Abstract
Purpose
Loss of the T2 vertebral artery flow void can be an ominous sign in patients with trauma. However, the significance of an absent vertebral artery flow void is less clear when discovered incidentally in patients without trauma or acute neurological symptoms. The purpose of this study was to review retrospectively the results of additional imaging and clinical evaluation in atraumatic patients without acute neurological symptoms found to have an incidentally discovered absent vertebral artery flow void on magnetic resonance imaging.
Materials and methods
An imaging database was reviewed for absent vertebral artery flow voids in atraumatic cervical spine magnetic resonance images. Imaging and long-term clinical follow-up were recorded.
Results
Fifty-four patients were included in the study. All patients had clinical follow-up and 22 patients (40% of cases) had vascular imaging follow-up. Nine patients had a hypoplastic but patent vertebral artery on follow-up vascular imaging, and no further action was taken. Ten patients had evidence of stenosis or occlusion of the vertebral artery on follow-up imaging, none with acute neurological symptoms or new symptoms/subsequent change in management during follow-up. Three additional patients had vertebral artery dissections on follow-up imaging, but all of them had acute neurological symptoms at the time of imaging and acute infarcts on current or subsequent magnetic resonance imaging. The other 32 patients had clinical follow-up and remained asymptomatic throughout the study period, without change in management.
Conclusion
In the absence of trauma or acute neurological symptoms an absent vertebral artery flow void has a low likelihood of altering patient management.
Keywords: Absent vertebral artery flow void, cervical spine MRI, MRI, vertebral artery dissection, incidental
Introduction
Loss of the T2 vertebral artery flow void on magnetic resonance imaging (MRI) of the cervical spine can be an ominous sign in patients with cervical spine trauma.1,2 Loss of the flow void usually indicates vertebral artery dissection or occlusion in acute trauma, particularly with cervical spine fractures extending to the foramen transversarium or with facet fracture/subluxation.3 The most feared complication is posterior circulation ischemia from vertebral artery occlusion or artery-to-artery embolism, and cerebral ischemia can be seen in up to 77% of patients with vertebral artery dissection.4 Additional confirmatory tests such as computed tomography (CT), MRI or conventional angiography are typically performed prior to instituting antithrombotic therapy. However, the significance of an absent vertebral artery flow void on cervical spine MRI is less clear when incidentally discovered on imaging performed for other reasons. The purpose of this study was retrospectively to review the results of additional imaging and clinical evaluation in atraumatic patients without acute neurological symptoms found to have an absent vertebral artery flow void on cervical spine MRI.
Methods
After institutional board review approval, the imaging database at our urban tertiary care center was interrogated for imaging reports of patients with an absent flow void on axial T2-weighted images of cervical spine MRIs. Patient with a history of trauma and traumatic or pathological cervical spine fractures were excluded. Patient charts were reviewed and additional imaging and long-term clinical follow-up were recorded.
Imaging protocol
All cervical spine MRIs were performed on 1.5 or 3 Tesla systems. Sagittal T1-weighted images (time to repetition (TR) 1900 ms, time to echo (TE) 9.6 ms, time to inversion (TI) 860 ms, number of excitations (NEX) 2, slice thickness 3 mm), axial T2-weighted (TR 3800 ms, TE 81 ms, NEX 2, slice thickness 3 mm) sagittal short tau inversion recovery images (TR 3800 ms, TE 66 ms, TI 170 ms, slice thickness 3 mm) and axial gradient-recalled echo images (TR 37 ms, TE 15 ms, flip angle 20°, slice thickness 1.5 mm) of the cervical spine were obtained in all cases. The imaging field of view extended from the mid-posterior fossa to the T3 vertebral body in sagittal and axial planes.
Follow-up imaging consisted of CT, MRI or conventional angiography. Our computed tomography angiography (CTA) protocol consisted of a helical scan of the neck approximately 20 seconds after the intravenous administration of 50 mL iodinated contrast at 5 mL/second, followed by a 50 mL saline flush. The exact timing of the scan was determined using automated bolus tracking software. Coverage was from the aortic arch to the circle of Willis with kVp 100 and 120 mAs at 0.75 mm slice thickness. Images were then reconstructed at 1.25 mm in the sagittal and coronal planes. Maximum intensity projection images of the brain in the axial, coronal and sagittal plane were also obtained and reviewed.
The neck magnetic resonance angiography (MRA) protocol consisted of two-dimensional time-of-flight images of the vertebral arteries in the axial plane from the aortic arch to the skull base, with TR 31 ms, TE 7.8 ms, NEX 1 and slice thickness 3 mm. Contrast-enhanced MRA was also performed in the coronal plane using postcontrast three-dimensional T1-weighted spoiled GRE imaging, with TR 3.5 ms, TE 1.2 ms, flip angle 25°, NEX 1 and slice thickness 1.2 mm. Maximum intensity projections of the neck vessels were performed in the coronal plane.
Digital subtraction angiography (DSA) of the neck was performed by our neurointerventional service after successful femoral artery cannulation and over-the-wire navigation of a 5 French diagnostic angiography catheter into the aortic arch. Angiographic runs of the neck vessels were performed with hand injections of iodinated contrast following catheter placement in the proximal vertebral artery or automated machine injections in subclavian artery with an inflated blood pressure cuff on the ipsilateral arm. Images were taken in the frontal, lateral and oblique projections, with attention to the vertebral artery in question.
Clinical follow-up
All patients with an abnormal vertebral artery flow void were evaluated by a neurologist or the primary care physician/ordering clinician for further work-up and management of potential vertebral artery dissection or occlusion. Clinical follow-up consisted of a complete history and physical exam, including a complete neurological exam. Results of additional confirmatory imaging were incorporated into the final decision-making process in all cases. Patients were followed in the neurology clinic or by their primary care provider to detect any new signs/symptoms. A minimum of 12 months of clinical follow-up was available for all patients.
Descriptive statistical analysis was performed using spreadsheet data analysis software (Excel 2013; Microsoft, Redmond, WA, USA).
Results
A total of 54 patients were included in the study. One patient with an abnormal vertebral flow void on an outpatient cervical spine MRI was excluded from the analysis. Follow-up CTA showed a vertebral artery dissection, and after further questioning by the neurologist, the patient revealed that he was involved in a motor vehicle collision a few weeks prior to his MRI, for which he did not seek medical attention. Of the 54 patients included in the study, 35 were men. The three most common indications for the cervical spine MRI were neck pain, gait disturbance and radiculopathy, seen in 16, 14 and 12 patients, respectively (76% of cases). All patients had clinical follow-up and 22 patients (40% of cases) had vascular imaging follow-up. MRA was the most common imaging follow-up performed (11 cases or 20%). CTA was performed in seven patients, including two out of three patients initially presenting with acute neurological symptoms. Two patients had ultrasounds of the neck including the vertebral arteries, which were normal. Both CTA and MRA were performed in one patient, and DSA was performed in a patient with acute neurological symptoms and acute posterior fossa infarcts on MRI of the cervical spine.
Nine patients had a hypoplastic but patent vertebral artery on follow-up vascular imaging, and no further action was taken.
Ten patients had evidence of stenosis or occlusion of the vertebral artery on follow-up vascular imaging (see Figure 1). Of these, four had known chronic infarcts. None of the 10 patients had acute neurological symptoms at the time of imaging or during the follow-up period, and no change in medical management was instituted as a result of the imaging findings.
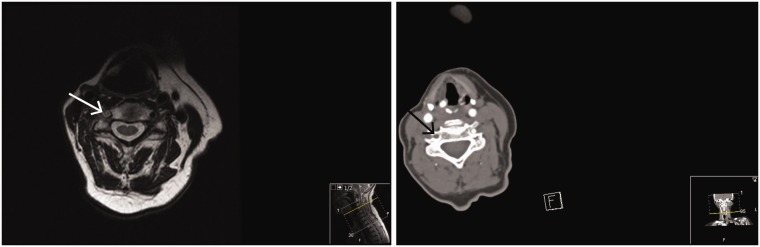
Figure 1.
A 72-year-old woman with occipital headaches and clinical concern for atlanto-occipital degeneration. She had a remote history of right neck dissection and irradiation for squamous cell carcinoma at an outside institution. Magnetic resonance imaging (MRI) of the cervical spine performed to assess for spondylosis showed an abnormal right vertebral flow void (arrow in first image). The patient was asymptomatic with no clinical signs or symptoms of posterior fossa ischemia. Computed tomography angiography of the head and neck performed for further evaluation showed occlusion of the right vertebral artery in the neck (arrow in second image). The intracranial circulation was widely patent. She was started on antiplatelet therapy and no further action was taken.
Three additional patients had left vertebral artery dissection on follow-up imaging, but all of them had acute neurological symptoms at the time of imaging and acute infarcts on current or subsequent MRI.
The remaining 32 patients with an abnormal vertebral flow void on cervical spine MRI had a normal clinical follow-up including a complete neurological exam with attention to the posterior circulation, and remained asymptomatic throughout the study period with no change in management. Follow-up was by a neurologist in approximately 66% of cases and by a primary care physician in 33% of cases.
Discussion
Our results show that the incidental discovery of an abnormal vertebral artery flow void on cervical spine MRI in patients without trauma or acute neurological symptoms usually does not result in any drastic change in management. None of the asymptomatic patients at the time of study had any new neurological event during the 12-month follow-up period.
The major concern with an abnormal vertebral artery flow void is a dissection.5 However, a hypoplastic vertebral artery can also look very similar, as detailed by Provenzale et al.5 In the authors’ experience, one way to distinguish a hypoplastic vertebral artery from a dissection is to compare the size of the ipsilateral foramen transversarium; the ipsilateral foramen is usually small in cases of a hypoplastic vertebral artery. This finding is not always reliable, and additional confirmatory tests may be needed. A long-standing arterial occlusion or a high-grade proximal arterial stenosis with distal slow flow may also present as an abnormal flow void.6
Three patients with acute vertebral artery dissections had acute onset of neurological symptoms that worsened soon after their MRI of the cervical spine. A 44-year-old roofer with known congenital cervical spine stenosis, who experienced sudden onset of numbness and lower extremity weakness, paresis, while looking up. The suspected diagnosis was acute myelopathy, and a cervical spine MRI was ordered. An abnormal flow void was seen, and he was found to have an acute left vertebral artery dissection on follow-up imaging. The second patient with a dissection was a 47-year-old woman with neck pain, who was cracking/twisting her neck for relief. Immediately after cracking her neck, she had a sudden onset of weakness and numbness down her neck and shoulders, which continued to worsen during the day. The third patient was a 43-year-old man with a history of a ‘pinched nerve’ and baseline arm numbness, who experienced worsening numbness and tingling while looking over his shoulder to back out of his garage, which progressed to weakness. He was found to have an abnormal flow void and a vertebral artery dissection on subsequent imaging.
There is significant anxiety among radiologists and clinicians over potentially missing a vertebral artery dissection on routine MRIs of the cervical spine, and the vertebral and carotid artery flow voids are included (appropriately) in any complete checklist of a cervical spine MRI review. This situation is further exacerbated by recent trends in medical malpractice litigation, in which successful lawsuits involving vertebral artery dissections have been filed against chiropractors.7 At least one famous internet social media star has died from an undiagnosed vertebral artery dissection,8 and some law firms specifically offer counsel for injury related to delayed diagnosis of a vertebral artery dissection.9 Despite the heightened societal awareness of vertebral artery dissections and increased vigilance on the part of radiologists for this diagnosis, data on the significance of absent vertebral artery flow voids in atraumatic patients are lacking. Our study attempts to bridge this gap and offer some clarity on the significance of this finding.
This study had several limitations. It was a retrospective study, with all the inherent biases specific to this methodology. Only the abnormal vertebral artery flow voids detected by the interpreting radiologist were included in the study. Any abnormal flow void that was present on a cervical spine MRI but was missed by the interpreting radiologist could not be included in the study, and it is difficult to predict how this could have affected our results. Follow-up was available for at least 12 months in all patients, but it is impossible to ascertain if some patients may have had delayed neurological symptoms beyond the 12-month mark. However, this is still an important result suggesting that the risk of serious neurological deficit and significant alteration in patient management within one year after the discovery of an absent vertebral artery flow void in a patient without a history of trauma or acute neurological symptoms is low.
Conclusion
All abnormal vertebral artery flow voids on cervical MRI should be documented and communicated, to be followed by thorough clinical and neurological evaluation. In the absence of trauma or acute neurological symptoms, however, an abnormal vertebral artery flow void has a low likelihood of changing patient management. The results of this study may have important implications in patient counselling and medicolegal cases.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. No unique patient identifiers were used.
References
- 1.Dreizin D, Letzing M, Sliker CW, et al. Multidetector CT of blunt cervical spine trauma in adults. Radiographics 2014; 34: 1842–1865. [DOI] [PubMed] [Google Scholar]
- 2.Rodallec MH, Marteau V, Gerber S, et al. Craniocervical arterial dissection: spectrum of imaging findings and differential diagnosis. Radiographics 2008; 28: 1711–1728. [DOI] [PubMed] [Google Scholar]
- 3.Willis BK, Greiner F, Orrison WW, et al. The incidence of vertebral artery injury after midcervical spine fracture or subluxation. Neurosurgery 1994; 34: 435–442. [DOI] [PubMed] [Google Scholar]
- 4.Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection. Stroke 2006; 37: 2499–2503. [DOI] [PubMed] [Google Scholar]
- 5.Provenzale JM, Sarikaya B, Hacein-Bey L, et al. Causes of misinterpretation of cross-sectional imaging studies for dissection of the craniocervical arteries. Am J Roentgenol 2011; 196: 45–52. [DOI] [PubMed] [Google Scholar]
- 6.Heinz ER, Yeates AE, Djang WT. Significant extracranial carotid stenosis: detection on routine cerebral MR images. Radiology 1989; 170: 843–848. [DOI] [PubMed] [Google Scholar]
- 7.Brian E. Clare. Attorney at law (advertisement). www.brianclare.com/Results.html (accessed 30 January 2018).
- 8.Pittsburgh Post-Gazette. https://www.post-gazette.com/local/region/2016/10/23/Neck-manipulation-killed-Internet-phenom/stories/201606140162 (accessed 30 January 2018).
- 9.The Beasley Firm LLC. A Failure to Diagnose a Vertebral Artery Dissection (VAD) Can Lead to a Stroke, Permanent Brain Damage, and Usually Disability or Death to a Child, 2011. www.beasleyfirm.com/blog/2011/july/a-failure-to-diagnose-a-vertebral-artery-dissect/ (accessed 30 January 2018).