Abstract
Background:
Sepsis-3 definitions have been published recently; however, their diagnostic value remains controversial. This study was to assess the accuracy of Sepsis-3 definitions compared to Sepsis-1 definitions by stratifying mortality among adult critically ill patients with suspected infection.
Methods:
A multicenter, prospective cohort study was conducted from November 10, 2017 to October 10, 2018, in five Intensive Care Units (ICUs) at four teaching hospitals. Thirty-day mortality was compared across categories for both Sepsis-3 definitions and Sepsis-1 definitions, which were evaluated by logistic regression analysis followed by measurement of the area under the receiver operating characteristic curve (AUROC) for predicting 30-day mortality rates.
Results:
Of the 749 enrolled patients, 644 (85.9%) were diagnosed with sepsis according to the Sepsis-1 definitions. Among those patients, 362 were diagnosed with septic shock (362/749, 48.3%). However, according to the Sepsis-3 definitions, there were 483 patients with a diagnosis of sepsis (483/749, 64.5%), among whom 299 patients were diagnosed with septic shock (299/749, 39.9%). According to the Sepsis-3 definitions, sepsis (sepsis and septic shock) patients had higher 30-day mortality (41.8%) than sepsis patients according to the Sepsis-1 definitions (31.8%, χ2 = 5.552, P = 0.020). The AUROC of systemic inflammatory response syndrome (SIRS) and quick sequential organ failure assessment (qSOFA) scores with regard to 30-day mortality rates were 0.609 (0.566–0.652) and 0.694 (0.654–0.733), respectively. However, the AUROC of SOFA scores (0.828 [0.795–0.862]) were significantly higher than that of SIRS or qSOFA scores (P < 0.001).
Conclusion:
In adult critically ill patients with suspected infection, the Sepsis-3 definitions were relatively accurate in stratifying mortality and were superior to the Sepsis-1 definitions.
Trial Registration:
www.chictr.org.cn (ChiCTR-OOC-17013223).
Keywords: Infection, Critically ill patients, Sepsis-3, Septic shock, Mortality
Introduction
In 1991, the American College of Chest Physicians and Society of Critical Care Medicine convened with the goal of developing a set of sepsis definitions to standardize the definition of sepsis and its spectrum of diseases, including septic shock.[1] The consensus defined sepsis as systemic inflammatory response syndrome (SIRS) resulting from an infection. Septic shock was defined as sepsis-induced hypotension persisting after adequate fluid resuscitation, along with the presence of perfusion abnormalities or organ dysfunction. At the second consensus conference,[2] although some specialists agreed that SIRS was not suitable for the definition of sepsis, the were no significant changes made to the definitions of sepsis.
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) were published recently, with significantly revised clinical criteria, adopting sequential organ failure assessment (SOFA) scores and the quick SOFA (qSOFA) screening tool.[3] Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. The definition of septic shock is clinically identified by the vasopressor requirement to maintain a mean arterial pressure (MAP) of more than 65 mmHg and a serum lactate level of more than 2 mmol/L after initial fluid resuscitation.[4]
Although these new criteria have been validated in large databases, their diagnostic value remains controversial.[5] Some retrospective studies have indicated that the new Sepsis-3 definitions were accurate in stratifying mortality and were superior to the previous definitions.[6,7] However, Sterling[8] suggested that although Sepsis-3 identified a group of patients at greater risk of worse clinical outcomes, it missed a large proportion of patients who may benefit from early resuscitative therapy.
To assess the ability of the Sepsis-1 and Sepsis-3 definitions to predict the primary endpoint, we conducted the present multicenter, prospective cohort study to evaluate the Sepsis-3 definitions and the Sepsis-1 definitions by logistic regression analysis followed by measurement of the area under the receiver operating characteristic curve (AUROC) for predicting 30-day mortality rates.
Methods
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of Northern Jiangsu People's Hospital (2017KY-021) and was registered in the Chinese Clinical Trial Registry with a registration number ChiCTR-OOC-17013223. Written informed consent was obtained from each participant/guardian prior to their enrollment in this study.
Study design and population
The present study was conducted at five Intensive Care Units (ICUs) with more than 180 beds in a total of four Jiangsu province teaching hospitals. This was a prospective cohort study of adult patients with suspected infection admitted to ICUs over an approximate 1-year span from November 10, 2017 to October 10, 2018, in ICUs of four teaching hospitals containing Northern Jiangsu People's Hospital, Jiangdu People's Hospital of Yangzhou, Affiliated Hospital of Yangzhou University, and Taizhou People's Hospital. The patients, who were less than 18 years of age or having any of the following primary conditions: trauma, epilepsy, cardiogenic pulmonary edema, stroke, or active bleeding, were excluded.
Definition of suspicion of infection
Suspicion of infection was defined as clinical documentation of this suspicion based on clinical presentation and radiological or laboratory examination by the attending physician on the first day of ICU admission with the subsequent administration of antimicrobials. This approach was carried out by following the definition of suspicion of infection used by Finkelsztein and colleagues.[9]
Sepsis-3 definitions
The Sepsis-3 categories are defined as follows [3,4]: Sepsis is identified as an acute change in the total SOFA score ≥2 points that is a result of the infection. The baseline SOFA score is assumed to be 0 in patients not known to have preexisting organ dysfunction.
Septic shock is identified with a clinical construct of sepsis if the patient has persistent hypotension that requires vasopressors to maintain a MAP >65 mmHg and if they have a serum lactate level >2 mmol/L despite adequate fluid resuscitation.
Sepsis-1 definitions
The Sepsis-1 categories (sepsis and septic shock) were defined according to previously published consensus.[1] Sepsis was identified with documented or as suspected infection and ≥2 signs of SIRS. Septic shock was defined as suspected infection, ≥2 SIRS signs and persistent hypotension that required vasopressors to maintain a MAP >65 mmHg despite adequate fluid resuscitation.
Assessment of qSOFA and SIRS
Patients with suspected infection were identified with the qSOFA score, including alterations in mental status, systolic blood pressure ≤100 mmHg, or a respiratory rate ≥22 breaths/min.
SIRS was identified with ≥2 of the following four signs: temperature >38°C or <36°C, heart rate >90 beats/min, respiratory rate >20 breaths/min, and white blood cell count >12,000/mm3 or <4000/mm3 or >10% immature forms. As proposed by Bone et al,[1] one point was awarded for each of the four conditions, and the score ranged from 0 to 4.
Data Collection
To ensure data validity and reliability, two data collectors were supported by a continuous online webchat. We provided important study information through emails and online training, including the protocol, answers to questions and a description of the electronic case report form (eCRF) on the electronic tablets. We collected data from medical and nursing records, including age; gender; worst and best vital signs during the first ICU day; Acute Physiology and Chronic Health Evaluation (APACHE) II score; first day total SOFA score; etiological diagnosis; Infection source; ICU length of stay (LOS); organ support measures; and initial lactate level on the first day. Laboratory variables were retrieved from the electronic health database. Patient visits were performed 30 days after enrollment through telephone interviews. The primary end point was all-cause 30-day mortality.
Statistical analysis
Continuous variables are presented as the mean ± standard deviation (SD), and compared using independent sample t-test. Differences in proportions were compared using Chi-square test or Fisher exact test. We evaluated Sepsis-3 definitions and Sepsis-1 definitions by logistic regression analysis followed by measurement of the AUROC for predicting 30-day mortality rates. AUROCs were compared using DeLong test. All statistical analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). A P < 0.05 (two-tailed) was considered as statistically significant.
Results
Characteristics
Of the 993 ICU patients with suspected infection during the study period, 244 patients were excluded. The remaining 749 patients were enrolled in the study [Figure 1]. The mean age of these 749 patients was 63.4 ± 12.3 years; 74.8% were male, and the mean APACHE II score was 21.4 ± 8.2. The most common infection was respiratory infections (429/749, 55.8%), followed by urinary tract infections (167/749, 20.9%) and abdominal infections (69/749, 8.7%; Table 1).
Figure 1.
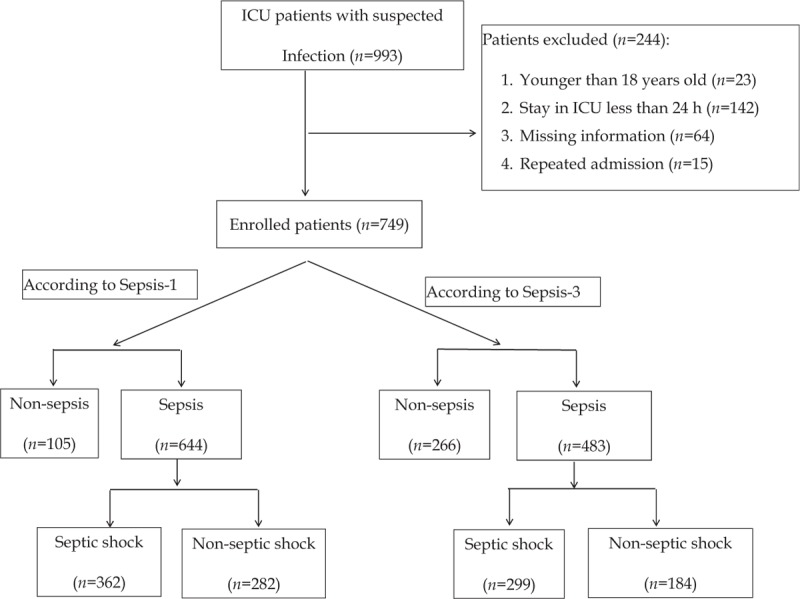
Flowchart of enrollment in the study. ICU: Intensive care unit.
Table 1.
General characteristics, support measures and outcomes of patients meeting different definitions.
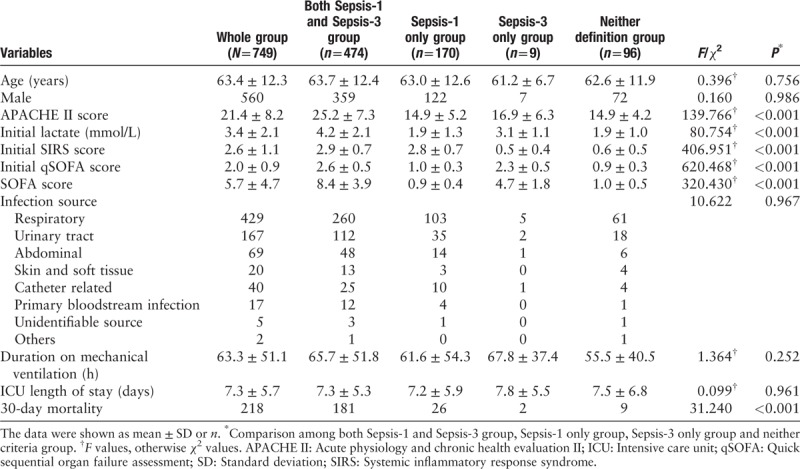
According to the Sepsis-1 definitions, there were 644 patients diagnosed with sepsis (644/749, 85.9%), among whom 362 patients were diagnosed with septic shock (362/749, 48.3%). According to the Sepsis-3 definitions, there were 483 patients diagnosed with sepsis (483/749, 64.5%), among whom 299 patients were diagnosed with septic shock (299/749, 39.9%) [Figure 1]. Among the 749 patients enrolled in the study, 170 (22.6%) patients only met the Sepsis-1 definitions, while nine (1.2%) patients only met the Sepsis-3 definitions. A total of 474 (63.3%) patients met both definitions. The remaining 96 (12.8%) met neither definitions. The APACHE II and SOFA scores were significantly higher in patients who met both sets of criteria than those in the other groups [Table 1].
Mortality
Of the 749 enrolled patients, the total 30-day mortality rate was 29.1% [Table 1]. The mortality of patients who met both definitions (38.2%) was significantly higher than those of patients who met Sepsis-1 definitions alone (15.3%, χ2 = 16.919, P < 0.010) or who met neither criteria (9.3%, χ2 = 17.537, P < 0.010) [Table 1]. The Sepsis-1 definitions and Sepsis-3 definitions showed significant differences in 30-day mortality among the three categories (non-sepsis, sepsis, and septic shock; all P < 0.001) [Figure 2]. Additionally, according to the Sepsis-3 definitions, sepsis (sepsis and septic shock) patients had higher 30-day mortality (41.8%) than sepsis patients according to the Sepsis-1 definitions (31.8%, χ2 = 5.552, P = 0.020).
Figure 2.
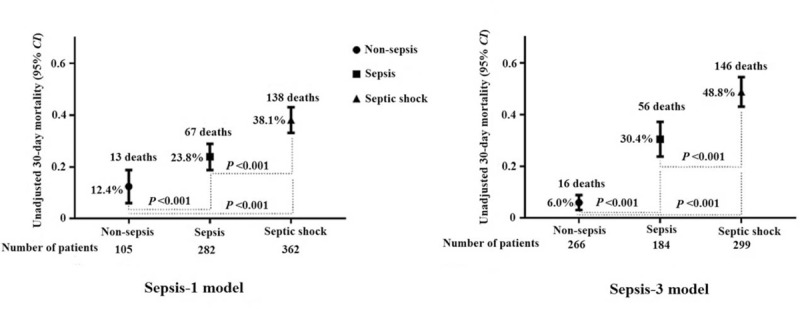
Thirty-day mortality stratified according to the Sepsis-1 and Sepsis-3 definitions (P < 0.001, among the three categories).
Logistic regression analysis
The patients were divided into survival group (n = 531) and non-survival group (n = 218) depending on outcome. Many demographic and other variables were collected from the patient medical records. The single variable analysis showed that there were significant differences in APACHE II score, qSOFA score, SOFA score, SIRS score, initial serum lactate level and the percentage of sepsis or septic shock patients between the two groups (P < 0.05) [Table 2]. Table 3 shows the associations of sepsis definitions with the 30-day mortality in the binary logistic regression, indicating that sepsis (odd ratio [OR]: 2.205, 95% confidence interval [CI]: 1.160–4.192, P < 0.001; and OR: 7.321, 95% CI, 3.985–13.450, P < 0.001) and septic shock (OR: 1.997, 95% CI: 1.398–2.796, P < 0.001; and OR: 2.211; 95% CI: 1.501–3.256, P < 0.001) diagnosed according to the Sepsis-1 or Sepsis-3 definitions were two independent risk factors for the 30-day mortality.
Table 2.
General characteristics and support measures of patients according to outcome.
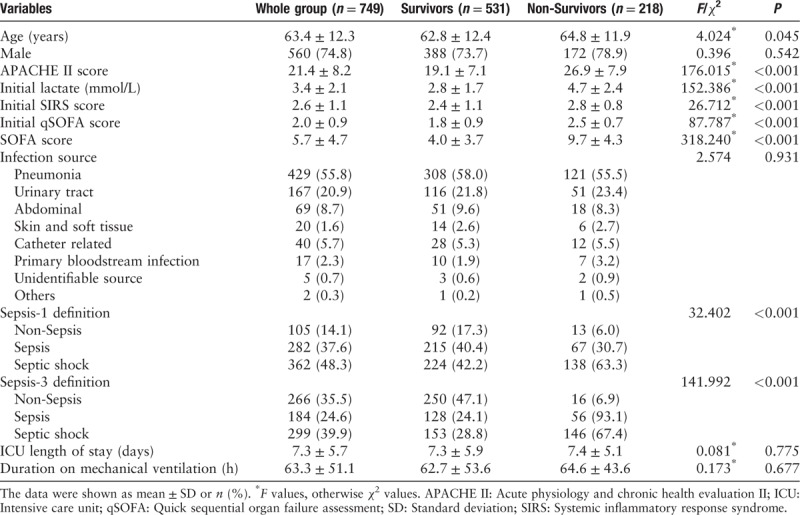
Table 3.
Multivariate regression models using 30-day mortality as a dependent variable.
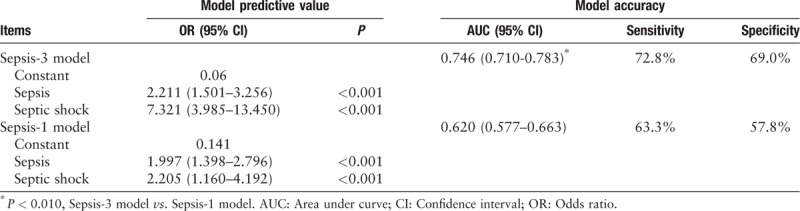
Sensitivity analyses
There is no gold standard for sepsis diagnosis. Therefore, this study evaluated the performance of Sepsis-1 and Sepsis-3 definitions in predicting the 30-day mortality using ROC curves. The AUROC of the Sepsis-3 model with regard to the 30-day mortality rates was 0.746 (0.710–0.783). However, the AUROC of the Sepsis-1 model (0.620 [0.577–0.663]) was significantly lower than that of the Sepsis-3 model (0.746 [0.710–0.783], P < 0.01; Table 3). Additionally, the sensitivity (72.8%) and the specificity (69.0%) of the Sepsis-3 model with respect to the 30-day mortality were higher than those of the Sepsis-1 model (63.3% and 57.8%, respectively).
We also evaluated the performance of SIRS, qSOFA, and SOFA in predicting the 30-day mortality using ROC curves. The results showed that the AUROC of SIRS and qSOFA with regard to the 30-day mortality were 0.609 (0.566–0.652) and 0.694 (0.654–0.733), respectively. However, the AUROC of SOFA (0.828 [0.795–0.862]) was significantly higher than that of SIRS (0.609 [0.566–0.652]) or qSOFA (0.694 [0.654–0.733]; all P < 0.001) [Figure 3].
Figure 3.
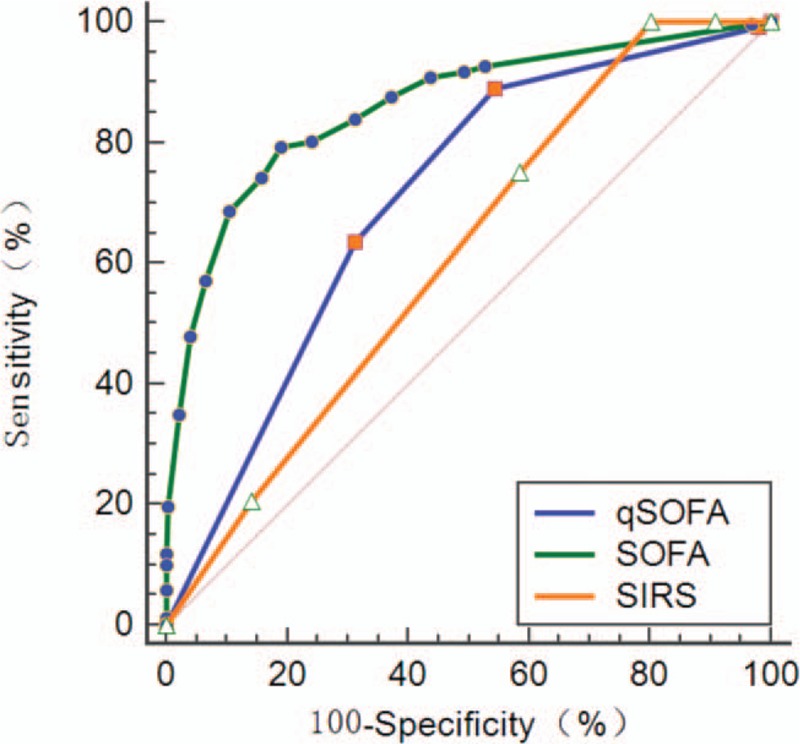
Receiver operating characteristic curves of SIRS, qSOFA, and SOFA scores for predicting the 30-day mortality of patients with suspected infection. The AUROC of SOFA scores (0.828 [0.795–0.862]) was significantly higher than that of SIRS (0.609 [0.566–0.652]) or qSOFA scores (0.694 [0.654–0.733]; all P < 0.001). AUROC: Area under the receiver operating characteristic curve; qSOFA: Quick sequential organ failure assessment; SOFA: Sequential organ failure assessment; SIRS: Systemic inflammatory response syndrome.
Discussion
In the present study, we demonstrated that the Sepsis-3 definition was better than the Sepsis-1 definition at stratifying mortality among adult critically ill patients with suspected infection. Logistic regression showed that sepsis and septic shock were two independent risk factors for the 30-day mortality. According to the Sepsis-3 definition, the 30-day mortality was higher in septic shock patients than that according to the Sepsis-1 definition. Furthermore, the AUROC of the Sepsis-3 model was significantly higher than that of the Sepsis-1 model when used to predict 30-day mortality in patients with suspected infection.
A higher specificity and a better distinction between sepsis and non-sepsis have always been demanded in the past.[10] In the present study, 85.9% of the patients with suspected infections admitted to the ICUs met the Sepsis-1 definition. A total of 22.6% of the patients were diagnosed with sepsis according to the Sepsis-1 definition but were excluded according to the Sepsis-3 definition, which differed from a previous study.[15] The main probable reason was that the patients included in this study were different from those in the previous study. All patients in this study were admitted to the ICU, while only 37.5% of patients in the study of Cheng et al[15] were admitted to the ICU. Furthermore, according to the Sepsis-3 definition, 64.5% of the suspected infection patients were diagnosed with sepsis. Thus, relative to the results with the Sepsis-1 definitions, fewer patients with suspected infection were classified as having sepsis according to the Sepsis-3 definitions. Additionally, this study indicated that sepsis patients as defined by the Sepsis-3 definitions had a higher mortality rate. Therefore, the findings supported the use of the Sepsis-3 definition to identify critically ill patients with suspected infection who are at high risk of death.
In the validation of clinical criteria for sepsis, the Sepsis-3 definition for identifying sepsis patients has been extensively questioned since its publication.[5,11–13] Retrospective cohort studies showed a better discriminative performance of the Sepsis-3 definition in predicting mortality compared to the Sepsis-1 or Sepsis-2 criteria.[6,14–15] In this multicenter, prospective cohort study, we further evaluated the Sepsis-3 and Sepsis-1 definitions by logistic regression analysis followed by measurement of the AUROC for predicting 30-day mortality rates. The AUROC of the Sepsis-3 model was significantly higher than that of the Sepsis-1 model when used to predict 30-day mortality rates in patients with suspected infection. Furthermore, the sensitivity and specificity of the Sepsis-3 model for predicting the 30-day mortality were relatively low (72.8% and 69.0%, respectively) but were higher than those of the Sepsis-1 model (63.3% and 57.8%, respectively). Therefore, the Sepsis-3 definition was more accurate in stratifying mortality and superior to the Sepsis-1 definition in adult critically ill patients with suspected infection.
The Sepsis-3 definition summarizes two conditions: sepsis and septic shock.[16–17] The additional request for a lactate level of ≥ 2 mmol/L in the septic shock definition enables the identification of a high-risk group.[18] The present study suggested that, by applying the Sepsis-3 definition, the proportion of septic shock decreased 8.4%, with a 9% mortality increase compared to the Sepsis-1 definitions. The Sepsis-3 definitions identified sepsis and septic shock patients as having higher mortality, while the non-sepsis patients had lower mortality compared to the Sepsis-1 definition. Thus, the critically serious patients were identified by the new definition. This also suggested that Sepsis-3 definition was better than Sepsis-1 definition at stratifying mortality among septic patients admitted to the ICU.
Previous studies indicated that the number of SIRS criteria present could not be used to stratify the severity of illness.[9–10,19–20] The Sepsis-3 definition exclude the concept of SIRS since this term is no longer considered useful.[21–22] The SOFA and qSOFA scores have been used as two diagnostic tools to identify sepsis with the Sepsis-3 definition.[3–4] We further evaluated the performance of SIRS and qSOFA and SOFA scores using an ROC curve to predict the 30-day mortality. The AUROC of SIRS and qSOFA scores with regard to 30-day mortality rates were 0.609 (0.566–0.652) and 0.694 (0.654–0.733), respectively. However, the AUROC of SOFA scores (0.828 [0.795–0.862]) was significantly higher than that of SIRS or qSOFA scores. This meant that the SOFA score was an excellent tool and superior to SIRS or the qSOFA score for predicting mortality in critically ill patients with suspected infection.
The present study had strength and some limitations. The strength was that the size of the cohort was relatively large. Our study had several limitations. First, we followed our patients for only 30 days and did not collect data beyond that point. Long-term survival rates will be explored in the future. Second, we evaluated only patients admitted to the ICU; thus, our findings could not be generalized to patients treated in regular wards and in the emergency room. Third, the validity of the Sepsis-3 definition in this study was assessed based on the 30-day mortality. Although the 30-day mortality is widely used, the 28-day mortality and ICU mortality were used as endpoints in some studies, possibly causing deviations in results among studies.[14–15,23–25]
In conclusion, this study showed that the new clinical criteria of sepsis proposed in the Sepsis-3 definitions predicted the 30-day mortality in adult critically ill patients with suspected infection. The Sepsis-3 definition was relatively accurate and superior to the Sepsis-1 definition in stratifying mortality. Our findings supported the translation of the Sepsis-3 definitions into sepsis definitions in adult critically ill patients with suspected infection.
Funding
This study was supported by grants from Social Development Funds of Jiangsu Province (No. BE2017691), National Natural Science Foundations of China (No. 81670065), and Social Development Funds of Yangzhou City (No. YZ2017086).
Conflicts of interest
None.
Footnotes
How to cite this article: Chen QH, Shao J, Liu WL, Wang HL, Liu L, Gu XH, Zheng RQ. Predictive accuracy of Sepsis-3 definitions for mortality among adult critically ill patients with suspected infection. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000166
Qi-Hong Chen and Jun Shao contributed equally to this work.
References
- 1.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101:1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 2.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med 2003; 29:530–538. doi: 10.1007/s00134-003-1662-x. [DOI] [PubMed] [Google Scholar]
- 3.Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: for the third international consensus defiitions for sepsis and septic Shock (sepsis-3). JAMA 2016; 315:762–777. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Sepsis Definitions Task Force. Developing a new defiition and assessing new clinical criteria for septic shock: for the third international consensus defiitions for sepsis and septic shock (sepsis-3). JAMA 2016; 315:775–787. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deutschman CS. Imprecise medicine: the limitations of Sepsis-3. Crit Care Med 2016; 44:857–858. doi: 10.1097/CCM.0000000000001834. [DOI] [PubMed] [Google Scholar]
- 6.Donnelly JP, Safford MM, Shapiro NI, Baddley JW, Wang HE. Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) Classification: a retrospective population-based cohort study. Lancet Infect Dis 2017; 17:661–670. doi: 10.1016/S1473-3099(17)30117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szakmany T, Pugh R, Kopczynska M, Lundin RM, Sharif B, Morgan P, et al. Defining sepsis on the wards: results of a multi-centre point-prevalence study comparing two sepsis definitions. Anaesthesia 2018; 73:195–204. doi: 10.1111/anae.14062. [DOI] [PubMed] [Google Scholar]
- 8.Sterling SA, Puskarich MA, Glass AF, Guirgis F, Jones AE. The Impact of the Sepsis-3 septic shock definition on previously defined septic shock patients. Crit Care Med 2017; 45:1436–1442. doi:10.1097/CCM.0000000000002512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finkelsztein EJ, Jones DS, Ma KC, Pabón MA, Delgado T, Nakahira K, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care 2017; 21:73–82. doi: 10.1186/s13054-017-1658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serafim R, Gomes JA, Salluh J, Póvoa P. A Comparison of the Quick-SOFA and systemic inflammatory response syndrome criteria for the diagnosis of sepsis and prediction of mortality: a systematic review and meta-analysis. Chest 2018; 153:646–655. doi: 10.1016/j.chest.2017.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Scheer CS, Kuhn SO, Rehberg S. Sepsis-3 is a positive evolution in discrimination between septic and nonseptic patients as well as sepsis entities, not a step backward. Crit Care Med 2018; 46:e273.doi: 10.1097/CCM.0000000000002866. [DOI] [PubMed] [Google Scholar]
- 12.Schlapbach L, Straney L, Bellomo R, MacLaren G, Pilcher D. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Med 2018; 44:179–188. doi: 10.1007/s00134-017-5021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shankar-Hari M, Harrison DA, Rubenfeld GD, Rowan K. Epidemiology of sepsis and septic shock in critical care units: comparison between sepsis-2 and sepsis-3 populations using a national critical care database. Br J Anaesth 2017; 119:626–636. doi: 10.1093/bja/aex234. [DOI] [PubMed] [Google Scholar]
- 14.Besen BAMP, Romano TG, Nassar AP, Jr, Taniguchi LU, Azevedo LCP, Mendes PV, et al. Sepsis-3 definitions predict ICU mortality in a low-middle-income country. Ann Intensive Care 2016; 6:107–116. doi: 10.1186/s13613-016-0204-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng B, Li Z, Wang J, Xie G, Xie G, Liu X, et al. Comparison of the performance between Sepsis-1 and Sepsis-3 in ICUs in China: a retrospective multicenter study. Shock 2017; 48:301–306. doi: 10.1097/SHK.0000000000000868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hotchkiss RS, Moldawer LL, Opal SM, Reinhart K, Turnbull IR, Vincent JL. Sepsis and septic shock. Nat Rev Dis Primers 2016; 2:16045.doi: 10.1038/nrdp.2016.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marik PE, Linde-Zwirble WT, Bittner EA, Sahatjian J, Hansell D. Fluid administration in severe sepsis and septic shock, patterns and outcomes: an analysis of a large national database. Intensive Care Med 2017; 43:625–632. doi: 10.1007/s00134-016-4675-y. [DOI] [PubMed] [Google Scholar]
- 18.Ranzani OT, Prina E, Menéndez R, Ceccato A, Cilloniz C, Méndez R, et al. New Sepsis Definition (Sepsis-3) and community-acquired pneumonia mortality. a validation and clinical decision-making study. Am J Respir Crit Care Med 2017; 196:1287–1297. doi: 10.1164/rccm.201611-2262OC. [DOI] [PubMed] [Google Scholar]
- 19.Costa RT, Nassar AP, Jr, Caruso P. Accuracy of SOFA, qSOFA, and SIRS scores for mortality in cancer patients admitted to an intensive care unit with suspected infection. J Crit Care 2018; 45:52–57. doi: 10.1016/j.jcrc.2017.12.024. [DOI] [PubMed] [Google Scholar]
- 20.Wu S, Zhou X, Ye Y. Goodbye to the SIRS, the reason why we do not need you. Am J Emerg Med 2018; 36:1317–1318. doi: 10.1016/j.ajem.2017.11.044. [DOI] [PubMed] [Google Scholar]
- 21.Solligård E, Damås JK. SOFA criteria predict infection-related in-hospital mortality in ICU patients better than SIRS criteria and the qSOFA score. Evid Based Med 2017; 22:211.doi: 10.1136/ebmed-2017-110727. [DOI] [PubMed] [Google Scholar]
- 22.Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA 2017; 317:290–300. doi: 10.1001/jama.2016.20328. [DOI] [PubMed] [Google Scholar]
- 23.Williams JM, Greenslade JH, McKenzie JV, Chu K, Brown AFT, Lipman J. Systemic inflammatory response syndrome, quick sequential organ function assessment, and organ dysfunction: insights from a prospective database of ED patients with infection. Chest 2017; 151:586–596. doi: 10.1016/j.chest.2016.10.057. [DOI] [PubMed] [Google Scholar]
- 24.Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, et al. french society of emergency medicine collaborators group, prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA 2017; 317:301–308. doi: 10.1001/jama.2016.20329. [DOI] [PubMed] [Google Scholar]
- 25.Khwannimit B, Bhurayanontachai R, Vattanavanit V. Comparison of the performance of SOFA, qSOFA and SIRS for predicting mortality and organ failure among sepsis patients admitted to the intensive care unit in a middle-income country. J Crit Care 2018; 44:156–160. doi: 10.1016/j.jcrc.2017.10.023. [DOI] [PubMed] [Google Scholar]


