Abstract
Background
Aggression occurs frequently within health and social care settings. It can result in injury to patients and staff and can adversely affect staff performance and well‐being. De‐escalation is a widely used and recommended intervention for managing aggression, but the efficacy of the intervention as a whole and the specific techniques that comprise it are unclear.
Objectives
To assess the effects of de‐escalation techniques for managing non‐psychosis‐induced aggression in adults in care settings, in both staff and service users.
Search methods
We searched CENTRAL, MEDLINE, Embase, PsycINFO, CINAHL and 14 other databases in September 2017, plus three trials registers in October 2017. We also checked references, and contacted study authors and authorities in the field to identify additional published and unpublished studies.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs comparing de‐escalation techniques with standard practice or alternative techniques for managing aggressive behaviour in adult care settings. We excluded studies in which participants had psychosis.
Data collection and analysis
We used the standard methodological procedures expected by Cochrane.
Main results
This review includes just one cluster‐randomised study of 306 older people with dementia and an average age of 86 years, conducted across 16 nursing homes in France. The study did not measure any of our primary or secondary outcomes but did measure behavioural change using three measurement scales: the Cohen‐Mansfield Agitation Inventory (CMAI; 29‐item scale), the Neuropsychiatric Inventory (NPI; 12‐item scale), and the Observation Scale (OS; 25‐item scale). For the CMAI, the study reports a Global score (29 items rated on a seven‐point scale (1 = never occurs to 7 = occurs several times an hour) and summed to give a total score ranging from 29 to 203) and mean scores (evaluable items (rated on the same 7‐point scale) divided by the theoretical total number of items) for the following four domains: Physically Non‐Aggressive Behaviour, such as pacing (13 items); Verbally Non‐Aggressive Behaviour, such as repetition (four items); Physically Aggressive Behaviour, such as hitting (nine items); and Verbally Aggressive Behaviour, such as swearing (three items). Four of the five CMAI scales improved in the intervention group (Global: change mean difference (MD) −5.69 points, 95% confidence interval (CI) −9.59 to −1.79; Physically Non‐Aggressive: change MD −0.32 points, 95% CI −0.49 to −0.15; Verbally Non‐Aggressive: change MD −0.44 points, 95% CI −0.69 to −0.19; and Verbally Aggressive: change MD −0.16 points, 95% CI −0.31 to −0.01). There was no difference in change scores on the Physically Aggressive scale (MD −0.08 points, 95% CI −0.37 to 0.21). Using GRADE guidelines, we rated the quality of this evidence as very low due to high risk of bias and indirectness of the outcome measures. There were no differences in NPI or OS change scores between groups by the end of the study.
We also identified one ongoing study.
Authors' conclusions
The limited evidence means that uncertainty remains around the effectiveness of de‐escalation and the relative efficacy of different techniques. High‐quality research on the effectiveness of this intervention is therefore urgently needed.
Plain language summary
Using de‐escalation to prevent violence in aggressive people
Review questions
Do de‐escalation techniques help to calm down adults who are being aggressive in care settings? Which techniques work best?
Background
There are many reasons why people may be aggressive in care settings, including mental or physical illness. People can use a range of techniques to help someone who is behaving aggressively to calm down, including talking to the person and interpreting non‐verbal gestures and body language. This approach is referred to as de‐escalation. Although it is widely taught and used, we know very little about how effective de‐escalation is, or which techniques work best.
Study characteristics
We looked for all available evidence on this topic, finding just two studies. One of these included 306 people with dementia and an average age of 86 years, living in 16 nursing homes in France. The second study is still in progress and did not provide results for the review.
Key results
The study did not assess areas important to us, such as the number of injuries sustained by staff or residents. It did, however, measure the impact of staff training on residents' level of aggression three months after the end of the training. Some measures of physical and verbal aggression showed reductions, but not all.
Quality of the evidence
The reliability of evidence available in the one included trial is very low and did not address important questions such as injury. Therefore, we cannot say whether de‐escalation techniques are effective.
Currentness of evidence
The evidence is current to September 2017.
Summary of findings
Summary of findings for the main comparison. De‐escalation versus standard care for managing aggression.
| De‐escalation versus standard care for managing aggression | |||||
| Patient or population: patients with dementia Setting: nursing homes Intervention: de‐escalation Comparison: standard care | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with standard care | Risk with de‐escalation | ||||
| Frequency of aggression‐related serious untoward incidents | No data available | ||||
| Frequency of aggression‐related injuries to staff | No data available | ||||
| Quality of life | No data available | ||||
|
Agitated behaviour (validated scale) Measured by: Cohen‐Mansfield Agitation Inventory ‐ Global (29 individual items rated on 7‐point scale, ranging from 1 (never occurs) to 7 (occurs several times an hour), and summed to give a total score ranging from 29 to 203; lower score indicates fewer behaviours) Follow‐up: mean change from baseline to 20 weeks |
The mean change (from baseline to 20 weeks) score in the control group was 0.83 points lower | The mean change (from baseline to 20 weeks) score in the intervention groups was 5.69 points lower (9.59 lower to 1.79 lower) | — | 306 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
|
Physically aggressive behaviour (validated scale) Measured by: Cohen‐Mansfield Agitation Inventory ‐ Physically Aggressive Behaviour Scale (9 items rated on 7‐point scale, ranging from 1 (never occurs) to 7 (occurs several times an hour); lower score indicates fewer behaviours) Follow‐up: mean change from baseline to 20 weeks |
The mean change (from baseline to 20 weeks) score in the control groups was 0.07 points lower | The mean change (from baseline to 20 weeks) score in the intervention groups was 0.08 points lower (0.37 lower to 0.21 higher) | — | 306 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
|
Verbally aggressive behaviour (validated scale) Measured by: Cohen‐Mansfield Agitation Inventory ‐ Verbally Aggressive Behaviour Scale (3 items rated on 7‐point scale, ranging from 1 (never occurs) to 7 (occurs several times an hour); lower score indicates fewer behaviours) Follow‐up: mean change from baseline to 20 weeks |
The mean change (from baseline to 20 weeks) score in the control groups was 0.09 points higher | The mean change (from baseline to 20 weeks) score in the intervention groups was 0.16 points lower (0.31 lower to 0.01 lower) | — | 306 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
|
Agitated behaviour (observational measure) Measured by: Observation Scale (25 items scored after 3 minutes of observation by clinical raters; lower score = less severe behaviours) Follow‐up: mean change from baseline to 20 weeks |
The mean change (from baseline to 20 weeks) score groups was 2.58 points lower | The mean change (from baseline to 20 weeks) score in the intervention groups was 7.92 points lower (13.19 lower to 2.65 lower) | — | 306 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aRandomisation procedures are unclear, and significant differences between groups at baseline suggest that effects may be influenced by the method of randomisation. bThe outcome was not one of our pre‐specified measures.
Background
Description of the condition
Aggression can occur in many settings, including inpatient settings, emergency settings (NICE 2015), and communities served by emergency services such as police or paramedics (Hester 2009). It can be defined as any behaviour directed toward another individual that has the immediate intent of causing harm (Anderson 2002). People can communicate aggression verbally, or it may manifest through a range of behaviours causing physical or psychological harm towards the self or others or damage to the environment (NICE 2015). Some authors have described aggression as an assault cycle comprising five stages (the trigger phase, escalation phase, crisis phase, recovery phase, and depression phase) (Kaplan 1983; Leadbetter 1995). There is a substantial body of literature on the origins of aggressive behaviour and theories to account for its causes. For example, the general aggression model assumes that specific context‐ and person‐centred factors are mediated by variables such as cognition, affect and arousal in the manifestation of aggression (Anderson 2002). On the other hand, the reactive/proactive model of child and adolescent aggression defines reactive aggression as an angry response to presumed threat, and proactive aggression as a planned response stemming from conditioned learning (Polman 2007). Aggression may be associated with intrinsic factors such as recognised mental health issues (Fazel 2006), including, for the purposes of this review, substance misuse, intellectual disability and other mental health issues (excluding psychosis), as well as extrinsic factors such as social and environmental conditions. Certain conditions also place individuals at increased risk of an episode of acute aggression such as head injury, Huntington's Disease (Johnson 2011), learning disability (Taylor 2005), and a combination of alcohol or substance misuse (Roizen 1997; Snowden 2001). The multi‐factorial origins of aggression mean that it can apply to a wide population.There is not scope within this review to fully explore all of the relevant literature on the aetiology of aggressive behaviour or its relevance in different settings, so we will focus on the management of these behaviours within the broad context of health services.
Unchecked aggression may escalate into violence, involving risks to the aggressor and those around them such as family and healthcare professionals (Bourget 2002; Maguire 2007). Workplace violence affects every country and healthcare setting, with reports estimating that 4% of the global employee population have experienced physical violence, and nurses are at three times greater risk of violence than any other profession (Di Martino 2003). A large international review of 424 studies reported an incidence rate of over 32% for violence in psychiatric hospitals but a greater risk of violence in acute healthcare settings (Bowers 2011). In the UK, there are an estimated 67,864 incidents of physical assaults against National Health Service (NHS) staff per annum, with 67% occurring in mental health settings, 28% in acute hospitals and the remainder in ambulance and primary care settings (NHS Protect 2015). In England alone, 14% of NHS staff reported having experienced physical violence from service users, relatives or the public (NHS 2014). Violence is also prevalent in community settings where around half of care workers experience verbal abuse, and over a third experience physical abuse (NCCMH 2015). Aggressive and violent behaviour may have a significant impact on staff with an estimated 26%, 11% and 6% of incidents respectively relating to mild, moderate or severe injury (Bowers 2011). Verbal aggression toward staff is common and may lead to poor performance and functioning (Stone 2010; Uzun 2003), as well as low morale (Bowers 2009; Sprigg 2007). Increased exposure to violence from service users is correlated with increased stress and reduced job satisfaction in social care and social work staff (Harris 2012).
Healthcare professionals in the UK are required to manage aggressive or violent incidents using strategies proportionate to the potential or immediate risk posed to self and others, commensurate with the principles of least restrictive practice (DoH 2005). Interventional measures such as physical restraint, rapid tranquillisation (for example, intramuscular injections) and seclusion are used to manage aggression (NICE 2015). The use of specialist nursing care, such as seclusion, is recommended only when the risk to self and others cannot be safely managed in communal or private environments, as containment is often aversive and unpleasant for both service users and staff (Olofsson 1995; Whittington 2009). Seclusion suites used for physical containment are commonly found in psychiatric intensive care units (PICUs) in the UK to manage a range of circumstances, including disruptive behaviour (Oldham 1983), acute psychiatric symptoms (Morrison 1991), verbal and physical aggression (Mason 2001; Sullivan 2004), damage to property (Ahmed 2001), self‐harm (O'Brien 2004), and risk of absconding (Morrison 1997). However, the use of seclusion varies both within and between countries (Bowers 2007; Crenshaw 1995), though rates are poorly reported in terms of specific context (Bowers 2000). However, as these invasive methods are associated with increased risk of injury to service users and staff (Farrell 2005; Hollins 2010), they are usually employed only when de‐escalation is unsuccessful.
To minimise the potential for harm, UK NICE guidance recommends that aggression be promptly defused using de‐escalation techniques as a first resort intervention (NICE 2015).
Description of the intervention
The National Institute for Health and Care Excellence (NICE) guideline on management of violence in healthcare settings describes de‐escalation as "staff members communicating with angry or agitated service users whilst assessing the situation for safety, seeking clarification with the service user and negotiating to resolve the situation in a non‐confrontational manner using emotional regulation and self‐management techniques to control verbal and non‐verbal expressions of anxiety or frustration" (NICE 2015, p 29). The term de‐escalation can be used to refer to any of a broad range of complex verbal and non‐verbal communication skills used by staff in a range of settings to prevent escalation of aggressive behaviour (CRAG 1996). Although de‐escalation training tends to be fairly heterogeneous in terms of the specific techniques taught (Richter 2007), it generally includes the same types of components (Heckemann 2015). De‐escalation techniques can be based on any one of a number of different theoretical models of aggression, but they nevertheless tend to focus on a small number of common aims as follows: for the person conducting the de‐escalation, aims are to project a sense of calm, increase the sense of autonomy of the potentially violent person, and encourage communication between the aggressor; for the person conducting de‐escalation, aims are to convey to the person that they are being listened to and taken seriously and to offer them alternatives to aggression (Price 2012). Recognised de‐escalation techniques include verbal strategies, such as maintaining a calm tone of voice and not shouting or verbally threatening the person. Non‐verbal techniques include an awareness of self, body stance, eye contact and personal safety (Cowin 2003; Johnson 2011). Verbal and non‐verbal communication skills may help to redirect someone to a "calmer personal space" (Cowin 2003). Although de‐escalation is recommended and widely used for managing aggression, there is little literature on specific techniques and efficacy (Richmond 2012; Robertson 2012). The consensus statement from the American Association for Emergency Psychiatry Project BETA De‐escalation Workgroup estimates that effective de‐escalation of an aggressive episode, in order to return the agitated person to a calm state, should take approximately 5 to 10 minutes. De‐escalation, therefore, is intended to ameliorate the immediate aggressive episode and is not associated with benefits in the longer term (Richmond 2012).
De‐escalation is a recommended early intervention for managing aggression in order to prevent escalation to the crisis phase (NICE 2015). Potential benefits to service users (such as improved health and well‐being) from approaches that avoid physical intervention are relatively well established (Paterson 1997; Robertson 2012).
Staff training in de‐escalation techniques is an important feature of aggression management programmes (Farrell 2005). Benefits for service users and staff are currently unclear: studies have reported improvements in staff morale and confidence (Gournay 2001; Nau 2009a), but there appears to be little impact on the frequency of aggressive incidents (Bowers 2006). In North America there are four widely used staff training programmes for the collective management of aggressive behaviour: the Mandt System (Mandt 1998), Non‐violent Crises Intervention (CPI 2005), Professional Assault Response Training (Smith 2004), and Therapeutic Options (Partie 2001). Elsewhere, these approaches are less common.
De‐escalation may be deployed in a range of settings, including accident and emergency, psychiatric hospitals, learning disability services, and custodial settings such as prisons where, for example, de‐escalation training may be embedded in conflict resolution techniques (NHS BSA 2013). The application of de‐escalation techniques may vary by specific context and population, for example, when working with people with a cognitive impairment such as dementia. In the UK, NICE guidelines for managing people with dementia recommend that health and care staff receive specific training in the anticipation of challenging behaviour and violence, including de‐escalation techniques and restraint methods (NCCMH 2015).
How the intervention might work
De‐escalation aims to arrest the progress of the assault cycle during the escalation phase (Kaplan 1983; Leadbetter 1995). Some of the skills and techniques used to arrest the assault cycle include the avoidance of confrontation, attitude and use of language, awareness of personal space and posture. Dix 2008 describes these components in the ACT (assessment, communication and tactics) cyclical model. There are a number of competing theoretical approaches to de‐escalation, but the key recommended components are: recognising the signs of escalating anger and approaching the person in a calm manner (NICE 2015). These techniques may help de‐escalate potentially aggressive situations by establishing a positive relationship between staff and aggressor in the management of appropriate behavioural expectations (Levenson 2004). The interventions may also act as a 'functionally equivalent response', defusing behaviour escalation as understood from a behaviourist perspective (e.g. Shukla‐Mehta 2002). In addition, de‐escalation techniques are likely to increase the self‐efficacy of both the potential aggressor and the staff member, both of which have been associated with reduced aggression (e.g. Dunn 2007; Jonker 2008; Mofrad 2015). De‐escalation techniques are recommended as a frontline response for defusing aggressive or agitated behaviour, but there is no universally accepted model, and the core skill set is poorly documented (Robertson 2012).
Why it is important to do this review
In the UK, the Winterbourne Enquiry into the abuse of patients in learning disability services, including inappropriate use of physical interventions and restraints, resulted in increased pressure on all mental health and learning disability care settings to find safe alternatives to physical intervention (CQC 2011). Evidence on the effectiveness of alternative methods for managing aggressive behaviour, other than with physical intervention such as restraint and seclusion, is unclear. Muralidharan 2006 suggests that evidence is inconclusive due to lack of high‐quality studies, and Gaskin 2007 argues for strong evidence in favour of alternative approaches on the basis of all available evidence. Although a number of guidelines for managing aggressive behaviour recommend de‐escalation techniques (for example, those of NICE or the American Psychological Association), there is no standard approach for the technique, and little published research compares the effectiveness of different methods or the effectiveness of de‐escalation training (Paterson 1997).
Improved staff morale and confidence have been reported as potential benefits of de‐escalation training (Cowin 2003), but evidence of impact on staff outcomes is currently unclear. Alternatives to physical intervention are associated with reduced risk of injury for both staff and patients (Hill 1987; Johnson 2012), but the relative effectiveness of different approaches to de‐escalation, in terms of both staff and patient outcomes, is also unclear. Therefore, there is a need to systematically review the evidence for the effectiveness of de‐escalation for managing aggression. A Cochrane Review evaluating de‐escalation techniques for psychosis‐induced aggression did not identify any eligible studies (Rao 2017). We propose a companion and complementary review that will evaluate techniques for people without psychosis.
Objectives
To assess the effects of de‐escalation techniques for managing non‐psychosis‐induced aggression in adults in care settings, in both staff and service users.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐RCTs (defined as trials where participants are allocated to study groups using, for example, date of birth or alternate allocation).
Types of participants
Adults (aged 18 years or more) in any care setting who use threatening or aggressive behaviour.
We excluded service users with a diagnosis of schizophrenia spectrum disorder or any other psychosis (APA 2013). A separate Cochrane Review covers people with psychosis‐induced aggression (Rao 2017). The definition of psychosis, according to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5) published in 2013, also includes drug‐induced psychosis (APA 2013).
Types of interventions
Experimental intervention
Any de‐escalation technique, as defined by NICE 2015 (described in the Description of the intervention section above).
Comparison intervention
Standard practice (including rapid tranquillisation, physical intervention, seclusion)
An alternate de‐escalation technique; for example, the Mandt System (Mandt 1998), Non‐violent Crises Intervention (CPI 2005), Professional Assault Response Training (Smith 2004), or Therapeutic Options (Partie 2001), as described in the Background section
Types of outcome measures
Effects of de‐escalation may be apparent after a period of a few minutes to several hours. The distinction between successful de‐escalation of the primary aggressive event and subsequent events may be complex, and we therefore collected outcome data at a range of follow‐up points that best reflected the available evidence from the included study.
Primary outcomes
Frequency of aggression‐related, serious untoward incidents (including mortality) leading to physical restraint or seclusion, or both, recorded in staff reports or routinely collected data
Frequency of aggression‐related injuries to staff, recorded in staff reports or routinely collected data such as untoward incident forms
Secondary outcomes
Length of stay in seclusion, recorded in staff reports or routinely collected data such as untoward incident forms
Validated (psychometric publication of scale properties; Streiner 2008; Zumbo 2007) generic or condition‐specific quality of life scales (for example, Short Form 36 Health Survey (SF‐36; Ware 1992), De‐escalating Aggressive Behaviour Scale (DABS; Mavandadi 2016; Nau 2009b), or both)
Staff absenteeism, based on administrative data
Costs of care, including cost‐benefit and cost‐effectiveness; for example, monetary benefit or quality‐adjusted life years (QALYs)
We prioritised outcomes based on formally or routinely collected data such as untoward incident or adverse event forms.
Search methods for identification of studies
Electronic searches
We ran the first set of searches in February 2016 and updated them between September and October 2017. We searched the electronic resources listed below, using the strategies in Appendix 1. We did not apply any language or time period restrictions to the searches.
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 8) in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register (searched 27 September 2017).
MEDLINE Ovid (1946 to September week 2, 2017; searched 27 September 2017).
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid (searched 27 September 2017).
MEDLINE Epub Ahead of Print Ovid (searched 27 September 2017).
Embase Ovid (1974 to September 26 2017: searched 27 September 2017).
PsycINFO Ovid (1806 to September week 3, 2017).
CINAHL EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1937 to 27 September 2017).
Science Citation Index ‐ Expanded Web of Science (SCI‐Expanded; 1970 to 27 September 2017).
Social Sciences Citation Index Web of Science (SSCI; 1970 to 27 September 2017).
Conference Proceedings Citation Index ‐ Science Web of Science (CPCI‐S; 1990 to 27 September 2017).
Conference Proceedings Citation Index ‐ Social Sciences & Humanities Web of Science (CPCI‐S; 1990 to 27 September 2017).
SciELO Citation Index Web of Science (Scientific Electronic Library Online; 1997 to 27 September 2017).
International Bibliography of the Social Sciences ProQuest (1951 to 27 September 2017).
British Education Index EBSCOhost (BEI; 1974 to 27 September 2017).
ERIC EBSCOhost (Education Resources Information Center; 1966 to 27 September 2017).
Cochrane Database of Systematic Reviews (CDSR; 2017, Issue 9) in the Cochrane Library (searched 27 September 2017).
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 2; final issue) in the Cochrane Library (searched 22 February 2016).
Criminal Justice Abstracts EBSCOhost (all available years; searched 27 September 2017).
Academic Search Complete EBSCOhost (1990 to 9 October 2017).
OpenGrey (opengrey.eu; searched 9 October 2017).
Campbell Collaboration Library of Systematic Reviews (www.campbellcollaboration.org/library.html; searched 9 October 2017).
ClinicalTrials.gov (clinicaltrials.gov; searched 9 October 2017).
ISRCTN (ISRCTN.com; searched 9 October 2017).
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; apps.who.int/trialsearch; searched 9 October 2017).
Searching other resources
We examined the reference lists of relevant studies and reviews for any additional trials not identified by the electronic searches listed above. We contacted authors of identified trials, as well as authorities in the field, in order to locate other published and unpublished studies.
Data collection and analysis
As we identified only one study that met our inclusion criteria, we report below only the methods required. Full details of the methods agreed for this review can be found in our protocol, Spencer 2016, and Table 2 ('Additional methods' table).
1. Unused methods.
| Unused method | Approach |
| Measures of treatment effects |
Continuous data Where different studies use the same outcome measure, we will use the mean difference (MD). If studies use different scales to measure the same outcome (for example, level of aggression), we will use the standardised mean difference (SMD) and its 95% CI, ensuring a consistent direction of effect by reversing scaling where necessary, supported by a statement in the text on direction of interpretation. If standard deviations (SD) are not reported but other measures of variance around the mean differences, such as standard error, CIs, or P value are reported, we will calculate these according to Section 7.3 in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). |
|
Binary data For dichotomous data, we will use risk ratios (RR) with 95% CIs. | |
| Unit of analysis issues |
Cross‐over trials We will only use data from the first, pre‐cross‐over phase to minimise potential bias from carry‐over effects. |
|
Cluster‐randomised trials We will analyse cluster‐randomised trials in accordance with methods described in Section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c), using the average cluster size and an estimate of the intraclass correlation coefficient (ICC) to adjust sample sizes to the 'effective sample size'. Where an estimate of the ICC is not available from the trial, we will use an estimate from a similar trial or a trial with a similar population. We will combine single RCTs with cluster‐RCTs only where the designs and interventions are considered sufficiently similar and the effect of the intervention unlikely to be influenced by the method of randomisation. | |
|
Multiple arm trials For trials with more than two arms, we will describe all study groups in the Characteristics of included studies but will only include in analyses the intervention groups that meet our review criteria (Criteria for considering studies for this review). Where the variance of the difference between the intervention and the comparator is not reported, we will calculate this from the variances of all trial arms. Where a study compares multiple relevant interventions groups to one eligible control group, we will divide the sample size for the shared comparator group evenly, in order to prevent the same participants from being included twice. Where a study compares one eligible intervention group to two or more distinct but eligible control groups, we will combine the groups to create a single, pairwise control comparison (Higgins 2011c). For dichotomous outcomes, we will sum both the sample sizes and the numbers of people with events across groups; and for continuous or time‐to‐event outcomes, we will combine means and SDs using methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c). Where this prevents identification of potential heterogeneity, we will compare each group separately as part of subgroup analyses. | |
| Dealing with missing data | Where a particular outcome includes substantial loss to follow‐up (50%), we will report this in the text, marking the data with an asterisk. Where trials include analyses based on the imputation of missing values, we will include data at low risk of bias and report data separately for those at higher risk of bias in the text of the review. Where missing data are related to the outcome it is not considered appropriate to impute data using carry‐forward methods such as last observation carried forward or baseline observation carried forward; for example, if a participant died due to an intervention‐related adverse event shortly after randomisation, it would not be appropriate to carry forward baseline data in order to complete missing data (Gewandter 2014). Where studies report per protocol data (that is, only those who completed the study), we will contact the authors for unreported data on all study participants, including those lost to follow‐up. If there are sufficient trials, we will use sensitivity analyses to determine the resistance of our results to the effects of missing data. |
| Assessment of heterogeneity | In this review, there is a strong likelihood of considerable variability between studies, in terms of the specification of the intervention, the study design and the outcomes. This variability may be attributable to clinical variation in the population or the intervention, differences in study quality, or random differences. We will assess potential sources of variability between studies in the following ways.
|
| Assessment of reporting biases | We will compare the results of data from published and unpublished studies as a direct test of publication bias. If we find a sufficient number of studies (approximately 10 or more), we will explore potential bias arising from small study effects using Egger's method, to test for asymmetry in funnel plots (Egger 1997). If smaller studies show larger intervention effects compared to larger studies, we will evaluate potential causes (for example, poor methodological quality; differences in populations or interventions) and report studies at high risk of bias in the text of the review. If we detect small study effects, we will explore whether this is due to heterogeneity (small studies give larger effects because they differ from large ones in some aspect that modifies the effect of the intervention) or because of poor quality, publication bias, etc. |
| Data synthesis | We will undertake separate meta‐analyses for the comparisons of interest in this review (de‐escalation versus physical intervention; de‐escalation A versus de‐escalation method B). We will include studies in meta‐analyses where the study designs, interventions and outcomes are similar. Where we identify substantial heterogeneity (> 50%; Deeks 2011), we will report outcomes in the text, giving the direction and the size of the effect along with strength of the evidence (risk of bias). It is likely that included studies will vary in their population, design and outcomes, and therefore data synthesis using meta‐analysis with a random‐effects model will be the most appropriate. However, where there are few studies or the effects of interventions across studies are not randomly distributed (for example, with publication bias), the random‐effects model estimates may be unreliable or biased. It was considered likely that this review would only include a small number of low‐powered studies, where meta‐analysis with a fixed‐effect model would give more reliable estimates. To resolve the uncertainty over model choice, we will only pool data using meta‐analysis where studies appear sufficiently similar (for example, all dementia populations or all learning disability), and we will compare pooled data estimates from both a random‐effects model and a fixed‐effect model, reporting both in the text. We will report the mean effect estimate and the CI around the estimate for both models. We will synthesise and report dichotomous and continuous data separately for a given outcome, should the need arise. We will report and analyse end‐of‐study point estimates and change from baseline scores separately. We will perform analyses using Review Manager 5 (Review Manager 2014). We will interpret with caution the results of analyses of head‐to‐head comparisons of de‐escalation techniques in the absence of data from trials comparing de‐escalation techniques versus physical intervention. |
| Subgroup analysis and investigation of heterogeneity |
Subgroup analysis If we find at least 10 trials (Deeks 2011), we will conduct subgroup analyses by staff training (trained versus untrained staff). Investigation of heterogeneity We will manage potential sources of heterogeneity as follows.
We will fully discuss and report our decisions in the review. |
| Sensitivity analysis | We will conduct sensitivity analyses for missing data, and for risk of bias based on random sequence generation, blinding of participants and incomplete outcome data, by including and excluding studies at high risk of bias and comparing the results. Although few data are available on the measurement of outcomes following de‐escalation of aggressive episodes, it is plausible that outcomes may vary by duration of follow‐up. Therefore, we will explore potential heterogeneity between studies according to length of follow‐up (that is, all studies versus excluding the longest studies). |
CI: confidence interval; MD: mean difference; RCTs: randomised controlled trials; SD: standard deviation; SMD: standardised mean difference.
Selection of studies
Two review authors (ICS and PJ) independently assessed the titles and abstracts of all records retrieved by the search for eligibility. The same two reviewers then examined the full texts of all reports identified as potentially relevant against the inclusion criteria (Criteria for considering studies for this review). We discussed any disagreements as a team (IC, PJ, SS), until reaching a consensus. We recorded our decisions in a PRISMA diagram (Moher 2009).
Data extraction and management
ICS and PJ independently read and extracted data from the included study using a form based on the predefined outcome measures (Types of outcome measures). We contacted the study authors for information on missing data or further information about the trial (see Dealing with missing data). We systematically recorded information on study design, participants, intervention, outcomes, methods, results and study withdrawals in the Characteristics of included studies table. We discussed any disagreements as a team (IC, PJ, SS) until reaching a consensus.
Assessment of risk of bias in included studies
Using the 'Risk of bias' criteria described in Higgins 2011a and set out in Table 3, two review authors (ICS and PJ) independently assessed the risk of bias of the included study as high, low or unclear, across the following seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. We discussed disagreements as a team (ICS, PJ, SS) until reaching a consensus. The results are presented in a 'Risk of bias' table, beneath the Characteristics of included studies table.
2. 'Risk of bias' criteria.
Random sequence generation
|
Allocation concealment
|
Blinding of participants and personnel
|
Blinding of outcome assessment
|
Incomplete outcome data
|
Selective reporting
|
Other bias
|
Measures of treatment effect
Continuous data
We estimated the intervention effect using the mean difference (MD) and its 95% confidence interval (CI). For additional methods to manage continuous data, please see our protocol, Spencer 2016, and Table 2.
Dealing with missing data
We contacted the authors of the included study to provide any unreported data such as missing outcomes, missing data, means or SDs. We noted differential dropout between study groups and reasons for withdrawal. We noted differential missing data and reasons for missing data, where reported. We used available cases for data analysis and did not impute missing data. We considered multiple imputation methods that included sensitivity analyses, pre‐specified in published protocols, to be at low risk of bias (Gewandter 2014; Little 2012). Missing data are described in the 'Risk of bias' table, and we discuss their influence on study outcomes in the text.
For additional methods to manage missing data, please see our protocol, Spencer 2016, and Table 2.
Assessment of reporting biases
To assess outcome reporting bias, we searched for trial protocols and compared planned versus reported outcome measures. We were unable to assess publication bias and other small study effects, as the review included only one study. Please see our protocol, Spencer 2016, and Table 2 for methods to assess reporting bias archived for use in future updates of this review.
Data synthesis
Given that this review includes only one study, we provide a narrative description of the study's results. For methods to synthesise data in future updates of this review, please see our protocol, Spencer 2016, and Table 2.
Summary of findings
We report both primary outcomes (frequency of aggression‐related, serious untoward incidents and frequency of aggression‐related injuries to staff) and one secondary outcome (validated generic or condition specific, or both, quality of life scales), in a 'Summary of findings' table for the following comparison: de‐escalation compared to standard care for managing aggression. We also report findings (mean change scores from baseline to 20 weeks) on a number of other outcomes in this table, notably agitated behaviour, physically aggressive behaviour, and verbally aggressive behaviour (see Differences between protocol and review). In addition to listing the important outcomes in this table, we present the illustrative mean on the control intervention, the absolute magnitude of effect, the number of participants and studies included for each outcome, and our ratings of the overall quality of evidence (see Table 4).
3. GRADE Working Group grades of evidence.
| Quality rating | Description |
| High | We are very confident that the true effect lies close to that of the estimate of the effect. |
| Moderate | We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. |
| Low | Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. |
| Very low | We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. |
Two reviewers (ICS and PJ) assessed the quality of the evidence using the GRADE approach, which considers within‐study risk of bias, directness of evidence, heterogeneity, precision of effect estimates, and risks of publication bias (GRADE 2004). We discussed any disagreements as a team (IC, PJ, SS) until reaching a consensus. We tabulated the 'Summary of findings' table using GRADEpro software (GRADEPro GDT 2015).
Results
Description of studies
Results of the search
We identified 6637 unique records of potentially relevant studies. Of these, we excluded 6610 as irrelevant following inspection of their titles and abstracts. We obtained and read the full texts of the remaining 27 records and formally excluded a further 25 reports that did not meet our review inclusion criteria (see Excluded studies). We included one study in the review, Deudon 2009, and identified one study as ongoing (ACTRN12614000735651). See Characteristics of included studies and Characteristics of ongoing studies.
See Figure 1 for the study flow diagram.
1.
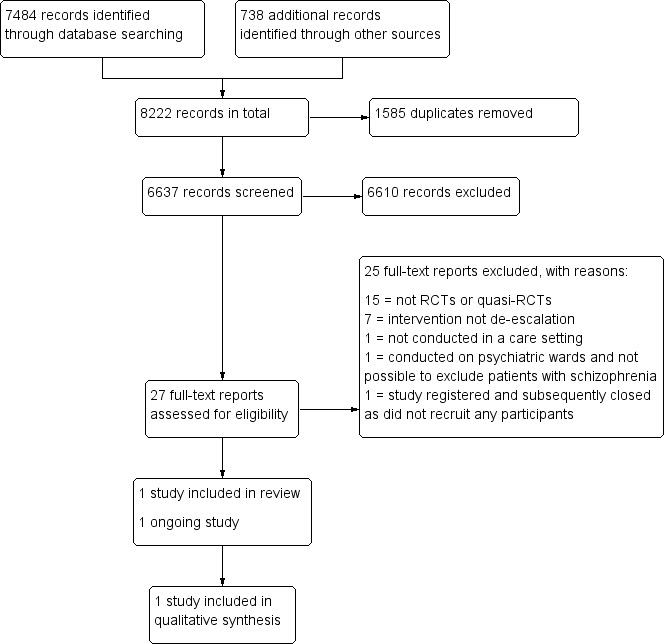
Study flow diagram.
Included studies
Study design
The one included study (306 participants) was a cluster‐randomised controlled trial involving 16 nursing homes in France between 2007 and 2008 (Deudon 2009).
Participants
All patients were diagnosed with dementia according to the International Classification of Diseases, 10th Revision (ICD‐10) criteria (WHO 1992), had a Mini Mental State Examination (MMSE) score of 24 or less, and had recorded behavioural and psychological symptoms of dementia at least once a week. Participants in the intervention group had a mean age of 86.5 years, and 23% were men. Participants in the control group had a mean age of 86 years, and 21.2% were men.
Authors did not report the characteristics of staff trained by the programme.
Intervention
The study assessed the effects of a staff training programme that comprised a 90‐minute teaching session on behavioural problems in dementia, the use of four instruction cards on managing key behaviours, and 24 hours of one‐to‐one support over a two‐month period.
Comparison
The control group received usual care.
Outcomes
Patients were followed up for a total of three months after the training period, with study measurements at baseline, 8 weeks (end of training) and 20 weeks (end of three‐month follow‐up). The study reported on two validated psychometric outcome measures: the Cohen‐Mansfield Agitation Inventory and the Neuropsychiatric Inventory (Cohen‐Mansfield 1995; Cummings 1994), as well as an observation scale derived from the Agitated Behaviour Mapping Instrument developed by Cohen‐Mansfield 1990.
The study did not measure our review's primary outcomes (frequency of aggression‐related, serious untoward incidents and frequency of aggression‐related injuries to staff) or secondary outcomes (length of stay in seclusion, staff absenteeism and costs of care). For quality of life, the measure used in the study did not include an outcome in a relevant domain and therefore was not eligible for inclusion in the review. We report behavioural measurement scales not established a priori but which we considered relevant to the aims of the review, as described below.
The Cohen‐Mansfield Agitation Inventory is widely used in nursing homes (Cohen‐Mansfield 1995). It examines the frequency of 29 types of agitated behaviour, including pacing, verbal or physical aggression, performing repetitious mannerisms, screaming and general restlessness. Each of the 29 behaviours are rated on a seven‐point scale (1 = never occurs to 7 = occurs several times an hour). Deudon 2009 reports a Global score (sum of individual item ratings; range = 29 to 203), and mean scores (evaluable items (rated on the same seven‐point scale) divided by the theoretical total number of items) for the following four domains: Physically Non‐Aggressive Behaviour, such as pacing (13 items); Verbally Non‐Aggressive Behaviour, such as repetition (four items); Physically Aggressive Behaviour, such as hitting (nine items); and Verbally Aggressive Behaviour, such as swearing (three items).
The Neuropsychiatric Instrument by Cummings 1994 is a 12‐item measure used to evaluate the frequency (1 = occasional, less than once a week to 4 = very frequent) and severity (1 = mild to 3 = severe) of behavioural and neuropsychiatric symptoms, including agitation and aggression, depression, anxiety, apathy, and aberrant motor behaviour. The product of frequency and severity ranges from 1 to 12 for each of 10 domains, with a total score ranging from 12 to 120. It includes four domain scores: Psychotic (items on hallucinations and delusions); Hyperactivity (items on agitation, irritability and aberrant motor behaviour); Apathy; and Affective. A lower score indicates fewer behaviours. Deudon 2009 used only the Psychotic and Hyperactivity scales.
Deudon 2009 specifically developed an observation scale to directly observe patient behaviours. It was derived from the Agitated Behaviour Mapping Instrument developed by Cohen‐Mansfield 1990 and focuses on agitation. The scale includes 25 items describing positive behavioural and psychological symptoms of dementia, such as screaming, hitting, tearing and biting, scored following three minutes of observation by clinical raters. Higher scores indicate more severe behaviours.
Excluded studies
We excluded a total of 25 studies from this review: 15 studies because they were not RCTs or quasi‐RCTs (Adams 2017; Allen 2000; Andersen 2017; Bowers 2003; Burns 2015; Cailhol 2007; Cowin 2003; DRKS00009723; Hallett 2015; Loi 2017; Martinez 2017; Small 2006; Üzar 2017; Valimaki 2017; Yeh 2001); 7 studies because the intervention was not de‐escalation (Huizing 2006; Kuske 2009; Proctor 1999; Testad 2005; Testad 2010; Testad 2016; Zwijsen 2014); and 1 study each for not taking place in a care setting (Cleary Bradley 2012); taking place on psychiatric wards where it was not possible to exclude patients with schizophrenia (communication with authors) (Bowers 2015); and not recruiting any patients (and subsequently being closed) despite being registered (communication with authors) (Hitchen 2007). See Characteristics of excluded studies.
Ongoing studies
One study, ACTRN12614000735651, is ongoing. This study plans to compare a bespoke training programme with a training programme based on UK NICE violence management guidelines for staff working in healthcare and disability settings. See Characteristics of ongoing studies.
Risk of bias in included studies
See the 'Risk of Bias' table (under the Characteristics of included studies table) and Figure 2 for more information.
2.
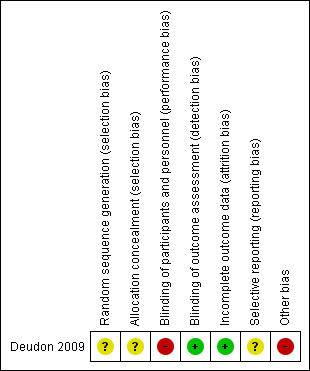
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We judged the Deudon 2009 study to be at unclear risk of bias for random sequence generation and allocation concealment, as authors provided insufficient information for either domain. We contacted the authors for more information but have not yet received a response. Potentially eligible patients were identified prior to within‐cluster selection, to minimise selection bias.
Blinding
Performance bias
We judged the Deudon 2009 study to be at high risk of performance bias, as the intervention was not concealed from either those providing the training or staff receiving the training.
Detection bias
We considered the risk of detection bias in the Deudon 2009 study to be low, as assessments were performed by independent raters blinded to group allocation.
Incomplete outcome data
We judged the risk of attrition bias in this study as low because the small number of participants lost to follow‐up was balanced between study groups and therefore unlikely to have introduced bias (Deudon 2009).
Selective reporting
We judged the study to be at unclear risk of reporting bias because we could not locate a trial protocol through searches or by contacting the study authors (Deudon 2009).
Other potential sources of bias
We judged the Deudon 2009 study to be at high risk of other bias for two reasons: lack of clarity with regard to why clusters were imbalanced and there were unequal numbers of participants between groups, and because baseline scores on all outcomes were significantly worse in the intervention group compared to the control group. As the study authors noted, the method of randomisation may have influenced the effects of the intervention.
Effects of interventions
See: Table 1
Comparison 1: de‐escalation versus standard care
Primary outcomes
Deudon 2009 did not measure either of our primary outcomes: frequency of aggression‐related serious untoward incidents and frequency of aggression‐related injuries to staff.
Secondary outcomes
Deudon 2009 did not report any of our secondary outcomes using measurement standards set out in our published protocol (Spencer 2016), namely:
length of stay in seclusion, recorded in staff reports or routinely collected data such as untoward incident forms;
validated (psychometric publication of scale properties; Streiner 2008; Zumbo 2007) generic or condition‐specific quality of life scales (for example, Short Form 36 Health Survey (SF‐36; Ware 1992) or De‐escalating Aggressive Behaviour Scale (DABS; Nau 2009b; Mavandadi 2016)), or both;
staff absenteeism, based on administrative data; and
costs of care, including cost‐benefit and cost‐effectiveness; for example, monetary benefit or quality‐adjusted life years (QALYs).
The authors reported MDs for an outcome described as 'quality of life' in the Results section of the paper, but further information on the specific measurement scale, its psychometric properties or a description of the scaling range were not provided. We were therefore unable to include it in the review. However, the authors did examine the impact of de‐escalation training on patient behaviour using three different scales (Deudon 2009).
Using the Cohen‐Mansfield Agitation Inventory (Cohen‐Mansfield 1995), which consists of 29 items rated on a 7‐point scale (ranging from 1 = never occurs to 7 = occurs several times an hour; lower scores = fewer behaviours), the Global score (range = 29 to 203), and mean scores (evaluable items divided by the theoretical total number of items) for the Physically Non‐Aggressive, Verbally Non‐Aggressive, Physically Aggressive and Verbally Aggressive domains were not significantly different at the end of the 20‐week follow‐up period (Global: MD −0.54 points, 95% CI −4.44 to 3.36; Physically Non‐Aggressive: MD −0.09 points, 95% CI −0.25 to 0.07; Verbally Non‐Aggressive: MD −0.14 points, 95% CI −0.36 to 0.08; Physically Aggressive: MD 0.10 points, 95% CI −0.06 to 0.26; Verbally Aggressive: MD 0.14 points, 95% CI −0.15 to 0.43). However, improvements in the Global score, and Physically Non‐Aggressive, Verbally Non‐Aggressive and Verbally Aggressive mean scores from baseline to 20 weeks were significantly greater in the intervention group compared to the control group (Global: change MD −5.69 points, 95% CI −9.59 to −1.79; Physically Non‐Aggressive: change MD −0.32 points, 95% CI −0.49 to −0.15; Verbally Non‐Aggressive: change MD −0.44 points, 95% CI −0.69 to −0.19; Verbally Aggressive: change MD −0.44 points, 95% CI −0.69 to −0.19). Changes in Physically Aggressive mean scores from baseline to 20 weeks were not significantly different between groups (MD −0.08 points, 95% CI −0.37 to 0.21).
Using the 12‐point Psychotic and Hyperactivity scales of the Neuropsychiatric Inventory, mean scores were not significant at 20 weeks (Psychotic: MD 2.18 points, 95% CI −0.61 to 4.97; Hyperactivity: MD 2.67 points, 95% CI −9.58 to 14.92), and changes in scores from baseline to 20 weeks were not significantly different between groups (Psychotic: change MD −1.78 points, 95% CI −4.36 to 0.80; Hyperactivity: change MD −14.09 points, 95% CI −26.52 to −1.66).
Using the 25‐point Observation Scale, mean scores at 20 weeks and mean changes in scores from baseline to 20 weeks were not significantly different between intervention and control groups (MD −2.33 points, 95% CI −5.80 to 1.14; change MD −7.92 points, 95% CI −13.19 to −2.65).
As noted by the study authors, with the exception of Verbally Aggressive scores on the Cohen‐Mansfield Agitation Inventory, all three scales and subscales were significantly worse in the intervention group at baseline. None of the planned analyses in the trial controlled for these baseline differences.
As stated, it was not possible to compile a 'Summary of findings' table for our pre‐specified outcomes, as none were included in the review. However, we considered the following behavioural scales as most relevant to the aims of the review and have included these in a 'Summary of findings' table using GRADE guidelines.
Cohen‐Mansfield Agitation Inventory: Global, Physically Aggressive, and Verbally Aggressive scales.
Neuropsychiatric Inventory: Hyperactivity.
Observation Scale.
We judged the evidence for all outcomes to be of very low quality. See Table 1.
Comparison 2: de‐escalation A versus de‐escalation B
The one study included in this review, Deudon 2009, did not compare one type of de‐escalation with another. One ongoing study, ACTRN12614000735651, aims to compare two different staff training programmes for managing de‐escalation (see Characteristics of ongoing studies).
Discussion
Summary of main results
Following an extensive search we identified only one study, Deudon 2009, which met our inclusion criteria (Criteria for considering studies for this review). Currently, there is insufficient evidence to determine the effectiveness of de‐escalation for managing aggression in people in care settings. The study did not measure any of our pre‐specified outcomes (Types of outcome measures), and of the three behavioural outcomes that we included, only one scale suggested limited benefit for people who received care from staff trained in de‐escalation techniques. Using the GRADE approach, we deemed the evidence for these outcome measures to be of very low quality.
Overall completeness and applicability of evidence
Our comprehensive search for RCTs on de‐escalation techniques for managing aggression identified only one study, comparing staff training with standard care for people with dementia living in nursing homes in France. The study did not report details of staff delivering the intervention and did not include any staff‐centred outcome measures. We identified one ongoing study assessing the effectiveness of two different staff training programmes for managing people in care settings in New Zealand, but it is currently unclear whether this study is progressing. We found no relevant studies that assessed de‐escalation in other settings, such as primary or secondary healthcare, or compared different types of de‐escalation or measured the impact of de‐escalation techniques on staff. Therefore, there is insufficient evidence on which to base a judgement of whether this intervention is an effective technique for managing aggression.
Quality of the evidence
There was a relatively high risk of bias in our included study due to lack of clarity in the method of randomisation and significant baseline imbalances in the outcome measures that were unaccounted for in the effect estimates. The potential impact of cluster randomisation was acknowledged by the study authors, but risks of bias across other domains was difficult to judge based on the information provided in the published paper alone.
According to our GRADE assessment, the overall quality of the evidence in the review is very low. This was primarily due to the small number of studies, the potential impact of cluster randomisation on the effect estimates leading to imprecise results, and indirectness of the outcomes.
Potential biases in the review process
To minimise our risk of bias during the review process, we made every effort to follow the protocol, but we identified only one study for inclusion. We judged that the study did not include an outcome in a relevant quality of life domain, so we did not include this outcome in the review. We included an observation scale that was derived by the study investigators, based on a validated measure, which was clearly described in the study methods. We excluded one study of patients on psychiatric wards because we could not rule out a diagnosis of schizophrenia (one of our review exclusion criteria, see Criteria for considering studies for this review), based on communication with the study authors (Bowers 2015). We judged a number of domains in the 'Risk of bias' assessment for the included study to be at unclear risk, but despite contacting the study authors for clarification, we had not received a reply at the time of writing (Deudon 2009).
Agreements and disagreements with other studies or reviews
To date, only one published Cochrane Review has focused on the use of de‐escalation techniques for managing psychosis‐induced aggression (Rao 2017). The review did not include any studies, and review authors also found no ongoing studies. Hockenhull 2012 evaluated prevention and intervention strategies for violent behaviour that included a broad range of pharmacological, psychological, and other interventions. Of the 51 RCTs included in the review, none included de‐escalation techniques. The results of our review are in broad agreement with the findings of these reviews in concluding that there is insufficient evidence to determine whether de‐escalation techniques are effective for reducing aggression.
Authors' conclusions
Implications for practice.
In the absence of robust evidence from clinical trials, and with the need to provide guidance on this topic, UK NICE guidance recommends the use of de‐escalation techniques for managing aggression and violence based on experience in clinical practice (NICE 2015; NCCMH 2015). The limited evidence included in this review means that uncertainty remains around the effectiveness of de‐escalation techniques in clinical practice. However, we acknowledge that given the urgent need to reduce harms arising from the use of physical restraint procedures, de‐escalation is likely to continue.
Implications for research.
This review and the companion review by Rao 2017 highlight the need for high‐quality research on the effectiveness of de‐escalation techniques. High‐quality RCTs, designed and reported according to current guidelines (Chan 2013; Loudon 2015; Rennie 2001), are required to inform the evidence base and provide robust recommendations for practice. Future research should also provide clear details of study methods with regard to patients, interventions, comparison group and selected outcome measures (PICO), with particular emphasis on clear and transparent reporting of study methods. When considering the choice of outcome measures, it is also important to report the impact of interventions on service users and staff delivering the intervention, with respect to both benefits and risks. Investigators should also ensure that selected patient‐ or staff‐reported outcome measures carry appropriate psychometric credentials. We identified few studies evaluating this intervention, which may reflect its common use in clinical practice and the difficulty of conducting research on such a volatile and unpredictable topic. Nonetheless, high‐quality research in this area is urgently needed and should be an important priority for commissioners.
Acknowledgements
We would like to the thank the Cochrane Developmental, Psychosocial and Learning Problems Editorial Team for their support during preparation of the review.
We would like to thank Edge Hill University (SS employer), Lancaster University (ICS employer) and Mersey Care NHS Foundation Trust (PJ former employer) for their support. The views expressed are those of the authors and not necessarily those of the National Health Service or the Department of Health.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register
Searched 22 February 2016 [553 records] Searched 27 September 2017. Deduplicated with previous records [145 records]
#1[mh ^Aggression] #2[mh ^"Psychomotor agitation"] #3[mh ^"Agonistic behavior"] #4[mh Violence] #5[mh "Workplace Violence"] #6[mh Anger] #7[mh Hostility] #8(aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*) #9((abusive or challenging or disturbed or disruptive) near/1 behav*) #10{or #1‐#9} #11[mh "Risk management"] #12[mh "Behavior control"] #13[mh "Safety management"] #14[mh "Security measures"] #15(de next escalat* or deescalat* or non next escalat* or nonescalat* or defus* or de next fus*) #16(non* next (authorit* or avers* or coerc* or co next erc* or combativ* or confrontation* or physical or provocative or violen*)) #17(non* next (drug* or pharma*)) #18((alternative* or avoid* or reduc* or without*) near/3 (seclusion or restrain*)) #19(talkdown or talk‐down or "one to one") #20(limit* near/1 setting) #21[mh Negotiating] #22negotiat* #23((verbal* or nonverbal* or non next verbal*) near/3 (communicat* or intervention* or strateg* or method* or technique*)) #24[mh "Crisis intervention"] #25((crisis or crises) near/3 (intervention* or manag* or resol* or respon* or team*)) #26(conflict near/3 (avoid* or manage* or prevent* or resol*)) #27(calm or calming) #28{or #11‐#27} #29 #10 and #28 in Trials
MEDLINE Ovid
Searched 22 February 2016 [1284 records] Searched 27 September 2017. Deduplicated with previous records [161 records]
Lines 29 to 39 form the Cochrane highly sensitive search strategy for identifying randomised trials in Medline (Lefebvre 2011).
1 Aggression/ 2 Psychomotor agitation/ 3 Agonistic Behavior/ 4 Violence/ 5 Workplace Violence/ 6 exp Anger/ 7 Hostility/ 8 (aggress$ or agitat$ or agonistic or anger or angry or assault$ or hostil$ or rage or threat$ or violen$).tw. 9 ((abusive or challenging or disturbed or disruptive) adj1 behav$).tw. 10 or/1‐9 11 Risk management/ 12 Behavior control/ 13 Safety management/ 14 Security measures/ 15 (de‐escalat$ or deescalat$ or non‐escalat$ or nonescalat$ or defus$ or de‐fus$).tw. 16 (non$ adj (authorit$ or avers$ or coerc$ or co‐erc$ or combativ$ or confrontation$ or physical or provocative or violen$)).tw. 17 (non$ adj (drug$ or pharma$)).tw. 18 ((alternative$ or avoid$ or reduc$ or without$) adj3 (seclusion or restrain$)).tw. 19 (talkdown or talk‐down).tw. 20 (limit$ adj1 setting).tw. 21 Negotiating/ 22 negotiat$.tw. 23 ((verbal$ or nonverbal$ or non‐verbal$) adj3 (communicat$ or intervention$ or strateg$ or method$ or technique$)).tw. 24 Crisis intervention/ 25 (cris#s adj3 (intervention$ or manag$ or resol$ or respon$ or team$)).tw. 26 (conflict adj3 (avoid$ or manage$ or prevent$ or resol$)).tw. 27 (calm or calming).tw. 28 or/11‐27 29 randomized controlled trial.pt. 30 controlled clinical trial.pt. 31 randomi#ed.ab. 32 placebo$.ab. 33 drug therapy.fs. 34 randomly.ab. 35 trial.ab. 36 groups.ab. 37 or/29‐36 38 exp animals/ not humans.sh. 39 37 not 38 40 10 and 28 and 39
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid
Searched 27 September 2017 [161 records]
1 (aggress$ or agitat$ or agonistic or anger or angry or assault$ or hostil$ or rage or threat$ or violen$).tw. 2 ((abusive or challenging or disturbed or disruptive) adj1 behav$).tw. 3 or/1‐2 4 (de‐escalat$ or deescalat$ or non‐escalat$ or nonescalat$ or defus$ or de‐fus$).tw. 5 (non$ adj (authorit$ or avers$ or coerc$ or co‐erc$ or combativ$ or confrontation$ or physical or provocative or violen$)).tw. 6 (non$ adj (drug$ or pharma$)).tw. 7 ((alternative$ or avoid$ or reduc$ or without$) adj3 (seclusion or restrain$)).tw. 8 (talkdown or talk‐down).tw. 9 (limit$ adj1 setting).tw. 10 negotiat$.tw. 11 ((verbal$ or nonverbal$ or non‐verbal$) adj3 (communicat$ or intervention$ or strateg$ or method$ or technique$)).tw. 12 (cris#s adj3 (intervention$ or manag$ or resol$ or respon$ or team$)).tw. 13 (conflict adj3 (avoid$ or manage$ or prevent$ or resol$)).tw. 14 (calm or calming).tw. 15 or/4‐14 16 3 and 15 17 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. (711525) 18 16 and 17
MEDLINE Epub Ahead of Print Ovid
Searched 27 September 2017 [108 records]
1 (aggress$ or agitat$ or agonistic or anger or angry or assault$ or hostil$ or rage or threat$ or violen$).tw. 2 ((abusive or challenging or disturbed or disruptive) adj1 behav$).tw. 3 or/1‐2 4 (de‐escalat$ or deescalat$ or non‐escalat$ or nonescalat$ or defus$ or de‐fus$).tw. 5 (non$ adj (authorit$ or avers$ or coerc$ or co‐erc$ or combativ$ or confrontation$ or physical or provocative or violen$)).tw. 6 (non$ adj (drug$ or pharma$)).tw. 7 ((alternative$ or avoid$ or reduc$ or without$) adj3 (seclusion or restrain$)).tw. 8 (talkdown or talk‐down).tw. 9 (limit$ adj1 setting).tw. 10 negotiat$.tw. 11 ((verbal$ or nonverbal$ or non‐verbal$) adj3 (communicat$ or intervention$ or strateg$ or method$ or technique$)).tw. 12 (cris#s adj3 (intervention$ or manag$ or resol$ or respon$ or team$)).tw. 13 (conflict adj3 (avoid$ or manage$ or prevent$ or resol$)).tw. (4 14 (calm or calming).tw. 15 or/4‐14 16 3 and 15 17 (random$ or trial$ or control$ or group$ or placebo$ or blind$ or prospectiv$ or longitudinal$ or meta‐analys$ or systematic review$).tw. (711525) 18 16 and 17
Embase Ovid
Searched 22 February 2016 [981 records] Searched 27 September 2017. Deduplicated with previous records [181 records]
1 aggression/ or aggressiveness/ 2 exp anger/ 3 hostility/ 4 verbal hostility/ 5 violence/ 6 workplace violence/ 7 physical violence/ 8 (aggress$ or agitat$ or agonistic or anger or angry or assault$ or hostil$ or rage or threat$ or violen$).tw. 9 ((abusive or challenging or disturbed or disruptive) adj1 behav$).tw. 10 or/1‐9 11 risk management/ 12 behavior control/ 13 (de‐escalat$ or deescalat$ or non‐escalat$ or nonescalat$ or defus$ or de‐fus$).tw. 14 (non$ adj (authorit$ or avers$ or coerc$ or co‐erc$ or combativ$ or confrontation$ or physical or provocative or violen$)).tw. 15 (non$ adj (drug$ or pharma$)).tw. 16 ((alternative$ or avoid$ or reduc$ or without$) adj3 (seclusion or restrain$)).tw. 17 (talkdown or talk‐down).tw. 18 (limit$ adj1 setting).tw. 19 negotiat$.tw. 20 ((verbal$ or nonverbal$ or non‐verbal$) adj3 (communicat$ or intervention$ or strateg$ or method$ or technique$)).tw. 21 crisis intervention/ 22 (cris#s adj3 (intervention$ or manag$ or resol$ or respon$ or team$)).tw. 23 (calm or calming).tw. 24 or/11‐23 25 Randomized controlled trial/ 26 controlled clinical trial/ 27 Single blind procedure/ 28 Double blind procedure/ 29 triple blind procedure/ 30 Crossover procedure/ 31 (crossover or cross‐over).tw. 32 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 33 Placebo/ 34 placebo.tw. 35 prospective.tw. 36 factorial$.tw. 37 random$.tw. 38 assign$.ab. 39 allocat$.tw. 40 volunteer$.ab. 41 or/25‐40 42 10 and 24 and 41
PsycINFO Ovid
Searched 22 February 2016 [631 records] Searched 27 September 2017. Deduplicated with previous records [73 records]
1 exp aggressive behavior/ 2 violence/ 3 patient violence/ 4 school violence/ 5 workplace violence/ 6 anger/ 7 tantrums/ 8 hostility/ 9 (aggress$ or agitat$ or agonistic or anger or angry or assault$ or hostil$ or rage or threat$ or violen$).tw. 10 ((abusive or challenging or disturbed or disruptive) adj1 behav$).tw. 11 or/1‐10 12 risk management/ or safety/ 13 risk management/ 14 safety/ 15 (de‐escalat$ or deescalat$ or non‐escalat$ or nonescalat$ or defus$ or de‐fus$).tw. 16 (non$ adj (authorit$ or avers$ or coerc$ or co‐erc$ or combativ$ or confrontation$ or physical or provocative or violen$)).tw. 17 (non$ adj (drug$ or pharma$)).tw. 18 ((alternative$ or avoid$ or reduc$ or without$) adj3 (seclusion or restrain$)).tw. 19 (talkdown or talk‐down).tw. 20 (limit$ adj1 setting).tw. 21 or/12‐20 22 11 and 21 23 clinical trials/ 24 treatment effectiveness evaluation/ 25 random sampling/ 26 placebo/ 27 Experiment controls/ 28 ((clinic$ or control$) adj (study or trial$ or experiment$)).tw. 29 ((compar$ or control$ or experiment$ or treat$) adj3 (subjects or group$)).tw. 30 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 31 (randomiz$ or randomis$).tw. 32 randomly.tw. 33 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 34 exp program evaluation/ 35 exp experimental methods/ 36 or/23‐35 37 22 and 36
CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature)
Searched 22 February 2016 [608 records] Searched 27 September 2017. Deduplicated with previous records [208 records]
S1 (MH "Aggression") S2 (MH "Psychomotor Agitation") S3 (MH "Violence") S4 (MH "Workplace Violence") S5 (MH "School Violence") S6 (MH "Anger") S7 (MH "Acting Out") S8 (aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*) S9 ((abusive or challenging or disturbed or disruptive) N1 behav*) S10 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 S11 (MH "Risk Management") S12 (MH "Security Measures") S13 (de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*) S14 (non* N1 (authorit* or avers* or coerc* or co‐erc* or combativ* or confrontation* or physical or provocative or violen*)) S15 (non* N1 (drug* or pharma*)) S16 ((alternative* or avoid* or reduc* or without*) N3 (seclusion or restrain*)) S17 talkdown or talk‐down S18 (limit* N1 setting) S19 (MH "Negotiation") S20 negotiat* S21 ((verbal* or nonverbal* or non‐verbal*) N3 (communicat* or intervention* or strateg* or method* or technique*)) S22 (MH "Crisis Intervention") S23 ((crisis or crises) N3 (intervention* or manag* or resol* or respon* or team*)) S24 (conflict N3 (avoid* or manage* or prevent* or resol*) S25 (MH "Conflict Management") S26 (calm or calming) S27 S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 S28 S10 AND S27 S29 (MH "Clinical Trials+") S30 MH random assignment S31 (MH "Meta Analysis") S32 TI(random*) OR AB (random*) S33 AB ((clinical trial*) or(control* trial*)) S34 AB ((singl* N3 mask*) or(singl* N3 blind*)) S35 AB ((doubl* N3 mask*) or (doubl* N3 blind*)) S36 AB((trebl* N3 mask*) or (trebl* N3 blind*)) S37 AB((tripl* N3 mask*) or (tripl* N3 blind*)) S38 (MH "Crossover Design") S39 AB("cross over") S40 TI ("follow‐up study" or "follow‐up research") or AB ("follow‐up study" or "follow‐up research") S41 TI (prospectiv* study or prospectiv* research) or AB(prospectiv* study or prospectiv* research) S42 TI (evaluat* study or evaluat* research) or AB (evaluate* study or evaluat* research) or TI (effectiv* study or effectiv* research) or AB(effectiv* study or effectiv* research) S43 (MH "Program Evaluation") S44 (MH "Treatment Outcomes") S45 S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 S46 S28 AND S45
Web of Science databases (Science Citation Index (SCI), Social Science Citation Index (SSCI), Conference Proceedings Index ‐ Science (CPCI‐S), Conference Proceedings Index ‐ Social Sciences & Humanities (CPCI‐SS&H), SciELO Citation Index)
SCI and SSCI searched 24 February 2016 [908 records] SCI and SSCI searched 27 September 2017. Deduplicated with previous records [123 records]
CPCI‐S and CPCI‐SS&H searched 24 February 2016 [105 records] CPCI‐S and CPCI‐SS&H searched 27 September 2017. Deduplicated with previous records [21 records]
SciELO searched 24 February 2016 [105 records] SciELO searched 27 September 2017. Deduplicated with previous records [34 records]
#15 #14 AND #13 DocType=All document types; Language=All languages; #14 TS=(random* or trial* or control or controlled or prospective or longitudinal or meta‐analysis or "systematic review" ) DocType=All document types; Language=All languages; #13 #12 AND #3 DocType=All document types; Language=All languages; #12 #11 OR #10 OR #9 OR #8 OR #7 OR #5 OR #4 DocType=All document types; Language=All languages; #11 TS= (calm or calming) DocType=All document types; Language=All languages; #10 TS=(conflict near/1 (avoid* or manage* or prevent* or resolv* or resolution)) DocType=All document types; Language=All languages; #9 TS= ((crisis or crises) near/1 (intervention* or manag* or resolv* or resolution or respons* or respond* or team*)) DocType=All document types; Language=All languages; #8 TS=((verbal* or nonverbal* or "non verbal*") near/1 (communicat* or intervention* or strateg* or method* or technique*)) DocType=All document types; Language=All languages; #7 TS= (talkdown or talk‐down) DocType=All document types; Language=All languages; #6 TS=((non) near/1 (drug* or pharmacolog*)) DocType=All document types; Language=All languages; #5 TS=((alternative* or avoid* or reduc* or without*) near/1 (seclusion or restrain*)) DocType=All document types; Language=All languages; #4 TS=(de‐escalat* or non‐escalat* or defuse* or de‐fuse*) DocType=All document types; Language=All languages; #3 #2 OR #1 DocType=All document types; Language=All languages; #2 TS =((abusive or challenging or disturbed or disruptive) near/1 behav*) DocType=All document types; Language=All languages; #1 TS=(aggress* or agitat* or anger or angry or assault* or hostil* or rage or threat* or violen*) DocType=All document types; Language=All languages;
International Bibliography of the Social Sciences ProQuest (IBSS)
Searched 23 February 2016 [186 records] Searched 27 September 2017. Deduplicated with previous records [34 records]
((SU.EXACT("Anti‐social behaviour") OR SU.EXACT("Violence") OR SU.EXACT("Personal aggression") OR ((aggress* or agitat* or anger or angry or assault* or hostil* or rage or threat* or violen*) OR ((abusive or challenging or disturbed or disruptive) N/1 behav*))) AND (((crisis or crises) N/3 (intervention* or manag* or resol* or respon* or team*)) OR ((non* N/1 (authorit* or avers* or coerc* or co‐erc* or combativ* or confrontation* or physical or provocative or violen*)) OR (de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*)) OR ((non* N/1 (drug* or pharma*)) OR ((verbal* or nonverbal* or non‐verbal*) N/3 (communicat* or intervention* or strateg* or method* or technique*))) OR (((alternative* or avoid* or reduc* or without*) N/3 (seclusion or restrain*)) OR ("talk down" or talkdown))))AND (((crisis OR crises) NEAR/3 (intervention* OR manag* OR resol* OR respon* OR team*)) OR ((non* N/1 (authorit* or avers* or coerc* or co‐erc* or combativ* or confrontation* or physical or provocative or violen*)) OR (de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*)) OR ((non* N/1 (drug* or pharma*)) OR ((verbal* or nonverbal* or non‐verbal*) N/3 (communicat* or intervention* or strateg* or method* or technique*))) OR (((alternative* or avoid* or reduc* or without*) N/3 (seclusion or restrain*)) OR ("talk down" or talkdown)) OR (SU.EXACT("Crisis management") OR SU.EXACT("Conflict resolution"))) AND (AB(random* or trial* or control* or blind* or prospective* or longitudinal or intervention* or assign* or group* or "meta‐analysis" or "systematic review") OR TI(random* or trial* or control* or blind* or prospective* or longitudinal or intervention* or assign* or group* or "meta‐analysis" or "systematic review")) violen*)
British Education Index EBSCOhost (BEI)
BEI searched 23 February 2016 [42 records] BEI searched 27 September 2017. Deduplicated with previous records [41 records]
S1 DE "AGGRESSION (Psychology)" or DE "Anger" S2 DE "SCHOOL violence" OR DE "CAMPUS violence" OR DE "SCHOOL shootings" OR DE "SCHOOL vandalism" S3 DE "BEHAVIOR disorders in children" S4 (aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*) S5 ((abusive or challenging or disturbed or disruptive) N1 behav*) S6 S1 OR S2 OR S3 OR S4 OR S S7 DE "BEHAVIOR modification" S8 DE "BEHAVIOR modification techniques" S9 DE "SCHOOLS ‐‐ Safety measures" OR DE "SCHOOLS ‐‐ Security measures S10 (de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*) S11 DE "CRISIS management" S12 DE "CONFLICT management" S13 DE "CRISIS intervention (Mental health services) S14 ((crisis or crises) N3 (intervention* or manag* or resol* or respon* or team*)) S15 (non* N1 (authorit* or avers* or coerc* or co‐erc* or combativ* or confrontation* or physical or provocative or violen*)) S16 (non* N1 (drug* or pharma*)) S17 ((alternative* or avoid* or reduc* or without*) N3 (seclusion or restrain*)) S18 (limit* N1 setting) S19 ((verbal* or nonverbal* or non‐verbal*) N3 (communicat* or intervention* or strateg* or method* or technique*)) S20 negotiat* S21 S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 S22 S6 AND S21 S23 DE "RANDOMIZED controlled trials" S24 DE "PROGRAM effectiveness (Education)" S25 DE "TREATMENT effectiveness" S26 systematic review* or meta‐analys*s S27 (random* or trial* or prospectiv* OR longitudinal or blind* or control*) S28 S23 OR S24 OR S25 OR S26 OR S27 S29 S22 AND S28
ERIC EBSCOhost (Education Resources Information Center)
Searched 23 February 2016 [377 records] Searched 27 September 2017. Deduplicated with previous records [11 records]
S1 DE "Violence" S2 DE "Aggression" S3 DE "Delinquency" S4 DE "Antisocial Behavior" S5 DE "Behavior Disorders" S6 TI(aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*)OR AB (aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*) S7 TI((abusive or challenging or disturbed or disruptive) N1 behav*) OR AB ((abusive or challenging or disturbed or disruptive) N1 behav*) S8 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 S9 DE "Behavior Modification" S10 DE "Crisis Management" S11 DE "Crisis Intervention" S12 TI((crisis or crises) N3 (intervention* or manag* or resol* or respon* or team*))OR AB((crisis or crises) N3 (intervention* or manag* or resol* or respon* or team*)) S13 TI(non* N1 (authorit* or avers* or coerc* or co‐erc* or combativ* or confrontation* or physical or provocative or violen*))OR AB(non* N1 (authorit* or avers* or coerc* or co‐erc* or combativ* or confrontation* or physical or provocative or violen*)) S14 TI(de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*)OR AB(de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*) S15 AB (non* N1 (drug* or pharma*)) OR TI(non* N1 (drug* or pharma*)) S16 TI ((alternative* or avoid* or reduc* or without*) N3 (seclusion or restrain*)) OR AB ((alternative* or avoid* or reduc* or without*) N3 (seclusion or restrain*)) S17 TI((verbal* or nonverbal* or non‐verbal*) N3 (communicat* or intervention* or strateg* or method* or technique*)) OR AB ((verbal* or nonverbal* or non‐verbal*) N3 (communicat* or intervention* or strateg* or method* or technique*)) S18 (limit* N1 setting) or ("talk down" or talkdown) S19 S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 S20 S8 AND S19 S21 DE "Meta Analysis" OR DE "Control Groups" OR DE "Experimental Groups" OR DE "Longitudinal Studies" OR DE "Followup Studies" S22 TI (random* or trial* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL*) OR AB (random* or trial* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL*) S23 S21 OR S22 S24 S20 AND S23 S25 DE "Adults" OR DE "Older Adults" OR DE "Young Adults" S26 DE "Students" OR DE "Adult Students" OR DE "College Students" S27 adult* or adolescent* or teen* or young person* or young people or youth* S28 18 N1 years S29 18 N1 plus S30 S25 OR S26 OR S27 OR S28 OR S29 S31 S24 AND S30
Cochrane Database of Systematic Reviews (CDSR) part of the Cochrane Library
Searched 22 February 2016 [49 records] Searched 27 September 2017. Deduplicated with previous records [16 records]
#1[mh ^Aggression] #2[mh ^"Psychomotor agitation"] #3[mh ^"Agonistic behavior"] #4[mh Violence] #5[mh "Workplace Violence"] #6[mh Anger] #7[mh Hostility] #8(aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*):ti,ab,kw #9((abusive or challenging or disturbed or disruptive) near/1 behav*):ti,ab,kw #10{or #1‐#9} #11[mh "Risk management"] #12[mh "Behavior control"] #13[mh "Safety management"] #14[mh "Security measures"] #15(de next escalat* or deescalat* or non next escalat* or nonescalat* or defus* or de next fus*):ti,ab,kw #16(non* next (authorit* or avers* or coerc* or co next erc* or combativ* or confrontation* or physical or provocative or violen*)):ti,ab,kw #17(non* next (drug* or pharma*)):ti,ab,kw #18((alternative* or avoid* or reduc* or without*) near/3 (seclusion or restrain*)):ti,ab,kw #19(talkdown or talk‐down or "one to one"):ti,ab,kw #20(limit* near/1 setting):ti,ab,kw #21[mh Negotiating] #22negotiat*:ti,ab,kw #23((verbal* or nonverbal* or non next verbal*) near/3 (communicat* or intervention* or strateg* or method* or technique*)):ti,ab,kw #24[mh "Crisis intervention"] #25((crisis or crises) near/3 (intervention* or manag* or resol* or respon* or team*)):ti,ab,kw #26(conflict near/3 (avoid* or manage* or prevent* or resol*)):ti,ab,kw #27(calm or calming):ti,ab,kw #28{or #11‐#27} #29#10 and #28 in Cochrane Reviews (Reviews and Protocols)
Database of Abstracts of Reviews of Effect (DARE) part of the Cochrane Library
Searched 22 February 2016 [16 records]
#1[mh ^Aggression] #2[mh ^"Psychomotor agitation"] #3[mh ^"Agonistic behavior"] #4[mh Violence] #5[mh "Workplace Violence"] #6[mh Anger] #7[mh Hostility] #8(aggress* or agitat* or agonistic or anger or angry or assault* or hostil* or rage or threat* or violen*):ti,ab,kw #9((abusive or challenging or disturbed or disruptive) near/1 behav*):ti,ab,kw #10{or #1‐#9} #11[mh "Risk management"] #12[mh "Behavior control"] #13[mh "Safety management"] #14[mh "Security measures"] #15(de next escalat* or deescalat* or non next escalat* or nonescalat* or defus* or de next fus*):ti,ab,kw #16(non* next (authorit* or avers* or coerc* or co next erc* or combativ* or confrontation* or physical or provocative or violen*)):ti,ab,kw #17(non* next (drug* or pharma*)):ti,ab,kw #18((alternative* or avoid* or reduc* or without*) near/3 (seclusion or restrain*)):ti,ab,kw #19(talkdown or talk‐down or "one to one"):ti,ab,kw #20(limit* near/1 setting):ti,ab,kw #21[mh Negotiating] #22negotiat*:ti,ab,kw #23((verbal* or nonverbal* or non next verbal*) near/3 (communicat* or intervention* or strateg* or method* or technique*)):ti,ab,kw #24[mh "Crisis intervention"] #25((crisis or crises) near/3 (intervention* or manag* or resol* or respon* or team*)):ti,ab,kw #26(conflict near/3 (avoid* or manage* or prevent* or resol*)):ti,ab,kw #27(calm or calming):ti,ab,kw #28{or #11‐#27} #29#10 and #28 in Other Reviews
Criminal Justice Abstracts EBSCOhost
CJA searched 24 February 2016 [254 records] CJA searched 27 September 2017. Deduplicated with previous records [33 records]
S4 S1 OR S2 OR S3 S3 talkdown or talk‐down S2 ((alternative* or avoid* or reduc* or without*) N3 (seclusion or restrain*)) S1 (de‐escalat* or deescalat* or non‐escalat* or nonescalat* or defus* or de‐fus*)
Academic Search Complete EBSCOhost
Searched 6 April 2016 [196 records] Searched 9 October 2017. Deduplicated with previous records [16 records]
S1 (violence or violent or aggression or hostility or anger) AND (de‐escalat* OR deescalat*)
OpenGrey (opengrey.eu)
Searched 6 April 2016 [15 records] Searched 9 October 2017. Deduplicated with previous records [0 records]
violen* OR aggress* or hostil* OR anger AND de‐escalat* OR deescalat*
Campbell Collaboration Library of Systematic Reviews ( www.campbellcollaboration.org/library.html )
Searched 6 April 2016 [103 records] Searched 9 October 2017. Deduplicated with previous records [0 records]
violen OR aggress OR hostil OR anger (in any text)
ClinicalTrials.gov ( clinicaltrials.gov )
Searched 6 April 2016 [138 records] Searched 9 October 2017. Deduplicated with previous records [113 records]
de‐escalate OR de‐escalation OR deescalate OR deescalation | Interventional Studies | violent OR violence OR aggression OR hostility OR anger
ISRCTN ( ISRCTN.com )
Searched 06 April 2016 [19 records] Searched 09 October 2017. Deduplicated with previous records [11 records]
violent OR violence OR aggression OR hostility OR anger | within Interventions | deescalation OR deescalate OR de‐escalation OR de‐escalate
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; apps.who.int/trialsearch )
Searched 6 April 2016 [64 records] Searched 9 October 2017. Deduplicated with previous records [57 records]
violence OR violent OR aggression OR hostility OR anger (in title) de‐escalation OR deescalation OR de‐escalate OR deescalate (in title)
1 AND 2
Data and analyses
Comparison 1. De‐escalation versus standard care.
1.1. Analysis.
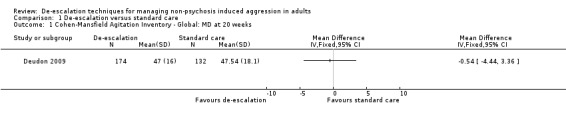
Comparison 1 De‐escalation versus standard care, Outcome 1 Cohen‐Mansfield Agitation Inventory ‐ Global: MD at 20 weeks.
1.2. Analysis.
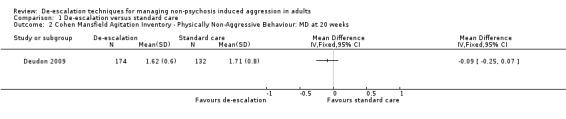
Comparison 1 De‐escalation versus standard care, Outcome 2 Cohen Mansfield Agitation Inventory ‐ Physically Non‐Aggressive Behaviour: MD at 20 weeks.
1.3. Analysis.
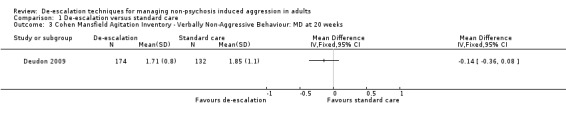
Comparison 1 De‐escalation versus standard care, Outcome 3 Cohen Mansfield Agitation Inventory ‐ Verbally Non‐Aggressive Behaviour: MD at 20 weeks.
1.4. Analysis.
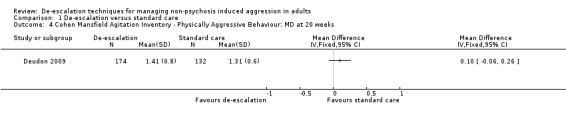
Comparison 1 De‐escalation versus standard care, Outcome 4 Cohen Mansfield Agitation Inventory ‐ Physically Aggressive Behaviour: MD at 20 weeks.
1.5. Analysis.
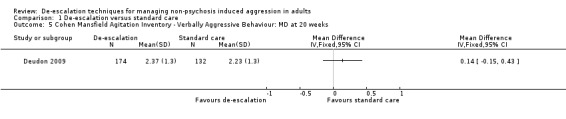
Comparison 1 De‐escalation versus standard care, Outcome 5 Cohen Mansfield Agitation Inventory ‐ Verbally Aggressive Behaviour: MD at 20 weeks.
1.6. Analysis.
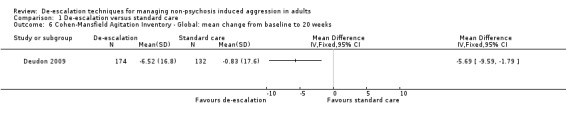
Comparison 1 De‐escalation versus standard care, Outcome 6 Cohen‐Mansfield Agitation Inventory ‐ Global: mean change from baseline to 20 weeks.
1.7. Analysis.
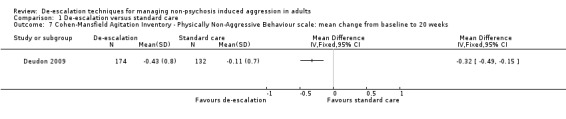
Comparison 1 De‐escalation versus standard care, Outcome 7 Cohen‐Mansfield Agitation Inventory ‐ Physically Non‐Aggressive Behaviour scale: mean change from baseline to 20 weeks.
1.8. Analysis.
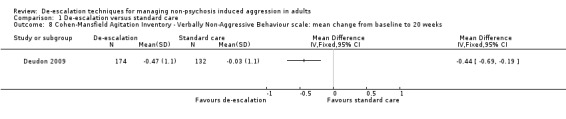
Comparison 1 De‐escalation versus standard care, Outcome 8 Cohen‐Mansfield Agitation Inventory ‐ Verbally Non‐Aggressive Behaviour scale: mean change from baseline to 20 weeks.
1.9. Analysis.
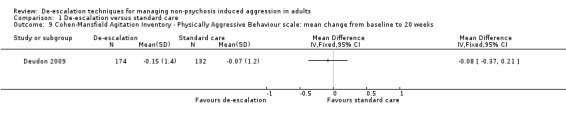
Comparison 1 De‐escalation versus standard care, Outcome 9 Cohen‐Mansfield Agitation Inventory ‐ Physically Aggressive Behaviour scale: mean change from baseline to 20 weeks.
1.10. Analysis.
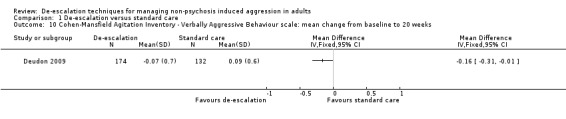
Comparison 1 De‐escalation versus standard care, Outcome 10 Cohen‐Mansfield Agitation Inventory ‐ Verbally Aggressive Behaviour scale: mean change from baseline to 20 weeks.
1.11. Analysis.
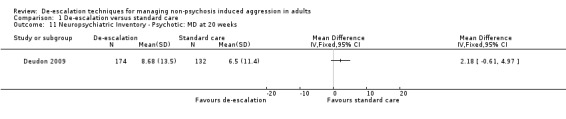
Comparison 1 De‐escalation versus standard care, Outcome 11 Neuropsychiatric Inventory ‐ Psychotic: MD at 20 weeks.
1.12. Analysis.
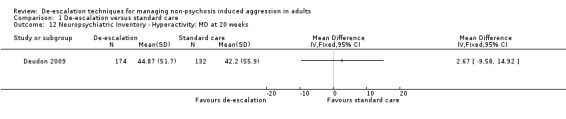
Comparison 1 De‐escalation versus standard care, Outcome 12 Neuropsychiatric Inventory ‐ Hyperactivity: MD at 20 weeks.
1.13. Analysis.
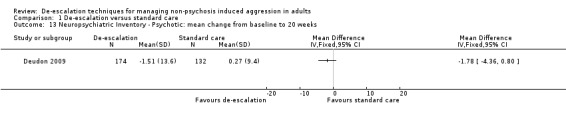
Comparison 1 De‐escalation versus standard care, Outcome 13 Neuropsychiatric Inventory ‐ Psychotic: mean change from baseline to 20 weeks.
1.14. Analysis.
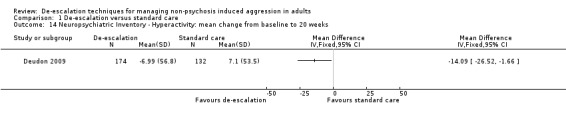
Comparison 1 De‐escalation versus standard care, Outcome 14 Neuropsychiatric Inventory ‐ Hyperactivity: mean change from baseline to 20 weeks.
1.15. Analysis.
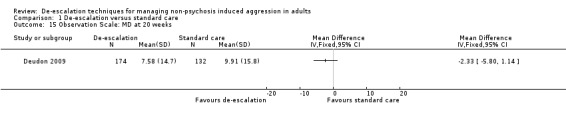
Comparison 1 De‐escalation versus standard care, Outcome 15 Observation Scale: MD at 20 weeks.
1.16. Analysis.
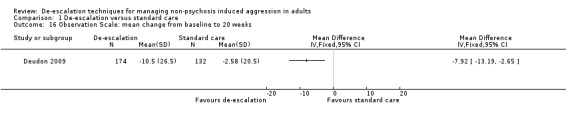
Comparison 1 De‐escalation versus standard care, Outcome 16 Observation Scale: mean change from baseline to 20 weeks.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Deudon 2009.
| Methods | Cluster‐randomised controlled trial with follow‐up at 8 and 20 weeks postbaseline | |
| Participants |
Location: 2 regions of France: Alpes Maritimes and Gironde Setting: 16 nursing homes Inclusion criteria: MMSE score ≤ 24 and at least one of the following BPSD at least once a week: opposition, denial of care, aberrant motor behaviour, agitation, delusions, hallucinations or screaming Sample size: N = 306 (22%) participants were selected for the study from among the 1369 residents living in the 16 nursing homes; intervention = 6 nursing homes with 174 participants, control = 10 nursing homes with 132 participants Sex (men/women): intervention = 40/134 (23%/77%), control = 28/104 (21.2%/78.8%) Dropouts/withdrawals: N = 34 (intervention = 2, control = 2 by week 8), intervention = 16, control =18 Diagnosis: dementia according to ICD‐10 criteria (WHO 1992) Mean age: intervention = 86.5 (SD 7.6), control = 86 (SD 6.7) |
|
| Interventions |
Intervention: a training programme, conducted in each nursing home by 2 independent professionals, consisting of the following: 90‐minute teaching session on dementia, BPSD and the use of 4 ‘how to' instruction cards summarising practical advice on what to do and what to avoid to prevent the emergence of aggression and agitation, what to do when faced with opposition, denial of care, aberrant motor activity, agitation, aggression, delusions, hallucinations or screaming, and recommendations on non‐pharmacological interventions. Individual and interactive constructive feedback sessions on how staff dealt with BPSD. Trainers provided, as required, personalised advice, training and feedback for 2 hours, twice a week, during the first month and then once a week during the second month, giving a total of 24 hours training Control: standard care |
|
| Outcomes | Data were collected at baseline, week 8 (end of the training programme) and week 20 (3 months after the end of the training programme) using the following 3 outcome measures
|
|
| Notes |
Study dates: 15 October to 15 December 2007, with 3‐month follow‐up in March 2008 Funding: grant from the French Ministry of Health (Direction Générale de la Santé) and the Fondation Médéric Alzheimer Declarations of interest: no competing interests |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Nursing homes were randomly assigned to the control group or the intervention group" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Nursing homes were randomly assigned to the control group or the intervention group" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Quote: "None of the nursing homes shared facilities or staff. No information concerning the existence of another group (control or intervention) was given to the directors and staff of the nursing homes of either group at any time during the study." Comment: it was not possible to blind participants to this intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Assessments were performed by four psychologists blind to the intervention condition and previously trained in the assessment tools. None of them participated in the staff training programme." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: attrition rate at week 0: intervention = 132, control = 174. Attrition rate at week 8: intervention = 130, control = 172. Attrition rate at week 20: intervention = 114, control = 158. Most participants were lost because of the death of participants |
| Selective reporting (reporting bias) | Unclear risk | Comment: we did not identify a trial protocol, but analyses described in the Methods section were reported in the Results section |
| Other bias | High risk | Comment: potentially eligible patients were identified in each nursing home prior to cluster randomisation. The number of nursing homes and participants was not balanced between groups. There were significant differences between the groups at baseline, particularly on BPSD severity |
BPSD: behavioural and psychological symptoms of dementia;ICD‐10: International Classification of Diseases, 10th Revision; MMSE: Mini‐Mental State Examination; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adams 2017 | The intervention was not de‐escalation; not an RCT or quasi‐RCT |
| Allen 2000 | Not an RCT or quasi‐RCT |
| Andersen 2017 | The intervention was not de‐escalation; not an RCT or quasi‐RCT; psychiatric patients so cannot rule out schizophrenia |
| Bowers 2003 | Not an RCT or quasi‐RCT |
| Bowers 2015 | All patients on psychiatric wards but data on diagnosis were not collected (personal communication), so cannot rule out schizophrenia |
| Burns 2015 | Not an RCT or quasi‐RCT |
| Cailhol 2007 | Not an RCT or quasi‐RCT |
| Cleary Bradley 2012 | Not conducted in a care setting |
| Cowin 2003 | Not an RCT or quasi‐RCT |
| DRKS00009723 | Not an RCT or quasi‐RCT |
| Hallett 2015 | Not an RCT or quasi‐RCT |
| Hitchen 2007 | The study was registered but did not recruit any participants and was subsequently closed (personal communication) |
| Huizing 2006 | The intervention was not de‐escalation |
| Kuske 2009 | The intervention was not de‐escalation |
| Loi 2017 | The intervention was not de‐escalation and the study was not an RCT or quasi‐RCT |
| Martinez 2017 | Not an RCT or quasi‐RCT |
| Proctor 1999 | The intervention was not de‐escalation |
| Small 2006 | Not an RCT or quasi‐RCT |
| Testad 2005 | The intervention was not de‐escalation |
| Testad 2010 | The intervention was not de‐escalation |
| Testad 2016 | The intervention was not de‐escalation |
| Valimaki 2017 | The intervention was not de‐escalation and the study was not an RCT or quasi‐RCT |
| Yeh 2001 | Not RCT or quasi‐RCT |
| Zwijsen 2014 | The intervention was not de‐escalation |
| Üzar 2017 | The intervention was not de‐escalation and the study was not an RCT or quasi‐RCT |
RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12614000735651.
| Trial name or title |
Public title: 'Communication skills training for healthcare workers as a technique to reduce patient perpetrated violence: a randomized clinical trial' Scientific title:'Among healthcare workers, does communication skills training or mentalization training reduce patient perpetrated violence?' |
| Methods |
Design: cluster‐randomised controlled trial Location: 2 regions of New Zealand Procedure for enrolment: potential participants to be met in their workplace and invited to participate. Groups of 7‐9 participants will be randomly assigned to intervention or control. Not possible to blind the intervention, and all outcomes are self‐reported. Third party random sequence generation by cluster from multiple organisations Sample size: for 80% power to detect a differences of 0.5 SD between groups at follow‐up (i.e. moderate effect sizes) on the primary continuous outcomes, using 2‐sided tests at the 0.05 level and allowing for 20% loss to follow‐up, 100 participants are required for each group (N = 200) Analyses: appropriate summary statistics will be presented for all outcomes of interest. Differences in change over time between groups using appropriate regression models (linear for continuous, binary logistic for dichotomised, and Poisson or negative binomial for count outcomes), adjusting for baseline values. Differences between ITT and per protocol to be analysed along with sensitivity analyses. All statistical tests to be conducted at the 2‐sided 0.05 level. Stata 13.1 and R 3.1.0 (or later versions) will be used for all analyses |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention: communication skills training. Scripted group training called 'It's All About Communication', which uses video examples of clinical situations together with a workbook and trainer's guide. The aim is for participants to reflect on their communication style and learn how to analyse, reflect, and modify their communication depending on the patient's or client's circumstances. The training programme consists of 4 weekly, face‐to‐face group sessions, administered by a facilitator using the training materials, lasting between 50 and 75 minutes Comparator: mentalization. The control group will receive 4 sessions of mentalization practice, using an acceptance and compassion model. The training programme consists of 4 weekly, face‐to‐face group sessions, administered by a facilitator using the training materials, lasting between 50 and 75 minutes |
| Outcomes |
Primary
Secondary
All outcomes completed at baseline and 1, 2, 3 and 6 months postintervention |
| Starting date | Proposed start date: 4 September 2014 |
| Contact information |
Contact person for public queries: Dr Nicola Swain, University of Otago. nicola.swain@otago.ac.nz Contact person for scientific queries: Dr Christopher Gale (Principal Investigator), University of Otago. chris.gale@otago.ac.nz |
| Notes |
Universal Trial Number: U1111‐1158‐6871 Website: www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366628 |
ITT: intention‐to‐treat; NZ: New Zealand; SD: standard deviation.
Differences between protocol and review
Authors. Ian C Smith joined the review team.
Methods. For methods that we described in the protocol, Spencer 2016, but did not use in the review, please see Table 2.
Included studies. Pre‐specified outcomes were either not reported in the included study or not eligible for inclusion in the review. We elected to include behavioural outcomes that were not pre‐specified in the protocol but reported in the included study, as they were considered relevant to the objectives of this review.
Electronic searches. We also searched MEDLINE In‐Process & Other Non‐Indexed Citations and MEDLINE Epub Ahead of Print which are updated daily, and Conference Proceedings Citation Index ‐ Social Sciences & Humanities.
Contributions of authors
All authors contributed to the writing and development of the review. Sally Spencer conducted the literature searches in collaboration with the Cochrane Developmental, Psychosocial and Learning Problem's Information Specialist, and she drafted the Methods and Results sections of the review. Paula Johnson and Ian C Smith screened records for eligibility, independently extracted data, entered data onto a data extraction form, assessed risk of bias and summarised the study. All authors contributed to resolving disagreements during screening and data extraction.
Sally Spencer has overall responsibility for the review.
Sources of support
Internal sources
-
Edge Hill University, UK.
Supports SS through employment
-
Lancaster University, UK.
Supports ICS through employment and supported SS through employment on earlier versions of the protocol for this review
-
Mersey Care NHS Foundation Trust, UK.
Supported PJ through former employment. The views expressed are those of the author and not necessarily the National Health Service or the Department of Health
External sources
None, Other.
Declarations of interest
Sally Spencer is an Editor with Cochrane Airways and Cochrane Dementia and Cognitive Improvement. Paula Johnson ‐ none known. Ian C Smith ‐ none known.
New
References
References to studies included in this review
Deudon 2009 {published data only}
- Deudon A, Maubourguet N, Gervais X, Leone E, Brocker P, Carcaillon L, et al. Non‐pharmacological management of behavioural symptoms in nursing homes. International Journal of Geriatric Psychiatry 2009;24(12):1386‐95. [DOI: 10.1002/gps.2275; PUBMED: 19370714] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adams 2017 {published data only}
- Adams J, Roddy A, Knowles A, Ashworth J, Irons G. Assessing the effectiveness of clinical education to reduce the frequency and recurrence of workplace violence. Australian Journal of Advanced Nursing 2017;34(3):6‐15. [www.ajan.com.au/Vol34/Issue3/1Adams.pdf] [Google Scholar]
Allen 2000 {published data only}
- Allen D, Tynan H. Responding to aggressive behaviour: impact of training on staff members' knowledge and confidence. Mental Retardation 2000;38(2):97‐104. [DOI: ; PUBMED: 10804700] [DOI] [PubMed] [Google Scholar]
Andersen 2017 {published data only}
- Andersen C, Kolmos A, Andersen K, Sippel V, Stenager E. Applying sensory modulation to mental health inpatient care to reduce seclusion and restraint: a case control study. Nordic Journal of Psychiatry 2017;71(7):525‐8. [DOI: 10.1080/08039488.2017.1346142; PUBMED: 28719249] [DOI] [PubMed] [Google Scholar]
Bowers 2003 {published data only}
- Bowers L, Alexander J, Gaskell C. A trial of anti‐absconding intervention in acute psychiatric wards. Journal of Psychiatric and Mental Health Nursing 2003;10(4):410‐6. [DOI: 10.1046/j.1365-2850.2003.00619.x; PUBMED: 12887632] [DOI] [PubMed] [Google Scholar]
Bowers 2015 {published data only}
- Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J. Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. International Journal of Nursing Studies 2015;52(9):1412‐22. [DOI: 10.1016/j.ijnurstu.2015.05.001; PMC4518134 ; www.journalofnursingstudies.com/article/S0020‐7489(15)00160‐1/abstract; PUBMED: 26166187] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson A. Re: Cochrane Review query [personal communication]. Email to: I Smith 27 November 2016.
Burns 2015 {published data only}
- Burns S. Using touch as a way to manage aggression. Mental Health Practice 2015;19(3):27‐33. [DOI: 10.7748/mhp.19.3.27.s18] [DOI] [Google Scholar]
Cailhol 2007 {published data only}
- Cailhol L, Allen M, Moncany A‐H, Cicotti A, Virgillito S, Barbe RP, et al. Violent behavior of patients admitted in emergency following drug suicidal attempt: a specific staff educational crisis intervention. General Hospital Psychiatry 2007;29(1):42‐4. [DOI: 10.1016/j.genhosppsych.2006.10.007; PUBMED: 17189744] [DOI] [PubMed] [Google Scholar]
Cleary Bradley 2012 {published data only}
- Cleary Bradley RP, Gottman JM. Reducing situational violence in low‐income couples by fostering healthy relationships. Journal of Marital and Family Therapy 2012;38(Suppl 1):187‐98. [DOI: 10.1111/j.1752-0606.2012.00288.x; PUBMED: 22765333] [DOI] [PubMed] [Google Scholar]
Cowin 2003 {published data only}
- Cowin L, Davies R, Estall G, Berlin T, Fitzgerald M, Hoot S. De‐escalating aggression and violence in the mental health setting. International Journal of Mental Health Nursing 2003;12(1):64‐73. [DOI: 10.1046/j.1440-0979.2003.00270; PUBMED: 14685961] [DOI] [PubMed] [Google Scholar]
DRKS00009723 {published data only}
- DRKS00009723. Evaluation of a deescalation management named OUTCOME to reduce aggression and violence in psychiatry. www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00009723 (first received 30 November 2015). [DRKS00009723; U1111‐1177‐0045 ]
Hallett 2015 {published data only}
- Hallett N, Dickens GL. De‐escalation: a survey of clinical staff in a secure mental health inpatient service. International Journal of Mental Health Nursing 2015;24(4):324‐33. [DOI: 10.1111/inm.12136; PUBMED: 25975221] [DOI] [PubMed] [Google Scholar]
Hitchen 2007 {published data only}
- Hitchen H, Magee WL. A comparison of the effects of verbal de‐escalation techniques with music based de‐escalation techniques on agitation levels in patients with neuro‐behavioural disorders. National Research Register 2007. [CENTRAL: cochranelibrary‐wiley.com/o/cochrane/clcentral/articles/869/CN‐00884869/frame.html; N0204175715]
- Magee W. Re: Cochrane Review [personal communication]. Email to: P Johnson 6 October 2016.
Huizing 2006 {published data only}
- Huizing AR, Hamers JPH, Gulpers MJM, Berger MPF. Short‐term effects of an educational intervention on physical restraint use: a cluster randomized trial. BMC Geriatrics 2006;6:17. [DOI: 10.1186/1471-2318-6-17; PMC1635553; PUBMED: 17067376] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuske 2009 {published data only}
- Kuske B, Luck T, Hanns S, Matschinger H, Angermeyer MC, Behrens J, et al. Training in dementia care: a cluster‐randomized controlled trial of a training program for nursing home staff in Germany. International Psychogeriatrics 2009;21(2):295‐308. [DOI: 10.1017/S1041610208008387; PUBMED: 19193252] [DOI] [PubMed] [Google Scholar]
Loi 2017 {published data only}
- Loi SM, Mazur A, Huppert D, Hoy B, Swan J, Lautenschlager NT. A pilot study using "apps" as a novel strategy for the management of challenging behaviors seen in people living in residential care. International Psychogeriatrics 2017;29(4):637–43. [DOI: 10.1017/S1041610216002039; PUBMED: 27974056] [DOI] [PubMed] [Google Scholar]
Martinez 2017 {published data only}
- Martinez AJS. Implementing a workplace violence simulation for undergraduate nursing students: a pilot study. Journal of Psychosocial Nursing and Mental Health Services 2017;55(10):39‐44. [DOI: 10.3928/02793695-20170818-04; PUBMED: 28840933] [DOI] [PubMed] [Google Scholar]
Proctor 1999 {published data only}
- Proctor R, Burns A, Powell HS, Tarrier N, Faragher B, Richardson G, et al. Behavioural management in nursing and residential homes: a randomised controlled trial. Lancet 1999;354(9172):26‐9. [DOI: 10.1016/S0140-6736(98)08237-3; PUBMED: 10406361] [DOI] [PubMed] [Google Scholar]
Small 2006 {published data only}
- Small JA, Montoro‐Rodriguez J. Conflict resolution styles: a comparison of assisted living and nursing home facilities. Journal of Gerontological Nursing 2006;32(1):39‐45. [DOI: 10.3928/0098-9134-20060101-14; PUBMED: 16475464] [DOI] [PubMed] [Google Scholar]
Testad 2005 {published data only}
- Testad I, Aasland AM, Aasland D. The effect of staff training on the use of restraint in dementia: a single‐blind randomised controlled trial. International Journal of Geriatric Psychiatry 2005;20(6):587‐90. [DOI: 10.1002/gps.1329; PUBMED: 15920716] [DOI] [PubMed] [Google Scholar]
Testad 2010 {published data only}
- Testad I, Ballard C, Brønnick K, Aarsland D. The effect of staff training on agitation and use of restraint in nursing home residents with dementia: a single‐blind, randomized controlled trial. Journal of Clinical Psychiatry 2010;71(1):80‐6. [DOI: 10.4088/JCP.09m05486oli; PUBMED: 20129008] [DOI] [PubMed] [Google Scholar]
Testad 2016 {published data only}
- Testad I, Mekki TE, Førland O, Øye C, Tveit EM, Jacobsen F, et al. Modeling and evaluating evidence‐based continuing education program in nursing home dementia care (MEDCED)—training of care home staff to reduce use of restraint in care home residents with dementia. A cluster randomized controlled trial. International Journal of Geriatric Psychiatry 2016;31(1):24‐32. [DOI: 10.1002/gps.4285; 25845462] [DOI] [PubMed] [Google Scholar]
Üzar 2017 {published data only}
- Üzar‐Özçetin YS, Hiçdurmaz D. Effects of structured group counselling on anger management skills of nursing students. Journal of Nursing Education 2017;56(3):174‐81. [DOI: 10.3928/01484834-20170222-10; PUBMED: 28263357] [DOI] [PubMed] [Google Scholar]
Valimaki 2017 {published data only}
- Valimaki M, Yang M, Normand S‐L, Lorig KR, Anttila M, Lantta T, et al. Study protocol for a cluster randomised controlled trial to assess the effectiveness of user‐driven intervention to prevent aggressive events in psychiatric services. BMC Psychiatry 2017;17(1):123. [DOI: 10.1186/s12888-017-1266-6; NCT02724748; PMC5379524; PUBMED: 28372555] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yeh 2001 {published data only}
- Yeh SH, Lin LW, Wang SY, Wu SZ, Lin JH, Tsai FM. The outcomes of restraint reduction program in nursing homes. Hu Li Yan Jiu 2001;9(2):183‐93. [PUBMED: 11548463] [PubMed] [Google Scholar]
Zwijsen 2014 {published data only}
- Zwijsen SA, Smalbrugge M, Eefsting JA, Twisk JW, Gerritsen DL, Pot AM, et al. Coming to grips with challenging behavior: a cluster randomized controlled trial on the effects of a multidisciplinary care program for challenging behavior in dementia. Journal of the American Medical Directors Association 2014;15(7):531.e1‐10. [DOI: 10.1016/j.jamda.2014.04.007; PUBMED: 24878214] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12614000735651 {published data only}
- ACTRN12614000735651. Communication skills training for healthcare workers as a technique to reduce patient perpetrated violence: a randomized clinical trial [Among healthcare workers, does communication skills training or mentalization training reduce patient perpetrated violence]. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366628 (first received 1 July 2014). [ACTRN12614000735651]
Additional references
Ahmed 2001
- Ahmed AG, Lepnurm M. Seclusion practice in a Canadian forensic psychiatric hospital. Journal of the American Academy of Psychiatry and the Law 2001;29(3):303‐9. [PUBMED: 11592458] [PubMed] [Google Scholar]
Anderson 2002
- Anderson CA, Bushman BJ. Human aggression. Annual Review of Psychology 2002;53:27‐51. [DOI: 10.1146/annurev.psych.53.100901.135231] [DOI] [PubMed] [Google Scholar]
APA 2013
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Washington (DC): American Psychiatric Association, 2013. [DOI: 10.1176/appi.books.9780890425596] [DOI] [Google Scholar]
Bourget 2002
- Bourget D, El‐Guebaly N, Atkinson MJ. The CPA Practice Research Network Findings from the Third Project, 2001. Part IV: assessing and managing violent patients. Canadian Psychiatric Association Bulletin 2002;34(5):25‐7. [ww1.cpa‐apc.org/Publications/Archives/Bulletin/2002/october/prn2001part4.asp] [Google Scholar]
Bowers 2000
- Bowers L. The expression and comparison of ward incident rates. Issues in Mental Health Nursing 2000;21(4):365‐74. [PUBMED: 11249355] [DOI] [PubMed] [Google Scholar]
Bowers 2006
- Bowers L, Nijman H, Allan T, Simpson A, Warren J, Turner L. Prevention and management of aggression training and violent incidents on UK acute psychiatric wards. Psychiatric Services 2006;57(7):1022‐6. [DOI: 10.1176/ps.2006.57.7.1022; PUBMED: 16816288] [DOI] [PubMed] [Google Scholar]
Bowers 2007
- Bowers L, Werf B, Vokkolainen A, Muir‐Cochrane E, Allan T, Alexander J. International variation in containment measures for disturbed psychiatric inpatients: a comparative questionnaire survey. International Journal of Nursing Studies 2007;44(3):357‐64. [DOI: 10.1016/j.ijnurstu.2006.01.005; PUBMED: 16524581] [DOI] [PubMed] [Google Scholar]
Bowers 2009
- Bowers L, Allan T, Simpson A, Jones J, Merwe M, Jeffery D. Identifying key factors associated with aggression on acute inpatient psychiatric wards. Issues in Mental Health Nursing 2009;30(4):260‐71. [DOI: 10.1080/01612840802710829; PUBMED: 19363731] [DOI] [PubMed] [Google Scholar]
Bowers 2011
- Bowers L, Stewart D, Papadopoulos C, Dack C, Ross J, Khanom D, et al. Inpatient Violence and Aggression: A Literature Review. Report from the Conflict and Containment Reduction Research Programme. London (UK): King's College London, 2011. [pdfs.semanticscholar.org/b98f/4ff17c264fd919542dcc14905b280c8776b8.pdf] [Google Scholar]
Chan 2013
- Chan A‐W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža‐Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Annals of Internal Medicine 2013;158(3):200‐7. [DOI: 10.7326/0003-4819-158-3-201302050-00583; PMC5114123; PUBMED: 23295957] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen‐Mansfield 1990
- Cohen‐Mansfield J, Werner P, Marx MS. The spatial distribution of agitation in agitated nursing home residents. Environment and Behavior 1990;22(3):408–19. [DOI: 10.1177/0013916590223005] [DOI] [Google Scholar]
Cohen‐Mansfield 1995
- Cohen‐Mansfield J. Assessment of disruptive behaviour/agitation in the elderly: function, methods and difficulties. Journal of Geriatric Psychiatry and Neurology 1995;8(1):52‐60. [PUBMED: 7710649] [PubMed] [Google Scholar]
CPI 2005
- Crises Prevention Institute (CPI). Instructor Manual for the Nonviolent Crisis Intervention Training Program. Milwaukee (WI): Crisis Prevention Institute, 2005. [Google Scholar]
CQC 2011
- Care Quality Commission (CQC). CQC review of Castlebeck Group Services. www.cqc.org.uk/sites/default/files/documents/20110726_castlebeck_summary.doc (accessed 24 March 2014).
CRAG 1996
- CRAG Working Group on Mental Illness, National Health Service in Scotland. The Prevention and Management of Aggression: A Good Practice Statement. Edinburgh (UK): Scottish Office, National Health Service in Scotland, 1996. [Google Scholar]
Crenshaw 1995
- Crenshaw WB, Francis PS. A national survey on seclusion and restraint in state psychiatric hospitals. Psychiatric Services 1995;46(10):1026‐31. [DOI: 10.1176/ps.46.10.1026; PUBMED: 8829783] [DOI] [PubMed] [Google Scholar]
Cummings 1994
- Cummings JL, Mega MS, Gray K, Rosenberg‐Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994;44(12):2308–14. [DOI: ; PUBMED: 7991117] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG, editor(s). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Di Martino 2003
- Martino V. Workplace Violence in the Health Care Sector. Relationship Between Work Stress and Workplace Violence in the Health Sector. Geneva: International Labour Office (ILO), 2003. [www.who.int/violence_injury_prevention/violence/interpersonal/WVstresspaper.pdf] [Google Scholar]
Dix 2008
- Dix R, Page MJ. De‐escalation. In: Beer MD, Pereira SM, Paton C editor(s). Psychiatric Intensive Care. 2nd Edition. Cambridge (UK): Cambridge University Press, 2008:24‐31. [Google Scholar]
DoH 2005
- Department of Health (DoH). Mental Capacity Act 2005. London (UK): Her Majesty's Stationary Office, 2005. [Google Scholar]
Dunn 2007
- Dunn K, Elsom S, Cross W. Self‐efficacy and locus of control affect management of aggression by mental health nurses. Issues in Mental Health Nursing 2007;28(2):201‐17. [DOI: 10.1080/0161284060196321; PUBMED: 17365168] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [PMC2127453; PUBMED: 9310563] [DOI] [PMC free article] [PubMed] [Google Scholar]
Farrell 2005
- Farrell G, Cubit K. Nurses under threat: a comparison of content of 28 aggression management programs. International Journal of Mental Health Nursing 2005;14(1):44‐53. [DOI: 10.1111/j.1440-0979.2005.00354.x; PUBMED: 15733285] [DOI] [PubMed] [Google Scholar]
Fazel 2006
- Fazel S, Grann M. The population impact of severe mental illness on violent crime. American Journal of Psychiatry 2006;163(8):1397‐403. [DOI: 10.1176/ajp.2006.163.8.1397] [DOI] [PubMed] [Google Scholar]
Gaskin 2007
- Gaskin CJ, Elsom SJ, Happell B. Interventions for reducing the use of seclusion in psychiatric facilities: review of the literature. British Journal of Psychiatry 2007;191(4):298‐303. [DOI: 10.1192/bjp.bp.106.034538; PUBMED: 17906239] [DOI] [PubMed] [Google Scholar]
Gewandter 2014
- Gewandter JS, McDermott MP, McKeown A, Smith SM, Williams MR, Hunsinger M, et al. Reporting of missing data and methods used to accommodate them in recent analgesic clinical trials: ACTTION systematic review and recommendations. Pain 2014;155(9):1871‐7. [DOI: 10.1016/j.pain.2014.06.018; PUBMED: 24993384] [DOI] [PubMed] [Google Scholar]
Gournay 2001
- Gournay K. The Recognition, Prevention and Therapeutic Management of Violence in Mental Health Care: A Consultation Document. London (UK): Department of Health Services Research, Institute of Psychiatry and South London and Maudsley NHS Trust, 2001. [Google Scholar]
GRADE 2004
- Grade Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490‐4. [DOI: 10.1136/bmj.328.7454.1490; PMC428525; PUBMED: 15205295] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEPro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed 27 June 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Harris 2012
- Harris B, Leather P. Levels and consequences of exposure to service user violence: evidence from a sample of UK social care staff. British Journal of Social Work 2012;42(5):851‐69. [DOI: 10.1093/bjsw/bcr128] [DOI] [Google Scholar]
Heckemann 2015
- Heckemann B, Zeller A, Hahn S, Dassen T, Schols J, Halfens R. The effect of aggression management training programmes for nursing staff and students working in an acute hospital setting. A narrative review of current literature. Nurse Education Today 2015;35(1):212‐9. [DOI: 10.1016/j.nedt.2014.08.003; PUBMED: 25200511] [DOI] [PubMed] [Google Scholar]
Hester 2009
- Hester M. Who Does What to Whom? Gender and Domestic Violence Perpetrators. Bristol (UK): University of Bristol, 2009. [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, editor(s). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011c
- Higgins JPT, Deeks JJ, Altman DG, editor(s). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hill 1987
- Hill J, Spreat S. Staff injury rates associated with implementation of contingent restraint. Mental Retardation 1987;25(3):141‐5. [PUBMED: 3600269] [PubMed] [Google Scholar]
Hockenhull 2012
- Hockenhull JC, Whittington R, Leitner M, Barr W, McGuire J, Cherry MG, et al. A systematic review of prevention and intervention strategies for populations at high risk of engaging in violent behaviour: update 2002–8. Health Technology Assessment 2012;16(3):1‐152. [DOI: 10.3310/hta16030; PMC4781592; PUBMED: 22330980] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollins 2010
- Hollins L. Managing the risks of physical intervention: developing a more inclusive approach. Journal of Psychiatric and Mental Health Nursing 2010;17(4):369‐76. [DOI: 10.1111/j.1365-2850.2009.01542.x; PUBMED: 20529189] [DOI] [PubMed] [Google Scholar]
Johnson 2011
- Johnson A. Caregiver's corner webinars: crisis situations and de‐escalation strategies. hdsa.org/living‐with‐hd/caregivers‐corner‐webinars/crisis‐situations‐de‐escalation‐strategies/ (accessed 3 February 2015).
Johnson 2012
- Johnson P. Staff injury arising from the use of physical intervention. Journal of Learning Disabilities and Offending Behaviour 2012;3(1):35‐43. [DOI: 10.1108/20420921211236870] [DOI] [Google Scholar]
Jonker 2008
- Jonker EJ, Goossens PJ, Steenhuis IHM, Oud NE. Patient aggression in clinical psychiatry: perceptions of mental health nurses. Journal of Psychiatric and Mental Health Nursing 2008;15(6):492‐9. [DOI: 10.1111/j.1365-2850.2008.01261.x; PUBMED: 18638210] [DOI] [PubMed] [Google Scholar]
Kaplan 1983
- Kaplan SG, Wheeler EG. Survival skills for working with potentially violent clients. Social Casework 1983;64(6):339‐46. [PUBMED: 10262529] [PubMed] [Google Scholar]
Leadbetter 1995
- Leadbetter D, Paterson B. De‐escalating aggressive behaviour. In: Kidd B, Stark C editor(s). Management of Violence and Aggression in Health Care. London (UK): Gaskell, 1995:49‐83. [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 20011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Levenson 2004
- Levenson JL. The American Psychiatric Publishing Textbook of Psychosomatic Medicine. Washington (DC): American Psychiatric Association, Inc, 2004. [Google Scholar]
Little 2012
- Little RJ, D'Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, et al. The prevention and treatment of missing data in clinical trials. New England Journal of Medicine 2012;367(14):1355‐60. [DOI: 10.1056/NEJMsr1203730; PMC3771340; PUBMED: 23034025] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loudon 2015
- Loudon K, Treweek S, Sullivan F, Donnan P, Thorpe KE, Zwarenstein M. The PRECIS‐2 tool: designing trials that are fit for purpose. BMJ 2015;350:h2147. [DOI: 10.1136/bmj.h2147; /www.precis‐2.org/; PUBMED: 25956159] [DOI] [PubMed] [Google Scholar]
Maguire 2007
- Maguire J, Ryan D. Aggression and violence in mental health services: categorizing the experiences of Irish nurses. Journal of Psychiatric and Mental Health Nursing 2007;14(2):120‐7. [10.1111/j.1365‐2850.2007.01051.x] [DOI] [PubMed] [Google Scholar]
Mandt 1998
- Mandt D. The Mandt System: Putting People First. Richardson (TX): David Mandt & Associates, 1998. [ASIN: B007YK158K] [Google Scholar]
Mason 2001
- Mason T, Whitehead E. Some specific problems of secluding female patients. Medicine, Science, and the Law 2001;41(4):315‐24. [DOI: 10.1177/002580240104100408; PUBMED: 11693227] [DOI] [PubMed] [Google Scholar]
Mavandadi 2016
- Mavandadi V, Bieling PJ, Madsen V. Effective ingredients of verbal de‐escalation: validating an English modified version of the ‘De‐Escalating Aggressive Behaviour Scale'. Journal of Psychiatric and Mental Health Nursing 2016;23(6‐7):357‐68. [DOI: 10.1111/jpm.12310; PUBMED: 27271938] [DOI] [PubMed] [Google Scholar]
Mofrad 2015
- Mofrad SHK, Mehrabi T. The role of self‐efficacy and assertiveness in aggression among high‐school students in Isfahan. Journal of Medicine and Life 2015;8(4):225‐31. [PMC5319278; PUBMED: 28316736] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLOS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097; PMC2707599; PUBMED: 19621072] [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrison 1991
- Morrison P, Lehane M. Use of environmental seclusion monitored. Nursing Times 1991;87(37):54. [PUBMED: 1896348] [PubMed] [Google Scholar]
Morrison 1997
- Morrison P, Lehane M, Palmer C, Meehan T. The use of behavioural mapping in a study of seclusion. The Australia and New Zealand Journal of Mental Health Nursing 1997;6(1):11‐8. [PUBMED: 9214855] [PubMed] [Google Scholar]
Muralidharan 2006
- Muralidharan S, Fenton M. Containment strategies for people with serious mental illness. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002084.pub2; PUBMED: 16855984] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nau 2009a
- Nau J, Dassen T, Needham I, Halfens R. The development and testing of a training course in aggression for nursing students: a pre‐ and post‐test study. Nurse Education Today 2009;29(2):196‐207. [DOI: 10.1016/j.nedt.2008.08.011; PUBMED: 18835068] [DOI] [PubMed] [Google Scholar]
Nau 2009b
- Nau J, Halfens R, Needham I, Dassen T. The De‐Escalating Aggressive Behaviour Scale: development and psychometric testing. Journal of Advanced Nursing 2009;65(9):1956‐64. [DOI: 10.1111/j.1365-2648.2009.05087.x; PUBMED: 19694859] [DOI] [PubMed] [Google Scholar]
NCCMH 2015
- National Collaborating Centre for Mental Health (NCCMH). Dementia: the NICE‐SCIE Guideline on supporting people with dementia and their carers in health and social care. www.scie.org.uk/publications/misc/dementia/dementia‐fullguideline.pdf?res=true (accessed prior to 21 May 2018).
NHS 2014
- NHS England. Briefing note: issues highlighted by the 2014 NHS staff survey in England. http://www.nhsstaffsurveys.com/Caches/Files/NHS%20staff%20survey_nationalbriefing_Final%2024022015%20UNCLASSIFIED.pdf (accessed 15 March 2015).
NHS BSA 2013
- National Health Service Business Services Authority (NHS BSA). Conflict resolution training: implementing the learning aims and outcomes. www.crisisprevention.com/CPI/media/Media/Specialties/pos/reports‐and‐guidelines/mapa/Conflict_resolution_training_guidance_July_2013.pdf (accessed 24 March 2014).
NHS Protect 2015
- NHS Protect. Reported physical assaults on NHS staff figures (2014 ‐ 2015). www.nwas.nhs.uk/media/865201/reported‐physical‐assaults‐2014‐15.pdf (accessed 15 December 2015).
NICE 2015
- National Institute for Health and Care Excellence (NICE). Violence and aggression: short‐term management in mental health, health and community settings. www.nice.org.uk/guidance/ng10/resources/violence‐and‐aggression‐shortterm‐management‐in‐mental‐health‐health‐and‐community‐settings‐pdf‐1837264712389 (accessed prior to 21 May 2018).
O'Brien 2004
- O'Brien L, Cole R. Mental health nursing practice in acute psychiatric close‐observation areas. International Journal of Mental Health Nursing 2004;13(2):89‐99. [DOI: ; PUBMED: 15318903] [DOI] [PubMed] [Google Scholar]
Oldham 1983
- Oldham JM, Russakoff LM, Prusnofsky L. Seclusion. Patterns and milieu. Journal of Nervous and Mental Disease 1983;171(11):645‐50. [PUBMED: 6631428] [PubMed] [Google Scholar]
Olofsson 1995
- Olofsson B, Norgberg A, Jacobsson L. Nurses' experience with using force in institutional care of psychiatric patients. Nordic Journal of Psychiatry 1995;49(5):325–30. [DOI: 10.3109/08039489509011924] [DOI] [Google Scholar]
Partie 2001
- Partie M. Therapeutic Options Instructor Manual. Newark (DE): Therapeutic Options, 2001. [Google Scholar]
Paterson 1997
- Paterson B, Leadbetter D, McComish A. De‐escalation in the management of aggression and violence. Nursing Times 1997;93(36):58‐61. [PUBMED: 9380578] [PubMed] [Google Scholar]
Polman 2007
- Polman H, Orobio de Castro B, Koops W, Boxtel HW, Merk WW. A meta‐analysis of the distinction between reactive and proactive aggression in children and adolescents. Journal of Abnormal Child Psychology 2007;35(4):522‐35. [DOI: 10.1007/s10802-007-9109-4; PUBMED: 17340178] [DOI] [PubMed] [Google Scholar]
Price 2012
- Price O, Baker J. Key components of de‐escalation techniques: a thematic synthesis. International Journal of Mental Health Nursing 2012;21(4):310‐9. [DOI: 10.1111/j.1447-0349.2011.00793.x; PUBMED: 22340073] [DOI] [PubMed] [Google Scholar]
Rao 2017
- Du M, Wang X, Yin S, Shu W, Hao R, Zhao S, et al. De‐escalation techniques for psychosis‐induced aggression or agitation. Cochrane Database of Systematic Reviews 2017, Issue 4. [DOI: 10.1002/14651858.CD009922.pub2; PUBMED: 28368091] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rennie 2001
- Rennie D. CONSORT revised—improving the reporting of randomized trials. JAMA 2001;285(15):2006‐7. [www.consort‐statement.org; PUBMED: 11308440] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richmond 2012
- Richmond JS, Berlin JS, Fishkind AB, Holloman GH Jr, Zeller SL, Wilson MP, et al. Verbal de‐escalation of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA De‐escalation Workgroup. Western Journal of Emergency Medicine 2012;13(1):17‐25. [DOI: 10.5811/westjem.2011.9.6864; PMC3298202; PUBMED: 22461917] [DOI] [PMC free article] [PubMed] [Google Scholar]
Richter 2007
- Richter D, Needham I. The effects of aggression management trainings for mental health care and disability care staff — systematic review [Effekte von mitarbeiterbezogenen Trainingsprogrammen zum aggressionsmanagement in einrichtungen der psychiatrie und behindertenhilfe ‐ systematische literaturübersicht]. Psychiatrische Praxis 2007;34(1):7‐14. [DOI: 10.1055/s-2006-940063; PUBMED: 17211780] [DOI] [PubMed] [Google Scholar]
Robertson 2012
- Robertson T, Daffern M, Thomas S, Martin T. De‐escalation and limit‐setting in forensic mental health units. Journal of Forensic Nursing 2012;8(2):94‐101. [DOI: 10.1111/j.1939-3938.2011.01125.x; PUBMED: 22621667] [DOI] [PubMed] [Google Scholar]
Roizen 1997
- Roizen J. Epidemiological issues in alcohol‐related violence. Recent Developments in Alcoholism 1997;13:7‐40. [PUBMED: 9122506] [DOI] [PubMed] [Google Scholar]
Shukla‐Mehta 2002
- Shukla‐Mehta S, Albin RW. Understanding behavioral escalation: from theory to practice. Behavioral Development Bulletin 2002;11(1):19‐26. [DOI: 10.1037/h0100487] [DOI] [Google Scholar]
Smith 2004
- Smith P, Fox L, Johnson L, Nihart MA, Smiar N. Pro‐ACT: Professional Assault Crisis Training. San Clemente (CA): Crisis Prevention Institute, 2004. [Google Scholar]
Snowden 2001
- Snowden P. Substance misuse and violence: the scope and limitations of forensic psychiatry's role. Advances in Psychiatric Treatment 2001;7(3):189‐97. [DOI: 10.1192/apt.7.3.189] [DOI] [Google Scholar]
Sprigg 2007
- Sprigg CA, Armitage CJ, Hollis K. Verbal abuse in the National Health Service: impressions of the prevalence, perceived reasons for and relationships with staff psychological well‐being. Emergency Medicine Journal 2007;24(4):281‐2. [DOI: 10.1136/emj.2006.038166; PMC2658236; PUBMED: 17384383] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stone 2010
- Stone TE, McMillan M, Hazelton M. Swearing: its prevalence in healthcare settings and impact on nursing practice. Journal of Psychiatric and Mental Health Nursing 2010;17(6):528‐34. [DOI: 10.1111/j.1365-2850.2010.01554.x; PUBMED: 20633080] [DOI] [PubMed] [Google Scholar]
Streiner 2008
- Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to their Development and Use. 4th Edition. Oxford (UK): Oxford University Press, 2008. [Google Scholar]
Sullivan 2004
- Sullivan D, Wallis M, Lloyd C. Effects of patient‐focused care on seclusion in a psychiatric intensive care unit. International Journal of Therapy & Rehabilitation 2004;11(11):503‐8. [DOI: 10.12968/ijtr.2004.11.11.17202] [DOI] [Google Scholar]
Taylor 2005
- Taylor JL, Novaco RW. Anger Treatment for People with Developmental Disabilities: A Theory, Evidence and Manual Based Approach. Chichester (UK): John Wiley & Sons, 2005. [Google Scholar]
Uzun 2003
- Uzun Ö. Profession and society. Journal of Nursing Scholarship 2003;35(1):81‐5. [DOI: 10.1111/j.1547-5069.2003.00081.x] [DOI] [PubMed] [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36): I. Conceptual framework and item selection. Medical Care 1992;30(6):473‐83. [PUBMED: 1593914] [PubMed] [Google Scholar]
Whittington 2009
- Whittington R, Bowers L, Nolan P, Simpson A, Neil L. Approval ratings of inpatient coercive interventions in a national sample of mental health service users and staff in England. Psychiatric Services 2009;60(6):792‐8. [DOI: 10.1176/ps.2009.60.6.792; PUBMED: 19487349] [DOI] [PubMed] [Google Scholar]
WHO 1992
- World Health Organization (WHO). The ICD‐10 Classification of Mental and Behavioural Disorders. Geneva (CH): World Health Organisation, 1992. [Google Scholar]
Zumbo 2007
- Zumbo BD. Validity: foundational issues and statistical methodology. In: Rao CR, Sinharay S editor(s). Handbook of Statistics: Psychometrics. Vol. 26, Amsterdam (NL): Elsevier, 2007:45‐79. [ISSN: (Series): 0169‐7161] [Google Scholar]
References to other published versions of this review
Spencer 2016
- Spencer S, Johnson P. De‐escalation techniques for managing aggression. Cochrane Database of Systematic Reviews 2016, Issue 1. [DOI: 10.1002/14651858.CD012034] [DOI] [PMC free article] [PubMed] [Google Scholar]


