Abstract
Background:
Hip-spine syndrome was originally described by Offierski and MacNab, who argued that the flexion deformity of the hip rotated the pelvis forward, causing the spine symptoms. We additionally hypothesized that in patients who have osteoarthritis (OA) of the hip, the pelvis is tilted anteriorly to compensate for the anterior acetabular coverage defect. We investigated the hip factors associated with anterior pelvic tilt (PT) in patients who had OA of the hip due to acetabular dysplasia.
Methods:
We retrospectively reviewed the medical records of patients who had undergone total hip arthroplasty between January 2009 and December 2017 to identify those who had unilateral secondary OA due to acetabular dysplasia. Patients who had spinal imbalance, a history of spinal or lower limb fracture or surgery, bilateral OA of the hip, or a severely subluxated hip were excluded, leaving 100 eligible patients. We defined the indicators of an anterior acetabular coverage defect, flexion deformity of the hip, and anterior PT as the acetabular anteversion angle (AAA), extension range of motion (ROM), and anterior tilt of the pelvis, respectively. We measured hip factors and spinal parameters on radiographs and the standardized axial and coronal planes on 3-dimensional computed tomography with reference to the anterior pelvic plane. Hip factors associated with PT were investigated.
Results:
Univariate analysis showed a significant correlation between PT and both AAA (r = –0.389, p < 0.001) and combined anteversion angle (r = –0.272, p = 0.03). Multivariate regression analysis identified AAA (β = –0.385, p < 0.001) and extension ROM (β = 0.212, p = 0.0496) as independent factors associated with PT. Lumbar lordosis and pelvic incidence minus lumbar lordosis were significantly correlated with AAA, but sagittal vertical axis was not.
Conclusions:
When treating patients who have acetabular dysplasia, surgeons should recognize the relationship between the anterior acetabular coverage and anterior PT. Correcting hyperlordosis of the lumbar spine can induce progression of hip OA because it may decrease the acetabular anterior coverage.
Hip-spine syndrome was originally reported by Offierski and MacNab in 19831. They described secondary hip-spine syndrome as the interrelationship of spine symptoms and deformity of the hip. Flexion deformity of the hip rotates the pelvis anteriorly and exaggerates the normal lumbar lordosis. Hyperlordosis of the lumbar spine causes subluxation of the posterior facet joint and foraminal stenosis1.
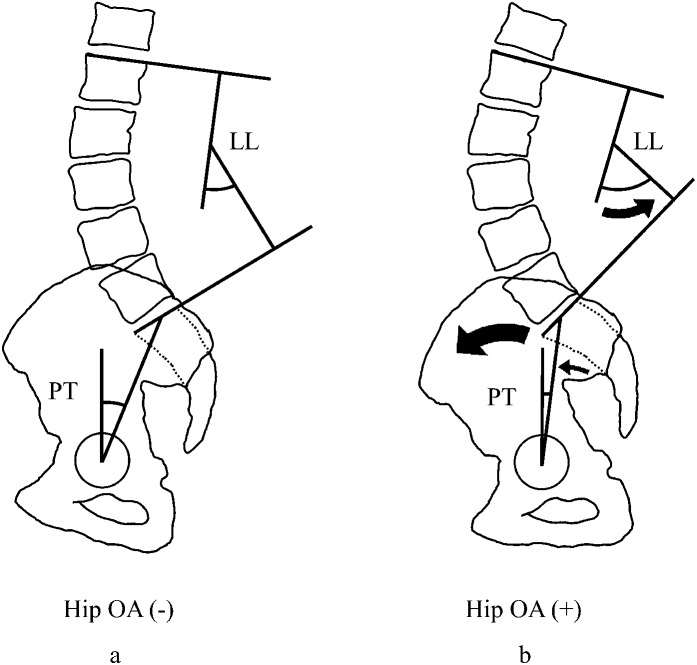
Recently, several studies have reported on the characteristics of sagittal spinopelvic alignment in patients with osteoarthritis (OA) of the hip, who had a lower pelvic tilt (PT) angle and a higher lumbar lordosis angle (Fig. 1)2,3. Furthermore, Piazzolla et al. reported that in patients who have hip OA, those with low back pain have a lower PT and a higher lumbar lordosis than those without back pain4. These results are consistent with the pathology of the hip-spine syndrome reported by Offierski and MacNab1. Therefore, the origin of the sequential pathology of the hip-spine syndrome is the anterior PT. Indeed, Offierski and MacNab argued that the flexion deformity of the hip rotates the pelvis anteriorly1. We hypothesized that in patients who have secondary OA of the hip due to acetabular dysplasia the pelvis tilts anteriorly because of the compensation of the anterior acetabular coverage defect. However, to our knowledge there have been no reports of hip factors associated with the anteriorly tilted pelvis as the first step of secondary hip-spine syndrome. In this study, we investigated hip factors associated with anterior PT in patients who had secondary OA of the hip due to acetabular dysplasia.
Fig. 1.
Figs. 1-A and 1-B The characteristics of PT and lumbar lordosis (LL) in patients with hip OA. Spinopelvic balance is shown in an individual without OA (Fig. 1-A) and in an individual with OA (Fig. 1-B).
Materials and Methods
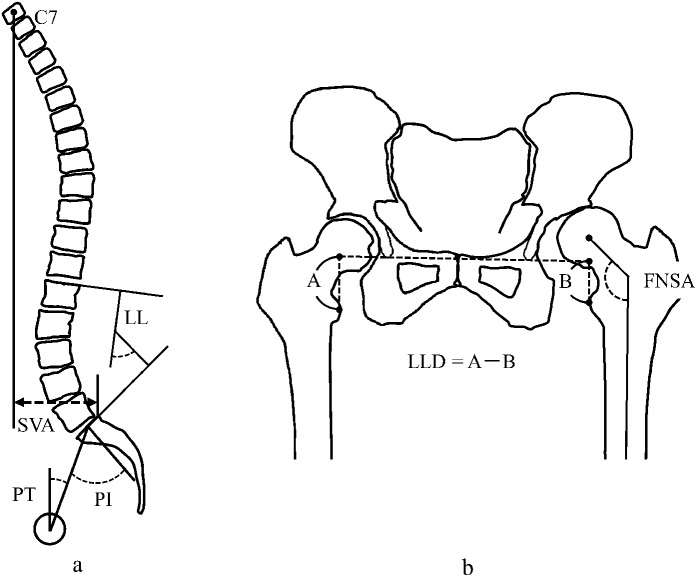
Between January 2009 and December 2017, we performed 732 primary total hip arthroplasties at our institution. For these patients, we routinely made preoperative standard anteroposterior radiographs of the hip, standing whole-spine radiographs, and computed tomography (CT) scans of the hip. Anteroposterior radiography of the hip and CT scanning were conducted with the patients in a supine and relaxed position, without lumbar support. The medical records of these patients were reviewed to identify patients who had undergone total hip arthroplasty as a treatment for unilateral OA due to developmental dysplasia of the hip with a normal contralateral hip, defined by absence of OA and of pain, a center-edge angle of >25°, and a Sharp angle5 of >45°. Patients were excluded if they met any of the following criteria (Table I): (1) a severely subluxated hip (Crowe et al.6 Group II, III, or IV) or bilaterally affected hip joints (because bilateral dislocation obviously may influence the measurement of PT or the pelvic incidence for cranial displacement of the femoral head) (Fig. 2-A), (2) a history of issues likely to have affected spinal alignment (because of its influence on PT), (3) sagittal spinal imbalance (because of its influence on PT), or (4) an age of ≥70 years. We defined sagittal spinal imbalance as PT of >25°, a sagittal vertical axis of >70 mm, or pelvic incidence minus lumbar lordosis of >15°, by reference to the SRS (Scoliosis Research Society)-Schwab 3 sagittal modifiers7. These measured spinal parameters are shown in Figure 2-A. After the exclusion criteria had been applied, 100 patients with unilateral developmental dysplasia of the hip were available for inclusion in the study. The study protocol was approved by our local institutional review board, and the study was carried out in accordance with the guidelines of the World Medical Association Declaration of Helsinki.
Fig. 2.
Figs. 2-A and 2-B Schematic drawing showing the parameters that were measured on radiographs. LL = lumbar lordosis, SVA = sagittal vertical axis, PI = pelvic incidence, LLD = leg-length discrepancy, and FNSA = femoral neck-shaft angle. Fig. 2-A Spinal parameters on a lateral whole-spine radiograph. Fig. 2-B Hip parameters on a standard anteroposterior radiograph.
TABLE I.
Exclusion Criteria*
| Crowe Group II/III/IV |
| Bilateral hip OA |
| History of fracture or surgery of spine, lower limb, or pelvis |
| Age ≥70 years |
| PT >25° |
| SVA >70 mm |
| PI – LL >15° |
| Secondary OA not due to AD (osteonecrosis, trauma, rapidly destructive coxarthrosis, etc.) |
SVA = sagittal vertical axis, PI = pelvic incidence, LL = lumbar lordosis, and AD = acetabular dysplasia.
We defined indicators of anterior coverage defect of the acetabulum, flexion deformity of the hip, and anterior tilt of the pelvis as the acetabular anteversion angle (AAA), extension range of motion (ROM), and PT, respectively. We also recorded the following hip measurements: femoral neck-shaft angle, leg-length discrepancy, femoral neck anteversion angle, combined anteversion angle (AAA plus femoral neck anteversion angle), center-edge angle, Sharp angle, flexion ROM, and abduction ROM. The femoral neck-shaft angle and leg-length discrepancy were measured on anteroposterior radiographs of the hip (Fig. 2-B). The femoral neck-shaft angle was measured as the angle formed by a line drawn through the long axis of the neck of the femur and a line drawn along its shaft. Leg-length discrepancy was determined by subtracting the perpendicular distance between the teardrop line and the top of the lesser trochanter on the involved side from the distance on the uninvolved side. Extension ROM was measured with the patient in the prone or lateral position, and flexion and abduction ROM were measured with the patient supine.
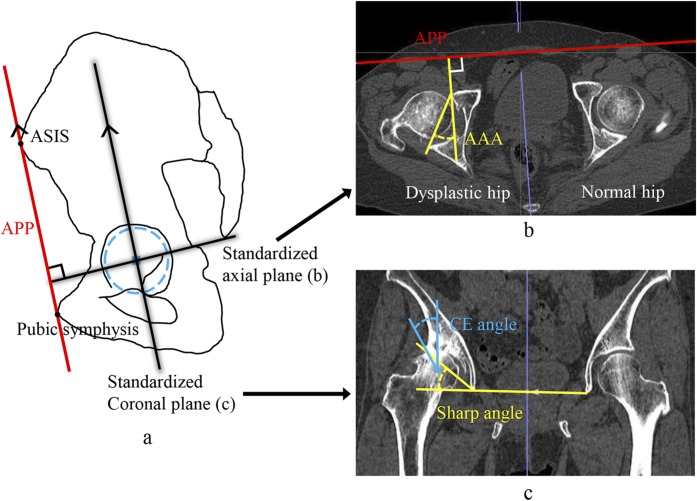
Analysis of CT Scans
Axial CT scans (Toshiba Aquilion; Toshiba Medical System) were performed using a 0.5-mm slice thickness from the level of the iliac crest to the lesser trochanter and at the level of the femoral condyles. Using the Aquarius iNtuition software (TeraRecon), a 3-dimensional reconstruction of the pelvis and femur was created from the CT image. Given that the position of the pelvis in patients who have acetabular dysplasia is compensated while CT scans are performed, the axial images were not symmetrical, and the sliced level differed between the left and right hips in an axial image. Therefore, we had to define the standardized measurement plane with reference to the anterior pelvic plane to exclude the influences of the pelvic position. The standardized axial plane was defined as the plane that was perpendicular to the anterior pelvic plane, was parallel to the teardrop line, and passed through the center of the femoral head on the unaffected side (Fig. 3-A). In this plane, we measured AAA as the angle formed by a line connecting the edges of the anterior and posterior walls of the acetabulum and a line perpendicular to the anterior pelvic plane (Fig. 3-B). The center-edge and Sharp angles generally are measured on the anteroposterior radiograph, but the angles can be influenced by the anteroposterior tilt of the pelvis. Therefore, those angles were measured on the standardized coronal plane that was parallel to the anterior plane of the pelvis and passed through the center of the femoral head on the unaffected side (Fig. 3-A). On the standardized coronal plane, we measured the center-edge angle as the angle formed by a perpendicular line and a line connecting the edge of the acetabular roof with the center of the femoral head. We measured the Sharp angle as the angle formed by the teardrop line and a line connecting the tip of the teardrop with the edge of the acetabular roof (Fig. 3-C).
Fig. 3.
Fig. 3-A The standardized axial and coronal planes with reference to the anterior pelvic plane (APP). ASIS = anterior superior iliac spine. Fig. 3-B The standardized axial plane and measurement of AAA. Fig. 3-C The standardized coronal plane and measurement of the center-edge (CE) angle and the Sharp angle.
Femoral neck anteversion was measured on axial CT images as the angle between a line drawn through the long axis of the neck of the femur and a line connecting the posterior surfaces of the medial and lateral femoral condyles (Fig. 4). We measured femoral neck anteversion in only 66 patients because CT imaging of the femoral condyles was not performed routinely for preoperative evaluation of patients after November 2011.
Fig. 4.
Measurement of the femoral neck anteversion angle (FNAA).
Statistical Analysis
The Shapiro-Wilk test was used to test for the normality of the patients’ characteristics and measured morphometric variables. To test for the correlation between the variables and PT as the indicator of anterior tilt of the pelvis, the Pearson correlation coefficient was used for normally distributed variables and the Spearman rank correlation coefficient was used for non-normally distributed variables. Multivariate regression analysis was performed to identify the variables associated with PT. Candidate variables were selected through a stepwise backward selection method using a p value of 0.3. Correlation between AAA and spinal parameters was also investigated. Statistical analyses were performed using JMP Pro 11.2.1 (SAS Institute).
To evaluate the error in measurement of the hip and spinal parameters, 2 examiners (Y. Okuzu and Y. Okutani) performed the measurements on 2 occasions, >1 month apart. For determination of interobserver reliability, 1 of the examiners performed the measurement for 50 randomly selected patients. Analyses were performed using the average values measured by 1 examiner. We calculated the intraclass correlation coefficients (ICCs) for intraobserver and interobserver reliability using Excel (Microsoft) Statistics 2015 for Windows (version 1.03; Social Survey Research Information).
Results
The demographics of the patients in this study are shown in Table II. Most of the patients were women. The mean AAA and PT were 24.9° and 11.3°, respectively.
TABLE II.
Demographic Characteristics of the Patients in This Study*
| Variable | Affected Hip | Contralateral Hip | |
| Sex, male/female | 11/89 | ||
| Age at operation† (yr) | 60 (35-69) | ||
| Height‡ (cm) | 155.9 ± 6.8 (142.7-178.0) | ||
| Body weight‡ (kg) | 58.2 ± 11.4 (40.2-114.6) | ||
| BMI‡ (kg/m2) | 24.2 ± 4.5 (16.1-43.4) | ||
| LLD† (mm) | 10.9 (0.0-37.8) | ||
| PT‡ (°) | 11.3 ± 6.4 (−3.3-24.9) | ||
| PI‡ (°) | 52.0 ± 9.1 (34.5-78.1) | ||
| LL‡ (°) | 50.8 ± 10.2 (30.8-82.9) | ||
| PI – LL‡ (°) | 1.2 ± 9.4 (−24.2-14.8) | ||
| SVA† (mm) | 19.1 (−41.9-69.5) | ||
| FNSA‡ (°) | 137.6 ± 5.4 (123.3-149.5) | 131.4 ± 3.8 (123.9-139.9) | |
| AAA‡ (°) | 24.9 ± 4.0 (16.3-33.9) | 24.0 ± 5.1 (13.5-38.7) | |
| FNAA‡ (°) | 24.8 ± 11.5 (−5.2-52.5) | 22.3 ± 11.6 (−2.7-52.8) | |
| CAA‡ (°) | 48.9 ± 13.8 (21.5-78.0) | 46.3 ± 13.9 (18.6-86.9) | |
| CE angle (°) | 13.9 ± 10.4 (−31.8-41.5)‡ | 30.1 (25.2-52.0)† | |
| Sharp angle‡ (°) | 47.0 ± 4.8 (32.2-56.9) | 41.7 ± 2.6 (34.2-44.8) | |
| Flexion ROM‡ (°) | 84.6 ± 20.0 (20.0-130.0) | 110.7 ± 11.6 (70.0-130.0) | |
| Abduction ROM‡ (°) | 18.6 ± 9.5 (−20.0-45.0) | 29.9 ± 8.5 (15.0-60.0) | |
| Extension ROM‡ (°) | 2.6 ± 5.5 (−20.0-20.0) | 8.8 ± 4.4 (0.0-25.0) |
BMI = body mass index, LLD = leg-length discrepancy, PI = pelvic incidence, LL = lumbar lordosis, SVA = sagittal vertical axis, FNSA = femoral neck-shaft angle, FNAA = femoral neck anteversion angle, CAA = combined anteversion angle, and CE = center-edge.
The values are given as the median, with the range in parentheses.
The values are given as the mean and standard deviation, with the range in parentheses.
The ICCs for the intraobserver and interobserver reliabilities of the measured parameters are shown in Table III. All of the ICCs were >0.7, indicating excellent or good consistency.
TABLE III.
Intraclass Correlation Coefficients (ICCs) of Measured Parameters
| Variable* | ICC (95% CI)† | |
| Intraobserver Reliability | Interobserver Reliability | |
| LLD | 0.912 (0.871-0.940) | 0.887 (0.809-0.934) |
| FNSA | 0.923 (0.888-0.948) | 0.781 (0.642-0.870) |
| AAA | 0.894 (0.847-0.928) | 0.822 (0.705-0.896) |
| FNAA | 0.882 (0.814-0.926) | 0.864 (0.747-0.929) |
| CE angle | 0.913 (0.873-0.940) | 0.803 (0.677-0.883) |
| Sharp angle | 0.879 (0.825-0.917) | 0.848 (0.747-0.911) |
| PT | 0.889 (0.839-0.924) | 0.854 (0.755-0.915) |
| PI | 0.927 (0.893-0.950) | 0.825 (0.709-0.897) |
| LL | 0.923 (0.888-0.948) | 0.870 (0.782-0.923) |
| SVA | 0.983 (0.974-0.988) | 0.978 (0.961-0.987) |
LLD = leg-length discrepancy, FNSA = femoral neck-shaft angle, FNAA = femoral neck anteversion angle, CE = center-edge, PI = pelvic incidence, LL = lumbar lordosis, and SVA = sagittal vertical axis.
CI = confidence interval.
The correlation coefficients between PT and the other variables are shown in Table IV. Only 2 variables showed a significant correlation: AAA (r = –0.389, p < 0.001) and combined anteversion angle (r = –0.272, p = 0.03). The results of the multivariate regression analysis are shown in Table V. The independent factors associated with PT were AAA (β = –0.385, p < 0.001) and extension ROM (β = 0.212, p = 0.0496); AAA was the stronger factor.
TABLE IV.
Correlation Coefficients Between PT and Patients’ Baseline Characteristics and Hip Joint Variables
| Variable* | Correlation Coefficient | P Value |
| Age at operation in yr | 0.056† | 0.58 |
| Height in cm | –0.089 | 0.38 |
| Body weight in kg | –0.003 | 0.97 |
| BMI in kg/m2 | 0.058 | 0.56 |
| LLD in mm | –0.061† | 0.55 |
| FNSA in degrees | –0.037 | 0.72 |
| AAA in degrees | –0.389 | <0.001 |
| FNAA in degrees | –0.174 | 0.16 |
| CAA in degrees | –0.272 | 0.03 |
| CE angle in degrees | 0.038 | 0.71 |
| Sharp angle in degrees | –0.117 | 0.28 |
| Flexion ROM in degrees | 0.073 | 0.46 |
| Abduction ROM in degrees | –0.034 | 0.74 |
| Extension ROM in degrees | 0.157 | 0.16 |
BMI = body mass index, LLD = leg-length discrepancy, FNSA = femoral neck-shaft angle, FNAA = femoral neck anteversion angle, CAA = combined anteversion angle, and CE = center-edge.
Spearman rank correlation coefficient.
TABLE V.
Multivariate Regression Analysis of Hip Factors Associated with PT
| Variable | Standardized Partial Regression Coefficient (β) | P Value |
| Height | –0.099 | 0.30 |
| AAA | –0.385 | <0.001 |
| Sharp angle | 0.018 | 0.86 |
| Abduction ROM | –0.154 | 0.15 |
| Extension ROM | 0.212 | 0.0496 |
Table VI shows the correlations between AAA and the spinal parameters. Both lumbar lordosis and pelvic incidence minus lumbar lordosis were significantly correlated with AAA, whereas the sagittal vertical axis was not.
TABLE VI.
Correlation Coefficients Between AAA and Spinal Parameters
LL = lumbar lordosis, PI = pelvic incidence, and SVA = sagittal vertical axis.
Spearman rank correlation coefficient.
Discussion
Anterior PT is considered to be the first step of secondary hip-spine syndrome. To the best of our knowledge, this is the first report about hip factors associated with anterior PT. Specifically, we identified a negative correlation between AAA and PT and a positive correlation between extension ROM and PT. Furthermore, AAA was positively correlated with lumbar lordosis and negatively correlated with pelvic incidence minus lumbar lordosis, but no correlation with the sagittal vertical axis was found. Assuming a causal relationship, the results can be understood to indicate that the larger AAA causes the lower PT, and this sequentially induces lumbar hyperlordosis. Furthermore, the lumbar spine is more lordotic than would be expected based on the pelvic incidence. However, AAA was not associated with global spinal alignment.
On the basis of the results of the current study, we postulate that in patients who have a large AAA, the anteriorly tilted pelvis increases the coverage of the femoral head by the acetabulum. Those patients may unconsciously tilt the pelvis anteriorly to avoid edge-loading the hip joint, thereby decreasing the pain in the hip. Conversely, the posteriorly tilted pelvis due to the sagittal spinopelvic imbalance may cause anterior coverage insufficiency of the acetabulum and induce progression of the hip OA, as argued by some authors2,8.
Hyperlordosis is considered to cause low back pain because of the increase in pressure on the posterior ligaments and facet joints5,9. In a CT analysis study, Jentzsch et al. found that hyperlordosis of the lumbar spine was associated with facet joint arthritis in the lower lumbar spine10. Furthermore, Sorensen et al. reported that lumbar lordosis in individuals who had low back pain when standing was greater than it was in individuals without low back pain11. They concluded that greater lumbar lordosis while standing might be a risk factor for the development of low back pain. In view of those findings, it is reasonable to postulate that a large AAA may be associated with spine symptoms such as low back pain.
The results of our study are useful for treating patients who have acetabular dysplasia with hip-spine syndrome. Most patients who have acetabular dysplasia also have an anterior acetabular coverage defect, and they may have anterior pelvic tilt and lumbar hyperlordosis12. During periacetabular osteotomy for patients who have acetabular dysplasia, surgeons internally rotate the acetabular fragment and tilt it anteriorly to achieve the increased lateral and anterior coverage13. That is reasonable not only for increasing anterior acetabular coverage but also for preventing or improving the anterior PT and consequently the hip-spine syndrome. Furthermore, in patients who have acetabular dysplasia with lumbar symptoms, possibly caused by lumbar hyperlordosis, surgeons should recognize the relationship between anterior coverage of the acetabulum and anterior tilt of the pelvis. Hyperlordosis of the lumbar spine may compensate for the anterior coverage of the acetabulum; correction of hyperlordosis can decrease the anterior tilt of the pelvis and the anterior coverage of the acetabulum, and consequently may cause progression of OA of the hip. Therefore, hip and spine surgeons must assess the anterior coverage of the acetabulum before treating a patient for lumbar hyperlordosis.
The position of the pelvis in patients who have acetabular dysplasia is rotated or tilted in 3 dimensions because of various hip and spine factors. Therefore, accurate assessment of hip morphology on normal axial CT images is not possible. To correct for the 3-dimensional pelvic rotation, we used the standardized axial and coronal planes with reference to the anterior pelvic plane. Cup anteversion and abduction angles in total hip arthroplasty are directly influenced by PT14,15, so the same effect would occur in the acetabular coverage in hip joints affected by OA. We think that correcting the pelvic rotation and defining accurate planes for measurement are the strengths of our study. We have identified pelvic axial rotation toward the affected hip in many patients with acetabular dysplasia (Fig. 3-B). We speculate that this axial rotation of the pelvis is caused by increasing the anterior coverage of the acetabulum.
Whether PT differs before and after total hip arthroplasty is controversial. In most studies, PT did not change16-19. However, it has been reported that in specific groups of patients, PT changed. These patients were older and had disc-space narrowing, lower lumbar lordosis, a wide contralateral joint space, or low-back pain4,18-20. Changes in the pelvic parameters are quite important for targeting the position of the acetabular component. The results of our study indicate that PT may increase after total hip arthroplasty in patients who have a large AAA, because they can have abnormally low PT to compensate for the anterior coverage defect. However, we did not investigate postoperative PT in this study. In the future, it will be useful to investigate the characteristics of patients in whom PT changes after total hip arthroplasty.
There are several limitations in our study. First, we evaluated the patients only in static positions. Evaluation in dynamic positions or gait analysis is needed to investigate more accurately and in detail the relationship between the hip and spine. Second, we cannot confirm a causal relationship between PT and both AAA and extension ROM, because our study was cross-sectional in design. However, a previous study suggested that in patients with hip OA and low back pain, the low PT and high lumbar lordosis improved and low back pain decreased after total hip arthroplasty4. Therefore, we postulate that greater AAA can cause anterior tilt of the pelvis and hyperlordosis of the lumbar spine. Third, we did not assess the spine symptoms, which is a major limitation of our study. However, many studies have reported that hyperlordosis of the lumbar spine can cause low back pain, as already discussed. Clarification of the relationship between AAA and spine symptoms requires additional studies. Fourth, it is unclear whether the reason for the results of our study is acetabular dysplasia or hip OA. A study in patients who have acetabular dysplasia without OA would be ideal; however, imaging studies of patients with no OA of the hip, and hence no planned surgical procedures, would not be acceptable. Fifth, the results of our study can be applied only to patients who have unilateral acetabular dysplasia. In our institution, acetabular dysplasia is the underlying cause in most of the patients with hip OA, the majority of whom have a large AAA. Given this characteristic, the results of the current study are justified. If the subjects had been patients with primary hip OA, different results might have been obtained. Sixth, we think that the measurement of the ROM of the hip might not be accurate, because compensation of the spine often occurs when hip ROM is measured. Ideally, measurement of ROM is based on the bone-to-bone relationship of the joints, using fluoroscopy for example, but this is not practical. Lastly, we might not have completely excluded the patients who had spinal imbalance. There is no gold standard to distinguish clearly between patients who do and do not have spinal imbalance. The standard of normal spinal balance has not yet been established, although spinal balance and imbalance may be a sequential pathology.
In conclusion, our study showed a correlation between PT and both AAA and extension ROM. Furthermore, AAA was associated with lumbar lordosis and pelvic incidence minus lumbar lordosis, indicating hyperlordosis of the lumbar spine. When treating patients who have acetabular dysplasia, surgeons should recognize the relationship between anterior coverage of the acetabulum and anterior tilt of the pelvis. Hyperlordosis of the lumbar spine may compensate for the anterior acetabular coverage, and its correction can decrease the anterior tilt of the pelvis and the anterior acetabular coverage, thereby leading to progression of OA in the hip.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Kyoto University Graduate School of Medicine, Kyoto, Japan
Disclosure: No external funding was received for this study. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A84).
References
- 1.Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976). 1983. April;8(3):316-21. [DOI] [PubMed] [Google Scholar]
- 2.Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, Yanagibashi Y. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976). 2005. July 15;30(14):1650-7. [DOI] [PubMed] [Google Scholar]
- 3.Weng WJ, Wang WJ, Wu MD, Xu ZH, Xu LL, Qiu Y. Characteristics of sagittal spine-pelvis-leg alignment in patients with severe hip osteoarthritis. Eur Spine J. 2015. June;24(6):1228-36. Epub 2014 Nov 25. [DOI] [PubMed] [Google Scholar]
- 4.Piazzolla A, Solarino G, Bizzoca D, Montemurro V, Berjano P, Lamartina C, Martini C, Moretti B. Spinopelvic parameter changes and low back pain improvement due to femoral neck anteversion in patients with severe unilateral primary hip osteoarthritis undergoing total hip replacement. Eur Spine J. 2018. January;27(1):125-34. Epub 2017 Mar 16. [DOI] [PubMed] [Google Scholar]
- 5.Adams MA, Hutton WC. The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J Bone Joint Surg Br. 1980. August;62(3):358-62. [DOI] [PubMed] [Google Scholar]
- 6.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979. January;61(1):15-23. [PubMed] [Google Scholar]
- 7.Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012. May 20;37(12):1077-82. [DOI] [PubMed] [Google Scholar]
- 8.Matsuyama Y, Hasegawa Y, Yoshihara H, Tsuji T, Sakai Y, Nakamura H, Kawakami N, Kanemura T, Yukawa Y, Ishiguro N. Hip-spine syndrome: total sagittal alignment of the spine and clinical symptoms in patients with bilateral congenital hip dislocation. Spine (Phila Pa 1976). 2004. November 1;29(21):2432-7. [DOI] [PubMed] [Google Scholar]
- 9.Chun SW, Lim CY, Kim K, Hwang J, Chung SG. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J. 2017. August;17(8):1180-91. Epub 2017 May 2. [DOI] [PubMed] [Google Scholar]
- 10.Jentzsch T, Geiger J, König MA, Werner CM. Hyperlordosis is associated with facet joint pathology at the lower lumbar spine. Clin Spine Surg. 2017. April;30(3):129-35. [DOI] [PubMed] [Google Scholar]
- 11.Sorensen CJ, Norton BJ, Callaghan JP, Hwang CT, Van Dillen LR. Is lumbar lordosis related to low back pain development during prolonged standing? Man Ther. 2015. August;20(4):553-7. Epub 2015 Jan 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okuda T, Fujita T, Kaneuji A, Miaki K, Yasuda Y, Matsumoto T. Stage-specific sagittal spinopelvic alignment changes in osteoarthritis of the hip secondary to developmental hip dysplasia. Spine (Phila Pa 1976). 2007. December 15;32(26):E816-9. [DOI] [PubMed] [Google Scholar]
- 13.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am. 2006. March;88(Suppl 1 Pt 1):65-83. [DOI] [PubMed] [Google Scholar]
- 14.Penenberg BL, Samagh SP, Rajaee SS, Woehnl A, Brien WW. Digital radiography in total hip arthroplasty: technique and radiographic results. J Bone Joint Surg Am. 2018. February 7;100(3):226-35. [DOI] [PubMed] [Google Scholar]
- 15.Buckland AJ, Vigdorchik J, Schwab FJ, Errico TJ, Lafage R, Ames C, Bess S, Smith J, Mundis GM, Lafage V. Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am. 2015. December 2;97(23):1913-20. [DOI] [PubMed] [Google Scholar]
- 16.Blondel B, Parratte S, Tropiano P, Pauly V, Aubaniac JM, Argenson JN. Pelvic tilt measurement before and after total hip arthroplasty. Orthop Traumatol Surg Res. 2009. December;95(8):568-72. [DOI] [PubMed] [Google Scholar]
- 17.Maratt JD, Esposito CI, McLawhorn AS, Jerabek SA, Padgett DE, Mayman DJ. Pelvic tilt in patients undergoing total hip arthroplasty: when does it matter? J Arthroplasty. 2015. March;30(3):387-91. Epub 2014 Oct 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suzuki H, Inaba Y, Kobayashi N, Ishida T, Ike H, Saito T. Postural and chronological change in pelvic tilt five years after total hip arthroplasty in patients with developmental dysplasia of the hip: a three-dimensional analysis. J Arthroplasty. 2016. January;31(1):317-22. Epub 2015 Jul 17. [DOI] [PubMed] [Google Scholar]
- 19.Nishiwaki T, Hata R, Oya A, Nakamura M, Matsumoto M, Kanaji A. Pelvic tilt displacement before and after artificial hip joint replacement surgery. J Arthroplasty. 2018. March;33(3):925-30. Epub 2017 Oct 16. [DOI] [PubMed] [Google Scholar]
- 20.Kyo T, Nakahara I, Miki H. Factors predicting change in pelvic posterior tilt after THA. Orthopedics. 2013. June;36(6):e753-9. [DOI] [PubMed] [Google Scholar]