Abstract
Introduction:
The explosion of mobile phone users along with the importance of user’s role in managing their health provides a unique opportunity for m-Health applications in the management of chronic illnesses such as Multiple sclerosis (MS).
Aim:
To identify available MS applications and to characterize the content of MS self-management applications.
Methods:
Two popular online application stores (iTunes, Google play) were searched for multiple sclerosis -related apps using the following keywords: multiple sclerosis, disseminated multiple sclerosis, disseminated sclerosis, and MS. Apps were considered eligible if they had been customized only on multiple sclerosis. First, data was extracted from the description page for any eligible application. To achieve the study goal, the secondary analysis was performed only for self-management applications.
Results:
Search of two popular markets identified 1042 applications (747 applications from Google play, and 295 applications from iTunes). Of these, 104 unique applications met the inclusion criteria. Almost a quarter of eligible applications (26%) had been designed for multiple sclerosis self-management. Other purposes of the identified applications were diagnosing & treating (7.7%), doing tests (7.7%), connecting & communication for MS patients (4.8%), raising awareness of multiple sclerosis (15.4%), accessing to journals & news (6.7%), conferences & meetings (17.3%), supporting & donating to MS community (14.4%).
Conclusion:
It appears the mobile applications provide a multidimensional tool for patient with Multiple Sclerosis to improve their condition self-management. These applications can contribute to empowerment of the patients, and help their adherence to the therapeutic and management regimen of their conditions. Moreover, they can be utilized to collect information on the MS progress pattern in personal level for each individual patient. This information may provide health care professionals with evidence to help their patients toward enhancing self-management of their disease.
Keywords: Multiple Sclerosis, Mobile application, Self-management, m-health
1. INTRODUCTION
The explosion of mobile phone users along with important user’s role in managing their health provides a unique opportunity for m-health applications (1). The report by Research 2 guidance has estimated that 2.6 billion application (app) users will be downloading at least one health app by 2020 (2). While mobile apps have been utilized in the various areas of health and medicine, from medical education and diagnosis to health behavior change (3-5), researchers identified the unique potential of apps to support chronic disease self-management (6-10). The evidence indicates that use of mobile applications can improve health outcomes among people with chronic diseases through enhanced symptoms control (9). Multiple sclerosis (MS) is a chronic condition in which self-management is considered as an important component of person-centered care (11).
Multiple sclerosis is one of the most common neurologic disorders in the world and one of the main causes of disability in young people. It affects around 2.5 million people worldwide (12-14). Usually it presents itself in young adults (aged 20-50 years) (15) with a wide range of symptoms, including limitations in mobility, pain, fatigue and emotional changes. Consequently, people with MS face many physical, emotional and mental challenges on a daily basis. Self-management can be a potential approach to mitigation of MS symptoms (16, 17). Adherence to self-management programs can be an appropriate solution to cope with MS. Using an effective approach to accommodate such programs can enhance patient’s adherence to self-management regimens (18, 19).
Increasing use of smartphones and tablets has made mobile apps as a promising tool for empowering and engaging high-need, and high-cost patients to self-management of their own health (20, 21). In recent years, mobile health applications have provided many functionalities for patients, including recording, storing and exchanging patient information, monitoring health status, managing lifestyle, increasing adherence to treatment, raising awareness, managing medication, communicating with the care team and a wide range of other capabilities (22-27). Considering the importance of these aspects in MS management, mobile apps for self-management of this disease can provide a personalized tool for the patients.
2. AIM
The aim of this research was to identify available multiple sclerosis applications with focusing on the MS self-management apps and their characteristics.
3. METHODS
Search strategy
Two popular online application stores (iTunes, Google play) were searched for multiple sclerosis-related apps on November 2017 using the following keywords: multiple sclerosis disseminated multiple sclerosis, disseminated sclerosis, and MS.
Selection criteria
Apps were considered eligible if their focus was only on multiple sclerosis and they were excluded if they: were written in a non-English language, or were not designed specifically for multiple sclerosis.
Selection methodology
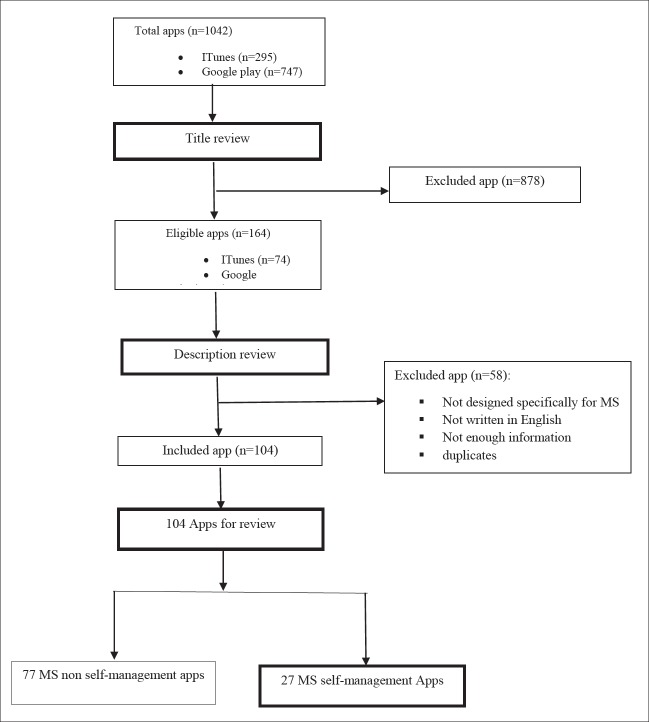
To select eligible mobile applications, titles of the apps were examined and apps that clearly did not meet criteria for inclusion were excluded. In the next step, three reviewers reviewed independently the full descriptions of remaining apps. Applications that did not meet the eligibility criteria were excluded. Eventually, a final list of eligible applications was obtained for data abstraction and analysis. Figure 1 shows an overview of the apps selection and their review process.
Figure 1. PRISMA diagram for searching and screening process for multiple sclerosis mobile applications.
Data extraction and analysis
In the primary analysis, data were extracted from the description page for any eligible app in each store. The following data were extracted for each application: name, platform (Android, IOS or both), its recent update, cost, star rating, number of reviews, and number of downloads. Then applications were categorized into eight different categories according to the main purpose of each app: MS diagnosis & treatment, MS tests, MS self-management, MS social networks, MS awareness, MS journal & news, MS conferences and meetings, and MS support & donation. Finally, descriptive statistics were calculated in terms of different variables. Statistical analyses were performed using SPSS V24. To achieve the study aim, the secondary analysis was carried out only for the self-management apps. Description pages of self-management apps and apps themselves were reviewed and explored for extracting their features and capabilities.
4. RESULTS
In total, the search of the two popular markets obtained 1042 applications (747 apps from Google play, and 295 apps from iTunes). After screening the title of apps, 164 apps were remained. Finally, after performing full description review and removing duplicates, 104 eligible MS applications were met the inclusion criteria and among them 27 applications were for the MS self-management.
Basic Characteristics of MS Applications
Twenty nine out of 104 MS applications (27.9 %) were available only on Google Play, while 25.0 %( 26) of them were accessible on iTunes. About 47 %( 49) had been designed for both platforms. The majority of applications (98/108) were free to download. For the six apps that were not free, the average cost was $1.97. Of 68 apps with customer rating, 55.9% had four or more stars and 2.9% had two stars or less. The average customers rating were 4 stars. The number of reviews had been provided only for the apps on Google Play. The mean number of reviews for android rated apps was 23.81 (ranging from one to 217). The iTunes did not provide any information on the number of apps downloads, only the number of downloads was available for 78 android applications. 2.9% of Android apps had been downloaded more than 10000 times and 21.2 percent of them had been downloaded less than 100 times. About 44.2 percent of the apps had been updated within 2017 year.
Figure 2. Key Characteristics of eligible MS mobile apps (n=104). *shows apps available in two platforms (Android and iTunes).
Almost a quarter of MS applications (26%) had been designed for multiple sclerosis self-management. Other apps were for different purposes including diagnosis & treatments (7.7%), doing tests (7.7%), connecting & communication for MS patients (4.8%), raise awareness of multiple sclerosis (15.4%), access to journals and news (6.7%), conferences & meetings (17.3%), and supporting & donating to MS community (14.4%). Figure 1 shows a summary of app characteristics and the list the application names in the self-management category.
MS self-management applications
Regarding the main purpose of the present study, the secondary analysis was carried out on eligible apps that were in the category of MS self-management applications (27 apps). Seventeen out of 27 apps focused on MS management and symptoms in general while 10 of them were specifically for self-managing of medications and injections in MS. 10 distinct features were identified in MS medication and injection management apps. The most frequent characteristics observed in these subcategories of apps include: entering medication names, recording medication dosage, managing injections, tracking injection sites, setting reminders, reporting and sharing data, notifying the end of medication stock, and accessing to pharmaceutical information (see table 1 for more details). While the number of features in general self-management apps ranged from 1 to14, the medication management apps had features ranging from 2 to 8 (Table 2).
Table 2. Present features in MS general self-management apps, Y: Present feature, ©Answering patient questions or offering necessary questions that patient should ask the physician.
| Apps | MSAA: My MS Manager | SymTrac MS | SymTrac CZHU | MS Care Connect | MS Self multiple sclerosis | MSAA selfcare manager | MS 101. me | Life and MS | MySidekick for MS | MS Management | Iwalk for MS | MS Mate | elevate MS | Health stories MS | My MS and Me | Multiple sclerosis | MCAMS Study | Total apps with feature |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Features | ||||||||||||||||||
| Information about MS | Y | Y | Y | Y | Y | Y | Y | 7 | ||||||||||
| Information on MS self- management and lifestyle | Y | Y | Y | Y | Y | Y | 6 | |||||||||||
| Recording daily status | Y | Y | Y | Y | Y | Y | Y | Y | 8 | |||||||||
| Recording symptoms | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 14 | |||
| Reporting | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12 | |||||
| Sharing reports or data | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 | ||||||
| Recording medical events and clinical encounters | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 | ||||||||
| Mobile-based MS tests | Y | Y | Y | Y | Y | Y | 6 | |||||||||||
| Recording allergies, exacerbations and stressors | Y | Y | Y | Y | Y | Y | Y | Y | 8 | |||||||||
| Recording medication | Y | Y | Y | Y | Y | Y | Y | 7 | ||||||||||
| Weather condition | Y | Y | Y | Y | Y | 5 | ||||||||||||
| Recording care team information | Y | Y | Y | Y | Y | 5 | ||||||||||||
| Reminders | Y | Y | Y | Y | Y | Y | Y | Y | 8 | |||||||||
| Recording notes | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 11 | |||||
| Accessing to MS information and news | Y | Y | Y | Y | 4 | |||||||||||||
| Answeringⲗ | Y | 2 | ||||||||||||||||
| Total features for every app | 14 | 13 | 12 | 10 | 10 | 9 | 8 | 8 | 6 | 6 | 6 | 6 | 6 | 3 | 3 | 2 | 1 |
The highest number of features was observed in MSAA and SymmetricMS apps with 14 and 13 features respectively. MCAMS study, Multiple sclerosis, My MS and Me apps were identified to have the minimum number of features. Among the general self-management apps, the most common features were the recording symptoms, reporting and sending & sharing the reports, and recording notes. Common features in the medication management apps were injection management, creating a reminder and recording notes. Almost half of 27 applications (51.8%) were capable of reporting, or sharing the reports with the third parties, such as their healthcare team.
Table 1. Present features in MS medication self-management apps. Y: Present feature, * Recording missed medication dosages and providing recommendations for missed dosages, ⲗManaging injections (recording names, location and time of injections, tracking injection sites), γOther features such as recording symptoms, medical events, recording necessary phone numbers.
| Features | Application names for MS medication Self-Management | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Basic MS Explorer | MS dialog | Noteness | MS Journal | Med Note Plus | My Multiple Sclerosis | Med Notes TP | RebiLink | MS injection | MS MAYA | |
| Medication management | Y | Y | ||||||||
| Recording missed medication dosages * | Y | |||||||||
| Managing injectionsⲗ | Y | Y | Y | Y | Y | Y | Y | Y | ||
| Set up reminders | Y | Y | Y | Y | Y | Y | Y | Y | ||
| Reporting | Y | Y | Y | Y | ||||||
| Sharing reports or sending data | Y | Y | Y | Y | Y (only sending data) | |||||
| Notifying the end dated of medications | Y | |||||||||
| Accessing to medication information | Y | |||||||||
| Recording notes | Y | Y | Y | Y | Y | Y | Y | |||
| Other featuresγ | Y | Y | Y | Y | Y | Y | Y | |||
5. DISCUSSION
This review used a stepwise process to identify apps developed for multiple sclerosis focusing on MS self-management apps. Based on the findings, more than a quarter of identified apps have been developed for self-management of multiple sclerosis. This is an indication of the significant increase in MS self-management applications compared with a previous study. The growing trend of self-management apps implies that a notable shift has occurred in comparison with the findings of Giunti (28). Considering the chronic nature of multiple sclerosis and importance of self-management in its control (17), the emerging trend observed in developing m-health apps seems to be in a right direction. Since m-health tools have the potential to better facilitate adherence of patients with chronic diseases to treatment and management regimens (29-31), the observed increase in the number of such apps for self-management of multiple sclerosis can lead to more involvement of the patients in managing their conditions. In addition, considering the fact that the attitude of people with MS is positive on the use of Smartphone technology for health care purposes (32, 33), this can be promising for the success of MS self-management apps. According to a previous study, people with multiple sclerosis had been stated that Smartphone use in healthcare might help them feel more independent, provide them with easier healthcare access, and might save their time. Other potential benefits that individuals with MS had been perceived about using Smartphone and mobile health apps included easy access to MS information, communication with healthcare professionals, usefulness for monitoring MS, improving the efficiency of MS administrative tasks, and the ability to communicate with other people with MS (32).
Considering the average stars obtained for the apps, although users might consider certain apps to be of high quality, some other apps need to be improved. It should be noted that star rating could be an unreliable metric, especially in cases with low user review. Furthermore, the star rating as an evaluation metric does not seem to be a reliable metric since it does not take into account the number of the reviewers and raters as well as their comments (34, 35). This reveals the need for formal evaluations. A brief overview of users’ comments revealed that the app malfunction is one of the primary reasons for the negative comments by the users. In some of the users’ reviews, it was reported that some apps crashed after a while or had problems in the registration or opening an account. Addressing these problems is necessary for obtaining patient confidence and supporting their reliable self-management. According to their comments, the users had the tendency to see complete MS symptoms list, to provide with a functionality of nutrition tracking and to see the sustainable updating and enhancing of the apps. Evidence shows that the most frequent complaints made by the users of the mobile applications include some functional errors, inadequate inclusion of features and functionalities as well as the app crashes (36).
Based on features contained in the apps, their functionalities range from providing information about MS, recording daily physical and mental status, recording symptoms, sending reports to health care professionals and others (in general self-management apps), to managing medication, and tracking injection sites (in medication self- management apps). The general MS self-management apps had focused on different aspects of MS management including injection management (e.g. my multiple sclerosis diary app), medication management (e.g. MS Explorer app), a special symptom control (e.g. Life and MS app), daily status monitoring (e.g. MS self app), motion management (I walk for MS app) and medical events entry (for example MS Mate app). These diverse aspects can be due to various inherent requirements necessary for successful self-management of MS. These dimensions include: learning about MS, symptoms, and treatments, monitoring health status, choosing the healthy lifestyle, exercising, psychological health management, fatigue management, cognitive restructuring and others (18). Multiple sclerosis is presented with a wide variety of symptoms; fatigue, pain, sleep disturbances, limitation of mobility, cognitive deficits and many other symptoms; therefore self-management can be a potential approach to controlling the symptoms. Considering unpredictable nature of MS, a wide variety of its symptoms which depends on each individual patient (15), and continuous and complex nature of the symptoms, make MS management more difficult. Therefore, learning different skills is essential for its self-management. Despite the growing trend of MS apps development, existing apps appear to be not comprehensive enough to cover all aspects of self-management programs toward helping the individuals with a wide range of MS symptoms (37). The designers of m-Health solutions for multiple sclerosis management should also take into account emerging aspects of MS, patient needs and management & treatment regimens. It appears that evidence-based development of apps should be taken into account for MS self-management programs, as there are emerging mechanisms and strategies for different dimensions of MS self-management. Results of studies that explore needs of persons with MS can provide invaluable information for designers and developers of mobile health solutions for multiple sclerosis. For example, some of the evidence-based features that have been suggested for physical activity in MS are as follows: customizable goal settings, energy profiles, and fatigue management, patient education, data visualization, positive feedback system, activity tracking, an exercise library, and game-like attitude (38). Such information can provide an evidence- based content required for MS M-health solutions. Reviewing features of existing MS self-management apps revealed that some needs of patient with MS for the self-management (such as recording energy levels, measuring fatigue and recording it, educating patients, and tracking of activities) have been somewhat considered in the apps. However, some other needs have not been addressed enough by the existing apps. People with MS need an application that helps them to manage the fatigue while the majority of existing apps focused only on recording the fatigue levels without providing an effective mechanism for its management by the patients (38). Fatigue management is one of the basic needs of people with MS. Evidence shows that use of the mobile application for supporting energy management in the patients can significantly reduce the level of fatigue and increase satisfaction with their performance (39).
Our findings shows that common features in medication self-management apps are injection management, medication reminders, note recording and other functionalities such as recording medical events, history and symptoms. These results are consistent with findings of a study conducted on the general medication self-management apps for different chronic diseases or conditions (40). Feature of the medication reminder is of great importance in MS self-management as the cognitive deficit is one of the MS symptoms that occurs in some patients depending on the location of the CNS lesions. This symptom can interfere with patient memory, and patient may forget injection schedule and may miss the injections or may make management of his/her medications and injections more difficult. As a result, development of MS medication management apps may be an innovative solution to these problems (41).
Considering the fact that no evidence was found in the literature on usability and utility evaluation of these apps by MS patients, it seems necessary to address these gaps in the future research. The researchers found only two brief reports plus one paper on patient and specialist perspectives on MS apps. The first report was on patient experience about performance of “MS self-multiple sclerosis” app in recording MS-related symptoms and daily activities. According to this report, the registration of MS symptoms has attracted the attention of most users, and the highest number of records was for MS symptoms (41%) and the user moods (25%) respectively. The number of recorded events in this app was 726123 (42). The second report was about the development of app (SymTrac app) for improving the report of multiple sclerosis relapses. Conducting an initial evaluation of this app, revealed its usefulness in “identifying the pattern of MS in order to diagnose the type of MS” and “recording and reporting relapses” from the perspective of MS nurses, although the patients highlighted some areas for improvement in future versions of the app (43). Another study has investigated patient and physician perspectives on “MSdialog” app. Its findings indicated that 82 % of the patients considered this app better than previous methods for tracking their health and 95 % of them mentioned that they would recommend its use to their peers. According to this report, patients felt “MSdialog” would help them to actively manage their conditions between interval of two consultations through improved communication with their healthcare team (44). It should be noted that the evaluation is a key component to the utility of m-health apps. Lack of evidence on evaluation of mobile health applications is expressed as the biggest challenge from the patients’ and health app consumer’s perspectives (45, 46), that will make it difficult for patients and even professionals to recommend high-quality apps for their patients.
Limitations: There were important limitations in this review that should be mentioned. First, the dynamic nature of mobile apps causes their daily changes; therefore, there was a change in the number of eligible applications during the review period. For instance, new apps may be added to both stores, updates and new features for existing apps may have occurred that all may influence the number of apps’ statistics. Second, this review focused on the presence or absence of different features of the apps without evaluating the quality of the features. In addition, determining application features relied on information presented in the full description of each application as well as their installation and usage. Third, only English-language apps were included in this study and the applications available in other languages were not considered for the analysis. There were a number of apps that did not report their download statistics, star ratings and customer reviews. Finally, there was no access to background knowledge on domain expertise support behind the development of these apps. It was unclear how these apps were developed, or how developers used the Multiple Sclerosis domain experts’ perspective in developing self-management apps.
6. CONCLUSION
It appears the mobile apps provide a multidimensional tool for patients with Multiple Sclerosis to improve self-management of their conditions. These apps can contribute to empowerment of the patients, and help their adherence to the therapeutic and disease management strategies. Moreover, they can facilitate information gathering of the MS progress pattern in personal level for each individual patient. This information may provide health care professionals with evidence for helping their patients to enhance self-management of their disease.
Acknowledgment:
This paper is based on an MSc thesis, financially funded by School of Management and Medical Informatics at Tabriz University of Medical Sciences.
Authors’ contributions:
LRK and ShD conceptualized the study, designed the research methodology for data collection, supervised in data collection and analysis, corrected the manuscript and revised it. ZS conducted the study, entered and analyzed the data and wrote the manuscript. RF supported data collection process as well as data analysis phases. All authors read and approved the final manuscript.
Conflict of interest:
None declared.
Financial support:
None.
References
- 1.Mendiola MF, Kalnicki M, Lindenauer S. Valuable features in mobile health apps for patients and consumers: content analysis of apps and user ratings. JMIR mHealth and uHealth. 2015;3(2):e40. doi: 10.2196/mhealth.4283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Research2guidance. mHealth app developer economics 2016 research2guidance. 2016.
- 3.Boulos MNK, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP. Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform. 2014;5(3):229. doi: 10.5210/ojphi.v5i3.4814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hebden L, Cook A, van der Ploeg HP, Allman-Farinelli M. Development of smartphone applications for nutrition and physical activity behavior change. JMIR Res Protoc. 2012;1(2):e9. doi: 10.2196/resprot.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14(5):e128. doi: 10.2196/jmir.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang H, Park H-A. A mobile app for hypertension management based on clinical practice guidelines: development and deployment. JMIR mHealth and uHealth. 2016;4(1):e12. doi: 10.2196/mhealth.4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vorrink SN, Kort HS, Troosters T, Lammers J-WJ. A mobile phone app to stimulate daily physical activity in patients with chronic obstructive pulmonary disease: development, feasibility, and pilot studies. JMIR mHealth and uHealth. 2016;4(1):e11. doi: 10.2196/mhealth.4741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goyal S, Morita P, Lewis GF, Yu C, Seto E, Cafazzo JA. The systematic design of a behavioural mobile health application for the self-management of type 2 diabetes. Can J Diabetes. 2016;40(1):95–104. doi: 10.1016/j.jcjd.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Whitehead L, Seaton P. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res. 2016;18(5):e97. doi: 10.2196/jmir.4883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zulman DM, Jenchura EC, Cohen DM, Lewis ET, Houston TK, Asch SM. How can eHealth technology address challenges related to multimorbidity? Perspectives from patients with multiple chronic conditions. J Gen Intern Med. 2015;30(8):1063–1070. doi: 10.1007/s11606-015-3222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martz E. Promoting self-Management of chronic health conditions: theories and practice. Oxford University Press; 2017. [Google Scholar]
- 12.Organization WH. World Health Organization; 2006. Neurological disorders: public health challenges. [Google Scholar]
- 13.Kingwell E, Marriott JJ, Jetté N, Pringsheim T, Makhani N, Morrow SA, et al. Incidence and prevalence of multiple sclerosis in Europe: a systematic review. BMC Neurol. 2013;13(1):128. doi: 10.1186/1471-2377-13-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pietrangelo A, Higuera V. Multiple sclerosis by the numbers: facts, statistics, and you 2015. Available from: https://www.healthline.com/health/multiple-sclerosis/facts-statistics-infographic.
- 15.Bishop M, Rumrill PD. Multiple sclerosis: Etiology, symptoms, incidence and prevalence, and implications for community living and employment. Work. 2015;52(4):725–734. doi: 10.3233/WOR-152200. [DOI] [PubMed] [Google Scholar]
- 16.Fraser R, Ehde D, Amtmann D, Verrall A, Johnson KL, Johnson E, et al. Self-management for people with multiple sclerosis: report from the first international consensus conference, November 15, 2010. Int J MS Care. 2013;15(2):99–106. doi: 10.7224/1537-2073.2012-044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kidd T, Carey N, Mold F, Westwood S, Miklaucich M, Konstantara E, et al. A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life. PloS one. 2017;12(10):e0185931. doi: 10.1371/journal.pone.0185931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghahari S, Khoshbin LS, Forwell SJ. The multiple sclerosis self-management scale: Clinicometric testing. Int J MS Care. 2014;16(2):61–67. doi: 10.7224/1537-2073.2013-019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ehde DM, Elzea JL, Verrall AM, Gibbons LE, Smith AE, Amtmann D. Efficacy of a telephone-delivered self-management intervention for persons with multiple sclerosis: a randomized controlled trial with a one-year follow-up. Arch Phys Med Rehabil. 2015;96(11):1945–1958. doi: 10.1016/j.apmr.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 20.Singh K, Drouin K, Newmark LP, et al. Developing a framework for evaluating the patient engagement, quality, and safety of mobile health applications. Issue Brief (Commonw Fund) 2016;5:1–11. [PubMed] [Google Scholar]
- 21.Jusoh S. A survey on trend, opportunities and challenges of mHealth apps. IJIM. 2017;11(6):73–85. [Google Scholar]
- 22.Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Using smartphone technology to monitor physical activity in the 10,000 Steps program: a matched case-control trial. J Med Internet Res. 2012;14(2):e55. doi: 10.2196/jmir.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mirkovic J, Kaufman DR, Ruland CM. Supporting cancer patients in illness management: usability evaluation of a mobile app. JMIR mHealth and uHealth. 2014;2(3):e33. doi: 10.2196/mhealth.3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen AB, Nahed BV, Sheth KN. Mobile medical applications in neurology. Neurol Clin Pract. 2013;3(1):52–60. doi: 10.1212/CPJ.0b013e318283ff4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beatty AL, Fukuoka Y, Whooley MA. Using mobile technology for cardiac rehabilitation: a review and framework for development and evaluation. J Am Heart Assoc. 2013;2(6):e000568. doi: 10.1161/JAHA.113.000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petersen M, Hempler NF. Development and testing of a mobile application to support diabetes self-management for people with newly diagnosed type 2 diabetes: a design thinking case study. BMC Med Inform Decis Mak. 2017;17(1):91. doi: 10.1186/s12911-017-0493-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dubey D, Amritphale A, Sawhney A, Amritphale N, Dubey P, Pandey A. Smart phone applications as a source of information on stroke. J Stroke. 2014;16(2):86–90. doi: 10.5853/jos.2014.16.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giunti G, Guisado-Fernandez E, Caulfield B, editors. Connected health in multiple sclerosis: a mobile applications review. 30th International Symposium on Computer-Based Medical Systems (CBMS); IEEE; Greece. 2017. [Google Scholar]
- 29.Bender JL, Yue RYK, To MJ, Deacken L, Jadad AR. A lot of action, but not in the right direction: systematic review and content analysis of smartphone applications for the prevention, detection, and management of cancer. J Med Internet Res. 2013;15(12) doi: 10.2196/jmir.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52. doi: 10.2196/jmir.3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR mHealth and uHealth. 2018;6(1):e23. doi: 10.2196/mhealth.8873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Griffin N, Kehoe M. A questionnaire study to explore the views of people with multiple sclerosis of using smartphone technology for health care purposes. Disabil Rehabil. 2017;40(12):1–9. doi: 10.1080/09638288.2017.1300332. [DOI] [PubMed] [Google Scholar]
- 33.Cohen M. Connected health and multiple sclerosis. Rev Neurol (Paris) 2018;174(6):480–485. doi: 10.1016/j.neurol.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 34.Kuehnhausen M, Frost VS, editors. Trusting smartphone apps? To install or not to install, that is the question. Cognitive Methods in Situation Awareness and Decision Support (CogSIMA), 2013 IEEE International Multi-Disciplinary Conference on; IEEE.2013. [Google Scholar]
- 35.Ali M, Joorabchi ME, Mesbah A, editors. Same app, different app stores: a comparative study. Proceedings of the 4th International Conference on Mobile Software Engineering and Systems; IEEE Press.2017. [Google Scholar]
- 36.Khalid H, Shihab E, Nagappan M, Hassan AE. What do mobile app users complain about? IEEE Software. 2015;32(3):70–77. [Google Scholar]
- 37.Ruzic L, Mahajan HP, Sanford JA, editors. Universally designed mHealth app for individuals aging with multiple sclerosis; The Third International Conference on Universal Accessibility in the Internet of Things and Smart Environments; Italy. 2018. [Google Scholar]
- 38.Giunti G, Kool J, Romero OR, Zubiete ED. Exploring the specific needs of persons with multiple sclerosis for mHealth solutions for physical activity: mixed-methods study. JMIR mHealth and uHealth. 2018;6(2):e37. doi: 10.2196/mhealth.8996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grant J, Gamueda MA, Ortega A, Song J. Dominican University of California; 2018. Managing fatigue with technology for individuals with multiple sclerosis. [Google Scholar]
- 40.Bailey SC, Belter LT, Pandit AU, Carpenter DM, Carlos E, Wolf MS. The availability, functionality, and quality of mobile applications supporting medication self-management. J Am Med Inform Assoc. 2013;21(3):542–546. doi: 10.1136/amiajnl-2013-002232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Costello K, Kennedy P, Scanzillo J. Recognizing nonadherence in patients with multiple sclerosis and maintaining treatment adherence in the long term. The Medscape Journal of Medicine. 2008;10(9):225. [PMC free article] [PubMed] [Google Scholar]
- 42.Guerra CB, Northcutt B, Muser R, Russo M, McBride J, Rabinowicz AL. MS self™, an educational application for people with Multiple Sclerosis (MS): patient experience in recording MS-related symptoms and daily activities ‘Annual Meeting of the Consortium of Multiple Sclerosis Centers. 2016.
- 43.Roberts M, Lush T, Pohorely J. Improving reporting of multiple sclerosis relapse. Nurs Times. 2015;111(48):12–14. [PubMed] [Google Scholar]
- 44.Greiner P, Sawka A, Imison E. Patient and physician perspectives on msdialog, an electronic PRO diary in multiple sclerosis. Patient. 2015;8(6):541–550. doi: 10.1007/s40271-015-0140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang C, Zhang X, Halstead-Nussloch R. Assessment, metrics, challenges and strategies for mobile health apps. Issues in Information Systems. 2014;15(2) [Google Scholar]
- 46.Masic I, Begic E. Mobile Clinical Decision Support Systems in Our Hands - Great Potential but also a Concern. Stud Health Technol Inform. 2016;226:63–66. [PubMed] [Google Scholar]