Abstract
BACKGROUND:
To respond to the growing expectations of the public and to meet the needs of the society, health systems have always tried to improve their performance. This study investigated the changes in the performance and quality of emergency department (ED) after implementation of the health transformation plan (HTP) in Iran.
METHODS:
This was a before–after study that was conducted in Tehran's Lolagar General Hospital in 2016. The data related to the performance indices and patients’ satisfaction indices were collected in the two periods of 6 months before and 6 months after the implementation of the HTP. The data were gathered by a checklist designed by the researchers.
RESULTS:
Among performance indices, the maximum positive change was related to the failure in cardiopulmonary resuscitation, which had a reduction of 18.27%. Discharge against medical advice had a reduction of 1.11%, which is considered to be significant. Among the factors related to patients’ satisfaction, the maximum changes belonged to the out-of-pocket payment, access to medicines, and giving information to the patients, which were 0.87%, 72%, and 61%, respectively.
CONCLUSIONS:
HTP and its supporting packages have led to positive changes in the performance of the ED of the hospital. Therefore, based on the results of this study, the continuation of this plan is recommended.
Keywords: Emergency department, health transformation plan, Iran, performance
Introduction
Today, the views toward the concept of health have changed. These changes can be investigated from various perspectives. Today, our definition of health is different from the past decades. According to the past definitions, health was the absence of diseases. In later definitions, a number of other factors were added to this definition.[1] These changes in the definition of health are continuing. As our knowledge and technology improve, some complementary aspects are being added to the definition of health. This complementary trend can clearly be seen in the latest definition presented by the World Health Organization. According to this definition, health is “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”[2] Furthermore, the factors that affect health have changed. Today, we see a shift from communicable diseases to noncommunicable diseases. This shift is the result of changes in the lifestyle and aging population.[3] Therefore, our knowledge and technology must be updated and accommodated to the new conditions.[4] To be efficient, necessary changes must be made in the health systems according to the current changes and developments. Such changes can clearly be seen in the health system development plans in most countries.[5,6] Simultaneous with developments in other countries, a lot of changes are taking place in the various areas of health system of Iran, such as education, research, and the behaviors of the service providers.
The Ministry of Health and Medical Education (MoHME) of Iran is conducting a plan to reach its objectives by 2025. Health sector evolution plan (HSEP) or health transformation plan (HTP) was designed by MoHME based on the fifth 5-year health development national strategies (2011–2016). HSEP is a stepwise national plan which includes several interventions in the health sector. The aim of this plan is the improvement of the health system of the country. The implementation of the plan started in May 4, 2014.[7,8,9] HSEP has three general objectives: financial support for people, equality in access to health services, and improvement in the quality of services. This plan has seven supporting packages: reduction of expenses, encouraging physicians to stay in poor areas, the presence of specialty physicians in the hospitals affiliated to MoHME, improving the quality of visits in the hospitals, improving the hospital hoteling services, financial support of patients suffering from refractory diseases, and encouraging women not to choose the cesarean section when giving birth. Reducing the out-of-pocket (OOP) payments by the patient, helping those patients who have to pay large amount of money, improving emergency services, and encouraging pregnant women to have normal delivery are the final objectives of the HSEP.[9,10,11] The plan is mainly supported through the following financial sources: increased public annual budget of health sector (around 59% increase in 2015 compared to 2014),[12] resources of the targeted subsidies’ law (10% of total subsidies), and a specific 1% value-added tax for health. The financial resources are estimated to be 70% higher in 2015 (March 21, 2015–March 20, 2016) compared to 2014 (March 21, 2014–March 20, 2015). Based on the approved program, copayments for the inpatient services at the MoHME affiliated hospitals must be limited to 10% for residents of the medium and large cities and 5% for nomadic people and the residents of rural areas, and small towns (with population <20,000).[8] In this plan, supporting packages and the improvement of services of the emergency departments (EDs) are particularly important. In addition to playing a key role in reducing the number of death cases in hospitals and improving the satisfaction of the patients, the hospital EDs are the starting points for patients coming to hospitals.[13,14] The necessity of quick and careful services in the EDs makes this department very special and sensitive.[15] Receiving patients, triage, stabilizing the conditions of the patients, and starting the process of emergency treatment are the main works that are done in the EDs.[16] Similar to the performance of the other sections of the hospital, the performance of the ED is affected by the general policies of the hospital, executive procedures, and operational processes.[17] Because of the importance of transformation plans in the quality of the services and operational processes, the implementation of the HSEP in Iran seems to be necessary. The majority of similar studies in various countries have focused on financial aspects. Results of a study conducted in Turkey showed that the execution of health system transformation plan could reduce the OOP.[18,19] Results of a similar study in Columbia showed that the implementation of the HSEP can improve equality and reduce the expenses for the patients.[20]
Since the ED is one of the most important departments in a hospital and the most sensitive services are provided in this department, and regarding its unique position on quality of the hospital services, the care in this department must be provided with maximum quality to make a good performance. Hence, a goal of the HSEP is improving the performance of the hospital EDs. However, until now, few studies have been conducted to investigate the efficiency of the HSEP in Iran. Therefore, this study was conducted to explore the effect of the HSEP in improving the performance of the ED of Tehran's Lolagar General Hospital. This study was conducted on the basis of indices of performance and patients’ satisfaction.
Methods
This research was conducted in Tehran's Lolagar General Hospital in 2016 using a before-after design. Lolagar hospital is a general hospital with 81 active beds. This hospital includes departments of emergency, general surgery, maternity block, obstetrics and gynecology, pediatrics, intensive care units, and operating rooms. On average, in the past 3 years, 25,602 patients have been admitted in the ED annually. This center is working under the organizational structure of the Iran University of Medical Sciences and operates under the supervision of MoHME.
The data gathered in this study were related to the performance of the ED and patients’ satisfaction. Because the aim of the study was to compare the conditions before and after the implementation of the HTP plan, the data of two periods of time (before and after the implementation of the plan) were gathered and analyzed. The data collection method has been explained in the following section.
Hospital's performance indices
The data of this study were collected in the two periods of 6 months before and 6 months after the implementation of the HSEP. To collect the data, a checklist designed by the researchers was used. This checklist was based on the indices confirmed by the MoHME.
These indices have been notified by the evaluation office of the health centers of the MoHME to evaluate the operation of the EDs of the hospitals. This evaluation is based on the following indices.[11]
The indices were as follows:
Disposition of the patients within 6 h
Patients discharged within 12 h
Failed cardiopulmonary resuscitation (CPR)
Discharge against medical advice
Time of triage.
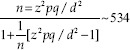
Satisfaction of patients coming into the emergency department
The data of this part were collected by forms filled by patients in the hospital. Statistical population included 4645 filled questionnaires (number of patients coming into the ED from 6 months before the implementation of the HSEP to 6 months after the implementation of the HSEP). The level of confidence was 95%. Among these questionnaires, 354 questionnaires were selected as the sample of the study. Half of these questionnaires (n = 177) belonged to the period before the implementation of the plan and the other half (n = 177) belonged to the period after the implementation of the HSEP. The questionnaires were selected randomly.
The data gathered by the questionnaires included patients’ opinions about ten scales: facilities of the department, waiting time, patient disposition, appearance of the staff, care for patients, giving information to the patients, quality of visits, access to medicine, OOP payments, and the patients’ satisfaction of the services. There was a question for each item. Patients’ opinions were collected on the basis of a five-option Likert scale (excellent, good, medium, bad, and very bad). Cronbach's alpha was computed for each scale using the SPSS-22 software (SPSS Inc., Chicago, IL, USA). The reliability coefficient was 0.91 for the patients’ satisfaction questionnaire.
Data analysis
All data were analyzed using the SPSS 22 (SPSS Inc., Chicago, IL, USA). Data analysis had two parts of descriptive and analytic. In the descriptive analysis, mean and standard deviation for the performance indices of the ED and the data of various aspects of patients’ satisfaction were obtained. In the analytic part, the differences between two periods of time before and after the implementation of the plan were tested with the Student's t-test and independent samples t-test.
Results
The findings of this study included descriptive and analytical parts. In the descriptive part, the values of variables of ED performance and patients’ satisfaction were presented by the three indices of percentage, mean, and standard deviation. Table 1 shows the performance indices of the studied ED in the two periods (before and after the implementation of the HSEP).
Table 1.
Performance indices of the emergency department in the two periods of 6 months before and 6 months after the implementation of the Health Sector Evolution Plan
| Performance indices | 6 months before the implementation of the HSEP | 6 months after the implementation of the HSEP | ||
|---|---|---|---|---|
| Percentage | SD | Percentage | SD | |
| Disposition of patients within 6 h | 94.86 | 6 | 99.55 | 0.17 |
| Patients discharged within 12 h | 99.74 | 0.63 | 100 | 00 |
| Failed CPR | 71 | 9.2 | 52.72 | 14.06 |
| Discharge against medical advice | 11.65 | 0.69 | 10.54 | 1.19 |
| Time of triage, mean±SD | 2.86 (0.41) | 2.20 (0.34) | ||
SD=Standard deviation, HSEP=Health Sector Evolution Plan
In Table 2, the data on patients’ satisfaction scales have been given. Among these scales, “attention to patient” and “appearance of staff” had the highest mean in the 6 months before the implementation of the HSEP. After the implementation of the HSEP, the highest means belonged to “attention to patient” and “OOP payment.”
Table 2.
Patients’ satisfaction indices in the two periods of 6 months before and 6 months after the implementation of the Health Sector Evolution Plan
| Scales | Cronbach's alpha | Mean±SD | |
|---|---|---|---|
| 6 months before the implementation of the HSEP | 6 months after the implementation of the HSEP | ||
| Facilities of the department | 0.83 | 2.83 (0.97) | 3.14 (1.14) |
| Waiting time | 0.81 | 2.58 (1.08) | 2.49 (1.31) |
| Disposition of patients | 0.78 | 2.94 (1.28) | 2.90 (1.32) |
| Appearance of the staff | 0.75 | 2.98 (1.13) | 2.94 (1.11) |
| Attention to patient | 0.87 | 3.25 (1.06) | 3.61 (1.17) |
| Giving information to the patients | 0.79 | 2.61 (1.17) | 3.22 (1.33) |
| Quality of visits | 0.89 | 2.96 (1.27) | 3.24 (1.11) |
| Access to medicines | 0.77 | 2.66 (1.16) | 3.38 (1.16) |
| Out-of-pocket payment | 0.71 | 2.63 (1.03) | 3.50 (1.15) |
| Overall patients satisfaction | 0.81 | 2.90 (1.01) | 3.45 (1.12) |
SD=Standard deviation, HSEP=Health Sector Evolution Plan
The next part of results was obtained by analyzing the data. Table 3 shows the results of statistical test for comparing the performance indices in the two periods of 6 months before and after the implementation of the plan. The maximum and minimum of mean differences belonged to “failed CPR” (18.27) and “patients discharged within 12 h” (0.25). Among the five indices, only the mean difference of “discharge against medical advice” in the two periods was statistically significant (P = 0.030).
Table 3.
The results of statistical test for investigating the mean difference of performance indices of emergency department
| Performance indices | Mean difference | Criterion of the test | Statistical significance |
|---|---|---|---|
| Disposition of patient within 6 h | 4.69 | −1.9 | 0.115 |
| Patients discharged within 12 h | 0.25 | −1 | 0.363 |
| Failed CPR | −18.27 | 2.29 | 0.070 |
| Discharge against medical advice | −1.11 | 3 | 0.030 |
| Time of triage | −0.65 | 2.31 | 0.068 |
CPR=Cardiopulmonary resuscitation
In Table 4, the mean differences of patients’ satisfaction indices have been given. According to these data, the highest mean difference belonged to “OOP payment,” “access to medicines,” and “giving information to the patients” (0.87, 0.72, and 0.61, respectively) in two periods before and after the implementation of the HSEP. The minimum mean difference belonged to “appearance of the staff,” “disposition of patient,” and “waiting time” (0.03, 0.03, and 0.09, respectively). Among the scales that were investigated, the mean differences of “facilities of department, “attention to patient,” “giving information to the patients,” quality of visits,” “access to medicines,” OOP payment, and overall patients satisfaction were significant in the two periods before and after the implementation of the plan (P < 0.05).
Table 4.
Results of statistical test for investigating the mean difference of scales of patients’ satisfaction
| Scales | Mean difference | Criterion of the test | P |
|---|---|---|---|
| Facilities of the department | 0.31 | −2.78 | 0.006 |
| Waiting time | 0.09 | 0.73 | 0.462 |
| Disposition | 0.03 | 0.30 | 0.761 |
| Appearance of the staff | 0.03 | 0.31 | 0.752 |
| Attention to patient | 0.36 | −3.25 | 0.001 |
| Giving information to the patients | 0.61 | −4.63 | 0.000 |
| Quality of visits | 0.28 | −2.20 | 0.029 |
| Access to medicines | 0.72 | −5.62 | 0.000 |
| Out-of-pocket payment | 0.87 | −7.37 | 0.000 |
| Overall patients satisfaction | 0.55 | −4.80 | 0.000 |
Discussion
This study was conducted to investigate the efficiency of the HSEP in improving the performance and quality of ED services in hospitals. To achieve this objective, the performance of ED was studied on the basis of performance indices of ED and also patients’ opinions and their degree of satisfaction. The data given in Table 1 show that the implementation of the plan has had a positive impact in all five investigated indices. Such achievements can be the result of strong emphasis on improving the quality of services.[10] Among the indices, the highest mean difference belonged to “failed CPR,” which had a reduction of 18.27. This significant reduction can be the result of triage time. After the implementation of the plan, a reduction of 0.65 was observed in this index. One of the most important factors in the success of CPR is the quick start of the resuscitation process.[21,22] The minimum index difference in the two periods of time belonged to the index of “patients discharged within 12 h.” This can be the result of a directive for temporary hospitalization of patients in ED. According to this directive, the maximum time of admission in ED is 12 h. After this time, the patient should be either discharged or transferred to one of the wards of the hospital. Among the indices of patients’ satisfaction, significant mean changes belonged to the scales of facilities of the department (0.31), attention to patient (0.36), giving information to the patients (0.61), quality of services (0.28), access to medicine (0.72), OOP payment (0.87), and overall patients satisfaction (0.55). The highest mean difference belonged to the scales of OOP. This can be the result of emphasis on financial support of the patients and also reducing the amount of payments made by patients.[10] In addition to these, some changes in insurance reimbursement laws might have been involved in such reduction. Before the implementation of the plan, hospitalized patients had to pay 10% of all expenses. In the period after the implementation of the HSEP, this reduced to 6% for patients living in cities and 3% for patients living in rural areas. This plan banned people to buy medicines and medical instruments from places outside hospital. This could be another reason for the reduction of the expenses.
The second rank of mean difference belonged to the scale of access to medicines. As mentioned before, making attempts to improve quality of services and to increase satisfaction of patients and also the ban of buying medicines from sources outside hospitals have paved the way for easy access to medicine. Improvement in “giving information to patients” can be the result of two factors. Emphasis on improving quality of services and increasing satisfaction among patients might have paved the way for their participation. Since patients’ participation involves their access to information, we can expect an increase in this scale. Furthermore, the growing of knowledge among people and pursuing their rights might have been another reason for the improvement in this scale.[23] Improvements in the scales of care for patients, facilities of department, and quality of services might have been the result of emphasis on hoteling services and patients’ satisfaction in the plan. The interaction among various factors and their impacts on each other is an undeniable issue. Providing more information for patients creates a sense of satisfaction among patients and they feel that they are being respected.[24] Furthermore, the quality of services is affected by other factors such as facilities of department, giving information to patients, and access to medicines.[25] Improving all of the above-mentioned factors can lead to a growth of satisfaction among patients. These results are consistent with the results of a number of studies in which the positive correlation between facilities of the department,[26] attention to patient, giving information to the patient,[27] OOP payment,[28] and access to medicines[29] on the one hand and patients satisfaction on the other hand. There were some limitations in our study. This study was conducted in only one hospital. Furthermore, performance and easily observable criteria were the only factors included in the study. These might have led to some limitations in this study.
Conclusions
HSEP and its supporting packages have created a number of positive changes in the performance of the EDs in the hospitals. These positive results can clearly be seen in the performance indices and those factors which are related to patients’ satisfaction. Therefore, the continuation of this plan can help health system improve the quality of its services. In spite of the improvement in the operational indices in the EDs and the patients’ satisfaction, it is necessary to evaluate the effectiveness of the mentioned plan in the studies and in other departments of the hospitals. Furthermore, because of the dependence to the present human resources, it is a need to evaluate some packages such as supporting the plan of the retention of the physicians in the deprived areas and the specialists that reside in the hospital in less developed environments such as the cities and states of the less developed areas in the country. Finally, what is worrying in this field is the efficiency of the foresaid project in creating the showed improvements. Considering the resources assigned to this project, it is important to study the efficiency and compare the cost-effectiveness. Beside all these, it is necessary to pay attention to the implementation of this project in the national level in relation to the efficiency of the applied resources.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank all officials and staff of the studied hospital for their sincere cooperation.
References
- 1.Awofeso N. Re-defining ‘Health’. Bull World Health Organ. 2005;83:802. [PMC free article] [PubMed] [Google Scholar]
- 2.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360:1083–8. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 3.Kelishadi R, Alikhani S, Delavari A, Alaedini F, Safaie A, Hojatzadeh E, et al. Obesity and associated lifestyle behaviours in Iran: Findings from the first national non-communicable disease risk factor surveillance survey. Public Health Nutr. 2008;11:246–51. doi: 10.1017/S1368980007000262. [DOI] [PubMed] [Google Scholar]
- 4.Kakeman E, Rahimi Forushani A, Dargahi H. Technical efficiency of hospitals in Tehran, Iran. Iran J Public Health. 2016;45:494–502. [PMC free article] [PubMed] [Google Scholar]
- 5.Shankar D. Health sector reforms for 21st century healthcare. J Ayurveda Integr Med. 2015;6:4–9. doi: 10.4103/0975-9476.154214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalhor R, Amini S, Sokhanvar M, Lotfi F, Sharifi M, Kakemam E, et al. Factors affecting the technical efficiency of general hospitals in Iran: Data envelopment analysis. J Egypt Public Health Assoc. 2016;91:20–5. doi: 10.1097/01.EPX.0000480717.13696.3c. [DOI] [PubMed] [Google Scholar]
- 7.Esmailzadeh H, Rajabi F, Rostamigooran N, Majdzadeh R. Iran health system reform plan methodology. Iran J Public Health. 2013;42:13–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Moradi-Lakeh M, Vosoogh-Moghaddam A. Health sector evolution plan in Iran; equity and sustainability concerns. Int J Health Policy Manag. 2015;4:637–40. doi: 10.15171/ijhpm.2015.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heshmati B, Joulaei H. Iran's health-care system in transition. Lancet. 2016;387:29–30. doi: 10.1016/S0140-6736(15)01297-0. [DOI] [PubMed] [Google Scholar]
- 10.Health System Reform Instruction. Iran: Iranian Ministry of Health. 2014. [cited 2018 Nov 1] Available from: http://www.behdashtgovir .
- 11.Baratta R, Degano C, Leonardi D, Vigneri R, Frittitta L. High prevalence of overweight and obesity in 11-15-year-old children from sicily. Nutr Metab Cardiovasc Dis. 2006;16:249–55. doi: 10.1016/j.numecd.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Physical status: The use and interpretation of anthropometry. Report of a WHO expert committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- 13.Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: Population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983. doi: 10.1136/bmj.d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright G, Causey S, Dienemann J, Guiton P, Coleman FS, Nussbaum M, et al. Patient satisfaction with nursing care in an urban and suburban emergency department. J Nurs Adm. 2013;43:502–8. doi: 10.1097/NNA.0b013e3182a3e821. [DOI] [PubMed] [Google Scholar]
- 15.Proper JS, Wong A, Plath AE, Grant KA, Just DW, Dulhunty JM, et al. Impact of clinical pharmacists in the emergency department of an Australian public hospital: A before and after study. Emerg Med Australas. 2015;27:232–8. doi: 10.1111/1742-6723.12384. [DOI] [PubMed] [Google Scholar]
- 16.Pitts SR, Pines JM, Handrigan MT, Kellermann AL. National trends in emergency department occupancy, 2001 to 2008: Effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med. 2012;60:679–86. doi: 10.1016/j.annemergmed.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 17.Godwin SA, Burton JH, Gerardo CJ, Hatten BW, Mace SE, Silvers SM, et al. Clinical policy: Procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2014;63:247–5.8E+19. doi: 10.1016/j.annemergmed.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 18.Yardim MS, Cilingiroglu N, Yardim N. Financial protection in health in Turkey: The effects of the health transformation programme. Health Policy Plan. 2014;29:177–92. doi: 10.1093/heapol/czt002. [DOI] [PubMed] [Google Scholar]
- 19.Akinci F, Mollahaliloǧlu S, Gürsöz H, Oǧücü F. Assessment of the Turkish health care system reforms: A stakeholder analysis. Health Policy. 2012;107:21–30. doi: 10.1016/j.healthpol.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 20.Castano RA, Arbelaez JJ, Giedion UB, Morales LG. Equitable financing, out-of-pocket payments and the role of health care reform in Colombia. Health Policy Plan. 2002;17(Suppl):5–11. doi: 10.1093/heapol/17.suppl_1.5. [DOI] [PubMed] [Google Scholar]
- 21.Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation. 2013;128:417–35. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 22.Xiangqian S, Yanhua Z, Min D, Ying X, Wei M, Shibing Z, et al. GW25-e0564 Influencing factors of the success rate of cardiopulmonary resuscitation. Am J Cardiol. 2014;64:C240. [Google Scholar]
- 23.Mayfield E, Laws MB, Wilson IB, Penstein Rosé C. Automating annotation of information-giving for analysis of clinical conversation. J Am Med Inform Assoc. 2014;21:e122–8. doi: 10.1136/amiajnl-2013-001898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeguers M, de Haes HC, Zandbelt LC, Ter Hoeven CL, Franssen SJ, Geijsen DD, et al. The information needs of new radiotherapy patients: How to measure? Do they want to know everything? And if not, why? Int J Radiat Oncol Biol Phys. 2012;82:418–24. doi: 10.1016/j.ijrobp.2010.09.032. [DOI] [PubMed] [Google Scholar]
- 25.Tajzadeh-Namin A, Pilevary N. Measuring customer satisfaction using SERQUAL survey. Manage Sci Lett. 2012;2:933–8. [Google Scholar]
- 26.Trout A, Magnusson AR, Hedges JR. Patient satisfaction investigations and the emergency department: What does the literature say? Acad Emerg Med. 2000;7:695–709. doi: 10.1111/j.1553-2712.2000.tb02050.x. [DOI] [PubMed] [Google Scholar]
- 27.Anderson R, Barbara A, Feldman S. What patients want: A content analysis of key qualities that influence patient satisfaction. J Med Pract Manage. 2007;22:255–61. [PubMed] [Google Scholar]
- 28.Gapenski LC, Pink GH. Understanding Healthcare Financial Management. 7th Edition. Chicago: Health Administration Press; 2007. [Google Scholar]
- 29.Naik Panvelkar P, Saini B, Armour C. Measurement of patient satisfaction with community pharmacy services: A review. Pharm World Sci. 2009;31:525–37. doi: 10.1007/s11096-009-9311-2. [DOI] [PubMed] [Google Scholar]


