Abstract
Introduction
Learners have repeatedly expressed a desire for more structured training in communicating with families, especially when sharing life-altering information and breaking bad news. Concurrently, parents have indicated that pediatricians could conduct difficult conversations with greater skill. Based on local needs assessments and available pediatric literature, this guide presents didactic materials and a workshop-style, case-based, longitudinal approach for teaching communication skills to learners in pediatrics.
Methods
The customizable guide can be implemented as a 1-hour didactic presentation, a 1- to 3-hour workshop, or an integrated longitudinal curriculum. Unlike other available resources for breaking bad news, this guide is specifically designed for pediatrics and uses evidence-based communication guidelines developed for pediatric settings. The guidelines are modified from the adult-centered SPIKES (setting, perception, involvement, knowledge, emotions, summary) approach. The material was created by clinicians, educators, and parents of pediatric patients. In addition to video-based didactic materials and pediatric case scenarios, the guide includes materials for assessment, evaluation, and personal reflection.
Results
The modified SPIKES approach and didactic portion of this resource were validated as an initial training tool, yielding significant improvements in self-efficacy of pediatric providers and learners. Evaluations of the role-playing components provided by pediatric residents and fellows have been positive for the format and value of the learning experience. Participants reported a particular benefit from the inclusion of parent perspectives.
Discussion
Without a formal communication curriculum, learners must rely on chance observation of life-altering conversations during clinical rotations. This guide provides pediatric educators with structured, evidence-based materials to teach advanced communication skills.
Keywords: Communication, Pediatrics, Breaking Bad News, Pediatric Hematology/Oncology, Sharing Life-Altering Information
Educational Objectives
By the end of this resource, learners will be able to:
-
1.
Apply a validated, structured approach for sharing life-altering information with pediatric patients and their families.
-
2.
Develop interpersonal skills through self-, peer, parent, and facilitator assessments.
-
3.
Evaluate personal communication skills in the context of specific Accreditation Council for Graduate Medical Education pediatric subcompetencies and milestones.
Introduction
Parents of pediatric patients repeatedly ask for clearer and more sensitive family-centered sharing of life-altering information (i.e., breaking bad news).1–3 Unfortunately, formal training in communication is often limited to brief didactic sessions, and providers often report that their only training in this skill is largely observational.4–6 Parents have also indicated a desire for greater interactivity with their children's doctors, emphasizing the importance of patient- and family-centered care in communications.1,2,6
Research focusing on practitioners in primary care and pediatric subspecialties has revealed a lack of training and comfort in conducting these discussions with patients and families.4 In pediatric oncology, these conversations are a crucial component of daily practice. The few published curricula for teaching these skills are provided in the context of pediatric oncology or palliative care. Despite the knowledge that strong advanced communication training is essential,5 there remains a need for more guidance on this topic among trainees and established providers within general pediatrics and the pediatric subspecialties.3,6 A recent study suggests that pediatric residents benefit from practicing skills in sharing life-altering information with bereaved parents,7 indicating the value of incorporating parent perspectives in training communication skills.
This resource guide is based on initial work at the University of Wisconsin–Madison (UW) to develop pediatric-focused guidelines for sharing life-altering information in all pediatric care settings based on the SPIKES (setting, perception, invitation, knowledge, emotions, summary) guidelines validated in adult oncology.8 The modifications of SPIKES (including changing invitation to involvement) for pediatric practice were made in order to refocus on avoiding paternalism and emphasizing patient- and family-centered care.9 The initial guidelines were taught as a simple 1-hour didactic session, and this didactic material is currently being used as required initial exposure to this topic for pediatric trainees at UW. This approach has been validated for improving provider self-efficacy.9 Subsequently, a hands-on experience derived from this work was offered as a 90-minute workshop at the American Society of Pediatric Hematology/Oncology (ASPHO) annual meeting on May 8, 2015. Approximately 60 attendees, primarily fellows in pediatric hematology/oncology, participated, along with some advanced practice providers and faculty. Most recently, the Children's Hospital of San Antonio (CHofSA) has adopted a full-year pediatric resident curriculum for sharing life-altering information.
The materials in this guide offer educators a structured approach for teaching how to share life-altering information in pediatric settings. Exercises are customizable for learners of all levels, including medical students, pediatric residents, and pediatric subspecialty fellows. These exercises provide hands-on experience sharing life-altering information using evidence-based materials.
Methods
The materials in this resource guide may be used in a longitudinal trainee curriculum or à la carte for singular educational experiences. Learners receive didactic instruction based on the available literature and using video prepared by parents of pediatric patients. They critique video performances of the communication skills and then perform these skills in facilitated small-group role-play sessions. The longitudinal curriculum employs periodic 360o assessments, based on the Accreditation Council for Graduate Medical Education (ACGME) milestones, to provide more practice and feedback to learners regarding their skills.
Based on the data from the UW self-efficacy study,9 the debrief and evaluations from the ASPHO meeting, and the evaluations obtained during the implementation of the curriculum at CHofSA, we suggest the following options for implementation. These suggestions may be customized for your learner group and the time frame over which you plan to utilize the resource guide.
Key Roles
Effective presentation and facilitated role-play require identifying and preparing a faculty facilitator and a role-play parent/respondent.
There should be one facilitator per learner group in the workshop experiences described below. Group sizes can range from three to 10 learners. It is also possible to have one facilitator working with two groups during role-play. Faculty facilitators should have adequate experience in sharing life-altering information in pediatrics and an interest in teaching these communication skills.
The facilitated role-play instructions (Appendix A) provide an overview of facilitated role-play and suggestions for leading a learner group through the exercise. Faculty facilitators may benefit from reviewing the didactic slide set (Appendix B), the pocket card (Appendix C), and the key points handout (Appendix D) prior to leading a learner group.
For the role-play respondent, consider soliciting volunteer parents from the patient-family advisory board or parent advocate group, if your facility has them. Alternatively, standardized patients or other care team members (e.g., child life specialists) can be trained as the respondents in the role-play. Our learners gave universally positive responses to working with parents of children with oncologic diseases as respondents in our role-play workshop at ASPHO and in the CHofSA residency curriculum. These individuals offer the perspective of parents who have experienced difficult conversations with their pediatricians.
We do not recommend having learners serve as the respondents in role-play. Feedback from residents has suggested that role-playing with people they know detracts from their ability to take the exercise seriously.
The case scenarios (Appendices E & F) include separate instructions for the respondent. These instructions should be provided before the role-play. The respondent's role is generally to start from the emotional state indicated in the scenario instructions and then proceed to exhibit appropriate and genuine responses to the physician's handling of the interview.
Respondents may benefit from reviewing the pocket card and the key points handout prior to working with a learner group.
Didactic Experience
Allow approximately 1 hour for this exercise (longer if group discussion is encouraged during or after the presentation). The purpose of the didactic presentation is to familiarize learners with the SPIKES approach to sharing life-altering information in pediatrics and to share parent perspective video clips on some of the guidelines (see the Table).
The facilitator is encouraged to review and modify the slide set as needed. The facilitator should then present the didactic slides to the learner group. Please note that the participants in all video segments have provided consent for the videos to be used for educational purposes.
If a flipped classroom approach is to be used, learners should be assigned to review the didactic presentation slide set prior to a workshop-based experience.
It is recommended that learners also be provided with handouts including the pocket card and key points. Individual learners may use the learner guide (Appendix G) or groups may choose to use the facilitator guide (Appendix H) to help with retention and discussion of the topics raised in the didactic presentation. Please note that it is further recommended that structured opportunities to practice these skills be offered to learners (see workshop and video experiences below).
Workshop-Based Experience
Allow 1.5 to 3.5 hours for this exercise. Learners should be provided with the handouts, including the pocket card and key points. For the first 15 minutes, the facilitator should provide a didactic review of the pediatric SPIKES guidelines using the brief slide set (Appendix I) and the pocket card. The large group then spends 15 minutes viewing and critiquing two sample case scenario videos (presented at the end of the slide file) emphasizing stronger and weaker examples of communication using SPIKES.
Table. Summary of SPIKES Approach and Illustrative Parent Video Perspectives Contained in the Didactic Slide Set.
| SPIKES Component | Action | Parent Video |
|---|---|---|
| Setting |
|
Slides 16–17 |
| Perception |
|
Slide 19 |
| Involvement |
|
Slide 21 |
| Knowledge |
|
N/Aa |
| Emotion/ empathy |
|
Slide 25 |
| Summary/ strategy/self-reflection |
|
Slide 27 |
Parents in the video project did not express critique of this component of SPIKES.
For general pediatrics learners (e.g., medical students and residents), get into small groups of four to six learners (plus a faculty facilitator and parent/respondent), and spend 20 to 30 minutes practicing facilitated role-play of the first case scenario. The 10 detailed scenarios provided (Appendix E) are based on real patient cases with sufficient details altered to protect patient confidentiality. The first page of the file contains a list of the cases as well as the emotional responses and clinical challenges likely to be encountered by the learner. The cases generally increase in complexity and emotional difficulty in the order presented. Each scenario includes separate instructions for the physician (i.e., the learner) and for the parent/respondent; provide only the physician instructions to the learners. Add 20- to 30-minute increments for each case scenario to be practiced in the small groups. Depending on available time, we recommend two to four scenarios.
For pediatric hematology/oncology learners (e.g., fellows), review and distribute the respondent instructions pages from the oncology scenarios document (Appendix F) to the respondents in your role-play small groups. Distribute the physician instructions page from this document to all learners in the group. Get into small groups of four to six learners, plus a faculty facilitator and parent/respondent. Spend 15 minutes following the group discussion/warm-up section of the oncology scenario, which extends the story of the patient illustrated in the sample videos from the slides. The case file includes separate handouts for the physician (i.e., the learner) and for the facilitator and parent/respondent. Next, spend 20 to 30 minutes facilitating the first part of the oncology role-play scenario (Role-play #1). Follow this up with 20 to 30 minutes facilitating the second part (Role-play #2).
For learners in other pediatric subspecialties, facilitators are encouraged to prepare their own detailed scenario following the template laid out by the oncology scenario; alternatively, they can use the general pediatrics scenarios as a starting point. As an option, 20 to 30 minutes can be spent with a panel discussion with parents (if patients’ parents are used as the role-play respondents). The focus of the discussion should be on allowing learners to ask parents about their personal experiences and perceptions of physician communication regarding their own child's diagnosis. Residents in our training program considered this portion of the workshop experience very valuable. Participants at the ASPHO workshop were not offered this experience, and many requested it in the postworkshop evaluation. For the final 20 to 30 minutes, the large group should come back together to debrief on the role-play experiences. Evaluate whether pediatric SPIKES was used effectively during role-play. Focus on lessons learned, challenges, and barriers to effective communication. Explore different approaches attempted by different learners in the groups.
Individual Role-Play With Video Self-Assessment Experience
Allow 10 to 20 minutes per learner per scenario for this exercise. Learners may participate without formal training (i.e., for baseline assessment) or after participating in the didactic and/or workshop experiences above.
Start by identifying a video-enabled space in which to record the encounters for later review and assessment. Provide the learner with a physician case scenario description (Appendix E) and the role-play respondent with the corresponding parent case scenario description.
Instruct the learner to role-play the scenario of the clinical encounter where information is shared. Assume that the initial intake, history, and physical examination have already been completed. Record the encounter for later review.
After the encounter (immediately or at a later date), the learner will review the video encounter, take notes on the communication skills exhibited, and have a one-on-one debrief with a facilitator who has also reviewed the video. For a recommended assessment tool, see the Learner Assessment section below.
Building a Longitudinal Curriculum
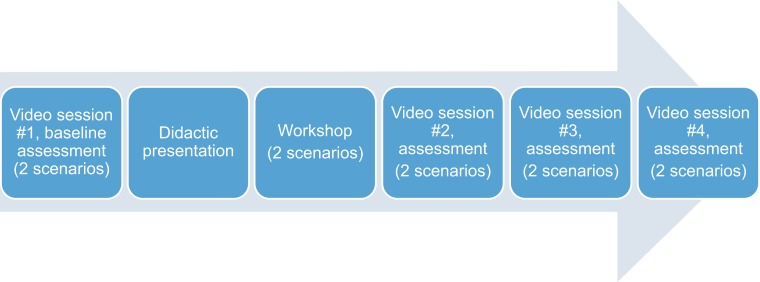
Using the three experiences described above, our yearlong intern curriculum consists of a baseline video role-play and assessment (two case scenarios), followed by a 1-hour didactic presentation and a 3-hour workshop experience with facilitated role-play using parent respondents (two case scenarios). Additionally, three video role-play and assessment encounters (each with two case scenarios) are conducted approximately 2 to 4 months apart throughout the academic year (see the Figure).
Figure. Sample longitudinal curriculum design (occurs over 1 year).
Learner Assessment
For self-reflection, provide learners with the reflective exercise worksheet (Appendix J). This asks them to describe a single personal experience in sharing life-altering information during their clinical encounters and to reflect on their skill in communication. Our approach has been to give residents 6 weeks to complete the activity, collect the worksheets, and then reconvene the full group to discuss collective experiences and lessons learned.
For self-assessment, learners are encouraged to use the self-assessment (Appendix G) to gauge their learning. The facilitator guide (Appendix H) contains sample discussion questions to encourage groups to consider the topics in the resource guide together.
ACGME Communication Milestones
The 21 pediatric subcompetencies and associated learning milestones prepared by the ACGME and the American Board of Pediatrics include three subcompetencies that pertain to communication skills with patients:
-
•
Professionalism 1: Humanism, compassion, integrity, and respect for others; based on the characteristics of an empathetic practitioner.
-
•
Interpersonal Communication Skills 1: Communicate effectively with patients, families, and the public, as appropriate, across a broad range of socioeconomic and cultural backgrounds.
-
•
Interpersonal Communication Skills 2: Demonstrate the insight and understanding into emotion and human response to emotion that allow one to appropriately develop and manage human interactions.10
These were originally developed for longitudinal assessment of learner progress during training. Our residents perform a self-assessment of their longitudinal performance of these subcompetencies every 6 months. Additionally, we use the three communication-related milestones for single encounter assessment after each of the four video sessions. We have developed a list of key verbal and nonverbal behaviors representing different milestones for each subcompetency that might guide assessment (Appendix K).
For milestone self-assessment, residents should privately review their own video encounters, critique their use of communication skills, and rate their milestone level on the three subcompetencies. They then debrief with a faculty member who has also reviewed the video encounters.
For a 360o assessment, faculty members and parent volunteers are recruited to review the video encounters and rate the residents on the three subcompetencies. These assessments are then shared individually with residents, and any discrepancies between the self-assessment and 360o assessment are explored.
Evaluation of the Curriculum
After each didactic or workshop, participants should be given an opportunity to evaluate the content and the speaker (Appendix L). During their four personalized video session debriefs, residents are encouraged to give feedback on the curriculum as a whole. This in-person debrief allows identification of opportunities to improve the timing and content of remaining components of the curriculum. Therefore, the evaluation process by learners is ongoing throughout the year.
Questions regarding effective communication skills are included in every rotation block evaluation completed by attending faculty. The residency or fellowship core competency committee then incorporates the data from these evaluations every 6 months to track progress of learners in communication subcompetencies.10 New trends in effective communication may necessitate future changes in this curriculum.
Results
The didactic presentation, using parent video to illustrate the steps of SPIKES, has been shared with multiple audiences ranging in size from groups of 10 learners to grand rounds environments of 70 to 80 attendees. Participants have included medical students; residents in pediatrics, emergency medicine, and surgery; fellows in pediatrics; and faculty groups. Presentations to subspecialties have included teams in emergency medicine, neonatology, behavioral pediatrics, genetics, hematology/oncology, general surgery, and cardiology. This presentation has also been shared with multidisciplinary teams including nurses and nursing students, physical and occupational therapists, emergency medical technicians, child life specialists, and chaplains. Evaluation data from these groups revealed a significant improvement in self-efficacy among participants on four primary learning objectives related to sharing life-altering information in pediatrics. These results were used to validate the modified SPIKES approach, which has subsequently been published.9
The workshop component of this resource guide was developed by faculty in pediatric hematology/oncology, hospital medicine, and palliative care from four children's hospitals. Workshop participants have included residents from two categorical pediatric residency programs, hematology/oncology fellows, and faculty. Evaluations of these workshops revealed that the addition of parents as respondents in role-play improved the quality of role-play and the satisfaction of learners. Evaluations also highly rated the discussion of parental experiences with physician communication as a way to add genuine personal stories to the experience. The ASPHO workshop evaluation responses, submitted by 24 participants, averaged from 4.70 to 4.82 on a 5-point Likert scale for all 19 items surveyed. The results included a mean of 4.79 out of 5 for “I can apply this new information to my practice” and a mean of 4.75 out of 5 for “I have opportunities to improve my professional skills.”
The yearlong longitudinal curriculum using the materials in this resource guide has been implemented at the CHofSA-Baylor College of Medicine residency program with the inaugural resident class. Evaluation of the curriculum by the residents has been positive. Residents have shown initial improvement in performance of ACGME communication subcompetencies10 during the intern year, both on individual rotation evaluations and on the summative 6-month evaluation by the clinical competency committee. The utility of the 360o milestone assessments for individual video role-play encounters is the subject of a funded research study. Residents in this curriculum have also shown subjective improvements in their confidence, ability to exhibit empathy, and attention to nonverbal details of communication as they have progressed through the curriculum. This observation has been made by the residents during video role-play feedback and has been corroborated by faculty observation of the encounters.
Participant comments on this resource identified several themes. Participants considered the topic timely and thought the structure and format of materials were appropriate. Participants thought including parent perspectives was informative and powerful; nearly every respondent included this sentiment. Also, there was an expressed desire to implement this resource in their home program.
The pediatric guidelines, key points, and pocket card summary were all considered useful. The participants also thought developing compassion and empathy was important and practicing communication skills was valuable. Additionally, the multidisciplinary approach was considered helpful.
Participants also identified several barriers and areas for improvement. Providers need more time to spend with families during these conversations. Providers need more practice and experience. During the workshop, facilitators should consider limiting how long each trainee spends with a respondent. More time talking to the parent panel during the workshop would be valuable.
Discussion
This resource guide of evidence-based, pediatric-centered educational materials for sharing life-altering information is the result of years of development and several plan, do, study, act (PDSA) cycles at two institutions, UW and CHofSA. Creation of these materials began as a quality-improvement initiative at UW as a result of feedback from parents of ill children that their initial diagnosis discussions could have been conducted more skillfully. Consequently, a needs assessment was conducted with medical students, pediatric residents, and teaching faculty. This revealed a lack of comfort and structure for approaching this topic among all stakeholders, and we determined that more formal teaching could be beneficial. Review of the literature revealed that while there are multiple proposed models for structuring the bad-news interview, none have been specifically designed for, or validated in, pediatric settings.6 The literature review also revealed multiple survey-based studies of parents who expressed a desire for more skillful sharing of life-altering information by their physicians.
Based on this initial needs assessment and literature review, the didactic materials in this resource guide were developed by a multidisciplinary team of pediatricians, pediatric subspecialists, advanced practice providers, nurses, nurse educators, social workers, child life specialists, chaplains, health psychologists, and parent advocates.9 The didactics are based on the SPIKES guidelines first validated in adult oncology,8 with evidence-based modifications to focus on pediatrics and family-centered care. The impact of the didactic presentation was evaluated through participant surveys and demonstrated an improvement in pediatric provider self-efficacy.9 This material has subsequently been presented at multiple institutions, with modifications after each presentation based on participant feedback.
Subsequent data suggest that a learner's gains from a single didactic experience in sharing life-altering information will wane over time, likely within 9 months of the training.11 The literature, as well as our own data, indicates that sharing life-altering information requires hands-on experiences for longitudinal retention and the development of skills. Prior to presenting this material as a workshop at the ASPHO meeting, another needs assessment was conducted by surveying participants in the weeks prior to the meeting. The qualitative responses garnered from this survey revealed the following needs:
-
•
Allowing families to maintain hope in the face of life-altering information.
-
•
Sharing information compassionately.
-
•
Maintaining a therapeutic alliance when medical news is bad.
-
•
Working with adolescent and young adult patients and their parents.
-
•
Learning how to teach these skills effectively.
Consequently, the workshop component of this resource guide was developed to meet the needs identified in this assessment. Responses to the workshop as presented to resident groups and at ASPHO have been overwhelmingly positive. This is consistent with the recent finding that including bereaved parents in communication training for pediatric residents can improve resident confidence in conducting difficult conversations.7
Results of our evaluations and review of the relevant literature continue to indicate that a longitudinal curriculum on sharing life-altering information is most effective in improving pediatrician–family communication. Consequently, we have implemented a longitudinal communication curriculum at CHofSA based on the materials developed from the initial PDSA cycles at UW and for ASPHO. This longitudinal curriculum at CHofSA provides structured opportunities for residents to practice difficult conversations, review their performance, and receive individualized feedback on their role-play encounters from faculty and parent reviewers. The individual scenario cases, which are based on authentic patient cases, have been rigorously reviewed and tested. The cases are designed to illustrate themes identified in the workshop needs assessment, such as working with adolescent patients, forming therapeutic alliances under difficult circumstances, and exhibiting compassion in the face of multiple different emotional responses.
Throughout this extensive curriculum development process, several key lessons have been learned. All stakeholders in pediatric care from physicians to allied health professionals to parents want providers to be more effective communicators, particularly in difficult conversations. However, these advanced skills are not consistently taught in a formal manner. Didactic materials developed by a multidisciplinary team including parent advocates have been found to be extremely valuable by all participants, particularly learners. Learners have repeatedly welcomed parent participation in this curriculum. One surprising lesson learned is that implementation of parent participation at local institutions has been much easier than anticipated as parents are willing and excited to help teach learners. Another important lesson is that learners often find role-playing to be challenging; however, learners consistently report in follow-up feedback sessions that they find these sessions to be very helpful and appreciate practicing communication skills prior to using these skills in real-life situations.
The next step for the continued development of this communication curriculum is applying ACGME subcompetencies/milestones to this curriculum and training senior residents and fellows to serve as facilitators. ACGME subcompetencies and milestones are key components in the development of competency-based education and in the current accreditation system for graduate medical education in the United States. The application of ACGME subcompetencies and milestones to this longitudinal communication curriculum is currently being studied. We are particularly interested in comparing resident, faculty, and parent longitudinal perceptions of resident communication using three ACGME subcompetencies.
Our second next step in the development of this curriculum is to incorporate more experienced learners, senior residents, and fellows in the education of interns. Over the next 2 years, we will train our senior residents to serve with faculty as facilitators throughout the curriculum. The ability to critique and educate their colleagues is expected to improve our senior residents’ leadership, teaching, and communication skills, and this approach will be the subject of future study.
Appendices
A. Facilitator Instructions.docx
B. Slides Full.pptx
C. Pocket Card.docx
D. Key Points.docx
E. Pediatric Scenarios.docx
F. Oncology Scenarios.docx
G. Didactic Learner Self-Assessment.doc
H. Didactic Facilitator Guide.doc
I. Slides Brief.pptx
J. Reflective Exercise.docx
K. Milestones Unpacked.docx
L. Evaluation.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
Adam D. Wolfe is a 2015–2016 recipient of the Texas Children's Hospital Educational Scholarship Award, a competitive intramural grant that provided funds to support implementation and evaluation of the curriculum described here.
Ethical Approval
Reported as not applicable.
References
- 1.Sharp MC, Strauss RP, Lorch SC. Communicating medical bad news: parents’ experiences and preferences. J Pediatr. 1992;121(4):539–546. http://dx.doi.org/10.1016/S0022-3476(05)81141-2 [DOI] [PubMed] [Google Scholar]
- 2.Strauss RP, Sharp MC, Lorch SC, Kachalia B. Physicians and the communication of “bad news”: parent experiences of being informed of their child's cleft lip and/or palate. Pediatrics. 1995;96(1):82–89. [PubMed] [Google Scholar]
- 3.Contro NA, Larson J, Scofield S, Sourkes B, Cohen HJ. Hospital staff and family perspectives regarding quality of pediatric palliative care. Pediatrics. 2004;114(5):1248–1252. http://dx.doi.org/10.1542/peds.2003-0857-L [DOI] [PubMed] [Google Scholar]
- 4.Dube CE, LaMonica A, Boyle W, Fuller B, Burkholder GJ. Self-assessment of communication skills preparedness: adult versus pediatric skills. Ambul Pediatr. 2003;3(3):137–141. http://dx.doi.org/10.1367/1539-4409(2003)003<0137:SOCSPA>2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 5.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;363(9405):312–319. http://dx.doi.org/10.1016/S0140-6736(03)15392-5 [DOI] [PubMed] [Google Scholar]
- 6.Harrison ME, Walling A. What do we know about giving bad news? A review. Clin Pediatr (Phila). 2010;49(7):619–626. http://dx.doi.org/10.1177/0009922810361380 [DOI] [PubMed] [Google Scholar]
- 7.Flint H, Meyer M, Hossain M, Klein M Discussing serious news: teaching communication skills through role play with bereaved parents [published online ahead of print November 24, 2015]. Am J Hosp Palliat Care. http://dx.doi.org/10.1177/1049909115617140 [DOI] [PubMed]
- 8.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–311. http://dx.doi.org/10.1634/theoncologist.5-4-302 [DOI] [PubMed] [Google Scholar]
- 9.Wolfe AD, Frierdich SA, Wish J, Kilgore-Carlin J, Plotkin JA, Hoover-Regan M. Sharing life-altering information: development of pediatric hospital guidelines and team training. J Palliat Med. 2014;17(9):1011–1018. http://dx.doi.org/10.1089/jpm.2013.0620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Pediatrics Milestone Project: a joint initiative of the Accreditation Council for Graduate Medical Education and the American Board of Pediatrics. Accreditation Council for Graduate Medical Education Web site. https://www.acgme.org/Portals/0/PDFs/Milestones/PediatricsMilestones.pdf Published 2012. Updated July 2015.
- 11.Nishisaki A, Hales R, Biagas K, et al. A multi-institutional high-fidelity simulation “boot camp” orientation and training program for first year pediatric critical care fellows. Pediatr Crit Care Med. 2009;10(2):157–162. http://dx.doi.org/10.1097/PCC.0b013e3181956d29 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Facilitator Instructions.docx
B. Slides Full.pptx
C. Pocket Card.docx
D. Key Points.docx
E. Pediatric Scenarios.docx
F. Oncology Scenarios.docx
G. Didactic Learner Self-Assessment.doc
H. Didactic Facilitator Guide.doc
I. Slides Brief.pptx
J. Reflective Exercise.docx
K. Milestones Unpacked.docx
L. Evaluation.docx
All appendices are peer reviewed as integral parts of the Original Publication.