Abstract
Objectives
Determine the specific aspects of health information and communications technologies (HICT), including electronic health records (EHRs), most associated with physician burnout, and identify effective coping strategies.
Materials and methods
We performed a qualitative analysis of transcripts from 2 focus groups and a burnout assessment of ambulatory physicians—each at 3 different health care institutions with 3 different EHRs.
Results
Of the 41 clinicians, 71% were women, 98% were physicians, and 73% worked in primary care for an average of 11 years. Only 22% indicated sufficient time for documentation. Fifty-six percent noted “a great deal of stress” because of their job. Forty-two percent reported “poor” or “marginal” control over workload. Even though 90% reported EHR proficiency, 56% indicated EHR time at home was “excessive” or “moderately high.” Focus group themes included HICT “successes” where all patients’ information is accessible from multiple locations. HICT “stressors” included inefficient user interfaces, unpredictable system response times, poor interoperability between systems and excessive data entry. “Adverse outcomes” included ergonomic problems (eg, eye strain and hand, wrist, and back pain) and decreased attractiveness of primary care. Suggested “organizational changes” included EHR training, improved HICT usability, and scribes. “Personal/resilience” strategies focused on self-care (eg, exercise, maintaining work-life boundaries, and positive thinking).
Discussion and conclusion
HICT use, while beneficial in many ways for patients and providers, has also increased the burden of ambulatory practice with personal and professional consequences. HICT and clinic architectural and process redesign are likely necessary to make significant overall improvements.
Keywords: professional burnout, health manpower, medical informatics, electronic health records
BACKGROUND AND SIGNIFICANCE
Physician stress and burnout levels are alarmingly high. A study published in 2015 showed that 54% of US physicians reported at least 1 symptom of burnout in 2014 and that this level had increased significantly from 46% reported in 2011 (1). High stress affects a physician’s health, professional performance, and the quality of care and is even associated with less academic productivity (2–5).
Previous research has demonstrated how information and communication technologies can cause stress and negatively impact user health and productivity in the business domain (6–9). In 2011, a national survey of more than 7000 physicians showed that physicians were significantly more likely to report symptoms of burnout than the general US working adult population (38% vs. 28%) (10). A physician survey conducted in 2014 showed that use of computerized physician order entry was associated with a higher risk of burnout, although at that time, electronic health record (EHR) use was not associated with burnout (11). A time motion study showed that for every hour of direct patient care, nearly 2 additional hours are spent using an EHR (12). An ethnographic study showed that physicians using EHRs often continue to use paper artifacts and handwritten notes as part of the documentation processes (13). Another study showed that physicians spend an average of 6 hours of their day using the EHR (14). As physician work becomes more centered on health information and communications technologies (HICT) and physicians spend more time using HICT, it becomes important to determine which features of HICT are associated with user stress and burnout.
OBJECTIVES
We designed the Minimizing Stress and Maximizing Success of Health Information and Communications Technologies (MS-Squared Study) to identify and characterize specific features of HICT used by physicians in the ambulatory setting that are most associated with stress and burnout. We also sought to identify physician strategies for coping with HICT-related stresses.
MATERIALS AND METHODS
Setting
From July through October 2015, we convened 2 physician focus groups at 3 separate institutions with different EHR vendors:
Centura Health Physician Group, a large multispecialty group in Colorado and Western Kansas, with geographically dispersed practices and an extensively deployed Meditech EHR;
University of New Mexico, a federally designated Hispanic-serving institution with a Cerner EHR;
Stanford University Medical Center, a large academic site with an Epic EHR.
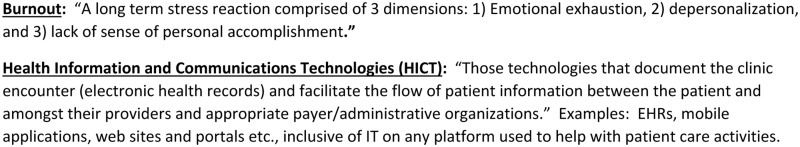
Because physicians use IT on a wide variety of platforms in addition to EHRs, we defined HICT broadly for focus group participants (see Figure 1).
Figure 1.
Definitions.
Subject recruitment
Subjects were recruited through posted flyers in clinical areas, email lists, announcements at gatherings, and word of mouth. The target group was physicians in family medicine, internal medicine, pediatrics, and subspecialties of the latter 2 groups practicing in ambulatory settings. Nurse practitioners and physician assistants were also invited to participate. No residents or other trainees were invited. Participants were provided snacks and received a $50 gift card for participating in the 90-min sessions.
This study’s research protocol was approved by the University of New Mexico’s Health Research Review Committee and informed consent was obtained from all focus group participants.
Focus group design and operation
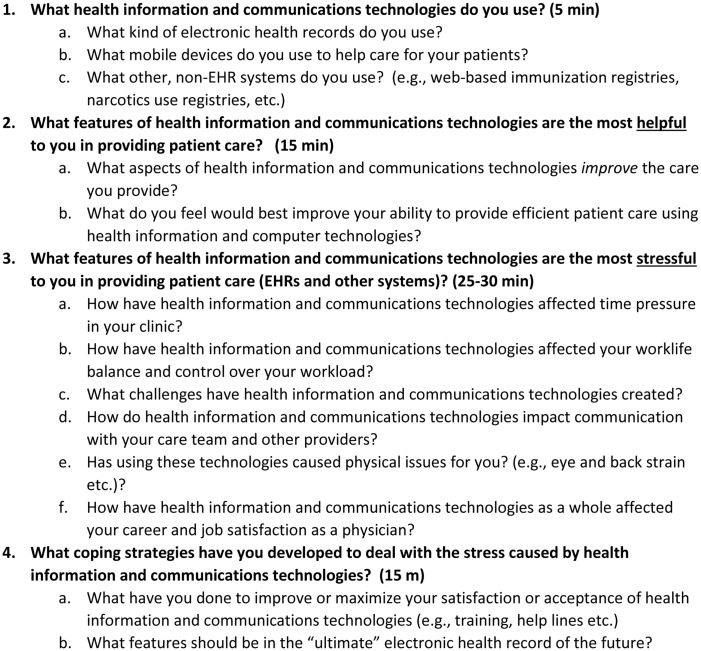
Draft focus group questions and follow-up probes were developed by the investigators, including experts in physician work-life issues, clinical informatics, health services research, qualitative research, and biostatistics. Questions were tested in a calibration focus group with participants recruited in the manner outlined above. The focus group questions along with their probes are listed in Figure 2.
Figure 2.
MS-Squared focus group questions.
Focus group participants completed an anonymous survey based on the previously validated Mini-z instrument (15) that measures physician stress, burnout, as well as burnout predictors (eg, level of control, time pressure, and office chaos) using questions with a 1–5 Likert scale and is freely available (16). Focus groups were led by trained facilitators who were not members of the investigator team. The investigator team did not have access to the audio files, which were deleted after production of de-identified transcripts.
Focus group analysis process
We used the content analysis approach to analyze focus group transcripts (17). Analyses were primarily descriptive and similar to those used in the MEMO (Minimizing Error Maximizing Outcome) study (18). One investigator at each of the 3 sites independently read and coded transcripts manually on article with identified themes from their sites (P.K., N.M., and S.V.). To ensure the reliability of the coding, 2 other investigators (M.L. and K.P.), not at any of the focus group sites, independently read and coded transcripts for themes from all sites. All 5 investigators then held conference calls to identify, correlate, and refine coded themes across all sites, using an iterative process, until no new themes were identified, all investigators agreed on the themes identified, and all investigators agreed that saturation had been obtained, and there was no need for additional focus groups. The final agreed upon themes were then sorted into 5 categories:
Things that work (successes)
Things that don’t work (stressors)
Personal consequences (outcomes)
How to make it better (organizational changes)
How to cope with HICT (personal/resilience)
RESULTS
Pre-session survey
Table 1 summarizes the demographics of 41 clinicians who participated in the 6 focus groups. Of these, 72% were women, 98% were physicians, and 73% had worked in primary care for an average of 11 years. Table 2 summarizes the responses from the anonymous survey (100% response rate). Fifty-six percent agreed or strongly agreed with the statement “I feel a great deal of stress because of my job.” Using the respondents’ own definition of burnout, 34% agreed with the statement “I am definitely burning out and have one or more symptoms of burnout, eg emotional exhaustion.” An additional 12% percent indicated “The symptoms of burnout won’t go away. I think about work frustrations a lot.” Forty-one percent reported “poor” or “marginal” control over their workload. Even though 90% reported satisfactory or better proficiency with their EHR, 56% felt the amount of time spent on the EHR at home was “excessive” or “moderately high.” Only 22% indicated sufficient time for documentation.
Table 1.
Focus group demographics
| Six focus groups | N = 41 |
|---|---|
| Provider type | |
| MD/DO | 40 (98%) |
| Nurse Practitioner | 1 (2%) |
| Experience (current practice) | |
| 0–1 year | 6 (15%) |
| 2–5 years | 8 (20%) |
| 6–10 years | 5 (12%) |
| 11–15 years | 3 (7%) |
| 16–20 years | 3 (7%) |
| 21+ years | 6 (15%) |
| No response | 10 (24%) |
| Mean | 10.8 years |
| Standard deviation | 10.1 years |
| Gender | |
| Male | 11 (27%) |
| Female | 29 (71%) |
| No response | 1 (2%) |
| Specialization | |
| Primary care | 30 (73%) |
| Non-procedural specialist | 9 (22%) |
| Procedural specialist | 2 (5%) |
Table 2.
Results of focus groups’ anonymous burnout survey using the mini-Z
| Item: | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree |
|---|---|---|---|---|---|
| Overall I am satisfied with my current job | 23 (56%) | 9 (22%) | 5 (12%) | 3 (7%) | 1 (2.4%) |
| Great deal of stress because of job | 6 (15%) | 17 (41%) | 12 (29%) | 4 (10%) | 2 (4.9%) |
| Professional values aligned with department leaders | 5 (12%) | 15 (37%) | 16 (39%) | 4 (10%) | 1 (2.4%) |
| Burnout symptoms won’t go away | Definitely burning out | Under stress but not burnt out | Enjoy work/no burnout | ||
| Symptoms of burnout | 5 (12%) | 14 (34%) | 14 (34%) | 8 (20%) | – |
| Poor | Marginal | Satisfactory | Good | Optimal | |
| Control over workload | 4 (10%) | 13 (32%) | 15 (37%) | 8 (20%) | 1 (2.4%) |
| Sufficient time for documentation | 12 (29%) | 20 (49%) | 7 (17%) | 2 (4.9%) | 0 |
| Degree that team works efficiently together | 1 (2.4%) | 8 (20%) | 18 (44%) | 11 (27%) | 3 (7.3%) |
| Proficiency with EHR use | 1 (2.4%) | 3 (7.3%) | 18 (44%) | 17 (39%) | 2 (4.9%) |
| Excessive | Moderately high | Satisfactory | Modest | Minimal/none | |
| Amount of time spent on EHR at home | 9 (22%) | 14 (34%) | 6 (15%) | 6 (15%) | 6 (15%) |
| Calm | Busy, but reasonable | Hectic, chaotic | |||
| Work atmosphere description | 1 (2.4%) | 3 (7.3%) | 12 (29%) | 23 (56%) | 2 (4.9%) |
Focus group analysis
Table 3 contains a summary of the categorized themes identified from the analysis of focus group transcripts. This table represents the themes as derived from the focus groups’ transcripts from 3 different institutions. This study’s methodology is not designed to identify differences between themes at different institutions.
Table 3.
Focus group themes
| Things that work (successes) | Things that don’t work (stress predictors) | Personal Consequences (outcomes) | How to make it better (organizational fixes) | How to cope with HICT (personal/resilience) |
|---|---|---|---|---|
|
|
|
|
|
Things that work (successes)
Respondents appreciate having all patients’ medical information in one place and the ability to access the EHR from multiple locations (eg, at home). Participants like the ability of EHRs to filter patient data and to display medical images. “I love being able to show patients their own X-rays…when they were taken 10 min ago.”
Electronic messaging to colleagues and patients was reported as both a HICT benefit and area needing improvement. “Messaging is pretty efficient for me. I spend a lot less time reviewing labs and messaging my nurse…than I would have in the old days of paper charts.” “I think that what I find challenging is it’s really hard to focus, because all of these different messaging things come in, so your [sic] focused on 1 patient, and in the meantime messages are popping up.”
Electronic access to medical references and the biomedical literature is also helpful. “I remember… when we had to pull out our textbooks, or I used to keep this ginormous file of articles and now it’s right there…” Participants listed a variety of mobile clinical applications and several innovative ways patients are using mobile devices to help with their care. “We get the parents to take pictures of… prescriptions, so instead of them not bringing them they’ll just say, here.”
Things that don’t work (stressors)
Questions on stressors elicited the most passionate and numerous responses. A common theme was the time pressure physicians experience to complete documentation. “When am I gonna do my notes?” Several commented that visit times are too short, with insufficient time to reflect on patient encounters. Many physicians routinely work through lunch, stay after hours, or work at home to complete documentation. “It’s every single night you’re dictating, every single weekend you’re dictating or typing charts.”
Many participants commented on inefficient user interface designs “too many clicks per task” and “opening like 10 screens to do one task.” Frequent comments cited unpredictable system response times, frequently broken or poorly maintained hardware, and excessive data entry. “They’re here for a sore throat. ‘Oh, when did you have your last mammogram?’ …. ‘I came in for a sore throat’…But we have to document this.” Others commenting on EHR design indicated that finding specific information is often difficult and not intuitive. Some said it is much harder to know whether critical information was missed after a complete review of a patient’s EHR compared with paper charts; scanned information was particularly problematic.
Participants felt the EHR had increased their clinical practice burden by requiring them to enter data for purposes other than patient care (eg, for billing, screening, research, and quality control).
Many participants said that body position such as turning their backs to patients to access and enter information interfered with patient relationships. “I’m asking a patient who’s sharing news about cancer, addiction, suicidal thoughts to accept the fact that their provider is 40% attuned to things flashing on the screen and typing…” Many feel they spend more time focused on the EHR than on the patient. It’s a constant balance and a constant real battle between being present and being efficient…”
Not having printers in exam rooms was associated with reduced time with patients. “The printer is down the hallway and the printer for prescriptions is someplace else.” Many participants reported that getting IT or technical support was too time-consuming and that IT staff may not appreciate clinical issues such as physicians’ time pressure.
Participants recognize the potential for HICT benefits not yet realized or poorly implemented. For example, physicians are required to type information already stored elsewhere in the EHR into forms or other documents. Also, participants do not understand why information from outside institutions is difficult to access. “What’s frustrating is that we’ve been talking about interoperability for a decade or so and we’re not any closer now than we were 10 years ago.”
Personal consequences (outcomes)
A major theme was how HICT makes it difficult to maintain healthy work-life boundaries. “The boundaries blur. The next thing you know, you’re always at work.”
Another common theme was ergonomics. Many participants reported headaches as well as wrist, neck, back, and eye strain attributed to HICT use. One participant indicated she suffers from “mouse shoulder.” Another said she spent $2000 to find the right eye glasses to reduce eye and neck strain. Another reported difficulties using many computer workstations each day: “I also spend all my time in the clinic trying to adjust my chair up and down and adjust the monitor. Some of them go up and down and some of them don’t, so I… run around the clinic trying to find which monitor I should sit at [and] to move the chairs around trying to find the right chair. I spend some time doing that and I still go home with neck spasms…”
Several concerns led to sleep difficulties and anxiety including meeting new regulations, concerns about missing documentation and finding time to complete documentation. Some said that the documentation burden in primary care was increasing the rate of turnover as well as making careers in primary care less attractive.
How to make it better (organizational changes)
Many participants said user interfaces should be improved and system response times should be predictable and fast. Other suggestions included the use of artificial intelligence, automated billing functions, badge or fingerprint login (eg, “tap and go”), and touchscreen functionality. System customization was recommended.
Another theme was increasing meaningful time with patients by reducing the data entry burden by employing scribes. One participant felt the need for scribes is an indicator of poor HICT design. “I see scribes as just a big workaround.” Related suggestions included creating “desktop slots” or blocked empty appointments in physicians’ schedules to allow time to catch up on documentation.
How to cope with HICT (personal/resilience)
A recurring theme was the need for physical exercise, self-care, and resilience training. Participants lauded activities such as walks during lunchtime, swimming, spinning, and other forms of exercise. Learning to be more intentional about work, writing more precise clinical notes, thinking positively, setting limits, sharpening work-life boundaries and protecting home time as much as possible were also mentioned. “When I’m there I’m there [at work], when I’m not, I’m not.”
Participants indicated that EHR training and periodic retraining helped them cope. An “adult learning approach” or elbow-to-elbow training was praised by several participants. Many also appreciated learning from colleagues and residents.
Other coping suggestions included “not eating lunch at your desk…because it’s hard to not keep working if you’re sitting right by your computer…” Some participants indicated that communicating with patients and staff face-to-face as opposed to electronically is helpful: “I think making a conscious effort to go and talk to somebody rather than sending them an instant message relieves stress.” Some used humor in the clinical environment to relieve stress: “We use a lot of humor …” Others have reduced the number of hours of clinical time: “I’ve cut my hours, and I probably will cut some more.” Sadly, some are leaving medicine: “I think each and every one of us would have to try to figure out a coping mechanism. And it could be, like for me, quitting primary care.”
DISCUSSION
This mixed methods study of 41 clinicians in academic and community-based settings showed that stress and burnout can be high, mirroring national findings (15). Physicians eager to discuss the pros and cons of HICT noted its benefits and great promise, and the desire not to return to paper charting. Most all participants had multiple criticisms of current HICT design and report many unintended consequences of HICT use. These included 1) excessive data entry requirements, 2) inefficiently designed user interfaces, 3) insufficient health information exchange from outside institutions, 4) information overload, 5) interference with the patient-physician relationship as factors associated with EHR use, and 6) ergonomic problems due to legacy clinical architecture poorly retrofitted with HICT equipment. The pre-focus group survey revealed physicians struggling with high stress and burnout, low control of workload, high time pressure for documentation at work, and too much documentation time spent at home. These data suggest beleaguered physicians struggling to maintain control of the workplace while remaining deeply involved in the care of their patients. This struggle is at the core of the daily challenge faced by health systems implementing HICT.
Some of the many important benefits of the EHR participants noted include having data all in one place, data accessible from many sites, and the ability to connect with subspecialists and other clinical staff. However, many participants also described challenges, in particular noting adverse physical outcomes due to ergonomic problems such as eye strain, neck, back, and wrist pain, and “mouse shoulder.” Physicians often use multiple, shared, suboptimally-placed workstations throughout their day, making it difficult to maintain proper positioning. Architectural designs that consider modern clinic workflow and reduce the number of different chairs and workstations a physician uses in a typical day would likely be helpful. This finding is consistent with prior studies that showed how proper height of the computer monitor impacts stress level, user comfort and performance (19, 20). It also suggests a role for occupational and physical therapy in making long term EHR use more manageable (21–23).
A similar mixed methods study sponsored by the American Medical Association was conducted by the RAND Corporation in 2012–2013 (24). The RAND study consisted of semi-structured interviews of 109 physicians at 30 practices. MS-Squared investigators conducted focus groups at 3 large institutions, 2 academic centers, and 1 community-based health care organization, each with a different EHR system. Approximately half of the RAND study physicians worked in physician-owned practices while all of the physicians in the MS-Squared study were employed by large health care systems. The RAND study used the same job satisfaction question used in the MS-Squared pre-focus group survey: “Overall, I am satisfied with my current job.” Eighty-one percent of the RAND study physicians responded “agree” or “strongly” agree compared with 78% of the MS-Squared physicians answering the same question.
Our study identified many of the same major problems identified in the RAND study (numbers 1–5 above). Two themes identified in the RAND study not present in the MS-Squared study were the high costs of EHRs, switching EHRs threatening practice finances, and the mismatch between Meaningful Use criteria and actual clinical practice. These themes are likely different from those our study identified because MS-Squared physicians are all employees and do not hold a direct financial stake in a practice while half of the RAND study physicians did.
Another qualitative study analyzed comments from the 2014 Rhode Island Health Information Technology Survey. Although derived from written comments from a survey that included a significant proportion of hospital-based physicians, the themes of less time with patients/more time on the computer, interference with the patient-physician relationship, and improved patient information access were identified (25).
As with the RAND and Rhode Island studies, MS-Squared identified many positive outcomes including ready access to patient information, improved communication with patients and colleagues, as well as some aspects of quality improvement attributed to HICT use. MS-Squared physicians also highlighted web-based medical teaching aids/resources and digital imaging as helpful and positive aspects of HICT.
Many participants called out their concern over how the presence of the EHR in the exam room impacts the patient-physician relationship (#6 above): “a constant balance between being present and being efficient.” This is also consistent with prior work that shows how the presence of the EHR in the exam room impacts patient–physician communication and patient satisfaction (26–28).
Participants felt that physician EHR time could be reduced by having support personnel perform more routine data entry. Many physicians believe that scribes are a particular kind of support that would be of help by relieving much of the data entry burden. The literature on medical scribes suggests substantial improvements in provider satisfaction and modest increases in productivity (29–32). Although not called out specifically, participant comments generally support the advanced care team approach where there are specially trained support staff to work closely with the physician throughout the patient’s visit. The additional staff remove much of the data entry and clinic process burden from the physician who can then focus more attention on patients. Periodic EHR re-training, improved user interface design, and greater interoperability may also help prevent the physician–patient relationship from eroding.
This study revealed another very important concern over how HICT use intrudes upon personal time, making primary care and other related medical careers with heavy “in-boxes” unattractive. In a time when US health care is gearing up for a more complex and older patient population, this is concerning and requires further study. Additional personnel may be needed for after hours, vacation, and in-box coverage.
This work strengthens an already excellent business case for health care institutions to invest in strategies to reduce physician stress and burnout. Costs to an institution for the turnover of one primary care physician have been estimated at $250 000 (1991 dollars) (33). More recent studies indicate average costs now approach half a million dollars per physician turnover (34). Even when burnout does not cause physician turnover, increased burnout levels have been shown to significantly reduce Relative Value Units (RVU) acquired and even academic productivity (5). Our study confirms that many physicians do feel HICT is a significant cause or contributing factor to burnout and when it does occur, causes high costs to the institution (financially as well as to the quality and continuity of care).
Recent estimates indicate up to half of today’s physician turnover is caused by burnout (35). Given a significant portion of burnout is likely caused by HICT consequences, health care institutions may be losing millions of dollars because of these HICT “side effects”. These potential costs suggest a return-on-investment benefit for allocating a fraction of these costs to focus on improving HICT similar to how institutions focus on improving safety and quality.
MS-Squared is the first study to our knowledge to ask physicians what helps mitigate unintended consequences of HICT use. Physicians offered constructive comments about ways to respond to the challenges, both personally and organizationally. Resilience was highlighted as a key skill to help survive the status quo. Exercise, wellness centers, self-care, meditation, walking, getting up from the computer at regular intervals, and setting limits on computer work outside of duty hours were ways noted to cope with the increasing documentation burden. However, respondents cautioned that these strategies alone were insufficient. Participants felt that organizational and system redesign is also necessary to effectively mitigate HICT-related stress. Our data suggest that health systems should consider the amount of support they can provide to decrease the rising burden of documentation.
Government programs such as PQRS (Physician Quality Reporting System), Meaningful Use, and MACRA (Medicare Access & CHIP Reauthorization Act of 2015), have led to increased documentation requirements (36–38). One participant noted that: “.the easier it is to start documenting, the more things we’re expected to document.” Whether the current HICT infrastructure is capable of meeting the increasing reporting requirements for MACRA remains to be seen (39). The “culture of endurance” where physicians have a tradition of doing whatever it takes to care for the patient (40), if carried too far with HICT, can become self-destructive.
Some of the themes identified conflict with each other. For example, physicians generally like being able to access patient information from home but also report that using the EHR at home intrudes on their personal lives. While many physicians work through lunch, others recommend taking a break at lunchtime. These conflicts suggest that HICT stress affects individual physicians differently. Likewise, what might be a stress mitigator for one physician might not help another.
This study was limited by a relatively small number of participants at 3 institutions. The majority of the participants were female (71%) and the results of the pre-focus group survey indicated that participants were highly stressed. Ergonomic findings are limited by the fact that the study was drawn from only 3 organizations with a finite number of clinical sites. Thus this group may not be representative of all physicians using HICT. Although not all physicians may be suffering from HICT-related burnout, this work does substantiate that, at the very least, there is a sizable proportion of physicians who are. Quantitative assessments will occur during the next phase of this work where a multi-site survey of hundreds of physicians will probe more deeply into issues and solutions surrounding HICT use. Topics to be addressed include: the most effective means of coping with HICT issues, the amount of variance in stress and burnout attributable to HICT, and how much HICT time is spent outside of work hours.
CONCLUSION
Over half a century of HICT research, development, deployment, government regulation, and incentives have promoted the widespread adoption of EHRs to improve the quality, ease of practice, and lower the cost of health care. Although no one suggested going back to paper, this study provides evidence that data entry requirements, inefficiently designed user interfaces, insufficient health information exchange from outside institutions, information overload, and interference with the patient–physician relationship are HICT factors associated with physician stress. This work also highlights the importance of ergonomic considerations when designing HICT into the clinical architectural and workflow. These issues raised by physicians are legitimate concerns that impact patient care, detract from career satisfaction, and decrease retention. Organizations should consider periodically measuring satisfaction, stress and burnout, their remediable predictors, and patient care outcomes such as quality and safety. Unintended consequences of HICT should be addressed in order to fully realize the potential benefits of these technologies to the Quadruple Aim of better patient care, population health, lower costs, and better health of providers (41).
ACKNOWLEDGMENTS
The authors thank Gale Hannigan, PhD for help with editing and literature searching, and Maria Livaudais for help developing this article’s title.
Funding
This work was supported by the Agency for Healthcare Research and Quality (AHRQ) [R18HS022065].
Conflict of interest statement. None declared.
Contributors
All the authors of this publication meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, including:
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work;
Drafting the work or revising it critically for important intellectual content;
Final approval of the version to be published;
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
REFERENCES
- 1. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general us working population between 2011 and 2014. Mayo Clin Proc 2015; 90 (12): 1600–13. [DOI] [PubMed] [Google Scholar]
- 2. Wallace JE, Lemaire JB, Ghali WA.. Physician wellness: A missing quality indicator. Lancet 2009; 374 (9702): 1714–21. [DOI] [PubMed] [Google Scholar]
- 3. Williams ES, Manwell LB, Konrad TR, et al. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: Results from the MEMO study. Health Care Manage Rev 2007; 32 (3): 203–12. [DOI] [PubMed] [Google Scholar]
- 4. Dewa CS, Loong D, Bonato S, et al. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open 2017; 7 (6): e015141.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Turner TB, Dilley SE, Smith HJ, et al. The impact of physician burnout on clinical and academic productivity of gynecologic oncologists: A decision analysis. Gynecol Oncol 2017; 146 (3): 642–6. [DOI] [PubMed] [Google Scholar]
- 6. Thomee S, Eklof M, Gustafsson E, et al. Prevalence of perceived stress, symptoms of depression and sleep disturbances in relation to information and communication technology use amoung young adults—an explorative prospective study. Comput Human Behav 2007; 23 (3): 1300–21. [Google Scholar]
- 7. Yun H, Kettinger WJ, Lee CC.. A new open door: The smartphone’s impact on work-to-life conflict, stress, and resistance. Int J Electronic Commerce 2012; 16 (4): 121–51. [Google Scholar]
- 8. Arnetz B, Berg M, Arnetz J.. Mental strain and physical symptoms among employees in modern offices. Arch Environ Health 1997; 52 (1): 63–7. [DOI] [PubMed] [Google Scholar]
- 9. Tarafdar M, Tu Q, Ragu-Nathan B, et al. The impact of technostress on role stress and productivity. J Manage Inf Syst 2007; 24 (1): 301–28. [Google Scholar]
- 10. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among us physicians relative to the general us population. Arch Intern Med 2012; 172 (18): 1377–85. [DOI] [PubMed] [Google Scholar]
- 11. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91 (7): 836–48. [DOI] [PubMed] [Google Scholar]
- 12. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med 2016; 165 (11): 753–60. [DOI] [PubMed] [Google Scholar]
- 13. Saleem JJ, Adams S, Frankel RM, et al. Efficiency strategies for facilitating computerized clinical documentation in ambulatory care. Stud Health Technol Inform 2013; 192: 13–7. [PubMed] [Google Scholar]
- 14. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: Primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 15 (5): 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Linzer M, Poplau S, Babbott S, et al. Worklife and wellness in academic general internal medicine: Results from a national survey. J Gen Intern Med 2016; 31 (9): 1004–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kroth PJ, Morioka-Douglas N, Vares S, et al. MS-Squared Focus Group Survey Instrument 2014. http://digitalrepository.unm.edu/ms2/1/ Accessed February 7, 2017.
- 17. Hsieh HF, Shannon SE.. Three approaches to qualitative content analysis. Qual Health Res 2005; 15 (9): 1277–88. [DOI] [PubMed] [Google Scholar]
- 18. Manwell LB, Williams ES, Babbott S, et al. Physician perspectives on quality and error in the outpatient setting. WMJ 2009; 108 (3): 139–44. [PubMed] [Google Scholar]
- 19. Kothiyal K, Bjornerem AM.. Effects of computer monitor setting on muscular activity, user comfort and acceptability in office work. Work 2009; 32 (2): 155–63. [DOI] [PubMed] [Google Scholar]
- 20. Smith WD, Berguer R, Nguyen NT.. Monitor height affects surgeons’ stress level and performance on minimally invasive surgery tasks. Stud Health Technol Inform 2005; 111: 498–501. [PubMed] [Google Scholar]
- 21. Griffiths KL, Mackey MG, Adamson BJ.. The impact of a computerized work environment on professional occupational groups and behavioural and physiological risk factors for musculoskeletal symptoms: A literature review. J Occup Rehabil 2007; 17 (4): 743–65. [DOI] [PubMed] [Google Scholar]
- 22. Mean M, Garnier A, Wenger N, et al. Computer usage and task-switching during resident’s working day: Disruptive or not? PLoS One 2017; 12 (2): e0172878.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ergonomic considerations loom large as hospitals and other health care organizations rapidly adopt IT tools. ED Manag 2013; 25 (3): 31–2. [PubMed] [Google Scholar]
- 24. Friedberg MW, Chen PG, Busum KRV, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Healthsystems, and Health Policy. Santa Monica, CA: RAND Corporation; 2013. [Google Scholar]
- 25. Pelland KD, Baier RR, Gardner RL.. It’s like texting at the dinner table”: A qualitative analysis of the impact of electronic health records on patient-physician interaction in hospitals. J Innov Health Inform 2017; 24 (2): 216.. [DOI] [PubMed] [Google Scholar]
- 26. Frankel RM. Computers in the examination room. JAMA Intern Med 2016; 176 (1): 128–9. [DOI] [PubMed] [Google Scholar]
- 27. Reis S, Visser A, Frankel R.. Health information and communication technology in healthcare communication: The good, the bad, and the transformative. Patient Educ Couns 2013; 93 (3): 359–62. [DOI] [PubMed] [Google Scholar]
- 28. Frankel RM, Saleem JJ.. Attention on the flight deck”: What ambulatory care providers can learn from pilots about complex coordinated actions. Patient Educ Couns 2013; 93 (3): 367–72. [DOI] [PubMed] [Google Scholar]
- 29. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: A prospective study. Clinicoecon Outcomes Res 2013; 5: 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yan C, Rose S, Rothberg MB, et al. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med 2016; 31 (9): 990–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arya R, Salovich DM, Ohman-Strickland P, et al. Impact of scribes on performance indicators in the emergency department. Acad Emerg Med 2010; 17 (5): 490–4. [DOI] [PubMed] [Google Scholar]
- 32. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: Patient and physician satisfaction. Urology 2010; 184 (1): 258–62. [DOI] [PubMed] [Google Scholar]
- 33. Buchbinder SB, Wilson M, Melick CF, et al. Estimates of costs of primary care physician turnover. Am J Manag Care 1999; 5 (11): 1431–8. [PubMed] [Google Scholar]
- 34. Schloss EP, Flanagan DM, Culler CL, et al. Some hidden costs of faculty turnover in clinical departments in one academic medical center. Acad Med 2009; 84 (1): 32–6. [DOI] [PubMed] [Google Scholar]
- 35. Shanafelt T, Goh J, Sinsky C.. The business case for investing in physician well-being. JAMA Intern Med 2017; 177 (12): 1826–32. [DOI] [PubMed] [Google Scholar]
- 36. Bendix J. Assessing the payoff from meaningful use of ehrs. More physicians are using electronic health records, but opinions are mixed over the value of digitization. Med Econ 2014; 91 (2): 72, 74–6.**** [PubMed] [Google Scholar]
- 37. Centers for Medicare and Medicaid Services. MACRA: Delivery System Reform, Medicare Payment Reform https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html Accessed September 5, 2017.
- 38. United States Department of Health and Human Services. Meaningful Use Regulations 2016. http://www.healthit.gov/policy-researchers-implementers/meaningful-use Accessed September 5, 2017.
- 39. Healthcare IT News. CMS Gets an Earful on Proposed MACRA Changes From HIMSS, AMA, AMGA, Others 2016. http://www.healthcareitnews.com/news/cms-gets-earful-proposed-macra-changes-himss-ama-amga-others Accessed August 12, 2016.
- 40. Viviers S, Lachance L, Maranda MF, et al. Burnout, psychological distress, and overwork: The case of Quebec’s ophthalmologists. Can J Ophthalmol 2008; 43 (5): 535–46. [DOI] [PubMed] [Google Scholar]
- 41. Bodenheimer T, Sinsky C.. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med 2014; 12 (6): 573–6. [DOI] [PMC free article] [PubMed] [Google Scholar]