Abstract
Child poverty leads to various negative consequences, including low self-esteem, which is a risk factor for mental illness, suicide, or poor academic achievement. However, little is known about why child poverty leads to low self-esteem. We aimed to elucidate the association of child poverty and low self-esteem based on the ecological model, which includes family-level, school-level, and community-level factors. Data were obtained from the Adachi Child Health Impact of Living Difficulty (A-CHILD) study in 2016, and participants included 1,652 children in fourth grade (534 pairs), sixth grade (530 pairs), and eighth grade (588 pairs) living in Adachi City, Tokyo, Japan. A questionnaire survey was implemented to assess child poverty, parental mental health, parental involvement with children, parental social capital by caregivers, and self-esteem and school social capital by children. The structural equation model was applied to elucidate the association between child poverty and low self-esteem, using family-level (parental mental health and parental involvement with children), school-level (school social capital), and community-level (parental social capital) factors. Child poverty was associated with low self-esteem. Child poverty leads to poor parental involvement, which can be indirectly associated with poor parental mental health and poor parental social capital, and poor parental involvement was directly or indirectly associated with low self-esteem through poor school social capital. To mitigate the impact of child poverty on low self-esteem, comprehensive health policies targeting family-level (parental mental health and parental involvement with children), school-level (school social capital), and community-level (parental social capital) factors may be effective.
Keywords: child poverty, self-esteem, ecological model, structural equation model, Japan
Introduction
Child poverty rates across countries in the Organisation for Economic Co-operation and Development (OECD) was 13.5% in 2014 (OECD, 2017), and is increasing in several OECD countries (OECD, 2017). The negative consequences of child poverty are known to include dental caries (Peres et al., 2005; Delgado-Angulo et al., 2009; Tanaka et al., 2013), eczema (Sasaki et al., 2016), wheezing (Lynch et al., 2014), decline in pulmonary function (Amemiya and Fujiwara, 2018), suspected autism spectrum disorders (Fujiwara, 2014), and low uptake of vaccination (Klevens and Luman, 2001; Nagaoka and Fujiwara, 2016; Sakai, 2018). Moreover, the long-term impacts of child poverty have also been established, such as risk of higher functional disability (Fujiwara et al., 2013), depression (Gilman et al., 2003; Tani et al., 2016), and dementia (Dekhtyar et al., 2015) among older adults.
Low self-esteem may influence how childhood poverty affects health, that is, children living in poverty may consider themselves as worthless, which leads to lower levels of self-care (Mann et al., 2004; Hedayati et al., 2012; Poorgholami et al., 2015). Self-esteem is defined as “an individual’s subjective evaluation of her or his worth as a person” (Donnellan et al., 2011). To date, many longitudinal studies indicated that low self-esteem in childhood leads to negative consequences. For instance, children with lower self-esteem are more likely to show mental illness such as depression (Sowislo and Orth, 2013; Orth et al., 2014; Steiger et al., 2014; van Tuijl et al., 2014), anxiety (Sowislo and Orth, 2013; van Tuijl et al., 2014), and suicidal ideation and attempted suicide (Overholser et al., 1995; McGee et al., 2001; Manani and Sharma, 2016), which might be caused by seeking reassurance from friends, negative feedback from friends to prove their negative self-concept, and ruminating negative aspect of self (Sowislo and Orth, 2013). Further, lower self-esteem in childhood lead to behavioral problems such as health-compromising behaviors (e.g., eating disorders) (McGee and Williams, 2000) and criminal behaviors during adulthood (Trzesniewski et al., 2006), which might be caused by peer pressure, that is, individuals with lower self-esteem are more likely to be influenced by others. Furthermore, adolescents with lower self-esteem are more likely to show physical health problems and limited economic prospects during adulthood (Trzesniewski et al., 2006), which might be caused by low persistence in the face of failure and poor social connectedness.
Previous studies have shown the association between child poverty and low self-esteem. For example, Twenge and Campbell (2002) indicated that, in their meta-analysis using 446 studies, low socioeconomic status (SES) was associated with low self-esteem among children, and they also reported that the effect size increased significantly with age (elementary school: effect size, d = 0.08; junior high school: d = 0.12; college: d = 0.10; young adults, 23–39 years old: d = 0.21; middle-aged adults, 40–59 years old: d = 0.25), suggesting a cumulative effect of low SES on low self-esteem among children. Thus, preventative approaches are needed among younger children, such as first-grade students, to mitigate the impact of low SES on low self-esteem.
To break the association between child poverty and low self-esteem, the pathway needs to be elucidated. Previous studies in the United States indicated that parenting practice, parental mental health, and parent–child relationship are possible mediators explaining the association between poverty and child’s self-esteem (Conger et al., 1992; Ho et al., 1995; Mayhew and Lempers, 1998; Yoder and Hoyt, 2005; Orth, 2018). However, self-esteem can be affected not only by familial factors, but also by other factors, such as school or community factors, when we apply the ecological perspective (Bronfenbrenner, 1997; Bronfenbrenner and Morris, 1998; Bronfenbrenner, 2005). The ecological model focuses on factors at individual, relationship, community, and societal levels and explains how to influence from factors at one level to factors at another level. Many previous studies have applied the ecological model to examine the impacts of child poverty on adverse health effects in children (e.g., Atilola, 2017) because it allows us to understand which factors we need to approach to prevent children’s adverse health effects. According to the ecological model, family environment (e.g., parent–child relationship and mental health of family members), school environment (e.g., peer and teacher relationships), and neighborhood (e.g., parental social capital) are important factors in child development.
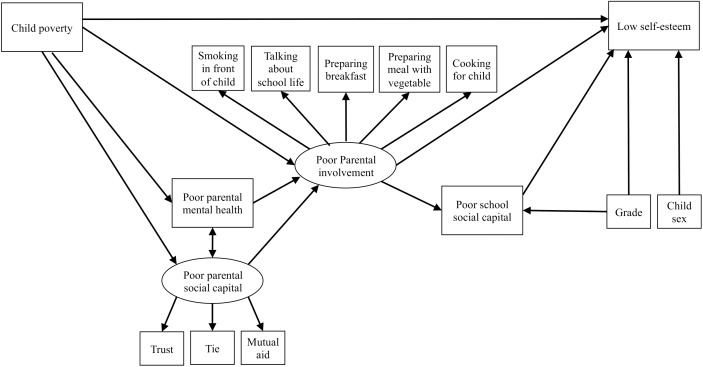
The theoretical framework of the ecological model on the association between child poverty and low self-esteem is as follows. First, according to the literature, child poverty can induce poor parental involvement (Evans, 2004) and poor parental involvement leads to low self-esteem (Bolger et al., 1998; Bean et al., 2003; Parker and Benson, 2004). These associations (i.e., family environment mediates the association between child poverty and self-esteem) have been found in previous studies as mentioned above (Conger et al., 1992; Ho et al., 1995; Mayhew and Lempers, 1998; Yoder and Hoyt, 2005; Orth, 2018). Second, poor maternal mental health (family environment) and maternal social capital (community environment), which are correlative (Balaji et al., 2007), mediate the association between child poverty and poor parental involvement (Pachter et al., 2006; Rijlaarsdam et al., 2013). Third, school social capital such as peer and teacher relationships are associated with a child’s self-esteem (Bolger et al., 1998; Laible et al., 2004), which is a possible mediator of the association between parental involvement and low self-esteem (Law et al., 2013). Additionally, some studies have found that school social capital mediates the association between parental involvement and child mental health outcomes (e.g., Oldfield et al., 2016) although there are a few studies focusing child self-esteem. Thus, it is plausible, based on theory and previous studies, that the association between child poverty and low self-esteem might be explained by family-level, school-level, and community-level factors (see hypothesized model in Figure 1). The aim of this study was to examine the validity of the hypothetical model in order to elucidate the association of child poverty and self-esteem based on the ecological model, which includes family-, school-, and community-level factors.
FIGURE 1.
Hypothetical model of the association between child poverty and low self-esteem.
Materials and Methods
Participants
This study is part of the Adachi Child Health Impact of Living Difficulty (A-CHILD) study conducted in 2016, which examined the living environment and health of elementary school and junior high school students and their parents in Adachi City, Tokyo, Japan. Self-reported questionnaires with anonymous unique IDs were distributed to children living in Adachi City, Tokyo, Japan, including fourth-grade (N = 616), sixth-grade (N = 623), and eighth-grade (N = 755) school students, who brought questionnaires home to their caregivers. This survey was conducted in nine elementary schools and seven junior high schools in Adachi City, Tokyo, Japan. A total of 1773 participants returned the questionnaire (response rate = 88.9%), and 1653 participants provided informed consent and submitted both caregiver’s and child’s questionnaires (valid response rate = 82.9%). Written informed consent was obtained from all adult participants and the caregivers of their child. We did not obtain written informed consent from children because we obtained it from their caregivers, which was within the Japan’s ethical guidelines for epidemiologic research and gained caregiver’s assent. Among the valid respondents, 73 participants were excluded due to missing data of variables used in the main analysis. Thus, the analytical sample was 1580 participants (caregiver–child pairs) (Figure 2). The participants who were excluded due to missing data of variables did not show significant differences in sex of child, grade, and educational level of mother and father compared with the analytical sample (all p > 0.05). Among 1580 participants, the responders included mother (N = 1,419; 89.8%), father (N = 137; 8.7%), grandparent (N = 10; 0.6%), and others or missing (N = 12; 0.8%). The A-CHILD protocol was approved by the Ethics Committee at the National Center for Child Health and Development (No. 1187) and the Ethics Committee at Tokyo Medical and Dental University (M2016-282-02).
FIGURE 2.
Participant flow chat.
Measurements
Demographic Data
The caregivers were asked about their relationship with their child (mother, father, or any other caregiver), mother’s age, and father’s age. The children were asked to indicate their sex (male or female).
Child Poverty
The caregivers were asked about their annual household income (<500,000 yen, 500,000 to <1 million yen, 1 million yen to <2 million yen, 2 million yen to <3 million yen, 3 million yen to <4 million yen, 4 million yen to <5 million yen, 5 million yen to <6 million yen, 6 million yen to <7.5 million yen, 7.5 million yen to <10 million yen, 10+ million yen, or unknown, where 1 million yen is equivalent to USD 10,000), basic necessities they have, including 14 items [i.e., books appropriate for their child’s age, sports items/toys/stuffed toys for children, a place where their child can study, a washing machine, a rice cooker, a vacuum cleaner, heater/heating appliances, an air conditioner, a microwave, a phone (includes both landlines and mobiles), a bathtub per household, a bed/mattress per person, >50,000 yen in savings for emergencies, none of the above], and their capacity to pay for lifeline utility costs including 12 items [e.g., school field trips/extracurricular activities, school textbooks, school lunches, rent, housing loans, electricity bills, gas bills, water bills, phone bills (includes both landlines and mobiles), insurance fees for public pension/national health insurance/public nursing care, bus, or train fees for commuting, none of the above]. Based on these three variables, child poverty is defined in this study as a child who falls into any one of the following categories: (1) annual household income is <3 million yen; (2) household lacks one or more basic necessities, and (3) family lacks the capacity to pay for one or more types of lifeline utility cost. This definition is based on the deprivation theory about relative poverty, which focuses on the combination of monetary and non-monetary criteria (Townsend, 1979; Nolan and Whelan, 2010) and has been used in a previous study (Nawa et al., 2018).
Self-Esteem
Children were asked about their self-esteem using one of the subscales from the Japanese version of the Children’s Perceived Competence Scale (Sakurai, 1992), which was developed based on the Perceived Competence Scale for Children (Harter, 1982). Ten items are related to self-esteem (e.g., “Are you satisfied with the way you are now?” or “Do you think you have few food points?”) and is rated using a scale of 1 (no) to 4 (yes). A higher total score denoted a higher level of self-esteem. The Cronbach’s alpha for the scale was 0.86 in this study.
Family-Level Factors
We assessed parental mental health and parental involvement with their child as family-level factors. Parental mental health was assessed using the Japanese version of the Kessler 6 (K6) (Furukawa et al., 2008). Higher scores, which range from 0 to 24, indicate frequent problems of psychological distress. The estimated cut-off point on this tool is a score of 4/5 (Sakurai et al., 2011). The Cronbach’s alpha for the scale was 0.89 in this study. Parental involvement with their child was assessed as a latent variable using five items, in which four of the five items were rated by the caregivers (i.e., smoking in front of a child, frequency of talking about school life, frequency of cooking for a child, and frequency of eating vegetables) and one of five items were rated by children (i.e., frequency of having breakfast). Smoking in front of a child was rated on a scale of 1 (often) to 4 (never), and was categorized into two groups (not smoking in front of a child and smoking in front of child). Frequency of talking about school life with their child and frequency of cooking for a child were rated on a scale of 1 (almost everyday) to 5 (rarely), and these scores were reversed to use in the analysis. Frequency of eating vegetables on a scale of 1 (everyday, for both breakfast and dinner) to 5 (less than 1 meal/week). Frequency of having breakfast was rated on a scale of 1 (everyday) to 4 (never), and was categorized into three groups (everyday, sometimes, and not very often/never). The confirmatory one-factor analysis showed the good model fit [Standardized Root Mean Square Residual {SRMR} = 0.014; Root Mean Square Error of Approximation {RMSEA} < 0.001 {90% Confidence Interval (CI) = < 0.001 to 0.039}; Comparative Fit Index {CFI} = 1.000].
School-Level Factors
Children were asked about school social capital using seven items on a scale of 1 (I do not agree at all) to 5 (I agree). The items were “I like the classroom atmosphere,” “I like my homeroom teacher,” “I think school is fun,” “I greet my teachers and my classmates,” “I trust my teacher,” “I trust my classmates,” and “I actively participate in school activities.” The total score was calculated using the sum of seven items and ranged from 7 to 35, in which the score of each item was reversed (Cronbach’s alpha = 0.88). Higher scores indicate that a child has poor school social capital.
Community-Level Factors
Parental social capital was assessed as a latent variable using the following three items, which have been used in earlier studies (Fujiwara et al., 2016; Nawa et al., 2018): “Do you agree or disagree with the following statements? (1) People in your community can be trusted (trust); (2) this community is close-knit (ties); (3) people in your community are willing to help their neighbors (mutual aid).” The caregivers rated these items on a scale of 1 (strongly agree) to 5 (strongly disagree). The Cronbach’s alpha was 0.87 in this study, and the confirmatory one-factor analysis showed the good model fit [SRMR < 0.001; RMSEA < 0.001 (90% CI = < 0.001 to < 0.001); CFI = 1.000].
Statistical Analysis
First, means and standard deviations or numbers and percentages were calculated for the total sample and for subgroups (i.e., children living in poverty and no poverty). Moreover, the differences of variables between subgroups were examined using the χ2-test or t-test. Second, Spearman’s correlation analysis was performed to explore the associations between variables used for structural equation modeling (SEM). Third, SEM was performed to test the model fit of the hypothetical model (Figure 1), in which we created the latent variables regarding parental involvement with children and parental social capital. We performed SEM in several steps as follows: (1) the path model examining the association between child poverty and low self-esteem; (2) the path model examining the mediation effect of poor parental involvement with their child on the association between child poverty and low self-esteem; (3) the path model examining the mediation effects of poor parental mental health and poor parental social capital on the association between child poverty and poor parental involvement in addition to the previous path model; (4) the path model examining the mediation effect of poor school social capital on the association between parental involvement and low self-esteem in addition to the previous path model; (5) the hypothetical model (Figure 1) including grade and child sex in the previous model. To assess the fitness of the hypothetical model, fit indices including SRMR, RMSEA, and CFI were used. In this study, we used the following criteria (Hu and Bentler, 1998) to evaluate model fit: SRMR value below 0.08; RMSEA value below 0.06, and CFI value above 0.95. The data were analyzed with STATA version 14.1.
Results
Characteristics of the Sample
Table 1 shows the distribution of characteristics and variables used in the SEM by status of child poverty. In this study, 434 of 1580 children were living in poverty (27.5%) in Adachi City, Tokyo, Japan. Mothers living in poverty were likely to be young compared with those who were not living in poverty (p < 0.001). Children living in poverty showed lower self-esteem (p < 0.001), their parents had lower social capital (trust: p < 0.001; tie: p = 0.001; mutual aid: p < 0.001) and a higher K6 score (p < 0.001), their parents were more likely to smoke in front of their child (p < 0.001), less likely to talk about school life with their child (p < 0.001), and less likely to cook for their child (p = 0.001). Children living in poverty were less likely to have breakfast (p < 0.001), less likely to eat vegetables (p < 0.001), and showed lower school social capital scores (p = 0.009) compared with those not living in poverty.
Table 1.
Characteristics of the sample.
| Child poverty |
||||||||
|---|---|---|---|---|---|---|---|---|
| All (N = 1580) |
Yes (N = 434) |
No (N = 1146) |
||||||
| Mean or N | SD or % | Mean or N | SD or % | Mean or N | SD or % | χ2 or t | p | |
| Grade | ||||||||
| Fourth | 514 | 32.5 | 142 | 32.7 | 372 | 32.5 | ||
| Sixth | 511 | 32.3 | 125 | 28.8 | 386 | 33.7 | ||
| Eighth | 555 | 35.1 | 167 | 38.5 | 388 | 33.9 | 4.24 | 0.12 |
| Sex of child | ||||||||
| Male | 768 | 48.6 | 205 | 47.2 | 563 | 49.1 | ||
| Female | 812 | 51.4 | 229 | 52.8 | 583 | 50.9 | 0.45 | 0.50 |
| Responder for caregiver’s questionnaire | ||||||||
| Mother | 1419 | 89.8 | 396 | 91.2 | 1023 | 89.3 | ||
| Father | 137 | 8.7 | 33 | 7.6 | 104 | 9.1 | ||
| Others | 15 | 0.9 | 5 | 1.2 | 10 | 1.5 | ||
| Missing | 9 | 0.6 | 0 | 0 | 9 | 0.1 | 10.17 | 0.12 |
| Age of parents | ||||||||
| Maternal age | 42.05 | 4.99 | 40.89 | 5.60 | 42.49 | 4.66 | 5.63 | <0.001 |
| Paternal age | 44.34 | 6.02 | 43.64 | 7.64 | 44.52 | 5.52 | 2.16 | 0.03 |
| Household income | ||||||||
| <JPY3,000,000 | 1248 | 79 | 189 | 43.5 | 1059 | 92.4 | ||
| ≧JPY3,000,000 | 202 | 12.8 | 202 | 46.5 | 0 | 0 | ||
| Missing | 130 | 8.2 | 43 | 9.9 | 87 | 7.6 | ||
| Number of lacking basic necessities | 0.32 | 1.06 | 1.15 | 1.76 | 0 | 0 | ||
| Number of lacking payment capacity | 0.19 | 0.75 | 0.70 | 1.31 | 0 | 0 | ||
| Self-esteem | 16.06 | 6.57 | 14.73 | 6.57 | 16.56 | 6.68 | 4.87 | <0.001 |
| Parental social capital | ||||||||
| Trust | ||||||||
| Strongly agree | 197 | 12.5 | 46 | 10.6 | 151 | 13.2 | ||
| Somewhat agree | 625 | 39.6 | 147 | 33.9 | 478 | 41.7 | ||
| Neither agree nor disagree | 640 | 40.5 | 189 | 43.5 | 451 | 39.3 | ||
| Somewhat disagree | 62 | 3.9 | 25 | 5.8 | 37 | 3.2 | ||
| Strongly disagree | 56 | 3.5 | 27 | 6.2 | 29 | 2.5 | 25.17 | <0.001 |
| Ties | ||||||||
| Strongly agree | 165 | 10.4 | 40 | 9.2 | 125 | 10.9 | ||
| Somewhat agree | 500 | 31.6 | 119 | 27.4 | 381 | 33.2 | ||
| Neither agree nor disagree | 750 | 47.5 | 208 | 47.9 | 542 | 47.3 | ||
| Somewhat disagree | 84 | 5.3 | 33 | 7.6 | 51 | 4.4 | ||
| Strongly disagree | 81 | 5.1 | 34 | 7.8 | 47 | 4.1 | 18.71 | 0.001 |
| Mutual aid | ||||||||
| Strongly agree | 136 | 8.6 | 31 | 7.1 | 105 | 9.2 | ||
| Somewhat agree | 527 | 33.3 | 127 | 29.3 | 400 | 34.9 | ||
| Neither agree nor disagree | 748 | 47.3 | 204 | 47.0 | 544 | 47.5 | ||
| Somewhat disagree | 90 | 5.7 | 35 | 8.1 | 55 | 4.8 | ||
| Strongly disagree | 79 | 5.0 | 37 | 8.6 | 42 | 3.7 | 25.27 | <0.001 |
| Parental mental health | ||||||||
| K6 score | 4.08 | 4.61 | 5.98 | 5.91 | 3.37 | 3.78 | -10.41 | <0.001 |
| Parental involvement | ||||||||
| Smoking in front of child | ||||||||
| Yes | 418 | 26.5 | 181 | 41.7 | 237 | 20.7 | ||
| No | 1162 | 73.5 | 253 | 58.3 | 909 | 79.3 | 71.52 | <0.001 |
| Frequency of talking about school life | ||||||||
| Almost everyday | 993 | 62.9 | 232 | 53.5 | 761 | 66.4 | ||
| 3–4 times/week | 305 | 19.3 | 105 | 24.2 | 200 | 17.4 | ||
| 1–2 times/week | 183 | 11.6 | 55 | 12.7 | 128 | 11.2 | ||
| 1–2 times/month | 65 | 4.1 | 27 | 6.2 | 38 | 2.2 | ||
| Rarely | 34 | 2.1 | 15 | 3.5 | 19 | 1.7 | 27.61 | <0.001 |
| Frequency of having breakfast (child) | ||||||||
| Everyday | 1383 | 87.5 | 330 | 76.0 | 1053 | 91.9 | ||
| Sometimes | 141 | 8.9 | 73 | 16.8 | 68 | 5.9 | ||
| Not very often/never | 56 | 3.5 | 31 | 7.1 | 25 | 2.2 | 72.70 | <0.001 |
| Frequency of eating vegetables | ||||||||
| Everyday, for both breakfast and dinner | 284 | 18.0 | 51 | 11.7 | 233 | 20.3 | ||
| Usually, for both breakfast and dinner | 301 | 19.0 | 66 | 15.2 | 235 | 20.5 | ||
| Everyday, for either breakfast or dinner | 779 | 49.3 | 232 | 53.5 | 547 | 47.7 | ||
| 2–3 meals/week | 102 | 11.5 | 72 | 16.6 | 110 | 9.6 | ||
| Less than 1 meal/week | 34 | 2.1 | 13 | 3.0 | 21 | 1.8 | 34.96 | <0.001 |
| Frequency of cooking for child | ||||||||
| Almost everyday | 1364 | 86.3 | 349 | 80.4 | 1015 | 88.6 | ||
| About 4–5 days/week | 102 | 6.5 | 42 | 9.7 | 60 | 5.2 | ||
| About 2–3 days/week | 34 | 2.2 | 15 | 3.5 | 19 | 1.7 | ||
| A few days during the month | 36 | 2.3 | 13 | 3.0 | 23 | 2.0 | ||
| Almost never | 44 | 2.8 | 15 | 3.5 | 29 | 2.5 | 19.09 | 0.001 |
| School social capital | 27.79 | 6.25 | 27.13 | 6.85 | 28.04 | 5.99 | 2.58 | 0.009 |
Correlations Between Variables Used in Structural Equation Modeling
Table 2 shows the results of Spearman’s correlation analysis to explore the association between variables used in the SEM. Child poverty showed a small (Cohen, 1988) but significant correlation with low self-esteem (r = 0.12, p < 0.001), poor parental social capital (trust: r = 0.12, p < 0.001; tie: r = 0.10, p < 0.001; mutual aid: r = 0.11, p < 0.001), poor maternal mental health (r = 0.25, p < 0.001), smoking in front of the child (r = 0.21, p < 0.001), low frequency of talking about school life with the child (r = 0.12, p < 0.001), low frequency of having breakfast (r = 0.21, p < 0.001), and low frequency of eating vegetables (r = 0.15, p < 0.001). Low self-esteem was correlated with grade (r = 0.27, p < 0.001), poor parental social capital (trust: r = 0.10, p < 0.001; tie: r = 0.09, p < 0.001; mutual aid: r = 0.11, p < 0.001), poor maternal mental health (r = 0.13, p < 0.001), smoking in front of the child (r = 0.11, p < 0.001), low frequency of talking about school life with the child (r = 0.15, p < 0.001), low frequency of having breakfast (r = 0.18, p < 0.001), low frequency of eating vegetables (r = 0.13, p < 0.001), and low school social capital (r = 0.36, p < 0.001). Sex of child showed no correlation with any variables. Grade was correlated with low frequency of talking about school life with the child (r = 0.16, p < 0.001) and low school social capital (r = 0.24, p < 0.001). Poor parental social capital, especially trust, was correlated with poor maternal mental health (r = 0.18, p < 0.001), smoking in front of the child (r = 0.10, p < 0.001), low frequency of having breakfast (r = 0.10, p < 0.001), and low frequency of eating vegetables (r = 0.10, p < 0.001). Poor parental social capital, especially ties, was correlated with poor maternal mental health (r = 0.11, p < 0.001), frequency of talking about school life with the child (r = 0.13, p < 0.001), low frequency of having breakfast (r = 0.12, p < 0.001), and low school social capital (r = 0.10, p < 0.001). Poor parental social capital, especially mutual aid, was correlated with poor maternal mental health (r = 0.16, p < 0.001), smoking in front of the child (r = 0.10, p < 0.001), frequency of talking about school life with the child (r = 0.13, p < 0.001), low frequency of having breakfast (r = 0.13, p < 0.001), low frequency of eating vegetables (r = 0.11, p < 0.001), and low school social capital (r = 0.13, p < 0.001). Low frequency of talking about school life was associated with low school social capital (r = 0.18, p < 0.001). Low frequency of having breakfast was associated with low school social capital (r = 0.15, p < 0.001).
Table 2.
Results of Spearman’s correlation analysis.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Child poverty | – | ||||||||||||
| 2. | Low self-esteem | 0.12∗∗∗ | – | |||||||||||
| 3. | Sex of child | 0.02 | 0.08∗∗ | – | ||||||||||
| 4. | Grade | 0.02 | 0.27∗∗∗ | 0.03 | – | |||||||||
| 5. | Poor caregiver’s social capital (Trust) | 0.12∗∗∗ | 0.10∗∗∗ | 0.01 | 0.04 | – | ||||||||
| 6. | Poor caregiver’s social capital (Tie) | 0.10∗∗∗ | 0.09∗∗∗ | 0.01 | 0.06∗ | 0.67∗∗∗ | – | |||||||
| 7. | Poor caregiver’s social capital (Mutual aid) | 0.11∗∗∗ | 0.11∗∗∗ | 0.02 | 0.06∗ | 0.70∗∗∗ | 0.72∗∗∗ | – | ||||||
| 8. | Poor maternal mental health (K6) | 0.25∗∗∗ | 0.13∗∗∗ | 0.01 | 0.03 | 0.18∗∗∗ | 0.11∗∗∗ | 0.16∗∗∗ | – | |||||
| 9. | Smoke in front of child | 0.21∗∗∗ | 0.11∗∗∗ | -0.03 | 0.06∗ | 0.10∗∗∗ | 0.07∗∗ | 0.10∗∗∗ | 0.08∗∗∗ | – | ||||
| 10. | Low frequency of talking about school life | 0.12∗∗∗ | 0.15∗∗∗ | -0.09∗∗∗ | 0.16∗∗∗ | 0.08∗∗ | 0.13∗∗∗ | 0.13∗∗∗ | 0.07∗∗ | 0.06∗ | – | |||
| 11. | Low frequency of having breakfast | 0.21∗∗∗ | 0.18∗∗∗ | 0.06∗ | 0.09∗∗∗ | 0.10∗∗∗ | 0.12∗∗∗ | 0.13∗∗∗ | 0.11∗∗∗ | 0.15∗∗∗ | 0.16∗∗∗ | – | ||
| 12. | Low frequency of eating vegetable | 0.15∗∗∗ | 0.13∗∗∗ | -0.06∗ | 0.02 | 0.10∗∗∗ | 0.08∗∗ | 0.11∗∗∗ | 0.10∗∗∗ | 0.17∗∗∗ | 0.15∗∗∗ | 0.18∗∗∗ | – | |
| 13. | Low frequency of cooking for child | 0.08∗∗ | 0.06∗ | 0.02 | 0.07∗∗ | 0.06∗ | 0.05 | 0.05∗ | 0.07∗∗ | 0.09∗∗∗ | 0.10∗∗∗ | 0.13∗∗∗ | 0.13∗∗∗ | – |
| 14. | Low school social capital | 0.06∗ | 0.37∗∗∗ | −0.09∗∗∗ | 0.24∗∗∗ | 0.07∗∗ | 0.10∗∗∗ | 0.13∗∗∗ | 0.09∗∗∗ | 0.03 | 0.18∗∗∗ | 0.15∗∗∗ | 0.05 | 0.07∗∗ |
∗p < 0.05, ∗∗p < 0.01, and ∗∗∗p < 0.001.
In this study, sex of the child and grade was used as covariates in the SEM. The results showed the sex of the child was significantly associated with low self-esteem (t, p, data not shown), which was consistent with the previous study (Birndorf et al., 2005). Grade was the most highly correlated variable with low self-esteem (r = 0.27, p < 0.001) and low school social capital (r = 0.36, p < 0.001), which was consistent with the previous studies (Twenge and Campbell, 2002).
Structural Equation Modeling
Firstly, SEM was performed to examine the association between child poverty and low self-esteem. The results showed the fit indices was good shown in Table 3. Standardized estimation of path coefficient was significant (β = 0.12, p < 0.001), indicating that child poverty leads to low self-esteem.
Table 3.
Results of SEM.
| RMSEA (90% CI) | CFI | SRMR | |
|---|---|---|---|
| Child poverty and low self-esteem | <0.001 (<0.001 to <0.001) | 1.000 | <0.001 |
| Add poor parental involvement | 0.030 (0.016–0.043) | 0.962 | 0.023 |
| Add poor parental mental health and poor parental social capital | 0.022 (0.013–0.030) | 0.990 | 0.020 |
| Add poor school social capital | 0.029 (0.022–0.036) | 0.981 | 0.025 |
| Add grade and child sex (final model) | 0.037 (0.032–0.043) | 0.959 | 0.036 |
RMSEA, root mean square error of approximation, 90% CI, 90% confidence interval; CFI, comparative fit index; SRMR, standardized root mean square residual.
Second, SEM was performed to examine the mediation effect of poor parental involvement with their child on the association between child poverty and low self-esteem. The results showed the fit indices was good (Table 3), in which poor parental involvement with their child fully mediated between child poverty and low self-esteem (from child poverty to poor parental involvement: β = 0.43, p < 0.001; from poor parental involvement to low self-esteem: β = 0.37, p < 0.001; from child poverty to low self-esteem: β = −0.03, p = 0.32).
Third, SEM was performed to examine the mediation effects of poor parental mental health and poor parental social capital on the association between child poverty and parental poor involvement in addition to the second analysis model. The results showed the fit indices was good (Table 3), in which the association between child poverty and poor parental involvement with their child was partially mediated by both poor parental mental health (from child poverty to poor parental mental health: β = 0.13, p < 0.001; from poor parental mental health to poor parental involvement: β = 0.12, p < 0.001) and poor parental social capital (from child poverty to poor parental social capital: β = 0.13, p < 0.001; from poor parental social capital to poor parental involvement: β = 0.25, p < 0.001). The association between child poverty and parental poor involvement with their child was significant (β = 0.36, p < 0.001).
Fourth, SEM was performed to examine the mediation effects of poor school social capital on the association between poor parental involvement with their child and low self-esteem in addition to the third analysis model. The results showed that the fit indices were good (Table 3), in which poor school social capital partially mediated between poor parental involvement with their child and low self-esteem (from parental poor involvement to poor school social capital: β = 0.26, p < 0.001; from poor school social capital to low self-esteem: β = 0.30, p < 0.001; from poor parental involvement to low self-esteem; β = 0.28, p < 0.001).
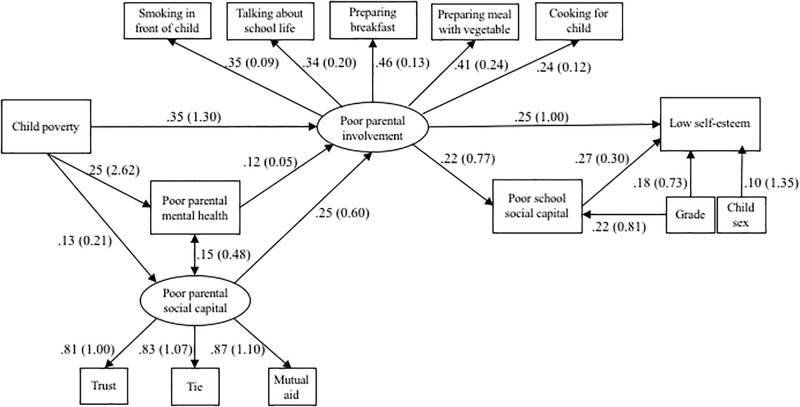
Finally, SEM was performed to examine model fit of the hypothesized model, which included the covariates such as grade and child sex (Figure 1). The results showed that the fit of the hypothetical model was good. Although we supposed the direct pathway between child poverty and low self-esteem in the hypothetical model, the results of all previous analysis models, which account for the mediated variables, did not show the significant association. Therefore, we excluded the direct pathway between child poverty and low self-esteem (Figure 3), in which the results of model testing were not changed.
FIGURE 3.
Results of structural equation model. Standardized beta and raw estimates in parenthesis of path coefficient are reported.
As shown in Figure 3, child poverty leads to poor parental involvement with the child (β = 0.35, p < 0.001), in which this pathway can be indirectly associated through poor parental mental health (from child poverty to poor parental mental health: β = 0.25, p < 0.001; from poor parental mental health to poor parental involvement; β = 0.12, p < 0.001) and poor parental social capital (from child poverty to poor parental social capital: β = 0.13, p < 0.001; from poor parental social capital to poor parental involvement; β = 0.25, p < 0.001). Then, poor parental involvement with the child was directly or indirectly associated with low self-esteem (directly pass: β = 0.25, p < 0.001) through poor school social capital (from poor parental involvement to poor school social capital: β = 0.22, p < 0.001; from poor school social capital to low self-esteem: β = 0.27, p < 0.001). In terms of the latent variables (i.e., poor parental social capital and poor parental involvement), both latent variables had the significant standardized beta for each effect indicator.
Discussion
In the current study, we found that the association between child poverty and low self-esteem was mediated by family-, school-, and community-level factors by performing SEM. Rather than child poverty being directly associated with low self-esteem, child poverty leads to poor parental involvement, in which this pathway can be indirectly associated through poor parental mental health and poor parental social capital. According to the standardized beta, child poverty was the most powerful determinant of poor parental involvement compared with poor parental mental health and poor parental social capital. Poor parental involvement was directly or indirectly associated through poor school social capital associated with low self-esteem. According to the standardized beta, poor parental involvement and poor school social capital had similar effects on low self-esteem.
Our findings consolidate the results of previous studies (Conger et al., 1992; Ho et al., 1995; Bolger et al., 1998; Mayhew and Lempers, 1998; Bean et al., 2003; Evans, 2004; Laible et al., 2004; Parker and Benson, 2004; Yoder and Hoyt, 2005; Pachter et al., 2006; Law et al., 2013; Rijlaarsdam et al., 2013; Oldfield et al., 2016; Orth, 2018) and elucidate the association between child poverty and low self-esteem. Although the impact of child poverty on low self-esteem increased significantly with age, many previous studies reported that the association between child poverty and low self-esteem was not strong (Twenge and Campbell, 2002), which is similar to the results of this study (β = 0.12, p < 0.001). The reason why the association between child poverty and low self-esteem is not strong can be explained by the fact found in this study, that is, family-, school-, and community-level factors mediated this association. In other words, child poverty and low self-esteem need to be interpreted in an ecological model incorporating individual-, family-, school-, and community-level factors as in previous studies (Robinson, 2008, e.g., Hindman et al., 2010; Park, 2018).
Considering the pathway of the association between child poverty and low self-esteem based on the ecological model, we may figure out several mediating factors which mitigate the negative impact of child poverty on low self-esteem. Focusing on parental involvement with the child, government agencies and schools may have opportunities to change parental involvement with children, although it is difficult for them to conduct an individual intervention to improve poor parental involvement directly. For example, Adachi City has conducted a strategy to increase vegetable consumption among school children by serving vegetables in the first course during school meals, which may lead to an increased chance of vegetable intake among children (Tani et al., 2016). Focusing on parental social capital, local government can also strengthen parental social capital as a strategy aimed at improving poor parental involvement with their child (Kimbrough-Melton and Melton, 2015; McDonell et al., 2015; Nawa et al., 2018). Additionally, parental mental health can be improved by a community-level intervention such as cognitive behavioral therapy and interpersonal therapy delivered by care providers who are not mental health specialists, which has the effect of decreasing common perinatal mental disorders (Clarke et al., 2013), and mindfulness-based stress reduction programs (Bazzano et al., 2015).
Shifting our perspective to the school level, the strengthening of school social capital may be helpful for increasing a child’s self-esteem because in this study the association between school social capital and self-esteem (β = 0.27) was as strong as parental involvement with the child (β = 0.25). Additionally, it may be easier to implement a school-level intervention than a community-level intervention because the group size of a classroom or school is smaller than that of a community. For example, various school-based interventions that may lead to promote school social capital have been found, such as a school-based social and emotional learning intervention aimed at enhancement of controls in social emotional skills and attitude (Taylor et al., 2017). Furthermore, because effect sizes of path coefficients were small, suggesting that other factors such as child’s social capital and relationship with family member other than parents may explain the association between child poverty and self-esteem, we need to consider other possible mediators to find more effective interventions to break the link between child poverty and self-esteem.
This study has several limitations. First, a causal relationship shown in the model (Figure 2) cannot be determined because there were still unmeasured confounders. In fact, the causal relationship between self-esteem and social support is controversial, that is, a previous study showed that a child’s perceived social support affects high self-esteem, and self-esteem is one of the determinants of receiving social support (e.g., Goodwin et al., 2004; Marshall et al., 2014). Second, measurement of parental involvement with the child consists of questions assessed by a questionnaire, which cannot be objective, thus measurement error can exist due to desirable response bias. Third, there might be sampling bias, that is, the caregivers who were living in poverty and the children with low self-esteem might be less likely to respond to the questionnaire. Even though the valid response rate in this study (82.9%) was not low, the caregivers who did not respond to the questionnaire might be more likely to be living in poverty and less likely to be interested in their own child. Moreover, children who did not respond to the questionnaire might be more likely to have low self-esteem. Nonetheless, this selection bias may induce underestimation of the association, which suggest that the coefficient in our study can be stronger. Further, our result is based on single community, which preclude the generalizability of our results, requiring careful extrapolation of our findings in other communities. That is, our findings may not generalize to rural area in Japan or other countries. Further studies need to replicates our findings in other setting.
In conclusion, comprehensive health policy targeting family-level (parental mental health and parental involvement with children), school-level (school social capital), and community-level (parental social capital) factors may be effective to mitigate the impact of child poverty on low self-esteem. To reinforce the pathway between child poverty and low self-esteem examined in this study, further studies using longitudinal methods are needed.
Ethics Statement
The A-CHILD protocol was approved by the Ethics Committee at the National Center for Child Health and Development (No. 1187) and the Ethics Committee at Tokyo Medical and Dental University (M2016-282-02).
Author Contributions
TF, AI, and MO designed the study. TF managed administration of the study, including the ethical review process. SD analyzed the data and drafted the manuscript. TF provided critical comments on the manuscript related to intellectual content. All authors have read and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are particularly grateful to the staff members and central office of Adachi City Hall for conducting the survey. We would like to thank everyone who participated in the surveys. In particular, we would also like to thank Mayor Yayoi Kondo, Mr. Syuichiro Akiu, Mr. Hideaki Otaka, and Ms. Yuko Baba of Adachi City Hall, all of whom contributed significantly to completion of this study.
Footnotes
Funding. We thank all the participants who contributed to the A-CHILD Study, which was supported by Comprehensive Research on Lifestyle Disease from the Japanese Ministry of Health, Labour and Welfare (H27-Jyunkankito-ippan-002), Research of Policy Planning and Evaluation from the Japanese Ministry of Health, Labour and Welfare (H29-Seisaku-Shitei-004), Innovative Research Program on Suicide Countermeasures (IRPSC), and Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS KAKENHI Grant Number 16H03276 and 16K21669), St. Luke’s Life Science Institute Grants, and the Japan Health Foundation Grants.
References
- Amemiya A., Fujiwara T. (2018). Association of low family income with lung function among children and adolescents: results of the J-SHINE study. J. Epidemiol. 29 50–56. 10.2188/jea.JE20170220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atilola O. (2017). Child mental-health policy development in sub-Saharan Africa: broadening the perspectives using Bronfenbrenner’s ecological model. Health Promot. Int. 32 380–391. 10.1093/heapro/dau065 [DOI] [PubMed] [Google Scholar]
- Balaji A. B., Claussen A. H., Smith D. C., Visser S. N., Morales M. J., Perou R. (2007). Social support networks and maternal mental health and well-being. J. Womens Health 16 1386–1396. [DOI] [PubMed] [Google Scholar]
- Bazzano A., Wolfe C., Zylowska L., Wang S., Schuster E., Barrett C., et al. (2015). Mindfulness based stress reduction (MBSR) for parents and caregivers of individuals with developmental disabilities: a community-based approach. J. Child Fam. Stud. 24 298–308. [Google Scholar]
- Bean R. A., Bush K. R., Mckenry P. C., Wilson S. M. (2003). The impact of parental support, behavioral control, and psychological control on the academic achievement and self-esteem of African American and European American adolescents. J. Adolesc. Res. 18 523–541. [Google Scholar]
- Birndorf S., Ryan S., Auinger P., Aten M. (2005). High self-esteem among adolescents: longitudinal trends, sex differences, and protective factors. J. Adolesc. Health 37 194–201. [DOI] [PubMed] [Google Scholar]
- Bolger K. E., Patterson C. J., Kupersmidt J. B. (1998). Peer relationships and self-esteem among children who have been maltreated. Child Dev. 69 1171–1197. [PubMed] [Google Scholar]
- Bronfenbrenner U. (1997). The Ecology of Human Development. Cambridge, MA: Harvard University Press. [Google Scholar]
- Bronfenbrenner U. (2005). Making Human beings Human: Bioecological Perspectives on Human Development. London: SAGE Publications, Inc. [Google Scholar]
- Bronfenbrenner U., Morris P. A. (1998). “The ecology of developmental processes,” in Handbook of Child Psychology: Theoretical Models of Human Development Vol. 1 eds Damon W., Lerner R. M. (New York, NY: Wiley; ), 993–1028. [Google Scholar]
- Clarke K., King M., Prost A. (2013). Psychosocial interventions for perinatal common mental disorders delivered by providers who are not mental health specialists in low-and middle-income countries: a systematic review and meta-analysis. PLoS Med. 10:e1001541. 10.1371/journal.pmed.1001541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical Power analysis for the Behavioral Sciences, 2nd Edn. Philadelphia, PA: Lawrence Erlbaum Associates. [Google Scholar]
- Conger R. D., Conger K. J., Elder G. H., Jr., Lorenz F. O., Simons R. L., Whitbeck L. B. (1992). A family process model of economic hardship and adjustment of early adolescent boys. Child Dev. 63 526–541. [DOI] [PubMed] [Google Scholar]
- Dekhtyar S., Wang H. X., Scott K., Goodman A., Koupil I., Herlitz A. (2015). A life-course study of cognitive reserve in dementia—from childhood to old age. Am. J. Geriatr. Psychiatry 23 885–896. 10.1016/j.jagp.2015.02.002 [DOI] [PubMed] [Google Scholar]
- Delgado-Angulo E. K., Hobdell M. H., Bernabe E. (2009). Poverty, social exclusion and dental caries of 12-year-old children: a cross-sectional study in Lima, Peru. BMC Oral Health 9:16. 10.1186/1472-6831-9-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnellan M. B., Trzesniewski K. H., Robins R. W. (2011). “Self-esteem: enduring issues and controversies,” in Handbook of Individual Differences, eds Chamorro-Premuzic S., Stumm V., Furnham A. (New York, NY: Wiley-Blackwell; ), 718–746. [Google Scholar]
- Evans G. W. (2004). The environment of childhood poverty. Am. Psychol. 59 77–92. [DOI] [PubMed] [Google Scholar]
- Fujiwara T. (2014). Socioeconomic status and the risk of suspected autism spectrum disorders among 18-month-old toddlers in Japan: a population-based study. J. Autism Dev. Disord. 44 1323–1331. 10.1007/s10803-013-1988-3 [DOI] [PubMed] [Google Scholar]
- Fujiwara T., Kondo K., Shirai K., Suzuki K., Kawachi I. (2013). Associations of childhood socioeconomic status and adulthood height with functional limitations among Japanese older people: results from the JAGES 2010 Project. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 69 852–859. 10.1093/gerona/glt189 [DOI] [PubMed] [Google Scholar]
- Fujiwara T., Yamaoka Y., Kawachi I. (2016). Neighborhood social capital and infant physical abuse: a population-based study in Japan. Int. J. Ment. Health Syst. 10:13. 10.1186/s13033-016-0047-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T. A., Kawakami N., Saitoh M., Ono Y., Nakane Y., Nakamura Y., et al. (2008). he performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 17 152–158. 10.1002/mpr.257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman S. E., Kawachi I., Fitzmaurice G. M., Buka S. L. (2003). Family disruption in childhood and risk of adult depression. Am. J. Psychiatry 160 939–946. [DOI] [PubMed] [Google Scholar]
- Goodwin R., Costa P., Adonu J. (2004). Social support and its consequences: ‘positive’ and ‘deficiency’ values and their implications for support and self-esteem. Br. J. Soc. Psychol. 43 465–474. [DOI] [PubMed] [Google Scholar]
- Harter S. (1982). The perceived competence scale for children. Child Dev. 53 87–97. [PubMed] [Google Scholar]
- Hedayati S. S., Yalamanchili V., Finkelstein F. O. (2012). A practical approach to the treatment of depression in patients with chronic kidney disease and end-stage renal disease. Kidney Int. 81 247–255. 10.1038/ki.2011.358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindman A. H., Skibbe L. E., Miller A., Zimmerman M. (2010). Ecological contexts and early learning: contributions of child, family, and classroom factors during Head Start, to literacy and mathematics growth through first grade. Early Child. Res. Q. 25 235–250. [Google Scholar]
- Ho C. S., Lempers J. D., Clark-Lempers D. S. (1995). Effects of economic hardship on adolescent self-esteem: a family mediation model. Adolescence 30 117–131. [PubMed] [Google Scholar]
- Hu L. T., Bentler P. M. (1998). Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol. Methods 3 424–453. [Google Scholar]
- Kimbrough-Melton R. J., Melton G. B. (2015). “Someone will notice, and someone will care”: how to build strong communities for children. Child Abuse Negl. 41 67–78. 10.1016/j.chiabu.2015.02.015 [DOI] [PubMed] [Google Scholar]
- Klevens R. M., Luman E. T. (2001). US children living in and near poverty: risk of vaccine-preventable diseases. Am. J. Prev. Med. 20 41–46. [DOI] [PubMed] [Google Scholar]
- Laible D. J., Carlo G., Roesch S. C. (2004). Pathways to self-esteem in late adolescence: the role of parent and peer attachment, empathy, and social behaviours. J. Adolesc. 27 703–716. [DOI] [PubMed] [Google Scholar]
- Law P. C., Cuskelly M., Carroll A. (2013). Young people’s perceptions of family, peer, and school connectedness and their impact on adjustment. J. Psychol. Couns. Sch. 23 115–140. [Google Scholar]
- Lynch S. V., Wood R. A., Boushey H., Bacharier L. B., Bloomberg G. R., Kattan M., et al. (2014). Effects of early-life exposure to allergens and bacteria on recurrent wheeze and atopy in urban children. J. Allergy Clin. Immunol. 134 593–601e512. 10.1016/j.jaci.2014.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manani P., Sharma S. (2016). Self esteem and suicidal ideation: a correlational study. MIER J. Educ. Stud. Trends Pract. 3 75–83. [Google Scholar]
- Mann M. M., Hosman C. M., Schaalma H. P., De Vries N. K. (2004). Self-esteem in a broad-spectrum approach for mental health promotion Journal: health education research. Health Educ. Res. 19 357–372. [DOI] [PubMed] [Google Scholar]
- Marshall S. L., Parker P. D., Ciarrochi J., Heaven P. C. (2014). Is self-esteem a cause or consequence of social support? A 4-year longitudinal study. Child Dev. 85 1275–1291. 10.1111/cdev.12176 [DOI] [PubMed] [Google Scholar]
- Mayhew K. P., Lempers J. D. (1998). The relation among financial strain, parenting, parent self-esteem, and adolescent self-esteem. J. Early Adolesc. 18 145–172. [Google Scholar]
- McDonell J. R., Ben-Arieh A., Melton G. B. (2015). Strong Communities for Children: results of a multi-year community-based initiative to protect children from harm. Child Abuse Negl. 41 79–96. 10.1016/j.chiabu.2014.11.016 [DOI] [PubMed] [Google Scholar]
- McGee R., Williams S., Nada-Raja S. (2001). Low self-esteem and hopelessness in childhood and suicidal ideation in early adulthood. J. Abnorm. Child Psychol. 29 281–291. [DOI] [PubMed] [Google Scholar]
- McGee R. O. B., Williams S. (2000). Does low self-esteem predict health compromising behaviours among adolescents? J. Adolesc. 23 569–582. [DOI] [PubMed] [Google Scholar]
- Nagaoka K., Fujiwara T. (2016). Impact of subsidies and socioeconomic status on Varicella Vaccination in greater Tokyo, Japan. Front. Pediatr. 4:19. 10.3389/fped.2016.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawa N., Isumi A., Fujiwara T. (2018). Community-level social capital, parental psychological distress, and child physical abuse: a multilevel mediation analysis. Soc. Psychiatry Psychiatr. Epidemiol. 53 1221–1229. 10.1007/s00127-018-1547-5 [DOI] [PubMed] [Google Scholar]
- Nolan B., Whelan C. T. (2010). Using non-monetary deprivation indicators to analyze poverty and social exclusion: lessons from Europe? J. Policy Anal. Manage. 29 305–325. [Google Scholar]
- OECD (2017). Child Poverty. Paris: OECD Publishing. [Google Scholar]
- Oldfield J., Humphrey N., Hebron J. (2016). The role of parental and peer attachment relationships and school connectedness in predicting adolescent mental health outcomes. Child Adolesc. Ment. Health 21 21–29. [DOI] [PubMed] [Google Scholar]
- Orth U. (2018). The family environment in early childhood has a jong-term effect on self-esteem: a longitudinal study from birth to age 27 years. J. Pers. Soc. Psychol. 114 637–655. 10.1037/pspp0000143 [DOI] [PubMed] [Google Scholar]
- Orth U., Robins R. W., Widaman K. F., Conger R. D. (2014). Is low self-esteem a risk factor for depression? Findings from a longitudinal study of Mexican-origin youth. Dev. Psychol. 50 622–633. 10.1037/a0033817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overholser J. C., Adams D. M., Lehnert K. L., Brinkman D. C. (1995). Self-esteem deficits and suicidal tendencies among adolescents. J. Am. Acad. Child Adolesc. Psychiatry 34 919–928. [DOI] [PubMed] [Google Scholar]
- Pachter L. M., Auinger P., Palmer R., Weitzman M. (2006). Do parenting and the home environment, maternal depression, neighborhood, and chronic poverty affect child behavioral problems differently in different racial-ethnic groups? Pediatrics 117 1329–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J. (2018). Predictors of health-promoting behaviors in children from low-income families: a n ecological approach. Nurs. Health Sci. 20 60–68. 10.1111/nhs.12388 [DOI] [PubMed] [Google Scholar]
- Parker J. S., Benson M. J. (2004). The impact of parental support, behavioral control, and psychological control on the academic achievement and self-esteem of African American and European American adolescents. Adolescence 39:519. [Google Scholar]
- Peres M. A., De Oliveira Latorre Mdo R., Sheiham A., Peres K. G., Barros F. C., Hernandez P. G., et al. (2005). Social and biological early life influences on severity of dental caries in children aged 6 years. Community Dent. Oral Epidemiol. 33 53–63. [DOI] [PubMed] [Google Scholar]
- Poorgholami F., Javadpour S., Saadatmand V., Jahromi M. K. (2015). Effectiveness of self-care education on the enhancement of the self-esteem of patients undergoing hemodialysis. Glob. J. Health Sci. 8 132–136. 10.5539/gjhs.v8n2p132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rijlaarsdam J., Stevens G. W., Van Der Ende J., Hofman A., Jaddoe V. W., Mackenbach J. P., et al. (2013). Economic disadvantage and young children’s emotional and behavioral problems: mechanisms of risk. J. Abnorm. Child Psychol. 41 125–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson T. (2008). Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. J. Commun. Health 33 395–406. 10.1007/s10900-008-9109-5 [DOI] [PubMed] [Google Scholar]
- Sakai Y. (2018). The Vaccination Kuznets Curve: do vaccination rates rise and fall with income? J. Health Econ. 57 195–205. 10.1016/j.jhealeco.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Sakurai K., Nishi A., Kondo K., Yanagida K., Kawakami N. (2011). Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin. Neurosci. 65 434–441. 10.1111/j.1440-1819.2011.02236.x [DOI] [PubMed] [Google Scholar]
- Sakurai S. (1992). The investigation of self-consciousness in the 5th-and 6th-grade children. Jpn. J. Exp. Soc. Psychol. 32 85–94. [Google Scholar]
- Sasaki M., Yoshida K., Adachi Y., Furukawa M., Itazawa T., Odajima H., et al. (2016). Environmental factors associated with childhood eczema: findings from a national web-based survey. Allergol. Int. 65 420–424. 10.1016/j.alit.2016.03.007 [DOI] [PubMed] [Google Scholar]
- Sowislo J. F., Orth U. (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol. Bull. 139 213–240. 10.1037/a0028931 [DOI] [PubMed] [Google Scholar]
- Steiger A. E., Allemand M., Robins R. W., Fend H. A. (2014). Low and decreasing self-esteem during adolescence predict adult depression two decades later. J. Pers. Soc. Psychol. 106 325–338. 10.1037/a0035133 [DOI] [PubMed] [Google Scholar]
- Tanaka K., Miyake Y., Sasaki S., Hirota Y. (2013). Socioeconomic status and risk of dental caries in Japanese preschool children: the Osaka Maternal and child health study. J. Public Health Dent. 73 217–223. 10.1111/jphd.12016 [DOI] [PubMed] [Google Scholar]
- Tani Y., Fujiwara T., Kondo N., Noma H., Sasaki Y., Kondo K. (2016). Childhood socioeconomic status and onset of depression among Japanese older adults: the JAGES prospective cohort study. Am. J. Geriatr. Psychiatry 24 717–726. 10.1016/j.jagp.2016.06.001 [DOI] [PubMed] [Google Scholar]
- Taylor R. D., Oberle E., Durlak J. A., Weissberg R. P. (2017). Promoting positive youth development through school-based social and emotional learning interventions: a meta-analysis of follow-up effects. Child Dev. 88 1156–1171. 10.1111/cdev.12864 [DOI] [PubMed] [Google Scholar]
- Townsend P. (1979). Poverty in the United Kingdom: A Survey of Household Resources and Standards of Living. Berkeley, CA: University of California Press. [Google Scholar]
- Trzesniewski K. H., Donnellan M. B., Moffitt T. E., Robins R. W., Poulton R., Caspi A. (2006). Low self-esteem during adolescence predicts poor health, criminal behavior, and limited economic prospects during adulthood. Dev. Psychol. 42 381–390. [DOI] [PubMed] [Google Scholar]
- Twenge J. M., Campbell W. K. (2002). Self-esteem and socioeconomic status: a meta-analytic review. Pers. Soc. Psychol. Rev. 6 59–71. [Google Scholar]
- van Tuijl L. A., De Jong P. J., Sportel B. E., De Hullu E., Nauta M. H. (2014). Implicit and explicit self-esteem and their reciprocal relationship with symptoms of depression and social anxiety: a longitudinal study in adolescents. J. Behav. Ther. Exp. Psychiatry 45 113–121. 10.1016/j.jbtep.2013.09.007 [DOI] [PubMed] [Google Scholar]
- Yoder K. A., Hoyt D. R. (2005). Family economic pressure and adolescent suicidal ideation: application of the family stress model. Suicide Life Threat. Behav. 35 251–264. [DOI] [PubMed] [Google Scholar]