Abstract
Background
Blood purification (BP) is one of the most important rescue measures for patients with critical illness in the intensive care unit (ICU), especially for those with acute kidney injury. The purpose of this nationwide survey was to reveal the real world of current BP practice in different ICUs all over China. This study was designed to be a multi-center cross-sectional study.
Methods
All adult patients (over 18 years of age), who were admitted to ICU and required BP in 35 sub-centers across China were included during 30-day survey period in 2018. Demographic characteristics and clinical data were recorded including the timing of treatment initiation, indications, modality, relative contraindication, establishment of vascular access, selection of filter/membrane, settings, anti-coagulation, executive department, complication, intake, and output.
Discussion
This nationwide survey may contribute to reveal the real world of current BP practice in different ICUs all over China.
Trial registration
Chinese Clinical Trial Registry, ChiCTR-EOC-17013119; http://www.chictr.org.cn/showproj.aspx?proj=22487.
Keywords: Blood purification, Acute kidney injury, Intensive care unit, Adult, China
Introduction
In intensive care unit (ICU), acute kidney injury (AKI) as a “silent killer,”[1] was a common and well-recognized complication of critical illnesses[2] and an independent increased risk factor for mortality, which had an expanding incidence year by year dramatically.[1,3–5] Although insight into the causes and pathogenesis of AKI is growing, the mortality associated with AKI remains high,[5–7] and has become a huge medical burden in China[8] as well as in the world.[5,9,10] No effective drug was available for the treatment of AKI in clinical practice, thus prevention may be the key to avoid the adverse events of AKI.[11] Approximately, 20% of patients with AKI required blood purification (BP),[12] and this demand continued to grow.[13] The purpose of BP had evolved from a single replacement of kidney function to multiple organ support therapy, which treated critically ill patients as a whole.
Apart from AKI, BP had been widely utilized for many non-AKI critical illnesses, including septic shock,[14] acute respiratory distress syndrome,[15] heart failure and cardiorenal syndrome,[16] pulmonary edema and fluid overload, drug and food poisonings,[17,18] acute pancreatitis,[19] liver failure,[20] rhabdomyolysis syndrome, life-threatening acid-base and ion disturbances,[21] and etc, which had obtained considerable clinical outcomes.
Therefore, it is obvious that BP was an important therapeutic weapon for clinicians during the treatment and rescue of patients with critical illness. However, there existed a great amount of disparity in clinical practice. Recommendations, in the relevant guidelines and consensus, were absent up to now, which further exacerbated the clinical confusion.
Although in the past decades, great progress in BP technology development and clinical practice had been achieved, many aspects of BP were still in controversial and only a few studies had formally followed with interest these aspects to date, for example the optimal timing of initiation of renal replacement therapy (RRT),[22–25] anti-coagulation,[26] and RRT dose,[27] which led to wide and huge variations in different ICUs all over the world. It was urgent to draft China standardized treatment guideline of BP in the near future in order to improve and standardize clinical practice, which would contribute to ameliorating the prognosis of patients with critical illness. However, as an initial step to achieve this goal, it was very important for us to entirely reveal and know well the current BP practical situation in different ICUs all over China. Thus, a multi-center cross-sectional survey on BP of ICU adult patients in China was warranted to resolve this issue. The key purpose of this nationwide survey is to reflect the real world of current BP practice in different ICUs all over China in order to lay the foundation for drafting China standardized treatment guideline of BP in the near future.
Methods
Study designs
A total of 35 sub-centers across the country (seen in http://www.chictr.org.cn/showproj.aspx?proj=22487), from Tier 1, 2, and 3 cities, were included in this multi-center cross-sectional survey. These sub-centers are located in 23 provinces, four municipalities, and five autonomous regions. Owing to the special population distribution and regional differences of Beijing, Shanghai, and Guangzhou, each one would recruit two tertiary grade A hospitals in this survey. The survey period is 30 days. All the physicians had been professionally trained before the study. Demographic characteristics and clinical data of enrolled patients will be collected in 35 sub-centers, including the timing of treatment initiation, indications, modality, relative contraindication, establishment of vascular access, selection of filter/membrane, settings, anti-coagulation, executive department, complication, intake and output, etc, and further collated and analyzed statistically. Acute Physiology and Chronic Health Evaluation II score, Sequential Organ Failure Assessment scores, and Glasgow Coma Scale score would be obtained by patient medical records review. The patients’ related personal information was confidential. The nationwide survey had been finished in 2019.
Ethics and dissemination
This study would be carried out in accordance with ethical principles of the Declaration of Helsinki (49th General Assembly of the World Medical Association), and survey protocol was reviewed and approved by the Ethics Committee of the Cancer Hospital of Harbin Medical University (No. KY2017-22). The final results of this survey will be disseminated through articles and national and international conference. The findings of this study will be conductive to reflect the real world of current BP practice in different ICUs all over China and further improve and standardize the clinical practice. Therefore, this survey will contribute to laying the foundation for drafting China standardized treatment guideline of BP in the near future.
Study participants
Written informed consent was achieved from each eligible adult participant or their legally authorized representative before their enrollment in this study. All patients in this survey could withdraw at any time, which would be counted and analyzed.
Inclusion criteria included: (1) ICU admission; (2) patients aged ≥18 years; (3) patients need BP. During the 30-day study period, the patients, who had repeatedly admitted to ICU, needed to be re-enrolled again.
There was no standard for exclusion in this survey. Certainly, patients without written informed consent or complete medical records should be excluded.
Sample size calculation
It was expected that at least 369 subjects would be enrolled in this survey. The sample size was calculated based on the following formula.
Infinite population sample formula: 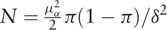 , in which,
, in which,  ; π(population rate) = 0.02; δ (allowable error) = 0.01. So, the sample size
; π(population rate) = 0.02; δ (allowable error) = 0.01. So, the sample size 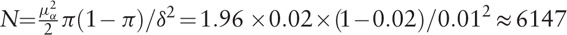 .
.
According to the latest reports,[5] of total 6147 patients, about 1229 cases (20%) were expected to develop into AKI. In patients with AKI, about 184 cases (15%) had indications for RRT.[28] Since BP was a series of clinical treatments including RRT, 369 cases, doubled on the previous basis, were expected to be enrolled in this survey ultimately.
Statistical analysis
SPSS 22.0 (SPSS Inc., Chicago, IL, USA) and SAS 9.1 (SAS Institute, Cary, NC, USA) softwares would be used for statistical analysis. Quantitative data would be shown as mean ± standard deviations for normally distributed data, while median (quantile) for non-normally distributed data. Qualitative data are shown as percentages. The Student's t test or Mann-Whitney U test would be used to compare quantitative data between groups, while the Chi-squared test would be used to compare qualitative data between groups. A P < 0.05 would be set to indicate statistical significance.
Discussion
BP is a generic name, which included a variety of BP technology in clinical practice, for example, intermittent hemodialysis (IHD), hemofiltration, hemodiafiltration, hemoperfusion, plasmapheresis, immune adsorption, and even peritoneal dialysis. BP was described as a process, during which the patient's blood was drawn out of the body and removed some pathogenic substances in order to achieve the purpose of BP and treat critical illnesses through a kind of BP device. Its working principle included diffusion, convection, and adsorption. Certainly, different clinical treatment modalities focused on different working principles and thus were suitable for different patients in clinical practice. For example, the working principle of IHD was mainly based on diffusion, while continuous RRT and hemoperfusion were dominated by convection and adsorption, respectively. The role of BP was non-selective in removing specific mediators.
In 1977, continuous arteriovenous hemofiltration was first applied to patients with AKI who was not suitable for peritoneal dialysis and hemodialysis.[29] This opened the door of ICUs to a flourishing evolution on BP technology in subsequent years. Although the benefits gained in this way were obvious, the morbidity associated with arterial cannulation was considerable. Along with the invention and application of double-lumen central venous catheter, continuous venovenous hemofiltration gradually occupied the mainstream of RRT in ICU because of its improved performance and safety. To date, this technique had been applied to a variety of clinical patients with critical illness. The advances had been made by using blood pumps, calibrated ultrafiltration control systems, and double-lumen central venous catheter.[30] Although tremendous improvements had been achieved in this field, a lot remained to be done.
As the world's most populous and the largest developing country, China was experiencing rapid development in the economy as well as in the medical care. However, compared with developed countries, AKI was still underestimated and/or undertreated in developing countries as a result of lacking awareness, shortage of medical resources, and low socio-economic status.[28,31] Due to lack of appropriate and available guidelines and consensus on BP, significant practice heterogeneity existed, which was mainly demonstrated in several aspects such as the timing of treatment initiation, indications, modality, relative contraindication, establishment of vascular access, selection of filter/membrane, settings, anti-coagulation, even executive department, etc. As a consequence, it was crucial for us to draft China standardized treatment guidelines on BP in the near future in order to improve and standardize clinical practice. However, the fundamental starting point of that is to entirely disclose and know well the real world of current BP practice in different ICUs all over China, which was the purpose of this nationwide survey.
So far, this nationwide survey contained the widest spectrum of hospitals and most enrolled patients in this field, which could be considered to be the largest and most representative survey, as far as we know. It would contribute to reflect the real world of current BP practice in different ICUs all over China and lay the foundation for drafting China standardized treatment guideline on BP in the near future, with high potential for improvement in outcomes of the patients with critical illness.
Acknowledgements
The authors thank the participants and colleagues from the ICU ward of the Second Affiliated Hospital of Harbin Medical University, those from other participant institutions, and those who offered advice and help to this survey.
Funding
This study was funded by grants from the National Natural Science Foundation of China (Nos. 81571871 and 81770276), Nn10 Program of Harbin Medical University Cancer Hospital, Postdoctoral Funding of Heilongjiang Province (No. LBH-Z16256), Talent Fund of Harbin Science and Technology Bureau (No. 2016RAQXJ154), Young and Middle-age Innovation Science Research Fund of the Second Affiliated Hospital of Harbin Medical University (No. CX2016-02), and Scientific Research Project of Heilongjiang Health and Family Planning Commission (No. 2018086).
Conflicts of interest
None.
Footnotes
How to cite this article: Gao Y, Qi ZD, Liu RJ, Liu HT, Han QY, Zhang X, Huang R, Li M, Yang ZY, Zheng JB, Qu JD, Wang SC, Liu YS, Wang HL, Yu KJ. A multi-center cross-sectional study on blood purification among adult patients in intensive care unit in China: a study protocol. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000180
References
- 1.Lewington AJ, Cerda J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int 2013; 84:457–467. doi: 10.1038/ki.2013.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pickkers P, Ostermann M, Joannidis M, Zarbock A, Hoste E, Bellomo R, et al. The intensive care medicine agenda on acute kidney injury. Intensive Care Med 2017; 43:1198–1209. doi: 10.1007/s00134-017-4687-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wald R, McArthur E, Adhikari NK, Bagshaw SM, Burns KE, Garg AX, et al. Changing incidence and outcomes following dialysis-requiring acute kidney injury among critically ill adults: a population-based cohort study. Am J Kidney Dis 2015; 65:870–877. doi: 10.1053/j.ajkd.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu CY. Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol 2013; 24:37–42. doi: 10.1681/asn.2012080800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol 2013; 8:1482–1493. doi: 10.2215/cjn.00710113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, Lo S, et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med 2009; 361:1627–1638. doi: 10.1056/NEJMoa0902413. [DOI] [PubMed] [Google Scholar]
- 7.Lafrance JP, Miller DR. Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol 2010; 21:345–352. doi: 10.1681/asn.2009060636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang L, Xing G, Wang L, Wu Y, Li S, Xu G, et al. Acute kidney injury in China: a cross-sectional survey. Lancet 2015; 386:1465–1471. doi: 10.1016/s0140-6736(15)00344-x. [DOI] [PubMed] [Google Scholar]
- 9.Mehta RL, Cerda J, Burdmann EA, Tonelli M, Garcia-Garcia G, Jha V, et al. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet 2015; 385:2616–2643. doi: 10.1016/s0140-6736(15)60126-x. [DOI] [PubMed] [Google Scholar]
- 10.Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, et al. Acute kidney injury: an increasing global concern. Lancet 2013; 382:170–179. doi: 10.1016/s0140-6736(13)60647-9. [DOI] [PubMed] [Google Scholar]
- 11.Li PK, Burdmann EA, Mehta RL. Acute kidney injury: global health alert. Kidney Int 2013; 83:372–376. doi: 10.1038/ki.2012.427. [DOI] [PubMed] [Google Scholar]
- 12.Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med 2015; 41:1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 13.Clark WR, Ding X, Qiu H, Ni Z, Chang P, Fu P, et al. Renal replacement therapy practices for patients with acute kidney injury in China. PLoS One 2017; 12:e0178509.doi: 10.1371/journal.pone.0178509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Servillo G, Vargas M, Pastore A, Procino A, Iannuzzi M, Capuano A, et al. Immunomodulatory effect of continuous venovenous hemofiltration during sepsis: preliminary data. Biomed Res Int 2013; 2013:108951.doi: 10.1155/2013/108951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han F, Sun R, Ni Y, Hu X, Chen X, Jiang L, et al. Early initiation of continuous renal replacement therapy improves clinical outcomes in patients with acute respiratory distress syndrome. Am J Med Sci 2015; 349:199–205. doi: 10.1097/maj.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 16.Premuzic V, Basic-Jukic N, Jelakovic B, Kes P. Continuous veno-venous hemofiltration improves survival of patients with congestive heart failure and cardiorenal syndrome compared to slow continuous ultrafiltration. Ther Apher Dial 2017; 21:279–286. doi: 10.1111/1744-9987.12516. [DOI] [PubMed] [Google Scholar]
- 17.Zakharov S, Rulisek J, Nurieva O, Kotikova K, Navratil T, Komarc M, et al. Intermittent versus continuous renal replacement therapy in acute methanol poisoning: comparison of clinical effectiveness in mass poisoning outbreaks. Ann Intensive Care 2017; 7:77.doi: 10.1186/s13613-017-0300-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mirrakhimov AE, Barbaryan A. The role of renal replacement therapy in the management of pharmacologic poisonings. Int J Nephrol 2016; 2016:3047329.doi: 10.1155/2016/3047329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kopecky K, Moreland A, Hebert C, Colbert GB. Plasmapheresis for recurrent acute pancreatitis from hypertriglyceridemia. Proc (Bayl Univ Med Cent) 2017; 30:358–359. doi: 10.1080/08998280.2017.11929648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cardoso FS, Gottfried M, Tujios S, Olson JC, Karvellas CJ. Continuous renal replacement therapy is associated with reduced serum ammonia levels and mortality in acute liver failure. Hepatology 2017; 67: Epub ahead of print. doi: 10.1002/hep.29488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mujtaba M, Geara AS, Madhrira M, Agarwala R, Anderson H, Cheng JT, et al. Toxicokinetics of metformin-associated lactic acidosis with continuous renal replacement therapy. Eur J Drug Metab Pharmacokinet 2012; 37:249–253. doi: 10.1007/s13318-012-0104-y. [DOI] [PubMed] [Google Scholar]
- 22.Zarbock A, Kellum JA, Schmidt C, Van Aken H, Wempe C, Pavenstadt H, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically Ill patients with acute kidney injury: the ELAIN randomized clinical trial. Jama 2016; 315:2190–2199. doi: 10.1001/jama.2016.5828. [DOI] [PubMed] [Google Scholar]
- 23.Gaudry S, Hajage D, Schortgen F, Martin-Lefevre L, Pons B, Boulet E, et al. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med 2016; 375:122–133. doi: 10.1056/NEJMoa1603017. [DOI] [PubMed] [Google Scholar]
- 24.Bagshaw SM, Wald R. Strategies for the optimal timing to start renal replacement therapy in critically ill patients with acute kidney injury. Kidney Int 2017; 91:1022–1032. doi: 10.1016/j.kint.2016.09.053. [DOI] [PubMed] [Google Scholar]
- 25.Yang XM, Tu GW, Gao J, Wang CS, Zhu DM, Shen B, et al. A comparison of preemptive versus standard renal replacement therapy for acute kidney injury after cardiac surgery. J Surg Res 2016; 204:205–212. doi: 10.1016/j.jss.2016.04.073. [DOI] [PubMed] [Google Scholar]
- 26.Liu C, Mao Z, Kang H, Hu J, Zhou F. Regional citrate versus heparin anticoagulation for continuous renal replacement therapy in critically ill patients: a meta-analysis with trial sequential analysis of randomized controlled trials. Crit Care 2016; 20:144.doi: 10.1186/s13054-016-1299-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borthwick EM, Hill CJ, Rabindranath KS, Maxwell AP, McAuley DF, Blackwood B. High-volume haemofiltration for sepsis in adults. Cochrane Database Syst Rev 2017; 1:Cd008075.doi: 10.1002/14651858.CD008075.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang F, Hong D. Renal replacement therapy in acute kidney injury from a Chinese cross-sectional study: patient, clinical, socioeconomic and health service predictors of treatment. BMC Nephrol 2017; 18:152.doi: 10.1186/s12882-017-0567-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lauer A, Saccaggi A, Ronco C, Belledonne M, Glabman S, Bosch JP. Continuous arteriovenous hemofiltration in the critically ill patient. Clinical use and operational characteristics. Ann Intern Med 1983; 99:455–460. doi: 10.1007/s11104-012-1406-1. [DOI] [PubMed] [Google Scholar]
- 30.Ronco C. Recent evolution of renal replacement therapy in the critically ill patient. Crit Care 2006; 10:123.doi: 10.1186/cc4843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cerda J, Bagga A, Kher V, Chakravarthi RM. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin Pract Nephrol 2008; 4:138–153. doi: 10.1038/ncpneph0722. [DOI] [PubMed] [Google Scholar]


