Abstract
Background:
Labels such as “addict” and “substance abuser” have been found to elicit implicit and explicit stigma among the general public previously. The difference in the levels of this bias among individuals in recovery and those employed in the health profession has not yet been identified, however. The current study seeks to answer this question using measures of implicit bias.
Methods:
A subset sample (n = 299) from a previously completed study (n = 1,288) was selected for analysis. Mixed-model ANOVA tests were completed to identify variance between d-prime automatic association scores with the terms “addict” and “substance abuser” among individuals in recovery and those identified as working in the health professions.
Results:
Individuals in recovery did not have lower negative associations with either term, whereas individuals employed as health professionals had greater negative associations with the term “substance abuser” but did not have greater negative associations with the term “addict”.
Conclusions:
Results provide further evidence that previously identified stigmatizing labels have the potential to influence medical care and medical practitioner perceptions of individuals with substance use disorders and should be avoided. Further exploration into the role negative associations derived from commonly used labels have in the individual recovery process are needed to draw appropriate recommendations.
Keywords: addiction, substance use disorder, stigma, bias, discrimination, linguistics, language, recovery, health professionals
An estimated 19.7 million people aged 12 or older met criteria for substance use disorder (SUD) in 2017; yet, only 4 million people aged 12 or older received any form of SUD treatment, and only 2.5 million received treatment from a facility specializing in SUD (SAMHSA, 2018). Of people aged 12 or older who perceived a need but did not receive treatment, 20.5% reported fear that receiving treatment would result in work consequences and 17.2% believed that there would be social consequences if they received treatment (SAMHSA, 2018). Combined, over 37% of these individuals not seeking care due to stigma and discrimination related reasons presents a significant obstacle.
Stigma is often cited as a significant barrier to treatment and overall help-seeking behaviors for individuals with SUDs (Clement et al, 2015). Stigma operates under the conditions of a label (i.e. addict) and an associated stereotype (i.e. unworthy) to produce a negative response (i.e. discrimination) (Link & Phelan, 2001). For SUD-related stigma, this holds true in both public and professional settings. For example, how SUD is characterized can impact public opinion of policies, funding, and desire for social distance (Barry, McGinty, Pescosolido, & Goldman, 2015; McGinty, Goldman, Pescosolido, & Barry, 2015). Kelly, Dow, and Westerhoff (2010) found that individuals labeled as “substance abusers” were more likely to be viewed as a threat and be assigned blame warranting punitive measures instead of medical treatment, but when an individual was characterized as “having a substance use disorder,” these opinions were more positive, with less blame and threat assigned, as well as stronger belief that treatment was more appropriate than punishment (Kelly et al., 2010).
In a follow-up study, medical professionals at two addiction-focused conferences assessed the same terms (substance abuser vs. person with a substance use disorder) and were more likely to associate fault and punishment with “substance abuser” than with “person with a substance use disorder” (Kelly & Westerhoff, 2010). This is important in light of van Boekel and colleagues’ 2013 study that found that people with SUDs are generally stigmatized by medical professionals, and that such stigma impinges on the way these professionals interact with clients, which negatively impacts treatment outcomes (van Boekel, Brouwers, van Weeghel, & Garretsen, 2013).
Understanding that the language used to describe people with SUD can impact social and clinical interactions, it is vital to explore the mechanisms and manifestations of stigma. Stigma can be explicit as found in the Kelly (2010) and van Boekel (2013) studies but can also manifest through implicit bias. Implicit biases are the subconscious attitudes and beliefs (Greenwald & Krieger, 2006) that are akin to the labels and stereotypes of stigma (Link & Phelan, 2001). Implicit bias has been shown to impact human behavior in a variety of ways, but exploration into how implicit bias manifests in the SUD field has only recently begun (Authors, 2018a; Authors, 2018b; Authors, 2018c).
One unanswered question in recent studies of SUD-related implicit bias is the way in which language found to elicit negative associations varies based on individual recovery status and between those employed in the health professions and those not. While previous research (van Boekel et al., 2013) would suggest that health professionals hold higher levels of bias towards individuals with SUD, the extent of this difference has not yet been studied. Conversely, given the theoretical insight into the “spoiled identity” mechanism of individuals in recovery (Goffman, 1963; Hughes, 2007; McIntosh & McKeganey, 2001), and qualitative work with individuals in recovery exploring the cathartic benefit of using seemingly derogatory labels (Tkach, 2017), we have hypothesized previously (Authors, 2018b, 2018c) that levels of bias associated with stigmatizing labels within a recovering population may be lower as compared to those in the general population.
External stigma has been associated with help-seeking behavior among individuals with a SUD (SAMHSA, 2018) and the quality of care delivered or recommended (Kelly & Westerhoff, 2010; van Boeckel et al., 2013; Luoma, Kulesza, Hayes, Kohlenberg, & Larimer, 2014). This external stigma may also become internalized for the individual with a SUD or in recovery, leading to self-stigma (Luoma, Kohlenberg, Hayes, Bunting, & Rye, 2008). As such, while the general population is an important population of focus when examining the role and impact of language on stigma, the specific relationship with those in recovery or working in the health-care professions as those with specific health and wellness outcomes associated with stigma is a critical area of focus.
This study is an extension of our previous work using the Go/No-Go Association Task (GNAT; Nosek & Banaji, 2001) to analyze implicit bias and stigmatizing language surrounding SUD among various groups (Authors, 2018a, 2018b, 2018c). We hypothesize that individuals who self-identify as in recovery, as compared to individuals not identifying as in recovery, will have lower negative associations with the terms “addict” and “substance abuser”. Our second hypothesis is that individuals employed as health professionals, as compared to those not employed as health professionals, will have greater negative associations with the terms “addict” and “substance abuser”.
Methods
Recruitment
Participants (n = 299) were individuals recruited through Research Match, a national health volunteer registry that was created by several academic institutions and supported by the U.S. National Institutes of Health as part of the Clinical Translational Science Award (CTSA) program. Research Match has a large population of volunteers who have consented to be contacted by researchers about research studies that they are eligible for. An initial interest email was sent to 98,000 random volunteers from the Research Match registry. Volunteers that elected to receive more information about the study (N = 7,500) were then provided a separate email that described the study in detail and provided a URL link to the informed consent The n = 299 reported here are a subsample of the 1,288 reported previously (Authors, 2018b). The justification for this secondary analysis is to identify the effects of either recovery status (i.e. in recovery or not in recovery) or employment type (i.e. health professional or other professional) on the implicit bias associated with two commonly used labels towards individuals with a SUD: “substance abuser” and “addict”. The study was reviewed and approved by the University of Pennsylvania Institutional Review Board #8.
Procedure
Participants that consented to participate in the study were randomly placed into groups representing each word pair option (e.g. substance abuser and person with a substance use disorder, or addict and person with a substance use disorder, in the current study). Each group of participants then completed one of two Go/No Go Association Tasks and provided basic demographics in a randomized order. All data was managed and collected through Qualtrics in an anonymous protocol. No IP addresses or geolocation information was collected. Following completion of all study items, participants could elect to complete a second survey, not tied in any way to the first, in which they provided their contact info to be eligible for a $100 department store gift card.
Go/No Go Association Task.
Administration of the Go/No Go Association Task (GNAT; Nosek & Banaji, 2001) began with four practice blocks to orient participants to the tasks, followed by the scored trial tasks which consisted of two practice and two evaluated blocks each. Each scored trial task appeared in partially randomized order and measured automatic attitudes (i.e. implicit bias) of both evaluative categories (e.g., good or bad) towards a stigmatizing word (e.g. substance abuser [trial 1] or addict [trial 2]) and non-stigmatizing word (e.g. person with a substance use disorder for both scored trial tasks). Following the procedure outlined by Nosek and Banaji (2001), the response deadline for the practice blocks was 1000 milliseconds (ms), and the evaluated blocks used response deadlines of 750 ms first and 600 ms second. Each practice block consisted of 20 practice activities, while evaluated blocks began with 16 practice activities, followed by 60 test activities that were used in final analysis.
Measures
Implicit Bias Measurement.
The GNAT trials administered in this study were a modified version of the GNAT designed by Nosek and Banaji (2001) for the Millisecond Inquisit web application. The GNAT requires classification of two objective categories (e.g. “Substance Abuser” and “Person with a Substance Use Disorder”) with two evaluative categories (e.g. “Good” and “Bad”) via a computer software application. For the current study, 2 different GNATs were used; 1) substance abuser and person with a substance use disorder, and 2) addict and person with a substance use disorder.
Scoring of the GNATs was done using the d-prime (d’) method described by Nosek and Banaji (2001), originally defined by Green and Swets (1966). The method calculates sensitivity, indexed by d’, by converting the proportion of correct responses for signal items and incorrect responses for noise items into z-scores and then calculating the difference between the z-score values. Values of d’ are standardized with scores further away from 0 representing progressively stronger associations than scores closer to 0. Values of d’ at 0 or below (negative) indicate that participants were either not performing the task as instructed or were unable to correctly identify signal items from noise items. As such, test blocks meeting these criteria (scores of 0 or below; 4% of participants in the current study) were removed from final analysis. Participants not included in the final GNAT analysis did not differ from those that were included on any demographic variable.
Recovery Status.
Recovery status was defined as participant response to a single self-report question, “Do you identify as a person in recovery from a substance use disorder?”. The question was dichotomous with participants able to select “Yes” (=1) or “No” (=0). This operationalization of recovery is consistent with previous work using a participant reported status using their own definitional parameters of recovery (White & Kurtz, 2005; White, Malinowski Weingartner, Levine, Evans, & Lamb, 2013; Kelly, Bergman, Hoeppner, Vilsaint, & White, 2017), which may be more salient as a single, consensus definition of recovery does not exist (Ashford et al., 2018). This method allows for individuals of various recovery pathways (including 12-step and other mutual aid abstinence based, moderation management and harm reduction, pharmacotherapy, and others) to be included in the milieu.
Employment Type.
Participants who reported they were currently employed were asked to provide an open-ended response to the question, “Please describe your current employment in your own words”. Open-ended responses were manually recoded as a dichotomous variable (1 = health professional, 0 = not a health professional) by two research team members (AA, AB) following definitions and description of health professionals lain out by the World Health Organization ((World Health Organization, 2013).
Analysis
All data analysis was completed via IBM SPSS V.24. Statistical significance for all tests was defined a priori at .05, with all multiple comparisons using the Sidak correction method. Analysis of the GNAT d’ prime scores was completed for each word pair, with recovery status and employment type as covariates, using a mixed-design ANOVA. Each mixed ANOVA was designed with four levels of the DV (term + evaluative category [good/bad]) measured at one-time interval, and two potential covariates (recovery status [yes/no] and employment type [health professional or other professional]). For each of the conducted analyses, covariates were limited to either recovery status or employment type, not both, in the same iteration of mixed ANOVA. Each level of the DV was measured via the GNAT, with each level representing either the stigmatizing term evaluated towards good and bad, or the non-stigmatizing word evaluated towards good and bad. In mixed ANOVA instances where the sphericity assumption was violated (using Mauchly’s test of sphericity), Greenhouse-Geisser adjusted results are provided.
Results
Participants
Participants had a mean age of 46.29 years (SD = 15.19), with the majority identifying as female (n = 225 / 75.3%), white (n = 271 / 90.6%), and either married or in a domestic partnership (n = 155 / 51.8%). Many participants had either a post-graduate degree (n = 135 / 45.2%) or a 4-year degree (n = 103 / 34.4%), were employed (n = 210 / 70.2%), and had a last year income over $50,000 (n = 200 / 66.9%). Less than a third of participants were in recovery (n = 87 / 29.1%) or were employed as health professionals (n = 63 / 21.1%). Full participant demographics are available in Table 1.
Table 1.
Combined Participant Demographic Characteristics
| (N = 299) |
||
|---|---|---|
| N | (%) | |
| Age (years) | ||
| M = 46.29, SD = 15.19 | ||
| Gender | ||
| Male | 74 | (24.7) |
| Female | 225 | (75.3) |
| Race / Ethnicity | ||
| White | 271 | (90.6) |
| Other | 28 | (9.4) |
| Marital Status | ||
| Single | 144 | (48.2) |
| Married / Domestic | 155 | (51.8) |
| Partnership | ||
| Education Level | ||
| Associates Degree or less | 61 | (20.4) |
| 4-year degree | 103 | (34.4) |
| Post-graduate degree | 135 | (45.2) |
| Employment Status | ||
| Employed | 210 | (70.2) |
| Unemployed | 89 | (29.8) |
| Household Income | ||
| Less than $10,000 | 11 | (3.7) |
| $10–29,999 | 40 | (13.4) |
| $30–49,999 | 48 | (16.1) |
| Over $50,000 | 200 | (66.9) |
| Recovery Status | ||
| In Recovery | 87 | (29.1) |
| Employment Type | ||
| Health Professional | 63 | (21.1) |
Recovery Status
Descriptive results for all groups d’ scores are available in Table 2.
Table 2.
d-prime positive and negative association scores by label and group
| Group | Label | Positive Association MS (SD) | Negative Association MS (SD) |
|---|---|---|---|
| In Recovery | |||
| Trial 1 (n = 51) | Substance Use Disorder | 1.26 (0.95) | 1.79 (1.19) |
| Trial 1 | Substance Abuser | 1.20 (0.92) | 2.03 (1.13) |
| Trial 2 (n = 36) | Addict | 1.34 (.85) | 2.58 (1.45) |
| Trial 2 | Substance Use Disorder | 1.52 (1.01) | 1.96 (0.66) |
| Not in Recovery | |||
| Trial 1 (n = 102) | Substance Use Disorder | 1.37 (1.00) | 1.90 (1.03) |
| Trial 1 | Substance Abuser | 1.23 (0.94) | 2.24 (1.21) |
| Trial 2 (n = 110) | Addict | 1.66 (0.98) | 2.33 (1.16) |
| Trial 2 | Substance Use Disorder | 1.61 (0.83) | 2.10 (0.79) |
| Health Professional | |||
| Trial 1 (n = 32) | Substance Use Disorder | 1.53 (0.98) | 1.98 (0.88) |
| Trial 1 | Substance Abuser | 1.63 (0.99) | 2.51 (1.43) |
| Trial 2 (n = 31) | Addict | 1.58 (0.73) | 2.75 (1.46) |
| Trial 2 | Substance Use Disorder | 1.63 (0.74) | 2.07 (0.65) |
| Other Professional | |||
| Trial 1 (n = 121) | Substance Use Disorder | 1.29 (0.98) | 1.83 (1.13) |
| Trial 1 | Substance Abuser | 1.11 (0.89) | 2.08 (1.09) |
| Trial 2 (n = 115) | Addict | 1.56 (1.01) | 2.30 (1.16) |
| Trial 2 | Substance Use Disorder | 1.57 (0.91) | 2.06 (0.80) |
MS = d-prime Mean Score, SD = d-prime Standard Deviation
Addict and SUD.
The results of the mixed ANOVA showed that there was no significant main effect of participant recovery status (F(1, 144) = .29, p = .589, ηp2 = .002) on d-prime scores. There was, however, a significant main effect of linguistic choice on d-prime scores (F(2.499, 359.891) = 46.96, p < .001, ηp2 = .215), with participants having the largest d-prime scores for addict + bad (M = 2.456), followed by SUD + bad (M = 2.034), SUD + good (M = 1.563), and addict + good (M = 1.501).
Additionally, results showed there was also a significant interaction between participant recovery status and linguistic choice (F(2.499, 359.891) = 2.76, p = .050, ηp2 = .019). Descriptive statistics showed that while participants not in recovery had stronger associations than participants in recovery with most linguistic choices (addict + good M = 1.66; SUD + good M = 1.61, SUD + bad M = 2.10), that participants in recovery had stronger associations than participants not in recovery for addict + bad (M = 2.58). Figure 1 shows this interaction effect of recovery status and d-prime scores.
Figure 1.
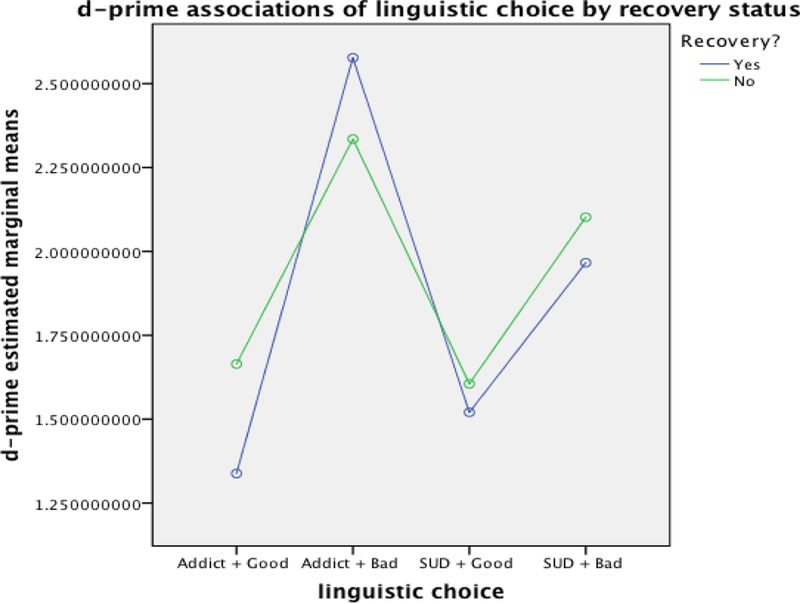
Effects of Recovery Status and Linguistic Choice on Automatic Associations
Abuse and SUD.
The results of the Mixed ANOVA showed that there was no significant main effect of participant recovery status (F(1, 151) = .65, p = .423, ηp2 = .004) on d-prime scores. There was, however, a significant main effect of linguistic choice on d-prime scores (F(2.702, 408.061) = 46.96, p < .001, ηp2 = .237), with participants having the largest d-prime scores for substance abuse + bad (M = 2.134), followed by SUD + bad (M = 1.845), SUD + good (M = 1.318), and substance abuse + good (M = 1.216). Additionally, results showed there was no significant interaction between participant recovery status and linguistic choice (F(2.702, 408.061) = .304, p = .304, ηp2 = .002).
Employment Type
Abuse and SUD.
The results of the mixed ANOVA showed that there was a significant main effect of participant job type (i.e. health professional or not a health professional), (F(1, 151) = 4.18, p = .027, ηp2 = .027) on d-prime scores. As seen in Figure 2, health professional participants had stronger associations than non-health professional participants for all linguistic choices, with mean differences of .511 for substance abuse + good, .431 for substance abuse + bad, .248 for SUD + good, and .145 for SUD + bad. Post hoc independent samples t-tests also showed that only for substance abuse + good were the differences statistically significant (T (151) = 2.82, p = .005 (95% CI, .153, .869), with health professional participants having on average .511 higher d-prime scores than non-health professional participants.
Figure 2.
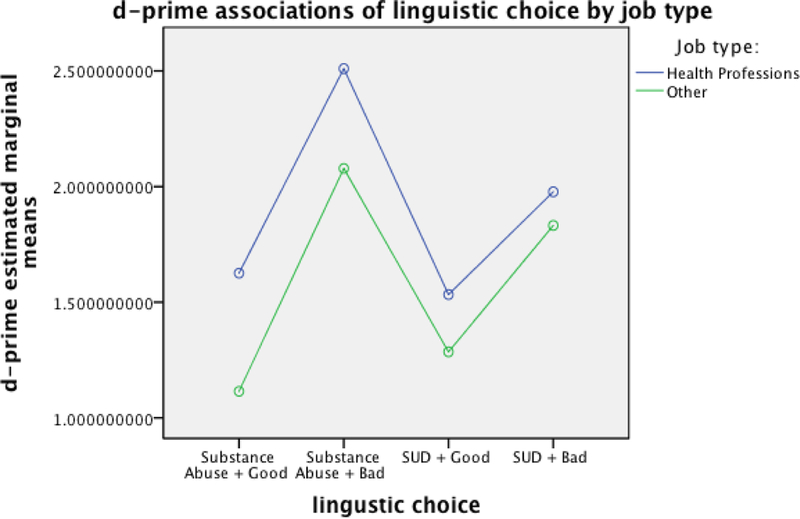
Effects of Employment Type and Linguistic Choice on Automatic Attitudes
There was also a significant main effect of linguistic choice on d-prime scores (F(2.701, 407.882) = 35.87, p < .001, ηp2 = .192), with participants having the largest d-prime scores for substance abuse + bad (M = 2.294), followed by SUD + bad (M = 1.905), SUD + good (M = 1.409), and substance abuse + good (M = 1.370). Additionally, results showed there was no significant interaction between participant job type and linguistic choice (F(2.702, 408.061) = 1.29, p = .277, ηp2 = .008).
Addict and SUD.
The results of the Mixed ANOVA showed that there was no significant main effect of participant job type (i.e. health professional or not a health professional) (F(1, 144) = .73, p = .395, ηp2 = .005) on d-prime scores.
There was, however, a significant main effect of linguistic choice on d-prime scores (F(2.492, 358.867) = 35.52, p < .001, ηp2 = .198), with participants having the largest d-prime scores for addict + bad (M = 2.525), followed by SUD + bad (M = 2.068), SUD + good (M = 1.602), and addict + good (M = 1.582). Additionally, results showed there was no significant interaction between participant job type and linguistic choice (F(2.492, 358.867) = 2.15, p = .106, ηp2 = .015).
Discussion
The labels used to describe individuals with a SUD have consistently been associated with implicit and explicit bias (Barry et al., 2015; Kelly et al., 2010; Kelly & Westerhoff, 2010; McGinty et al., 2015; van Boekel et al., 2013). However, the relationship between bias magnitude and either the recovery status or employment type of an individual has to date been unexamined (Authors, 2018b, 2018c; van Boekel et al., 2013). Results from the current study suggest that both an individual’s recovery status and employment as a health professional does have an effect on the magnitude of the implicit bias elicited when presented with the previously identified stigmatizing terms “substance abuser” and “addict” (Authors; 2018a, 2018b, 2018c; Kelly et al., 2010; Kelly & Westerhoff, 2010), though the type of effect varies. Our first hypothesis, that individuals in recovery would have lower negative associations with the terms “addict” and “substance abuser” was rejected. For individuals in recovery, both the label (“addict” versus “person with a SUD”) and the interaction of recovery status and label, are associated factors. Descriptive results suggest that participants in recovery had similar association strength as participants not in recovery towards the labels tested. However, while most associations for participants in recovery were on average less than participants not in recovery, the level of the negative association with “addict” was found to be greater, not lower as hypothesized.
Previously, we had considered that individuals in recovery, especially those utilizing a 12-step recovery programs, may exhibit less negative association with terms such as “addict” due to the use of the term as an identity reformation tool and sense of catharsis (Authors et al., 2018b; 2018c). While the reasons (e.g. identity reformation or catharsis) for the use of the term “addict” by individuals in recovery may still be true and should be explored, the overall benefits of such usage even by those in recovery may be mitigated by the negative associations elicited, as shown in the results of this study. It may be of greater importance to determine the role of negative associations in identity reformation and catharsis, particularly with a disorder that involves high degrees of self-deception, denial, and blame, such as SUD. This may be particularly true of 12-step members who often adopt such labels as a form of self-truth or honesty as a means of counterbalancing against self-deception (Ferrari, Groh, Rulka, Jason, & Davis, 2008). Thus, negative associations do not necessarily translate to negative effects for the individual if the negativity serves an identity function and is a plausible divergent explanation for our results.
While it is likely that many of the individuals in recovery in our sample were members of 12-step recovery programs, as it is the most prominent in the United States (Kelly et al., 2017), it is also possible that given our operationalization of recovery (i.e., self-identification by the participant) that the sample was made up of those from other recovery pathways. However, a much more plausible explanation is that those in any form of recovery have strong negative associations with terms such as “addict” and “substance abuser”, similar to those in the general population (Authors, 2018b).
We must also consider social identity classification, a process of signifying similarities and differences to others in efforts to garner respectability among categorical ingroups, as a potential explanation of these results. Even negatively associated identities may create ingroup bonding and shared meaning (Copes, Hochstetler, & Williams, 2008). Identifying as an “ex-con” for example, may not elicit positive associations, but may garner respect and function as a means of rapport building within certain groups (Goffman, 1963; Hirschfield & Piquero, 2010 ). Face-value positive and negative association research may create a misleading binary which overlooks role, commitment, and identity salience and the conceptualization of the self within social contexts (Stryker & Serpe, 1982). Therefore, we maintain, as previously stated, that individuals in recovery should retain the autonomy to self-identify however they choose. The interpretation of the current results should be used to inform the decision about what labels to use to self-identify, not as a specific guideline for those holding a recovery status.
Our second hypothesis, that individuals employed as health professionals, would have greater negative associations with the terms “addict” and “substance abuser” was partially confirmed. For those employed in the health professions, label choice is perhaps more critical and firm suggestions of label usage can follow from the results here and previously presented (Kelly & Westerhoff, 2010; van Boekel et al., 2013). Health professionals are often a first point of contact for individuals with a SUD, and previous research has suggested that the level of bias held by health professionals is high (van Boekel et al., 2013). Compared to participants not employed in the health professions, those in this study had descriptively, but not statistically significant, greater levels of implicit bias when presented with the label “addict” versus “person with a SUD”. However, when presented with the label “substance abuser” versus “person with a SUD”, the employment type of participants had a significant main effect on levels of bias. Descriptively, health professional participants had greater negative and positive associations than participants that are not health professionals. As a vital component of the SUD treatment system, and often the only resource individuals with a SUD will be able to access, it is critical that health professionals take all steps necessary to reduce the potential for stigma and negative bias. This should include not only the removal of the term “substance abuser” from common jargon and discourse (both with other professionals and with patients), but also in any medical charts (Goddu et al., 2018), diagnostic reports (Goddu et al., 2018), and in professional health communication materials (Authors, 2018b).
We believe the right to autonomy that should be afforded to individuals in recovery to self-identify however they choose, does not extend to health professionals at any level. The responsibility for effective and non-stigmatizing language should be considered a high priority for the health professions. We recommend that SUD language directives from national organizations such as the American Society of Addiction Medicine (ASAM; American Society of Addiction Medicine, 2014) not only be adhered to, but also perhaps adopted by individual healthcare systems and regional associations to improve the potential to mitigate elicited bias from language in all medical settings. Additionally, in light of the success of previous campaigns to reduce public bias (Clement et al., 2013; Dumesnil & Verger, 2009; Livingston, Milne, Fang, & Amari, 2012; Luty, Rao, Arokiadass, Easow, & Sarkhel, 2008), efforts to address stigma and raise public awareness may benefit from actively considering linguistic choices as outlined in this study. Progress in how SUD is discussed has the potential to impact how people with SUD are treated, and thereby, how they recover.
Limitations
The study’s findings should be viewed in light of several limitations. While recruitment through Research Match provided certain strengths, it also resulted in an oversampling of white, female participants, limiting external validity. This is a known limitation of the volunteer participant pool enrolled at Research Match, and future study should strive to recruit a more representative sample. Additionally, without collecting the primary pathway of recovery (e.g. 12-step mutual aid, use of medication, natural, etc.) of participants, the utility and generalizability of the results of participants in recovery is limited. While it is common for individuals in recovery to self-label as “addicts” for example, the rate at which this happens outside of 12-step mutual aid organizations is unknown. It is also unknown if the potential benefits of using such a label extend to individuals outside of the respective fellowships. Future replication studies should collect recovery pathway so as to answer this question with more detail and rigor. More representative sampling derived from groups, environments, or contexts in which labels such as “addict” are a known self-identifier (such as Narcotics Anonymous) may help provide more detailed and population-specific conclusions.
Future Research
While many research questions and hypotheses regarding language used in the SUD field have been answered in the last 10 years, many still remain. From the current findings, future research should identify both the real and perceived benefits and harms of using stigmatizing labels by individuals in recovery. This study should also compare these benefits and harms as they vary across different types of recovery programs and pathways, and by demographic characteristics such as gender, race/ethnicity, age, etc. Similarly, the differences in explicit bias elicited from certain labels should be explored by individual recovery status and employment type. Particularly helpful to the future of study on this topic would be the examination of compounding or moderating effects of concurrently held identities or roles – such as being an individual in recovery working in the health professions, or as an individual in recovery and a policy maker. It is possible that such duality could elicit a synergistic effect, increasing the magnitude of bias, or perhaps serve as a moderator, minimizing the magnitude of bias.
SUD-related stigma and language researchers should also begin to conduct experimental studies concerned with the development of health communication materials (i.e. public health campaigns, marketing materials, etc.) that use non-stigmatizing language in an effort to decrease levels of stigma. While language that elicits SUD-related stigma and bias has been identified, the amount and direction of change in stigma and bias through language shifts is not yet known.
Conclusion
The labels that are often used to identify and describe individuals with a SUD or in recovery can often be stigmatizing. Terms such as “addict’ and “substance abuser” are also associated with greater levels of bias among individuals in recovery and health professionals. While those in recovery deserve the right to autonomy to self-identify with any label, it is important that those in recovery realize that words commonly held as a source of power, such as addict, are more negatively associated among individuals in the recovery community. However, the way in which such negative associations interplay with identity dynamics and ingroup cohesion is still unknown. Health professionals, having greater levels of negative association with stigmatizing terms, should commit to improving their linguistic choices in all manner of communication.
Acknowledgements:
The authors would like to thank J. Kelly, S. Wakeman, and A. Ashford for their previous research endeavors and assistance with the current study.
Funding: This work was supported by NIDA [grant number R01DA039457].
Footnotes
COI: The authors report not conflicts of interest.
References
- American Society of Addiction Medicine. (2014). The standard of care for the addiction specialist physician. Chevy Chase, MD: American Society of Addiction Medicine. [Google Scholar]
- Ashford RD, Brown A, Brown T, Callis J, Cleveland HH, Eisenhart E, ... Whitney J (In Press). Defining and Operationalizing the Phenomena of Recovery: A Working Definition from the Recovery Science Research Collaborative. Addiction Research and Theory 10.1080/16066359.2018.1515352 [DOI] [Google Scholar]
- Barry CL, McGinty EE, Pescosolido BA, & Goldman HH (2014). Stigma, discrimination, treatment effectiveness, and policy: Public views about drug addiction and mental illness. Psychiatric Services, 65, 1269–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement S, Lassman F, Barley E, Evans-Lacko S, Williams P, Yamaguchi S, ... Thornicroft G (2013). Mass media interventions for reducing mental health-related stigma. The Cochrane Database of Systematic Reviews, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement S Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, … Thornicroft G (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45, 11–27. [DOI] [PubMed] [Google Scholar]
- Copes H, Hochstetler A, & Williams JP (2008). “We weren’t like no regular dope fiends”: Negotiating hustler and crackhead identities. Social Problems, 55, 254–270. [Google Scholar]
- Dumesnil H, & Verger P (2009). Public awareness campaigns about depression and suicide: A review. Psychiatric Services, 60, 1203–1213. doi: 10.1176/ps.2009.60.9.1203 [DOI] [PubMed] [Google Scholar]
- Ferrari JR, Groh DR, Rulka G, Jason LA, & Davis MI (2008). Coming to terms with reality: Predictors of self-deception within substance abuse recovery. Addictive Disorders & Their Treatment, 7, 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E (1963). Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Green DM, & Swets JA (1966). Signal detection theory and psychophysics. Oxford, England: John Wiley. [Google Scholar]
- Greenwald AG, & Krieger LH (2006). Implicit bias: Scientific foundations. California Law Review, 94 945–967. [Google Scholar]
- Goddu A,P, O’Conor KJ, Lanzkron S, Saheed MO, Saha S, Peek ME, … Beach MC (2018). Do Words Matter? Stigmatizing Language and the Transmission of Bias in the Medical Record. Journal of General Internal Medicine, 33(5), 685–691. 10.1007/s11606-017-4289-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfield PJ, & Piquero AR (2010). Normalization and legitimation: Modeling stigmatizing attitudes toward ex‐offenders. Criminology: An Interdisciplinary Journal, 48(1), 27–55. 10.1111/j.1745-9125.2010.00179.x [DOI] [Google Scholar]
- Hughes K (2007). Migrating identities: The relational constitution of drug use and addiction. Sociology of Health & Illness, 29, 673–691. doi: 10.1111/j.1467-9566.2007.01018.x [DOI] [PubMed] [Google Scholar]
- Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, & White WL (2017). Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug and Alcohol Dependence, 181, 162–169. 10.1016/j.drugalcdep.2017.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Dow SJ, & Westerhoff C (2010). Does our choice of substance-related terms influence perceptions of treatment need? An empirical investigation with two commonly used terms. Journal of Drug Issues, 40, 805–818. 10.1177/002204261004000403 [DOI] [Google Scholar]
- Kelly JF, & Westerhoff CM (2010). Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. International Journal of Drug Policy, 21(3), 202–207. doi: 10.1016/j.drugpo.2009.10.010 [DOI] [PubMed] [Google Scholar]
- Link BG, & Phelan JC (2001). Conceptualizing stigma. Annual Review of Sociology, 27, 363–385. [Google Scholar]
- Livingston JD, Milne T, Fang ML, & Amari E (2012). The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction, 107(1), 39–50. doi: 10.1111/j.1360-0443.2011.03601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Kohlenberg BS, Hayes SC, Bunting K, & Rye AK (2008). Reducing self-stigma in substance abuse through acceptance and commitment therapy: Model, manual development, and pilot outcomes. Addiction Research & Theory, 16(2), 149–165. 10.1080/16066350701850295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoma JB, Kulesza M, Hayes SC, Kohlenberg B, & Larimer M (2014). Stigma predicts residential treatment length for substance use disorder. The American Journal of Drug and Alcohol Abuse, 40(3), 206–212. 10.3109/00952990.2014.901337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luty J, Rao H, Arokiadass SMR, Easow JM, & Sarkhel A (2008). The repentant sinner: Methods to reduce stigmatised attitudes towards mental illness. Psychiatric Bulletin, 32(9), 327–332. 10.1192/pb.bp.107.018457 [DOI] [Google Scholar]
- McGinty EE, Goldman HH, Pescosolido B, & Barry CL (2015). Portraying mental illness and drug addiction as treatable health conditions: Effects of a randomized experiment on stigma and discrimination. Social Science & Medicine, 126, 73–85. 10.1016/j.socscimed.2014.12.010 [DOI] [PubMed] [Google Scholar]
- McIntosh J, & McKeganey N (2001). Identity and recovery from dependent drug use: The addict’s perspective. Drugs: Education, Prevention, and Policy, 8(1), 47–59. [Google Scholar]
- Nosek BA, & Banaji MR (2001). The go/no-go association task. Social Cognition, 19, 625–664. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Stryker S, & Serpe RT (1982). Commitment, identity salience, and role behavior: Theory and research example In Ickes W & Knowles ES (Eds.), Personality, roles, and social behavior (pp. 199–218). New York, NY: Springer. [Google Scholar]
- van Boekel LC, Brouwers EP, van Weeghel J, & Garretsen HF (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug & Alcohol Dependence, 131(1), 23–35. [DOI] [PubMed] [Google Scholar]
- White W, & Kurtz E (2005). The varieties of recovery experience: A primer for addiction treatment professionals and recovery advocates. International Journal of Self Help and Self Care, 21–61. [Google Scholar]
- White WL, Malinowski Weingartner R, Levine M, Evans AC, & Lamb R (2013). Recovery Prevalence and Health Profile of People in Recovery: Results of a Southeastern Pennsylvania Survey on the Resolution of Alcohol and Other Drug Problems. Journal of Psychoactive Drugs, 45(4), 287–296. 10.1080/02791072.2013.825031 [DOI] [PubMed] [Google Scholar]
- World Health Organization; (2013). Transforming and scaling up health professionals’ education and training: World Health Organization guidelines 2013 Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK298953/ [PubMed] [Google Scholar]


