Abstract
Background.
Prior studies have supported the efficacy of diabetes group visits. However, the benefit of diabetes group visits for low-income and underserved individuals is not clear. The purpose of this study was to conduct a narrative review in order to clarify the efficacy of diabetes group visits in low-income and underserved settings.
Methods.
The authors performed a narrative review, categorizing studies into nonrandomized and randomized.
Results.
A total of 14 studies were identified. Hemoglobin A1c was the most commonly measured outcome, which improved for the majority of group visit participants. Preventive care showed consistent improvement for intervention arms. There were several other study outcomes including metabolic (i.e., blood pressure), behavioral (i.e., exercise), functional (i.e., quality of life), and system-based (i.e., cost).
Conclusions.
Diabetes group visits for low-income and underserved individuals resulted in superior preventive care but the impact on glycemic control remains unclear.
Keywords: Group visits, diabetes, low-income, underserved, chronic disease, shared medical appointments
GRAPHICAL ABSTRACT
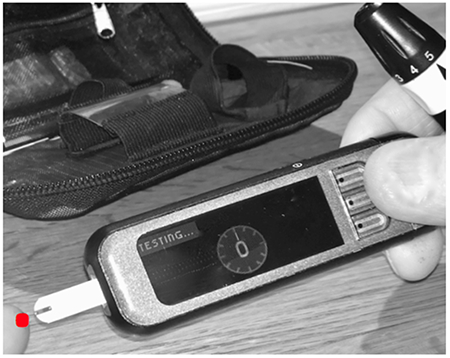
Diabetes affects millions worldwide, yet many lack access to care. Diabetes group visits are promising to improve healthcare in low-income and underserved populations.
1. INTRODUCTION
Diabetes is the sixth leading cause of death worldwide [1]. There are 422 million individuals living with diabetes globally, compared to 180 million in 1980 [1]. Because of the sheer number of individuals with diabetes, innovative ways to provide adequate care are needed. The efficacy for diabetes group visits has been examined as a way to provide care to a large number of individuals. Results have supported strong efficacy for these programs, both in cost and in clinical outcomes [2–7]. Treatment effect models have shown that group visits significantly reduce outpatient charges (p<0.001) and may be preferred in lieu of more expensive specialty care visits [8]. A systematic review that included a meta-analysis (n=26 studies) of diabetes group visits found that participants resulted in positive Hemoglobin A1c (HbA1c) outcomes (−0.46%) [7]. Another systematic review concluded that these programs improved participant HbA1c and systolic blood pressure levels (−0.55%, −5.2 mmHg, respectively) when compared to usual care [3]. However, investigators have noted the need for rigorous evaluation of diabetes group visits to fully understand the variables (i.e., educational strategies) that have led to their efficacy [9].
The cost effectiveness and positive clinical outcomes attributed to diabetes group visits could be of particular importance where healthcare is often suboptimal, such as in low-income settings [10]. Social determinants of health are a particular concern in diabetes [11]. Data from a Canadian study showed that men and women in the lowest income category (less than $15,000 annual income) were four times as likely to develop type 2 diabetes compared to those in the highest income category (greater than $80,000 annual income) [11]. Similarly, the National Health and Nutrition Examination Survey and US Census data found a race-poverty-place gradient for diabetes among non-Hispanic blacks and low-income whites [12].
Unfortunately, there is a paucity of data evaluating diabetes group visits in subpopulations including those within a specific socioeconomic status [2, 6]. Also, within these studies there is diversity of study design, methodology, and measured outcomes. This hinders the ability to conduct a robust systematic review or meta-analysis. Though the chronic disease burden is often greater in low-income settings, clinical trials are severely underrepresented in these areas [13]. This is often due to logistical barriers of designing and implementing such studies [13, 14]. Although randomized controlled trials (RCTs) are considered the gold standard to establish standard of care practices and treatment guidelines, nonrandomized studies are also of value [15]. Since exclusion criteria for RCTs are often rigid, nonrandomized studies may provide information for patients who cannot be generalized to the population [15]. They may also describe actual clinical practice including adherence to a specific intervention [15].
2. METHODS
To gain a better understanding of the efficacy and value of diabetes group visits for low-income and underserved participants, the authors performed a narrative review. The authors structured the review using the PICOS model: participants (individuals with type 2 diabetes), intervention (diabetes group visits), comparison (i.e., usual care), outcomes (behavioral, functional, metabolic, and system-level), and study design (nonrandomized including quasi-experimental (QE) and RCTs) [16]. Included studies specifically stated that patients were low-income or underserved i.e., low-income, underserved, indigent, underinsured, uninsured, resource-poor and participated in a diabetes group visit i.e., group medical visit, chronic care clinic, cluster visits, shared medical appointments, cooperative health clinics, drop-in group medical appointments. Based on published literature, the authors defined group visits as a program that comprises of education, goal development, signed confidentiality agreements, and an integrated primary care visit (e.g., referrals, physical examination, medication reconciliation) [4]. Authors excluded studies that did not perform group visits according to this definition. For example, although diabetes self-management education (DSME) classes may have overlap with group visits, they do not require an integrated primary care visit nor signed confidentiality agreements [4].
3. RESULTS
The authors grouped studies based on their overall design, nonrandomized or randomized. Within the nonrandomized studies, the authors further identified quasi-experimental (QE) studies, defined as nonrandomized, practice-based research that evaluate interventions in real world circumstances where RCTs may not be suitable or feasible [17]. Studies that included participants with an equal chance of being randomized into either a treatment or a control arm were categorized as randomized controlled trials. Table 1 and 2 summarize the included studies. Table 3 illustrates the outcome measures and instruments used in the studies.
Table 1.
Characteristics of diabetes group visits for low-income and underserved individuals in nonrandomized studies
| Study and Design | N I/C | Primary Race/Ethnicity | Setting | Frequency Duration | HbA1c | Significant findings *p-value not significant/not reported |
|
|---|---|---|---|---|---|---|---|
|
1. Bray et al., 2005[18, 19] Feasibility |
160 112/48 |
AA | Rural | Every 1-2 mo 6-mo (data: 12-mo) |
8.2 to 7.1% (I) 8.3 to 8.6% (C) |
HbA1c Preventive care Self-mgt |
|
|
2. Calhane-Pera et al., 2005[20] Pre/post |
277 39/238 |
Asian (Hmong) | Urban | Every 1-4 mo 13-mo |
9.5 to 9.6% (I) 8.7 to NR% (C) |
Mental health | |
|
3. Mallow et al., 2013[22, 23] Chart review |
111 53/58 |
White | Rural | Monthly 6-mo (data: 12-mo) | NR to 8.7% (I) NR to 7.5% (C) |
HbA1c (C<I) Blood pressure |
|
|
4. Vachon et al., 2007[24] Feasibility |
737 294/443 |
AA | Urban | Once or more (data: 17-mo) | 8.2 to NR% (I) 8.5 to NR% (C) |
Access to care* Preventive care* |
|
|
5. Dickman et al., 2011[25] QE |
37 | Hispanic | Urban | Monthly 4-mo | 7.3 to 7.0% (I) |
HbA1c* Blood pressure* Lipids* |
Exercise Access to care* Self-mgt |
|
6. Jessee et al., 2012[26] QE |
26 11/15 |
not reported | Rural | Weekly 3-weeks (data: 7 mo) | 9.3 to 7.3% (I) 9.0 to 8.1% (C) |
HbA1c, Glucose* Knowledge* Self-efficacy* |
|
|
7. Reitz et al., 2012[27] QE |
288 52/236 |
AA | Urban | Weekly 1-month | not reported | HbA1c Blood pressure |
|
AA-African American. I/C-Intervention/Control. NR-not reported. QE-quasi-experimental.
Table 2.
Characteristics of diabetes group visits for low-income and underserved individuals in randomized controlled trials
| Study | N I/C | Primary Race/ethnicity | Setting | Frequency Duration | HbA1c | Significant findings *p-value not significant/not reported |
|
|---|---|---|---|---|---|---|---|
| 1. Berry et al., 2015[28] | 80 40/40 |
AA | Urban | Quarterly 15-mo | 8.8 to 7.6% (I) 8.0 to 9.3% (C) |
HbA1c: I Preventive care Health status |
Heart rate Lipids |
| 2. Clancy et al., 2003[30–32] | 120 59/61 |
AA | Rural | Monthly 6-mo | 10.6 to 9.5% (I) 10.3 to 9.7% (C) |
Preventive care Physician trust Days in bed |
Culturally competent* Costs (I>C) |
| 3. Clancy et al., 2007[8, 33, 34] | 186 96/90 |
AA | Rural | Monthly 12-mo | 9.3 to 9.1%(I) 8.9 to 9.0% (C) |
Preventive care Ongoing care Culturally competent |
Community orientation Cost (I<C) |
| 4. Gutierrez et al., 2011[38] | 103 50/53 |
Hispanic | Suburban | Bimonthly 6-mo (data: 17-mo) | not reported | HbA1c: I, C Quality of life Preventive care |
Knowledge Lipids |
|
5. Schillinger et al., 2009[39, 40] |
339 112A/113B/114 |
Hispanic Asian AA |
Urban | Monthly 9-mo | 9.3 to 8.7%A 9.3 to 9.0%B 9.8 to 9.0% (C) |
Patient satisfaction Self-mgt Blood pressure |
Communication |
|
6. Vaughan et al., 2017[42] |
50 25/25 |
Hispanic | Urban | Monthly 6-mo | 8.7 to 8.0% (I) 8.3 to 8.2% (C) |
HbA1c: I Preventive care |
Weight loss Patient satisfaction |
| 7.Wagner et al., 2001[43] | 707 278/429 |
White | Suburban | Every 3-6 mo 24 mo |
7.5 to 7.9% (I) 7.4 to 7.9% (C) |
Preventive care Education Health status |
Days in bed Cost (I~C) |
ATSM-Automated Telephone Self-Management.
Group Visits.
AA-African American. I/C-Intervention/Control.
Table 3.
Overview of outcomes measures and instruments in studies that evaluated group visits in low-income and underserved settings
| Variable | n | Instrument (if applicable) |
|---|---|---|
| Metabolic/Physical | ||
| A1C | 14 | |
| Blood glucose | 2 | |
| Blood pressure | 9 | |
| Body mass index/body weight | 7 | |
| BUN/creatinine/urine microalbumin | 8 | |
| Heart rate | 1 | |
| Lipid profile | 12 | |
| Functional | ||
| Competence (orientation, cultural, healthcare) | 3 | Patient Care Assessment Tool[35] |
| DM knowledge/self-efficacy |
3 | Diabetes Empowerment Scale Short Form[53] Diabetes Knowledge Questionnaire[54] Diabetes Knowledge Test[55] |
| Health status | 3 | Subdomains of the SF-36[56] |
| Locus of control | 1 | Diabetes-Specific Locus of Control[36] |
| Mental health/anxiety/depression | 4 | Center for Epidemiologic Studies Depression Scale[57] Hmong-Hopkins Symptom Checklist-25[21] Short Form-12 (mental health)[58] |
| Quality of life | 3 | Short Form-12 Instrument[58] Diabetes Quality of Life Brief Clinical Inventory[59] |
| Behavioral | ||
| Annual physical exam | 1 | |
| Diabetes foot exam | 7 | |
| Diabetes self-management | 3 | Stanford Self-Management Questionnaire[29] The Summary of Diabetes Self-care Activities Measure (revised scale)[60] |
| Guideline concordance | 5 | American Diabetes Association[61] US Preventive Task Force[62] |
| Influenza/pneumonia vaccine | 4 | |
| Physical health/exercise | 3 | Modified Version of the Behavioral Risk Factor Surveillance System (BRFSS)[63] Short Form-12 (physical health)[58] |
| Retinal exam | 5 | |
| System-based | ||
| Access/barriers to care | 3 | |
| Cost: emergency department, outpatient, inpatient visits | 3 | |
| Emergency department visits | 3 | |
| Feasibility/acceptability | 4 | Primary Care Assessment Tool[35] Trust in Physician Scale[37] |
| Patient satisfaction | 2 | Patient Assessment of Chronic Illness Care[64] Primary Care Assessment Tool[35] |
| Physician trust/communication | 2 | Trust in Physician Scale[37] |
3.1. Nonrandomized Studies
A 12-month feasibility study of underserved patients (N=160) who received care in primary care practices in rural North Carolina compared group visits (intervention=112) to a control group (chart review of nonparticipating clinic patients, n=48) [18, 19]. For six months, participants attended four group visits led by a multidisciplinary team and received education and case management with an evaluation by an advanced practice nurse and physician. Median HbA1c in the intervention group improved (−1.1%, p<0.001), whereas the control group worsened (0.3%, p<0.05). The number of participants in the intervention group who met HbA1c target levels (<7% (53 mmol/mol)) also improved (p<0.01) [19]. In addition, the program improved self-management goals (0 to 42%), aspirin use (25 to 37%), diabetes foot examinations (12 to 54%), lipid profile (55 to 76%), and average daily encounter rate (20.2 to 31.6). Investigators considered the advanced practice nurse a key component of the results [18].
A 13-month pre/post study of Hmong refugees (N=277) in St. Paul, Minnesota compared group visits (intervention=39) to a control group (chart review of nonparticipating clinic patients, n=238) [20]. HbA1c levels slightly worsened in the intervention group (0.1%). Twelve-month HbA1c values were not reported for the control group. There were no other statistically significant metabolic outcomes. Mental health measured by Hmong-Hopkins Symptom Checklist-25 [21] improved in the intervention group (p<0.05) but was not measured in the control patients. Investigators suggested that study duration, patient medication resistance, and social or cultural barriers to change contributed to the lack of positive metabolic outcomes [20].
A retrospective chart review in rural West Virginia explored the characteristics of low-income, uninsured individuals (N=111) who chose a six-month group program (intervention=53) to nonparticipating clinic patients (control=60) [22, 23]. HbA1c levels were significantly higher at baseline and 12-months in the intervention group (p<0.001) [22, 23]. Specific baseline HbA1c numbers were not reported, but 12-month values were 8.7% (72 mmol/mol) and 7.5% (58 mmol/mol) in the intervention and control groups, respectively. The intervention group also had higher baseline BMI, depression, and pain levels when compared to the control group. There were no significant metabolic differences after one year between groups, but blood pressure significantly decreased (p<0.05) within the intervention group. The majority of participants attended two or fewer group visits in the 12-month period yet the amount of visits (range 1-6) did not impact outcomes [23]. Investigators recommended seeking patient input for study design and that overcoming barriers of attendance and attrition may improve study outcomes [22, 23].
A 22-month group visit study among low-income patients (N=737) in Chicago, Illinois compared group visits (intervention=294) to chart review data from nonparticipating clinic patients (control=443) [24]. Group visits were offered monthly and participants could choose to come one day or more during subsequent months. The visits consisted of a multidisciplinary team who led several stations during a four-hour period. Stations included comprehensive diabetes care (i.e., foot and eye exams, medication reconciliation, laboratory testing, vaccinations, and classes including exercise and nutrition). The analysis included patients who attended at least one day. The intervention group did not have significant baseline or 22-month differences (i.e., gender, race, clinical measures) compared to the control group. Twenty percent of participants attended at least four sessions. Investigators found that the program increased access to care (p-value not reported). Investigators developed this station-based group visit strategy in response to the high attrition rates (74% drop-out) observed during previous group visit programs (series of visits for 12-months), in spite of cash incentives. The multi-station approach was found to be feasible and an avenue to provide comprehensive care in this setting [24].
3.2. Quasi-Experimental (QE) Studies
A four-month pre/posttest QE study for low-income, uninsured participants (N=37) at a free clinic in Fairfax, Virginia compared a three-armed group visit program: English (n=11), Spanish (n=15), bilingual (n=11) [25]. The descriptive analysis revealed improved HbA1c (−0.25%), LDL (−4 mg/dL), and systolic blood pressure (−30 mmHg) (individual study arm and statistical significance results were not provided). The intervention also resulted in improved physical activity (p<0.01) with males reporting longer exercise intervals than females (p<0.01). Almost all participants successfully identified goals and reported achieving or almost achieving their goals (97%). Authors noted the need and importance for future studies to address the impact of language-specific diabetes group visits on patient self-management behaviors [25].
A three-week prospective QE study of underserved Appalachian patients (N=26) in southwest Virginia compared participants in group visits (intervention=11) to those not randomly enrolled into usual care (control=15) [26]. Both groups improved metabolic outcomes including blood glucose (intervention: −50.4 mg/dL, control: −21.6mg/dL) and HbA1c (intervention: −2.0%, control: −0.9%), and self-efficacy (statistical significance not reported). Knowledge scores increased in the intervention group only. Barriers to care consisted of transportation (i.e., fuel), time, family, and work. These group visits were feasible, but in order to expand the study, barriers to care need to be addressed [26].
A one-month QE pre/post study of low-income patients (N=288) in Philadelphia, Pennsylvania compared group visits (intervention=52) to case-matched (gender, age, race/ethnicity, zip code) nonparticipants in usual care (control=236) [27]. Primary outcomes were metabolic and were gathered seven months after the group visits. More individuals in the intervention group achieved target HbA1c (<7% (53 mmol/mol)) and blood pressure (<140/90) values but not optimal LDL levels (<100 mmol/L) when compared to the control group (p<0.01, p<0.05, p=0.67, respectively). Overall, the intervention group had a greater percent HbA1c reduction (76.9% vs. 54.3%, p<0.01). Attendance was variable: patients averaged 2.7 sessions (SD+2.8, median 1) and 46% attended three or more sessions. Investigators suggested that group visits are effective in an urban, minority population [27].
3.3. Conclusions for Nonrandomized Studies
From these seven nonrandomized studies, it is clear that diabetes group visits are feasible in low-income and underserved settings. A common outcome measure, preventive care, was effective overall. The three QE studies suggest that glycemic control improves as a result of group visits in these settings.
3.4. Review of Randomized Controlled Trials
A 15-month cluster randomized repeated measures study (N=80) of low-income patients in Raleigh, North Carolina compared group visits (intervention=40) to individual care (control=40) [28]. Individual care consisted of a total of five quarterly one-on-one sessions during a 15-month time period. The investigators designed an interdisciplinary approach for the group visits with eight providers and analyzed the efficacy of group visits tailored to low-income, urban individuals. Compared to the control group, the intervention group had significant improvements of HbA1c (p=0.001), HDL (p<0.05), triglycerides (p<0.01), and heart rate (p<0.05). Within the control group, HbA1c, LDL, triglycerides, and heart rate worsened. Participants in the intervention group also had a significant difference in the number of foot exams compared to the control group (p=0.049). The majority of the responses on the 52-question Stanford Self-Management Questionnaire [29] were not significant between groups. Study conclusions suggested that diabetes group visits for low-income, urban population were beneficial, reducing the likelihood of diabetes sequelae [28].
A six-month feasibility and acceptability RCT of uninsured or inadequately insured patients (N=120) in rural South Carolina compared group visits (intervention=59) to usual care in the clinic (control=61) [30–32]. Group visits were co-led by a general internist and a diabetes nurse educator. HbA1c levels improved [intervention: −1.0%, control: −0.5%) and lipid levels also decreased but were not statistically significant compared to the control group. A mixed model analysis of clinical outcomes implied that the intervention group had greater improvement, though this finding was also not significant (p=0.095-0.590). The intervention participants showed significant concordance with American Diabetes Association standards compared to the control group (p<0.001) [30, 31. The intervention patients had higher overall costs (emergency room, inpatient, outpatient, p<0.001). In addition, the intervention group improved trust in physicians (p<0.05) and, while not statistically significant, showed positive trends in other areas including: community orientation (p=0.096), cultural competency (p=0.096), and coordination of care (p=0.07) [30, 32]. Investigators found group visits as a form of healthcare delivery feasible and acceptable [32].
These investigators subsequently performed a larger trial (N=186; intervention=96) in the same setting that was longer in duration (12-months) and involved multiple providers [8, 33, 34]. This study resulted in similar outcomes as the prior study: there were no significant metabolic outcomes including HbA1c (intervention: −0.2, control: 0.1%), lipid levels, or blood pressure compared to control group. The intervention group also had greater guideline concordance (p<0.001) and cancer screening rates (breast: p<0.01; cervical: p<0.05) compared to the control group [33]. The intervention participants had higher scores on the Primary Care Assessment Tool [35] (ongoing care, p=0.001; community orientation, p<0.001; cultural competence, p<0.05) and in components of the Diabetes-Specific Locus of Control [36] survey. The higher scores on the Trust in Physician Scale [37] observed among intervention participants in the six-month study (p<0.05) were not replicated in the 12-month study [30, 32, 34]. Group visit (intervention) participants had less total cost expenditures (p<0.05). A treatment effect model suggested that group visits may be used in lieu of more costly specialist appointments [8. Authors concluded that modifications to group visits are needed for improved clinical outcomes while maintaining guideline concordance and cost efficiency integrity [8, 33, 34].
A descriptive, feasibility study of uninsured, indigent Hispanics (N=103) in the Texas metropolitan area compared 50 intervention patients to 53 controls (usual care in the clinic) and collected data for 17 months [38]. Both the intervention and control groups significantly decreased HbA1c levels (intervention: −1.19%, p<0.01; control: −0.67%, p<0.05). The intervention group also significantly improved quality-of-life (p<0.01), diabetes knowledge (p<0.01), aspirin use (p<0.01), lipid profile measurement (p<0.05), pneumococcal vaccine (p<0.05), and obtained eye (p<0.01), foot (p<0.01) and annual (<0.05) examinations, whereas the control group only significantly improved in foot examinations (p<0.05). Investigators noted that this was the first group visit RCT reporting a Hispanic-only population and suggested using the group visit structure in lieu of traditional models [38].
A 12-month, clinical trial of low-income patients (N=339) who received care in county-run clinics in San Francisco compared three arms: a weekly automated telephone self-management support (n=112), group visits (n=113), and usual care in the clinic (n=114) [39]. All three arms did not result in statistical differences for HbA1c levels when compared to each other. Group visits improved in Patient Assessment of Chronic Illness Care scores (p<0.01) and telephone support significantly increased communication processes (p<0.05). In addition, the telephone support group resulted in fewer days in bed per month than individuals in usual care (−1.7 days, p=0.05) and group visits (−2.3 days, p<0.01). Overall, telephone support appeared most effective in improving diabetes self-management behavior and quality of life. All three modalities improved clinical outcomes [39].
A subsequent analysis of this study evaluated the influence of patient characteristics including age, ethnicity, income, and sex on the Patient Assessment of Chronic Illness Care scores [40, 41]. At baseline, being female (p<0.05), having a low-income (p<0.01), and an older age (p<0.05) were associated with lower ratings. African American and Asian ethnicities had higher baseline scores compared to whites though not statistically significant (p=0.076, p=0.045, respectively). Patient characteristics appeared to influence their perceptions of healthcare quality independent of clinical processes [40].
A six-month feasibility study of low-income Hispanic patients (N=50) in Houston, Texas compared group visit participants that integrated Community Heath Workers as part of the leadership team (intervention=25) to patients who received usual care in the clinic (control=25) [42]. The main measures included baseline and six-month metabolic outcomes (i.e., HbA1c, blood pressure) in addition to concordance with eight US Preventive Task Force and American Diabetes Association standards (i.e., colon, breast, and cervical cancer screening). When compared to the control group, the intervention participants resulted in superior clinical outcomes and standard concordance for target HbA1c levels (p<0.05), retinal screening tests (p<0.001), diabetes foot exams (p<0.001), mammograms (p<0.01), and urine microalbumin (p<0.01). Additionally, more individuals in the intervention group lost weight (p<0.01), whereas a greater number of control participants gained weight (p<0.05). Patients expressed high satisfaction levels with Community Health Workers as part of the leadership team (mean 9.7/10). Authors noted that the study was the first reported to integrate Community Health Workers as part of the diabetes group visit leadership team and attributed the study findings to their involvement (i.e., overcoming barriers of medication adherence by improved cultural competency, weekly contact via texts/phone calls) [42].
A 24-month study of low-income patients (N=707, intervention=278) in Puget Sound, Washington compared primary care practices randomized to the intervention (group visits) and control (usual care in the clinic) [43]. For both groups, HbA1c levels worsened (intervention: 0.4%, control: 0.5%; p=0.99) but total cholesterol improved (p=0.58). The intervention group resulted in better preventive care procedures (p<0.05), including microalbumin testing (p<0.05). Participants found the education materials (written, classes, face-to-face) beneficial (p<0.05, p<0.001, p<0.001; respectively), but there were no significant differences in satisfaction of medical (p=0.96) or diabetes care (p=0.10) between groups. General health status (p<0.05) and bed disability days (p<0.05), but not depression scores (p=0.87), were better in the intervention group. Total costs (primary care, emergency department, specialty visits, hospital admissions) were not significant (p=0.79) between groups. Authors concluded the group visit structure met the complex needs of patients with diabetes without excess burden on the healthcare system or worsening of glycemic control compared to usual care [43].
3.5. Conclusions for Randomized Controlled Trials
These seven RCTs clearly demonstrate that preventive care improves as a result of diabetes group visits. These data also suggest that, compared to usual care, participants in diabetes group visits will have equivalent or better glycemic control. Yet, further examination is needed to standardize HbA1c measurements (i.e., mean HbA1c, target HbA1c, or both) and to determine if this is the most appropriate main outcome given the short duration of classes. Further, though group visits reach many individuals at once, they require a large amount of resources and personnel. Cost analyses remain indeterminate and, therefore, investigations are needed to elucidate the resource-effectiveness of these programs.
3.6. Summary of Results
The authors identified a total of 14 diabetes group visit studies for underserved and low-income populations. These included seven nonrandomized studies (three QEs) and seven RCTs. Of these studies all participants were adults. African Americans were the most represented (46%) while Hispanics, Whites, and Asians were underrepresented (31%, 17%, 8%, respectively). More studies are needed in other races/ethnicities to determine if group visits are more efficacious within certain population subgroups.
The average study evaluated 230 patients (mean: intervention=94, control=164) and met every 5.7 weeks for 8.4 months. All studies consisted of a multidisciplinary team. With the exception of one study [43], more females attended group visits than males. Half (50%) of the studies were conducted in urban environments and 36% occurred in rural areas. The authors did not identify any studies conducted outside of the US. There is a concern of the variability in size of the control versus the intervention groups, particularly in the nonrandomized studies. Additionally, there is a need for future studies that focus on male retention to assess the efficacy of these programs for men versus women. This knowledge is important to understand target recruitment, particularly for programs that expand beyond the US.
Standardization of outcomes measured for group visits is critical to allow for the expansion and robust analysis of programs’ value. The authors combined outcome measures if similar (i.e., depression and anxiety) (Table 3). However, prior to this grouping, the authors identified 50 different measured outcomes and 23 types of instruments used. Although all studies evaluated HbA1c outcomes, analysis of metabolic, functional, behavioral, and system-based outcomes differed across studies.
4. DISCUSSION
The most commonly observed pattern for patients who participated in a diabetes group medical visit was improved preventive care (i.e., foot exam, cancer screening). This pattern is likely due to the structure of group visits, which promotes continuity of care, ongoing follow-up, and the ability to build on educational principles. This contrasts with individual care where, particularly in underserved settings, patients face poor access to care and suboptimal disease management [24] Preventive care is of particular importance in diabetes in order to reduce the risk of its negative additive effects on other chronic diseases or conditions [44]. Yet, US adults with diabetes receive inadequate preventive care compared to other countries [45].
With the exception of one study [42], the authors noted an inability of group visits to significantly reduce participant weight. This pattern is also evident in diabetes group visits for the general population [2, 7]. Weight loss is a challenging and complex epidemic that requires shifting paradigms around the causes [46]. Poor socioeconomic settings bring additional challenges including lack of food availability and financial constraints to consume healthy food [12]. It is possible that Community Health Workers played a role in the study with significant weight loss findings by assisting patients in overcoming social barriers to healthy eating [42].
An advantage to group visits in underserved settings is consistent access to care. Nevertheless, attrition remains problematic in this population [47]. Of the studies included in this review, programs with intermittent follow-up between visits, such as from nurses or Community Health Workers, had fewer issues with attrition [18, 19, 42]. Rationale for this includes a personal contact for patients in order to answer questions, provide reminders, and assist in medication adherence.
4.1. Glycemic Control
In the general population, systematic reviews have consistently shown that diabetes group visits have a positive impact on HbA1c levels [3, 4, 7]. Yet, the current study revealed a paucity of data in low-income and underserved settings and, therefore, an inability to make definitive conclusions regarding glycemic outcomes. Of the 14 studies the authors identified, most resulted in improved HbA1c levels, but many did not reach statistical significance when compared to the control group (Tables 1, 2). For example, four of 14 studies resulted in significantly lower HbA1c levels: two RCTs [28, 42] and two nonrandomized (one QE) studies [18, 19, 27]. Trends in these four studies include minority participants (n=3 African American, n=1 Hispanic), six-month median duration, and inclusion of preventive care or a diabetes self-management/self-efficacy component.
Seven of the 14 studies showed glycemic improvement but investigators either did not report statistical significance or the control and intervention groups improved similarly [24–26, 30–34, 38, 39]. Trends in these studies are similar to the three that showed statistical significance including in minorities and study duration. Furthermore, three of the 14 studies resulted in worsened HbA1c values: a retrospective chart review where the intervention group started and ended significantly higher [22, 23], a RCT where both groups increased similarly [43], and a nonrandomized study in which the intervention increased 0.1% and the control group was not reported [20]. Commonalities in these three negative studies included White or Asian ethnicities and a varied meeting frequency.
One reason for the variation of glycemic control in low-income participants may be related to medication adherence. Financial and social situations are determinants of health and are often barriers to obtaining medications for underserved individuals [12]. For example, a patient who is not able to buy medications during a group visit study but is able to afterwards, or visa versa, will skew the results. In the US, two oral hypoglycemic classes (biguanides, sulfonylureas) are available at a low cost ($4/month) at major pharmaceutical retailers. Pioglitazone is available at a low-cost (e.g., $8/month) with coupons though navigating this system can be cumbersome. Additionally Regular, NPH, and 70/30 insulins are offered at discounted rates ($25/vial) at limited pharmacies but are associated with additional expenses due to test strips, lancets, and syringes [48].
4.2. Future Studies
To fully understand the benefits of diabetes group visits and appropriate outcome measures, program standardization is vital. Currently, the literature on group visits in low-income populations is difficult to compare due to variable methodology and multiple outcome measures. The need for standardization and rigorous evaluation has also been clearly expressed for group visits in the in the general population [4, 9].
One difficulty in standardization is determining appropriate main outcomes. For example, qualitative data provides important insight but would be difficult to standardize. Though glycemic control, specifically HbA1c, is an important outcome, it may not be the best marker to determine the long-term value of these programs since red blood cells turnover every three months and most programs last six months or less. Standardizing clinically meaningful outcomes measures for diabetes is a recognized need by numerous societies [49]. For low-income settings in particular, this marker may not be reliable due to the fluidity of socioeconomic barriers (e.g., transportation, finances, employment). In this life-long disease, longitudinal HbA1c values are needed to clearly understand the impact of these programs. Meeting preventive care measures including the American Diabetes Association or US Preventive Task Force standard concordance may be more suitable to determine the efficacy of these programs. While their impact is long-term, objective data may be obtained short-term. They provide vital information for diabetes care that can be standardized across studies, allowing for a systematic review process.
Another important consideration is sustainability of clinical outcomes once patients return to clinical care. One systematic review found that though some group visit studies may last for several years, the long-term effects once discharged from the programs were unclear [7]. However, a recent review found that the clinical outcomes obtained during diabetes group visits were sustained long-term [50]. Specifically, at a minimum of nine months and up to three years after discharge from diabetes group visits, patients maintained their diabetes and cardiovascular outcomes [50].
Since research in diabetes group visits for this population outside of the US is scant, generalization of findings may be limited. However, there are several areas that show promise in expanding diabetes group visits beyond the US. For example, outcomes in differing forms of group visits in other developed nations appear to be similar [51]. Also, though all investigations in the current study used a multidisciplinary approach, most were a simple team such as a physician and a nurse or dietitian. Additionally, one study found that the multidisciplinary approach of a physician and Community Health Workers improved diabetes and other healthcare outcomes [42]. Community Health Workers are frontline workers who are well known to low- and middle-income countries as they have played a critical role in the delivery of healthcare [52]. The group visit model could be a pivotal strategy among resource-poor nations to reach more patients. Future work should address infrastructural challenges to translating the group visit model to resource-poor countries.
5. CONCLUSION
The current study demonstrated common patterns of diabetes group visit studies that improved glycemic control including consistent meeting frequency, six-month duration, African American and Hispanic ethnicities, and incorporating preventive care. Meeting consistency reduces the likelihood of forgetting appointments or medications. A longer duration allows time for patient education, obtaining coupons, finding optimal dosing, etc. Preventive care involves patients into their care. Given the potential of group interventions, further work is warranted that addresses program standardization, barriers to medication adherence, integrating and boosting programs with other healthcare personnel including Community Health Workers, and the system burden of the intervention.
6. ACKNOWLEDGEMENTS
The National Institutes of Health, National Institute of Diabetes, Digestive, and Kidney Diseases have supported this work, Federal Award Identification Number K23DK110341.
Footnotes
Conflicts of Interest. None
Contributor Information
Elizabeth M. Vaughan, Email: elizabeth.vaughan@bcm.edu.
Craig A. Johnston, Email: cajohn25@Central.UH.EDU.
Katherine R. Arlinghaus, Email: krarling@Central.UH.EDU.
David J. Hyman, Email: dhyman@bcm.edu.
John P. Foreyt, Email: jforeyt@bcm.edu.
REFERENCES
- 1.World Health Organization. Global report on diabetes. Geneva, CH: World Health Organization; 2016. [Google Scholar]
- 2.Riley SB, Marshall ES Group visits in diabetes care: A systematic review. Diabetes Educ. 2010;36(6):936–944. [DOI] [PubMed] [Google Scholar]
- 3.Edelman D, Gierisch JM McDuffie JR, Oddone E, Williams JW, Shared medical appointments for patients with diabetes mellitus: A systematic review. J Gen Intern Med. 2015;30(1):99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burke RE, OGrady ET Group visits hold great potential for improving diabetes care and outcomes, but best practices must be developed. Health Affairs. 2012;31(1):103–109. [DOI] [PubMed] [Google Scholar]
- 5.Davis A, Sawyer DR, Vinci LM The potential of group visits in diabetes care. Clin Diabetes. 2008;26(2):58–62. [Google Scholar]
- 6.Burke RE, Ferrara SA, Fuller AM, Kelderhouse JM, Ferrara LR The effectiveness of group medical visits on diabetes mellitus type 2 (DM2) specific outcomes in adults: A systematic review. JBI Libr Syst Rev. 2011;9(23):833–885. [DOI] [PubMed] [Google Scholar]
- 7.Housden L, Wong ST, Dawes M Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ. 2013;185(13):E635–E644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clancy DE, Dismuke CE, Magruder KM, Simpson KN, Bradford D Do diabetes group visits lead to lower medical care charges? Am J Manag Care. 2008;14(1):39–44. [PubMed] [Google Scholar]
- 9.Kirk JK, Devoid HM, Strickland CG, Educational strategies of diabetes group medical visits: A review. Curr Diab Rev. 2018;14(3):227–236. [DOI] [PubMed] [Google Scholar]
- 10.Purnell TS, Calhoun EA, Golden SH, Halladay JR, Krok-Schoen JL, Appelhans BM, et al. Achieving health equity: Closing the gaps in health care disparities, interventions, and research. Health Aff (Millwood). 2016;35(8):1410–1415. [DOI] [PubMed] [Google Scholar]
- 11.Dinca-Panaitescu S, Dinca M, Bryant T, Raphael D, Diabetes prevalence and income: Results of the Canadian Community Health Survey. Health Policy. 2011;99(2):116–123. [DOI] [PubMed] [Google Scholar]
- 12.Gaskin DJ, Thorpe RJ Jr., McGinty EE, Bower K, Rohde C, Young JH, et al. Disparities in diabetes: The nexus of race, poverty, and place. Am J Public Health. 2014;104(11):2147–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lang T The challenges and opportunities of conducting a clinical trial in a low resource setting: The case of the Cameroon mobile phone SMS (CAMPS) trial, an investigator initiated trial. Trials. 2011;12:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kunutsor SK, Walley J Randomized controlled trial designs for operations research in low-income countries: Reality or delusion? Front Public Health. 2013; 1(14). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onder G The advantages and limitations of observational studies. G Ital Cardiol (Rome). 2013;14(3 Suppl 1):35–39. [DOI] [PubMed] [Google Scholar]
- 16.Institute of Medicine (US) committee on standards for systematic reviews of comparative effectiveness research; Editors: Eden J, Levit L, Berg A, Morton S Finding what works in health care: Standards for systematic reviews. Washington DC: National Academy of Sciences; 2011. [PubMed] [Google Scholar]
- 17.Handley MA, Schillinger D, Shiboski S Quasi-experimental designs in practice-based research settings: Design and implementation considerations. J Am Board Fam Med. 2011;24(5):589–596. [DOI] [PubMed] [Google Scholar]
- 18.Bray P, Roupe M, Young S, Harrell J, Cummings DM, Whetstone LM Feasibility and effectiveness of system redesign for diabetes care management in rural areas: The Eastern North Carolina experience. Diabetes Educ. 2005;31(5):712–718. [DOI] [PubMed] [Google Scholar]
- 19.Bray P, Thompson D Wynn JD, Cummings DM, Whetstone L Confronting disparities in diabetes care: The clinical effectiveness of redesigning care management for minority patients in rural primary care practices. J Rural Health. 2005;21(4):317–321. [DOI] [PubMed] [Google Scholar]
- 20.Culhane-Pera KA, Peterson KA, Crain AL, Center BA, Lee M, Her B, et al. Group visits for Hmong adults with type 2 diabetes mellitus: A pre-post analysis. J Health Care Poor Underserved. 2005;16(2):315–327. [DOI] [PubMed] [Google Scholar]
- 21.Mouanoutoua VL, Brown L Hopkins Symptom Checklist-25, Hmong Version: A screening instrument for psychological distress. J Pers Assess. 1995;64(2):376–383. [DOI] [PubMed] [Google Scholar]
- 22.Mallow JA, Theeke LA, Whetsel T, Barnes ER, Diabetes group medical visits and outcomes of care in low-income, rural, uninsured persons. Open J Nurs. 2013;3(3):314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mallow JA, Theeke LA, Barnes ER, Whetsel T Examining dose of diabetes group medical visits and characteristics of the uninsured. West J Nurs Res. 2015;37(8):1033–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vachon GC, Ezike N, Brown-Walker M, Chhay V, Pikelny I, Pendergraft TB Improving access to diabetes care in an inner-city, community-based outpatient health center with a monthly open-access, multistation group visit program. J Natl Med Assoc. 2007;99(12):1327–1336. [PMC free article] [PubMed] [Google Scholar]
- 25.Dickman K, Pinz C, Gold K, Kivlahan C Behavior changes in patients with diabetes and hypertension after experiencing shared medical appointments. J American Academy of Nurse Practiioners. 2011;2012(24):43–51. [DOI] [PubMed] [Google Scholar]
- 26.Jessee BT, Rutledge CM Effectiveness of nurse practitioner coordinated team group visits for type 2 diabetes in medically underserved Appalachia. J Am Acad Nurse Pract. 2012;24(12):735–743. [DOI] [PubMed] [Google Scholar]
- 27.Reitz JA, Sarfaty M, Diamond JJ, Salzman B The effects of a group visit program on outcomes of diabetes care in an urban family practice. J Urban Health. 2012;89(4):709–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berry DC, Williams W, Hall EG, Heroux R, Bennett-Lewis T Imbedding interdiciplinary diabetes group visits into a community-based medical setting. Diabetes Educ. 2015;42(1):96–107. [DOI] [PubMed] [Google Scholar]
- 29.Stanford chronic disease self-management study psychometrics of the chronic disease self-management program questionnaire; Editors: Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, et al. Outcome measures for health education and other health care interventions. Thousand Oaks, CA, US: Sage Publications; 1996. [Google Scholar]
- 30.Clancy DE, Brown SB, Magruder KM, Huang P Group visits in medically and economically disadvantaged patients with type 2 daibetes and their relationships to clinical outcomes. Top Health Inf Manage 2003;24(1):8–14. [PubMed] [Google Scholar]
- 31.Clancy DE, Huang P, Cope DW, Wolfman TE, Magruder KM Evaluating concordance to American Diabetes Association standards of care for type 2 diabetes through group visits in an uninsured or inadequately insured patient population. Diabetes Care. 2003;26:2032–2036. [DOI] [PubMed] [Google Scholar]
- 32.Clancy DE, Cope DW, Magruder KM, Huang P, Salter KH, Fields AW Evaluating group visits in an uninsured or inadequately insured patient population with uncontrolled type 2 diabetes. Diabetes Educ. 2003;29(2):292–302. [DOI] [PubMed] [Google Scholar]
- 33.Clancy DE, Huang P, Okonofua E, Yeager D, Magruder KM Group visits: Promoting adherence to diabetes guidelines. J Gen Intern Med. 2007;22(5):620–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clancy DE, Yeager DE, Huang P, Magruder KM Further evaluating the acceptability of group visits in an uninsured or inadequately insured patient population with uncontrolled type 2 diabetes. Diabetes Educ. 2007;33(2):309–314. [DOI] [PubMed] [Google Scholar]
- 35.Shi L, Starfield B, Xu J Validating the adult primary care assessment tool. J Fam Pract. 2001;50:161–170. [Google Scholar]
- 36.Peyrot M, Rubin RR Structure and correlates of diabetes-specific locus of control. Diabetes Care. 1994;17:994–1001. [DOI] [PubMed] [Google Scholar]
- 37.Anderson LA, Dedrick RF Development of the trust in physician scale: A measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67:1091–1100. [DOI] [PubMed] [Google Scholar]
- 38.Gutierrez N, Gimpel NE, Dallo FJ, Foster BM, Ohagi EJ Shared medical appointments in a residency clinic: An exploratory study among Hispanics with diabetes. Am J Manag Care. 2011;17(6):e212–e214. [PubMed] [Google Scholar]
- 39.Schillinger D, Wang F, Handley M, Hammer H Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes. Diabetes Care. 2009;32:559–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wallace A, Perkhounkova Y, Tseng H, Schillinger D Influence of patient characteristics on assessment of diabetes self-management support. Nurs Res. 2013;62(2):106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Green SM Development and validation of the patient assessment of chronic illness care. Med Care. 2005;43(436):436–444. [DOI] [PubMed] [Google Scholar]
- 42.Vaughan EM, Johnston CA, Moreno JP, Cardenas VC, Foreyt JP Integrating CHWs as part of the team leading diabetes group visits: A randomized controlled feasibility study. Diabetes Educ. 2017;43(6):589–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wagner EH, Grothaus LC, Sandhu N, Galvin MS, McGregor M, Artz K, et al. Chronic care clinics for diabetes in primary care: A system-wide randomized trial. Diabetes Care. 2001;24(4):695–700. [DOI] [PubMed] [Google Scholar]
- 44.Wee HL, Cheung YB, Li SC, Fong KY, Thumboo J The impact of diabetes mellitus and other chronic medical conditions on health-related quality of life: Is the whole greater than the sum of its parts? Health Qual Life. 2005;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schoen C, Osborn R, How SK, Doty MM, Peugh J In chronic condition: Experiences of patients with complex health care needs, in eight countries, 2008. Health Affairs. 2009;28(1):w1–w16. [DOI] [PubMed] [Google Scholar]
- 46.Frood S, Johnston LM, Matteson CL, Finegood DT Obesity, complexity, and the role of the health system. Curr Obes Rep. 2013;2(4):320–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kuo CR, Quan J, Kim S, Tang AH, Heuerman DP, Murphy EJ Group visits to encourage insulin initiation: Targeting patient barriers. J Clin Nurs. 2017;26(11-12):1705–1713. [DOI] [PubMed] [Google Scholar]
- 48.Yeaw J, Lee WC, Aagren M, Christensen T Cost of self-monitoring of blood glucose in the United States among patients on an insulin regimen for diabetes. J Manag Care Pharm. 2012;18(1):21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Agiostratidou G, Anhalt H, Ball D, Blonde L, Gourgari E, Harriman KN, Kowalski AJ, et al. Standardizing clinically meaningful outcome measures beyond HbA1c for type 1 diabetes: A consensus report of the American Association of Clinical Endocrinologists, the American Association of Diabetes Educators, the American Diabetes Association, the Endocrine Society, JDRF International, The Leona M. and Harry B. Helmsley Charitable Trust, the Pediatric Endocrine Society, and the T1D Exchange. Diabetes Care. 2017;40(12):1622–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leung AK, Buckley K, Kurtz J Sustainability of clinical benefits gained during a multidisciplinary diabetes shared medical appointment after patients return to usual care. Clinical Diabetes. 2018;36(3)226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong ST, Browne A, Lavoie J, Macleod MLP, Chongo M, Ulrich C Incorporating group medical visits into primary healthcare: Are there benefits? Health Policy. 2015;11(2)27–42. [PMC free article] [PubMed] [Google Scholar]
- 52.Pallas SW Minhas D, Perez-Escamilla RP, Taylor L, Curry L, Bradley EH Community Health Workers in low- and middle-income countries: What do we know about scaling up and sustainability? Am J Public Health. 2013; 103(7)e74–e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Anderson RM, Fitzgerald JT, Gruppen LD, Funnell MM, Oh MS The diabetes empowerment scale-short form (DES-SF). Diabetes Care. 2003;26(5):1641–1642. [DOI] [PubMed] [Google Scholar]
- 54.Garcia AA, Villagomez ET, Brown SA, Kouzekanani K, Hanis CL The Starr County Diabetes Education Study: Development of the Spanish-language Diabetes Knowledge Questionnaire. Diabetes Care. 2001;24(1 and 5):16–21 and 972. [DOI] [PubMed] [Google Scholar]
- 55.University of Michigan Diabetes Research Center. Survey Instruments: Diabetes Knowledge Test. Last accesssed November 1, 2018 Available from: http://diabetesresearch.med.umich.edu/Tools_SurveyInstruments.php#dkt.
- 56.Stewart AL, Hays RD, Ware JE The MOS short-form general health survey. Reliability and validity in a patient population. 1988; 26(7):724–735. [DOI] [PubMed] [Google Scholar]
- 57.Radloff LS The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 58.Ware J Jr., Kosinski M, Keller SD A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 59.Burroughs TE, Desikan R, Waterman BM, Gilin D, McGill J Development and validation of the Diabetes Quality of Life Brief Clinical Inventory. Diabetes Spectr. 2004;17(1):41–49. [Google Scholar]
- 60.Toobert DJ, Hampson SE, Glasgow RE The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. [DOI] [PubMed] [Google Scholar]
- 61.American Diabetes Association. Standards of medical care in diabetes 2017. Diabetes Care. 2017;40(S1):S1–S134. [DOI] [PubMed] [Google Scholar]
- 62.US Preventive Services Task Force. Published Recommendations. Last accesssed November 1, 2018 Available from: https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations.
- 63.Behavrioal Risk Factor Surveillance System. Behavioral risk factor surveillance survey: Comparability of data BRFSS 2013. Atlanta, GA, US: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 64.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Green SM Development and validation of the patient assessment of chronic illness care. Med Care. 2005;43(436):436–444. [DOI] [PubMed] [Google Scholar]


