Abstract
Background
Rheumatic heart disease (RHD) is an important public health problem in Sudan.
Methods
Clinical and echocardiographic findings from an RHD registry in Khartoum (January 2005–March 2018) are described. Operated and un-operated children were prospectively followed. The quality of life (QOL) for children who had surgery was evaluated using pediatric QOL cardiac module.
Results
A total of 818 children (51% males) were included, patients were clustered in White Nile and Kordofan area. RHD was found in 78% and acute rheumatic fever (ARF) in 22% of cases. RHD was severe in 65% and the most common lesion was mitral regurgitation (MR) in 37%. Follow-up of 107 un-operated children for a mean of 2 years revealed major complications in 38% including a mortality of 14%. Severe valve dysfunction tended to remain unchanged. There were 3 deaths in children with severe valve lesions immediately following benzathine penicillin injections. Only 19% of patients underwent surgery with an average post-operative mortality of 10.5% in the last 8 years. Of those, only 34 were reached for follow-up (23%), all were in New York Heart Association (NYHA) class 1, however adverse outcomes were observed including noncompliance with benzathine penicillin and warfarin (51% and 29% respectively) and more than mild valve dysfunction in 35%. All children who had valve surgery have a good QOL scores. In the last 3 years, the outpatient visits, admissions and mortality rates decreased by 20%, 48% and 22% respectively.
Conclusions
RHD is clustered in certain areas and presents with severe valve lesions with a high mortality for un-operated patients. Operative mortality improved over the last years but the follow-up rates are poor and adverse outcomes are common. There is an apparent trend of decline in the number of patients with RHD seen at referral hospitals.
Keywords: Rheumatic heart disease (RHD), outcomes, trends, Sudan
Introduction
Rheumatic heart disease (RHD) is heart valve inflammation and scarring triggered by infection with group A streptococci (GAS) (1). Worldwide, it is estimated that 15 to 20 million people have RHD of whom about 2.4 million are children between the ages of 5 and 14 years (2). RHD has been largely neglected although it is estimated to cause deaths up to 250,000 per year mostly in young people (3).
In Sudan, RHD is an important public health problem with an echocardiographic (echo) prevalence of up to 61 per 1,000 (4). A control program was established in 2012 based on primary & secondary prevention, increasing public awareness, advocacy, and surveillance (5). A hospital register was established aiming to monitor RHD-related health outcomes towards the achievement of the Sudan RHD control program objectives of 25% reduction in the prevalence of RHD by the year 2025.
Data on RHD patients’ outcomes are deficient worldwide, particularly in Africa. The RMEDY study looked at 3,343 adults and children, mostly from Africa, and revealed that the majority had moderate to severe multivalve disease (6). A study from South Africa reported a 60-day hospital mortality for un operated patients of 24% and early operative mortality of 2% (7).
In this report, we reviewed the demographic, clinical and echo patterns and trends in hospital visits as well as the outcomes of operated and un-operated children with RHD. We also investigated the quality of life (QOL) of children after valve surgery, to our knowledge; this has not been previously reported.
Methods
This is a combined retrospective and prospective cohort study. First phase through reviewing of the data of RHD patients, including surgical and mortality reports of the hospitals’ statistics departments, of two referral hospitals, Jafar Ibn Ouf Children’s Hospital and Sudan Heart Center, Khartoum, Sudan from January 2005 to March 2018. Patients with clinical and echo evidence of RHD were included and demographic, clinical and echo data were registered. In the second phase data was obtained prospectively from outpatient and inpatient records. Children who did not attend for follow-up were contacted by telephone and invited to attend. The QOL scores for children/adolescents who had valve surgery were evaluated using Pediatric Quality of Life (PedQOL) module (8).
Statistical methods
The data was first described in detailed flow chart diagram in different levels according to the time flow. Each level described in number and percentage. The data was summarized in bar charts, trends, percentages and ratios.
In addition, inferential statistics was conducted for some related variables. Paired chi square test was run to assess outcome for some variables at two different point’s time with statistical significance set as P value 0.05.
Definitions
ϖ Compliance with benzathine penicillin G (BPG): regular use of BPG every 3 weeks without missing a single dose;
ϖ BPG related complications: occurrence of adverse reactions within few minutes of administration of the injection;
ϖ Degree of valve dysfunction: defined by the criteria of the American Society of Echocardiography (9) as mild, moderate and severe;
ϖ Early surgical mortality: death due to cardiac complications within 1 month of surgery;
ϖ Late surgical mortality: death due to cardiac complications 1 month or more after surgery;
ϖ BPG administration methods: BPG was administered according to the protocol of Sudan Guidelines for rheumatic fever and RHD management (10).
Ethical considerations
The study protocol conforms to 1975 Declaration of Helsinki guidelines. Approval to conduct the study was obtained from the two hospitals. For the prospective part, Ethics Committee approval was obtained from the Sudan Medical Specialization Counsel. Patients/families who were contacted by telephone were asked to give an informed written consent.
Results
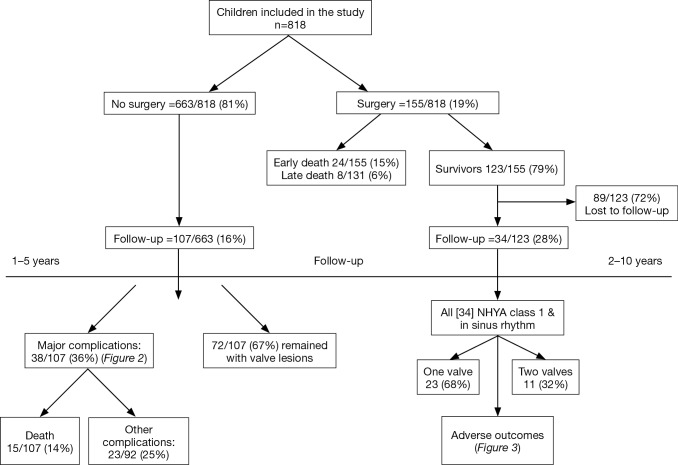
In the study period, 1,188 children were registered, the first 370 patients were reviewed and a report was published in 2014 (11). In this report we reviewed children up to 18 years of age (n=818). The patients’ flow chart is shown on Figure 1.
Figure 1.
Flow chart showing the patients course. Complications (%) seen in 38 out of 107 un-operated patients (Figure 2). Adverse outcomes after valve surgery in 34 children (Figure 3).
Demographic features
Males were 51%. The age ranged from 3 to 18 years and the highest incidence is observed in children aged 10 to 15 (46%). White Nile and Kordofan areas have the highest rate of RHD (5.3 and 4.7 cases/100,000 population) compared with <3.6/10,000 in other areas.
Clinical features
The New York Heart Association (NYHA) class was I–II in 57% and it was III–IV in 43% of patients. In 78% of patients, there was established RHD, acute rheumatic fever (ARF) was present in 22% of cases. Compliance with BPG was found in 45% of patients.
Benzathine penicillin-related complications
There were no reports of serious adverse effects related to BPG from 2005 to November 2017 (about 300 thousand injections). In the period November 2017–January 2018; 3 cases of BPG-related hospital deaths occurred. All the patients were girls, 6, 7 and 8 years old, one is a new case and 2 are known cases of RHD on regular BPG. All cases had severe mitral regurgitation (MR) and were admitted with severe heart failure which was controlled and BPG was planned to be administered on the day of discharge. Investigations of these events revealed that the injections were given intramuscularly by trained nurses under physician’s supervision and all patients collapsed within few minutes of injection and did not respond to proper resuscitation. Non of them showed signs of allergy.
Echocardiographic features
The most common valve lesion was mitral regurgitation (MR) in 37%, 3 valves were affected in 15.1% and 2 patients had all 4 valves affected (Table 1). RHD was severe in 65% of patients. Of the patients with severe form of RHD and known residence, 22.4% were from Kordofan, and 19% from Darfur areas. Pulmonary hypertension was present in 22% of patients and a low ejection fraction in 6%.
Table 1. Valve lesions seen in 803 patients with RHD.
| Valve lesion/s | No. of cases | Percentage |
|---|---|---|
| MR | 297 | 37.0 |
| MR/AR | 293 | 36.5 |
| Three valves | 122 | 15.2 |
| MR/MS | 37 | 4.6 |
| AR | 22 | 2.7 |
| MS | 18 | 2.2 |
| AR/MS | 6 | 0.7 |
| AR/TR | 6 | 0.7 |
| All 4 valves | 2 | 0.2 |
| Total | 803 | 100 |
RHD, rheumatic heart disease; MR, mitral regurgitation; AR, aortic regurgitation; MS, mitral stenosis; TR, tricuspid regurgitation.
Follow-up of un-operated patients
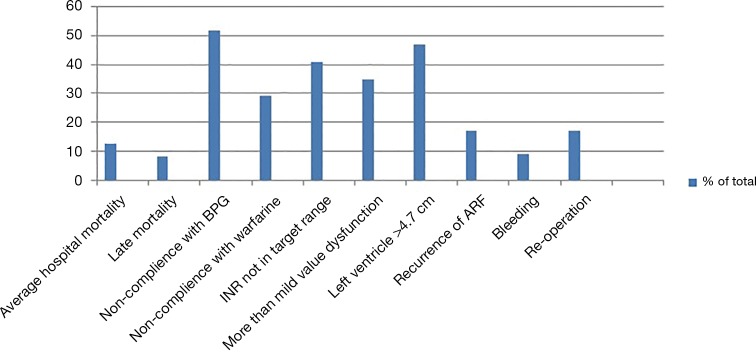
Only 107 out of 663 patients (16%) showed for follow-up. The follow-up period was 1–2 years for 48% of patients, 2–3 years for 30% and more than 3 years for 22% of patients, mean duration was 2 years. Major complications occurred in 38 patients (36%), including the death of 15 patients (14%) as shown in (Figure 2). Most of the patients who died (87%) were females from Kordofan (46%) and Darfur (26%) areas. In most patients with MR (57%) the echo severity remained the same, the subgroup with severe MR showed more tendency to remain the same (34%). Out of all MR, 12% showed echo deterioration and 33% showed improvement. In the subclinical category, 3.8% showed deterioration of MR. Chi-square test showed no significant differences between MR at diagnosis and at follow (P value was 0.061>0.05) (Figure 4).
Figure 2.
Complications (%) seen in 38 out of 107 un-operated patients.
Figure 4.
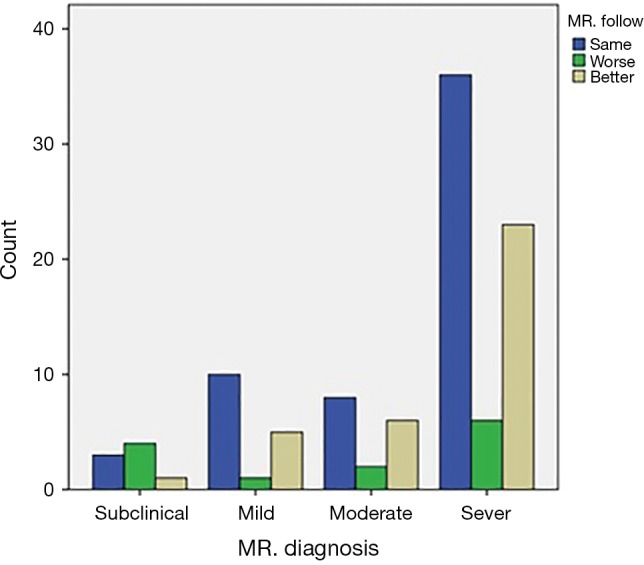
The follow-up of patients with subclinical, mild, moderate and sever MR. MR, mitral regurgitation.
For AR, there was a tendency for improvement in the degree in all categories (mild, moderate and severe) but not reaching statistical significance (P value was 0.40>0.05).
Pulmonary hypertension was found in 29% of patients on presentation and a similar percentage on follow-up.
Interventional procedures
Interventional procedures were performed in 167 pediatric patients (20%). Surgery was done in 155 (19%) and included mitral valve repair in 40%, and replacement in 18%. Combined mitral and aortic surgery was done in 21% of patients. Balloon mitral commissurotomy (transcatheter dilatation of the mitral valve) was performed in 12 patients (7%).
Follow-up of children who had surgery
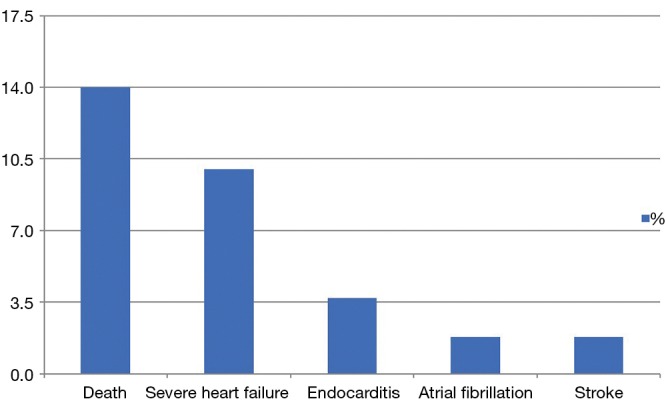
From 2005 to 2015, 155 children (5–18 years of age) had valve surgery. There were 24 (15%) hospital and 8 (5%) late deaths, reoperation rate was 17%. All the 123 survivors were contacted by telephone, 73 patients could not be reached (59%) and 16 could not afford to attend, therefore only 34 (28%) were included in the analysis. Patients were followed for 2–10 years with a mean of 7 years after the surgery. Most patients (92%) reside outside Khartoum.
Twenty-three patients (68%) had one valve and 11 (32%) had 2 valves operated on. All 34 patients were in NYHA class I and in sinus rhythm. Adverse outcomes encountered are depicted in (Figure 5). The hospital mortality decreased from 20% (2005 to 2008) to 10.5% in the last 8 years.
Figure 5.
Adverse outcomes after valve surgery in 34 children.
QOL of children who had surgery
Four domains were tested including patients’ suffering of health and activities, others and schooling. There was no significant affection of the QOL as the mean for all answers was 1–1.79 which is corresponding to “Never” according to the Likert scale as shown in Table 2. The consistency of data was calculated as 0.9 (Cronbach’s alpha score) (12,13).
Table 2. QOL assessment of patients who had valve surgery (n=34).
| Scale | N | Weighted mean | St. deviation | Result |
|---|---|---|---|---|
| Suffering with your health and activities | 34 | 1.22 | 0.432 | Never |
| Your feelings | 34 | 1.18 | 0.349 | Never |
| Relationship with others | 34 | 1.19 | 0.383 | Never |
| Problems at school | 34 | 1.52 | 0.572 | Never |
QOL, quality of life.
Trends in hospital visits, admissions, and mortality
In the period 2012–2017, there were 325 patients with RHD admitted to Jafaar Ibn Ouf Children’s Hospital, of these 42 patients died in the hospital (13%). In the last 3 years, the outpatient visits rates decreased from 225 to 180 (20%), admissions from 88 to 45 (48%) and mortality from 9 to 7 cases per year (22%). Admissions due to ARF decreased from 19 [2012] to 9 [2015] while admissions due to RHD increased in the same period (Figure 3).
Figure 3.
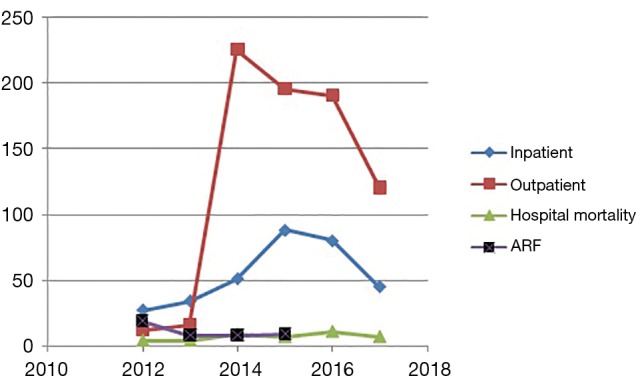
Outpatient visits, admissions and mortality due to RHD in the years 2012–2017 and admissions due to acute rheumatic fever in 2012–2015 at Jafar Ibn Ouf Children’s Hospital. RHD, rheumatic heart disease.
Discussion
RHD in Sudan is clustered in certain areas; Kordofan and White Nile bear the maximum burden. This is also apparent in the higher rate of patients with severe disease and higher mortality in these areas. Similar patterns were documented by echo screening studies that showed an echo prevalence of 0.3 per 1,000 in Khartoum compared with 19 per 1,000 in Darfur and up to 61/1,000 in Kordofan (4,14). Clustering of RHD in certain geo-ethnic groups within the same country has been observed in Australia and New Zealand’s endogenous populations as well as in South Africa where it was attributed to variation in socioeconomic conditions as well as poor accessibility to health services (15-17). Understanding these variations in RHD epidemiology is important for planning of RHD control programs that need to be directed to endemic areas. The majority of patients have established RHD and the frequency of ARF was low, a finding that has been consistently observed in other regions of the world (18). This is also reflected on the hospital admission patterns between 2012–2017 which showed an inverse relationship between ARF and RHD incidence.
The patterns of valve affection seen in this cohort are similar to that reported by us in 2014, however, in the current study, severe RHD is present in 65% of patients compared to 83% in 2014 (11). This may be attributed to the increasing awareness of physicians leading to the earlier referral of cases particularly after echo screening and training campaigns that were conducted in highly endemic areas.
Follow-up data was obtained in only 16% of un-operated patients; living far from cardiac services coupled with poor socioeconomic conditions are the most important factors contributing to this finding. In addition, most of the patients who were reached were followed-up for only 1–2 years and this raises concerns about the fate of the other patients. Considering the 2-year mortality rate of 16%, by 10 years, 80% of these patients might not be alive.
Few studies looked at the outcomes of un-operated patients in Africa. When compared with the REMEDY study which included older patients (median age 28 years), our patients have a similar frequency of severe disease indicating a more aggressive nature in our younger population while other complications like atrial fibrillation, stroke, and endocarditis were all far less than that in the REMDY (6). For similar reasons, the 2-year mortality in a study that included adults and children in South Africa, was significantly higher than our patients (25% vs. 16%) (7). In a sharp contrast, in developed countries where well-organized control programs are available such as Australia, severe RHD was found in only 16% of patients (19).
Deaths that occurred immediately following BPG injections were clustered in a short period raising possibilities of drug-quality related issues. Similar events of deaths had been reported (20) and a notion that BPG can lead to arrhythmias in patients with severe heart disease has been clearly made (21). Our patients received about 300,000 injections over 12 years with only 3 such cases, representing 1/100,000 injections. As there were no signs of anaphylaxis, or a response to adrenalin, these deaths might be due to arrhythmias. This poses challenges to RHD control programs as patients with severe valve lesions will be considered to have a high-risk for BPG complications. The value of giving BPG to patients who already have 2 or more severely affected valves is questionable and the risk may outweigh the benefits in such patients. This emphasizes the need to develop an alternative to the current long acting penicillin formulation in order to prevent such complications.
Surgery was performed in only 19% of pediatric patients and this highlights the deficiency of surgical resources. In addition to the limited slots, the cost of surgery (4–8,000 US dollars) is not affordable by these families. Follow-up rates are poor due to remoteness and this has also been observed by other authors who found similarly low follow-up rates in Mozambique (22). Our surgical mortality is higher than that of South Africa where cardiac surgery is better established. Many factors contribute to this; most importantly the late presentation, long waiting time due to limited surgical slots (especially in the early years of this study) and multiple-valve affection. Noncompliance with warfarin and BPG as has been documented in this cohort, is likely to increase the late mortality and morbidity (7).
However, those who survived surgery were all in NYHA 1 indicating a much better outcome than un-operated patients. Although most of them do not have heart failure, adverse outcomes were frequent and echo revealed more than mild valve dysfunction in a third of patients indicating a guarded longer-term outcome. Patients who had valve replacement were commonly not compliant with warfarin and international normalization ratio testing, largely because of the difficulties of accessing medical services. These difficulties in managing post-operative patients emphasize the importance of primary and secondary prevention and the need for decentralization of advanced cardiac services.
The QOL scores showed a good outcome for post-operative patients, this finding needs to be taken with caution. It has been shown that children and adolescents with chronic cardiac conditions do have a worse QOL compared with their normal peers (23). The response of patients and families to the QOL questionnaire may reflect Sudanese families’ traditions that consider it socially unacceptable to admit having an emotional or psychological compromise. Therefore, the impact of RHD on QOL needs to be reassessed considering this limitation.
The RHD control program was initiated in 2012, in the following 2 years; a sudden rise in hospital visits and admissions was documented followed by a steady decline in the last 3 years. We believe that it is too early to consider this a true decline in RHD burden; however, it is a positive trend that could be attributed to increasing awareness of health workers. Further studies are needed to evaluate the true trends in the incidence of RHD in high burden areas.
Limitations
The small numbers of patients who responded to phone calls or could afford to come limited the total numbers available for analysis of outcomes.
Conclusions
RHD is clustered in certain areas and presents with severe valve lesions but there is a trend of decreasing severity compared to 2014. Follow-up rates are poor and showed a 2-year mortality of 14% for un-operated patients. Deaths occur following BPG and need to be further investigated. Surgery is done for a limited number of children, operative mortality improved over the last years. Follow-up rates are poor and adverse outcomes are common. There is an apparent trend of decline in the number of patients with RHD seen at referral hospitals.
Acknowledgements
We would like to acknowledge the contribution and of Dr. Laila Elmahdi, Prof. Siragedeen M. Khair and Dr. Ibrahim Adam for referring their patients and for Dr. Intisar Ibrahim, Dr. Fouada Mohamed and Dr. Tasneem Abdallha for their contribution in data entry.
Ethical Statement: Ethics Committee approval was obtained from the Sudan Medical Specialization Counsel. Patients/families who were contacted by telephone were asked to give an informed written consent.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Guilherme L, Kalil J, Cunningham M. Molecular mimicry in the autoimmune pathogenesis of rheumatic heart disease. Autoimmunity 2006;39:31-9. 10.1080/08916930500484674 [DOI] [PubMed] [Google Scholar]
- 2.Carapetis JR, Steer AC, Mulholland EK, et al. The global burden of group A streptococcal diseases. Lancet Infect Dis 2005;5:685-94. 10.1016/S1473-3099(05)70267-X [DOI] [PubMed] [Google Scholar]
- 3.Marijon E, Mirabel M, Celermajer DS, et al. Rheumatic heart disease. Lancet 2012;379:953-64. 10.1016/S0140-6736(11)61171-9 [DOI] [PubMed] [Google Scholar]
- 4.Ali S, Domi SB, Elfaki AM, et al. The echocardiographic prevalence of rheumatic heart disease in North Kordofan and initiation of a control program. Sudan Med J 2017;53:63-8. 10.12816/0039456 [DOI] [Google Scholar]
- 5.Ali SK. Rebuilding the rheumatic heart disease program in Sudan. Glob Heart 2013;8:285-6. 10.1016/j.gheart.2013.07.002 [DOI] [PubMed] [Google Scholar]
- 6.Zühlke L, Engel ME, Karthikeyan G, et al. Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J 2015;36:1115-22a. 10.1093/eurheartj/ehu449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zühlke LJ, Engel ME, Watkins D, et al. Incidence, prevalence and outcome of rheumatic heart disease in South Africa: a systematic review of contemporary studies. Int J Cardiol 2015;199:375-83. 10.1016/j.ijcard.2015.06.145 [DOI] [PubMed] [Google Scholar]
- 8.PedsQL™ contact information and permission to use: Mapi Research Trust, Lyon, France. Available online: https://eprovide.mapi-trust.org and www.pedsql.org
- 9.Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003;16:777-802. 10.1016/S0894-7317(03)00335-3 [DOI] [PubMed] [Google Scholar]
- 10.Ali S, Alkhalifa MS, Khair SM. Acute Rheumatic Fever and Rheumatic Heart Disease, Sudan’s Guidelines for diagnosis, management and control. Available online: http://sudankidsheart.org/images/rhd/ARF_RHD%20Book.pdf
- 11.Khalid E, El Banna H, Mahmoud R, et al. Clinical and echocardiographic features of 370 children with rheumatic heart disease seen in Khartoum. Sudan Med J 2014;50:151-4.
- 12.Likert R. A Technique for the Measurement of Attitudes. Available online: https://legacy.voteview.com/pdf/Likert_1932.pdf
- 13.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297-334. 10.1007/BF02310555 [DOI] [Google Scholar]
- 14.Ali S, Domi S, Abbo B, et al. Echocardiographic screening for rheumatic heart disease in 4 515 Sudanese school children: marked disparity between two communities. Cardiovasc J Afr 2018;29:273-7. 10.5830/CVJA-2018-022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parnaby MG, Carapetis JR. Rheumatic fever in indigenous Australian children. J Paediatr Child Health 2010;46:527-33. 10.1111/j.1440-1754.2010.01841.x [DOI] [PubMed] [Google Scholar]
- 16.Milne RJ, Lennon DR, Stewart JM, et al. Incidence of acute rheumatic fever in New Zealand children and youth. J Paediatr Child Health 2012;48:685-91. 10.1111/j.1440-1754.2012.02447.x [DOI] [PubMed] [Google Scholar]
- 17.Engel ME, Haileamlak A, Zühlke L, et al. Prevalence of rheumatic heart disease in 4720 asymptomatic scholars from South Africa and Ethiopia. Heart 2015;101:1389-94. 10.1136/heartjnl-2015-307444 [DOI] [PubMed] [Google Scholar]
- 18.Seckeler MD, Hoke TR. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clin Epidemiol 2011;3:67-84. 10.2147/CLEP.S12977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cannon J, Roberts K, Milne C, et al. Rheumatic Heart Disease Severity, Progression and Outcomes: A Multi-State Model. J Am Heart Assoc 2017. doi: . 10.1161/JAHA.116.003498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Benzathine penicillin: three fatal reports following mega unit injections. Available online: http://apps.who.int/medicinedocs/en/d/Jh1466e/3.2.html
- 21.WHO Model Prescribing Information: Drugs Used in the Treatment of Streptococcal Pharyngitis and Prevention of Rheumatic Fever. Available online: http://apps.who.int/medicinedocs/en/d/Js2252e/3.2.1.html
- 22.Mirabel M, Lachaud M, Offredo L, et al. Cardiac surgery in low-income settings: 10 years of experience from two countries. Arch Cardiovasc Dis 2017;110:82-90. 10.1016/j.acvd.2016.05.006 [DOI] [PubMed] [Google Scholar]
- 23.Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL™ 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5:43. 10.1186/1477-7525-5-43 [DOI] [PMC free article] [PubMed] [Google Scholar]