Abstract
Background:
Individuals often report allergy to specific aeroallergens, but allergy testing can reveal disparate sensitization.
Objective:
To characterize the agreement between perceived and actual sensitization to individual aeroallergens in an urban pediatric population.
Methods:
253 children were enrolled from pediatric clinics in New York, NY. Detailed questionnaires regarding perceived sensitization and serum specific IgE measurements to ten common aeroallergens were completed. Agreement between perceived and actual sensitization (sIgE ≥ 0.35 kUA/L) to individual aeroallergens was assessed by Cohen’s Kappa. Multivariable logistic regression models adjusted for potential confounders were used to test for associations between perceived and actual sensitization.
Results:
161 (63.6%) of the 253 children reported perceived sensitization to ≥1 aeroallergen, and 203 (80.2%) were actually sensitized to ≥1 aeroallergen. Agreement between perceived and actual aeroallergen sensitization was fair for most aeroallergens, with greatest agreement for cat dander (Kappa 0.42, 95% CI 0.32–0.53) and dust (Kappa 0.32, 95% CI 0.20–0.44). Models adjusted for potential confounders showed nearly 6-fold odds of sensitization to cat dander given perceived cat allergy (aOR 5.82, 95%CI 2.91–11.64), and over 2-fold odds of sensitization to D. pteronyssinus, D. farinae, dog dander, or grass pollen given perceived sensitization to their respective allergens. Among children with no perceived sensitization, actual sensitization ranged from 5.4% to 30.4%, and was more common for indoor vs. outdoor allergens, including cockroach.
Conclusion:
Children who perceive allergen sensitization to cat, dog, dust or grass are likely to demonstrate actual sensitization to these individual allergens. Children with no perceived sensitization to allergens are nonetheless frequently sensitized.
Keywords: Sensitization, aeroallergen, environment, urban, pediatric, cat dander, dog dander, pollen, dust mite, cockroach
Introduction
Management of allergic disorders is shaped by appropriate recognition of allergens. Conditions driven by aeroallergen sensitization, including allergic rhinitis and asthma, affect a significant proportion of the population. Characterized by naso-ocular symptoms to indoor and/or outdoor allergen exposure (i.e. dust, pollen, animal dander), allergic rhinitis (AR) affects up to 40% of children and 10–30% of adults.1, 2 Asthma is also widely prevalent, affecting 8.3% of US children,3 with symptoms also commonly trigged by aeroallergen exposure.
Allergen avoidance is contingent upon accurate recognition of allergens so that exposure can be minimized.1, 4 Suboptimal understanding and perception of disease can lead to incorrect avoidances and inadequate disease control.5–7 Because obtaining history from the patient is the initial step in allergy care, knowledge of the degree of agreement between patients’ reported allergen sensitization versus actual allergen sensitization is vital background.
Although there have been many studies on the prevalence of aeroallergen sensitization8–11, far fewer studies have specifically examined the agreement between perceived versus actual sensitization to individual aeroallergens.12–15 Only two studies to date have examined this topic in children. One was a relatively small study limited to 95 asthmatic children seen at a tertiary care military medical center that encompassed only three allergens,13 while the other study was of rural Canadian children.15 The aim of our study was to quantify the agreement between perceived vs. actual sensitization to ten common aeroallergens in an urban pediatric population.
Methods
Study Population
Two hundred fifty-three participants were enrolled from general pediatric and subspecialty pediatric clinics within the Mount Sinai Health System, New York, NY. Participation involved a detailed questionnaire regarding demographic and allergy history that was completed by the participant and their parent(s) together. A peripheral blood sample was also obtained from each subject. The research protocol was approved by the Mount Sinai Institutional Review Board.
Assessment of perceived allergen sensitization and related variables
Perceived allergen sensitization was assessed by the following question: “Check any of the following to which you seem to have allergies that trigger or cause symptoms that bother you.” Individual checkboxes were provided for tree pollen, grass pollen, weed pollen, mold, dust, cat, dog, cockroach, mouse, and other with directions to specify other. Participants were asked if they had doctor-diagnosed allergic rhinitis/hay fever, and their asthma status was determined based on reported symptoms, asthma medication use, and lung function testing. Family history of atopy was assessed via questions about asthma, allergic rhinitis, atopic dermatitis, or other allergic disorder for each first-degree family member. Season of enrollment was categorized as spring (March-May), summer (June-July), fall (August-November), or winter (December-February).
Measurement and definition of aeroallergen sensitization
Serum specific IgE levels to common aeroallergens were measured by ImmunoCAP (Thermo Fisher – PHADIA) for the following ten allergens and allergen mixes: tree pollen mix, grass pollen mix, weed pollen mix, mold mix, Dermatophagoides pteronyssinus (DP) Dermatophagoides farinae (DF), cat dander, dog dander, Blatella germanica (cockroach), and mouse urine. The tree mix included box elder, white birch, hazel, white oak, and London plane tree pollens. The grass mix included Bermuda, English Rye, Timothy, Kentucky bluegrass, Johnson, and Bahia grass pollens. The weed mix included ragweed, mugwort, plantain, lamb’s quarters, and Russian thistle weed pollens. The mold mix included Penicillium, Cladosporium, Aspergillus, and Alternaria. Sensitization to an aeroallergen was defined as serum specific IgE level (sIgE) ≥ 0.35 kUA/L to that specific aeroallergen. Any sensitization was defined as sIgE ≥ 0.35 kUA/L to any aeroallergen. Secondary analyses were also performed using alternative cutoffs, including sIgE > 0.10 kUA/L (detection limit) and sIgE ≥10 kUA/L.
Statistical Analyses
Statistical calculations were conducted using R version 3.2.2 and SPSS Statistics for Macintosh Version 22.0. Comparisons between groups were made using student t-test for continuous variables and Fisher’s Exact test for categorical variables. Cohen’s Kappa tests were performed to evaluate the agreement between perceived and actual allergen sensitization.16 Kappa coefficients were interpreted according to this scale: > 0.80 (very good agreement), 0.61–0.80 (good), 0.41–0.60 (moderate), 0.21–0.40 (fair), 0.00–0.20 (slight), and <0 (poor, i.e. worse than random chance).16 Multivariable logistic regression models were constructed to calculate adjusted odds ratios for actual sensitization given perceived sensitization, adjusted for potential confounders including age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history.
Results
Characteristics of the cohort
The baseline characteristics of the study participants are shown in Table 1. Of the 253 subjects who participated, 161 (63.6%) perceived allergen sensitization to at least one aeroallergen, while 92 (36.4%) had no perceived allergen sensitization. The prevalence of aeroallergen sensitization was 76.3% in the overall study. Half of the cohort endorsed physician diagnosed allergic rhinitis or asthma.
Table 1 –
Baseline Characteristics of the Participating Subjects
| All subjects | Perceived Allergen Sensitization | |||
|---|---|---|---|---|
| N=253 | Yes N=161 |
No N=92 |
P value* | |
| Age: Years | 13.5±4.2 | 12.9±4.0 | 14.5±4.5 | 0.005 |
| Sex: Female | 120 (47.4%) | 69 (42.9%) | 51 (55.4%) | 0.07 |
| Race/ethnicity | 0.17 | |||
| Caucasian | 111 (43.9%) | 74 (46.0%) | 37 (40.2%) | |
| African American | 39 (15.4%) | 27(16.8%) | 12 (13.0%) | |
| Latino | 61 (24.1%) | 37 (23.0%) | 24 (26.1%) | |
| Asian | 19 (7.5%) | 7 (4.3%) | 12 (13.0%) | |
| Multiracial | 21 (8.3%) | 15 (9.3%) | 6 (6.5%) | |
| Unknown | 2 (0.8%) | 1 (0.6%) | 1 (1.1%) | |
| Aeroallergen sensitization to ≥1 aeroallergen | 193 (76.3%) | 141 (87.6%) | 52 (57.8%) | 7.3×10−8 |
| Season of enrollment | 0.008 | |||
| Spring | 59 (23.3%) | 28 (17.4%) | 31 (33.7%) | |
| Summer | 41 (16.2%) | 25 (15.5%) | 16 (17.4%) | |
| Fall | 88 (34.8%) | 58 (36.0%) | 30 (32.6%) | |
| Winter | 65 (25.7%) | 50 (31.1%) | 15 (16.3%) | |
| Family history of atopy | 189 (74.7%) | 133 (82.6%) | 56 (58.7%) | 5.9×10−5 |
| Allergic rhinitis | 127 (50.2%) | 117 (72.7%) | 10 (10.9%) | 8.4×10−23 |
| Asthma | 118 (46.6%) | 96 (59.6%) | 22 (23.9%) | 3.18×10−8 |
Values are number (%) or mean ±SD.
Fisher’s Exact Test was used for all variables except for age where t-test was used.
Perceived allergen sensitization
The baseline characteristics of the cohort stratified by perceived allergen sensitization are additionally shown in Table 1. As expected, subjects who perceived allergen sensitization (n=161) were more likely to have actual aeroallergen sensitization to at least one allergen (OR 5.42, 95% CI 2.91–10.12). Children with perceived allergen sensitization were more likely to be younger with comorbid allergic rhinitis (OR 21.8, 95% CI 10.4–45.8), asthma (OR 4.7, 95%CI 2.6–8.3), and a family history of atopy (OR 3.4, 95% CI 1.9–6.2). Regarding family history, a paternal history of atopy was associated with perceived allergen sensitization to at least one aeroallergen with the highest odds (OR 2.8, 95% CI 1.6–4.8), followed by maternal history of atopy (OR 2.4, 95% CI 1.4–4.1), and sibling history of atopy (OR 2.0, 95% CI 1.1–3.5). Interestingly, 57.8% of subjects with no perceived allergen sensitization were still sensitized to at least one aeroallergen.
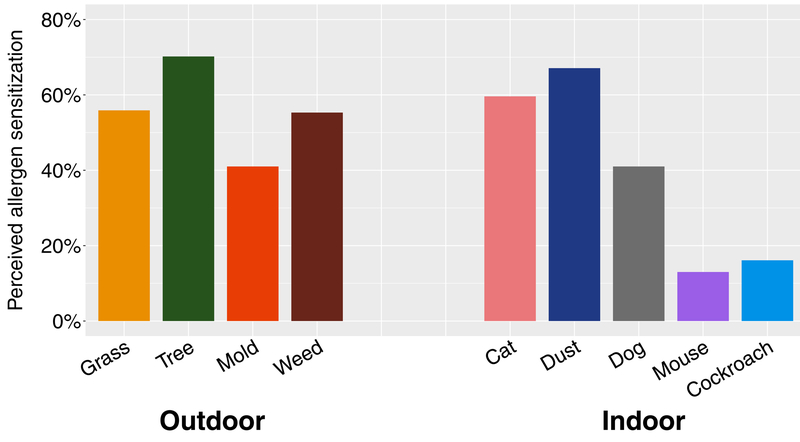
Among the 161 subjects with perceived allergen sensitization, prevalence of perceived sensitization to outdoor and indoor allergens were similar – 85.7% perceived allergen sensitization to at least one indoor allergen and 83.9% perceived allergen sensitization to at least one outdoor allergen. The mean number of perceived allergens was 4 (SD = 2.3). Figure 1 shows the prevalence of perceived allergen sensitization for each aeroallergen among the subjects. Tree pollen was the most commonly reported allergen (70.2%) followed by dust (67.1%).
Figure 1. Perceived sensitization to individual aeroallergens.
Among children reporting perceived sensitization to at least one aeroallergen (n=161), the prevalence of perceived sensitization to individual aeroallergens are shown.
Given the possibility that in-season enrollment could influence perceived culprit allergens, we tested whether season of enrollment was associated with perceived sensitization to seasonal allergens. There was no association between spring enrollment and perceived tree pollen allergy (Fisher’s exact P=0.23), no association between summer enrollment and perceived grass pollen allergy (Fisher’s exact P=0.60), and no association between fall enrollment and perceived weed pollen allergy (Fisher’s exact P=0.41).
Actual allergen sensitization
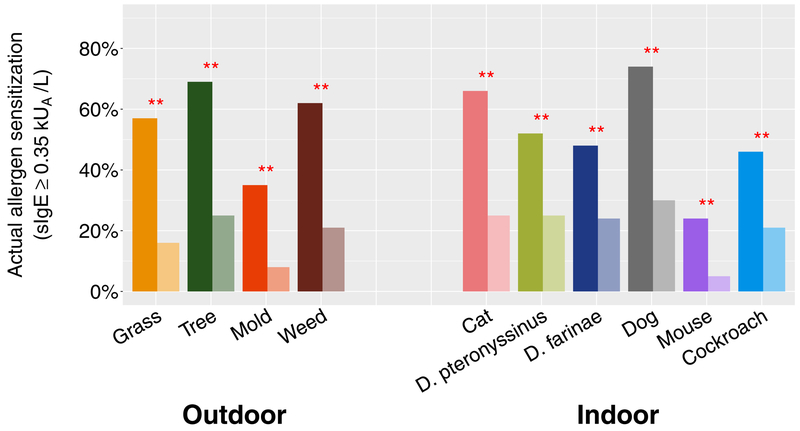
Figure 2 shows the prevalence of actual sensitization (sIgE ≥ 0.35 kUA/L) to each aeroallergen among subjects with perceived allergen sensitization (darker bars) juxtaposed against prevalence in subjects with no perceived allergen sensitization (lighter bars). Among children with perceived allergen sensitization, actual sensitization was highest to dog dander, tree pollen mix, cat dander, and weed pollen mix. Although prevalences of actual sensitization among children with no perceived allergen sensitization were significantly lower than those of their counterparts who perceived allergen sensitization, the prevalence of actual sensitization to each aeroallergen in these non-perceivers was still substantial for each aeroallergen, including cockroach. The mean number of aeroallergens to which subjects were sensitized was 4.1 (SD = 3.3). Subjects sensitized to at least one outdoor allergen were 13-fold (95%CI 7.1–26.9) more likely to also be sensitized to an indoor allergen.
Figure 2. Actual sensitization to individual aeroallergens.
Prevalence of actual sensitization (sIgE ≥ 0.35 kUA/L) to individual aeroallergens are shown for children with perceived sensitization (darker bars) and children with no perceived sensitization (lighter bars). Fisher’s exact P-values are indicated for comparisons between children with and without perceived allergen sensitization. *P value ≤ 0.05, **P value ≤0.001.
Agreement Between Perceived and Actual Sensitization to Specific Aeroallergens
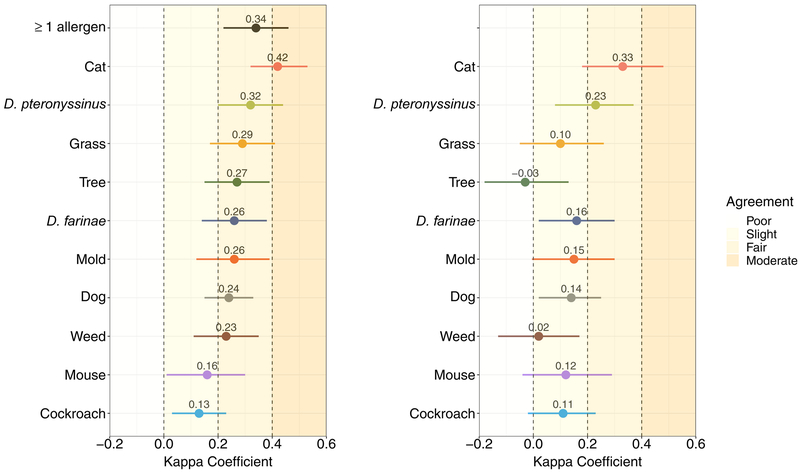
Overall, there was fair agreement between perceived and actual sensitization to at least one aeroallergen (K 0.34, 95% CI 0.22–0.46) (Figure 3A). In focused analyses where we examined for agreement between perceived and actual sensitization to specific aeroallergens, Kappa statistics showed good agreement for cat dander and fair agreement for most aeroallergens except mouse and cockroach, where there was only slight agreement (Figure 3A). In the overall study population, there was greatest agreement between perceived and actual sensitization to cat dander ((K 0.42, 95% CI 0.32–0.53), followed by DP (K 0.26, 95% CI 0.200.44) and grass pollen (K 0.29, 95% CI 0.17–0.41). There was least agreement between perceived and actual cockroach allergen sensitization (K 0.13, 95%CI, 0.03–0.23).
Figure 3. Agreement Between Perceived and Actual Sensitization to Individual Aeroallergens.
Kappa coefficients for tests of agreement, along with their 95% confidence intervals, are shown for (A) the overall study cohort (n=253), and (B) subjects with perceived sensitization to ≥1 aeroallergen (n=161).
In stratified analyses of subjects with perceived allergen sensitization only, agreement between perceived and actual sensitization to cat dander continued to have the highest agreement (K 0.33, 95% CI 0.18–0.48) (Figure 3B). Similar to results from the overall analysis, agreement between perceived and actual sensitization to DP (K 0.23, 95% CI 0.08–0.37) had the next highest Kappa coefficient. There was slight agreement among the remaining aeroallergens, except tree pollen, for which there was poor agreement among perceivers.
The coefficients for agreement between perceived and actual sensitization in analyses stratified by allergic rhinitis, asthma, and family history of atopy are shown in Table 2. Cat continued to demonstrate the highest agreement in all strata except those without a family history of atopy, where there was the best agreement between perceived and actual sensitization to mouse. Agreement between perceived and actual sensitization to cockroach allergy remained slight throughout. For most aeroallergens, subjects with a family history of atopic disease had lower agreement between perceived and actual sensitization compared to those without a family history of atopy. This trend was also similar in subjects with a history of asthma compared to those without a history of asthma.
Table 2. Agreement Between Perceived and Actual Sensitization (sIgE ≥ 0.35 kUA/L) to Specific Aeroallergens, Stratified by Allergic Rhinitis, Asthma, and Family History.
Kappa coefficients are shown.
| Allergen | Allergic Rhinitis | Asthma | Family History of Atopy | |||
|---|---|---|---|---|---|---|
| Yes (n=127) |
No (n=126) |
Yes (n=118) |
No (n=135) |
Yes (n=189) |
No (n=61) |
|
| Any Aeroallergen | 0.26 | 0.11 | 0.46 | 0.26 | 0.32 | 0.24 |
| Cat dander | 0.38 | 0.29 | 0.36 | 0.44 | 0.38 | 0.46 |
| Dust mite - DF | 0.15 | 0.26 | 0.23 | 0.31 | 0.24 | 0.33 |
| Dust mite - DP | 0.25 | 0.25 | 0.30 | 0.33 | 0.29 | 0.39 |
| Grass pollen | 0.18 | 0.12 | 0.20 | 0.36 | 0.28 | 0.27 |
| Tree pollen | 0.03 | 0.07 | 0.19 | 0.32 | 0.23 | 0.26 |
| Mold | 0.15 | 0.09 | 0.24 | 0.24 | 0.22 | 0.35 |
| Weed pollen | 0.04 | 0.16 | 0.20 | 0.21 | 0.17 | 0.37 |
| Dog dander | 0.13 | 0.14 | 0.16 | 0.26 | 0.17 | 0.378 |
| Mouse | 0.15 | 0.19 | 0.15 | 0.06 | 0.04 | 0.70 |
| Cockroach | 0.09 | 0.11 | 0.09 | 0.13 | 0.11 | 0.22 |
DF = D. farinae, DP = D. pteronyssinus
Odds of Actual Sensitization Given Perceived Sensitization to a Specific Aeroallergen
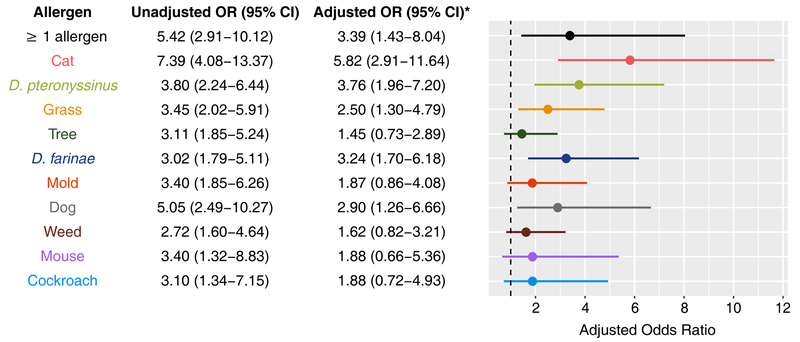
Because multiple factors such as age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history of atopic disease can influence perception of allergy, and may themselves be associated with actual sensitization as well, we built multivariable models adjusted for these potential confounders. The adjusted odds of actual sensitization given perceived sensitization to each specific aeroallergen are shown in Figure 4. The adjusted odds of actual sensitization given perceived sensitization were greatest for cat (aOR 5.82, 95%CI 2.9111.64) and dust (DP aOR 3.76, 95%CI 1.96–7.20 and DF aOR 3.24, 95%CI 1.70–6.18) followed by dog (aOR 2.90, 95%CI 1.26–6.66) and grass pollen (aOR 2.50, 95%CI 1.30–4.79). After covariate adjustment, there were no significant associations between perceived and actual sensitization to tree pollen, mold, weed pollen, mouse, and cockroach.
Figure 4. Odds of Actual Sensitization Given Perceived Sensitization to Individual Aeroallergens.
Multivariable logistic regression models were built to estimate odds ratios for actual sensitization (sIgE ≥ 0.35 kUA/L) given perceived sensitization to individual aeroallergens, adjusted for potential confounders including age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history of atopy. Unadjusted and adjusted ORs are shown, with the forest plot displaying adjusted odds ratios and their 95% confidence intervals for each aeroallergen.
Alternative sIgE thresholds
Recognizing that clinicians and researchers may consider alternative sIgE thresholds when assessing allergen sensitization, we additionally performed secondary analyses using alternate sIgE cut-offs, including sIgE ≥ 0.10 kUA/L (detection limit) and sIgE ≥10 kUA/L (high threshold perhaps indicative of more convincing sensitization). These secondary analyses were possible for indoor but not outdoor allergens because sIgE results for allergen mixes (i.e. tree, grass, and weed pollens and mold) yield a binary output of positive or negative at a detection threshold of 0.35 kUA/L with no numerical output. The prevalence of actual allergen sensitization to an indoor allergen based on sIgE ≥ 0.10 kUA/L in children who perceived and did not perceive sensitization were similar to the results when an sIgE threshold of ≥ 0.35 kUA/L was used (Figure E1). Kappa coefficients (Figures E2) were also similar in the overall study cohort and in the group of subjects who perceived sensitization to ≥1 aeroallergen. The odds of actual sensitization based on sIgE ≥ 0.10 kUA/L given perceived allergy to an indoor allergen also remained similar in magnitude to when the sIgE≥ 0.35 kUA/L threshold was used and was again greatest for cat (aOR 6.42, 95% CI 2.99–13.79), followed by dust (DF aOR 3.84, 95% CI 1.95–7.54; DP aOR 3.60, 95% CI 1.81–7.17) and dog (aOR 3.04, 95% CI 1.20–7.70) (Figure E3).
When a high sIgE threshold of ≥ 10 kUA/L for sensitization was used, the prevalence of actual sensitization in children who perceived and did not perceive sensitization decreased across the board as would be expected (Figure E4). Still, actual sensitization based on this higher threshold remained high for cat, dust mite (DF and DP), and dog (Figure E4). Kappa coefficients for agreement between perceived and actual sensitization decreased for cat dander and dust allergens (DF and DP), but increased for dog dander, mouse, and cockroach (Figure E5). With the higher sIgE ≥ 10 kUA/L threshold, there continued to be greatest agreement between perceived and actual sensitization to cat dander but agreement was then next best for dog dander (Figure E5). The odds of actual sensitization based on sIgE ≥ 10 kUA/L given perceived allergy was highest for dust - DP (aOR 6.10, 95% CI 2.02–18.45) and cat dander (aOR 5.02, 95% CI 2.35–10.73) (Figure E6)
Given the possibility of sIgE levels falling between 0.10 kUA/L (detection limit) and 0.35 kUA/L (conventional threshold), we also considered performing secondary analyses to examine agreement between perceived and actual sensitization based on this indeterminate range of 0.10 kUA/L ≤ sIgE< 0.35 kUA/L. However, few individuals had sIgE values falling in this narrow range to allow for a powered analysis, so this secondary analysis was deferred.
Discussion
Our study is the first to characterize the agreement between perceived and actual sensitization to individual aeroallergens in an urban pediatric population. Multiple prior studies have examined reported allergic airway disease in broad terms (e.g. reported AR or asthma) and its relationship with non-specific sensitization (i.e. any allergen).17–20 Because patients presenting to allergy clinic often have concerns about specific aeroallergen triggers, we were interested in conducting a more precise analysis at the level of individual aeroallergen. We found that agreement between perceived vs. actual sensitization to each individual allergen was fair for most aeroallergens, with the greatest agreement observed for cat dander and dust (DF and DP). Models adjusted for potential confounders (Figure 4) showed 5.8-fold odds of sensitization to cat dander given perceived cat allergy, and over 2-fold odds of sensitization to DF, DP, dog dander, or grass given perceived sensitization to these respective allergens. Children with no perceived allergen sensitization still had high prevalence of actual sensitization and were more likely to be sensitized to indoor rather than outdoor allergens, especially cockroach.
Compared to our findings of fair agreement between perceived vs. actual sensitization to individual aeroallergens among children, prior studies of broadly defined airway allergy and non-specific sensitization reported both consistent and contrasting findings. These prior studies were of populations with varying geographic, age, and asthma backgrounds. Among Finnish adults, self-reported nasal allergy symptoms had poor specificity (31%) for any positive sIgE.17. A US study of 247 adults with asthma found no significant correlation between reported allergy to pollens and SPT size to pollens, and mild correlation for reported pet allergy and SPT size to cat and dog18. In contrast, a separate Finnish study of 290 young adults found that reported AR from pollen or animals had a specificity and sensitivity of 87% for sensitization to any allergen by sIgE or SPT.19 In a large cohort of Swiss children, reported hay fever was found to be associated with sensitization to any allergen (OR 5.7, 95%CI 4.4–7.4).20
Although a few studies have similarly examined the relationship between perceived and actual sensitization to individual allergens, none studied an urban pediatric population as we did here. A study of 73 adults in Minnesota with chronic rhinitis or asthma found that these allergy patients had limited ability to correctly predict which of six allergens to which they would subsequently test positive by allergen SPT (12–56% accuracy).14 Among 258 Swedish adults with reported allergic rhinitis by electronic questionnaire, significant associations were found for reported allergy and positive SPT to cat, Timothy grass, Birch pollen, DP, and mugwort, but not mold; ORs were not provided in this study.12 Similar to our findings, investigators of rural schoolchildren in Saskatchewan, Canada found fair agreement (K=0.34) for reported allergy and sensitization by SPT to cat, but only slight agreement for dust and grass (K=0.03–0.07).15 In contrast, among 95 children with asthma seen at a US military medical center, parental report of allergy was no better than chance at predicting SPT reactivity for their children to three common allergens: cat, dust mite, and grass.13 Our study is distinct from these prior studies by focusing on urban children with comprehensive assessment of perceived and actual sensitization to a wide array of aeroallergens.
Our study is the first to evaluate the relationship between perceived and actual sensitization to cockroach and mouse. Sensitization to these indoor pests is important to consider given the prevalence of cockroach and mouse allergens in urban environments and their role in asthma.21 A study of New York City Dominican and African-American households found that 90.8% of subjects had at least one measurement of major cockroach allergen Bla g 2 protein in kitchen dust during regular evaluations between age 1–5 years.22 Mouse allergen is also frequently detected in most urban homes and schools in New York City.8, 23, 24 Sensitization to mouse and cockroach have each been associated with asthma morbidity in multiple urban cohorts.11, 25–27 Among the children we studied, 8.3% and 10.3% had perceived allergy to mouse and cockroach, respectively, while 17.0% and 36.8% were actually sensitized. The reported prevalence of sensitization to these allergens has been variable in other studies. One study in low-income New York City reported a similar prevalence of mouse and cockroach sensitization (14.3% and 31.0%, respectively) in children aged 5 to 7 years22. Another study based in Baltimore showed slightly higher sensitization prevalence (mouse 52% and cockroach 62%) than the sensitization prevalences observed in our New York City population.26 Given low prevalence of perceived sensitization relative to actual sensitization to cockroach and mouse, our Kappa analyses accordingly showed slight agreement between perceived and actual allergen sensitization to these pests. This is likely due to the fact that mouse and cockroach allergies are under-recognized aeroallergens compared to pollens, dust, and pet danders.
Subjects who perceived sensitization to at least one aeroallergen were younger than those who perceived no sensitization (mean age 12.9 years vs. 14.5 years, P = 0.005. This may seem counter-intuitive, as the incidence of environmental allergen sensitization increases as children age.9, 22 However, because younger children were more likely to have their parents complete their questionnaire, this difference likely reflects parental understanding of aeroallergen sensitization based on their own or their other children’s histories. Indeed, participants with perceived allergen sensitization had a 3.4 greater odds of having a first-degree relative with a history of atopic disease. It is known that atopy is heritable,28–32 although exact mechanisms for this are still not completely understood.29–32 Our results supports that family history could influence awareness and perception of allergen sensitization. We also found that perceived allergen sensitization was more common in children with asthma (59.6%) compared to non-asthmatic children (23.9%) (Fisher’s Exact P value 3.2×10−8), likely reflecting an enhanced familiarity with allergies among asthmatics as well as higher odds of concurrent AR in subjects with asthma (OR 2.98, 95%CI 1.78–4.98).
Although children in this urban study had a high prevalence of aeroallergen sensitization (76.3% in the overall study population and 77.1% in the asthmatic group) compared to the general US population1, 2 previously reported prevalence for inner city populations with asthma were also high, with one study in northeastern schools showing aeroallergen sensitization in 69% of their asthmatic students27 Indeed, half of our cohort endorsed physician diagnosed allergic rhinitis or asthma, supporting that children with allergic rhinitis and/or asthma were more likely to participate, likely due to enhanced interest in the study’s goals as well as our recruitment of subjects from multiple pediatrics clinics, including allergy/immunology clinic. Inclusion of children with and without asthma enabled us to perform stratified analyses that showed differential results by asthma status. For example, in comparison to the overall cohort, children with asthma had the highest agreement between perceived and actual sensitization to ≥1 aeroallergen as well as indoor aeroallergens, perhaps indicative of more accurate self-recognition of allergens (Table 2). Additionally, there was better agreement between perceived and actual sensitization to mouse among those without a family history of atopy vs. those from atopic families. This likely reflects that parents and children in general under-recognize mouse allergy, and its under-recognition leads to less disagreement (i.e. more agreement) in children from nonatopic families who less likely to have actual mouse sensitization.
Our secondary analyses showed that adopting the alternative sIgE threshold of sIgE ≥ 0.10 kUA/L to define sensitization yielded similar prevalence and decreased agreement across the indoor allergens, while use of a high threshold such as 10 kUA/L led to lower prevalence of sensitization (as expected) and changes in agreement for individual allergens. The clinical utility of sIgE levels between 0.10 and 0.35 kUA/L remains an area of inquiry.
We recognize that our study focuses on sensitization, which does not equate to clinically active allergy. sIgE results may be positive in some individuals with no clinical symptoms of allergy and negative in others with highly suggestive symptoms33, 34. We also acknowledge that parental input to the study’s questionnaire on behalf of their children influenced our measure of a child’s perceived sensitization, but parental input into reporting pediatric histories to clinicians reflects real-life care settings, rendering results from our study generalizable to practice. We note that our study’s multivariable models adjusted for family history among other potential confounders yielded major results consistent with our unadjusted models.
The results from this study of perceived vs. actual allergen sensitization in an urban cohort of children highlight important considerations for the practicing allergist when eliciting history from an urban pediatric patient. First, if the patient perceives allergen sensitization to cat dander, dust, dog dander, or grass pollen, then there are 2 to 6-fold odds of actual sensitization based on the tests of agreement and models from this study. Second, even if a child does not perceive sensitization to any allergen per se, actual allergen sensitization is still possible, as we noted 5.4–30.4% prevalence of allergen sensitization in children who denied any perceived allergen sensitization. This is particularly true for indoor allergens. Variable awareness of aeroallergens and varying clinical manifestation of allergy symptoms contribute to differences between perceived vs. actual allergen sensitization. Our findings highlight the importance of combining patient-driven history with diagnostic tests to evaluate patients with aeroallergen concerns.
Supplementary Material
Actual Sensitization to Individual Aeroallergens based on sIgE≥0.10 kUA/L Prevalence of actual sensitization (sIgE ≥0.10 kUA/L) to individual aeroallergens are shown for children with perceived sensitization (darker bars) and children with no perceived sensitization (lighter bars). Fisher’s exact P-values are indicated for comparisons betwen children with and without perceived allergen sensitization. *P value ≤ 0.05, **P value ≤ 0.001.
Figure E2: Agreement Between Perceived and Actual Sensitization (sIgE≥0.10 kUA/L) to Individual Aeroallergens. Kappa coefficients for tests of agreement, along with their 95% confidence intervals, are shown for (A) the overall study cohort (n=253), and (B) subjects with perceived sensitization to ≥1 aeroallergen (n=161)
Figure E3: Odds of Actual Sensitization Given Perceived Sensitization (sIgE≥0.10 kUA/L) to Individual Aeroallergens. Multivariable logistic regression models were built to estimate odds ratios for actual sensitization (sIgE≥0.10 kUA/L) given perceived sensitization to individual aeroallergens, adjusted for potential confounders including age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history of atopy. Unadjusted and adjusted ORs are shown, with the forest plot displaying adjusted odds ratios and their 95% confidence intervals for each aeroallergen.
Figure E4: Actual Sensitization to Individual Aeroallergens based on sIgE≥10 kUA/L Prevalence of actual sensitization (sIgE ≥10 kUA/L) to individual aeroallergens are shown for children with perceived sensitization (darker bars) and children with no perceived sensitization (lighter bars). Fisher’fs exact P-values are indicated for comparisons betwen children with and without perceived allergen sensitization. *P value ≤ 0.05, **P value ≤0.001.
Figure E5: Agreement Between Perceived and Actual Sensitization (sIgE≥10 kUA/L) to Individual Aeroallergens. Kappa coefficients for tests of agreement, along with their 95% confidence intervals, are shown for (A) the overall study cohort (n=253), and (B) subjects with perceived sensitization to ≤1 aeroallergen (n=161)
Figure E6: Odds of Actual Sensitization Given Perceived Sensitization (sIgE≥10 kUA/L) to Individual Aeroallergens. Multivariable logistic regression models were built to estimate odds ratios for actual sensitization (sIgE≥10 kUA/L) given perceived sensitization to individual aeroallergens, adjusted for potential confounders including age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history of atopy. Unadjusted and adjusted ORs are shown, with the forest plot displaying adjusted odds ratios and their 95% confidence intervals for each aeroallergen.
Highlights box:
1. What is already known about this topic?
Allergy management depends upon appropriate recognition of allergens. Prior studies have examined the relationship between allergic rhinitis, asthma, and sensitization, but few have specifically examined the agreement between perceived and actual sensitization to individual allergens.
2. What does this article add to our knowledge?
Among urban children, agreement between perceived and actual sensitization for most allergens is fair. Perceived sensitization to cat, dust, dog, or grass was associated with 2 to 6-fold odds of corresponding sensitization.
3. How does this study impact current management guidelines?
Children with perceived sensitization to cat, dust, dog, or grass have high odds of actual sensitization to these allergens. In children with no perceived sensitization, sensitization is still common, particularly for indoor allergens including cockroach.
Acknowledgments
Funding/Support: This study was supported by the National Institutes of Health (NIH AI118833)
Abbreviations:
- aOR
adjusted odds ratio
- AR
allergic rhinitis
- DF
Dermatophagoides farinae
- DP
Dermatophagoides pteronyssinus
- IgE
immunoglobulin E
- K
Kappa
- sIgE
serum-specific immunoglobulin E
- SPT
skin prick test
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
The authors have no conflict of interests to declare.
References
- 1.Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, et al. The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol 2008; 122:S1–84. [DOI] [PubMed] [Google Scholar]
- 2.Adkinson NFB, Bruce S, Burks AW, Busse WW, Holgate ST, Lemanske J, Robert F, O’Hehir RE. Middleton’s Allergy. 8th ed: Saunders; 2014. [Google Scholar]
- 3.Zahran HS, Bailey CM, Damon SA, Garbe PL, Breysse PN. Vital Signs: Asthma in Children - United States, 2001–2016. MMWR Morb Mortal Wkly Rep 2018; 67:149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Janssens T, Ritz T. Perceived triggers of asthma: key to symptom perception and management. Clin Exp Allergy 2013; 43:1000–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silva CM, Barros L. Asthma knowledge, subjective assessment of severity and symptom perception in parents of children with asthma. J Asthma 2013; 50:1002–9. [DOI] [PubMed] [Google Scholar]
- 6.Su N, Lin J, Chen P, Li J, Wu C, Yin K, et al. Evaluation of asthma control and patient’s perception of asthma: findings and analysis of a nationwide questionnaire-based survey in China. J Asthma 2013; 50:861–70. [DOI] [PubMed] [Google Scholar]
- 7.Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med 2014; 24:14009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olmedo O, Goldstein IF, Acosta L, Divjan A, Rundle AG, Chew GL, et al. Neighborhood differences in exposure and sensitization to cockroach, mouse, dust mite, cat, and dog allergens in New York City. J Allergy Clin Immunol 2011; 128:284–92 e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stoltz DJ, Jackson DJ, Evans MD, Gangnon RE, Tisler CJ, Gern JE, et al. Specific patterns of allergic sensitization in early childhood and asthma & rhinitis risk. Clin Exp Allergy 2013; 43:233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Codispoti CD, LeMasters GK, Levin L, Reponen T, Ryan PH, Biagini Myers JM, et al. Traffic pollution is associated with early childhood aeroallergen sensitization. Ann Allergy Asthma Immunol 2015; 114:126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fishbein AB, Lee TA, Cai M, Oh SS, Eng C, Hu D, et al. Sensitization to mouse and cockroach allergens and asthma morbidity in urban minority youth: Genes-environments and Admixture in Latino American (GALA-II) and Study of African-Americans, Asthma, Genes, and Environments (SAGE-II). Ann Allergy Asthma Immunol 2016; 117:43–9.e1. [DOI] [PubMed] [Google Scholar]
- 12.Lindberg S, Malm L. Comparison of allergic rhinitis and vasomotor rhinitis patients on the basis of a computer questionnaire. Allergy 1993; 48:602–7. [DOI] [PubMed] [Google Scholar]
- 13.Carter ER, Pulos E, Delaney J, Matheson EJ, Moffitt DR. Allergy history does not predict skin test reactivity in asthmatic children. J Asthma 2000; 37:685–90. [DOI] [PubMed] [Google Scholar]
- 14.Li JT, Andrist D, Bamlet WR, Wolter TD. Accuracy of patient prediction of allergy skin test results. Ann Allergy Asthma Immunol 2000; 85:382–4. [DOI] [PubMed] [Google Scholar]
- 15.Chu L, Rennie D, Cockcroft D, Pahwa P, Dosman J, Hagel L, et al. Agreement between questionnaire report of allergy-related outcomes in school-age children and objective measures of atopy: the Saskatchewan rural health study. Clin Exp Allergy 2015; 45:1337–45. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33:159–74. [PubMed] [Google Scholar]
- 17.Kauppi P, Laitinen LA, Laitinen H, Kere J, Laitinen T. Verification of self-reported asthma and allergy in subjects and their family members volunteering for gene mapping studies. Respir Med 1998; 92:1281–8. [DOI] [PubMed] [Google Scholar]
- 18.Ritz T, Steptoe A, Bobb C, Harris AH, Edwards M. The asthma trigger inventory: validation of a questionnaire for perceived triggers of asthma. Psychosom Med 2006; 68:956–65. [DOI] [PubMed] [Google Scholar]
- 19.Kilpelainen M, Terho EO, Helenius H, Koskenvuo M. Validation of a new questionnaire on asthma, allergic rhinitis, and conjunctivitis in young adults. Allergy 2001; 56:377–84. [DOI] [PubMed] [Google Scholar]
- 20.Braun-Fahrländer C, Wüthrich B, Gassner M, Grize L, Sennhauser FH, Varonier HS, et al. Validation of a rhinitis symptom questionnaire (ISAAC core questions) in a population of Swiss school children visiting the school health services. SCARPOL-team. Swiss Study on Childhood Allergy and Respiratory Symptom with respect to Air Pollution and Climate. International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol 1997; 8:75–82. [DOI] [PubMed] [Google Scholar]
- 21.Milligan KL, Matsui E, Sharma H. Asthma in Urban Children: Epidemiology, Environmental Risk Factors, and the Public Health Domain. Curr Allergy Asthma Rep 2016; 16:33. [DOI] [PubMed] [Google Scholar]
- 22.Perzanowski MS, Chew GL, Divjan A, Jung KH, Ridder R, Tang D, et al. Early-life cockroach allergen and polycyclic aromatic hydrocarbon exposures predict cockroach sensitization among inner-city children. J Allergy Clin Immunol 2013; 131:886–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chew GL, Perzanowski MS, Miller RL, Correa JC, Hoepner LA, Jusino CM, et al. Distribution and determinants of mouse allergen exposure in low-income New York City apartments. Environ Health Perspect 2003; 111:1348–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chew GL, Correa JC, Perzanowski MS. Mouse and cockroach allergens in the dust and air in northeastern United States inner-city public high schools. Indoor Air 2005; 15:228–34. [DOI] [PubMed] [Google Scholar]
- 25.Grant T, Aloe C, Perzanowski M, Phipatanakul W, Bollinger ME, Miller R, et al. Mouse Sensitization and Exposure Are Associated with Asthma Severity in Urban Children. J Allergy Clin Immunol Pract 2017; 5:1008–14.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Torjusen EN, Diette GB, Breysse PN, Curtin-Brosnan J, Aloe C, Matsui EC. Doseresponse relationships between mouse allergen exposure and asthma morbidity among urban children and adolescents. Indoor Air 2013; 23:268–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheehan WJ, Permaul P, Petty CR, Coull BA, Baxi SN, Gaffin JM, et al. Association Between Allergen Exposure in Inner-City Schools and Asthma Morbidity Among Students. JAMA Pediatr 2017; 171:31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zimmerman B, Feanny S, Reisman J, Hak H, Rashed N, McLaughlin FJ, et al. Allergy in asthma. I. The dose relationship of allergy to severity of childhood asthma. J Allergy Clin Immunol 1988; 81:63–70. [DOI] [PubMed] [Google Scholar]
- 29.Johnson CC, Ownby DR, Peterson EL. Parental history of atopic disease and concentration of cord blood IgE. Clin Exp Allergy 1996; 26:624–9. [PubMed] [Google Scholar]
- 30.Arshad SH, Karmaus W, Raza A, Kurukulaaratchy RJ, Matthews SM, Holloway JW, et al. The effect of parental allergy on childhood allergic diseases depends on the sex of the child. J Allergy Clin Immunol 2012; 130:427–34.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Westman M, Kull I, Lind T, Melén E, Stjärne P, Toskala E, et al. The link between parental allergy and offspring allergic and nonallergic rhinitis. Allergy 2013; 68:1571–8. [DOI] [PubMed] [Google Scholar]
- 32.Cook-Mills JM. Maternal influences over offspring allergic responses. Curr Allergy Asthma Rep 2015; 15:501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Migueres M, Dávila I, Frati F, Azpeitia A, Jeanpetit Y, Lhéritier-Barrand M, et al. Types of sensitization to aeroallergens: definitions, prevalences and impact on the diagnosis and treatment of allergic respiratory disease. Clin Transl Allergy 2014; 4:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burte E, Bousquet J, Siroux V, Just J, Jacquemin B, Nadif R. The sensitization pattern differs according to rhinitis and asthma multimorbidity in adults: the EGEA study. Clin Exp Allergy 2017; 47:520–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Actual Sensitization to Individual Aeroallergens based on sIgE≥0.10 kUA/L Prevalence of actual sensitization (sIgE ≥0.10 kUA/L) to individual aeroallergens are shown for children with perceived sensitization (darker bars) and children with no perceived sensitization (lighter bars). Fisher’s exact P-values are indicated for comparisons betwen children with and without perceived allergen sensitization. *P value ≤ 0.05, **P value ≤ 0.001.
Figure E2: Agreement Between Perceived and Actual Sensitization (sIgE≥0.10 kUA/L) to Individual Aeroallergens. Kappa coefficients for tests of agreement, along with their 95% confidence intervals, are shown for (A) the overall study cohort (n=253), and (B) subjects with perceived sensitization to ≥1 aeroallergen (n=161)
Figure E3: Odds of Actual Sensitization Given Perceived Sensitization (sIgE≥0.10 kUA/L) to Individual Aeroallergens. Multivariable logistic regression models were built to estimate odds ratios for actual sensitization (sIgE≥0.10 kUA/L) given perceived sensitization to individual aeroallergens, adjusted for potential confounders including age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history of atopy. Unadjusted and adjusted ORs are shown, with the forest plot displaying adjusted odds ratios and their 95% confidence intervals for each aeroallergen.
Figure E4: Actual Sensitization to Individual Aeroallergens based on sIgE≥10 kUA/L Prevalence of actual sensitization (sIgE ≥10 kUA/L) to individual aeroallergens are shown for children with perceived sensitization (darker bars) and children with no perceived sensitization (lighter bars). Fisher’fs exact P-values are indicated for comparisons betwen children with and without perceived allergen sensitization. *P value ≤ 0.05, **P value ≤0.001.
Figure E5: Agreement Between Perceived and Actual Sensitization (sIgE≥10 kUA/L) to Individual Aeroallergens. Kappa coefficients for tests of agreement, along with their 95% confidence intervals, are shown for (A) the overall study cohort (n=253), and (B) subjects with perceived sensitization to ≤1 aeroallergen (n=161)
Figure E6: Odds of Actual Sensitization Given Perceived Sensitization (sIgE≥10 kUA/L) to Individual Aeroallergens. Multivariable logistic regression models were built to estimate odds ratios for actual sensitization (sIgE≥10 kUA/L) given perceived sensitization to individual aeroallergens, adjusted for potential confounders including age, sex, race, season of enrollment, allergic rhinitis, asthma, and family history of atopy. Unadjusted and adjusted ORs are shown, with the forest plot displaying adjusted odds ratios and their 95% confidence intervals for each aeroallergen.