Abstract
Background
Stress, anxiety, and depression have been reported as very common comorbidities in smokers with chronic obstructive pulmonary disease (COPD). This study was aimed to investigate the effectiveness of smoking cessation on stress, anxiety, and depression in smokers with COPD.
Methods
Three block-randomized controlled trial groups with a block size of 6 and 9 including guided self-change (GSC) (n = 19), nicotine replacement therapy (NRT) (n = 19), and combined GSC-NRT (n = 19) with a follow-up of 29 weeks were considered in this research. Participants included elderly adult smokers with COPD. The patients carried out 5 weekly GSC counseling sessions and NRT for smoking cessation. Transtheoretical Model (TTM) questionnaire, Fagerstrom Test for Nicotine Dependence (FTND), Depression Anxiety Stress Scale (DASS), the Beck Depression Inventory-II (BDI-II), and Hospital Anxiety and Depression Scale (HADS) as well as the exhaled carbon monoxide (CO) were evaluated over the baseline and 12 and 29 weeks following treatments.
Findings
COPD participants with mean of 23 daily cigarette smoking completed the current study. The odds ratio (OR) of smoking cessation in GSC and GSC-NRT groups decreased more than NRT group. In addition, DASS, FTND, and the exhaled CO in GSC and GSC-NRT groups showed a better performance compared with the NRT group.
Conclusion
The results showed that GSC and combined GSC-NRT therapy were significantly more effective than NRT alone. Also, the findings showed that GSC, NRT, and combined GSC-NRT were effective on stress, depression, and anxiety decreasing in smoking cessation. It seems that reducing smoking is associated with recovery in stress, anxiety, and depression in smokers with COPD.
Keywords: Smoking cessation, Chronic obstructive pulmonary disease, Life stress, Depression, Anxiety
Introduction
Chronic obstructive pulmonary disease (COPD) is often accompanied by anxiety and depression.1,2 Smoking as one of the important risk factors of COPD causes anxiety and depression and may contribute to the development of them.3 Anxiety and depression are the most common problems in people with COPD, resulting in severe health outcomes, a decrease in quality of life, and a significant increase in health care costs.4 Depression is significantly associated with mortality and permanent smoking in six months. Additionally, depression in patients with COPD is associated with a low survival rate and sustained smoking.5 Furthermore, smoking is the main cause of COPD.6 Smokers with any severity of obstructive airway disease should have a cessation program with regular and long-term follow-up.7 Also, the severity of nicotine dependency and withdrawal symptoms in smoking cessation programs are related to psychiatric disorders such as anxiety and depression.8 Smoking cessation can help prevent progression and complications of COPD.9 In this regard, health professionals should prioritize counseling and treatment for cigarette smoking for smokers with COPD.6 Nicotine replacement therapy (NRT) has been proven to be effective when it comes to counseling10 in helping to quit smoking and persistent abstinence in smokers with COPD.11 An approach in this regard is the guided self-change (GSC) combined with NRT.11 The GSC program is a harm reduction motivational cognitive-behavioral therapy (CBT) that was first implemented by Linda and Mark Sobell and Sobell in 1996 at the Nova Southeastern University.12 GSC is based on CBT principles and is a powerful tool for the treatment of substance-related disorders.13 This is a short-term CBT and cost-effective therapy that can be implemented by a wide range of mental health care providers to smoking cessation.13
Methods
This trial was conducted in the Psychiatry and Behavioral Sciences Research Center of the Addiction Institute and Lung Research Center of Mazandaran University of Medical Sciences, Sari, Iran. The trial procedure was registered at the Iranian Clinical Trials Registry (IRCT201609271457N11) and carried out according to the Declaration of Helsinki and its subsequent revisions. Participants were informed of the research protocol and their rights to leave the study at any time and then they signed an informed consent. The research was carried out from December 2016 to November 2017. The statistical population included all participants with COPD referred to the pulmonary clinic of Imam Khomeini Hospital in Sari City.
Inclusion criteria included being over 45 years old and COPD and nicotine-dependent patients diagnosed and referred by a pulmonologist who had diagnosed airway obstruction.
Exclusion criteria were having other systemic medical diseases including diabetes mellitus (DM), respiratory failure, normal primary spirometry, contraindications for consuming nicotine gum (i.e., allergy, recent heart attacks, risky arrhythmias, severe angina, hyperthyroidism, insulin-dependent DM, active peptic ulcers, pregnancy, and lactation), being under 45 years old, and having no history of psychosis diagnosis.
Randomization, concealment, and blinding
A computerized random number creator was applied to generate a randomization schedule utilizing block randomization (block size of 6 and 9) with an independent clinical epidemiologist who was not involved in any of the research steps (i.e., recruitment, intervention, and evaluation). To conceal the randomization sequences, they were kept in lightproof sealed envelopes. Eligible participants were randomly assigned to the three parallel groups with an allocation ratio of 1:1:1 based on the randomization list following signing informed agreement form. Participants and the therapist were blinded in the initial valuation for inclusion criteria; however, neither participants nor the therapist was blinded over the trial because it was not possible to mask participants for assigning to GSC, NRT, or combined group.
Interventions
Interventions including GSC, NRT, and GSC-NRT were performed in three groups.
GSC intervention protocol
GSC intervention protocol included 5 sessions: screening and assessment, deciding to change, discussing risky situations, identifying different solutions to action, and steps to the future. GSC was executed in 5 one-hour sessions over 5 weeks.14
Outcomes
Primary outcomes: Primary outcomes included depression, anxiety, and stress changes, smoking cessation rate, and daily consumption of cigarette in participants over baseline and 12 and 29 weeks following the treatments.
Secondary outcomes: Secondary outcomes included nicotine dependency, exhaled CO, and CO binding to hemoglobin.
Procedures and measurements
Nicotine (Nicolife®) blisters (labeled 30 gums) included 2 mg nicotine in each gum. All randomized participants were referred to Mostafavian Pulmonary Clinic of Imam Khomeini Hospital in Sari City. Following the randomization, additional baseline information including smoking and cessation history, medical history, and other relevant data were collected. A sample size including 57 participants (19 in every group) was computed (conferred 80% power, with two-sided P = 0.050) to identify an absolute difference of 10% in cessation rates over the three groups. No eligible woman was found in the patients with COPD in our study. After describing the research protocol, participants completed the demographic information questionnaires, Transtheoretical Model (TTM) questionnaire,15 and the Fagerstrom Test for Nicotine Dependence (FTND).10 The pulmonary function was assessed according to the outcomes of the exhaled CO16 using Bedfont PiCO+ Smokerlyzers (Bedfont Scientific Ltd., UK). Next, in addition to routine treatments (i.e., bronchodilator corticosteroid, beta-agonists, and anticholinergic inhalers), a trained psychotherapist carried out NRT and GSC. In the current research, NRT was made to participants through transmucosally-carried nicotine polacrilex (nicotine gum) in an ad lib dose schedule.17 Following the intervention, the participants were again requested to complete the questionnaires during 12 and 29 weeks following the therapy. The exhaled CO and daily cigarette smoking were also evaluated for each patient over following up every three weeks.
Hospital Anxiety and Depression Scale (HADS)
The HADS consists of two subscales: one for experiencing depression and the other for experiencing anxiety.18,19 It is a questionnaire containing a total of 14 items and 4 categories for each. It can be applied for categorizing participants into 3 groups: no anxiety and/or depression (scores between 0 and 7), probable anxiety and/or depression (scores between 8 and 10), and having anxiety and/or depression (scores between 11 and 21).20 There is a slight correlation between the anxiety subscale corresponding to the HADS and both the emotional functions.21
Depression Anxiety Stress Scale (DASS)
The DASS is a 42-item self-report measure for depression, anxiety, and stress.22 It contains three 14-item subscales with every item scored on a 4-point Likert scale, ranging between 0 (never used to me) and 3 (used to me very much or mostly). Total scores are computed through the summation of the items on each subscale, resulting in a score range of 0-42 on every single subscale. Scores more than 20, 14, and 25 revealed the severe levels of depression, anxiety, and stress subscales, respectively.23 The DASS indicates acceptable convergent and discriminant validity and excellent internal consistency and reliability.22
The Beck Depression Inventory-II (BDI-II)
The reliability and concurrent validity corresponding to the BDI-II-Persian were determined in nonclinical participants.24 The BDI is a multiple-choice self-report inventory containing 21 questions that was first improved by Beck25 and Beck et al.26 The optimum BDI
cut-off is 14 for screening.24 Consequently, in current research, a score of 14 was the cut-off point for depression screening.
The Shapiro-Wilk test was utilized for evaluating whether the distribution of data was normal. Descriptive baseline features for comparing three groups were presented as mean and standard deviation (SD), median (inter-quartile range), and their percentages. Three groups were compared and the chi-square test or Fisher’s exact test was used to analyze categorical data statistically. In addition, the Mann-Whitney U test was used to analyze continuous data statistically. The primary efficiency data on smoke quitting were studied through intention-to-treat analysis. The General Linear Model (GLM) results among three groups were compared using repeated measures analysis of variance (ANOVA) test. Time of assessment and intervention state (GSC and NRT) were taken into account as within-subject factor and between-subject factor, respectively. The time groups (interaction term) were taken into account as group differences (amongst three groups) in their response over the time. We examined Mauchly’s Sphericity Test for the assumption of compound normality. Moreover, we applied a Generalized Estimating Equation (GEE) model to approximate the differences of values corresponding to smoking cessation, stress, anxiety, and depression among the three groups and also the time trend following the intervention. A P-value of 0.050 or less was considered as statistically significant. Data were analyzed using SPSS software (version 16, SPSS Inc., Chicago, IL, USA) and Stata software (version 12, Stata Corporation, College Station, TX, USA).
Ethical issues
Mazandaran University of Medical Sciences approved the protocol of the study and informed agreement form (IR.MAZUMS.REC.95.2137). The volunteers qualified for contributing based on the eligibility screening process were requested to fill the consent form. The informed consent form included information about the program, assurance of absolute confidentiality, and that the participants were free to exit the study at any phase during the trial.
Results
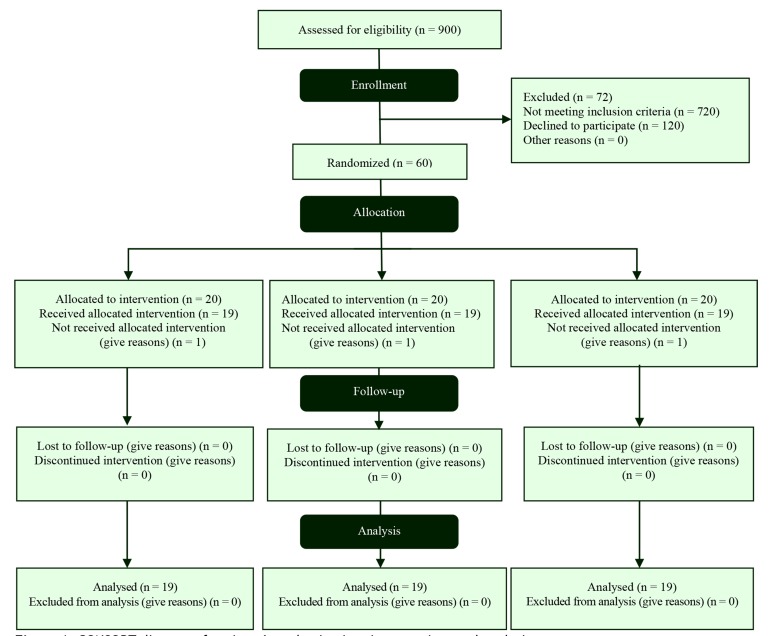
Participants: In the current study, 57 men with 45 to 75 years of age and a mean age of 53.60 ± 8.43 years were randomly assigned to three groups: 19 to the GSC, 19 to the NRT, and 19 to the combined GSC and NRT groups (Figure 1). The mean age of their first smoking was 19.6 years old, ranging from 8 to 34 years. Mean duration of smoking was 32.9 years, with a range of 9-59 years.
Figure 1.
Figure 1. CONSORT diagram of patients’ randomization, intervention, and analysis
Their cigarette consumption per day was 23 cigarettes (with a range of 5-60). The nicotine dependency level of 42.1% of participants was obtained more than 5 through the FTND. All the participants were in the preparation stage of TTM. Self-reported daily smoking decreased gradually during the baseline and 12 and 29 weeks from 23.2 ± 1.7 to 7.6 ± 1.0 and 6.0 ± 1.0 (P = 0.001), respectively. A total of 9 (47.4%) participants in the GSC, 9 (47.4%) participants in combined groups, and 4 (21.1%) participants in the NRT group stated complete abstinence from smoking by the end of 29 weeks. Additionally, the mean exhaled CO reduced from 22.6 ± 1.5 to 12.8 ± 0.9 and 8.6 ± 0.7 ppm (P = 0.001) during the baseline, 12, and 29 weeks, confirming a reduction in smoking. Basic demographic and clinical characteristics of patients in three groups are presented in table 1. As shown in table 1, no significant difference was detected in age (GSC vs. NRT vs. combined group, P = 0.080), marital status (GSC vs. NRT vs. combined group, P = 0.360), and other characteristics (job, motivation of quitting, importance of smoking cessation, smoker friends, craving, FTND, daily cigarette smoking, and other related variables).
Table 1.
Basic demographic and clinical characteristics of patients in three groups
| Variables | Groups |
P | ||||
|---|---|---|---|---|---|---|
| GSC (n = 19) | NRT (n = 19) | Combined (n = 19) | ||||
| Age (year) (mean ± SD) | 53.60 ± 8.43 | 50.00 ± 6.00 | 56.00 ± 10.00 | 54.00 ± 8.00 | 0.08 | |
| Marital status [n (%)] | Married | 15 (30.6) | 16 (32.2) | 18 (36.7) | 0.36 | |
| Single /Divorced/Widow | 4 (50.0) | 3 (37.5) | 1 (12.5) | |||
| Occupation [n (%)] | Self-employee | 14 (38.9) | 11 (30.6) | 11 (30.6) | 0.50 | |
| Employed | 5 (23.8) | 8 (38.1) | 8 (38.1) | |||
| Quitting motivation [n (%)] | Desperate and unwilling | 1 (50.0) | 0 (0) | 1 (50.0) | 0.60 | |
| Hopeful and very hopeful to give up | 18 (32.7) | 19 (34.5) | 18 (32.7) | |||
| Importance of smoking quitting [n (%)] | Trivial and somewhat | 1 (50.0) | 0 (0) | 1 (50.0) | 0.60 | |
| Very much and too much | 18 (32.7) | 19 (34.5) | 18 (32.7) | |||
| Smoker friends [n (%)] | None of them and a bit | 13 (36.1) | 13 (36.1) | 10 (27.8) | 0.50 | |
| Half and the most | 6 (28.6) | 6 (28.6) | 9 (42.9) | |||
| Temptation (mean ± SD) | 22.0 ± 7.7 | 23.0 ± 6.0 | 26.0 ± 8.0 | 0.20 | ||
| HSI (mean ± SD) | 1.8 ± 1.2 | 2.0 ± 1.3 | 1.7 ± 1.0 | 0.74 | ||
| FTND (mean ± SD) | FTND was more than 5 in 42.1% of patients | 4.7 ± 2.1 | 4.9 ± 2.9 | 4.9 ± 2.1 | 0.93 | |
| Daily cigarette (mean ± SD) | 5-60 (mean = 23) cigarettes in a day | 24.0 ± 13 | 26.0 ± 18 | 20.0 ± 7.0 | 0.70 | |
| Substance (opium or alcohol or methadone) use [n (%)] | 8 (17.5) | 10 (19.3) | 8 (17.5) | 0.11 | ||
| History of smoking in father or brother [n (%)] | 10 (17.5) | 15 (26.3) | 13 (22.8) | 0.22 | ||
| Depression (Beck questionnaire) [n (%)] | 14.8 (8.5) | 18.1 (13.7) | 19.7 (10.3) | 0.35 | ||
| Anxiety (HADS) [n (%)] | 10.3 (4.7) | 9.4 (5.6) | 9.4 (6.2) | 0.23 | ||
| Depression (HADS) [n (%)] | 6.7 (3.8) | 8.4 (4.8) | 9.1 (5.5) | 0.80 | ||
| Stress (HADS) [n (%)] | 6.1 (2.5) | 7.2 (3.1) | 7.9 (3.1) | 0.90 | ||
| Anxiety (DASS) [n (%)] | 3.7 (2.8) | 4.3 (2.7) | 5.1 (3.2) | 0.20 | ||
| Depression (DASS) [n (%)] | 3.9 (2.4) | 4.7 (2.9) | 4.9 (2.5) | 0.34 | ||
HSI: Heaviness of smoking index; FTND: Fagerstrom test for nicotine dependence; GSC: Guided self-change; NRT: Nicotine replacement therapy; HADS: Hospital anxiety and depression scale; DASS: Depression anxiety stress scale; SD: Standard deviation
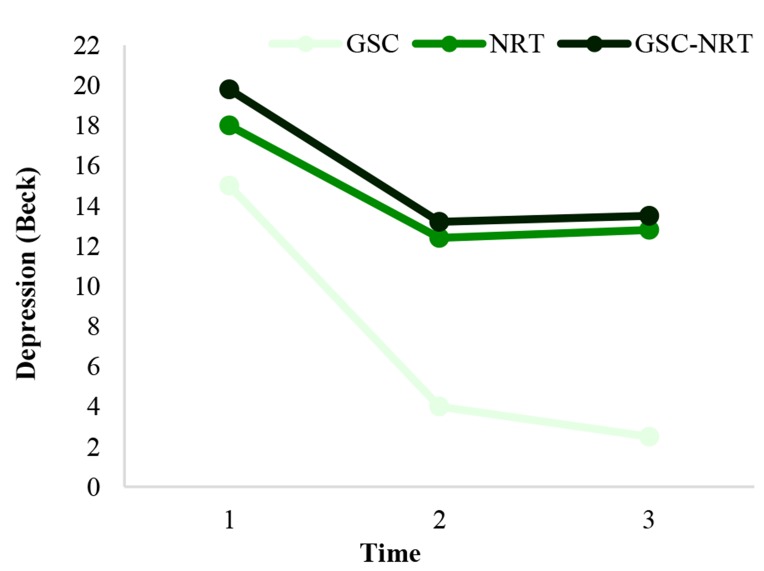
Depression, stress, and anxiety: Depression, stress, and anxiety variables declined significantly and statically in three intervention groups after 29 weeks (Table 2). The level of depression with Beck inventory during 29 weeks in the NRT group was more than that in the GSC group but not significant: [odds ratio (OR) = -3.2, 95% confidence interval (CI): -2.9-9.4, P = 0.300]. Also, the level of this variable in the combined group was more than that in the GSC group and marginally significant: (OR = -0.09, 95% CI: -0.67-9.30, P = 0.090) (Figure 2).
Table 2.
Stress, anxiety, and depression of participants (scores at baseline and time intervals of after intervention in three groups of study)
| Variables | Groups |
F statistic |
|||||
|---|---|---|---|---|---|---|---|
| Baseline (mean ± SD) | Follow up after 12 weeks (mean ± SD) | Follow up after 29 weeks (mean ± SD) | Time | Group | Time * group | ||
| Depression (Beck) | GSC | 14.78 ± 8.44 | 9.36 ± 6.50 | 9.05 ± 6.56 | 75.06** | 1.03 | 0.22 |
| NRT | 18.10 ± 13.71 | 12.26 ± 10.91 | 12.26 ± 10.91 | ||||
| Combination of NRT-GSC | 19.68 ± 10.25 | 13.00 ± 8.30 | 12.89 ± 8.38 | ||||
| Depression (HADS) | GSC | 6.68 ± 3.83 | 4.42 ± 2.61 | 4.10 ± 2.64 | 53.26** | 1.30 | 0.35 |
| NRT | 8.37 ± 4.84 | 5.26 ± 3.56 | 5.10 ± 3.59 | ||||
| Combination of NRT-GSC | 9.05 ± 5.49 | 5.95 ± 3.26 | 5.68 ± 3.01 | ||||
| Stress (HADS) | GSC | 10.26 ± 4.75 | 6.79 ± 3.14 | 3.32 ± 2.29 | 67.93** | 0.04 | 0.45 |
| NRT | 9.37 ± 5.57 | 6.05 ± 3.58 | 4.11 ± 4.43 | ||||
| Combination of NRT-GSC | 9.37 ± 6.19 | 6.79 ± 3.77 | 3.47 ± 2.80 | ||||
| Anxiety (DASS) | GSC | 3.74 ± 2.77 | 1.68 ± 2.14 | 3.16 ± 2.65 | 75.86** | 1.67 | 0.76 |
| NRT | 4.32 ± 2.73 | 2.89 ± 2.28 | 2.84 ± 2.32 | ||||
| Combination of NRT-GSC | 5.11 ± 3.16 | 3.16 ± 2.65 | 3.11 ± 2.70 | ||||
| Stress (DASS) | GSC | 6.05 ± 2.46 | 4.53 ± 2.44 | 4.47 ± 2.46 | 70.48** | 2.47*** | 1.59 |
| NRT | 7.16 ± 3.08 | 4.47 ± 2.39 | 4.43 ± 2.37 | ||||
| Combination of NRT-GSC | 7.95 ± 3.14 | 6.16 ± 2.46 | 6.00 ± 2.54 | ||||
| Depression (DASS) | GSC | 3.95 ± 2.42 | 2.05 ± 1.62 | 2.00 ± 1.67 | 53.86** | 1.75 | 0.37 |
| NRT | 4.68 ± 2.96 | 3.16 ± 2.41 | 3.21 ± 2.37 | ||||
| Combination of NRT-GSC | 4.95 ± 2.64 | 3.37 ± 2.14 | 3.32 ± 2.16 | ||||
Interaction between time and group
Significance level less than 0.010
Significance level less than 0.100
GSC: Guided self-change; NRT: Nicotine replacement therapy; HADS: Hospital anxiety and depression scale; DASS: Depression anxiety stress scale; SD: Standard deviation
Figure 2.
Depression trends over the time (baseline, 12 and 29 weeks after treatment) in groups GSC: Guided self-change; NRT: Nicotine replacement therapy
The level of depression variable with HADS questionnaire in the combined group was more than that of the GSC group and marginally significant: (OR = -1.80, 95% CI: -0.35-4.10, P = 0.090). The level of stress variable with HADS questionnaire in the combined group was more than that in the GSC group and statically significant: (OR = -1.7, 95% CI: -0.15-3.20, P = 0.030).
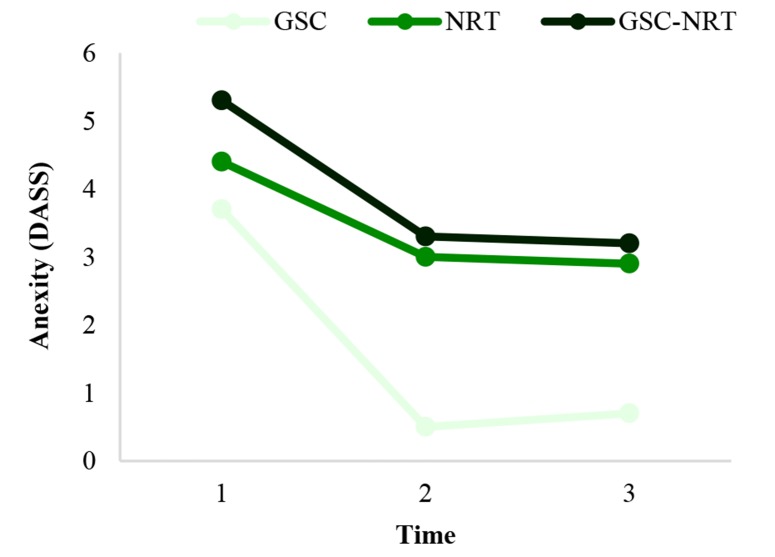
The level of depression variable with DASS questionnaire in the combined group was more than that in the GSC group and marginally significant: (OR = -1.2, 95% CI: -0.05-2.40, P = 0.060). The level of anxiety variable with DASS questionnaire in the combined group was more than that in the GSC group and marginally significant: (OR = -1.4, 95% CI: -0.18-2.90, P = 0.080) (Figure 3).
Figure 3.
Anxiety trends over the time (baseline, 12 and 29 weeks after treatment) in groups GSC: Guided self-change; NRT: Nicotine replacement therapy; DASS: Depression anxiety stress scale
In addition, depression (P = 0.300) and stress (P = 0.500) with HADS and stress (P = 0.200) and depression (P = 0.300) with DASS questionnaires in the NRT group were higher than GSC and combined groups but were not statically significant. As can be noticed, these variables declined significantly and statically in three intervention groups (Table 2).
Relapse after 29 weeks of follow-up: After 29 weeks of follow-up by telephone call, one subject (5.3%) in the NRT group, 4 participants (21.0%) in the combined group, and 2 participants (10.5%) in the GSC group reported relapse. The overall relapse was found in 7 participants (12.0% of the total participants). The daily smoking, however, did not return to the initial level, and the participants continued smoking fewer than the early level. Consequently, the mean daily cigarette smoking in these participants reached 6 cigarettes per day following relapse from 22 cigarettes a day initially.
Discussion
In this study, a 29-week follow-up of GSC and combined treatment in 57 participants resulted in increased smoking abstinence and decreased stress, anxiety, and depression compared with NRT.
Several investigations have been performed on the effectiveness of GSC. In addition, other psychological interventions have been conducted in quitting substances such as smoking of cigarettes. Despite numerous studies conducted in this regard, no investigation was done on GSC in stress, anxiety, and depression of smokers with COPD. To the best of our knowledge, the current research is the first randomized controlled trial that has shown the efficacy of GSC, NRT, and their combination for quitting smoking on stress, anxiety, and depression of smokers with COPD. The most important result of this study is that GSC and combined GSC-NRT treatment were significantly more successful than NRT alone and GSC and GSC-NRT were similarly successful, suggesting the prominent role of GSC in quitting smoking and decreasing stress, anxiety, and depression.
Moreover, the outcomes of the current research are related with earlier studies assessing the efficacy of individual counseling in quitting smoking on stress, anxiety, and depression in Iran and other countries, which is discussed as follows:
Among the reviewed papers, 26 studies evaluated mental health using questionnaires planned for measuring anxiety, depression, mixed anxiety and depression, psychological quality of life, positive impact, and stress in a meta-analysis. Measurement of follow-up mental health scores was performed between 7 weeks and 9 years following the baseline. Anxiety, depression, combined anxiety and depression, and stress significantly reduced between baseline and follow-up in quitters compared with continuing smokers.27 Though smokers with and without mental illnesses believe that smoking provides mental health benefits, they might misunderstand the effect of cigarettes in withdrawal of nicotine as a useful effect on mental health. Smokers with mental disorders feel irritability, anxiety, and depression if they do not smoke for a short time; and these bad feelings disappear by smoking.28 So, they make the notion that smoking has psychological advantages, making them neglect the fact that the first reason for such psychological disorders is smoking. Smoking and depression showed a strong correlation. Depressed smokers interested in cessation may benefit from enhanced psychological support to increase self-confidence, management of mood, and motivation as well as a supportive common social help.29
In a cohort study on 142 participants in a smoking cessation program in Cuiabل, Brazil, to assess changes in the levels of anxiety, depression, motivation, and stress during the course of smoking cessation therapy, participants were evaluated at enrollment evaluation (E1), following 45 days of therapy with medicine and CBT (E2); and at the end of the six-month duration (E3). Amongst the 142 participants, the improvements were observed in terms of the degree of depression, anxiety, motivation, and stress between E1 and E2, and also between E1 and E3. Furthermore, success in treatment was related significantly to the degrees of anxiety and motivation during the study, whereas it was related significantly to the degree of depression only at E2 and E3. It was concluded that smokers changed in terms of the degree of anxiety, depression, motivation, and stress during treatment. Those changes seemed to be more noticeable in participants with successful therapy.30 Changes in the levels of patient anxiety and depression, in our study were considerable as well.
In the study of Bentsen et al. on participants with COPD, all participants reported breathlessness, 28% sleeplessness, 64% anxiety, and 69% depression.31 In a cross-sectional research on 100 participants with COPD, Bentsen et al. reported 31% anxiety, 13% depression, and 45% pain.32 Moreover, in an investigation on 74 participants with COPD, depression was detected in 48.6% of the participants.33 In our study, which was performed on smokers with COPD, we observed a high prevalence of depression.
Though depression severely restricts the efficiency of quitting smoking programs,34,35 in our research, the smoking cessation rate was considerable in three groups. Enhanced system-level changes and insurance coverage for smoking cessation therapy could be applied for the reduction of stress, anxiety, and depression symptoms to all smokers, regardless of COPD status.6
There is no evidence for the concern that quitting smoking would result in smokers’ enhanced risk for mental problems. On contrary, quitting smoking is related to a risk decrease for depression and anxiety.27
It seems that dependency of nicotine exacerbates the stress. Moreover, this is proved in the daily mood patterns explained by smokers, with normal moods during smoking and declining moods between cigarettes. Therefore, the relaxant effect of smoking only reflects the irritability and tension that develop during depletion of nicotine.28 Dependent smokers require nicotine to keep on their normal feeling. The statement that cigarette smoking does not decline stress but actually increases it needs to be more known in the future study.28 Smokers can be motivated for abstinence from smoking by reassuring them that smoking cessation is related to mental health benefits. Moreover, this could defeat barriers that clinicians have in smoking cessation interventions with smokers with mental health disorders.36 Smokers reported significantly more total levels of stress comparing with non-smokers. Post-hoc analyses proposed that scores of depression, anxiety, and anger were more amongst smokers than non-smokers.36
It has been evidenced that adding a management component of psychosocial mood to a standard program of cessation of smoking enhances long-term quitting rates in smokers with both current and previous depression compared with the standard program alone.36
Conclusion
The results of the present study indicate that individual motivational CBT such as GSC with NRT is effective in assisting smokers to quit and in decreasing stress, anxiety, and depression in smokers with COPD. In conclusion, GSC smoking cessation counseling is an effective method for helping patients with COPD to quit and results in decreased stress, anxiety, and depression without NRT. Then, motivational individual counseling is a significant factor associated with smoking cessation results. Reducing tobacco smoking is strongly an essential component of stress, anxiety, and depression reduction for all patients, especially those with COPD.
Acknowledgments
This paper was originated from the first author’s PhD thesis at School of Medicine, Addiction Research Institute, Mazandaran University of Medical Sciences. The authors are grateful to Mazandaran University of Medical Sciences, all the patients who participated in this study, and the assistants and colleagues who kindly collaborated in the conduct of the study.
Footnotes
Conflicts of Interest
The Authors have no conflict of interest.
REFERENCES
- 1.Usmani ZA, Carson KV, Heslop K, Esterman AJ, De Soyza A, Smith BJ. Psychological therapies for the treatment of anxiety disorders in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;3:CD010673. doi: 10.1002/14651858.CD010673.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pommer AM, Pouwer F, Denollet J, Pop VJ. Managing co-morbid depression and anxiety in primary care patients with asthma and/or chronic obstructive pulmonary disease: Study protocol for a randomized controlled trial. Trials. 2012;13:6. doi: 10.1186/1745-6215-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodwin RD, Lavoie KL, Lemeshow AR, Jenkins E, Brown ES, Fedoronko DA. Depression, anxiety, and COPD: The unexamined role of nicotine dependence. Nicotine Tob Res. 2012;14(2):176–83. doi: 10.1093/ntr/ntr165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, et al. Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest. 2008;134(4 Suppl):43S–56S. doi: 10.1378/chest.08-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Covic T, Cumming SR, Pallant JF, Manolios N, Emery P, Conaghan PG, et al. Depression and anxiety in patients with rheumatoid arthritis: Prevalence rates based on a comparison of the Depression, Anxiety and Stress Scale (DASS) and the hospital, Anxiety and Depression Scale (HADS). BMC Psychiatry. 2012;12:6. doi: 10.1186/1471-244X-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schauer GL, Wheaton AG, Malarcher AM, Croft JB. Health-care provider screening and advice for smoking cessation among smokers with and without COPD: 2009-2010 national adult tobacco survey. Chest. 2016;149(3):676–84. doi: 10.1378/chest.14-2965. [DOI] [PubMed] [Google Scholar]
- 7.Gratziou C, Florou A, Ischaki E, Eleftheriou K, Sachlas A, Bersimis S, et al. Smoking cessation effectiveness in smokers with COPD and asthma under real life conditions. Respir Med. 2014;108(4):577–83. doi: 10.1016/j.rmed.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 8.John U, Meyer C, Rumpf HJ, Hapke U. Smoking, nicotine dependence and psychiatric comorbidity-a population-based study including smoking cessation after three years. Drug Alcohol Depend. 2004;76(3):287–95. doi: 10.1016/j.drugalcdep.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Schauer GL, Wheaton AG, Malarcher AM, Croft JB. Smoking prevalence and cessation characteristics among U.S. adults with and without COPD: Findings from the 2011 Behavioral Risk Factor Surveillance System. COPD. 2014;11(6):697–704. doi: 10.3109/15412555.2014.898049. [DOI] [PubMed] [Google Scholar]
- 10.Heydari G, Marashian M, Ebn Ahmady A, Masjedi M, Lando HA. Which form of nicotine replacement therapy is more effective for quitting smoking? A study in Tehran, Islamic Republic of Iran. East Mediterr Health J. 2012;18(10):1005–10. doi: 10.26719/2012.18.10.1005. [DOI] [PubMed] [Google Scholar]
- 11.Tashkin DP. Smoking cessation in chronic obstructive pulmonary disease. Semin Respir Crit Care Med. 2015;36(4):491–507. doi: 10.1055/s-0035-1555610. [DOI] [PubMed] [Google Scholar]
- 12.Sobell MB, Sobell LC. Guided self-change model of treatment for substance use disorders. J Cogn Psychother. 2005;19(3):199–210. [Google Scholar]
- 13.Wilson GT, Zandberg LJ. Cognitive-behavioral guided self-help for eating disorders: Effectiveness and scalability. Clin Psychol Rev. 2012;32(4):343–57. doi: 10.1016/j.cpr.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Camarelles F, Asensio A, Jimenez-Ruiz C, Becerril B, Rodero D, Vidaller O. Effectiveness of a group therapy intervention to quit smoking. Randomized clinical trial. Med Clin (Barc) 2002;119(2):53–7. doi: 10.1016/s0025-7753(02)73312-5. [DOI] [PubMed] [Google Scholar]
- 15.Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N. Decisional balance measure for assessing and predicting smoking status. J Pers Soc Psychol. 1985;48(5):1279–89. doi: 10.1037//0022-3514.48.5.1279. [DOI] [PubMed] [Google Scholar]
- 16.Javors MA, Hatch JP, Lamb RJ. Cut-off levels for breath carbon monoxide as a marker for cigarette smoking. Addiction. 2005;100(2):159–67. doi: 10.1111/j.1360-0443.2004.00957.x. [DOI] [PubMed] [Google Scholar]
- 17.Killen JD, Fortmann SP, Newman B, Varady A. Evaluation of a treatment approach combining nicotine gum with self-guided behavioral treatments for smoking relapse prevention. J Consult Clin Psychol. 1990;58(1):85–92. doi: 10.1037//0022-006x.58.1.85. [DOI] [PubMed] [Google Scholar]
- 18.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 19.Olsson I, Mykletun A, Dahl AA. The Hospital Anxiety and Depression Rating Scale: A cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. 2005;5:46. doi: 10.1186/1471-244X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 21.Parreira VF, Kirkwood RN, Towns M, Aganon I, Barrett L, Darling C, et al. Is there an association between symptoms of anxiety and depression and quality of life in patients with chronic obstructive pulmonary disease? Can Respir J. 2015;22(1):37–41. doi: 10.1155/2015/478528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nilges P, Essau C. Depression, anxiety and stress scales: DASS-A screening procedure not only for pain patients. Schmerz. 2015;29(6):649–57. doi: 10.1007/s00482-015-0019-z. [DOI] [PubMed] [Google Scholar]
- 23.Eslami AA, Rabiei L, Afzali SM, Hamidizadeh S, Masoudi R. The effectiveness of assertiveness training on the levels of stress, anxiety, and depression of high school students. Iran Red Crescent Med J. 2016;18(1):e21096. doi: 10.5812/ircmj.21096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21(4):185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 25.Beck AT. Measuring depression: The depression inventory. In: Williams TA, Katz MM, Shield JA, editors. Recent Advances in the Psychobiology of the Depressive Illnesses: Proceedings of a Workshop. Washington, DC: U.S. National Institute of Mental Health; 1972. pp. 299–302. [Google Scholar]
- 26.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 27.Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: Systematic review and meta-analysis. BMJ. 2014;348:g1151. doi: 10.1136/bmj.g1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parrott AC. Does cigarette smoking cause stress? Am Psychol. 1999;54(10):817–20. doi: 10.1037//0003-066x.54.10.817. [DOI] [PubMed] [Google Scholar]
- 29.Clancy N, Zwar N, Richmond R. Depression, smoking and smoking cessation: A qualitative study. Fam Pract. 2013;30(5):587–92. doi: 10.1093/fampra/cmt032. [DOI] [PubMed] [Google Scholar]
- 30.Brose LS, Simonavicius E, McNeill A. Maintaining abstinence from smoking after a period of enforced abstinence-systematic review, meta-analysis and analysis of behaviour change techniques with a focus on mental health. Psychol Med. 2018;48(4):669–78. doi: 10.1017/S0033291717002021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bentsen SB, Gundersen D, Assmus J, Bringsvor H, Berland A. Multiple symptoms in patients with chronic obstructive pulmonary disease in Norway. Nurs Health Sci. 2013;15(3):292–9. doi: 10.1111/nhs.12031. [DOI] [PubMed] [Google Scholar]
- 32.Bentsen SB, Miaskowski C, Rustoen T. Demographic and clinical characteristics associated with quality of life in patients with chronic obstructive pulmonary disease. Qual Life Res. 2014;23(3):991–8. doi: 10.1007/s11136-013-0515-5. [DOI] [PubMed] [Google Scholar]
- 33.Iguchi A, Senjyu H, Hayashi Y, Kanada R, Iwai S, Honda S, et al. Relationship between depression in patients with COPD and the percent of predicted FEV(1), BODE index, and health-related quality of life. Respir Care. 2013;58(2):334–9. doi: 10.4187/respcare.01844. [DOI] [PubMed] [Google Scholar]
- 34.Cinciripini PM, Wetter DW, Fouladi RT, Blalock JA, Carter BL, Cinciripini LG, et al. The effects of depressed mood on smoking cessation: Mediation by postcessation self-efficacy. J Consult Clin Psychol. 2003;71(2):292–301. doi: 10.1037/0022-006x.71.2.292. [DOI] [PubMed] [Google Scholar]
- 35.Wilson I. Depression in the patient with COPD. Int J Chron Obstruct Pulmon Dis. 2006;1(1):61–4. doi: 10.2147/copd.2006.1.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van der Meer RM, Willemsen MC, Smit F, Cuijpers P. Smoking cessation interventions for smokers with current or past depression. Cochrane Database Syst Rev. 2013;(8):CD006102. doi: 10.1002/14651858.CD006102.pub2. [DOI] [PubMed] [Google Scholar]