Abstract
This study examined the associations between four types of screen-based activities and depressive symptoms among adolescents. We further investigated whether sleep characteristics (i.e., insomnia symptoms and sleep duration) mediate these associations.
Data come from 2865 U.S. adolescents (mean age=15.53, SD=.73, 51.8% male) in the age 15 follow-up of the Fragile Families and Child Wellbeing Study. Adolescents completed surveys regarding sleep duration and insomnia symptoms, typical daily duration of four screen activities (social messaging, web surfing, TV/movie watching, and gaming), and depressive symptoms. We constructed a multiple mediation model to elucidate the associations between age 15 screen time, sleep and depressive symptoms, while adjusting for age 9 depressive symptoms.
Structural Equation Modeling analyses revealed that the association between screen time and depressive symptoms is partially or fully mediated by sleep. For social messaging, web surfing and TV/movie watching, the three sleep variables fully mediated the positive association between screen time and depressive symptoms. For gaming, the three sleep variables acted as partial mediators in the model, accounting for 38.5% of the association between gaming and depressive symptoms.
Our results highlight both screen-based activities and sleep behaviors as potential intervention targets to reduce depressive symptoms among adolescents.
Keywords: screen time, gaming, social messaging, insomnia symptoms, sleep duration, depressive symptoms
Introduction
Screen-based activity is positively associated with depressive symptoms among adolescents and young adults (Demirci, Akgönül, & Akpinar, 2015; Owens & Adolescent Sleep Working Group; 2014; Thomée, Eklöf, Gustafsson, Nilsson, & Hagberg, 2007). Yet, we know little about the mechanisms linking screen-based activities and depressive symptoms. While sleep may play a mediating role in the association between screen use and depression, few studies have tested the mediation models (for an exception, see Lemola, Perkinson-Gloor, Brand, Dewald-Kaufmann, & Grob, 2015). In addition, less is known about whether specific types of screen-based activities have stronger associations with sleep and depressive symptoms than others. To address these gaps in the literature, the current study (1) investigated the association between four types of screen activities (social messaging, web surfing, TV/movie watching, and gaming) and adolescent’s depressive symptoms, and (2) examined whether insomnia symptoms and sleep duration mediated these associations.
Screen Time and Depressive Symptoms
Screen-based media use is associated with adolescent depressive symptoms. For example, Twenge and colleagues (2017) found a positive association between new media screen activities (such as smartphone or Facebook) and adolescents’ depressive symptoms using two U.S. adolescent national datasets from 2010 to 2015. Steers, Wickham and Acitelli (2014) also found a positive association between time spent on social media (Facebook) and depressive symptoms using both survey and daily diary data. Similarly, Maras and colleagues (2015) found that both video gaming and computer use were associated with Canadian teens’ depressive symptoms. These studies demonstrate that a greater amount of screen time is associated with more depressive symptoms among adolescents across contexts.
Type of Screen Activities and Depressive Symptoms
Less research has investigated whether specific types of screen use have differential associations with depressive symptoms. Most prior studies include only one or two types of screen-based activities at a time (Grøntved et al., 2015; Nuutinen et al., 2014; Thomée, Härenstam, & Hagberg, 2012) or use an aggregated measure of overall screen time (Drescher, Goodwin, Silva, & Quan, 2011; Wu, Tao, Zhang, Zhang, & Tao, 2015). In addition, the few studies investigating multiple types of screen activities have found contradictory results. For instance, Maras and colleagues (2015) found that video gaming and computer use, but not TV viewing, were associated with greater depressive symptoms. In contrast, another study found associations between prolonged TV viewing, but not computer use, with greater depressive symptoms (Grøntved et al., 2015). The current study extends existing work by systematically comparing associations of multiple types of screen activities with adolescent depressive symptoms. Specifically, we chose four types of screen-based activities – social messaging, web surfing, TV/movie watching and gaming, that are prevalent among adolescents.
The Potential Mediating Role of Sleep
The association between screen-based activities and depressive symptoms may be mediated through an increase in sleep-related problems associated with screen time and particularly screen-based activities (Cain and Gradisar, 2010). The theoretical association between these variables is supported by two emerging literatures showing associations between screen use and sleep, and between sleep and depressive symptoms.
Screen use and sleep.
Results from the National Sleep Foundation’s 2014 Sleep in America Poll indicate that 56% of parents report that 15-17 year-old adolescents sleep 7 hours or less per night, and about 44% of parents were concerned their child did not obtain sufficient sleep during school nights (Buxton et al., 2015). The widespread use of digital media devices (smartphone and tablets) contributes to insufficient and disrupted adolescent sleep (Bartel & Gradisar, 2017; Calamaro, Mason, & Ratcliffe, 2009; LeBourgeois et al., 2017; Owens & Adolescent Sleep Working Group; 2014). Recent reviews of studies that focus on school-age children and adolescents document a robust inverse association between screen activities and sleep health. Screen use has been hypothesized to disrupt sleep quality and duration for several reasons: (1) time displacement such that screen time may be substituted for potential sleep time; (2) physiological and psychological arousal from the content of electric media use may delay or disrupt sleep; and (3) blue light from digital devices may disturb circadian rhythms and cause poor sleep outcomes (Bartel, Gradisar, & Williamson, 2015; Cain & Gradisar, 2010; Hale & Guan, 2015; LeBourgeois et al., 2017). Empirical evidence demonstrates that adolescents who spend more time using screens have shorter sleep durations, delayed bedtimes, later sleep latency, more sleep disturbance symptoms, and greater sleep deficiency (Arora, Broglia, Thomas, & Taheri, 2014; Nuutinen et al., 2014; Thomée et al., 2012). In addition to bedtime screen activities, both daytime and pre-bedtime screen use have been found to be associated with poor sleep outcomes (Hysing et al., 2015; Kubiszewski, Fontaine, Rusch, & Hazouard, 2014; Munezawa et al., 2011).
Sleep and depressive symptoms.
Poor sleep is a risk factor for the development and relapse of depression (Lopez, Hoffmann, & Armitage, 2010; Lovato & Gradisar, 2014; Okun et al., 2011; Regestein et al., 2010; Roane & Taylor, 2008). Research indicates that sleep problems (insufficient sleep, insomnia symptoms, irregular sleep patterns), are positively associated with child depressive mood (Chen, Burley, & Gotlib, 2012; Coulombe, Reid, Boyle, & Racine, 2009; Lofthouse, Gilchrist, & Splaingard, 2009). In light of evidence linking screen use to both poor sleep and greater depressive symptoms, it is plausible that sleep problems play a mediating role in the association between screen use and depressive symptoms, but limited prior research has examined the mediating role of poor sleep in this context.
The current study
The present study investigated the association of daily screen-based activity time with adolescent depressive symptoms, and the mediating role of insomnia symptoms (problems falling asleep, problems staying asleep) and sleep duration in the association. We extended previous research by evaluating the associations of four most prevalent types of screen-based activities with adolescent sleep and depressive symptoms.
We tested the following hypotheses. First, more screen time (operationalized by time spent in each of the four screen-based activities) is associated with more depressive symptoms (Hypothesis 1). Second, more time spent in each of the four screen-based activities—social messaging, web-surfing, TV/movie watching, and gaming—is associated with more problems falling and staying asleep, as well as shorter sleep duration (Hypothesis 2). Third, associations between screen-based activities and depressive symptoms are at least partially mediated by problems falling and staying asleep, and sleep duration (Hypothesis 3).
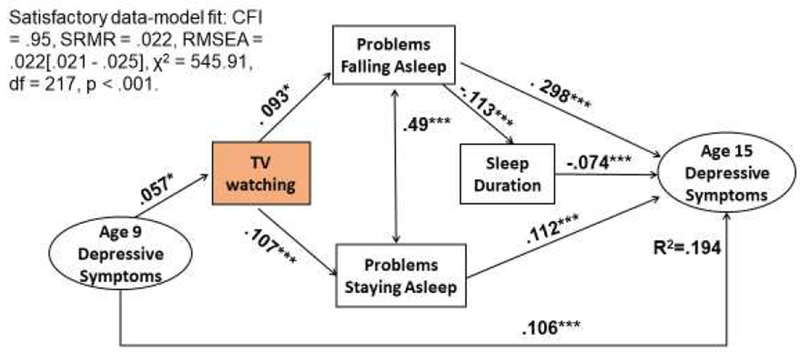
Our analytic model (Figure 1) examined whether problems falling asleep, problems staying asleep, and sleep duration serve as mediators for the association between adolescent screen time and depressive symptoms. We tested this multiple mediation model adjusting for age 9 depressive symptoms that may be associated with age 15 screen time and depressive symptoms.
Figure 1.
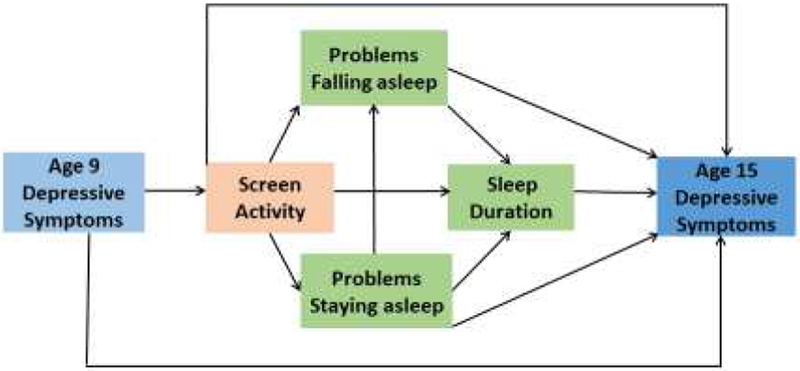
The research model of three sleep variables mediating the association between adolescent screen time and depressive symptoms.
Method
Participants and design
We used data from the Fragile Families and Child Wellbeing study (FFCWS), a longitudinal urban birth cohort study with an over-sampling of non-marital births (see Reichman, Teitler, Garfinkel, & McLanahan, 2001, for a detailed description of the study sample and design). Six waves of data have been collected, including at the time of the child’s birth and ages 1, 3, 5, 9, and 15. A total of 3,444 adolescents participated in the age 15 follow up. Most adolescents and their primary caregiver interviews were conducted between 2014 and 2016, with less than 1% of the families interviewed in 2017. We excluded 579 participants due to missing full records on variables of interest (described below) from either the age 9 or 15 interviews, thus the final analytic sample included 2,865 adolescents (mean age=15.53 years, SD=.71, 48.2% female). The excluded sample exhibited slightly higher scores on age 9 depressive symptoms, but did not differ in age 15 screen-based activities, depressive symptoms, or sleep variables. In the current sample, 47.4% of adolescent self identified as African American or Black, 23.7% as Hispanic/Latino, 16.8% were White and 12.1% were other race or Multi-racial. Each adolescent’s primary caregiver provided information related to family structure, primary caregiver education level, and household income at the age 15 interview. 17.5% of participants’ primary caregivers had less than high school education; 31.1% of the adolescents lived in households below 100% of poverty; 38.2% of adolescents come from single mother family and only 26.9% of adolescents lived with both biological parents (see Table 1). The study was conducted in accordance with principles in the Declaration of Helsinki and approved by appropriate Institutional Review Boards.
Table1.
Descriptive statistics for analytic sample (N=2865).
| Variables | M or proportion | Observed range | |||||||||
| Adolescent’s Age (month) | 186.35 | 173-221 | |||||||||
| Adolescent Male (female as reference group) | 51.8% | 0-1 | |||||||||
| Adolescent White (reference group) | 16.8% | 0-1 | |||||||||
| Adolescent Black | 47.4% | 0-1 | |||||||||
| Adolescent Hispanic/Latino | 23.7% | 0-1 | |||||||||
| Adolescent Others or Multi-racial | 12.1% | 0-1 | |||||||||
| PCG Has Less Than High School Education (reference group) | 17.5% | 0-1 | |||||||||
| PCG Has High School Diploma or GED | 19.3% | 0-1 | |||||||||
| PCG Has Some College or Tech | 44.7% | 0-1 | |||||||||
| PCG Graduated from College Or Above | 18.5% | 0-1 | |||||||||
| Poverty Threshold < 49% (reference group) | 14.1% | 0-1 | |||||||||
| Poverty Threshold 50-99% | 17% | 0-1 | |||||||||
| Poverty Threshold 100-199% | 28.9% | 0-1 | |||||||||
| Poverty Threshold 200-299% | 14.3% | 0-1 | |||||||||
| Poverty Threshold 300% Or Above | 25.7% | 0-1 | |||||||||
| Family Structure –Both biological parents (reference group) | 26.9% | 0-1 | |||||||||
| Family Structure –Biological mom with new partner | 23.4% | 0-1 | |||||||||
| Family Structure –Biological mom only | 38.2% | 0-1 | |||||||||
| Family Structure –Biological dad with new partner | 3.6% | 0-1 | |||||||||
| Family Structure –Biological dad only | 2.7% | 0-1 | |||||||||
| Family Structure –Other PCG | 5.1% | 0-1 | |||||||||
| Pearson correlation | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | M /SD | Observed range |
| 1.Social messaging | -- | 4.14/3.86 | 0-24 | ||||||||
| 2.Web surfing | .23*** | -- | 1.01/1.67 | 0-16 | |||||||
| 3.TV/movies | .26*** | .22*** | -- | 2.66/2.17 | 0-16 | ||||||
| 4.Gaming | .16*** | .21*** | .24*** | -- | 1.97/2.36 | 0-16 | |||||
| 5.Problems falling asleep | .04** | .10*** | .09*** | .06** | -- | 1.76/2.03 | 0-7 | ||||
| 6.Problems staying asleep | .06** | .08*** | .11*** | .05* | .50*** | -- | 1.28/1.95 | 0-7 | |||
| 7.Weekday sleep duration | −.17** | −.06** | −.05** | −.04* | −.13*** | −.09*** | -- | 8.0/1.25 | 2-13 | ||
| 8.Age 15 Depressive symptoms | .06** | .06*** | .07*** | .08*** | .35*** | .27*** | −.09*** | -- | .60/.60 | 0-3 | |
| 9.Age 9 Depressive symptoms | −.05** | −.007 | −.05* | .06** | .05* | .04 | .05* | .12*** | -- | .17/.23 | 0-2 |
Measures
Screen time
In the age 15 interview, adolescents were asked “How many hours per day do you usually spend on screen-based activities on weekdays” for (1) Social messaging: “communicating with friends by email, instant messaging, texting on your phone, or through social media sites, such as Facebook or Twitter?”; (2) Web-surfing: “ visiting websites or shopping on the internet?”; (3) TV/movie watching: “watching TV, videos, and movies?”; (4) Gaming: “playing games on the computer, TV, or a handheld device?” Answers ranged from 0 to 24 hours per day, with higher values representing longer duration on that specific screen activity.
Insomnia symptoms
Insomnia symptoms were assessed with 2 separate items. Adolescents were asked: “How many nights out of seven in a typical week do you have: (1) problems falling asleep throughout the night?” and (2) problems staying asleep throughout the night?” Responses ranged from 0 to 7, with higher scores representing higher frequency of problems falling asleep or problems of staying asleep, both reflecting more insomnia symptoms.
Sleep duration
Adolescents were asked about their bedtime Sunday through Thursday: “What time do you usually go to bed on school nights?” and wake up time next school day morning, “What time do you usually wake up on school day morning?” Responses were coded as hour, minute, and AM/PM, and sleep duration was calculated as the difference (in hours) between bedtime and wake time. In the current study, the mean sleep duration is 8 hours (SD= 1.25), which is consistent with self-reported data from other studies (Lemola et al., 2015; Nuutinen et al., 2014).
Age 15 depressive symptoms
Age 15 depressive symptoms were assessed by five items from the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977). This measure excluded sleep-related items from the larger CES-D. Similar items were used in the National Longitudinal Study of Adolescent Health (Add Health). Perreira and colleagues (2005) found these five items to be an improvement over the full 20-item CES-D in cross-cultural comparability. The scale includes “feel sad,” “feel depressed,” “feel life is not worth living,” “cannot shake off the blues, even with help from my family and my friends,” and “feel happy” (reverse coded). These items were answered on a 4-point Likert scale ranging from 0 (strongly disagree) to 3 (strongly agree) describing the respondent’s depressive feelings in the past week. A mean score was calculated if no more than 2 items were missing, with higher mean scores reflecting a higher level of depressive symptoms (Cronbach’s alpha= 0.76). In the current study, most adolescents’ depressive symptoms were low (Median=0.4 and Mode = 0), the mean depressive symptoms score was 0.6 (SD=0.6), which is comparable with other studies ( Lemola et al., 2015; Twenge et al., 2017). Age 15 depressive symptoms were modeled as a latent variable in the subsequent structural equation modeling analyses.
Covariates
We included the following sociodemographic and family characteristics of adolescents as covariates: age in months, sex, race, primary caregiver’s education, ratio of household income to poverty threshold and family structure. Each of these factors is correlated with screen time, sleep, and depressive symptoms. Given FFCW’s oversample of unmarried births, it is important to control for family structure (e.g., living with both biological parents, or living with biological mother only, etc.). All categorical covariates were entered as dummy variables in our analyses (see Table 1).
We adjusted for the potential confounding effects of age 9 depressive symptoms on screen use and depressive symptoms at age 15. Age 9 depressive symptoms were assessed with eight items from the withdrawn/depressed subscale of the Child Behavior Checklist (Achenbach & Rescorla, 2001). The primary caregiver rated their child’s behavior (i.e., “Child is unhappy, sad, or depressed”) on a 3-point Likert scale. Mean scores were calculated, and Cronbach’s alpha was 0.70. In the structural equation modeling analyses, age 9 depressive symptoms were modeled as a latent variable, indicated by three-item parcels (3-3-2). To reduce model complexity while retaining the benefits of using a latent variable, we used the item-to-construct balance method to build the item parcel (Little, Cunningham, Shahard & Widaman, 2002).
Statistical analyses
We first calculated descriptive statistics and a correlation matrix for the variables of interest. Second, we conducted ordinary least squares (OLS) regressions to reveal the direct association between four types of screen time and adolescents’ depressive symptoms, after adjusting for covariates. Third, we followed the two-step procedure proposed by Hayes (2017) to test the mediating role of sleep. This procedure requires: (a) significant associations between screen activities (the predictors) and sleep variables (the mediators); and (b) significant associations between the sleep variables (mediators) and depressive symptoms (the outcomes) after adjusting for the screen time (the predictors). A p-value <0.05 was considered significant.
Finally, we conducted structural equation modeling in Mplus 8.0 (Muthén, & Muthén, 1998-2017) to further elucidate the multiple mediation paths among screen time, insomnia symptoms and sleep duration, and depressive symptoms (see Figure 1), adjusting for childhood (age 9) depressive symptoms. The adequacy of data-model fit was determined by examining a combination of recommended indices (Hoyle, 2012; Hu & Bentler, 1999): the Comparative Fit Index (CFI) value ≥ 0.95; the Root Mean Square Error of Approximation (RMSEA) value ≤ 0.06; and the Standardized Root-Mean-Square Residual (SRMR) value ≤ 0.09. To determine the indirect effects associated with adolescent screen time and depressive symptoms, we employed the recommended bias-corrected bootstrap 95% confidence intervals (CIs) in 10,000 samples, CIs not overlapping with zero indicate a significant indirect effect (MacKinnon, Lockwood & Williams, 2004; Preacher & Hay, 2008).
Results
Table 1 shows descriptive statistics of the study variables, and the correlation matrix for the screen time, sleep, and depressive symptoms. Pearson’s r correlations indicated that all four types of screen activity time were positively correlated with insomnia symptoms and age 15 depressive symptoms, and negatively correlated with weekday sleep duration. Importantly, the correlations among the four types of screen activities ranged from 0.16 to 0.26, suggesting that they are not highly correlated and thus appear to be relatively independent constructs. As expected, sleep duration was negatively associated with both insomnia symptoms, and age 9 depressive symptoms was positively correlated with age 15 depressive symptoms.
Associations between screen-based activities and depressive symptoms.
Our first aim was to test the direct associations between screen activities and adolescent depressive symptoms. As hypothesized, after adjusting for covariates, all four screen-based activities were positively associated with adolescent depressive symptoms (Unstandardized Bs ranged from .007 to .026, p<.01, see Table 2). The results confirmed Hypothesis 1 that more screen time—social messaging, web-surfing, TV/movie watching and gaming—in each domain was consistently associated with greater depressive symptoms. As shown in Table 2, comparisons of the width of 95% confidence intervals revealed that the association of social messaging with depressive symptoms was significantly different than that of gaming, as indicated by the non-overlapping confidence interval (Cumming, 2009; Knezevic, 2008), but no differences exist among social messaging, web-surfing and TV/movie watching.
Table 2.
Direct association between screen times and depressive symptom (N=2865).
| Predictor | Model 1 Outcome = Year 15 Depressive Symptoms |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | B | 95% CI | B | 95% CI | B | 95% CI | ||
| Screen Activities | Social messaging | .007** | [.001, .012] | ||||||
| Web-Surfing | .018*** | [.005 , .031] | |||||||
| TV watching | .017*** | [.007 , .03] | |||||||
| Gaming | .026*** | [.016 , .035] | |||||||
| Child characteristics | |||||||||
| Adolescent age (month) | .001 | [−.02 , .004] | .001 | [−.002,.004] | .002 | [−.001 ,.004] | .002 | [−.001, .005] | |
| Female (RF) | --- | --- | -- | --- | --- | --- | -- | -- | |
| Gender | Male | −.12*** | [−.17 , −.08] | −.12*** | [−.17 , −.08] | −.13*** | [−.17 , −.08] | −.15*** | [−.15 , −.11] |
| White (RF) | --- | --- | --- | --- | --- | --- | --- | --- | |
| Ethnicity | Black | −.06 | [−.13 , .01] | −.06 | [−.13 , .01] | −.06* | [−.13 , −.01] | −.05 | [−.12 , .02] |
| Hispanic/Latino | −.01 | [−.09 , .06] | −.01 | [−.08 , .06] | −.01 | [−.09 , .06] | −.01 | [−.08 , .07] | |
| Others & Multiracial | .06 | [−.03 , .14] | .06 | [−.03 , .14] | .05 | [−.03 , .13] | −.06 | [−.02 , .14] | |
| Household and caregiver characteristics | |||||||||
| < High school (RF) | --- | --- | --- | --- | --- | --- | --- | --- | |
| PCG Education | High school | −.02 | [−.09 , .06] | −.02 | [−.09 , .05] | −.02 | [−.09 , .06] | −.02 | [−.09 , .05] |
| Some college | −.07 | [−.13 , .01] | −.07 | [−.13 , .01] | −.07* | [−.13 , .01] | −.07* | [−.13 , .01] | |
| College or + | −.08 | [−.16 , .01] | −.08 | [ −.16 , .01] | −.08 | [−.16 , .01] | −.07 | [−.16 , .01] | |
| Ratio of household income to poverty threshold | < 49% (RF) | --- | --- | --- | --- | --- | --- | --- | --- |
| 50-99% | −.03 | [−.11 , .04] | −.04 | [−.11 , .04] | −.03 | [−.11 , .04] | −.04 | [−.11 , .04] | |
| 100-199% | −.10** | [−.17 , −.03] | −.10** | [−.17 , −.03] | −.10** | [−.17 , −.03] | −.10** | [−.17 , −.03] | |
| 200-299% | −.10* | [−.18 , −.01] | −.10** | [−.18 , −.01] | −.09* | [−.18 , −.01] | −.10* | [−.18 , −.02] | |
| 300% or + | −.19*** | [−.27 , −.11] | −.19*** | [−.27 , −.10] | −.18*** | [−.26 , −.10] | −.18*** | [−.26 , −.10] | |
|
Family Structure |
Both biological parents (RF) | --- | --- | --- | --- | --- | --- | --- | --- |
| Biological mom with new partner | .10*** | [ .04 , .16] | .10*** | [ .04 , .17] | .10** | [.04 , .16] | 11*** | [.04 , .17] | |
| Biological mom only | .06 | [−.01 , .11] | .06* | [−.01 , . 12] | .06* | [−.01, .12] | .06* | [.01 , .12] | |
| Biological dad with new partner | 19** | [ .07 , .31] | .20** | [ .07 , .32] | .20** | [.07 , .32] | .20** | [.08 , .32] | |
| Biological dad only | .05 | [−.09 , .19] | .06 | [−.08 , .19] | .05 | [−.09 ,.19] | .05 | [−.08 , .19] | |
| Other PCG | 14** | [ .04 , .25] | .14** | [ .04 , .25] | .14* | [.04 , .25] | .15* | [.04 , .25] | |
| Adjusted R2 | .036 | .037 | .038 | .044 | |||||
| F | 6.99*** | 7.15*** | 7.31*** | 8.36*** | |||||
Note. B=Unstandardized Coefficients (for ordinary least squares [OLS] regression). RF=Reference group.
p<.05
p<.01
p<.001.
Tests for mediation
The second purpose was to examine the potentially mediating roles of poor sleep (problems falling asleep, problems staying asleep, and shorter sleep duration) in the link between screen activities and adolescent depressive symptoms. To establish the mediation model (Hayes 2017), we first tested the associations between screen activities and three sleep variables. Consistent with Hypothesis 2, results revealed that the four screen activities were positively associated with problems falling asleep (Bs:.019 ~ .105, p<.05, see Equation 1-4 in Table 3) and with problems staying asleep (Bs: .023 ~ .094, p<.01, see Equation 5-8), and were negatively associated with weekday sleep duration (Bs:−.05 ~ −.027, p<.01, see Equation 9-12).
Table 3.
Associations between screen activities and sleep variables (N=2865).
| Predictor | Outcome Problems falling asleep (0-7 day) | Outcome Problems staying asleep (0-7 day) | Outcome School day sleep duration (hours) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Equation number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| Screen Activities: Messaging | .019* | .023** | −.05*** | ||||||||||
| Web-Surfing | .105*** | .078** | −.038** | ||||||||||
| TV | .084*** | .094*** | −.027** | ||||||||||
| Game | .073*** | −.054*** | −.029*** | ||||||||||
| Child characteristics | |||||||||||||
| Adolescent age (month) | .004 | .005 | .005 | .006 | .005 | .004 | .006 | .006 | −.004 | −.005 | −.005 | −.005 | |
| Female (RF) | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | |
| Gender | Male | −.48*** | −.47*** | −.48*** | −.56*** | −.38*** | −.37*** | −.39*** | −.45*** | .11* | .14** | .15** . | 18*** |
| White (RF) | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | |
| Ethnicity | Black | −.48*** | −.48*** | −.52*** | −.47*** | −.20 | −.18 | −.25* | −.18 | −.24*** | −.28*** | −.26*** | −.29*** |
| Hispanic/Latino | −.35** | −.35** | −.38*** | −.36** | −.32** | −.31** | −.34** | −.31** | .05 | .05 | .07 | .05 | |
| Others & Multiracial | −.05 | −.06 | −.12 | −.12 | −.10 | −.13 | −.18 | −.13 | −.11 | −.11 | −.09 | −.11 | |
| Household and caregiver characteristics | |||||||||||||
| PCG Education | < High school (RF) | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| High school | −.11 | −.12 | −.12 | −.12 | −.01 | .004 | .003 | −.001 | −.001 | .01 | −.001 | .013 | |
| Some college | −.11 | −.09 | −.18 | −.08 | −.001 | .032 | −.04 | .03 | −.10 | −.11 | −.11 | −.10 | |
| College or + | −.03 | −.03 | −.03 | −.01 | −.17 | −.16 | −.16 | −.15 | −.16 | −.15 | −.15 | −.14 | |
| Ratio of household income to poverty threshold | < 49% (RF) | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| 50-99% | −.06 | −.06 | −.05 | −.04 | −.05 | −.06 | −.05 | −.04 | −. 23** | −.24** | −.24** | −.24** | |
| 100-199% | −.04 | −.01 | −.02 | −.01 | −.003 | −.01 | −.001 | .005 | −.24** | −.26*** | −.27*** | −.27** | |
| 200-299% | .02 | .05 | .01 | .05 | −.12 | −.12 | −.09 | −.12 | −.29*** | −.31*** | −.33*** | −.32*** | |
| 300% or + | −.33* | −.30* | −.29* | −.29* | −.34** | −.36* | −.34** | −.35* | −.30*** | −.31*** | −.31*** | −.32*** | |
|
Family structure |
Both biological parents (RF) | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| Biological mom with new partner | .27** | .28* | .28* | .29** | .20 | .22* | .20 | .22* | −.002 | .07 | −.01 | .07 | |
| Biological mom only | .18 | .19 | .18 | .19 | .03 | .05 | .05 | .06 | .06 | .07 | .03 | .07 | |
| Biological dad with new partner | .46* | .48* | .49* | .46* | .11 | .13 | .14 | .14 | .003 | .14 | −.04 | .13 | |
| Biological dad only | .02 | .10 | .03 | .01 | −.35 | −.33 | −.37 | −.32 | −.05 | .15 | .05 | .15 | |
| Other PCG | .005 | .054 | .03 | .05 | −.09 | −.04 | −.07 | −.04 | .19 | .12 | .15 | .12 | |
| Adjusted R2 | .021 | .027 | .028 | .027 | .02 | .022 | .029 | .022 | .044 | .022 | .022 | .023 | |
| F | 4.38*** | 5.40*** | 5.49*** | 5.32*** | 4.24*** | 4.64*** | 5.67*** | 4.58*** | 8.23*** | 4.65*** | 4.58*** | 4.75*** | |
Note. B=Unstandardized Coefficients (for ordinary least squares [OLS] regression). RF=Reference group.
p<.05,
p<.01,
p<.001.
95% Confidence Interval available upon request.
We next examined associations of the screen activities with depressive symptoms while adjusting for sleep characteristics. Regression results (see Model 2 of Table 4) indicated that, after adjusting for covariates and three sleep variables, three of the four screen activities (social messaging, web-surfing and TV/movie watching) were no longer associated with depressive symptoms (compared with the direct effects shown in Model 1 of Table 4). That is, problems falling asleep, problems staying asleep, and sleep duration fully mediated the associations between these three screen activities and depressive symptoms. In contrast, gaming continued to have a significant residual direct association with age 15 depressive symptoms when sleep variables were included, but the association was attenuated by about 38.5% (B drop from .026 to .016), demonstrating a partial mediation between gaming and depressive symptoms. Gaming was still significantly associated with age 15 depressive symptoms, even after adjusting for the adolescent’s age 9 symptoms of depression (Model 3 in Table 4). Therefore, problems falling asleep, problems staying asleep, and sleep duration mediated the link between the four types of screen activities and depressive symptoms (Hypothesis 3 supported).
Table 4.
Mediation of sleep quality/duration on association between screen activities and age 15 depressive symptom (N=2865).
| Predictor | Model 1 Outcome: Age 15 Depressive Symptoms Direct Association |
Model 2 Outcome: Age 15 Depressive SymptomsMediators Added |
Model 3 Outcome: Age 15 Depressive SymptomsMediators and Age 9 Depression Added |
|---|---|---|---|
| Screen activities : Social messaging (hours) | .007** | .003 | .004 |
| Problems falling asleep (0-7 day) | 079*** | 078*** | |
| Problems staying asleep (0-7 day) | .034*** | .034*** | |
| Sleep duration (hours) | −.025** | −.026*** | |
| Age 9 depressive symptoms (0-2) | .237*** | ||
| Adjusted R2 | .036 | .15 | .16 |
| Screen activities : Web-surfing (hours) | .018*** | .007 | .007 |
| Problems falling asleep (0-7 day) | 079 *** | 078 *** | |
| Problems staying asleep (0-7 day) | .034*** | .034*** | |
| Sleep duration (hours) | −.026*** | −.028*** | |
| Age 9 depressive symptoms (0-2) | .24*** | ||
| Adjusted R2 | .037 | .154 | .162 |
| Screen activities : TV/movies (hours) | .017** | .006 | .005 |
| Problems falling asleep (0-7 day) | 079 *** | 078 *** | |
| Problems staying asleep (0-7 day) | .034*** | .033*** | |
| Sleep duration (hours) | −.026*** | −.028*** | |
| Age 9 depressive symptoms (0-2) | .232*** | ||
| Adjusted R2 | .038 | .155 | .162 |
| Screen activities : Gaming (hours) | .026*** | .017*** | .016*** |
| Problems falling asleep (0-7 day) | 078*** | 078*** | |
| Problems staying asleep (0-7 day) | .033*** | .033*** | |
| Sleep duration (hours) | −.025*** | −.027*** | |
| Age 9 depressive symptoms (0-2) | .222*** | ||
| Adjusted R2 | .044 | .159 | .166 |
Note. B=Unstandardized Coefficients (for ordinary least squares [OLS] regression).
p<.05
p<.01
p<.001.
Demographic covariates included in the analyses, but not shown in table for visual simplicity.
Path analyses for multiple mediation model.
To further elucidate the interplay among screen time, sleep, and depressive symptoms, we conducted latent variable path analyses to test the research model depicted in Figure 1. Both age 9 and age 15 depressive symptoms were modeled as latent variables, and covariates were included in the analyses but not shown in the figure for visual simplicity. Figure 2A–2D illustrate the path analysis results for each screen-based activity with standardized path coefficients. Each model took into account the inter-relations between the three sleep variables (problems falling asleep, problems staying asleep, and sleep duration), and thus allowed us to understand the pathways from screen activities to depressive symptoms through various sleep characteristics.
Figure 2A.
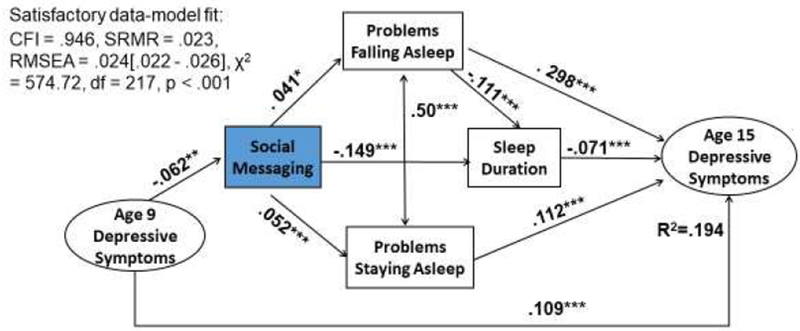
Latent variable path models of social messaging and depressive symptoms mediated by sleep problems and sleep duration. Coefficients are standardized path coefficients controlling for covariates, N=2,865.
* p<.05, **p<.01, ***p<.001.
Figure 2D.
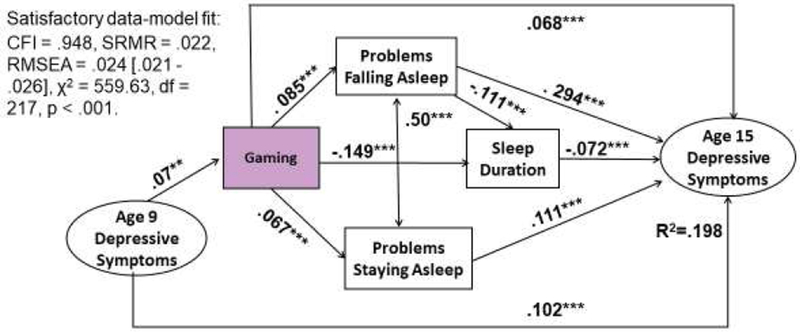
Latent variable path models of gaming and depressive symptoms mediated by sleep problems and sleep duration. Coefficients are standardized path coefficients controlling for covariates, N=2,865.
* p<.05, **p<.01, ***p<.001.
We estimated the path model for four screen activities, all four models yielded satisfying fit for the hypothesized relations. Figure 2A shows that the model for social messaging was mostly consistent with the theoretical prediction. Age 9 depressive symptoms negatively predicted age 15 social messaging (β = − .062, p<.01). After adjusting for the influence of age 9 depressive symptoms on age 15 depressive symptoms (β = .109, p<.001), social messaging was positively associated with problems falling asleep (β= .041, p<.05) and problems staying asleep (β = .052, p<.001), and negatively associated with sleep duration (β = − .149, p<.001), which each independently contributed to greater adolescent depressive symptoms (βs: −.071 ~ .298, p<.001). These three sleep variables fully mediated the link between social messaging and depressive symptoms, and the indirect effects were all significant with a 95% confidence interval (CI) in a 10,000 bias-corrected bootstrap sample (see Table 5 for the illustration of the indirect effects). Furthermore, the path from social messaging to age 15 depressive symptoms did not reach significance, suggesting full mediation of the three sleep variables. Together, the model explained 19.4% of the variance of adolescent depressive symptoms.
Table 5.
Bootstrap Tests of Statistical Significance of Indirect Effects. (N=2865).
| Independent and mediator variables | Dependent variable | β (standardized indirect effects) | 95% Confidence Interval | |
|---|---|---|---|---|
| Social messaging → PFS | Age 15 Depressive symptoms | .041 × .298 = .012 | [.001 , .024] | |
| Social messaging → Sleep Duration | Age 15 Depressive symptoms | −.149 × −.071 = .011 | [.001 , .011] | |
| Social messaging → PSS | Age 15 Depressive symptoms | .052 × .112 = .006 | [.004 , .018] | |
| Social messaging → PFS | Sleep Duration | .041 × −.111 = −.005 | [−.009, .000] | NS |
| Web-surfing → PFS | Age 15 Depressive symptoms | .088 × .298 = .026 | [.013, .04] | |
| Web-surfing → PSS | Age 15 Depressive symptoms | .068 × .113 = .008 | [.002 , .014] | |
| Web-surfing → PFS | Age 15 Sleep Duration | .088 × −.111 = − .009 | [−.014, −.004] | |
| TV → PFS | Age 15 Depressive symptoms | .093 × .298 = .028 | [.015, .04] | |
| TV → PSS | Age 15 Depressive symptoms | .107 × .112 = .012 | [.005 , .019] | |
| TV → PFS | Sleep Duration | .093 × −.113 = −.010 | [−.017, −.004] | |
| Gaming → PFS | Age 15 Depressive symptom | .085 x.294 = .025 | [.012, .035] | |
| Gaming → PSS | Age 15 Depressive symptom | .067 × .111 = .007 | [.002 , .013] | |
| Gaming → PFS | Sleep Duration | .085 × −.111 = −.009 | [−.015, −.004] | |
Note. Based on 10,000 bootstrap samples. Bias-corrected 95% confidence interval that exclude zero indicated significant indirect effects (p<.05). PFS = problems falling asleep; PSS = problems staying asleep.
For the path models for web-surfing and TV/movie watching (as shown in Figure 2B and2C), age 9 depressive symptoms had no effect on age 15 web-surfing but positively predicted age 15 TV watching (β= .057, p<.05); both screen activities produced significant paths to problems falling asleep and problems staying asleep, which were further associated with greater depressive symptoms at age 15. However, the direct association between TV watching and sleep duration was fully mediated by problems falling asleep and thus no longer significant (see Table 5). Together, the model explained 19.4% of the variances of age 15 depressive symptoms for both web surfing and TV.
Figure 2B.
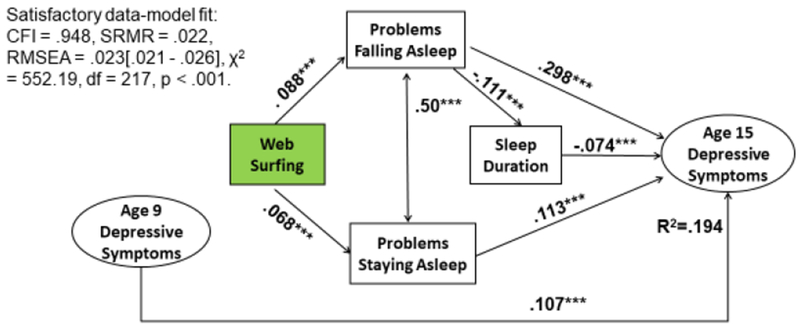
Latent variable path models of web surfing and depressive symptoms mediated by sleep problems and sleep duration. Coefficients are standardized path coefficients controlling for covariates, N=2,865.
* p<.05, **p<.01, ***p<.001.
Figure 2C.
Latent variable path models of TV watching and depressive symptoms mediated by sleep problems and sleep duration. Coefficients are standardized path coefficients controlling for covariates, N=2,865.
* p<.05, **p<.01, ***p<.001.
For gaming (Figure 2D), the results indicate that age 9 depressive symptoms positively predicted age 15 gaming (β = .07, p<.01), which was further associated with three sleep variables, and in turn with age 15 depressive symptoms. However, gaming still had a residual direct association with adolescent depressive symptoms (β = .068, p<.001), even after age 9 depressive symptoms adjustment (β = .102, p<.001). Together, the model accounted for 19.8 % of the variance of depressive symptoms.
Discussion
Sufficient and high quality sleep are vital components of adolescent psychological well-being. The pervasive role of screen-based media may affect both adolescent sleep duration and sleep quality, and therefore influence depressive symptoms. In the present study, we examined the associations between four types of screen-based activities (social messaging, web surfing, TV/movie watching, gaming) and depressive symptoms, as well as the mediating role of three sleep characteristics. Overall, our results indicated that all four types of screen-based activities were associated with greater depressive symptoms and poorer sleep characteristics, supporting both Hypotheses 1 and 2. Consistent with Hypothesis 3, more insomnia symptoms (i.e., problems falling and maintaining asleep) and shorter sleep duration mediated the association between each type of screen activity and depressive symptoms. These mediation results persisted even after accounting for earlier (age 9) parent-reported depressive symptoms.
We found that all four screen-based activities had direct associations with adolescent depressive symptoms and sleep problems. Consistent with previous research, more adolescent screen time (computer use, gaming, social networking sites) was associated with more depressive symptoms (Steers et al., 2014; Maras et al., 2015). Further, each of the screen-based activities were associated with more problems falling asleep and staying asleep, and shorter weekday sleep duration, a new finding that shows the disturbance of various types of screen activities with three distinct measures of adolescent sleep.
Our mediation analyses also revealed that all four types of screen-based activities were indirectly associated with more depressive symptoms through their sleep characteristics (e.g., more problems falling asleep and staying asleep, shorter weekday sleep duration). Our findings are consistent with theoretical models (Cain & Gradisar, 2010) and empirical findings (Lemola et al., 2015), in which sleep problems and insufficient sleep duration are mediating mechanisms through which electronic media use is associated with depressive symptoms.
Path analyses revealed four patterns of associations for the different screen-based activities. Full mediation by sleep characteristics was observed for social messaging, web-surfing and television/movie watching, whereas for gaming, only partial mediation by sleep characteristics was observed. In this case, other unmeasured variables might have contributed to the association between gaming and depression. For example, more gaming may reflect particular individual characteristics (e.g., trait neuroticism, self-control) that may be strongly associated with depressive symptoms (Mehroof & Griffiths, 2010) but not via sleep pathways. Alternatively, this association may also reflect a selection behavior in which more depressive individuals turn to gaming behavior as an escape (Kuss & Griffiths, 2012), as we found the significant link between age 9 depressive symptoms and age 15 gaming behavior.
Our findings contribute to the previous literature in several ways. First, this study utilized population-based national birth cohort of diverse U.S. urban families with extensive family and socioeconomic characteristics, which increases our confidence for external validity. Second, our study extended the literature by separately investigating the associations of four typical screen activities with depressive symptoms. The comparisons revealed that, the association between gaming and depressive symptoms is less likely to function through poor sleep than the other three screen activities, thus, interventions among heavy gamers to reduce depression may need to consider other mechanisms. Third, this study tested several dimensions of sleep, including insomnia symptoms (i.e., problems falling and staying asleep) and sleep duration. By doing so, our findings suggest that screen-based activities have negative implications for both sleep quality and sleep quantity, which further relates to depressive symptoms. Finally, our path analysis results highlight that the association between screen time and depressive symptoms during adolescence are above and beyond early life depressive symptoms.
Several limitations should be considered in interpreting our results. First, the data on screen-based activity, sleep, and depressive symptoms were measured concurrently at age 15, thus making it impossible to tease apart both causality and temporality. We statistically tested a plausible theoretical model (in which screen time leads to impaired sleep which affects depressive symptoms), but alternative models with other temporal orderings (e.g., depressive symptoms as the mediator and sleep as outcome) are also plausible. Second, the screen activities measures captured only the duration but not the content or interactivity of the screen activity. Third, although adolescents were asked to specify the amount of time spent in each screen activity, self-reported screen activity durations might be subject to recall error or overlap, it is plausible that adolescents were “multi-tasking” with different screen devices, for instance, watching a movie on a laptop while text messaging friends by phone. Meanwhile, three study constructs relied on adolescent self-report, which might introduce mono-informant bias. Also, our current data only assessed screen activities and sleep duration in weekdays, weekend screen time and sleep duration also contribute to depressive symptoms. Finally, although the relationships in the models are statistically significant, the effect sizes in the study as a whole are small. Future research should investigate the temporal sequencing of these three variables, in addition to adding more enriched (multiple informants: self-report, parent report, and teacher report) and objective measurement for screen activities and sleep (e.g. accelerometer-derived sleep data).
Using a large-scale national birth cohort of diverse urban U. S. families, this study highlights the potential roles of both screen-based activities and sleep deficiency in the development of adolescent mental health. Parents, educators and health care professionals could consider educating adolescents and regulating their screen times, as possible interventions for improving sleep health and reducing depression among adolescents (LeBourgeois et al., 2017).
Highlights.
Sleep variables fully mediated the association between social messaging, web-surfing, television/movie watching and depressive symptoms.
Sleep variables partially mediated the association between gaming and depressive symptoms.
The association between screen time and adolescent depressive symptoms were above and beyond childhood depressive symptoms.
Acknowledgments
Research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) under award numbers R01HD073352 (PI: Hale), R01HD36916, R01HD39135, and R01 HD40421, as well as a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The other authors declare that they have no conflict of interest. Outside of the current work, Orfeu M. Buxton discloses that he received two subcontract grants to Penn State from Mobile Sleep Technologies (NSF/STTR #1622766, NIH/NIA SBIR R43AG056250). Dr. Lauren Hale receives an honorarium from the National Sleep Foundation for serving as Editor-in-Chief of the journal Sleep Health.
References
- Achenbach TM, & Rescorla LA1 (2001). Manual for the ASEBA School-Age Forms & Profiles: Burlington, VT: University of Vermont, Research Center for Children, Youth & Families. [Google Scholar]
- Arora T, Broglia E, Thomas GN, & Taheri S (2014). Associations between specific technologies and adolescent sleep quantity, sleep quality, and parasomnias. Sleep Medicine, 15(2), 240–247. [DOI] [PubMed] [Google Scholar]
- Bartel K, & Gradisar M (2017). New directions in the link between technology use and sleep in young people In Nevšímalová S, & Bruni O (Eds.) Sleep disorders in children (pp. 69–80). New York, NY: Springer. [Google Scholar]
- Bartel KA, Gradisar M, & Williamson P (2015). Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Medicine Reviews,21, 72–85. [DOI] [PubMed] [Google Scholar]
- Buxton OM, Chang AM, Spilsbury JC, Bos T, Emsellem H, & Knutson KL (2015). Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health, 1(1), 15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calamaro CJ, Mason TB, & Ratcliffe SJ (2009). Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics, 123(6), e1005–e1010. [DOI] [PubMed] [Google Scholar]
- Cain N, & Gradisar M (2010). Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Medicine, 11(8), 735–742. [DOI] [PubMed] [Google Scholar]
- Chen MC, Burley HW, & Gotlib IH (2012). Reduced sleep quality in healthy girls at risk for depression. Journal of Sleep Research, 21(1), 68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulombe JA, Reid GJ, Boyle MH, & Racine Y (2009). Concurrent associations among sleep problems, indicators of inadequate sleep, psychopathology, and shared risk factors in a population-based sample of healthy Ontario children. Journal of Pediatric Psychology, 35(7), 790–799. [DOI] [PubMed] [Google Scholar]
- Cumming G (2009). Inference by eye: reading the overlap of independent confidence intervals. Statistics in medicine, 28(2), 205–220. [DOI] [PubMed] [Google Scholar]
- Demirci K, Akgönül M, & Akpinar A (2015). Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. Journal of Behavioral Addictions, 4(2), 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drescher AA, Goodwin JL, Silva GE, & Quan SF (2011). Caffeine and screen time in adolescence: associations with short sleep and obesity. Journal of Clinical Sleep Medicine, 7(4), 337–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grøntved A, Singhammer J, Froberg K, Møller NC, Pan A, Pfeiffer KA, & Kristensen PL (2015). A prospective study of screen time in adolescence and depression symptoms in young adulthood. Preventive Medicine, 81, 108–113. [DOI] [PubMed] [Google Scholar]
- Hale L, & Guan S (2015). Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Medicine Reviews, 21, 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis. A Regression-Based Approach. (2nd ed.). New York: Guilford. [Google Scholar]
- Hoyle RH (2012). Handbook of Structural Equation Modeling. New York: Guilford Press. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Hysing M, Pallesen S, Stormark KM, Jakobsen R, Lundervold AJ, & Sivertsen B (2015). Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open, 5(1), e006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knezevic A (2008). Overlapping confidence intervals and statistical significance. StatNews: Cornell University Statistical Consulting Unit, 73(1). [Google Scholar]
- Kubiszewski V, Fontaine R, Rusch E, & Hazouard E (2014). Association between electronic media use and sleep habits: an eight-day follow-up study. International Journal of Adolescence and Youth, 19(3), 395–407. [Google Scholar]
- Kuss DJ, & Griffiths MD (2012). Internet gaming addiction: A systematic review of empirical research. International Journal of Mental Health and Addiction, 10(2), 278–296. [Google Scholar]
- LeBourgeois MK, Hale L, Chang AM, Akacem LD, Montgomery-Downs HE, & Buxton OM (2017). Digital media and sleep in childhood and adolescence. Pediatrics, 140 (Supplement 2), S92–S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, & Grob A (2015). Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. Journal of Youth and Adolescence, 44(2), 405–418. [DOI] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, & Widaman KF (2002). To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling, 9(2), 151–173. [Google Scholar]
- Lovato N, & Gradisar M (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Medicine Reviews, 18(6), 521–529. [DOI] [PubMed] [Google Scholar]
- Lofthouse N, Gilchrist R, & Splaingard M (2009). Mood-related sleep problems in children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 18(4), 893–916. [DOI] [PubMed] [Google Scholar]
- Lopez J, Hoffmann R, & Armitage R (2010). Reduced sleep spindle activity in early-onset and elevated risk for depression. Journal of the American Academy of Child & Adolescent Psychiatry, 49(9), 934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maras D, Flament MF, Murray M, Buchholz A, Henderson KA, Obeid N, & Goldfield GS (2015). Screen time is associated with depression and anxiety in Canadian youth. Preventive Medicine,73, 133–138. [DOI] [PubMed] [Google Scholar]
- Mehroof M, & Griffiths MD (2010). Online gaming addiction: the role of sensation seeking, self-control, neuroticism, aggression, state anxiety, and trait anxiety. Cyberpsychology, behavior, and social networking, 13(3), 313–316. [DOI] [PubMed] [Google Scholar]
- Munezawa T, Kaneita Y, Osaki Y, Kanda H, Minowa M, Suzuki K, … & Ohida T (2011). The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents: a nationwide cross-sectional survey. Sleep, 34(8), 1013–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nuutinen T, Roos E, Ray C, Villberg J, Välimaa R, Rasmussen M, … & Tynjälä J. (2014). Computer use, sleep duration and health symptoms: a cross-sectional study of 15-year olds in three countries. International Journal of Public Health, 59(4), 619–628. [DOI] [PubMed] [Google Scholar]
- Okun ML, Luther J, Prather AA, Perel JM, Wisniewski S, & Wisner KL (2011). Changes in sleep quality, but not hormones predict time to postpartum depression recurrence. Journal ofAffective Disorders, 130(3), 378–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens J, & Adolescent Sleep Working Group. (2014). Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics, 134(3), e921–e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreira KM, Deeb-Sossa N, Harris KM, & Bollen K (2005). What Are We Measuring? An Evaluation of the CES-D Across Race/Ethnicity and Immigrant Generation. Social Forces, 83(4): 1567–1601. [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Regestein Q, Natarajan V, Pavlova M, Kawasaki S, Gleason R, & Koff E (2010). Sleep debt and depression in female college students. Psychiatry Research, 176(1), 34–39. [DOI] [PubMed] [Google Scholar]
- Reichman NE, Teitler JO, Garfinkel I, & McLanahan SS (2001). Fragile families: Sample and design. Children and Youth Services Review, 23, 303–326. [Google Scholar]
- Roane BM, & Taylor DJ (2008). Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep, 31(10), 1351–1356. [PMC free article] [PubMed] [Google Scholar]
- Steers MLN, Wickham RE, & Acitelli LK (2014). Seeing everyone else’s highlight reels: How Facebook usage is linked to depressive symptoms. Journal of Social and Clinical Psychology, 33(8), 701–731. [Google Scholar]
- Thomée S, Eklöf M, Gustafsson E, Nilsson R, & Hagberg M (2007). Prevalence of perceived stress, symptoms of depression and sleep disturbances in relation to information and communication technology (ICT) use among young adults-an explorative prospective study. Computers in Human Behavior, 23(3), 1300–1321. [Google Scholar]
- Thomée S, Härenstam A, & Hagberg M (2012). Computer use and stress, sleep disturbances, and symptoms of depression among young adults-a prospective cohort study. BMC Psychiatry, 12(1), 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, Joiner TE, Rogers ML, & Martin GN (2017). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science, 6(1), 3–17. [Google Scholar]
- Wu X, Tao S, Zhang Y, Zhang S, & Tao F (2015). Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS One, 10(3), e0119607. [DOI] [PMC free article] [PubMed] [Google Scholar]


