 1.7 (T1, T2) | Unique starting point | 30 | NA | NA | 129 |
| 4.0 (T4–7) | 5.7 ± 1.6 (T4–7) | ||||||
| 4.5 (T9, T10) | 7.1 ± 1.5 (T9, T10) | ||||||
| Fujimoto et al32a | |||||||
| Group 1 | 4.7 ± 0.8 (T2) | 6.7 ± 0.3 (T2) | NA | NA | Vertex System, CD Horizon Legacy Spinal System, Medtronic Sofamor-Danek, Memphis, Tenn | 56 (31–79) | 16 |
| 4.0 ± 0.0 (T3) | 6.3 ± 0.2 (T3) | ||||||
| 5.5 ± 0.0 (T8) | 6.4 ± 0.2 (T8) | ||||||
| 5.5 ± 0.8 (T9) | 6.5 ± 0.4 (T9) | ||||||
| Group 2 | 4.2 ± 0.3 (T2) | 5.4 ± 0.4 (T2) | NA | NA | Vertex System, CD Horizon Legacy Spinal System, Medtronic Sofamor-Danek, Memphis, Tenn | 56 (31–79) | 22 |
| 4.0 ± 0.0 (T3) | 4.7 ± 0.4 (T3) | ||||||
| 4.5 ± 0.0 (T4) | 4.6 ± 0.4 (T4) | ||||||
| 4.2 ± 0.3 (T5) | 4.8 ± 0.9 (T5) | ||||||
| 4.7 ± 0.9 (T6) | 5.2 ± 1.1 (T6) | ||||||
| 5.5 ± 0.0 (T7) | 6.3 ± 0.2 (T7) | ||||||
| 5.3 ± 0.4 (T8) | 5.6 ± 0.2 (T8) | ||||||
| 4.5 ± 0.9 (T9) | 4.6 ± 1.2 (T9) | ||||||
| Xie et al46 | 5.5 (T1) | 5.0 ± 0.2 (T1) | Anatomical | 30–40 | NA | 9.2 (6–12) | 206 |
| 5.5 (T2) | 4.7 ± 0.2 (T2) | ||||||
| 5.0 and 5.5 (T3) | 4.3 ± 0.2 (T3) | ||||||
| 4.5, 5.0, and 5.5 (T4–6) | 3.3 ± 0.3 (T4) | ||||||
| 5.0 and 5.5 (T7, T8) | 3.3 ± 0.2 (T5) | ||||||
| 3.1 ± 0.2 (T6) | |||||||
| 3.7 ± 0.1 (T7) | |||||||
| 3.9 ± 0.2 (T8) | |||||||
| Heller et al26b | 3.5 (T1–4) | 8.0 (T1) | NA | NA | Cortical Screw, Synthes, West Chester, Pa | 75 (NA) | 35 |
| 7.0 (T2) | |||||||
| 6.4 (T3) | |||||||
| 6.4 (T4) | |||||||
| Hongo et al27b | 5.5 (T5–12) | 6.4 ± 1.6 (T5–12) | Anatomical | NA | Polyaxial, Abbott Spine, Bordeaux, France | 75.8 (±12) | 8 |
| Matsukawa et alb | 5.5 or 6.5 (T9–12) | 6.0 ± 1.1 (T9) | Anatomical | 35–40 | Polyaxial SOLERA, Medtronic, Sofamor-Danek, Memphis, Tenn | 77.3 (65–83) | 44 |
| 6.8 ± 1.4 (T10) | |||||||
| 8.6 ± 1.3 (T11) | |||||||
| 9.1 ± 1.6 (T12) | |||||||
Abbreviation: NA, not available.
Fixation strength.
Breach rate.
Not disclosed but estimated from the figures shown.
Fixation Strength
Eight studies reported POS in relation to SD,10,22,25–27,38 3 studies reported maximum insertional torque, and 1 study by Carmouche et al21 offered both measures (Table 3). Due to the heterogeneity of the patient populations (age, bone mineral density [BMD], living versus cadaveric, etc), screw insertion techniques, and testing methods, it is not possible to concurrently analyze results across studies. Screw diameters and POSs were often reported as an average across multiple levels, in some cases across the entire thoracic spine, making meaningful comparisons between vertebral level and/or screw sizes impractical across studies. In 4 pullout studies, however, we see a clear intrastudy relationship between increased SD and increased POS.21,22,25,39 A similar relationship is observed in the 3 studies of maximal insertional torque wherein Carmouche et al21 and Mishiro et al40 report increases of 0.43 and 0.033 Nm of torque, respectively, with increasing SDs. The values reported by Matsukawa et al28 appear to break this trend, but this can be accounted for by their use of a novel insertion trajectory that achieved greater cortical bone purchase with a smaller 5.5 mm screw as opposed to a 6.5 mm screw inserted in the standard straightforward technique. The influence of insertion technique on POS has been revealed by studies instrumenting the lower thoracic segments with SDs of about 5.5 mm that have shown higher pullout loads when inserted in the straightforward technique25,38 than in the anatomical trajectory.27
Table 3.
Summary of data from studies which reported screw diameter in relation to a measure of fixation strength.
|
Study |
Screw Diameter, mm (Vertebral Level) |
Average Pullout Strength, N (Vertebral Level) |
Max. Insertional Torque, Nm (Vertebral Level) |
Insertion Technique |
Screw Length, mm |
Screw Type/Brand |
Average Age (range) |
Average BMD [g/cm2] |
Sample Size |
| Gayet et al39 | 4.0 or 5.0 (T1–12) | 820 ± 418, 1395 ± 435 (T1–12) | NA | 40 | NA | 62 (NA) | Normal | 24 | |
| Carmouche et al56 | 4.2 (T1–6) | 288.2 (T1–6) | NA | NA | USS, Synthes West Chester, PA | NA | 0.833 | 102 | |
| 5 (T7–12) | 361.5 (T7–12) | ||||||||
| Helgeson et al25 | 5.0 (±0.80) or 5.70 (±1.05) (T1–12) | 712.3 ± 223.1, 877.9 ± 235.2 (T1–12) | Straightforward | NA | Monoaxial, Medtronic Sofamor-Danek, Memphis, TN | NA | 0.6 ± 0.07 | 30 | |
| Paik et al38 | 5 (T1–12) | Normal BMD = 1049 ± 202, osteoporotic = 813 ± 228 (T1–12) | Straightforward | 35–45 | Polyaxial, CD Horizon Legacy Medtronic Sofamor-Danek | 81.5 (69–88) | 1.05, 0.563 | 15 | |
| Heller et al26 | 3.5 (T1–4) | 775 (T1) | NA | NA | Cortical Screw, Synthes, West Chester, PA | 75 (NA) | NA | 35 | |
| 747.5 (T2) | |||||||||
| 596.0 (T3) | |||||||||
| 544.2 (T4) | |||||||||
| Liljenqvist et al22 | 4.8 or 5.5 (T4–8) | 531.7 ± 213.8 (T4–8) | NA | T4–8: 35–40 T9–12: 45–50 | Munster System, Schorndorf, Germany | 74.3 (60–89) | 1.097 | 45 | |
| 5.5, 6.5 or 7.2 (T9–12) | 807.9 ± 207 (T9–12) | ||||||||
| Brasiliense et al10 | 4.5 (T6–11) | 839.6 ± 337.2 (T6–11) | Straightforward | 50 | Pangea System, Medtronic Spinal and Biologics | 53 (32–82) | 0.674 | 10 | |
| Hongo et al27 | 5.5 (T5–12) | 672 ± 412 (T5–12) | Anatomical | NA | Polyaxial, Abbott Spine, Bordeaux France | 75.8 ± 12 | 0.8 ± 0.28 | 8 | |
| Carmouche et al56 | 4.2 (T1–6) | 1.36 (T1–6) | NA | 40 | USS, Synthes, West Chester, PA | NA | 0.833 | 102 | |
| 5 (T7–12) | 1.79 (T7–12) | ||||||||
| Mishiro et al40 | 3.5 and 4.0 (T1–12) | 0.550 (±0.116), 0.588 (T1–12) | NA | NA | NA | 62.3 (48–70) | NA | 33 | |
| Matsukawa et al28 | 5.5 and 6.5 (T9–12) | 1.02 (±0.25) and 0.66 (±0.15) (T9–12) | Anatomical | 35-40 | Polyaxial Medtronic Sofamaor-Danek, Memphis, TN | 77.3 (65–83) | NA | 44 |
Abbreviation: BMD, bone mass density, NA, not available.
Breach Ratio
Of the studies that reported breach rates in relation to SD, screw sizes ranged from 3.5 to 7.9 mm, and breach rates ranged from 100% at T3 with a 4.0 mm screw, to 0% at multiple levels with varying SDs (Table 4). Breach was defined differently by multiple studies. In Koktekir et al,41 greater than 25% of the outer SD needed to reside outside the pedicle wall in order to count as breach, whereas Fujimoto et al32 stated that a screw was either contained fully within the pedicle or was counted as breach. Most studies appear to follow the latter model of recording any perforation of the pedicle wall, and Payer et al5 states that, in their analysis, cases of questionable cortical integrity were counted as breach. Furthermore, Belmont et al42 states that medial perforations are safe up to 2 mm, while lateral perforations are safe up to 6 mm. Similarly, Chan et al29 defines safe perforations as less than 2 mm. In the 5 studies that defined the safety of their breaches, only 10 of the 310 cumulative perforations, just 3.23%, were deemed unsafe.
Table 4.
Summary of data from studies which reported screw diameter in relation to breach rate.
|
Study |
Screw Diameter, mm (Vertebral Level) |
Breach Rate, % (Vertebral Level) |
Insertion Technique |
Screw Length (mm) |
Average Age (Range) |
Sample Size |
| Belmont et al42 | 4.5 (T1) | 50 (T1) | NA | NA | 24 (6–56) | 279 |
| 4.5 (T2) | 75 (T2) | |||||
| 4.5 (T3) | 60 (T3) | |||||
| 4.5 (T4) | 79 (T4) | |||||
| 4.5 (T5) | 79 (T5) | |||||
| 4.5 (T6) | 65 (T6) | |||||
| 4.5 (T7) | 55 (T7) | |||||
| 4.5 (T8) | 47 (T8) | |||||
| 4.5 (T9) | 43 (T9) | |||||
| 5.5 or 6.5 (T10) | 28 (T10) | |||||
| 5.5 or 6.5 (T11) | 25 (T11) | |||||
| 5.5 or 6.5 (T12) | 24 (T12) | |||||
| Koktekir et al41 | 4.0–5.0 (T1–12) | 0 (T1) | NA | 30–50 | 56.5 (14–82) | 256 |
| 0 (T1) | ||||||
| 0 (T2) | ||||||
| 0 (T3) | ||||||
| 0 (T4) | ||||||
| 0 (T5) | ||||||
| 0 (T6) | ||||||
| 0 (T7) | ||||||
| 0 (T8) | ||||||
| 0 (T9) | ||||||
| 2.40 (T10) | ||||||
| 4.20 (T11) | ||||||
| 1.50 (T12) | ||||||
| Cho et al45 | >7.7 (T1) | 100 (T1–12) | Anatomical | NA | 74.5 (61–82) | 162 |
| >6.5 (T2) | ||||||
| >6.5 (T3) | ||||||
| >5.8 (T4) | ||||||
| >6.6 (T5) | ||||||
| >6.5 (T6) | ||||||
| >6.5 (T7) | ||||||
| >7.5 (T8) | ||||||
| >7.7 (T9) | ||||||
| >7.7 (T10) | ||||||
| >7.5 (T11) | ||||||
| >7.9 (T12) | ||||||
| Holly et al30 | 4, 4.5 and 5.5 (T1–12) | 7.80 (T1–12) | †Anatomical | NA | NA | 64 |
| Chan et al29 | 5 (T1–6) | 10.40 (T1–12) | NA | NA | NA | 240 |
| 6 (T7–12) | ||||||
| Ranade et al43 | 3.5–5.5 (T1–12) | 0 (T1) | NA | 25–30 | 4.6 (3.25–7.9) | 30 |
| 25 (T2) | ||||||
| 0 (T3) | ||||||
| 0 (T4) | ||||||
| 0 (T5) | ||||||
| 0 (T6) | ||||||
| 0 (T10) | ||||||
| 25 (T11) | ||||||
| 12.50 (T12) | ||||||
| Mac-Thiong et al44 | 4.5 (T1–11) | 16.70 (T1) | Sagittal angle of 15° | 38 | NA “elderly” | 66 |
| 0 (T2) | ||||||
| 0 (T3) | ||||||
| 16.70 (T4) | ||||||
| 0 (T5) | ||||||
| 0 (T6) | ||||||
| 0 (T7) | ||||||
| 16.70 (T8) | ||||||
| 16.70 (T9) | ||||||
| 16.70 (T10) | ||||||
| 0 (T11) | ||||||
| Hart et al31 | 4 (T1, T2) | 9 (T1, T2) | Unique starting point | 30 | NA | 129 |
| 4 (T4–7) | 47 (T4–7) | |||||
| 4.5 (T9, T10) | 16 (T9, T10) | |||||
| Fujimoto et al32 | ||||||
| Group 1 | 4.7 ± 0.8 (T2) | 0 (T1) | NA | NA | 56 (31–79) | 16 and 22 |
| 4.0 ± 0.0 (T3) | 0 (T3) | |||||
| 5.5 ± 0.0 (T8) | 0 (T8) | |||||
| 5.5 ± .8 (T9) | 14 (T9) | |||||
| Group 2 | 4.2 ± 0.3 (T2) | 33 (T2) | ||||
| 4.0 ± 0.0 (T3) | 100 (T3) | |||||
| 4.5 ± 0.0 (T4) | 67 (T4) | |||||
| 4.2 ± 0.3 (T5) | 50 (T5) | |||||
| 4.7 ± 0.9 (T6) | 75 (T6) | |||||
| 5.5 ± 0.0 (T7) | 0 (T7) | |||||
| 5.3 ± 0.4 (T8) | 50 (T8) | |||||
| 4.5 ± 0.9 (T9) | 67 (T9) | |||||
| Payer et al5 | 4.5 (T1–7) | 10 (T1–7) | Straightforward | 30–40 | 40 (20–65) | 62 |
Abbreviation: NA, not available.
Holly et al30 reported breaches mainly in the segments T4–8, where screws 4 mm in diameter were placed in PWs ranging from 4.1 to 4.4 mm. Hart et al31 detailed PW values as well as breach rates. He used 4.0 and 4.5 mm screws and found lateral breach of 100% for 2.99 mm pedicles, which is reduced to 61% for PWs of 4.0 to 4.99 mm, and a minimal breach rate of 13% for PWs of 9.0 to 9.99 mm. Lastly, Fujimoto et al32 divided their specimens into 2 groups which warranted separate reporting in the table. Group 1 screws had a diameter less than the inner PW (ie, the transverse diameter of the inner cortical walls of the pedicle), while Group 2 screws had a diameter greater than the inner PW. According to the findings of Fujimoto et al,32 when SD is selected to be larger than the inner PW, the average breach rate can be as high as 54.5% but can be reduced to 6.3% for screws smaller than the inner PW.
Most of the studies reporting on breach rate did not provide any indication of the insertion technique adopted.43,44 However, a comparison can be made for a 4.5 mm SD inserted into the upper thoracic segments, for which the straightforward technique5 has shown higher breach rates than the anatomical trajectory.30,45
Screw Diameter Selection in Relation to Pedicle Width
Of the 10 studies that concurrently reported PW and SD, Holly et al30 and Liljenqvist et al22 were not included in SD/PW calculations because they reported nonspecific SDs across vertebral levels, making it impossible to calculate meaningful ratios by vertebral level. This left 8 studies with SD/PW ratios to report. In relation to PW, screws inserted with the straightforward technique25 were smaller than screws adopted with the anatomical technique.27,46,47 Xie et al46 provided their own SD/PW ratios with calculated standard deviations, so these were reported without additional calculation and can be considered exact.
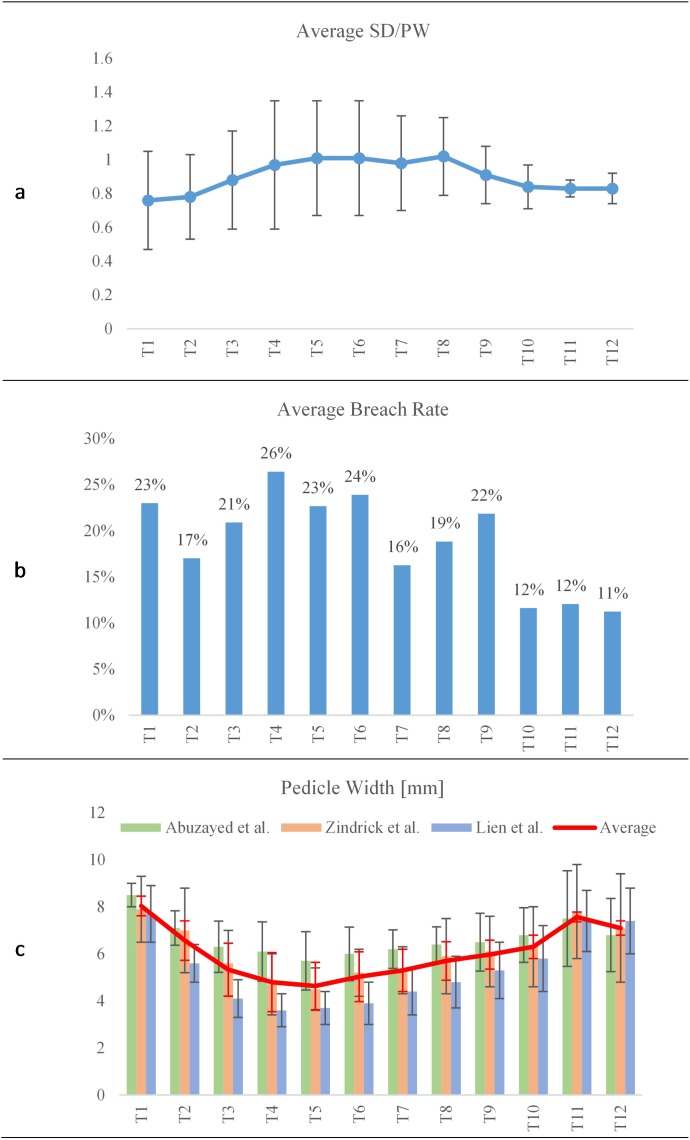
Regardless of the insertion technique adopted, when we calculated the average SD/PW for each vertebral level, we found the lowest value at T1 with a ratio of 0.76 ± 0.29 (see Figure 3), which increased through the midthoracic vertebrae to a peak of 1.02 ± 0.23 at T8 before decreasing towards T12 with a ratio of 0.83 ± 0.09 (Table 5).
Figure 3.
Average values calculated for screw diameter (SD) to pedicle width (PW), breach rate, and PW.
Table 5.
Screw diameter (SD) to pedicle width (PW) ratios calculated in the current study (□ indicates studies also reporting on fixation strength and ⋄ indicates studies also reporting on breach rate).
|
Study |
Insertion Technique |
SD/PW Ratio (Vertebral Level) |
| ⋄Chan et al28 | NA | 0.96 (T1) |
| 1.02 (T2) | ||
| 1.16 (T3) | ||
| 1.19 (T4) | ||
| 1.22 (T5) | ||
| 1.14 (T6) | ||
| 1.20 (T7) | ||
| 1.22 (T8) | ||
| 1.13 (T9) | ||
| 0.95 (T10) | ||
| 0.87 (T11) | ||
| 0.91 (T12) | ||
| □Helgeson et al25 | Straightforward | 0.72 and 0.82 (T1–12) |
| ⋄Hart et al31 | Unique starting point | 0.48 (T1, T2) |
| 0.7 (T4–7) | ||
| 0.63 (T9, T10) | ||
| ⋄Fujimoto et al32 | ||
| Group 1 | NA | 0.7 (T2) |
| 0.63 (T3) | ||
| 0.86 (T8) | ||
| 0.85 (T9) | ||
| Group 2 | 0.78 (T2) | |
| 0.85 (T3) | ||
| 0.98 (T4) | ||
| 0.88 (T5) | ||
| 0.9 (T6) | ||
| 0.87 (T7) | ||
| 0.95 (T8) | ||
| 0.98 (T9) | ||
| Xie et al46 | Anatomical | 1.101 ± 0.051 (T1) |
| 1.166 ± 0.042 (T2) | ||
| 1.278 ± 0.050 (T3) | ||
| 1.586 ± 0.0112 (T4) | ||
| 1.596 ± 0.089 (T5) | ||
| 1.640 ± 0.068 (T6) | ||
| 1.444 ± 0.069 (T7) | ||
| 1.390 ± 0.066 (T8) | ||
| □Heller et al26 | NA | 0.44 (T1) |
| 0.5 (T2) | ||
| 0.55 (T3) | ||
| 0.55 (T4) | ||
| □Hongo et al27 | Anatomical | 0.86 (T5–12) |
| □Matsukawa et al28 | Anatomical | 1.08 (T9) |
| 0.96 (T10) | ||
| 0.76 (T11) | ||
| 0.71 (T12) | ||
Abbreviation: NA, not available.
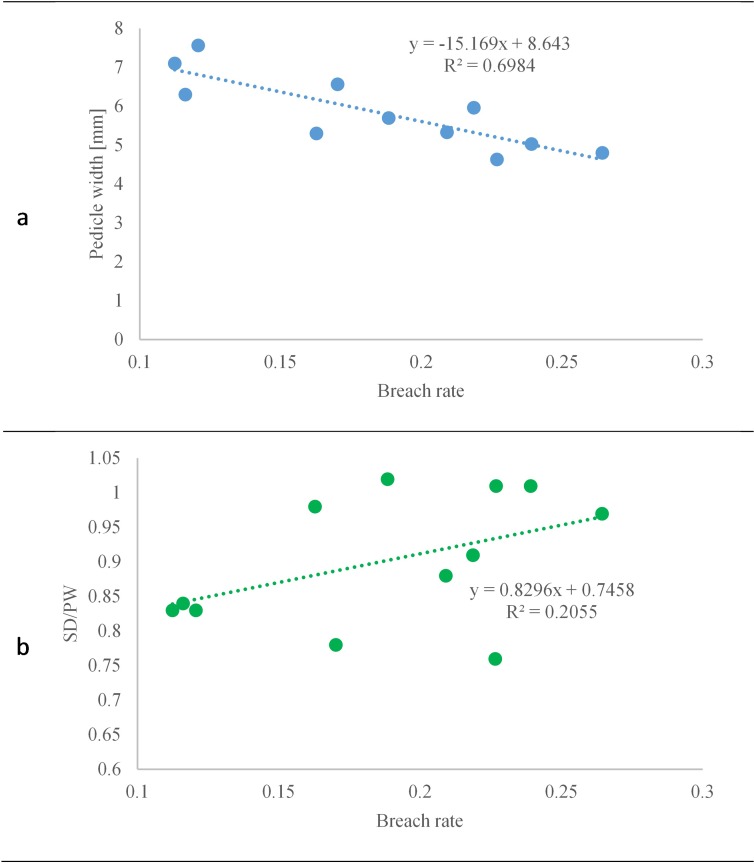
The breach rate has been evaluated as being inversely proportional to the PW, with a coefficient of determination of 0.7 (see Figure 4). The smallest value of breach rate is associated with pedicles of 7.1 mm in width. Considering the entire thoracic spine, a weak correlation (R2 = 0.20) has been found between the breach rate and the SD/PW ratio; however, the smallest values of breach rate are associated with the lower vertebrae T10–12, where very similar ratios within the range of 0.83 ± 0.05 to 0.84 ± 0.13 are used.
Figure 4.
Breach rate correlation with (a) pedicle width and (b) screw diameter to pedicle width ratio.
DISCUSSION
The data collected in this review allowed for an overview of SD selection in relation to vertebral level and insertion technique adopted. Despite our best efforts, there are some limitations of this review that should be mentioned. Gender of cadaveric and human subjects was rarely reported in the included studies, even though pedicle diameter has been clearly demonstrated to differ between men and women. As such, we were unable to consider the effect of this variation in our study. Additionally, screw design is clearly an important variable, especially for measures of fixation strength. Screw design and manufacturer were reported where available; however, many studies did not report on screw type. The variability of results among studies is almost certainly due in part to differences in screw design such as thread crest and pitch, which were rarely reported, much less discussed by the included studies.
Furthermore, the SD in relation to PW is meaningless when insertion technique is not disclosed. For example, Helgeson et al,25 using the straightforward technique, reports a mean POS of 877.9 ± 235.2 N with a calculated SD/PW of 0.82, while Hongo et al,27 using the anatomical technique, reports a mean POS of 672 ± 412 N with a calculated SD/PW of 0.86. In addition, Helgeson et al25 reported an average BMD of 0.6 ± 0.07g/cm2, while Hongo et al27 reported an average BMD of 0.8 ± 0.28g/cm2, with the commonly accepted cutoff for osteoporosis stated as density less than 0.9g/cm2. In cases of osteoporosis, BMD has been shown to strongly correlate with POS,38 and the large difference in reported POS between Gayet et al39 and Carmouche et al21 with similar sized screws is likely due to the parallel difference in the BMD of their specimens. Studies such as Carmouche et al,21 cited in this review, have clearly demonstrated the correlation between increased insertional torque and increased pullout resistance in osteoporotic bone. This is likely due to the advantage it provides in achieving greater bony purchase of cortical bone, which can be highly variable between patients due to age,48 as well as demonstrated differences between men and women.34 In recent biomechanical studies, it has been demonstrated that the density of the bone in contact with the screw threads is strongly correlated with POS.49,50 As a result, the variable of SD can be seen as a means of achieving increased cortical bone purchase.
Breach rate peaked among found studies from T4–6 (see Figure 3b), which can be predicted by many studies which characterize T3–7 as having the smallest pedicles, with T5 often reported as the smallest overall.29,35,51 To confirm these relationships, we combined data from 3 frequently cited morphological studies of PW (see Figure 3c), which showed a minimum of 4.63 mm at T5 and a maximum of 7.57 mm at T11.52–54 A direct comparison of average breach rate by vertebral level with the average morphologic values of PW shows a clear inverse relationship between PW and breach rate (see Figure 4a). Considering the entire thoracic spine, a weak correlation (R2 = 0.20) has been found between the breach rate and the SD/PW ratio (see Figure 4b), as seen in previous studies.29,31,32 Despite the poor correlation, breach rates associated with an SD/PW ratio of around 0.8 are consistently among the lowest overall. A ratio of 0.8 then can be reasonably suggested as a conservative starting point for SD selection for the inexperienced surgeon. When we consider the average SD/PW ratios calculated by vertebral level, we see an increase in ratio from T1 to T4 through T8 and a decrease in the lower thoracic spine towards T12. This can be accounted for by the fact that most studies do not make SD selections by individual segment, but rather utilize 1 or 2 SDs over multiple segments, or sometimes over the entire thoracic spine.25,38,55,56 The bandwidth in breach rates seen in Figure 3a can be reduced by greater specificity of screw selection by vertebral level. It should be noted that screw sizes available from the major manufacturers are limited, typically in 0.5 mm increments. Two studies in the current review specifically noted the inadequacy of current pedicle screw systems for instrumenting the midthoracic levels, with Liau et al34 commenting that current systems are not suitable for the majority of the Malay population, and Gstoettner et al36 concluding that one-third of midthoracic pedicles of scoliosis patients cannot be instrumented safely.
A final point of discussion we would like to propose is the clear difference in acceptable SD/PW in pediatric versus adult populations. Of the qualitative studies found, 3 made SD/PW recommendations relevant for pediatric populations and averaged 1.18.24,36,37 These high SD/PW values can be explained by the relative plasticity of the pedicle cortex in the pediatric spine, which has been suggested to be capable of expanding 25% upon screw insertion.24,37
CONCLUSIONS
A commonly accepted criteria for pedicle SD selection in adult thoracic fixation has yet to be proposed in the literature. Although 80% of the PW defines the SD as reported by several authors, this assertion is rarely reported for the midthoracic region of the spine. These vertebras are characterized by relatively narrower pedicles where high pedicle breaches are usually found. This could be associated with the unavailability of SD sizes. In addition, fixation strength has been shown to be associated with BMD and cortical bone purchase, but it is not directly related to the SD/PW ratio. Based on this review of the literature, we believe that proper selection of the SD for individual vertebral level directly affects the insertion technique and the potential breach.
REFERENCES
- 1.Cuartas E, Rasouli A, O'Brien M, Shufflebarger HL. Use of all-pedicle-screw constructs in the treatment of adolescent idiopathic scoliosis. J Am Acad Orthop Surg. 2009;17(9):550–561. doi: 10.5435/00124635-200909000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Lykissas MG, Jain VV, Nathan ST, et al. Mid- to long-term outcomes in adolescent idiopathic scoliosis after instrumented posterior spinal fusion: a meta-analysis. Spine (Phila Pa 1976) 2013;38(2):E113–E119. doi: 10.1097/BRS.0b013e31827ae3d0. https://doi.org/10.1097/BRS.0b013e31827ae3d0. [DOI] [PubMed] [Google Scholar]
- 3.Crawford AH, Lykissas MG, Gao X, Eismann E, Anadio J. All-pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery: a comparative radiographical study with a minimum 2-year follow-up. Spine (Phila Pa 1976) 2013;38(14):1199–1208. doi: 10.1097/BRS.0b013e31828ce597. https://doi.org/10.1097/BRS.0b013e31828ce597. [DOI] [PubMed] [Google Scholar]
- 4.Hartl R, Theodore N, Dickman CA, Sonntag VKH. Technique of thoracic pedicle screw fixation for trauma. Oper Tech Neurosurg. 2004;7(1):22–30. https://doi.org/10.1053/j.otns.2004.04.005. [Google Scholar]
- 5.Payer M. Unstable upper and middle thoracic fractures. Preliminary experience with a posterior transpedicular correction-fixation technique. J Clin Neurosci. 2005;12(5):529–533. doi: 10.1016/j.jocn.2004.11.006. https://doi.org/10.1016/j.jocn.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, Benes V. Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine. 2014;20(2):150–156. doi: 10.3171/2013.11.SPINE13479. https://doi.org/10.3171/2013.11.SPINE13479. [DOI] [PubMed] [Google Scholar]
- 7.Toyone T, Ozawa T, Inada K, et al. Short-segment fixation without fusion for thoracolumbar burst fractures with neurological deficit can preserve thoracolumbar motion without resulting in post-traumatic disc degeneration: a 10-year follow-up study. Spine (Phila Pa 1976) 2013;38(17):1482–1490. doi: 10.1097/BRS.0b013e318297bdb7. https://doi.org/10.1097/BRS.0b013e318297bdb7. [DOI] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Georges J, Rongming X, Yeasting R. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine (Phila Pa 1976) 1997;22(14):1553–1556. doi: 10.1097/00007632-199707150-00002. [DOI] [PubMed] [Google Scholar]
- 9.Sarwahi V, Suggs W, Wollowick AL, et al. Pedicle screws adjacent to the great vessels or viscera: a study of 2132 pedicle screws in pediatric spine deformity. J Spinal Disord Tech. 2014;27(2):64–69. doi: 10.1097/BSD.0b013e31825bfecd. https://doi.org/10.1097/BSD.0b013e31825bfecd. [DOI] [PubMed] [Google Scholar]
- 10.Brasiliense LBC, Theodore N, Lazaro BCR, et al. Quantitative analysis of misplaced pedicle screws in the thoracic spine: how much pullout strength is lost? J Neurosurg Spine. 2010;12(5):503–508. doi: 10.3171/2009.11.SPINE09408. https://doi.org/10.3171/2009.11.SPINE09408. [DOI] [PubMed] [Google Scholar]
- 11.Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 2010;35(11):E465–E470. doi: 10.1097/BRS.0b013e3181d1021a. https://doi.org/10.1097/BRS.0b013e3181d1021a. [DOI] [PubMed] [Google Scholar]
- 12.Gelalis ID, Paschos NK, Pakos EE, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21(2):247–255. doi: 10.1007/s00586-011-2011-3. https://doi.org/10.1007/s00586-011-2011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32(3):E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. https://doi.org/10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 14.Wood M, Jason M. The surgical learning curve and accuracy of minimally invasive lumbar pedicle screw placement using CT based computer-assisted navigation plus continuous electromyography monitoring—a retrospective review of 627 screws in 150 patients. Int J Spine Surg. 2015;8:1–20. doi: 10.14444/1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen G, Li H, Li F, Chen W, Chen Q. Learning curve of thoracic pedicle screw placement using the free-hand technique in scoliosis: how many screws needed for an apprentice? Eur Spine J. 2012;21(6):1151–1156. doi: 10.1007/s00586-011-2065-2. https://doi.org/10.1007/s00586-011-2065-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kretzer RM, Chaput C, Sciubba DM, et al. A computed tomography-based morphometric study of thoracic pedicle anatomy in a random United States trauma population. J Neurosurg Spine. 2011;14(2):235–243. doi: 10.3171/2010.9.SPINE1043. https://doi.org/10.3171/2010.9.SPINE1043. [DOI] [PubMed] [Google Scholar]
- 17.Fennell VS, Palejwala S, Skoch J, Stidd DA, Baaj AA. Freehand thoracic pedicle screw technique using a uniform entry point and sagittal trajectory for all levels: preliminary clinical experience. J Neurosurg Spine. 2014;21(5):778–784. doi: 10.3171/2014.7.SPINE1489. https://doi.org/10.3171/2014.7.SPINE1489. [DOI] [PubMed] [Google Scholar]
- 18.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976) 2004;29(3):333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 19.Nottmeier EW, Seemer W, Young PM. Placement of thoracolumbar pedicle screws using three-dimensional image guidance: experience in a large patient cohort. J Neurosurg Spine. 2009;10(1):33–39. doi: 10.3171/2008.10.SPI08383. https://doi.org/10.3171/2008.10.SPI08383. [DOI] [PubMed] [Google Scholar]
- 20.Rampersaud YR, Simon DA, Foley KT. Accuracy requirements for image-guided spinal pedicle screw placement. Spine (Phila Pa 1976) 2001;26(4):352–359. doi: 10.1097/00007632-200102150-00010. [DOI] [PubMed] [Google Scholar]
- 21.Carmouche JJ, Molinari RW, Gerlinger T, Devine J, Patience T. Effects of pilot hole preparation technique on pedicle screw fixation in different regions of the osteoporotic thoracic and lumbar spine. J Neurosurg Spine. 2005;3(5):364–370. doi: 10.3171/spi.2005.3.5.0364. https://doi.org/10.3171/spi.2005.3.5.0364. [DOI] [PubMed] [Google Scholar]
- 22.Liljenqvist U, Hackenberg L, Link T, Halm H. Pullout strength of pedicle screws versus pedicle and laminar hooks. Acta Orthop Belg. 2001;67(2):3–9. [PubMed] [Google Scholar]
- 23.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976) 2007;32(15):1655–1661. doi: 10.1097/BRS.0b013e318074d604. https://doi.org/10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 24.Takeshita K, Maruyama T, Chikuda H, et al. Diameter, length, and direction of pedicle screws for scoliotic spine: analysis by multiplanar reconstruction of computed tomography. Spine (Phila Pa 1976) 2009;34(8):798–803. doi: 10.1097/BRS.0b013e3181895c36. https://doi.org/10.1097/BRS.0b013e3181895c36. [DOI] [PubMed] [Google Scholar]
- 25.Helgeson MD, Kang DG, Lehman RA, Dmitriev AE, Luhmann SJ. Tapping insertional torque allows prediction for better pedicle screw fixation and optimal screw size selection. Spine J. 2013;13(8):957–965. doi: 10.1016/j.spinee.2013.03.012. https://doi.org/10.1016/j.spinee.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 26.Heller JG, Shuster JK, Hutton WC. Pedicle and transverse process screws of the upper thoracic spine: biomechanical comparison of loads to failure. Spine (Phila Pa 1976) 1999;24(7):654–658. doi: 10.1097/00007632-199904010-00008. [DOI] [PubMed] [Google Scholar]
- 27.Hongo M, Ilharreborde B, Gay RE, et al. Biomechanical evaluation of a new fixation device for the thoracic spine. Eur Spine J. 2009;18(8):1213–1219. doi: 10.1007/s00586-009-0999-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matsukawa K, Yato Y, Hynes RA, et al. Cortical bone trajectory for thoracic pedicle screws: a technical note. J Spinal Disord Tech. 2017;30(5):E497–E504. doi: 10.1097/BSD.0000000000000130. https://doi.org/10.1097/BSD.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 29.Chan CYW, Kwan MK, Saw LB. Thoracic pedicle screw insertion in Asian cadaveric specimen: does radiological pedicle profile affect outcome? Surg Radiol Anat. 2011;33(1):19–25. doi: 10.1007/s00276-010-0726-1. https://doi.org/10.1007/s00276-010-0726-1. [DOI] [PubMed] [Google Scholar]
- 30.Holly LT, Foley KT. Three-dimensional fluoroscopy-guided percutaneous thoracolumbar pedicle screw placement. J Neurosurg Spine. 2003;99(3 Suppl):324–329. doi: 10.3171/spi.2003.99.3.0324. [DOI] [PubMed] [Google Scholar]
- 31.Hart RA, Hansen BL, Shea M, Hsu F, Anderson GJ. Pedicle screw placement in the thoracic spine: a comparison of image-guided and manual techniques in cadavers. Spine (Phila Pa 1976) 2005;30(12):E326–E331. doi: 10.1097/01.brs.0000166621.98354.1d. [DOI] [PubMed] [Google Scholar]
- 32.Fujimoto T, Sei A, Taniwaki T, Okada T, Yakushiji T, Mizuta H. Pedicle screw diameter selection for safe insertion in the thoracic spine. Eur J Orthop Surg Traumatol. 2012;22(5):351–356. https://doi.org/10.1007/s00590-011-0846-2. [Google Scholar]
- 33.Lehman R a, Polly DW, Kuklo TR, Cunningham B, Kirk KL, Belmont PJ. Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine (Phila Pa 1976) 2003;28(18):2058–2065. doi: 10.1097/01.BRS.0000087743.57439.4F. https://doi.org/10.1097/01.BRS.0000087743.57439.4F. [DOI] [PubMed] [Google Scholar]
- 34.Liau KM, Yusof MI, Abdullah MS, Abdullah S, Yusof AH. Computed tomographic morphometry of thoracic pedicles: safety margin of transpedicular screw fixation in Malaysian Malay population. Spine (Phila Pa 1976) 2006;31(16):E545–E550. doi: 10.1097/01.brs.0000225978.97652.e0. [DOI] [PubMed] [Google Scholar]
- 35.Christodoulou AG, Apostolou T, Ploumis A, Terzidis I, Hantzokos I, Pournaras J. Pedicle dimensions of the thoracic and lumbar vertebrae in the Greek population. Clin Anat. 2005;18(6):404–408. doi: 10.1002/ca.20155. [DOI] [PubMed] [Google Scholar]
- 36.Gstoettner M, Lechner R, Glodny B, Thaler M, Bach CM. Inter- and intraobserver reliability assessment of computed tomographic 3D measurement of pedicles in scoliosis and size matching with pedicle screws. Eur Spine J. 2011;20(10):1771–1779. doi: 10.1007/s00586-011-1908-1. https://doi.org/10.1007/s00586-011-1908-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suk S-I, Kim W-J, Lee S-M, Kim J-H, Chung E-R. Thoracic pedicle screw fixation in spinal deformities. Spine (Phila Pa 1976) 2001;26(18):2049–2057. doi: 10.1097/00007632-200109150-00022. https://doi.org/10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 38.Paik H, Kang DG, Lehman RA, Gaume RE, Ambati D V, Dmitriev AE. The biomechanical consequences of rod reduction on pedicle screws: should it be avoided? Spine J. 2013;13(11):1617–1626. doi: 10.1016/j.spinee.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 39.Gayet L, Pries P, Hamcha H, Clarac J-P, Texereau J. Biomechanical study and digital modeling of traction resistance in posterior thoracic implants. Spine (Phila Pa 1976) 2002;27(7):707–714. doi: 10.1097/00007632-200204010-00007. [DOI] [PubMed] [Google Scholar]
- 40.Mishiro T, Sairyo K, Shinohara A, Chikawa T, Kosaka H, Dezawa A. Assessment of maximal insertional torque of cervical and thoracic screws during posterior spinal surgery. J Med Investig. 2014;61(3–4):393–398. doi: 10.2152/jmi.61.393. [DOI] [PubMed] [Google Scholar]
- 41.Koktekir E, Ceylan D, Tatarli N, Karabagli H, Recber F, Akdemir G. Accuracy of fluoroscopically-assisted pedicle screw placement: analysis of 1,218 screws in 198 patients. Spine J. 2014;14(8):1702–1708. doi: 10.1016/j.spinee.2014.03.044. https://doi.org/10.1016/j.spinee.2014.03.044. [DOI] [PubMed] [Google Scholar]
- 42.Belmont PJ, Kemme W, Dhavan A, Polly D. In vivo accuracy of thoracic pedicle screws. Spine (Phila Pa 1976) 2001;26(21):2340–2346. [Google Scholar]
- 43.Ranade A, Samdani AF, Williams R, et al. Accuracy of pedicle screws in children younger than eight years of age. Spine (Phila Pa 1976) 2009;34(26):2907–2911. doi: 10.1097/BRS.0b013e3181b77af3. https://doi.org/10.1097/BRS.0b013e3181b77af3. [DOI] [PubMed] [Google Scholar]
- 44.Mac-Thiong J-M, Labelle H, Rooze M, Feipel V, Aubin C-E. Evaluation of a transpedicular drill guide for pedicle screw placement in the thoracic spine. Eur Spine J. 2003;12(5):542–547. doi: 10.1007/s00586-003-0549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cho SK, Skovrlj B, Lu Y, Caridi JM, Lenke LG. The effect of increasing pedicle screw size on thoracic spinal canal dimensions: an anatomic study. Spine (Phila Pa 1976) 2014;39(20):E1195–E1200. doi: 10.1097/BRS.0000000000000514. https://doi.org/10.1097/BRS.0000000000000514. [DOI] [PubMed] [Google Scholar]
- 46.Xie J, Wang Y, Zhao Z, Zhang Y. The safe placement of upper and middle thoracic pedicle screws in pediatric deformity. J Spinal Disord Tech. 2011;24(1):55–59. doi: 10.1097/BSD.0b013e3181d4c877. https://doi.org/10.1097/BSD.0b013e3181d4c877. [DOI] [PubMed] [Google Scholar]
- 47.Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K. In vivo analysis of insertional torque during pedicle screwing using cortical bone trajectory technique. Spine (Phila Pa 1976) 2014;39(4):E240–E245. doi: 10.1097/BRS.0000000000000116. https://doi.org/10.1097/BRS.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 48.Zhuang Z, Xie Z, Ding S, et al. Evaluation of thoracic pedicle morphometry in a Chinese population using 3D reformatted CT. Clin Anat. 2012;25(4):461–467. doi: 10.1002/ca.21265. https://doi.org/10.1002/ca.21265. [DOI] [PubMed] [Google Scholar]
- 49.Amirouche F, Solitro GF, Magnan BP. Stability and spine pedicle screws fixation strength—a comparative study of bone density and insertion angle. Spine Deform. 2016;4(4):261–267. doi: 10.1016/j.jspd.2015.12.008. https://doi.org/10.1016/j.jspd.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 50.Chou W-K, Chien A, Wang J-L. Pullout strength of thoracic pedicle screws improved with cortical bone ratio: a cadaveric study. J Orthop Sci. 2014;19(6):900–906. doi: 10.1007/s00776-014-0614-3. https://doi.org/10.1007/s00776-014-0614-3. [DOI] [PubMed] [Google Scholar]
- 51.Kim J-H, Choi G-M, Chang I-B, Ahn S-K, Song J-H, Choi H-C. Pedicular and extrapedicular morphometric analysis in the Korean population: computed tomographic assessment relevance to pedicle and extrapedicle screw fixation in the thoracic spine. J Korean Neurosurg Soc. 2009;46(3):181–188. doi: 10.3340/jkns.2009.46.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abuzayed B, Tutunculer B, Kucukyuruk B, Tuzgen S. Anatomic basis of anterior and posterior instrumentation of the spine: morphometric study. Surg Radiol Anat. 2010;32(1):75–85. doi: 10.1007/s00276-009-0545-4. https://doi.org/10.1007/s00276-009-0545-4. [DOI] [PubMed] [Google Scholar]
- 53.Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine (Phila Pa 1976) 1987;12(2):160–166. doi: 10.1097/00007632-198703000-00012. https://doi.org/10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 54.Lien S-B, Liou N-H, Wu S-S. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 2007;16(8):1215–1222. doi: 10.1007/s00586-006-0245-2. https://doi.org/10.1007/s00586-006-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brasiliense LBC, Theodore N, Lazaro BCR, et al. Quantitative analysis of misplaced pedicle screws in the thoracic spine: how much pullout strength is lost? Presented at the 2009 Joint Spine Section Meeting. J Neurosurg Spine. 2010;12(5):503–508. doi: 10.3171/2009.11.SPINE09408. https://doi.org/10.3171/2009.11.SPINE09408. [DOI] [PubMed] [Google Scholar]
- 56.Carmouche JJ, Molinari RW, Gerlinger T, Devine J, Patience T. Effects of pilot hole preparation technique on pedicle screw fixation in different regions of the osteoporotic thoracic and lumbar spine. J Neurosurg Spine. 2005;3(5):364–370. doi: 10.3171/spi.2005.3.5.0364. [DOI] [PubMed] [Google Scholar]