Abstract
Objective:
To describe presenting clinical features and surgical techniques that are associated with successful surgical repair of pediatric rhegmatogenous retinal detachment (RRD).
Design:
Retrospective interventional case series.
Subjects:
212 eyes of 191 patients, aged 0–18 years, undergoing surgical repair for RRD between 2001 and 2015 with a minimum follow up of 3 months.
Methods:
Patients were divided into three age groups (0–6 years, 7–12 years, 13–18 years) and comparisons were made using bivariate and multivariable generalized estimating equation models. A mixed means model was used to examine visual acuity in each age group over time.
Main Outcome Measures:
Complete reattachment of the retina at final follow up.
Results:
Of a total of 212 eyes, 166 (78%) achieved total reattachment at final follow up. Mean follow up was 36.3 months. RRD associated with Stickler syndrome was more likely to occur in the younger cohorts (odds ratio [OR] 0.45, 95 % confidence interval [CI] 0.22 – 0.91), while RRD associated with blunt trauma was more likely to occur in the oldest cohort (OR 2.3, 95% CI 1.2–4.4). Subtotal RRD was more likely to be successfully repaired than total RRD (OR 3.6, 95% CI 1.5 – 8.4, p = 0.0100), and eyes with previous vitreoretinal surgery were less likely to have successful repair (OR 0.30, 95% CI 0.12 – 0.78, p = 0.0258). There was no significant difference between age groups in the rate of surgical success (p = 0.55). There was a significantly higher success rate with primary scleral buckle (SB) (63%, OR 2.2, 95% CI 1.1–4.5) and combined scleral buckle/vitrectomy (SB/PPV) (68%, OR 2.3 95% CI 1.1–5.1) compared to vitrectomy (PPV) alone (51%).
Conclusions:
Most pediatric patients with RRD achieved complete reattachment with surgery. Success was more common in patients with a subtotal RRD at presentation. Previous vitreoretinal surgery was a risk factor for failure. Younger patients were more likely to present with RRD involving the macula but there was no difference between age groups in successful reattachment at final follow up. Primary PPV had a lower rate of success than SB or combined SB/PPV.
PRECIS
We identified differences between younger and older children for etiology, symptoms, and vision outcomes. No difference in rate of successful repair was identified based on age, but other factors did predict success including lower success with primary vitrectomy.
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) in children is a distinct and challenging condition to treat. Compared with adult RRD, pediatric detachments tend to present late, and subsequent management is often complicated by proliferative vitreoretinopathy (PVR) and lower rates of primary reattachment after a single operation.1, 2 Additional challenges are posed by systemic comorbidities (prematurity, connective tissue disorders), poor cooperation for examinations, difficulty with postoperative positioning, bilateral detachments, and a relatively high rate of trauma.1, 3, 4 Despite the difficulty in managing these cases, successful reattachment of the retina is possible in the majority of cases.
Previous reviews of pediatric RRD provide useful insight into the anatomic and clinical features of this disease, but the largest of these series were done before the era of modern vitrectomy techniques.5, 6 Because of the complexity of these cases and the evolution of surgical approaches, we chose to review our surgical outcomes. Herein we analyze surgical outcomes for a large group of patients managed at a single institution over a period of 14 years to identify factors predictive of successful surgical repair.
PATIENTS AND METHODS
We retrospectively reviewed medical records of pediatric patients (aged 0–18 years) who underwent surgery for RRD at Emory University Hospital, the Emory Eye Center, or Children’s Healthcare of Atlanta between January 1, 2001 and September 21, 2015. This study was approved by the institutional review board at Emory University. Patients with tractional or exudative retinal detachments were excluded. At least three months’ follow up was required for inclusion. Prior to beginning the study, approval to proceed was obtained through the institutional review board. This study complied with the Health Insurance Portability and Accountability Act (HIPPA) and adhered to the tenets of the Declaration of Helsinki.
Charts were reviewed and the following information extracted: age, gender, dates of presentation and follow up, family history of RRD, symptoms, duration of symptoms, previous intraocular surgery, and previous RRD in the fellow eye. Specific risk factors for RRD were recorded, including Stickler syndrome, Marfan syndrome, high myopia, prematurity with or without known retinopathy of prematurity (ROP), familial exudative vitreoretinopathy (FEVR), and blunt or penetrating ocular trauma. Examination findings were recorded, including visual acuity at presentation and at each follow up visit, lens status, presence and extent of retinal detachment, type and location of retinal breaks, presence and grade of PVR, and fundus findings in the fellow eye. Follow up information was recorded after each operation at 1 month, 3 months, 6 months, 1 year, and at the latest follow up. For each follow up, visual acuity (VA), status of the retina, and postoperative complications were recorded. Not all eyes had examinations in our office at each of these specified time points. Some of the post-operative visits for some patients were performed by their local referring ophthalmologist and these data are not included. Among those who were seen by us at any given time point, not all had VA measurements. Some of the examinations were performed under anesthesia and no VA data were obtained. Also, in some cases the children would not cooperate for VA testing. Surgical success was defined as complete reattachment of the retina with one or more operations at the latest follow up.
Descriptive statistics (frequencies and percentages for categorical data and means and standard deviations for continuous data) were calculated per eye for the presenting features and the type of surgery. To explore relationships between age, presenting features, and outcomes, patients were divided into 3 age groups: 0–6 years, 7–12 years, and 13–18 years. The relationships between age groups and each of the presenting features were tested with bivariate general estimating equation (GEE) models to control for the correlation between the eyes of the patients. The influence of presenting features on surgical success was also tested using the same methodology. Adjusted odds ratios and 95% confidence intervals were calculated. A multivariable, GEE model using an exchangeable correlation matrix was constructed to examine the relationship of surgical success and age group controlling for the following presenting features: blunt trauma, penetrating trauma, previous cataract or glaucoma surgery, previous retinal surgery, subtotal retinal detachment (RD), PVR Grade C, dialysis, giant retinal tear, Stickler syndrome, and high myopia.
The secondary outcome, visual acuity, was converted to logarithm of the minimum angle of resolution (logMAR) equivalents (when possible), and descriptively examined at all available follow-up time points in the first year for all those with surgical success. Some visual acuity measurements were not convertible to logMAR. In our study, these included LP, NLP, central-steady-maintained (CSM), fix and follow (FF), and blink to light (BTL) measurements. The percentage of patients with a visual acuity of 20/40 or better, as well as the percentage who improved, remained the same, and worsened were calculated for those with surgical success. The repeated measures analysis of logMAR visual acuity was performed with a means model in SAS version 9.4 (PROC MIXED, mixed linear models) with three predictors: time on study (baseline, 1 month, 3 months, 6 months, 12 months), age group, and the interactions with time and age group. A compound symmetric variance covariance was assumed for each outcome, and robust estimates of the standard errors of parameters were used to perform statistical tests and construct 95% confidence intervals. The model-based means are unbiased with unbalanced and missing data, assuming that the missing data are noninformative.
RESULTS
A computerized search of billing records identified 246 pediatric patients with RRD. Of these, 22 were excluded due to miscoding of diagnosis, 11 were deemed to be inoperable at the initial evaluation, and 22 had inadequate follow-up, leaving 212 eyes of 191 patients included for review. The median age was 10.5 ± 5.29 years. Forty-seven (25%) patients were female and 144 (75%) were male. Bilateral detachments at presentation were seen in 21 patients (10%). Surgical repair resulting in total reattachment of the retina at final follow up occurred in 166/212 (78%) of eyes. The mean number of operations per eye was 1.34. Mean follow up was 36.3 months (interquartile range 12.9 months – 53.7 months).
Table 1 shows demographic and clinical features at first presentation, divided by age group. RRD associated with Stickler syndrome was more prevalent in children under 13 years (odds ratio [OR] 0.45, (95% confidence interval [CI] 0.22–0.91), as was RRD in patients with a history of treated ROP (OR 0.26, 95% CI 0.11–0.62). Blunt trauma was a significantly more common cause of RRD in the oldest cohort of patients (OR 2.25, 95% CI 1.15–4.42). Symptoms reported by the parent were more common in the youngest cohort, while symptoms reported by the child were more common in the oldest cohort. RRD with the macula attached at presentation was more common in the oldest cohort compared to the younger ones.
Table 1.
Clinical Factors by Age Group
| Overall (n=212 eyes) | Age 0–6 (n=57 eyes) | Age 7–12 (n=56 eyes) | Age 13–18 (n=99 eyes) | Odds ratio (95% CI) | p-value | |||
|---|---|---|---|---|---|---|---|---|
| Eye with RRD | Right eye | 114/212 (54%) | 33/57 (58%) | 33/56 (59%) | 48/99 (48%) | -- | ||
| Left eye | 97/212 (46%) | 24/57 (42%) | 23/56 (41%) | 51/99 (52%) | 0.71 (0.45, 1.1) | 0.15 | ||
| Sex | Female | 53/212 (25%) | 17/57 (30%) | 16/56 (29%) | 20/99 (20%) | 0.65 (0.36, 1.2) | 0.17 | |
| Male | 159/212 (75%) | 40/57 (70%) | 40/56 (71%) | 79/99 (80%) | -- | |||
| Predisposing factor | ||||||||
| Stickler syndrome | 39/212 (18%) | 14/57 (25%) | 15/56 (27%) | 10/99 (10%) | 0.45 (0.22, 0.91) | 0.021 | ||
| Marfan syndrome | 7/212 (3%) | 2/57 (4%) | 3/56 (5%) | 2/99 (2%) | 0.64 (0.14, 2.8) | 0.55 | ||
| Myopia | 71/212 (33%) | 17/57 (30%) | 21/56 (38%) | 33/99 (33%) | 1.1 (0.60, 2.0) | 0.81 | ||
| History of treated ROP | 18/212 (8%) | 9/57 (16%) | 7/56 (13%) | 2/99 (2%) | 0.26 (0.11, 0.62) | 0.0026 | ||
| Prematurity without treated ROP | 10/212 (5%) | 1/57 (2%) | 1/56 (2%) | 8/99 (8%) | 4.7 (0.93, 24) | 0.06 | ||
| FEVR | 5/212 (2%) | 2/57 (4%) | 2/56 (4%) | 1/99 (1%) | 0.43 (0.095, 1.9) | 0.26 | ||
| Penetrating trauma | 32/212 (15%) | 7/57 (12%) | 9/56 (16%) | 16/99 (16%) | 1.2 (0.61, 2.5) | 0.56 | ||
| Blunt trauma | 46/212 (22%) | 8/57 (14%) | 9/56 (16%) | 29/99 (29%) | 2.3 (1.2, 4.4) | 0.019 | ||
| Previous cataract or glaucoma surgery | 39/212 (18%) | 7/57 (12%) | 10/56 (18%) | 15/99 (15%) | 1.0 (0.51, 2.0) | 0.95 | ||
| Previous retinal surgery | 29/212 (14%) | 9/57 (16%) | 6/56 (11%) | 14/99 (14%) | 0.96 (0.44, 2.1) | 0.91 | ||
| Family history of RRD | 34/191 (18%) | 9/57 (16%) | 9/56 (16%) | 16/99 (16%) | 1.0 (0.46, 2.2) | 0.96 | ||
| Symptoms from child | 112/212 (53%) | 12/57 (21%) | 29/56 (52%) | 71/99 (72%) | 5.2 (2.9, 9.2) | <0.0001 | ||
| Symptoms from parent | 31/212 (15%) | 19/57 (33%) | 8/56 (14%) | 4/99 (4%) | 0.16 (0.067, 0.38) | <0.0001 | ||
| Weeks of symptoms | 7.3 (16.7), (n=138) | 10.8 (30.14), (n=28) | 7.0 (12.1), (n=36) | 6.1 (10.6), (n=74) | 0.99 (0.97, 1.1) | 0.39 | ||
| Examination findings | ||||||||
| Severity | Macula on | 19/212 (9%) | 2/57 (4%) | 4/56 (7%) | 13/99 (13%) | 3.2 (1.2, 8.6) | 0.045 | |
| Macula off | 64/212 (30%) | 16/57 (28%) | 15/56 (27%) | 33/99 (33%) | 1.4 (0.83, 2.5) | |||
| Total RD | 129/212 (61%) | 39/57 (68%) | 37/56 (66%) | 53/99 (53%) | -- | |||
| PVR Grade C or worse | 84/212 (40%) | 18/57 (32%) | 24/56 (43%) | 42/99 (42%) | 1.4 (0.80, 2.3) | 0.25 | ||
| Retinal dialysis | 37/212 (17%) | 10/57 (18%) | 11/56 (20%) | 16/99 (16%) | 0.90 (0.46, 1.8) | 0.75 | ||
| Giant retinal tear | 30/212 (14%) | 7/57 (12%) | 9/56 (16%) | 14/99 (14%) | 1.1 (1.5, 2.2) | 0.84 | ||
| Mean logMAR VA (std) at baseline and Snellen eq | 1.77 (1.03), (n=137) 20/1178 | 2.00 (0.87), (n=20) 20/2000 | 1.86 (1.00), (n=42) 20/1449 | 1.66 (1.08), (n=75) 20/914 | 0.79 (0.57, 1.09) | 0.15 | ||
| Number with non-logMAR VA at baseline | 44/212 (21%) | 19/57 (33%) | 9/56 (16%) | 16/99 (16%) | 0.48 (0.25, 0.91) | 0.0363 | ||
| Number with no VA at baseline | 31/212 (15%) | 18/57 (32%) | 5/56 (9%) | 8/99 (8%) | 0.24 (0.10, 0.57) | 0.0041 | ||
| Mean follow-up duration in months (std) | 36.3 (31.1), (n=212) | 42.3 (38.3), (n=57) | 35.3 (29.8), (n=56) | 33.4 (26.7), (n=99) | ||||
ROP: retinopathy of prematurity; FEVR: familial exudative vitreoretinopathy; RRD: rhegmatogenous retinal detachment; RD: retinal detachment; PVR: proliferative vitreoretinopathy; CI: confidence int
rval; std: standard deviation; VA: visual acuity; eq: equivalent
Clinical factors associated with successful surgical repair are listed in Table 2. Successful repair was more likely in subtotal RRD. RRD associated with Stickler syndrome, retinal dialysis, and non-syndromic myopia trended toward more successful outcomes but did not reach statistical significance. A multivariable model, shown in Table 3, identifies subtotal RD as a factor predictive of successful repair and identifies previous retinal surgery as predictive of failure (OR 0.30, 95% CI 0.12–0.78). Stickler syndrome again trended toward more successful outcomes but did not reach statistical significance. Age group, Marfan syndrome, history of treated ROP, prematurity without treated ROP, FEVR, penetrating trauma, blunt trauma, previous cataract or glaucoma surgery, family history of RRD, duration of symptoms, PVR grade C or worse, and giant retinal tear were not significantly associated with successful repair.
Table 2.
Clinical Factors Predictive of Successful Retinal Reattachment With 1 Or More Operations
| Overall (n=212) | Surgical success (n=166) | Surgical failure (n=46) | Odds ratio (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| Eye with RRD | Right eye | 114/212 (54%) | 92/166 (55%) | 22/46 (48%) | 1.4 (0.72, 2.6) | 0.35 |
| Left eye | 98/212 (46%) | 74/166 (45%) | 24/46 (52%) | -- | ||
| Sex | Female | 53/212 (25%) | 42/166 (25%) | 11/46 (24%) | 1.1 (0.48, 2.4) | 0.85 |
| Male | 159/212 (75%) | 124/166 (75%) | 35/46 (76%) | -- | ||
| Age group | 0–6 | 57/212 (27%) | 43/166 (26%) | 14/46 (30%) | -- | 0.49 |
| 7–12 | 56/212 (26%) | 47/166 (28%) | 9/46 (20%) | 1.7 (0.63, 4.6) | ||
| 13–18 | 99/212 (47%) | 76/166 (46%) | 23/46 (50%) | 1.1 (0.50, 2.3) | ||
| Predisposing factor | ||||||
| Stickler syndrome | 39/212 (18%) | 35/166 (21%) | 4/46 (9%) | 2.8 (0.77, 10) | 0.12 | |
| Marfan syndrome | 7/212 (3%) | 6/166 (4%) | 1/46 (2%) | 0.65 (0.26, 11) | 0.53 | |
| Myopia | 71/212 (33%) | 61/166 (37%) | 10/46 (22%) | 2.1 (0.93, 4.7) | 0.05 | |
| History of treated ROP | 18/212 (8%) | 16/166 (10%) | 2/46 (4%) | 2.4 (0.51, 10) | 0.18 | |
| Prematurity without treated ROP | 10/212 (5%) | 6/166 (4%) | 4/46 (9%) | 0.39 (0.12, 1.3) | 0.12 | |
| FEVR | 5/212 (2%) | 3/166 (2%) | 2/46 (4%) | 0.40 (0.066, 2.5) | 0.43 | |
| Penetrating trauma | 32/212 (15%) | 22/166 (13%) | 10/46 (22%) | 1.8 (0.24, 1.3) | 0.21 | |
| Blunt trauma | 46/212 (22%) | 39/166 (23%) | 7/46 (15%) | 1.7 (0.71, 4.1) | 0.19 | |
| Previous cataract or glaucoma surgery | 39/212 (18%) | 24/166 (14%) | 15/46 (33%) | 0.49 (0.21, 1.1) | 0.13 | |
| Previous retinal surgery | 29/212 (14%) | 17/166 (10%) | 12/46 (26%) | 0.32 (0.14, 0.74) | 0.02 | |
| Family history of RRD | 34/191 (18%) | 29/166 (17%) | 5/46 (11%) | 1.7 (0.56, 5.4) | 0.27 | |
| Symptoms from child | 112/212 (53%) | 91/166 (55%) | 21/46 (46%) | 1.4 (0.75, 2.8) | 0.28 | |
| Symptoms from parent | 31/212 (15%) | 23/166 (14%) | 8/46 (17%) | 0.76 (0.30, 1.9) | 0.59 | |
| Weeks of symptoms | 7.3 (16.7), (n=138) | 5.1 (5.7), (n=46) | 7.9 (18.5), (n=109) | 1.0 (0.99, 1.0) | 0.19 | |
| Examination findings | ||||||
| Severity | Macula on | 19/212 (9%) | 16/166 (10%) | 3/46 (7%) | 3.9 (1.5, 9.8) | 0.0035 |
| Macula off | 64/212 (30%) | 58/166 (35%) | 6/46 (13%) | 2.1 (0.63, 7.3) | ||
| Total RD | 129/212 (61%) | 92/166 (55%) | 37/46 (80%) | -- | ||
| PVR Grade C or worse | 84/212 (40%) | 65/166 (39%) | 19/46 (41%) | 0.91 (0.46, 1.8) | 0.80 | |
| Retinal dialysis | 37/212 (17%) | 33/166 (20%) | 4/46 (9%) | 2.6 (0.86, 7.9) | 0.09 | |
| Giant retinal tear | 30/212 (14%) | 20/166 (12%) | 10/46 (22%) | 0.49 (0.20, 1.2) | 0.18 |
ROP: retinopathy of prematurity; FEVR: familial exudative vitreoretinopathy; RRD: rhegmatogenous retinal detachment; RD: retinal detachment; PVR: proliferative vitreoretinopathy; CI: confidence interval
Table 3.
Multivariable Relationship Between Presenting Factors and Anatomic Success with One or More Operation.
| Odds ratio | 95% Confidence Interval | p-value | ||
|---|---|---|---|---|
| Age group | 0.55 | |||
| 0–6 | 1.2 | (0.49, 3.1) | ||
| 7–12 | 1.7 | (0.64, 4.7) | ||
| 13–181 | -- | -- | ||
| Blunt Trauma | 2.2 | (0.61, 7.7) | 0.18 | |
| Penetrating Trauma | 0.81 | (0.29, 2.2) | 0.68 | |
| Previous Surgery (Cataract or Glaucoma) | 0.53 | (0.19, 1.4) | 0.27 | |
| Previous Retinal Surgery (SB, PPV, SO) | 0.30 | (0.12, 0.78) | 0.026 | |
| Subtotal RD (Macula Off + Macula On) | 3.6 | (1.5, 8.4) | 0.010 | |
| PVR Grade C or worse | 1.3 | (0.60, 2.9) | 0.49 | |
| Dialysis | 1.7 | (0.52, 5.6) | 0.35 | |
| Giant Retinal Tear | 0.46 | (0.16, 1.3) | 0.28 | |
| High Myopia (Non-Stickler Syndrome) | 1.4 | (0.50, 3.8) | 0.53 | |
| Stickler Syndrome | 3.1 | (0.76, 13) | 0.061 |
SB: scleral buckle; PPV: pars plana vitrectomy; SO: silicone oil; RD: retinal detachment; PVR: proliferative vitreoretinopathy
Serves as the reference group
We examined single operation success by surgical technique (SB, PPV, combined SB/PPV) for patients whose first operation was performed at our institution. The overall rate of successful retinal reattachment with a single operation was 119/183 (65%). There was a significantly higher success rate with primary SB (63%, OR 2.2, 95% CI 1.1–4.5) or combined SB/PPV (68%, OR 2.3 95% CI 1.1–5.1) compared to vitrectomy alone (51%). Pars plana lensectomy was a part of the initial surgical procedure in 20% of cases, and there was no significant difference in the rate of retinal reattachment for these cases (OR 1.3, 95% CI 0.64–2.7), p= 0.461).
Table 4 shows rates of retinal reattachment as well as visual acuity of patients with successful surgical repair at various follow up time points. Rates of retinal reattachment were 80% at 1 month after surgery and 81% at 12 months after surgery. Mean vision was better at each follow-up compared to baseline (mean 1.68, standard deviation 1.03) and was better at 1 year (mean 1.11, standard deviation 0.85) than at 6 months (mean 1.30, standard deviation 0.36). The percentage of patients with 20/40 or better vision likewise improved from baseline (12%) and was higher at 1 year (21%) than 6 months (14%). Analysis of change in vision shows that most patients had better vision, compared to baseline, at each time point after surgery. Approximately 1 in 10, however, had worse vision even at 6 and 12 months after surgery despite successful repair.
Table 4.
Retinal Reattachment and Visual Acuity at Follow-Up for Patients with Surgical Success
| Patients with Total Retinal Reattachment | No Visual Acuity Data | Non-logMAR vision | logMAR | VA of 20/40 or better | Change in Acuity vs. Baseline | |||
|---|---|---|---|---|---|---|---|---|
| N (%) | N (%) | mean (std), (n) | N (%) | Better | Same | Worse | ||
| Baseline | 23/1661 (14%) | 35/166 (21%) | 1.68 (1.03), (n=108) | 13/108 (12.0%) | -- | -- | -- | |
| 1 Month | 115/143(80%) | 16/115 (14%) | 8/115 (7%) | 1.24 (0.78), (n=91) | 9/91 (9.9%) | 48/922 (52.2%) | 26/92 (28.3%) | 18/92 (19.6%) |
| 3 Months | 124/161 (77%) | 12/124 (10%) | 12/124 (10%) | 1.27 (0.88), (n=100) | 13/100 (13.0%) | 59/101 (58.4%) | 29/101 (11.7%) | 13/101 (24.5%) |
| 6 Months | 123/154 (80%) | 10/123 (8%) | 12/123 (10%) | 1.30 (0.86), (n=101) | 14/101 (13.9%) | 66/103 (64.1%) | 26/103 (25.2%) | 11/103 (10.7%) |
| 12 Months | 133/165 (81%) | 8/133 (6%) | 20/133 (15%) | 1.11 (0.85), (n=105) | 22/105 (21.0%) | 72/109 (66.1%) | 25/109 (22.9%) | 12/109 (11.0%) |
logMAR: logarithm of minimum angle of resolution; VA: visual acuity; std: standard deviation
Snellen Equivalents
Baseline: 1.68 = 20/957
1 Month: 1.24 = 20/348
3 Months: 1.27 = 20/372
6 Months: 1.30 = 20/399
12 Months: 1.11 = 20/258
The denominator of 166 was used for the baseline data. 166 is the number of eyes that had multiple surgery success at their last study visit.
Note that denominators for better, same, worse analysis include non-logMAR visions when possible so the values are larger than those in columns 5 and 6.
Visual acuity can be difficult or impossible to measure in young children and some measurements were not convertible to logMAR. Supplemental Table S1 shows how many eyes had data for reattachment status and visual acuity at each visit out to 12 months. Supplemental Table S4 shows how many eyes had non-logMAR visions and how many had no visual acuity data at each visit (either due to lack of cooperation with testing or due to the examination being performed under anesthesia). Importantly, not all non-logMAR measurements equate to poor vision. For instance, preverbal children with BTL, CSM, and FF measurements may have excellent vision. Note that it was impossible to perform logMAR analysis on our complete data set due to the problem with non-convertible measurements. However, as shown in supplemental Table S4, the non-logMAR visions that were excluded from analysis were fairly evenly divided between good (BTL, CSM, FF) and bad (LP, NLP, No CSM, and No FF) vision measurements. The analysis of change in vision shown in Table 4 does include some eyes with non-logMAR vision.
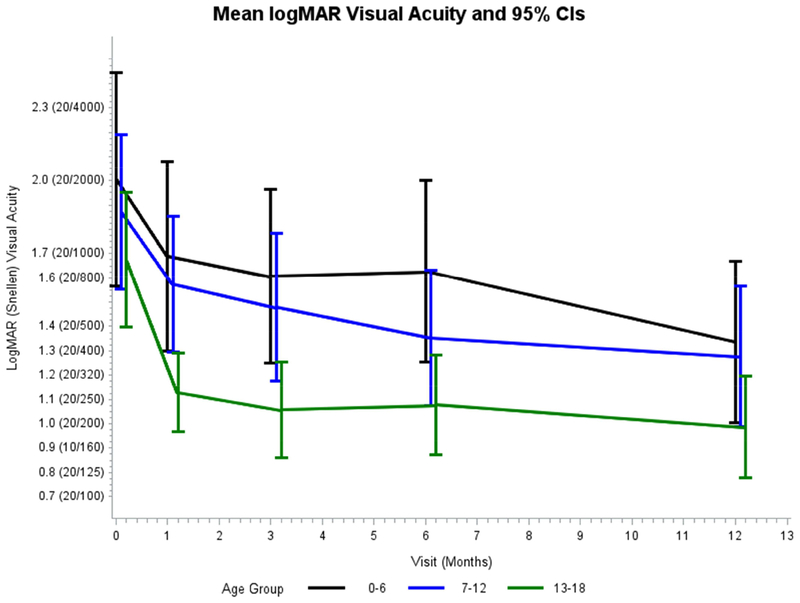
Table 5 shows visual acuity of patients with successful surgical repair by age group. The mean values listed are adjusted for the fact that a single patient can contribute two eyes to the data set. Mean logMAR visual acuity improved compared to baseline at each time point for each age group as shown in Figure 1. Supplemental Table S3 and supplemental Figure S1 show comparisons of mean logMAR visions for those with and without successful surgical repair.
Table 5.
Multivariable Model Results of LogMAR VA Adjusted for Age Group, Visit, and Interaction of Age and Visit1
| Age 0–6 | Age 7–12 | Age 13–18 | ||||
|---|---|---|---|---|---|---|
| N eyes | Adjusted Mean (95% CI) | N eyes | Adjusted Mean (95% CI) | N eyes | Adjusted Mean (95% CI) | |
| Baseline | 20 | 2.01 (1.57, 2.44) | 42 | 1.87 (1.55, 2.19) | 75 | 1.67 (1.40, 1.95) |
| 1 Month | 15 | 1.69 (1.30, 2.08) | 34 | 1.57 (1.30, 1.85) | 61 | 1.13 (0.97, 1.29) |
| 3 Months | 22 | 1.61 (1.25, 1.96) | 38 | 1.48 (1.17, 1.79) | 65 | 1.06 (0.86, 1.25) |
| 6 Months | 21 | 1.63 (1.25, 1.99) | 38 | 1.35 (1.07, 1.63) | 62 | 1.08 (0.87, 1.28) |
| 12 Months | 22 | 1.34 (1.00, 1.67) | 36 | 1.28 (0.98, 1.57) | 67 | 0.99 (0.78, 1.20) |
VA: visual acuity; CI: confidence interval
Snellen Equivalents
Baseline: 2.01 = 20/2047; 1.87 = 20/1483; 1.67 = 20/935
1 Month: 1.69 = 20/979; 1.57 = 20/743; 1.13 = 20/270
3 Months: 1.61 = 20/815; 1.48 = 20/604; 1.06 = 20/230
6 Months: 1.63 = 20/853; 1.35 = 20/448; 1.08 = 20/240
12 Months: 1.34 = 20/438; 1.28 = 20/381; 0.99 = 20/195
p values: Visit <0.0001, Age Group = 0.0124, Visit*Age Group = 0.5434
Figure 1.
Adjusted mean logMAR visual acuity and 95% confidence intervals for patients with multiple surgery success divided by age group.
DISCUSSION
In this analysis of a large cohort of pediatric patients with RRD we found differences between younger and older patients with regard to etiology, symptoms, and visual acuity outcomes. We did not, however, identify any significant difference in rate of successful surgical repair between age groups. Aside from age, several other factors did predict higher or lower success rate including macula attached status (higher), subtotal RD (higher), and history of previous retinal surgery (lower). In addition, we found that pediatric RRD patients treated with primary SB or combined SB/PPV had higher rates of single operation success than those treated with primary PPV. Overall, 78% of patients in this series had successful repair with a mean of 1.4 operations. To our knowledge, no other studies have analyzed factors associated with successful repair of pediatric RRD and no other studies have compared clinical features of RRD in different age groups of children.
Pediatric RRD accounts for a small subgroup of all retinal detachments but represents a distinct clinical challenge. Surgical management is often complex and reoperation is common.1, 3, 7 Visual outcomes are generally poorer, even when anatomic reattachment is achieved.1, 4 Many of these children suffer from hereditary disorders with systemic comorbidities.7, 8 A high proportion of detachments present bilaterally, which occurred in 10% of patients in this series, and 18–26% in other series.1, 4, 7 In spite of these difficulties, reattachment is generally achieved in 70–80% of eyes reported in the literature.1, 4, 7, 9, 10 Consistent with previous studies, in this series we achieved reattachment in 78% of eyes.
Almost all pediatric RRDs can be linked to an identifiable risk factor.9 In recent series, trauma was identified as the causative factor in around 40% of cases, similar to the 37% seen in our series.1–4, 7, 9 Congenital anomalies, such as Stickler syndrome or Marfan syndrome are present in 16–50% of these patients in previous series, and 18% in our series.1, 3, 4, 7, 9, 10 A history of intraocular surgery is a common risk factor in pediatric RRD. Gonzales et al reported previous surgery in 61% of eyes in their series, compared with 34% in Fivgas and Capone’s series and 51% in Weinberg et al’s series.1, 4, 9 In a recent large review of pediatric cataract surgeries, Agarkar et al estimated a cumulative incidence of postoperative RRD to be 5.5%, well above the reported annual incidence of 0.38–0.69 per 100,000 children.1, 8, 11 In our series, 39 eyes (18%) had previous cataract or glaucoma surgery before RRD occurred. An additional 29 eyes (14%) had previous surgery for retinal detachment before their first presentation to our service.
Because of the differences in physiology between younger and older children, we divided our patients into 3 age groups for analysis (0–6 years, 7–12 years, and 13–18 years). We found that the common causes of RRD varied between age groups. Stickler syndrome and treated ROP were significantly more common in the two youngest cohorts in our series, whereas blunt trauma was more common in the oldest cohort. We expected to find more advanced retinal detachments in the younger cohort due to inattentiveness to monocular changes in young patients, and indeed we did find the macula was detached at presentation more commonly in younger patients. Surprisingly, we found no difference in the rate of PVR, or rate of total RD at presentation between age groups. One possible explanation for this finding is that RRD in our younger patients was commonly associated with Stickler syndrome and treated ROP, and both of these underlying conditions may have prompted more regular eye examinations. Another explanation is the comparatively higher frequency of blunt trauma in the older cohort, a factor that could have raised the frequency of PVR in older patients. Not surprisingly, older children tended to report symptoms themselves, while younger children more often had symptoms reported by their parents. The low rate of self-reported symptoms in younger children highlights the need for regular dilated examinations, particularly in those with risk factors for RRD, such as myopia or a history of ROP with or without previous treatment.
While our data showed variations in etiology of RRD in each age group, it unexpectedly did not show a significant difference in final reattachment rate based on age, despite younger age being associated with worse outcomes in previous reviews.7, 9, 10 The factor most predictive of anatomic success in the multivariable analysis of presenting features was subtotal (as opposed total) retinal detachment on initial presentation (OR 3.3, 95% CI 1.4–7.6, p<0.01). The factor most predictive of failure was previous retinal surgery prior to presentation to our service (OR 0.3, 95% CI 0.12–0.76, p=0.01). Other clinical findings associated with successful outcome were simple (non-syndromic) myopia (OR 2.1, 95% CI 0.93–4.7, p=0.05) and retinal dialysis (OR 2.6, 95% CI 0.86–7.9, p=0.09). Although neither reached statistical significance, they both trended toward better outcomes, a finding consistent with anecdotal experience. Stickler syndrome patients also trended toward more successful reattachment outcomes (OR 3.5, p=0.07) but did not reach statistical significance. The explanation for better outcomes in Stickler syndrome is not clear. Surprisingly, the presence of grade C or worse PVR was not significantly associated with anatomic failure, but total RD was, a finding also seen in the series by Soheilian et al.7
Among patients with successful retinal reattachment, visual acuity remained stable or improved postoperatively in 89% by month 12 of follow up, with 11% experiencing a decrement compared to baseline. Acuity was 20/40 or better in 21% of patients by month 12. These figures are slightly higher than those published in comparable series by Gonzales et al and by Soheilian et al.7, 9 As expected, we saw lower levels of visual acuity in the youngest cohort of patients, a trend that persisted across all follow up time points. Potential explanations for this finding include amblyopia, both from the initial detachment and subsequent cataract, as well as strabismus and refractive error. In spite of the challenges the youngest children face, our data shows significant improvement in visual acuity after surgery in all age groups and over all follow up time points, underscoring the benefit of prompt surgical intervention regardless of age. Also, VA continued to improve between 6 and 12 months in all age groups. While it is difficult to compare our visual acuity data to other similar series because of the varying ways visual acuity results have been reported, the data taken as whole clearly support the conclusion that surgery to reattach the retina improves visual outcomes in pediatric patients across all age groups.1, 3, 4, 10
While the benefits of surgical intervention for pediatric RRD are clear, what has been less clear in previous studies is the type of operation most likely to result in retinal reattachment. In this series, single operation success was lower with primary PPV than with SB or combined SB/PPV. There are several good reasons to approach pediatric RRD with a scleral buckle. The pediatric vitreous is more formed and the posterior hyaloid is more firmly adherent to the retinal surface. These features may improve the tamponade effect achieved with scleral buckle and may make vitrectomy less effective at alleviating vitreoretinal traction.
This study is limited by its retrospective design. Cases referred to our service may have been more or less severe than what is found in other communities. Follow-up for the study was good with all patients having at least 3 months and 85% having 1 year or more of follow-up. Nevertheless, patients with worse vision or recurrent RRD may have been more or less likely to follow-up than patients with good vision and attached retinas and it is possible that our results are biased by variable follow-up. We did not, however, find any significant difference in baseline features or retinal reattachment outcome between patients with different lengths of follow-up (supplemental Table S2), although our power to find statistical significance was limited by relatively small sample size in the subgroups with shorter follow-up. Nonetheless, out of 212 eyes in the study, all but 32 had at least 1 year of follow-up and even if we assume that all 32 with less than 1 year of follow-up were surgical failures, the success rate would have been 67.9% (144/212) compared to our reported 78.3% (166/212). We believe that even by assuming the worst for eyes without 1 year of follow-up, the resulting relatively small difference in success rate is not clinically important. In addition, the main outcome measure was retinal reattachment at final follow-up. There are inherent biases in reporting outcomes at final follow up as opposed to specified intervals12, 13 To partially mitigate this limitation, we also include retinal reattachment rates as specific time points for the subset of patients whose data was available at those time points. Another limitation of this study is that it does not address functional outcomes such as enrollment in school or requirement for visual aids. Long term studies are needed to more precisely determine the functional capacity children have after repair of RRD. The visual acuity outcomes we do report must be interpreted with caution. Vision can be difficult or impossible to measure in children and testing can be unreliable. Some vision data could not be converted to logMAR (LP, NLP, Fix and Follow, Central-Steady-Maintained, and Blink to Light) so logMAR analysis is not available for the complete data set (see supplemental Table S4 for additional data on non-logMAR visions). The strength of this study is the large number of patients with long-term follow-up and analysis of outcomes based on age and presenting clinical features.
In summary, pediatric RRD is a difficult condition to treat but successful repair is possible in the majority of patients. Younger patients are more likely to have Stickler syndrome or treated ROP and older children are more likely to have traumatic etiology. Previous retinal surgery is an independent risk factor for failure of surgical repair, while subtotal RD is predictive of success. Anatomic success in this series did not vary with age but younger children tended to have worse VA outcomes. Repair of RRD was more successful with primary SB or combined SB/PPV compared to primary PPV. Despite the challenges in managing these cases, good anatomic outcomes are achievable in the majority of patients.
Supplementary Material
Figure S1. Adjusted mean logMAR visual acuity and 95% confidence intervals for patients with and without multiple surgery success.
Figure S2. Boxplots showing range, 25th – 75th percentile (box), mean (diamond), and median (middle line) for eyes with multiple surgery success at baseline, 1 month, 3 months, 6 months, and 12 months.
Acknowledgments
Financial Support: National Eye Institute Core Grant P30 EY006360
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No conflicting relationship exists for any author.
REFERENCES
- 1.Fivgas GD, Capone A Jr. Pediatric rhegmatogenous retinal detachment. Retina 2001;21(2):101–6. [DOI] [PubMed] [Google Scholar]
- 2.Rumelt S, Sarrazin L, Averbukh E, et al. Paediatric vs adult retinal detachment. Eye 2007;21(12):1473–8. [DOI] [PubMed] [Google Scholar]
- 3.Wadhwa N, Venkatesh P, Sampangi R, Garg S. Rhegmatogenous retinal detachments in children in India: clinical characteristics, risk factors, and surgical outcomes. J AAPOS 2008;12(6):551–4. [DOI] [PubMed] [Google Scholar]
- 4.Weinberg DV, Lyon AT, Greenwald MJ, Mets MB. Rhegmatogenous retinal detachments in children: risk factors and surgical outcomes. Ophthalmology 2003;110(9):1708–13. [DOI] [PubMed] [Google Scholar]
- 5.Okinami S, Ogino N, Nishimura T, Tano Y. Juvenile retinal detachment. Ophthalmologica 1987;194(2–3):95–102. [DOI] [PubMed] [Google Scholar]
- 6.Winslow RL, Tasman W. Juvenile rhegmatogenous retinal detachment. Ophthalmology 1978;85(6):607–18. [DOI] [PubMed] [Google Scholar]
- 7.Soheilian M, Ramezani A, Malihi M, et al. Clinical features and surgical outcomes of pediatric rhegmatogenous retinal detachment. Retina 2009;29(4):545–51. [DOI] [PubMed] [Google Scholar]
- 8.Wenick AS, Baranano DE. Evaluation and management of pediatric rhegmatogenous retinal detachment. Saudi J Ophthalmol 2012;26(3):255–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonzales CR, Singh S, Yu F, et al. Pediatric rhegmatogenous retinal detachment: clinical features and surgical outcomes. Retina 2008;28(6):847–52. [DOI] [PubMed] [Google Scholar]
- 10.Chen SN, Jiunn-Feng H, Te-Cheng Y. Pediatric rhegmatogenous retinal detachment in taiwan. Retina 2006;26(4):410–4. [DOI] [PubMed] [Google Scholar]
- 11.Agarkar S, Gokhale VV, Raman R, et al. Incidence, Risk Factors, and Outcomes of Retinal Detachment after Pediatric Cataract Surgery. Ophthalmology 2018;125(1):36–42. [DOI] [PubMed] [Google Scholar]
- 12.Jabs DA. Improving the reporting of clinical case series. Am J Ophthalmol 2005;139(5):900–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiLoreto DA Jr., Bressler NM, Bressler SB, Schachat AP. Use of best and final visual acuity outcomes in ophthalmological research. Arch Ophthalmol 2003;121(11):1586–90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Adjusted mean logMAR visual acuity and 95% confidence intervals for patients with and without multiple surgery success.
Figure S2. Boxplots showing range, 25th – 75th percentile (box), mean (diamond), and median (middle line) for eyes with multiple surgery success at baseline, 1 month, 3 months, 6 months, and 12 months.