Abstract
In the Eastern European and Central Asian (EECA) region, the only one globally where HIV incidence and mortality are increasing, HIV is concentrated among high risk groups like prisoners. HIV prevalence is higher among women than men in both prison and community settings. Data are lacking on the HIV care continuum among female prisoners in the EECA to inform effective HIV prevention and treatment interventions. This study examined HIV risk, prevalence of infectious diseases, access to care, and other medical and psychiatric comorbidities among a representative sample of 220 female prisoners in three EECA countries: Azerbaijan, Kyrgyzstan, and Ukraine. Participants were recruited using stratified random sampling. Prevalence of comorbid substance use and psychiatric disorders was high with nearly one-third of the women reporting pre-incarceration drug injection and alcohol use disorder (AUD). Half of the sample reported anxiety and depression. Among the subset of 26 (11.8%) women testing HIV+, 44% had CD4 counts <350 cells/μL but less than 2% were on antiretroviral therapy (ART). Most (88.5%) women with HIV were in Ukraine, where women also experienced higher rates of hepatitis C than in Azerbaijan or Kyrgyzstan. Similarly, women in Kyrgyzstan prisons experienced higher rates of syphilis compared to the other two countries. Findings suggest that, to achieve global HIV prevention and treatment targets, HIV testing and linkage to care must be scaled up among incarcerated women in the EECA. Women also require testing and treatment for comorbid psychiatric and substance use disorders to effectively reduce their post-incarceration HIV risk.
Keywords: Women, prison, Eastern Europe and Central Asia, HIV care continuum, epidemiological outcomes
Introduction
Nearly 700,000 women are incarcerated worldwide, accounting for 9% of the global prison population; 16% of these are in Eastern Europe and Central Asia (EECA) (Lakobishvili, 2012). Incarcerated women, relative to incarcerated men, have a higher burden of medical and psychiatric diseases and experience poorer health outcomes (UNAIDS, 2016b), including HIV and sexually transmitted infections (STIs) (Azbel, Grishaev, et al., 2016; El-Bassel et al., 2017). Substance use and sex work contribute to women’s incarceration and simultaneously exacerbate risk of HIV and other infectious diseases (De Groot, 2000; Rich et al., 1999).
Prisoners bear a substantially higher burden of HIV and other blood-borne infections than community-based populations (F. L. Altice et al., 2016). In all three countries, prisoners most commonly acquire HIV via injection drug use (IDU) (Dolan et al., 2016). The estimated HIV prevalence among prisoners in Ukraine is 19.4% (Azbel, Wickersham, Grishaev, Dvoryak, & Altice, 2013), 5.8% in Azerbaijan, and 7.6% in Kyrgyzstan (Azbel, Polonsky, et al., 2016).
The HIV care continuum provides a framework to understand and evaluate the effectiveness of HIV programs from diagnosis to viral suppression (Gardner, McLees, Steiner, del Rio, & Burman, 2011). Despite UNAIDS 90–90-90 targets to end AIDS, overall coverage of antiretroviral therapy (ART) in the EECA region is <10% (WHO, 2013). Although incarcerated women bear a substantial burden of HIV, there is limited information about their access to and utilization of evidence-based HIV prevention and treatment services in prisons. This information is crucial to identify gaps in service delivery and develop effective strategies to prevent and treat HIV among incarcerated women.
Methods
Three bio-behavioral surveys were conducted in Azerbaijan, Kyrgyzstan, and Ukraine between 2011 and 2014 (Azbel, Polonsky, et al., 2016; Azbel et al., 2013; Azbel et al., 2015). In all three countries, a nationally representative, cross-sectional comprehensive health survey and sero-surveillance assessment of infectious diseases were conducted among men and women awaiting release from prison. Participants were selected using a random stratified sampling strategy (Azbel et al., 2013). Inclusion criteria for women were: a) >18 years of age; b) within six (Ukraine), 12 (Kyrgyzstan), or 18 months (Azerbaijan) of scheduled release date; and c) serving a sentence in a non-specialized facility (that excluded juvenile facilities, pre-trial detention, and hospitals).
Measures
Participants were assessed for detention history, alcohol use disorders (AUDs) using the Alcohol Use Disorders Inventory Test (AUDIT) (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993), depression using the CES-D with scores ≥11 suggesting major depressive disorder (Irwin, Artin, & Oxman, 1999), and anxiety (Kyrgyzstan and Azerbaijan only) using the 20-item Zung anxiety scale (Zung, 1971) with scores ≥45 indicating clinical anxiety (Dunstan, Scott, & Todd, 2017). HIV risk behaviors 30 days before incarceration were assessed, including condomless sex with multiple partners or an HIV+ partner and sharing injection paraphernalia. The assessment included HIV testing experiences, chronic illnesses (high blood pressure, liver problems, heart disease, and tuberculosis) and serological testing for HIV, HCV, HBV, and syphilis.
Results
Sample characteristics stratified by country (Table 1) shows differences among women in the three countries including education and marital status. Prior incarceration (mean times=2.9; SD=1.7) differed significantly between the three countries and nearly one-third of women met criteria for an AUD, with significantly higher prevalence in Ukraine (Table 2). Nearly half met screening criteria for major depression, significantly more in Ukraine (23.0%) than in Azerbaijan (5.3%) or in Kyrgyzstan (19.1%). Anxiety disorders were similarly prevalent in Azerbaijan and Kyrgyzstan but were not assessed in Ukraine.
Table 1.
Demographic characteristics and criminal history of women prisoners in Azerbaijan (AZE), Kyrgyzstan (KYR) and Ukraine (UKR) (N=220)
| N (%)1 | |||||||
|---|---|---|---|---|---|---|---|
| Total (N = 220) | AZE (n = 58) | KYR (n = 81) | UKR (n = 81) | F or χ2 | p | ||
| Mean age (SD), years | 38.7 (10.5) | 42.4 (10. 8) | 40.62 (10.9) | 33.97 (7.8) | 14.7 | <.01 | |
| Ethnicity | Azerbaijani | 48 (21.8) | 48 (82.7)* | 331.95 | <.01 | ||
| Kyrgyz | 30 (13.6) | 30 (37.0)* | |||||
| Ukrainian | 50 (22.7) | 50 (61.7)* | |||||
| Russian | 57 (25.9) | 30 (37.0)* | 27 (33.3) | ||||
| Uzbek | 8 (3.6) | 8 (9.9)* | |||||
| Roma | 1 (0.5) | 1 (1.2) | |||||
| Religion | Orthodox | 59 (26.8) | 59 (72.8)* | 275.76 | <.01 | ||
| Protestant | 3 (1.4) | 3 (3.37)* | |||||
| Greek Orthodox | 5 (2.3) | 5 (6.2)* | |||||
| Muslim | 91 (41.4) | 46 (79.3)* | 45 (55.6)* | ||||
| Christian | 35 (15.9) | 35 (43.2)* | |||||
| Marital status | Single | 73 (34.6) | 14 (24.1) | 20 (24.7) | 39 (17.7)* | 29.4 | <.01 |
| Have a partner | 12 (5.7) | 6 (10.3)* | 2 (2.5) | 4 (1.8) | |||
| Married/unregistered marriage | 46 (21.8) | 11 (19) | 17 (21)* | 18 (8.2) | |||
| Divorced | 45 (21.3) | 14 (24.1) | 21 (25.9) | 10 (4.5) | |||
| Widowed | 34 (16.1) | 3 (5.2) | 21 (25.9) | 10 (4.5) | |||
| In a sexual relationship | Yes | 58 (27.5) | 17 (8.1) | 19 (9.0) | 22 (10.4) | 1.9 | 0.37 |
| Education | No Education | 12 (5.7) | 8 (3.8) * | 0 | 4 (1.9) | 18.3 | <.01 |
| High school and below | 134 (63.5) | 24 (11.4) | 53 (25.1) | 57 (27.0) | |||
| Above high school | 65 (30.8) | 17 (8.1) | 28 (13.3) | 20 (9.5) | |||
| Recidivist | Yes | 94 (42.7) | 19 (32.8) | 36 (44.4) | 39 (48.1) | 3.4 | 0.18 |
| Mean number of previous incarcerations for recidivists (SD) | 2.9 (1.7) | 1.1 (0.3) | 2.67 (1.8) | 3.41 (1.5) | 8.2 | <.01 | |
| Mean incarceration, years (SD) | 2.9 (2.1) | 3.9 (2.4) | 2.9 (1.7) | 2.3 (1.8) | 10.5 | <.01 | |
Note.
= p≤.05.
Adjusted standardized residual greater than 1.96
May not sum to 100% because of missing values
Table 2.
Substance use, mental health and sexual behavior of women prisoners in Azerbaijan (AZE), Kyrgyzstan (KYR) and Ukraine (UKR)
| Country N (%) | ||||||
|---|---|---|---|---|---|---|
| Total (n = 220) | AZE (n = 58) | KYR (n = 81) | UKR (n = 81) | χ 2 | p | |
| Alcohol use disorder (AUD) | 68 (31.9) | 3 (5.2) | 21 (25.9) | 44 (54.3) * | 37.3 | <.01 |
| Depression | 99 (47.4) | 11 (18.9) | 40 (49.4) | 48 (59.3) * | 16.7 | <.01 |
| Anxiety Disorder | 9 (6.9) | 2 (3.4) | 7(8.6) | |||
| Condomless sex 30 days prior to arrest | 87 (40.8) | 15 (15.5) | 27 (33.3) | 45 (55.6)* | 13.8 | <.01 |
| Had unprotected sex with >1 person in 30 days prior to arrest | 21 (9.9) | 9 (15.5) * | 3 (3.7) | 9 (11.1) | 6.6 | <.05 |
| Had sex with HIV+ partner without a condom | 9 (4.3) | 0 (0.0) | 0 (0.0) | 9 (4.3) * | 15.7 | <.01 |
| Engaged in transactional sex 30 days prior to arrest | 16 (7.6) | 10 (17.2) * | 1 (1.2) | 5 (6.2) | 15.8 | <.01 |
| Injected drug even once | 65 (30.7) | 8 (13.8) | 13 (16.0) | 44 (54.3) * | 37.1 | <.01 |
| Reused injection equipment 30 days prior to arrest | 33 (15.8) | 5 (8.6) | 3 (3.7) | 25 (30.9) * | 24.9 | <.01 |
Note.
= p≤.05.
Adjusted standardized residual greater than 1.96.
Anxiety disorder was not measured in Ukraine.
In the 30 days before incarceration, 40.8% of women reported any condomless sex, including 10% with multiple partners and 4.3% with an HIV+ partner. One-third of women reported prior drug injection, among whom 15.8% reported sharing equipment in the 30 days before incarceration, mostly in Ukraine. Serological screening (Table 3) confirmed high levels of HIV (N=26; 11.8%), HCV (N=72; 33.5%) and syphilis (N=38; 17.7%), with significantly higher prevalence of HIV and HCV in Ukraine and significantly higher prevalence of syphilis in Kyrgyzstan. High levels of co-morbid health conditions were also self-reported, including hypertension (39.4%), liver problems (24.4%), heart disease (26.4%), and prior tuberculosis (8.2%).
Table 3.
Contingency table of sexually transmitted infection (STI) and self-reported history of chronic illnesses in Azerbaijan (AZE), Kyrgyzstan (KYR) and Ukraine (UKR)
| Country |
||||||
|---|---|---|---|---|---|---|
| N (%) |
||||||
| Total (n = 220) | AZE (n = 58) | KYR (n = 81) | UKR (n = 81) | χ 2 | p | |
| Ever been tested for HIV? | 181 (82.2) | 49 (84.5) | 71 (87.7) | 61 (75.3) | 6.2 | .04 |
| Received HIV test result | 139 (63.2) | 46 (79.3) | 44(54.3) | 49 (60.5) | 14.9 | <.01 |
| HIV+ | 26 (11.8) | 1 (1.7) | 2 (2.7) | 23 (28.4) * | 33.8 | <.01 |
| Hepatitis C | 72 (32.7) | 6 (10.3) | 14 (17.3) | 52 (64.2) * | 57.9 | <.01 |
| Hepatitis B | 7 (3.2) | 0 | 5 (6.2) | 2 (2.5) | 4.6 | 0.09 |
| Syphilis | 38 (17.7) | 0 | 25 (30.9) * | 13 (16.1) | 24.7 | <.01 |
| Have you been told by a doctor you have high blood pressure | 82 (39.4) | 7 (12.1) | 27 (33.3) | 48 (59.5) * | 27.3 | <.01 |
| Have you been told by a doctor you have liver problems | 51 (24.4) | 3 (5.2) | 24 (29.6) | 24 (29.6) | 11.1 | <.01 |
| Have you been told by a doctor you have heart disease | 55 (26.4) | 8 (13.8) | 19 (23.5) | 28 (34.6) * | 5.6 | .06 |
| Have you been told by a doctor you have tuberculosis | 17 (8.2) | 0 | 8 (9.9) | 9 (11.1) | 5.5 | .06 |
Note.
= p≤.05.
Adjusted standardized residual appear greater than 1.96.
In the HIV care continuum (Figure 1), 8 (30.8%) of the 26 women with HIV were unaware of their status and 11 (44%) had a CD4 count <350 cells/μL, meeting immunologic criteria for ART at the time of the study (i.e. prior to universal treatment recommendations); nearly all were Ukrainian. Only three (11.5%) women were ever prescribed or currently taking ART.
Figure 1.
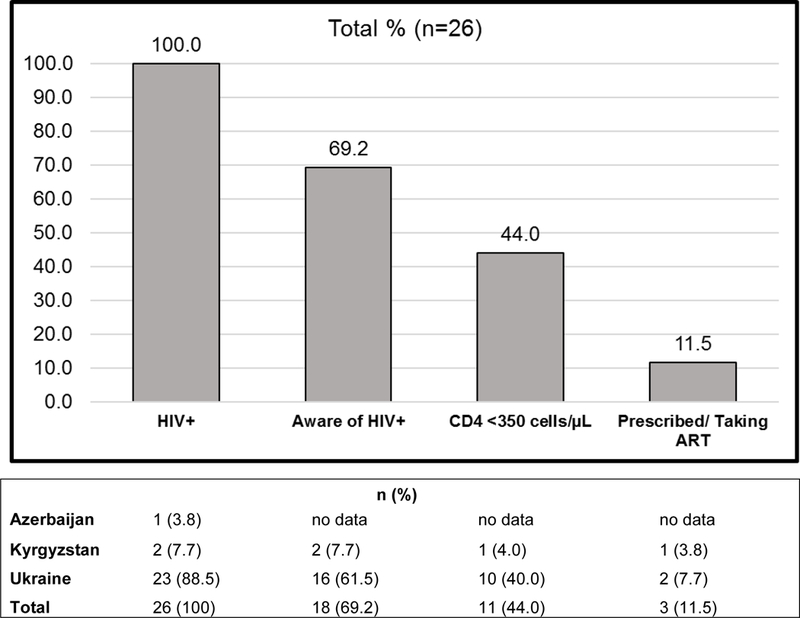
HIV Care Continuum among incarcerated women with HIV+ in Azerbaijan, Kyrgyzstan and Ukraine, n = 26.
Discussion
We assessed the health conditions of incarcerated women in three EECA countries where the HIV epidemic is rapidly escalating, though prisoners, and particularly women, are often excluded from the national and regional dialogue about HIV prevention and treatment. In a randomly-selected, representative sample of female prisoners awaiting release in three EECA countries, we found high prevalence of HIV, viral hepatitis, STIs and pre-incarceration HIV-related risk behaviors. We similarly, found high levels of co-morbid medical, psychiatric, and substance use disorders that may complicate delivery of care post-release and portend poor health outcomes, if not identified and treated.
Optimization of the HIV care continuum is crucial for achieving better health outcomes for people with HIV (PWH) and for limiting onward HIV transmission (McNairy & El-Sadr, 2012). Despite seemingly high testing levels, testing was still likely suboptimal given that nearly one-third of women were unaware of their HIV status. This finding suggests that “opt-in” HIV testing strategies, like the ones throughout EECA prisons, is inadequate and falls markedly short of the 90% UNAIDS target. Undiagnosed or unaware PWH accounts for a large proportion of all transmissions of HIV to others (Hall, Holtgrave, & Maulsby, 2012; Skarbinski, Rosenberg, Paz-Bailey, & et al., 2015). In these women, however, the most concerning component of the HIV continuum occurred after diagnosis. Though linkage to care data were not available, only 11.5% of women with HIV had ever been prescribed ART. Even if immunological criteria for ART (CD4 <350 cells/μL) were applied, only 27.2% of potentially eligible women had ever received ART. These findings raise major concerns about effectively implementing 2015 WHO recommendations to provide universal treatment to all PWH (WHO, 2015).
Nearly all (90%) of the incarcerated women with HIV were in Ukraine, despite comparable rates of prior testing. The prevalence of HIV among women in Ukrainian prisons approached 30%, which is significantly higher than in both Azerbaijan and Kyrgyzstan, and similar to HIV prevalence in prisons in Sub-Saharan Africa where there is a generalized HIV epidemic (Telisinghe et al., 2016). This finding is consistent with other epidemiological studies that show Ukraine has the highest HIV prevalence in Europe (UNAIDS, 2016a). Findings here suggest an urgent need for marked improvements in the HIV continuum of care among women in prison settings, particularly in Ukraine, to achieve UNAIDS 90–90-90 goals for 2020. ART within prison, must be yoked to effective interventions that retain women in HIV care after release (Loeliger, Altice, Ciarleglio, et al., 2018; Loeliger, Altice, Desai, et al., 2018).
Extraordinarily high pre-incarceration risk behaviors point to the need for targeted HIV prevention after release. Settings like Azerbaijan and Kyrgyzstan may serve as cautionary tales for an impending HIV epidemic given the high reported HIV risk behaviors in communities by women prisoners. In the absence of sufficiently-scaled HIV prevention services for transitioning prisoners, HIV incidence will likely increase (Altice et al., 2016). Prisons can facilitate improved clinical outcomes for individuals by providing sufficient resources to expand evidence-based HIV prevention, including: universal opt-out HIV testing, screening and treatment of STIs, condom distribution, opioid agonist therapies (OAT) with methadone, syringe service programs, and delivery of adequate medical care, including ART, for PWH (Springer et al., 2004). Among non-incarcerated women who inject drugs in Ukraine, OAT improved addiction treatment outcomes and was broadly stabilizing (Hoff et al., 2017). Unfortunately, OAT is woefully low throughout EECA and is unavailable in prisons except for a few countries such as Kyrgyzstan and Moldova (Azbel et al., 2018).
Despite important findings from a nationally representative samples of incarcerated women in the EECA, some limitations remain. Pre-incarceration risk behaviors may have been under-reported due to recall bias and questions specific to women, like reproductive and maternal health, were not included.
Conclusion
The HIV care continuum in women prisoners in the EECA reflects suboptimal HIV testing and treatment in the context of high HIV risk behaviors, especially in Ukraine. Effective treatment of HIV requires management of co-morbid substance use and psychiatric disorders, which were highly prevalent. These findings point to the urgent need to scale up evidence-based HIV prevention and treatment strategies for women in prisons in this region.
References
- Altice, Azbel L, Stone J, Brooks-Pollock E, Smyrnov P, Dvoriak S, … Vickerman P (2016). The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. Lancet (London, England), 388(10050), 1228–1248. doi: 10.1016/S0140-6736(16)30856-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Azbel L, Stone J, Brooks-Pollock E, Smyrnov P, Dvoriak S, … Vickerman P (2016). The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. The Lancet, 388(10050), 1228–1248. doi: 10.1016/S0140-6736(16)30856-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Grishaev Y, Wickersham JA, Chernova O, Dvoryak S, Polonsky M, & Altice FL (2016). Trials and tribulations of conducting bio-behavioral surveys in prisons: implementation science and lessons from Ukraine. International journal of prisoner health, 12(2), 78–87. doi: 10.1108/IJPH-10-2014-0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Polonsky M, Wegman M, Shumskaya N, Kurmanalieva A, Asanov A, … Altice FL (2016). Intersecting epidemics of HIV, HCV, and syphilis among soon-to-be released prisoners in Kyrgyzstan: Implications for prevention and treatment. International Journal of Drug Policy, 37, 9–20. doi: 10.1016/j.drugpo.2016.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wegman MP, Polonsky M, Bachireddy C, Meyer JP, Shumskaya N, … Altice FL (2018). Drug injection within prison in Kyrgyzstan: elevated HIV risk and implications for scaling up opioid agonist treatments. Int J Prison Health, 14(3), 175–187. doi: 10.1108/ijph-03-2017-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, & Altice FL (2013). Burden of Infectious Diseases, Substance Use Disorders, and Mental Illness among Ukrainian Prisoners Transitioning to the Community. PLoS ONE, 8(3), e59643. doi: 10.1371/journal.pone.0059643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azbel L, Wickersham JA, Wegman MP, Polonsky M, Suleymanov M, Ismayilov R, … Altice FL (2015). Burden of substance use disorders, mental illness, and correlates of infectious diseases among soon-to-be released prisoners in Azerbaijan. Drug and alcohol dependence, 151, 68–75. doi: 10.1016/j.drugalcdep.2015.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Groot AS (2000). HIV infection among incarcerated women: epidemic behind bars. AIDS Read, 10(5), 287–295. [PubMed] [Google Scholar]
- Dolan K, Wirtz AL, Moazen B, Ndeffo-mbah M, Galvani A, Kinner SA, … Altice FL (2016). Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. The Lancet, 388(10049), 1089–1102. doi: 10.1016/S0140-6736(16)30466-4 [DOI] [PubMed] [Google Scholar]
- Dunstan DA, Scott N, & Todd AK (2017). Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC psychiatry, 17(1), 329. doi: 10.1186/s12888-017-1489-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Marotta PL, Shaw SA, Chang M, Ma X, Goddard-Eckrich D, … Gilbert L (2017). Women in community corrections in New York City: HIV infection and risks. Int J STD AIDS, 28(2), 160–169. doi: 10.1177/0956462416633624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, del Rio C, & Burman WJ (2011). The Spectrum of Engagement in HIV Care and its Relevance to Test-and-Treat Strategies for Prevention of HIV Infection. Clinical Infectious Diseases, 52(6), 793–800. doi: 10.1093/cid/ciq243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall HI, Holtgrave DR, & Maulsby C (2012). HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS, 26(7), 893–896. doi: 10.1097/QAD.0b013e328351f73f [DOI] [PubMed] [Google Scholar]
- Hoff E, Marcus R, Bojko MJ, Makarenko I, Mazhnaya A, Altice FL, & Meyer JP (2017). The effects of opioid-agonist treatments on HIV risk and social stability: A mixed methods study of women with opioid use disorder in Ukraine. J Subst Abuse Treat, 83, 36–44. doi: 10.1016/j.jsat.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin M, Artin K, & Oxman MN (1999). Screening for depression in the older adult: Criterion validity of the 10-item center for epidemiological studies depression scale (ces-d). Archives of Internal Medicine, 159(15), 1701–1704. doi: 10.1001/archinte.159.15.1701 [DOI] [PubMed] [Google Scholar]
- Lakobishvili E (2012). Cause for alarm: The incarcerated women for drug offences in Europe and Central Asia, and the need for legislative and sentencing reform: International Harm Reduction Association
- Loeliger KB, Altice FL, Ciarleglio MM, Rich KM, Chandra DK, Gallagher C, … Meyer JP (2018). All-cause mortality among people with HIV released from an integrated system of jails and prisons in Connecticut, USA, 2007–14: a retrospective observational cohort study. The Lancet HIV, 5(11), e617–e628. doi: 10.1016/S2352-3018(18)30175-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeliger KB, Altice FL, Desai MM, Ciarleglio MM, Gallagher C, & Meyer JP (2018). Predictors of linkage to HIV care and viral suppression after release from jails and prisons: a retrospective cohort study. The Lancet HIV, 5(2), e96–e106. doi: 10.1016/S2352-3018(17)30209-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNairy ML, & El-Sadr WM (2012). The HIV care continuum: no partial credit given. AIDS, 26(14), 1735–1738. doi: 10.1097/QAD.0b013e328355d67b [DOI] [PubMed] [Google Scholar]
- Rich JD, Dickinson BP, Macalino G, Flanigan TP, Towe CW, Spaulding A, & Vlahov D (1999). Prevalence and Incidence of HIV Among Incarcerated and Reincarcerated Women in Rhode Island. JAIDS Journal of Acquired Immune Deficiency Syndromes, 22(2), 161–166. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Skarbinski J, Rosenberg E, Paz-Bailey G, & et al. (2015). Human immunodeficiency virus transmission at each step of the care continuum in the united states. JAMA Internal Medicine, 175(4), 588–596. doi: 10.1001/jamainternmed.2014.8180 [DOI] [PubMed] [Google Scholar]
- Springer SA, Pesanti E, Hodges J, Macura T, Doros G, & Altice FL (2004). Effectiveness of Antiretroviral Therapy among HIV-Infected Prisoners: Reincarceration and the Lack of Sustained Benefit after Release to the Community. Clinical Infectious Diseases, 38(12), 1754–1760. doi: 10.1086/421392 [DOI] [PubMed] [Google Scholar]
- Telisinghe L, Charalambous S, Topp SM, Herce ME, Hoffmann CJ, Barron P, … Amon JJ (2016). HIV and tuberculosis in prisons in sub-Saharan Africa. Lancet doi: 10.1016/S0140-6736(16)30578-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2016a). Country Factsheets
- UNAIDS. (2016b). Prevention Gap Report
- WHO. (2013). Global Update on HIV Treatment 2013: Results, impact and opportunities
- WHO. (2015). Guideline on when to start Antiretroviral Therapy and on Pre-exposure Prophylaxis for HIV [PubMed]
- Zung WW (1971). A rating instrument for anxiety disorders. Psychosomatics, 12(6), 371–379. doi: 10.1016/s0033-3182(71)71479-0 [DOI] [PubMed] [Google Scholar]


