Abstract
This study examined the empirical structure (i.e., size, density, duration) of transgender women’s social networks and estimated how network alters’ perceived HIV risk/protective behaviors influenced transgender women’s own HIV risk/protective behaviors. From July 2015 through September 2016, 271 transgender women completed surveys on sociodemographic characteristics, HIV risk/protective behaviors, and social networks. Hierarchical generalized linear models examined the associations of social network alter member data ‘nested’ within participant data. Analyses revealed that social network factors were associated with HIV risk/protective behaviors, and that the gender identity of the alters (cisgender vs. transgender), and social network sites and technology use patterns (“SNS/tech”) moderated these associations. Among network alters with whom the participant communicated via SNS/tech, participants’ HIV risk behavior was positively associated with alters’ HIV risk behavior (cisgender alters aOR=4.10; transgender alters aOR=5.87). Among cisgender alters (but not transgender alters) with whom the participant communicated via SNS/tech, participants’ HIV protective behavior was positively associated with alters’ HIV protective behavior (aOR=8.94).
Keywords: transgender, social networks, technology, HIV
Introduction
Transgender women (hereafter “trans women”) experience numerous cofactors for HIV acquisition and transmission (1). Among LGBT (i.e., lesbian, gay, bisexual, transgender) populations, trans women experience more severe discrimination and social and economic marginalization than LGB individuals (2–3). Trans women are often forced outside the legal economy (4), leading to increased rates of homelessness (5–7), alcohol and drug use (7–8), and sex work (8–9). HIV prevalence among trans women is elevated (18.4%−30.6%) (8, 10) relative to other U.S. adult populations (0.3%−0.4%) (11); odds of being HIV positive among trans women are estimated to be over 34 times higher than other U.S. adult populations, (10) and rates of unidentified HIV infection are also high (8, 11–13). Unidentified infection impacts the health of trans women not receiving HIV medical care, as well as members of their sexual networks.
Over the past two decades, research has demonstrated the strong influence of social network dynamics on HIV risk/protective behaviors among vulnerable groups (14–15). Elements of social network structure, including network size (number of network members), density (connectedness between network members), and duration (length of relationship to network members) have been shown to influence HIV risk behaviors, including condom use among networks of drug users (15–17). However, no studies to date have examined how the egocentric structure and composition of trans women’s social networks might affect their engagement in HIV risk/protective behaviors, or how the effects of intra-network communication may be influenced by how such communication takes place (e.g., face-to-face or mediated through a computer or phone).
Research has demonstrated that it is the perception of engagement in HIV risk behaviors by one’s social network members (hereafter “alters”) that influences participant’s own behavior, regardless of whether such perceptions are an accurate reflection of alters’ actual behavior (18). While there is a dearth of research examining the specific effect of social network structure on trans women’s HIV risk/protective behaviors, research suggests that social network dynamics might be particularly influential on trans women’s HIV risk behaviors. Social network dynamics have shown significant associations with patterns of sex work among trans women, and even suggest that among more marginalized trans women, participation in sex work may provide a broad social support network and sense of community (19–20).
The desire to belong to networks of similar others drives the underlying mechanism of social network homophily (21), a principle dictating that over time members of the same social network will tend to resemble one another demographically and behaviorally, with prior examples including similarities in substance use behaviors, religious beliefs, and political orientation (22). Social network homophily has also been previously used to describe patterns in HIV risk behaviors, highlighting that members of the same social network often share similar norms, attitudes, and beliefs around HIV risk and protective behaviors (23–24).
Structured social networks have in recent decades gone from residing predominantly in the pages of academic essays and corporate organizational charts to fundamental and intuitive aspects of persons’ everyday lives in the form of social networking sites and technology use (hereafter “SNS/tech”) such as Facebook, Twitter, and Instagram. Studies of SNS/tech have demonstrated that the principle of social network homophily also applies to virtual communities; people are more likely to be online “friends” with similar others (25). Trans women were early adopters of the Internet and quickly developed online communities of support; (26) the new digital communication medium provided trans women with a means of locating and connecting with other trans women who shared similar struggles and/or triumphs, though they were divided by geographic distance (27). The Internet provided trans women with a way to overcome issues related to small absolute population size, and created a disembodied zone in which new identities and new personas could be more easily adopted and expressed.
Many trans women report using SNS/tech, text messages or chat rooms to develop crucial social support structures (27–28), connect with members of their communities, and gain positive and confirming perspectives on their gender identity (29). Increased social support has been shown to reduce high-risk behaviors among young adult trans women (30) and may improve mental and physical health later in life (31). Conversely, evidence has demonstrated that trans women use SNS/tech to inform and establish high-risk behavioral norms and obtain transgender-specific resources (e.g., non-prescribed hormones, sex work partners) (32–33). Given that trans women may be excluded from other common social networks due to discrimination and/or prejudice (e.g., familial rejection, housing/employment discrimination), many may rely heavily on social networks with other trans women, often formed and maintained online.
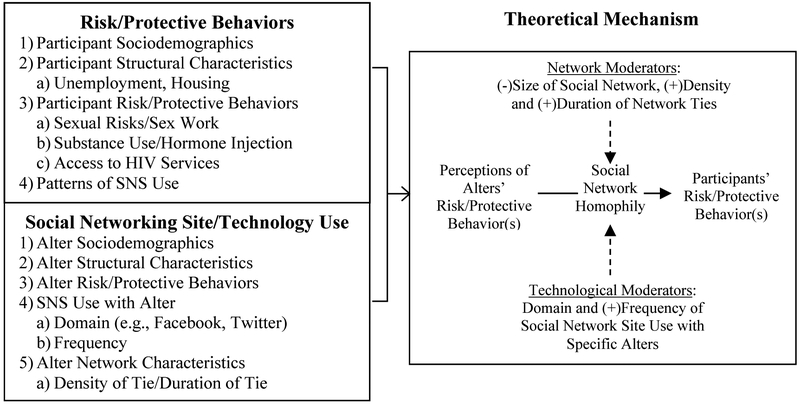
Given the scarcity of research examining trans women’s egocentric social network structure and the influence of alters on HIV risk/protective behaviors, the current study analyzed the empirical structure (i.e., size, density, duration) of trans women’s social networks and estimated how perceived HIV risk/protective behaviors engaged in by alters influenced trans women’s own HIV risk/protective behaviors. Additionally, this study tested whether SNS/tech use moderated the associations between alters’ and participants’ HIV risk/protective behaviors. It was hypothesized that HIV risk/protective behaviors of trans women’s social network alters would be positively associated with trans women’s own HIV risk/protective behaviors (i.e., network homophily). Additionally, it was hypothesized that egocentric network structure and SNS/tech use would moderate such associations so that each of the following network characteristics would result in a larger magnitude alter-participant homophily association: 1) smaller network size (the number of alters nominated by a participant); 2) greater network density (the interconnections between alters); 3) greater network duration (how long a participant has known alters); and 4) SNS/tech use with alters. Figure 1 illustrates these hypothesized associations and how the principle of social network homophily was theorized as the primary mechanism by which perception of alters’ and participants’ behaviors were associated.
Figure 1:
Theoretical Mechanism of Social Network Homophily
Method
Participants
Participants were self-identified trans women (N=271), regardless of their stage of social and/or medical gender transition. Inclusion criteria for study participation were: (1) 18 years of age or older; (2) current gender identity as female/woman/transgender woman/ transsexual woman (or any term along the trans feminine spectrum); (3) assigned biological sex of male at birth; (4) any self-reported alcohol and/or drug use (including non-medically prescribed marijuana) in the previous six months or self-reported condomless anal intercourse (either insertive or receptive) in the previous six months. Individuals were excluded from study participation if they did not meet all criteria or were unable to understand the Informed Consent Form.
Procedure
Participants were enrolled from July 2015 through September 2016. A two-pronged recruitment strategy was utilized to enroll a diverse sample of moderate- to high-risk trans women: (1) street- and venue-based outreach (to recruit trans women who were unlikely to be engaged with a service provider); and, (2) community-based organization outreach (to recruit trans women who were likely to be receiving social services). Recruitment sites varied to sample from as many discrete networks as possible. Two trained research assistants, both of whom identified as trans women, conducted street- and venue-based recruitment at street locations and social venues in which trans women were known to congregate (e.g., bars, cruising areas, clubs, hotels, nail shops, wig stores, electrolysis offices). Potential participants were also recruited in social service agencies providing services to trans women and via word-of-mouth among trans women. Recruitment flyers were posted at collaborating agencies. All outreach locations were reviewed by a trans-specific Community Advisory Board prior to study implementation. Outreach hours included evenings and weekends. Research assistants were trained on non-invasive outreach strategies, such as how to safely approach trans women in the street and how to conduct confidential screening and assessments on site. All participants were enrolled and interviewed in Los Angeles County.
Following screening and informed consent, participants completed an Audio Computer Assisted Self Interview (ACASI) administered on an iPad. An ACASI was utilized for this study to minimize non-response rates to sensitive questions about engagement in risk behaviors. The ACASI permitted participants to enter answers to questions privately into the computer, as questions were read to them through headphones. After responses were entered, the computer selected the next question to be answered based on preprogrammed skip patterns. The ACASI included the Los Angeles Transgender Health Survey (34) and a tailored Social Network Interview (SNI; 35) based on formative work with trans women, which was used for egocentric data collection methods. The study was approved by the Institutional Review Boards at Friends Research Institute and the University of California, Los Angeles. Upon completion of the assessment, all participants were compensated $50.
Measures
Assessments.
Los Angeles Transgender Health Survey.
Originally developed by the first author and colleagues in 1997 (34), in consultation with members of trans women communities in Los Angeles County, and updated as community needs have changed. The Los Angeles Transgender Health Survey consists of six modules: sociodemographics; health care access and medical history including HIV services, hormone use/misuse, gender confirmation surgeries; sexual behaviors (at all stages of gender transition) including HIV risk/protective behaviors; substance use; legal and psychosocial issues including stigma and discrimination; and, HIV prevention and knowledge. For this study, a seventh module on technology use was developed to solicit responses on SNS, Internet, text messaging and email frequency and with whom, and included 7-point Likert scale questions to elicit the participants’ likelihood to participate in various types of technology-based HIV prevention interventions. All behavioral questions were asked with a six-month recall period.
Social Network Interview (SNI).
The SNI, originally developed by Dr. Eric Rice for a social network study with homeless youth (35), was modified for this study in consultation with Dr. Rice and members from the local Los Angeles County trans communities. The SNI asked participants to name social network alters and then answer simple questions about each alter, including specific HIV risk/protective behaviors the participant believed the alter had engaged in, the specific SNS/tech platforms used to communicate with the alter, and how long the participant had known each alter. All participant responses were recorded on an iPad application streamlined to enhance the participant’s ability to provide a large quantity of social network data in a short amount of time with minimal fatigue.
Individual-Level Factors.
Sociodemographics.
Participants reported their age (in years), and their educational attainment in years, which was then coded categorically (less than high school/GED [< 12]; high school/GED [12]; greater than high school/GED [>12]). Participant race/ethnicity was self-reported and coded categorically (Hispanic/Latina; African-American/Black; Mixed Race/Ethnicity; Non-Hispanic White; Native American/Alaskan Native; Asian/Pacific Islander; Other). Participants who reported their current living situation as, “On the streets, in a parked car, in an abandoned building,” were categorized as experiencing homelessness.
Network Alter-Level Factors.
Alter HIV Risk Behaviors.
Engagement in HIV risk behavior(s) for each alter was operationalized as a “no” response to the question, “In the past month, has ALTER NAME consistently used condoms during anal or vaginal sex?,” OR a “yes” response to the question, “Does ALTER NAME engage in sex work?”. A “1” value on the alter HIV risk behavior(s) variable denotes the participant believed this alter engaged in inconsistent condom use and/or sex work.
Alter Protective Behavior.
HIV protective behaviors were operationalized differently for HIV-positive/HIV-negative alters. When discussing HIV positive alters, participants were asked, “In the past month, has ALTER NAME consistently taken their HIV medications?”. When discussing HIV-negative alters, participants were asked, “Has ALTER NAME ever gotten an HIV test or another STD test?”. A “yes” answer to the question asked would warrant a value of “1” on the alter protective behavior(s) variable and would indicate perceived HIV medication adherence (for HIV-positive alters) or HIV/STI status self-monitoring (for HIV-negative alters).
SNS/Technology Use.
SNS/tech use was operationalized as communication with a specific alter through any of the following platforms: Facebook, Instagram, email, Skype/FaceTime, an online/mobile dating site, or via texting. Communication with a specific alter using any of these platforms generated a SNS/tech use value of “1” for that alter, “0” otherwise (e.g., face-to-face communication; telephone voice calls).
Alter Transgender Status.
Participants reported whether or not each alter identified as transgender using a binary yes/no question.
Social Network Size.
Participants were encouraged to list all alters in their social network. The number of reported alters was summed into a count value representing social network size.
Social Network Density.
Using a touchscreen matrix on the iPad, participants reported which alters in their network knew each other. This touchscreen interface was translated into a data matrix whereby each alter was assigned a value of “1” for every other alter they knew and a “0” for those they did not. Values were then summed representing a count value of network density.
Social Network Duration.
Participants reported how long they had known each alter. All reported durations were re-scaled to indicate length of relationship in years with each alter (i.e., 7 days = 7/365.25 = 0.019 duration).
Dependent Variables: Outcomes.
In each case, participant outcomes were operationalized in the same fashion as perceived alter behaviors:
Participant HIV Risk Behavior.
Participants who reported any condomless anal intercourse or sex work as a source of income in the past six months were assigned a value of “1”, “0” otherwise.
Participant HIV Protective Behavior.
HIV-positive participants were asked, “Are you currently receiving any prescribed medications for your HIV infection?”. HIV-negative participants were asked, “Have you ever been tested for HIV, the AIDS virus?”. The HIV protective behavior(s) variable was coded as “1” if the participant answered “yes,” “0” otherwise.
Data Analysis
Stata SE (v13) was used to conduct all analyses. Descriptive and bivariate analyses were conducted on sociodemographics, social network characteristics and HIV risk/protective behaviors. Means and standard deviations were calculated for all continuous or counted variables (e.g., age, number of sex partners), while counts and proportions were calculated for all categorical variables (e.g., race/ethnicity, HIV status, education level). The primary analyses were conducted utilizing multilevel hierarchical generalized linear models (HLM). Multilevel analyses allow for complex modeling of hierarchically structured data: usually, individuals nested within communities (36); here, social network alter data was “nested” within each participant’s data. All multilevel modeling was conducted with a binomial distribution and the logit link function for the dichotomous outcomes of participant HIV risk or protective behavior(s). To isolate hypothesized effects of alter trans status and SNS/tech use, contingency models were conducted for each dichotomous outcome, stratified by SNS/tech use and trans status, for a total of eight analytic models.
The primary hypothesis testing focused on the effects of alter risk/protective behavior(s) homophily. Models assessed moderation of the homophily-HIV risk/protective behavior(s) association by egocentric network morphology (i.e., size, density, duration), contingent upon alter gender (i.e., trans/cisgender) and SNS/tech use. In each model, individual-level covariates included age, race/ethnicity, education level, and homelessness. Coefficient estimates of the multilevel analysis are reported as adjusted odds ratios (aOR) and 95% confidence intervals (CI). Results were flagged for discussion at α ≤ 0.10.
Results
Table 1 details sociodemographic and social network characteristics. Participants mean age was 35.0 (SD: 12.0), most identified as transgender (90.0%), were Hispanic/Latina (42.6%) or African American/Black (30.4%) and identified as heterosexual (73.4%). A majority of participants had attained a high school degree/GED (38.4%) or below (36.5%), and just over half of participants (55.3%) reported earning less than $500 in the previous 30 days. About one-in-six participants (14.8%) were currently experiencing homelessness, and just over one-third (35.4%) were HIV positive. About one-quarter of the participants reported a lifetime history of syphilis (26.7%) or gonorrhea (24.4%). Over one-quarter of the participants reported binge alcohol use (i.e., five or more drinks at one time; 40.2%), non-medical marijuana use (36.2%), or methamphetamine use (27.3%). Most of participants reported some history of incarceration (67.9%).
Table 1:
Participant Sociodemographic and Social Network Characteristics (N=271)
| Mean | SD | |
| Age | 35.03 | 12.01 |
| n | (%) | |
| Racial/Ethnic Identity (N=270) | ||
| Hispanic/Latina | 115 | (42.6%) |
| African American/Black | 82 | (30.4%) |
| Mixed Race/Ethnicity | 24 | (8.9%) |
| Caucasian/White | 20 | (7.4%) |
| Native American/Alaskan Native | 17 | (6.3%) |
| Asian/Pacific Islander | 6 | (2.2%) |
| Other | 6 | (2.2%) |
| Gender Identity | ||
| Transgender | 244 | (90.0%) |
| Woman | 24 | (8.9%) |
| Other | 3 | (1.1%) |
| Sexual Orientation | ||
| Heterosexual/Straight | 199 | (73.4%) |
| Homosexual/Gay/Lesbian | 28 | (10.3%) |
| Bisexual | 17 | (6.3%) |
| Other/Don’t Know/Refused | 27 | (9.9%) |
| Education Level | ||
| Less than High School/GED | 99 | (36.5%) |
| High School/GED | 104 | (38.4%) |
| Greater than High School/GED | 68 | (25.1%) |
| Income (past 30 days) | ||
| ≤ $50 | 41 | (15.1%) |
| $51-$250 | 70 | (25.8%) |
| $250-$499 | 39 | (14.4%) |
| $500-$999 | 61 | (22.5%) |
| $1000-$2999 | 28 | (10.3%) |
| ≥$3000 | 13 | (4.8%) |
| Don’t Know/Refused | 19 | (7.0%) |
| Homelessness Status | ||
| Homeless | 40 | (14.8%) |
| Not Homeless | 228 | (84.1%) |
| Don’t Know/Refused | 3 | (1.1%) |
| HIV Status | ||
| HIV Positive | 96 | (35.4%) |
| HIV Negative | 159 | (58.7%) |
| Don’t Know/Refused | 16 | (5.9%) |
| Lifetime STI History | ||
| Gonorrhea (N=266) | 65 | (24.4%) |
| Syphilis (N=266) | 71 | (26.7%) |
| Chlamydia (N=269) | 48 | (17.8%) |
| Genital Warts (N=266) | 25 | (9.4%) |
| Genital Herpes (N=267) | 16 | (6.0%) |
| Health Care Insurance | ||
| No Health Insurance | 54 | (19.9%) |
| Has Health Insurance | 209 | (77.1%) |
| Don’t Know/Refused | 8 | (3.0%) |
| Substance Use (Past 6 Months)a | ||
| Binge Alcohol Use (5+ Drinks) | 109 | (40.2%) |
| Non-medical Marijuana | 98 | (36.2%) |
| Methamphetamine | 74 | (27.3%) |
| Powder Cocaine | 27 | (10.0%) |
| Ecstasy | 19 | (7.0%) |
| Poppers, Nitrates, or other inhalants | 14 | (5.2%) |
| Uppers or Speed (not Methamphetamine) | 13 | (4.8%) |
| Crack Cocaine | 11 | (4.1%) |
| Tranquilizers (i.e., Valium, Xanax) | 10 | (3.7%) |
| Other Drugs | 10 | (3.7%) |
| Incarceration History (N=268) | ||
| Ever Incarcerated (Jail and/or Prison) | 182 | (67.9%) |
| Never Incarcerated (Jail and/or Prison) | 86 | (32.1%) |
| Mean | SD | |
| Social Network Characteristics | ||
| Network Size (# of alters) | 9.67 | 6.42 |
| range | 1 | 60 |
| Network Duration (N=250) | 11.45 | 8.33 |
| Network Density | 3.35 | 2.96 |
The following substances were reported by 2% or less of sample and not included in table: barbituates/”downers,” LSD/Hallucinogens, ketamine, and heroin.
Participants reported an average of 9.7 (SD: 6.4) alters in their social network and an average alter duration of 11.5 years (SD: 8.3). On average, participant alters were connected with 3.4 (SD: 3.0) other network alters.
Table 2 details HIV risk and protective behaviors in the past six months. Participants reported an average of 23.4 (SD: 56.3) sex partners, and just over half (54.2%) reported condomless anal intercourse (insertive or receptive). Over one-third (36.2%) reported sex work as a main source of income, and the majority (95.2%) reported ever having had an HIV test; among HIV positive participants, 82.3% reported currently being prescribed HIV medications.
Table 2:
HIV Risk and Protective Behaviors (N=271)
| Risk Behaviors | Mean | SD |
|---|---|---|
| Number of Sex Partners (Past 6 months) | 23.4 | 56.3 |
| Condomless Anal Intercourse (Past 6 months) | n | (%) |
| Main partner | 83 | (30.6%) |
| Casual partner | 89 | (32.8%) |
| Exchange partner | 45 | (16.6%) |
| Any partner | 147 | (54.2%) |
| Main Source of Income (Past 6 months) | ||
| Sex work as main income source | 98 | (36.2%) |
| Sex work not main income source | 173 | (63.8%) |
| Protective Behaviors | n | (%) |
| Ever Had HIV Test | 258 | (95.2%) |
| Used Internet to Find HIV/STD Information (N=270) | 167 | (61.9%) |
| Used Internet to Find HIV Test Information (N=270) | 118 | (43.7%) |
| HIV+ Participants’ Protective Behaviors (N=96) | n | (%) |
| Medical Care for HIV | ||
| Receiving medical care for HIV | 82 | (85.4%) |
| Not receiving medical care for HIV | 13 | (13.5%) |
| Don’t know/Refused | 1 | (1.0%) |
| HIV Medication | ||
| Taking medication for HIV | 79 | (82.3%) |
| Not taking medication for HIV | 14 | (14.6%) |
| Don’t know/Refused | 3 | (3.1%) |
| Viral Load Count | ||
| “Undetectable” level (≤500) | 48 | (50.0%) |
| “Detectable” level (≥500) | 23 | (24.0%) |
| Never had test | 1 | (1.0%) |
| Don’t know/Refused | 24 | (25.0%) |
Tables 3 and 4 present the results from the multilevel analyses regressing HIV risk/protective behaviors on participants’ social network factors, contingent on the gender status of that alter and the SNS/tech use engaged in with that alter. Table 3 provides all HIV risk outcomes, while Table 4 provides all HIV protective outcomes.
Table 3:
Social Network Factors, SNS/Technology Use, and Trans Status Association with HIV Risk Behaviors through Robust Hierarchical Logistic Regression
| No Technology Use with Alters | Technology Use with Alters | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome: HIV Risk Behaviors | Trans Alters | Cisgender Alters | Trans Alters | Cisgender Alters | ||||||||
| aOR | 95% CI | Sig. | aOR | 95% CI | Sig. | aOR | 95% CI | Sig. | aOR | 95% CI | Sig. | |
| Age (in years) | 0.92 | 0.88 – 0.97 | p =0.001 | 0.93 | 0.89 – 0.97 | p = 0.001 | 0.96 | 0.93 – 0.99 | p = 0.045 | 0.95 | 0.92 – 0.98 | p = 0.002 |
| Racial/Ethnic Identity | ||||||||||||
| Hispanic/Latina | ref. cat. | ref. cat. | ref. cat. | ref. cat. | ||||||||
| African American/Black | 0.77 | 0.20 – 3.01 | p =0.709 | 0.52 | 0.15 – 1.82 | p = 0.304 | 0.70 | 0.27 – 1.81 | p = 0.460 | 0.56 | 0.23 – 1.34 | p = 0.193 |
| Non-Black/Non-Hispanic | 1.23 | 0.32 – 4.66 | p =0.762 | 0.59 | 0.15 – 1.83 | p = 0.440 | 0.79 | 0.27 – 2.28 | p = 0.657 | 0.64 | 0.23 – 1.80 | p = 0.394 |
| Education Level | ||||||||||||
| Less than High School/GED | ref. cat. | ref. cat. | ref. cat. | ref. cat. | ||||||||
| High School/GED | 3.07 | 0.83 – 11.34 | p =0.093 | 1.39 | 0.38 – 5.14 | p = 0.623 | 0.56 | 0.22 – 1.40 | p = 0.213 | 0.69 | 0.30 – 1.61 | p = 0.393 |
| Greater than High School/GED | 3.49 | 0.75 – 16.13 | p =0.110 | 1.17 | 0.32 – 4.31 | p = 0.814 | 1.47 | 0.46 – 4.74 | p = 0.520 | 0.67 | 0.26 – 1.73 | p = 0.410 |
| Homelessness | ||||||||||||
| Yes | 5.36 | 0.36 – 80.80 | p =0.225 | 67.79 | 0.57 – 8087.38 | p = 0.084 | 7.25 | 1.17 – 45.0 | p = 0.033 | 6.61 | 1.25 – 34.9 | p = 0.026 |
| Alter Homophily | ||||||||||||
| Risk Behavior Homophily | 7.12 | 0.34 −149.83 | p =0.207 | 0.32 | 0.01 – 13.78 | p = 0.552 | 5.87 | 1.33 – 25.8 | p = 0.019 | 4.10 | 1.27 – 13.2 | p = 0.018 |
| Social Network Characteristics | ||||||||||||
| Size | 1.01 | 0.73 – 1.38 | p =0.976 | 0.79 | 0.59 – 1.07 | p = 0.127 | 1.02 | 0.96 – 1.08 | p = 0.569 | 1.03 | 0.97 – 1.10 | p = 0.331 |
| Density | 0.99 | 0.76 – 1.30 | p =0.951 | 0.98 | 0.70 – 1.38 | p = 0.913 | 1.10 | 0.91 – 1.33 | p = 0.340 | 1.21 | 1.03 – 1.42 | p = 0.022 |
| Duration | 1.05 | 0.99 – 1.12 | p =0.091 | 0.99 | 0.93 – 1.06 | p = 0.930 | 1.01 | 0.96 – 1.05 | p = 0.820 | 1.00 | 0.97 – 1.02 | p = 0.682 |
| Social Network Variables Interaction Effects | ||||||||||||
| Size*Homophily | 0.96 | 0.70 – 1.32 | p =0.798 | 1.21 | 0.89 – 1.65 | p = 0.223 | 0.94 | 0.88 – 1.02 | p = 0.121 | 0.96 | 0.89 – 1.04 | p = 0.382 |
| Density*Homophily | 1.04 | 0.78 – 1.39 | p =0.792 | 1.05 | 0.73 – 1.51 | p = 0.796 | 0.93 | 0.75 – 1.13 | p = 0.469 | 0.80 | 0.67 – 0.97 | p = 0.020 |
| Duration*Homophily | 0.92 | 0.85 – 0.99 | p =0.022 | 0.99 | 0.93 – 1.06 | p = 0.797 | 1.01 | 0.95 – 1.08 | p = 0.644 | 1.01 | 0.98 – 1.04 | p = 0.554 |
Table 4:
Social Network Factors, SNS/Technology Use, and Trans Status Association with HIV Protective Behaviors through Robust Hierarchical Logistic Regression
| No Technology Use with Alters | Technology Use with Alters | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome: HIV Protective Behaviors | Trans Alters | Cisgender Alters | Trans Alters | Cisgender Alters | ||||||||
| aOR | 95% CI | Sig. | aOR | 95% CI | Sig. | aOR | 95% CI | Sig. | aOR | 95% CI | Sig. | |
| Age (in years) | 0.99 | 0.90 – 1.11 | p = 0.985 | 0.98 | 0.92 – 1.03 | p = 0.516 | 1.07 | 1.00 – 1.14 | p = 0.049 | 1.02 | 0.98 – 1.07 | p = 0.313 |
| Racial/Ethnic Identity | ||||||||||||
| Hispanic/Latina | ref. cat. | ref. cat. | ref. cat. | ref. cat. | ||||||||
| African American/Black | 1.12 | 0.09 – 13.40 | p = 0.928 | 0.90 | 0.14 – 5.74 | p = 0.908 | 3.10 | 0.42 – 23.1 | p = 0.270 | 1.85 | 0.44 – 7.79 | p = 0.403 |
| Non-Black/Non-Hispanic | 0.46 | 0.03 – 6.67 | p = 0.573 | 0.27 | 0.04 – 1.74 | p = 0.170 | 0.77 | 0.12 – 4.85 | p = 0.782 | 1.49 | 0.24 – 8.95 | p = 0.665 |
| Education Level | ||||||||||||
| Less than High School/GED | ref. cat. | ref. cat. | ref. cat. | ref. cat. | ||||||||
| High School/GED | 12.55 | 0.28 – 554.5 | p = 0.191 | 7.26 | 0.96 – 55.1 | p = 0.055 | 1.00 | 0.22 – 4.56 | p = 0.997 | 0.65 | 0.15 – 2.76 | p = 0.555 |
| Greater than High School/GED | 0.82 | 0.15 – 4.56 | p = 0.820 | -- | -- | -- | 1.83 | 0.35 – 9.53 | p = 0.471 | 0.63 | 0.13 – 2.94 | p = 0.553 |
| Homelessness | ||||||||||||
| Yes | 0.17 | 0.02 – 1.81 | p = 0.140 | 0.06 | 0.01 – 0.68 | p = 0.023 | 0.07 | 0.01 – 0.33 | p = 0.001 | 0.12 | 0.02 – 0.56 | p = 0.007 |
| Alter Homophily | ||||||||||||
| Protective Behavior Homophily | 1.17 | 0.01 – 98.91 | p = 0.944 | 0.63 | 0.07 – 6.92 | p = 0.686 | 4.42 | 0.57 – 33.9 | p = 0.153 | 8.95 | 2.48 – 32.2 | p = 0.001 |
| Social Network Characteristics | ||||||||||||
| Size | 1.37 | 1.01 – 1.86 | p = 0.043 | 1.08 | 1.02 – 1.14 | p = 0.007 | 0.94 | 0.87 – 1.01 | p = 0.103 | 0.95 | 0.86 – 1.05 | p = 0.346 |
| Density | 2.29 | 1.10 – 4.80 | p = 0.027 | 0.92 | 0.75 – 1.13 | p = 0.435 | 1.19 | 0.87 – 1.63 | p = 0.285 | 1.09 | 0.83 – 1.42 | p = 0.536 |
| Duration | 1.23 | 1.00 – 1.52 | p = 0.049 | 0.98 | 0.94 – 1.02 | p = 0.324 | 1.04 | 0.94 – 1.14 | p = 0437 | 1.03 | 0.99 – 1.07 | p = 0.204 |
| Social Network Variables Interaction Effects | ||||||||||||
| Size*Homophily | 1.17 | 0.71 – 1.91 | p = 0.543 | 0.89 | 0.74 – 1.06 | p = 0.184 | 1.08 | 0.97 – 1.21 | p = 0.168 | 1.04 | 0.95 – 1.14 | p = 0.380 |
| Density*Homophily | 0.78 | 0.19 – 3.19 | p = 0.726 | 1.35 | 0.97 – 1.87 | p = 0.075 | 0.75 | 0.58 – 0.96 | p = 0.023 | 0.78 | 0.63 – 0.97 | p = 0.026 |
| Duration*Homophily | 0.81 | 0.66 – 0.99 | p = 0.047 | 1.03 | 0.94 – 1.11 | p = 0.551 | 1.00 | 0.84 – 1.19 | p = 0.988 | 0.96 | 0.91 – 1.02 | p = 0.179 |
Presentation of multilevel analyses results will use the term “ego” to describe participant behavior and characteristics, as is common in social network literature.
HIV Risk Behavior Models by Alter’s Gender
Cisgender Alters.
Among cisgender alters with whom the ego did not communicate via SNS/tech (n = 128 egos; n = 490 alters), there were no significant effects between an ego’s social networks and their own HIV risk behavior. In contrast, among cisgender alters with whom the ego did report communicating via SNS/tech (n = 227 egos; n = 1,215 alters), analyses demonstrated that egos with increasingly dense networks were significantly more likely to report engagement in HIV risk behaviors (Coef. = 0.19; Adjusted Odds Ratio [aOR] = 1.21). Additionally, results demonstrated statistically significant behavioral homophily between egos and their alters (Coef. =1.41; aOR = 4.10). The main effects of network density and HIV risk behavior homophily also demonstrated statistically significant interaction effects (Coef. = −0.22; aOR = 0.80).
Transgender Alters.
Among transgender alters with whom the ego did not communicate via SNS/tech use (n = 98 egos; n = 257 alters), results demonstrated a significant interaction between the length of time the ego had known an alter (i.e., duration) and the HIV sexual risk behaviors of that alter on the ego’s estimated likelihood of engagement in HIV risk behaviors (Coef. = −0.09; aOR = 0.92). Among transgender alters with whom the ego reported communicating via SNS/tech use (n = 190 egos; n = 575 alters), results again demonstrated significant HIV risk behavior homophily between egos and their alters (Coef. = 1.77; aOR = 5.87).
HIV Protective Behavior Models by Alter’s Gender
Cisgender Alters.
Analyses of data from cisgender alters with whom the participant did not communicate via SNS/tech use (n = 85 egos; n = 336 alters) indicated that participants with larger networks were more likely to report engagement in HIV protective behaviors (Coef. = 0.08; aOR = 1.08) but did not demonstrate any further significant effects. Among alters with whom the ego did report communicating with via SNS/tech use (n = 186 egos; n = 989 alters), results again demonstrate both a main effect of perceived behavioral homophily (Coef. = 2.19; aOR = 8.95), as well as an interaction between perceived behavioral homophily and network density (Coef. = −0.24; aOR = 0.78).
Transgender Alters.
Among transgender alters with whom the ego did not communicate via SNS/tech use (n = 85 egos; n = 215 alters), participants with larger networks (Coef. = 0.32; aOR = 1.37) and more dense networks (Coef. = 0.83; aOR = 2.29) were more likely to report engagement in HIV protective behaviors. In addition, the length of time a participant had known a specific alter demonstrated both a significant main effect (Coef. = 0.21; aOR = 1.23), as well as a significant interaction (Coef. = −0.21; aOR = 0.81) with the HIV protective behaviors of that specific alter. In contrast, among trans alters with whom the participant did report communicating with via SNS/tech use (n = 157 egos; n = 486 alters), it was network density (rather than relationship duration) which significantly interacted with the perceived HIV protective behaviors of the alter in its effects on participant’s own HIV protective behaviors (Coef. = −0.29; aOR = 0.75). Overall, the eight multivariate models demonstrated a good fit to the data, with Pseudo R2 estimates ranging from 0.12 to 0.42. Table 5 presents narrative explanations of model findings for the eight multivariate models.
Table 5.
Narrative explanations of HLM models investigating Social Network Factors and Alter SNS/Technology Use and Gender Status
| Model contingency on alter tech use and alter gender status | NARRATIVE EXPLANATIONS OF MODEL FINDINGS* |
|---|---|
| HIV RISK BEHAVIORS OUTCOME | |
|
No technology use; Cisgender alters |
No theoretically explanatory variables reached statistical significance. Cisgender alters not communicating with ego via technology demonstrated no behavioral similarities with ego. |
|
No technology use; Transgender alters |
The longer ego has known a transgender alter with whom they do not communicate via technology, the more likely they are to engage in HIV risk. If that transgender alter was perceived to also be engaged in HIV risk behavior, the effect was mitigated. |
|
Technology use; Cisgender alters |
Increased perception of engagement in HIV risk by cisgender alters with whom ego communicates via technology was associated with increased HIV risk behaviors by ego. The effect was somewhat mitigated as the density of ego’s network increased. |
|
Technology use; Transgender alters |
Increased perception of engagement in HIV risk by transgender alters with whom ego communicates via technology was associated with increased HIV risk behaviors by ego. |
| HIV PROTECTIVE BEHAVIORS OUTCOME | |
|
No technology use; Cisgender alters |
The greater the size of ego’s network, the more likely ego was to engage in HIV protective behaviors. Further, as the density of the alters engaged in HIV protective behaviors increased, ego was more likely to engage in HIV protective behaviors. |
|
No technology use; Transgender alters |
Egos with larger, more dense, and longer-lasting networks that include transgender alters were more likely to engage in HIV protective behaviors. The effect was somewhat mitigated for transgender alters engaged in HIV protective behaviors who ego has known longest. |
|
Technology use; Cisgender alters |
Increased perception of engagement in HIV protective behaviors by cisgender alters with whom ego communicates via technology was associated with increased HIV protective behaviors by ego. The effect was somewhat mitigated as the density of ego’s network increased. |
|
Technology use; Transgender alters |
As alters who were perceived to engage in protective behaviors evidenced more dense connections, ego was less likely to engage in protective behaviors. |
Note: Narrative explanations are focused on social network theory and do not include associations with known constructs of age, homelessness or education.
Discussion
The findings presented here are among the first to empirically document trans women’s egocentric social network structure and the influence of trans women’s social networks on HIV risk/protective behaviors. Participants were predominately trans women of color (81.9%) and reported low income/educational attainment. Over two-thirds of the sample reported a history of incarceration, a gross overrepresentation of lifetime likelihood of incarceration relative to other adult U.S. populations (6.6%) (37). In the past six months, over half of the sample reported condomless anal intercourse and over one-third of the sample reported engaging in sex work for income. Despite having an acute profile of risk, sample demographics were similar to other community samples of trans women from urban centers across the U.S. (38–39), reinforcing the widespread vulnerability of trans women and critical need for innovative and effective targeted health interventions.
Trans women rely on social networks for the acquisition of both valued resources and culturally relevant behavioral norms (19, 32). Following social network theory’s established mechanism of social network homophily (21), it was hypothesized that trans women’s HIV risk/protective behaviors would be positively associated with the perceived HIV risk/protective behaviors of their network alters, and that these associations would be larger in magnitude in smaller/denser networks, with network alters whom they have known for a longer duration, and with network alters with whom they had interacted via SNS/tech. Findings presented here demonstrated that HIV risk/protective behaviors among moderate- and high-risk trans women were indeed influenced by social network structure and the dynamics of perceived behavioral homophily, and that these findings were contingent on SNS/tech use (as well as gender identity of alters, though this was not originally hypothesized). These findings clearly indicated the importance of social network structure on the risk of HIV transmission and acquisition among trans women and highlight the potential for effectively developing SNS/tech-based HIV prevention interventions designed specifically to operate within trans women’s social networks.
HIV Risk Behaviors
Participants’ HIV risk behaviors were positively associated with alters’ HIV risk behaviors, though only with alters with whom the participant reported communicating via SNS/tech use. Participants demonstrated significant behavioral homophily with their cisgender alters, though examination of the moderating effects of network density suggest that such homophily was decremented by increasingly dense networks, and could potentially be obviated entirely in a large, dense social network (e.g., 1.41 + (X)0.19 - (X)0.22 = 0 at X ≥ 47, where X equals the calculated density of the social network). Participants exhibited strong HIV risk behavior homophily with trans alters with whom they communicated via SNS/tech use, and this effect was not moderated by network size, density, or the duration of acquaintance with the trans alter.
Interestingly, analysis of trans alters with whom the participant did not communicate via SNS/tech use indicated that the longer the participant had known such an alter the less likely the participant was to engage in HIV risk behaviors if the alter was perceived to engage in HIV risk behaviors. Thus, results imply that although these trans women were likely to be behaviorally similar to network alters with whom they communicated over SNS/tech use, their HIV risk behaviors perhaps negatively associated with the perceived HIV risk behaviors of alters with whom they did not communicate with using SNS/tech. Previous research has demonstrated substance use homophily within networks of MSM who use social networking apps, another group at high risk for HIV acquisition and transmission (40). Additional research is needed to fully understand processes of influence that may occur via SNS/tech platforms for sexual and gender minority status individuals.
HIV Protective Behaviors
Participants’ HIV protective behaviors demonstrated significant positive association with the perceived HIV protective behaviors of their cisgender alters, but only for those with whom the participant communicated over SNS/tech use. The specific pattern of results for cisgender alters mirrored the results observed for HIV risk behaviors: participants demonstrated significant positive associations with cisgender alters with whom they interacted over SNS/tech use, but this behavioral homophily was decremented by increasingly dense networks. Results for trans alters, however, strongly contrasted with HIV risk behavior findings. Participants did not demonstrate positive associations between their own HIV protective behaviors and the perceived HIV protective behaviors of their trans alters. Instead, for trans alters with whom the participant both did and did not communicate over SNS/tech use, the perceived HIV protective behaviors of trans alters interacted with network density and relationship duration (respectively) to reduce the likelihood that the participant would themselves report engagement in HIV protective behaviors. This implies that the trans women sampled here were more likely to mimic the HIV risk behaviors of their transgender network alters, and less likely to follow suit if they perceive a transgender alter was engaged in HIV protective behaviors.
Social Network Homophily and SNS/Tech Use
Network homophily was strongly influential in predicting both HIV risk and protective behaviors among this sample of trans women, but this effect was almost exclusively apparent among alters with whom a participant communicated via SNS/tech use. This finding demonstrates that technology portals and SNS sites have become a primary source of behavioral norm retrieval for trans women. Such a finding is critically relevant to the development of mobile HIV prevention interventions for trans women at moderate to high risk for HIV. Development of mobile health (mHealth) HIV prevention has the potential to offer interventions that are easily accessible, culturally relevant, and private (41). For trans women facing discrimination, stigma and prejudice, and/or who may not have locally available trans-specific HIV prevention services, SNS/tech-based interventions might provide a more confidential, familiar, accessible, and potentially more effective platform for HIV prevention than currently available in-person services at brick-and-mortar agencies. HIV prevention interventions informed by social network dynamics have been efficacious in other high-risk populations such as MSM (42–43) and injection drug users (44); however, trans women express different needs and risk behaviors than MSM (7), making existing social network interventions designed for MSM inappropriate for trans women. These findings demonstrate that SNS/tech use is essential in HIV risk/protective behavioral norms among trans women, and should be incorporated into HIV prevention interventions targeting this population.
Alters’ Gender Identity Influences HIV Risk/Protective Behaviors
These results also demonstrated that trans women mirrored perceived HIV risk behaviors of other trans women, but did not mirror (and perhaps even eschewed) the perceived HIV protective behaviors of other trans women. Interestingly, participants appeared to act counter to the protective behaviors of their trans alters. Among trans alters with whom participants did not communicate via SNS/tech use, the longer their relationship with an alter who was engaged in protective behaviors, the less likely the participant was to engage in protective behaviors, herself. Similarly, among trans alters with whom participants did communicate via SNS/tech use, a denser network of trans alters engaged in HIV protective behaviors actually decreased participants’ own engagement in protective behaviors. Much of the prior literature on trans women’s social networks has shown that trans women often turn to networks of other trans women to obtain high-risk resources (e.g., non-prescribed hormones, sex work partners), but also to gain social support and capital (29, 32); thus, it was expected, but not proven, that trans alters would exert strong influence on both HIV risk and protective behaviors.
Instead, these findings demonstrated that it was the HIV protective behavior of cisgender alters that exerted positive influence on the HIV protective behaviors of trans women. It was possible that the trans women and their cisgender alters might have been connected through very strong ties (i.e., parent, close relative) from whom behavioral influence on HIV protective behaviors was more impactful than trans peers. This suggests that trans women who have close relationships outside of a network of homophilous trans women may be more likely to engage in HIV protective behaviors than trans women embedded in a network of exclusively comprised of other trans women. It was surmised that when trans women have more supportive cisgender individuals in their social networks, they may feel more accepted, which in turn has been shown to buffer the negative effects of stigma and discrimination that are associated with negative health behaviors (45–46). In a study of networks among homeless youth, another population at high risk for HIV, “pro-social” connections to home-based peers were found to be protective against engagement in HIV-risk behaviors; similar dynamics may apply here (44). Additional research is necessary to investigate the influence of cisgender close relationships (i.e., parents, friends, siblings) on trans women’s behavioral norms. However, findings here suggest that cisgender connections were particularly influential to trans women’s protective behaviors, and that might be a valuable place to intervene in social network interventions.
Social Network Size, Density and Duration
Findings on the influence of social network structure beyond homophily demonstrated that network size, density and duration played particularly important roles in participants’ HIV protective behaviors; however, these characteristics were predominantly relevant only among alters with whom the participant was not connected via SNS/tech use. Indeed, among cisgender alters not engaged through SNS/tech use, social network size and density influenced HIV protective behaviors of participants. Among trans alters not engaged through SNS/tech use, network size, density, and duration were each associated with participants’ HIV protective behaviors. It appears that network size, specifically, is a proxy for social support, and is particularly important for trans women who are not connected to others through SNS/tech. It is plausible that network size may be less relevant for trans women who are in continual online communication with fewer alters. Numerous studies have highlighted the importance of perceived social support on the health and protective behaviors of trans women (47–49). For trans women who are less active on social media or less embedded in supportive communities online, in-person networks should be considered as necessary modes of intervention to influence HIV protective behaviors.
Limitations
These findings must be interpreted within the context of the study’s limitations, including the use of convenience sampling and self-report data. Participants were recruited solely from Los Angeles County and may not represent trans women residing in other regions of the U.S., particularly in less urban or rural locations. Finally, perceived alter behaviors and HIV status were reported by participants, the study team did not contact alters to confirm the responses of the participants. Although it is the perception that alter behaviors have influenced participant behaviors in studies of substance use (50) and sex work (18), differential overestimation or underestimation of alter behaviors may have biased results.
Conclusions
As the first known empirical investigation of trans women’s egocentric social network structure on HIV risk/protective behaviors, this study has demonstrated the importance of social network homophily on HIV risk/protective behaviors among trans women. These findings are especially important in concert with findings showing the influence of SNS/tech use with alters, highlighting the importance of technology-based interventions in HIV prevention for trans women. Indeed, interventions targeting moderate- and high-risk trans women should be especially cognizant of the utility of SNS/tech use as a pathway to intervention participation for trans women who might otherwise be concerned about facing stigma and/or discrimination in a brick-and-mortar healthcare setting, are hard-to-reach due to economic and/or social factors, who live in regions without trans-specific HIV services, or who have not disclosed their gender identity to others. Findings also preliminarily shed light on the vital role that cisgender members of trans women’s social networks play in influencing HIV protective behaviors. More research is needed on the mechanisms by which these social connections are protective. Finally, these findings highlight that the network size, density, and duration are critical in influencing HIV protective behaviors among trans women not connected to others through SNS/tech use. In sum, this study demonstrated the impactful role that social network structure plays in influencing HIV risk/protective behaviors among trans women, laying the foundation for future studies on trans women’s social networks and the development of technology-based network interventions to reduce HIV risk among this vulnerable population.
Acknowledgements:
This study was supported by the National Institute on Drug Abuse, grant #R21DA037816. Drs. Reback and Holloway acknowledge additional support from the National Institute of Mental Health (P30 MH58107). Ms. Clark acknowledges funding support from the Graduate Division, UCLA Fielding School of Public Health (Fellowship in Epidemiology, #104733842). Dr. Holloway acknowledges funding support from the California HIV/AIDS Research Program (RP15-LA-007). The authors would like to acknowledge, thank, and express deep gratitude to the research assistants, without their dedication to both the participants and the aims of the study, this study would have been lacking.
Footnotes
Disclosure of potential conflicts of interest: The authors declare that they have no conflict of interest.
Compliance with Ethical Standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
REFERENCES
- 1.Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R, Adolescent Medicine Trials NEtwork for HIV/AIDS Interventions Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization.Am J Public Health. 2012;102(9): 1751–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lombardi EL, Wilchins RA, Priesing D, Malouf D. Gender violence: Transgender experiences with violence and discrimination. J Homosex. 2002;42(1):89–101. [DOI] [PubMed] [Google Scholar]
- 3.Operario D, Nemoto T. HIV in transgender communities: syndemic dynamics and a need for multicomponent interventions. J Acquir Immune Defic Syndr (1999). 2010;55(Suppl 2):S91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi Ma. The Report of the 2015 U.S. Transgender Survey. 2016.
- 5.Grant JM, Mottet L, Tanis JE, Harrison J, Herman J, Keisling M. Injustice at every turn: A report of the national transgender discrimination survey. National Center for Transgender Equality; 2011. [Google Scholar]
- 6.Sevelius JM, Reznick OG, Hart SL, Schwarcz S. Informing interventions: the importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Educ Prev. 2009;21(2):113–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rohde Bowers J, Branson CM, Fletcher J, Reback CJ. Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Cult Health Sex. 2011;13(06):629–42. [DOI] [PubMed] [Google Scholar]
- 8.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. [DOI] [PubMed] [Google Scholar]
- 9.Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385(9964):274–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. HIV Surveillance Report. US Department of Health and Human Services; Atlanta, GA: US Department of Health and Human Services; 2015. [Google Scholar]
- 12.De Santis JP. HIV infection risk factors among male-to-female transgender persons: a review of the literature. J Assoc Nurses AIDS Care. 2009;20(5):362–72. [DOI] [PubMed] [Google Scholar]
- 13.Operario D, Nemoto T, Iwamoto M, Moore T. Risk for HIV and unprotected sexual behavior in male primary partners of transgender women. Arch Sex Behav. 2011;40(6):1255–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montgomery SB, Hyde J, De Rosa CJ, et al. Gender differences in HIV risk behaviors among young injectors and their social network members. Am J Drug Alcohol Abuse. 2002;28(3):453–75. [DOI] [PubMed] [Google Scholar]
- 15.Latkin C, Mandell W, Oziemkowska M, et al. Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug Alcohol Depend. 1995;38(1):1–9. [DOI] [PubMed] [Google Scholar]
- 16.Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med. 2003;56(3):465–76. [DOI] [PubMed] [Google Scholar]
- 17.Suh T, Mandell W, Latkin C, Kim J. Social network characteristics and injecting HIV-risk behaviors among street injection drug users. Drug Alcohol Depend. 1997;47(2):137–43. [DOI] [PubMed] [Google Scholar]
- 18.Silva-Santisteban A, Raymond HF, Salazar Xet al. Understanding the HIV/AIDS epidemic in transgender women of Lima, Peru: results from a sero-epidemiologic study using respondent driven sampling. AIDS Behav. 2012;16(4):872–81. [DOI] [PubMed] [Google Scholar]
- 19.Sausa LA, Keatley J, Operario D. Perceived risks and benefits of sex work among transgender women of color in San Francisco. Arch Sex Behav. 2007;36(6):768–77. [DOI] [PubMed] [Google Scholar]
- 20.Wilson E, Garofalo R, Harris RD, et al. Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS Behav. 2009;13(5):902–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: Homophily in social networks. Annu Rev Sociol. 2001;27(1):415–44. [Google Scholar]
- 22.Lewis K, Gonzalez M, Kaufman J. Social selection and peer influence in an online social network.Proc Natl Acad Sci USA. 2012;109(1):68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Veinot TC, Caldwell E, Loveluck J, Arnold MP, Bauermeister J. HIV Testing Behavior and Social Network Characteristics and Functions Among Young Men Who have Sex with Men (YMSM) in Metropolitan Detroit. AIDS Behav. 2016;20(11):2739–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amirkhanian YA. Social networks, sexual networks and HIV risk in men who have sex with men. Curr HIV/AIDS Rep. 2014;11(1):81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ellison NB, Steinfield C, Lampe C. The benefits of Facebook “friends:” Social capital and college students’ use of online social network sites. J Comput Mediat Commun. 2007;12(4):1143–68. [Google Scholar]
- 26.Rosser BS, Oakes JM, Bockting WO, Miner M. Capturing the social demographics of hidden sexual minorities: An internet study of the transgender population in the United States. Sex Res Social Policy. 2007;4(2):50–64. [Google Scholar]
- 27.Green-Hamann S, Sherblom JC. Developing a transgender identity in a virtual community. Social networking and impression management. 2013: 185–205. [Google Scholar]
- 28.Shapiro E ‘Trans’ cending barriers: Transgender organizing on the internet. J Gay Lesbian Soc Serv. 2004;16(3–4):165–79. [Google Scholar]
- 29.Singh AA. Transgender youth of color and resilience: Negotiating oppression and finding support. Sex Roles. 2013;68(11–12):690–702. [Google Scholar]
- 30.Stotzer RL. Family Cohesion among Hawai ‘i’s Māhūwahine. Journal of GLBT Family Studies. 2011;7(5):424–35. [Google Scholar]
- 31.Fredriksen-Goldsen KI, Cook-Daniels L, Kim H-J, et al. Physical and mental health of transgender older adults: An at-risk and underserved population. Gerontologist. 2013;54(3):488–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pinto RM, Melendez RM, Spector AY. Male-to-female transgender individuals building social support and capital from within a gender-focused network. J Gay lesbian Soc Serv. 2008;20(3):203–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reisner SL, Mimiaga MJ, Bland S, Mayer KH, Perkovich B, Safren SA. HIV risk and social networks among male-to-female transgender sex workers in Boston, Massachusetts. J Assoc Nurses AIDS Care. 2009;20(5):373–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reback CJ, Simon PA, Bemis CC, Gatson B. The Los Angeles Transgender Health Study: Community Report. Report Funded by the University wide AIDS Research Program. Los Angeles.; 2001. [Google Scholar]
- 35.Rice E, Milburn NG, Rotheram-Borus MJ. Pro-social and problematic social network influences on HIV/AIDS risk behaviours among newly homeless youth in Los Angeles. AIDS Care. 2007;19(5):697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hutchinson P, Mahlalela X, Yukich J. Mass media, stigma, and disclosure of HIV test results: multilevel analysis in the Eastern Cape, South Africa. AIDS Educ Prev. 2007;19(6):489–510. [DOI] [PubMed] [Google Scholar]
- 37.Bonczar TP. Prevalence of Imprisonment in the US Population, 1974–2001. Office of Justice Programs: U.S. Department of Justice; 2003. [Google Scholar]
- 38.Kenagy GP. Transgender health: Findings from two needs assessment studies in Philadelphia. Health Soc Work. 2005;30(1):19–26. [DOI] [PubMed] [Google Scholar]
- 39.Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health. 2009;99(4):713–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holloway IW. Substance use homophily among geosocial networking application using gay, bisexual, and other men who have sex with men. Arch Sex Behav. 2015;44(7):1799–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Catalani C, Philbrick W, Fraser H, Mechael P, Israelski DM. mHealth for HIV treatment & prevention: a systematic review of the literature. Open AIDS J. 2013;7:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amirkhanian YA, Kelly JA, Kabakchieva E, McAuliffe TL, Vassileva S. Evaluation of a social network HIV prevention intervention program for young men who have sex with men in Russia and Bulgaria. AIDS Educ Prev. 2003;15(3):205–20. [DOI] [PubMed] [Google Scholar]
- 43.Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16(2):139–50. [DOI] [PubMed] [Google Scholar]
- 44.Latkin CA, Donnell D, Metzger D, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Social Sci Med. 2009;68(4):740–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ryan C, Russell ST, Huebner D, Diaz R, Sanchez J. Family acceptance in adolescence and the health of LGBT young adults.J Child Adolesc Psychiatr Nurs. 2010;23(4):205–13. [DOI] [PubMed] [Google Scholar]
- 46.Golub SA, Walker JNJ, Longmire-Avital B, Bimbi DS, Parsons JT. The role of religiosity, social support, and stress-related growth in protecting against HIV risk among transgender women. J Health Psychol. 2010;15(8):1135–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Budge SL, Adelson JL, Howard KA. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J. 2013;81(3):545. [DOI] [PubMed] [Google Scholar]
- 48.Factor RJ, Rothblum ED. A study of transgender adults and their non-transgender siblings on demographic characteristics, social support, and experiences of violence. J LGBT Health Res. 2008;3(3):11–30. [DOI] [PubMed] [Google Scholar]
- 49.Nemoto T, Bödeker B, Iwamoto M. Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health. 2011;101(10):1980–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neighbors C, Dillard AJ, Lewis MA, Bergstrom RL, Neil TA. Normative misperceptions and temporal precedence of perceived norms and drinking. J Stud Alcohol. 2006;67(2):290–9. [DOI] [PMC free article] [PubMed] [Google Scholar]