Abstract
Background
Current literature only reports variable information from single‐center studies on the recurrence rate, the complications, and the outcome of patients with Takotsubo syndrome (TTS) experiencing recurrent TTS. Therefore, a detailed description of clinical characteristics, predictors, and the prognostic impact of patients with TTS and recurrences in a multicenter registry is needed.
Methods and Results
We analyzed 749 patients with TTS from 9 European centers being part of the international, multicenter GEIST (German Italian Stress Cardiomyopathy) Registry. Patients were divided into the recurrence group and the nonrecurrence group. The recurrence rate at a median follow‐up of 830 days (interquartile range, 118–1701 days) was 4%. Most recurrences were documented in the first 5 years after the index TTS episode. Up to 2 TTS recurrences were documented in 2 of 30 patients (6%). A variable ballooning pattern (n=6, 0.8%) with, in particular, involvement of the right ventricular occurred in 3 cases (0.4%) at the recurrence event. Except for the higher presence of arterial hypertension (86.7% versus 68.3%; P=0.03) in the recurrence group, no other baseline characteristics were different between groups. Observation of TTS complications during follow‐up, including stroke, thromboembolic events, in‐hospital death, and cardiogenic shock, revealed no significant differences between groups (P>0.05), except the higher presence of pulmonary edema in the recurrence group versus the nonrecurrence group (13.3% versus 4.9%; P=0.04).
Conclusions
The incidence of TTS recurrence is estimated to be 4% in this multicenter TTS registry. A variable TTS pattern at recurrence is common in up to 20% of recurrence cases.
Keywords: heart failure, Takotsubo cardiomyopathy, recurrence
Subject Categories: Cardiomyopathy, Heart Failure
Clinical Perspective
What Is New?
Takotsubo syndrome (TTS) is associated with a recurrence rate of 4%.
A variable TTS pattern at recurrence is common in up to 20% of recurrence cases.
What Are the Clinical Implications?
Patients with TTS are at risk of TTS recurrence.
In patients with a history of TTS and new symptoms mimicking acute coronary syndrome, physicians should consider the possibility of recurrent TTS.
Introduction
Takotsubo syndrome (TTS) is characterized by a transient ventricular dysfunction. Patients have symptoms mimicking an acute coronary syndrome.1, 2 Despite the transient character of TTS, a significant number of adverse events has been reported.3 Mainly in the short‐term phase of TTS, patients are experiencing arrhythmias, including sudden cardiac death,4, 5, 6 cardiogenic shock,7 and thromboembolic events, including stroke.8, 9 First, it has been thought that TTS may affect only the left ventricle (LV), whereas some years later right ventricular or biventricular involvement has been also reported.10, 11 The recovery of these wall motion abnormalities is observed within days to weeks. The following 4 different TTS forms have been reported to date: apical form, midventricular form, basal form, and rare focal form.12, 13 In the past decade, different studies have shown that TTS is not associated with a favorable prognosis, with a mortality rate comparable to that of acute coronary syndrome.3, 14
Current literature reports a recurrence rate of 1% to 6%.15, 16, 17 However, these data are inconsistent and frequently limited by its single‐center character. Moreover, it is not known which patients are at risk for recurrence and if the presence of TTS recurrences is associated with future cardiovascular events or mortality. In view of these limitations, we sought to comprehensively describe the incidence, clinical characteristics, predictors, and impact of recurrence in TTS in a large multicenter European registry.
Methods
The data, analytic methods, and study materials will be made available to other researchers for purposes of reproducing the results or replicating the procedure; they will be provided on request to the corresponding author. This multicenter GEIST (German Italian Stress Cardiomyopathy) Registry included 906 consecutive patients with TTS, enrolled from 9 centers: University Heart Center Lübeck (Lübeck, Germany); Heart Center Leipzig–University Hospital (Leipzig, Germany); University Medical Center Mannheim (Mannheim, Germany); University Hospital of Foggia (Foggia, Italy); Casa Sollievo della Sofferenza Hospital (San Giovanni Rotondo, Italy); San Paolo Hospital (Bari, Italy); University Hospital of Palermo (Palermo, Italy); University Hospital of Rome “Tor Vergata,” (Rome, Italy); and University Hospital “Umberto I–Lancisi–Salesi” (Ancona, Italy). Patients were prospectively included in accordance with diagnostic criteria for TTS.1 These criteria essentially highlight transient wall motion abnormality in the LV or right ventricle; and also describe an event that occurs frequently, but not always, in the wake of a stressful trigger. Other salient points mandate the absence of obstructive coronary disease related to wall motion abnormalities; focus on the appearance of new electrocardiographic pathological features, which mimic acute coronary syndrome or modest elevations in cardiac troponin levels; and underline the absence of pheochromocytoma or myocarditis in the patient. A ballooning pattern was defined, according to defined criteria, as being a transient systolic dysfunction with marked LV contraction abnormality attributable to akinesia or dyskinesia of the LV apical and/or midventricular or basal segments, extending beyond a single coronary perfusion bed.12, 18
Recurrence of TTS was defined as new wall motion abnormalities in the absence of obstructive coronary disease after recovery of the index TTS events. The recurrence of TTS was assessed by medical record review and/or telephonic review. If medical records, treating physicians, patients, or relatives were able to provide further information about the circumstances of recurrence, the angiograms, echocardiograms, and ECGs were independently reviewed by 2 experienced cardiologists (I.E.‐B., I.A., F.S., F. Gustafierro, N.D.B., T.S., C.M., I.E., G.N., S.N., E.M., Francesco Romeo, H.T., F. Guerra, A.C., I.G.) to evaluate the diagnosis of TTS. The study protocol was approved by the local Ethics Committee. All methods were performed in accordance with the relevant guidelines and regulations. The study was conducted in compliance with the Declaration of Helsinki on investigations in human subjects. Informed consent was waived by the Ethics Committee.
Statistical Analysis
Data are presented as means±SD for continuous variables with a normal distribution, median (interquartile range) for continuous variables with a nonnormal distribution, and frequency (percentage) for categorical variables. The Kolmogorov‐Smirnov test was used to assess normal distribution. The Student t test and the Mann‐Whitney U‐test were used to compare continuous variables with normal and nonnormal distributions, respectively. The χ2 test or Fisher's exact test was used to compare categorical variables. The log‐rank test was used to compare Kaplan‐Meier survival curves between the cardiopulmonary failure group and the noncardiopulmonary failure group. Factors with P<0.10 on univariate analysis were entered into the Cox multivariate regression to define independent risk factors for the end point. Statistical analysis was performed with SPSS 23.0 in all analyses; P≤0.05 (2 tailed) indicated statistical significance.
Results
Of the 906 consecutive patients included in the GEIST Registry, follow‐up was documented in 749. Baseline characteristics are illustrated in Table 1. Most patients were postmenopausal women (90.2%). A stressful event was documented in 70% of cases, with a predominance of a physical stress trigger (38.7%). The moderate reduced LV ejection fraction at the index event (median, 40% [interquartile range, 15%–71%]) was almost normalized through follow‐up (median, 53% [interquartile range, 20%–77%]). Overall, TTS recurrence was documented in 30 patients (4%) at a median follow‐up of 830 days (interquartile range, 118–1701 days; 95% CI, 981–1128 days).
Table 1.
Baseline Clinical Characteristics
| Variable | All Patients (n=749) | Patients With No Recurrence (n=719) | Patients With Recurrence (n=30) | P Value |
|---|---|---|---|---|
| Age, y | 70±10 | 70±11 | 68±13 | 0.30 |
| Women | 676 (90.2) | 651 (90.5) | 25 (83.3) | 0.19 |
| Hypertension | 596 (70.1) | 491 (68.3) | 25 (86.7) | 0.03 |
| Current smoking | 187 (22.7) | 159 (22.1) | 10 (33.3) | 0.15 |
| Malignancy | 123 (13.9) | 95 (13.2) | 3 (10.0) | 0.61 |
| Stressful event | 526 (70.2) | 505 (70.2) | 21 (70.0) | 0.98 |
| Emotional | 290 (38.7) | 281 (39.1) | 9 (30.0) | 0.31 |
| Physical | 238 (31.8) | 224 (31.1) | 12 (40.0) | 0.10 |
| Ballooning pattern | ||||
| Apical | 616 (82.2) | 590 (82.4) | 26 (86.7) | 0.54 |
| Midventricular | 134 (17.8) | 129 (17.9) | 5 (16.7) | 0.86 |
| Basal | 17 (2.3) | 17 (2.4) | 0 (0.0) | 1.00 |
| Focal | 1 (0.1) | 1 (0.2) | 0 (0.0) | 1.00 |
| LVEF, % | 40 (15–71) | 40 (15–71) | 40 (25–59) | 0.87 |
| Time of hospitalization, d | 8 (1–96) | 8 (1–96) | 6 (2–16) | 0.29 |
| Follow‐up LVEF, % | 53 (20–77) | 53 (20–77) | 54 (40–72) | 0.58 |
Data are presented as number (percentage) of patients, mean±SD for normal distribution, and median (interquartile range) for nonnormal distribution. P values were calculated for the comparison between patients with Takotsubo syndrome and recurrence. LVEF indicates left ventricular ejection fraction.
Clinical Characteristics of the Patients With TTS Recurrence
Patients with TTS who experienced recurrence events tended to be younger (mean±SD, 68±13 versus 70±11 years; P=0.3). Cardiovascular risk factors, such as arterial hypertension (86.7% versus 68.3%; P=0.03), were significantly higher in the recurrence group. Observing the different TTS forms/ballooning patterns and the LV ejection fraction at index event and/or follow‐up, there was no difference between both groups. Even more, further baseline characteristics, including malignancy and current smoking, were not different between both groups. At the recurrence episode, most patients (n=21) presented with the apical form, whereas the midventricular form was evident in 7 patients. In our cohort, 20% of patients presented with variable ballooning at the recurrence episode: 3 patients with an apical pattern at the index event and a midventricular pattern at the recurrence event and a further 3 patients with right ventricular involvement at the recurrence event. Detailed information of triggers of TTS recurrence is illustrated in Table 2. Interestingly, in 14 patients (46%), TTS has been triggered by a new stressor compared with the first TTS event (9 patients experienced an emotional trigger, and 5 patients experienced a physical trigger).
Table 2.
In‐Hospital Events of Patients With TTS
| Variable | All Patients (n=749) | Patients With No Recurrence (n=719) | Patients With Recurrence (n=30) | P Value |
|---|---|---|---|---|
| Cardiac electronic device implantation | 9 (1.2) | 9 (1.3) | 0 (0.0) | 1.00 |
| In‐hospital death | 19 (2.5) | 18 (2.5) | 1 (3.3) | 0.55 |
| Thromboembolic events | 21 (2.8) | 20 (2.8) | 1 (3.3) | 0.58 |
| Stroke | 10 (1.3) | 9 (1.3) | 1 (3.3) | 0.34 |
| Cardiogenic shock | 59 (7.8) | 59 (8.2) | 0 (0.0) | 0.16 |
| Pulmonary edema | 39 (5.2) | 35 (4.9) | 4 (13.3) | 0.04 |
Data are given as number (percentage) of patients. TTS indicates Takotsubo syndrome.
Predictors of Recurrence in TTS and Triggers of Recurrence
Using univariate Cox regression, no factors were identified as predictive for TTS recurrence (Table 3).
Table 3.
Trigger Factors of Recurrence Episode of 30 TTS Cases
| Case No. | No. of Recurrences | Physical Stressor | Emotional Stressor |
|---|---|---|---|
| 1 | 1 | − | − |
| 2 | 1 | − | + |
| 3 | 1 | Not documented | Not documented |
| 4 | 1 | − | − |
| 5 | 1 | + | − |
| 6 | 1 | − | + |
| 7 | 1 | − | + |
| 8 | 1 | − | + |
| 9 | 1 | − | − |
| 10 | 1 | − | + |
| 11 | 2 | − | − |
| 12 | 1 | − | + |
| 13 | 1 | + | − |
| 14 | 1 | − | − |
| 15 | 1 | + | − |
| 16 | 1 | − | + |
| 17 | 1 | + | − |
| 18 | 2 | + | + |
| 19 | 1 | + | − |
| 20 | 2 | + | − |
| 21 | 1 | + | − |
| 22 | 1 | Not documented | Not documented |
| 23 | 1 | + | − |
| 24 | 1 | Not documented | Not documented |
| 25 | 1 | Not documented | Not documented |
| 26 | 1 | − | − |
| 27 | 1 | − | + |
| 28 | 1 | − | + |
| 29 | 1 | − | + |
| 30 | 1 | − | − |
+ Indicates yes; −, no; TTS, Takotsubo syndrome.
In‐Hospital Events of the Recurrences of Patients With TTS
Different in‐hospital events, including thromboembolic events (2.8% versus 3.3%), stroke (1.3% versus 3.3%), cardiogenic shock (8.2% versus 0%), and the use of cardiac electronic device implantation (1.3% versus 0%), were evaluated (Table 4. No significant difference was documented between both groups. Although pulmonary edema was more often documented in the recurrence group than in the nonrecurrence group (13.3% versus 4.9%; P=0.04) at the index event, the in‐hospital mortality and the duration of hospital stay did not differ between both groups. Of 30 patients, 2 (6%) developed an in‐hospital TTS recurrence.
Table 4.
Predictors of Recurrence in TTS
| Variable | Univariate | |
|---|---|---|
| Hazard Ratio (95% CI) | P Value | |
| Diabetes mellitus | 0.52 (0.15–1.73) | 0.289 |
| Age, y | 0.99 (0.96–1.02) | 0.700 |
| Men | 2.44 (0.93–6.38) | 0.069 |
| Current smoking | 1.51 (0.71–3.19) | 0.276 |
| Hypertension | 2.37 (0.82–6.79) | 0.109 |
| Malignancy | 0.83 (0.25–2.74) | 0.760 |
| Physical trigger | 0.72 (0.33–1.60) | 0.431 |
| Emotional trigger | 1.20 (0.57–2.50) | 0.622 |
| Apical ballooning | 2.10 (0.73–6.05) | 0.165 |
| Initial LVEF, % | 0.98 (0.95–1.02) | 0.467 |
| Cardiogenic shock | 0.55 (0.07–4.09) | 0.564 |
LVEF indicates left ventricular ejection fraction; TTS, Takotsubo syndrome.
Follow‐Up Data Treatment and Clinical Outcome
The earliest time of recurrence was 8 days, and the latest time of recurrence was 2555 days. The Figure presents the recurrence‐free survival of patients with TTS. Except for 2 patients with 2 recurrences, only 1 recurrence event was documented in all other patients.
Figure 1.
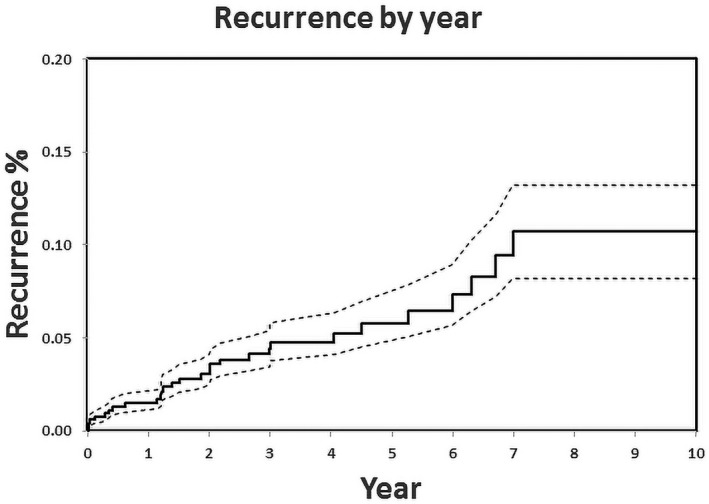
Recurrence‐free survival presents that most recurrences are common the first years after a Takotsubo syndrome event.
Information about drugs at admission and discharge was documented in 22 patients experiencing a recurrence. At admission, these drugs included a β blocker (54%, n=12), an angiotensin‐converting enzyme (ACE) inhibitor or AT (angiotensin‐converting‐enzyme)‐II antagonist (36.6%, n=11), and a combination of a β blocker and an ACE inhibitor or AT‐II antagonist (20%, n=6); and at discharge, these drugs included a β blocker (50%, n=15), an ACE inhibitor or AT‐II antagonist (54%, n=12), and a combination of a β blocker and an ACE inhibitor or AT‐II antagonist (33.3%, n=10).
Discussion
The present European multicenter TTS registry is one of the largest TTS cohorts reported yet. The main results of this study focusing on TTS recurrences are as follows: (1) the recurrence rate of TTS is 4%, with a predominance of a single recurrence event; (2) a variable TTS pattern at recurrence is common in up to 20% of recurrence cases; and (3) most clinical baseline characteristics and in‐hospital complications are comparable between the recurrence and nonrecurrence group.
Incidence of TTS Recurrence
In the present large multicenter study, we describe a recurrence rate of 4.0% during a median follow‐up of 830 days (interquartile range, 118–1701 days). The recurrence rate of TTS has been estimated to be between 1% and 11.4% in single‐center studies and meta‐analyses.11, 15, 16, 17, 19, 20, 21, 22 Although, previous studies have commented on the recurrence rate of TTS, these studies have had a single‐center character with a low number of patients and variable information. Our study investigates in depth the characteristics of patients with TTS experiencing recurrence. Overall, it shows that most baseline characteristics, except arterial hypertension, and in‐hospital events might be similar in the recurrence and nonrecurrence groups of patients with TTS. The mechanism of recurrence in TTS remains unclear. A genetic predisposition is still debated.23
Interestingly, our data, for the first time, demonstrate that in up to 20% of recurrence cases, a variable TTS pattern is presented. In addition, 46% of patients have had a new stress trigger at TTS recurrence. This observation has been reported elsewhere in small case series of TTS.19 In our study, 3 patients with TTS (10%) showed a right ventricular involvement at the recurrence event and 3 patients (10%) with the apical form at initial TTS presented a midventricular TTS form at the recurrence event. This could not be explained by the proposed theory of TTS association with the gradient of β receptors. Although myocardial responsiveness to adrenergic stimulation is increased in the apical region, norepinephrine content is lower in the apex than in the base.24 Another proposed hypothesis is that a previous episode of TTS form may protect this region of TTS involved in the TTS recurrence, with a higher vulnerability of other regions. However, we demonstrate, consistent with other reports, that there are recurrent cases of TTS with the same ballooning pattern, similar to the index event.12
Drug Therapy and Recurrence
Another interesting data point is that 2 patients (0.26%) experienced 2 recurrence episodes, and the highest number of recurrences was observed at an early time (up to 5 years) after the initial TTS event. It could be speculated that the myocardium remains vulnerable at this first stage after the first TTS event. Another possible explanation could be that the prescription of drugs, including β blockers, could be abandoned by patients and physicians after the first TTS event. In our study, >50% of patients were admitted with a β blocker, an ACE inhibitor, or an AT‐II antagonist. Although TTS is associated with hyperadrenergic stimulation, the ACE inhibitor or AT‐II antagonist was more able to reduce the recurrence rate than β blockers15, 25, 26, 27 in nonrandomized trials. Moreover, a combined treatment might be more effective than stand‐alone treatment.27 A combination of a β blocker and ACE inhibitor or AT‐II antagonist was documented in 28% of recurrence cases. This might increase the speculation that a combined treatment is more effective. A possible explanation is that a reduction in sympathetic activity through interaction with the renin‐angiotensin system or suppression inflammatory reactions on the myocardium is more effective on the combined treatment than on stand‐alone treatment.
Finally, because our data are presenting that >50% of patients with TTS at the recurrence event are admitted with a β blocker, an ACE inhibitor or AT‐II antagonist, or a combination of a β blocker and an ACE inhibitor or AT‐II antagonist, this might raise the question of what is the optimal treatment strategy to avoid recurrences in TTS. This issue should be evaluated in future well‐designed prospective randomized trials.
Limitations
Despite the multicenter character of the current study and high number of patients, the analysis has some limitations. First, it is a registry‐based design with differences on the recorded parameters between centers. Some data are missing, such as the compliance of patients regarding drug treatment after the index event. In addition, the duration of medical treatment could not be evaluated because of the small number of recurrences. However, the current report is the largest report of patients with TTS recurrence. Mortality analysis is not meaningful because of the low number of observations.
Conclusions
The recurrence rate of TTS is 4% in this multicenter registry. Up to 2 recurrences could be documented in patients with TTS and variable patterns. A variable TTS pattern at recurrence is documented in up to 20% of recurrence cases. In the present study, no predictors could be identified for recurrence of TTS.
Author Contributions
Akin and Eitel designed the study. Stiermaier, Santoro, Novo, Francesco Romeo, Giannini, El‐Battrawy, Brunetti, and Eitel contributed to the design of the study. All authors collected the data. Akin and Eitel analyzed the data and wrote the manuscript. All authors discussed the results and implications and commented on the manuscript at all stages. Akin and Eitel are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures
None.
(J Am Heart Assoc. 2019;8:e010753 DOI: 10.1161/JAHA.118.010753.)
References
- 1. Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, Sheppard MN, Figtree GA, Parodi G, Akashi YJ, Ruschitzka F, Filippatos G, Mebazaa A, Omerovic E. Current state of knowledge on Takotsubo syndrome: a Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2016;18:8–27. [DOI] [PubMed] [Google Scholar]
- 2. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako‐Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417. [DOI] [PubMed] [Google Scholar]
- 3. Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschope C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfister R, Ukena C, Bohm M, Erbel R, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun‐Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T, Airaksinen KE, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Luscher TF. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. [DOI] [PubMed] [Google Scholar]
- 4. El‐Battrawy I, Lang S, Ansari U, Behnes M, Hillenbrand D, Schramm K, Fastner C, Zhou X, Bill V, Hoffmann U, Papavassiliu T, Elmas E, Haghi D, Borggrefe M, Akin I. Impact of concomitant atrial fibrillation on the prognosis of takotsubo cardiomyopathy. Europace. 2016;19:1288–1292. [DOI] [PubMed] [Google Scholar]
- 5. El‐Battrawy I, Lang S, Ansari U, Tulumen E, Schramm K, Fastner C, Zhou X, Hoffmann U, Borggrefe M, Akin I. Prevalence of malignant arrhythmia and sudden cardiac death in Takotsubo syndrome and its management. Europace. 2017;20:843–850. [DOI] [PubMed] [Google Scholar]
- 6. Stiermaier T, Eitel C, Denef S, Desch S, Schuler G, Thiele H, Eitel I. Prevalence and clinical significance of life‐threatening arrhythmias in takotsubo cardiomyopathy. J Am Coll Cardiol. 2015;65:2148–2150. [DOI] [PubMed] [Google Scholar]
- 7. Stiermaier T, Eitel C, Desch S, Fuernau G, Schuler G, Thiele H, Eitel I. Incidence, determinants and prognostic relevance of cardiogenic shock in patients with takotsubo cardiomyopathy. Eur Heart J Acute Cardiovasc Care. 2015;5:489–496. [DOI] [PubMed] [Google Scholar]
- 8. Santoro F, Stiermaier T, Tarantino N, De Gennaro L, Moeller C, Guastafierro F, Marchetti MF, Montisci R, Carapelle E, Graf T, Caldarola P, Thiele H, Di Biase M, Brunetti ND, Eitel I. Left ventricular thrombi in Takotsubo syndrome: incidence, predictors, and management: results from the GEIST (German Italian Stress Cardiomyopathy) Registry. J Am Heart Assoc. 2017;6:e006990 DOI: 10.1161/JAHA.117.006990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. El‐Battrawy I, Borggrefe M, Akin I. Takotsubo syndrome and embolic events. Heart Fail Clin. 2016;12:543–550. [DOI] [PubMed] [Google Scholar]
- 10. Becher T, El‐Battrawy I, Baumann S, Fastner C, Behnes M, Lossnitzer D, Elmas E, Hoffmann U, Papavassiliu T, Kuschyk J, Dosch C, Roger S, Hillenbrand D, Schramm K, Borggrefe M, Akin I. Characteristics and long‐term outcome of right ventricular involvement in takotsubo cardiomyopathy. Int J Cardiol. 2016;220:371–375. [DOI] [PubMed] [Google Scholar]
- 11. Elesber AA, Prasad A, Lennon RJ, Wright RS, Lerman A, Rihal CS. Four‐year recurrence rate and prognosis of the apical ballooning syndrome. J Am Coll Cardiol. 2007;50:448–452. [DOI] [PubMed] [Google Scholar]
- 12. Eitel I, von Knobelsdorff‐Brenkenhoff F, Bernhardt P, Carbone I, Muellerleile K, Aldrovandi A, Francone M, Desch S, Gutberlet M, Strohm O, Schuler G, Schulz‐Menger J, Thiele H, Friedrich MG. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306:277–286. [DOI] [PubMed] [Google Scholar]
- 13. Kato K, Sakai Y, Ishibashi I, Kobayashi Y. Transient focal left ventricular ballooning: a new variant of takotsubo cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2015;16:1406. [DOI] [PubMed] [Google Scholar]
- 14. Stiermaier T, Thiele H, Eitel I. Long‐term excess mortality in Takotsubo syndrome: is it justified to charge takotsubo for the excess long‐term mortality? Reply. Eur J Heart Fail. 2016;18:879. [DOI] [PubMed] [Google Scholar]
- 15. Singh K, Carson K, Usmani Z, Sawhney G, Shah R, Horowitz J. Systematic review and meta‐analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int J Cardiol. 2014;174:696–701. [DOI] [PubMed] [Google Scholar]
- 16. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–1529. [DOI] [PubMed] [Google Scholar]
- 17. El‐Battrawy I, Ansari U, Behnes M, Hillenbrand D, Schramm K, Haghi D, Hoffmann U, Papavassiliu T, Elmas E, Fastner C, Becher T, Baumann S, Dosch C, Heggemann F, Kuschyk J, Borggrefe M, Akin I. Clinical and echocardiographic analysis of patients suffering from recurrent takotsubo cardiomyopathy. J Geriatr Cardiol. 2016;13:888–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee PH, Song JK, Sun BJ, Choi HO, Seo JS, Na JO, Kim DH, Song JM, Kang DH, Kim JJ, Park SW. Outcomes of patients with stress‐induced cardiomyopathy diagnosed by echocardiography in a tertiary referral hospital. J Am Soc Echocardiogr. 2010;23:766–771. [DOI] [PubMed] [Google Scholar]
- 19. Singh K, Parsaik A, Singh B. Recurrent takotsubo cardiomyopathy: variable pattern of ventricular involvement. Herz. 2014;39:963–967. [DOI] [PubMed] [Google Scholar]
- 20. Parodi G, Bellandi B, Del Pace S, Barchielli A, Zampini L, Velluzzi S, Carrabba N, Gensini GF, Antoniucci D; Tuscany Registry of Tako‐Tsubo Cardiomyopathy . Natural history of tako‐tsubo cardiomyopathy. Chest. 2011;139:887–892. [DOI] [PubMed] [Google Scholar]
- 21. Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nakama Y, Maruhashi T, Kagawa E, Dai K, Matsushita J, Aokage T, Ikenaga H. Assessment of medications in patients with tako‐tsubo cardiomyopathy. Int J Cardiol. 2009;134:e120–e123. [DOI] [PubMed] [Google Scholar]
- 22. Looi JL, Wong CW, Khan A, Webster M, Kerr AJ. Clinical characteristics and outcome of apical ballooning syndrome in Auckland, New Zealand. Heart Lung Circ. 2012;21:143–149. [DOI] [PubMed] [Google Scholar]
- 23. Eitel I, Moeller C, Munz M, Stiermaier T, Meitinger T, Thiele H, Erdmann J. Genome‐wide association study in Takotsubo syndrome—preliminary results and future directions. Int J Cardiol. 2017;236:335–339. [DOI] [PubMed] [Google Scholar]
- 24. Pierpont GL, DeMaster EG, Cohn JN. Regional differences in adrenergic function within the left ventricle. Am J Physiol. 1984;246:H824–H829. [DOI] [PubMed] [Google Scholar]
- 25. Santoro F, Ieva R, Musaico F, Ferraretti A, Triggiani G, Tarantino N, Di Biase M, Brunetti ND. Lack of efficacy of drug therapy in preventing takotsubo cardiomyopathy recurrence: a meta‐analysis. Clin Cardiol. 2014;37:434–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sharkey SW, Windenburg DC, Lesser JR, Maron MS, Hauser RG, Lesser JN, Haas TS, Hodges JS, Maron BJ. Natural history and expansive clinical profile of stress (tako‐tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341. [DOI] [PubMed] [Google Scholar]
- 27. Brunetti ND, Santoro F, De Gennaro L, Correale M, Gaglione A, Di Biase M. Drug treatment rates with beta‐blockers and ACE‐inhibitors/angiotensin receptor blockers and recurrences in takotsubo cardiomyopathy: a meta‐regression analysis. Int J Cardiol. 2016;214:340–342. [DOI] [PubMed] [Google Scholar]


