Abstract
This study evaluates the patient demographics and clinical characteristics of 14 095 opioid-related hospitalizations from the US National Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project (HCUP).
Opioids are routinely prescribed for cancer-related pain, but little is known about the prevalence of opioid-related hospitalizations among patients with cancer. Opioid addiction among these patients has been estimated to be as high as 7.7%,1 but our understanding of opioid misuse among patients with cancer is based on small, preliminary studies.2 In light of the wider opioid epidemic, oncologists and palliative care clinicians frequently balance providing patients with legitimate access to opioids while protecting them and the general public from the risks associated with prescribing these medications.3
Methods
We examined trends and risk factors of opioid-related hospitalizations among patients with cancer between January 1, 2006, and December 31, 2014, using the US National Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project (HCUP).4 The database contained deidentified patient information and was deemed exempt from institutional review by the Partners Healthcare Human Research Committee. All analysis was conducted between December 2017 and September 2018. Our primary outcome was the number of opioid-related hospitalizations among adults with cancer (≥18 years old). We identified opioid-related hospitalizations using the International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes for heroin poisoning, opioid poisoning, and opioid dependence or abuse in the primary diagnosis field.5 We identified these patients using ICD-9 codes (140.0-239.9, 258.01-258.03, 789.51), while excluding conditions that rarely require opioids for pain control. We excluded the following: carcinomas in situ, benign neoplasms, hematologic cancers in remission, macroglobulinemia, polycythemia vera, essential thrombocythemia, and nonmelanoma skin cancers.
A multivariable logistic regression model evaluated the association between opioid-related hospitalizations and age, sex, race/ethnicity, primary insurance type, median household income quartile, hospital type, geographic region, alcohol abuse, drug abuse, depression, psychotic disorder, comorbidities, and year of hospital discharge. Comorbidities were identified using the Elixhauser comorbidity software from HCUP4 but excluded alcohol abuse, depression, drug abuse, metastatic cancer, lymphoma, psychotic disorder, and solid tumors without metastasis since these were analyzed independently. Weighted frequencies, proportions, and 95% confidence intervals (CIs) were calculated to reflect national estimates using inverse sampling weights provided by the NIS.4 Trend weights were used for 2006 through 2011 to adjust for the sampling redesign that was implemented in 2012.4
Results
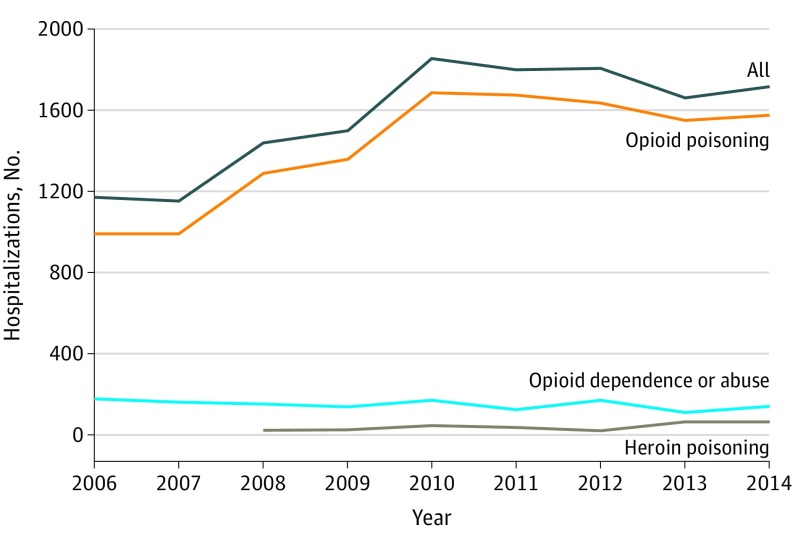
Among 25 004 243 hospitalizations overall for patients with cancer, 14 095 (0.06%) were opioid-related hospitalizations. Using a linear regression model, we approximated the trend in the overall number of opioid-related hospitalizations from 2006 to 2014 and observed an average increase of 78.9 admissions per year (from 1170 to 1715, P = .01). After adjusting for all-cause hospitalizations, the linear time trend of opioid-related hospitalizations increased on average by 0.003% per year (P = .003). Further decomposition by diagnosis type shows that nonheroin opioid poisoning made up 88.0% of all opioid-related hospitalizations (Figure). Factors associated with opioid-related hospitalizations for patients with cancer included drug abuse (odds ratio [OR], 7.92; 95% CI, 6.95-9.02), depression (OR, 2.34; 95% CI, 2.13-2.58), psychotic disorder (OR, 4.13; 95% CI, 3.66-4.65), white race, younger age, and year of hospitalization (Table). Alcohol abuse was associated with opioid-related hospitalizations, but the association was not significant (OR, 1.15; 95% CI, 0.99-1.35).
Figure. Opioid-Related Hospitalizations for US Patients With Cancer by Primary Diagnosis Type, 2006-2014.
Opioid-related hospitalizations due to heroin poisoning for 2006 and 2007 are not reported because there were fewer than 10 per year.
Table. Multivariable Characteristics for Opioid-Related Hospitalizations Among Patients With Cancer.
| Characteristic | Opioid-Related Hospitalization, OR (95% CI) |
|---|---|
| Age category, y | |
| 18-29 | 3.56 (2.75-4.61) |
| 30-49 | 3.49 (3.00-4.06) |
| 50-69 | 2.61 (2.34-2.91) |
| >70 | 1 [Reference] |
| Race/ethnicity | |
| White | 1 [Reference] |
| Black | 0.76 (0.67-0.87) |
| Hispanic | 0.56 (0.46-0.67) |
| Othera | 0.65 (0.52-0.81) |
| Substance abuse | |
| Alcohol | 1.15 (0.99-1.35) |
| Drugs | 7.92 (6.95-9.02) |
| Mental illness | |
| Depression | 2.34 (2.13-2.58) |
| Psychotic disorders | 4.13 (3.66-4.65) |
| Year range | |
| 2006-2008 | 1 [Reference] |
| 2009-2011 | 1.18 (1.06-1.31) |
| 2012-2014 | 1.17 (1.05-1.31) |
Includes Asian or Pacific Islander, Native American, and other.
Discussion
Opioid-related hospitalizations among patients with cancer are rare, are increasing at a very low rate over time, and are largely associated with nonheroin opioid poisoning. The characteristics associated with opioid-related hospitalizations among patients with cancer are consistent with established risk factors for opioid abuse in the noncancer population. Prior to prescribing opioids for cancer-related pain, routinely screening patients using standardized tools based on these associated factors (eg, Opioid Risk Tool6) may identify those patients with the greatest risk of an opioid-related hospitalization. Currently, no validated opioid risk screening tools exist specifically for patients with cancer, and little guidance is available on pain management in patients with both cancer and aberrant opioid use behavior.3 Additional research on opioid risk screening and management for patients with combined cancer and substance use disorders is needed.
References
- 1.Højsted J, Sjøgren P. Addiction to opioids in chronic pain patients: a literature review. Eur J Pain. 2007;11(5):490-518. doi: 10.1016/j.ejpain.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 2.Childers JW, King LA, Arnold RM. Chronic pain and risk factors for opioid misuse in a palliative care clinic. Am J Hosp Palliat Care. 2015;32(6):654-659. doi: 10.1177/1049909114531445 [DOI] [PubMed] [Google Scholar]
- 3.Arthur J, Bruera E How to use opioid therapy in patients at risk for aberrant opioid use. 2017. https://www.researchgate.net/publication/317539837_How_to_Use_Opioid_Therapy_in_Patients_at_Risk_for_Aberrant_Opioid_Use. Accessed on November 1, 2018.
- 4.Healthcare Cost and Utilization Project NIS Database Documentation. https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed November 1, 2018.
- 5.Song Z. Mortality quadrupled among opioid-driven hospitalizations, notably within lower-income and disabled white populations. Health Aff (Millwood). 2017;36(12):2054-2061. doi: 10.1377/hlthaff.2017.0689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6(6):432-442. doi: 10.1111/j.1526-4637.2005.00072.x [DOI] [PubMed] [Google Scholar]