Abstract
Background
Chronic antipsychotic drug treatment may cause tardive dyskinesia (TD), a long‐term movement disorder. Gamma‐aminobutyric acid (GABA) agonist drugs, which have intense sedative properties and may exacerbate psychotic symptoms, have been used to treat TD.
Objectives
1. Primary objective
The primary objective was to determine whether using non‐benzodiazepine GABA agonist drugs for at least six weeks was clinically effective for the treatment of antipsychotic‐induced TD in people with schizophrenia, schizoaffective disorder or other chronic mental illnesses.
2. Secondary objectives
The secondary objectives were as follows.
To examine whether any improvement occurred with short periods of intervention (less than six weeks) and, if this did occur, whether this effect was maintained at longer periods of follow‐up.
To examine whether there was a differential effect between the various compounds.
To test the hypothesis that GABA agonist drugs are most effective for a younger age group (less than 40 years old).
Search methods
We searched the Cochrane Schizophrenia Group Trials Register (last searched April 2017), inspected references of all identified studies for further trials, and, when necessary, contacted authors of trials for additional information.
Selection criteria
We included randomised controlled trials of non‐benzodiazepine GABA agonist drugs in people with antipsychotic‐induced TD and schizophrenia or other chronic mental illness.
Data collection and analysis
Two review authors independently selected and critically appraised studies, extracted and analysed data on an intention‐to‐treat basis. Where possible and appropriate we calculated risk ratios (RRs) and their 95% confidence intervals (CIs). For continuous data we calculated mean differences (MD). We assumed that people who left early had no improvement. We contacted investigators to obtain missing information. We assessed risk of bias for included studies and created a 'Summary of findings' table using GRADE.
Main results
We included 11 studies that randomised 343 people. Overall, the risk of bias in the included studies was unclear, mainly due to poor reporting; allocation concealment was not described, generation of the sequence was not explicit, participants and outcome assessors were not clearly blinded. For some studies we were unsure if data were complete, and data were often poorly or selectively reported.
Data from six trials showed that there may be a clinically important improvement in TD symptoms after GABA agonist treatment compared with placebo at six to eight weeks follow‐up (6 RCTs, n = 258, RR 0.83, CI 0.74 to 0.92; low‐quality evidence). Data from five studies showed no difference between GABA agonist treatment and placebo for deterioration of TD symptoms (5 RCTs, n = 136, RR 1.90, CI 0.70 to 5.16; very low‐quality evidence). Studies reporting adverse events found a significant effect favouring placebo compared with baclofen, sodium valproate or progabide for dizziness/confusion (3 RCTs, n = 62 RR 4.54, CI 1.14 to 18.11; very low‐quality evidence) and sedation/drowsiness (4 RCTS, n = 144, RR 2.29, CI 1.08 to 4.86; very low‐quality evidence). Studies reporting on akathisia (RR 1.05, CI 0.32 to 3.49, 2 RCTs, 80 participants), ataxia (RR 3.25, CI 0.36 to 29.73, 2 RCTs, 95 participants), nausea/vomiting (RR 2.61, CI 0.79 to 8.67, 2 RCTs, 64 participants), loss of muscle tone (RR 3.00, CI 0.15 to 59.89, 1 RCT, 10 participants), seizures (RR 3.00, CI 0.24 to 37.67, 1 RCT, 2 participants), hypotension (RR 3.04, CI 0.33 to 28.31, 2 RCTs, 119 participants) found no significant difference between GABA drug and placebo (very low‐quality evidence). Evidence on mental state also showed no effect between treatment groups (6 RCTS, n = 121, RR 2.65, CI 0.71 to 9.86; very low‐quality evidence) as did data for leaving the study early (around 10% in both groups, 6 RCTS, n = 218, RR 1.47, CI 0.69 to 3.15; very low‐quality evidence). No study reported on social confidence, social inclusion, social networks, or personalised quality of life, a group of outcomes selected as being of particular importance to patients.
Authors' conclusions
We are uncertain about the evidence of the effects of baclofen, progabide, sodium valproate or tetrahydroisoxazolopyridinol (THIP) for people with antipsychotic‐induced TD. Evidence is inconclusive and unconvincing. The quality of data available for main outcomes ranges from very low to low. Any possible benefits are likely to be outweighed by the adverse effects associated with their use.
Plain language summary
Gamma‐aminobutyric acid agonists for antipsychotic‐induced tardive dyskinesia
Review question.
To determine the effects of gamma‐aminobutyric acid (GABA) agonist drugs in the treatment of tardive dyskinesia for people with schizophrenia or similar mental health problems.
Background.
People with schizophrenia often hear voices and see things (hallucinations) and have strange beliefs (delusions). The main treatment of schizophrenia is antipsychotic drugs. However, these drugs can have debilitating side effects. Tardive dyskinesia is an involuntary movement that causes the face, mouth, tongue and jaw to convulse, spasm and grimace. It is caused by long‐term or high‐dose antipsychotic drugs, is difficult to treat and can be incurable. GABA agonist drugs have been used to treat tardive dyskinesia but have intense sedative properties and may make mental health or psychotic symptoms worse. GABA agonist drugs include baclofen, progabide, sodium valproate, and tetrahydroisoxazolopyridinol (THIP).
Study characteristics.
The review includes 11 studies investigating the use of GABA agonist drugs compared with placebo. All studies involved small numbers of participants (2 to 80 people) with schizophrenia or other chronic mental illnesses who had also developed antipsychotic‐induced tardive dyskinesia.
Key results.
Evidence of the effects of GABA agonist drugs in the treatment of tardive dyskinesia is not conclusive and not convincing. Any possible benefits of GABA agonist drugs are likely to be outweighed by the adverse effects associated with their use.
Quality of the evidence.
Evidence is weak, short term, small scale and poorly reported. It is not possible to recommend these drugs as a treatment for tardive dyskinesia.
This plain language summary was adapted by the review authors from a summary originally written by Ben Gray, Senior Peer Researcher, McPin Foundation (http://mcpin.org/).
Summary of findings
Summary of findings for the main comparison. GABA DRUGS for antipsychotic‐induced tardive dyskinesia.
| GABA DRUGS for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: patients with antipsychotic‐induced TD Settings: Inpatients and outpatients Intervention: GABA drugs | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | GABA drugs | |||||
|
Tardive dyskinesia: Not improved to a clinically important extent follow‐up: 6‐8 weeks |
Medium risk population1 | RR 0.83 (0.74 to 0.92) | 258 (3 studies) | ⊕⊕⊝⊝ low2,3 | Studies on baclofen, progabide and sodium valproate contributed to this outcome. | |
| 929 per 1000 | 771 per 1000 (687 to 854) | |||||
|
Tardive dyskinesia: Deterioration of symptoms follow‐up: 3‐6 weeks |
Medium risk population1 | RR 1.90 (0.70 to 5.16) | 136 (5 studies) | ⊕⊝⊝⊝ very low2,4 | Studies on baclofen and sodium valproate contributed to this outcome. | |
| 71 per 1000 | 136 per 1000 (50 to 369) | |||||
|
Adverse events follow‐up: 3‐8 weeks |
Studies reporting on dizziness/confusion (RR 4.54 CI 1.14 to 18.11, 3 RCTs, 62 participants) and sedation/drowsiness (RR 2.29 CI 1.08 to 4.86, 4 RCTs, 144 participants) found a significant effect favouring placebo compared with baclofen, sodium valproate or progabide. Studies reporting on akathisia (RR 1.05 CI 0.32 to 3.49, 2 RCTs, 80 participants), ataxia (RR 3.25 CI 0.36 to 29.73, 2 RCTs, 95 participants), nausea/vomiting (RR 2.61 CI 0.79 to 8.67, 2 RCTs, 64 participants), loss of muscle tone (RR 3.00 CI 0.15 to 59.89, 1 RCT, 10 participants), seizures (RR 3.00 CI 0.24 to 37.67, 1 RCT, 2 participants), hypotension (RR 3.04 CI 0.33 to 28.31, 2 RCTs, 119 participants) found no significant difference between GABA drug and placebo. | 284 (9 studies) | ⊕⊝⊝⊝ very low2,4 | Studies on baclofen, progabide, sodium valproate and THIP contributed to this outcome. | ||
|
Mental state: Deterioration follow‐up: 3‐6 weeks |
Medium risk population1 | RR 2.65 (0.71 to 9.86) | 121 (6 studies) | ⊕⊝⊝⊝ very low2,4 | Studies on baclofen, progabide, sodium valproate and THIP contributed to this outcome. | |
| 18 per 1000 | 46 per 1000 (12 to 173) | |||||
|
Acceptability of treatment: Leaving the study early follow‐up: 3‐6 weeks |
Medium risk population1 | RR 1.47 (0.69 to 3.15) | 218 (6 studies) | ⊕⊝⊝⊝ very low2,4,5 | Studies on baclofen, progabide and sodium valproate contributed to this outcome. | |
| 75 per 1000 | 111 per 1000 (52 to 238) | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life measures | No studies reported on this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 This risk approximately equates with control risk of trial participants. 2 Downgraded one step for risk of bias. 3 Downgraded one step for imprecision: number of events and participants is small. 4 Downgraded two steps for imprecision: number of events and participants is small, and 95% CIs are wide and include both no effect and appreciable benefit or harm for the intervention.
5 Downgraded one step for indirectness: Leaving the study early can give an indication of, but is not a direct measure of, acceptability of the treatment.
Background
Description of the condition
Tardive dyskinesia (TD) is a movement disorder characterised by abnormal, repetitive and involuntary movements primarily including tongue protrusion, side‐to‐side or rotatory movement of the jaw, lip smacking, puckering and pursing, and rapid eye blinking (Casey 1999). Its occurrence is estimated to be 20% to 50% of those on long‐standing therapy with conventional antipsychotics depending on the characteristics of the population studied (Glazer 2000). Every year 4% to 5% of those who continually use these drugs begin to show signs of TD (APA 1992). Elderly patients are at five to six times greater risk to develop TD (Jeste 2000). This disorder can result in considerable social and physical disability (Barnes 1993).
The exact mechanisms of the pathophysiology of TD are unknown. Many preclinical models, one of them being the dopamine receptor hypersensitivity hypothesis, have been developed to explain the underlying pathophysiology, but none has yet provided an unequivocal explanation (Casey 2000). Although the most frequent cause of TD is the use of antipsychotic medication, it is striking that dose reduction can lead to a temporary exacerbation in symptoms. Conversely, increasing the dose is often associated with a temporary remission. Antipsychotic drugs block certain chemical receptor sites in the brain ‐ one of these is specific for dopamine (Casey 1994). The interaction between antipsychotic drugs and the dopamine cells has been proposed as the mechanism for their beneficial effects in psychoses as well as the cause of the movement side effects (Jeste 1982). The most interesting and consistent findings regarding candidate gene studies of TD have focused on the dopamine D3 receptor gene (DRD3). Several groups have reported an association between a serineto‐glycine polymorphism in exon 1 of the DRD3 gene and TD (Bakker 2006). Specifically, each group found that either the glycine/glycine genotype or the glycine allele conferred an elevated risk for TD compared with serine/serine homozygotes. One study found a high frequency of this type of homozygosity (22% to 24%) among patients with TD compared with the relative under‐representation (4% to 6%) of this genotype in patients without TD (Steen 1997). This may be an explanation to the susceptibility for TD development in some but not most patients.
Description of the intervention
There are many drugs in the gamma‐aminobutyric acid (GABA) family. Baclofen (Figure 1), gamma‐vinyl‐GABA, gamma‐acetylenic‐GABA, progabide, muscimol (Figure 2), sodium valproate (Figure 3), and tetrahydroisoxazolopyridine (THIP) are the focus of this review, and the benzodiazepines, a large group in themselves, have been reviewed elsewhere (Bergman 2018). The GABA agonist drugs have been trialled as a treatment for people with TD, despite their sedative properties, and the possibility that they may exacerbate psychotic symptoms (Barnes 1988; Gardos 1994).
1.
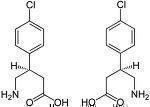
Baclofen
2.

Muscimol
3.
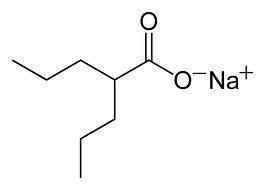
Sodium valproate
How the intervention might work
One hypothesis explaining the cause of antipsychotic‐induced TD is that chronic blockade of dopamine receptors in specific cells of the brain (neurones from the nigrostriatum) causes an overgrowth of these receptors (Casey 1994). This, in turn, leads to inactivity in another set of cells in the brain, which employ another neurochemical, GABA (Barnes 1993). The GABA agonists supplement the function of these underactive cells. There is also evidence from animal experiments to suggest that GABA dysfunction may be associated with movement disorders (Gunne 1984).
Why it is important to do this review
Several atypical antipsychotic drugs have been produced in the last decades that claim to cause less or no TD (Lieberman 1996). These claims may or may not be true, and certainly evidence does point to the fact that thoughtful use of older generation drugs is not associated with any more problems of TD than with newer treatments (Chouinard 2008). However, in a global context, it is likely that the less expensive and more familiar drugs ‐ such as chlorpromazine or haloperidol ‐ will continue to be the mainstay of treatment of people with schizophrenia (WHO Essential List 2010). Use of drugs such as these is associated with emergence of TD and, therefore, TD will remain a problem for years to come.
Given the high incidence and prevalence of TD among people taking antipsychotic medication, the need for prevention or treatment is clear. Unfortunately, there has been sparse evidence to guide clinicians (NICE 2014; Taylor 2009). Although many treatments have been tested, no one intervention has been shown clearly to be effective. Cessation or reduction of the dose of antipsychotic medication is the ideal management for TD. In clinical practice this is not always possible, not least because in many individuals such a reduction would lead to relapse. This review focuses on whether the addition of benzodiazepines to those already receiving antipsychotic medication is likely to help TD.
This review is one in a series of Cochrane reviews (see Table 2) evaluating treatments for antipsychotic‐induced TD, and is an update of a Cochrane review first published in 2000 (Soares‐Weiser 2000), and previously updated in 2001 (Soares‐Weiser 2001), in 2004 (Rathbone 2004) and in 2011 (Alabed 2011).
1. Series of related reviews.
| Review title | Reference |
| Anticholinergic medication for neuroleptic‐induced tardive dyskinesia | Bergman 2018a |
| Benzodiazepines for neuroleptic‐induced tardive dyskinesia | Bergman 2018 |
| Calcium channel blockers for neuroleptic‐induced tardive dyskinesia | Essali 2011 |
| Cholinergic medication for neuroleptic‐induced tardive dyskinesia | Tammenmaa 2002 |
| Gamma‐aminobutyric acid agonists for neuroleptic‐induced tardive dyskinesia | This review |
| Miscellaneous treatments for neuroleptic‐induced tardive dyskinesia | Soares‐Weiser 2003 |
| Neuroleptic reduction and/or cessation and neuroleptics as specific treatments for tardive dyskinesia | Bergman 2018b |
| Non‐neuroleptic catecholaminergic drugs for neuroleptic induced tardive dyskinesia | El‐Sayeh 2006 |
| Vitamin E | Soares‐Weiser 2018 |
Objectives
1. Primary objective
The primary objective was to determine whether using non‐benzodiazepine gamma‐aminobutyric acid (GABA) agonist drugs for at least six weeks was clinically effective for the treatment of antipsychotic‐induced tardive dyskinesia (TD) in people with schizophrenia, schizoaffective disorder or other chronic mental illnesses.
2. Secondary objectives
The secondary objectives were as follows.
To examine whether any improvement occurred with short periods of intervention (less than six weeks) and, if this did occur, whether this effect was maintained at longer periods of follow‐up.
To examine whether there was a differential effect between the various compounds.
To test the hypothesis that GABA agonist drugs are most effective for a younger age group (less than 40 years old).
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised controlled trials (RCTs). Where a trial was described as 'double‐blind' but it was implied that the study was randomised and the demographic details of each group were similar, we have included it. We excluded quasi‐randomised studies, such as those allocated by using alternate days of the week.
Types of participants
People with schizophrenia or other chronic mental illness, diagnosed by any criteria, irrespective of gender, age or nationality who:
required the use of antipsychotics for more than three months;
developed TD (diagnosed by any criteria at baseline and at least one other occasion) during antipsychotic treatment; and
for whom the dose of antipsychotic medication had been stable for one month or more (the same applies for those free of antipsychotics).
Types of interventions
1. The non‐benzodiazepine GABA agonist drugs
This includes baclofen, gamma‐vinyl‐GABA (GVG), gamma‐acetylenic‐GABA (GAG), muscimol, progabide, sodium valproate and tetrahydroisoxazolopyridinol (THIP): any dose or means of administration
compared with:
a. placebo or no intervention
or
b. any other intervention for the treatment of tardive dyskinesia (TD)
For this current update a post hoc decision was made to also include studies evaluating the above mentioned non‐benzodiazepine GABA agonist drugs compared with any other intervention for the treatment of TD.
Types of outcome measures
We have defined clinical efficacy as an improvement in the symptoms of TD of more than 50%, on any scale. When appropriate, we grouped the outcomes into time periods ‐ short term (less than six weeks), medium term (between six weeks and six months) and long term (more than six months).
Primary outcomes
1. Tardive dyskinesia (TD)
No clinically important improvement in the symptoms of individuals, defined as more than 50% improvement on any TD scale ‐ any time period.
2. Adverse effects
Other than deterioration of symptoms of TD, as reported in the trials ‐ any time period.
Secondary outcomes
1. Tardive dyskinesia (TD)
1.1 Any improvement in the symptoms of individuals on any TD scale, as opposed to no improvement. 1.2 Deterioration in the symptoms of individuals, defined as any deleterious change on any TD scale. 1.3 Average change in severity of TD during the trial period. 1.4 Average difference in severity of TD at the end of the trial.
2. General mental state changes
2.1 Deterioration in general psychiatric symptoms (such as delusions and hallucinations) defined as any deleterious change on any scale. 2.2 Average difference in severity of psychiatric symptoms at the end of the trial.
3. Acceptability of the treatment
3.1 Acceptability of the intervention to the participant group as measured by numbers of people dropping out during the trial.
4. Adverse effects
4.1 Use of any anti‐parkinsonism drugs. 4.2 Average score/change in extrapyramidal adverse effects. 4.3 Acute dystonia.
5. Hospital and service utilisation outcomes
5.1 Hospital admission. 5.2 Average change in days in hospital. 5.3 Improvement in hospital status (for example: change from formal to informal admission status, use of seclusion, level of observation).
6. Economic outcomes
6.1 Average change in total cost of medical and mental health care. 6.2 Total indirect and direct costs.
7. Social confidence, social inclusion, social networks, or personalised quality of life measures
7.1. No significant change in social confidence, social inclusion, social networks, or personalised quality of life measures. 7.2 Average score/change in social confidence, social inclusion, social networks, or personalised quality of life measures.
8. Behaviour
8.1 Clinically significant agitation. 8.2 Use of adjunctive medication for sedation. 8.3 Aggression to self or others.
9. Cognitive state
9.1 No clinically important change. 9.2 No change, general and specific.
'Summary of findings' table
We used the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach to interpret findings (Schünemann 2011) and used GRADEpro to export data from this review to create a 'Summary of findings' table. These tables provide outcome‐specific information concerning the overall quality of evidence from each included study in the comparison, the magnitude of effects of interventions examined and the sum of available data on all outcomes rated as important to patient care and decision making. We selected the following main outcomes for inclusion in the 'Summary of findings' table.
1. Tardive dyskinesia 1.1 Improved to a clinically important extent 1.2 Any improvement 1.3 Deteriorated
2. Mental state 2.1 Deteriorated
3. Adverse effect 3.1 Any adverse event
4. Acceptability of treatment 4.1 Leaving the study early
5. Social confidence, social inclusion, social networks, or personalised quality of life measures* 5.1 No significant change in social confidence, social inclusion, social networks, or personalised quality of life measures for either recipients of care or caregivers
This summary table was used to guide our conclusions and recommendations.
* Outcome designated important to patients. We wished to add perspectives from people’s personal experience with TD to the research agenda. A consultation with service users was planned where a previously published version of a review in the TD series (Soares‐Weiser 2018; Table 2) and a lay overview of the review gave the foundation for the discussions. The session was planned to provide time to reflect on current research on TD and consider gaps in knowledge. The report is not completed but we will add a link to it within this review and have added one figure showing service user expression of frustration concerning this neglected area of research (Figure 4). Informed by the results of the consultation, for this review, we updated outcomes for the 'Summary of findings' table.
4.
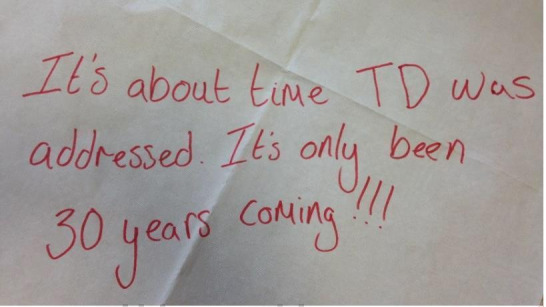
Message from one of the participants of the 'Public and patient involvement consultation of service user perspectives on tardive dyskinesia research'.
Search methods for identification of studies
Electronic searches
The searches in 2015 and 2017 were carried out in parallel with the updating of eight other TD reviews, see Table 2 for details. The searches covered all nine TD reviews.
1. Cochrane Schizophrenia Group’s Register
We searched Cochrane Schizophrenia Group’s Study‐Based Register of Trials on 16 July 16, 2015 and April 26, 2017 using the following string:*Tardive Dyskinesia* in Healthcare Condition Field of Study. In such a study‐based register, searching the major concept retrieves all the synonym keywords and relevant studies because all the studies have already been organised based on their interventions and linked to the relevant topics. The Cochrane Schizophrenia Group’s Register of Trials is compiled by systematic searches of major resources (including AMED, BIOSIS, CINAHL, Embase, MEDLINE, PsycINFO, PubMed, and registries of clinical trials) and their monthly updates, handsearches, grey literature, and conference proceedings (see Group’s Module). There is no language, date, document type, or publication status limitations for inclusion of records into the register.
2. Details of previous electronic searches
See Appendix 1.
Searching other resources
1. Reference searching
We searched references of all identified studies for further relevant studies.
2. Personal contact
Where necessary, we contacted the first author of each included study for information regarding unpublished trials. We noted the outcome of this contact in the Characteristics of included studies table.
Data collection and analysis
Data collection and analyses methods used by review authors for the 2015 and 2017 searches are listed below. For previous methods please see Appendix 1.
Selection of studies
Rosie Asher (RA) and Antonio Grande (AG) (see Acknowledgements) inspected all abstracts of studies identified as above and identified potentially relevant reports. We resolved disagreements by discussion, or where there was still doubt, we acquired the full‐text article for further inspection. We acquired the full‐text articles of relevant reports/abstracts meeting initial criteria for reassessment and carefully inspected for a final decision on inclusion (see Criteria for considering studies for this review). RA and AG were not blinded to the names of the authors, institutions or journal of publication. Where difficulties or disputes arose, we asked review author Hanna Bergman (HB) for help and where it was impossible to decide or if adequate information was not available to make a decision, we initially added these studies to those awaiting assessment and contacted the authors of the papers for clarification.
Data extraction and management
1. Extraction
RA and HB independently extracted data from all included studies. Again, we discussed any disagreement and documented decisions. With remaining problems Karla Soares‐Weiser (KSW) helped clarify issues and we documented these final decisions. We extracted data presented only in graphs and figures whenever possible, but included only if two review authors independently had the same result. We attempted to contact authors through an open‐ended request in order to obtain missing information or for clarification whenever necessary. If studies were multi‐centre, where possible, we extracted data relevant to each component centre separately.
2. Management
2.1 Forms
For this update we extracted data to simple forms. Extracted data are available here with a link to the original source PDF for each item.
2.2 Scale‐derived data
We included continuous data from rating scales only if:
the psychometric properties of the measuring instrument have been described in a peer‐reviewed journal (Marshall 2000); and
the measuring instrument has not been written or modified by one of the trialists for that particular trial.
Ideally, the measuring instrument should either be i. a self‐report or ii. completed by an independent rater or relative (not the therapist). We realise that this is not often reported clearly, we noted in Description of studies if this was the case or not.
2.3 Endpoint versus change data
There are advantages of both endpoint and change data. Change data can remove a component of between‐person variability from the analysis. On the other hand, calculation of change needs two assessments (baseline and endpoint), which can be difficult in unstable and difficult to measure conditions such as schizophrenia. We decided primarily to use endpoint data, and only use change data if the former were not available. We combined endpoint and change data in the analysis as we preferred to use mean differences (MD) rather than standardised mean differences (SMD) throughout (Higgins 2011).
2.4 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we applied the following standards to relevant data before inclusion.
Please note, we entered data from studies of at least 200 participants in the analysis, because skewed data pose less of a problem in large studies. We also entered all relevant change data as when continuous data are presented on a scale that includes a possibility of negative values (such as change data), it is difficult to tell whether data are skewed or not.
For endpoint data from studies < 200 participants:
(a) when a scale starts from the finite number zero, we subtracted the lowest possible value from the mean, and divided this by the standard deviation (SD). If this value was lower than 1, it strongly suggests a skew and we excluded these data. If this ratio was higher than one but below 2, there is suggestion of skew. We entered these data and tested whether their inclusion or exclusion changed the results substantially. Finally, if the ratio was larger than 2 we included these data, because skew is less likely (Altman 1996; Higgins 2011).
(b) if a scale starts from a positive value (such as the Positive and Negative Syndrome Scale (PANSS), (Kay 1986), which can have values from 30 to 210), we modified the calculation described above to take the scale starting point into account. In these cases skew is present if 2 SD > (S‐S min), where S is the mean score and 'S min' is the minimum score.
2.5 Common measure
Where relevant, to facilitate comparison between trials, we converted variables that can be reported in different metrics, such as days in hospital (mean days per year, per week or per month) to a common metric (e.g. mean days per month).
2.6 Conversion of continuous to binary
Where possible, we converted continuous outcome measures to dichotomous data. This can be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It is generally assumed that if there is a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the Positive and Negative Syndrome Scale (PANSS, Kay 1986), this can be considered as a clinically significant response (Leucht 2005; Leucht 2005a). If data based on these thresholds were not available, we used the primary cut‐off presented by the original authors.
2.7 Direction of graphs
Where possible, we entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for GABA agonist drugs. Where keeping to this made it impossible to avoid outcome titles with clumsy double‐negatives (e.g. 'Not un‐improved'), we presented data where the left of the line indicates an unfavourable outcome and noted this in the relevant graphs.
Assessment of risk of bias in included studies
RA and HB independently assessed risk of bias within the included studies by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions to assess trial quality (Higgins 2011). This set of criteria is based on evidence of associations between overestimate of effect and high risk of bias of the article such as sequence generation, allocation concealment, blinding, incomplete outcome data and selective reporting.
If the raters disagreed, we made the final rating by consensus, with the involvement of another member of the review group. Where inadequate details of randomisation and other characteristics of trials were provided, we contacted authors of the studies in order to obtain further information. If non‐concurrence occurred, we reported this.
We noted the level of risk of bias in the text of the review and in Figure 5; Figure 5 and Table 1.
5.
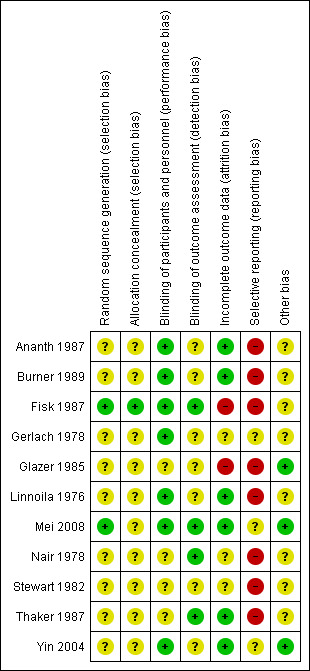
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
1. Binary data
For binary outcomes we calculated a standard estimation of the risk ratio (RR) and its 95% confidence interval (CI). It has been shown that RR is more intuitive (Boissel 1999) than odds ratios as odds ratios tend to be interpreted as RR by clinicians (Deeks 2000).
2. Continuous data
For continuous outcomes we estimated mean difference (MD) between groups. We preferred not to calculate effect size measures (standardised mean difference (SMD)). However, if scales of very considerable similarity were used, we presumed there was a small difference in measurement, and calculated effect size and transformed the effect back to the units of one or more of the specific instruments.
Unit of analysis issues
1. Cluster trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice), but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intra‐class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby P values are spuriously low, confidence intervals unduly narrow and statistical significance overestimated. This causes type I errors (Bland 1997; Gulliford 1999).
If any of the included trials had randomised participants by clusters, and where clustering had not been accounted for in primary studies, we would have presented such data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intra‐class correlation coefficients (ICCs) for their clustered data and to adjust for this by using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will present these data as if from a non‐cluster randomised study, but adjust for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the ICC [Design effect = 1+(m‐1)*ICC] (Donner 2002). If the ICC is not reported it will be assumed to be 0.1 (Ukoumunne 1999).
If cluster studies have been appropriately analysed taking into account ICCs and relevant data documented in the report, synthesis with other studies would be possible using the generic inverse variance technique.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state despite a wash‐out phase. For the same reason cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in severe mental illness, we only used data of the first phase of cross‐over studies.
3. Studies with multiple treatment groups
Where a study involved more than two treatment arms, if relevant, we presented the additional treatment arms in comparisons. If data were binary, we simply added and combined within the two‐by‐two table. If data were continuous, we combined data following the formula in section 7.7.3.8 (Combining groups) of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We did not use data where the additional treatment arms were not relevant.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss of follow‐up, data must lose credibility (Xia 2009). We chose that, for any particular outcome, should more than 50% of data be unaccounted for, we would not reproduce these data or use them within analyses. If, however, more than 50% of those in one arm of a study were lost, but the total loss was less than 50%, we addressed this within the 'Summary of findings' table by down‐rating quality. We also downgraded quality within the 'Summary of findings' table should loss be 25%‐50% in total.
2. Binary
In the case where attrition for a binary outcome was between 0% and 50% and where these data were not clearly described, we presented data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat (ITT) analysis). We assumed all those leaving the study early had no improvement. We undertook a sensitivity analysis to test how prone the primary outcomes were to change by comparing data only from people who completed the study to that point to the ITT analysis using the above assumptions.
3. Continuous
3.1 Attrition
We reported and used data where attrition for a continuous outcome was between 0% and 50%, and data only from people who completed the study to that point were reported.
3.2 Standard deviations
If standard deviations (SDs) were not reported, we first tried to obtain the missing values from the authors. If not available, where there were missing measures of variance for continuous data, but an exact standard error (SE) and confidence intervals available for group means, and either a P value or t value available for differences in mean, we calculated them according to the rules described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011): When only the SE is reported, sSDs are calculated by the formula SD = SE * square root (n). Chapters 7.7.3 and 16.1.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) present detailed formulae for estimating SDs from P values, t or F values, confidence intervals, ranges or other statistics. If these formulae did not apply, we calculated the SDs according to a validated imputation method which is based on the SDs of the other included studies (Furukawa 2006). Although some of these imputation strategies can introduce error, the alternative would be to exclude a given study’s outcome and thus to lose information. We nevertheless examined the validity of the imputations in a sensitivity analysis excluding imputed values.
3.3 Assumptions about participants who left the trials early or were lost to follow‐up
Various methods are available to account for participants who left the trials early or were lost to follow‐up. Some trials just present the results of study completers, others use the method of last observation carried forward (LOCF), while more recently methods such as multiple imputation or mixed‐effects models for repeated measurements (MMRM) have become more of a standard. While the latter methods seem to be somewhat better than LOCF (Leon 2006), we feel that the high percentage of participants leaving the studies early and differences in the reasons for leaving the studies early between groups is often the core problem in randomised schizophrenia trials. We therefore did not exclude studies based on the statistical approach used. However, we preferred to use the more sophisticated approaches. (e.g. MMRM or multiple‐imputation) and only presented completer analyses if some kind of ITT data were not available at all. Moreover, we addressed this issue in the item "incomplete outcome data" of the 'Risk of bias' tool.
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all included studies initially, without seeing comparison data, to judge clinical heterogeneity. We simply inspected all studies for clearly outlying people or situations which we had not predicted would arise and discussed in the text if they arose.
2. Methodological heterogeneity
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We simply inspected all studies for clearly outlying methods which we had not predicted would arise and discussed in the text if they arose.
3. Statistical heterogeneity
3.1 Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
3.2 Employing the I2 statistic
We investigated heterogeneity between studies by considering the I2 method alongside the Chi2 P value. The I2 provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2003). The importance of the observed value of I2 depends on i. magnitude and direction of effects and ii. strength of evidence for heterogeneity (e.g. P value from Chi2 test, or a confidence interval for I2). An I2 estimate greater than or equal to around 50% accompanied by a statistically significant Chi2 statistic, can be interpreted as evidence of substantial levels of heterogeneity (Section 9.5.2 Cochrane Handbook for Systematic Reviews of InterventionsHiggins 2011). We explored and discussed in the text potential reasons for substantial levels of heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in Section 10 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects. We did not use funnel plots for outcomes where there were 10 or fewer studies, or where all studies were of similar sizes. In future versions of this review, if funnel plots are possible, we will seek statistical advice in their interpretation.
Data synthesis
We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us and the random‐effects model takes into account differences between studies even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model. It puts added weight onto small studies which often are the most biased ones. Depending on the direction of effect, these studies can either inflate or deflate the effect size. We chose the fixed‐effect model for all analyses.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analyses
1.1 GABA agonist compound
As different GABA agonist compounds may have differential effects on antipsychotic‐induced TD, we performed a subgroup analysis to compare the effects of different GABA agonists. We proposed to undertake comparisons only for primary outcomes to minimise the risk of multiple comparisons.
1.2 Younger participants
We anticipated a subgroup analysis to test the hypothesis that the use of GABA agonists is most effective in younger patients (less than 40 years old). We had hoped to present data for this subgroup for the primary outcomes.
1.3 Duration of treatment
We also anticipated a subgroup analysis to examine whether any improvement occurred with short periods of intervention (less than six weeks) and, if this did occur, whether this effect was maintained at longer periods of follow‐up.
2. Investigation of heterogeneity
We reported when inconsistency was high. First, we investigated whether data were entered correctly. Second, if data were correct, we visually inspected the graph and successively removed outlying studies to see if homogeneity was restored. For this review we decided that should this occur with data contributing to the summary finding of no more than around 10% of the total weighting, we would present data. If not, we would not pool such data but discuss the issues. We know of no supporting research for this 10% cut off‐but are investigating use of prediction intervals as an alternative to this unsatisfactory state.
When unanticipated clinical or methodological heterogeneity were obvious, we simply discussed these. We did not undertake sensitivity analyses relating to these.
Sensitivity analysis
1. Implication of randomisation
If trials were described in some way as to imply randomisation, we undertook a sensitivity analyses for the primary outcomes. We included these studies in the analyses and if there was no substantive difference when the implied randomised studies were added to those with better description of randomisation, then we used relevant data from these studies.
2. Assumptions for lost binary data
Where assumptions had to be made regarding people lost to follow‐up (see Dealing with missing data), we compared the findings of the primary outcomes when we used our assumption compared with completer data only. If there was a substantial difference, we reported and discussed these results but continued to employ our assumption.
Where assumptions had to be made regarding missing SDs data (see Dealing with missing data), we compared the findings on primary outcomes when we used our assumption compared with completer data only. We undertook a sensitivity analysis to test how prone results were to change when 'completer' data only were compared to the imputed data using the above assumption. If there was a substantial difference, we reported and discussed these results but continued to employ our assumption.
3. Risk of bias
We analysed the effects of excluding trials that we judged to be at high risk of bias across one or more of the domains of randomisation (implied as randomised with no further details available), allocation concealment, blinding and outcome reporting for the meta‐analysis of the primary outcome. If the exclusion of trials at high risk of bias did not substantially alter the direction of effect or the precision of the effect estimates, we included data from these trials in the analysis
4. Imputed values
Had cluster trials been included, we would have undertaken a sensitivity analysis to assess the effects of including data from trials where we used imputed values for ICC in calculating the design effect.
If we found substantial differences in the direction or precision of effect estimates in any of the sensitivity analyses listed above, we did not pool data from the excluded trials with the other trials contributing to the outcome, but presented them separately
5. Fixed‐effect and random‐effects
We synthesised data using a fixed‐effect model, however, we also synthesised data for the primary outcome using a random‐effects model to evaluate whether this altered the significance of the results.
Results
Description of studies
Please see Characteristics of included studies and Characteristics of excluded studies.
Results of the search
The 2015 and 2017 updated searches were part of an update of nine Cochrane reviews, see Table 2. The 2015 search retrieved 704 references for 344 studies, see Figure 6 for study flow diagram. After having excluded irrelevant references at title and abstract screening, we screened full texts of 53 references (41 studies). Two of these studies (Mei 2008; Yin 2004) are new additions in Chinese to the eight already included studies of this review. Another study was previously excluded because only completers were analysed and numbers randomised were not available (Glazer 1985), however, in this update we decided to include it as we thought it might add value to the evidence. As a precaution we conducted sensitivity analyses excluding it (see Effects of interventions). We could also group four previously excluded references into one excluded study (Sikich 1999). The review now contains 30 excluded studies (39 references) and 11 included (14 references); no studies await assessment. As far as the review authors are aware there are no ongoing studies that would be relevant to this review.
6.
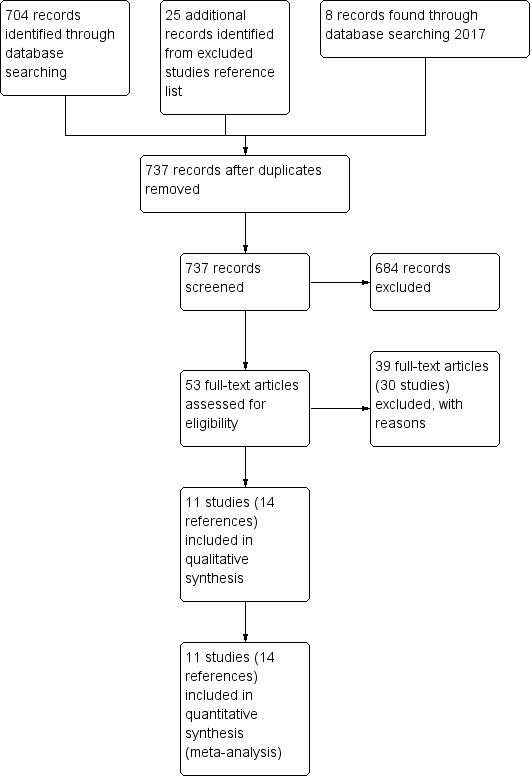
Study flow diagram for study selection.
The 2017 search found eight records (five studies). The editorial base of Cochrane Schizophrenia screened these records and no new studies were considered relevant to this review. They could be relevant to the other reviews in this series of tardive dyskinesia (TD) reviews (see Table 2), and have been put into awaiting assessment reference section of the Miscellaneous treatments for neuroleptic‐induced tardive dyskinesia review Soares‐Weiser 2003.
Included studies
The current update of this review now includes 11 studies with 343 participants published between 1976 and 2008. Three of these included studies are new to this update (Glazer 1985; Mei 2008; Yin 2004).
1. Methods
All studies were stated to be randomised and double‐blind. In general, however, allocation was poorly described. For further details please see sections below on Allocation and Blinding.
2. Design
All included studies presented a parallel longitudinal design. Five of the 11 studies used a cross‐over design (Ananth 1987; Gerlach 1978; Linnoila 1976; Nair 1978, Thaker 1987) with two periods. We had considered this as likely when embarking on the review and have used only the data from before the first cross‐over for the reasons outlined above (Unit of analysis issues).
3. Duration
Overall, the length of the trials were short. No study followed people up for longer than eight weeks and five of the 11 relevant studies fell into the short‐term category (less than six weeks). Six trials just fell into the medium term category (six to 26 weeks) and lasted between six (Burner 1989; Fisk 1987; Glazer 1985; Stewart 1982; Yin 2004) and eight weeks (Mei 2008).
4. Participants
Participants, now totaling 343 people with diagnoses of various chronic psychiatric disorders, but mainly schizophrenia. All had antipsychotic‐induced TD diagnosed using various methods. The number of participants ranged from two to 80 (median 31). People included in relevant trials were commonly quite elderly, with an average age of 50 and over.
5. Setting
Most trials were conducted with hospital inpatients. The studies themselves were from around the world, with four conducted in the USA (Glazer 1985; Nair 1978; Stewart 1982; Thaker 1987), two in China (Mei 2008; Yin 2004), and one each in Finland (Linnoila 1976), Denmark (Gerlach 1978), Canada (Ananth 1987), Switzerland (Burner 1989) and the UK (Fisk 1987).
6. Interventions
6.1 Non‐benzodiazepine gamma‐aminobutyric acid (GABA) agonist drugs
6.1.1 Baclofen
Baclofen was used in five trials. Ananth 1987 used it in a dose increasing over three days to 40 mg/day, whereas Gerlach 1978 used it in a dose increasing over two weeks to 120 mg/day max; range 20 mg to 120 mg/day. Glazer 1985 used a maximum baclofen dose of 90 mg/day. It was also used by Nair 1978 in a dose increasing gradually to 90 mg/day. In the Stewart 1982 study the dose was increased over four weeks to 90 mg/day unless efficacy was observed.
6.1.2 Gamma‐aminobutyric acid
Two gamma‐aminobutyric acid capsules three times per day was used by Mei 2008. the dose was not specified further.
6.1.3 Progabide
Progabide was used by Burner 1989 in the doses 20 mg, 30 mg or 45 mg/kg/day.
6.1.4 Sodium valproate
Sodium valproate was used by Linnoila 1976 in a fixed dose of 900 mg/day and by Fisk 1987 in a dose increasing over six days to 1500 mg/day. Yin 2004 applied doses of between 200 mg/day and 400 mg/day.
6.1.5 THIP
Thaker 1987 used tetrahydroisoxazolopyridinol (THIP) in a dose increasing over five days to 120 mg/day in the first patient and to 60 mg/day in the second patient.
6.2 Comparison group
All studies used placebo as a comparison. None of the included studies compared GABA agonists with another active intervention.
Participants remained on stable schizophrenia treatment antipsychotic medication during the trials.
7. Outcomes
7.1 General
Some outcomes were presented only in graphs, with inexact P values of differences, or a statement of significant or non‐significant difference. This made it impossible to acquire raw data for synthesis. Some continuous outcomes could not be extracted due to missing numbers of participants or missing means, standard deviations, or standard errors. All included studies used the LOCF strategy for the ITT analysis of dichotomous data. Details of the scales used in this review to quantify both TD and psychiatric symptoms are provided below. Data from these scales were reported either in continuous form or as binary figures where study authors have stipulated a cut‐off point at which they feel an outcome is reached (for example, 'Tardive dyskinesia: not improved to an important extent'). We have accepted these judgements and not cross‐checked the cut‐off points.
7.2 Scales used to measure TD symptoms
7.2.1 Abnormal Involuntary Movement Scale (AIMS)
This 12‐item scale consists of a standard examination followed by questions rating the orofacial, extremity and trunk movements, the dental status, and three global measurements (Guy 1976). Each of these items can be scored from zero (none) to four (severe). The AIMS ranges from four to 40 with higher scores indicating greater severity. This scale was used in Ananth 1987, Glazer 1985, Mei 2008; Nair 1978; Stewart 1982 and Yin 2004.
7.2.2 Abbreviated Dyskinesia Rating Scale ‐ Simpson Rating Scale (SRS)
This 15‐item scale measures the movements around the orofacial region, neck, trunk and extremities (Simpson 1979). Each of these items can be scored from one (absent) to six (severe). This scale ranges from 10 to 102 with higher scores indicating greater severity, and was used in Burner 1989.
7.2.3 Gerlach Scoring Scale for Oral Tardive Dyskinesia
This is a videotape technique where the oral movements (lingual and masticatory) are recorded for 10 minutes and evaluated according to their frequency zero to 18), amplitude (zero to six) and duration (zero to three) (Gerlach 1976). This scale was used in Gerlach 1978.
7.3 Scales used to measure mental state and behaviour
7.3.1 Brief Psychiatric Rating Scale (BPRS)
The BPRS is an 18‐item scale measuring positive symptoms, general psychopathology and affective symptoms (Overall 1962). The original scale has 16 items, although a revised 18‐item scale is commonly used. Total scores can range from zero to 126. Each item is rated on a seven‐point scale, with high scores indicating more severe symptoms. This scale was used in Mei 2008.
7.4 Scales used to measure adverse events
7.4.1 Treatment Emergent Symptom Scale (TESS)
This checklist assesses a variety of characteristics for each adverse event, including severity, relationship to the drug, temporal characteristics, contributing factors, course, and action taken to counteract the effect (Guy 1976). Symptoms can be listed a priori or can be recorded as observed by the investigator. High scores indicate worse symptoms. TESS was used in Yin 2004.
Studies awaiting classification
No studies await classification.
Ongoing studies
We know of no ongoing trials.
Excluded studies
We excluded 30 studies (39 references), 16 of which were not randomised: in four RCTs participants did not have TD (Gulmann 1976; Raptis 1990; Sikich 1999; Tamminga 1978), in two RCTs use of antipsychotics was not in stable dosages (Cassady 1992; Tamminga 1979), and two RCTs did not use a relevant intervention, i.e. a GABA agonist (Chiu 2006; Nordic 1986). We excluded other randomised trials including relevant participants and interventions because it was impossible to extract first period data from five cross‐over trials (Chien 1978; Friis 1983; Korsgaard 1976; Nasrallah 1986; Tamminga 1983), and because we could extract no data at all from one trial (Frangos 1980). We contacted the authors of five of these studies; one author confirmed the data had been destroyed (Friis 1983), one author replied but did not provide any more data (Tamminga 1983), and three authors did not reply (Frangos 1980; Korsgaard 1976; Nasrallah 1986). We could not identify up‐to‐date contact details for authors of one of the studies published over 35 years ago (Chien 1978); it was also excluded as we assumed it very unlikely to receive data so many years later.
Risk of bias in included studies
Please refer to Figure 5 for graphical overview of the risk of bias in the included studies.
Allocation
Only one study (Mei 2008) reported explicit details about how randomisation was undertaken (random number table). One set of authors kindly provided information on how randomisation was carried out (stratified, computer program co‐ordinated by hospital pharmacists) (Fisk 1987). As a result, we could judge only these two studies to be of reasonable quality within this category. The other nine studies were not explicit about how allocation was achieved other than using the word "randomized"; we classified them as unclear risk of selection of bias.
Blinding
Although all studies stated that they were conducted on a double‐blind basis, only seven studies (Ananth 1987; Burner 1989; Fisk 1987; Gerlach 1978; Linnoila 1976; Mei 2008; Yin 2004) explicitly described how this was undertaken and were rated at low risk of performance bias. Only four studies (Fisk 1987; Mei 2008; Nair 1978; Thaker 1987) explicitly described how outcome assessors were blinded and were rated at low risk of detection bias. The remaining studies were rated as unclear risk of performance and detection bias. None of the included studies tested the blindness of raters, clinicians and trial participants.
Incomplete outcome data
No study had a greater than 30% loss to follow‐up. Fisk 1987 reported in a mixed population that 24% of participants dropped‐out before the end of the intervention. Glazer 1985 did not explicitly state the number of participants enrolled and randomised. These two studies were at high risk of attrition bias.
Selective reporting
The majority of data in this review originates from published reports. Expected outcomes (impact on TD symptoms) were reported for most of the trials, however, in eight trials (Ananth 1987; Burner 1989; Fisk 1987; Glazer 1985; Linnoila 1976; Nair 1978; Stewart 1982; Thaker 1987) the data were insufficiently reported and these studies were rated at high risk of reporting bias. We have had no opportunity to see protocols of the trials to compare the outcomes reported in the full‐text publications with what was measured during the conduct of the trial, therefore, the remaining trials were at unclear risk of reporting bias.
Other potential sources of bias
Taking into account the poor description of randomisation and blinding, these studies did not fully minimise the introduction of bias so all findings should be viewed with caution. Many of the studies used small, and sometimes extremely small, sample sizes, which increases the likelihood of treatment effects going undetected. Five of the studies also used a cross‐over design (Ananth 1987; Gerlach 1978; Linnoila 1976; Nair 1978, Thaker 1987).
Effects of interventions
See: Table 1
1. Comparison: GABA drugs versus placebo
1.1 TD symptoms
We had chosen 'any improvement in tardive dyskinesia symptoms of more than 50% on any tardive dyskinesia scale ‐ any time period' as a primary outcome. Although the data we found in trials did not fit this exactly, we feel that the outcome 'not improved to a clinically important extent' fits best with what we had hoped to find.
1.1.1 Not improved to a clinically important extent
The overall results for 'clinically relevant improvement' found a small benefit in favour of GABA agonist drugs against placebo across all time points (six to eight weeks) and types of GABA agonist drugs (low‐quality evidence, 6 RCTs, n = 258, RR 0.83, CI 0.74 to 0.92, I2 = 0%, Analysis 1.1).
1.1. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 1 Tardive dyskinesia: 1. Not improved to a clinically important extent ‐ medium term.
1.1.2 Not any improvement
For the outcome of 'not any improvement in TD symptoms', again added across all time periods and types of GABA agonist drugs, we found a small difference in favour of GABA agonist drugs against placebo (8 RCTs, n = 271, RR 0.72, CI 0.60 to 0.86, I2 = 57%, Analysis 1.2).
1.2. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 2 Tardive dyskinesia: 2. Not any improvement.
1.1.3 Average endpoint/change scores
TD symptoms were also measured on different scales (see Included studies above) by five studies. We did not combine data on symptom scores, both endpoint scores and change ratings, as trials used different scales to assess TD that are not directly comparable. Two trials suggested a significant effect for the GABA drugs and three did not (see Analysis 1.3; Analysis 1.4).
1.3. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 3 Tardive dyskinesia: 3. Average endpoint scores (different scales, high score = poor, data skewed).
| Tardive dyskinesia: 3. Average endpoint scores (different scales, high score = poor, data skewed) | ||||||
|---|---|---|---|---|---|---|
| Study | Intervention | Mean | SD | N | Scale | Notes |
| Gerlach 1978 | Baclofen | 3.7 | 2.4 | 10 | Gerlach scale | |
| Gerlach 1978 | Placebo | 5.3 | 2.2 | 8 | ||
| Mei 2008 | GABA | 6.02 | 3.03 | 20 | AIMS | suggests a statistically significant effet in favour of GABA |
| Mei 2008 | Placebo | 9.35 | 4.26 | 20 | ||
| Stewart 1982 | Baclofen | 11 | 7.35 | 13 | AIMS | |
| Stewart 1982 | Placebo | 12.35 | 6.79 | 17 | ||
| Yin 2004 | Sodium valproate | 6.05 | 3.01 | 39 | AIMS | suggests a statistically significant effet in favour of sodium valproate |
| Yin 2004 | Placebo | 9.36 | 4.16 | 40 | ||
1.4. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 4 Tardive dyskinesia: 4. Average change scores (different scales, high score = poor, data skewed).
| Tardive dyskinesia: 4. Average change scores (different scales, high score = poor, data skewed) | ||||||
|---|---|---|---|---|---|---|
| Study | Intervention | Mean | SD | N | Scale | Notes |
| Burner 1989 | Progabide | 7.3 decline | 3.9 | 9 | Simpson Rating Scale | |
| Burner 1989 | Placebo | 2.6 decline | 1.5 | 3 | ||
| Stewart 1982 | Baclofen | 6.3 decline | 5.66 | 13 | AIMS | |
| Stewart 1982 | Placebo | 4.2 decline | 4.68 | 17 | ||
1.1.4 Deterioration of symptoms
There was no difference in deterioration of symptoms between GABA agonist drugs compared with placebo (very low‐quality evidence, 5 RCTs, n = 136, RR 1.90, CI 0.70 to 5.16, I2 = 0%, Analysis 1.5).
1.5. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 5 Tardive dyskinesia: 5. Deterioration of symptoms.
1.2 Adverse effects
1.2.1 Specific adverse effects
Nine of the 11 trials reported specific adverse effects that are included in the analysis (Analysis 1.6). Ananth 1987 reported that none of the 10 included people suffered adverse effects (baclofen versus placebo study). Unfortunately the reporting of adverse effects in Linnoila 1976 was ambiguous and we could not present data (sodium valproate versus placebo study). Compared with placebo, GABA agonist drugs (baclofen, progabide) resulted in increased dizziness/confusion (3 RCTs, n = 62, RR 4.54, 95% CI 1.14 to 18.11, I2 = 0%), increased sedation/drowsiness (4 RCTs, n = 144, RR 2.29, 95% CI 1.08 to 4.86, I2 = 0%), and low platelets (1 RCT, n = 79, RR 17.43 95% CI 1.04 to 291.96). For all other adverse effects (ataxia, loss of muscle tone, nausea/vomiting, restlessness/akathisia, seizures, hypotension, leucocyte decrease) there were no statistically significant differences between GABA agonist drugs and placebo.
1.6. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 6 Adverse effects.
In one trial (Thaker 1987) the presence of tonic‐clonic seizures after withdrawal of THIP led to the termination of the study (n = 2).
1.3 Mental state
Six trials reported 'deterioration in mental state' as an outcome, two of the trials reported no events. No difference was found for this outcome between GABA agonist drugs and placebo (very low‐quality evidence, 6 RCTs, n = 121, RR 2.65, CI 0.71 to 9.86, Analysis 1.7).
1.7. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 7 Mental state: 1. Deterioration.
One study reported average endpoint Brief Psychiatric Rating Scale (BPRS) score and found no significant difference between GABA agonist and placebo (1 RCT, n = 40, MD 0.03, CI ‐3.29 to 3.35; Analysis 1.8).
1.8. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 8 Mental state: 2. Average endpoint score (BPRS, high score = poor).
1.4 Leaving the study early
A greater proportion of people allocated GABA medication failed to complete the trial compared with those allocated placebo (13% versus 8%) but this difference was not statistically significant (very low‐quality evidence, 6 RCTs, n = 218, RR 1.47 CI 0.69 to 3.15, Analysis 1.9).
1.9. Analysis.
Comparison 1 GABA AGONIST DRUGS versus PLACEBO, Outcome 9 Leaving the study early.
We did not identify any studies that reported on hospital and service utilisation outcomes, economic outcomes, social confidence, social inclusion, social networks, personalised quality of life, behaviour, or cognitive state.
1.5 Subgroup analysis
1.5.1 GABA agonist compound
We stratified the primary outcome by type of GABA agonist drug. There was no significant heterogeneity between baclofen, progabide, sodium valproate and GABA (I2 = 0%, P = 0.54, Analysis 1.1). However, studies evaluating sodium valproate (2 RCTs, n = 141, RR 0.86, CI 0.76 to 0.96; I2 = 53%) and GABA (RR 0.67, CI 0.45 to 0.98; 40 participants; 1 study) found significant differences favouring GABA drug, whereas studies evaluating baclofen (2 RCTs, n = 64, RR 0.89, CI 0.70 to 1.13; I2 = 0%) and progabide (1 RCT, n = 13, RR 0.68, CI 0.36 to 1.25) found no significant differences.
1.5.2 Younger participants
It was not possible to evaluate whether those younger than 40 years old responded differently compared to older participants, since no trial reported data for different age groups that could be extracted for separate analyses.
1.5.3 Duration of treatment
It was not possible to ascertain the medium‐ or long‐term effects of these drugs since all trials reporting data on the primary outcome reported at medium term (six to eight weeks).
1.6 Heterogeneity
Data were homogeneous. We did not detect clinical, methodological or statistical heterogeneity as described in Assessment of heterogeneity.
1.7 Sensitivity analyses
1.7.1 Implication of randomisation
We aimed to include trials in a sensitivity analysis if they were described in some way as to imply randomisation. As all studies were stated to be randomised we did not undertake this sensitivity analysis.
1.7.2 Assumptions for lost binary data
The above results are based on data as presented in the original study reports, with the assumption that those who left early before the end of the trial had not improved (see Dealing with missing data). When the sensitivity of the results to this assumption was tested, we found no appreciable differences in the results. Using completer‐only data for no clinically important improvement in TD symptoms, we found that the direction of effect in favour of GABA agonist drugs did not change, though there was a minor shift in the effect estimate and the precision of the effect estimate (RR 0.81, CI 0.72 to 0.91; 239 participants; six studies, analysis not shown). If there had been a substantial difference, we would have reported results and discussed them but continued to employ our assumption.
1.7.3 Risk of bias
When excluding two trials that we judged to be at high risk of bias across one or more of the domains (Fisk 1987; Glazer 1985), there was no substantial alteration to the direction of effect or the precision of the effect estimates (4 RCTs, n = 165, RR 0.78, CI 0.67 to 0.90; analysis not shown).
1.7.4 Imputed values
We would have undertaken a sensitivity analysis to assess the effects of including data from cluster‐randomised trials where we used imputed values for intra‐class correlation coefficients (ICCs) in calculating the design effect. No cluster‐randomised trials were included.
1.7.5 Fixed and random effects
We also synthesised data for the primary outcome using a random‐effects model. This did not alter the significance of the results (6 RCTs, n = 258; RR 0.85, CI 0.77 to 0.94).
1.7.6 Study with unknown number of randomised participants
One study (Glazer 1985) had an unknown number of participants randomised, and study authors could not provide this information as data had been destroyed (communicated to review authors of a previous version of this review). For this update we nevertheless decided to include this study, but carried out sensitivity analyses examining the impact of this study. There were no substantial alterations to the direction of effects or the precision of the effect estimates when this study was excluded from analyses.
Discussion
Summary of main results
1. The search
This area of research does not seem to be active. The 2017 update has identified additional data, but most trials predate the year 2000, only two were carried out after then, published in 2004 and 2008. This could be because of reasons such as less concern with tardive dyskinesia (TD), or less emergence of the problem in research‐active communities because of more thoughtful use of antipsychotic drugs, or loss of faith in GABA agonists as a potential treatment.
2. Few data
Only a little under 350 people have been involved in placebo‐controlled trials of GABA agonists for TD. It is possible that real, and important, effects have not been highlighted because of the necessarily wide confidence intervals (CIs) of the findings. Many outcomes were not measured at all (see Overall completeness and applicability of evidence), including one of our pre‐stated outcome measures. We may have been overambitious in hoping for some of these outcomes in TD trials but simple reporting of satisfaction with care or quality of life still does not seem too demanding and does remain of interest.
3. Comparison 1: GABA agonist drugs versus placebo
3.1 TD symptoms
There was low‐quality evidence from six trials that there may be a clinically important improvement in TD symptoms after GABA agonist treatment compared with placebo at six to eight weeks follow‐up (6 RCTs, n = 258, RR 0.83, CI 0.74 to 0.92). The evidence on deterioration of TD symptoms was of very low quality (5 RCTs, n = 136, RR 1.90, CI 0.70 to 5.16).
3.2 Adverse effects
All GABA agonist drugs are associated with adverse effects and a possible deleterious (harmful to the mind or body) effect on people's mental state. Even with the very limited data in this review, there are suggestions that these adverse effects could be prohibitive of use of GABA agonist drugs. Adverse effects seem to be a major problem for these drugs when used for people with antipsychotic‐induced TD. Traditional reviews have also reported that high side‐effect rates limit the use of GABA agonists (APA 1992; Jeste 1988).
3.3 Mental state
Seven trials reported on mental state. Six reported on number of participants that experienced a deterioration in mental state, and one trial used the Brief Psychiatric Rating Scale (BPRS) scale. There was no suggestion that GABA agonists had any more effect on mental state than placebo (very low‐quality evidence, RR 2.65, CI 0.71 to 9.86; 6 RCTs, 121 people).
3.4 Leaving the study early
It is always unclear what leaving the study early means. It could be to do with the participant not accepting treatment for a series of reasons, or of participants finding the trial intolerable. It also could be a function of a trial design in which willing participants are still asked to leave because of some degree of protocol violation. In any event, around 10% of people left the study early, and this was not significantly different for those allocated to either group (6 RCTs, n = 218, RR 1.47, CI 0.69 to 3.15).
3.5 Social confidence, social inclusion, social networks, or personalised quality of life
This group of outcomes was selected as being of importance to patients for the 2016 review update following a service user consultation. No studies were identified that reported on any of these outcomes.
Overall completeness and applicability of evidence
1. Completeness
The majority of studies had a duration of less than six weeks, whilst only three actually had a duration of six weeks. Whether the effects of the drugs were maintained at longer periods of follow‐up may therefore be under‐reported in short‐term studies.
Outcome reporting was mainly symptom‐ and physician‐oriented. Patient‐oriented global and functional outcomes, such as social functioning, ability to work, patient and carer satisfaction and family burden were not reported. There is clearly a need for studies focusing not only on symptoms, but also on general and social functioning, family burden and patient acceptability.
Overall, sample sizes in relevant studies were particularly small and the completeness of evidence for those suffering from antipsychotic‐induced TD is poor.
2. Applicability
The setting of trials were a mixture of inpatient and outpatient, reflecting the situation of most people with antipsychotic‐induced TD.
Quality of the evidence
All of the trials are small and prone to multiple biases. The largest trial in this area randomised only 80 people. A trial of this size is unable to detect subtle, yet important differences due to GABA agonists with any confidence. Overall, the quality of reporting of these trials was poor (see Figure 5). Allocation concealment was not described, generation of the sequence was not explicit, studies were not clearly blinded. We are also unsure if data are incomplete or selectively reported or if other biases were operating. The small trial size, along with the poor reporting of trials, would be associated with an exaggeration of effect of the experimental treatment (Jűni 2001) if an effect had been detected. This is only evident for the outcome of ‘Tardive dyskinesia: Not improved to a clinically important extent’ where there is indeed an effect favouring the GABA agonist drug group. This interesting finding may be real – but could equally be a function of biases or of chance.
Potential biases in the review process
1. Missing studies
Every effort was made to identify relevant trials. However, these studies are all small and it is likely that we have failed to identify other studies of limited power. It is likely that such studies would also not be in favour of the GABA agonist group. If they had been so, it is more likely that they would have been published in accessible literature. We do not, however, think it likely that we have failed to identify large relevant studies.
2. Introducing bias
We have tried to be balanced in our appraisal of the evidence but could have inadvertently introduced bias. We welcome comments or criticisms. New methods and innovations now make it possible to report data where, in the past, we could not report data at all or had to report data in a different way. We think the 'Summary of findings' table to be a valuable innovation – but problematic to those not ‘blind’ to the outcome data. It is possible to ‘cherry pick’ significant findings for presentation in this table. We have tried to decrease the chance of doing this by asking a new review author (HB) to select outcomes relevant for this table before becoming familiar with the data.
Agreements and disagreements with other studies or reviews
This review substantially updates and largely concurs with findings from the previous version of this review (Alabed 2011). Previous reviews concluded that approximately 50% of those who use GABA agonists for TD show some improvement (APA 1992; Jeste 1988). These reviews probably overestimate the positive effects of these treatments. This systematic review suggests that the difference in improvement rates between those who received the GABA intervention and those who received placebo was, if present at all, around 15%.
Authors' conclusions
Implications for practice.
1. For people with antipsychotic‐induced tardive dyskinesia (TD)
Currently, evidence of any positive effect of baclofen, progabide, sodium valproate or THIP (tetrahydroisoxazolopyridinol) for people with antipsychotic‐induced TD is weak. It would seem advisable to take such medications only if the problem is intractable and in the context of a well‐designed study.
2. For clinicians
Any possible benefits are likely to be outweighed by the adverse effects associated with the use of these drugs. This category of drugs should be used as a last resort and THIP should not be used at all. The experimental use of these drugs, and their current use will always be experimental, should be in the context of a well‐designed study.
3. For funders and policy makers
It seems evident that there are better projects for funders to invest support in. These compounds should represent a policy of last resort. There are, however, many unanswered questions in this area. This unattractive adverse effect is caused, to a greater or lesser extent, by antipsychotic drugs. Clinicians and researchers should feel responsible enough to continue to try to help it. Those compiling guidance could encourage supportive activity and more research into this neglected area.
Implications for research.
1. Destruction of data
Authors have destroyed data from relevant studies conducted only nine years before being requested for the first version of this review (Ananth 1987; Friis 1983; Glazer 1985 ‐ personal communication). It would be helpful for trialists to archive their data, in perpetuity, to allow them to be used to their full value. This would help give recognition to the important, and often pioneering, work of researchers.
2. Incomplete reporting
Randomised trials in this review were poorly or incompletely reported. Assumptions about the allocation of people who left early had to be made in order to allow intention‐to‐treat (ITT) analyses. Only two studies specified how randomisation was undertaken (Fisk 1987; Mei 2008). In one trial, personal communication with the principal investigator clarified that people who left early during the intervention were excluded from final analysis (Glazer 1985), and that it was unclear exactly how many were initially randomised. Complete reporting of both methodological details and information about those who entered but did not complete the study would be helpful.
3. Study design
All included studies used the treatments for no longer than eight weeks and for small groups of people (fewer than 40 people in each group). Half the included trials used a cross‐over design. This design is not well‐suited to evaluate interventions for TD. Brief interventions make the detection of change difficult to separate out from background variations, and there is a high risk of carry‐over effects after people have received active treatment. Another problem to be considered is the use of different scales to measure the symptoms of TD. These scales have been validated to measure the severity of the TD symptoms, but their use to measure change directly related to treatment is less clear (Bergen 1984). Poor design influences the estimation of treatment effects in trials and systematic reviews (Schulz 1995). Based on the weak and unpromising evidence of positive effects and the known adverse effects of GABA agonists, we believe that the drugs in this review are not good candidates for future trials and therefore discourage further investigations into them.
What's new
| Date | Event | Description |
|---|---|---|
| 1 November 2017 | New citation required but conclusions have not changed | New data added do not substantially change previous conclusions. |
| 26 April 2017 | New search has been performed | Title updated, three new included studies added from 2015 searching (Glazer 1985; Mei 2008; Yin 2004), outcomes list updated due to patient consultation, PRISMA study flow chart added, conclusions not substantially changed. Update search run 26 April, 2017. Eight records found and assessed by editorial base Cochrane Schizophrenia, no new studies relevant to this review found. The 8 records were added to Studies awaiting classification of Miscellaneous treatments for antipsychotic‐induced tardive dyskinesia (see also Results of the search). |
History
Review first published: Issue 1, 2000
| Date | Event | Description |
|---|---|---|
| 2 March 2011 | New citation required but conclusions have not changed | Authorship change and new studies added but conclusions not changed |
| 7 August 2010 | New search has been performed | Converted to new review format. |
| 27 July 2010 | New search has been performed | Substantial update: results of 2010 search added, six studies added to Characteristics of excluded studies table. |
| 14 April 2010 | Amended | Contact details updated. |
| 5 August 2009 | Amended | Contact details updated. |
| 25 April 2008 | Amended | Converted to new review format. |
| 3 July 2004 | New citation required and conclusions have changed | Substantive amendment |
| 18 September 2003 | New search has been performed | Search strategy was run again, no new studies were found for inclusion. |
Acknowledgements
1. Original review
Without John McGrath (Brisbane, Queensland, Australia), it is difficult to know if this review would have happened. He was a review author on the first version but did not wish to continue with the other versions of this review. It is with regret that we remove his name, with affectionate and enduring gratitude.
The review authors wish to thank Professor J Ananth, Dr J Gerlach, Dr M Linnoila, and Dr C Tamminga, for replying to enquiries, and Professor W Glazer and Dr M Viukari for their replies and provision of additional information. The authors wish to thank Clive Adams for extremely helpful editorial support (and all headaches etc.), and Nicola Mayaan (nee Smith) for her substantial contribution to the the review up to 2009.
2. 2010 update
The review authors acknowledge the previous authors (Karla Soares‐Weiser, John Rathbone and Jon Deeks) for their efforts in writing the original review. We also want to thank Clive Adams for his help and support during this update and Abdullah Al Rifai for help with trial selection.
Throughout the Methods section, the generic text found in the reviews of the Cochrane Schizophrenia Group was used and modified to the needs of this review.
3. 2016 update
We wish to thank Rosie Asher and Antonio Grande for screening literature and helping with data extraction. We are also grateful to Sai Zhao for helping to assess and data extract Chinese articles, to Ben Gray for writing the Plain language summary, and to Farhad Sokraneh for carrying out the trial searches and finding papers. We also acknowledge Dawn‐Marie Walker, Ruth Sayers, Megan Lees, and Vanessa Pinfold from McPin Foundation for organising and holding the public and patient involvement consultation with TD service users that contributed to updating outcomes for the 'Summary of findings' table and to guide future research.
Appendices
Appendix 1. Previous searches, data collection and analyses
1. Electronic searches
1.1 For the update of 2010
Cochrane Schizophrenia Group Trials Register was searched in June 2010 using the phrase:[((GABA* or baclofen* or gamma‐vinyl‐GABA* or gamma‐acetylenic‐GABA* or muscimol* or progabide* or valproate* or THIP* in title) or (* GABA* or *baclofen* or *gamma‐vinyl‐GABA* or *gamma‐acetylenic‐GABA* or *muscimol* or *progabide* or *valproate* or *THIP* in title, abstract or index terms of REFERENCE)) or (GABA* or baclofen* or gamma‐vinyl‐GABA* or gamma‐acetylenic‐GABA* or muscimol* or progabide* or valproate* or THIP* in interventions of STUDY)]
This register is compiled by systematic searches of major database, hand searches and conference proceedings (see group module).
1.2 For the update of 2006
We searched the Cochrane Schizophrenia Group Trials Register (November 2005) using the phrase:[benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]This register is compiled by systematic searches of major databases, hand searches and conference proceedings (see Group Module). The previous updates were searched for relevant randomised trials by searching several electronic databases (Biological Abstracts, the Cochrane Schizophrenia Group's Register of trials, EMBASE, LILACS, MEDLINE, PsycLIT and SCISEARCH).
1.3 For previous versions of this review
1.3.1 Biological Abstracts (January 1982 to February 2002) This database was searched using the Cochrane Schizophrenia Group's phrase for randomised controlled trials (see Group search strategy) combined with the phrase:[and (tardive near (dyskine* or diskine*) or (abnormal near movement* near disorder*) or (involuntar* near movement*)] and [benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]
1.3.2 Cochrane Schizophrenia Group's Register (February 2002) This was searched using the phrase:[benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]
1.3.3 EMBASE (January 1980 to February 2002) This was searched using the Cochrane Schizophrenia Group's phrase for randomised controlled trials (see Group search strategy) combined with the phrase:[and (tardive dyskinesia in thesaurus ‐subheadings, prevention, drug therapy, side effect and therapy) or (neuroleptic dyskinesia in thesaurus ‐all subheadings) or (tardive and dyskines*) or (movement* and disorder*) or (abnormal and movement* and disorder*)] and [benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]
1.3.4 LILACS (January 1982 to February 2002) This was searched using the Cochrane Schizophrenia Group's phrase for randomised controlled trials (see Group search strategy) combined with the phrase:[and (tardive and (dyskinesia* or diskinesia*)) or (drug induced movement disorders in thesaurus)] and [benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]
1.3.5 MEDLINE (January 1966 to February 2002) This was searched using the Cochrane Schizophrenia Group's phrase for randomised controlled trials (see Group search strategy) combined with the phrase:[and (movement‐disorders in MeSH / explode all subheadings) or (anti‐dyskinesia‐agents in MeSH / explode all subheadings) or (dyskinesia‐drug‐induced in MeSH / explode all subheadings) and (psychosis in MeSH / explode all subheadings) or (schizophrenic disorders in MeSH / explode all subheadings) or (tardive near (dyskine* or diskine*)) or (abnormal* near movement* near disorder*) or (involuntar* near movement*)] and [benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]
1.3.6 PsycLIT (January 1974 to February 2002) This was searched using the Cochrane Schizophrenia Group's phrase for randomised controlled trials (see Group search strategy) combined with the phrase:[and (explode movement‐disorders in DE) or (explode tardive‐dyskinesia in DE) or (tardive near (dyskine* or diskine*) or (abnormal* near movement* near disorder*) or (involuntar* near movement*)] and [benzodiazep* or alprazolam or bromazepam or chlordiazepoxide or clobazam or clonazepam or clorazepate dipotassium or diazepam or flunitrazepam or flurazepam or loprazolam or lorazepam or lormetazepam or medazepam or midazolam or nitrazepam or oxazepam or temazepam]
1.3.7 SCISEARCH ‐ Science Citation Index Each of the included studies was sought as a citation on the SCISEARCH database. Reports of articles that had cited these studies were inspected in order to identify furth
Selection of studies
For the previous update (July 2004), NS (see Acknowledgements) inspected all abstracts of studies identified as above and identified potentially relevant reports. In addition, to ensure reliability, KSW inspected a random sample of these abstracts, comprising 10% of the total. Where disagreement occurred we resolved this by discussion, or where there was still doubt, acquired the full article for further inspection. We acquired the full articles of relevant reports for reassessment and carefully inspected them for a final decision on inclusion (see Criteria for considering studies for this review). Once we obtained the full articles, NS and KSW in turn inspected all full reports and independently decided whether they met inclusion criteria. NS and KSW were not blinded to the names of the authors, institutions or journal of publication. Where difficulties or disputes arose, we asked author JM for help and if it was impossible to decide, added these studies to those awaiting assessment and contacted the authors of the papers for clarification. For the current update (July 2010) AS and RA independently inspected each report identified by the search to identify relevant studies.
Data extraction and management
1. Extraction
For the update (July 2004), NS extracted data from all included studies. In addition, to ensure reliability, KSW independently extracted data from a random sample of these studies, comprising 10% of the total. Again, we discussed any disagreement, documented decisions and, if necessary, contacted authors of studies for clarification. With remaining problems JM helped clarify issues, and we documented those final decisions. We extracted data presented only in graphs and figures whenever possible, but included these only if two authors independently had the same result. We attempted to contact authors through an open‐ended request in order to obtain missing information or for clarification whenever necessary. Where possible, we extracted data relevant to each component centre of multi‐centre studies separately. For the update (July 2010) AS and RA (see Acknowledgements) independently inspected each report identified by the search, and discussed any doubts with LY and MH.
2. Management
2.1 Forms
We extracted data onto standard, simple forms.
2.2 Scale‐derived data
We included continuous data from rating scales only if: a. the psychometric properties of the measuring instrument had been described in a peer‐reviewed journal (Marshall 2000); b. the measuring instrument was not written or modified by one of the trialists for that particular trial; and c. the measuring instrument is either i. a self‐report or ii. completed by an independent rater or relative (not the therapist).
2.3 Endpoint versus change data
There are advantages of both endpoint and change data. Change data can remove a component of between‐person variability from the analysis. On the other hand, calculation of change needs two assessments (baseline and endpoint) which can be difficult in unstable and difficult to measure conditions such as schizophrenia. We decided to primarily use endpoint data and only use change data if the former were not available. We combined endpoint and change data in the analysis as we used mean differences rather than standardised mean differences throughout (Higgins 2008, Chapter 9.4.5.2).
2.4 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we aim to apply the following standards to all data before inclusion. a) Standard deviations and means are reported in the paper or obtainable from the authors. b) When a scale starts from the finite number zero, the standard deviation, when multiplied by two, is less than the mean (as otherwise the mean is unlikely to be an appropriate measure of the centre of the distribution (Altman 1996). c) If a scale started from a positive value (such as the Positive and Negative Syndrome Scale (PANSS), which can have values from 30 to 210), we modified the calculation described above to take the scale starting point into account. In these cases skew is present if 2SD>(S‐S min), where S is the mean score and S min is the minimum score. Endpoint scores on scales often have a finite start and end point and these rules can be applied. When continuous data are presented on a scale that includes a possibility of negative values (such as change data), it is difficult to tell whether data are skewed or not. We entered skewed data from studies of less than 200 participants in additional tables rather than into an analysis. Skewed data pose less of a problem when looking at means if the sample size is large and were entered into syntheses.
2.5 Common measure
To facilitate comparison between trials, we intended to convert variables that can be reported in different metrics, such as days in hospital (mean days per year, per week or per month) to a common metric (e.g. mean days per month).
2.6 Conversion of continuous to binary
Where possible, we made efforts to convert outcome measures to dichotomous data. This could be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. We generally assumed that if there had been a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the Positive and Negative Syndrome Scale (PANSS, Kay 1986), we could consider this as a clinically significant response (Leucht 2005a; Leucht 2005). If data based on these thresholds were not available, we used the primary cut‐off presented by the original authors.
2.7 Direction of graphs
Where possible, we entered data in such a way that the area to the left of the line of no effect indicates a favourable outcome for intensive case management.
2.8 Studies with multiple treatment groups
Where a study involved more than two treatment arms, if relevant, we presented the additional treatment arms in comparisons. Where the additional treatment arms were not relevant, we did not reproduce these data.
2.9 'Summary of findings' table
We anticipated including the following short‐ or medium‐term outcomes in a 'Summary of findings' table. (NS was not biased by being familiar with the data.)
1. Tardive dyskinesia
1.1 Not improved to an important extent 1.2 Not improved 1.3 Deteriorated
2. Adverse effect
2.1 Any adverse event 2.2 Specific adverse event
3. Quality of life
3.1 Not improved to an important extent
Assessment of risk of bias in included studies
We assessed the risk of bias using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) to assess trial quality. This set of criteria is based on evidence of associations between overestimate of effect and high risk of bias of the article such as sequence generation, allocation concealment, blinding, incomplete outcome data and selective reporting.
The categories are defined below.
‐ Yes ‐ low risk of bias ‐ NO ‐ high risk of bias ‐ UNCLEAR ‐ uncertain risk of bias
For example, if the sequence generation process within the trial was by quasi‐random means, such as by hospital record numbers, we noted this and gave the study a "No ‐ high risk of bias" rating. If data from such studies did not differ from the results of higher grade trials, we have presented these. We have not included trials with high risk of bias (defined as at least three out of five domains categorized as 'No') in the meta‐analysis. If the raters disagreed, we made the final rating by consensus with the involvement of another member of the review group. Where inadequate details of randomisation and other characteristics of trials are provided, we contacted authors of the studies in order to obtain further information. We have reported non‐concurrence in quality assessment, but if disputes arose as to which category a trial had to be allocated, again, we achieved resolution by discussion.
Measures of treatment effect
1. Binary data
For binary outcomes we calculated a standard estimation of the risk ratio (RR) and its 95% confidence interval (CI). It has been shown that RR is more intuitive (Boissel 1999) than odds ratios and that odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). For statistically significant results we had planned to calculate the number needed to treat to provide benefit/to induce harm statistic (NNTB/H), and its 95% confidence interval (CI) using Visual Rx (http://www.nntonline.net/) taking account of the event rate in the control group. This, however, was superseded by 'Summary of findings' table 1 and the calculations therein.
2. Continuous data
2.1 Summary statistic
For continuous outcomes we estimated mean difference (MD) between groups. We preferred not to calculate effect size measures (standardised mean difference SMD). However, had scales of very considerable similarity been used, we would have presumed there was a small difference in measurement, and we would have calculated effect size and transformed the effect back to the units of one or more of the specific instruments.
Unit of analysis issues
1. Cluster trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intra‐class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby P values are spuriously low, confidence intervals unduly narrow and statistical significance overestimated. This causes type I errors (Bland 1997; Gulliford 1999).
Where clustering is not accounted for in primary studies, we presented data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intra‐class correlation coefficients (ICC) for their clustered data and to adjust for this by using accepted methods (Gulliford 1999). Where clustering had been incorporated into the analysis of primary studies, we present these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the ICC (Design effect=1+(m‐1)*ICC) (Donner 2002). If the ICC was not reported we assumed it to be 0.1 (Ukoumunne 1999).
If cluster studies has been appropriately analysed taking into account ICC and relevant data documented in the report, synthesis with other studies would have been possible using the generic inverse variance technique.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state despite a wash‐out phase. For the same reason, cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in severe mental illness, we only use data of the first phase of cross‐over studies.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss of follow‐up data must lose credibility (Xia 2007). For any particular outcome, should more than 50% of data be unaccounted for, we did not reproduce these data or use them within analyses. If, however, more than 50% of those in one arm of a study were lost, but the total loss was less than 50%, we marked such data with (*) to indicate that such a result may well be prone to bias.
2. Binary
In the case where attrition for a binary outcome is between 0 and 50% and where these data were not clearly described, we have presented data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat (ITT) analysis). Those leaving the study early were all assumed to have the same rates of negative outcome as those who completed, with the exception of the outcome of death. We undertook a sensitivity analysis testing how prone the primary outcomes were to change when 'completed' data only were compared to the ITT analysis using the above assumption.
3. Continuous
3.1 Attrition
In the case where attrition for a continuous outcome is between 0 and 50% and completer‐only data were reported, we have reproduced these.
3.2 Standard deviations
We first tried to obtain the missing values from the authors. If not available, where there were missing measures of variance for continuous data but an exact standard error and confidence interval (CI) were available for group means, and either 'P' value or 'T' value were available for differences in mean, we calculated them according to the rules described in the Cochrane Handbook (Higgins 2008). When only the standard error (SE) is reported, standard deviations (SDs) are calculated by the formula SD=SE * square root (n). Chapters 7.7.3 and 16.1.3 of the Cochrane Handbook (Higgins 2008) present detailed formula for estimating SDs from P values, T or F values, CIs, ranges or other statistics. If these formula do not apply, we calculated the SDs according to a validated imputation method which is based on the SDs of the other included studies (Furukawa 2006). Although some of these imputation strategies can introduce error, the alternative would be to exclude a given study’s outcome and thus to lose information. We nevertheless examined the validity of the imputations in a sensitivity analysis excluding imputed values.
3.3 Last observation carried forward
We anticipated that in some studies the method of last observation carried forward (LOCF) would be employed within the study report. As with all methods of imputation to deal with missing data, LOCF introduces uncertainty about the reliability of the results. Therefore, where LOCF data have been used in the trial, if less than 50% of the data had been assumed, we reproduced these data and indicated that they are the product of LOCF assumptions.
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all included studies initially, without seeing comparison data, to judge clinical heterogeneity. We simply inspected all studies for clearly outlying situations or people which we had not predicted would arise. When such situations or participant groups arose, we discussed these fully.
2. Methodological heterogeneity
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We simply inspected all studies for clearly outlying methods which we had not predicted would arise. When such methodological outliers arose, we fully discussed these.
3. Statistical heterogeneity
3.1 Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
3.2 Employing the I2 statistic
We investigated heterogeneity between studies by considering the I2 method alongside the Chi2 P value. The I2 provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2003). The importance of the observed value of I2 depends on i. magnitude and direction of effects and ii. strength of evidence for heterogeneity (e.g. P value from Chi2 test, or a CI for I2). We interpreted I2 estimate greater than or equal to 50% accompanied by a statistically significant Chi2 statistic as evidence of substantial levels of heterogeneity (Section 9.5.2 ‐ Higgins 2008). When we found substantial levels of heterogeneity in the primary outcome, we explored reasons for heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in Section 10 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). We tried to locate protocols of included trials. If the protocol was available, we compared outcomes in the protocol and in the published report. If the protocol was not available, we compared outcomes listed in the methods section of the trial report with actually reported results. In addition a funnel plot (included trial effect size versus included trial size) may be useful in investigating publication biases but are of limited power to detect small‐study effects. We did not use funnel plots for outcomes where there were 10 or fewer studies, or where all studies were of similar sizes. In other cases, where funnel plots were possible, we sought statistical advice in their interpretation.
Data synthesis
We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us and the random‐effects model takes into account differences between studies even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model. It puts added weight onto small studies which often are the most biased ones. Depending on the direction of effect these studies can either inflate or deflate the effect size. Therefore, we chose the fixed‐effect model for all analyses. The reader is, however, able to choose to inspect the data using the random model.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analyses
We anticipated one subgroup analyses to test the hypothesis that the use of GABA agonist drugs are most effective for a younger age group (less than 40 years old). We had hoped to present data for this subgroup for the primary outcomes.
2. Investigation of heterogeneity
If inconsistency was high, we reported this. First, we investigated whether data had been entered correctly. Second, if data had been correct, we visually inspected the graph and successively removed studies outside of the company of the rest to see if heterogeneity was restored. Should this occur with no more than 10% of the data being excluded, we presented data. If not, we did not pool data and discussed issues.
Should unanticipated clinical or methodological heterogeneity be obvious, we simply stated hypotheses regarding these for future reviews or versions of this review. We did not anticipate undertaking analyses relating to these.
Sensitivity analysis
1. Implication of randomisation
We aimed to include trials in a sensitivity analysis if they were described in some way as to imply randomisation. For the primary outcomes we included these studies and if there was no substantive difference when the implied randomised studies were added to those with better description of randomisation, then we employed all data from these studies.
2. Assumptions for lost binary data
Where we had to make assumptions regarding people lost to follow‐up (see Dealing with missing data), we compared the findings of the primary outcomes when we used our assumption compared with completer data only. If there was a substantial difference, we reported results and discuss them but continue to employ our assumption.
Where assumptions had to be made regarding missing SDs data (see Dealing with missing data), we compared the findings on primary outcomes when we used our assumption compared with complete data only. A sensitivity analysis was undertaken testing how prone results were to change when 'complete' data only were compared to the imputed data using the above assumption. If there was a substantial difference, we reported results and discuss them but continue to employ our assumption.
Data and analyses
Comparison 1. GABA AGONIST DRUGS versus PLACEBO.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Tardive dyskinesia: 1. Not improved to a clinically important extent ‐ medium term | 6 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.74, 0.92] |
| 1.1 baclofen | 2 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.70, 1.13] |
| 1.2 progabide | 1 | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.36, 1.25] |
| 1.3 sodium valproate | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.76, 0.96] |
| 1.4 gamma‐aminobutyric acid | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.45, 0.98] |
| 2 Tardive dyskinesia: 2. Not any improvement | 8 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.60, 0.86] |
| 2.1 baclofen ‐ short term | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.22, 4.56] |
| 2.2 baclofen ‐ medium term | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.27, 3.84] |
| 2.3 progabide ‐ medium term | 1 | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.05, 21.67] |
| 2.4 sodium valproate ‐ short term | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.32, 0.83] |
| 2.5 sodium valproate ‐ medium term | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.71, 1.01] |
| 2.6 THIP ‐ short term | 1 | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.03, 4.19] |
| 2.7 gamma‐aminobutyric acid ‐ medium term | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.16, 0.80] |
| 3 Tardive dyskinesia: 3. Average endpoint scores (different scales, high score = poor, data skewed) | Other data | No numeric data | ||
| 4 Tardive dyskinesia: 4. Average change scores (different scales, high score = poor, data skewed) | Other data | No numeric data | ||
| 5 Tardive dyskinesia: 5. Deterioration of symptoms | 5 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [0.70, 5.16] |
| 5.1 baclofen ‐ short term | 2 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.11, 53.25] |
| 5.2 baclofen ‐ medium term | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.13, 4.30] |
| 5.3 sodium valproate ‐ medium term | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.41 [0.77, 15.19] |
| 6 Adverse effects | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 ataxia (baclofen, sodium valproate) | 2 | 95 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.36, 29.73] |
| 6.2 dizzy/confused (baclofen, progabide) | 3 | 62 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.54 [1.14, 18.11] |
| 6.3 loss of muscle tone (baclofen) | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.15, 59.89] |
| 6.4 nausea/vomiting (baclofen) | 2 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [0.79, 8.67] |
| 6.5 restlessness/akathisia (baclofen, sodium valproate) | 2 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.32, 3.49] |
| 6.6 sedation/drowsiness (baclofen, sodium valporate) | 4 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [1.08, 4.86] |
| 6.7 seizures (THIP) | 1 | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.24, 37.67] |
| 6.8 Hypothension (Gamma‐ Aminobutyric acid, Sodium Valproate) | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.04 [0.33, 28.31] |
| 6.9 Diarrhoea (Gamma‐ Aminobutyric acid) | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.52] |
| 6.10 Leucocyte decrease (sodium valporate) | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.13, 73.27] |
| 6.11 Low platelet (sodium valporate) | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.43 [1.04, 291.96] |
| 6.12 any ‐ baclofen | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Mental state: 1. Deterioration | 6 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.65 [0.71, 9.86] |
| 7.1 baclofen ‐ short term | 2 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.09 [0.22, 74.78] |
| 7.2 baclofen ‐ medium term | 1 | 31 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 progabide ‐ medium term | 1 | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [0.11, 30.27] |
| 7.4 sodium valproate ‐ medium term | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.27 [0.22, 23.38] |
| 7.5 THIP ‐ short term | 1 | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.24, 37.67] |
| 8 Mental state: 2. Average endpoint score (BPRS, high score = poor) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Gamma‐Aminobutyric acid ‐ medium term | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐3.29, 3.35] |
| 9 Leaving the study early | 6 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.69, 3.15] |
| 9.1 baclofen | 3 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.07, 2.24] |
| 9.2 progabide | 1 | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.05, 21.67] |
| 9.3 sodium valproate | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.48 [0.93, 6.61] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ananth 1987.
| Methods | Allocation: randomised, not described.
Blindness: double, "The medication was supplied in identical capsules containing 10 mg of the active drug baclofen or an inert substance, placebo."
Design: cross‐over (each preceded by 1 week washout).
Setting: Veterans Hospital, St Anne de Bellevue, Quebec, Canada. Duration: 4 weeks, each treatment period. |
|
| Participants | Diagnosis: schizophrenia (no criteria). TD on the basis of the chart diagnoses, clinical interviews, and structured neurological examinations performed independently by three psychiatrists; buccolingual as well as facial movements, in addition to involuntary movements in other parts of the body.
Duration of TD: not reported. N = 10. Sex: 10 male. Age: mean 39 years, range 30‐58 years |
|
| Interventions | 1. Baclofen: dose day 1 20 mg/d; dose day 2, 30 mg/d; dose day 3 onwards 40 mg/d for 4 weeks. N = 5 2. Placebo. N = 5. Stable dose of antipsychotic medication: an exclusion criteria was change in the antipsychotic dosage within two months prior to inclusion. All patients were on antiparkinsonian (trihexyphenidyl or benzotropine) agents at the time of entry in to the study. |
|
| Outcomes | TD symptoms: AIMS, deterioration of symptoms.
Adverse effects. Leaving the study early. Mental state: BPRS. |
|
| Notes | Sponsorship source: Sponsorship source not reported No information about compliance. Authors contacted. Data destroyed ‐ no more information available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "patients were randomly assigned", further details not reported. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The medication was supplied in identical capsules containing 10 mg of the active drug baclofen or an inert substance, placebo." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | TD symptoms and mental state: Blinding details of outcome assessors not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants seem to have completed the trial. Results for all 10 participants (in the two periods of the cross‐over trial) have been reported. |
| Selective reporting (reporting bias) | High risk | AIMS, BPRS scores have not been reported as mean (SD) but as total scores. |
| Other bias | Unclear risk | Insufficient information to make a judgement. Very small sample size. |
Burner 1989.
| Methods | Allocation: randomly allocated, not described.
Blindness: double, described, adequate Design: parallel group Setting: not reported Duration: 6 weeks (preceded by 1 week washout). |
|
| Participants | Diagnosis: schizophrenia (ICD‐9), manic depressive illness (ICD‐9) and antipsychotic induced TD. Duration of TD: 2‐13 years. N = 13. Sex: 7 male and 5 female, 1 not specified. Age: mean 56 years. |
|
| Interventions | 1. Progabide: dose 20 mg, 30 mg or 45 mg/kg/day for 6 weeks. N = 10. 2. Placebo. N = 3. Stable but unspecified dose of antipsychotic drugs; benzodiazepines not permitted. |
|
| Outcomes | TD symptoms: SRS. Adverse effects. Leaving study early. Mental state: BPRS. | |
| Notes | Sponsorship source: Sponsorship source not reported. However, all but the first author are affiliated with Synthelabo‐Recherche. Duration of TD longer in placebo group. 1 person left progabide group early (day 19) ‐ confusional state & depressive symptoms. Person with manic‐depressive illness (1) not possible to separate from final analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ...."patients were randomly enrolled", further details not reported. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | ....."double‐blind" "They received progabide (20, 30, or 45 mg/kg/day) or placebo as identical capsules for 6 weeks." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “Response to treatment was assessed on a weekly basis by the investigator”, no further details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One patient dropped out of the progabide group (45 mg/kg/day) on day 19 because of a confusional state and depressive symptoms. This patient was the only one who suffered from manic‐depressive psychosis. The other 12 patients completed the study." Dropout rate: 8%. 1/10 in the progabide and 0/3 in the placebo group. Reason reported. |
| Selective reporting (reporting bias) | High risk | "Response to treatment was assessed on a weekly basis by the investigator using the Simpson Rating Scale and the therapeutic effect item from the Clinical Global Impression Scale" Data for CGI not reported. Also, SRS and BPRS data not reported as mean (SD). |
| Other bias | Unclear risk | Very small sample size. The duration of dyskinesia was longer in the placebo group (mean 92 vs. 49.4 months). |
Fisk 1987.
| Methods | Allocation: randomised, described.
Blindness: double, described. Design: parallel group Duration: 6 weeks baseline, followed by 6 weeks treatment. Setting: Inpatients and outpatients from three mental hospitals, UK. Compliance: assessed by records or tablet returns. |
|
| Participants | Diagnosis: schizophrenia, manic‐depressive illness and recurrent depression (no criteria) and antipsychotic induced TD, defined by a score of two or more on the central portion of the BRS.
Duration of TD: at least 6 months. N = 62. Sex: 42 males and 20 females. Age: mean age 58.1(SD 8.83) years. |
|
| Interventions | 1. Sodium valproate: dose increasing over 6 days to 1500 mg/day for 12 weeks. People < 50 kg received 1200 mg/day. N = 33. 2. Placebo. N = 29. Stable dose of antipsychotic medication: dose (CPE) < 300 mg/day (SV = 12; Pl = 9); 300 mg to 900 mg/day (SV = 17; Pl = 12); > 900 mg/day (SV = 4; Pl = 8). Benzodiazapines and anticholinergic medication permitted. |
|
| Outcomes | TD symptoms: BRS, SRS. Adverse effects. Leaving study early. Mental state: Krawiecka Scale. | |
| Notes | Sponsorship source: Sanofi‐Labaz (UK) Not possible to separate people with manic‐depressive psychosis or recurrent depression from the analysis. 15 people left early (11 on SV group and 4 on Pl); reasons ‐ protocol violation, poor compliance, ill‐health, pneumonia, unstable medication. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Trial entrants were randomised between SV and placebo treatment groups, with stratification for age, sex, hospital, in‐patient or community‐based status, and high or low pretrial TD, using a computer program" |
| Allocation concealment (selection bias) | Low risk | "Hospital pharmacists acted as coordinators of treatment dispensation with emergency access to treatment allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Double‐blind procedures were used throughout. Medication was pre packed and labelled with the patient's name." "Hospital pharmacists acted as coordinators of treatment dispensation..." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As treatment was assigned by the central pharmacist and medications were prepackaged, it seems that everybody including the outcome assessors (except the pharmacist) were blind to treatment group. Moreover: "In addition to a 'live' TD rate each patient was videotaped simultaneously, ... Thus, each patient was videotaped in a standard environment and was given a standard task. The videotapes were used to provide two further blind TD ratings by experienced independent raters. " |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not possible to separate people with manic‐depressive psychosis or recurrent depression from the analysis. 15 people left early (11 in sodium valproate group and 4 on placebo); reasons ‐ protocol violation, poor compliance, ill, pneumonia, unstable medication. Details not reported per intervention group. |
| Selective reporting (reporting bias) | High risk | TD outcomes not reported as mean (SD); fig 1 report only means. For TD symptoms and mental state, only, improvement and deterioration data reported. Adverse effects fully reported, leaving the study early: reasons not reported per intervention group. |
| Other bias | Unclear risk | Small sample size; similar baseline characteristics: “A check on randomisation showed no significant difference between SV and placebo treatment groups for age, sex, in‐patient vs community‐patient status, diagnosis, duration of antipsychotic treatment, maintenance medication level and type of medication.” |
Gerlach 1978.
| Methods | Allocation: randomised ‐ no further information.
Blindness: double, not described.
Design: two period cross‐over (no washout).
Duration: 3 weeks in each period. Setting: inpatients, Denmark. |
|
| Participants | Diagnosis: schizophrenia, manic‐depressive illness, dementia and chronic alcoholism (no criteria) and antipsychotic induced TD. Duration of TD: not reported. N = 20. Sex: 15 males and 3 females, 2 not specified. Age: median 66 years, range 47‐ 79 years. |
|
| Interventions | 1. Baclofen: dose increasing over 2 weeks to 120 mg/day max; range 20 mg to 120 mg/day. N = 10. 2. Placebo. N = 8. Stable but unspecified dose of antipsychotic medication. Anticholinergics and benzodiazepines allowed. |
|
| Outcomes | TD symptoms: GRS. Adverse effects. Leaving study early. Behaviour: NOSIE. | |
| Notes | Source of support: Baclofen and placebo tablets were supplied by Ciba‐Geigy Ltd. 2 people left study early (refusal to continue medication); unclear about the treatment status of these people. Not possible to separate people with manic‐depressive, dementia or chronic alcoholism from the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Random allocation", no further details. |
| Allocation concealment (selection bias) | Unclear risk | No further details. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Double" "Baclofen, 10 mg, and placebo were administered in tablets of identical appearance" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "The patients were evaluated by means of live and video‐taped interviews, first before the study, then weekly during the two treatment phases" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Two people left study early (refusal to continue medication); unclear about the treatment status of these people. Not possible to separate people with manic‐depressive, dementia or chronic alcoholism from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Unclear if all outcomes have been reported. |
| Other bias | Unclear risk | The groups seem to have been similar in their baseline characteristics (except for diagnosis). Very small sample size; cross‐over design. |
Glazer 1985.
| Methods | Allocation: randomised. Blindness: double. Design: parallel. Duration: 6 weeks. Setting: TD Clinic at the Connecticut Mental Health Center, Yale University School of Medicine. |
|
| Participants | Diagnosis: schizophrenia (25), schizoaffective disorder (4), other; unspecified (2). antipsychotic medication for at least 6 months; TD (AIMS) for at least 6 months prior to the study. Duration of TD: around 2 years. N = 31. Sex: 16 male and 15 female. Age: baclofen, 46.5 (SD 12.2) years; range 27‐65 years. Placebo, 47.1 (SD14.1) years; range 26‐67 years. |
|
| Interventions | 1. Baclofen: maximum dose 90 mg/d for 6 weeks. N = 16 (completers).* 2. Placebo: 6 weeks. N = 15 (completers).* Doses of antipsychotic medications stable for at least 4 weeks prior to randomisation. During the study, patients were maintained on the dose of antipsychotic medication that they were on upon entry into the study. Concomitant medication: not reported. |
|
| Outcomes | TD symptoms: AIMS. Mental state. Adverse effects. |
|
| Notes | Sponsorship source: Supported in part by NIMH and CIBA‐GEIGY Corporation. "Patients were dropped from the study if poor compliance was suspected." *No information about numbers initially randomised (only those completing were analysed); authors contacted and confirmed that those who left early were not included in analyses. No additional data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" Details not reported |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "double‐blind" Details not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | TD symptoms and mental state: "double‐blind". Details not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number of participants enrolled and randomised to each group not reported. Only participants who completed were reported and analysed. |
| Selective reporting (reporting bias) | High risk | TD symptoms (total AIMS scores) reported as means only. |
| Other bias | Low risk | Mean duration of TD, antipsychotic use (dose), mean duration of psychiatric diagnoses, and psychiatric diagnoses reported for both groups are similar. The study seems to be free of other sources of bias. |
Linnoila 1976.
| Methods | Allocation: randomised, using 2 X 2 Latin square.
Blindness: double.
Design: two period cross‐over (no washout).
Duration: 1 week each period. Setting: Psychogeriatric unit of Koskela Geriatric Hospital, Helsinki, Finland. |
|
| Participants | Diagnosis: schizophrenia (DSM‐III), dementia and other psychosis and antipsychotic‐induced TD. Duration of TD: at least one year prior to the study. N = 32. Sex: 8 males and 23 females, 1 not specified. Age: hospital 1: mean 78 (SD 6) years; hospital 2: mean 62 (SD 13) years. |
|
| Interventions | 1. Sodium valproate: dose fixed 900 mg/day. N = 16. 2. Placebo. N = 16. Stable but unspecified dose of antipsychotic medication. Concomitant medication: not reported. |
|
| Outcomes | TD symptoms. Leaving study early. Mental state: BPRS. | |
| Notes | Sponsorship source: Sponsorship source not reported Rated orofacial dyskinesia: range 0 (no dyskinesia) ‐ 3 (severe). 1 person left early (valproate). Not possible to separate people with dementia or other psychosis from the analysis. Authors contacted and provided more information about randomisation procedure. No other data available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were allocated to the treatments using a 2 X 2 Latin square design." |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The design of the experiment was double blind, cross‐over, and without a wash‐out period. The placebo used was lactose in tablets identical with the active drug." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Double‐blind. Details of outcome assessor blinding not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One patient in the geriatric group was not willing to continue sodium valproate after a two‐day administration." 3%(1/32) dropout. Group and reason reported. Cross‐over period not reported. |
| Selective reporting (reporting bias) | High risk | TD symptom outcomes (Primary outcome) have not been reported as mean (SD). Adverse effects not reported. |
| Other bias | Unclear risk | Small sample size; cross‐over design. |
Mei 2008.
| Methods | Allocation: "random number table"
Blinding: "double‐blind" "The interventions were coded as intervention I or II by the researcher. Participants and personnel did not know the allocation result." "The two drugs were contained in capsules with same appearance" "The outcome assessor did not know the group assignment"
Duration: 8 weeks Setting: "inpatients", China |
|
| Participants | Diagnosis: Patients with schizophrenia (CCMD‐3) and antipsychotics‐induced TD (Schooler 1982). Duration of TD: mean 3.6 (2.3) years. N = 40 Sex: not reported. Age:mean 43 (SD 7) years old. |
|
| Interventions | 1. Gamma‐aminobutyric acid: two capsules each time, three times per day for 8 weeks. N = 20 2. Placebo Group: two capsules each time, three times per day for 8 weeks. N = 20 All participants received stable doses of antipsychotics. Other concomitant medication was not reported. |
|
| Outcomes | TD symptoms: clinical response, AIMS. Mental state: BPRS. Adverse events: orthostatic hypotension, diarrhoea. | |
| Notes | Funding source: not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ”random number table” |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "double blind" “The interventions were coded as intervention I or II by the researcher. Participants and personnel did not know the allocation result.” “The two drugs were contained in capsules with same appearance” Blinding of participants and key study personnel ensured. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The outcome assessor did not know the group assignment.“ Blinding of outcome assessor ensured. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the study. |
| Selective reporting (reporting bias) | Unclear risk | Unclear if all outcomes have been reported. |
| Other bias | Low risk | None obvious. |
Nair 1978.
| Methods | Allocation: randomised ‐ no further information.
Blindness: double, no details.
Design: cross‐over.
Duration: 8 weeks (3 weeks followed by 2 weeks placebo and then crossed over to another 3 weeks). Setting: Norristown State Hospital, USA. |
|
| Participants | Diagnosis: schizophrenia (no criteria) and antipsychotic induced TD.
Duration of TD: not reported. N = 10. Sex: 5 males, 5 females. Age: average 56 years, range 40‐64. |
|
| Interventions | 1. Baclofen: dose increasing gradually to 90 mg/day. N = 5. 2. Placebo. N = 5. Antipsychotic medication free for > 3 months, other concomitant mediation was not reported. |
|
| Outcomes | TD symptoms: AIMS (unable to use ‐ not reported for phase before crossing over separately). Adverse effects. | |
| Notes | Data about improvement and compliance not possible to extract. Authors contacted but have not replied. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Random allocation", no further details. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "double blind" no details reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Interviews using the Abnormal Involuntary Movement Scale (AIMS) were videotaped to assess response. Coded tapes were rated under blind conditions.” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition data not reported. |
| Selective reporting (reporting bias) | High risk | Data about improvement not possible to extract. |
| Other bias | Unclear risk | Very small sample size; cross‐over design. |
Stewart 1982.
| Methods | Allocation: randomised ‐ sequential assignment determined by prepackaged medication bottles.
Blindness: double, no details
Design: parallel group.
Duration: 6 weeks (no washout). Setting: not reported. |
|
| Participants | Diagnosis: schizophrenia, major depressive disorder and neurosis (no criteria) and antipsychotic induced TD. Duration of TD: not reported. N = 36. Sex: 25 males and 11 female. Age: mean 52 years. |
|
| Interventions | 1. Baclofen: dose increasing over 4 weeks to 90 mg/day unless efficacy observed. N = 14. 2. Placebo. N = 19. Stable but unspecified dose of antipsychotic medication. Concomitant medication: not reported. |
|
| Outcomes | TD symptoms: AIMS. Mental state: BPRS. General improvement: CGI. Adverse effects. Leaving study early. | |
| Notes | Not possible to separate people with major depressive disorder or neurosis from analysis. 3 (1 baclofen) people left study early due to poor compliance, protocol violation, adverse reactions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Random allocation", sequential assignment determined by prepackaged medication bottles. |
| Allocation concealment (selection bias) | Unclear risk | No details. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "double blind" No further details |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "double blind" No further details |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 (1 baclofen) people left study early due to poor compliance, protocol violation, adverse reactions. No further details were given about these patients. |
| Selective reporting (reporting bias) | High risk | BPRS results not reported. |
| Other bias | Unclear risk | Small sample size; the base‐line characteristics of the 33 patients who entered the double‐blind study were similar in both treatment groups. |
Thaker 1987.
| Methods | Allocation: randomised ‐ no further information. Blindness: double. Duration: 3 weeks each period. Design: two period cross‐over (preceded by 1‐2 weeks washout). Setting: Inpatients at psychiatric facility, USA | |
| Participants | Diagnosis: schizophrenia (DSM‐III) and antipsychotic induced TD, stable dyskinesia ratings (< 20% variation).
Duration of TD: not reported. N = 9. Sex: 5 male and 4 female. Age: range 22‐36. |
|
| Interventions | First study 1. Gamma‐vinyl gamma aminobutyric acid (GVG): dose titrated over 5 days: from 250 mg/d to a maximum dose of 3000 mg/d for three weeks. N = 7. 2. Placebo. N = 7. Free of antipsychotic medication for > 5 weeks. Concomitant medication not reported. Second study 1. THIP: dose increasing over 5 days to 120 mg/day (patient 1); 60 mg/day (patient 2). N = 1. 2. Placebo. N = 1. Antipsychotic free at least 4 weeks prior to study. Concomitant medication not reported. |
|
| Outcomes | TD symptoms: SEPS. Mental state: BPRS. Adverse effects. | |
| Notes | No person left study early. THIP produced mental state change and tonic‐clonic seizures 8 days after its withdrawal. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The order of drug and placebo periods was randomized", no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "patients, staff, and evaluators were blind to the treatment course." Further blinding details not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | TD symptoms and Mental state: "...evaluators were blind to the treatment course." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the trial. |
| Selective reporting (reporting bias) | High risk | Not all outcomes have been reported. TD symptoms outcome data reported for the whole population (not per period) in the GVG trial and not reported in the THIP trial. Improvement data not reported for placebo groups. |
| Other bias | Unclear risk | Very small sample size; cross‐over design. Insufficient information to make a judgement |
Yin 2004.
| Methods | Allocation: "randomly assigned".
Blinding: "double blind" "the sodium valproate and starch placebo were enclosed in capsule with same appearance, the interventions were coded by researchers as drug I and drug II".
Duration: 6 weeks. Location: inpatients, China. |
|
| Participants | Diagnosis: Antipsychotics‐induced TD (Schooler criteria). Duration of TD: not reported. N = 80. Sex: 80 male. Age:mean 44 (SD 8) years old. |
|
| Interventions | 1. Sodium valproate group: The initial dosage of sodium valproate was 0.2 g each time, three times per day; after 4 weeks if no adverse events, the dosage was titrated to 0.4 g each time, three times a day for 2 weeks, the treatment lasted for 6 weeks. N = 40. 2. Placebo group: starch capsule was the placebo treatment for 6 weeks. N = 40. All participants received stable doses of antipsychotics. Other concomitant medication was not reported. |
|
| Outcomes | TD clinical response. TD: AIMS. Mental state: BPRS. Adverse events: TESS, hypotension and disturbance of consciousness, leukocyte decrease, low platelet count. | |
| Notes | Funding source: not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ....."randomly assigned…", no further details |
| Allocation concealment (selection bias) | Unclear risk | The author did not state the method of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | ....."double blind" "the sodium valproate and starch placebo were enclosed in capsule with same appearance, the interventions were coded by researchers as drug I and drug II" : Blinding of participants and key study personnel ensured. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant in the treatment group left the study early. |
| Selective reporting (reporting bias) | Unclear risk | Unclear if all outcomes have been reported. |
| Other bias | Low risk | None obvious. |
TD ‐ tardive dyskinesia
TD scales AIMS ‐ Abnormal Involuntary Movement Scale. BRS ‐ Barnes & Kidger Rating Scale. GRS ‐ Gerlach Rating Scale. SEPS ‐ Smith Extrapyramidal Scale. SRS ‐ Simpson Rating Scale.
Global state scales CGI ‐ Clinical Global Improvement
Mental/behaviour state scales BPRS ‐ Brief Psychiatric Rating Scale NOSIE ‐ Nurses Observation Scale for Inpatient Evaluation
General scales TESS ‐ Treatment Emergent Symptom Scale
Medication abbreviations CPE ‐ chlorpromazine equivalent dosages GVG ‐ Gamma‐vynil GABA SV ‐ Sodium valproate THIP ‐ tetrahydroisoxazolopyridinol
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Casey 1979 | Allocation: not randomised, cohort study. |
| Casey 1980 | Allocation: not randomised. |
| Cassady 1992 | Allocation: randomised. Participants: people with TD. Intervention: muscimol versus placebo, unstable dose of antipsychotic drugs. Outcomes: only reported after 2 hours |
| Cassady 1993 | Allocation: not randomised, ABA study. |
| Chien 1978 | Allocation: randomised. Participants: people with TD. Intervention: sodium valproate versus oxypertine versus deanol. Outcomes: Unable to extract data from first cross‐over phase (TD improvement, AIMS, Leaving the study early). We were unable to identify up‐to‐date study author contact details for this over 35‐year old study. |
| Chiu 2006 | Allocation: randomised, cross‐over design. Participants: people with Schizophrenia. Interventions: ginseng versus placebo, not GABA agonist. |
| Danion 1984 | Allocation: not randomised. |
| Frangos 1980 | Allocation: randomised. Participants: people with TD. Intervention: baclofen versus placebo. Outcomes: not possible to extract data; published only as a conference proceeding ‐ authors contacted in 1996 and did not reply. |
| Friis 1983 | Allocation: randomised, cross‐over design. Participants: people with TD. Interventions: valproate versus biperiden versus placebo. Outcomes: no data from first period; Dr Gerlach contacted and replied promptly; data were destroyed and no more information is available. |
| Gibson 1978 | Allocation: not randomised, cohort study. |
| Gulmann 1976 | Allocation: randomised. Participants: people with schizophrenia, not TD. Interventions: baclofen versus placebo; 19/20 participants were given chlorpromazine. |
| Korsgaard 1976 | Allocation: randomised, cross‐over design. Participants: people with antipsychotic‐induced TD. Intervention: baclofen versus placebo. Outcomes: not possible to extract data from first period; authors contacted in 1996 and did not reply. The study was excluded as it is over 35 years old and further attempts to contact authors will likely not be fruitful. |
| Korsgaard 1982 | Allocation: not randomised. |
| Korsgaard 1983 | Allocation: not randomised. |
| Lambert 1982 | Allocation: not randomised. |
| Monteleone 1988 | Allocation: not randomised, case‐control study. |
| Morselli 1985 | Allocation: not randomised. |
| Nagao 1979 | Allocation: not randomised. |
| Nasrallah 1985 | Allocation: not randomised. |
| Nasrallah 1986 | Allocation: randomised. Participants: schizophrenia, paranoid disorder, and schizoaffective disorder + Schooler and Kane criteria for persistent TD. Interventions: AMPT vs L‐DOPA vs Choline chloride vs Valproic acid vs Hydroxytryptophan Outcomes: No outcome data have been provided for the first period before cross‐over. Study author was contacted for data; no additional information was received, so this 25‐year old study was excluded. |
| Nordic 1986 | Allocation: randomised, cross‐over design. Interventions:chlorprothixene, perphenazine, haloperidol and haloperidol + biperiden versus placebo, not GABA agonist. |
| Raptis 1990 | Allocation: randomised. Participants: people with schizophrenia without TD. |
| Rondot 1987 | Allocation: not randomised. |
| Sikich 1999 | Allocation: randomised, double‐blind. Participants: 8 to 19 year olds with active psychotic symptoms, not TD. Interventions: haloperidol, risperidone, and olanzapine, not GABA agonist. |
| Simpson 1978 | Allocation: not randomised. |
| Stahl 1985 | Allocation: not randomised. |
| Tamminga 1978 | Allocation: double‐blind methodology, randomisation not stated. Participants: people with schizophrenia without TD. |
| Tamminga 1979 | Allocation: randomised. Participants: people free from antipsychotic drugs for < 1 month: dose unstable. Intervention: muscimol versus placebo. Outcomes: no usable data. |
| Tamminga 1983 | Allocation: randomised, cross‐over design. Participants: people with TD. Intervention: GVG versus placebo. Outcomes: not possible to extract data from first period; authors contacted three times in 1996, did reply, but did not provide any further information. |
| Tell 1981 | Allocation: not randomised. |
TD ‐ tardive dyskinesia TD scales AIMS ‐ Abnormal Involuntary Movement Scale
GABA ‐ Gamma‐aminobutyric acid GABA compounds GVG ‐ Gamma‐vynil GABA GAG ‐ Gamma‐acetylenic GABA THIP ‐ Tetrahydroisoxazolopyridinol
Outcome SCD ‐ Saccadic distractibility
Differences between protocol and review
We have substantially reformatted this review in light of changes to software (RevMan 5). We add a 'Summary of findings' table, which was prepared using Grade Pro 3.2, and a PRISMA study flow chart. We have also updated the title from 'Gamma‐aminobutyric acid agonists for neuroleptic‐induced tardive dyskinesia' to Gamma‐aminobutyric acid agonists for antipsychotic‐induced tardive dyskinesia,and updated the list of outcomes following consultation with consumers.
The previous methods are reproduced in Appendix 1.
Contributions of authors
1. Original review
Karla Soares‐Weiser ‐ protocol writing, searching, trial selection, data extraction and assimilation, report writing.
John Rathbone ‐ update ‐ trial selection, data extraction and assimilation, report writing.
Jon Deeks ‐ data extraction and assimilation, statistical support, report writing.
2. 2010 update
Youssef Latifeh, Husam Aldeen Mohammad ‐ trial selection. Samer Alabed ‐ update ‐ trial selection, protocol update, report update.
3. 2017 update
Hanna Bergman ‐ trial selection, data extraction and assimilation, report update.
Sources of support
Internal sources
Faculty of Medicine, Damascus University, Syrian Arab Republic.
Queensland Health, Australia.
Universidade Federal de Sao Paulo, Brazil.
NHS Anglia & Oxford Region R & D Programme, England, UK.
-
Enhance Reviews Ltd., UK.
Logistics support for Hanna Bergman
External sources
CAPES ‐ Ministry of Education, Brazil, Other.
-
NIHR HTA Project Grant, reference number: 14/27/02, UK.
Salary support for Hanna Bergman. Support for patient involvement. Support for traceable data database.
Declarations of interest
Samer Alabed ‐ None known. Youssef Latifeh ‐ None known. Husam Aldeen Mohammad ‐ None known. Hanna Bergman ‐ worked for Enhance Reviews Ltd. during preparation of this review and was paid for her contribution to this review. Enhance Reviews Ltd. is a private company that performs systematic reviews of literature. Hanna Bergman now has a consultancy contract with Cochrane Response, an evidence services unit operated by the Cochrane Collaboration, to carry out systematic reviews on various topics.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Ananth 1987 {published data only}
- Ananth J, Djenderedjian A, Beshay M, Kamal M, Kodjian A, Barriga C. Baclofen in the treatment of tardive dyskinesia. Current Therapeutic Research 1987;42(1):111‐4. [Google Scholar]
Burner 1989 {published data only}
- Burner M, Giroux C, L'Heritier C, Garreau M, Morselli PL. Preliminary observations on the therapeutic action of progabide in tardive dyskinesia. Brain Dysfunction 1989;2(6):289‐96. [Google Scholar]
Fisk 1987 {published data only}
- Fisk GG, York SM. The effect of sodium valproate on tardive dyskinesia ‐ revisited. British Journal of Psychiatry 1987;150:542‐6. [DOI] [PubMed] [Google Scholar]
Gerlach 1978 {published data only}
- Gerlach J. The relationship between parkinsonism and tardive dyskinesia. American Journal of Psychiatry 1977;134(7):781‐4. [DOI] [PubMed] [Google Scholar]
- Gerlach J, Rye T, Kristjansen P. Effect of baclofen on tardive dyskinesia. Psychopharmacology 1978;56(2):145‐51. [PUBMED: 417365] [DOI] [PubMed] [Google Scholar]
Glazer 1985 {published data only}
- Glazer WM, Moore DC, Bowers MB, Bunney BS, Roffman M. The treatment of tardive dyskinesia with baclofen. Psychopharmacology 1985;87(4):480‐3. [DOI] [PubMed] [Google Scholar]
Linnoila 1976 {published data only}
- Linnoila M, Viukari M, Kietala O. Effect of sodium valproate on tardive dyskinesia. British Journal of Psychiatry 1976;129:114‐9. [PUBMED: 786416] [DOI] [PubMed] [Google Scholar]
Mei 2008 {published data only}
- Mei H, Zhu Q. γ‐aminobutyric acid in the treatment of 20 cases of tardive dyskinesia. Herald of Medicine 2008;27(3):304‐5. [Google Scholar]
Nair 1978 {published data only}
- Nair NP, Lal S, Schwartz G, Thavundayil JX. Effect of sodium valproate and baclofen in tardive dyskinesia: clinical and neuroendocrine studies. Advances in Biochemical Psychopharmacology 1980;24:437‐41. [PUBMED: 6773303] [PubMed] [Google Scholar]
- Nair NPV, Yassa R, Ruiz‐Navarro J, Schwartz G. Baclofen in the treatment of tardive dyskinesia. American Journal of Psychiatry 1978;135:1562‐3. [DOI] [PubMed] [Google Scholar]
Stewart 1982 {published data only}
- Stewart RM, Rollins J, Beckam B, Roffman M. Baclofen for tardive dyskinesia: a double‐blind placebo‐controlled trial. Neurology 1982;32(4 II):A114. [Google Scholar]
- Stewart RM, Rollins J, Beckham B, Roffman M. Baclofen in tardive dyskinesia patients maintained on neuroleptics. Clinical Neuropharmacology 1982;5(4):365‐73. [PUBMED: 6130838] [DOI] [PubMed] [Google Scholar]
Thaker 1987 {published data only}
- Thaker GK, Tamminga CA, Alphs LD, Lafferman J, Ferraro TN, Hare TA. Brain gamma‐aminobutyric acid abnormality in tardive dyskinesia. Reduction in cerebrospinal fluid GABA levels and therapeutic response to GABA agonist treatment. Archives of General Psychiatry 1987;44(6):522‐9. [PUBMED: 3034188] [DOI] [PubMed] [Google Scholar]
Yin 2004 {published data only}
- Yin XR, Xie BQ, Jiang L. A double‐blind comparative study of sodium valproate in treating of TD. Journal of Clinical Psychological Medicine 2004;14(2):92‐93. [Google Scholar]
References to studies excluded from this review
Casey 1979 {published data only}
- Casey DE, Hammerstad JP. Sodium valproate in tardive dyskinesia. Journal of Clinical Psychiatry 1979;40:483‐5. [PubMed] [Google Scholar]
Casey 1980 {published data only}
- Casey DE, Gerlach J, Magelund G, Christensen TR. Gamma‐acetylenic GABA in tardive dyskinesia. Advances in Biochemical Psychopharmacology 1980;24:577‐80. [PubMed] [Google Scholar]
- Casey DE, Gerlach J, Magelund G, Christensen TR. Gamma‐acetylenic GABA in tardive dyskinesia. Archives of General Psychiatry 1980;37(12):1376‐9. [DOI] [PubMed] [Google Scholar]
Cassady 1992 {published data only}
- Cassady SL, Thaker GK, Moran M, Birt A, Tamminga CA. GABA agonist‐induced changes in motor, oculomotor, and attention measures correlate in schizophrenics with tardive dyskinesia. Biological Psychiatry 1992;32(4):302‐11. [DOI] [PubMed] [Google Scholar]
Cassady 1993 {published data only}
- Cassady SL, Thaker GK, Tamminga CA. Pharmacologic relationship of anti saccade and dyskinesia in schizophrenic patients. Psychopharmacology Bulletin 1993;29(2):236‐40. [PubMed] [Google Scholar]
Chien 1978 {published data only}
- Chien CP, Jung K, Ross‐Townsend A. Efficacies of agents related to GABA, dopamine and acetylcholine in the treatment of tardive dyskinesia. Psychopharmacology Bulletin 1978;14(2):20‐2. [PubMed] [Google Scholar]
Chiu 2006 {published data only}
- Chiu SS. A placebo‐controlled cross study of panax ginseng in augmentation of antipsychotics in 60 partially treatment responsive patients with schizophrenia. http://www.clinicaltrials.gov 2006.
Danion 1984 {published data only}
- Danion JM, Singer L, Tell G, Schechter P. Gamma‐vinyl‐GABA et dyskinesies tardives: une etude en simple insu contre placebo. Annales Medico‐Psychologiques Paris 1984;142(1):101‐10. [PubMed] [Google Scholar]
Frangos 1980 {published data only}
- Frangos E, Athanasenas E. Lioresal in the treatment of neuroleptic‐induced tardive dyskinesia. Proceedings of the12th CINP Congress; 1980 June 22‐26; Goteborg, Sweden. 1980.
Friis 1983 {published data only}
- Friis T, Rosted‐Christensen T, Gerlach J. Sodium valproate and biperiden in neuroleptic‐induced akathisia, parkinsonism and hyperkinesia: a double‐blind crossover study with placebo. Acta Psychiatrica Scandinavica 1983;67(3):178‐87. [DOI] [PubMed] [Google Scholar]
Gibson 1978 {published data only}
- Gibson AC. Sodium valproate and tardive dyskinesia. British Journal of Psychiatry 1978;133:82. [DOI] [PubMed] [Google Scholar]
Gulmann 1976 {published data only}
- Gulmann NC, Bahr B, Andersen B, Eliassen HM. A double‐blind trial of baclofen against placebo in the treatment of schizophrenia. Acta Psychiatrica Scandinavica 1976;54(4):287‐93. [DOI] [PubMed] [Google Scholar]
Korsgaard 1976 {published data only}
- Korsgaard S. Baclofen (lioresal) in the treatment of neuroleptic‐induced tardive dyskinesia. Acta Psychiatrica Scandinavica 1976;54(1):17‐24. [DOI] [PubMed] [Google Scholar]
Korsgaard 1982 {published data only}
- Korsgaard S, Casey DE, Gerlach J, Hetmar O, Kaldan B, Mikkelsen LB. The effect of tetrahydroisoxazolopyridinol (THIP) in tardive dyskinesia: a new gamma‐aminobutyric acid agonist. Archives of General Psychiatry 1982;39(9):1017‐21. [DOI] [PubMed] [Google Scholar]
Korsgaard 1983 {published data only}
- Korsgaard S, Casey D, Gerlach J. GABA agonist treatment of tardive dyskinesia. Proceedings of the 13th Congress of Collegium Internationale Neuro‐psychopharmacologicum; 1982 Jun 20‐25; Jerusalem, Israel. 1982.
- Korsgaard S, Casey DE, Gerlach J. Effect of gamma‐vinyl GABA in tardive dyskinesia. Psychiatry Research 1983;8(4):261‐9. [DOI] [PubMed] [Google Scholar]
Lambert 1982 {published data only}
- Lambert PA, Cantiniaux P, Chabannes JP, Tell GP, Schechter PJ, Koch‐Weser J. Therapeutic trial of gamma‐vinyl GABA, an inhibitor of GABA transaminase, in tardive dyskinesias induced by neuroleptics [Essai therapeutique du gamma‐vinyl GABA, un inhibiteur de la GABA‐transaminase, dans les dyskinesies tardives induites par les neuroleptiques]. L'Encephale 1982;8(3):371‐6. [PubMed] [Google Scholar]
Monteleone 1988 {published data only}
- Monteleone P, Maj M, Ariano MG, Iovino M, Fiorenza L, Steardo L. Prolactin response to sodium valproate in schizophrenics with and without tardive dyskinesia. Psychopharmacology 1988;96:223‐6. [DOI] [PubMed] [Google Scholar]
Morselli 1985 {published data only}
- Morselli PL, Fournier V, Bossi L, Musch B. Clinical activity of GABA agonists in neuroleptic and L‐dopa‐induced dyskinesia. Psychopharmacology 1985;2(Suppl):128‐36. [DOI] [PubMed] [Google Scholar]
Nagao 1979 {published data only}
- Nagao T, Ohshimo T, Mitsunobu K, Sato M, Otsuki S. Cerebrospinal fluid monoamine metabolites and cyclic nucleotides in schizophrenic patients with tardive dyskinesia or drug‐induced tremor. Biological Psychiatry 1979;14(3):509‐23. [PubMed] [Google Scholar]
Nasrallah 1985 {published data only}
- Nasrallah HA, Dunner FJ, McCalley‐Whitters M. A placebo‐controlled trial of valproate in tardive dyskinesia. Biological Psychiatry 1985;20(2):205‐8. [DOI] [PubMed] [Google Scholar]
Nasrallah 1986 {published data only}
- Nasrallah HA, Dunner FJ, McCalley‐Whitters M, Smith RE. Pharmacologic probes of neurotransmitter systems in tardive dyskinesia: implications for clinical management. Journal of Clinical Psychiatry 1986;47(2):56‐9. [PubMed] [Google Scholar]
Nordic 1986 {published data only}
- Nordic Dyskinesia Study Group. Effect of different neuroleptics in tardive dyskinesia and parkinsonism. A video‐controlled multicenter study with chlorprothixene, perphenazine, haloperidol and haloperidol + biperiden. Psychopharmacology 1986;90(4):423‐9. [PubMed] [Google Scholar]
Raptis 1990 {published data only}
- Raptis C, Garcia‐Borreguero D, Webef MM, Sode M, Bremer D, Emrich HM. Anticonvulsants as adjuncts for the neuroleptic treatment of schizophrenic psychoses: a clinical study with beclamide. Acta Psychatrica Scandinavica 1990;81:162‐7. [DOI] [PubMed] [Google Scholar]
Rondot 1987 {published data only}
- Bathien N, Sevestre P, Rondot P, Morselli PL, Landeghem V. The effect of progabide, a specific GABAergic agonist, on neuroleptic‐induced tardive dyskinesia ‐ a result of a pilot study. Proceedings of the 13th Collegium Internationale Neuropsychopharmacologicum Congress; 1982 June 20‐25; Jerusalem, Israel. 1982.
- Rondot P, Bathien N. Movement disorders in patients with coexistent neuroleptic‐induced tremor and tardive dyskinesia: EMG and pharmacological study. Advances in Neurology 1987;45:361‐6. [PubMed] [Google Scholar]
Sikich 1999 {published data only}
- Sikich L. Critical decisions in the treatment of adolescent and pediatric psychosis. Proceedings of the 154th Annual Meeting of the American Psychiatric Association; 2001 May 5‐10; New Orleans, Louisiana, USA. Marathon Multimedia, 2001.
- Sikich L. Critical decisions in the treatment of adolescent and pediatric psychosis. Proceedings of the 155th Annual Meeting of the American Psychiatric Association; 2002 May 18‐23; Philadelphia, Pennsylvania, USA. 2002.
- Sikich L, Horrigan JP, Lieberman JA, Barnhill LJ, Sheitman BB, Courvoisie HE. Comparative use of olanzapine and risperidone in psychotic youth. Proceedings of the 154th Annual Meeting of the American Psychiatric Association; 2001 May 5‐10; New Orleans, Louisiana, USA. Marathon Multimedia, 2001.
- Sikich L, Williamson K, Malekpour A, Bashford RA, Hooper S, Sheitman B, Lieberman JA. Interim results of a randomized controlled trial of haloperidol, risperidone, and olanzapine in psychotic youth. Proceedings of the 38th Annual Meeting of the American College of Neuropsychopharmacology; 1999 Dec 12‐16; Acapulco, Mexico. USA, 1999.
Simpson 1978 {published data only}
- Simpson GM, Lee JH, Shrivastava RK, Branchey MH. Baclofen in the treatment of tardive dyskinesia and schizophrenia. Psychopharmacology Bulletin 1978;14(2):16‐8. [PubMed] [Google Scholar]
Stahl 1985 {published data only}
- Stahl SM, Thornton JE, Simpson ML, Berger PA, Napoliello MJ. Gamma‐vinyl‐GABA treatment of tardive dyskinesia and other movement disorders. Biological Psychiatry 1985;20(8):888‐93. [DOI] [PubMed] [Google Scholar]
Tamminga 1978 {published data only}
- Tamminga CA, Crayton JW, Chase TN. Muscimol: GABA agonist therapy in schizophrenia. American Journal of Psychiatry 1978;135:746‐7. [DOI] [PubMed] [Google Scholar]
Tamminga 1979 {published data only}
- Tamminga CA, Crayton JW, Chase TN. Improvement in tardive dyskinesia after muscimol therapy. Archives of General Psychiatry 1979;36(5):595‐8. [DOI] [PubMed] [Google Scholar]
Tamminga 1983 {published data only}
- Nguyen JA, Thaker GK, Tamminga CA. Gamma‐aminobutyric‐acid (GABA) pathways in tardive dyskinesia. Psychiatric Annals 1989;19(6):302‐9. [Google Scholar]
- Tamminga CA, Thaker GK, Ferraro TN, Hare TA. GABA agonist treatment improves tardive dyskinesia. Lancet 1983;2:97‐8. [DOI] [PubMed] [Google Scholar]
- Tamminga CA, Thaker GK, Goldberg ST. Tardive dyskinesia: GABA agonist treatment. In: Usdin E, Carlsson A, Dahlstrom A, Engel J editor(s). Catecholamines: Neuropharmacology and Central Nervous System ‐ Therapeutic Aspects. New York: Alan R Liss, 1984. [Google Scholar]
- Thaker GK, Hare TA, Tamminga CA. GABA system: clinical research and treatment of tardive dyskinesia. Modern Problems of Pharmacopsychiatry 1983;21:155‐67. [DOI] [PubMed] [Google Scholar]
Tell 1981 {published data only}
- Tell GP, Schechter PJ, Koch‐Weser J, Cantiniaux P, Chabannes JP, Lambert PA. Effects of gamma‐vinyl GABA. New England Journal of Medicine 1981;305(10):581‐2. [PubMed] [Google Scholar]
Additional references
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313(7066):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
APA 1992
- American Psychiatric Association. Tardive Dyskinesia: A Task Force Report of the American Psychiatric Association. Washington, DC: American Psychiatric Association, 1992. [Google Scholar]
Bakker 2006
- Bakker PR, Harten PN, Os J. Antipsychotic‐induced tardive dyskinesia and the Ser9Gly polymorphism in the DRD3 gene: a meta analysis. Schizophrenia Research 2006;83(2‐3):185‐92. [PUBMED: 16513329] [DOI] [PubMed] [Google Scholar]
Barnes 1988
- Barnes TRE. Tardive dyskinesia: risk factors, pathophysiology and treatment. In: Granville‐Grossman K editor(s). Recent Advances in Clinical Psychiatry. Vol. 6, London: Churchill Livingstone, 1988. [Google Scholar]
Barnes 1993
- Barnes TRE, Edwards JG. The side‐effects of antipsychotic drugs. I. CNS and neuromuscular effects. In: Barnes TRE editor(s). Antipsychotic Drugs and their Side‐Effects. London: Academic Press, Harcourt Brace & Company, 1993. [Google Scholar]
Bergen 1984
- Bergen JA, Griffiths DA, Rey JM, Beumont PJV. Tardive dyskinesia: fluctuating patient or fluctuating rater. British Journal of Psychiatry 1984;144:498‐502. [DOI] [PubMed] [Google Scholar]
Bergman 2018
- Bergman H, Bhoopathi PS, Soares‐Weiser K. Benzodiazepines for antipsychotic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2018, Issue 1. [DOI: 10.1002/14651858.CD000205.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergman 2018a
- Bergman H, Soares‐Weiser K. Anticholinergic medication for antipsychotic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2018, Issue 1. [DOI: 10.1002/14651858.CD000204.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergman 2018b
- Bergman H, Rathbone J, Agarwal V, Soares‐Weiser K. Antipsychotic reduction and/or cessation and antipsychotics as specific treatments for tardive dyskinesia. Cochrane Database of Systematic Reviews 2018, Issue 2. [DOI: 10.1002/14651858.CD000459.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bland 1997
- Bland JM. Statistics notes. Trials randomised in clusters. BMJ 1997;315:600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boissel 1999
- Boissel JP, Cucherat M, Li W, Chatellier G, Gueyffier F, Buyse M, et al. The problem of therapeutic efficacy indices. 3. Comparison of the indices and their use [Apercu sur la problematique des indices d'efficacite therapeutique, 3: comparaison des indices et utilisation. Groupe d'Etude des Indices D'efficacite]. Therapie 1999;54(4):405‐11. [PUBMED: 10667106] [PubMed] [Google Scholar]
Casey 1994
- Casey DE. Tardive dyskinesia: pathophysiology. In: Bloom FE, Kupfer DJ editor(s). Psychopharmacology. The Fourth Generation of Progress. New York: Raven Press, 1994. [Google Scholar]
Casey 1999
- Casey DE. Tardive dyskinesia and atypical antipsychotic drugs. Schizophrenia Research 1999;35:31‐6. [DOI] [PubMed] [Google Scholar]
Casey 2000
- Casey DE. Tardive dyskinesia: pathophysiology and animal models. Journal of Clinical Psychiatry 2000;61(Suppl 4):5‐9. [PubMed] [Google Scholar]
Chouinard 2008
- Chouinard G, Chouinard VA. Atypical antipsychotics: CATIE study, drug‐induced movement disorder and resulting iatrogenic psychiatric‐like symptoms, supersensitivity rebound psychosis and withdrawal discontinuation syndromes. Psychotherapy and Psychosomatics 2008; Vol. 77, issue 2:69‐77. [DOI] [PubMed]
Deeks 2000
- Deeks J. Issues in the selection for meta‐analyses of binary data. Proceedings of the 8th International Cochrane Colloquium; 2000 Oct 25‐28; Cape town. Cape Town: The Cochrane Collaboration, 2000.
Divine 1992
- Divine GW, Brown JT, Frazier LM. The unit of analysis error in studies about physicians' patient care behavior. Journal of General Internal Medicine 1992;7(6):623‐9. [DOI] [PubMed] [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta‐analysis of cluster randomized trials. Statistics in Medicine 2002;21:2971‐80. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
El‐Sayeh 2006
- El‐Sayeh HG, Lyra da Silva JP, Rathbone J, Soares‐Weiser K. Non‐neuroleptic catecholaminergic drugs for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD000458.pub2] [DOI] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne D, Altman DG, Higgins JPT, Curtina F, Worthingtond HV, Vaile A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
Essali 2011
- Essali A, Deirawan H, Soares‐Weiser K, Adams CE. Calcium channel blockers for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD000206.pub3] [DOI] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta‐analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(7):7‐10. [DOI] [PubMed] [Google Scholar]
Gardos 1994
- Gardos G, Cole JO. The treatment of tardive dyskinesia. In: Bloom FE, Kupfer DJ editor(s). Psychopharmacology. The Fourth Generation of Progress. Raven Press, 1994. [Google Scholar]
Gerlach 1976
- Gerlach J, Thorsen K. The movement pattern of oral tardive dyskinesia in relation to anticholinergic and antidopaminergic treatment. International Pharmacopsychiatry 1976;11(1):1‐7. [DOI] [PubMed] [Google Scholar]
Glazer 2000
- Glazer WM. Review of incidence studies of tardive dyskinesia associated with typical antipsychotics. Journal of Clinical Psychiatry 2000;61(Suppl 4):15‐20. [PubMed] [Google Scholar]
Gulliford 1999
- Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community‐based surveys and intervention studies: data from the health survey for England 1994. Journal of American Epidemiology 1999;149:876‐83. [DOI] [PubMed] [Google Scholar]
Gunne 1984
- Gunne LM, Haggstrom JE, Sjoquist B. Association with persistent neuroleptic induced dyskinesia of regional changes in brain GABA synthesis. Nature 1984;309:347‐9. [DOI] [PubMed] [Google Scholar]
Guy 1976
- Guy W. ECDEU Assessment Manual for Psychopharmacology. National Institute of Mental Health Publication No. 76‐338. Washington, DC: US Government Printing Office, 1976. [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons, 2008. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Jeste 1982
- Jeste DV, Wyatt RJ. Understanding and Treating Tardive Dyskinesia. New York: Guilford Press, 1982. [Google Scholar]
Jeste 1988
- Jeste DV, Lohr JB, Clark K, Wyatt RJ. Pharmacological treatments of tardive dyskinesia in the 1980s. Journal of Clinical Psychopharmacology 1988;8(4 Suppl):38S‐48S. [PubMed] [Google Scholar]
Jeste 2000
- Jeste DV. Tardive dyskinesia in older patients. Journal of Clinical Psychiatry 2000;61(Suppl 4):27‐32. [PubMed] [Google Scholar]
Jűni 2001
- Jűni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kay 1986
- Kay SR, Opler LA, Fiszbein A. Positive and Negative Syndrome Scale (PANSS) Manual. North Tonawanda, NY: Multi‐Health Systems, 1986. [Google Scholar]
Leon 2006
- Leon AC, Mallinckrodt CH, Chuang‐Stein C, Archibald DG, Archer GE, Chartier K. Attrition in randomized controlled clinical trials: methodological issues in psychopharmacology. Biological Psychiatry 2006;59(11):1001‐5. [PUBMED: 16905632] [DOI] [PubMed] [Google Scholar]
Leucht 2005
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean?. Schizophrenia Research 2005;79(2‐3):231‐8. [PUBMED: 15982856] [DOI] [PubMed] [Google Scholar]
Leucht 2005a
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. Clinical implications of brief psychiatric rating scale scores. British Journal of Psychiatry 2005;187:366‐71. [DOI] [PubMed] [Google Scholar]
Lieberman 1996
- Lieberman JA, Fleishhacker W. Introduction. British Journal of Psychiatry 1996;168(Suppl 29):7‐8. [Google Scholar]
Marshall 2000
- Marshall M, Lockwood A, Bradley C, Adams CE, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
NICE 2014
- NICE. Psychosis and schizophrenia in adults: treatment and management. NICE clinical guideline 178 (guidance.nice.org.uk/cg178) 2014.
Overall 1962
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychological Reports 1962;10:799‐812. [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Simpson 1979
- Simpson GM, Lee JH, Zoubok B, Gardos G. A rating scale for tardive dyskinesia. Psychopharmacology 1979;64(2):171‐9. [DOI] [PubMed] [Google Scholar]
Soares‐Weiser 2003
- Soares‐Weiser K, Irving CB, Rathbone J. Miscellaneous treatments for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD000208] [DOI] [PubMed] [Google Scholar]
Soares‐Weiser 2018
- Soares‐Weiser K, Maayan N, Bergman H. Vitamin E for antipsychotic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2018, Issue 1. [DOI: 10.1002/14651858.CD000209.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steen 1997
- Steen VM, Lovlie R, MacEwan T, McCreadie RG. Dopamine D3‐receptor gene variant and susceptibility to tardive dyskinesia in schizophrenic patients. Molecular Psychiatry 1997;2(2):139‐45. [PUBMED: 9106238] [DOI] [PubMed] [Google Scholar]
Tammenmaa 2002
- Tammenmaa I, McGrath J, Sailas E, Soares‐Weiser K. Cholinergic medication for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD000207] [DOI] [PubMed] [Google Scholar]
Taylor 2009
- Taylor D, Paton C, Kapur S. The Maudsley Prescribing Guidelines (10th Edition). London: Informa Healthcare, 2009. [Google Scholar]
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area‐wide and organistation‐based intervention in health and health care: a systematic review. Health Technology Assessment 1999;3(5):1‐75. [PubMed] [Google Scholar]
Xia 2007
- Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, Pinfold V, Takriti Y. The Leeds Outcomes Stakeholders Survey (LOSS) Study. Proceedings of the 15th Cochrane Colloquium; 2007 Oct 23‐27; Sao Paulo. 2007.
Xia 2009
- Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, El‐Sayeh H, et al. Loss to outcomes stakeholder survey: the LOSS study. Psychiatric Bulletin 2009;33(7):254‐7. [Google Scholar]
References to other published versions of this review
Alabed 2011
- Alabed S, Latifeh Y, Mohammad HA, Rifai A. Gamma‐aminobutyric acid agonists for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2011, Issue 4. [DOI: 10.1002/14651858.CD000203.pub3] [DOI] [PubMed] [Google Scholar]
Rathbone 2004
- Rathbone J, Deeks JJ, Soares‐Weiser K. Gamma‐aminobutyric acid agonists for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD000203.pub2] [DOI] [PubMed] [Google Scholar]
Soares‐Weiser 2000
- Soares‐Weiser K, McGrath J, Deeks J. Gamma‐aminobutyric acid agonists for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: 10.1002/14651858.CD000203.pub2] [DOI] [PubMed] [Google Scholar]
Soares‐Weiser 2001
- Soares‐Weiser K, McGrath J, Deeks J. Gamma‐aminobutyric acid agonists for neuroleptic‐induced tardive dyskinesia. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD000203.pub2] [DOI] [PubMed] [Google Scholar]


