Abstract
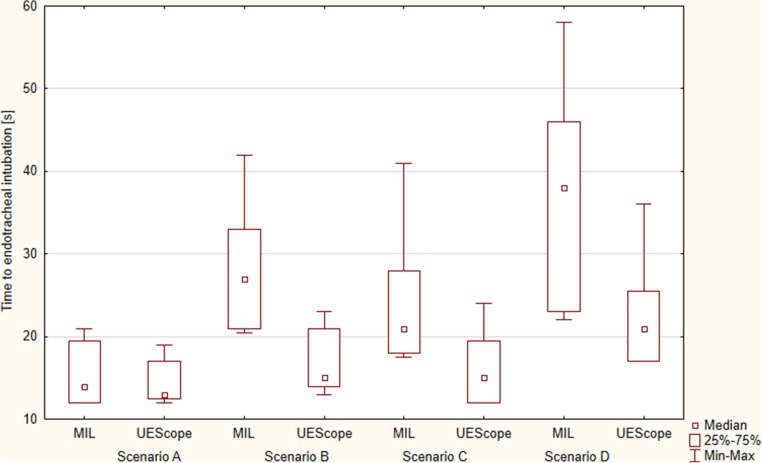
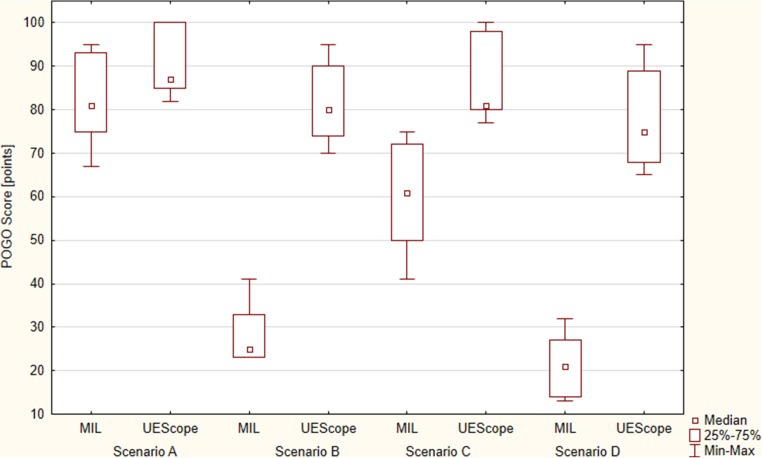
With different videolaryngoscopes for pediatric patients available, UEScope can be used in all age groups. The aim of this study was to compare the Miller laryngoscope and UEScope in pediatric intubation by paramedics in different scenarios. Overall, 93 paramedics with no experience in pediatric intubation or videolaryngoscopy performed endotracheal intubation in scenarios: (A) normal airway without chest compressions, (B) difficult airway without chest compressions, (C) normal airway with uninterrupted chest compressions, (D) difficult airway with uninterrupted chest compressions. Scenario A. Total intubation success with both laryngoscopes: 100%. First-attempt success: 100% for UEScope, 96.8% for Miller. Median intubation time for UEScope: 13 s [IQR, 12.5–17], statistically significantly lower than for Miller: 14 s [IQR, 12–19.5] (p = 0.044). Scenario B. Total efficacy: 81.7% for Miller, 100% for UEScope (p = 0.012). First-attempt success: 48.4% for Miller, 87.1% for UEScope (p = 0.001). Median intubation time: 27 s [IQR, 21–33] with Miller, 15 s [IQR, 14–21] with UEScope (p = 0.001). Scenario C. Total efficiency: 91.4% with Miller, 100% with UEScope (p = 0.018); first-attempt success: 67.7 vs. 90.3% (p = 0.003), respectively. Intubation time: 21 s [IQR, 18–28] for Miller, 15 s [IQR, 12–19.5] for UEScope. Scenario D. Total efficiency: 65.6% with Miller, 98.9% with UEScope (p < 0.001); first-attempt success: 29.1 vs. 72% (p = 0.001), respectively. Intubation time: 38 s [IQR, 23–46] for Miller, 21 s [IQR, 17–25.5] for UEScope.
Conclusion: In pediatric normal airway without chest compressions, UEScope is comparable with Miller. In difficult pediatric airways without chest compressions, UEScope offers better first-attempt success, shorted median intubation time, and improved glottic visualization. With uninterrupted chest compressions in normal or difficult airway, UEScope provides a higher first-attempt success, a shorter median intubation time, and a better glottic visualization than Miller laryngoscope.
|
What is Known:
• Endotracheal intubation is the gold standard for adult and children airway management. • More than two direct laryngoscopy attempts in children with difficult airways are associated with a high failure rate and increased incidence of severe complications. | |
|
What is New:
• In difficult pediatric airways with or without chest compressions, UEScope in inexperienced providers in simulated settings provides better first-attempt efficiency, median intubation time, and glottic visualization. |
Keywords: Cardiopulmonary resuscitation, Endotracheal intubation, Pediatric, Physician, Videolaryngoscopy
Introduction
In pediatric acute care settings, endotracheal intubation is the golden standard for securing the airway in situations where the provider is unable to ventilate the patient adequately with a bag-and-mask or by a supraglottic airway device, or if an open airway is compromised. Cases of inability to perform bag-mask ventilation or to obtain correct placement of supraglottic airway devices, especially among non-anesthesiological personnel or in patients with difficult airway, emphasize the role of videolaryngoscopes [3]. The pediatric and adult airway anatomy and physiology differ, and medical personnel experience in direct pediatric intubation can be limited [23].
A complication of failed endotracheal intubation is hypoxemia [4]. A way to reduce the potential complications, including airway edema, is to decrease the number of total intubation attempts and the procedure duration, which is possible with better or alternative intubation technique, including videolaryngoscopy [14, 18]. Fiadjoe et al. suggest that more than two direct laryngoscopy attempts in children with difficult airway are associated with a high rate of failure and severe complications [4]. Moreover, direct pediatric laryngoscopy is bound with significant interruptions in chest compressions [2].
Videolaryngoscopy offers a better viewing angle and less traumatic intubation, can reduce the complication rate [15, 17, 30], and supports intubation training [13].
Many different videolaryngoscopes for pediatric patients are available, but not all can be used in all age groups [23, 30]. UEScope is a portable videolaryngoscope [29] invented in 2010, equipped with several blades for different age groups. Its specific feature is the angulated blade [29]. The technique for introducing UEScope does not demand tongue sweep. UEScope has been tested in various clinical conditions and most of the studies were performed in Chinese pediatric patients [23, 24]. The results, though inconsistent, suggest that UEScope is not inferior to direct laryngoscopy. As is true for many videolaryngoscopes, the UEScope learning curve is better than that for direct laryngoscopy. Owing to the slim design and low weight, UEScope is easy to manipulate [29].
Videolaryngoscopy with the use of numerous devices in difficult pediatric airway with continuous chest compressions has been tested in several studies. Comparing GlideScope and direct laryngoscopy in a pediatric simulator by novice physicians, Rabiner et al. found that GlideScope did not improve time to intubation or intubation success rates in normal or difficult airway scenarios [16]. In turn, in a study by Szarpak et al. concerning pediatric endotracheal intubation with chest compressions, the first-attempt intubation and overall intubation success were better with GlideScope than with Miller direct laryngoscopy [25]. TruView offered better intubation conditions than Macintosh in a pediatric manikin scenario with chest compressions with and without cervical stabilization [24].
The UEScope was selected because it is a portable device with angulated or Miller’s blade which can be used in all age group and the results concerning effectiveness in endotracheal intubation obtained so far were inconsistent.
The aim of the study was to compare the Miller laryngoscope and UEScope during pediatric intubation performed by paramedics in different airway conditions.
Methods
The study was designed as a prospective, multicenter, randomized, crossover simulation trial. It was performed in Warsaw, Wroclaw, and Poznan, Poland, between December 2017 and May 2018, in accordance with the Consolidated Standards of Reporting Trials (CONSORT) [17]. The protocol was approved by the Institutional Review Board of the Polish Society of Disaster Medicine (approval No. 21.11.2017.IRB).
Participants
The study included 93 paramedics participating in Pediatric Advance Life Support courses based on the American Heart Association guidelines. Voluntary written informed consent was obtained from all participants. The inclusion criteria were the following: (1) not having performed more than 100 clinical adult intubations with direct laryngoscopy and no experience in clinical pediatric intubation; (2) no experience in clinical or experimental training in videolaryngoscopy [24]. Wrist or back injury up to 1 month before the study was the exclusion criterion.
Scenarios
To simulate endotracheal tube immediate airway management conditions in a 5-year-old child, the Pediatric HAL® S3005 simulator was used (Gaumard® Scientific, Miami, USA). The participants performed intubation in four scenarios:
Scenario A: normal airway without chest compressions.
Scenario B: difficult airway without chest compressions. The simulator control software inflated the tongue to simulate conditions of Mallampati scale grade III [18].
Scenario C: normal airway with uninterrupted chest compressions. To standardize the difficulties resulting from chest compressions, the Corpuls system (GS Elektromedizinische Geräte G. Stemple GmbH, Kaufering, Germany) was used to apply chest compressions (depth, 5 cm; frequency, 100 per minute).
Scenario D: difficult airway with uninterrupted chest compressions. As in scenario B, tongue inflation was applied. The Corpuls system performed chest compressions as in scenario C.
In all scenarios, the simulator was placed on a flat surface in a well-lit room with the head in neutral position. In both tested devices, the blade size No. 2 was used. In both tested devices, Miller’s blade was used. Endotracheal intubation was performed with a standard sealed tube of 5.5 internal diameter. A stylet was used, moistened with a lubricant, like the endotracheal tube itself. The shape of the stylet was standard and the tip of the stylet was bent to form a 90° angle. After each intubation attempt, the participant had to confirm ventilation correctness using a self-inflating bag (Ambu, Copenhagen, Denmark).
Study protocol
Prior to the study, all paramedics participated in a 30-min training, covering the anatomy, physiology, and pathophysiology of the pediatric respiratory tract, as well as endotracheal intubation with the tested devices. The training with the Miller laryngoscope (Heine USA Ltd., Dover, USA) and UEScope (Zhejiang UE Medical Corp., Zhejiang, China) was performed by an experienced anesthesiologist (Fig. 1). Then, the participants had up to 10 min to practice intubation with the tested devices in normal adult airways with the AT Kelly Torso manikin (Laerdal, Stavanger, Norway).
Fig. 1.

Intubation with a UEScope videolaryngoscope
One week after the training, the paramedics performed endotracheal intubation in the pediatric patient in various scenarios of simulated cardiopulmonary resuscitation using the tested devices.
The order of participants and intubation methods was random: the Research Randomizer program (randomizer.org) was used. Figure 2 presents the detailed randomization procedure. Each participant had up to three attempts to intubate with each laryngoscope. Then a 10-min break was taken before the participant performed the intubation scenarios with the remaining intubation device. The paramedics were informed that the patient required immediate endotracheal intubation.
Fig. 2.
Time to intubation during the study
Measurements and outcomes
The primary outcome was first intubation attempt success, defined as effective ventilation with an endotracheal tube, accompanied by a chest rise in the simulator and air flow in the lungs recorded by the simulator software. The following criteria determined failed intubation: more than three unsuccessful attempts, intubation procedure exceeding 120 s, or unrecognized esophageal intubation.
The secondary outcomes included intubation time, time to best glottic view, percentage of glottic opening and the Cormack-Lehane grade, and the ease of intubation. The intubation time was defined as the time from grasping the laryngoscope to the first attempt of effective ventilation with a self-expanding bag. The measured “time to best glottic view” was defined as “I can see the vocal cords.” The study participants assessed the glottic visibility degree: using percentage of glottic opening (POGO) [28] and the Cormack-Lehane grade [5]. A 100% POGO score indicates visualization of the entire glottic, while a 0% POGO score means no visualization of the laryngeal structures. After each intubation, the paramedics also described the ease of intubation on a scale from 1 (very easy) to 100 (very difficult).
Sample size calculation and statistical analysis
The sample size was calculated with the G*Power 3.1 software, and the two-tailed t test was applied (Cohen’s d, 0.8; alpha error, 0.05; power, 0.95). The minimum of 61 participants turned out necessary to achieve an acceptable level of significance and power of the study; 93 were involved.
Results
Demographics
The study involved 93 paramedics (26 female; 27.9%) with no experience in videolaryngoscopy. All were employees of Emergency Medical Service teams. Their median age was 32 years [IQR, 29–37.5], and median work experience in emergency medicine equaled 6.5 years [IQR, 4–9].
Scenario A: normal airway without chest compressions
The overall success with UEScope as well as with Miller was 100%. The first-attempt success was 100% for UEScope, and 96.8% for Miller (Table 1). The median intubation time for UEScope was 13 s [IQR, 12.5–17], lower than with Miller (14 s [IQR, 12–19.5]) (p = 0.044; Fig. 2).
Table 1.
Study outcomes by laryngoscope devices (n = 93)
| Outcome | Miller laryngoscope | UEScope videolaryngoscope | p value |
|---|---|---|---|
| Scenario A: normal airway without chest compressions | |||
| Success of intubation attempts [%] | |||
| 1st | 90 (96.8%) | 93 (100%) | NS |
| 2nd | 3 (3.2%) | – | |
| 3rd | – | – | |
| Overall intubation success rate [%] | 93 (100%) | 93 (100%) | NS |
| Time to endotracheal intubation [s] | 14 (12–19.5) | 13 (12.5–17) | 0.044 |
| Cormack and Lehane grade | |||
| 1 | 71 (76.3%) | 93 (100%) | 0.012 |
| 2 | 22 (24.6%) | – | |
| 3 | – | – | |
| 4 | – | – | |
| POGO score, 1–100 | 81 (75–93) | 87 (85–100) | 0.037 |
| Ease of use, 1–100 | 18 (15–22) | 15 (10–19) | 0.021 |
| Scenario B: difficult airway without chest compressions | |||
| Success of intubation attempts [%] | |||
| 1st | 45 (48.4%) | 81 (87.1%) | 0.001 |
| 2nd | 21 (22.6%) | 12 (12.9%) | |
| 3rd | 10 (10.7%) | – | |
| Overall intubation success rate [%] | 76 (81.7%) | 93 (100%) | 0.012 |
| Time to endotracheal intubation [s] | 27 (21–33) | 15 (14–21) | 0.001 |
| Cormack and Lehane grade | |||
| 1 | – | 51 (54.8%) | < 0.001 |
| 2 | 14 (15.1%) | 39 (42%) | |
| 3 | 68 (73.1%) | 3 (3.2%) | |
| 4 | 11 (11.8%) | – | |
| POGO score, 1–100 | 25 (23–33) | 80 (74–90) | < 0.001 |
| Ease of use, 1–100 | 74 (68–82) | 27 (16–35) | < 0.001 |
| Scenario C: normal airway with chest compressions | |||
| Success of intubation attempts [%] | |||
| 1st | 63 (67.7%) | 84 (90.3%) | 0.003 |
| 2nd | 20 (21.5%) | 9 (6.7%) | |
| 3rd | 2 (2.2%) | – | |
| Overall intubation success rate [%] | 85 (91.4%) | 93 (100%) | 0.018 |
| Time to endotracheal intubation [s] | 21 (18–28) | 15 (12–19.5) | 0.005 |
| Cormack and Lehane grade | |||
| 1 | 43 (46.2%) | 90 (96.8%) | 0.011 |
| 2 | 39 (41.9%) | 3 (3.2%) | |
| 3 | 10 (10.7%) | – | |
| 4 | – | – | |
| POGO score, 1–100 | 61 (50–72) | 81 (80–98) | < 0.001 |
| Ease of use, 1–100 | 39 (31–53) | 17 (14–23) | < 0.001 |
| Scenario D: difficult airway with chest compressions | |||
| Success of intubation attempts [%] | |||
| 1st | 27 (29.1%) | 67 (72%) | 0.001 |
| 2nd | 31 (33.3%) | 20 (21.5%) | |
| 3rd | 3 (3.2%) | 5 (5.4%) | |
| Overall intubation success rate [%] | 61 (65.6%) | 92 (98.9%) | < 0.001 |
| Time to endotracheal intubation [s] | 38 (23–46) | 21 (17–25.5) | 0.004 |
| Cormack and Lehane grade | |||
| 1 | – | 47 (50.5%) | < 0.001 |
| 2 | 7 (7.5%) | 37 (39.8%) | |
| 3 | 70 (75.3%) | 9 (9.7%) | |
| 4 | 16 (17.2%) | – | |
| POGO score, 1–100 | 21 (14–27) | 75 (68–89) | < 0.001 |
| Ease of use, 1–100 | 85 (77–92) | 30 (28–39) | < 0.001 |
NS not statistically significant, POGO percentage of glottis opening
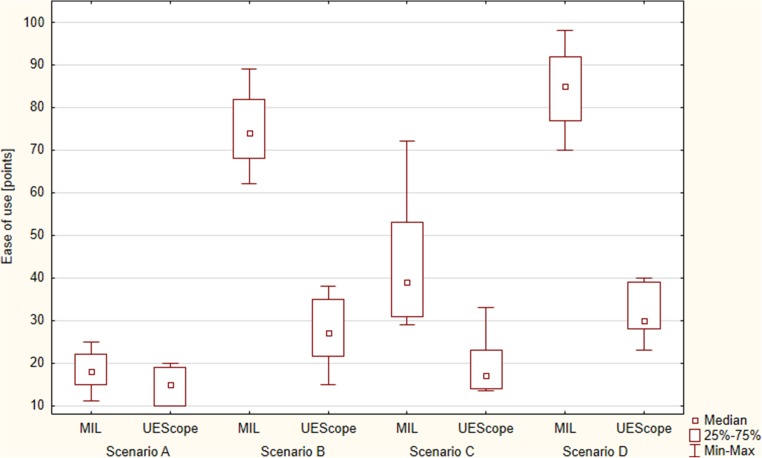
Intubation using UEScope compared with Miller was associated with a better glottic visualization based on the Cormack-Lehane scale (p = 0.012). The POGO score was 81% [IQR, 75–93] for Miller and 87% [IQR, 85–100] for UEScope (p = 0.037; Fig. 3). Intubation with UEScope proved easier in the subjective assessment as compared with Miller (15 [IQR, 10–19] vs. 18 points [IQR, 15–22]) (p = 0.021; Fig. 4).
Fig. 3.
Percentage of glottic opening (POGO score)
Fig. 4.
Ease of intubation with different airway scenarios
Scenario B: difficult airway without chest compressions
The total endotracheal intubation efficacy with Miller and UEScope varied and equaled 81.7 vs. 100%, respectively (p = 0.012). Successful endotracheal intubation on first-attempt success was 48.4% for Miller and 87.1% for UEScope (p = 0.001; Table 1). The median intubation time was 27 s [IQR, 21–33] for Miller and 15 s [IQR, 14–21] for UEScope (p = 0.001; Fig. 2). The degree of glottic visualization based on the Cormack-Lehane scale proved better for UEScope (p < 0.001). The POGO score was 25% [IQR, 23–33] for Miller and 80% [IQR, 74–90] for UEScope (p < 0.001; Fig. 3). The ease of use amounted to 74 points [IQR, 68–82] for Miller and 27 points [IQR, 16–25] for UEScope (p < 0.001; Fig. 4).
Scenario C: normal airway with uninterrupted chest compressions
The overall success was 91.4% with Miller and 100% with UEScope (p = 0.018), with the successful endotracheal intubation on first-attempt success 67.7 vs. 90.3%, respectively (p = 0.003; Table 1). The intubation time was 21 s [IQR, 18–28] for Miller and 15 s [IQR, 12–19.5] for UEScope. The UEScope procedure was statistically significantly shorter than that with Miller (p = 0.005; Fig. 2). Glottic visualization with UEScope compared with Miller was also statistically significantly better (p = 0.011). The POGO score equaled 61% [IQR, 50–72] for Miller and 81% [IQR, 80–98] for UEScope (p < 0.001; Fig. 3). The intubation ease with UEScope was 17 points [IQR, 14–23], statistically significantly better than that with Miller (39 points [IQR, 31–53]) (p < 0.001; Fig. 4).
Scenario D: difficult airway with uninterrupted chest compressions
The intubation efficiency was higher for UEScope compared with Miller both overall (98.9 vs. 65.6%; p < 0.001) and for the first attempt (72 vs. 29.1%; p = 0.001). UEScope proved superior to Miller also with regard to the procedure duration (21 [IQR, 17–25.5] vs. 38 s [IQR, 23–46]; p = 0.004; Fig. 2), glottic visualization based on the Cormack-Lehane scale (p < 0.001), POGO score (75% [IQR, 68–89] vs. 21% [IQR, 14–27]; p < 0.001; Fig. 3), and ease of use (30 [IQR, 28–39] vs. 85 points [IQR, 77–92]; p < 0.001; Fig. 4).
Discussion
The use of videolaryngoscopy in normal and difficult airway has been widely tested in adults. However, videolaryngoscopes are still not regarded as the standard first-attempt devices for normal airway intubation in children [6, 10, 22]. Their application depends on the clinical settings and the intubator’s experience. Many studies have been carried out on the role of videolaryngoscopy in normal and difficult airway in pediatric patients [12, 18, 23, 24, 30, 32]. Some suggest that videolaryngoscopes offer no benefit over direct laryngoscopy performed by emergency department personnel with regard to the rate of first-pass intubation success, complications, or successful intubation [3]. Other studies reveal advantages of videolaryngoscopy in children, especially with difficult airway [9, 16, 20, 24].
In our study in normal airway without chest compressions, the median intubation time was comparable, and the differences were statically significant although not relevant from a practical point of view. In difficult airway without chest compressions, the total endotracheal intubation efficacy and median intubation time using Miller and UEScope varied, and the differences were statistically and practically important. In normal airway with uninterrupted chest compressions, those differences were also statistically important. The biggest differences were found in difficult airway with uninterrupted chest; they were statistically significant and noticeable practical significance.
UEScope has been tested in different clinical conditions in adult and pediatric patients, generally Chinese; the role of UEScope for non-Chinese patients is raised [7, 8, 21, 22, 31, 32], with the consideration of potential differences in airway anatomy. These studies were published mainly in Chinese, and their results are available thanks to publications by Xue et al. [29, 30].
Most studies concerning videolaryngoscopes in pediatric patients analyzed normal airway [19]. We investigated various situations, including difficult airway and intubation accompanied by continuous chest compressions.
Although inexperienced providers are not expected to perform pediatric intubation in their daily practice routinely, comparing personnel more experienced in direct laryngoscopy than in the use of videolaryngoscopy would be a source of methodological bias.
Wan [24] proved a better glottic view, a higher first-attempt success rate, and shorter intubation time with UEScope than with Macintosh in normal airway pediatric patients. In our simulation, endotracheal tube placement was equal in UEScope and direct laryngoscopy groups, but still the UEScope intubation time turned out shorter than that with direct laryngoscopy. The differences can be explained by the assumed definitions of time to intubation and the clinical vs. simulation setting.
In a study by Jiang and Jin [8] among 200 children with normal airway, videolaryngoscopy improved the laryngeal view and the success rate compared with Macintosh, but the intubation time was similar. We found a shorter intubation time in the difficult airway scenario, comparable with that in the clinical study by Jiang and Jin.
UEScope was also compared with direct laryngoscopy for endotracheal intubation in neonates for planned surgery. Its first-attempt success was non-inferior or better and the intubation time was shorter [1, 26, 27, 31]. The size of the groups in these studies was limited and the intubator’s experience; this can be the reason for the first-attempt success inconsistency.
Limitations and strengths
One of the limitations is that the study was performed with a pediatric simulator. However, medical simulation allows for multiple procedures with no potential harm to the patient, and for standardization of conditions [11, 21]. Secondly, the study group was limited to paramedics. Although being inexperienced intubators, they work in emergency situations and face pediatric patients, including those requiring advanced airway management. The third limitation is the shorter learning curve and better glottic visualization with the use of videolaryngoscopy comparing to direct laryngoscopy.
The study strengths include the randomization, crossover design, comparison of various scenarios, and advanced research methods.
Conclusions
In pediatric normal airway without chest compressions, UEScope is comparable with Miller. In difficult pediatric airways without chest compressions, UEScope offers better first-attempt success, shorted median intubation time, and improved glottic visualization. With uninterrupted chest compressions in normal or difficult airway, UEScope provides a higher first-attempt success, a shorter median intubation time, and a better glottic visualization than Miller laryngoscope.
Acknowledgments
We would like to thank all the participants for their involvement in our study.
Abbreviations
- CONSORT
Consolidated Standards of Reporting Trials
- POGO
percentage of glottic opening
Authors’ contributions
JS, MM, and LS contributed significantly to the planning of the study and the study design. All authors recruited the participants and collected the data. JS and LS were the principal investigators of this study and did major manuscript preparation. LS and JS prepared the statistical analysis. JS, MM, DD, EMS, and LS contributed significantly to manuscript editing and expertise.
Conflict of interests
The authors declare that they have no conflict of interest.
Ethical approval
Approval was granted by the Institutional Review Board of the Polish Society of Disaster Medicine (approval no. 21.11.2017.IRB).
Informed consent
Informed consent was obtained from all participants included in the study.
Source of support
No sources of financial or material support to be declared.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jacek Smereka, Email: smereka.icu@gmail.com.
Marcin Madziala, Email: mmadziala262@gmail.com.
Dominika Dunder, Email: src.emergency@gmail.com.
Elzbieta Makomaska-Szaroszyk, Email: ptmk.kontakt@gmail.com.
Lukasz Szarpak, Phone: (+48) 500186225, Email: lukasz.szarpak@gmail.com.
References
- 1.Donoghue AJ, Ades AM, Nishisaki A, Deutsch ES. Videolaryngoscopy versus direct laryngoscopy in simulated pediatric intubation. Ann Emerg Med. 2013;61(3):271–277. doi: 10.1016/j.annemergmed.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Donoghue A, Hsieh TC, Nishisaki A, Myers S. Tracheal intubation during pediatric cardiopulmonary resuscitation: a videography-based assessment in an emergency department resuscitation room. Resuscitation. 2016;99:38–43. doi: 10.1016/j.resuscitation.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Eisenberg MA, Green-Hopkins I, Werner H, Nagler J. Comparison between direct and video-assisted laryngoscopy for intubations in a pediatric emergency department. Acad Emerg Med. 2016;23(8):870–877. doi: 10.1111/acem.13015. [DOI] [PubMed] [Google Scholar]
- 4.Fiadjoe JE, Nishisaki A, Jagannathan N, Hunyady AI, Greenberg RS, Reynolds PI, Matuszczak ME, Rehman MA, Polaner DM, Szmuk P, Nadkarni VM, McGowan FX, Jr, Litman RS, Kovatsis PG. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4(1):37–48. doi: 10.1016/S2213-2600(15)00508-1. [DOI] [PubMed] [Google Scholar]
- 5.Glosser L. Assessment of endotracheal tube intubation. Review of existing scales. Disaster Emerg Med J. 2017;2(2):91–93. [Google Scholar]
- 6.He W, Huang MM, Liu TS, et al. Comparison of HC videolaryngoscope and Macintosh direct laryngoscope for tracheal intubation in pediatric patients. Chin J Anesthesiol. 2014;34:1357–1360. [Google Scholar]
- 7.Jagannathan N, Hajduk J, Sohn L, Huang A, Sawardekar A, Albers B, Bienia S, De Oliveira GS. Randomized equivalence trial of the King Vision aBlade videolaryngoscope with the Miller direct laryngoscope for routine tracheal intubation in children <2 yr of age. Br J Anaesth. 2017;118(6):932–937. doi: 10.1093/bja/aex073. [DOI] [PubMed] [Google Scholar]
- 8.Jiang Y, Jin QY. Comparison between home-made UE videolaryngoscope and direct laryngoscope for tracheal intubation in pediatric patients. J Chin Pract Diagn Ther. 2014;28:59–60. [Google Scholar]
- 9.Karczewska K, Szarpak L, Smereka J, Dabrowski M, Ladny JR, Wieczorek W, Robak O, Frass M, Ahuja S, Ruetzler K. ET-View compared to direct laryngoscopy in patients with immobilized cervical spine by unexperienced physicians: a randomized crossover manikin trial. Anaesthesiol Intensive Ther. 2017;49(4):274–282. doi: 10.5603/AIT.a2017.0047. [DOI] [PubMed] [Google Scholar]
- 10.Ladny JR, Sierzantowicz R, Kedziora J, Szarpak L. Comparison of direct and optical laryngoscopy during simulated cardiopulmonary resuscitation. Am J Emerg Med. 2017;35(3):518–519. doi: 10.1016/j.ajem.2016.12.026. [DOI] [PubMed] [Google Scholar]
- 11.Ladny JR, Smereka J, Szarpak L. Comparison of the Trachway video intubating stylet and Macintosh laryngoscope for endotracheal intubation. Preliminary data. Am J Emerg Med. 2017;35(4):574–575. doi: 10.1016/j.ajem.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 12.Madziala M. The ETView tracheoscopic ventilation tube for trauma patient intubation. Disaster Emerg Med J. 2018;3(2):69–70. [Google Scholar]
- 13.O’Shea JE, Thio M, Kamlin CO, McGrory L, Wong C, John J, et al. Videolaryngoscopy to teach neonatal intubation: a randomized trial. Pediatrics. 2015;136:912–919. doi: 10.1542/peds.2015-1028. [DOI] [PubMed] [Google Scholar]
- 14.Parker MM, Nuthall G, Brown C, 3rd, Biagas K, Napolitano N, Polikoff LA, Simon D, Miksa M, Gradidge E, Lee JH, Krishna AS, Tellez D, Bird GL, Rehder KJ, Turner DA, Adu-Darko M, Nett ST, Derbyshire AT, Meyer K, Giuliano J, Jr, Owen EB, Sullivan JE, Tarquinio K, Kamat P, Sanders RC, Jr, Pinto M, Bysani GK, Emeriaud G, Nagai Y, MA MC, Walson KH, Vanderford P, Lee A, Bain J, Skippen P, Breuer R, Tallent S, Nadkarni V, Nishisaki A, Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network Relationship between adverse tracheal intubation associated events and PICU outcomes. Pediatr Crit Care Med. 2017;18(4):310–318. doi: 10.1097/PCC.0000000000001074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pouppirt NR, Nassar R, Napolitano N, Nawab U, Nishisaki A, Nadkarni V, Ades A, Foglia EE. Association between video laryngoscopy and adverse tracheal intubation-associated events in the neonatal intensive care unit. J Pediatr. 2018;201:281–284.e1. doi: 10.1016/j.jpeds.2018.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rabiner JE, Auerbach M, Avner JR, Daswani D, Khine H. Comparison of GlideScope videolaryngoscopy to direct laryngoscopy for intubation of a pediatric simulator by novice physicians. Emerg Med Int. 2013;2013:407547–407546. doi: 10.1155/2013/407547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schulz KF, Altman DG, Moher D, CONSORT Group CONSORT 2010 statement: up-dated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shiima Y, Hsieh TC, Long A, Donoghue A. Videographic assessment of pediatric tracheal intubation technique during emergency airway management. Pediatr Crit Care Med. 2018;19(3):e136–e144. doi: 10.1097/PCC.0000000000001423. [DOI] [PubMed] [Google Scholar]
- 19.Sinha PK, Mitra S, Gombar S, Gombar KK. A new class for modified Mallampati sign. Anesth Analg. 1999;89(1):259–260. doi: 10.1097/00000539-199907000-00059. [DOI] [PubMed] [Google Scholar]
- 20.Smereka J, Czyzewski L, Szarpak L, Ladny JR. Comparison between the TrueView EVO2 PCD and direct laryngoscopy for endotracheal intubation performed by paramedics: preliminary data. Am J Emerg Med. 2017;35(5):789–790. doi: 10.1016/j.ajem.2016.11.063. [DOI] [PubMed] [Google Scholar]
- 21.Smereka J, Ladny JR, Naylor A, Ruetzler K, Szarpak L. C-MAC compared with direct laryngoscopy for intubation in patients with cervical spine immobilization: a manikin trial. Am J Emerg Med. 2017;35(8):1142–1146. doi: 10.1016/j.ajem.2017.03.030. [DOI] [PubMed] [Google Scholar]
- 22.Sun Y, Lu Y, Huang Y, Jiang H. Pediatric video laryngoscope versus direct laryngoscope: a meta-analysis of randomized controlled trials. Paediatr Anaesth. 2014;24(10):1056–1065. doi: 10.1111/pan.12458. [DOI] [PubMed] [Google Scholar]
- 23.Sunder RA, Haile DT, Farrell PT, Sharma A. Pediatric airway management: current practices and future directions. Paediatr Anaesth. 2012;22(10):1008–1015. doi: 10.1111/pan.12013. [DOI] [PubMed] [Google Scholar]
- 24.Szarpak L, Czyzewski L, Kurowski A, Truszewski Z. Comparison of the TruView PCD video laryngoscope and Macintosh laryngoscope for pediatric tracheal intubation by novice paramedics: a randomized crossover simulation trial. Eur J Pediatr. 2015;174(10):1325–1332. doi: 10.1007/s00431-015-2538-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szarpak L, Czyżewski L, Kurowski A. Can GlideScope® videolaryngoscope be an alternative to direct laryngoscopy for child and infant tracheal intubation during chest compression? Eur J Pediatr. 2015;174(7):981–982. doi: 10.1007/s00431-015-2495-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wan XX. Comparative analysis of application of domestic UE videolaryngoscope and direct laryngoscope in pediatric tracheal intubation. Mod J Interg Tradit Chin Wes Med. 2015;24:1232–1234. [Google Scholar]
- 27.Wang JL, Huang HQ, Shi XH, Fei J. Clinical application of HC videolaryngoscope for intubation in the neonate with a cleft lip. J Clin Anesthesiol. 2014;30:785–787. [Google Scholar]
- 28.Wojewodzka-Zelezniakowicz M, Madziala A, Madziala M. Comparison of the Miller and Macintosh laryngoscopes in simulated pediatric trauma patient: a pilot study. Disaster Emerg Med J. 2017;2(1):1–6. [Google Scholar]
- 29.Xue FS, Yang BQ, Liu YY, Li HX, Yang GZ. Current evidences for the use of UEscope in airway management. Chin Med J. 2017;130(15):1867–1875. doi: 10.4103/0366-6999.211536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xue FS, Liu YY, Li HX, Yang GZ. Paediatric video laryngoscopy and airway management: what’s the clinical evidence? Anaesth Crit Care Pain Med. Available online 10 Jan 2018. 10.1016/j.accpm.2017.11.018 [DOI] [PubMed]
- 31.Zheng Y. Application of videolaryngoscope in tracheal intubation in neonates. Henan J Surg. 2014;20:30–32. [Google Scholar]
- 32.Zheng P, He QW. Application of HC videolaryngoscope in endotracheal intubation in children undergoing general anesthesia. Chin J Endosc. 2015;21:948–951. [Google Scholar]