Abstract
Importance
Deficits in fine motor skills and slow reading speed have been reported in school-aged children and adults with amblyopia. These deficits were correlated with lower self-perception of athletic and cognitive competence. Although perceived competence and social acceptance are key determinants of developing self-perception in young children, the association of amblyopia with self-perception and the association of altered self-perception with fine motor skills to date have not been reported for young children aged 3 to 7 years.
Objectives
To investigate whether amblyopia is associated with altered self-perception in young children and to assess whether any differences in self-perception are associated with deficits in vision and fine motor skills.
Design, Setting, and Participants
In this cross-sectional study, conducted at a pediatric vision laboratory from January 10, 2016, to May 4, 2018, healthy children aged 3 to 7 years (preschool to second grade) were enrolled, including 60 children with amblyopia; 30 children who never had amblyopia but had been treated for strabismus, anisometropia, or both; and 20 control children.
Main Outcomes and Measures
Self-perception was assessed using the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children, which includes the following 4 specific domains: cognitive competence, peer acceptance, physical competence, and maternal acceptance (total score range, 1-4; higher scores indicate higher perceived competence or acceptance). Fine motor skills were evaluated with the Manual Dexterity and Aiming and Catching scales of the Movement Assessment Battery for Children, second edition (score range, 1-19; higher scores indicate better skill performance). Visual acuity and stereoacuity also were assessed.
Results
Children with amblyopia (28 girls and 32 boys; mean [SD] age, 6.3 [1.3] years) had significantly lower mean (SD) peer acceptance and physical competence scores compared with the control children (peer acceptance, 2.74 [0.66] vs 3.11 [0.36]; mean difference, 0.37; 95% CI for difference, 0.06-0.68; P = .04; and physical competence, 2.86 [0.60] vs 3.43 [0.52]; mean difference, 0.57; 95% CI for difference, 0.27-0.87; P = .009). Among the children with amblyopia, self-perception of physical competence was significantly correlated with aiming and catching skills (r = 0.43; 95% CI, 0.10-0.67; P = .001) and stereoacuity (r = −0.39; 95% CI, −0.05 to −0.65; P = .02). Children treated for strabismus or anisometropia, but who never had amblyopia, also had significantly lower mean (SD) physical competence scores compared with control children (2.89 [0.54] vs 3.43 [0.52]; 95% CI for difference, 0.23-0.85; P = .03).
Conclusions and Relevance
These findings suggest that lower self-perception of peer acceptance and physical competence identify the broad effects of altered visual development in the everyday life of children with amblyopia.
This cross-sectional study examines whether amblyopia is associated with altered self-perception in children aged 3 to 7 years and assesses whether any differences in self-perception are associated with deficits in vision and fine motor skills.
Key Points
Question
Does amblyopia affect self-perception in children aged 3 to 7 years?
Findings
In a cross-sectional study, 60 children with amblyopia had lower peer acceptance and physical competence scores derived from the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children compared with 20 controls; among the children with amblyopia, self-perception of physical competence was correlated with aiming and catching skills as well as stereoacuity. Thirty children treated for strabismus or anisometropia, but who never had amblyopia, also had lower physical competence scores compared with controls.
Meaning
Lower self-perception of peer acceptance and physical competence may identify the broad effects of altered visual development for children with amblyopia.
Introduction
Deficits in fine motor skill and slow reading speed have been reported in school-aged children and adults with amblyopia.1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 These deficits are correlated with lower self-perception of scholastic, athletic, and social competence.16 Although perceived competence and social acceptance are key determinants of developing self-perception in young children,17,18,19 the influence of amblyopia on self-perception and its association with fine motor skills have not been reported for children aged 3 to 7 years, to our knowledge.
Children aged 3 to 7 years do not verbalize concepts about their overall worth as a person (ie, their global self-worth).20,21 Nonetheless, they are able to make judgments about how competent they are in particular areas and whether they receive support from friends, parents, and teachers.22 Cognitive research shows that young children are able to recognize similar action patterns between themselves and others and can judge the extent to which others are similar to themselves (ie, “like me”).23 On this basis, we chose to use the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children, a test instrument that presents pairs of pictures that ask “Which child is more like you?”22 This instrument assesses self-perception in the following 4 specific domains: cognitive and physical competence and peer and maternal acceptance.
The objectives of this study were to examine whether amblyopia is associated with altered self-perception of competence and acceptance in children aged 3 to 7 years and to assess whether any differences in self-perception are associated with deficits in vision or fine motor skills.
Methods
Participants
Sixty children with amblyopia aged 3 to 7 years (preschool to second grade) were enrolled in this study, which was conducted from January 10, 2016, to May 4, 2018. Eligibility criteria were a current diagnosis of strabismic, anisometropic, or combined mechanism amblyopia (diagnostic criteria developed by the Pediatric Eye Disease Investigator Group for the Amblyopia Treatment Studies24); best-corrected visual acuity (BCVA) in the amblyopic eye of 0.2 logMAR or worse (Snellen equivalent, 20/30 or worse); BCVA in the fellow eye of 0.1 logMAR or better (Snellen equivalent, 20/25 or better); and interocular difference in BCVA of 0.2 logMAR or greater (Snellen equivalent, ≥2 lines). To evaluate the influence of amblyogenic factors in the absence of amblyopia, 30 age-similar children who never had amblyopia but had been treated for strabismus, anisometropia, or both were enrolled. As a comparison group for both of these cohorts, 20 age-similar controls were also enrolled. None of the children were born prematurely (>32 weeks’ postmenstrual age), had coexisting ocular or systemic disease, or had a history of congenital malformation or infection. Characteristics of each group are summarized in Table 1. Written informed consent was obtained from a parent after explanation of the nature and possible consequences of the study. All procedures and the protocol were approved by the University of Texas Southwestern Medical Center Institutional Review Board, followed the tenets of the Declaration of Helsinki,25 and complied with the requirements of the US Health Insurance Portability and Accountability Act of 1996.
Table 1. Participant Characteristics.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Amblyopia | Never Amblyopic but Treated for Strabismus, Anisometropia, or Botha | Control | |
| No. of children | 60 | 30 | 20 |
| Self-perception | 60 | 30 | 20 |
| Vision | 60 | 30 | 20 |
| Motor skills | 33 | NA | NA |
| Female sex | 28 (47) | 16 (53) | 11 (55) |
| Race/ethnicity | |||
| Non-Hispanic white | 40 (67) | 16 (53) | 14 (70) |
| Hispanic white | 11 (18) | 7 (23) | 2 (10) |
| African American | 4 (7) | 3 (10) | 2 (10) |
| Asian | 1 (2) | 1 (3) | 0 |
| Middle Eastern | 1 (2) | 1 (3) | 0 |
| >1 Race/ethnicity | 3 (5) | 3 (10) | 1 (5) |
| Age, mean (SD), y | 6.3 (1.3) | 5.9 (1.3) | 6.1 (1.1) |
| Associated eye conditions | |||
| Strabismus | 22 (37) | 19 (63) | NA |
| Anisometropia | 17 (28) | 6 (20) | NA |
| Combined | 21 (35) | 5 (17) | NA |
| Amblyopic eye visual acuity, logMARb | |||
| ≤0.1 | 0 | 30 (100) | 20 (100) |
| 0.2-0.3 | 22 (37) | 0 | 0 |
| 0.4-0.5 | 21 (35) | 0 | 0 |
| 0.6-0.7 | 5 (8) | 0 | 0 |
| >0.7 | 12 (20) | 0 | 0 |
| Mean (SD) [range] | 0.49 (0.27) [0.2 to 1.4] |
0.04 (0.07) [−0.1 to 0.2] |
−0.01 (0.07) [−0.1 to 0.2] |
| Fellow eye visual acuity, logMAR (Snellen equivalent)c | |||
| −0.1 (20/16) | 12 (20) | 5 (17) | 11 (55) |
| 0.0 (20/20) | 27 (45) | 18 (60) | 8 (40) |
| 0.1 (20/25) | 21 (35) | 7 (23) | 1 (5) |
| Mean (SD) [range] | |||
| logMAR | 0.01 (0.07) [−0.1 to 0.1] |
0.01 (0.06) [−0.1 to 0.1] |
−0.05 (0.06) [−0.1 to 0.1] |
| Snellen equivalent | 20/20 [20/16 to 20/25] |
20/20 [20/16 to 20/25] |
20/20 [20/16 to 20/25] |
| Stereoacuity, mean (SD) [range], log arcsec d | 3.75 (0.58) [1.8 to nil] |
3.33 (0.83) [1.8 to nil] |
1.83 (0.33) [1.6 to 2.3] |
| Amblyopia treatment | |||
| Current spectacle wear | 58 (97) | 20 (67) | NA |
| History of spectacle wear | 59 (98) | 24 (80) | NA |
| Current patching | 27 (45) | NA | NA |
| History of patching | 46 (77) | NA | NA |
| Current atropine or optical penalization | NA | NA | NA |
| History of atropine or optical penalization | 4 (7) | NA | NA |
Abbreviations: BCVA, best-corrected visual acuity; NA, not applicable.
Children without amblyopia but with strabismus and/or anisometropia had no history of amblyopia and had no prior amblyopia treatment.
Best-corrected visual acuity of the amblyopic eye or, for participants without amblyopia and for controls, BCVA of the eye with worse visual acuity.
Best-corrected visual acuity of the fellow eye or, for participants without amblyopia and for controls, BCVA of the eye with better visual acuity.
Nil stereoacuity was assigned a value of 4.0 log arcsec.
Vision
Every participant with or without amblyopia underwent a comprehensive eye examination performed by a fellowship-trained pediatric ophthalmologist who diagnosed whether amblyopia was present and identified the etiologic factor(s). Children wore optical correction, if needed, in accordance with American Association for Pediatric Ophthalmology and Strabismus guidelines.26 Monocular BCVA was obtained for each eye with an opaque occluder patch and the Amblyopia Treatment Study HOTV method (for children aged 3-6 years) or electronic Early Treatment Diabetic Retinopathy Study (E-ETDRS) method (for children aged 7 years).27,28,29,30 Random dot stereoacuity was evaluated using the Randot Preschool Stereoacuity Test (Stereo Optical Co Inc) and the Stereo Butterfly Test (Stereo Optical Co Inc), which were administered and scored according to the manufacturer’s instructions and reported in log arcsec.
Self-perception
Self-perception was assessed in every participant with the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children.22 This instrument uses a multidimensional approach to the measurement of self-perception by assessing self-perception in the following 4 specific domains: cognitive competence (eg, counting, alphabet, and early reading and writing skills), physical competence (eg, climbing, running, and bouncing a ball), peer acceptance (eg, activities with friends and sharing), and maternal acceptance (activities and social interactions with mother). Young children comprehend the pictures and response options, the psychometric properties are sound, and the item scores have moderate to good internal consistency (Cronbach α = 0.53-0.83 for the individual scales and 0.87 for the total scale).22 Total scores can range from 1 to 4, and higher scores indicate higher perceived competence or acceptance. The SDs are consistent with scale sensitivity to individual differences in perceived competence and acceptance among young children.22 This instrument is widely used for research with preschool-aged children, including the measurement of the effects of intellectual disability, stuttering, and obesity on self-concept31,32,33 and the effects of physical activity programs on self-concept.34,35,36
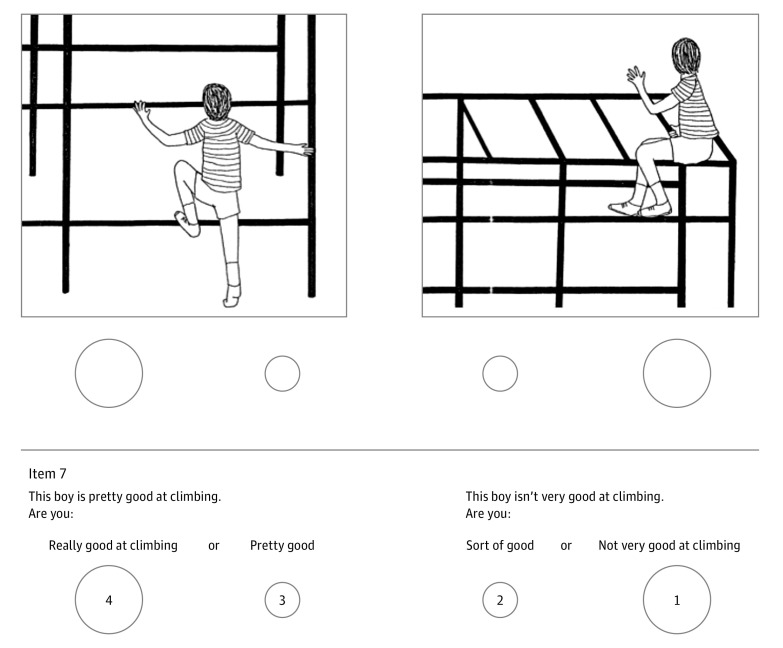
There are 6 pairs of pictures for each domain, presented in a 2-alternative format. There are 4 versions of the pictorial questionnaire, with a male and female version for each of 2 age groups (preschool and kindergarten and first and second grades). A sample question from the physical competence scale for boys in first or second grade is provided in Figure 1. As instructed in the procedural manual for the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children, the tester began the test by telling the child, “I have something here that’s kind of like a picture game and it’s called ‘Which Boy (Girl) Is the Most Like Me.’ I’m going to tell you about what each of the boys (girls) in the picture is doing.” The tester showed the child the pair of pictures and read the statements describing each picture. The child was first asked to decide which child in the pictures is most like him or her. After this initial choice, the child was asked to make a second choice about whether they are a lot like the child in the picture or just a little like the child in the picture, by pointing to the larger or smaller circle under the picture they chose. Harter and Pike,22 developers of the Self-perception Profile for Children, argue that the effectiveness of this approach lies in the implication that half the children in the world view themselves one way and half view themselves the other way, legitimizing either choice. Refining their answer into the category of “A lot like me” or “A little like me” broadens the range of choices into a 4-point scale (where 1 represents the lowest perceived competence or adequacy and 4 represents the highest perceived competence or adequacy). Within each domain, the first alternative is phrased in a positive manner for 3 of the 6 items (eg, “This boy is good at climbing”) and in a negative manner for the remaining 3 questions (eg, “This boy isn’t very good at bouncing the ball”). A mean score was calculated for each subscale.
Figure 1. Sample Item and Question From the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children.
A pair of pictures from the physical competence scale for boys in first or second grade is shown above a statement read to the child describing each picture. The child was first asked to decide which child is most like him and then to refine that choice by pointing to a response indicated by a larger or smaller circle under the picture he chose.
All children had practice with a sample question to ensure that they understood the 2-alternative format and the subsequent choice to refine their answer. Ideally, the child’s parent was seated in the next room, but if that was not possible, he or she sat behind the child and was instructed to not assist or coach the child in any way. Self-perception scale scores were not available to the examiner responsible for testing vision and motor skills.
Fine Motor Skills
A convenience sample composed of a subset of 33 of the children with amblyopia were tested with the Manual Dexterity and Aiming and Catching Scales of the Movement Assessment Battery for Children, second edition (Pearson Clinical Assessment),37 a standardized test of motor skills and coordination administered in age bands (ages 3-6 years and 7-10 years for the present study). Raw scores per task were combined, and tables provided in the test manual were used to convert the combined raw scores into standardized scores, with higher scores indicating better performance.
Statistical Analysis
One-way analysis of variance was used to evaluate group differences (children with amblyopia, children who never had amblyopia, and healthy controls) for each self-perception domain (cognitive competence, physical competence, peer acceptance, and maternal acceptance). Significant analysis of variance results were followed with post hoc Bonferroni-corrected pairwise comparisons of the groups with and without amblyopia with the controls; 2-sided P values are reported. For the group with amblyopia, Pearson r was used to evaluate correlations of BCVA, stereoacuity, and fine motor skills with self-perception domain scores. Independent t tests were conducted to assess whether children with amblyopia with nil vs measurable stereoacuity and with or without strabismus differed on any self-perception domain.
Results
Self-perception
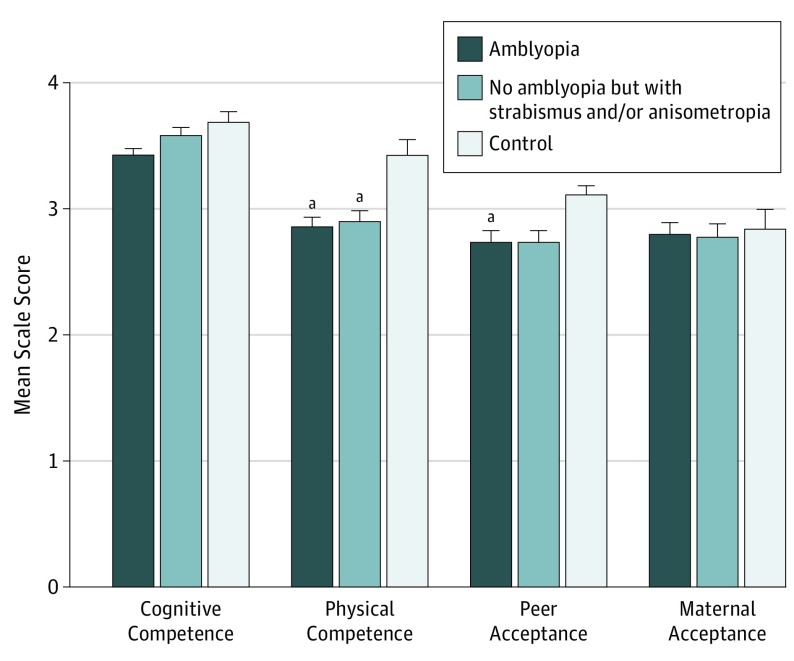
Mean self-perception scale scores for the 60 children with amblyopia (28 [47%] girls; mean [SD] age, 6.3 [1.3] years), 30 children who never had amblyopia (16 [53%] girls; mean [SD] age, 5.9 [1.3] years), and control children (11 [55%] girls; mean [SD] age, 6.1 [1.1] years) are summarized in Figure 2 and Table 2. Peer acceptance and physical competence were significantly different among groups (peer acceptance, F2,106 = 3.43; P = .04; and physical competence, F2,106 = 4.94; P = .009), but self-perception of cognitive competence and of maternal acceptance did not differ between the groups. Post hoc Bonferroni-corrected pairwise comparisons showed that children with amblyopia had lower mean (SD) scores than did control children for peer acceptance and physical competence (peer acceptance, 2.74 [0.66] vs 3.11 [0.36]; mean difference, 0.37; 95% CI for difference, 0.06-0.68; P = .04, Cohen d = 0.70; and physical competence, 2.86 [0.60] vs 3.43 [0.52]; mean difference, 0.57, 95% CI for difference, 0.27-0.87; P = .009, Cohen d = 1.02). Children who never had amblyopia had significantly lower mean (SD) scores than did control children for physical competence (2.89 [0.54] vs 3.43 [0.52]; mean difference, 0.54; 95% CI for difference, 0.23-0.85; P = .03, Cohen d = 1.58), but we were not able to confidently identify differences from controls for self-perception of cognitive competence, peer acceptance, or maternal acceptance.
Figure 2. Mean (SD) Domain Scores Derived From the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children.
Scores are depicted for children with amblyopia, children who were never amblyopic but had been treated for strabismus and/or anisometropia, and control children. Scores can range from 1 to 4; higher scores indicate higher perceived competence or acceptance.
aSignificantly different than control mean. For peer acceptance: children with amblyopia vs controls, P = .04; for physical competence: children with amblyopia vs controls, P = .009; and children who were never amblyopic but had been treated for strabismus and/or anisometropia vs controls, P = .03.
Table 2. Domain Scale Scores.
| Domain | Score, Mean (SD)a | ||
|---|---|---|---|
| Amblyopia | Never Amblyopic but Treated for Strabismus, Anisometropia, or Both | Control | |
| Cognitive competence | 3.41 (0.55) | 3.56 (0.47) | 3.69 (0.37) |
| Peer acceptance | 2.74 (0.66)b | 2.74 (0.51) | 3.11 (0.36) |
| Physical competence | 2.86 (0.60)c | 2.89 (0.54)d | 3.43 (0.52) |
| Maternal acceptance | 2.81 (0.64) | 2.79 (0.52) | 2.84 (0.70) |
Scores can range from 1 to 4; higher scores indicate higher perceived acceptance or competence.
P = .04 Bonferroni-corrected post hoc t test amblyopia group vs control group.
P = .009 Bonferroni-corrected post hoc t test amblyopia group vs control group.
P = .03 Bonferroni-corrected post hoc t test never amblyopia group vs control group.
Self-perception and Fine Motor Skills in Children With Amblyopia
Correlations between competence scores and fine motor skills were examined for amblyopic children. Physical competence scores were positively correlated with catching scores (ability to catch a bean bag or ball; r = 0.43; 95% CI, 0.10-0.67; P = .001), but the lower bound of the 95% CI indicated only a weak correlation. No correlations between self-perception domain scores and peer acceptance scores were confidently identified.
Self-perception and Clinical Factors in Children With Amblyopia
No correlations for BCVA in the amblyopic eye and self-perception domain scores were confidently identified. Stereoacuity was significantly correlated with physical competence scores (r = −0.39; 95% CI, −0.05 to −0.65; P = .02) but the lower bound of the 95% CI indicates a weak correlation. Mean (SD) physical competence scores of children with amblyopia and nil stereoacuity were significantly lower than scores of children with measurable stereoacuity (2.73 [0.61] vs 3.38 [0.28]; 95% CI for difference, 0.27-1.03; t58 = 3.11; P = .003). We were not able to confidently identify differences in scores of subgroups of children with amblyopia with vs without strabismus nor in subgroups with vs without treatment for amblyopia (current or prior) in any self-perception domain. Because nearly every child with amblyopia (59 [98%]) wore spectacles, we were not able to compare domain scores of subgroups with and without spectacles. Most of the children who never had amblyopia (24 of 30 [80%]) also wore spectacles.
Discussion
Amblyopia was associated with lower self-perception scores for peer acceptance and physical competence in children aged 3 to 7 years (preschool to second grade) compared with healthy controls, with mean score differences of 0.37 for peer acceptance and 0.57 for physical competence. The difference in peer acceptance scores is similar to that observed between children who were or were not participating in after-school programs and the difference between children with chronic health conditions vs controls (0.40-0.55).38,39,40 The difference in physical competence scores is similar to the lower scores observed in 5- to 9-year-old children with developmental coordination disorder compared with controls (0.49 lower).41 Risk factors for amblyopia (strabismus and anisometropia) were also associated with lower self-perception scores for physical competence to a similar extent. No differences in self-perception of cognitive competence or maternal acceptance were found among the 3 groups. Self-perception of physical competence was weakly associated with performance of catching skills and with stereoacuity.
Our finding that both children with amblyopia and those who never had amblyopia have comparably lower physical competence scores than controls suggests that discordant binocular visual experience, and not amblyopia, is influencing children’s self-perception of physical competence. This hypothesis is also consistent with the significant difference in physical competence domain scores we found for children with amblyopia and nil stereoacuity compared with those who had measurable stereoacuity.
There is scant literature addressing the influence of amblyopia on self-perception, self-esteem, or quality of life for children aged 3 to 7 years. Instead, most studies of young children with amblyopia have focused on parent report of the effects of patching treatment on child well-being and behavior42,43,44,45,46 or on patching treatment–related stigma, bullying, or family stress.43,44,47,48 Using the Pediatric Quality of Life Inventory, Wen et al49 reported that strabismus, but not amblyopia, was associated with quality of life in preschool-aged children. However, they noted that an instrument to evaluate vision-related quality of life may have been needed to fully assess the effect of amblyopia.
To our knowledge, only 2 prior studies have addressed the association of amblyopia with fine motor skills in children aged 3 to 7 years and have reported diminished ball catching skills50 and slower precision reach-to-grasp a familiar household object.51 One additional study reported no effect of amblyopia on motor development but evaluated a sample of only 9 children with amblyopia using a composite measure of motor development derived from multiple testing instruments, each administered at different points when the child was aged 3 to 11 years.52
Whether rehabilitation of visual acuity or stereoacuity after treatment of amblyopia will result in improved self-perception of peer acceptance and physical competence is unknown. The lack of a correlation between BCVA and peer acceptance or physical competence domain scores suggests that amblyopia treatment that monocularly treats visual acuity may not improve self-perception. On the other hand, the correlation between stereoacuity and physical competence domain scores suggests that rehabilitation of binocular vision may yield improved self-perception. In an older cohort of children aged 7 to 12 years, Webber et al3 reported that binocular treatment of amblyopia resulted in improvement of fine motor skills, suggesting that binocular treatment could improve self-perception of physical competence. However, we know that the foundations of self-perception are already established by age 5 years,17,18,19 and it is unclear whether treatment that rehabilitates vision will be able to alter self-perception. Because of this uncertainty, we included only children with no history of amblyopia diagnosis or treatment (patching, atropine penalization, or optical penalization) in our group of children who never had amblyopia, unlike other studies that included successfully treated children with amblyopia. Our finding of altered self-perception in children with amblyopia who were enrolled in preschool to second grade suggests that remediation of amblyopia may be needed prior to entry into formal schooling when peer comparisons begin to emerge.
Limitations
Our study had several limitations. Our findings cannot be generalized to children with other types of amblyopia, including bilateral amblyopia and deprivation amblyopia. Second, we were unable to assess the association of spectacles with self-perception because 98% of the children with amblyopia wore spectacles. However, we also evaluated a group of children who never had amblyopia, most of whom (80%) wore spectacles. Children with amblyopia scored lower than controls on peer acceptance and physical competence domains, while the children who never had amblyopia scored lower than controls only on the physical competence domain. Third, because the group of children who never had amblyopia included only children with no prior amblyopia diagnosis or treatment, we could not assess whether a history of amblyopia or amblyopia treatment may be associated with self-perception. Fourth, the Pictorial Scale of Perceived Competence and Social Acceptance for Young Children cannot be administered to children older than 7 years, limiting our cohort to young children.
Conclusions
During early childhood, fine motor skills serve an essential function in supporting the emergence of a child’s independence, including manipulation of objects and self-care, and are crucial for acquiring positive self-esteem, proficiency, and academic skills. Positive self-perception has an important influence on well-being and quality of life. Lower self-perception of peer acceptance and physical competence, along with the modest correlation between self-perception of physical competence and performance of aiming and catching tasks, identifies the broad effects of altered visual development in the everyday life of children with amblyopia.
References
- 1.Webber AL, Wood JM, Gole GA, Brown B. Effect of amblyopia on self-esteem in children. Optom Vis Sci. 2008;85(11):1074-1081. doi: 10.1097/OPX.0b013e31818b9911 [DOI] [PubMed] [Google Scholar]
- 2.Webber AL, Wood JM, Gole GA, Brown B. The effect of amblyopia on fine motor skills in children. Invest Ophthalmol Vis Sci. 2008;49(2):594-603. doi: 10.1167/iovs.07-0869 [DOI] [PubMed] [Google Scholar]
- 3.Webber AL, Wood JM, Thompson B. Fine motor skills of children with amblyopia improve following binocular treatment. Invest Ophthalmol Vis Sci. 2016;57(11):4713-4720. doi: 10.1167/iovs.16-19797 [DOI] [PubMed] [Google Scholar]
- 4.O’Connor AR, Birch EE, Anderson S, Draper H; FSOS Research Group . The functional significance of stereopsis. Invest Ophthalmol Vis Sci. 2010;51(4):2019-2023. doi: 10.1167/iovs.09-4434 [DOI] [PubMed] [Google Scholar]
- 5.O’Connor AR, Birch EE, Anderson S, Draper H. Relationship between binocular vision, visual acuity, and fine motor skills. Optom Vis Sci. 2010;87(12):942-947. doi: 10.1097/OPX.0b013e3181fd132e [DOI] [PubMed] [Google Scholar]
- 6.Niechwiej-Szwedo E, Goltz HC, Colpa L, Chandrakumar M, Wong AM. Effects of reduced acuity and stereo acuity on saccades and reaching movements in adults with amblyopia and strabismus. Invest Ophthalmol Vis Sci. 2017;58(2):914-921. doi: 10.1167/iovs.16-20727 [DOI] [PubMed] [Google Scholar]
- 7.Niechwiej-Szwedo E, Goltz HC, Chandrakumar M, Wong AM. Effects of strabismic amblyopia on visuomotor behavior, part II: visually guided reaching. Invest Ophthalmol Vis Sci. 2014;55(6):3857-3865. doi: 10.1167/iovs.14-14543 [DOI] [PubMed] [Google Scholar]
- 8.Niechwiej-Szwedo E, Goltz HC, Chandrakumar M, Wong AM. Effects of strabismic amblyopia and strabismus without amblyopia on visuomotor behavior, III: temporal eye-hand coordination during reaching. Invest Ophthalmol Vis Sci. 2014;55(12):7831-7838. doi: 10.1167/iovs.14-15507 [DOI] [PubMed] [Google Scholar]
- 9.Niechwiej-Szwedo E, Goltz HC, Chandrakumar M, Hirji Z, Wong AM. Effects of anisometropic amblyopia on visuomotor behavior, III: temporal eye-hand coordination during reaching. Invest Ophthalmol Vis Sci. 2011;52(8):5853-5861. doi: 10.1167/iovs.11-7314 [DOI] [PubMed] [Google Scholar]
- 10.Niechwiej-Szwedo E, Goltz HC, Chandrakumar M, Hirji Z, Crawford JD, Wong AM. Effects of anisometropic amblyopia on visuomotor behavior, part 2: visually guided reaching. Invest Ophthalmol Vis Sci. 2011;52(2):795-803. doi: 10.1167/iovs.10-6092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly KR, Morale SE, Felius J, Jost RM, Birch EE Amblyopia disrupts the development of eye-hand coordination. Presented at: 42nd Annual Meeting of the American Association for Pediatric Ophthalmology and Strabismus; April 7, 2016; Vancouver, BC. [Google Scholar]
- 12.Kelly KR, Jost RM, De La Cruz A, Birch EE. Amblyopic children read more slowly than controls under natural, binocular reading conditions. J AAPOS. 2015;19(6):515-520. doi: 10.1016/j.jaapos.2015.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grant S, Suttle C, Melmoth DR, Conway ML, Sloper JJ. Age- and stereovision-dependent eye-hand coordination deficits in children with amblyopia and abnormal binocularity. Invest Ophthalmol Vis Sci. 2014;55(9):5687-57015. doi: 10.1167/iovs.14-14745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grant S, Melmoth DR, Morgan MJ, Finlay AL. Prehension deficits in amblyopia. Invest Ophthalmol Vis Sci. 2007;48(3):1139-1148. doi: 10.1167/iovs.06-0976 [DOI] [PubMed] [Google Scholar]
- 15.Kelly KR, Jost RM, De La Cruz A, et al. Slow reading in children with anisometropic amblyopia is associated with fixation instability and increased saccades. J AAPOS. 2017;21(6):447-451.e1. doi: 10.1016/j.jaapos.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birch EE, Castañeda YS, Cheng-Patel CS, et al. Self-perception of school-aged children with amblyopia and its association with reading speed and motor skills [published online November 15, 2018]. JAMA Ophthalmol. 2018. doi: 10.1001/jamaophthalmol.2018.5527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harter S. Developmental perspective on the self-system In: Hetherington M, ed. Handbook of Child Psychology. Vol 3. New York, NY: Wiley; 1983:275-386. [Google Scholar]
- 18.Harter S. Causes, correlates, and the functional role of global self-worth: a life-span perspective In: Kolligian J, Sternberg R, eds. Integrative Processes and Socialization: Early to Middle Childhood. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988:67-97. [Google Scholar]
- 19.Bandura A. Conclusion: reflections on nonability determinants of competence In: Kolligian J, Sternberg R, eds. Integrative Processes and Socialization: Early to Middle Childhood. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988:315-362. [Google Scholar]
- 20.Harter S. The Construction of the Self: Developmental and Sociocultural Foundations. New York, NY: Guilford Press; 2012. [Google Scholar]
- 21.Harter S. The development of self-representations In: Fischer C, Lerner R, eds. Applied Developmental Science: An Encyclopedia of Research, Policies, and Programs. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- 22.Harter S, Pike R. The Pictorial Scale of Perceived Competence and Social Acceptance for Young Children. Child Dev. 1984;55(6):1969-1982. doi: 10.2307/1129772 [DOI] [PubMed] [Google Scholar]
- 23.Meltzoff A. Origins of social cognition: bi-directional self-other mapping and the “likeme” hypothesis In: Banaji M, Gelman S, eds. Navigating the Social World: What Infants, Children, and Other Species Can Teach Us. New York, NY: Oxford University Press; 2013:139-144. doi: 10.1093/acprof:oso/9780199890712.003.0025 [DOI] [Google Scholar]
- 24.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268-278. doi: 10.1001/archopht.120.3.268 [DOI] [PubMed] [Google Scholar]
- 25.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 26.American Association for Pediatric Ophthalmology and Strabismus Policy statement: medical need for glasses. https://www.aapos.org/client_data/files/2017/506_aaposmedialneedforglasses.pdf. Accessed January 8, 2019.
- 27.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS. 2008;12(2):145-149. doi: 10.1016/j.jaapos.2007.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holmes JM, Beck RW, Repka MX, et al. ; Pediatric Eye Disease Investigator Group . The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119(9):1345-1353. doi: 10.1001/archopht.119.9.1345 [DOI] [PubMed] [Google Scholar]
- 29.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the Early Treatment Of Diabetic Retinopathy Study testing protocol. Am J Ophthalmol. 2003;135(2):194-205. doi: 10.1016/S0002-9394(02)01825-1 [DOI] [PubMed] [Google Scholar]
- 30.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the Amblyopia Treatment Study visual acuity testing protocol. Am J Ophthalmol. 2001;132(6):903-909. doi: 10.1016/S0002-9394(01)01256-9 [DOI] [PubMed] [Google Scholar]
- 31.Hertsberg N, Zebrowski PM. Self-perceived competence and social acceptance of young children who stutter: initial findings. J Commun Disord. 2016;64:18-31. doi: 10.1016/j.jcomdis.2016.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fiasse C, Nader-Grosbois N. Perceived social acceptance, theory of mind and social adjustment in children with intellectual disabilities. Res Dev Disabil. 2012;33(6):1871-1880. doi: 10.1016/j.ridd.2012.05.017 [DOI] [PubMed] [Google Scholar]
- 33.Spessato BC, Gabbard C, Robinson L, Valentini NC. Body mass index, perceived and actual physical competence: the relationship among young children. Child Care Health Dev. 2013;39(6):845-850. [DOI] [PubMed] [Google Scholar]
- 34.Crane JR, Naylor PJ, Cook R, Temple VA. Do perceptions of competence mediate the relationship between fundamental motor skill proficiency and physical activity levels of children in kindergarten? J Phys Act Health. 2015;12(7):954-961. doi: 10.1123/jpah.2013-0398 [DOI] [PubMed] [Google Scholar]
- 35.Folleto JC, Pereira KR, Valentini NC. The effects of yoga practice in school physical education on children’s motor abilities and social behavior. Int J Yoga. 2016;9(2):156-162. doi: 10.4103/0973-6131.183717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vazou S, Mantis C, Luze G, Krogh JS. Self-perceptions and social-emotional classroom engagement following structured physical activity among preschoolers: a feasibility study. J Sport Health Sci. 2017;6(2):241-247. doi: 10.1016/j.jshs.2016.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henderson SE, Sugden DA, Barnett AL. The Movement Assessment Battery for Children—Second Edition. London, England: Pearson Education Inc; 2007. [Google Scholar]
- 38.Mobley CE, Harless LS, Miller KL. Self-perceptions of preschool children with spina bifida. J Pediatr Nurs. 1996;11(4):217-224. doi: 10.1016/S0882-5963(96)80094-7 [DOI] [PubMed] [Google Scholar]
- 39.Russo RN, Goodwin EJ, Miller MD, Haan EA, Connell TM, Crotty M. Self-esteem, self-concept, and quality of life in children with hemiplegic cerebral palsy. J Pediatr. 2008;153(4):473-477. doi: 10.1016/j.jpeds.2008.05.040 [DOI] [PubMed] [Google Scholar]
- 40.Scurlock D. Effect of occupation-based groups on self-concept of children aged 5-8: a pilot study. Occup Ther Health Care. 2015;29(1):63-76. doi: 10.3109/07380577.2014.968942 [DOI] [PubMed] [Google Scholar]
- 41.Engel-Yeger B, Sido R, Mimouni-Bloch A, Weiss PL. Relationship between perceived competence and performance during real and virtual motor tasks by children with developmental coordination disorder. Disabil Rehabil Assist Technol. 2017;12(7):752-757. doi: 10.1080/17483107.2016.1261305 [DOI] [PubMed] [Google Scholar]
- 42.Felius J, Chandler DL, Holmes JM, et al. ; Pediatric Eye Disease Investigator Group . Evaluating the burden of amblyopia treatment from the parent and child’s perspective. J AAPOS. 2010;14(5):389-395. doi: 10.1016/j.jaapos.2010.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holmes JM, Beck RW, Kraker RT, et al. ; Pediatric Eye Disease Investigator Group . Impact of patching and atropine treatment on the child and family in the Amblyopia Treatment Study. Arch Ophthalmol. 2003;121(11):1625-1632. doi: 10.1001/archopht.121.11.1625 [DOI] [PubMed] [Google Scholar]
- 44.Holmes JM, Strauber S, Quinn GE, Cole SR, Felius J, Kulp M; Pediatric Eye Disease Investigator Group . Further validation of the Amblyopia Treatment Index parental questionnaire. J AAPOS. 2008;12(6):581-584. doi: 10.1016/j.jaapos.2008.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hrisos S, Clarke MP, Wright CM. The emotional impact of amblyopia treatment in preschool children: randomized controlled trial. Ophthalmology. 2004;111(8):1550-1556. doi: 10.1016/j.ophtha.2003.12.059 [DOI] [PubMed] [Google Scholar]
- 46.Tyrrell RA, Owens DA. A rapid technique to assess the resting states of the eyes and other threshold phenomena: the modified binary search (MOBS). Behav Res Methods Instrum Comput. 1988;20(2):137-141. doi: 10.3758/BF03203817 [DOI] [Google Scholar]
- 47.Drews-Botsch CD, Hartmann EE, Celano M; Infant Aphakia Treatment Study Group . Predictors of adherence to occlusion therapy 3 months after cataract extraction in the Infant Aphakia Treatment Study. J AAPOS. 2012;16(2):150-155. doi: 10.1016/j.jaapos.2011.12.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams C, Horwood J, Northstone K, Herrick D, Waylen A, Wolke D; ALSPAC Study Group . The timing of patching treatment and a child’s wellbeing. Br J Ophthalmol. 2006;90(6):670-671. doi: 10.1136/bjo.2006.091082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wen G, McKean-Cowdin R, Varma R, et al. ; Multi-ethnic Pediatric Eye Disease Study Group . General health-related quality of life in preschool children with strabismus or amblyopia. Ophthalmology. 2011;118(3):574-580. doi: 10.1016/j.ophtha.2010.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Engel-Yeger B. Evaluation of gross motor abilities and self perception in children with amblyopia. Disabil Rehabil. 2008;30(4):243-248. doi: 10.1080/09638280701257221 [DOI] [PubMed] [Google Scholar]
- 51.Suttle CM, Melmoth DR, Finlay AL, Sloper JJ, Grant S. Eye-hand coordination skills in children with and without amblyopia. Invest Ophthalmol Vis Sci. 2011;52(3):1851-1864. doi: 10.1167/iovs.10-6341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wilson GA, Welch D. Does amblyopia have a functional impact? findings from the Dunedin Multidisciplinary Health and Development Study. Clin Exp Ophthalmol. 2013;41(2):127-134. doi: 10.1111/j.1442-9071.2012.02842.x [DOI] [PubMed] [Google Scholar]