Introduction
For several decades, the focus on understanding autism spectrum disorder (ASD) seemed to leave little room for research on co-occurring affective disorders. Additionally, diagnostic overshadowing, or the tendency for clinicians to overlook or dismiss depressive symptoms or behaviors as attributes of ASD, largely obscured clinical awareness of depression in youth with ASD. Pioneering work5,6 raised awareness of the syndrome of depression in ASD, and over the past decade, there has been a sharp increase in the number of research publications on this topic. The number of youth presenting with co-occurring ASD and depression often exceeds the clinical capacity to intervene in many (possibly the majority of) regions throughout North American, as well as globally. Stakeholders and funding agencies are swiftly coming to realize the importance and urgency of research on depression in ASD. Here we provide an overview of the prevalence, impact, presentation, and risk factors associated with co-occurring depression in children and adolescents with autism spectrum disorder (ASD). Clinical guidelines for the assessment and treatment of depression in the ASD population are also provided, with the caveat that these are emerging fields in which research is ongoing.
Prevalence and impact of depression in ASD
Establishing accurate and reliable prevalence rates of depression in ASD is challenging due to method variance (e.g., population-based versus convenience sample estimates; self-report versus caregiver report of depressive symptoms). However, the literature suggests that depression commonly co-occurs with ASD, with prevalence estimates that exceed estimates from the general population and comparable subpopulations, such as those with Intellectual Disability (ID).7 In samples of children and adolescents with ASD, current rates of depression generally fall in the range of 1–10% as diagnosed by parent report; these same studies tend to report elevated subsyndromal depression rates for an additional 10–15% of their samples.8,9 In a convenience sample of 1272 youth with ASD enrolled in the Autism Speaks Autism Treatment Network (ATN), parents reported depression diagnoses for 20.2% of adolescents aged 13–17.10 By approximate comparison, 8.4% of typically developing early adolescents (13–14 year olds) had major depressive disorder or dysthymia in a large U.S. representative study.11
A recent meta-analysis1 found that individuals with ASD are approximately four times more likely to experience depression compared to the general population when age ranges are pooled. Significantly elevated lifetime depression rates in ASD are associated with:
Increasing age (40.2% in adult samples vs 7.7% in samples < 18 years old)
Average to above average IQ (52.8% vs 12.2% when mean IQ is below average)
Structured interviews to assess depression (28.5% vs 6.7% for other assessment instruments)
Self-report (48.6% vs 14.4% via caregiver report)
Co-occurring depression has significant emotional, social, and behavioral consequences for individuals with ASD, including:
Exacerbated impairments associated with ASD (e.g., diminished social motivation and adaptive functioning)5,12,13
Diminished quality of life, and increased caregiver burden, medication and service use2,3
Heightened physical (e.g., gastrointestinal problems, seizures), emotional (e.g., anxiety), and behavioral (e.g., aggression, inattention) comorbidities10,14
Increased suicidality in a population with elevated rates of suicidal ideation and attempts compared to the general population15,16
Phenomenology of depression in ASD
Individuals with ASD exhibit traditional DSM-517 depressive symptoms (e.g. sadness, decreased pleasure in most activities, cognitive and somatic symptoms, and suicidality). As shown in Table 1, they may also exhibit more atypical presentations of depression 18,19,13 that focus on changes in engagement of special interests or other repetitive behaviors, and decreases in adaptive behavior skills and self-care. Within the heterogeneous autism spectrum, depression presentation likely depends on a variety of factors, several covered below in the section on vulnerability factors. While we lack prototypical benchmarks, we offer hypothetical “snapshots” of cases here:
Cognitively-able and socially-motivated youth with ASD may experience sadness, increased irritability, anhedonia, sleep disturbance, diminished appetite, self-deprecatory thoughts, coupled with an exacerbation of their ASD symptoms (e.g., more intense circumscribed interests and increased rigidity).
Youth with ASD and intellectual disability may present with increased crying, self-injury, aggression, perseveration, weight gain or loss, and toileting accidents.
Table 1.
Symptom presentation of depression in Autism Spectrum Disorder (ASD)
| Prototypical depression symptoms that commonly mark depression in ASD | Depression symptoms that may be more specific to ASD |
|---|---|
| • Depressed and/or irritable mood | • Increased irritability |
| • Loss of pleasure in previously enjoyed activities | • Changes in circumscribed interests (CI): |
| • Hopelessness and tearfulness | ■ Decreased pleasure in |
| • Negative beliefs about oneself | ■ Increased intensity |
| • Feelings of failure or worthlessness | ■ Change to darker/morbid content |
| • Constricted affect | • Increased repetitive behaviors |
| • (Increased) Social withdrawal | • Increased anxiety or insistence on sameness |
| • Change in appetite (increased or decreased) | • Increase in aggression or self-injury |
| • (Increased) Sleep problems | • Regressive behavior |
| • Poor concentration abilities | • Decline in self-care |
| • Lack of motivation | |
| • Thoughts about death or suicidal ideation |
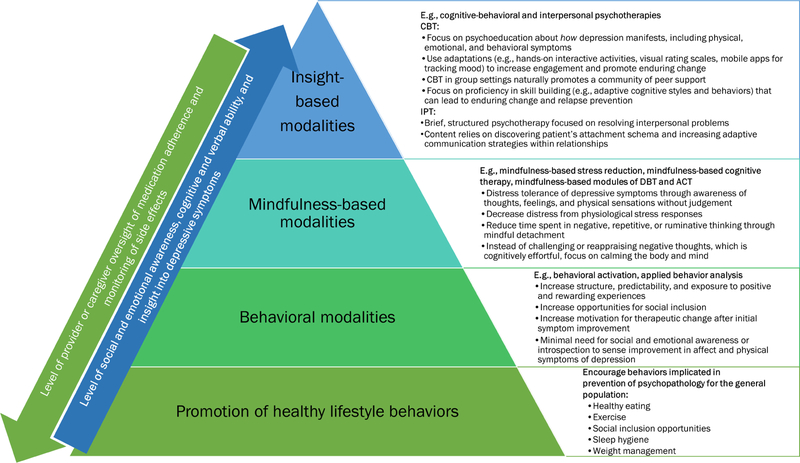
ASD and depression have overlapping features in several key areas (see Figure 1), most notably more constricted or flat affect and social withdrawal. Historically, this has led to diagnostic overshadowing, which has hindered awareness, characterization, and diagnostic precision of depression in ASD samples.
Figure 1.
Potential symptom overlap in Major Depressive Disorder and Autism Spectrum Disorder.
Little is known about the course of depression in children and adolescents with ASD, though preliminary data indicate that depression may persist longitudinally. Specifically, girls may show a steeper increase in depressive symptoms throughout adolescence, on par with typically developing girls, whereas boys with ASD may have elevated symptoms in school-age years (compared to typically developing children and to girls with ASD) that persist into adulthood.21 Depressive symptoms may also be more likely to persist in children who are experiencing bullying or greater social communication difficulties.22
Risk Factors
Researchers have posited several potential vulnerability factors for depression in ASD. Most of these come from independent studies of ASD and of typically developing depressed samples, with no direct comparison of the two clinical populations. Very few studies have employed longitudinal designs to capture the interplay between depressed mood and ASD symptoms over time. Below is a summary of data on potential candidate vulnerability factors associated with ASD and/or depression that may further our understanding of their co-occurrence.
Genetic/Neurobiological
Higher familial rates of affective disorders have been reported in family members of individuals with autism, even prior to having a child with a developmental disability.23
ASD, major depressive disorder, and other mental health conditions have been found to share common genetic variance.24 Serotonin and dopamine gene variants have been linked to more severe depressive symptoms in children with ASD.14
Atypical neural processes related to serotonin,25 microglia (indicating inflammatory processes),26 amygdala anatomy and function,27 and other functional or connectivity disruptions20 have been associated with both depression and ASD in independent samples.
Demographic and individual characteristics
Age: Evidence suggests that the risk for depression in ASD increases in adolescence,1,21,22 similar to patterns observed in the general population.11 Adult ASD depression rates are significantly higher still than child rates in ASD1 (several studies report lifetime depression rates ranging from 50% to 77% in adults with ASD28,29), which provides context for the importance of recognizing and treating this issue at younger ages.
Sex/gender: It is still unclear whether or not females with ASD are at a greater risk for depression than are males, in line with general population findings.30 Studies suggest that girls with ASD are at equal, greater, or less risk of developing depression than boys with ASD.14,20 With emerging data on more frequent non-binary interpretations of gender in youth with ASD, it will also be important to study how gender identity influences mood in this special population.31
Intellectual and verbal ability: Individuals with lower ASD severity, and average to above average IQ are at greater risk for depressive symptoms and suicidality1 This finding suggests that greater insight into their social difficulties might confer risk for depression, and/or depressive symptoms are more easily overlooked in individuals with lower verbal ability and intellectual disability.20
- Poor emotion regulation, and maladaptive coping strategies and/or thought patterns:
- Children, adolescents, and transition-age youth with ASD have been reported to exhibit higher rates of negative self-perceptions (e.g., guilt, shame, feelings of worthlessness), maladaptive coping strategies (e.g., repetitive negative thinking), and perceived stress and inability to cope, all of which are associated with depression in the general population.20
- Children with ASD who employ adaptive coping strategies (i.e., problem-solving, seeking social support) compared to those who engage in rumination and other maladaptive coping strategies appear to be at lower risk of depression.32
Other psychiatric comorbidities: Depression is associated with the presence of additional psychiatric comorbidities, such as anxiety, in children and adolescents with ASD.33
Social motivation: A desire to make meaningful connections paired with social communication impairments and negative social feedback in ASD could increase risk for depression.34,35 In adults with ASD as a proxy, greater social interest was associated with loneliness36, and loneliness in turn has been associated with higher rates of depression and suicidality in individuals with ASD.36–38
External variables that may function as vulnerability factors for depression in ASD
Socioeconomic status (SES): The limited research on SES and depression risk in ASD is inconclusive, with findings of no relationship or a significant positive relationship.39–41
Social support: Adults with ASD who perceived greater social support and acceptance reported lower depressive symptoms,42 whereas lower perceived social support and social satisfaction has been associated with elevated depressive symptoms.38 We do not know of equivalent data in children, but this suggested pathway may reasonably apply across the lifespan.
Life stress/Trauma: People with ASD tend to have higher rates of stressful life experiences including stigma, bullying, and poor prospects for independence, employment, and romantic fulfillment.43 Bullying and other stressful life experiences that were considered traumatic have been associated with depression in transition age youth and young adults with ASD in independent studies.22,44
Diagnostic evaluation of depression
Multi-method multi-informant approach
As diagnostic instruments for assessing depression in ASD have not yet been psychometrically validated, and given the diagnostic complexity due to symptom overlap, a multi-method, multi-informant approach is strongly recommended to assess symptoms across multiple contexts. This includes gathering information from the individual with ASD, parents, teachers, and other professionals. The psychiatric evaluation includes but it is not limited to assessing the following domains:
Current and past psychiatric history, onset and phenotype of depressive symptoms, typical and atypical presentations, teasing apart overlapping symptoms between depression and ASD, presence of other co-occurring conditions
Family history of affective disorders and other psychopathology
Developmental history and current level of functioning
Educational placement and supports
Psychosocial history which includes family functioning, trauma, and current stressful life events (e.g., recent traumatic experiences, bullying, changes in the home environment, social support)
Psychological and interpersonal functioning (e.g., social interests, friendships, self-awareness of disability, isolation, recreational activities, ego strengths, self-attitude)
Assessment of baseline behavior to determine recent behavioral changes and impact on functioning
Medical history to rule out other conditions that may be contributing to depression (e.g., anemia, hypothyroidism)
Suicidal risk assessment
Mental status examination
Special diagnostic considerations in ASD
While conducting these assessments, clinicians are encouraged to keep in mind several factors that are unique to the diagnostic assessment in the ASD population. These include the following:
Assessing symptom overlap between mood problems and autism (e.g., irritability, sleep and eating problems, inconsistent eye contact, constricted affect, and social isolation) (see Figure 1). Some symptoms may be part of the ASD, depression, or both. It is therefore important to carefully assess whether symptoms are new or are an exacerbation of baseline symptoms.
Determining the validity of self-report: Social-communication deficits and inability to recognize and label emotions (i.e., alexithymia)45 may prevent individuals on the spectrum from identifying and expressing emotional states, causing depressive symptoms to be overlooked by family and clinicians.
Using depression measures with caution: At this time, there is not enough evidence to determine if instruments designed for the general population may be valid to assess depressed mood in ASD.46
Assessing for atypical presentations of depression in ASD (see Table 1).
Evaluate for other comorbidities, particularly anxiety, gastrointestinal problems, seizures, and others known to co-occur with depression in ASD.14
Screening for suicidality at every visit: Individuals with ASD are at high risk for suicidal thoughts and behaviors.47 In addition to well-established suicidality assessment practices, it is important to gauge impulsivity and the repetitive nature of thinking about death or self-harm in patients with ASD.
Treatment of Depression in ASD
Development of evidence-based practices for treating depression in ASD is an ongoing and emerging area of research. Preliminary evidence indicates the effectiveness of adapted psychotherapeutic interventions from the general population to the ASD population. Medications for depression in typically developing youth can be also considered although data are lacking for their use in ASD.
Clinicians are encouraged to consider the following when making treatment decisions:
Use a multi-modal approach that tailors the intervention to the patient’s needs and interests (the authors refer readers to these detailed case studies20)
Employ a multi-disciplinary care team with coordination of services across relevant systems (i.e., home, social, educational, and vocational environments)
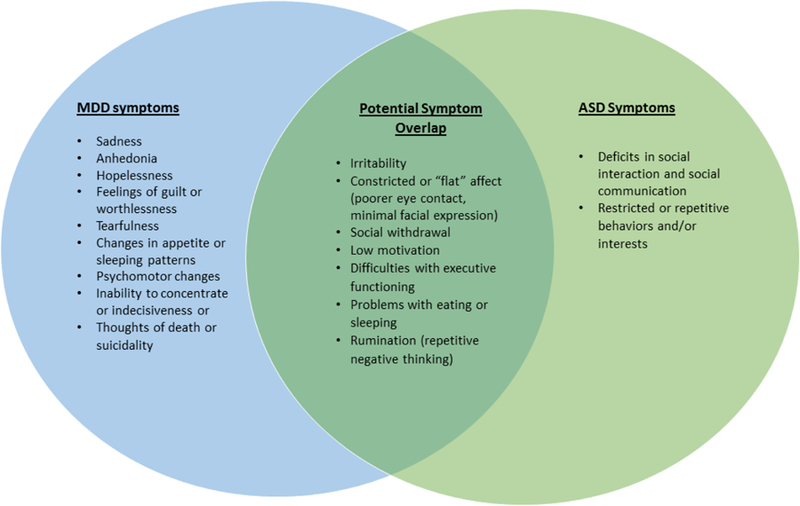
Coordinate treatment modality with patient’s level of cognitive functioning and social-emotional insight
Figure 2 presents therapeutic options with consideration of the patient’s cognitive and verbal abilities and social-emotional insight. As noted in the bottom band of Figure 2, all patients may benefit from healthy living behaviors that have been shown to ameliorate and prevent depressive symptoms for the general population. Approaches that rely less on meta-cognitive skills (e.g., behavioral activation) may be better initial choices for minimally verbal or intellectually disabled patients with depression. Finally, cognitive behavioral and interpersonal therapies may be more appropriate for individuals with requisite cognitive, social, and emotional insight. Importantly, these treatment options are not equivalently evidenced-based and must be considered of potential utility on a case-by-case basis.
Figure 2.
Considerations in potential treatments for depression in ASD. These treatment modalities are neither equivalently nor thoroughly evidenced-based at this point in time, particularly with regard to youth with ASD, and must be considered of potential utility on a case-by-case basis.
Psychotherapeutic treatments
Recent evidence suggests that cognitive behavioral therapy (CBT) can be effective in treating children and adolescents with comorbid ASD and depression.48,49 CBT approaches focus on helping clients identify and change common unhelpful thoughts and behaviors to encourage improvement in mood and overall functioning50. Modifications to CBT protocols for ASD populations (see Kerns et al.51) include incorporating or considering:
Psychoeducation to increase the individual’s understanding of the depression diagnosis as a descriptor for maladaptive emotional symptoms (e.g., prolonged sadness), physical symptoms (e.g., fatigue, aberrant sleep patterns), and social consequences (e.g., social withdrawal and isolation), which helps to identify core skills for symptom improvement
Hands-on interactive activities (e.g., role-playing, games)
Visual analogue scales (e.g., fear thermometer)
Technology (e.g., using phone applications to monitor daily mood)
Parent and family involvement
Group therapy to foster a community of social support and accountability, and to help the adolescent transition from family-centered support to peer support
The well-validated depression treatment protocol known as behavioral activation (BA)52 also may benefit youth on the spectrum. People with depression tend to isolate themselves and withdraw from pleasant activities. Using BA, individuals work on modifying behavior to i006Ecrease opportunities for rewarding and positive experiences, thus improving mood over time. With less emphasis on insight and cognitive work, BA might be considered a first-line treatment for patients with co-occurring intellectual disability and depression. Additionally, BA may be particularly effective in the following circumstances:
During transition periods (e.g., moving, changing schools, transitioning into adulthood), as it provides structured activities to promote goal setting, attainment of goals, and mitigates tendencies for social withdrawal and isolation.51
Patients with high levels of negative affect and minimal motivation for change. Increasing patient’s access to rewarding experiences facilitates initial improvement in affect to provide hope and readiness to engage in other psychosocial interventions (e.g., CBT).
Finally, some studies have provided support for mindfulness-based interventions in decreasing depressive symptoms in adults with ASD,53,54 so we await results of child research on this modality. This approach is defined as being aware of thoughts, feelings, physical sensations and experiences in the present moment, without judgement.55 Through meditation exercises (e.g., breathing, guided imagery, relaxation methods), patients learn to accept their feelings as a temporary state of mind, without over-analyzing the causes of their thoughts and emotions. Mindfulness interventions reduce maladaptive coping strategies, such as rumination, which is seen in ASD and in depressed individuals in the general population.56,57 Though research is limited, mindfulness remains a promising treatment for reducing depression in ASD.
Psychopharmacological treatments
Despite pharmacological evidence supporting the use of selective serotonin reuptake inhibitors (SSRIs) for depression in typically developing youth,58 evidence for their efficacy in children and adolescents with ASD are lacking. In fact, to date, there are no randomized controlled trials of antidepressant medications for the treatment of depression in children and adolescents with ASD. Yet, SSRIs are one of the most commonly prescribed class of medications in individuals on the spectrum.59 Existing studies examining the efficacy of SSRIs for other conditions (e.g., repetitive behaviors) in youth ASD indicate high rates of behavioral activation (e.g., impulsivity, aggression, disinhibition60; note that this is different from behavioral activation mentioned above as a therapeutic modality). Therefore, these medications should be prescribed cautiously for depression in youth with ASD with careful analysis of the risk/benefit ratio and close monitoring. Particular considerations when prescribing SSRIs include:
Obtaining consent from the parent and from the individual with ASD if possible
Eliciting a family history of bipolar disorder
Starting with low doses and titrating slowly
Routine monitoring of side effects making every effort to elicit information from both the caregiver and individual with ASD
Psychoeducation about medication side effects, with particular attention to providing parents with a clear plan about how to address behavioral activation and risk of mania should this occur
Identifying objective treatment targets that can be tracked over time
Establishing a timeline for assessing treatment efficacy, with a plan to taper and discontinue the medication if there is no benefit
Summary and Future directions
Depression is common in youth with ASD, particularly for adolescents and those individuals with average or greater cognitive ability. Depression is associated with several negative outcomes, including functional impairments beyond those associated with autism itself and significant burden on the family system. Accurate screening and assessment of depression in people with ASD is complicated by uncertain validity of self-report, alexithymia and poor insight common to ASD, and overlapping symptoms between ASD and depression. Research is needed to elucidate the presentation of depression in people with ASD across age, gender, and ability ranges, in order to refine assessment practices for this commonly co-occurring disorder. In addition, identifying specific pathways to mood problems in this population will be important to understanding risk factors and contributing mechanisms, potentially informing targets for more precise and effective intervention.
KEY POINTS.
Depression is a commonly co-occurring disorder in individuals with autism spectrum disorder (ASD), with lifetime rates approximately four times greater than the general population when pooled across age ranges (7.7% in child ASD samples; 40.2% in adults with ASD).1
Depression in ASD compromises adaptive functioning and quality of life, and is associated with increased risk of medication and service use, suicidality, other forms of self-injury, and caregiver burden.2–5
Assessment and diagnosis of depression in young people with ASD is challenging due to symptom overlap between the disorders and lack of validated psychometric instruments for assessing depressive symptoms in ASD.
Evidence for effective treatment of depression in youth with autism spectrum disorder is limited, but adapted psychotherapies show some promise.
SYNOPSIS.
Depression is both common and impactful in youth with autism spectrum disorder (ASD), and is swiftly growing in recognition as a major public health concern within the autism community. This article is intended to provide a brief overview of the prevalence, impact, presentation, and risk factors associated with co-occurring depression in children and adolescents with ASD. Clinical guidelines for the assessment and treatment of depression in the ASD population are offered in line with the small existing evidence base.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE STATEMENT
The authors have nothing to disclose.
Contributor Information
Florencia Pezzimenti, Department of Psychiatry and Behavioral Sciences, Vanderbilt University Medical Center, Nashville, TN, USA.
Gloria T. Han, Department of Psychology, Vanderbilt University, Nashville, TN, USA.
Roma A. Vasa, Department of Psychiatry and Behavioral Sciences, John Hopkins School of Medicine, Baltimore, MD, USA.
Katherine Gotham, Department of Psychiatry and Behavioral Sciences, Vanderbilt University Medical Center, Nashville, TN, USA.
References:
- 1.Hudson CC, Hall L, Harkness KL. Prevalence of Depressive Disorders in Individuals with Autism Spectrum Disorder: a Meta-Analysis. Journal of Abnormal Child Psychology March 2018. doi: 10.1007/s10802-018-0402-1 [DOI] [PubMed]
- 2.Cadman T, Eklund H, Howley D, et al. Caregiver Burden as People With Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder Transition into Adolescence and Adulthood in the United Kingdom. Journal of the American Academy of Child & Adolescent Psychiatry 2012;51(9):879–888. doi: 10.1016/j.jaac.2012.06.017 [DOI] [PubMed] [Google Scholar]
- 3.Joshi G, Wozniak J, Petty C, et al. Psychiatric Comorbidity and Functioning in a Clinically Referred Population of Adults with Autism Spectrum Disorders: A Comparative Study. Journal of Autism and Developmental Disorders 2013;43(6):1314–1325. doi: 10.1007/s10803-012-1679-5 [DOI] [PubMed] [Google Scholar]
- 4.Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, Baron-Cohen S. Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: a clinical cohort study. The Lancet Psychiatry 2014;1(2):142–147. doi: 10.1016/S2215-0366(14)70248-2 [DOI] [PubMed] [Google Scholar]
- 5.Ghaziuddin M, Ghaziuddin N, Greden J. Depression in persons with autism: implications for research and clinical care. J Autism Dev Disord 2002;32(4):299–306. [DOI] [PubMed] [Google Scholar]
- 6.Lainhart JE, Folstein SE. Affective disorders in people with autism: a review of published cases. J Autism Dev Disord 1994;24(5):587–601. [DOI] [PubMed] [Google Scholar]
- 7.Mayes SD, Calhoun SL, Murray MJ, Ahuja M, Smith LA. Anxiety, depression, and irritability in children with autism relative to other neuropsychiatric disorders and typical development. Research in Autism Spectrum Disorders 2011;5(1):474–485. doi: 10.1016/j.rasd.2010.06.012 [DOI] [Google Scholar]
- 8.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric Disorders in Children With Autism Spectrum Disorders: Prevalence, Comorbidity, and Associated Factors in a Population-Derived Sample. Journal of the American Academy of Child & Adolescent Psychiatry 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f [DOI] [PubMed] [Google Scholar]
- 9.Leyfer OT, Folstein SE, Bacalman S, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord 2006;36(7):849–861. doi: 10.1007/s10803-006-0123-0 [DOI] [PubMed] [Google Scholar]
- 10.Greenlee JL, Mosley AS, Shui AM, Veenstra-VanderWeele J, Gotham KO. Medical and Behavioral Correlates of Depression History in Children and Adolescents With Autism Spectrum Disorder. PEDIATRICS 2016;137(Supplement):S105–S114. doi: 10.1542/peds.2015-2851I [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merikangas KR, He J, Burstein M, et al. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magnuson KM, Constantino JN. Characterization of Depression in Children With Autism Spectrum Disorders Journal of Developmental & Behavioral Pediatrics 2011;32(4):332–340. doi: 10.1097/DBP.0b013e318213f56c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stewart ME, Barnard L, Pearson J, Hasan R, O’Brien G. Presentation of depression in autism and Asperger syndrome: A review. Autism 2006;10(1):103–116. doi: 10.1177/1362361306062013 [DOI] [PubMed] [Google Scholar]
- 14.Menezes M, Robinson L, Sanchez MJ, Cook B. Depression in Youth with Autism Spectrum Disorders: a Systematic Review of Studies Published Between 2012 and 2016. Review Journal of Autism and Developmental Disorders August 2018. doi: 10.1007/s40489-018-0146-4 [DOI]
- 15.Cassidy S, Rodgers J. Understanding and prevention of suicide in autism. Lancet Psychiatry 2017;4(6):e11. doi: 10.1016/S2215-0366(17)30162-1 [DOI] [PubMed] [Google Scholar]
- 16.Storch EA, Lewin AB, Collier AB, et al. A randomized controlled trial of cognitive-behavioral therapy versus treatment as usual for adolescents with autism spectrum disorders and comorbid anxiety: CBT for Adolescents with ASD and Anxiety. Depression and Anxiety 2015;32(3):174–181. doi: 10.1002/da.22332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diagnostic and Statistical Manual of Mental Disorders : DSM-5 Fifth edition Arlington, VA: : American Psychiatric Association, [2013]; 2013. https://search.library.wisc.edu/catalog/9910187853902121. [Google Scholar]
- 18.Charlot L, Deutsch CK, Albert A, Hunt A, Connor DF, McIlvane WJ. Mood and Anxiety Symptoms in Psychiatric Inpatients with Autism Spectrum Disorder and Depression. Journal of Mental Health Research in Intellectual Disabilities 2008;1(4):238–253. doi: 10.1080/19315860802313947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chandrasekhar T, Sikich L. Challenges in the diagnosis and treatment of depression in autism spectrum disorders across the lifespan. Dialogues Clin Neurosci 2015;17(2):219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gotham KO, Pezzimenti F, Eydt-Beebe M, Han G, Herrington C. The Oxford Handbook of Psychiatric Comorbidity in Autism Oxford University Press; In print. [Google Scholar]
- 21.Gotham K, Brunwasser SM, Lord C. Depressive and Anxiety Symptom Trajectories From School Age Through Young Adulthood in Samples With Autism Spectrum Disorder and Developmental Delay. Journal of the American Academy of Child & Adolescent Psychiatry 2015;54(5):369–376. 10.1016/j.jaac.2015.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rai D, Culpin I, Heuvelman H, et al. Association of autistic traits with depression from childhood to age 18 years. JAMA Psychiatry 2018;75(8):835–843. doi: 10.1001/jamapsychiatry.2018.1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bolton PF, Pickles A, Murphy M, Rutter M. Autism, affective and other psychiatric disorders: patterns of familial aggregation. Psychol Med 1998;28(2):385–395. [DOI] [PubMed] [Google Scholar]
- 24.Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. The Lancet 2013;381(9875):1371–1379. doi: 10.1016/S0140-6736(12)62129-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muller CL, Anacker AMJ, Veenstra-VanderWeele J. The serotonin system in autism spectrum disorder: From biomarker to animal models. Neuroscience 2016;321:24–41. doi: 10.1016/j.neuroscience.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frick LR, Williams K, Pittenger C. Microglial Dysregulation in Psychiatric Disease. Clinical and Developmental Immunology 2013;2013:1–10. doi: 10.1155/2013/608654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dichter GS, Damiano CA, Allen JA. Reward circuitry dysfunction in psychiatric and neurodevelopmental disorders and genetic syndromes: animal models and clinical findings. Journal of Neurodevelopmental Disorders 2012;4(1). doi: 10.1186/1866-1955-4-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lugnegård T, Hallerbäck MU, Gillberg C. Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Research in Developmental Disabilities 2011;32(5):1910–1917. doi: 10.1016/j.ridd.2011.03.025 [DOI] [PubMed] [Google Scholar]
- 29.Gotham K, Siegle G, Han G, Crist R, Simon D, Bodfish J. Pupil response to social-emotional materials is associated with rumination and depressive symptoms in adults with autism spectrum disorder. PLOS One 2018:In press. [DOI] [PMC free article] [PubMed]
- 30.Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology 1998;107(1):128–140. doi: 10.1037/0021-843X.107.1.128 [DOI] [PubMed] [Google Scholar]
- 31.van Schalkwyk GI, Klingensmith K, Volkmar FR. Gender identity and autism spectrum disorders. Yale J Biol Med 2015;88(1):81–83. [PMC free article] [PubMed] [Google Scholar]
- 32.Rieffe C, De Bruine M, De Rooij M, Stockmann L. Approach and avoidant emotion regulation prevent depressive symptoms in children with an Autism Spectrum Disorder. Int J Dev Neurosci 2014;39:37–43. doi: 10.1016/j.ijdevneu.2014.06.003 [DOI] [PubMed] [Google Scholar]
- 33.Vasa RA, Kalb L, Mazurek M, et al. Age-related differences in the prevalence and correlates of anxiety in youth with autism spectrum disorders. Research in Autism Spectrum Disorders 2013;7(11):1358–1369. doi: 10.1016/j.rasd.2013.07.005 [DOI] [Google Scholar]
- 34.Meyer JA, Mundy PC, Van Hecke AV, Durocher JS. Social attribution processes and comorbid psychiatric symptoms in children with Asperger syndrome. Autism 2006;10(4):383–402. doi: 10.1177/1362361306064435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sterling L, Dawson G, Estes A, Greenson J. Characteristics Associated with Presence of Depressive Symptoms in Adults with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders 2008;38(6):1011–1018. doi: 10.1007/s10803-007-0477-y [DOI] [PubMed] [Google Scholar]
- 36.Han GT, Tomarken AJ, Gotham KO. Social and non-social reward moderate the relation between autism symptoms and loneliness in adults with ASD, depression, and controls. Manuscript submitted for publication 2018. [DOI] [PMC free article] [PubMed]
- 37.Mazurek MO. Loneliness, friendship, and well-being in adults with autism spectrum disorders. Autism 2014;18(3):223–232. doi: 10.1177/1362361312474121 [DOI] [PubMed] [Google Scholar]
- 38.Hedley D, Uljarević M, Foley K-R, Richdale A, Trollor J. Risk and protective factors underlying depression and suicidal ideation in Autism Spectrum Disorder. Depression and Anxiety 2018;35(7):648–657. doi: 10.1002/da.22759 [DOI] [PubMed] [Google Scholar]
- 39.Gray K, Keating C, Taffe J, Brereton A, Einfeld S, Tonge B. Trajectory of Behavior and Emotional Problems in Autism. American Journal on Intellectual and Developmental Disabilities 2012;117(2):121–133. doi: 10.1352/1944-7588-117-2.121 [DOI] [PubMed] [Google Scholar]
- 40.Midouhas E, Yogaratnam A, Flouri E, Charman T. Psychopathology Trajectories of Children With Autism Spectrum Disorder: The Role of Family Poverty and Parenting. Journal of the American Academy of Child & Adolescent Psychiatry 2013;52(10):1057–1065. 10.1016/j.jaac.2013.07.011 [DOI] [PubMed] [Google Scholar]
- 41.Taylor JL, Seltzer MM. Changes in the Autism Behavioral Phenotype During the Transition to Adulthood. Journal of Autism and Developmental Disorders 2010;40(12):1431–1446. doi: 10.1007/s10803-010-1005-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cage E, Di Monaco J, Newell V. Experiences of Autism Acceptance and Mental Health in Autistic Adults. Journal of Autism and Developmental Disorders 2018;48(2):473–484. doi: 10.1007/s10803-017-3342-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Henninger NA, Taylor JL. Outcomes in adults with autism spectrum disorders: a historical perspective. Autism 2013;17(1):103–116. doi: 10.1177/1362361312441266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taylor JL, Gotham KO. Cumulative life events, traumatic experiences, and psychiatric symptomatology in transition-aged youth with autism spectrum disorder. Journal of Neurodevelopmental Disorders 2016;8(1). doi: 10.1186/s11689-016-9160-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bird G, Cook R. Mixed emotions: the contribution of alexithymia to the emotional symptoms of autism. Translational Psychiatry 2013;3(7):e285. doi: 10.1038/tp.2013.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cassidy SA, Bradley L, Bowen E, Wigham S, Rodgers J. Measurement properties of tools used to assess depression in adults with and without autism spectrum conditions: A systematic review. Autism Res 2018;11(5):738–754. doi: 10.1002/aur.1922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Horowitz LM, Thurm A, Farmer C, et al. Talking About Death or Suicide: Prevalence and Clinical Correlates in Youth with Autism Spectrum Disorder in the Psychiatric Inpatient Setting. J Autism Dev Disord 2018;48(11):3702–3710. doi: 10.1007/s10803-017-3180-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Keefer A, White SW, Vasa RA, Reaven J. Psychosocial interventions for internalizing disorders in youth and adults with ASD. Int Rev Psychiatry 2018;30(1):62–77. doi: 10.1080/09540261.2018.1432575 [DOI] [PubMed] [Google Scholar]
- 49.Santomauro D, Sheffield J, Sofronoff K. Depression in Adolescents with ASD: A Pilot RCT of a Group Intervention. Journal of Autism and Developmental Disorders 2016;46(2):572–588. doi: 10.1007/s10803-015-2605-4 [DOI] [PubMed] [Google Scholar]
- 50.Beck AT, Rush AJ, eds. Cognitive Therapy of Depression 13 print. New York: Guilford Press; 1979. [Google Scholar]
- 51.Kerns CM, Roux AM, Connell JE, Shattuck PT. Adapting Cognitive Behavioral Techniques to Address Anxiety and Depression in Cognitively Able Emerging Adults on the Autism Spectrum. Cognitive and Behavioral Practice 2016;23(3):329–340. doi: 10.1016/j.cbpra.2016.06.002 [DOI] [Google Scholar]
- 52.Jacobson NS, Martell CR, Dimidjian S. Behavioral Activation Treatment for Depression: Returning to Contextual Roots. Clinical Psychology: Science and Practice 2006;8(3):255–270. doi: 10.1093/clipsy.8.3.255 [DOI] [Google Scholar]
- 53.Spek AA, van Ham NC, Nyklíček I. Mindfulness-based therapy in adults with an autism spectrum disorder: a randomized controlled trial. Res Dev Disabil 2013;34(1):246–253. doi: 10.1016/j.ridd.2012.08.009 [DOI] [PubMed] [Google Scholar]
- 54.Sizoo BB, Kuiper E. Cognitive behavioural therapy and mindfulness based stress reduction may be equally effective in reducing anxiety and depression in adults with autism spectrum disorders. Res Dev Disabil 2017;64:47–55. doi: 10.1016/j.ridd.2017.03.004 [DOI] [PubMed] [Google Scholar]
- 55.Kabat-Zinn J Mindfulness-Based Interventions in Context: Past, Present, and Future. Clinical Psychology: Science and Practice 2003;10:144–156. doi: 10.1093/clipsy.bpg016 [DOI] [Google Scholar]
- 56.Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy 2004;35(4):639–665. doi: 10.1016/S0005-7894(04)80013-3 [DOI] [PubMed] [Google Scholar]
- 57.Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med 2007;33(1):11–21. doi: 10.1207/s15324796abm3301_2 [DOI] [PubMed] [Google Scholar]
- 58.March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA 2004;292(7):807–820. doi: 10.1001/jama.292.7.807 [DOI] [PubMed] [Google Scholar]
- 59.Houghton R, Ong RC, Bolognani F. Psychiatric comorbidities and use of psychotropic medications in people with autism spectrum disorder in the United States. Autism Res 2017;10(12):2037–2047. doi: 10.1002/aur.1848 [DOI] [PubMed] [Google Scholar]
- 60.King BH, Hollander E, Sikich L, et al. Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior: citalopram ineffective in children with autism. Arch Gen Psychiatry 2009;66(6):583–590. doi: 10.1001/archgenpsychiatry.2009.30 [DOI] [PMC free article] [PubMed] [Google Scholar]