Abstract
Background
Epilepsy is still very prevalent in Sub-Saharan Africa, particularly in remote, poverty-confronted onchocerciasis-endemic villages. It constitutes a significant burden for the families and communities. However, the financial costs of managing persons with epilepsy (PWE) have not been assessed in these settings. Proper cost analyses will facilitate future health interventions.
Methods
In November 2017, persons with epilepsy (PWE) and their caretakers were recruited at health centres of the Logo health zone in the Democratic Republic of Congo. A pre-tested questionnaire was administered to collect information on both direct and indirect costs of epilepsy, as well as household income of participants.
Findings
The weighted mean cost of epilepsy was 241.2 USD per PWE per year (50.2% direct cost, 49.8% indirect cost). Epilepsy-related expenses represented 46.5% of the mean household income. Traditional medicine accounted for 68.2% of the direct cost. An estimated cumulative cost of 1929.6 USD attributable to epilepsy had been incurred by the populations of the Logo health zone for each PWE in the community.
Interpretation
Almost half of the household revenue was spent on epilepsy care. Expenses on traditional medicine must be discouraged via education and regular provision of affordable anti-epileptic drugs. Prevention of onchocerciasis-associated epilepsy using optimal control measures will avert additional epilepsy-related costs on the community. Early diagnosis and proper management of epilepsy would be economically beneficial in the study villages.
Keywords: Epilepsy, Cost, Democratic Republic of Congo, Onchocerciasis, Traditional medicine, Burden
Research in context
Evidence before this study
Epilepsy is a major public health problem in Sub-Saharan Africa, where wide treatment gaps result in high comorbidity and mortality. Previous studies have suggested that financial limitations to acquire antiepileptic drugs are the main reasons for the poor treatment adherence by persons with epilepsy. We searched PubMed for studies reporting the economic burden of epilepsy in Africa and realized that no data is available in the Democratic Republic of Congo, where epilepsy prevalence is very high especially in onchocerciasis-endemic areas with inadequate control measures.
Added value of this study
In this study, we analysed the different costs relating to epilepsy and reported for the first time the economic burden of epilepsy for families and communities in the Democratic Republic of Congo. Our findings reveal that the cost of managing a person with epilepsy in rural Democratic Republic of Congo amounts to almost half of the household income of our study participants. Additionally, persons with epilepsy spend the greater part of their limited resources on traditional medicine. Consequently, they are unable to afford proper medical treatment and frequently develop complications which further increase cost. We also show the economic benefits of preventing epilepsy and providing recommended care to affected persons.
Implications of all available evidence
The economic burden of epilepsy in rural settings can be reduced by ensuring continuous availability of cheap antiepileptic drugs. In villages which are endemic for onchocerciasis, reinforcing onchocerciasis elimination measures may prevent new cases of epilepsy in children, thereby curbing related costs.
Alt-text: Unlabelled Box
1. Background
Epilepsy remains a major public health concern around the world and especially in developing countries where 80% of the affected 50 million persons currently live. The situation is even more deplorable as 75% of persons with epilepsy (PWE) in resource-poor settings do not receive treatment [1]. One of the main reasons for this wide epilepsy treatment gap is the limited finances to afford continuous treatment by affected families [2], [3]. The financial burden is exacerbated by the absence of health insurance in most developing countries, resulting in most expenditures being out-of-pocket [4]. A good understanding of the economic costs associated with epilepsy care could help stakeholders to address the root causes of the wide treatment gap, thus ensuring better health outcomes for the PWE. However, data on epilepsy cost is relatively scarce in developing countries, as only a few studies have been realized in that domain [4], [5], [6], [7] and none in the Democratic Republic of Congo.
The components of a cost-of-illness analysis can be categorized into direct costs (cost of medical treatment, paraclinical workups and other non-medical expenditures directly related to patient management such as transportation cost to the hospital or home care expenses); indirect costs (due to lost productivity and/or earnings because of the illness); and intangible costs (related to the emotional and social impacts of the illness on the economy) [4]. Obtaining data on the economic cost of epilepsy can be a daunting task because PWE have different treatment options, seizure severity and accessibility to health facility, all of which can influence expenditure and losses [8]. Moreover, the total economic cost of any condition cannot be fully grasped because of the near impossibility of estimating intangible costs in monetary terms. Notwithstanding, evaluating direct cost alone and addressing its causes can potentially reduce indirect cost (due to increased productivity) and intangible cost (due to improved quality of life) [4]. Therefore, assessing health-related expenses will go a long way to reduce cost by implementing optimal solutions based on evidence [9]. This holds true for epilepsy which is a chronic, stigmatizing condition for which entire families often lose money, labour and time because of a single PWE. This study throws some light on the cost of managing PWE in rural Ituri as well as the financial burden for the family and community, so as to make recommendations for better outcomes at the least cost.
2. Methods
2.1. Study Site
This study was carried out in the Ituri province of the Democratic Republic of Congo (DRC), more precisely in the Logo Health Zone in the villages of Draju and Kanga. The total population in this health zone at the time of the study was 255,485 [10]. Although this area is hyperendemic for onchocerciasis, some villages had never received ivermectin for onchocerciasis control [11]. Previous surveys have established epidemiological evidence suggesting that areas with high onchocerciasis transmission are prone to increased prevalence of epilepsy, in what is known as onchocerciasis-associated epilepsy (OAE) [12]. A recent community-based study by our research team showed an epilepsy prevalence of 4.6% in the villages where this study was performed [13]. Most of the population was involved in subsistence farming and living standards were very low as a result of poverty. Consequently, many PWE were not properly treated. Due to the proximity with the Ugandan border, the main currency used in this part of the country was the Ugandan shilling. The American dollar (USD) was also accepted by some farmers and petty traders.
The Logo health zone had one reference hospital with five doctors, and 26 health centres headed by nurses. There was no neurologist, no electroencephalogram (EEG) nor imaging facilities (CT scan, Magnetic Resonance Imaging) for adequate investigation of epilepsy. Also, there was no health insurance to cover medical expenses. Drug supply followed a regional distribution network established by the government. Antiepileptic drugs (AEDs) were supplied to the reference hospital irregularly. Each PWE was expected to pay a monthly sum of 7000 Ugandan shillings (about 2 USD) for a medical consultation and AED refill at the reference hospital; however, these AEDs did not reach the local health centres. As a result, there was a proliferation of private drug vendors who retailed AEDs locally at arbitrarily high costs, up to 20 USD in some cases [14]. Recently, our research team at the Global Health Institute (University of Antwerp, Belgium) partnered with the organization Malteser International to continuously provide free AEDs for all PWE in the Logo Health Zone [13]. There were several traditional healers in the villages as well.
2.2. Definition of Terms and Data Collection
Epilepsy was defined as the occurrence of at least two unprovoked seizures separated by 24 h or more [15]. Based on this definition, we recruited PWE and their families to participate in an epilepsy study by our research team in the Draju and Kanga health centres of the Logo Health Zone during the month of November 2017. A questionnaire to investigate the financial burden of epilepsy on the affected families was elaborated and pre-tested on the local population (see Supplementary appendix 1). Villages were sensitized by community health workers and PWE reported to the health centres with at least one caretaker. Potential participants were informed and clarified about the study in the local Alur language by one of the investigators (DWR). After giving their signed informed consent at a registration desk, participants were sent to a consultation room to be clerked by a physician who doubled as investigator in charge of administering the questionnaire. Local community health workers served as interpreters to communicate the questions in the local Alur language. Questions were asked about their monthly expenditure on AEDs, hospital consultations and follow-up for epilepsy, paraclinical examinations, transport for epilepsy-related purposes (AED purchase or coming to the hospital for follow-up), as well as expenses on traditional healers; all these constituted epilepsy-related direct cost. Indirect cost was evaluated by asking for the number of days lost by the PWE due to seizures, and the number of days lost by a caretaker when watching over the PWE. Finally, the average monetary revenue per month was noted for each investigated household.
2.3. Estimation of Costs in Monetary Terms
Direct costs such as consultation fee, paraclinical exams, hospitalization fee and price of AED were obtained from the PWE and their families. Given that the major means of transport in such rural settings was by motor bikes, the cost of transport for epilepsy-related issues was estimated based on the amount of money paid by the PWE and/or the caretaker to a transporting motor bike driver. Participants or families who owned motor bikes by themselves were asked for the cost of fuel when running epilepsy-related errands. Some PWE consulted traditional healers on an irregular basis; for each PWE who did, we asked what it costs them every year (in cash and in kind), under normal circumstances, to visit the traditional healer because of epilepsy. The average traditional medicine expenditure for a normal year was divided by 12 to obtain monthly costs. To quantify in-kind payments, we averaged the cost of a chicken to be worth 10,000 Ugandan shillings, and a goat/sheep to cost 60,000 Ugandan shillings based on local prices at the time of the study. The total monthly income of a household was taken as the total amount of money all household members can cumulatively generate on average from their respective activities every month, which in most cases was the sales of agricultural products.
For indirect costs, we attributed a monetary value to the number of days of work lost by the PWE and their caretakers because of epilepsy-related causes. This was done by expressing these lost days as multiples of the Gross Domestic Product (GDP) per capita per day as previously described by other authors [5].
Direct, indirect and total costs were converted to the American dollar (USD) using the exchange rate of 1 USD = 3600 Ugandan shillings which was routinely applicable at our study site in November 2017. Comparison of epilepsy cost across countries and years was done by converting all values to 2016 international dollars. We proceeded by first inflating all values in local currency from the study year to 2016 values using the Consumer Price Index, and thereafter converting the local currency to 2016 international dollars by means of the power purchasing parity (PPP) for private consumption. All indicators were obtained from the World Bank official website (https://data.worldbank.org/indicator/).
2.4. Data Analysis
The collected information was entered into Microsoft Excel 2016 spreadsheets (Microsoft Corporation, USA) and analysed using GraphPad Prism version 5. We constructed a Tornado diagram using RStudio Version 0.99.491. For each epilepsy-related expenditure, only PWE who spent in that particular aspect were included in the analysis. For instance, the mean cost of AEDs was calculated using only the sub-population of PWE who reported spending on AED purchase. Categorical data was presented as percentages, while continuous cost data was expressed as mean ± standard deviation (SD) [16]. During statistical testing, any p-value < 0.05 was considered to be significant.
2.5. Ethical Considerations
All participants gave an informed consent to answer epilepsy cost-related questions. For minors, consent was given by the parent or legal guardian who also provided the answers to the questions. All data was treated confidentially. In addition, a community-based epilepsy treatment programme was established to care for PWE in the study villages.
3. Results
3.1. Socio-demographic Characteristics of Study Participants
A total of 258 PWE were recruited into the study, with 124 (48.1%) being female. The median age was 20 years (IQR: 15–29), and the median duration of epilepsy was 8 years (IQR: 3–14). Of the 258 PWE, 201 (77.9%) were farmers. Twelve (4.9%) of the 244 households had two or more PWE.
3.2. Direct Cost of Epilepsy
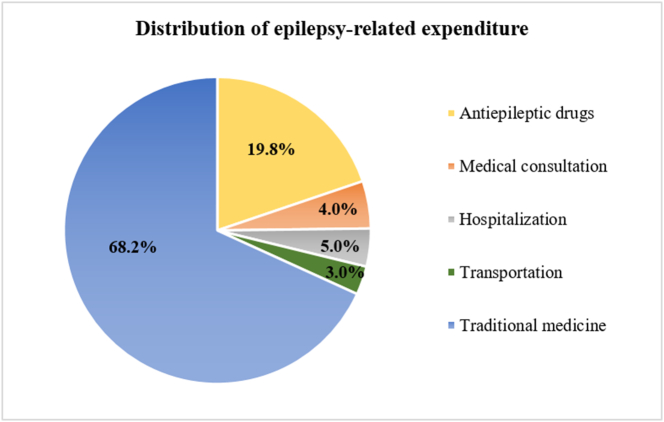
The mean direct cost of epilepsy, after weighting with the proportion of PWE spending on the respective items, was 10.1 USD per PWE per month (Table 1). Traditional medicine cost was most prominent, accounting for 68.2% of the mean direct cost (Fig. 1). Sixty-five percent of traditional medicine cost was paid in cash, while 35% was supplied in kind. However, these proportions were estimated based on interviews of only 68 PWE, because some investigators reported the total traditional medicine cost without distinguishing cash and kind payments. Nothing was spent on paraclinical investigations for epilepsy because they were unavailable at the study site. The weighted median direct cost of epilepsy was 3.8 USD per month.
Table 1.
Monthly direct costs of epilepsy.
| Item | Number of PWE spending on this item (%) | Cost in USD: mean (SD) | Weighted mean direct cost (USD) | Proportion of direct cost |
|---|---|---|---|---|
| Antiepileptic drugs | 163 (63.2%) | 3.2 (5.4) | 2.0 | 19.8% |
| Medical consultation | 44 (17.1%) | 3.0 (5.0) | 0.5 | 5.0% |
| Hospitalization | 11 (4.3%) | 8.8 (11.3) | 0.4 | 4.0% |
| Paraclinical investigations | 0 (0%) | 0 | 0 | 0% |
| Transportation | 30 (11.6%) | 2.8 (4.8) | 0.3 | 3.0% |
| Traditional medicine | 126 (48.8%) | 14.2 (23.8) | 6.9 | 68.2% |
| Total weighted mean direct cost | 10.1 | 100.0% | ||
Weighted median direct cost of epilepsy: [(0.632 ∗ 1.4) + (0.171 ∗ 0.2) + (0.043 ∗ 0.5) + (0.116 ∗ 1.4) + (0.488 ∗ 5.6)] = 3.8 USD.
PWE: Person(s) with epilepsy; SD: Standard deviation; USD: American dollar.
Fig. 1.
Distribution of epilepsy-related expenditure in Ituri, DRC.
3.3. Indirect Cost of Epilepsy
When considering all 258 PWE and their 244 caretakers in the households, the total number of work days lost due to epilepsy was 2790.2 days/month giving an average of 5.6 days lost per person per month. PWE lost more days compared with caretakers (mean number of days lost: 7.4 days vs 3.9 days; unpaired t-test: p < 0.0001). Given that the Gross Domestic Product (GDP) of DRC in 2017 was 37.241 billion American dollars (USD) for a total population of 81,339,988 persons [17], the GDP per capita was calculated as 457.8 USD and the GDP per capita per day was 1.25 USD. Using this unit of conversion, the weighted mean indirect cost due to epilepsy was 10.0 USD per PWE monthly (Table 2). Although children are considered not to actively contribute to the family income because they do not work, in the event of seizures, they prevent their adult parents/guardians from working as well. The resulting economic impact is included in the 28.0% of indirect cost due to the days of work lost by the caretaker (Table 2). The weighted median indirect cost was 4.6 USD per month.
Table 2.
Monthly indirect costs of epilepsy.
| Item | Number of persons affected (%) | Number of days of work lost: mean (SD) | Cost in USD | Weighted mean cost (USD) | Percentage of indirect cost |
|---|---|---|---|---|---|
| Indirect cost incurred by PWE | 199/258 (77.1%) | 7.4 (8.4) | 9.3 | 7.2 | 72.0% |
| Indirect cost incurred by caretaker or family | 138/244 (56.6%) | 3.9 (5.8) | 4.9 | 2.8 | 28.0% |
| Total weighted mean indirect cost | 10.0 | 100.0% | |||
Weighted median indirect cost of epilepsy: [(0.771 ∗ 5) + (0.566 ∗ 1.3)] = 4.6 USD.
PWE: Person(s) with epilepsy; SD: Standard deviation; USD: American dollar.
3.4. Total Cost of Epilepsy
Summing up the weighted means of the direct and indirect costs of epilepsy, we obtained a monthly total epilepsy cost of 20.1 USD (50.2% direct cost, 49.8% indirect cost). This corresponds to an annual cost of 241.2 USD per PWE. Considering the median duration of epilepsy in this community to be 8 years, the estimated cumulative cost incurred due to epilepsy amounted to 1929.6 USD per PWE. With a prevalence of 4.6% and a total population of 255,485 in the Logo Health zone, we estimate 11,752 PWE in this area corresponding to an economic burden of 2,834,582.4 USD annually. Table 3 shows a comparison of epilepsy cost as reported in our study with findings in other developing countries.
Table 3.
Annual costs of epilepsy in developing countries.
| Country/year of study | Settings and methods | Annual direct cost (I$a) | Annual indirect cost (I$a) | Annual total cost (I$a) |
|---|---|---|---|---|
| India, 1998 [4] |
|
580.7 | 1563.9 | 2144.6 |
| Burundi, 2001 [5] |
|
26.3b | 134.7b | 161.0b |
| South Africa, 2011 [6] |
|
116.3 | NA | 116.3 |
| Nigeria, 2009 [7] |
|
Varied. Overall 71.8% of total mean cost | Varied. Overall 28.2% of total mean cost | 1819.6 (median) |
| DRC, 2017 (this study) |
|
343.6 | 340.2 | 683.8 |
I$: 2016 International dollars.
Only PWE treated with AED.
The tornado diagram in Fig. 2 shows a non-parametric one-way sensitivity analysis of the different elements contributing to epilepsy cost, using the weighted median costs as baseline for each parameter. In this diagram, the extent of variation for the different epilepsy-related costs (using the 25th and 75th percentiles) are shown, as well as their possible deviations from the total weighted median cost of 8.4 USD reported in our study population. We observed that indirect costs and traditional medicine costs had the widest margins of variation, with a tendency to overestimate.
Fig. 2.
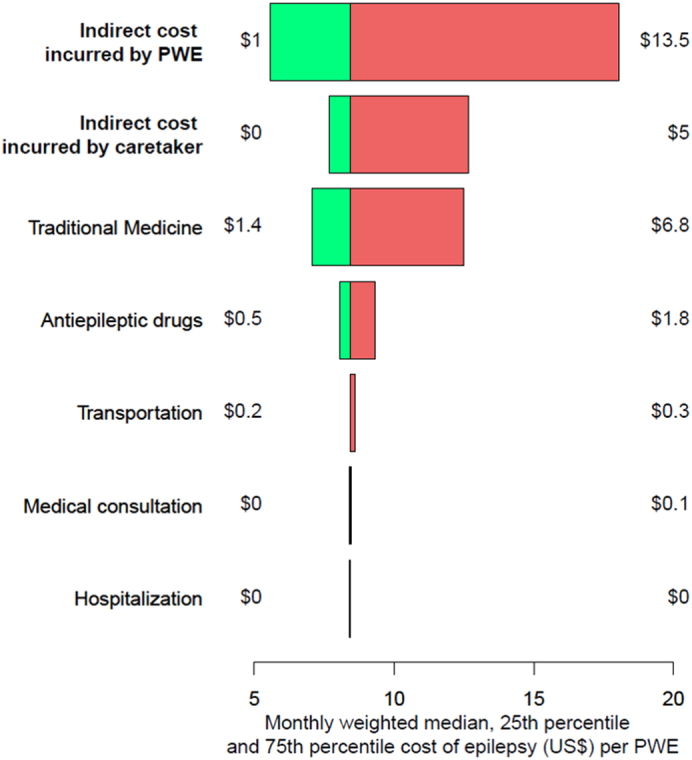
Tornado diagram for the cost of epilepsy per PWE in Ituri. The horizontal axis represents the monthly weighted median cost of epilepsy per PWE, for different cost inputs. The central baseline value is 8.4 USD, corresponding to the total weighted median cost per month. The values beside the horizontal bars represent the variation in cost if the 25th percentile (green: decrease from median cost) or 75th percentile (red: increase from median cost) are used as input parameters. Indirect costs in bold. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
The mean monetary income per month in the study households was 21.7 ± 27.6 USD (median = 13.9 USD; IQR: 8.0–27.8). The monetary expenses (direct costs) due to epilepsy represented 46.5% of the household income; in addition, the total economic cost of epilepsy amounted to 52.7% of the GDP per capita (Fig. 3). The annual cost of providing recommended epilepsy care to one PWE in rural DRC was estimated at 58.0 USD in the first year and 7.0 USD per year subsequently, much lower than the reported epilepsy expenditure in our study (see Supplementary appendix 2).
Fig. 3.
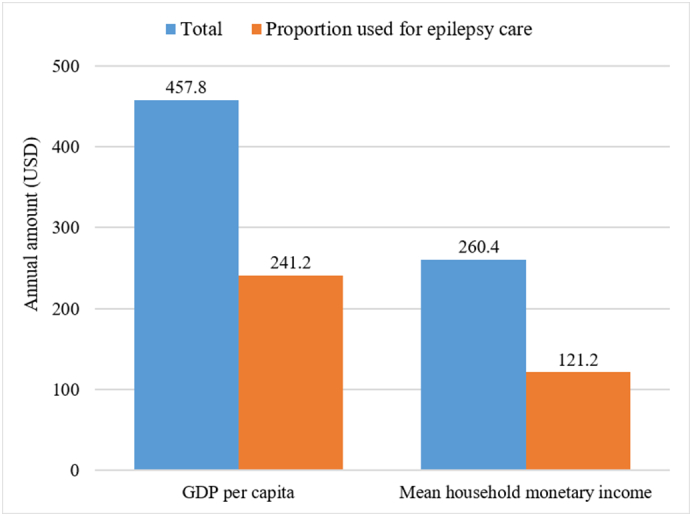
Comparison between annual household income, GDP per capita and epilepsy cost in rural Ituri.
4. Discussion
To the best of our knowledge, this is the first study investigating the economic cost of epilepsy in onchocerciasis-endemic communities in the DRC. Although our one-way sensitivity analysis showed a tendency to overestimate, we were able to provide the approximate costs incurred by a family due to epilepsy, and to calculate a realistic community burden of epilepsy in Ituri using weighted means. Our findings could prove useful in conducting cost-effectiveness analyses for appropriate interventions such as AED provision and ivermectin mass drug administration in affected communities, more so as we show that providing recommended epilepsy care in these remote villages would be less costly than the reported epilepsy expenditures.
The cost of managing a PWE in rural Ituri amounted to almost half of the household income. This leaves the family with very little for monthly subsistence, and therefore results in a vicious circle of poverty. Compared to other developing countries, the annual epilepsy cost in DRC was lower than that reported in Nigeria and India, but still higher than findings from South Africa and Burundi. Possible reasons for this discrepancy include the fact that in South Africa, AED expenditure was zero (provided for free) and indirect costs were not reported; while in Burundi, cost due to traditional medicine was not taken into account (Table 3). The differences in methodological approaches when conducting cost-of-illness studies [18] must also be taken into account when comparing epilepsy cost between countries. Although our data was obtained from declarations of the PWE and families which are subject to recall bias, we consider it to be fairly accurate because the chronic nature of epilepsy warrants habitual expenses which are usually well calculated and known in advance by the household. In fact, a previous study on epilepsy cost in India noted a good concordance between the cost reported by the patient and the cost computed as per the hospital prescriptions [4].
The bulk of the direct epilepsy cost went into traditional medicine. The high demand for traditional healers despite their exorbitant cost may seem paradoxical, but can be explained by their proximity to the population and their flexible payment modalities which range from cash, kind, labour or even credit/differed payments [19]. Also, the population is strongly rooted in cultural beliefs that epilepsy is mystical and prefers to take their PWE to traditional healers whom they believe have the power to solve their problem unlike modern medicine [14], [20]. Notwithstanding, the practise of traditional medicine has been shown to be detrimental to PWE, as this delays medical treatment and increases the risk of refractory scenarios upon initiation of AEDs [20]. In addition, despite the high cost of traditional treatment, it was not observed to yield superior clinical outcomes. It should therefore be discouraged among PWE, and medical services be made more available, affordable and attractive for the local population. It is expected that the cost due to traditional medicine should reduce if subsidized AEDs and epilepsy education are provided.
Expenditures on AED purchase were also important, constituting the second highest contributor to the direct cost. This finding concurs with data from other developing countries where AEDs constitute a major expenditure in epilepsy management [4], [5], [7]. In addition to being expensive for the local population, AEDs are not always available resulting in poor adherence to treatment [21]. Poor AED adherence can result in increased seizure frequency, increased cost for managing comorbidities, less productivity, greater social impact on the PWE and ultimately a multiplied economic burden from all fronts (direct, indirect and intangible costs). Indeed, epilepsy cost was shown to vary significantly depending on the severity of the condition and the response to treatment [22]. Therefore, an intervention aimed at increasing access to AEDs will have ripple effects on the overall economic cost of epilepsy. In our study, PWE spent on average 24 USD annually on AED because the drug was often unavailable at the health centres. Meanwhile, annual treatment with phenobarbital can be obtained for as low as 1 USD per year in the DRC [2], provided appropriate policies are adopted by the stakeholders to ensure routine availability of the drug at affordable prices.
The indirect cost of epilepsy calculated on the basis of days lost by the PWE and/or caretaker due to seizures was 10.0 USD per month. This was however expected to vary depending on seizure control, because PWE with less seizures are likely to be more productive resulting in reduced indirect cost. Indirect cost constituted only 49.8% of the total epilepsy cost in our study population in contrast with findings from other developing countries [4], [5] as well as developed countries, where indirect costs are usually higher due to sick leaves [23]. The main reason accounting for this difference is the frequent resort to expensive traditional healers by our study participants which inflates the direct cost. Indirect costs further reduce the family's purchasing power thus narrowing the chances of buying AEDs. This cycle ultimately results in more poverty and catastrophic health outcomes.
The cumulative economic cost of epilepsy and the financial burden it constitutes for the community were high. This cost could be greatly reduced if early diagnosis of epilepsy and early seizure control are achieved. Therefore, a community-based framework for epilepsy management adapted for these rural settings is needed to fill this gap in epilepsy care [24]. In addition, for onchocerciasis-endemic areas like our study site where most cases of epilepsy are due to OAE, strengthening onchocerciasis control programs will reduce the incidence of epilepsy in the community [25]. This would save the community 241.2 USD per prevented new epilepsy case every year.
This study had some limitations: Our findings are far from being exhaustive because many items that contribute to direct cost were not taken into account, such as the extra home care expenses for PWE. Due to the incomplete nature of the data collected on traditional medicine cost, we were unable to perform sensitivity analyses on the in-kind payments for traditional treatment. Also, the management of epilepsy-related complications was not included in the analyses. Although GDP per capita had been used by other authors to estimate individual living standards [5], this approach may not be ideal in our case because of the much lower economic status in rural villages compared to urban settings, and the scarcity of data to calculate GDP reliably in the DRC. Furthermore, the cross-sectional design of our study did not permit us to account for potential future costs such as unemployment resulting from early school dropout, or denied professional opportunities due to epilepsy. Finally, the socio-economic background, patient history and remission with treatment vary greatly among PWE and this influences cost at the individual level.
5. Conclusion
The economic cost of epilepsy constitutes a major burden for PWE and their families in rural Ituri. Besides consulting traditional healers, most of the direct cost was attributed to the purchase of AEDs. Therefore, strategies to ensure regular access to affordable AEDs will not only cut down direct cost, but will ensure better health outcomes hence reducing indirect and intangible costs as well. Improved onchocerciasis control will also prevent new cases of OAE thus reducing community cost for epilepsy. In addition, community education is needed to reduce stigma and limit consultation of traditional healers, as this practice substantially increases costs but without a corresponding improvement in the quality of life of PWE.
Ethics Approval and Consent to Participate
This study was nested within an ongoing study (Ivermectin Treatment in Patients With Onchocerciasis-Associated Epilepsy: A Randomized Clinical Trial) in the DRC [11] and information was collected from consenting participants during recruitment and follow-up visits. Ethical approval for the trial was obtained from the University of Antwerp, Belgium (Registration number: B300201730821) and the University of Kinshasa, DRC (Approval number: ESP/CE/013/2018).
Availability of Data and Material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Funding
ERCPoC (European Research Council) grant 768815 (Robert Colebunders).
Authors' Contributions
JNSF and RC conceived the study. JNSF, MM, DWR, FN, RL, AA collected the data. JNSF and YI did data entry and cleaning. JNSF analysed the data. FV complemented the economic analyses, conceived the sensitivity analysis and the tornado diagram. JNSF wrote the first manuscript. All authors critically read and approved the final manuscript.
Acknowledgements
We thank the health authorities and the communities of the Logo Health Zone for their collaboration.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eclinm.2019.03.010.
Appendix. Supplementary Data
Supplementary material
References
- 1.World Health Organization Epilepsy fact sheet. 2018. http://www.who.int/mediacentre/factsheets/fs999/en/
- 2.World Health Organisation . WHO; Geneva: 2004. Epilepsy in the WHO African region: bridging the gap. [Google Scholar]
- 3.Dongmo L., Echouffo T.J.B., Njamnshi A., Poyi M.K., Victor S., Nourdi P.M. Difficulties faced in the management of epilepsy in rural Cameroon: the case of Mbangassina locality. Afr J Neurol Sci. 2003;22 [Google Scholar]
- 4.Thomas S.V., Sarma P.S., Alexander M., Pandit L., Shekhar L., Trivedi C. Economic burden of epilepsy in India. Epilepsia. 2001;42:1052–1060. doi: 10.1046/j.1528-1157.2001.0420081052.x. [DOI] [PubMed] [Google Scholar]
- 5.Nsengiyumwa G., Druet-Cabanac M., Nzisabira L., Preux P.M., Vergnenègre A. Economic evaluation of epilepsy in Kiremba (Burundi): a case-control study. Epilepsia. 2004;45:673–677. doi: 10.1111/j.0013-9580.2004.36303.x. [DOI] [PubMed] [Google Scholar]
- 6.Wagner R.G., Bertram M.Y., Gómez-Olivé F.X., Tollman S.M., Lindholm L., Newton C.R. Health care utilization and outpatient, out-of-pocket costs for active convulsive epilepsy in rural northeastern South Africa: a cross-sectional survey. BMC Health Serv Res. 2016;16 doi: 10.1186/s12913-016-1460-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lagunju I.A., Imam Z.O., Adedokun B.O. Cost of epilepsy in children attending a tertiary centre in Nigeria. Int Health. 2011;3:213–218. doi: 10.1016/j.inhe.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Begley C.E., Annegers J.F., Lairson D.R., Reynolds T.F. Estimating the cost of epilepsy. Epilepsia. 1999;40(Suppl. 8):8–13. doi: 10.1111/j.1528-1157.1999.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 9.Rabarison K.M., Bish C.L., Massoudi M.S., Giles W.H. Economic evaluation enhances public health decision making. Front Public Health. 2015;3 doi: 10.3389/fpubh.2015.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Division Provinciale de la Santé Ituri . Ministère de la Santé; Ituri, République Démocratique du Congo: 2017. Plan d'Action Opérationnel 2017 (DPS Ituri) [Google Scholar]
- 11.Colebunders R., Mandro M., Mukendi D., Dolo H., Suykerbuyk P., Van Oijen M. Ivermectin treatment in patients with onchocerciasis-associated epilepsy: protocol of a randomized clinical trial. JMIR Res Protoc. 2017;6:e137. doi: 10.2196/resprot.7186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaiser C., Pion S.D., Boussinesq M. Case-control studies on the relationship between onchocerciasis and epilepsy: systematic review and meta-analysis. PLoS Negl Trop Dis. 2013;7 doi: 10.1371/journal.pntd.0002147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lenaerts E., Mandro M., Mukendi D., Suykerbuyk P., Dolo H., Wonya'Rossi D. High prevalence of epilepsy in onchocerciasis endemic health areas in Democratic Republic of the Congo. Infect Dis Poverty. 2018;7 doi: 10.1186/s40249-018-0452-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dolo H., Mandro M., Wonya'Rossi D., Ngave F., Fraeyman J., Siewe J.N. Community perceptions of epilepsy and its treatment in an onchocerciasis endemic region in Ituri, Democratic Republic of Congo. Infect Dis Poverty. 2018;7 doi: 10.1186/s40249-018-0498-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher R.S., Acevedo C., Arzimanoglou A., Bogacz A., Cross J.H., Elger C.E. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 16.Doshi J.A., Glick H.A., Polsky D. Analyses of cost data in economic evaluations conducted alongside randomized controlled trials. Value Health. 2006;9:334–340. doi: 10.1111/j.1524-4733.2006.00122.x. [DOI] [PubMed] [Google Scholar]
- 17.The World Bank Data: Democratic Republic of Congo. 2017. https://data.worldbank.org/country/congo-dem-rep
- 18.Onukwugha E., McRae J., Kravetz A., Varga S., Khairnar R., Mullins C.D. Cost-of-illness studies: an updated review of current methods. PharmacoEconomics. 2016;34:43–58. doi: 10.1007/s40273-015-0325-4. [DOI] [PubMed] [Google Scholar]
- 19.Muela S.H., Mushi A.K., Ribera J.M. The paradox of the cost and affordability of traditional and government health services in Tanzania. Health Policy Plan. 2000;15:296–302. doi: 10.1093/heapol/15.3.296. [DOI] [PubMed] [Google Scholar]
- 20.Ma T.M., Ma T.M., Lelo G.M., Nkosi M.M., Madinga J., Kola C.K. Are the children with epilepsy treated traditionally a disadvantaged group? A pilot study. Pan Afr Med J. 2016;23 [Google Scholar]
- 21.Chin J.H. Epilepsy treatment in sub-Saharan Africa: closing the gap. Afr Health Sci. 2012;12 doi: 10.4314/ahs.v12i2.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tetto A., Manzoni P., Millul A., Beghi E., Garattini L., Tartara A. The costs of epilepsy in Italy: a prospective cost-of-illness study in referral patients with disease of different severity. Epilepsy Res. 2002;48:207–216. doi: 10.1016/s0920-1211(02)00013-x. [DOI] [PubMed] [Google Scholar]
- 23.Pugliatti M., Beghi E., Forsgren L., Ekman M., Sobocki P. Estimating the cost of epilepsy in Europe: a review with economic modeling. Epilepsia. 2007;48:2224–2233. doi: 10.1111/j.1528-1167.2007.01251.x. [DOI] [PubMed] [Google Scholar]
- 24.Van Diessen E., van der Maas F., Cabral V., Otte W.M. Community-based rehabilitation offers cost-effective epilepsy treatment in rural Guinea-Bissau. Epilepsy Behav. 2018;79:23–25. doi: 10.1016/j.yebeh.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Colebunders R., Siewe F.J.N., Hotterbeekx A. Onchocerciasis-associated epilepsy, an additional reason for strengthening onchocerciasis elimination programs. Trends Parasitol. 2018;34:208–216. doi: 10.1016/j.pt.2017.11.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.