Abstract
Introduction:
The 12-lead ECG at admission of patients suffering from acute myocardial infarction (AMI) is mandatory for accurate diagnosis and prompt therapeutic measures, mainly reperfusion. It has been shown that recording additional ECG leads may improve the diagnostic accuracy and therefore, the prognosis of selected cases.
Aim:
The aim of the study was to assess the usefulness of the 15-lead ECG (12 classic plus 3 posterior leads) in the management of chest pain patients, especially when 12-lead ECG is not diagnostic of AMI.
Methods:
Total amount of 186 consecutive patients (127 men, 59 women, mean age 69.7±13.8 years) were admitted with an acute coronary syndrome. The initial ECG recorded the 12 classic leads, and subsequently, the 3 additional posterior leads. Demographic and clinical data, including ECG alterations and selected treatment strategy, were also studied. The cumulative impact of the 15-lead ECG on the diagnosis and management of AMI were, overall, evaluated.
Results:
The 12-lead ECG was diagnostic of ST-elevation AMI (STEMI) in 158 patients (Group A–84.5%) who were promptly reperfused. On the other hand, the interpretation of the posterior leads was required in 28 patients (Group B–15.1%) to establish the STEMI diagnosis warranting reperfusion therapy. Multivariate analysis illustrated that the 15-lead ECG was the only factor associated with achieving the STEMI diagnosis in non-conclusive 12-lead ECG cases (OR=2.43–p=0.04).
Conclusion:
The use of the 15-lead ECG contributes to a faster and more accurate diagnosis of STEMI, particularly in the Emergency Department, facilitating the prompt reperfusion therapy.
Keywords: 15-lead ECG, posterior leads, acute myocardial infarction
1. INTRODUCTION
The 12-lead ECG is the proper diagnostic method to establish the diagnosis of acute myocardial infarction (AMI), particularly in the early phase. However, the sensitivity of a single 12-lead ECG for the diagnosis of AMI is relatively weak (1). It has been advocated that the initial 12-lead ECG of patients proved to suffer from AMI, shows ST segment elevation in less than 50%, while in other cases it might show only minor ischemic changes, such as ST segment depression and T wave inversion (1). One has to keep in mind that ST depression in leads V1-V3 should raise strong suspicion of posterior wall infarction (2).
Moreover, in up to 30% of patients with acute coronary syndrome (ACS), the initial 12-lead ECG may be normal or showing non-specific abnormalities only (3). Nonetheless, a diagnostic initial ECG in a patient with AMI will allow the physician to promptly start the appropriate therapy, mainly reperfusion. It has repeatedly been demonstrated that recording additional leads on initial ECG may improve its sensitivity and the prognosis of selected cases of ACS patients (4, 5). Moreover, additional lead ECGs may reveal more accurately the extend of the myocardial injury (6). It is known that posterior or postero-lateral AMI might not be manifested with ST elevation on the classic 12-lead ECG (7). If this were the case, especially in the Emergency Department, then these patients could be offered specific reperfusion therapy, either thrombolysis or percutaneous coronary intervention (8). Therefore, the recording of posterior leads (V7, V8, V9) seems to be valuable and practical (9). Surprisingly, less than 40% of physicians request the posterior leads on the initial ECG of patients hospitalized for ACS (10).
2. AIM
The aim of the study was to assess the usefulness of the 15-lead ECG (12 classic plus posterior leads V7, V8, V9) in the management of chest pain patients, with special focus on those whose 12-lead ECG was not diagnostic of AMI.
3. METHODS
We enrolled 186 consecutive patients (127 men, 59 women, mean age 69.7±13.8 years) who were admitted to the Coronary Care Unit (CCU) with the working diagnosis of ACS. The initial ECG recorded the 12 classic leads, and subsequently, the 3 additional posterior leads (V7: on the posterior axillary line, V8: on the posterior scapular line, V9: on the left border of the spine). Demographic and clinical data, including ECG alterations (ST elevation, ST depression, T wave inversion, Q waves and appearance of new bundle brand block) and selected treatment strategy, were studied. ST elevation on the posterior leads V7, V8, V9 was considered when it was ≥0.5 mm. The supplemental impact of the 15-lead ECG on the diagnosis and management of AMI was, overall, evaluated.
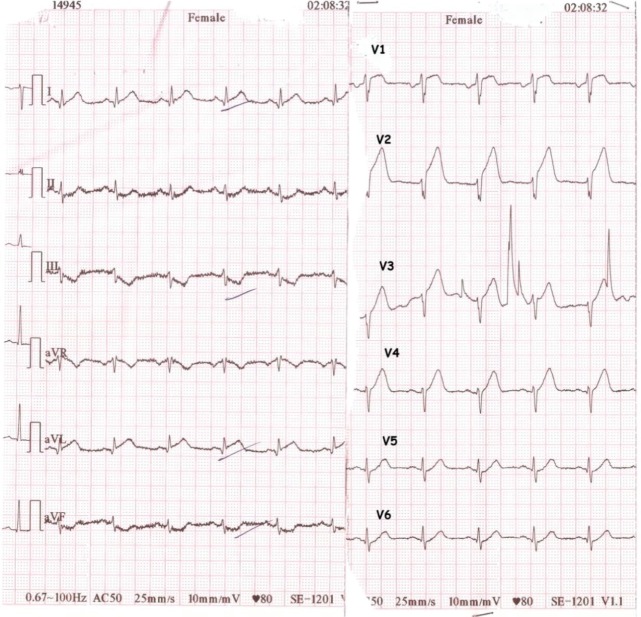
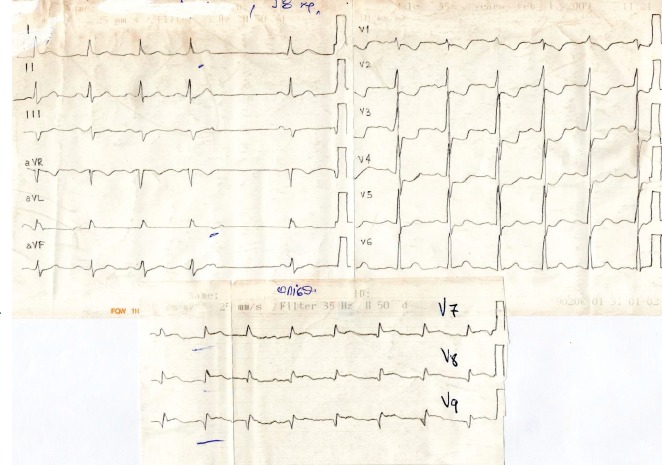
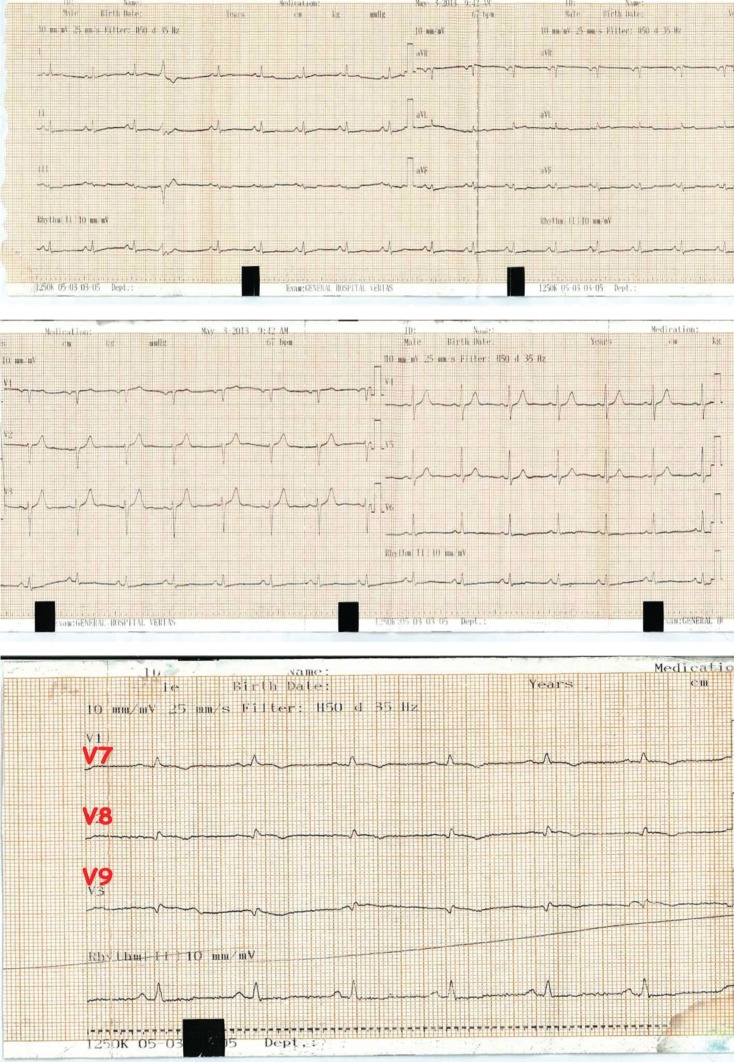
Patients were divided into two groups according to whether the initial 12-lead ECG could establish the STEMI diagnosis–Group A (158 patients, 127 men–59 women, mean age 66.7±13.8 years (Figure 1) or the additional posterior leads were required–Group B (28 patients, 20 men–8 women, mean age 68.9±18.8 years (Figures 2 and 3).
Figure 1. 12-lead ECG of a patient from group A: the AMI diagnosis was readily established and the patient received the indicated reperfusion therapy.
Figure 2. 15-lead ECG of a patient from group B: the ECG abnormalities on the classic 12 leads (e.g. ST segment depression on V1, V2, V3) raised the suspicion of posterior ischaemia, which was confirmed when the additional leads were recorded (ST elevation on posterior leads V7, V8, V9).
Figure 3. 15-lead ECG of a patient from group B: there were no ECG abnormalities on the classic 12 leads to indicate posterior AMI, which was confirmed when the additional leads were recorded (ST elevation on posterior leads V7, V8, V9).
Statistical analysis
The Kolmogorov-Smirnoff test (sample >50 patients) was applied to evaluate the normality of distribution of quantitative variables. Continuous variables (quantitative) were recorded with the mean±SD values and the categorical variables (qualitative) as a percentage (%). The t-test (Student test) was used to compare the continuous variables and the x2-test or Fischer test to compare the categorical variables. Forward stepwise multiple regression model, a model of multivariate regression analysis, was used to determine the factors associated with the final diagnosis of AMI (independent variable). Probability p < 0.05 (2-way) was considered statistically significant. The study protocol was approved by the Scientific Council of the Hospital (Number 16/2014). The statistical analysis was made using the SPSS.19 for Windows statistical package.
4. RESULTS
Table 1 shows the demographic and clinical data of the patients of the two groups. No significant differences were observed in gender, age, AMI diagnosis between the two groups. The 12-lead ECGs of Group B patients were not diagnostic of STEMI. Nevertheless, in 17 patients (60.7%), the ECG alterations would raise suspicion of isolated posterior infarction entailing the recording of the additional posterior leads (Figure 2). Notably, there was no such indicative ECG abnormality in the 12-lead ECGs of the remaining 11 patients (39.3%), who would fail the STEMI diagnosis and would not be offered reperfusion therapy if the posterior leads were not recorded (Figure 3). Multivariate analysis revealed that the 15-lead ECG was the sole factor significantly associated with achieving the STEMI diagnosis (OR=2.43–p=0.04, Table 2). On the whole, the 15-lead ECG was diagnostic of STEMI in more patients than the classic 12-lead ECG. Table 2 presents the factors which contribute successfully to the diagnosis of STEMI.
Table 1.
| Group A n=158 |
Group B n=28 |
Total n=186 |
p | ||
|---|---|---|---|---|---|
| Age | years | 65.8±15.7 | 66.8±13.5 | 65.9±14.1 | 0.3 |
| Male Gender | n (%) | 107 (67.7) | 20 (79.4) | 127 (68.3) | 0.08 |
| Angina | n (%) | 34 (21.52) | 8 (28.57) | 42 (22.58) | 0.1 |
| Leads with ST elevation | n | 5.4±1.8 | 2.7±1.9 | 4.8±2.6 | 0.1 |
| Leads with ST depression | n | 4.8±2.6 | 3.2±2.4 | 4.3±2.40 | 0.2 |
| ST depression in V1-V4 | n (%) | 85 (53.8) | 12 (42.9) | 97 (52.15) | 0.07 |
| Interval from symptoms onset | min | 123.7±26.25 | 120.4±21.51 | 122.3±24.1 | 0.1 |
| CPK | IU | 1656.8±373.4 | 1276.4±287.7 | 1465.4±325.7 | 0.1 |
| LVEF | % | 46.21±7.8 | 48.37±8.2 | 4.8±5.0 | 0.2 |
| CPK: Creatine Phosphokinase, LVEF: Left ventricular ejection fraction, IU: international unit | |||||
Table 2. Stepwise multivariate regression analysis for predicting the correct diagnosis of acute myocardial infarction. The 15-lead ECG was the sole factor associated significantly with the correct diagnosis.
| OR | CI | p | |
|---|---|---|---|
| 15-lead ECG | 2.43 | 1.87-2.98 | 0.04 |
| 12-lead ECG | 0.32 | 0.35-1.47 | 0.1 |
| ST segment depression in V1-V4 | 1.24 | 0.65-1.1 | 0.67 |
5. DISCUSSION
The study showed that the addition of the 3 posterior leads (V7, V8, and V9) to the standard 12 leads allows the detection of ST elevation in more patients. Prompt STEMI diagnosis is paramount for timely offered reperfusion therapy. The findings of our study demonstrate the usefulness of the 15-lead ECG on the detection of posterior and posterior-lateral AMIs, facilitating the decision for reperfusion therapy. The preferred reperfusion strategy is primary PCI. However, 60-70% of patients initially arrive at non-PCI capable hospitals and therefore, thrombolysis should be administered (11).
It has previously been reported that approximately 11% of patients (15% in our study) with ST elevation in the posterior leads do not exhibit indicative abnormalities on the classic 12-lead ECG (ST elevation or depression) that would warrant the recording of additional leads (12).
The ECG sensitivity of STEMI diagnosis is increased with the use of additional leads improving, as a result, the prognosis of AMI patients (6, 13, 14). Of note, the sole recording of the standard 12-lead ECG may subdiagnose the posterior and right ventricular involvement in AMI, as these leads do not directly reflect those segments. The commonest additional leads are the posterior leads (V7, V8 and V9) that view the posterior and lateral walls, and the right V4 (RV4) that examine the right ventricle. Therefore, the use of the 15-lead ECG may confirm the STEMI diagnosis while determining its actual extent.
The term “posterior infarction” identifies an AMI that insults the left ventricular wall by occlusion of the right coronary artery–posterior descending branch or the circumflex artery (15). It accounts for 15-21% of all AMI (4, 5, 6, 13), often in conjunction with inferior or lateral ones. The true posterior AMI is a rare entity, as it has been shown in our study. Patients with inferior-posterior AMI suffer from more severe AMI with lower left ventricular ejection fraction and present more complications in comparison with inferior AMI patients (16).
The standard 12-lead ECG does not include posterior leads, and thus changes associated with necrosis in this region are reflected in the anterior leads. These changes are reversed in the standard leads because the electrodes are pointing away from the lesion area. Thus, the ST elevation on posterior leads in posterior infarctions will be manifested as ST depression on the anterior V1-V3 leads. The ischaemic criteria, in the same way, are the horizontal ST depression, the tall R waves and the prominent upright T waves on leads V1-V3 (7, 17). The prominent R waves in the anterior leads are simply the electrical equivalents of the recorded Q waves in the posterior leads (13, 17). Posterior leads illustrate ST elevations in posterior-lateral MI and a coronary vessel obstruction, predominantly the circumflex artery (15). There are limited and conflicting data on their utility in clinical practice.
Zalensky et al. (18) concluded that the application of posterior leads to AMI detection has a sensitivity of 60%, specificity of 89%, a positive predictive value of 91% and negative predictive value of 55%. In many cases, however, the analyses are affected by the definition of pathological ST elevation (≥0.5mm or 1mm) on the posterior leads (18, 19). In our study pathognomonic ST elevation was defined as ≥0.5 mm.
Posterior leads recording is useful in detecting AMI in patients with strong suspicion as shown in previous and in our study (20, 21). However, they may be under-utilized in clinical practice. In an earlier intriguing study, approximately only 10% of cardiologists and emergency physicians used them routinely (22).
In addition, the use of the 15-lead ECG confirms the posterior MI and is superior to the findings in the anterior leads (4). Besides, the incidence of isolated posterior MI is not defined and has been reported in studies ranging from 0% to 7-12% (18, 23).
Also, a more detailed description of the extent of MI impairment and prognosis is achieved by using the additional posterior leads (6, 14). In the same way, an isolated posterior MI could be detected only with the additional posterior leads. This means that immediate reperfusion could be succeeded, either by thrombolysis or by emergency PCI. Therefore, the additional posterior leads on the ECG affect not only diagnostic but therapeutic decisions as well (3, 16).
The clinical experience with the use of the 15-lead ECG is reportedly limited. Nonetheless, multiple studies have confirmed that the ECG diagnostic sensitivity and specificity for AMI is improved, and in doing so, facilitating the prompt application of the indicated reperfusion therapy (24). Moreover, the addition of the posterior leads offers more to the diagnosis of the posterior MI than the ECG changes on the V1-V3 leads (5, 6).
Extrapolating the findings of our study, it seems that patients with chest pain may benefit by the routine use of the 15-lead ECG, as demonstrated in those with AMI, and especially inferior AMI. It should be noted that the additional leads should be recorded by experienced personnel as misplaced electrodes may yield false diagnoses.
Limitations: The sample is relatively limited, which is fully justified by the rarity of the isolated posterior AMI and is comparable with similar published series.
Clinical applications: Based on the findings of the study, the routine use of 15-lead ECG for Emergency Department patients with chest pain should be supported and recommended.
6. CONCLUSION
The use of the 15-lead ECG contributes to a faster and more accurate diagnosis of STEMI facilitating the prompt reperfusion therapy.
Author’s contribution:
Ioannis Vogiatzis: led the writing of the protocol and the manuscript, carried out literature searches, conducted the analysis, paper preparation and paper editing. Efstathios Koulouris: provided clinical experience, carried out literature search, contributed to the paper preparation and editing. Antonios Ioannidis: provided clinical experience, paper editing and approved the final manuscript. Evangelos Sdogkos: provided clinical experience and contributed to the paper preparation and editing. Maria Pliatsika: provided clinical experience and contributed to the paper preparation and editing. Pavlos Roditis: provided clinical experience and contributed to the paper preparation and editing. Markos Goumenakis: provided clinical experience and contributed to the paper preparation and editing.
Conflicts of interest:
The authors report no relationships that could be construed as a conflict of interest.
Financial support:
Nil.
REFERENCES
- Wang JJ, Pahlm O, Warren JW, Sapp JL, Horáček BM. Criteria for ECG detection of acute myocardial ischemia: Sensitivity versus specificity. J Electrocardiol. 2018;51(6):S12–S17. doi: 10.1016/j.jelectrocard.2018.08.018. [DOI] [PubMed] [Google Scholar]
- Jia X, Heiberg E, Sejersten Ripa M, Engblom H, Carlsson M, Halvorsen S, Arheden H, Atar D, Clemmensen P, Birnbaum Y. Cardiac magnetic resonance evaluation of the extent of myocardial injury in patients with inferior ST elevation myocardial infarction and concomitant ST depression in leads V1-V3: analysis from the MITOCARE Study. Cardiology. 2018;140(3):178–185. doi: 10.1159/000491745. [DOI] [PubMed] [Google Scholar]
- Somers MP, Brady WJ, Bateman DC, Mattu A, Perron AD. Additional electrocardiographic leads in the ED chest pain patient: right ventricular and posterior leads. Am J Emerg Med. 2003;21(7):563–573. doi: 10.1016/j.ajem.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Russi CS, Myers LA, Kolb LJ, Steever K, Nestler DM, Bjerke MC, White RD, Ting HH. Prehospital diagnosis of ST-segment elevation myocardial infarction using an “all-posterior” 12-lead electrocardiogram. Prehosp Emerg Care. 2011;15(3):410–413. doi: 10.3109/10903127.2011.561414. [DOI] [PubMed] [Google Scholar]
- Carley SD. Beyond the 12 lead: review of the use of additional leads for the early electrocardiographic diagnosis of acute myocardial infarction. Emerg Med (Fremantle) 2003;15(2):143–154. doi: 10.1046/j.1442-2026.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- Rosengarten P, Kelly AM, Dixon D. Does routine use of the 15-lead ECG improve the diagnosis of acute myocardial infarction in patients with chest pain? Emerg Med (Fremantle) 2001;13(2):190–193. doi: 10.1046/j.1442-2026.2001.00210.x. [DOI] [PubMed] [Google Scholar]
- Brady WJ, Erling B, Pollack M, Chan TC. Electrocardiographic manifestations: acute posterior wall myocardial infarction. J Emerg Med. 2001;20(4):391–401. doi: 10.1016/s0736-4679(01)00318-3. [DOI] [PubMed] [Google Scholar]
- Matetzky S, Freimark D, Feinberg MS, Novikov I, Rath S, Rabinowitz B, Kaplinsky E, Hod H. Acute myocardial infarction with isolated ST-segment elevation in posterior chest leads V7-9: “hidden” ST-segment elevations revealing acute posterior infarction. J Am Coll Cardiol. 1999;34(3):748–753. doi: 10.1016/s0735-1097(99)00249-1. [DOI] [PubMed] [Google Scholar]
- Porter A, Vaturi M, Adler Y, Sclarovsky S, Strasberg B, Herz I, Kuzniec H, Birnbaum Y. Are there differences among patients with inferior acute myocardial infarction with ST depression in leads V2 and V3 and positive versus negative T waves in these leads on admission? Cardiology. 1998;90(4):295–298. doi: 10.1159/000006861. [DOI] [PubMed] [Google Scholar]
- Nallamothu B, Fox KA, Kennelly BM, Van de Werf F, Gore JM, Steg PG, Granger CB, Dabbous OH, Kline-Rogers E, Eagle KA. GRACE Investigators. Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart. 2007;93(12):1552–1555. doi: 10.1136/hrt.2006.112847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson DM, McKavanagh P, Henry TD, Cantor WJ. Reperfusion options for ST elevation myocardial infarction patients with expected delays to percutaneous coronary intervention. Interv Cardiol Clin. 2016;5(4):439–450. doi: 10.1016/j.iccl.2016.06.004. [DOI] [PubMed] [Google Scholar]
- Wong CK. Usefulness of leads V7, V8, and V9 ST elevation to diagnose isolated posterior myocardial infarction. Int J Cardiol. 2011;146(3):467–469. doi: 10.1016/j.ijcard.2010.10.137. [DOI] [PubMed] [Google Scholar]
- Boden WE, Kleiger RE, Gibson RS, Schwartz DJ, Schechtman KB, Capone RJ, Roberts R. Electrocardiographic evolution of posterior acute myocardial infarction: importance of early precordial ST-segment depression. Am J Cardiol. 1987;59(8):782–787. doi: 10.1016/0002-9149(87)91091-5. [DOI] [PubMed] [Google Scholar]
- Zalenski RJ, Rydman RJ, Sloan EP, Hahn K, Cooke D, Tucker J, Fligner D, Fagan J, Justis D, Hessions W, Pribble JM, Shah S, Zwicke D. ST segment elevation and the prediction of hospital life-threatening complications: the role of right ventricular and posterior leads. J Electrocardiol. 1998;31(Suppl):164–171. doi: 10.1016/s0022-0736(98)90311-9. [DOI] [PubMed] [Google Scholar]
- Aqel RA, Hage FG, Ellipeddi P, Blackmon L, McElderry HT, Kay GN, Plumb V, Iskandrian AE. Usefulness of three posterior chest leads for the detection of posterior wall acute myocardial infarction. Am J Cardiol. 2009;103(2):159–164. doi: 10.1016/j.amjcard.2008.09.008. [DOI] [PubMed] [Google Scholar]
- Vogiatzis I, Prodromidis P, Karamitsos T, Kambitsi E, Xinogalou V, Papahatzi S. Prognostic value of ST-Segment elevation in posterior precordial leads (V7, V8, V9) on the initial ECG of patients with inferior acute myocardial infarction who received thrombolysis. Hellenic J Cardiol. 2004;45:154–163. [Google Scholar]
- Brady WJ. Acute posterior wall myocardial infarction: electrocardiographic manifestations. Am J Emerg Med. 1998;16(4):409–413. doi: 10.1016/s0735-6757(98)90143-7. [DOI] [PubMed] [Google Scholar]
- Zalenski RJ, Cooke D, Rydman R, Sloan EP, Murphy DG. Assessing the diagnostic value of an ECG containing leads V4R, V8, and V9: the 15-lead ECG. Ann Emerg Med. 1993;22(5):786–793. doi: 10.1016/s0196-0644(05)80792-9. [DOI] [PubMed] [Google Scholar]
- Wung SF, Drew BJ. New electrocardiographic criteria for posterior wall acute myocardial ischemia validated by a percutaneous transluminal coronary angioplasty model of acute myocardial infarction. Am J Cardiol. 2001;87(8):970–974. doi: 10.1016/s0002-9149(01)01431-x. [DOI] [PubMed] [Google Scholar]
- Trzeciak S, Erickson T, Bunney EB, Sloan EP. Variation in patient management based on ECG interpretation by emergency medicine and internal medicine residents. Am J Emerg Med. 2002;20(3):188–1895. doi: 10.1053/ajem.2002.32628. [DOI] [PubMed] [Google Scholar]
- Kaul P, Armstrong PW, Sookram S, Leung BK, Brass N, Welsh RC. Temporal trends in patient and treatment delay among men and women presenting with ST-elevation myocardial infarction. Am Heart J. 2011;161(1):91–97. doi: 10.1016/j.ahj.2010.09.016. [DOI] [PubMed] [Google Scholar]
- Novak PG, Davies C, Gin KG. Survey of British Columbia cardiologists’ and emergency physicians’ practice of using nonstandard ECG leads (V4R to V6R and V7 to V9) in the diagnosis and treatment of acute myocardial infarction. Can J Cardiol. 1999;15(9):967–972. [PubMed] [Google Scholar]
- Brady WJ, Hwang V, Sullivan R, Chang N, Beagle C, Carter CT, Martin ML, Aufderheide TP. A comparison of 12- and 15-lead ECGS in ED chest pain patients: impact on diagnosis, therapy, and disposition. Am J Emerg Med. 2000;18(3):239–243. doi: 10.1016/s0735-6757(00)90112-8. [DOI] [PubMed] [Google Scholar]
- Choudhury T, West NE, El-Omar M. ST elevation myocardial infarction. Clin Med (Lond) 2016;16(3):277–282. doi: 10.7861/clinmedicine.16-3-277. [DOI] [PMC free article] [PubMed] [Google Scholar]