Abstract
Non-communicable diseases (NCDs) are a major cause of deaths globally, and cardiovascular disease (CVD) is the leading cause of these deaths. 42% of NCD deaths are premature (occurring before the age of 70 years). As part of the United Nations 3rd Sustainable Development Goal (SDG) on health and wellbeing, target 3.4 is to reduce premature mortality from NCDs by one third between 2015 and 2030. This target adds to the World Health Organization (WHO) target of reducing premature deaths from NCDs by 25% between 2010 and 2025. As diabetes is a major risk factor for CVD, it is important to account for the trends in diabetes when considering premature CVD mortality. We aimed to describe the global trends in diabetes prevalence and mortality, critically review the literature on the estimated attainability of the WHO and SDG targets, and determine if and how these studies accounted for trends in diabetes. Worldwide, the prevalence of diabetes is rising, with an estimated 9.0% global prevalence in adults aged 20–69 by 2030, and low- and middle-income countries (LMICs) having the largest increase of the burden in absolute numbers and age-standardized prevalence. There is a lack of data from most LMICs on the excess CVD mortality associated with diabetes and therefore no consensus on the global risk of CVD mortality in people with diabetes. Where data do exist, there are discrepancies between studies on the direction of mortality trends from diabetes over time. We reviewed 12 studies that estimated the attainability of the WHO or SDG targets for premature NCD mortality. Seven of these considered the potential impacts of achieving the 2025 WHO risk factor targets. Six studies modelled the impact of current trends in risk factors, including diabetes, continuing toward the target dates. Four studies compared this ‘business as usual’ model with the attainment of the risk factor targets for the world as whole and individual regions, 2 studies for NCD mortality overall, and 2 specifically for CVD mortality. On the impact of diabetes with regards to attainment of the WHO or SDG targets for premature CVD mortality, the overall results were inconclusive. Some concluded that none of the countries or regions considered would meet the targets, and others predicted that in some areas, the targets would be met. Examining the potential impact of trends in diabetes on future CVD mortality rates in LMICs is limited by a relative lack of high quality studies, including on the age specific excess mortality associated with diabetes. Filling these data gaps will enable better estimates of the potential impacts on future CVD mortality of the rapidly increasing prevalence of diabetes in LMICs and help to better inform health policy and the attainment of SDG target 3.4.
Keywords: Cardiovascular diseases (CVD), diabetes mellitus, mortality, premature
Introduction
Non-communicable diseases (NCDs) such as cardiovascular disease (CVD), diabetes, chronic respiratory disease and cancers are a significant cause of death worldwide. The Global Burden of Disease study (GBD) estimated that deaths from NCDs accounted for 72.3% of all deaths globally in 2016 (1). The WHO reported that CVD was the largest cause of deaths from NCDs, accounting for 17.6 million deaths, or 46.2% of NCD deaths in 2012 (2). They also reported that diabetes directly caused 1.5 million deaths worldwide, or 4% of NCD deaths. However, these figures for diabetes deaths are likely to be an underestimate as it did not fully take into account the contribution of diabetes to other causes of death, particularly CVD. A more realistic estimate is that at least 5% of all deaths are attributable to diabetes (3).
Globally, 42% of all NCD deaths are premature (occurring before the age of 70 years), and in low-and middle-income countries (LMIC) almost half (48%) of NCD deaths are premature (2). Thirty-seven percent of premature deaths are due to CVD, which accounts for the largest proportion of deaths caused by NCDs, followed by cancers at 27%. Diabetes directly caused 4% of premature deaths. Again, this estimate underestimates the total contribution of diabetes to mortality which operates indirectly, by increasing the risk of dying from CVD, kidney disease, infectious diseases and some cancers.
In 2011, UN countries agreed nine global NCD targets across a range of risk factors and diseases, and a WHO Global Action plan was developed with the overall aim “to reduce the preventable and avoidable burden of morbidity, mortality and disability due to non-communicable diseases” (4). These voluntary global targets focused on the reduction of premature mortality, prevalence of risk factors contributing to these diseases and improving treatments. In particular, there was a pledge by countries to reduce premature mortality from the main NCDs of diabetes, cardiovascular diseases, respiratory disease and cancers by 25% by 2025 (25×25). Premature mortality was defined as the unconditional probability of dying between 30–70 years old, and baseline levels were set at the year 2010. Other targets aimed to reduce biological risk factors of NCDs, and included a pledge to halt the rise in prevalence of diabetes and obesity.
In September 2015, Sustainable Development Goals (SDG) were announced by the UN General Assembly to support a new sustainable development agenda (5). There are 11 health-related goals, with goal 3 specifically associated with health with the aim to “ensure healthy lives and promote wellbeing for all at all ages”. Within each goal are targets, and 3.4 is related to NCDs, with the objective to: “reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being” by 2030. The baseline for the SDG targets is 2010.
People with diabetes are more likely to develop CVD than those without diabetes, and have a higher probability to do so at a younger age (6). As diabetes is an important risk factor for cardiovascular disease morbidity and mortality, it is important to understand the trends in diabetes incidence, prevalence and mortality when considering premature CVD mortality.
The aims of this review are as follows:
To describe global trends in diabetes prevalence, with a particular focus on LMICs;
To review the mortality rates in people with diabetes compared to people without diabetes, how these differ between settings (e.g., high-income countries versus LMICs) and is changing over time;
To identify and summarize the findings of studies that have estimated the attainability of the 2030 and 2025 SDG and WHO NCD premature mortality targets, with particular focus on CVD;
To determine whether and how these studies have factored in trends in diabetes and provide a critical summary of what is currently known about the potential impact of trends in diabetes on the attainment of the SDG and WHO targets.
Methods
For the first and second aim, we used International Diabetes Federation (IDF) estimates for diabetes prevalence and mortality. As the SDG targets related to the year 2030, we decided to use data published in the 2011 IDF Atlas as this estimated prevalence and mortality to 2030 by IDF geographical location (7). We contacted the IDF directly to obtain data on diabetes prevalence based on countries’ income level and IDF regions, which were not published in the IDF Atlas. We also accessed data from the NCD Risk Factor Collaboration (NCD-RisC) as they published projections of global diabetes prevalence to 2025 (8). For relative risk of death from diabetes we referred to a paper by Roglic et al. and a systematic review by the IDF for estimates of the risk of CVD mortality in people with diabetes (3,6). A review of the time trends of diabetes mortality was also undertaken in PubMed.
For the third and fourth aims, we undertook a review to identify studies that have estimated the attainability of the 2025 WHO NCD and 2030 SGD premature mortality targets, focusing on CVD. We searched for [(“sustainable development goals” or SDG or “25 × 25” or “25×25”)] AND [(noncommunicable disease or NCD)] in the PMC database and the search was limited to papers published in the English language. This generated 438 hits. The titles and abstracts were then screened. Papers were included if they referred to the WHO or SDG NCD or CVD targets and if they included projections or conclusions about attainment of the targets in 2025 or 2030, using any methodology. Studies were excluded if they were review articles, the subject matter was not specifically related to attainment of WHO or SDG NCD or CVD targets, duplicates or abstract only was available. Further studies were also found by checking references and citations of studies already identified by the search. Using these inclusion and exclusion criteria, 12 relevant studies were found (9-20). Details of these studies are found in online: http://cdt.amegroups.com/public/addition/cdt/supp-cdt.2018.09.04-t1.pdf (9-20). Consideration of the strengths and limitations of the studies are summarized in Table 1.
Table 1. Strengths and limitations of studies included in review.
| Authors | Year of pub’ | SDG 3.4 2030/WHO 2025 (1) target | CVD/NCD/all deaths | Strengths/limitations of papers |
|---|---|---|---|---|
| Su et al. (9) | 2017 | WHO | CVD | Analysis of single risk factors without consideration of multiple risk factors on a condition |
| Assumption of prevalence of hyperlipidemia in 2009 carried forward to future years | ||||
| Used 5-year calculation of age-period-cohort analysis instead of single year calculation. Authors believe reduces likelihood of errors | ||||
| Li et al. (13) | 2017 | SDG and WHO | NCD | Used GBD 2013, with limitations in estimation of deaths, mortality and attributable burden as other papers using GBD 2013 data |
| Relative risk specific to Chinese population may be different to GBD, and could affect attributable burden of risk factors and the size and direction of associations | ||||
| Unable to take into account unattributable deaths | ||||
| Many risk factors not included that could affect the prevalence of CVD e.g., other dietary intakes | ||||
| Cobiac et al. (17) | 2017 | SDG and WHO | NCD | Many risk factors not included that could affect the prevalence of CVD e.g., other dietary intakes |
| Data is based on limited evidence on the associations between risk factors and impact of NCDs | ||||
| González-Pier et al. (11) | 2016 | SDG | All | Unforeseen factors could affect future trends, and analysis assumed that 2010 mortality rates continued into the future. Trends from 2000–2014 also used to avoid coding biases as ICD-10 introduced in Mexico in 1998 |
| Mexican specific data set combined with UN population data | ||||
| Sacco et al. (18) | 2016 | WHO | CVD | Used GBD 2013, with limitations in estimation of deaths, mortality and attributable burden as other papers using GBD 2013 data. Limited databases in LMICs |
| Analysis of single risk factors without consideration of multiple risk factors on a condition | ||||
| GBD (20) | 2016 | SDG | NCD | GBD has access to local country specific data sources due to their extensive global collaborative network. Variable quality of data, but multiple sources of data used e.g., vital registration data, verbal autopsy data and surveillance data |
| Uncertainty analysis undertaken | ||||
| Multiple co-variates accounted for | ||||
| Ordunez et al. (12) | 2015 | WHO | CVD | Limited databases in LMICs, especially with death rates and cause of deaths |
| Small numbers in countries with smaller populations should be interpreted with caution | ||||
| Roth et al. (14) | 2015 | WHO | CVD | Used GBD 2013, with limitations in estimation of deaths, mortality and attributable burden as other papers using GBD 2013 data |
| Analysis of single risk factors without consideration of multiple risk factors on a condition | ||||
| Some countries (e.g., LMICs) have issues with reliability of data due to lack of data or inaccuracies | ||||
| Assumptions including changes in BP would result in shift in whole distribution of BP rather than only those with hypertension | ||||
| Relative risk may not be accurate to the specific countries actual relative risk | ||||
| UN lifetables used for population projections do not take into account the CVD reduction that may have happened | ||||
| Norheim et al. (10) | 2015 | SDG | All | Some countries (e.g., LMICs) have issues with reliability of data due to lack of data or inaccuracies |
| Limited databases in LMICs, especially with death rates and cause of deaths | ||||
| Kontis et al. (16) | 2014 | WHO | NCD | Some countries (e.g., LMICs) have issues with reliability of data due to lack of data or inaccuracies |
| Relative risk was derived from observational studies, with a possibility of residual confounding, but only used relative risk from studies with well-adjusted studies | ||||
| Analysis of single risk factors without consideration of multiple risk factors on a condition | ||||
| Unforeseen factors could affect future trends, and base year in analysis was 2010, so there may be changes to risk factors since this time | ||||
| Kontis et al. (15) | 2015 | WHO | NCD | See Kontis et al. 2014 (16) |
| Santosa et al. (19) | 2015 | WHO | NCD | Swedish specific data |
| Lack of data on obesity, smoking, alcohol consumption and physical activity so was not included in analysis |
NCD, non-communicable diseases; CVD, cardiovascular disease; SDG, Sustainable Development Goal.
Results
Global trends in diabetes and cardiovascular disease prevalence
Using data from 216 countries and territories, the IDF estimated that in 2011, global prevalence of diabetes in adults aged 20–69 years was 7.7% (7). This has been projected to rise worldwide to 9.0% in 2030 (Table 2). For this age group, North America and the Caribbean have the highest projected prevalence of diabetes, with 11.8% in 2030 from 10.8% in 2011, followed by Middle East and North Africa with 10.6% in 2030 from 8.8%. In 2011, the aggregated prevalence of diabetes in low and middle-income countries (LMIC) in adults aged 20–69 was 7.5%, and is estimated to rise to 9.0% in 2030. In African countries, the diabetes prevalence is predicted to rise from 3.7% in 2011 to 4.1% in 2030. This rise in projected prevalence will place even greater pressures on those countries with fewer resources and existing infrastructure for treatment and prevention.
Table 2. Diabetes prevalence for adults aged 20–69 years in 2011 and projected for 2030 (IDF, unpublished data).
| Prevalence of diabetes | 2011 (%) | 2030 (%) | % increase in prevalence between 2011 and 2030 |
|---|---|---|---|
| Global prevalence | 7.7 | 9.0 | 16.9 |
| High income countries | 8.3 | 9.5 | 14.5 |
| Upper middle income | 8.6 | 10.7 | 24.4 |
| Low middle-income | 7.0 | 8.5 | 21.4 |
| Low income | 3.6 | 4.0 | 11.1 |
| IDF regions | |||
| Africa | 3.7 | 4.1 | 10.8 |
| Europe | 6.8 | 8.0 | 17.6 |
| Middle East and North Africa | 8.8 | 10.6 | 20.5 |
| North America and Caribbean | 10.8 | 11.8 | 9.3 |
| South and Central America | 7.8 | 9.4 | 20.5 |
| South East Asia | 8.1 | 10.0 | 23.5 |
| Western Pacific | 7.8 | 9.6 | 23.1 |
| Aggregated prevalence in low and middle-income countries (LMICs) | 7.5 | 9.0 | 26.7 |
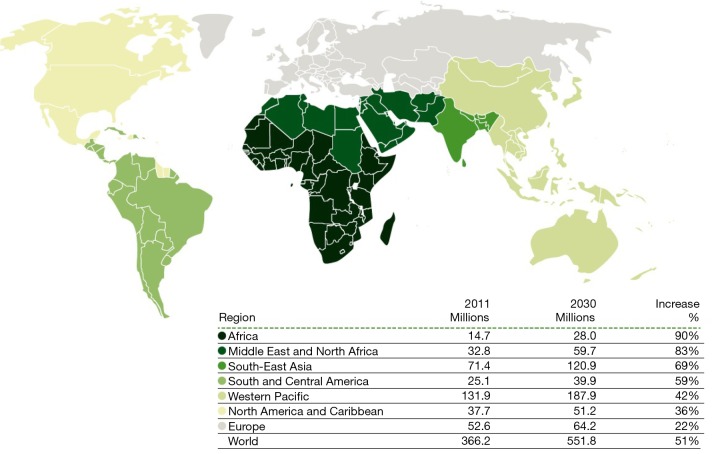
For adults aged 20–79 years, Figure 1 shows that the African region has been projected to have the highest increase in the number of people with diabetes by 2030, increasing by 90%, followed by the Middle East and North Africa, and South-East Asia, with 83% and 69% increases, respectively.
Figure 1.
IDF regions and global projections of the number of people with diabetes (20–79 years) in 2011 and 2030 (7). IDF, International Diabetes Federation.
These rising trends in diabetes have also been described by the NCD Risk Factor Collaboration (NCD-RisC) (8). Their findings from combined worldwide population-based studies across 200 countries and territories concluded that global age-standardized diabetes prevalence from 1980 to 2014 has increased, from 4.3% (95% credible interval 2.4–7.0%) in 1980 to 9.0% (7.2–11.1%) in 2014 in men, and from 5.0% (2.9–7.9%) to 7.9% (6.4–9.7%) in women. The study compared different regions and reported that East Asia and South Asia had the largest increase in absolute numbers of people with diabetes. In 2014, East Asia had 106 million and South Asia had 86 million people with diabetes. If the post year 2000 trends continued, the age-standardized prevalence of diabetes would increase to 12.8% in men and 10.4% in women. Worldwide, the study estimated that probability of meeting the target of halting the rise in diabetes by 2025 was <1% in men and 1% in women.
From these data, it is very likely that age-standardized diabetes prevalence will increase by 2030, but precise estimates are not possible. IDF estimates of projected diabetes prevalence are conservative, with conclusions drawn from changes in population age structure and trends in urbanization, but these estimates do not explicitly factor in trends in risk factors for diabetes such as the rising prevalence of obesity, although by including urbanization, it could be argued that these risk factors are indirectly included. The NCD-RisC base their prevalence of diabetes in 2025 on the assumption that 2000 trends continue, which also does not consider the consequences of increasing trends in risk factors for diabetes. Both studies recognize that LMICs will have the largest increase and burden in prevalence, both in terms of absolute numbers and in terms of age-standardized prevalence.
Mortality from diabetes and cardiovascular disease
Despite the paucity of data from LMICs, it is well known from studies in high income countries that people with diabetes, compared to those without, are at an increased risk of death. The relative risk of death is highest in the younger age groups but remains substantial even at older age: for example, from a relative risk of around 3 to 6 in men and women aged 20–29, to 1.5 to 2.5 in those aged 60 to 69 (3). By sex, the deaths attributable to diabetes is estimated to be higher in women than men (21). However, in the North America and Caribbean region, there are more deaths caused diabetes in men than women.
Globally, IDF estimated for 2017 that South East Asia was the region with the highest number of deaths attributable to diabetes before the age of 60, at 0.58 million, followed by the Western Pacific with 0.48 million and Africa with 0.23 million (21). Africa had the highest proportion of all deaths due to diabetes before the age of 60 (77.0%), followed by the Middle East and North Africa, and South East Asia at 51.8% and 51.5% respectively.
A systematic review by the IDF concluded that due to heterogeneity of the data, it was not possible to estimate global risk of CVD mortality in people with diabetes. However, in studies of middle-aged people (mean age of study population of 49 to 69 years) with diabetes, between 2 and 27 people out of 1,000 died from CVD a year (6). The review also noted that there was a lack of data for low-income countries.
Due to both heterogeneity and paucity data, it is difficult to give global estimates of the CVD risk (incidence and mortality) in people with diabetes (6). However, one systematic review by the IDF gave an estimated range of 9–41% of middle aged people (range of the mean ages from the study populations: 49–69 years) with diabetes as having CVD. These were estimates were only for high and middle-income countries only, as there is a paucity of data for low-income countries.
Time trends in diabetes mortality
Over time, in high-income countries, such as the United States (US), there is some evidence supporting an improvement in relative mortality in people with diabetes, compared to those without diabetes (22,23). There is also evidence in the US of a declining absolute mortality in diabetes, which has been observed in other high income countries such as Canada, United Kingdom (UK), Denmark and Australia (24-26).
Between the sexes, there is evidence of inequalities in absolute or relative mortality rates over time. Faerch et al. reported that among Danish men with diabetes, the reduction in mortality compared to the background population was significantly more than that of women, and the overall decline in absolute mortality in those with diabetes was caused by the reduction in CVD mortality (25).
However, not all studies found a decline in mortality in people with diabetes. A US study by Gregg et al. concluded a reduction in all-cause and cardiovascular mortality in men with diabetes, but, this was not seen in women (27). In Scotland, another high income setting, there was no evidence of relative improvements in mortality in either men or women (28). How these variations in reported trends of mortality rates apply to LMICs is uncertain, due to the difference in prevention and treatment from differing health care systems, and trends in risk factors for diabetes.
Attainability of the SDG and WHO premature mortality targets
Out of the 12 relevant studies, 7 related to WHO NCD targets specifically (9,12,14-16,18,19), 3 to SDG targets (9,10,19), and 2 considered both WHO and SDG goals (13,17). Six studies concentrated on premature deaths from NCDs (13,15-17,19,20), 4 on the reduction of premature deaths specifically from CVD (9,12,14,18), and 2 modelled the reduction of all premature deaths from NCD and communicable causes (9,10). All the papers that examined premature CVD mortality focused on the WHO 2025 target, and did not consider the SDG 3.4 target. Nearly all considered premature mortality to be deaths for adults aged 30–69 or 30–70 years old, but three studies defined premature mortality as 0–69 years (9,10,13). Half of the papers considered a global or regional approach, and the other half of the papers were country specific. These country specific studies focused mainly on high income (Taiwan, UK and Sweden) (9,17,19) and upper middle income countries (Mexico and China) (11,13). Further details of the studies are shown in Table 1.
The methodology of the papers from the search were categorized into 3 groups of modelling: (I) projecting current CVD mortality trends into the future (not considering trends in risk factors), (II) if the WHO targets for risk factors for NCDs/CVD were met, would it meet the overall SDG/WHO target, (III) using trends in risk factors for CVD (such as diabetes) and projecting their impact onto CVD mortality.
There were a few papers that had methodologies outside these categories. One modelled a 40% reduction in premature mortality of NCDs (instead of 25% or 33% reduction) (10), a Swedish study calculated if there had been a historical 25% reduction in premature NCD mortality between 1991–2006 and the likelihood of a further 25% reduction (18) and the GBD group calculated health-related SDG indices overall, and for each SDG indicator (19).
Four papers considered premature CVD mortality only (9,12,14,18), and another 4 that focused mainly on NCDs in general, also mentioned CVD mortality in their results (13,15-17). Within these, there was a range of methodologies, with 6 of the papers applying a mixture of using current trends in risk factors to project future mortality rates, and predicting the differences in mortality in the future if WHO risk factors were met. There was also a range of databases used to provide the data, with some using the GBD (13,14,18), but others using local population studies or surveys (9,12,15-17).
The results for premature CVD mortality from these studies were inconclusive, with conclusions ranging from no countries or regions meeting the target if the current risk factors trends were to continue, to Kontis et al. deducing that some countries such as Europe and the Americas would meet a 25% reduction by 2025 (15). Ordunez et al., by projecting current premature mortality trends onto the future population predicted that the most countries in the Americas would reach the 2025 targets (12). Su et al. concluded that the reduction in premature deaths in women from CVD in Taiwan would meet the target even if no risk factor targets were met (9).
If the risk factor targets stipulated by the WHO were met, findings from some studies were more optimistic, predicting that although with current trends continuing it was unlikely, but by meeting the risk factor targets, it may be possible (13,14). Kontis et al. noted that all regions will meet or exceed the target for CVD mortality if the risk factor targets were achieved (15), but Roth et al. also concluded that if the 4 risk factor targets were met in 2025, even though all countries would have a predicted reduction, many would not achieve the 25% premature CVD mortality target (14).
Out of the 12 studies, six studies used estimates of current trends in risk factors trends including diabetes in their models of attainability of the targets (13-18). Four of the studies compared a ‘business as usual’ model with regions in the world and overall globally (13-15,17). Of these, four studies predicted if the overall NCD target would be met (13,15-17), and two focused on the premature CVD mortality target (13,17).
Discussion
The results of the literature search show that out of 12 studies that modelled whether SDG or WHO targets related to premature CVD mortality were to be met, six used estimates of future diabetes prevalence in their models (13-18). It is important that accurate estimates of trends are included in models, as predictions that do not include adverse future trends in prevalence of diabetes may be inaccurate and make attainment of the targets more difficult to achieve. Not only does diabetes increases the risk of cardiovascular mortality, but it is a major cause of mortality in its own right.
It is also essential to consider the current trends in cardiovascular disease mortality. There have been studies from high income countries such as Iceland, Sweden, the Czech Republic and the US, and the upper middle income countries of Turkey, and lower middle income country of Tunisia into the effects of risk factors and treatments on trends in coronary heart disease (CHD) mortality (29-34). The conclusions of these were that although the overall mortality from CHD was falling, mainly due to improvements in risk factors such as smoking prevalence and hypertension, and medical and surgical treatments, these gains are offset by the worsening prevalence of other risk factors including physical inactivity, obesity and diabetes. Although these studies did not specifically consider premature mortality rates, there is no reason to believe there would be a significant difference in the conclusion on the importance that increasing diabetes prevalence plays in the mortality rates of CHD. Not all studies have shown a reduction in CHD. One study by Cheng et al. reported opposite trends in mortality from coronary heart disease in Beijing, China (35). These results concluded that CHD deaths were predicted to rise in Beijing with population aging, should baseline trends in CHD risk factors, including the prevalence of diabetes prevail. This study also modelled a 0.5% annual reduction in each major risk factor, which would offset the adverse effects of population aging on the increasing CHD death rate.
Based on the current literature, diabetes prevalence is conservatively estimated to increase, with a rise in global prevalence by 1.3% and increase of 2% in LMICs in people aged 20–69 years old in 2030 (IDF, unpublished data). Due to a lack of good quality data on the relationship between diabetes and excess mortality, particularly from LMICs, the impact of future diabetes trends on CVD mortality is difficult to estimate. The mortality from cardiovascular disease attributable to diabetes may be much worse in LMICs than currently predicted by published models. In these countries it may also be more difficult to implement prevention strategies and reduce mortality from diabetes and CVD due to limited resources.
To our knowledge, this is the first review of studies that assess whether if SDG or WHO targets will be met, particularly in relation to cardiovascular disease mortality and diabetes trends. The conclusions of this review are contingent on the strengths and weaknesses of the modelling studies included. As shown in Table 2, there are limitations in the data sources used by the studies, including data on mortality rates, and diabetes and risk factor prevalence, in particular, in LMICs. In addition, assumptions have often had to be made on the mortality risks associated with diabetes and other risk factors in specific national populations (9,14). Finally, some studies have acknowledged that their analysis have not been able to account for the effect of multiple risk factors on a condition.
Although a search strategy was employed, this was not a systematic review, and it is possible that studies may not have been found and subsequently not included. There is also chance of publication bias. There were few studies found on this topic and in particular on LMICs, so conclusions on these countries should be taken cautiously.
Predictions in premature CVD death rates should strive to take more accurate estimates of future diabetes prevalence and age specific excess mortality associated with diabetes into account. In LMICs, this is currently limited by a relative lack of high quality studies. Improved estimates will ensure that health policy makers will be able to develop more precise and pragmatic action plans to increase the likelihood of meeting the SDG or WHO targets for premature mortality.
Acknowledgements
None.
Disclaimer: The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151-210. 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global status report on noncommunicable diseases 2014. 2014.
- 3.Roglic G, Unwin N, Bennett PH, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care 2005;28:2130-5. 10.2337/diacare.28.9.2130 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO). Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013.
- 5.United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication
- 6.International Diabetes Federation. Diabetes and cardiovascular disease. 2016.
- 7.International Diabetes Federation. IDF Diabetes Atlas 5th edition. 2011. [Google Scholar]
- 8.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513-30. 10.1016/S0140-6736(16)00618-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su SY, Lee WC, Chen TT, et al. An evaluation of the 25 by 25 goal for premature cardiovascular disease mortality in Taiwan: an age-period-cohort analysis, population attributable fraction and national population-based study. Heart Asia 2017;9:e010905. 10.1136/heartasia-2017-010905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norheim OF, Jha P, Admasu K, et al. Avoiding 40% of the premature deaths in each country, 2010-30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet 2015;385:239-52. 10.1016/S0140-6736(14)61591-9 [DOI] [PubMed] [Google Scholar]
- 11.González-Pier E, Barraza-Lloréns M, Beyeler N, et al. Mexico’s path towards the Sustainable Development Goal for health: an assessment of the feasibility of reducing premature mortality by 40% by 2030. Lancet Glob Health 2016;4:e714-25. 10.1016/S2214-109X(16)30181-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ordunez P, Prieto-Lara E, Pinheiro Gawryszewski V, et al. Premature Mortality from Cardiovascular Disease in the Americas - Will the Goal of a Decline of "25% by 2025" be Met? PLoS One 2015;10:e0141685. 10.1371/journal.pone.0141685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Y, Zeng X, Liu J, et al. Can China achieve a one-third reduction in premature mortality from non-communicable diseases by 2030? BMC Med 2017;15:132. 10.1186/s12916-017-0894-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roth GA, Nguyen G, Forouzanfar MH, et al. Estimates of global and regional premature cardiovascular mortality in 2025. Circulation 2015;132:1270-82. 10.1161/CIRCULATIONAHA.115.016021 [DOI] [PubMed] [Google Scholar]
- 15.Kontis V, Mathers CD, Bonita R, et al. Regional contributions of six preventable risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: A modelling study. Lancet Glob Health 2015;3:e746-57. 10.1016/S2214-109X(15)00179-5 [DOI] [PubMed] [Google Scholar]
- 16.Kontis V, Mathers CD, Rehm J, et al. Contribution of six risk factors to achieving the 25×25 non-communicable disease mortality reduction target: a modelling study. Lancet 2014;384:427-37. 10.1016/S0140-6736(14)60616-4 [DOI] [PubMed] [Google Scholar]
- 17.Cobiac LJ, Scarborough P. Translating the WHO 25×25 goals into a UK context: The PROMISE modelling study. BMJ Open 2017;7:e012805. 10.1136/bmjopen-2016-012805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sacco RL, Roth GA, Reddy KS, et al. The Heart of 25 by 25: Achieving the Goal of Reducing Global and Regional Premature Deaths From Cardiovascular Diseases and Stroke: A Modeling Study From the American Heart Association and World Heart Federation. Circulation 2016;133:e674-90. 10.1161/CIR.0000000000000395 [DOI] [PubMed] [Google Scholar]
- 19.Santosa A, Rocklöv J, Högberg U, et al. Achieving a 25% reduction in premature non-communicable disease mortality: The Swedish population as a cohort study. BMC Med 2015;13:65. 10.1186/s12916-015-0313-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.GBD 2016 SDG Collaborators. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: An analysis from the Global Burden of Disease Study 2016. Lancet 2017;390:1423-59. 10.1016/S0140-6736(17)32336-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Interantional Diabetes Federation. IDF Diabetes Atlas Eighth Edition 2017. 2017. [Google Scholar]
- 22.Butala NM, Johnson BK, Dziura JD, et al. Decade-long trends in mortality among patients with and without diabetes mellitus at a major academic medical center. JAMA Intern Med 2014;174:1187-8. 10.1001/jamainternmed.2014.1803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsujimoto T, Kajio H, Sugiyama T. Favourable changes in mortality in people with diabetes: US NHANES 1999–2010. Diabetes Obes Metab 2018;20:85-93. 10.1111/dom.13039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lind M, Garcia-Rodriguez LA, Booth GL, et al. Mortality trends in patients with and without diabetes in Ontario, Canada and the UK from 1996 to 2009: a population-based study. Diabetologia 2013;56:2601-8. 10.1007/s00125-013-3063-1 [DOI] [PubMed] [Google Scholar]
- 25.Faerch K, Carstensen B, Almdal TP, et al. Improved Survival Among Patients With Complicated Type 2 Diabetes in Denmark: A Prospective Study (2002–2010). J Clin Endocrinol Metab 2014;99:E642-6. 10.1210/jc.2013-3210 [DOI] [PubMed] [Google Scholar]
- 26.Harding JL, Shaw JE, Peeters A, Guiver T, Davidson S, Magliano DJ. Mortality trends among people with type 1 and type 2 diabetes in Australia: 1997-2010. Diabetes Care 2014;37:2579-86. 10.2337/dc14-0096 [DOI] [PubMed] [Google Scholar]
- 27.Gregg EW, Gu Q, Cheng Y, et al. Mortality Trends in Men and Women with Diabetes, 1971 to 2000. Ann Intern Med 2007;147:149-55. 10.7326/0003-4819-147-3-200708070-00167 [DOI] [PubMed] [Google Scholar]
- 28.Read SH, Kerssens JJ, McAllister DA, et al. Trends in type 2 diabetes incidence and mortality in Scotland between 2004 and 2013. Diabetologia 2016;59:2106-13. 10.1007/s00125-016-4054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aspelund T, Gudnason V, Magnusdottir BT, et al. Analysing the large decline in coronary heart disease mortality in the Icelandic population aged 25-74 between the years 1981 and 2006. PLoS One 2010;5:e13957. 10.1371/journal.pone.0013957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Björck L, Rosengren A, Bennett K, et al. Modelling the decreasing coronary heart disease mortality in Sweden between 1986 and 2002. Eur Heart J 2009;30:1046-56. 10.1093/eurheartj/ehn554 [DOI] [PubMed] [Google Scholar]
- 31.Bruthans J, Cífková R, Lánská V, et al. Explaining the decline in coronary heart disease mortality in the Czech Republic between 1985 and 2007. Eur J Prev Cardiol 2014;21:829-39. 10.1177/2047487312469476 [DOI] [PubMed] [Google Scholar]
- 32.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med 2007;356:2388-98. 10.1056/NEJMsa053935 [DOI] [PubMed] [Google Scholar]
- 33.Unal B, Sözmen K, Arık H, et al. Explaining the decline in coronary heart disease mortality in Turkey between 1995 and 2008. BMC Public Health 2013;13:1135. 10.1186/1471-2458-13-1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saidi O, Ben Mansour N, O'Flaherty M, et al. Analyzing recent coronary heart disease mortality trends in Tunisia between 1997 and 2009. PLoS One 2013;8:e63202. 10.1371/journal.pone.0063202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheng J, Zhao D, Zeng Z, et al. The impact of demographic and risk factor changes on coronary heart disease deaths in Beijing, 1999-2010. BMC Public Health 2009;9:30. 10.1186/1471-2458-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]