Abstract
Women with previous Gestational Diabetes Mellitus (GDM) have seven times the risk of Type 2 diabetes later in life compared to women without GDM. Physical activity can reduce this risk and most women with previous GDM are not physically active.
Aims
To explore: (1) effectiveness of physical activity interventions for women with previous GDM; (2) factors that women with previous GDM perceive influence their physical activity; (3) how these factors are addressed by the interventions.
Methods
A systematic review of quantitative (aim 1) and qualitative (aim 2) studies with a mixed-methods synthesis (aim 3) was conducted in October 2017 following Cochrane methodology. Of 8101 articles identified, twenty-eight studies were included in total: 18 in Review 1 and 10 in Review 2.
Results
Four interventions significantly increased physical activity and 14 had either mixed effectiveness or no changes in physical activity. Reporting of intervention components and study quality varied greatly. Relevant qualitative factors included accounting for childcare issues, social support and cultural sensitivities. Interventions that incorporated these factors were associated with effectiveness. Education about how to reduce future risk of Type 2 diabetes and using pedometers in interventions were not associated with intervention effectiveness. Other factors that future interventions should address consist of ‘putting others before yourself’; ‘putting off lifestyle change’; ‘lack of support from healthcare professionals’ and ‘being a healthy role model for families’.
Conclusion
Combining the results of qualitative and quantitative studies can provide a nuanced understanding of the effectiveness of physical activity and lifestyle interventions.
Abbreviations: GDM, gestational diabetes mellitus; T2D, type 2 diabetes mellitus
Keywords: Female; Diabetes, gestational; Diabetes mellitus, type 2; Exercise; Life style; Systematic review
Highlights
-
•
Women with previous gestational diabetes are at high risk for type 2 diabetes.
-
•
Interventions to increase physical activity have not worked for this group.
-
•
Mixed-methods reviews allow us to identify effective intervention components.
-
•
Childcare, social support and cultural relevance are part of successful interventions.
-
•
Interventions should incorporate this review's results to improve effectiveness.
1. Introduction
Gestational diabetes mellitus (GDM) is glucose intolerance with first onset during pregnancy and affects approximately 1 in 29 pregnancies worldwide (Amorim and Katz, 2011; Guideline, 2015). There are significant health risks to a mother and baby including preeclampsia, emergency caesarean section and neonatal hypoglycaemia. After delivery, mothers experience seven-times increased risk of Type 2 diabetes (T2D) compared to women who had normoglycaemic pregnancies. The National Institute for Health and Care Excellence (NICE) guidelines advise education about lifestyle change to reduce or delay future risk of T2D (Guideline, 2015).
Participation in physical activity improves blood glucose levels and can prevent or delay onset of T2D (Amer Diabet, 2017). The Diabetes Prevention Programme demonstrated that lifestyle intervention can reduce risk of T2D onset by 34% at 10-years (“10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study”, 2009). This also holds true for women with a history of GDM (Aroda et al., 2015). A US-based prospective cohort study of 4554 women with previous GDM found that women who met current guidelines of 150 min of moderate-vigorous physical activity per week, had 47% lower risk of developing T2D (RR, 0.53; 95%CI, 0.38–0.75), even after adjusting for BMI (Bao et al., 2014). However, the majority of women with previous GDM are not physically active to levels recommended by guidelines. An Australian study found that only one-third of women with previous GDM were physically active (Smith et al., 2005).
Previous systematic reviews have examined whether interventions can improve lifestyle behaviours, including physical activity, in women with a history of GDM (Chasan-Taber, 2015; Gilinsky et al., 2015b; Guo et al., 2016; Jones et al., 2017; Miyazaki et al., 2017; Peacock et al., 2014; Pedersen et al., 2017). Five systematic reviews examined randomised control trials for this group (Chasan-Taber, 2015; Gilinsky et al., 2015b; Guo et al., 2016; Miyazaki et al., 2017; Pedersen et al., 2017), whereas others examined all study designs (Jones et al., 2015; Peacock et al., 2014). Taken together, these reviews showed lifestyle interventions lead to either insignificant or small but positive effects on T2D risk reduction in women with previous GDM. However, interventions that aimed to increase only physical activity have largely been ineffective in changing physical activity or anthropometric measurements, whereas dietary interventions or combination (e.g. dietary and physical activity) interventions were more effective in changing anthropometric measurements (Jones et al., 2015). This discrepancy in overall effectiveness between solely physical activity interventions and dietary or combination interventions may be due to overemphasis on diet with physical activity being considered less important, or time constraints limiting physical activity more than dietary changes (Gilinsky et al., 2015a; Jones et al., 2017). Sample sizes in most intervention studies are also small due to the studies being feasibility or pilot studies, and there are significant difficulties in recruiting and retaining participants (Guo et al., 2016; Jones et al., 2017). Previous research has shown that physical activity can reduce risk of T2D, but current interventions for women with previous GDM have largely been unable to change their physical activity behaviour.
It is important to understand why interventions to increase physical activity have largely been ineffective and how they can be modified to better fit women's lives. Understanding why could have practical implications in determining what interventions should be tested in the future. Therefore, the current systematic review aims to explore the effectiveness of physical activity interventions for women with a history of GDM, using both quantitative and qualitative review methods.
Part of the Six Steps in Quality Intervention Development (6SQuID) framework informed the methodology of this systematic review. 6SQuID was developed due to the recognition that there was a gap in guidance to develop public health interventions in a way that was rigorous, evidence-based and participatory (Wight et al., 2015). It encourages co-production of interventions with stakeholders and the use of theory alongside research to maximise the impact of interventions. The first two steps of 6SQuID are to 1) define and understand the public health problem and its cause, and to 2) clarify which modifiable and non-modifiable causal and contextual factors shape the problem. The remaining steps of 6SQuID are 3) identifying the change mechanism; 4) identifying how to deliver the change mechanism, then 5) and 6) testing and refining the intervention and collecting sufficient evidence of effectiveness to justify more rigorous evaluation (Wight et al., 2015). The current review informs the first two steps of 6SQuID by understanding the factors that women with previous GDM say influence their physical activity and reviewing how interventions have tried to address the problem of physical inactivity in this group. This lays the foundation for future physical activity intervention development using sound evidence and theory for women with previous GDM.
To review both interventions and factors to understand what works and why, respectively, a systematic review method of both quantitative and qualitative studies was undertaken (Thomas and Harden, 2008). This type of review integrates quantitative and qualitative research to understand why certain interventions may be effective or ineffective. Qualitative data can aid in understanding the contextual factors that may influence intervention effectiveness (Gilinsky et al., 2015b). This may allow practitioners and policy-makers to make pragmatic decisions regarding the development and implementation of future physical activity interventions in this population.
The aims of this review were three-fold:
-
1.
To evaluate the effectiveness of interventions to increase physical activity in women who have had GDM (Review 1);
-
2.
To understand the modifiable and non-modifiable factors that influence the physical activity of women with a history of GDM (Review 2); and.
-
3.
To synthesise the previous two aims to understand which factors (of Review 2) may influence the effectiveness of the interventions (of Review 1) (Mixed-methods synthesis).
2. Methods
The protocol of this systematic review was registered on the International prospective register of systematic reviews (PROSPERO) in February 2018 (CRD42018085863) and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (Moher et al., 2009). This review was conducted to inform future intervention development within the 6SQuID framework (Wight et al., 2015).
2.1. Inclusion criteria
Table 1 shows the inclusion criteria for the qualitative and quantitative reviews using the SPIDER and PICOS eligibility criteria, respectively. PICOS (Population, Intervention, Comparison group, Outcome, Study design) systematically defines the eligibility criteria for a quantitative intervention review (Schardt et al., 2007), and SPIDER (Sample, Phenomena of Interest, Design, Evaluation, Research type) is a similar qualitative tool (Cooke et al., 2012). As the majority of studies were short-term, we have used changes in physical activity as the primary end point, but have included details of studies with T2D as one endpoint (alongside physical activity) because it is a clinically significant end point.
Table 1.
Eligibility criteria for the qualitative and qualitative reviews, prior to synthesis. The bolded eligibility criteria are the common terms between the reviews and therefore were used in the search strategy.
| Quantitative review - PICOS | Qualitative review - SPIDER |
|---|---|
| Population: Women with previous gestational diabetes. | Sample: Women with previous gestational diabetes. |
| Intervention: Lifestyle interventions specifically designed for women with previous gestational diabetes. | Phenomena of Interest: At least one overall theme about physical activity or a related term (e.g. exercise). |
| Comparison: any control group. | Design: Any qualitative methods including in-depth interviews, focus groups, ethnography, reflective diaries and case-study methodologies. |
| Outcome: Physical activity or a related outcome (e.g. exercise) must be at least one of the outcomes - either self-report or objective measurements. | Evaluation: Factors, beliefs, perceptions, attitudes, opinions, etc. |
| Study design: Randomised control trials or quasi-experimental study designs. | Research type: Qualitative. |
2.2. Search strategy
An electronic search was conducted in October 2017 across the following databases: Medline, Cinahl, EMBASE, Wiley Cochrane, PsycINFO, Web of Science, ASSIA, ProQuest, EthOs, OpenGrey and ClinicalTrials.gov with no date or language restrictions. The search terms used were related to the phrases “gestational diabetes” and “physical activity”, as these were commonalities in the quantitative and qualitative reviews' eligibility criteria. The search strategy was developed and refined with the help of a subject specialist librarian (Supplementary Table 1).
After the databases were searched, all resultant records were imported into referencing software (EndNote). Duplicates were removed using software and hand-searching. Forward and backward citations for all included studies were conducted in May 2018, to check reference lists of cited studies and subsequent citations of included studies for additional relevant studies, respectively (Greenhalgh and Peacock, 2005).
2.3. Applying the inclusion criteria
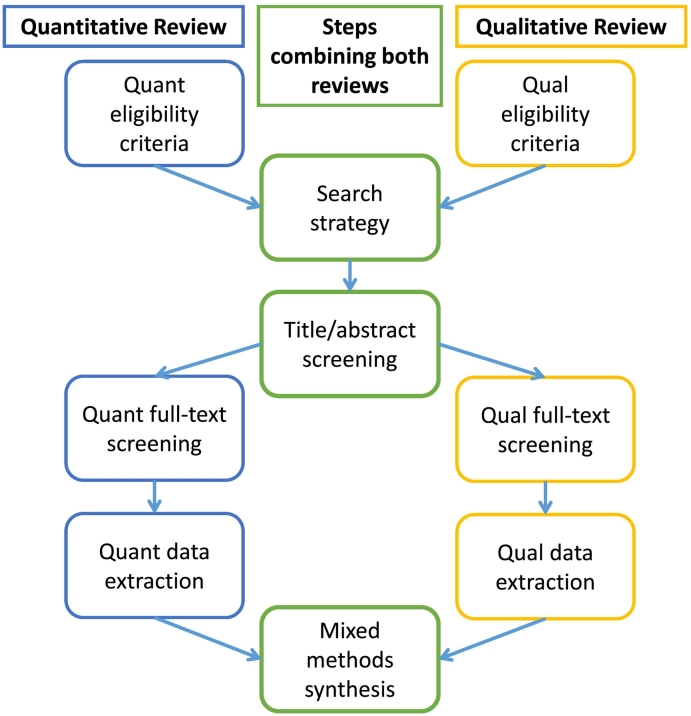
Two reviewers (AB and RP or DH) screened the titles and abstracts for relevant records (Fig. 1). RP and DH were research assistants for the review: RP conducted the qualitative review and DH conducted the quantitative review, whereas AB conducted both reviews simultaneously. If records appeared potentially relevant to the quantitative or qualitative records based on eligibility criteria, they were separated into respective folders to have their full-texts searched. Two reviewers subsequently screened full-texts and determined what studies to include in the reviews. Disagreements were resolved through discussion. Authors were contacted for further information if data was missing, or it was unclear if the study should be included.
Fig. 1.
This figure shows the search process for combining the two reviews (searched in October 2017) into a more efficacious search strategy.
2.4. Quality assessment
Study quality was duplicate-assessed using The Cochrane Collaboration's tool for assessing risk of bias and the Critical Appraisal Skills Programme (CASP) qualitative checklist. Disagreements were resolved through discussion (AB and RP or DH). No studies were excluded on the basis of their quality assessment but accounted for in later synthesis.
2.5. Data extraction
The data from the included quantitative studies were extracted into a modified Cochrane Collaboration data extraction form using Microsoft Excel. Additional intervention details were added, including intervention development, timing, delivery, theoretical basis, and content. Two reviewers (DH and AB) extracted the quantitative data independently and compared data extraction forms.
The data from the qualitative review were extracted into QSR International NVivo 10.0 software. Two reviewers extracted and analysed the qualitative data independently and discussed themes together to improve rigor (RP and AB) (Mays and Pope, 1995).
2.6. Data synthesis
For the quantitative studies, clinical heterogeneity was assessed after data extraction to see if the quantitative synthesis could be performed using meta-analysis. Meta-analysis was not feasible due to the heterogeneity of study designs, intervention components, and outcome definitions present, therefore a narrative analysis was undertaken.
Thematic analysis and synthesis was used in accordance with Clarke and Braun's method to develop common themes between included studies (Braun and Clarke, 2006). Line-by-line coding to generate nodes preceded development of descriptive themes based on general themes and categories. The themes were divided into barriers and facilitators to physical activity in line with Dahlgren and Whitehead's determinants of health model (Dahlgren and Whitehead, 1991). Details about qualitative method, study objectives, sample size, and analysis method were also extracted for comparison.
2.7. Mixed-methods synthesis of the quantitative and qualitative studies together (aim 3)
In the synthesis of the quantitative and qualitative reviews, the findings were combined in a matrix that juxtaposed the qualitative factors influencing physical activity with the quantitative interventions, according to Thomas and Harden's mixed methods synthesis technique (Thomas and Harden, 2008). One reviewer (AB) developed the matrix and thoroughly reviewed the intervention descriptions to determine if it addressed the barriers and facilitators found in the qualitative synthesis, then gaps, matches and mismatches were identified. Gaps were defined by previous studies as when the interventions included did not address the qualitative factors women discussed as important to them. Matches were when the interventions did address the qualitative factors and were more effective. Mismatches were when the interventions did not address the qualitative factors but were not more effective (Thomas and Harden, 2008). Quality was considered at this stage: confidence in the synthesis was determined based on the number and quality assessment of the studies addressing each factor.
3. Results
From the database searches, 8101 records were identified. After duplicates were removed, 5564 records remained. Screening of the titles and abstracts and eliminating irrelevant records resulted in 343 full-texts to screen. This included 109 studies that were qualitative, 206 that were quantitative, and 28 with an unclear study design (see Fig. 2). After forward and backward searches, 20 quantitative (18 separate studies) and 10 qualitative studies were included in the analysis.
Fig. 2.
PRISMA diagram of the qualitative and quantitative studies included in the systematic review. GDM = gestational diabetes mellitus; PA = physical activity; NR = not reported.
3.1. Characteristics of quantitative studies
Of the eighteen quantitative intervention studies included twelve of these were randomised controlled trials (RCTs) and six were single-arm pre-post study design. Studies were based in Australia (7), United States (5), Canada (4), China (1) and Spain (1).
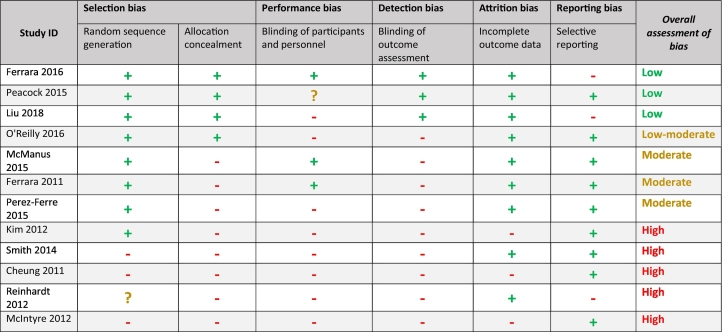
Study quality was judged to be poor based on the Cochrane risk of bias tool. Seven studies were deemed high risk of bias, six were moderate or low-moderate, and two studies had low risk of bias (Table 2, Table 3). The sample sizes varied significantly between studies (median size N = 54, range N = 17 to 2280). Recruitment rates were generally poor: only 5 of 18 studies had recruitment rates over 50%. Two studies did not report recruitment rates but sample sizes were small. One paper suggested recruitment difficulties were due to childcare pressures, employment and general time constraints not allowing potential participants to take part (Nicklas et al., 2014). Interventions with more strict eligibility requirements had lower rates (below 50%) of recruitment. Studies that had higher rates (above 50%) of recruitment recruited during pregnancy (Ferrara et al., 2011; Nicholson et al., 2016; Perez-Ferre et al., 2015); waived consent for participation (Ferrara et al., 2014) or used culture-specific methods of recruitment (Philis-Tsimikas et al., 2014).
Table 2.
The Cochrane risk of bias tool for the quantitative studies with a randomised controlled trial study design. Green = quality domain is present; red = quality domain is absent; yellow = unclear if domain is present or absent.
Table 3.
The risk of bias tool for the quantitative studies with a pre-post study design included in the review. Green = quality domain is present; red = quality domain is absent; yellow = unclear if domain is present or absent.
Nine studies focussed on improving both physical activity behaviour and diet (Brazeau et al., 2014b; Brazeau et al., 2018; Ferrara et al., 2016; Liu et al., 2018; Mukerji et al., 2015; Nicholson et al., 2016; O'Reilly et al., 2016; Peacock et al., 2015; Reinhardt et al., 2012; Smith et al., 2014), six were more general lifestyle-based interventions that included physical activity, diet and other components (such as breastfeeding) (Cheung et al., 2007; Ferrara and Ehrlich, 2011; Mcmanus et al., 2015; Perez-Ferre et al., 2015; Philis-Tsimikas et al., 2014), and three interventions were solely focussed on physical activity (Cheung et al., 2011; Kim et al., 2012; McIntyre et al., 2012). Refer to Table 4 for a summary of the included intervention studies (Supplementary Table 2 contains more detail).
Table 4.
A summary of the included intervention studies and their characteristics. N = sample size; I = intervention group sample size; C = control group sample size; sig. = significant.
| Study ID, country, study design | Sample size | Focus of intervention | Mode and length of intervention | Physical activity-specific results |
|---|---|---|---|---|
| Brazeau 2014 Canada, single arm pre-post |
N = 36 | Diet and physical activity | Group, telephone, website; 13 weeks | No change in accelerometer measures; pedometer measures increased by 733 steps/day (95% CI 85, 1391) |
| Brazeau 2018 Canada, single arm pre-post |
N = 118 (59 couples) | Diet and physical activity | Group, website, texting; 13 weeks | Sig. incr. in step counts and moderate-vigorous physical activity in mothers and partners. Partners decreased sitting time sig. and similar trend in mothers. |
| Cheung 2007 Australia, single arm pre-post |
N = 25 | Diet, physical activity, breastfeeding, child nutrition | Group, telephone, newsletters; 12 months | Sig. incr. in walking. No sig. changes in vigorous activity or total leisure time. |
| Cheung 2011 Australia, RCT |
N = 43 I = 96, C = 101 |
Physical activity | Individual, telephone, postcards; 12 months | No sig. changes in physical activity. |
| Ferrara 2011 USA, RCT |
N = 197 I = 1097, C = 1193 |
Diet, physical activity, breastfeeding | Individual, telephone; 12 months | No sig. changes in physical activity. |
| Ferrara 2016 USA, RCT |
N = 2280 | Diet and physical activity | Telephone, newsletters, website; 12 months | Vigorous physical activity levels sig. higher in intervention group as compared to control group. No sig. differences in moderate intensity activity. |
| Kim 2012 USA, RCT |
N = 49 I = 21, C = 28 |
Physical activity | Website; 13 weeks | No sig. changes in physical activity. |
| Liu 2017 China, RCT |
N = 1180 I = 586, C = 594 |
Diet and physical activity | Individual, telephone; 12 months | Sig. incr. in physical activity. |
| McIntyre 2012 Australia, RCT |
N = 28 I = 15, C = 13 |
Physical activity | Individual, telephone; 12 weeks | No sig. changes in physical activity. |
| McManus 2015 Canada, RCT |
N = 170 I = 89, C = 81 |
Diet and physical activity | Individual, website, group; 12 months | No sig. changes in physical activity. |
| Mukerji 2015 Canada, single arm pre-post |
N = 17 | Diet and physical activity | Individual, telephone; 6 months | Sig. incr. in exercise capacity. |
| Nicholson 2016 USA, single arm pre-post |
N = 23 | Diet and physical activity | Website; 30 weeks | No sig. changes in physical activity. |
| O'Reilly 2016 Australia, RCT |
N = 573 I = 284, C = 289 |
Diet and physical activity | Group, individual, telephone; 12 months | No sig. changes in physical activity. |
| Peacock 2015 Australia, RCT |
N = 31 I = 16, C = 15 |
Diet and physical activity | Group, website; 4 weeks | No sig. changes in physical activity. |
| Perez-Ferre 2015 Spain, RCT |
N = 260 I = 130, C = 130 |
Diet and physical activity | Group, individual; 6 months | No sig. changes in physical activity. |
| Philis-Tsimikas 2012 USA, single arm pre-post | N = 84 | Diet, physical activity and mental health | Group; 8 weeks | Sig. incr. in aerobic capacity, flexibility and strength training. |
| Reinhardt 2012 Australia, RCT |
N = 38 I = 18, C = 20 |
Diet and physical activity | Booklet, telephone; 6 months | Sig. incr. in leisure time physical activity, but no changes in total activity levels. |
| Smith 2014 Australia, RCT |
N = 59 I = 29, C = 30 |
Diet and physical activity | Individual, telephone, postcards; 6 months | No sig. changes in physical activity. |
Intervention components also varied significantly: nine interventions took place with individual participants, either in-person or on the telephone (Cheung et al., 2011; Ferrara et al., 2011; Ferrara et al., 2016; Liu et al., 2018; McIntyre et al., 2012; Mcmanus et al., 2015; Mukerji et al., 2015; Reinhardt et al., 2012; Smith et al., 2014). Five used a web platform (Brazeau et al., 2014a; Ferrara et al., 2016; Kim et al., 2012; Mcmanus et al., 2015; Nicholson et al., 2016), three were group-based (in-person) (Brazeau et al., 2018; Peacock et al., 2015; Philis-Tsimikas et al., 2014), and four were a combination of individual and group-based (Brazeau et al., 2014a; Cheung et al., 2007; O'Reilly et al., 2016; Perez-Ferre et al., 2015). The median intervention length was six months and ranged from four weeks to one year.
3.2. Summary of intervention effectiveness
Four studies – three pre-post study design with moderate risk of bias and one RCT with low-moderate risk of bias – demonstrated significantly increased physical activity as a result (Brazeau et al., 2018; Liu et al., 2018; Mukerji et al., 2015; Philis-Tsimikas et al., 2014). Five studies had mixed results, in which there was at least one significant and one insignificant result relating to physical activity measures (Brazeau et al., 2014a; Cheung et al., 2007; Ferrara et al., 2016; Nicholson et al., 2016; Reinhardt et al., 2012). Nine studies had no significant changes in physical activity (Cheung et al., 2011; Ferrara et al., 2011; Kim et al., 2012; McIntyre et al., 2012; Mcmanus et al., 2015; O'Reilly et al., 2016; Peacock et al., 2015; Perez-Ferre et al., 2015; Smith et al., 2014).
3.3. Characteristics and quality of qualitative studies
Ten studies published from 2009 to 2015 were included in the qualitative review (Table 5). The median sample size was 18 participants, ranging from 7 to 57 participants. Five studies partially focussed on experiences and belief surrounding physical activity by ethnic minority or indigenous women in high-income countries, including Aboriginal and immigrant women in Australia (Bandyopadhyay et al., 2011; Razee et al., 2010); Algonquin women in Canada (Gaudreau and Michaud, 2012); and Hispanic and African American women in America (Tang et al., 2015). The remainder of the studies were interviews primarily with white women in high-income countries, and one with Tongan women in Tonga.
Table 5.
Summary of included qualitative studies. PA = physical activity; GDM = gestational diabetes mellitus; DM = diabetes mellitus; GTT = glucose tolerance test.
| Study ID | Location | Data collection method | Focus | Sample size |
|---|---|---|---|---|
| Bandyopadhyay 2015 | Australia | Interview | Postpartum GTT, lifestyle | 33 |
| Bieda 2009 | USA | Interview | GDM, lifestyle change | 25 |
| Doran 2008 | Australia | Interview | GDM, lifestyle change | 8 |
| Doran 2010 | Australia | Interview | GDM, PA | 11 |
| Gaudreau 2012 | Canada | Observation/interview | Lifestyle | 7 |
| Graco 2009 | Australia | Interview | PA | 10 |
| Lie 2013 | UK | Interview | Lifestyle | 31 |
| Razee 2010 | Australia | Interview | Lifestyle | 57 |
| Tang 2015 | USA | Interview | T2D, lifestyle | 23 |
| Tierney 2015 | Ireland | Interview | Lifestyle | 13 |
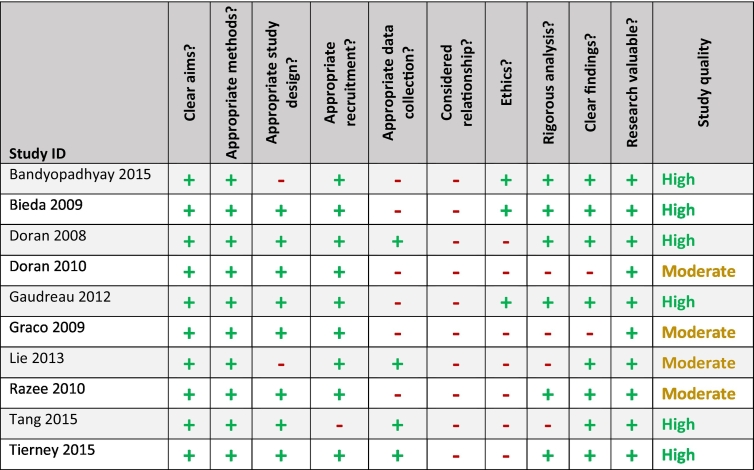
The studies assessed by the Critical Appraisal Skills Programme (CASP) were of moderate or high quality. All studies were rated lower in quality because they did not adequately consider the relationship between researcher and participant, describe ethical issues in sufficient detail or discuss data analysis rigorously. The remaining categories were largely addressed (Table 6).
Table 6.
The Critical Appraisal Skills Programme (CASP) checklist for qualitative studies. Green = quality domain is present; red = quality domain is absent; yellow = unclear if domain is present or absent.
3.4. Synthesis of qualitative studies
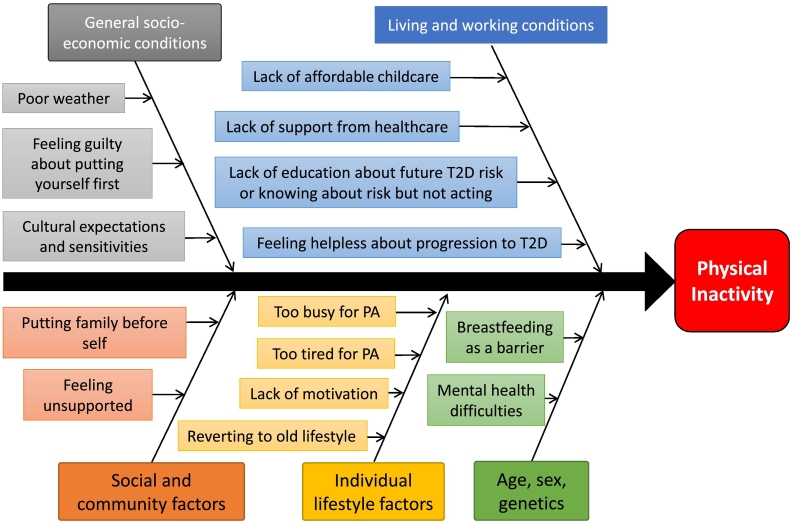
In inductively coding and developing themes for the included qualitative studies, the nodes (and subsequent themes) were grouped into Dahlgren and Whitehead's social determinants of health model. All themes found fit into the model, as it encompasses all layers of health determinants (Dahlgren and Whitehead, 1991). In Fig. 3, the barriers to physical activity identified during the thematic synthesis have been grouped into the following levels: 1. Constitutional factors; 2. Individual lifestyle factors; 3. Social and community networks; 4. Living and working conditions and 5. General socio-economic, cultural and environmental conditions. The following sections will discuss the most prevalent factors that women said influenced their physical activity.
Fig. 3.
This fishbone diagram shows the primary barriers identified in the qualitative synthesis. The themes are grouped according to Dahlgren and Whitehead's determinants of health model.
3.4.1. Constitutional factors
Mental health and breastfeeding were both described as constitutional factors that influenced physical activity in women with previous GDM. A significant theme that emerged from the Razee and colleagues' study was the importance of mental health in influencing physical activity behaviours (Razee et al., 2010). Both mental health and breastfeeding as physical activity-limiting factors were present in one study each, but were included in the review as the authors have been unable to find these factors reported in other reviews.
3.4.2. Individual lifestyle factors
Women commonly mentioned not having the time or energy to be more physically active due to competing demands, including motherhood and childcare, working and domestic responsibilities (N = 7) (Bandyopadhyay et al., 2011; Doran, 2008; Graco et al., 2009; Lie et al., 2013; Razee et al., 2010; Tang et al., 2015; Tierney et al., 2015). Several women mentioned being disorganised as something that influenced their lack of time: “I think time has a lot to do with it. It's just time to get organised” (Tierney et al., 2015).
3.4.3. Social and community networks
Family responsibilities played a large role in women's likelihood of participating in physical activity, both positively and negatively. Women discussed how being the primary caregiver and household manager made finding time to be active difficult: “I don't really spend too much time thinking about [my risk for diabetes]. Because I've got two kids under four and I am too busy to spend my day worrying about [my health]” (Razee et al., 2010). Other women were motivated to be more active and healthy to be role models for their family and to “be there to bring up their children” (Razee et al., 2010).
3.4.4. Living and working conditions
Education about the risk of T2D with a history of GDM played a large role in this level of the socioecological model: women spoke at length about being unsure and uneducated about the risk of future T2D (Doran, 2008; Lie et al., 2013; Razee et al., 2010; Tang et al., 2015; Tierney et al., 2015). They were unsure of how to prevent T2D in the future and if it was even possible (Doran, 2008). Some women were aware of their increased risk for T2D but wanted more information about prevention. Overall, there was high variability in women's knowledge and understanding of ability to prevent T2D.
One theme found in the qualitative synthesis was a lack of support and follow-up from their healthcare providers (N = 5) (Doran, 2008; Doran and Davis, 2010; Graco et al., 2009; Lie et al., 2013; Tierney et al., 2015). Women spoke of “being left high and dry” after their post-natal check (Lie et al., 2013). They felt solely responsible to schedule follow-up post-GDM care, at times stating that their “GPs don't seem to have expertise in that particular field” (Tierney et al., 2015). The lack of follow-up care seems to have played an important role in their lack of education about preventing future diabetes risk: “Nobody told me anything about type 2 diabetes…they were so focused on the immediate pregnancy problems” (Doran, 2008). Some said their doctor was an exception, but overall women were dissatisfied with their postpartum care relating to their GDM.
Lack of access to affordable childcare was mentioned in six studies as being prohibitive to physical activity (Bandyopadhyay et al., 2015; Doran, 2008; Graco et al., 2009; Lie et al., 2013; Razee et al., 2010; Tang et al., 2015).
3.4.5. General socio-economic, cultural and environmental conditions
The theme of putting others before oneself and feeling guilty when putting yourself first was decided by the reviewers to fit into the broadest macro-category, as it represents a cultural norm that many women feel is important for them to fit into their roles of mother and caregiver (Currie, 2004). The majority of studies (N = 6) addressed these overlapping themes in some way (Gaudreau and Michaud, 2012; Graco et al., 2009; Lie et al., 2013; Razee et al., 2010; Tang et al., 2015; Tierney et al., 2015): women described feeling guilty about taking time for themselves (especially if that required asking a friend or family member to watch their children) and also felt that “[they] tend to put [themselves] down the pile a bit … everything else comes first really” (Tierney et al., 2015).
Other themes in this category included the importance of culture-appropriate information and interventions (Doran and Davis, 2010; Gaudreau and Michaud, 2012; Razee et al., 2010; Tang et al., 2015), though one study refuted that by suggesting that there are universal challenges of being a mother (Tang et al., 2015). Lastly, poor weather was mentioned as a barrier to exercise (Bandyopadhyay et al., 2015; Tierney et al., 2015).
3.4.6. Suggesting physical activity intervention ideas
Seven studies explored potential physical activity interventions, either by explicitly asking women or women suggesting ideas (Bandyopadhyay et al., 2011; Doran, 2008; Gaudreau and Michaud, 2012; Lie et al., 2013; Razee et al., 2010; Tang et al., 2015; Tierney et al., 2015). Women emphasised that walking was “the most helpful and practical form of physical activity” (Razee et al., 2010) as it “both energises and relaxes” (Gaudreau and Michaud, 2012). Several studies reiterated having social support to facilitate long-term lifestyle change (Doran, 2008; Razee et al., 2010; Tierney et al., 2015). This included linking family wellbeing with physical activity as an opportunity to be seen as a role model for children (Bandyopadhyay et al., 2015; Razee et al., 2010; Tang et al., 2015).
3.5. Mixed-methods synthesis
The mixed-methods synthesis compared the included intervention components with the qualitative factors and revealed several matches, gaps, and mismatches. Table 7 provides an in-depth analysis of the mixed-methods synthesis.
Table 7.
A table summarising the results of the mixed-methods synthesis. The assessed strength of the evidence takes into account the number of relevant studies, their respective quality and the consistency of the evidence. The factors on the furthest left column are a summary of the factors found in the qualitative review and are listed in order of prevalence in the literature. The next column describes the extent to which the interventions addressed these themes and whether or not they were effective. Using this, an assessment was made about whether this factor represented a match, mismatch or gap. The confidence in that assessment was evaluated based on the number and quality of the relevant studies. Finally, recommendations for future interventions are provided.
|
Match: Factors are associated with effective interventions |
Mismatch: Factors are associated with ineffective interventions |
Gap: No association with effective or ineffective interventions |
Inconclusive: Insufficient evidence to determine if a match, mismatch or gap. |
|---|---|---|---|
| Factors that influence physical activity (# qualitative studies that mentioned factor) | Extent to which addressed in interventions | Match, mismatch, gap? |
Recommendations for future interventions |
| Confidence in synthesis? | |||
| Lack of time and energy to be more active (7) | Eight interventions addressed these factors and ten did not. There was no discernible pattern of effective and ineffective interventions addressing lack of time or energy. | Gap |
|
| Moderate confidence | |||
| Feeling guilty about taking time to oneself/putting others first (7) | One ineffective intervention assessed changes in “feeling you should put the needs of others in your family before yours” in a lifestyle survey. No other interventions addressed these factors. | Gap |
|
| Moderate-high confidence | |||
| Knowing about increased risk but not doing anything about it/putting off lifestyle change (6) | No interventions addressed women knowing about their increased risk of T2D but not acting on it, nor putting off lifestyle change into the future. | Gap |
|
| High confidence | |||
| Walking as a preferred form of physical activity (6) | One effective study used walking as a tool, whereas the other two significant studies did not use walking. All studies that used pedometers as motivation to increase walking/activity were either ineffective (N = 4) or of mixed effectiveness (N = 1). |
Inconclusive |
|
| Moderate confidence | |||
| Lack of affordable childcare (6) | All three significant interventions provided access to childcare during the intervention. Two non-significant and one mixed-effectiveness studies also provided access to childcare, leaving 12 studies that did not address childcare at all. |
Match |
|
| Moderate confidence | |||
| Lack of support from healthcare professionals (5) | Two effective and two ineffective studies addressed this factor by holding the intervention at a hospital, having healthcare professionals lead the sessions or demonstrating that as a result of the intervention, women felt increased support and encouragement from doctors. | Gap |
|
| Moderate confidence | |||
| Lack of awareness or concern about T2D risk and how to reduce that risk (5) | All three effective physical activity interventions did not directly address this factor. The effective physical activity interventions were more generally focussed on changing lifestyle behaviours and the studies did not mention education about T2D risk and risk reduction techniques. The ineffective and mixed-effectiveness interventions primarily addressed education as a component of the programme (10 of 15). | Mismatch |
|
| Low-moderate confidence | |||
| Feeling helpless about getting T2D (5) | Three studies addressed this barrier by educating about how to prevent T2D after having GDM – two were ineffective and one was of mixed-effectiveness. The remainder of the studies (N = 15) did not address this barrier explicitly. | Gap |
|
| Moderate confidence | |||
| Social and community support helps women to be more physically active (5) | All three interventions that effectively increased physical activity behaviour included social support as a component of the intervention. Four ineffective and two mixed-effectiveness interventions also aimed to address this using peer support. Two interventions attempted to provide social support through online message boards or inviting partners to attend, but these were not used by participants. | Match |
|
| Moderate confidence | |||
| Importance of culturally sensitive interventions (4) | Two effective interventions and one mixed-effectiveness studies accounted for cultural factors in their studies. | Match |
|
| Moderate-high confidence | |||
| Being a healthy role model for family (3) | No studies explicitly included this factor as part of their intervention. | Gap |
|
| High confidence | |||
| Reverting back to pre-GDM lifestyle (3) | No interventions explicitly addressed this factor. | Gap |
|
| High confidence | |||
| Difficulties in physical activity while breastfeeding (2) | One successful intervention addressed breastfeeding while considering exercise programme planning. Other studies educated about the importance of breastfeeding, but did not address it as a barrier to physical activity | Gap |
|
| High confidence | |||
| Mental health difficulties (2) | Three studies addressed dealing difficulties in mental health during the intervention. One intervention was effective, another ineffective, and the final was of mixed-effectiveness. | Inconclusive |
|
| High confidence |
There did not appear to be a relationship between the prevalence of themes in the qualitative synthesis and the number of intervention studies that addressed that factor – one of the most prevalent themes (in 7 qualitative studies), ‘feeling guilty about taking time to oneself’, was only addressed directly in one intervention. The theme addressed most often by interventions was social and community support (8 interventions), whereas three themes were not addressed explicitly by any interventions: ‘putting off lifestyle change’, ‘being a healthy role model for family’, and ‘reverting back to pre-GDM lifestyle’. In the mixed-methods synthesis, three matches were evident in which effective interventions appeared to address the qualitative factors more than ineffective interventions. These included ‘lack of affordable childcare’, ‘social and community support’ and ‘provision of culturally sensitive interventions’. Walking as a preferred form of activity and education about T2D were mismatches between the qualitative literature and the quantitative interventions. Women identified walking as their preferred form of physical activity and a lack of education about T2D to be prohibitive to taking action, but intervention studies in the review that addressed these factors were no more likely to be effective than studies that did not address these factors.
4. Discussion
By synthesising qualitative and quantitative literature together, we gain a new perspective of physical activity interventions and their effectiveness for women with previous GDM, which can help practitioners and researchers develop more effective interventions. There have been other reviews that summarise the intervention literature systematically, but none have synthesised both qualitative and quantitative literature together.
The qualitative synthesis separated all factors influencing physical activity into discrete groupings by Dahlgren and Whitehead's determinants of health model, but these factors clearly relate and interplay within and between levels. For example, mental health difficulties as a constitutional factor can also relate to an individual's lack of motivation (a common symptom of depression); feeling unsupported by healthcare professionals and feelings of guilt about prioritising oneself (Liss et al., 2013).
Walking and education about T2D were mismatches, meaning interventions that addressed these factors were not associated with effectiveness. This may be due to over-estimating the benefits and sustainability of walking for time-constrained women with previous GD. Education about risk of T2D should be combined with other intervention tools (social support, cultural-specific activities) to increase intervention effectiveness, as previous research has shown that education alone is insufficient to change behaviour (Marmot, 2005).
Health behaviours are significantly influenced by systems such as environment and culture (Marmot, 2005). However, the qualitative synthesis only identified a few factors that lay within these larger spheres, such as cultural expectations and sensitivities. This may be due to cultural overemphasis on individual behaviour determining lifestyle and health and therefore, women not realising the extent that larger systems influence our behaviour (Robert et al., 2008).
This review demonstrates disconnect between the perceptions of women with previous GDM's towards physical activity and the target of current physical activity interventions. New approaches to intervention development are needed to ensure that barriers to behaviour change are being addressed. Co-production is an increasingly popular methodology that involves research participants being active members of the research process (Hawkins et al., 2017) and could help to close this gap between perceptions and interventions.
4.1. Strengths and limitations of the study
The strengths of this systematic review include being a highly practical method of reviewing the literature with immediate and practical recommendations for practice. Using methods such as these can lead to practical improvements in diabetes prevention and management interventions to understand what works for whom, in what contexts and why. This review provided added value compared with conventional reviews, as it uses qualitative data to explore why certain interventions are effective or ineffective, and what interventions should be trialled in the future. We also followed a rigorous and comprehensive methodology, with duplicate screeners throughout title and abstract screening, full-text review and data extraction.
For the mixed-methods synthesis, we were highly dependent on descriptions of the interventions to determine which factors the intervention addressed. It was clear that some descriptions of the interventions were poorly detailed and therefore our mixed methods synthesis may have incorrectly categorised some interventions to be lacking certain factors that they actually did address. Additionally, as the method of sorting qualitative themes in the Dahlgren and Whitehead model is novel, some may contest the sorting decisions made of the authors. However, the model is used primarily to frame the qualitative synthesis and did not impact on the thematic analysis or subsequent mixed-methods synthesis conducted.
Importantly, the conclusions of this review are correlative in nature and it would be inappropriate to assume causation due to the observational nature of the analyses. Due to the quality of the quantitative studies being mainly of moderate or high risk of bias, the results should be interpreted with caution. Future intervention studies should comprehensively report intervention components and implementation and work to improve quality of their study designs.
A practical limitation of the mixed-methodology used is the time-intensive nature of the review. The review involves conducting two separate systematic reviews, and adding an additional synthesis to the qualitative and quantitative synthesis. While steps were taken to reduce the workload (e.g. searching for the qualitative and quantitative literature together), it may not be a practical method of reviewing the literature for researchers or practitioners with limited resources.
4.2. Comparisons with other studies
Some findings of this review support previous reviews. Two recent qualitative reviews on general perceptions of women with current and previous GD found several similar barriers to physical activity, including putting family before themselves; lack of time; limited childcare and bad weather (Dennison et al., 2019; Parsons et al., 2014). Another review looked exclusively at randomised controlled trials to increase physical activity in women with previous GDM and found no interventions resulted in significant changes in physical activity (Jones et al., 2017). The current review found four studies that significantly increased physical activity, three with pre-post study designs. Pre-post study designs cannot determine causality in interventions, but can provide a pragmatic and cost-effective ways of exploring an interventions' effects.
A recent review by Nielsen and colleagues highlighted the importance of family-contextualised interventions to increase physical activity in women with a history of GDM (Nielsen et al., 2018). Their narrative review highlighted that “much remains to be understood about what such strategies should involve if they are to be effective” (p. 717), and emphasised the need for multiple avenues of intervention, from psychological to social approaches (Nielsen et al., 2018). This review aimed to fill that gap in understanding by exploring what factors women with previous GDM say is important to them when considering physical activity and how well these factors are represented in previous trials of physical activity interventions.
5. Conclusions
The mixed-methods review process can help design more effective T2D management and prevention techniques for high-risk groups. Exploring what the target audience for an intervention says is an important step in understanding the problem the intervention is trying to address, as is reviewing what has been done before and why it has not worked previously. This review methodology systematically reviews both of these points effectively and efficiently to help design better interventions going forward.
The findings of this systematic review should be incorporated into future multifaceted interventions to effectively increase physical activity in women with previous GDM in a way that is participatory and theory-based. This review identified factors that should be addressed in effective interventions (e.g. childcare), which factors should perhaps be minimised or removed from interventions (e.g. education-only interventions about future risk of T2D and pedometer use), and which may be promising for future interventions (e.g. being a healthy role model for families). It is clear from this review that access to affordable childcare, providing appropriate social and community support and using relevant cultural activities are associated with more effective physical activity interventions for women with a history of GDM. Future interventions and research should explore the gaps and mismatches this review set out, including the effectiveness of addressing the following factors: lack of time and energy for physical activity; feeling guilty about taking time for oneself; putting off lifestyle change; walking interventions; healthcare support; lack of awareness or feeling helpless about future T2D risk; being a role model for family; going back to pre-GDM lifestyle and mental health and breastfeeding difficulties.
The following are the supplementary data related to this article.
Search strategies: final.
Summary of quantitative intervention studies.
Acknowledgments
Acknowledgements
This systematic review was undertaken as part of a Diabetes UK PhD studentship. The views expressed in this publication are those of the authors and not necessarily those of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to thank Russell Penman and Daniel Hillhouse for their assistance in duplicate-screening the studies, Marshall Dozier for her assistance in developing the search strategy and Jane Noyes for her advice about methodology.
Funding
This systematic review was undertaken as part of a Diabetes UK PhD studentship (16/0005562).
Conflicts of interest
The authors declare no conflicts of interest.
References
- 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study Lancet. 2009;374(9702):1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amer Diabet A. Management of diabetes in pregnancy. Obstet Gynec Survey. 2017;72(5):264–266. [Google Scholar]
- Amorim M.M.R., Katz L. InTech; 2011. Gestational Diabetes: Evidence-based Screening, Diagnosis and Treatment Gestational Diabetes. [Google Scholar]
- Aroda V.R., Christophi C.A., Edelstein S.L., Zhang P., Herman W.H., Barrett-Connor E.…Diabetes Prevention Program Research, G The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J. Clin. Endocrinol. Metab. 2015;100(4):1646–1653. doi: 10.1210/jc.2014-3761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay M., Small R., Davey M.A., Oats J.J., Forster D.A., Aylward A. Lived experience of gestational diabetes mellitus among immigrant South Asian women in Australia. Australian & New Zealand Journal of Obstetrics & Gynaecology. 2011;51(4):360–364. doi: 10.1111/j.1479-828X.2011.01322.x. [DOI] [PubMed] [Google Scholar]
- Bandyopadhyay M., Small R., Davey M.A. Attendance for postpartum glucose tolerance testing following gestational diabetes among South Asian women in Australia: a qualitative study. Int. J. Gynaecol. Obstet. 2015;131:E149. [Google Scholar]
- Bao W., Tobias D.K., Bowers K., Chavarro J., Vaag A., Grunnet L.G.…Zhang C. Physical activity and sedentary behaviors associated with risk of progression from gestational diabetes mellitus to type 2 diabetes mellitus. JAMA Intern. Med. 2014;174(7):1047. doi: 10.1001/jamainternmed.2014.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3(2):77–101. [Google Scholar]
- Brazeau, A. S., Leong, A., Meltzer, S. J., Cruz, R., DaCosta, D., Hendrickson-Nelson, M., … Mo, M. M. s. g. (2014a). Group-based activities with on-site childcare and online support improve glucose tolerance in women within 5 years of gestational diabetes pregnancy. Cardiovasc. Diabetol., 13(104), 104. doi: 10.1186/1475-2840-13-104. [DOI] [PMC free article] [PubMed]
- Brazeau A.S., Leong A., Meltzer S.J., Dacosta D., Hendrickson-Nelson M., Joseph L., Das-Gupta K. A novel intervention to improve glucose tolerance in women with past gestational diabetes. Diabetes. 2014;63:A171. doi: 10.1186/1475-2840-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazeau, A. S., Meltzer, S. J., Pace, R., Garfield, N., Godbout, A., Meissner, L., … Dasgupta, K. (2018). Health behaviour changes in partners of women with recent gestational diabetes: a phase IIa trial. BMC Public Health, 18(1), 575. doi: 10.1186/s12889-018-5490-x. [DOI] [PMC free article] [PubMed]
- Chasan-Taber L. Lifestyle interventions to reduce risk of diabetes among women with prior gestational diabetes mellitus. Best Practice & Research in Clinical Obstetrics & Gynaecology. 2015;29(1):110–122. doi: 10.1016/j.bpobgyn.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung N.W., Smith B.J., Henriksen H., Tapsell L.C., McLean M., Bauman A. A group-based healthy lifestyle program for women with previous gestational diabetes. Diabetes Res. Clin. Pract. 2007;77(2):333–334. doi: 10.1016/j.diabres.2006.10.025. [DOI] [PubMed] [Google Scholar]
- Cheung N.W., Smith B.J., van Der Ploeg H.P., Cinnadaio N., Bauman A. A pilot structured behavioural intervention trial to increase physical activity among women with recent gestational diabetes. Diabetes Res. Clin. Pract. 2011;92(1):e27–e29. doi: 10.1016/j.diabres.2011.01.013. [DOI] [PubMed] [Google Scholar]
- Cooke A., Smith D., Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012;22(10):1435–1443. doi: 10.1177/1049732312452938. [DOI] [PubMed] [Google Scholar]
- Currie J. Motherhood, stress and the exercise experience: freedom or constraint? Leis. Stud. 2004;23(3):225–242. [Google Scholar]
- Dahlgren G., Whitehead M. Institute for future studies; Stockholm: 1991. Policies and Strategies to Promote Social Equity in Health. [Google Scholar]
- Dennison R., Ward R., Griffin S., Usher-Smith J. Women's views on lifestyle changes to reduce the risk of developing type 2 diabetes after gestational diabetes: a systematic review, qualitative synthesis and recommendations for practice. Diabet. Med. 2019:1–16. doi: 10.1111/dme.13926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran F. Gestational diabetes mellitus: perspectives on lifestyle changes during pregnancy and post-partum, physical activity and the prevention of future type 2 diabetes. Australian Journal of Primary Health. 2008;14(3):85–92. [Google Scholar]
- Doran F., Davis K. Gestational diabetes mellitus in Tonga: insights from healthcare professionals and women who experienced gestational diabetes mellitus. N. Z. Med. J. 2010;123(1326):59–67. [PubMed] [Google Scholar]
- Ferrara A., Ehrlich S.F. Strategies for diabetes prevention before and after pregnancy in women with GDM. Curr. Diabetes Rev. 2011;7(2):75–83. doi: 10.2174/157339911794940738. [DOI] [PubMed] [Google Scholar]
- Ferrara A., Hedderson M.M., Albright C.L., Ehrlich S.F., Quesenberry C.P., Jr., Peng T.…Crites Y. A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial. Diabetes Care. 2011;34(7):1519–1525. doi: 10.2337/dc10-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrara, A., Hedderson, M. M., Albright, C. L., Brown, S. D., Ehrlich, S. F., Caan, B. J., … Quesenberry, C. P., Jr. (2014). A pragmatic cluster randomized clinical trial of diabetes prevention strategies for women with gestational diabetes: design and rationale of the Gestational Diabetes' Effects on Moms (GEM) study. BMC Pregnancy & Childbirth, 14, 21. doi: 10.1186/1471-2393-14-21. [DOI] [PMC free article] [PubMed]
- Ferrara A., Hedderson M.M., Brown S.D., Albright C.L., Ehrlich S.F., Tsai A.L.…Quesenberry C.P. The comparative effectiveness of diabetes prevention strategies to reduce postpartum weight retention in women with gestational diabetes mellitus: the Gestational Diabetes' Effects on Moms (GEM) cluster randomized controlled trial. Diabetes Care. 2016;39(1):65–74. doi: 10.2337/dc15-1254. http://onlinelibrary.wiley.com/ Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaudreau S., Michaud C. Cultural factors related to the maintenance of health behaviours in Algonquin women with a history of gestational diabetes. Chronic Diseases and Injuries in Canada. 2012;32(3):140–148. [PubMed] [Google Scholar]
- Gilinsky A.S., Dale H., Robinson C., Hughes A.R., McInnes R., Lavallee D. Efficacy of physical activity interventions in post-natal populations: systematic review, meta-analysis and content coding of behaviour change techniques. Health Psychol. Rev. 2015;9(2):244–263. doi: 10.1080/17437199.2014.899059. [DOI] [PubMed] [Google Scholar]
- Gilinsky A.S., Kirk A.F., Hughes A.R., Lindsay R.S. Lifestyle interventions for type 2 diabetes prevention in women with prior gestational diabetes: a systematic review and meta-analysis of behavioural, anthropometric and metabolic outcomes. Prev. Med. Rep. 2015;2:448–461. doi: 10.1016/j.pmedr.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graco M., Garrard J., Jasper A.E. Participation in physical activity: perceptions of women with a previous history of gestational diabetes mellitus. Health Promot J Austr. 2009;20(1):20–25. doi: 10.1071/he09020. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T., Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. Bmj. 2005;331(7524):1064–1065. doi: 10.1136/bmj.38636.593461.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guideline N. 2015. Diabetes in Pregnancy: Management From Preconception to the Postnatal Period. February. [Google Scholar]
- Guo J., Chen J.L., Whittemore R., Whitaker E. Postpartum lifestyle interventions to prevent type 2 diabetes among women with history of gestational diabetes: a systematic review of randomized clinical trials. J. Women's Health. 2016;25(1):38–49. doi: 10.1089/jwh.2015.5262. [DOI] [PubMed] [Google Scholar]
- Hawkins, J., Madden, K., Fletcher, A., Midgley, L., Grant, A., Cox, G., … Bonell, C. (2017). Development of a framework for the co-production and prototyping of public health interventions. BMC Public Health, 17(1), 689. [DOI] [PMC free article] [PubMed]
- Jones E., Fraley H., Mazzawi J. Appreciating culture and recent motherhood: tailoring postpartum lifestyle interventions to promote cardiometabolic health in women with prior gestational diabetes. Nurs. Res. 2015;64(2):E75–E76. doi: 10.1007/s10995-016-2092-z. [DOI] [PubMed] [Google Scholar]
- Jones E.J., Fraley H.E., Mazzawi J. Appreciating recent motherhood and culture: a systematic review of multimodal postpartum lifestyle interventions to reduce diabetes risk in women with prior gestational diabetes. Matern. Child Health J. 2017;21(1):45–57. doi: 10.1007/s10995-016-2092-z. [DOI] [PubMed] [Google Scholar]
- Kim C., Draska M., Hess M.L., Wilson E.J., Richardson C.R. A web-based pedometer programme in women with a recent history of gestational diabetes. Diabet. Med. 2012;29(2):278–283. doi: 10.1111/j.1464-5491.2011.03415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lie M.L., Hayes L., Lewis-Barned N.J., May C., White M., Bell R. Preventing type 2 diabetes after gestational diabetes: women's experiences and implications for diabetes prevention interventions. Diabet. Med. 2013;30(8):986–993. doi: 10.1111/dme.12206. [DOI] [PubMed] [Google Scholar]
- Liss M., Schiffrin H.H., Rizzo K.M. Maternal guilt and shame: the role of self-discrepancy and fear of negative evaluation. J. Child Fam. Stud. 2013;22(8):1112–1119. [Google Scholar]
- Liu H., Wang L., Zhang S., Leng J., Li N., Li W.…Hu G. One-year weight losses in the Tianjin Gestational Diabetes Mellitus Prevention Programme: a randomized clinical trial. Diabetes Obes. Metab. 2018;20(5):1246–1255. doi: 10.1111/dom.13225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- Mays N., Pope C. Rigour and qualitative research. Bmj. 1995;311(6997):109–112. doi: 10.1136/bmj.311.6997.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre H.D., Peacock A., Miller Y.D., Koh D., Marshall A.L. Pilot study of an individualised early postpartum intervention to increase physical activity in women with previous gestational diabetes. Int. J. Endocrinol. 2012;2012 doi: 10.1155/2012/892019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcmanus R.M., Donovan L., Miller D., Mottola M., Giroux I., Rosas-Arellano P. Families Defeating Diabetes (FDD): a Canadian intervention for family-centered diabetes prevention following gestational diabetes (GDM): initial results. Diabetes. 2015;64:A632. [Google Scholar]
- Miyazaki C., Tanase-Nakao K., Arata N., Mori R., Kawasaki M., Ota E. Nonpharmacological interventions to prevent type 2 diabetes in women diagnosed with gestational diabetes mellitus: a systematic overview. Diabetol. Int. 2017;8(2):160–180. doi: 10.1007/s13340-017-0316-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Mukerji G., McTavish S., Glenn A., Delos-Reyes F., Price J., Wu W.…Lipscombe L.L. An innovative home-based cardiovascular lifestyle prevention program for women with recent gestational diabetes: a pilot feasibility study. Can. J. Diabetes. 2015;39(6):445–450. doi: 10.1016/j.jcjd.2015.08.002. [DOI] [PubMed] [Google Scholar]
- Nicholson W.K., Beckham A.J., Hatley K., Diamond M., Johnson L.S., Green S.L., Tate D. The Gestational Diabetes Management System (GooDMomS): development, feasibility and lessons learned from a patient-informed, web-based pregnancy and postpartum lifestyle intervention. BMC Pregnancy & Childbirth. 2016;16(1):277. doi: 10.1186/s12884-016-1064-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicklas J.M., Zera C.A., England L.J., Rosner B.A., Horton E., Levkoff S.E., Seely E.W. A web-based lifestyle intervention for women with recent gestational diabetes mellitus: a randomized controlled trial. Obstet. Gynecol. 2014;124(3):563. doi: 10.1097/AOG.0000000000000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen K.K., Grunnet L.G., Maindal H.T., Worksh D.D.A.W. Prevention of type 2 diabetes after gestational diabetes directed at the family context: a narrative review from the Danish Diabetes Academy symposium. Diabet. Med. 2018;35(6):714–720. doi: 10.1111/dme.13622. [DOI] [PubMed] [Google Scholar]
- O'Reilly, S. L., Dunbar, J. A., Versace, V., Janus, E., Best, J. D., Carter, R., … Group, M. S. (2016). Mothers after gestational diabetes in Australia (MAGDA): a randomised controlled trial of a postnatal diabetes prevention program. PLoS Med., 13(7), e1002092. doi: 10.1371/journal.pmed.1002092. [DOI] [PMC free article] [PubMed]
- Parsons J., Ismail K., Amiel S., Forbes A. Perceptions among women with gestational diabetes. Qual. Health Res. 2014;24(4):575–585. doi: 10.1177/1049732314524636. [DOI] [PubMed] [Google Scholar]
- Peacock A.S., Bogossian F., McIntyre H.D., Wilkinson S. A review of interventions to prevent type 2 diabetes after gestational diabetes. Women & Birth: Journal of the Australian College of Midwives. 2014;27(4):e7–e15. doi: 10.1016/j.wombi.2014.09.002. [DOI] [PubMed] [Google Scholar]
- Peacock A.S., Bogossian F.E., Wilkinson S.A., Gibbons K.S., Kim C., McIntyre H.D. A randomised controlled trial to delay or prevent type 2 diabetes after gestational diabetes: walking for exercise and nutrition to prevent diabetes for you. Int. J. Endocrinol. 2015;2015:423717. doi: 10.1155/2015/423717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen A.L.W., Terkildsen Maindal H., Juul L. How to prevent type 2 diabetes in women with previous gestational diabetes? A systematic review of behavioural interventions. Prim Care Diabetes. 2017;11(5):403–413. doi: 10.1016/j.pcd.2017.05.002. [DOI] [PubMed] [Google Scholar]
- Perez-Ferre, N., Del Valle, L., Torrejon, M. J., Barca, I., Calvo, M. I., Matia, P., … Calle-Pascual, A. L. (2015). Diabetes mellitus and abnormal glucose tolerance development after gestational diabetes: a three-year, prospective, randomized, clinical-based, Mediterranean lifestyle interventional study with parallel groups. Clinical nutrition (Edinburgh, Scotland), 34(4), 579–585. doi: 10.1016/j.clnu.2014.09.005. [DOI] [PubMed]
- Philis-Tsimikas A., Fortmann A.L., Dharkar-Surber S., Euyoque J.A., Ruiz M., Schultz J., Gallo L.C. Dulce mothers: an intervention to reduce diabetes and cardiovascular risk in Latinas after gestational diabetes. Transl. Behav. Med. 2014;4(1):18–25. doi: 10.1007/s13142-014-0253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razee H., van Der Ploeg H., Blignault I., Smith B., Bauman A., McLean M., Cheung N. Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promotion Journal of Australia. 2010;21(2):130–137. doi: 10.1071/he10130. [DOI] [PubMed] [Google Scholar]
- Reinhardt J.A., Grzegrzulka R., Timperley J.G., Van Der Ploeg H.P. Implementing lifestyle change through phone-based motivational interviewing in rural-based women with previous gestational diabetes mellitus. Health Promotion Journal of Australia. 2012;23(1):5–9. doi: 10.1071/he12005. [DOI] [PubMed] [Google Scholar]
- Robert S.A., Booske B.C., Rigby E., Rohan A.M. Public views on determinants of health, interventions to improve health, and priorities for government. WMJ. 2008;107(3):124–130. [PubMed] [Google Scholar]
- Schardt C., Adams M.B., Owens T., Keitz S., Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC medical informatics and decision making. 2007;7(1):16. doi: 10.1186/1472-6947-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.J., Cheung N.W., Bauman A.E., Zehle K., McLean M. Postpartum physical activity and related psychosocial factors among women with recent gestational diabetes mellitus. Diabetes Care. 2005;28(11):2650–2654. doi: 10.2337/diacare.28.11.2650. [DOI] [PubMed] [Google Scholar]
- Smith B.J., Cinnadaio N., Cheung N.W., Bauman A., Tapsell L.C., Ploeg H.P. Investigation of a lifestyle change strategy for high-risk women with a history of gestational diabetes. Diabetes Res. Clin. Pract. 2014;106(3):e60–e63. doi: 10.1016/j.diabres.2014.09.035. http://onlinelibrary.wiley.com/ Retrieved from. [DOI] [PubMed] [Google Scholar]
- Tang J.W., Foster K.E., Pumarino J., Ackermann R.T., Peaceman A.M., Cameron K.A. Perspectives on prevention of type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African-American and White women. Matern. Child Health J. 2015;19(7):1526–1534. doi: 10.1007/s10995-014-1657-y. [DOI] [PubMed] [Google Scholar]
- Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008;8(1):45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tierney, M., O'Dea, A., Danyliv, A., Noctor, E., McGuire, B., Glynn, L., … Dunne, F. (2015). Factors influencing lifestyle behaviours during and after a gestational diabetes mellitus pregnancy. Health Psychol Behav Med, 3(1), 204–216. doi: 10.1080/21642850.2015.1073111. [DOI]
- Wight D., Wimbush E., Jepson R., Doi L. Six steps in quality intervention development (6SQuID) J. Epidemiol. Community Health. 2015;70(5):520–525. doi: 10.1136/jech-2015-205952. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies: final.
Summary of quantitative intervention studies.