Abstract
Men who have sex with men (MSM) disclose same-sex behaviors with others, creating disclosure networks. This study examined the characteristics of disclosure networks that are associated with HIV testing among MSM in China through an online nationwide survey. Name-generator questions were used to ask each participant (“ego”) to nominate up to five social network members (“alters”) with whom he had disclosed same-sex behaviors. Among the 806 men, the average disclosure network size was 4.05. MSM who reported larger disclosure networks were more likely to have been tested for HIV (aOR =1.21, 95%CI: 1.08–1.34). The most common disclosure network alters were friends (45.1%), followed by sex partners (18.7%) and healthcare professionals (2.5%). Men who disclosed to healthcare professionals were more likely to test for HIV compared to men who disclosed to family members (aOR =5.43, 95%CI: 2.11–14.04). Our findings can inform disclosure network-based interventions to promote MSM HIV testing.
Keywords: HIV, MSM, China, Ego, Network
INTRODUCTION
HIV testing uptake rates among men who have sex with men (MSM) remain low [1,2]. Achieving UNAIDS 90–90-90 targets [3] will require increased HIV testing rates, particularly in low- and middle-income countries. Leveraging social and sexual networks for peer education and partner referral have been useful in facilitating HIV testing [4]. Many social media interventions promote HIV testing among MSM through networks [5–7]. However, these networks are often coarsely described and few studies have examined the composition or characteristics of disclosure of same-sex behaviors among MSM. Understanding men’s disclosure networks may be useful for spurring HIV testing and downstream components of the HIV care continuum.
As MSM disclose their same-sex behavior to others, they create disclosure networks. MSM often disclose to family members, friends, colleagues or healthcare professionals [8–12]. These disclosure targets can offer MSM support, provide access to information, and potentially facilitate HIV testing [13,14]. Disclosing to others, especially to health professionals, is positively correlated with HIV testing across different settings [14,15].
However, in a social context where MSM are highly stigmatized [16], men are often reluctant to disclose MSM behaviors. Disclosure of same-sex behavior can contribute to discrimination, isolation, and bullying [17–19]. Given the potential negative consequences, men often choose to selectively disclose to those who make them feel safe and reserve judgment when they disclose [20]. Men’s choices about to whom they disclose (e.g., strong ties or weak ties) create a variety of network structures [21]. In line with the strength of weak ties theory, people turn to their strong ties (e.g., close family members) for social support and their weak ties (e.g., acquaintance) for access to nonredundant information [22]. As both social support and sharing HIV-related information could motivate MSM to get HIV tested, HIV testing behaviors may spread within disclosure networks [23,24]. This establishes the rationale for peer education and other network-based interventions to enhance HIV testing [25]. Understanding disclosure networks may help us to design future HIV testing interventions.
China is a place where MSM face substantial discrimination [26,27]. Despite this, same-sex behavior disclosure is gradually expanding. Approximately 60% of MSM in China reported ever disclosing to anyone, and more than 15% disclosed to healthcare professionals [15]. This study examined the characteristics of men’s disclosure networks (e.g., disclosure size and relationship with disclosure targets) and their association with HIV testing in China.
METHODS
Participant Recruitment
An online nationwide survey was conducted in January 2017 among Chinese MSM. We followed the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) for reporting the development and findings of online surveys [28]. The pre-test survey was field tested by 30 MSM in July and August 2016, and their feedback was incorporated to finalize the survey. We calculated that a sample size of 452 would be sufficient to provide 80% power to detect a difference between the MSM HIV testing rates among those with larger disclosure networks compared to MSM with smaller disclosure networks.
Participants were recruited through the social media platforms (WeChat and Weibo) of China’s largest gay mobile application, Blued. The Weibo page of Blued has 100,000 followers and each WeChat post has an average of 20,000 reads. An announcement containing the survey link was published on these platforms. To ensure greater diversity among participants, quota sampling was used to ensure sufficient representation of participants from differing education backgrounds (half above and half below high school), monthly income levels (half above and half below 3000 RMB), and outness (half disclosed and another half not disclose to healthcare worker).
Eligibility criteria of participants included born biologically male, had ever engaged in anal sex with a man, were at least 16 years of age (no requirement for parental consent), were willing to provide their cell phone number, and were willing to complete an informed consent procedure. Participants signed an electronic informed consent form before starting the survey and received a 50 RMB (around 7.5 USD) for participating.
Measures
Demographics and behaviors
We collected information on participants’ sociodemographic characteristics, including age, education, income, and marital status. Participants were also asked about their sexual behaviors, including the number of sex partners and condom use practices in the past three months. We also asked participants whether they ever tested for HIV in one’s life time.
Ego-centric approach
We used the name-generator method [29,30] to obtain an egocentric network dataset. We asked each participant (ego) to provide up to five social network members (alters) with whom he disclosed his same-sex behavior. In the instructions, we encouraged egos to use pseudo- but self-recognizable names to label the alters.
Relationship and HIV testing behaviors among the disclosure network
Egos were instructed to report their relationships with each alter they named, i.e., family members, friends, colleagues, casual sex partners, stable sex partners, healthcare professionals, or others. We also collected information about alters’ HIV testing behaviors. Participants were asked to respond to their best knowledge whether the alters had ever tested for HIV.
Statistical Analysis
Descriptive statistics were used to depict men’s socio-demographic information and characteristics of MSM disclosure networks. Egocentric network analysis was used to describe the network characteristics, such as network size (i.e., the total number of alters in ego’s disclosure network). Bivariate and multivariate logistic regressions were used to investigate the association between network size and ego’s HIV testing using STATA 14 program.
In addition, the egocentric network dataset was converted to a dyadic dataset, with each ego-alter dyad as a unit of analysis. Logistic regressions with robust clustered standard errors were conducted to adjust for clustering among ego who nominated multiple alters [31]. Binary and multivariate logistic regressions were conducted to examine the relationship between HIV testing behaviors among each ego-alter dyad. A directed acyclic graph was used to identify the covariates used in this analysis [32]. The covariates were age, education, and marital status.
RESULTS
Characteristics of Egos
Overall, 1,046 men participated in the survey, 836 individuals completed the questionnaire, and 806 (96.4%) who reported at least one alter were included in this analysis.
Of the 806 men, 14.3% (115) were 16–19 years old, most (59.7%, 481) were 20–29, and a quarter (26.1%, 210) were 30 or older. More than half of men (55.3%, 446) had education level at or lower than high school, 16.1% (130) had some college and around thirty percent (28.5%, 230) received education at or above college. Half of men (53.4%, 431) had an annual income less than US$5,500. Most men (90.8%, 732) were single or divorced.
Around one-fourth (22.3%, 145) had multiple sexual partners in recent three months, and half (49.9%, 402) did not consistently use condoms among MSM in the last three months. Around three-fourths (72.2%, 582) of respondents had ever been tested for HIV, and close to half of the egos (46.4%, 374) had at least one alter who ever tested for HIV (Table 1).
Table 1.
Socio-demographic and characteristics of MSM egos, China, 2017 (N=806)
| Total | ||
|---|---|---|
| n | Percentage | |
| Age (years) | ||
| 16–19 | 115 | 14.3% |
| 20–29 | 481 | 59.7% |
| >=30 | 210 | 26.1% |
| Education | ||
| High school or below | 446 | 55.3% |
| Some college | 130 | 16.1% |
| College or above | 230 | 28.5% |
| Annual income (USD) | ||
| <2700 | 176 | 21.8% |
| 2700–5500 | 255 | 31.6% |
| 5501–9200 | 237 | 29.4% |
| 9201–15000 | 86 | 10.7% |
| >15000 | 52 | 6.5% |
| Marital status | ||
| Married | 74 | 9.2% |
| Divorced/Single | 732 | 90.8% |
| Sexual orientation | ||
| Gay | 636 | 78.9% |
| Others a | 170 | 21.1% |
| Number of sexual partners in the past 3 months | ||
| 0–1 | 505 | 77.7% |
| Multiple | 145 | 22.3% |
| Consistent condom use in the past 3 months | ||
| Yes | 404 | 50.1% |
| No | 402 | 49.9% |
| Ever tested for HIV | ||
| Yes | 582 | 72.2% |
| No | 224 | 27.8% |
| Disclosure network size | ||
| 1 | 93 | 11.5% |
| 2 | 74 | 9.2% |
| 3 | 70 | 8.7% |
| 4 | 32 | 4.0% |
| 5 | 537 | 66.6% |
| Number of alters who had ever tested for HIV | ||
| 1 | 141 | 17.5% |
| 2 | 93 | 11.5% |
| 3 | 69 | 8.6% |
| 4 | 34 | 4.2% |
| 5 | 37 | 4.6% |
Note:
Others refer to heterosexual and bisexual.
Characteristics of Alters
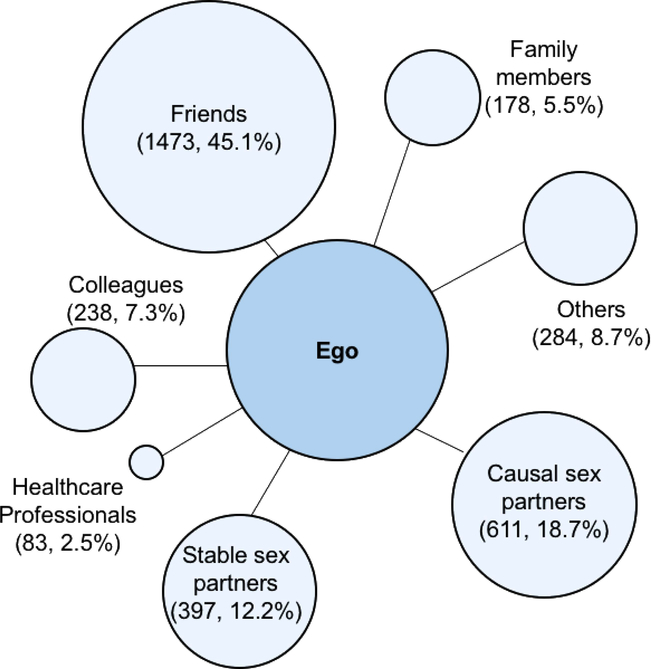
The 806 egos named a total of 3,264 alters. Among the 3,264 alters, 45.1% (1,473/3,264) were friends and only 2.5% (83/3,264) were healthcare professionals. 5.5% (178/3,264) were the ego’s family members and 7.3% (238/3,264) were colleagues (Figure 1).
Figure 1.
The relationship between ego and alters, China, 2017 (N = 3264)
Around two-thirds of egos (66.6%, 537) named five alters (network size = 5), and over one-tenth egos (11.5%, 93) reported one alter (network size = 1). 9.2% (74) egos named two alters (network size = 2), 8.7% (70) ego reported three alters (network size = 3), and 4.0% (32) ego named four alters (network size = 4). Around one-quarter of all alters (26.2%, 855) had ever tested for HIV (Table 1).
Egocentric Network Analysis and HIV Testing Behavior
Disclosure network size was associated with ego’s HIV testing behaviors (Crude OR = 1.21, 95% CI 1.09 – 1.34). Multivariate logistic regression showed that ego’s disclosure network size was significantly associated with his HIV testing behaviors (aOR = 1.18, 95% CI 1.07 – 1.31) after adjusting for age, education, and marital status.
The total number of alters who tested for HIV were associated with ego’s HIV testing behaviors (Crude OR = 2.53, 95% CI 2.03 – 3.16). Multivariate logistic regression showed that men with more alters who tested for HIV were more likely to have tested for HIV (aOR = 2.42, 95%CI 1.94 – 3.02), adjusting for age, education, and marital status.
Dyadic Analysis Between Ego and Alters
3,264 ego-alter dyads were created. The result of multivariate logistic regression analysis (Table 2) with robust clustered standard errors showed that alter’s HIV testing behaviors was associated with the ego’s HIV testing behaviors (aOR = 5.65, 95% CI 3.99 – 8.03). Meanwhile, among ego’s different relationships with alters, disclosing to professionals was more likely to be associated with HIV testing (aOR = 4.78, 95% CI 1.79 –12.73) as compared with disclosing to others.
Table 2.
Multivariate logistic regressions of factors associated with ego’s ever tested for HIV behaviors, China, 2017 (N = 806)
| Ego ever tested for HIV | ||||
|---|---|---|---|---|
| OR | 95%CI | aOR | 95% CI | |
| Disclosure network size | 1.21 | 1.09–1.34 | 1.18 | 1.07–1.31 |
| The total number of alters who ever tested for HIV | 2.53 | 2.03–3.16 | 2.42 | 1.94–3.02 |
| Alter ever tested for HIV | 6.06 | 4.28–8.59 | 5.65 | 3.99–8.03 |
| Ego-alter relationship | ||||
| Family | 0.96 | 0.56–1.64 | 0.92 | 0.54–1.58 |
| Friends | 0.84 | 0.56–1.25 | 0.09 | 0.60–1.35 |
| Colleague | 0.97 | 0.56–1.66 | 0.99 | 0.57–1.74 |
| Casual sex partner | 0.97 | 0.62–1.53 | 0.95 | 0.60–1.51 |
| Stable sex partner | 1.34 | 0.87–2.08 | 1.33 | 0.85–2.07 |
| Health professionals | 5.20 | 1.97–13.75 | 4.78 | 1.79–12.73 |
| Others* | Reference group | |||
Note:
Others refers to other relationships besides friends, colleagues, causal sex partners, stable sex partners, family members, and health professionals.
Multivariate logistic regression controlled for age, education and marital status and clustering among 806 egos.
aOR refers to adjusted odds ratio, and 95%CI refers to 95% confidence intervals.
DISCUSSION
In social contexts where MSM are stigmatized, disclosing same-sex behavior carries substantial risks but also substantial benefits [21,26]. This study examined the relationship between characteristics of same-sex behavior disclosure networks and HIV testing. Most previous studies used egocentric networks to examine MSM sexual partners [33,34]. This study extends the literature by focusing on disclosure networks, using data from a middle-income country, and drawing from a large nationwide survey.
Men disclosed their same-sex behavior to different types of individuals, but the disclosure rate to family members was low. This study found that less than ten percent MSM reported disclosure of same-sex behavior to their family members. The result is similar with others studies reporting that 15 to 25 % of participants disclosed their same-sex behavior to parents in China [35,36]. Traditional perspectives on interpersonal relationships (strong tie vs. weak ties) suggest that men may turn to strong ties when they need social support [35]. However, since disclosing same-sex behavior remains a sensitive topic in many social contexts, men might not disclose to strong ties (i.e. family members). As a sensitive topic of same-sex behavior may put stress on a strong tie relationship and/or by sharing the sensitive information with one’s strong tie, it can easily spread to other strong ties because strong ties are often well-connected [8,37]. Under these circumstances, MSM might not disclose to their family members but activate weak ties (i.e., casual sex partners, others) for access to information about HIV testing as well as social support that cannot be accessed among their strong ties. In addition, the Chinese culture on masculinity, family expectation on marriage and patrilineal structure also stress MSM and make them hesitant to disclose to family members [38–40]. We suggest that future studies pay more attention to MSM’s same-sex behavior disclosure to family members for more support. Interventions need to consider how MSM’s strong ties can provide positive, safe, and nonjudgmental reactions to encourage men’s disclosure of same-sex behaviors [14].
Men who reported more alters who had received HIV testing were in turn more likely to receive an HIV test. This is consistent with the literature that larger social networks who have tested for HIV could facilitate men’s HIV testing uptake in China [41] and globally [42]. This finding suggests a behavioral homophily between men and their same-sex behavior disclosure networks. It is possible that men chose to disclose MSM behaviors to alters with whom they feel similar, and thus they also share similar health concerns and HIV testing behaviors. It is also likely that a man might be easily influenced by his social network, particularly those he trusts to disclose his MSM behaviors, in the adoption of health behaviors [43]. Previous studies observed behavioral homophily from factors including age, gender, ethnicity, and organizational role [44], while this study found behavioral homophily between men and those with whom they disclosed same-sex behavior. This could be useful for developing couples-based [45,46], peer-based [47], or network-based interventions [48,49].
We found disclosing same-sex behavior to healthcare professionals was associated with HIV testing. This finding is consistent with other non-network based survey studies in China [15] and in the US [50]. Disclosure to healthcare professionals is important for provider-driven HIV testing [14,50,51]. However, the rates of men who disclosed their same-sex behaviors to healthcare professionals remain low in many places, ranging from 16% to 90% with a median of 61% [50,52]. Disclosing same-sex behavior to healthcare professionals potentially influences men’s health [53], but some studies also reported MSM being discriminated by health professionals when disclosing their same-sex behaviors [54,55]. A large proportion of MSM reported discomfort in discussing their same-sex behavior with healthcare professionals [52,56]. Medical training and education to improve patient-provider communication and optimize MSM-provider communication about same-sex behavior are needed.
This study has practical and research implications. From a practical perspective, first, personal networks with whom men disclosed their same-sex behavior can potentially impact MSM’s access to HIV testing information and influence their HIV testing behaviors. Public health professionals can motivate peers who received other MSM’s disclosure to promote HIV testing. This approach can also be added to other peer-education intervention programs as peers who can receive same-sex behavior disclosure from MSM may have stronger effects in promoting HIV testing [57]. Second, as far as we know, this study is the first study to examine the same-sex behavior disclosure network and how such networks influence HIV testing. Future research can help us to better understand disclosure networks that could be used for interventions. From a research perspective, disclosure of same-sex behavior network is a sub-field worthy of more attention. This study used a name-generated method and examined the disclosure networks in China. Given that comparative studies found significant differences in disclosure behaviors across different cultures [58,59], exploring same-sex behavior disclosure network in other countries or cultures are needed to fully understand the relationship between disclosure networks and HIV testing.
This study comes with limitations. First, all the egocentric data were based on the ego’s self-report. The network may be biased by the ego’s memory and self-perception. For instance, men may easily recall disclosure to friends whom they encountered more often rather than healthcare professionals whom they only visited occasionally. Still, whom MSM recalled had an effect on their HIV testing behaviors [60]. Second, although this study limited the number of named alters to be a maximum of five informed by prior studies [29,30], the ego network structure may be affected by this limit. Third, this study is a cross-sectional study, therefore we could not draw any causal inferences. Future studies are suggested to qualitatively examine how men disclose to their complete network and acquire some basic information of alters (e.g., age, education, and living areas) to better investigate the relationship between same-sex behavior disclosure and HIV testing.
CONCLUSION
Having a large same-sex behavior disclosure networks, disclosure networks’ HIV testing behaviors, having disclosed MSM behaviors to healthcare professionals, were associated with HIV testing. This study uncovers MSM’s same-sex behavior disclosure network and finds the characteristics of MSM’s disclosure to social networks. In addition, this study suggests the behavioral homophily between MSM and their same-sex behavior disclosure network, indicating potential effectiveness of leveraging network-based interventions to promote HIV testing among MSM.
Acknowledgements
We would like the thank the SESH (Social Entrepreneurship to Spur Health) Global team for assistance.
Funding: This study was funded by National Institutes of Health [National Institute of Allergy and Infectious Diseases 1R01AI114310]; UNC-South China STI Research Training Centre [Fogarty International Centre 1D43TW009532]; UNC Center for AIDS Research [National Institute of Allergy and Infectious Diseases 5P30AI050410]; National Social Science Foundation of China [18CXW017]; Youth Talent Grant of Guangdong Province, China [2017WQNCX129]; Shenzhen University Grant [18QNFC46] and the Bill & Melinda Gates Foundation to the MeSH Consortium (BMGF-OPP1120138). This publication was also supported by Grant Number UL1TR001111 from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health.
Footnotes
Compliance with Ethical Standards:
Conflicts of Interest: Dr. Tucker and Weiming Tang, co-investigators on this study, participate in unpaid activities and as advisors for SESH Global, the coordinating center for this study. No other authors have conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Mitchell S, Cockcroft A, Lamothe G, Andersson N. Equity in HIV testing: evidence from a cross-sectional study in ten Southern African countries. BMC Int. Health Hum. Rights 2010;10:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong Y, Zhang C, Li X, Fang X, Lin X, Zhou Y, et al. HIV testing behaviors among female sex workers in southwest China. AIDS Behav. 2012;16:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNAIDS. 90–90-90: An ambitious treatment target to help end the AIDS epidemic. Http://Www.Unaids.Org/Sites/Default/Files/Media_Asset/90-90-90_En_0.Pdf [Internet]. 2014. [cited 2017 Jul 11];40 Available from: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf [Google Scholar]
- 4.Young SD, Cumberland WG, Nianogo R, Menacho LA, Galea JT, Coates T. The HOPE social media intervention for global HIV prevention in Peru: A cluster randomised controlled trial. Lancet HIV. Elsevier Ltd; 2015;2:e27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tso LS, Tang W, Li H, Yan HY, Tucker JD. Social media interventions to prevent HIV: A review of interventions and methodological considerations. Curr. Opin. Psychol 2015;9:6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tucker JD, Cao B, Li H, Tang S, Tang W, Wong NS, et al. Social Media Interventions to Promote HIV Testing. Clin. Infect. Dis [Internet]. Oxford University Press; 2016. [cited 2016 Oct 24];63:282–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27161778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rhodes SD, McCoy TP, Tanner AE, Stowers J, Bachmann LH, Nguyen AL, et al. Using social media to increase HIV testing among gay and bisexual men, other men who have sex with men, and transgender persons: Outcomes from a randomized community trial. Clin. Infect. Dis Oxford University Press; 2016;62:1450–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Augelli AR, Hershberger SL, Pilkington NW. Lesbian, gay, and bisexual youth and their families: disclosure of sexual orientation and its consequences. Am. J. Orthopsychiatry [Internet]. 1998;68:361–71; discussion 372–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9686289 [DOI] [PubMed] [Google Scholar]
- 9.Durso LE, Meyer IH. Patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbians, gay men, and bisexuals. Sex. Res. Soc. Policy [Internet]. NIH Public Access; 2013. [cited 2017 Jul 4];10:35–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23463442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garofalo R, Mustanski B, Donenberg G. Parents know and parents matter; is it time to develop family-based HIV prevention programs for young men who have sex with men? J. Adolesc. Health [Internet]. NIH Public Access; 2008. [cited 2017 Jul 10];43:201–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18639797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shilo G, Savaya R. Effects of Family and Friend Support on LGB Youths’ Mental Health and Sexual Orientation Milestones. Fam. Relat [Internet]. Blackwell Publishing Ltd; 2011. [cited 2017 Jul 10];60:318–30. Available from: http://doi.wiley.com/10.1111/j.1741-3729.2011.00648.x [Google Scholar]
- 12.Willoughby BLB, Doty ND, Malik NM. Parental Reactions to Their Child’s Sexual Orientation Disclosure: A Family Stress Perspective. Parenting [Internet]. Taylor & Francis Group; 2008. [cited 2017 Jul 4];8:70–91. Available from: http://www.tandfonline.com/doi/abs/10.1080/15295190701830680 [Google Scholar]
- 13.Lin X, Chi P, Zhang L, Zhang Y, Fang X, Qiao S, et al. Disclosure of HIV Serostatus and Sexual Orientation Among HIV-Positive Men Who Have Sex with Men in China. Community Ment. Health J [Internet]. Springer Netherlands; 2016. [cited 2017 May 22];52:457–65. Available from: http://link.springer.com/10.1007/s10597-015-9879-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metheny N, Stephenson R. Disclosure of Sexual Orientation and Uptake of HIV Testing and Hepatitis Vaccination for Rural Men Who Have Sex With Men. Ann. Fam. Med [Internet]. American Academy of Family Physicians; 2016. [cited 2017 Jul 7];14:155–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26951591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang W, Mao J, Tang S, Liu C, Mollan K, Cao B, et al. Disclosure of sexual orientation to health professionals in China: Results from an online cross-sectional study. J. Int. AIDS Soc. [Internet]. International AIDS Society; 2017. [cited 2017 May 23];20 Available from: http://www.jiasociety.org/index.php/jias/article/view/21416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feng Y, Wu Z, Detels R. Evolution of men who have sex with men community and experienced stigma among men who have sex with men in Chengdu, China. J. Acquir. Immune Defic. Syndr [Internet]. NIH Public Access; 2010. [cited 2017 Jul 10];53 Suppl 1:S98–103. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20104118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull [Internet]. NIH Public Access; 2003. [cited 2018 Jun 15];129:674–97. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12956539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henrickson M“You Have to Be Strong to Be Gay”: Bullying and Educational Attainment in LGB New Zealanders. J. Gay Lesbian Soc. Serv [Internet]. Taylor & Francis Group; 2007. [cited 2018 Jun 15];19:67–85. Available from: https://www.tandfonline.com/doi/full/10.1080/10538720802161565 [Google Scholar]
- 19.Daley A, Solomon S, Newman PA, Mishna F. Traversing the Margins: Intersectionalities in the Bullying of Lesbian, Gay, Bisexual and Transgender Youth. J. Gay Lesbian Soc. Serv [Internet]. Taylor & Francis Group; 2007. [cited 2018 Jun 15];19:9–29. Available from: https://www.tandfonline.com/doi/full/10.1080/10538720802161474 [Google Scholar]
- 20.Witzel T, Guise A, Nutland W, Bourne A. It starts with me: privacy concerns and stigma in the evaluation of a Facebook health promotion intervention. Sex. Health [Internet]. 2016. [cited 2017 Jul 10]; Available from: http://sci-hub.cc/http://sci-hub.cc/http://www.publish.csiro.au/sh/sh15231 [DOI] [PubMed]
- 21.Schope RD. The decision to tell: Factors influencing the disclosure of sexual orientation by gay men. J. Gay Lesbian Soc. Serv [Internet]. Taylor & Francis Group; 2002. [cited 2017 Jul 11];14:1–22. Available from: http://www.tandfonline.com/doi/abs/10.1300/J041v14n01_01 [Google Scholar]
- 22.Granovetter MS. The Strength of Weak Ties. Am. J. Sociol [Internet]. University of Chicago Press; 1973. [cited 2018 Aug 5];78:1360–80. Available from: https://www.journals.uchicago.edu/doi/10.1086/225469 [Google Scholar]
- 23.Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer Social Support is Associated with Recent HIV Testing Among Young Black Men Who Have Sex with Men. AIDS Behav. [Internet]. Springer US; 2014. [cited 2018 Aug 5];18:913–20. Available from: http://link.springer.com/10.1007/s10461-013-0608-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cao B, Liu C, Durvasula M, Tang W, Pan S, Saffer AJ, et al. Social media engagement and HIV testing among men who have sex with men in China: A nationwide cross-sectional survey. J. Med. Internet Res. Journal of Medical Internet Research; 2017;19:e251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amirkhanian YA, Kelly JA, Kabakchieva E, McAuliffe TL, Vassileva S. Evaluation of a social network HIV prevention intervention program for young men who have sex with men in Russia and Bulgaria. AIDS Educ. Prev [Internet]. Guilford Publications Inc.; 2003. [cited 2017 Jul 11];15:205–20. Available from: http://guilfordjournals.com/doi/10.1521/aeap.15.4.205.23832 [DOI] [PubMed] [Google Scholar]
- 26.Feng Y, Wu Z, Detels R. Evolution of Men Who Have Sex With Men Community and Experienced Stigma Among Men Who Have Sex With Men in Chengdu, China. JAIDS J. Acquir. Immune Defic. Syndr [Internet]. NIH Public Access; 2010. [cited 2017 Jul 11];53:S98–103. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20104118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neilands TB, Steward WT, Choi K-H. Assessment of Stigma Towards Homosexuality in China: A Study of Men Who Have Sex with Men. Arch. Sex. Behav [Internet]. Springer US; 2008. [cited 2017 Jul 17];37:838–44. Available from: http://link.springer.com/10.1007/s10508-007-9305-x [DOI] [PubMed] [Google Scholar]
- 28.Eysenbach G Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res [Internet]. Journal of Medical Internet Research; 2004. [cited 2017 Jan 3];6:e34 Available from: http://www.jmir.org/2004/3/e34/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marsden P V Network data and measurement. Annu. Rev. Sociol [Internet]. 1990;16:435–463. Available from: http://www.annualreviews.org/doi/abs/10.1146/annurev.so.16.080190.002251%5Cnhttp://www.jstor.org/stable/10.2307/2083277 [Google Scholar]
- 30.Marin A, Hampton KN. Simplifying the personal network name generator. Field methods [Internet]. 2007;19:163–193. Available from: http://fmx.sagepub.com/content/19/2/163.short [Google Scholar]
- 31.Lindgren KO. Dyadic regression in the presence of heteroscedasticity-An assessment of alternative approaches. Soc. Networks 2010;32:279–89. [Google Scholar]
- 32.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology [Internet]. 1999. [cited 2018 Nov 26];10:37–48. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9888278 [PubMed] [Google Scholar]
- 33.Liu H, Feng T, Liu H, Feng H, Cai Y, Rhodes AG, et al. Egocentric Networks of Chinese Men Who Have Sex with Men: Network Components, Condom Use Norms, and Safer Sex. AIDS Patient Care STDS [Internet]. 2009. [cited 2018 Jul 20];23:885–93. Available from: http://www.liebertpub.com/doi/10.1089/apc.2009.0043 [DOI] [PubMed] [Google Scholar]
- 34.Flom PL, Friedman SR, Kottiri BJ, Neaigus A, Curtis R, Des Jarlais DC, et al. Stigmatized drug use, sexual partner concurrency, and other sex risk network and behavior characteristics of 10–24 year old youth in a high-risk neighborhood. Sex. Transm. Dis [Internet]. 2001. [cited 2018 Jul 20];28:598–607. Available from: https://journals.lww.com/stdjournal/Abstract/2001/10000/Stigmatized_Drug_Use,_Sexual_Partner_Concurrency,.6.aspx [DOI] [PubMed] [Google Scholar]
- 35.Zhao Y, Ma Y, Chen R, Li F, Qin X, Hu Z. Non-disclosure of Sexual Orientation to Parents Associated with Sexual Risk Behaviors Among Gay and Bisexual MSM in China. AIDS Behav. [Internet]. Springer US; 2016. [cited 2017 May 22];20:193–203. Available from: http://link.springer.com/10.1007/s10461-015-1135-6 [DOI] [PubMed] [Google Scholar]
- 36.Guo Y, Li X, Liu Y, Jiang S, Tu X. Disclosure of same-sex behavior by young Chinese migrant men: context and correlates. Psychol. Health Med. [Internet]. Routledge; 2014. [cited 2018 Aug 5];19:190–200. Available from: http://www.tandfonline.com/doi/abs/10.1080/13548506.2013.793367 [DOI] [PubMed] [Google Scholar]
- 37.Small ML, Sukhu C. Because they were there: Access, deliberation, and the mobilization of networks for support. Soc. Networks [Internet]. 2016. [cited 2018 Aug 5];47:73–84. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0378873316301708 [Google Scholar]
- 38.Liu JX, Choi K. Experiences of Social Discrimination Among Men Who Have Sex with Men in Shanghai, China. AIDS Behav. [Internet]. 2006. [cited 2018 Aug 5];10:25–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16715344 [DOI] [PubMed] [Google Scholar]
- 39.Choi K-H, Steward WT, Miège P, Hudes E, Gregorich SE. Sexual Stigma, Coping Styles, and Psychological Distress: A Longitudinal Study of Men Who Have Sex With Men in Beijing, China. Arch. Sex. Behav [Internet]. NIH Public Access; 2016. [cited 2018 Aug 5];45:1483–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26679303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wah-Shan C. Homosexuality and the Cultural Politics of Tongzhi in Chinese Societies. J. Homosex [Internet]. Taylor & Francis Group; 2001. [cited 2018 Aug 5];40:27–46. Available from: http://www.tandfonline.com/doi/abs/10.1300/J082v40n03_03 [DOI] [PubMed] [Google Scholar]
- 41.Huang ZJ, He N, Nehl EJ, Zheng T, Smith BD, Zhang J, et al. Social Network and Other Correlates of HIV Testing: Findings from Male Sex Workers and Other MSM in Shanghai, China. AIDS Behav. [Internet]. 2012. [cited 2018 Aug 5];16:858–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22223298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amirkhanian YA, Kelly JA, Takacs J, Mcauliffe TL, Kuznetsova A V., Toth TP, et al. Effects of a social network HIV/STD prevention intervention for MSM in Russia and Hungary. AIDS [Internet]. 2015. [cited 2018 Aug 5];29:1 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25565495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centola D An Experimental Study of Homophily in the Adoption of Health Behavior. Science (80-.). [Internet]. 2011. [cited 2017 Jul 12];334:1269–72. Available from: http://science.sciencemag.org/content/334/6060/1269 [DOI] [PubMed] [Google Scholar]
- 44.Shrum W, Cheek NH, Hunter SM, Hunter SM. Friendship in School: Gender and Racial Homophily. Sociol. Educ [Internet]. American Sociological Association; 1988. [cited 2017 Jul 12];61:227 Available from: http://www.jstor.org/stable/2112441?origin=crossref [Google Scholar]
- 45.Orne-Gliemann J, Balestre E, Tchendjou P, Miric M, Darak S, Butsashvili M, et al. Increasing HIV testing among male partners. AIDS [Internet]. 2013;27:1167–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23343912 [DOI] [PubMed] [Google Scholar]
- 46.Boeras DI, Luisi N, Karita E, McKinney S, Sharkey T, Keeling M, et al. Indeterminate and discrepant rapid HIV test results in couples’ HIV testing and counselling centres in Africa. J. Int. AIDS Soc 2011;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: The social networks demonstration project. Am. J. Public Health. 2009;99:1093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valente TW. Network interventions [Internet]. Science (80-. ). 2012. [cited 2018 Aug 15]. p. 49–53. Available from: http://science.sciencemag.org/content/337/6090/49.short [DOI] [PubMed]
- 49.Valente TW, Fosados R. Diffusion of Innovations and Network Segmentation: The Part Played by People in Promoting Health. Sex. Transm. Dis [Internet]. 2006. [cited 2018 Aug 15];33:S23–31. Available from: https://insights.ovid.com/crossref?an=00007435-200607001-00005 [DOI] [PubMed] [Google Scholar]
- 50.Stupiansky NW, Liau A, Rosenberger J, Rosenthal SL, Tu W, Xiao S, et al. Young Men’s Disclosure of Same Sex Behaviors to Healthcare Providers and the Impact on Health: Results from a US National Sample of Young Men Who Have Sex with Men. AIDS Patient Care STDS [Internet]. 2017. [cited 2018 Jun 23];31:342–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28753396 [DOI] [PubMed] [Google Scholar]
- 51.Coleman TA, Bauer GR, Pugh D, Aykroyd G, Powell L, Newman R. Sexual Orientation Disclosure in Primary Care Settings by Gay, Bisexual, and Other Men Who Have Sex with Men in a Canadian City. LGBT Heal. [Internet]. Mary Ann Liebert, Inc. 140 Huguenot Street, 3rd Floor New Rochelle, NY 10801 USA; 2017. [cited 2018 Jun 23];4:42–54. Available from: http://online.liebertpub.com/doi/10.1089/lgbt.2016.0004 [DOI] [PubMed] [Google Scholar]
- 52.Qiao S, Zhou G, Li X. Disclosure of Same-Sex Behaviors to Health-care Providers and Uptake of HIV Testing for Men Who Have Sex With Men: A Systematic Review. Am. J. Mens. Health [Internet]. 2018. [cited 2018 Aug 5];155798831878414. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29947563 [DOI] [PMC free article] [PubMed]
- 53.Calabrò RS, Quattrini F. Disclosing Sexual Orientation to Healthcare Providers: Still a Taboo or Time for a Change? J. Natl. Med. Assoc [Internet]. Elsevier; 2018. [cited 2018 Jun 23];0. Available from: http://linkinghub.elsevier.com/retrieve/pii/S002796841730295X [DOI] [PubMed]
- 54.Fisher CB, Fried AL, Macapagal K, Mustanski B. Patient–Provider Communication Barriers and Facilitators to HIV and STI Preventive Services for Adolescent MSM. AIDS Behav. [Internet]. Springer US; 2018. [cited 2018 Jun 23];1–12. Available from: http://link.springer.com/10.1007/s10461-018-2081-x [DOI] [PMC free article] [PubMed]
- 55.Stojisavljevic S, Djikanovic B, Matejic B. ‘The Devil has entered you’: A qualitative study of Men Who Have Sex With Men (MSM) and the stigma and discrimination they experience from healthcare professionals and the general community in Bosnia and Herzegovina. Ross MW, editor. PLoS One [Internet]. Public Library of Science; 2017. [cited 2018 Jun 23];12:e0179101 Available from: http://dx.plos.org/10.1371/journal.pone.0179101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bernstein KT, Liu K-L, Begier EM, Koblin B, Karpati A, Murrill C. Same-Sex Attraction Disclosure to Health Care Providers Among New York City Men Who Have Sex With Men<subtitle>Implications for HIV Testing Approaches</subtitle> Arch. Intern. Med [Internet]. American Medical Association; 2008. [cited 2018 Aug 5];168:1458 Available from: http://archinte.jamanetwork.com/article.aspx?doi=10.1001/archinte.168.13.1458 [DOI] [PubMed] [Google Scholar]
- 57.Young SD, Cumberland WG, Nianogo R, Menacho LA, Galea JT, Coates T. The HOPE social media intervention for global HIV prevention in Peru: a cluster randomised controlled trial. Lancet HIV. 2015;2:e27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chu S-C, Choi SM. Social capital and self-presentation on social networking sites: a comparative study of Chinese and American young generations. Chinese J. Commun [Internet]. 2010. [cited 2018 Aug 5];3:402–20. Available from: http://www.tandfonline.com/doi/abs/10.1080/17544750.2010.516575 [Google Scholar]
- 59.Mazur E, Li Y. Identity and self-presentation on social networking web sites: A comparison of online profiles of Chinese and American emerging adults. Psychol. Pop. Media Cult. [Internet]. 2016. [cited 2018 Aug 5];5:101–18. Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/ppm0000054 [Google Scholar]
- 60.Reilly KH, Neaigus A, Shepard CW, Cutler BH, Sweeney MM, Rucinski KB, et al. It’s Never Just HIV : Exposure to an HIV Prevention Media Campaign and Behavior Change Among Men Who Have Sex with Men Participating in the National HIV Behavioral Surveillance System in New York City. LGBT Heal. [Internet]. 2016. [cited 2018 Jun 23];3:314–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26651497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tang W, Mao J, Tang S, Liu C, Mollan K, Cao B, et al. Disclosure of sexual orientation to health professionals in China: results from an online cross-sectional study. J. Int. AIDS Soc [Internet]. 2017. [cited 2017 Jul 7];20:1–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28361498 [DOI] [PMC free article] [PubMed] [Google Scholar]