Abstract
Introduction
The use of zirconia based all-ceramic restorations are preferred nowadays owing to superior biologic and esthetic properties. However, these restorations have also reported higher incidences of fracture and chipping. The clinical success may be enhanced by optimizing the core design, through the introduction of monolithic zirconia, or the layered crowns can be strengthened by adding the cervical collar to them.
Objective
This study was performed with the objective to compare and evaluate the fracture load of monolithic and bilayered zirconia crowns with and without a cervical collar.
Methods
A prospective observational study was carried out to compare 45 fabricated zirconia crowns of three different designs on a customized metal mould. The samples were oriented on the metal mould and subjected to confocal microscope for the evaluation of marginal integrity followed by cementing the crown on the metal mould and subjecting it to the universal testing machine for the analysis for the flexural strength. Data were analyzed using one way Anova and t- test for inter and intra groups. The significance level was set at P ≤ 0.05.
Results
The monolith zirconia crowns and layered zirconia crowns with cervical collar reported more flexural strength.
Conclusion
The amount of force required to fracture the zirconia crowns was higher in the case of monolith zirconia crown and layered zirconia crown with cervical collar as compared to the layered zirconia crown without cervical collar.
Keywords: bilayered, flexural strength, monolithic, zirconia
Introduction
CAD/CAM based zirconia restorations are probably one of the greatest recent advances in dentistry [1]. All ceramic restorations are nowadays preferred over conventional metal ceramic restorations because of their biocompatibility and their ability to meet esthetic requirements [2,3]. However, various technical complications of all ceramic crowns such as ceramic chipping, fracture of the ceramic core and/or veneer layer, framework fracture etc. have been widely reported and this has limited its applications in various clinical situations [4]. Thus it becomes imperative to incorporate design characteristics in Zirconia restorations which would reduce the failure.
The chipping of veneering porcelain has been reported to be one of the most common problems and has been documented to be seen more often with zirconia based systems than all other ceramic crowns [5]. Most common posterior zirconia restoration failures were reported either as minor or major chipping, with the chipping rate reported to be as high as 25% [6].
This unusually high incidence of chipping in zirconia based fixed prostheses suggest that there may be an escalation of the usual factors which are involved in the veneer fracture phenomenon in the bilayer systems [7]. Various authors have suggested the fabrication of mono-block restorations from pure zirconia in order to increase the mechanical stability of the finished prostheses. This in turn would lead to an increase in the range of clinical indications of zirconia based prostheses. The introduction of monolithic, anatomic contour zirconia crowns have been reported to provide viable alternatives to conventional veneered prostheses [8]. These restorations have the added advantage of increased fracture resistance and a consequent reduction in the probability of development of adhesive fractures. Colored zirconia mono blocks can thus provide esthetic alternatives to conventional layered restorations.
The fabrication guidelines of zirconia restorations have traditionally mimicked the conventional metal-ceramic systems. At present, most CAD/CAM systems manufacture zirconia frameworks with a traditional metal-ceramic design and a circumferential ledge finish line [9,10]. However, the analyses of mechanical properties reveal that zirconia is harder, stiffer and more stable at higher temperatures than the conventional casting alloys. Recent studies have proposed that the fracture resistance of zirconia restorations can be improved with alternative core designs such as the incorporation of a cervical core collar [11,13]. It has been variously reported that the stresses generated during mastication may be higher at the cervical margins than on the occlusal surfaces and thin margins may be a contributing factor in the fracture of zirconia crowns [12,14–16].
Hence this study was planned to evaluate the effects of two different crown margin designs in monolithic and bilayered zirconia crowns on load at fracture. The working hypothesis was that an increased thickness at the cervical margin would result in an increase in the load at fracture of zirconia crowns [5].
Methods
The present study was undertaken to evaluate the effects of two different crown margin designs for bilayered restorations and monolithic anatomic contoured zirconia crowns on load at fracture. For evaluating the following, three coping preparation designs in a one-way layout were tested in the experiments.
Sample size determination
The sample size was determined using power analysis with an assumed effect size of 0.50. This effect size was estimated as the ratio of the largest difference between experimentally observed means to the (SD) in a previous study. The total number of specimens estimated for 90% power at α = 0.05 was 30 [8]. We used a higher total sample size of 45, corresponding to approximately 96% power.
Ethical clearance
Permissions and Ethical clearance to conduct the study were obtained from Ethical and Scientific committee of institute review board.
Study sample
From a solid metal rod, one single 12 mm long cylindrical metal die with a 60 taper, shallow chamfer finish line, with an orientation groove extending 0.5 mm above the finish line and rounded internal angles was fabricated (Figure 1). From this single customized metal die 45 zirconia crowns (Koho), with a cement space of 30 microns, were produced by computerized and milling unit ((LAVA Scan ST; 3M ESPE). The crowns that were fabricated are as follows:
Figure 1.
Custom made metal mold.
Group 1: 15 bilayered zirconia crowns with standard coping for core veneer crowns with additional 1 mm cervical zirconia collar.
Group 2: 15 monolithic anatomic contour crowns.
Group 3: 15 bilayered zirconia crowns with standard coping for core veneer crowns.
The copings of the bilayered crowns were veneered using veneering ceramic (e.max, Ceram; Ivoclar Vivadent AG) (Figure 2). The marginal integrity of the fabricated crowns was evaluated both prior to and after cementation by confocal microscopy (Figure 3). The crowns were luted to the metal mould using Zinc phosphate cement (Pyrex, India). Excess cement was removed and crowns were stored in distilled water at room temperature for 24±2 hours. The crowns were subsequently loaded centrally at the occlusal surface with a steel ball 25 mm in diameter and were cushioned with a 3 mm ethylene propylene diene rubber disc to prevent any contact damage. The load was applied with a Universal Testing Machine with a crosshead speed of 1.08 mm/min till the fracture occurred. The assembly was placed in the water at room temperature during the flexure testing and the load at fracture was recorded (Figure 4).
Figure 2.
Zirconia crowns. Group 1: bilayered zirconia crowns with standard coping for core veneer crowns with additional 1 mm cervical zirconia collar. Group 2: monolithic anatomic contour crown. Group 3: bilayered zirconia crowns with standard coping for core veneer crowns.
Figure 3.
Confocal Microscopic analysis of Zirconia crowns to evaluate for the marginal integrity. (a) shows the evaluation of cement space under the confocal microscopy prior to cementation of the crown to the metal mold (b) shows evaluation of cement space under the confocal microscopy after the cementation of the crown to the metal mold. It was seen that there was minimum or no discrepancies in cement space both before and after cementation hence marginal integrity of the crown was maintained both before and after cementation.
Figure 4.
Samples placed in water assembly for Testing of flexure strength.
Statistical analysis
The data collected were entered into a Microsoft Excel data sheet and analyzed using Statistical Package for Social Sciences (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Data were analyzed using non-parametric statistics to calculate the differences among the group and between the groups. The significance level was set at P ≤ 0.05.
Results
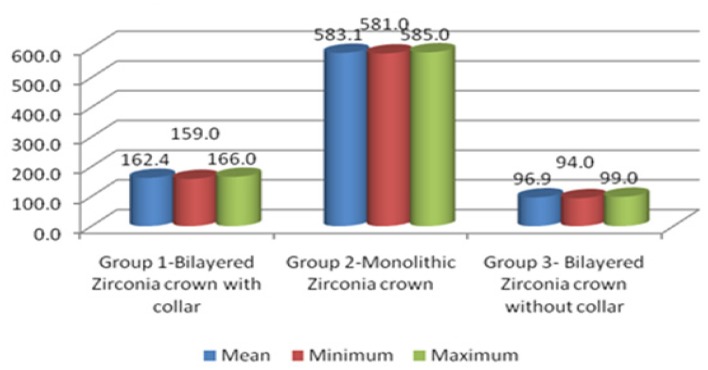
The mean fracture loads value of the zirconia crowns were analyzed using one way ANOVA test which shows the significant difference among the mean fracture loads value of group 2 (monolithic zirconia crown) 583.1±1.2 is higher than that of group 1 (bilayered zirconia crown with collar) 162.4±2.0 and group 2 (bilayered zirconia crown without collar) 96.9±1.3. p – value ≤ 0.05 (Table I).
Table I.
Comparison among groups using one way ANOVA.
| Group | Mean | Minimum | Maximum | ±SD | ‘F’ value | ‘p’ value |
|---|---|---|---|---|---|---|
| Group 1-Bilayered Zirconia crown with collar | 162.4 | 159.0 | 166.0 | 2.0 | 432112 | 0.000 |
| Group 2-Monolithic Zirconia crown | 583.1 | 581.0 | 585.0 | 1.2 | ||
| Group 3- Bilayered Zirconia crown without collar | 96.9 | 94.0 | 99.0 | 1.3 |
P ≤ 0.05 signifies significant; p = 0.000 signifies highly significant
For the intra group comparison ‘t’ test was used (Table II). When the comparison was made between Group 1 and Group 2 the ‘t’ value was found to be 696.0 and p=0.000 i.e. the results were highly significant.
Table II.
Inter group comparison using ‘t’ test.
| Group | Mean | Mean | ‘t’ value | ‘p’ value | Sig/Non-sig |
|---|---|---|---|---|---|
| Group 1 & Group 2 | 162.8 | 583.2 | 606.0 | 0.000 | Highly significant |
| Group 1 & Group 3 | 162.8 | 96.8 | 87.5 | 0.000 | Highly significant |
| Group 2 & Group 3 | 583.2 | 96.8 | 777.7 | 0.000 | Highly significant |
P ≤ 0.05 signifies significant; p = 0.000 signifies highly significant
The mean values of amount of force required to fracture the zirconia crowns are shown in the graph. It shows that the maximum amount of force was required to fracture the monolithic zirconia crowns (583.1±1.2) followed by the bilayered zirconia crown with the cervical collar (162.4±2.0) followed by bilayered zirconia crown without cervical collar (96.9±1.3). p – value ≤ 0.05 (Figure 5).
Figure 5.
Mean values of the force ( Newtons).
Discussion
The advent of zirconia-based restorations for prosthodontics rehabilitation has brought about a significant change in the design and application limits of all-ceramic restorations. At present, long-span zirconia prostheses are being fabricated with a high degree of accuracy and with predictable success rates [6]. In the most commonly established procedure, an opaque zirconia framework is veneered with a layer of glass-ceramic thus providing superior strength properties with acceptable esthetics [15].
However, all ceramic restorations have reported certain technical complications i.e. ceramic chipping, fracture of veneering ceramic, framework fracture, loss of retention and marginal discoloration. The chipping of veneering porcelain has been reported to be a common problem and literature suggests that they are more frequent with zirconia-based crowns than other all ceramic crowns [4].
Various clinical studies have shown that the high incidence of fracture of veneering porcelain in zirconia based restorations are related to both material-specific and non-material-specific factors, i.e. the thickness ratio or the coping design [17]. A 1:1 ratio of coping is to porcelain thickness - when the coping and porcelain thickness are taken in the ratio of 1:1, it has been reported to provide the required strength, optimal esthetics and at the same time decrease the internal stresses [18]. A porcelain thickness of 1.5 mm has also been recommended to reduce the fracture incidence of the veneering porcelain [18].
Design factors aimed at decreasing tensile loading has also been suggested. A high palatal shoulder with a horizontal butt-joint design in molar copings have been recommended by Marchack et al., for decreasing cohesive porcelain fractures [19,20]. Several investigators have suggested the use of a cervical collar in bilayered zirconia restorations in order to prevent veneering porcelain fracture. Many have reported that incorporation of such a feature would improve the clinical longevity of these restorations.
The fabrication of mono-block restorations from pure zirconia has also been introduced to increase the mechanical stability and reduce the incidences of failure. The introduction of colored zirconia monolithic materials has expanded the range of clinical applications of these materials. Researchers have suggested that by optimizing the core design, the success rates of these restorations may be enhanced and the use of a colored monolithic zirconia material would help achieve esthetically acceptable outcomes [8]. It has also been said that a single layer design would need a more conservative tooth preparation, thus improving the pulp response.
In the present study, the effects of two different crown margin designs for bilayered restorations were evaluated and compared to monolithic crowns on load at fracture. It is known that restorations are especially vulnerable at the margins and during clinical use these marginal flaws may result in the initiation of core fractures. The fracture modes were further analyzed by fractographic analysis to identify the fracture features so that clinically relevant inferences can be drawn. It was hypothesized that an increased axial wall thickness at the marginal areas would cause a resultant increase in load at fracture of zirconia crowns.
The results of the present study show that monolithic zirconia crowns fracture at a significantly higher load and they present more complicated fracture modes than bilayered crowns. Thus the hypothesis that crown wall thickness affects the fracture strength of zirconia crowns is validated. On the basis of the above findings, it may be inferred that monolithic crowns are more suited for use in high-stress situations and also that material thickness is more significant than crown margin design for improvement of strength properties. Significant differences in the fracture load between bilayered crowns with and without cervical collar were also reported. This suggests that modifications in margin geometry result in a reduction in the risk of both core as well as adhesive fractures. Previous researchers have hypothesized that the cervical collar may function as a circumferential ferrule. This helps in reducing the stresses at the cervical margin thus increasing the load at fracture [8].
A further advantage of a cervical collared design in bilayered crowns is that it provides for a simplified application of veneering material. Several authors have reported that the incidence of veneering material on the inside of the core is relatively common and this in turn may cause a discrepancy in the crown seating, thus affecting the marginal fit and compromising the stress distribution pattern which may be a cause of clinical failures. The presence of a cervical collar will help to reduce this possibility. This may also help in ensuring a smooth transition between the tooth, core and veneer material, thus facilitating biofilm removal [8]. An inadequate cement space has also been shown to affect the marginal fit of crowns. This variable was eliminated in the present study by providing for a uniform cement space of 30 microns for all the specimens and by further evaluation of fit of all the prepared crowns before and after cementation by confocal microscopy.
The findings of the present study thus indicate that anatomic contoured zirconia crowns as well as bilayered crowns with a cervical collar design have improved strength properties as indicated by increased load at fracture. Thus the incidences of chipping, a common drawback of zirconia restorations may be reduced. Also the use of an anatomic contour or a collared bilayered design will result in less invasive tooth preparations. Presently, zirconia core materials are available in varying shades of translucency and multiple shades. Thus, the esthetic requirements in various clinical situations, especially in high stress posterior regions may be more easily achievable.
Through the result of the present study it was concluded that monolithic crown had higher fracture resistance as compared to monolithic bilayered zirconia crown with and without cervical collar. Also, for the intra group comparisons t test was used (Table II). When the comparison was made between Group 1 and Group 2, the t value was found to be 696.0 and p=0.000 i.e; the results were highly significant.
Conclusion
Within the limitation of the current study it can be concluded that the amount of force required for the fracture of the zirconia crown was higher in case of monolithic zirconia crowns followed by bilayered zirconia crowns with cervical collar and least amount of force was required to fracture bilayered zirconia crown without cervical collar. Thus, in areas where high amounts of force are anticipated, the use of monolithic zirconia crown should be advocated rather than bilayered zirconia crown. Further studies should focus on optimizing the core design further so that there is further improvement in the flexural strength of the prostheses.
References
- 1.Christopher SM, Robert LR, Richard JI. The effect of coping/veneer thickness on the fracture toughness and residual stress of implant supported, cement retained zirconia and metal–ceramic crowns. Dental Materials. 2012;28:250–58. doi: 10.1016/j.dental.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Raigrodski AJ, Chiche GJ, Potiket N, Hochstedler JL, Mohamed SE, Billiot S, et al. The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: a prospective clinical pilot study. J Prosthet Dent. 2006;96:237–244. doi: 10.1016/j.prosdent.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 3.Sailer I, Gottnerb J, Kanelb S, Hammerle CH. Randomized controlled clinical trial of zirconia–ceramic and metal–ceramic posterior fixed dental prostheses: a 3-year follow-up. Int J Prosthodont. 2009;22:553–560. [PubMed] [Google Scholar]
- 4.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All- ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs) Dent Mater. 2015;31:603–623. doi: 10.1016/j.dental.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Ha Seung-Ryong, Kim Sung-Hun, Lee Jai-Bong, Han Jung-Suk, Yeo In-Sung. Effects of coping designs on fracture modes in zirconia crowns: Progressive load test. Ceramics International. 2016;42:7380–7389. [Google Scholar]
- 6.Triwatana P, Nagaviroj N, Tulapornchai C. Clinical performance and failures of zirconia-based fixed partial dentures: a review literature. J Adv Prosthodont. 2012;4:76–83. doi: 10.4047/jap.2012.4.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belli R, Frankenberger R, Appelt A, Schmitt J, Baratieri LN, Greil P, et al. Thermal-induced residual stresses affect the lifetime of zirconia–veneer crowns. Dent Mater. 2013;29:181–190. doi: 10.1016/j.dental.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Øilo M, Kvam K, Gjerdet NR. Load at fracture of monolithic and bilayered zirconia crowns with and without a cervical zirconia collar. J Prosthet Dent. 2013;115:630–636. doi: 10.1016/j.prosdent.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Aboushelib MN. Fatigue and fracture resistance of zirconia crowns prepared with different finish line designs. J Prosthodont. 2012;21:22–27. doi: 10.1111/j.1532-849X.2011.00787.x. [DOI] [PubMed] [Google Scholar]
- 10.Takeichi T, Katsoulis J, Blatz MB. Clinical outcome of single porcelain-fused-to-zirconium dioxide crowns: a systematic review. J Prosthet Dent. 2013;110:455–461. doi: 10.1016/j.prosdent.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 11.Marchack BW, Sato S, Marchack CB, White SN. Complete and partial contour zirconia designs for crowns and fixed dental prostheses: a clinical report. J Prosthet Dent. 2011;106:145–152. doi: 10.1016/S0022-3913(11)60112-1. [DOI] [PubMed] [Google Scholar]
- 12.Øilo M, Quinn GD. Fracture origins in twenty-two dental alumina crowns. J Mech Behav Biomed Mater. 2015;53:93–103. doi: 10.1016/j.jmbbm.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Ferrari M, Giovannetti A, Carrabba M, Bonadeo G, Rengo C, Monticelli F, et al. Fracture resistance of three porcelain-layered CAD/CAM zirconia frame designs. Dent Mater. 2014;30:e163–e168. doi: 10.1016/j.dental.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Z, Guazzato M, Sornsuwan T, Scherrer SS, Rungsiyakull C, Li W, et al. Thermally induced fracture for core-veneered dental ceramic structures. Acta Biomater. 2013;9:8394–8402. doi: 10.1016/j.actbio.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Øilo M, Kvam K, Reisegg K, Gjerdet NR. The effects of margin curvature on load at fracture of ceramic crowns. Int J Prosthodont. 2015;28:357–359. doi: 10.11607/ijp.4191. [DOI] [PubMed] [Google Scholar]
- 16.Øilo M, Kvam K, Tibballs JE, Gjerdet NR. Clinically relevant fracture testing of all-ceramic crowns. Dent Mater. 2013;29:815–823. doi: 10.1016/j.dental.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 17.Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008;24:299–307. doi: 10.1016/j.dental.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Lawn BR, Pajares A, Zhang Y, Deng Y, Polack MA, Lloyd IK, et al. Materials design in the performance of all-ceramic crowns. Biomaterials. 2004;25:2885–2892. doi: 10.1016/j.biomaterials.2003.09.050. [DOI] [PubMed] [Google Scholar]
- 19.Luthardt RG, Holzhüter MS, Rudolph H, Herold V, Walter MH. CAD/CAM-machining effects on Y-TZP zirconia. Dent Mater. 2004;20:655–662. doi: 10.1016/j.dental.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Aboushelib MN, Dozic A, Liem JK. Influence of framework color and layering technique on the final color of zirconia veneered restorations. Quintessence Int. 2010;41:e84–e89. [PubMed] [Google Scholar]