Abstract
Objectives:
Therapeutic and procedural aspects have been primarily focused on the bone graft treatments with least priority to patients’ perception and preferences. Therefore, the aim of this study was to assess the patient’s choices about various bone grafts used in the bone replacement dental treatments.
Methods:
A self-structured, an anonymous questionnaire with eight items was administered to 100 patients. The questionnaire recorded the responses of selected patients regarding their acceptance and refusal to each type of bone grafts; intraoral and extraoral autograft, allograft, xenograft, and alloplast. The patients’ responses were compared with age, gender, and educational level. The descriptive statistical analysis was performed for the collected data, and with P < 0.05 was considered statistically significant.
Results:
The overall acceptance ratio for intraoral autografts, extraoral autografts, allografts, xenografts, and alloplasts was 89%, 72%, 46%, 33%, and 87%, respectively. The xenograft (67%) had the highest rate of refusal followed by allografts (54%), extraoral autogenous grafts (28%), alloplast (13%), and intraoral autograft (11%) being the least refused bone graft. Age had no statistically significant influence on the acceptance rate to different types of bone grafts, whereas the gender and educational levels were associated with higher acceptance rates.
Conclusions:
The xenograft (67%) had the highest rate of refusal, followed by allografts (54%), extraoral autogenous grafts (28%), alloplast (13%), and intraoral autograft (11%) being the least refused bone graft among the surveyed participants. Moreover, age had no statistically significant influence on the acceptance and refusal to different types of bone grafts, whereas the gender and education level was associated with the acceptance and rejection rates.
Keywords: Bone graft, bone loss, dentistry, periodontitis
Introduction
The clinical usefulness of bone grafting was established even before the grafting of other organs and tissues. Over 2 million bone grafting procedures were performed annually worldwide which is the second most frequent tissue transplantation after blood transfusion.[1] Bone grafting procedures are performed in dental practice to restore the bone to its previous form that has been altered due to periodontitis, tooth loss, or systemic diseases and conditions.
A bone graft can be defined as an implanted material that promotes healing alone or in combination with other materials.[2] The materials used in bone grafting can be grouped into several major categories that include autologous grafts, allografts, and xenografts.[3] Alloplasts that are synthetic and biologically based, tissue engineered materials, and combination of these substitutes are other options.[4] Autogenous grafts are harvested from an anatomic site within the same individual whereas allografts are harvested from one individual and transplanted to a genetically different individual of same species.[5] Xenografts are made of naturally derived deproteinized cancellous bone from another species such as bovine or porcine bone.[6] Alloplasts are synthetic substitutes functioning as defect fillers without adverse tissue reaction or immunogenic response.
The selection of an ideal bone graft relies on several factors such as tissue viability, defect site, graft size and shape, cost, ethical issues, and biological and biomechanical characteristics.[7] However, the patient’s choices and perceptions are least considered while selecting a bone graft. Patients’ participation and expectations have an impact on the utilization of dental services. Successful dental treatment does not depend solely on the provision of adequate dental care; it also depends on the patient’s compliance and participation in decision-making. Due to shortcomings of patient’s participation in decision-making, patient’s expectation of their dental procedures including placement of bone grafts can be unrealistically high which in turn may lead to patient’s dissatisfaction. Patients’ beliefs, attitudes, customs, knowledge, social environment, and choices determine and limit the health behaviors.[8] Beliefs and preferences potentially conflict with the treatment outcomes and possess the risk of non-adherence.
Identifying the patients’ preferences and barriers to seek the treatment increases their compliance, acceptance, and utilization of bone graft treatment modalities. Obtaining information through patients’ survey has proven to be a successful way of strategic evaluation and improving the quality of treatment.[9] Majority of the studies, however, have been focused on the therapeutic and procedural aspect of bone graft therapy; thus, there is a scarcity of evidence regarding the patients’ preferences and perception about bone grafts. Therefore, the aims of this study were to assess the patient’s choices about various bone grafts used in the bone replacement dental treatments and to determine the effects of educational level, age, and gender on the acceptance and refusal to different types of bone grafts.
Methods
The questionnaire survey was cross-sectional in design and conducted between October 2017 and May 2018. The study protocol was in accordance with the Declaration of Helsinki and approved by the scientific ethics committee of Qassim University. Patients satisfying the eligibility criteria were randomly selected at Dental Clinics of College of Dentistry, Qassim University. The patients were designated with the numerical digit 1–10 and randomly two patients were chosen each day. The inclusion criteria for study participants were:
Patients age of ≥18 years
Without any history of drug or alcohol abuse
No previous history of treatments with bone grafts.
The study objectives and protocols were explained to the patients, written and informed consent was obtained. An anonymous self-structured questionnaire was administered to 100 patients also a paper that is explained that the basic knowledge of bone grafting (indications and sources of bone graft materials) was attached to the questionnaire. The sample size at a 95% confidence interval was calculated using Cochran’s formula. The questionnaire consisted of close-ended questions that collect the information on predisposing factors (sex and age) and enabling factors (educational level). The questionnaire recorded the responses of selected patients regarding their acceptance and rejection to each type of bone grafts; intraoral and extraoral autograft, allograft, xenograft, and alloplast. The patients’ responses were compared with age, gender, and educational level. Based on age, the patients were categorized into teenagers (18–25 years), young adults (26–40 years), and older adults (>40 years). Patients were further grouped into lower education and higher education for the comparison of responses.
The standardization and validity of the questionnaire were verified before the administration. A pilot study comprising 15 patients was conducted to recognize the variability. Depending on the variation in responses to each question, their choices were revised and standardized. The consistency, comprehension, and clarity were determined for the content validity by subject experts of the college.
Statistical analysis
The descriptive statistical analysis was performed for the collected data using a statistical package for the social sciences software (version 21: SPSS, Chicago, IL, USA). The frequencies and percentages for all study variables were estimated. Chi-square test was used to determine the relationship of variables with the choices given for different types of grafts. The test results with P < 0.05 were considered statistically significant.
Results
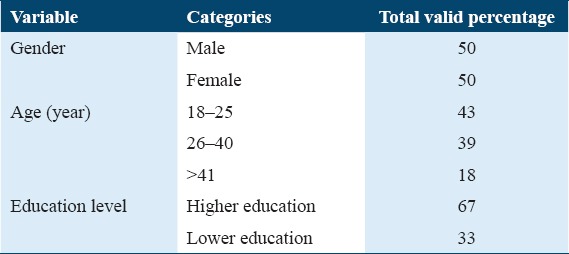
A total of 100 subjects participated in the study. Of these respondents, 50% (n = 50) were males and 50% (n = 50) were females. The sociodemographic characteristics of study respondents are presented in Table 1. The overall acceptance ratio for intraoral autografts, extraoral autografts, allografts, xenografts, and alloplasts was 89%, 72%, 46%, 33%, and 87%, respectively. The xenograft (67%) had the highest rate of refusal, followed by allografts (54%), extraoral autogenous grafts (28%), alloplast (13%), and intraoral autograft (11%) being the least refused bone graft.
Table 1.
Demographic characteristics of the study participants (n=100)
The frequencies and percentages of acceptance and rejection responses to the different types of bone grafts are shown in Table 2. The comparison was done among various sociodemographic variables such as age, gender, and education level for their acceptance and rejection to different types of bone grafts, which are summarized in Table 3.
Table 2.
Frequency and percentage of acceptance/rejection response to the different types of grafts (n=100)
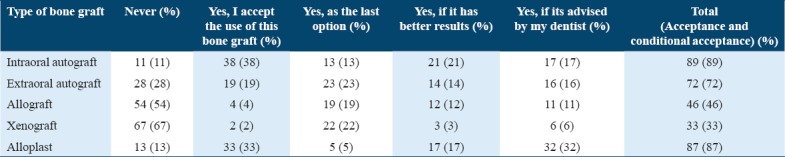
Table 3.
Comparison of acceptance and rejection ratio among age groups, gender, and educational levels
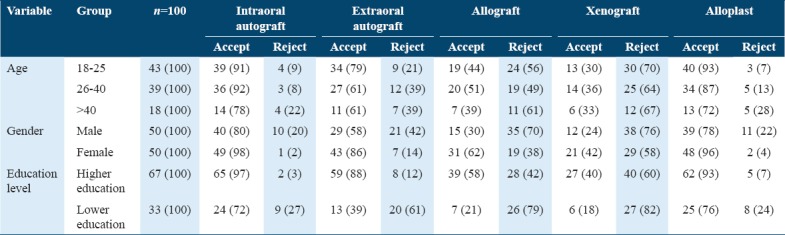
Age had no statistically significant influence on the acceptance and refusal to different types of bone grafts, whereas the gender was associated with the acceptance and rejection rates. Women had significantly better acceptance of the placement of bone grafts than men at P < 0.001. The statistically significant relationships were observed with education level. 67 patients with higher education had higher acceptance of the bone grafts than the 33 patients with lower education.
Discussion
One of the biggest challenges remaining in dentistry is to regenerate the alveolar bone destroyed by periodontitis and other dental conditions.[10] Periodontitis is a pathogen-induced chronic inflammatory destruction of tooth-supporting structures.[11] Although many attempts have been made to regenerate alveolar bone support and attachment apparatus, predictable success has proved elusive.[12] Bone grafts are the only type for which ample histological evidence is available for reconstruction.[12] Dental bone grafts are safe for human use if proper exclusionary technique and processing are employed.[13] Evaluating the patient’s outcome represents is also a major challenge for the health-care provider.[8] Patients’ participation in decision-making can be seen as an offshoot of respect for patient autonomy.[14]
While acknowledging the importance of patients’ participation and choices in the success of bone graft therapy, the present study assessed the patient’s choices about various bone grafts used in bone replacement dental treatments. In this cross-sectional questionnaire survey comprising 100 patients, the intraoral autografts (89%) was the most accepted bone graft by patients surveyed as treatment option which was followed by alloplasts (87%) and extraoral autografts (72%). Autografts are regarded as gold standard in treating bone defects and the benchmark in evaluating other bone grafts and substitutes.[15,16] The autogenous grafts possess the osteoconductive, osteoinductive, and osteogenic properties and can integrate into the host tissue most rapidly and completely,[17] whereas alloplasts are synthetic bone substitutes that are readily available and also eliminate the need for a patient donor site.[18] Alloplasts have the ability to be resorbed, undergo replacement process during which they are partially or completely resorbed by macrophages/osteoblasts before the native bone is deposited by osteoblasts.[19,20]
The results of this study also showed the least patient’s preference for xenografts (33%) followed by allograft (46%). Refusal of xenografts is often influenced by religious reasons and religious belief and dietary restrictions affected by graft selection.[21] Xenografts carry the risk of transmission of zoonotic diseases and rejection of graft is more likely and aggressive.[22,23] Allografts render activation of major histocompatibility complex (MHC) antigens that, in turn, leads to a high failure rate in comparison to autografts.[24] However, some rate of acceptance was seen for xenografts as the last option (22%) when there was no alternative is available. The use of animal-derived bone grafts may be avoidable in some situation and has the potential to cause ethical dilemmas that could influence consenting practices.[25] The findings of our study were in accordance with the similar study conducted by Fernández et al. that demonstrated the high refusal rates for allografts and xenografts by surveyed patients with autogenous and alloplasts being the most accepted bone grafts.[26] Another study by Zeynep and Metin showed the similar results that autogenous bone grafts were the most preferred followed by alloplasts and xenografts and allografts were the least preferred bone graft materials.[21]
Influence of predisposing factors such as sex and age and enabling factors such as educational level on patients preferences were also studied in this survey. Andersen behavioral model explains that the service utilization is determined by predisposing, enabling, and need factors and affected by individuals’ demographic, sociostructural, and economic factors.[13] The present study demonstrated the influence of gender and educational level on patient preferences. Women had lower refusal rates than men. Similarly, patients with higher educational level had better acceptance of different types of bone grafts than the patients with lower or secondary educational level. However, the age of the patient had no influence on the acceptance/refusal rates. Literature reveals the gender differences in the utilization of dental services. Females visited dentists and used dental services more frequently than males.[27] However, these findings of this study were in contrary to the findings of a study by Fernández et al. that showed no difference in the sociodemographic variables in terms of acceptance/refusal rates of different bone grafts.[26] Although the present study highlights the significance of patients’ perception and choices in decision-making and successful outcomes, further qualitative studies are warranted to understand the subject in depth.
Conclusions and Recommendations
The xenograft (67%) had the highest rate of refusal followed by allografts (54%), extraoral autogenous grafts (28%), alloplast (13%), and intraoral autograft (11%) being the least refused bone graft among the surveyed participants. Moreover, age had no statistically significant influence on the acceptance and refusal to different types of bone grafts, whereas the gender and education level was associated with the acceptance and rejection rates. Women had significantly better acceptance of the placement of bone grafts than men. The statistically significant relationships were observed with education level. 67 patients with higher education had higher acceptance of the bone grafts than the 33 patients with lower education. Based on the findings of this study, the author suggests the following recommendations:
Both dental care providers and patients should be well informed of various bone graft products especially those containing animal derivatives.
Patients’ choices should be prioritized in decision making for better compliance and long-term success.
Government policies should be implemented in dental practice to defend patients’ individual choice.
Conflicts of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Campana V, Milano G, Pagano E, Barba M, Cicione C, Salonna G, et al. Bone substitutes in orthopaedic surgery:From basic science to clinical practice. J Mater Sci Mater Med. 2014;25:2445–61. doi: 10.1007/s10856-014-5240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elsalanty ME, Genecov DG. Bone grafts in craniofacial surgery. Craniomaxillofac Trauma Reconstr. 2009;2:125–34. doi: 10.1055/s-0029-1215875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oryan A, Alidadi S, Moshiri A, Maffulli N. Bone regenerative medicine:Classic options, novel strategies, and future directions. J Orthop Surg Res. 2014;9:18. doi: 10.1186/1749-799X-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dimitriou R, Jones E, McGonagle D, Giannoudis PV. Bone regeneration:Current concepts and future directions. BMC Med. 2011;9:66. doi: 10.1186/1741-7015-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts TT, Rosenbaum AJ. Bone grafts, bone substitutes and orthobiologics:The bridge between basic science and clinical advancements in fracture healing. Organogenesis. 2012;8:114–24. doi: 10.4161/org.23306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sukumar S, Drízhal I. Bone grafts in periodontal therapy. Acta Medica. 2008;51:203–7. [PubMed] [Google Scholar]
- 7.Brydone AS, Meek D, Maclaine S. Bone grafting, orthopaedic biomaterials, and the clinical need for bone engineering. Proc Inst Mech Eng H. 2010;224:1329–43. doi: 10.1243/09544119JEIM770. [DOI] [PubMed] [Google Scholar]
- 8.Luzzi L, Spencer AJ. Factors influencing the use of public dental services:An application of the theory of planned behaviour. MC Health Serv Res. 2008;8:93. doi: 10.1186/1472-6963-8-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Hussyeen AJ. Factors affecting utilization of dental health services and satisfaction among adolescent females in Riyadh city. Saudi Dent J. 2010;22:19–25. doi: 10.1016/j.sdentj.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brunsvold MA, Mellonig JT. Bone grafts and periodontal regeneration. Periodontol 2000. 1993;1:80–91. [PubMed] [Google Scholar]
- 11.Jayanthi MD, Faizuddin M, Ahamadi MH. Association of interferon lambda-1 with herpes simplex viruses-1 and 2, epstein-barr virus, and human cytomegalovirus in chronic periodontitis. J Investig Clin Dent. 2017;8:e12200. doi: 10.1111/jicd.12200. [DOI] [PubMed] [Google Scholar]
- 12.Yukna RA. Synthetic bone grafts in periodontics. Periodontol 2000. 1993;1:92–9. [PubMed] [Google Scholar]
- 13.Kim HK, Lee M. Factors associated with health services utilization between the years 2010 and 2012 in Korea:Using Andersen's Behavioral model. Osong Public Health Res Perspect. 2016;7:18–25. doi: 10.1016/j.phrp.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glasdam S, Oeye C, Thrysoee L. Patients'participation in decision-making in the medical field 'projectification'of patients in a neoliberal framed healthcare system. Nurs Philos. 2015;16:226–38. doi: 10.1111/nup.12092. [DOI] [PubMed] [Google Scholar]
- 15.Wang W, Yeung KW. Bone grafts and biomaterials substitutes for bone defect repair:A review. Bioact Mater. 2017;2:224–47. doi: 10.1016/j.bioactmat.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Athanasiou VT, Papachristou DJ, Panagopoulos A, Saridis A, Scopa CD, Megas P. Histological comparison of autograft, allograft-DBM, xenograft, and synthetic grafts in a trabecular bone defect:An experimental study in rabbits. Med Sci Monit. 2010;16:BR24–31. [PubMed] [Google Scholar]
- 17.Goldberg VM, Akhavan S. Biology of bone grafts. In: Lieberman JR, Friedlaender GE, editors. Bone Regeneration and Repair. New York: Springer; 2005. pp. 57–65. [Google Scholar]
- 18.Mah J, Hung J, Wang J, Salih E. The efficacy of various alloplastic bone grafts on the healing of rat calvarial defects. Eur J Orthod. 2004;26:475–82. doi: 10.1093/ejo/26.5.475. [DOI] [PubMed] [Google Scholar]
- 19.Sheikh Z, Abdallah MN, Hanafi AA, Misbahuddin S, Rashid H, Glogauer M. Mechanisms of in vivo degradation and resorption of calcium phosphate based biomaterials. Materials. 2015;8:7913–25. doi: 10.3390/ma8115430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheikh Z, Brooks PJ, Barzilay O, Fine N, Glogauer M. Macrophages, foreign body giant cells and their response to implantable biomaterials. Materials. 2015:5671–701. doi: 10.3390/ma8095269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeynep G, Metin G. Effect of religious belief on selecting of graft materials used in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2017;75:2347–53. doi: 10.1016/j.joms.2017.07.160. [DOI] [PubMed] [Google Scholar]
- 22.Moshiri A, Oryan A. Role of tissue engineering in tendon reconstructive surgery and regenerative medicine:Current concepts, approaches and concerns. Hard Tissue. 2012;1:11. [Google Scholar]
- 23.Oryan A, Alidadi S, Moshiri A. Current concerns regarding healing of bone defects. Hard Tissue. 2013;2:13. [Google Scholar]
- 24.Stevenson S, Horowitz M. The response to bone allografts. J Bone Jt Surg. 1992;74:939–50. [PubMed] [Google Scholar]
- 25.Easterbrook C, Maddern G. Porcine and bovine surgical products. Jewish, Muslim, and Hindu perspectives. Arch Surg. 2008;143:366–70. doi: 10.1001/archsurg.143.4.366. [DOI] [PubMed] [Google Scholar]
- 26.Fernández RF, Bucchi C, Navarro P, Beltrán V, Borie E. Bone grafts utilized in dentistry:An analysis of patients'p. BMC Med Ethics. 2015;16:71. doi: 10.1186/s12910-015-0044-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farsi JM. Dental visit patterns and periodontal treatment needs among Saudi students. EMHJ. 2010;16:801–6. [PubMed] [Google Scholar]


