Abstract
We describe the case of an 8-year old female patient with an open pelvic fracture after being run over by a bus. Open pelvic injuries in pediatric patients are very rare and are associated with high mortality rates and long-term morbidity. In this case, a multidisciplinary surgical approach is described. The injuries include a complex pelvic ring fracture, which was treated with an internal external fixator, together with severe urogenital and soft-tissue injury. The internal external fixator, a surgical technique involving a temporary internal fixation device, is well described in adults, but has not been described in pediatric patients before. This case presentation shows the severity and complexity of the treatment of open pelvic fractures with severe associated injures. Albeit the treatment of her orthopaedic injuries has been successful so far, our patient unfortunately still suffers notable morbidity from her other injuries.
INFIX (internal external fixator) use has been described in adults with open pelvic fractures, but its use has not been described for pediatric patients.1,2,3,4,5
Pediatric pelvic fractures as a presenting diagnosis are very rare even in major trauma centers, occurring at an estimated incidence of 1 per 100,000 children per year.6,7 Nevertheless, given the high number of pediatric patients suffering from trauma-related injuries, the incidence of pelvic fractures is relatively high at 2.4% (as estimated in Ismail et al) and 7.5% (in Peltier's study), respectively.8,9
In the adult population, open pelvic fractures have been reported in up to 2% to 5%10,11 of all pelvic ring injuries with an overall mortality rate of up to 50%,12,13,14 although in the pediatric population it was historically mentioned to be as high as 25%.15 More recently, mortality rates have fallen to approximately 3.6%, as reported in the study by Silber et al,16 because of the use of more modern surgical techniques and standards of care. One of the techniques that have contributed to this fall in mortality rates has been the use of INFIX, which is the object of the case study discussed later.
The pelvic INFIX and external fixation (EXFIX) are surgical temporary stabilizing techniques for the treatment of unstable closed or open pelvic ring injuries. The use of an INFIX technique over that of an EXFIX is mainly related to its subcutaneous position, which is an advantage in cases of severe soft-tissue envelope injuries overlying the pin insertion sites, such as was the case in our study. This allows for plastic surgery procedures to be performed with no external metalwork interference and also permits an easier rehabilitation period for the patient, facilitating nursing immediately postoperatively and also aiding mobilization.
In 2012, Vaidya et al described the use of supra-acetabular spinal pedicle screws and a subcutaneous connecting rod (constitutive for the technique of INFIX) for the treatment of unstable pelvic ring injuries. It was described as biomechanically stronger than an external fixator because of its internal profile, and it also provided the advantage of improved patient comfort/mobility. In addition, the rate of pin-site infection dropped dramatically after using this implant type.14,17 In 2016, Vaidya et al4 described the use of the INFIX technique in three cases of open pelvic fractures in adults.
Case Presentation
An 8-year-old girl was presented at the Accident and Emergency department of the Royal London Hospital, a Major Trauma Centre, after being hit and run over by a bus. She was brought in by the members of the London Air Ambulance (Helicopter Emergency Medical Service [HEMS]) with the suspicion of an open pelvic fracture. On primary survey, her airway was patent, she had a Glasgow Coma Score of 14 and she was ventilating well. She was hemodynamically unstable and had a pelvic binder on, and the pelvic radiograph showed a pelvic ring fracture (Figure 1).
Figure 1.

Radiograph showing initial AP pelvis.
After the patient was intubated, she was taken for CT, which showed bilateral superior and inferior pubic rami fracture, a right iliac bone fracture, and bilateral sacrum fractures (Figures 2 and 3). Furthermore, the scan evidenced the presence of a large pelvic hematoma with active hemorrhage and free extra-peritoneal gas in the pelvis. She had a skull fracture (calvarial fracture extending into the right petrous temporal bone as described with an associated hemotympanum but no disruption of the ossicular chain or otic capsule) with an associated hemotympanum and a nondisplaced left-sided clavicle fracture.
Figure 2.
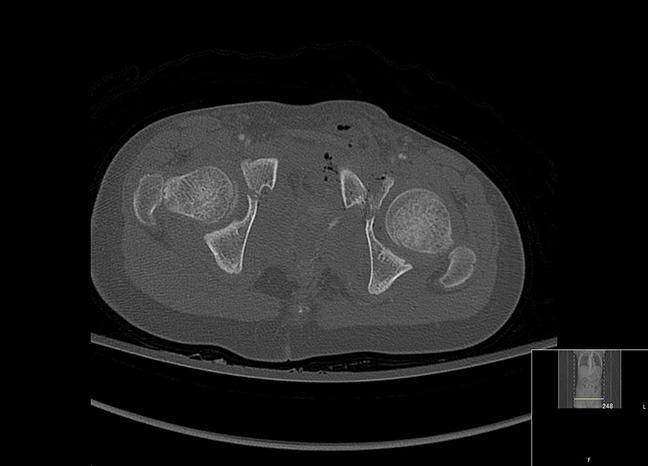
CT showing axial view of lateral compression-type injury.
Figure 3.
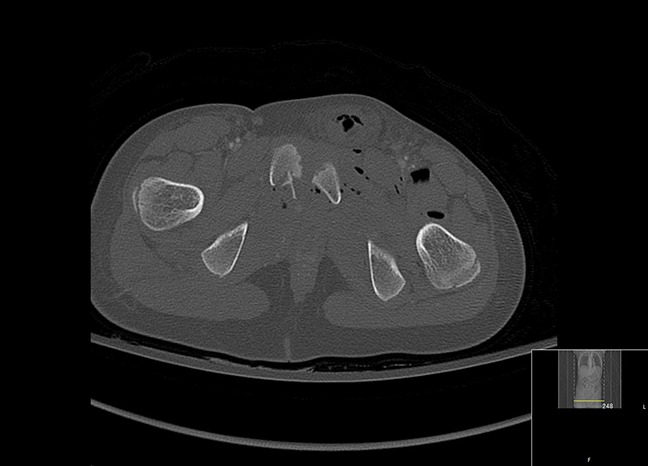
CT showing further axial view.
She remained hemodynamically unstable with an elevated heart rate despite resuscitation with blood products. The venous blood gas showed a lactate of 3.7 and a base excess of −2.
She was then transferred to interventional radiology where she underwent embolization of the side branches of both internal iliac arteries.
After embolization, she was brought to theatre. She had continuing bleeding from the vaginal lacerations and a trial and cystoscopy-assisted urethral catheterization failed. Rectal examination was performed and showed an intact anus. She was found to have extensive perineal, mainly urogenital, left thigh, groin, and right buttock degloving injuries, and the pubic fragments were exposed in the lacerations. It was then decided to do a laparotomy, perform a colostomy, and place a suprapubic catheter. Meanwhile, her pelvis remained stable with a pelvic binder. After the procedure, the abdomen was closed and the patient was transferred to the pediatric intensive care unit.
Her condition stabilized overnight and the following day she was brought back to theatre for a pelvic manipulation under anesthetic and fixation. The patient's pelvic fracture could best be described as a bilateral unstable lateral compression type 1 fracture as per Young and Burgess classification18 and type IV Torode and Zieg.19
Method
It was decided to reduce the pelvic ring and to stabilize the anterior pelvic ring by using an INFIX surgical technique (Anterior Subcutaneous Internal Pelvic Fixator) after the insertion of one transiliac transsacral cannulated partially threaded screw (7.3/16 mm). Fluoroscopy was used to place the supra-acetabular pedicle screws (NuVasive spinal system; NuVasive U.K). The starting point Anterior Inferior Iliac Spine was determined by the use of an obturator-outlet view (teardrop view) and an iliac oblique view. A small transverse incision was made (2 to 3 cm), two finger-breadths below anterior superior iliac spine (ASIS). Dissection was performed on the Anterior Inferior Iliac Spine, taking the Lateral Femoral Cutaneous Nerve (LFCN) into account. The entry point was determined by considering both the abovementioned views, and a Jamshidi needle was used aiming just slightly lateral toward the sciatic notch to access the column of bone through which fixation was desired. This column of bone extended from the anterior iliac spine to the posterior inferior iliac spine as seen on an oblique iliac view. After the needle was positioned, a guidewire was used to access the bone a bit further taking into account the inner and outer tables of the ilium and the top of the greater sciatic notch posteriorly. After this, a tap was used and the pedicle screws were placed under imaging guidance. After both screws were inserted, a tunneling device was used to create a subcutaneous route for the bar to be placed in both pedicle screws. These screws can then be used as reduction devices before the bar is locked with a set screw in the pedicle screws. In general, this is a fast operation of approximately 45 minutes, but it does depend on the quality of the acquired imaging20,21 (Figure 4).
Figure 4.
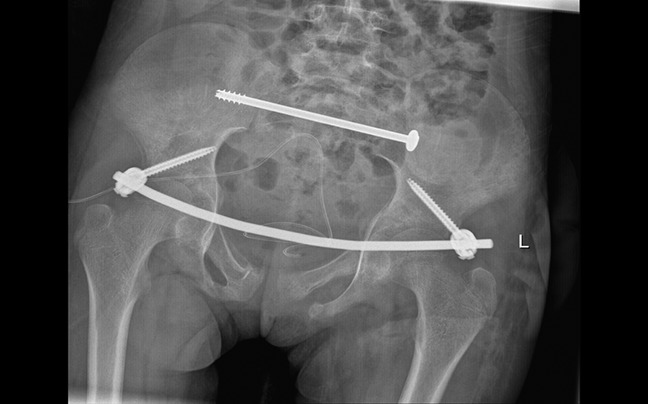
Radiograph showing postoperative AP pelvis.
Postoperatively, she was allowed to transfer from bed to chair. With help from physiotherapists and with the aid of a walking frame, she also started mobilizing 3 days after the procedure, full weight-bearing on the left side and non–weight-bearing on the right. Her neurovascular status remained intact.
The following days and weeks, the patient underwent several wound débridements, wound closure by INTEGRA (Integra Life Sciences), and a split skin graft by the plastic surgeons.
After a hospital stay of 5 weeks, the patient was discharged in a good condition, though with a suprapubic catheter still in place.
The orthopaedic team removed the metalwork after 8 weeks.
Currently, after more than 6 months, our 8-year-old patient is still under wound care and awaiting urethral and possibly vaginal reconstruction (Figure 5 AP pelvis radiograph, 6 months after removal of metalwork).
Figure 5.

Radiograph showing the latest AP pelvis.
Discussion
In a large published pediatric series of pelvic fractures (166 overall), only five patients could be identified who required surgery for their pelvic injuries, involving open reduction and internal fixation, because these injuries are extremely rare in the pediatric population.16 Most patients had left-sided pelvic injuries as a result of being hit by motor vehicles while crossing the road on the near lane, whereas our patient had a bilateral injury with an unstable pattern (Torode/Zieg IV).
Injuries such as open pelvic fractures require a considerably bigger impact to produce such large-scale damage when compared with adults. The key anatomic differences between adults and children lie in how they react to blunt trauma, mainly due to the biomechanical properties of their bodies. A larger amount of energy (bigger impact) translates into more pelvic and abdomen visceral damage. Our patient had a bilateral rami injury; hence this can be termed as a straddle fracture. This type of fracture results from an anterior directed force and is often associated with urogenital injuries. The incidence of these types of fracture has been mentioned to be as high as 10% in some series,22,23 with urethral/bladder injuries of 5% in the Canale and Beaty24 study.
Given the relatively rare occurrence of such type of pelvic injuries in the pediatric population, Torode and Zeig's popular classification of pediatric pelvic fractures, still in use, is, in most cases, adequate. However, this was originally set up to describe the injuries of the whole child rather than the particularities of an isolated fracture; thus, it does not take into account the ever-changing maturity of the bony pelvis and does not fully explain the differences in the kinds of fractures that can occur, nor does it analyze the differences among the surgical technique used to treat them. The following discussion provides a brief overview of the way pelvic fractures in the pediatric population have been approached, and makes the case for the procedure we have used in the case study presented as being comparatively more advantageous and beneficial.
Unstable pelvic ring injuries have historically been managed with open reduction and internal fixation using plates and screws, or external fixation.25 However, open reduction has many associated risks, including extensive soft-tissue stripping and the potential risk of neurovascular injury.26
External fixation is a less invasive procedure, but may be poorly tolerated if used for a long period of time and is also associated with a high risk of pin-site infection.27 By contrast, the INFIX procedure has been considered more successful in treating injuries of the pelvic ring.28,29 The procedure involves placing pedicle polyaxial screws in the supra-acetabular corridor, which are then connected by a subcutaneous bar across the abdomen. This construct has multiple surgical and medical advantages: as can be deduced from the description of the method applied in the case study discussed earlier, it can be used to treat anterior pelvic ring injuries, has a lower surgical time, is less invasive, and can function as an indirect reduction tool before the final tightening.20 It also improves patient’s overall satisfaction, with better reported outcomes in terms of being able to roll in bed and a lower rate of infections.17,19 The rate of bone union has been successfully reported to be as high as 98% in the study by Dahill et al,20 and similarly in others that examined this technique.17,30
In our case, the patient did not show signs of LFCN injury, although in many cases this was reported to be as high as 30%17 and 19%30 in previous studies. Other complications associated with surgery, such as infection, revision surgery, loss/malreduction, loosening, rod or screw breakage, excessive tightness of the rod, and heterotopic ossification, have been reported to be close to 5%.17,30 These risks could potentially be higher, especially the irritation to LFCN due to its proximity to the screw, given the size of the pediatric patient. However, all these potential risks were successfully avoided in the case of the INFIX procedure we used. LFCN injury in particular, which was the main risk concern given the incidence of occurrence reported in previous studies, was avoided using an appropriate size incision, as described, which allowed for better soft-tissue protection and prevented soft-tissue entrapment when advancing the screw in the supra-acetabular corridor. In terms of the danger of postoperative loosening, existing statistics in the adult population show a relatively low risk factor (1/36 patients in the study by Muller et al30) and there is no evidence that this would be higher in the pediatric population; nonetheless, the use of an internal rather than external fixation device, which reduces the likelihood of infection—itself an element conducive to loosening—further reduces the risk of its occurrence.
One of the most obvious conclusions of this study is that such very rare injuries are best treated in a multidisciplinary manner in highly specialized major trauma centers.
In terms of the particular orthopaedic procedures used, the closed reduction of the anterior pelvic ring injury with the use of the INFIX technique was, in this case, particularly beneficial due to the nature of the open injury and the notable soft-tissue damage in the genito-urinary tract. When compared with the risks and outcomes described in previous studies that analyzed similar traumatic events, it is evident that the INFIX technique presents multiple surgical and medical advantages, particularly when compared with the other frequently used procedure, the EXFIX.
The EXFIX technique can often be more readily used because of the implant readiness in trauma centers and the lack of availability of specialized kit such as the one described in our study and others,17 but the INFIX technique is superior due to its positioning, allowing for better soft-tissue reconstruction procedures after severe degloving injuries of the anterior pelvis and vastly superior bedside nursing, inferior pin-site complication rate, and overall superior quality of life for the patient in the period the device is applied. A larger series of comparative analyses would be useful for a better assessment of the risks associated with this technique in the children's pelvis, and it would provide a larger field of data for improving the management of the potential risks described earlier. Contributing further to such a series is one of the desired outcomes for all the authors of this case study.
Footnotes
Mr. Bates or an immediate family member is a member of a speakers’ bureau or has made paid presentations on behalf of DePuy, Smith and Nephew, Stryker, and Zimmer Biomet and serves as a paid consultant to Orthofix. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Mr. Rad, Ms.van Embden, and Ms. Bijlsma.
References
- 1.Vaidya R, Martin AJ, Roth M, Tonnos F, Oliphant B, Carlson J: Midterm radiographic and functional outcomes of the anterior subcutaneous internal pelvic fixator (INFIX) for pelvic ring injuries. J Orthop Trauma 2017;31:252-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaidya R, Martin AJ, Roth M, Nasr K, Gheraibeh P, Tonnos F: INFIX versus plating for pelvic fractures with disruption of the symphysis pubis. Int Orthop 2017;41:1671-1678. [DOI] [PubMed] [Google Scholar]
- 3.Hoskins W, Bucknill A, Wong J, et al. : A prospective case series for a minimally invasive internal fixation device for anterior pelvic ring fractures. J Orthop Surg Res 2016;11:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaidya R, Nasr K, Feria-Arias E, Fisher R, Kajy M, Diebel LN: INFIX/EXFIX: Massive open pelvic injuries and review of the literature. Case Rep Orthop 2016;2016:9468285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaidya R, Tonnos F, Nasr K, Kanneganti P, Curtis G: The anterior subcutaneous pelvic fixator (INFIX) in an anterior posterior compression type 3 pelvic fracture. J Orthop Trauma 2016;30(Suppl 2):S21-S22. [DOI] [PubMed] [Google Scholar]
- 6.Amorosa LF, Kloen P, Helfet DL: High-energy pediatric pelvic and acetabular fractures. Orthop Clin North Am 2014;45:483-500. [DOI] [PubMed] [Google Scholar]
- 7.DeFrancesco CJ, Sankar WN: Traumatic pelvic fractures in children and adolescents. Semin Pediatr Surg 2017;26:27-35. [DOI] [PubMed] [Google Scholar]
- 8.Ismail N, Bellemare JF, Mollitt DL, DiScala C, Koeppel B, Tepas JJ: Death from pelvic fracture: Children are different. J Pediatr Surg 1996:31:82-85. [DOI] [PubMed] [Google Scholar]
- 9.Peltier LF: Complications associated with fractures of the pelvis. J Bone Joint Surg Am 1965;47:1060-1069. [PubMed] [Google Scholar]
- 10.Brenneman FD, Katyal D, Boulanger BR, Tile M, Redelmeier DA: Long-term outcomes in open pelvic fractures. J Trauma 1977;42:773-777. [DOI] [PubMed] [Google Scholar]
- 11.Rothenberger D, Velasco R, Strate R, Fischer RP, Perry JF: Open pelvic fracture: A lethal injury. J Trauma 1978;18:184-187. [PubMed] [Google Scholar]
- 12.Davidson BS, Simmons GT, Williamson PR, Buerk CA: Pelvic fractures associated with open perineal wounds: A survivable injury. J Trauma 1993;35:36-39. [DOI] [PubMed] [Google Scholar]
- 13.Dente CJ, Feliciano DV, Rozycki GS, et al. : The outcome of open pelvic fractures in the modern era.; Am J Surg 2005;190:830-835. [DOI] [PubMed] [Google Scholar]
- 14.Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A: Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: Initial clinical series. J Orthop Trauma 2012;26:1-8. [DOI] [PubMed] [Google Scholar]
- 15.Quinby WC: Fractures of the pelvis and associated injuries in children. J Pediatr Surg 1996;1:353-364. [DOI] [PubMed] [Google Scholar]
- 16.Silber JS, Flynn JM, Koffler KM, Dormans JP, Drummond DS: Analysis of the cause, classification, and associated injuries of 166 consecutive pediatric pelvic fractures. J Ped Ortho 2001. 21:446-450. [PubMed] [Google Scholar]
- 17.Vaidya R, Kubiak EN, Bergin PF, et al. : Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: A multicenter study. Clin Orthop Relat Res 2012;470:2124-2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burgess AR, Eastridge BJ, Young JW, et al. : Pelvic ring disruptions: Effective classification system and treatment protocols. J Trauma 1990;30:848-856. [PubMed] [Google Scholar]
- 19.Torode I, Zieg D: Pelvic fractures in children. J Pediatr Orthop 1985;5:76-84. [DOI] [PubMed] [Google Scholar]
- 20.Dahill M, McArthur J, Roberts GL, Acharya MR, Ward AJ, Chesser TJS: The use of anterior pelvic internal fixator to treat disruptions of the anterior pelvic ring, Bone Joint J 2017;99-B:1232-1236. [DOI] [PubMed] [Google Scholar]
- 21.Court-Brown, Charles M, Heckman JD, et al. : Rockwood and Green's Fractures in Adults. Philadelphia, PA: Wolters Kluwer Health, 2015. [Google Scholar]
- 22.Lane-O'Kelly A, Fogarty E, Dowling F: The pelvic fracture in childhood: A report supporting nonoperative management. Injury 1995;26:327-329. [DOI] [PubMed] [Google Scholar]
- 23.Reed MH: Pelvic fractures in children. J Can Assoc Radiol 1976;27:255-261. [PubMed] [Google Scholar]
- 24.Canale ST, Beaty JH: Pelvic and hip fractures, in Rockwood CA, Jr, Wilkins KE, Beaty JH, eds: Fractures in children, ed 4 Philadelphia: Lippincott-Raven, 1996, pp 1109-1193. [Google Scholar]
- 25.Tile M: Pelvic ring fractures, should they be fixed?. J Bone Joint Surg (Br) 1988;70-B:1-12. [DOI] [PubMed] [Google Scholar]
- 26.Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ: Complications of temporary and definitive external fixation of pelvic ring injuries. Injury 2005:36:599-604. [DOI] [PubMed] [Google Scholar]
- 27.Cole PA, Gauger EM, Anavian J, et al. : Anterior pelvic external fixator versus subcutaneous internal fixator in the treatment of anterior pelvicring fractures. J Orthop Trauma 2012;26:269-277. [DOI] [PubMed] [Google Scholar]
- 28.Vigdorchik JM, Esquivel AO, Jin X, et al. : Biomechanical stability of a supracetabular pedicle screw internal fixation device (INFIX) vs external fixation and plates for vertical unstable pelvic fractures. J Orthop Surg 2012;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gardner MJ, Mehta S, Mirza A, Ricci WM: Anterior pelvic reduction and fixation using a percutaneous internal fixator. J Orthop Trauma 2012;26:314-21. [DOI] [PubMed] [Google Scholar]
- 30.Müller FJ, Stosiek W, Zellner M, Neugebauer R, Füchtmeier B: The anterior subcutaneous internal fixator (ASIF) for unstable pelvic ring fractures: Clinical and radiological midterm results. Int Orthop 2013;37:2239-2245. [DOI] [PMC free article] [PubMed] [Google Scholar]


