Abstract
Background:
The presence of midwives in a health system may affect perinatal outcomes but has been inadequately described in United States settings. Our objective was to compare labor processes and outcomes for low-risk nulliparous women birthing in United States medical centers with interprofessional care (midwives and physicians) versus noninterprofessional care (physicians only).
Methods:
We conducted a retrospective cohort study using Consortium on Safe Labor data from low-risk nulliparous women who birthed in interprofessional (n = 7393) or noninterprofessional centers (n = 6982). Unadjusted, adjusted (age, race, health insurance type), propensity-adjusted, and propensity-matched logistic regression models were used to compare outcomes.
Results:
There was concordance across logistic regression models, the most restrictive and conservative of which were propensity-matched models. With this approach, women at interprofessional medical centers, compared with women at noninterprofessional centers, were 74% less likely to undergo labor induction (risk ratio [RR] 0.26; 95% CI 0.24–0.29) and 75% less likely to have oxytocin augmentation (RR 0.25; 95% CI 0.22–0.29). The cesarean birth rate was 12% lower at interprofessional centers (RR 0.88; 95% CI 0.79–0.98). Adverse neonatal outcomes occurred in only 0.3% of births and were thus too rare to be modeled.
Conclusions:
The care processes and birth outcomes at interprofessional and noninterprofessional medical centers differed significantly. Nulliparous women receiving care at interprofessional centers were less likely to experience induction, oxytocin augmentation, and cesarean than women at noninterprofessional centers. Labor care and birth outcome differences between interprofessional and noninterprofessional centers may be the result of the presence of midwives and interprofessional collaboration, organizational culture, or both.
Keywords: cesarean, culture, induced labor, midwifery, nulliparous, obstetrics, oxytocin, parturition
1. INTRODUCTION
In 2016, 98.4% of births in the United States occurred in hospitals.1 Physicians attended 90.9% of hospital births, whereas midwives attended 8.6%.1 The proportion of hospital births attended by midwives is at an all-time high in the United States, and rates have steadily increased since 1975 when midwives attended <1% of hospital births.2 Certified nurse-midwives (CNMs) provided care for 98.5% of all in-hospital, midwife-attended births.1
Midwife-led care (ie, midwifery care from the first appointment to the postpartum period) is associated with favorable birth outcomes over other models of care.3 These favorable outcomes may be due to the midwifery philosophy of care that includes watchful waiting and nonintervention in normal processes, appropriate use of interventions and technology for current or potential health problems, and interdisciplinary collaboration as needed to provide optimal health care.4 These philosophical tenets may also shape maternal care cultures wherein midwives are team members. It is important to evaluate whether differences in outcomes exist between hospitals with different professional models because increasing evidence suggests that rates of obstetric interventions vary widely across hospitals and are not explained by patient risk factors.5,6
Attanasio and Kozhimannil7 recently reported that New York hospitals with more midwife-attended births had fewer cesarean births among low-risk women than hospitals without midwives. This difference may have been a result of direct care provided by midwives in these hospitals or of institutional culture and practice pattern differences in hospitals with midwives that influence how maternity care teams (eg, clinicians, nurses, and support personnel) care for childbearing women. Interprofessional hospitals provide greater opportunities for midwife-obstetrician collaboration; therefore, Attanasio and Kozhimannil’s7 finding that New York hospitals with midwives had fewer cesarean births gives credence to the joint statement by the American College of Obstetricians and Gynecologists and the American College of Nurse-Midwives that the highest quality care for women occurs when physicians and midwives work in health systems fostering collaboration.8 Collaborative practice and team-based care have been shown to improve the quality, efficiency, and value of health care.9 If interprofessional hospitals across the United States have better outcomes than noninterprofessional hospitals, administrators might consider adding midwives to their practitioner mix to improve care for low-risk women and their children.
Nulliparous women with a term, single, vertex fetus have been identified by leading maternal care organizations10–14 as a crucial population to consider when strategizing to improve obstetrical care quality and decrease cesarean rates. The major driver of the overall cesarean rate in the United States is the 25.7% cesarean rate among these low-risk first-time mothers.1 Improving care for this population is key to reducing total cesareans because approximately 90% of first-time mothers who delivered by cesarean will have repeat cesareans in subsequent pregnancies.1,14 Since the course of a woman’s first birth largely dictates the course and management of her future childbearing, optimizing care with the initial birth will indirectly improve subsequent obstetrical care while decreasing cost. Our study objective was to compare labor care processes and birth outcomes between healthy, low-risk nulliparous women birthing in United States medical centers with interprofessional versus noninterprofessional care.
2. METHODS
To obtain a large and diverse sample, we used data from the Consortium on Safe Labor (CSL), a multisite observational cohort study conducted between 2002 and 2008 in 12 clinical centers (19 hospitals) across the United States.15 The database includes detailed data from women’s health records including demographics, medical history, reproductive and prenatal history, labor interventions, birth outcomes, postpartum and discharge information, and newborn information. Characteristics of the participating clinical centers are also in the database, including levels for obstetrical and neonatal care (eg, secondary or tertiary) and whether there was 24hour coverage by obstetricians, maternal-fetal medicine specialists, anesthesia personnel, and neonatologists at the time of data collection.
Two variables in the CSL database specifically indicated whether women labored and birthed at an interprofessional medical center (where midwives and physicians practice) or noninterprofessional medical center (where only physicians practice). We consulted Katherine Laughon Grantz, MD, MS, Principal Investigator of the CSL, and ascertained that there was no variable in the data set that reliably indicated whether labor care for a particular woman at an interprofessional medical center was provided by a midwife or physician. Therefore, we organized comparisons between institutions with or without midwives within the broader maternity care team rather than focusing on which team member attended particular births. The attendant variable was, however, used to provide conservative estimates of the proportion of births at interprofessional centers with midwifery care involvement. Vanderbilt University Institutional Review Board approval was obtained for secondary analyses of CSL data, and all authors had CSL data use agreements with The Eunice Kennedy Shriver National Institute of Child Health and Human Development.
We limited our sample to healthy, nulliparous women who gave birth to a single, cephalic-presenting fetus at or after 37.0 weeks’ gestation. These low-risk women are candidates for either midwifery or obstetrical care at interprofessional medical centers. Limiting analyses to only healthy women eliminated the potential confounding influence of different prevalence and severity of health conditions across centers.
Figure 1 depicts the sample selection process for this study. Women with a previous birth, preterm birth, multiple gestation, fetus in a noncephalic or unknown presentation, previous uterine scar (eg, myomectomy), or fetus with a chromosomal or congenital anomaly were excluded. We also excluded women with preexisting and antepartum health conditions including diabetes, hypertension, heart disease, renal disease, gastrointestinal disease, depression, seizure disorders, thyroid disease, asthma, anemia, or HIV/herpes. Women without documented age, race, or health insurance type were excluded because those variables were considered critical potential confounders of the analyses since maternal age,1,16–19 race,1,20 and health insurance type21 are associated with variations in cesarean rates and certain labor processes. Finally, we excluded medical centers where the presence or absence of midwife practitioners could not be explicitly determined. Specifically, we excluded two clinical centers that gave mixed responses about whether midwives attended births or provide care and four clinical centers that indicated midwives attended births but did not identify midwives as practitioners in the data set.
FIGURE 1.
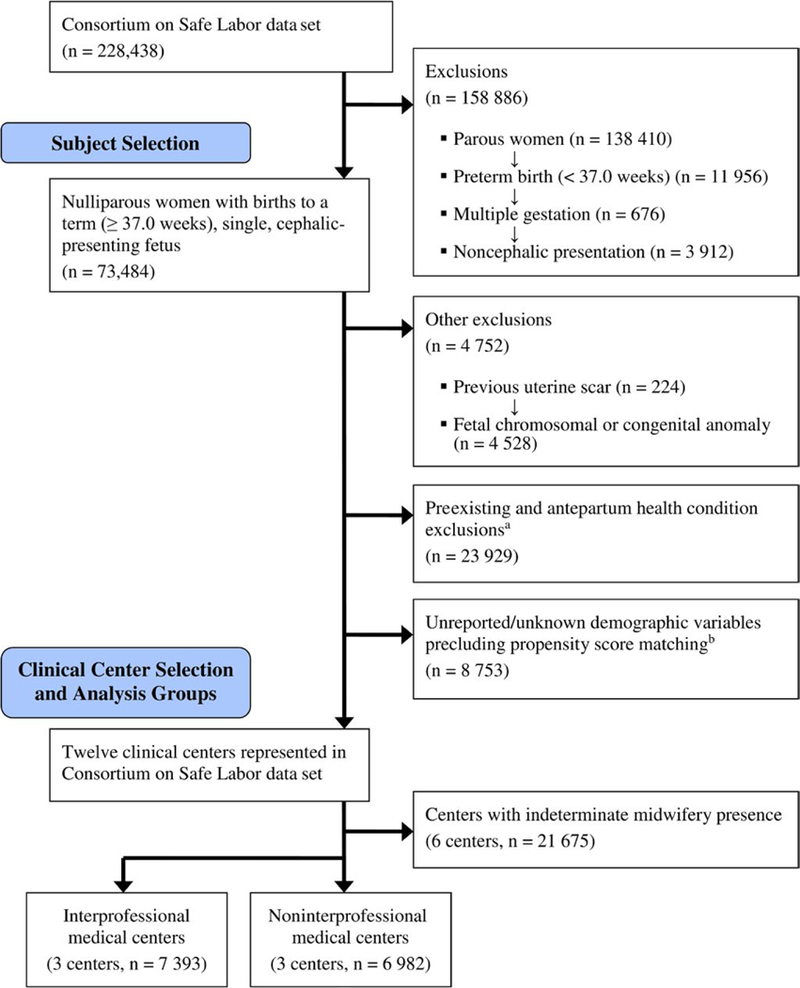
Diagram of patient selection. aConditions excluded were diabetes, hypertension, heart disease, renal disease, gastrointestinal disease, depression, seizure disorders, thyroid disease, asthma, anemia, HIV/herpes. bMaternal age, race, and health insurance type
The main labor care processes and birth outcome measures used for our analyses included gestational age of newborn at birth, type of labor onset (ie, spontaneous onset and trial of labor, induction of labor, cesarean without a trial of labor), rupture of membrane type (eg, spontaneous or amniotomy), oxytocin augmentation use, mode of birth, maternal postpartum blood transfusion, maternal postpartum intensive care unit admission, neonatal intensive care unit admission, and adverse neonatal outcomes.
A composite of adverse neonatal outcomes was used because of the large sample sizes needed to separately study each outcome. Adverse outcomes assessed included stillbirth or neonatal asphyxia, seizure, intracranial hemorrhage, paraventricular/intraventricular hemorrhage, necrotizing enterocolitis, hypoxic-ischemic encephalopathy, and/or death. Even in aggregate, adverse neonatal outcomes occurred too rarely in the sample to be modeled.
Statistical analyses were conducted using IBM SPSS Statistics 24 (IBM Corporation, Armonk, NY, USA) and Stata/ SE 14.0 (StataCorp LP, College Station, TX, USA). A critical alpha of 0.05 was used for determining statistical significance. Frequencies and percentages were used to describe the categorical data used in this study; median and associated percentiles were used for the continuous data. Comparisons between interprofessional and noninterprofessional centers were conducted using Mann-Whitney U (continuous data) and likelihood ratio (categorical) tests. The propensity (or predicted probability) of a woman giving birth in a medical center with midwifery presence was generated using her respective values for the critical confounding demographic characteristics (age, race, and health insurance type).22,23 The propensity value or score for each woman ranged from 0.000 to 1.000 with values closer to 0 suggesting very little probability of giving birth in such a center given the three demographic characteristics; values closer to 1.00 indicated a very high probability of giving birth in an interprofessional medical center.
Depending on the number of categories defining the study outcome, the effects of interprofessional presence (ie, midwives and physicians) on each of the outcomes were generated and replicated using either binomial (two categories) or multinomial (two categories) logistic regression models. The first three models included the entire sample of women.
Unadjusted logistic regression: These models included only the effect of interprofessional presence.
Adjusted models using observed covariates: These models estimated the effect of midwifery presence after adjusting for the observed values for maternal age, race, and health insurance type.
Adjusted models using the propensity scores: Rather than including the observed values for the demographic confounders, the effect of interprofessional presence was estimated after adjusting for the propensity (probability) values generated from those variables.
Finally, the most restrictive and conservative regression models estimated the effect of interprofessional presence within a sample of women matched in a pairwise approach by their propensity values. With this approach, we required a propensity score within 0.001 for “paired” cases from the midwifery and nonmidwifery groups. In other words, every woman included in this analysis that gave birth at an interprofessional medical center was matched with a woman who gave birth at a noninterprofessional center only when their propensity scores were within 0.001 of each other. This stringent approach actually resulted in matched pairs of cases on age, race, and insurance status.
3. RESULTS
The final sample included 14 375 healthy, nulliparous women who gave birth to a single, cephalic-presenting fetus at or after 37.0 weeks’ gestation. These women birthed at one of three interprofessional medical centers (n = 7393) or at one of three noninterprofessional centers (n = 6982). All six centers were teaching facilities and offered tertiary-level obstetrical care. Five centers had level III neonatal intensive care units (NICUs), and one interprofessional center had a level II NICU. There was 24-hour coverage by obstetricians, maternal-fetal medicine specialists, anesthesia personnel, and neonatologists at all centers. There was a mix of moderate-to-high annual birth volumes in both the interprofessional centers (center 1, 20 329 births; center 2, 20 779 births; center 3, 7749 births) and noninterprofessional centers (center 1, 6420 births; center 2, 23 141 births; center 3, 18 392 births) during 2006. Among the interprofessional medical centers, midwives attended approximately 18% of births to low-risk nulliparous women in the current study (center 1, 21.1%; center 2, 15.3%, center 3, 13.4%). Physicians attended all births at noninterprofessional medical centers.
Characteristics and birth outcomes for nulliparous women birthing in interprofessional and noninterprofessional medical centers before propensity score matching (n = 14 375) are presented in Table 1. Women birthing at interprofessional centers were younger and more likely to be white and/or have private insurance. Birth interventions such as induction of labor, amniotomy, oxytocin augmentation, and cesarean birth were used less often at interprofessional centers (P < 0.001 for each). The duration of in-hospital time from admission to birth was 2.7 hours shorter for women birthing at interprofessional medical centers, and postpartum blood transfusions were administered less often at these centers. No differences were found in adverse neonatal outcomes between groups.
TABLE 1.
Characteristics and birth outcomes of nulliparous women from the Consortium on Safe Labor with a single, cephalic-presenting fetus at term gestation before propensity score matching, United States, 2002–2008 (N = 14 375)
| Interprofessional centers (N = 7393), n (%) or median [5th, 95th percentile] | Noninterprofessional centers (N = 6982), n (%) or median [5th, 95th percentile] | P | |
|---|---|---|---|
| Demographics | |||
| Maternal age (y) | 24 [17, 35] | 25 [17, 37] | <0.001 |
| Race | |||
| White, non-Hispanic | 4921 (66.6) | 2649 (37.9) | <0.001 |
| Black, non-Hispanic | 673 (9.1) | 2223 (31.8) | |
| Hispanic | 914 (12.4) | 1453 (20.8) | |
| Asian/Pacific Islander | 695 (9.4) | 593 (8.5) | |
| Other | 190 (2.6) | 64 (0.9) | |
| Health insurance | |||
| Private | 6115 (82.7) | 4118 (59.0) | <0.001 |
| Public | 1235 (16.7) | 2553 (36.6) | |
| Self-pay/other | 43 (0.6) | 311 (4.5) | |
| Birth admission information | |||
| Gestational age | |||
| Early term (37 0/7–38 6/7) | 1732 (23.4) | 2265 (32.4) | <0.001 |
| Full term (39 0/7–40 6/7) | 4557 (61.6) | 4121 (59.0) | |
| Late term (41 0/7–41 6/7) | 1014 (13.7) | 556 (8.0) | |
| Postterm (≥ 42 0/7) | 90 (1.2) | 40 (0.6) | |
| Body mass index (kg/m2)a | 28.8 [23.0, 40.6] | 28.5 [22.7, 39.8] | <0.001 |
| Cervical dilatation (cm) | 3.5 [0.5, 9.0] | 2.5 [0.0, 6.0] | <0.001 |
| Cervical effacement (%) | 90 [40, 100] | 80 [20, 100] | <0.001 |
| Fetal station | −2 [−3, 0] | −2 [−4, 0] | <0.001 |
| Birth process and outcome information | |||
| Type of labor | |||
| Spontaneous onset and trial of labor | 5389 (72.9) | 2884 (41.3) | <0.001 |
| Induction and trial of labor | 1852 (25.1) | 3836 (54.9) | |
| Cesarean without trial of labor | 152 (2.1) | 262 (3.8) | |
| Amniotomy | 3988 (53.9) | 4381 (62.7) | <0.001 |
| Oxytocin augmentationb | 1688 (31.3) | 1912 (66.3) | <0.001 |
| Mode of birth | |||
| Vaginal—spontaneous | 5259 (71.1) | 4541 (65.0) | <0.001 |
| Vaginal—assisted | 765 (10.3) | 667 (9.6) | |
| Cesarean | 1369 (18.5) | 1774 (25.4) | |
| Indication for cesareans without trial of labor | |||
| Elective | 14 (9.2) | 62 (23.7) | <0.01 |
| Suspected macrosomia | 39 (25.7) | 64 (24.4) | |
| Nonreassuring fetal testing | 42 (27.6) | 45 (17.2) | |
| Placenta previa or abruption | 9 (5.9) | 9 (3.4) | |
| Otherc | 48 (31.6) | 82 (31.3) | |
| Indication for cesarean after trial of labor | |||
| Dystocia | 667 (54.8) | 939 (62.1) | <0.001 |
| Abnormal or indeterminate fetal heart rate tracing | 325 (26.7) | 501 (33.1) | |
| Dystocia + abnormal or indeterminate fetal heart rate tracing (combined) | 121 (9.9) | 15 (1.0) | |
| Otherd | 104 (8.5) | 57 (3.8) | |
| Admission to birth duration (h)e | 9.6 [2.1, 28.0] | 12.3 [3.6, 26.9] | <0.001 |
| Maternal postpartum blood transfusion | 6 (0.1) | 38 (0.5) | <0.001 |
| Maternal postpartum intensive care unit admission | 0 | 2 (0.0) | NS |
| Maternal mortality | 0 | 0 | NS |
| Neonatal information | |||
| Weight (infant) (kg) | 3.32 [2.66, 4.07] | 3.29 [2.64, 4.03] | <0.001 |
| Composite adverse neonatal outcomef | 22 (0.3) | 20 (0.3) | NS |
| Neonatal intensive care unit admission | 342 (4.6) | 323 (4.6) | NS |
Percentages may not add to 100% due to rounding. Denominator for some variables is different from column total due to missing/unknown values. Mann-Whitney U tests performed for continuous-level data comparisons due to non-normal distributions (Kolmogorov-Smirnov test for normality <0.001). Likelihood ratio tests were performed for categorical-level data comparisons. NS, not statistically significant.
Values not reported for 24.5% (3516) women.
Limited to women with spontaneous labor onset and a trial of labor.
Documented in CSL data set primarily as “other.”
Documented in CSL data set primarily as “other” (n = 121) or suspected fetal macrosomia (n = 18) although a smaller proportion of these cesareans were also performed for chorioamnionitis, failed operative vaginal delivery, placental abruption, or placenta/vasa previa (n = 22).
Limited to women with a trial of labor.
Defined as stillbirth or neonatal asphyxia, seizure, intracranial hemorrhage, paraventricular/intraventricular hemorrhage, necrotizing enterocolitis, hypoxic-ischemic encephalopathy, or death.
Pairwise, propensity score matching across center types resulted in a sample of 7042 women (see Table 2). Among these women, birth interventions such as induction of labor, amniotomy, and oxytocin augmentation were used significantly less often at interprofessional medical centers (P < 0.001 for each) although mode of birth did not differ between center types. The duration of time from admission to the medical center to birth was, on average, 2 hours shorter for women birthing at interprofessional medical centers (P < 0.001). Postpartum blood transfusions were administered less often at interprofessional centers (P < 0.01). Neonatal intensive care unit admissions occurred more often in interprofessional centers (5.5% vs 4.3%, respectively), but no differences were found in adverse neonatal outcomes between center type (0.3% each).
TABLE 2.
Characteristics and birth outcomes of nulliparous women from the Consortium on Safe Labor with a single, cephalic-presenting fetus at term gestation after propensity score matching, United States, 2002–2008 (N = 7042)
| Interprofessional centers (N = 3521), n (%) or median [5th, 95th percentile] |
Noninterprofessional centers (N = 3521), n (%) or median [5th, 95th percentile] | P | |
|---|---|---|---|
| Demographics | |||
| Maternal age (y) | 27 [17, 35] | 27 [17, 35] | NS |
| Race | |||
| White, non-Hispanic | 1937 (55.0) | 1937 (55.0) | NS |
| Black, non-Hispanic | 660 (18.7) | 660 (18.7) | |
| Hispanic | 606 (17.2) | 606 (17.2) | |
| Asian/Pacific Islander | 306 (8.7) | 306 (8.7) | |
| Other | 12 (0.3) | 12 (0.3) | |
| Health insurance | |||
| Private | 2650 (75.3) | 2650 (75.3) | NS |
| Public | 848 (24.1) | 848 (24.1) | |
| Self-pay/other | 23 (0.7) | 23 (0.7) | |
| Birth admission information | |||
| Gestational age | |||
| Early term (37 0/7–38 6/7) | 861 (24.5) | 1187 (33.7) | <0.001 |
| Full term (39 0/7–40 6/7) | 2143 (60.9) | 2062 (58.6) | |
| Late term (41 0/7–41 6/7) | 479 (13.6) | 262 (7.4) | |
| Postterm (≥ 42 0/7) | 38 (1.1) | 10 (0.3) | |
| Body mass index (kg/m2)a | 29.7 [23.5, 41.4] | 28.3 [22.8, 39.1] | <0.001 |
| Cervical dilatation (cm) | 3.5 [0.5, 9.0] | 2.5 [0.0, 6.5] | <0.001 |
| Cervical effacement (%) | 90 [40, 100] | 80 [20, 100] | <0.001 |
| Fetal station | −2 [−3, 0] | −2 [−4, 0] | <0.001 |
| Birth process and outcome information | |||
| Type of labor | |||
| Spontaneous onset and trial of labor | 2515 (71.4) | 1396 (39.6) | <0.001 |
| Induction and trial of labor | 940 (26.7) | 2004 (56.9) | |
| Cesarean without trial of labor | 66 (1.9) | 121 (3.4) | |
| Amniotomy | 1835 (52.1) | 2252 (64.0) | <0.001 |
| Oxytocin augmentationb | 780 (31.0) | 900 (64.5) | <0.001 |
| Mode of birth | |||
| Vaginal—spontaneous | 2451 (69.6) | 2364 (67.1) | NS |
| Vaginal—assisted | 291 (8.3) | 302 (8.6) | |
| Cesarean | 779 (22.1) | 855 (24.3) | |
| Indication for cesareans without trial of labor | |||
| Elective | 4 (6.1) | 28 (23.1) | <0.05 |
| Suspected macrosomia | 21 (31.8) | 34 (28.1) | |
| Nonreassuring fetal testing | 16 (24.2) | 21 (17.4) | |
| Placenta previa or abruption | 4 (6.1) | 2 (1.7) | |
| Otherc | 21 (31.8) | 36 (29.8) | |
| Indication for cesarean after trial of labor | |||
| Dystocia | 374 (52.5) | 464 (63.2) | <0.001 |
| Abnormal or indeterminate fetal heart rate tracing | 177 (24.8) | 232 (31.6) | |
| Dystocia +abnormal or indeterminate fetal heart rate tracing (combined) | 90 (12.6) | 6 (0.8) | |
| Otherd | 72 (10.1) | 32 (4.4) | <0.001 |
| Admission to birth duration (h)e | 10.4 [2.5, 29.3] | 12.4 [3.5, 26.1] | <0.001 |
| Maternal postpartum blood transfusion | 2 (0.1) | 12 (0.3) | <0.01 |
| Maternal postpartum intensive care unit admission | 0 | 1 (0.0) | NS |
| Maternal mortality | 0 | 0 | NS |
| Neonatal information | |||
| Weight (infant) (kg) | 3.34 [2.65, 4.10] | 3.31 [2.65, 4.05] | <0.05 |
| Composite adverse neonatal outcomef | 15 (0.4) | 8 (0.2) | NS |
| Neonatal intensive care unit admission | 192 (5.5) | 151 (4.3) | <0.05 |
Percentages may not add to 100% due to rounding. Denominator for some variables is different from column total due to missing/unknown values. Mann-Whitney U tests performed for continuous-level data comparisons due to non-normal distributions (Kolmogorov-Smirnov test for normality <0.001). Likelihood ratio tests were performed for categorical-level data comparisons. NS, not statistically significant.
Values not reported for 21.5% (1516) women.
Limited to women with spontaneous labor onset and a trial of labor.
Documented in CSL data set primarily as “other.”
Documented in CSL data set primarily as “other” (n = 75) or suspected fetal macrosomia (n = 12) although a smaller proportion of these cesareans were also performed for chorioamnionitis, failed operative vaginal delivery, placental abruption, or placenta/vasa previa (n = 17).
Limited to women with a trial of labor.
Defined as stillbirth or neonatal asphyxia, seizure, intracranial hemorrhage, paraventricular/intraventricular hemorrhage, necrotizing enterocolitis, hypoxic-ischemic encephalopathy, or death.
There was concordance across unadjusted, adjusted (age, race, health insurance type), and propensity-adjusted logistic regression models, supporting the robustness of our findings (see Table 3). With the adjusted models, women at interprofessional medical centers were 27% less likely to birth at early term (P < 0.001) but more likely to birth at late term or postterm, relative to women at noninterprofessional centers. In propensity-adjusted models, there was a 74% lower risk of labor induction at interprofessional centers (risk ratio [RR] 0.26; 95% CI 0.24–0.28) and a 63% lower risk of a cesarean birth before a trial of labor (RR 0.37; 95% CI 0.30–0.47). Oxytocin augmentation was used less frequently (RR 0.26; 95% CI 0.24–0.29), and amniotomy use was 17% less likely (P < 0.001) at interprofessional medical centers. At interprofessional centers, the risk of cesarean birth was 13% lower in the propensity-adjusted model (RR 0.87; 95% CI 0.79–0.95). No significant difference was found in NICU admission rates in the unadjusted, adjusted (age, race, health insurance type), and propensity-adjusted models. Adverse neonatal outcomes occurred in only 0.3% of births (42 of 14 375), which was too rare to be modeled.
TABLE 3.
Risk ratios for labor interventions and birth outcomes among low-risk nulliparous women from the Consortium on Safe Labor receiving intrapartum care at interprofessional versus noninterprofessional medical centers, United States, 2002–2008: Results of logistic regression analyses
| Outcome | Unadjusted model (N = 14 375), RR (95% CI) | Adjusted modela (N = 14 375), =RR (95% CI) | Propensity score-adjusted model (N = 14 375), RR (95% CI) | Propensity score-matched model (N = 7042), RR (95% CI) |
|---|---|---|---|---|
| Gestational age | ||||
| Early term (37 0/7–38 6/7) | 0.69 (0.64–0.74)*** | 0.73 (0.67–0.79)*** | 0.73 (0.67–0.80)*** | 0.70 (0.63–0.78)*** |
| Full term (39 0/7–40 6/7) | Reference | Reference | Reference | Reference |
| Late term (41 0/7–41 6/7) | 1.65 (1.48–1.84)*** | 1.67 (1.47–1.90)*** | 1.68 (1.48–1.90)*** | 1.76 (1.50–2.07)*** |
| Postterm (≥ 42 0/7) | 2.04 (1.40–2.96)*** | 1.90 (1.25–2.88)** | 1.90 (1.25–2.89)** | 3.66 (1.82–7.36)*** |
| Type of labor | ||||
| Spontaneous onset and trial of labor | Reference | Reference | Reference | Reference |
| Induction and trial of labor | 0.26 (0.24–0.28)*** | 0.25 (0.23–0.27)*** | 0.26 (0.24–0.28)*** | 0.26 (0.24–0.29)*** |
| Cesarean without trial of labor | 0.31 (0.25–0.38)*** | 0.35 (0.28–0.43)*** | 0.37 (0.30–0.47)*** | 0.30 (0.22–0.41)*** |
| Rupture of membranes | ||||
| Spontaneous | Reference | Reference | Reference | Reference |
| Amniotomy | 0.83 (0.77–0.89)*** | 0.82 (0.76–0.89)*** | 0.83 (0.77–0.90)*** | 0.71 (0.64–0.78)*** |
| Oxytocin augmentationb | ||||
| Yes | 0.23 (0.21–0.26)*** | 0.26 (0.23–0.29)*** | 0.26 (0.24–0.29)*** | 0.25 (0.22–0.29)*** |
| No | Reference | Reference | Reference | Reference |
| Mode of birth | ||||
| Vaginal—spontaneous | Reference | Reference | Reference | Reference |
| Vaginal—assisted | 0.99 (0.89–1.11) | 1.00 (0.88–1.14) | 1.01 (0.88–1.14) | 0.93 (0.78–1.10) |
| Cesarean | 0.67 (0.62–0.72)*** | 0.86 (0.79–0.94)** | 0.87 (0.79–0.95)** | 0.88 (0.79–0.98)* |
| Neonatal intensive care unit admission | ||||
| Yes | 1.00 (0.86–1.17) | 1.11 (0.93–1.32) | 1.12 (0.94–1.34) | 1.29 (1.04–1.60)* |
| No | Reference | Reference | Reference | Reference |
Noninterprofessional centers (physician practitioners only) are the reference group
Adjusted for maternal age, race, and health insurance type.
Limited to women with spontaneous labor onset and a trial of labor.
P < 0.05
P < 0.01
P < 0.001.
Propensity score matching limited the analysis sample to 7042 healthy, low-risk nulliparous women but allowed for the most restrictive and conservative regression modeling (Table 3). With this approach, women at interprofessional medical centers were 30% less likely to birth at early term (RR 0.70; 95% CI 0.63–0.78) but more likely to birth at or after 41 weeks’ gestation, relative to women at noninterprofessional centers. There was a 74% lower risk of labor induction at interprofessional centers (RR 0.26; 95% CI 0.24–0.29) and 70% lower risk of a cesarean before a trial of labor (RR 0.30; 95% CI 0.22–0.41). Oxytocin augmentation was less likely at interprofessional centers (RR 0.25; 95% CI 0.22–0.29), as was amniotomy. The risk of cesarean birth was 12% lower at interprofessional centers (RR 0.88; 95% CI 0.79–0.98). NICU admissions were more likely at interprofessional medical centers (RR 1.29; 95% CI 1.04–1.60), but adverse neonatal outcomes occurred in only 0.3% of births (23 of 7042), which was too rare to be modeled.
4. DISCUSSION
In this sample of low-risk pregnant women, receiving intrapartum care in an interprofessional medical center was associated with significantly higher rates of spontaneous labor onset, greater cervical dilation on admission, and shorter duration of time between hospital admission and birth, and lower rates of induction, augmentation, and cesarean birth. Even in our most conservative modeling, these differences between medical center types were significant. These findings are consistent with other studies comparing physician-only care to midwifery24 or collaborative25 models of care. These findings may also reflect the influence of core aspects of midwifery philosophy of care, including watchful waiting and nonintervention in normal processes.4 Taken together, our findings suggest that when low-risk women are cared for at interprofessional medical centers, they are cared for within a culture that favors waiting for spontaneous labor to begin, admitting women when labor is more advanced, and that is more conservative with applying pharmacological or surgical interventions as labor progresses.
We found a significant pattern of birth at later gestational ages among interprofessional institutions and birth at earlier gestational ages among centers without interprofessional care. This pattern may reflect differences in care preferences among women choosing maternity care teams with or without midwives or may reflect differences in care practices related to gestational age and induction recommendations between medical centers with and without interprofessional care models.
Questions surrounding the optimal gestational age for birth link closely to questions with respect to induction practices, and our findings may reflect different beliefs about end-of-pregnancy care relevant to both the timing and process of induction. The gestational age when it is more appropriate to await spontaneous onset of labor versus when it is more appropriate to induce labor is a subject of debate. Emerging science seeks to estimate risks and benefits of induction of labor.26–30 Investigators of a recent study of low-risk nulliparous women (n = 6106) randomized to either induction at 39.0–39.4 weeks’ gestation or expectant management found lower cesarean birth rates among the induced women (18.6% and 22.2%, respectively).31 Further work with a more broadly representative sample (73% of low-risk women declined to participate in this trial31) is needed to better understand this low cesarean rate after induction. In our study, low-risk nulliparous women between 39.0 and 39.4 weeks’ gestation undergoing induction had a cesarean rate of 24.5%, whereas all other women ≥39 weeks’ gestation with a trial of labor (either induced or spontaneous) had a cesarean rate of 20.2%.
Women admitted in spontaneous labor were less frequently augmented in interprofessional medical centers. This finding is consistent with other studies of midwifery care models.25,32 Previous analysis of nulliparous women in the CSL showed that nearly half received oxytocin augmentation.33 In our analysis, less than one-third of the nulliparous women who received care in interprofessional medical centers received oxytocin augmentation, whereas more than two-thirds of women in noninterprofessional centers were augmented. This finding may, in part, be related to differences in hospital admission practices as the nulliparous women who received care in interprofessional medical centers were admitted with more advanced dilatation and effacement and had shorter time durations from hospital admission to birth.
Our adjusted and matched model analyses indicated that low-risk nulliparous women receiving care at interprofessional medical centers had a 12%-14% lower risk of cesarean birth. The lower incidence of cesarean births in interprofessional centers is attributable to lower rates of cesareans before a trial of labor (2.1% vs 3.8%) and after spontaneous labor onset with a trial of labor (12.6% vs 13.8%). Cesarean rates after induction of labor were similar among women receiving care at interprofessional and noninterprofessional medical centers (28.9% vs 29.0%). Patterns of cesarean use were also notably different between interprofessional and physician-only centers. For example, 23.7% of cesareans without trial of labor were elective in medical centers without midwives, compared with 9.2% among centers with midwives. Given broad national efforts to lower primary cesarean births in this population,10–14,34 this is an important finding.
Greater involvement of midwives with low-risk laboring women has the potential to improve maternal-child outcomes relevant to both the first and subsequent births. Increasing access to interprofessional models of care for low-risk women could further lower the rate of cesarean births, including repeat cesarean delivery, in the United States. Previous studies of midwifery care models found that women cared for by midwives have lower cesarean rates,7,24,35 and our study further validates these findings.
We also found differences in NICU admission frequency between interprofessional medical centers and noninterprofessional centers (ie, 41 more babies born in interprofessional centers were admitted to the NICU), but no significant differences in adverse neonatal outcomes or low Apgar scores. NICU admission criteria vary by hospital, and there was no variable in the CSL data set that differentiated NICU admission for observation versus admission for serious morbidity. Therefore, we were unable to truly understand neonatal outcomes across center types by using the NICU admission variable in the CSL. NICU admission has been a variable in prior research,25 which motivated our decision to include it in analyses despite its known limitations.36,37 Variables that reliably and validly indicate neonatal health and transition to extrauterine life are currently lacking.38 Development of such variables is an important area for future research.
It is important to note that the presence of midwives as part of a maternity care team may catalyze important differences in the care of low-risk women during childbearing; however, it is equally possible that institutions that value physiologic maternity care may recruit and retain midwives. Determining whether midwives affect maternity care culture or whether certain maternity care cultures engage practices that lead to midwifery presence is an important direction for future research.
There are several limitations to our study. First, CSL data were collected across 12 medical centers and, as with any data set drawn from clinical care, there may be data entry errors that decrease internal validity. However, the CSL represents the most robust collection of information about the provision of intrapartum care in the United States and has been a foundational data set from which many clinical practice improvements have been suggested. Second, we could not reliably ascertain which women in interprofessional centers received care directly from midwives nor do we know the scope of practice of midwives in these centers. To the greatest extent possible, it would be prudent for researchers to collect reliable data about care practitioner types and roles so their influence on care provision and health outcomes can be specifically evaluated. Finally, the size of the CSL data set and the geographic, cultural, and racial/ethnic diversity of women contributing data strengthen the generalizability of our study findings that the presence of midwives in large medical centers may have important influences on birth outcomes. However, rural hospitals, community-based hospitals, and nonteaching hospitals were underrepresented in the CSL; thus, generalizability of our findings to these types of institutions may be limited.
4. 1. Conclusions
Improving the maternity care of low-risk nulliparous childbearing women is a national priority in the United States. The presence of midwives as part of interprofessional medical center teams was associated with fewer interventions during labor and greater likelihood for vaginal birth for this population. Our findings support prior research with respect to the association between midwifery care and low-risk pregnant women’s decreased risk of medical interventions, including cesarean birth. Future research on collaborative care models with improved neonatal measures is needed. Maternity care systems striving to lower rates of intervention and shorten the length of time in hospital for childbearing may benefit from greater incorporation of midwives into their maternity care teams.
Acknowledgments
Funding information
Dr. Rachel B. Breman was a Jonas Scholar during manuscript production. Dr. Nicole Carlson was supported by Grant Number K01NR016984 from the National Institute of Nursing Research during manuscript production. Dr. Julia Phillippi was supported by Grant Number K08HS024733 from the Agency for Healthcare Research and Quality during manuscript production. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Dr. Ellen L. Tilden was supported by Grant Number K12HD043488–14 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and National Institutes of Health Office of Research on Women’s Health, Oregon BIRCWH Scholars in Women’s Health Research Across the Lifespan.
REFERENCES
- 1.Martin JA, Hamilton BE, Osterman M, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep 2018;67(1):1–55 & Supplemental tables. [PubMed] [Google Scholar]
- 2.Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Births: final data for 1997. Natl Vital Stat Rep 1999;47(18):1–96. [PubMed] [Google Scholar]
- 3.Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016;4:CD004667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Nurse-Midwives. Philosophy of the American College of Nurse-Midwives http://www.midwife.org/index.asp?bxml:id=59&cat=2&button=Search&rec=49. Updated 2004. Accessed September 30, 2018.
- 5.Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 2013;32(3):527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glance LG, Dick AW, Glantz JC, et al. Rates of major obstetrical complications vary almost fivefold among US hospitals. Health Aff (Millwood) 2014;33(8):1330–1336. [DOI] [PubMed] [Google Scholar]
- 7.Attanasio L, Kozhimannil KB. Relationship between hospital-level percentage of midwife-attended births and obstetric procedure utilization. J Midwifery Womens Health 2018;63(1):14–22. [DOI] [PubMed] [Google Scholar]
- 8.American College of Obstetricians and Gynecologists, American College of Nurse-Midwives. Joint statement of practice relations between obstetrician-gynecologists and certified nurse-midwives/certified midwives https://www.acog.org/-/media/Statements-of-Policy/Public/87ACNMCollegePolicy-StatementJuly-21-2017.pdf?dmc=1&ts=20180116T2001142928. Updated 2017. Accessed September 28, 2018.
- 9.Jennings J, Nielsen P, Buck ML, et al. Executive summary: collaboration in practice: implementing team-based care: report of the American College of Obstetricians and Gynecologists’ task force on collaborative practice. Obstet Gynecol 2016;127(3):612–617. [DOI] [PubMed] [Google Scholar]
- 10.Caughey AB, Cahill AG, Guise J, Rouse DJ. Safe preven-tion of the primary cesarean delivery. Am J Obstet Gynecol 2014;210(3):179–193. [DOI] [PubMed] [Google Scholar]
- 11.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists workshop. Obstet Gynecol 2012;120(5):1181–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Nurse-Midwives. birthtools.org. tools for optimizing the outcomes of labor safely. http://birthtools.org/Reducing-Primary-Cesareans-NEW. Updated 2018. Accessed September 5, 2018.
- 13.American College of Nurse-Midwives, Midwives Alliance, National Association of Certified Professional Midwives. Supporting healthy and normal physiologic childbirth: a consensus statement by ACNM, MANA, and NACPM http://midwife.org/index.asp?bxml:id=59&cat=3&button=Search. Updated 2012. Accessed August 12, 2018.
- 14.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy people 2020 https://www.healthypeople.gov/. Accessed August 5, 2018.
- 15.Eunice Kennedy Shriver National Institute of Child Health and Human Development. Consortium on Safe Labor https://csl.nichd.nih.gov/. Accessed September 10, 2018.
- 16.Zaki MN, Hibbard JU, Kominiarek MA. Contemporary labor patterns and maternal age. Obstet Gynecol 2013;122(5):1018–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Omih EE, Lindow S. Impact of maternal age on delivery outcomes following spontaneous labour at term. J Perinat Med 2016;44(7):773–777. [DOI] [PubMed] [Google Scholar]
- 18.Yoshioka-Maeda K, Ota E, Ganchimeg T, Kuroda M, Mori R. Caesarean section by maternal age group among singleton deliveries and primiparous Japanese women: a secondary analysis of the WHO global survey on maternal and perinatal health. BMC Pregnancy Childbirth 2016;16 10.1186/s12884-016-0830-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waldenstrom U, Ekeus C. Risk of labor dystocia increases with maternal age irrespective of parity: a population-based register study. Acta Obstet Gynecol Scand 2017;96(9):1063–1069. [DOI] [PubMed] [Google Scholar]
- 20.Yee LM, Costantine MM, Rice MM, et al. Racial and ethnic differences in utilization of labor management strategies intended to reduce cesarean delivery rates. Obstet Gynecol 2017;130(6):1285–1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kozhimannil KB, Shippee TP, Adegoke O, Vemig BA. Trends in hospital-based childbirth care: the role of health insurance. Am J Manag Care 2013;19(4):e125–e132. [PMC free article] [PubMed] [Google Scholar]
- 22.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46(3):399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 2011;10(2):150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carlson NS, Corwin EJ, Hernandez TL, Holt E, Lowe NK, Hurt KJ. Association between provider type and cesarean birth in healthy nulliparous laboring women: a retrospective cohort study. Birth 2018;45(2):159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newhouse RP, Stanik-Hutt J, White KM, et al. Advanced practice nurse outcomes 1990–2008: a systematic review. Nurs Econ 2011;29(5):230–250; quiz 251. [PubMed] [Google Scholar]
- 26.Kjerulff KH, Attanasio LB, Edmonds JK, Kozhimannil KB, Repke JT. Labor induction and cesarean delivery: a prospective cohort study of first births in Pennsylvania, USA. Birth 2017;44(3):252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zenzmaier C, Leitner H, Brezinka C, Oberaigner W, Konig-Bachmann M. Maternal and neonatal outcomes after induction of labor: a population-based study. Arch Gynecol Obstet 2017;295(5):1175–1183. [DOI] [PubMed] [Google Scholar]
- 28.Walker KF, Bugg GJ, Macpherson M, et al. Randomized trial of labor induction in women 35 years of age or older. N Engl J Med 2016;374(9):813–822. [DOI] [PubMed] [Google Scholar]
- 29.Gibbs Pickens CM, Kramer MR, Howards PP, Badell ML, Caughey AB, Hogue CJ. Term elective induction of labor and pregnancy outcomes among obese women and their offspring. Obstet Gynecol 2018;131(1):12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bleicher I, Vitner D, Iofe A, Sagi S, Bader D, Gonen R. When should pregnancies that extended beyond term be induced? J Matern Fetal Neonatal Med 2017;30(2):219–223. [DOI] [PubMed] [Google Scholar]
- 31.Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med 2018;379(6):513–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johantgen M, Fountain L, Zangaro G, Newhouse R, Stanik-Hutt J, White K. Comparison of labor and delivery care provided by certified nurse-midwives and physicians: a systematic review, 1990 to 2008. Womens Health Issues 2012;22(1):e73–e81. [DOI] [PubMed] [Google Scholar]
- 33.Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol 2010;116(6):1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Council on Patient Safety in Women’s Health. Alliance for innovation on maternal health http://safehealthcareforeverywoman.org/aim-program-3/about-aim/. Updated 2018. Accessed August 28, 2018.
- 35.Rosenstein MG, Nijagal M, Nakagawa S, Gregorich SE, Kuppermann M. The association of expanded access to a collaborative midwifery and laborist model with cesarean delivery rates. Obstet Gynecol 2015;126(4):716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ziegler KA, Paul DA, Hoffman M, Locke R. Variation in NICU admission rates without identifiable cause. Hosp Pediatr 2016;6(5):255–260. [DOI] [PubMed] [Google Scholar]
- 37.Wiegerinck MM, Danhof NA, Van Kaam AH, Tamminga P, Mol BW. The validity of the variable “NICU admission” as an outcome measure for neonatal morbidity: a retrospective study. Acta Obstet Gynecol Scand 2014;93(6):603–609. [DOI] [PubMed] [Google Scholar]
- 38.Phillippi JC, Danhausen K, Alliman J, Phillippi RD. Neonatal outcomes in the birth center setting: a systematic review. J Midwifery Womens Health 2018;63(1):68–89. [DOI] [PubMed] [Google Scholar]


