Abstract
Background
The delivery of effective, high‐quality patient care is a complex activity. It demands health and social care professionals collaborate in an effective manner. Research continues to suggest that collaboration between these professionals can be problematic. Interprofessional education (IPE) offers a possible way to improve interprofessional collaboration and patient care.
Objectives
To assess the effectiveness of IPE interventions compared to separate, profession‐specific education interventions; and to assess the effectiveness of IPE interventions compared to no education intervention.
Search methods
For this update we searched the Cochrane Effective Practice and Organisation of Care Group specialised register, MEDLINE and CINAHL, for the years 2006 to 2011. We also handsearched the Journal of Interprofessional Care (2006 to 2011), reference lists of all included studies, the proceedings of leading IPE conferences, and websites of IPE organisations.
Selection criteria
Randomised controlled trials (RCTs), controlled before and after (CBA) studies and interrupted time series (ITS) studies of IPE interventions that reported objectively measured or self reported (validated instrument) patient/client or healthcare process outcomes.
Data collection and analysis
At least two review authors independently assessed the eligibility of potentially relevant studies. For included studies, at least two review authors extracted data and assessed study quality. A meta‐analysis of study outcomes was not possible due to heterogeneity in study designs and outcome measures. Consequently, the results are presented in a narrative format.
Main results
This update located nine new studies, which were added to the six studies from our last update in 2008. This review now includes 15 studies (eight RCTs, five CBA and two ITS studies). All of these studies measured the effectiveness of IPE interventions compared to no educational intervention. Seven studies indicated that IPE produced positive outcomes in the following areas: diabetes care, emergency department culture and patient satisfaction; collaborative team behaviour and reduction of clinical error rates for emergency department teams; collaborative team behaviour in operating rooms; management of care delivered in cases of domestic violence; and mental health practitioner competencies related to the delivery of patient care. In addition, four of the studies reported mixed outcomes (positive and neutral) and four studies reported that the IPE interventions had no impact on either professional practice or patient care.
Authors' conclusions
This updated review reports on 15 studies that met the inclusion criteria (nine studies from this update and six studies from the 2008 update). Although these studies reported some positive outcomes, due to the small number of studies and the heterogeneity of interventions and outcome measures, it is not possible to draw generalisable inferences about the key elements of IPE and its effectiveness. To improve the quality of evidence relating to IPE and patient outcomes or healthcare process outcomes, the following three gaps will need to be filled: first, studies that assess the effectiveness of IPE interventions compared to separate, profession‐specific interventions; second, RCT, CBA or ITS studies with qualitative strands examining processes relating to the IPE and practice changes; third, cost‐benefit analyses.
Plain language summary
Training health and social care professionals to work together effectively
Interprofessional education (IPE) is defined as an intervention where the members of more than one health or social care profession, or both, learn interactively together, for the explicit purpose of improving interprofessional collaboration or the health/well being of patients/clients, or both. This review evaluated the effectiveness of IPE compared to educational interventions in which different professional groups were learning separately from one another and IPE compared with interventions in which no IPE was offered to a comparison group. This review was restricted to studies that measured patient outcomes or healthcare processes. This excluded qualitative studies and quantitative studies that reported on the impact that IPE can have on participants' attitudes, knowledge and skills of collaboration. This does not imply that qualitative studies and those focused on attitudes, knowledge and skills do not offer useful insights for certain purposes; simply that they are not the focus of this review.
Nine studies met the inclusion criteria for the review. These studies were added to the six that we found the last time we updated the review, bringing the total to 15 studies. Seven of these studies reported positive outcomes for healthcare processes or patient outcomes, or both, four studies reported mixed outcomes (positive and neutral) and four reported no effects of IPE. The studies differed in many respects. They were conducted in different areas of clinical practice and included different IPE interventions. The study designs and outcome measures were also different. All 15 studies compared outcomes following an IPE intervention to outcomes, either in similar clinical settings that did not receive the IPE intervention, or in the same clinical setting before the intervention was made. Because no studies compared an interprofessional intervention to a profession‐specific intervention, our understanding of interprofessional interventions is limited. The small number of studies included in this review, and their varied nature, limit our understanding of the key components of IPE and its effectiveness. More studies are needed to allow sound conclusions to be reached about the effectiveness of IPE, as well as to inform IPE policy development. In particular, these should include: first, studies that assess the effectiveness of IPE interventions compared to separate, profession‐specific interventions; second, RCT, CBA or ITS studies with qualitative strands examining processes relating to the IPE and practice changes; third, cost‐benefit analyses.
Summary of findings
for the main comparison.
| Interprofessional education to improve professional practices | |||
|
Patient or population: professionals or patients involved in interprofessional education intervention Settings: primarily USA and the UK Intervention: use of interprofessional education to improve collaboration and patient care Comparison: separate, profession‐specific education interventions; or no education intervention | |||
| Outcomes | Impacts | No of studies | Quality of the evidence (GRADE)* |
| Patient outcomes | The care provided by use of interprofessional education may lead to improved outcomes for patients | 6 | ⊕⊕⊖⊖ Low |
| Adherence rates | The use of interprofessional education may lead to changes in the use of guidelines or standards (e.g. adherence to clinical guidelines) among different professions | 3 | ⊕⊕⊖⊖ Low |
| Patient satisfaction | Patients may be more satisfied with care provided by professionals who have participated in an interprofessional education intervention | 2 | ⊕⊕⊖⊖ Low |
| Clinical process outcomes | Changes in clinical processes (e.g. shared decisions on surgical incisions) may be linked to the use of interprofessional education | 1 | ⊕⊕⊖⊖ Low |
| Collaborative behaviour | We are unable to assess adequately the extent to which different professions behave collaboratively in the delivery of care to patients | 3 | ⊕⊖⊖⊖ Very low |
| Error rates | We are unable to assess adequately the reduction of error due to improved interprofessional education | 1 | ⊕⊖⊖⊖ Very low |
| Practitioner competencies | We are unable to assess adequately the competencies (e.g. skills, knowledge) of professionals to work together in the delivery of care | 1 | ⊕⊖⊖⊖ Very low |
| *GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
Background
This review is an update to a previous Cochrane interprofessional education (IPE) review wherein four of the six included studies reported a range of positive outcomes (Reeves 2008). While that review was an improvement from the original Cochrane IPE review that identified no studies for inclusion (Zwarenstein 2000), it marked only a small step forward in establishing the evidence base for IPE due to the small number of studies, methodological limitations, and the heterogeneity of IPE interventions. This updated review is timely not only due to the passage of time but also given the continued interest and investment in IPE by policymakers, educators, healthcare professionals and researchers worldwide.
IPE occurs when members of more than one health or social care profession (or both) learn interactively together, for the explicit purpose of improving interprofessional collaboration or the health/well being of patients/clients (or both). The widespread advocacy and implementation of IPE reflects the premise that IPE will contribute to developing healthcare providers with the skills and knowledge needed to work in a collaborative manner (CIHC 2010; Interprofessional Educ Collab Expert Panel 2011; WHO 2010). Interprofessional collaboration, in turn, is identified as critical to the provision of effective and efficient health care, given the complexity of patients' healthcare needs and the range of health‐care providers and organisations. Interprofessional collaboration has been linked to a range of outcomes, including improvements in patient safety and case management, the optimal use of the skills of each healthcare team member and the provision of better health services (Berridge 2010; Reeves 2010; Suter 2012; Zwarenstein 2000).
Professional and academic leaders from diverse countries have developed a shared vision and strategy for postsecondary education in medicine, nursing and public health. This commission called for, among other recommendations, IPE that breaks down professional silos while promoting collaborative relationships (Frenk 2010). Similarly, the World Health Organization (WHO) published a report that outlined the role of IPE in preparing healthcare providers to enter the workplace as a member of the collaborative practice team (WHO 2010). National organisations have created core competencies for interprofessional collaborative practice, positioning IPE as fundamental to practice improvement (CIHC 2010; Interprofessional Educ Collab Expert Panel 2011).
Ideally, IPE should begin in the early training period and extend throughout a person's professional career (Barr 2005). Many examples of IPE at different stages of professional development continue to be published. From this work, it is possible to see that IPE can have an impact on learners' attitudes, knowledge and skills of collaboration (e.g. Charles Campion‐Smith 2011; Makowsky 2009; Sargeant 2011). These are important educational outcomes, but not the focus of the current review.
Given the ongoing emphasis on the importance of IPE to collaborative practice and ultimately to healthcare processes and outcomes, ongoing attention is needed to advancing the research evidence related to IPE. It is timely to undertake this updating review to identify whether there are additional studies with research designs that meet the criteria of this Cochrane review, which can further inform the evidence of IPE.
The definition of an IPE intervention used in this review is the following:
An IPE intervention occurs when members of more than one health or social care (or both) profession learn interactively together, for the explicit purpose of improving interprofessional collaboration or the health/well being (or both) of patients/clients. Interactive learning requires active learner participation, and active exchange between learners from different professions.
Objectives
The two objectives of this review are:
to assess the effectiveness of IPE interventions compared to separate, profession‐specific education interventions in which the same professions were learning separately from one another;
to assess the effectiveness of IPE interventions compared with control groups which received no education intervention.
In the first objective we are seeking to understand the effects of IPE better in relation to the current dominant uniprofessional education model, where ideally the control group should receive the same education in a uniprofessional manner. We included the second objective as there was a lack of studies addressing the first objective. Our rationale for doing so was that while studies that do not meet the first objective are not as rigorous as those that do, such studies do nevertheless have value in providing some indication of the effects of IPE.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), controlled before and after (CBA) studies and interrupted time series (ITS) studies.
Types of participants
Health and social care professionals (e.g. chiropodists/podiatrists, complementary therapists, dentists, dieticians, doctors/physicians, hygienists, psychologists, psychotherapists, midwives, nurses, pharmacists, physiotherapists, occupational therapists, radiographers, speech therapists and social workers).
Types of interventions
All types of educational, training, learning or teaching initiatives, involving more than one profession in joint, interactive learning, as described in the IPE definition above.
Types of outcome measures
1. Objectively measured or self reported (validated instrument) patient/client outcomes in the following areas: health status measures; disease incidence, duration or cure rates; mortality; complication rates; readmission rates; adherence rates; satisfaction; continuity of care; use of resources (e.g. cost‐benefit analyses). 2. Objectively measured or self reported (validated instrument) healthcare process measures (e.g. skills development, changes in practice style, interprofessional collaboration, teamwork).
Search methods for identification of studies
See: Cochrane Effective Practice and Organisation of Care Group methods used in reviews.
Effective Practice and Organisation of Care Group (EPOC) specialized register (epoc.cochrane.org/epoc‐register‐studies), July 2006 to 2 August 2011.
The search strategy from the previous IPE Cochrane review was adapted for each of the following databases searched:
MEDLINE August week 4 2006 to July week 3 2011;
CINAHL, July 2006 to 2 August 2011.
See Appendix 1 and Appendix 2 for the search strategies
No language restrictions were placed on the search strategy. We also handsearched the Journal of Interprofessional Care (2006 to 2011), proceedings from key interprofessional conferences ‐ 'All Together Better Health' (Sydney, April 2010) and 'Collaborating Across Borders' (Minneapolis, October 2007 and Halifax, May 2008) and the grey literature contained on the websites of the UK Centre for the Advancement of Interprofessional Education (date accessed: 15 September 2011) and the Canadian Interprofessional Health Collaborative (date accessed 16 September 2011). In addition, we drew on our international networks to ensure that all relevant published and unpublished work in the field would be identified. These searches generated 76 abstracts. See Figure 1.
1.
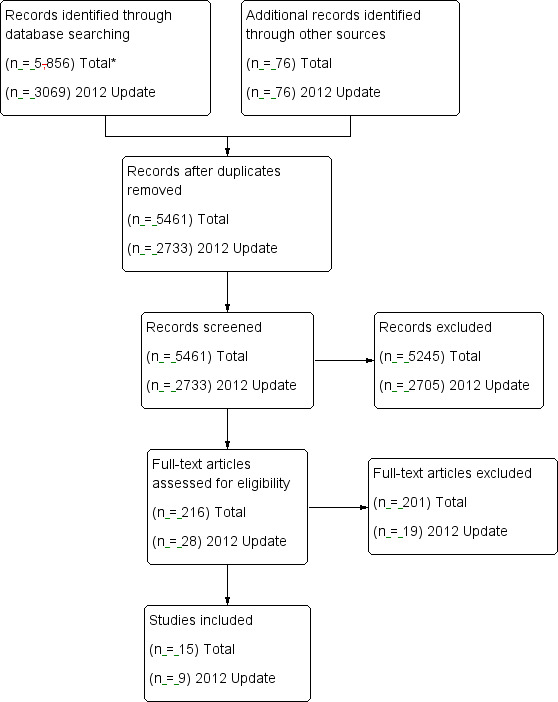
Flow diagram.
(*Total refers to sum of 1999 review and updates in 2008 and 2012).
A total of 3069 abstracts were found: 1248 from CINAHL, 285 from EPOC, 1460 from MEDLINE, 76 from handsearching and conference abstracts. After duplicates were removed, 2733 abstracts remained. While the abstract search was sensitive to identifying a high proportion of relevant IPE intervention studies, it exhibited low specificity in relation to differentiating between IPE interventions and other interprofessional teamwork interventions without IPE components, such as continuous quality improvement and total quality improvement initiatives. See Figure 1 for further information.
Data collection and analysis
Three review authors (SR, LP and JG) independently reviewed the 2733 abstracts retrieved by the searches to identify all those that suggested that:
there was an intervention where interprofessional exchange occurred;
education took place;
professional practice, patient care processes or health or patient satisfaction outcomes were reported;
the intervention was evaluated using an RCT, CBA or ITS design.
Twenty‐eight studies were identified from this abstract search as potentially meeting these criteria. The full text of these articles was obtained. These three review authors independently assessed each full‐text article to examine whether it met all of the criteria further. Any disagreements and uncertainties were resolved by discussion, and the input of a fourth review author (MZ), who reviewed all of the final papers as a further quality check for inclusion in the review. Nine studies met the outlined criteria; these nine studies were added to the six studies from the previous review for a total of 15 studies.
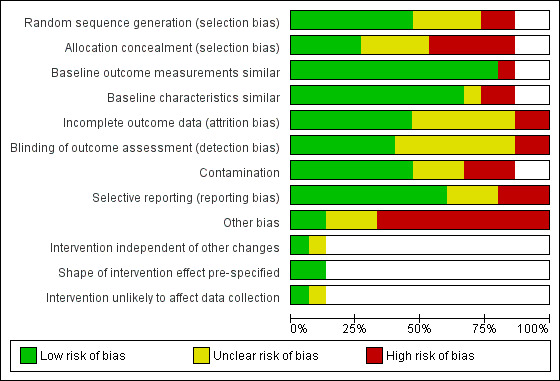
Assessment of the risk of bias in included studies
Two review authors (SR and LP) assessed the risk of bias for each study using a form with the standard criteria described in EPOC (2002). The 'Risk of bias' assessments are displayed in Figure 2 and Figure 3. The 'Risk of bias' summary is in Figure 4.
2.
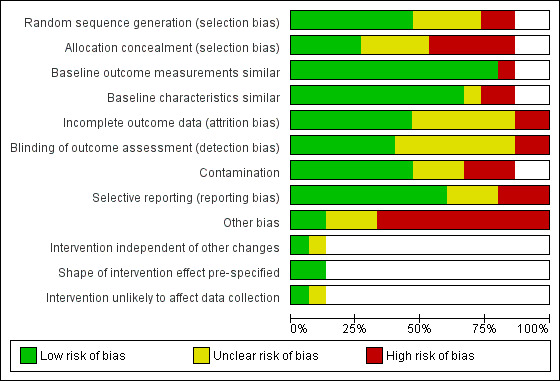
3.
4.
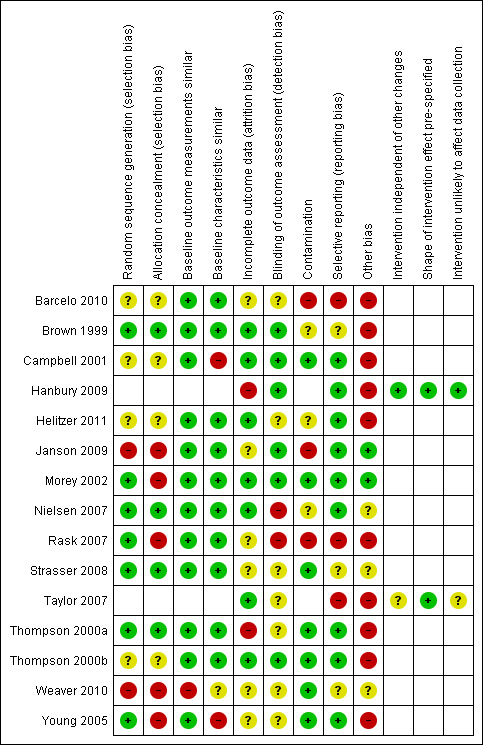
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
We did not exclude studies on the grounds of risk of bias, but sources of bias are reported when presenting the results of studies.
Data extraction
Three review authors (SR, LP and JG) extracted the following information from included studies:
type of study (RCT, CBA, ITS);
study setting (country, healthcare setting);
types of study participants;
description of education programme;
description of any other interventions in addition to the education;
main outcome measures;
results for the main outcome measures;
any additional information that potentially affected the results.
Analysis
Ideally, a meta‐analysis of study outcomes would have been conducted for this review. However, this was not possible due to heterogeneity of study designs, interventions and outcome measures among the small number of included studies (n = 15). Consequently, the results are presented in a narrative format.
Results
Description of studies
All 15 studies addressed objective number two – to assess the effectiveness of IPE interventions compared with control groups that received no education intervention. Given the major differences between the included studies, a description of each is provided below. A formal calculation of the evidence, including the creation of a 'Summary of findings' table, was not feasible given the lack of overlap among the outcomes reported. The included studies are presented in three sections according to the type of research design they employed.
Randomised controlled trials
Barcelo 2010 described an RCT that aimed to improve the quality of diabetes care in primary healthcare centres using the chronic care model. Forty‐three primary care teams based in 10 public health centres participated in this study. Teams were made up mainly of physicians and nurses with other professionals, such as nutritionists and psychologists also participating in some teams. All 10 health centres implemented a clinical information system and provided the opportunity for patients to participate in peer support groups. Beyond this, five health centres were randomly assigned to receive the intervention, and five received no intervention. The intervention consisted of a multifaceted quality improvement initiative during which teams and patients participated in three interprofessional learning sessions within a period of 18 months. These included a structured patient diabetes education programme, training in foot care and in‐service training. In each of the three learning sessions, the teams selected specific objectives for 'plan‐do‐study‐act' (PDSA) improvement cycles. The objectives were based on problems identified in the practice of each health centre (e.g. organisation of care, decision support, information sharing). Other aspects of the multifaceted quality improvement programme included support from hospital specialists and a case management advisor. Reported outcome measures included clinical observations (e.g. metabolic control and cholesterol) and adherence to clinical protocols (e.g. conducting periodic foot and eye examinations). The authors reported that multilevel logistic regression models were adjusted for the clustering of participants within health centres.
Brown 1999 undertook an RCT that aimed to examine whether an interprofessional communication skills training programme for physicians, physician assistants, nurse practitioners and optometrists increased participants' ratings of clinicians' communication skills. The healthcare professionals worked for a 'not for profit' group‐model health maintenance organisation (HMO) in the US. The IPE intervention, led by two physicians, consisted of two four‐hour workshops delivered one month apart with two hours of homework and a telephone call from an instructor inbetween. The intervention involved didactic components, role playing and interactive dialogue. Of the 69 participants (75% of whom were physicians), 37 were randomly assigned to receive the intervention and 32 were assigned to the control group (which received the IPE intervention after the study). Pre‐ and post‐intervention patient satisfaction scores were drawn from routine data collection, which yielded clinician‐specific patient satisfaction ratings every six months. The HMO contracted out the routine data collection. The contractor randomly sampled clinical consultations and mailed a questionnaire to the relevant participants within 10 days of each consultation in the sample.
Campbell 2001 described an RCT that evaluated an interprofessional training programme for emergency department (ED) physicians, nurses, social workers, hospital administrators and representatives from local domestic violence service organisations. The intervention aimed to increase the identification of acutely abused women in EDs, and improve staff and institutional responses. The two‐day programme, developed and implemented by violence prevention organisations, involved didactic instruction, role play, team planning and team work to develop a written action plan. Participants from each ED were asked to meet before and after the training. The programme addressed systems change and coalition building as well as provider attitudes and skill building. The attendees were expected to collaborate in order to implement system changes in their respective EDs, including implementing training for ED staff. The instructors were available for telephone assistance during the implementation phase. Six EDs were randomly assigned to receive either the IPE intervention (three hospitals) or to be in a control group that received no intervention (three hospitals). Follow‐up data were collected at nine to 12 months and 18 to 24 months.
Helitzer 2011 reported an RCT that evaluated the effects of an intervention aimed at improving patient‐centred communication skills and proficiency in discussing patients' health risks. Twenty‐six primary care professionals (physicians, physician assistants and nurse practitioners) based in a single academic setting participated in the intervention. A total of 12 professionals were allocated to the intervention group and 14 to the control group. The intervention consisted of training focused on patient‐centred communication about behavioural risk factors and included a full day of IPE, individualised feedback on video‐taped interactions with simulated patients, and optional workshops to reinforce strategies for engaging the patient. Data were gathered from patients on professionals' patient‐centred communication behaviour during two clinic visits that were held at six and 18 months following the intervention.
Nielsen 2007 described a cluster RCT study to evaluate the effectiveness of a teamwork training intervention in reducing adverse outcomes and improving the process of care in hospital labour and delivery units. Fifteen hospitals took part in this study, seven as intervention sites and eight as control sites. Participants included labour and delivery room personnel from obstetrics, anaesthesiology and nursing (n = 1307). The intervention consisted of a three‐day instructor training session comprising four hours of didactic lessons, video scenarios and interactive training covering team structure and processes, planning and problem solving, communication, workload management and team skills. The intervention also included assistance with creation and structure of interprofessional teams at each intervention site, which entailed facilitators conducting onsite training sessions to structure each unit into core interprofessional teams. In addition, a contingency team, a group of physicians and nurses drawn from practitioners that were on call during a 24‐hour period, were trained to respond in a co‐ordinated way to obstetric emergencies. Data were gathered on adverse maternal or neonatal outcomes as well as clinical process data from 28,536 deliveries.
Strasser 2008 described a cluster RCT aimed at evaluating the effects of an IPE intervention on team functioning in stroke rehabilitation units. A total of 227 staff on 14 intervention teams and 237 clinical staff on 15 control teams participated in this study. All teams had representatives from medicine, nursing, occupational therapy, speech‐language pathology, physiotherapy and social work. The team training intervention consisted of a multi‐phase IPE programme delivered over six months, including: an interactive workshop emphasising team dynamics, problem solving, the use of performance feedback data and the creation of action plans for process improvement. The intervention also included follow‐up telephone and video‐conference consultations. Patient outcomes data (functional improvement, community discharge, length of stay) were gathered from 579 stroke patients treated by these teams before and after the intervention.
Thompson 2000a described a group RCT aimed at evaluating the effectiveness of IPE and a clinical practice guideline aimed at improving the recognition and improvement of depression in primary care practices. A primary care physician, practice nurse and community mental health nurse delivered the four‐hour IPE seminars to general practitioners and practice nurses in groups of two or three practices when convenient. Teaching was supplemented by video‐tape recordings, small‐group discussion of cases and role play. The educators were available for nine months after the seminars to facilitate guideline implementation and promote use of teamwork. Fifty‐nine primary care practices were assigned to the intervention group (29 practices) or control group (30 practices). Practices in the control group received the IPE intervention after the study had been completed. Data were collected six weeks and six months after patient visits.
Thompson 2000b undertook a cluster RCT to examine the effectiveness of a one‐year intervention linked to improving identification of domestic violence and the collaborative management of primary care clinics. The intervention for teams of physicians, nurse practitioners, physician assistants, registered nurses, practical nurses and medical assistants, consisted of two half‐day IPE sessions, a bimonthly newsletter, clinic educational rounds, system support (posters, cue cards, questionnaires) and feedback of results. Five primary care clinics were randomly assigned to receive the intervention (two clinics) or to the control group (three clinics). Data were collected at baseline, nine to 10 months, and 21 to 23 months.
Controlled before and after studies
Janson 2009 reported a CBA study aimed at improving the care and outcomes of people with type 2 diabetes by improving the care delivered by interprofessional teams. Participants consisted of interprofessional teams of 120 learners (56 second/third‐year medicine residents, 29 second‐year nurse practitioner students and 35 fourth‐year pharmacy students) who delivered team‐based diabetes care to 221 people. The control group consisted of 28 traditional‐track internal medicine residents who provided usual care to 163 people. The study was undertaken in two general medicine clinics. The intervention involved weekly didactic presentations, clinical discussions and clinic visits with participants. A quality improvement approach was offered by planning and implementing projects using the plan‐do‐study‐act model. The intervention group also received quarterly patient panel reports on process of care benchmarks and clinical status markers.
Morey 2002 presented a CBA study to evaluate the effectiveness of a programme aimed at improving collaborative behaviour of hospital ED staff (physicians, nurses, technicians and clerks). The intervention consisted of an emergency team co‐ordination education course as well as implementation of formal teamwork structures and processes. A physician‐nurse pair from each ED was involved in developing and implementing the curriculum. The course consisted of eight hours of instruction in one day. The format was lectures, discussion of behaviours, practical exercises and discussion of video‐segments. Teamwork implementation involved forming teams by shift and delivering care in a team structure. Each staff member completed a four‐hour practicum in which teamwork behaviours were practised and critiqued by an instructor. Staff supported the adoption of collaborative behaviour during normal shifts. This teamwork implementation phase lasted six months. Nine hospital EDs self selected to receive either the IPE intervention (six EDs, 684 clinicians) or act as a control (three EDs, 374 clinicians). Control group departments received the intervention at a later date. Data were collected at two four‐month intervals following the training.
Rask 2007 presented a CBA study that aimed to evaluate an interprofessional fall management quality improvement project in nursing homes. Participants consisted of 19 interprofessional falls teams (made up of a nurse, physiotherapist or occupational therapist, certified nursing assistants, a member of maintenance staff). The control group comprised 23 falls teams. The intervention consisted of a full‐day interprofessional workshop and a second workshop approximately one month later to address arising challenges. Organisational interventions were also provided in the form of seeking leadership buy‐in and support, providing a designated facility‐based falls co‐ordinator, and ongoing consultation and oversight by advanced practice nurses with expertise in falls management. Data were gathered on process of care documentation, trends in fall rates and changes in physical restraint use.
Weaver 2010 described a CBA study that evaluated an intervention aimed at improving teamwork for operating room staff based at two community‐based hospitals. In total, 55 professionals participated in the intervention: 29 in the intervention group (three surgeons, nine nurses, three surgical technicians, 12 anaesthesiologists, two physician assistants); and 26 in the control group (two surgeons, 18 nurses, three surgical technicians, three anaesthesiologists). The intervention consisted of one four‐hour session that included didactic presentations and interactive role‐playing activities between participants aimed at improving their knowledge and skills of teamwork and collaboration. Data were gathered by observed changes in collaborative behaviour (frequency of team briefings in which information was shared among team members and patient care was planned).
Young 2005 presented a CBA study that evaluated effects of a consumer‐led innovation aimed at improving the competence of mental health practitioners working in community mental health provider organisations. The practitioner intervention for psychiatrists, nurses, therapists, case managers, residential staff, mental health workers, and administrative support involved six educational components held over a one‐year period that included presentations, discussions, small groups and role‐playing techniques, as well as three or four full‐day follow‐up visits to sites. An additional 16 hours was also spent with staff at the sites. The intervention was developed and delivered by two people who were consumers of mental health services. The innovation also involved a consumer‐focused intervention. The study was conducted at five organisations in two states; one organisation in each state received the intervention (total of 269 mental health practitioners, 151 in intervention groups and 118 in control groups). Data were collected at baseline and one year.
Time interrupted series studies
Hanbury 2009 described an ITS study that aimed to test the effectiveness of a theory of planned behaviour intervention to increase community mental health professionals' adherence to a national suicide prevention guideline. The intervention was delivered to 49 participants. The intervention comprised three components designed to target normative beliefs. First, a presentation that contained factual statements, statistics and graphs taken from key government publications highlighting and supporting the guideline evidence base. Second, an interprofessional group discussion was facilitated to ensure that positive normative beliefs were emphasised and any negative normative beliefs challenged. Third, interprofessional group work based on two real life vignettes was undertaken by participants. Data in the form of aggregated, monthly audit adherence data were collected for nearly four years (28 months before the intervention and 18 months afterwards) to evaluate patterns of adherence to using the national suicide prevention guideline. Data from a control site was also included to evaluate the level of adherence.
Taylor 2007 presented an ITS study that assessed the effects an intervention designed to improve the delivery of standard diabetes services and patient care. Professionals based in a single primary care clinic participated in the study. An eight‐hour intervention was delivered to participants. The intervention consisted of a range of interactive activities (task redistribution, standardised communication methods and decision‐support tool development) that aimed to improve interprofessional communication, teamwork, workflow organisation and information exchange in order to enhance the care of 619 people with diabetes. Data were collected from medical records. Using 1805 clinic visits completed during the study period (160 pre‐intervention clinic days and 122 post‐intervention clinic days), diabetic services and associated patient outcomes were evaluated for adherence to the American Diabetes Association periodicity recommendations and treatment targets: quarterly blood sugar; quarterly blood pressure; annual low‐density lipoprotein; annual urine microalbumin; and annual lower extremity amputation prevention check.
Risk of bias in included studies
The risk of bias in studies was variable. Data are presented for RCTs and CBA studies (Figure 2), and separately for ITS studies (Figure 3).
All studies
For the eight studies that were RCTs, four met five of the nine EPOC 'Risk of bias' criteria (Brown 1999; Nielsen 2007; Thompson 2000a; Thompson 2000b). Three of the five CBA studies met five of the nine EPOC 'Risk of bias' criteria (Janson 2009; Morey 2002; Young 2005). The EPOC 'Risk of bias' criteria have seven elements for ITS studies and one of the two studies met four of the seven EPOC 'Risk of bias' criteria (Hanbury 2009).
Randomised controlled trials
Four of the eight RCTs reported adequately protecting against contamination (Campbell 2001; Strasser 2008; Thompson 2000a; Thompson 2000b). All of the RCTS demonstrated adequate similar baseline outcome measurements. Only one study was inadequate with regards to baseline characteristics being similar (Campbell 2001). Inadequate allocation concealment was an issue in four of the RCTs, with studies either failing to conceal allocation or not making this clear (Barcelo 2010; Campbell 2001; Helitzer 2011; Thompson 2000b). The same four RCTs were unclear or failed in their reporting of adequate sequence generation (Barcelo 2010; Campbell 2001; Helitzer 2011; Thompson 2000b). Four RCTs were unclear or inadequate with regards to the adequacy of blinding in the assessment of outcomes (Barcelo 2010; Helitzer 2011; Nielsen 2007; Strasser 2008). Three RCTs were unclear or had evidence of selective outcome reporting (Barcelo 2010; Brown 1999; Thompson 2000a). All RCTs had evidence of other bias.
Controlled before and after studies
Allocation concealment was an issue for all CBA studies. Four of the CBA studies did not address incomplete outcome data (Janson 2009; Rask 2007; Weaver 2010; Young 2005). Two of the studies did not demonstrate adequate sequence generation (Janson 2009; Weaver 2010); or selective outcome reporting and adequate blinding (Rask 2007; Weaver 2010). All CBA studies ensured baseline outcome measurements were similar with the exception of one (Weaver 2010). Two studies did not report similar baseline characteristics (Weaver 2010; Young 2005); or that the study was adequately protected against contamination (Rask 2007; Weaver 2010). Only two studies were free of other bias (Janson 2009; Morey 2002) (see Figure 2).
Interrupted time series studies
Both ITS studies were adequate for pre‐specifying the shape of the intervention effect and for the intervention to be unlikely to affect data collection. Taylor 2007 was unclear in their reporting of whether the intervention was independent of other changes, and were inadequate with regards to selective outcome reporting. Hanbury 2009 did not address all incomplete outcome data. Both ITS studies were not free of other bias (see Figure 3).
Effects of interventions
See: Table 1
Effects of IPE interventions reported in each of the studies are presented by the research design each employed.
Randomised controlled trials
The results of the study by Barcelo 2010 indicated that the proportion of people with good glycaemic control (glycosylated haemoglobin (HbA1c) < 7% (53 mmol/mol)) among those in the intervention group increased from 28% to 39% after the intervention (p value < 0.05). The proportion of people achieving three or more quality improvement goals increased from 16.6% to 69.7% (p value < 0.001) among the intervention group while the control group experienced a non‐significant decrease from 12.4% to 5.9% (p value = 0.118).
In the study by Brown 1999, the communication skills training programme did not improve patient satisfaction scores. Based on an average of 81 responses for each of the 69 participating clinicians, there was no significant difference in the mean satisfaction scores for the intervention and control groups: each group showed a very small increase in mean scores on 9‐point scales (intervention group 0.03 points and control group 0.05).
The results in Campbell 2001 study indicated that the EDs that received the intervention to improve responses to acutely abused women recorded significantly higher levels on all components of the "culture of the emergency department" system‐change indicator (e.g. appropriate protocols; materials such as posters, brochures, medical record intervention checklists and referral information available to staff; and staff training) (F = 5.72, p value = 0.04) and higher levels of patient satisfaction (F = 15.43, p value < 0.001) than the EDs in the control group.
Helitzer 2011 reported that the intervention generated significant and persistent changes in patient‐centred communication in the intervention group. After six months, a significant difference was found in scores for patient‐centredness, which favoured the intervention group (F(1, 20.59) = 8.43, p value < 0.01). After 18 months, the intervention group's significantly higher patient‐centredness scores were sustained (F(1, 17.16) = 5.48, p value = 0..032).
Nielsen 2007 found overall no statistically significant differences between the intervention and control groups. Data on adverse outcome prevalence were similar in the control and intervention groups, both at baseline and after implementation of teamwork training (9.4% versus 9.0% and 7.2% versus 8.3%, respectively). However, the time from the decision to the incision for an immediate caesarean delivery was significantly shorter in the intervention group (p value = 0.03). In addition, one process measure, the time from the decision to perform an immediate caesarean delivery to the incision, differed significantly after team training (33.3 minutes versus 21.2 minutes, p value = 0.03).
Strasser 2008 reported a significant difference in improvement in motor score between the intervention group and the control group (13.6% of people in the intervention gained more than 23 points, p value = 0.038). There was no significant difference for the other two outcome measures (p value = 0.1) for both. The proportion of people who had had a stroke making greater than the median functional gain increased by 4.4% in the intervention group, whereas it decreased by 9.2% in the control group, lending further support to the effect of the intervention. At the same time, the intervention had no measurable effect on participants' length of stay.
Thompson 2000a reported no differences between the intervention and control groups in relation to the recognition of depressive symptoms in their evaluation of the effectiveness of an IPE and clinical practice guideline intervention. The outcome for people diagnosed with depression did not significantly improve at six weeks or six months after the intervention.
Thompson 2000b reported that following the intervention, documentation of domestic violence incidents increased by 14.3%. It is also stated that there was a 3.9‐fold relative increase of documentation at nine months in intervention clinics compared to the control sites. Overall case finding increased by 30%, but this was not statistically significant. Recorded quality of domestic violence patient assistance did not change.
Controlled before and after studies
Janson 2009 reported that, at study completion, intervention group participants more frequently received assessments of HbA1c (79% versus 67%; p value = 0.01), low‐density‐lipoprotein cholesterol (69% versus 55%; p value = 0..009), blood pressure (86% versus 79%; p value = 0.08), microalbuminuria (40% versus 30%; p value = 0.05), smoking status (43% versus 31%; p value = 0.02), and foot examinations (38% versus 20%; p value = 0.0005). It was also reported that intervention group participants had more planned general medicine visits (7.9 = 6.2 versus 6.2 = 5.7; p value = 0.006) than did control group participants.
The results of Morey 2002 evaluation of the effectiveness of an interprofessional teamwork training programme on collaborative behaviour in EDs, showed a statistically significant improvement in quality of observed team behaviours between the intervention and control groups following training (p value = 0.012). The clinical error rate significantly decreased from 30.9% to 4.4% in the intervention group (p value = 0.039).
Rask 2007 reported that several key areas of documentation regarding assessment and management of fall risk factors improved. All except two were statistically significant for the intervention teams. Fall rates were not significantly different for the intervention nursing homes (p value = 0.92) and were significantly positive (p value = 0.008) for the control sites. Restraint use decreased substantially during the project period, from 7.9% to 4.4% in the intervention nursing homes (a relative reduction of 44%) and from 7.0% to 4.9% at the control sites (a relative reduction of 30%).
Weaver 2010 reported that intervention participants engaged in significantly more team pre‐case briefings after attending training (F [1, 147] = 35.01, p value < 0.001). There was also a significant increase in the proportion of information sharing (e.g. intervention team members were more willing to speak up and participate during briefings) (F [1,128] = 11.47, p value < 0.001). This pattern was also present in the frequency of care plan discussions (F [1,145] = 5.00, p value < 0.05).
Young 2005 reported that in comparison to mental health practitioners in the control group, practitioners in the intervention group reported significantly higher scores in relation to the following competencies: teamwork (r = 0.28, p value = 0.003); holistic approaches (r = 0.17, p value = 0.06); education about care (r = 0.22, p value = 0.03); rehabilitation methods (r = 0.25, p value = 0.007) and overall competency (r = 0.21, p value = 0.02).
Time interrupted series studies
Hanbury 2009 reported that the intervention did not significantly increase adherence to the national guideline. Multiple regression was used to calculate the proportion of variance in intention accounted for by the predictors, and identify the most significant predictor. The intervention was found to account for 58% of the variance (adjusted R2 = 0.58) in intention to adhere to the guideline, a statistically significant finding (F = 23.586, 3 degrees of freedom (df), p value = 0.0001).
Taylor 2007 found that the intervention achieved improvements in microalbumin testing (+7.40%, p value = 0.001) and HbA1c testing (+3.80%, p value = 0.029). A significant increase in microalbumin levels that were at target (+3.87%, p value = 0.018), and a significant decrease in HbA1c levels that were also at target (–3.81%, p value = 0.011). It is unclear in the reporting if the intervention is independent of other changes. In addition, outcomes were not assessed blindly.
Discussion
In total, this review included 15 studies, locating nine new studies, which were added to the six studies from the previous update (Reeves 2008). This small growth of eligible studies marks continued development of the IPE field, as the first IPE review found no eligible studies (Zwarenstein 2000).
Seven of the studies reported positive outcomes in the following areas: improvements in diabetes clinical outcomes and healthcare quality improvement goals (Barcelo 2010); improvements in patient‐centred communication (Helitzer 2011); improved clinical outcomes for people with diabetes (Janson 2009); collaborative team behaviour and reduction of clinical error rates for ED teams (Morey 2002); increased rates of diabetes testing and improved patient outcomes (Taylor 2007); improved mental health practitioner competencies related to the delivery of patient care (Young 2005); and improved team behaviours and information sharing for operating room teams (Weaver 2010). Three of the studies also reported that the gains attributed to IPE were sustained over time: eight months (Morey 2002) and 18 months (Barcelo 2010; Helitzer 2011).
In addition, four studies (Campbell 2001; Rask 2007; Strasser 2008; Thompson 2000b) reported a mixed set of outcomes. As well as reporting positive outcomes in relation to changes in professional practice and patient satisfaction, Campbell 2001 found no differences in the identification rates of victims of domestic violence between their intervention and control groups. While Rask 2007 reported improvements in care documentation and decreases in the use of restraint for people in nursing homes, they found no change in fall rates. Despite reporting functional gains for patients, Strasser 2008 also reported no significant difference in length of stay or rates of community discharge for stroke rehabilitation patients. Thompson 2000b found that documented asking about domestic violence significantly increased, yet the increase in case finding was not significant.
Four studies reported that the IPE interventions had no impact on either healthcare processes or patient health care or outcomes: Brown 1999 found no significant difference in the improvement of routinely collected patient satisfaction scores between intervention and control groups; Hanbury 2009 reported that the intervention did not significantly increase adherence among participants; Nielsen 2007 reported no statistically significant differences between the intervention and control groups; and Thompson 2000a reported that there were no differences between the intervention and control groups in relation to the recognition or treatment of patients with depression.
Although overall the results indicate some positive outcomes related to IPE, its effectiveness remains unclear at this time due to the heterogeneity among the 15 studies as well as their methodological limitations, as outlined above. The studies were heterogeneous in relation to the objectives and format of the educational intervention, the existence of other interventions in addition to the education, and the clinical areas and settings. The IPE component in these studies ranged from a few hours, to a few days, to longitudinal programmes that were delivered over one year or more. The professional mix of participants also varied from surgeons, nurses, surgical technicians, anaesthesiologists and physician assistants (Weaver 2010), to nurses, physiotherapists, occupational therapists, nursing assistants and maintenance staff (Rask 2007). The aims of the interventions also varied. For example in studies by Brown 1999 and Helitzer 2011, the emphasis was on communication between clinicians and participants, whereas other studies explicitly focused on interprofessional team work in the context of particular settings (ED, operation room) (e.g. Morey 2002; Weaver 2010).
Despite three studies sharing a focus on improving diabetes care (Barcelo 2010; Janson 2009; Taylor 2007), each employed a different research design: an RCT (Barcelo 2010), a CBA (Janson 2009) and an ITS (Taylor 2007). The interventions were different: from a single eight‐hour IPE session (Barcelo 2010), to three workshops (Taylor 2007), to weekly seminars (Janson 2009). The participants also varied, from physicians, nurses, nutritionists and psychologists based at 10 public health centres (Barcelo 2010), to 120 students (medical residents, senior nurse practitioner and pharmacy students) (Janson 2009), to an existing team of professionals (who were not identified) based in a single clinic (Taylor 2007). These few examples are some indication of the degrees of heterogeneity and why it is difficult to summarise and identify key elements of successful IPE.
Eight of the studies (Barcelo 2010; Campbell 2001; Janson 2009; Morey 2002; Nielsen 2007; Rask 2007; Thompson 2000b; Young 2005) contained multi‐faceted interventions, of which the IPE was only one component. The other interventions included team restructuring, tools such as posters and questionnaires, measurement and feedback, and consumer‐directed interventions. In these studies, the authors commented on the importance of system change and the time and resources required to facilitate it (Campbell 2001), the need for leaders who support teamwork within organisations (Morey 2002; Rask 2007) and the use of quality improvement projects (Barcelo 2010; Janson 2009).
Methodologically, the studies shared a common key limitation. All comparative studies (RCTs and CBAs, n = 13) compared the effects of the IPE interventions with control groups that received no educational intervention. As a result, it is difficult to assess the effects of the IPE. Furthermore, most of the included studies involved small samples (defined as fewer than 100 individually randomised practitioners or fewer than 20 randomised clusters), which limited their ability to provide a convincing level of generalisable evidence for the effects of the IPE interventions.
It is also worth noting that there was little evidence of preliminary studies to optimise the IPE interventions and evaluation strategies. IPE interventions are complex, multifaceted interventions in which the components may act both independently and interdependently. Guidance on the development and testing of complex interventions stresses the importance of stepwise work to understand the context for the intervention fully, and optimise the design and implementation of the intervention and evaluation before proceeding to a trial (Craig 2008).
When planning future trials of IPE, thought should be given to the following dimensions: better randomisation procedures, allocation concealment, larger sample sizes and more appropriate control groups. Importantly, studies should include at least one common outcome for measurement of teamwork to enable a formal weighing up of the evidence; in addition, the remainder of the outcomes should include a clear patient health outcome rather than only process measures. Given that IPE is delivered by two or more providers, future trials should have cluster randomised designs, and researchers are advised to be thoughtful about their unit of analysis. In addition, given a lack of evidence on the impact of IPE on resources (e.g. costs and benefits), attention is needed in this area.
While uniprofessional education remains the dominant model for delivering education for health and social care professionals, IPE is increasingly becoming common. Advocacy and implementation of IPE reflects the premise that IPE will contribute to developing healthcare providers with the skills and knowledge needed to work in a collaborative manner (Barr 2005; CIHC 2010; Interprofessional Educ Collab Expert Panel 2011; WHO 2010). Interprofessional collaboration, in turn, is identified as critical to the provision of effective and efficient health care, given the complexity of patients' healthcare needs and the range of healthcare providers and organisations. In relation to implementing IPE at differing stages of the professional development continuum, it is worth remembering that pre‐qualification IPE can be regarded as an investment in the future and, in general, studies with short periods of follow‐up would not be expected to detect effects on patient outcomes or healthcare processes, which would be difficult to pinpoint, due to a wide variety of potentially confounding variables. Measuring patient outcomes or care process outcomes arising from IPE after qualification (e.g. during continuing professional development and quality improvement initiatives) is more feasible. But it still presents methodological challenges, particularly identifying the influence of IPE within multifaceted interventions and, further, identifying key attributes of effective IPE.
Although this review located nine new IPE studies (which were added to the six studies from the last update) their heterogeneity limits the conclusions we can draw from this work. Nevertheless, a continued increase in eligible studies represents a further positive step forward in establishing a robust evidence base for the effects of IPE on professional practice and healthcare outcomes.
Authors' conclusions
Implications for practice.
Our first IPE review published in 1999 found no eligible studies, our 2008 update located six studies, and this update located a further nine studies. At 15 eligible studies, this demonstrates that the IPE field is growing steadily in terms of publishing rigorous IPE research (those employing RCTs, CBA or ITS designs). Although these studies reported a range of positive outcomes, the heterogeneity of IPE interventions means it is not possible to draw generalisable inferences for the effects of IPE. Despite marking a step forward in beginning to establish an evidence base for IPE, more rigorous IPE research (those employing RCTs, CBA or ITS designs) is needed to demonstrate evidence of the impact of this type of intervention on professional practice or healthcare outcomes, or both.
Implications for research.
Despite a growth of IPE studies in the past few years, most of this research does not employ rigorous designs. Future RCTs explicitly focused on IPE with rigorous randomisation procedures and allocation concealment, larger sample sizes and more appropriate control groups would improve the evidence base of IPE. A focus on understanding the use of IPE in relation to resources is also needed. These studies should also include data collection strategies that provide insight into how IPE affects changes in healthcare processes and patient outcomes as research to date has not sufficiently addressed this critical issue.
To improve the quality of evidence relating to IPE and patient outcomes or healthcare process outcomes, the following three gaps will need to be filled: studies that assess the effectiveness of IPE interventions compared to separate, profession‐specific interventions; RCT, CBA or ITS studies with qualitative strands examining processes relating to the IPE and practice changes; and cost‐benefit analyses.
What’s new
We completed a substantive update of review from 2008 to 2011. Nine new studies were found and added to the six studies located from the previous update.
Feedback
Lack of Evidence
Summary
Received 20/04/2003 13:47:02
I am assuming this excellent work is a follow up from earlier published material from 1999 (J. Int. Care 13 (4)417‐4). What I cannot understand is why, therefore is IPE still 'flavour of the month'? We wouldn't push ideas forward without adequate evidence of effectiveness first! Isn't anyone else out there brave enough to concur with the authors? I certify that I have no affiliations with or involvement in any organisation or entity with a direct financial interest in the subject matter of my criticisms.
Reply
Thank you for your positive comment. The article to which you refer is indeed a print version of this Cochrane review, and we will note that in the review. We would like to stress that the 'absence of evidence of effect is not evidence of absence of effect' (Cochrane Reviewers' Handbook 4.1.5, section 9.7). We therefore suggest that interprofessional education (IPE) interventions ought to be implemented widely, but ONLY in the context of rigorous evaluations, ideally randomised controlled trials of their effects. This is not as difficult as it might at first seem, and we would encourage those who are interested enough in IPE to want to subject it to reliable test to contact us or other groups of researchers with randomised controlled trial experience for advice and help.
Merrick Zwarenstein [on behalf of the reviewers.]
The most recent update to this review is published in Issue 1, 2008. The update now has 6 studies. However, it still remains very difficult to draw conclusions about the effectiveness of this intervention and we continue to require further research in the area.
Alain Mayhew [on behalf of the authors and the editorial staff and team]
Contributors
Jane Warner, Practice Nurse
What's new
| Date | Event | Description |
|---|---|---|
| 24 July 2018 | Amended | Contact person/author Scott Reeves deceased May 2018. Contact person role reassigned to Merrick Zwarenstein |
History
Protocol first published: Issue 3, 2000 Review first published: Issue 1, 2001
| Date | Event | Description |
|---|---|---|
| 28 February 2013 | New search has been performed | Substantive amendment, search up to Aug 2011, nine additonal studies |
| 28 February 2013 | New citation required but conclusions have not changed | Nine new studies, but no change in conclusions |
| 29 July 2008 | Amended | Converted to new review format. |
| 12 November 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Amber Fitzsimmons, doctoral student at University of California, San Francisco, for her help with preliminary abstraction notes of some of the included studies.
Appendices
Appendix 1. MEDLINE search strategy
MEDLINE search strategy 1 (interprofession$ or inter‐profession$).tw.
2 (interdisciplin$ or inter‐disciplin$).tw.
3 (interoccupation$ or inter‐occupation$).tw.
4 (interinstitut$ or inter‐institut$).tw.
5 (interagen$ or inter‐agen$).tw.
6 (intersector$ or inter‐sector$).tw.
7 (interdepartment$ or inter‐department$).tw.
8 (interorgani?ation$ or inter‐organi?ation$).tw.
9 interprofessional relations/
10 team$.tw.
11 (multiprofession$ or multi‐profession$).tw.
12 (multidisciplin$ or multi‐disciplin$).tw.
13 (multiinstitution$ or multi‐institution$).tw.
14 (multioccupation$ or multi‐occupation$).tw.
15 (multiagenc$ or multi‐agenc$).tw.
16 (multisector$ or multi‐sector$).tw.
17 (multiorgani?ation$ or multi‐organi?ation$).tw.
18 exp professional‐patient relations/
19 (transprofession$ or trans‐profession$).tw.
20 (transdisciplin$ or trans‐disciplin$).tw
21 or/1‐20
22 (education$ or train$ or learn$ or teach$ or course$).tw.
23 exp education, continuing/
24 exp education, graduate/
25 or/22‐24
26 21 and 25
27 program evaluation/
28 "health care outcome?".tw.
29 (education$ adj outcome?).tw.
30 or/27‐29
31 26 and 30
Appendix 2. CINAHL search strategy
CINAHL search strategy
(TX interprofession*) or (TX inter‐profession*) or (TX interdisciplin*) or (TX inter‐disciplin*) or (TX interoccupation*) or (TX inter‐occupation*) or (TX interinstitut*) or (TX inter‐institut*) or (TX interagen*) or (TX inter‐agen*) or (TX intersector*) or (TX inter‐sector*) or (TX interdepartment*) or (TX inter‐department*) or (TX interorgani?ation*) or (TX inter‐organi?ation*) or (MH interprofessional relations) or (TX team*) or (TX multiprofession*) or (TX multi‐profession*) or (TX multidisciplin*) or (TX multi‐disciplin*) or (TX multiinstitution*) or (TX multi‐institution*) or (TX multioccupation*) or (TX multi‐occupation*) or (TX multiagenc*) or (TX multi‐agenc*) or (TX multisector*) or (TX multi‐sector*) or (TX multiorgani?ation*) or (TX multi‐organi?ation*) or (MH "Professional‐Patient Relations+") or (TX transprofession*) or (TX trans‐profession*) or (TX transdisciplin*) or (TX trans‐disciplin*) AND (TX education*) or (TX train*) or (TX learn*) or (TX teach*) or (TX course*) or (MH "education, continuing+") or (MH "education, graduate+") AND (MH "student performance appraisal+") or (MH "course evaluation") or (MH "program evaluation") or (MH "evaluation research+") or (MH "health care outcome*") or (education* N1 outcome*)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barcelo 2010.
| Methods | RCT where teams based in 10 public health centers were randomised to intervention project to improve the quality of diabetes care (n = 5) or control group (n = 5) | |
| Participants | Physicians, nurses, patients, nutritionists and psychologists | |
| Interventions | The intervention group received learning sessions focused on the implementation of strategies to improve quality of diabetes care | |
| Outcomes | Clinical outcomes, healthcare process quality improvement goals | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Describes that health centres were " randomly selected" (p. 146) but random component in the sequence generation process is not described |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Table 5 (p. 150) |
| Baseline characteristics similar | Low risk | Reported in Table 1 (p. 148) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Contamination | High risk | Quote "…avoiding the contamination' of centers that acted as controls…was not possible" (p. 151) |
| Selective reporting (reporting bias) | High risk | Quote "…did not collect data on intermediate process variables" (p. 151) |
| Other bias | High risk | Short follow‐up (p. 151) |
Brown 1999.
| Methods | RCT where clinicians were randomly assigned to attend immediate (intervention) or later sessions of the programme (control group) | |
| Participants | Physicians, nurse practitioners, physician assistants, optometrists | |
| Interventions | 2 physicians gave a communication skills training programme consisting of a 4‐hour interactive workshop and a 4‐hour follow‐up workshop 1 month later. Between workshops participants were asked to audio record and review at least 2 consultations, and an instructor made an encouraging telephone call to each participant | |
| Outcomes | Routinely collected patient satisfaction scores, self reported ratings of communication skills | |
| Notes | Reported increases in patient satisfaction were not significant. However baseline scores were high in both groups, leaving little room for increase. The study authors state that longer and more intensive training, performance incentives, ongoing feedback and possibly practice restructuring may be needed to improve general patient satisfaction. They also note that the content of the routinely conducted patient satisfaction survey was not well‐aligned to the particular focus of the communication skills training. The Art of Medicine survey used in this study is not a validated instrument | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "…we used a random‐number table" (p. 823) |
| Allocation concealment (selection bias) | Low risk | Quote "we used a random‐number table to assign persons to the intervention or control group" (p. 823) |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Table 2 (p. 826) |
| Baseline characteristics similar | Low risk | Quote "Table 1 compares the characteristics of the intervention and control groups at study entry. No statistically significant differences were seen…" (p. 825) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reported and intention‐to‐treat analysis was modified (p. 825) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes were obtained from quote "an anonymous questionnaire that was mailed to patients by a contractor to the HMO" (p. 823) |
| Contamination | Unclear risk | Not specified if control group could have received similar training through other educational opportunities |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to make an assessment |
| Other bias | High risk | Survey not validated (p. 824) |
Campbell 2001.
| Methods | RCT with baseline (pre‐test), immediate (9‐12 months), and long‐term (18‐24 months) post assessments. Hospitals randomly assigned to experimental and control groups | |
| Participants | Emergency department teams (physicians, nurses, social workers, administrators) and local domestic violence advocates | |
| Interventions | 2‐day information and team planning intervention | |
| Outcomes | Rates of reported domestic violence, patient satisfaction, audit of clinical documentation | |
| Notes | Only 1 hospital sent a complete team as requested; 2 hospitals did not send a physician; social worker sent from 5 of 6 hospitals. Limited institutional support for IPE noted as a possibility for poor outcomes in this study. The components of the culture of emergency department system‐change indicator instrument used in this study is not a validated tool | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Baseline outcome measurements similar All outcomes | Low risk | Quote "This evaluation used an experimental design with baseline (pretest), immediate (9–12 months), and long‐term (18–24 months) post‐assessments…" (p. 132) |
| Baseline characteristics similar | High risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Response rates reported (p. 134) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Reviewers had "no knowledge of an individual woman's responses to acute abuse" (p. 136) |
| Contamination | Low risk | Sites geographically spread across California and Pennsylvania (p. 132) |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in results |
| Other bias | High risk | Only 1 intervention hospital sent a complete team for training (p. 134); insufficient sample size (p. 136); external events may have impacted treatment of battered women at California hospitals (OJ Simpson trial) (p. 136) |
Hanbury 2009.
| Methods | ITS study to test the effectiveness of an intervention to increase adherence to a national suicide prevention guideline at a single trust hospital | |
| Participants | Community mental health professionals (individual professions not specified) | |
| Interventions | A didactic presentation, an interprofessional group discussion stressing positive normative beliefs, interactive group work based on 2 real‐life vignettes | |
| Outcomes | Adherence rates to guideline use | |
| Notes | Needs assessment data (interviews and questionnaires) were gathered in 2 earlier phases of the study to inform the design of the intervention. The impact of 2 extraneous events was also included – the national introduction of the guideline, and a local change in the system for monitoring service‐user discharges | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote "...discontinuity occurred between those who returned the questionnaire and those who attended the intervention" (p. 516) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Routinely collected audit adherence data used (p. 505) |
| Selective reporting (reporting bias) | Low risk | Routinely collected audit adherence data used (p. 505) |
| Other bias | High risk | High staff turnover at intervention site (p. 516). Discontinuities in the samples |
| Intervention independent of other changes | Low risk | 2 events were identified and 6 separate analyses were done in order to accommodate the events (p. 509) |
| Shape of intervention effect pre‐specified | Low risk | Point of analysis is the point of intervention |
| Intervention unlikely to affect data collection | Low risk | Routinely collected audit adherence data used (p. 505) |
Helitzer 2011.
| Methods | An RCT of an IPE intervention aimed to improve patient‐centred care with follow‐up data gathered at 6 and 18 months. Individual professionals were randomised to receive the intervention (n = 13) or act as a control group (n = 14) | |
| Participants | Physicians, physician assistants and nurse practitioners | |
| Interventions | A full‐day interprofessional training, individualised feedback on video‐taped interactions with simulated patients, and optional workshops to reinforce strategies for engaging the patient | |
| Outcomes | Observations of patient‐centred communication | |
| Notes | Data were also gathered on simulated professional‐patient interactions to detect the efficacy of the intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Baseline outcome measurements similar All outcomes | Low risk | Patient‐centredness summary score reported for training and medical visits (Tables 4 and 5) |
| Baseline characteristics similar | Low risk | Quote "…no significant differences between the groups in terms of sex or practice type, either at baseline or at the final medical visit" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop‐outs indicated in Figure 1. Adjusted for in analysis |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote "The simulated patients were blind to the provider group assignment", however no statement is made about whether coders were blinded |
| Contamination | Unclear risk | Sample size is small and recruited from departments of General Internal Medicine and Family Practice of 1 university medical system |
| Selective reporting (reporting bias) | Low risk | See Tables 4 and 5 |
| Other bias | High risk | Sampling bias |
Janson 2009.
| Methods | A CBA study that aimed to evaluate interprofessional team‐based diabetes care. 120 clinical students received the intervention, while 28 medical residents acted as the control group | |
| Participants | Medicine residents, nurse practitioner students, pharmacy students | |
| Interventions | Weekly intervention consisting of didactic presentations, clinical discussions and clinic visits with patients. Quality improvement projects were also developed and implemented. Quarterly patient panel reports also received | |
| Outcomes | Clinical outcomes, planned visits | |
| Notes | As intervention team members were clinical learners enrolled in different training programmes, they had different rotational schedules, which resulted in a changing team membership | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote "This study was designed as a nonrandomized, parallel‐group clinical trial" (p. 1541) |
| Allocation concealment (selection bias) | High risk | EPOC indicates: CBA studies should be scored ‘high risk’ |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Tables 3 and 4 (p. 1544‐1545) |
| Baseline characteristics similar | Low risk | Quote "Table 2 shows the demographic characteristics of the two cohorts; there were no significant differences between them" (p. 1543) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Table 2 has data missing for 1 participant |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data came in from clinical info system directly and loaded into SPSS (p. 1543). Aggregate data stripped of identifiers was analysed (p. 1541) |
| Contamination | High risk | 1 institution, team members from intervention group could readily interact with control group |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in results |
| Other bias | Low risk | Study patients were pre‐assigned to the medicine residents in both groups and were not randomised (p. 1546) |
Morey 2002.
| Methods | CBA study with data gathered 8 months after the intervention. 6 emergency departments received the intervention, while 3 emergency departments acted as the control group | |
| Participants | Physicians, nurses, technicians, and clerks based in 9 teaching and community hospital emergency departments | |
| Interventions | An 8‐hour intervention delivered to groups of physicians, nurses, technicians and clerks involving lectures, discussion of video‐taped segments of teamwork and clinical vignettes and interactive teamwork exercises | |
| Outcomes | Collaborative behaviour, clinical error rates | |
| Notes | Also gathered survey data which indicated no change in attitudes for participants following the delivery of the IPE intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "A prospective investigation using a quasi‐experimental, untreated control group design" (p. 1556) |
| Allocation concealment (selection bias) | High risk | EPOC indicates: CBA studies should be scored ‘high risk’ |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Tables 3 and 4 (pp. 1569‐1570) |
| Baseline characteristics similar | Low risk | Quote "The control and experimental group patients who participated in the study were similar in both Period 1 and Period 2…" (p. 1563) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data was minimal, amounting to 8.1% or less for each of the outcome measures (p. 1563) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Reported use of "blinded raters…" (p. 1566) |
| Contamination | Low risk | 9 separate teaching and community hospital sites (p. 1553) |
| Selective reporting (reporting bias) | Low risk | Reported in Table 2 (pp. 1555‐1556) |
| Other bias | Low risk | Quote "91 percent agreement rate of observed errors that was significantly above chance, we feel that the lack of blinding was unlikely to introduce appreciable bias into the observed error results" (p. 1575) |
Nielsen 2007.
| Methods | A cluster RCT to evaluate the effectiveness of an interprofessional intervention aimed at reducing adverse outcomes and improving processes of care in labour and delivery units. Fifteen hospitals were randomised to either receive the intervention (n = 7) or act as the control (n = 8) | |
| Participants | Obstetricians, anaesthesiologists and nurses | |
| Interventions | A 3‐day intervention consisting of 4 hours of didactic lessons, video scenarios, and interactive training covering team structure and processes, planning and problem solving, communication, workload management and team skills, assistance with creation of interprofessional teams by use of onsite training sessions, and an on‐call contingency team to respond to obstetric emergencies | |
| Outcomes | Adverse maternal/neonatal outcomes, clinical process outcomes | |
| Notes | Explanations for lack of significant impact include training not effective, teamwork that results in a detectable impact may require more than a 4‐hour training session and more than 4 months to practice behaviours regularly | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "…a table of random numbers was used to simulate the toss of a coin" (p. 49) |
| Allocation concealment (selection bias) | Low risk | Quote "A balanced, masked randomization scheme at the hospital (cluster) level was implemented by the project biostatistician" (p. 49) |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Table 3 (p. 52) |
| Baseline characteristics similar | Low risk | Reported in Table 3 (p. 52) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote "All analyses were by intention to treat" (p. 51) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote "The trial was not blinded, with personnel at each site aware of their assignment to either the intervention or control arm" (p. 49) |
| Contamination | Unclear risk | Hospitals are in different US states but unclear if some personnel may be in contact (e.g. if they are in the military) |
| Selective reporting (reporting bias) | Low risk | See Table 4 (p. 53) |
| Other bias | Unclear risk | Unclear if data were collected independently by co‐ordinators that were not hospital personnel |
Rask 2007.
| Methods | A CBA study aimed to evaluate an interprofessional fall management quality improvement project in nursing homes 19 nursing homes received the intervention while 23 acted as the control |
|
| Participants | Nurses, physiotherapists, occupational therapists, nursing assistants, maintenance staff | |
| Interventions | A full‐day interprofessional workshop and a second follow‐up workshop approximately 1 month later to address arising challenges, organisational leadership buy‐in and support , a facility‐based falls coordinator, ongoing consultation by advanced practice nurses with expertise in falls management | |
| Outcomes | Care documentation, fall rates, restraint use | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Convenience sample of 19 nursing homes (p. 342) |
| Allocation concealment (selection bias) | High risk | EPOC indicates: CBA studies should be scored ‘high risk’ |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Table 2 (p. 347) |
| Baseline characteristics similar | Low risk | Table 1 indicates no statistically significant differences (p. 346) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Table 2 reports results of care processes for 14 of 19 nursing homes – no explanation of missing data on 5 nursing homes |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Chart audits done by individuals who quote "were not blind to the intervention status of the facilities" (p. 345) |
| Contamination | High risk | Nursing homes owned and operated by a single non‐profit organisation (p. 342) |
| Selective reporting (reporting bias) | High risk | Chart audits only done on 14 out of 19 intervention nursing homes |
| Other bias | High risk | Not randomised, chart audit incomplete |
Strasser 2008.
| Methods | Cluster RCT involving 31 stroke rehabilitation clinics that were randomised to either receive an IPE intervention designed to improve the care of people who had had a stroke (n = 15) or act as a control group (n = 16) | |
| Participants | Physicians, nurses, occupational therapists, speech‐language pathologists, physiotherapists and social workers | |
| Interventions | A 6‐month intervention consisting of an interactive workshop emphasising team dynamics, problem solving, and the use of performance feedback data and action plans for process improvement. Follow‐up telephone and video‐conference consultations were also offered | |
| Outcomes | Functional gains, length of stay, rates of community discharge | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "…randomized sites to either intervention or control group using a computer…" (pp. 11‐12) |
| Allocation concealment (selection bias) | Low risk | Quote "…randomized sites to either intervention or control group using a computer…" (pp. 11‐12) |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Table 2 |
| Baseline characteristics similar | Low risk | Reported in Table 1. Description of adjustments in analyses (pp. 12‐13) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Acknowledge sites dropped out but do not discuss if necessary to adjust analyses (p. 12) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported if data collectors and assessors were blinded |
| Contamination | Low risk | Sites randomised across US |
| Selective reporting (reporting bias) | Unclear risk | Lack of reporting on sites that dropped out of study |
| Other bias | Unclear risk | Lack of reporting on sites that dropped out of study |
Taylor 2007.
| Methods | An ITS study to assess the effects of an IPE intervention on the delivery of standard diabetes services and clinical outcomes for patients based at 1 site | |
| Participants | Healthcare professionals based in a single primary care clinic | |
| Interventions | An education intervention that aimed to improve communication, teamwork, workflow to improve diabetes care and patient outcomes. The intervention included task redistribution, standardised communication and decision‐support tool development | |
| Outcomes | Rates of diabetes testing, clinical outcomes | |
| Notes | Participants are reported as a "team" but different professional groups are not described. Clinicians and staff revised existing diabetes care protocols and processes using the American Diabetes Association clinical guidelines. The new process and diabetes checklist were implemented | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Pre‐intervention visit and post‐intervention visit reported for 277 individuals (p. 246) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | High risk | Table 2 analyses reported inconsistently for 3 months or 12 months (p. 246) |
| Other bias | High risk | Lack of a control group (p. 247) |
| Intervention independent of other changes | Unclear risk | Lack of a comparator as no control group in the study |
| Shape of intervention effect pre‐specified | Low risk | Point of analysis is the point of intervention |
| Intervention unlikely to affect data collection | Unclear risk | Not reported |
Thompson 2000a.
| Methods | RCT involving 59 primary care practices which were randomly assigned to an intervention group (29 practices) or a control group (30 practices) | |
| Participants | Physician and nursing teams from the participating primary care practices | |
| Interventions | 4‐hour seminar delivered to the primary healthcare teams. The seminars included video‐tapes, small group discussion of cases, and role play | |
| Outcomes | Recognition and treatment of patient depression | |
| Notes | While actual number of physicians is reported (n = 152), actual number of nurses is not recorded. Qualitative data relating to participants' views of the intervention were also gathered | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "Practices were randomly assigned by computer" (p. 186) |
| Allocation concealment (selection bias) | Low risk | Quote "Practices were randomly assigned by computer" (p. 186) |
| Baseline outcome measurements similar All outcomes | Low risk | Quote "Analyses controlled for ... baseline differences in outcome measures between groups" (p. 187) |
| Baseline characteristics similar | Low risk | Quote "Randomisation produced adequate matching between the intervention and control groups" (p. 188). Also reported in Table 2 |
| Incomplete outcome data (attrition bias) All outcomes | High risk | An intention‐to‐treat analysis was reported (p. 187) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Contamination | Low risk | Sites were geographically spread across county of Hampshire |
| Selective reporting (reporting bias) | Low risk | Reported in Tables 4 and 5 |
| Other bias | High risk | Large drop‐out rates reported in the control group |
Thompson 2000b.
| Methods | RCT involving 5 clinics which were randomly assigned to 2 intervention groups and 3 control groups. Follow‐up data were gathered at 9‐10 months and 21‐23 months | |
| Participants | Primary care practice teams of physicians, nurse practitioners, physician assistants, registered nurses, licensed practical nurses, medical assistants | |
| Interventions | 2 half‐day training sessions based on Precede/Proceed model for behaviour change; 3 extra training sessions for opinion leaders, newsletter, 4 additional educational sessions to teams, system support (e.g. posters in waiting areas, cue cards for providers) | |
| Outcomes | Provider knowledge, attitudes and beliefs, rates of asking, case finding, quality of assistance | |
| Notes | Unvalidated survey and qualitative data on provider views of the intervention were gathered | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Table 2 (p. 258) |
| Baseline characteristics similar | Low risk | "Intervention and control groups at baseline did not differ…" (p. 256) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adjustments in analysis made for this (p. 256) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "Chart abstractors, blinded to intervention status, ascertained any mention of possible DV in the records" (p. 256) |
| Contamination | Low risk | Clinics spread across large metropolitan area (p 254) |
| Selective reporting (reporting bias) | Low risk | Reported in Table 2 (p. 258) |
| Other bias | High risk | Small number of clinics (p. 260) |
Weaver 2010.
| Methods | A CBA study to evaluate an interprofessional intervention designed to improve team‐based collaboration for operating room clinicians. Staff at 1 hospital site received the intervention, while staff based at 1 other site acted as a control | |
| Participants | Surgeons, nurses, surgical technicians, anaesthesiologists, physician assistants | |
| Interventions | The intervention consisted of a 4‐hour session which included interactive role‐playing activities between participants | |
| Outcomes | Observed collaborative behaviour between participants | |
| Notes | Other outcomes reported included changes in perceptions and attitudes from the use of the Hospital Survey on Patient Safety Culture and Operating Room Management Attitudes Questionnaire | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote "teams...volunteered to participate in the training and evaluation efforts" (p. 135) |
| Allocation concealment (selection bias) | High risk | EPOC indicates: CBA studies should be scored ‘high risk’ |
| Baseline outcome measurements similar All outcomes | High risk | Reported in Tables 3 and 4 (p. 136‐137) |
| Baseline characteristics similar | Unclear risk | Not reported (p. 135) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | For example, analyses not conducted for initial observations with regards to debriefing (p. 139) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported if observers were blinded (p. 137) |
| Contamination | Low risk | Groups located at separate campuses (p. 133) |
| Selective reporting (reporting bias) | Unclear risk | For example, analyses not conducted for initial observations with regards to debriefing (p. 139) |
| Other bias | Unclear risk | Observation tool not validated (p. 137). Small sample size of volunteers used in the study. Attrition of control group (p. 139) |
Young 2005.
| Methods | CBA study involving 2 mental health provider organisations which received the intervention, while 3 acted as the control group | |
| Participants | Psychiatrists, mental health nurses, therapists, case managers | |
| Interventions | 6 educational components delivered over 1 year involving presentations, small group discussions, role play and 3‐ to 4‐day detailing visits 16 hours of follow‐up discussions to monitor progress |
|
| Outcomes | Practitioner professional competencies | |
| Notes | Semi‐structured interviews were gathered to qualitatively explore the effects of the intervention in more detail | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "This study used a quasi‐experimental design" (p. 968) |
| Allocation concealment (selection bias) | High risk | EPOC describes that CBAs should be scored high for first 2 items |
| Baseline outcome measurements similar All outcomes | Low risk | Reported in Tables 4 and 5 |
| Baseline characteristics similar | High risk | Site selection based on clinics which "served a large population with severe and persistent mental illness, and provided similar types of services" (p. 986) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analyses undertaken "using multiple imputation to replace missing data" (p. 970) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Contamination | Low risk | Sites based in 2 US states – Quote "each state included both intervention and control organizations, ensuring that external events would not be confounded with the intervention" (p. 986) |
| Selective reporting (reporting bias) | Low risk | See Tables 4 and 5 |
| Other bias | High risk | Small sample size, authors did not measure change in the appropriateness of care or client outcomes (p. 974) |
CBA: controlled before and after; EPOC: Effective Practice and Organisation of Care; IPE: interprofessional education; ITS: interrupted time series; RCT: randomised controlled trial.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ammentorp 2007 | Not an IPE intervention |
| Anderson 2009 | Not an RCT, CBA or ITS |
| Antunez 2003 | Post‐intervention study design |
| Armitage 2009 | Not an RCT, CBA or ITS |
| Barrett 2001 | Description of IPE intervention that reports no outcomes |
| Barton 2006 | Not an IPE intervention. 1 group pre‐/post‐test study design |
| Bashir 2000 | Not an IPE intervention |
| Bauer 2009 | Not an IPE intervention |
| Beal 2006 | Not an IPE intervention |
| Belardi 2004 | Not an IPE intervention |
| Bell 2000 | Not an IPE intervention |
| Bellamy 2006 | 1 group pre‐/post‐test study design |
| Benjamin 1999 | Not an IPE intervention |
| Berg 2009 | Not an RCT, CBA or ITS |
| Berggren 2008 | Not an IPE intervention |
| Birch 2007 | Not an RCT, CBA or ITS |
| Bluespruce 2001 | 1 group pre‐/post‐test study design |
| Boyle 2004 | 1 group pre‐/post‐test study design |
| Bradshaw 2011 | Not an IPE intervention |
| Buck 1999 | Post‐intervention study design |
| Burns 2003 | Not an IPE intervention |
| Buxton 2004 | Not an IPE intervention |
| Cameron 2009 | Not an IPE intervention |
| Carew 2001 | Post‐intervention study design |
| Cobia 1995 | Before and after study with no controls |
| Coggrave 2001 | Not an IPE intervention |
| Connolly 1995 | Post‐intervention study with no controls |
| Cooper 2005 | A CBA study that gathered self report data related to attitudes and knowledge change |
| Corso 2006 | 1 group post‐intervention study design |
| Crutcher 2004 | A clinical controlled trial of an IPE intervention. Reports outcomes related to self reported knowledge change |
| Dacey 2010 | Not an RCT, CBA or ITS |
| Dalton 1999 | Not an IPE intervention |
| DeVita 2005 | 1 group post‐intervention study design |
| Dienst 1981 | CBA study. Failed to meet comparison group criteria |
| Dobson 2002 | 1 group pre‐/post‐test study design |
| Falconer 1993 | Post‐intervention study with control group. Failed to meet comparison group criteria |
| Fields 2005 | Not an IPE intervention |
| Gandara 2010 | Not an IPE intervention |
| Hanson 2005 | Not an IPE intervention |
| Harmon 1998 | 5‐year longitudinal study with no controls |
| Hayward 1996 | Before and after study with no controls |
| Hien 2008 | Not an IPE intervention |
| Hook 2003 | 1 group post‐intervention study design |
| Hope 2005 | 1 group pre‐/post‐intervention study design |
| Horbar 2001 | Not an IPE intervention |
| Hughes 2000 | Descriptive study |
| James 2005 | 1 group pre‐/post‐intervention study design |
| Jones 2006 | Not an IPE intervention |
| Jordan‐Marsh 2004 | 1 group pre‐/post‐test study with follow‐up data collection points |
| Kenward 2009 | Not an RCT, CBA or ITS |
| Ketola 2000 | Not an IPE intervention |
| Kwan 2006 | Outcomes did not meet inclusion criteria |
| Landon 2004 | Not an IPE intervention |
| Lawrence 2002 | Not an IPE intervention |
| Lia‐Hoagberg 1997 | Before and after study with no controls |
| Llewellyn‐Jones 1999 | Not an IPE intervention |
| McBride 2000 | Not an IPE intervention |
| Monette 2008 | Not an IPE intervention |
| Nash 1993 | Before and after study with no controls |
| O'Boyle 1995 | Before and after study with no controls |
| Olivecrona 2010 | Not an RCT, CBA or ITS |
| Ouslander 2001 | Not an IPE intervention |
| Phillips 2002 | Not an IPE intervention |
| Price 2005 | Not an IPE intervention |
| Rogowski 2001 | Not an IPE intervention |
| Rubenstein 1999 | Not an IPE intervention |
| Ryan 2002 | Not an IPE intervention |
| Sauer 2010 | Not an IPE intervention |
| Smarr 2003 | Not an IPE intervention |
| Smith 2005 | 1 group pre‐/post‐intervention study design |
| Stewart 2010 | Not an IPE intervention |
| Taylor 2002 | Not an IPE intervention |
| Thomas 2007 | Not an IPE intervention |
| Trummer 2006 | No control group |
| Tschopp 2005 | 1 group pre‐/post‐intervention study design |
| Umble 2003 | Not an IPE intervention |
| Unutzer 2001 | Not an IPE intervention |
| Ward 2004 | Not an IPE intervention |
| Wells 2000 | Not an IPE intervention |
| Westfelt 2010 | Not an RCT, CBA or ITS |
| Wisborg 2009 | Not an RCT, CBA or ITS |
CBA: controlled before and after; IPE: interprofessional education; ITS: interrupted time series; RCT: randomised controlled trial.
Contributions of authors
SR, LP and JG searched and reviewed the literature and extracted data with input from MZ. SR interpreted the data and wrote the main draft of the review with input from LP, JG, DF and MZ. MZ Is guarantor for the review.
Scott Reeves (SR); Author deceased May 2018. His contributions to the published review are listed above.
Sources of support
Internal sources
Center for Innovation in Interprofessional Education, University of California, San Francisco, USA.
Li Ka Shing Knowledge Institute of St Michael's Hospital, Canada.
Continuing Education and Professional Development, Faculty of Medicine, University of Toronto, Canada.
Institute of Health Sciences Education, Queen Mary University London, UK.
Institute for Clinical Effectiveness, Toronto, Canada.
External sources
No sources of support supplied
Declarations of interest
None known. Scott Reeves; (deceased May 2018), This declaration was provided before the author died.
Deceased
Edited (no change to conclusions)
References
References to studies included in this review
Barcelo 2010 {published data only}
- Barcelo A, Cafiero E, Boer M, Mesa AE, Lopez MG, Jimenez RA, et al. Using collaborative learning to improve diabetes care and outcomes: the VIDA project. Primary Care Diabetes 2010;4(3):145‐53. [DOI] [PubMed] [Google Scholar]
Brown 1999 {published data only}
- Brown JB, Boles M, Mullooly JP, Levinson W. Effect of clinician communication skills training on patient satisfaction: a randomized controlled trial. Annals of Internal Medicine 1999;131(11):822‐9. [DOI] [PubMed] [Google Scholar]
Campbell 2001 {published data only}
- Campbell JC, Coben JH, McLoughlin E, Dearwater S, Nah G, Glass N, et al. An evaluation of a system‐change training model to improve emergency department response to battered women. Academic Emergency Medicine 2001;8(2):131‐8. [DOI] [PubMed] [Google Scholar]
Hanbury 2009 {published data only}
- Hanbury A, Wallace L, Clark M. Use of a time series design to test effectiveness of a theory‐based intervention targeting adherence of health professionals to a clinical guideline. British Journal of Health Psychology 2009;14(Pt 3):505‐18. [DOI] [PubMed] [Google Scholar]
Helitzer 2011 {published data only}
- Helitzer DL, Lanoue M, Wilson B, Hernandez BU, Warner T, Roter D. A randomized controlled trial of communication training with primary care providers to improve patient‐centeredness and health risk communication. Patient Education & Counseling 2011;82(1):21‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Janson 2009 {published data only}
- Janson SL, Cooke M, McGrath KW, Kroon LA, Robinson S, Baron RB. Improving chronic care of type 2 diabetes using teams of interprofessional learners. Academic Medicine 2009;84(11):1540‐8. [DOI] [PubMed] [Google Scholar]
Morey 2002 {published data only}
- Morey JC, Simon R, Jay GD, Wears RL, Salisbury M, Dukes KA, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Services Research 2002;37(6):1553‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nielsen 2007 {published data only}
- Nielsen PE, Goldman MB, Mann S, Shapiro DE, Marcus RG, Pratt SD, et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial. Obstetrics & Gynecology 2007;109(1):48‐55. [DOI] [PubMed] [Google Scholar]
Rask 2007 {published data only}
- Rask K, Parmelee PA, Taylor JA, Green D, Brown H, Hawley J, et al. Implementation and evaluation of a nursing home fall management program. Journal of the American Geriatrics Society 2007;55(3):342‐9. [DOI] [PubMed] [Google Scholar]
Strasser 2008 {published data only}
- Strasser DC, Falconer JA, Stevens AB, Uomoto JM, Herrin J, Bowen SE, et al. Team training and stroke rehabilitation outcomes: a cluster randomized trial. Archives of Physical Medicine & Rehabilitation 2008;89(1):10‐5. [DOI] [PubMed] [Google Scholar]
Taylor 2007 {published data only}
- Taylor CR, Hepworth JT, Buerhaus PI, Dittus R, Speroff T. Effect of crew resource management on diabetes care and patient outcomes in an inner‐city primary care clinic. Quality & Safety in Health Care 2007;16(4):244‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 2000a {published data only}
- Thompson C, Kinmonth AL, Stevens L, Peveler RC, Stevens A, Ostler KJ, et al. Effects of a clinical‐practice guideline and practice‐based education on detection and outcome of depression in primary care: Hampshire depression project randomised controlled trial. Lancet 2000a;355(9199):185‐91. [DOI] [PubMed] [Google Scholar]
Thompson 2000b {published data only}
- Thompson RS, Rivara FP, Thompson DC, Barlow WE, Sugg NK, Maiuro RD, et al. Identification and management of domestic violence: a randomized trial. American Journal of Preventive Medicine 2000b;19(4218):253‐63. [DOI] [PubMed] [Google Scholar]
Weaver 2010 {published data only}
- Weaver SJ, Rosen MA, DiazGranados D, Lazzara EH, Lyons R, Salas E, et al. Does teamwork improve performance in the operating room? A multilevel evaluation. Joint Commission Journal on Quality & Patient Safety 2010;36(3):133‐42. [DOI] [PubMed] [Google Scholar]
Young 2005 {published data only}
- Young AS, Chinman M, Forquer SL, Knight EL, Vogel H, Miller A, et al. Use of a consumer‐led intervention to improve provider competencies. Psychiatric Services 2005;56(8):967‐75. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ammentorp 2007 {published data only}
- Ammentorp J, Sabroe S, Kofoed PE, Mainz J. The effect of training in communication skills on medical doctors' and nurses' self‐efficacy. A randomized controlled trial. Patient Education & Counseling 2007;66(3):270‐7. [DOI] [PubMed] [Google Scholar]
Anderson 2009 {published data only}
- Anderson ES, Lennox A. The Leicester Model of Interprofessional education: developing, delivering and learning from student voices for 10 years. Journal of Interprofessional Care 2009;23(6):557‐73. [DOI] [PubMed] [Google Scholar]
Antunez 2003 {published data only}
- Antunez HG, Steinmann WC, Marten L, Escarfuller J. A multidisciplinary, culturally diverse approach to training health professions students. Medical Education 2003;37(10):921. [DOI] [PubMed] [Google Scholar]
Armitage 2009 {published data only}
- Armitage H, Pitt R, Jinks A. Initial findings from the TUILIP (Trent Universities Interprofessional Learning in Practice) project. Journal of Interprofessional Care 2009;23(1):101‐3. [DOI] [PubMed] [Google Scholar]
Barrett 2001 {published data only}
- Barrett J, Gifford C, Morey J, Risser D, Salisbury M. Enhancing patient safety through teamwork training. Journal of Healthcare Risk Management 2001;21(4):57‐65. [DOI] [PubMed] [Google Scholar]
Barton 2006 {published data only}
- Barton C, Miller B, Yaffe K. Improved evaluation and management of cognitive impairment: results of a comprehensive intervention in long‐term care [see comment]. Journal of the American Medical Directors Association 2006;7(2):84‐9. [DOI] [PubMed] [Google Scholar]
Bashir 2000 {published data only}
- Bashir K, Blizard B, Bosanquet A, Bosanquet N, Mann A, Jenkins R. The evaluation of a mental health facilitator in general practice: effects on recognition, management, and outcome of mental illness. British Journal of General Practice 2000;50(457123):626‐9. [PMC free article] [PubMed] [Google Scholar]
Bauer 2009 {published data only}
- Bauer G, Bossi L, Santoalla M, Rodriguez S, Farina D, Speranza AM. [Impact of a respiratory disease prevention program in high‐risk preterm infants: a prospective, multicentric study]. Archivos Argentinos de Pediatria 2009;107(2):111‐8. [DOI] [PubMed] [Google Scholar]
Beal 2006 {published data only}
- Beal T, Kemper K J, Gardiner P, Woods C. Long‐term impact of four different strategies for delivering an on‐line curriculum about herbs and other dietary supplements. BMC Medical Education 2006;6:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Belardi 2004 {published data only}
- Belardi FG, Weir S, Craig FW. A controlled trial of an advanced access appointment system in a residency family medicine center. Family Medicine 2004;36(5):341‐5. [PubMed] [Google Scholar]
Bell 2000 {published data only}
- Bell CM, Ma M, Campbell S, Basnett I, Pollock A, Taylor I. Methodological issues in the use of guidelines and audit to improve clinical effectiveness in breast cancer in one United Kingdom health region. European Journal of Surgical Oncology 2000;26(2):130‐6. [DOI] [PubMed] [Google Scholar]
Bellamy 2006 {published data only}
- Bellamy A, Fiddian M, Nixon J. Case reviews: promoting shared learning and collaborative practice. International Journal of Palliative Nursing 2006;12(4):158‐62. [DOI] [PubMed] [Google Scholar]
Benjamin 1999 {published data only}
- Benjamin EM, Schneider MS, Hinchey KT. Implementing practice guidelines for diabetes care using problem‐based learning: a prospective controlled trial using firm systems. Diabetes Care 1999;22(1019):1672‐8. [DOI] [PubMed] [Google Scholar]
Berg 2009 {published data only}
- Berg BW, Sampaga A, Garshnek V, Hara KM, Phrampus PA. Simulation crisis team training effect on rural hospital safety climate (SimCritter). Hawaii Medical Journal 2009;68(10):253‐5. [PubMed] [Google Scholar]
Berggren 2008 {published data only}
- Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall‐prevention program in older people after femoral neck fracture: a one‐year follow‐up. Osteoporosis International 2008;19(6):801‐9. [DOI] [PubMed] [Google Scholar]
Birch 2007 {published data only}
- Birch L, Jones N, Doyle PM, Green P, McLaughlin A, Champney C, et al. Obstetric skills drills: evaluation of teaching methods. Nurse Education Today 2007;27(8):915‐22. [DOI] [PubMed] [Google Scholar]
Bluespruce 2001 {published data only}
- Bluespruce J, Dodge WT, Grothaus L, Wheeler K, Rebolledo V, Carey JW, et al. HIV prevention in primary care: impact of a clinical intervention. AIDS Patient Care & STDS 2001;15(5):243‐53. [DOI] [PubMed] [Google Scholar]
Boyle 2004 {published data only}
- Boyle DK, Kochinda C. Enhancing collaborative communication of nurse and physician leadership in two intensive care units. Journal of Nursing Administration 2004;34(2):60‐70. [DOI] [PubMed] [Google Scholar]
Bradshaw 2011 {published data only}
- Bradshaw LM, Gergar ME, Holko GA. Collaboration in wound photography competency development: a unique approach. Advances in Skin & Wound Care 2011;24(2):85‐92. [DOI] [PubMed] [Google Scholar]
Buck 1999 {published data only}
- Buck MM, Tilson ER, Andersen JC. Implementation and evaluation of an interdisciplinary health professions core curriculum. Journal of Allied Health 1999;28(3):174‐8. [PubMed] [Google Scholar]
Burns 2003 {published data only}
- Burns JP, Mello MM, Studdert DM, Puopolo AL, Truog RD, Brennan TA. Results of a clinical trial on care improvement for the critically ill. Critical Care Medicine 2003;31(8):2107‐17. [DOI] [PubMed] [Google Scholar]
Buxton 2004 {published data only}
- Buxton L, Pidduck D, Marston G, Perry D. Development of a multidisciplinary care pathway for a specialist learning disability inpatient treatment and assessment unit. Journal of Integrated Care Pathways 2004;8(3):119‐26. [Google Scholar]
Cameron 2009 {published data only}
- Cameron TS, McKinstry A, Burt SK, Howard ME, Bellomo R, Brown DJ, et al. Outcomes of patients with spinal cord injury before and after introduction of an interdisciplinary tracheostomy team. Critical Care & Resuscitation 2009;11(1):14‐9. [PubMed] [Google Scholar]
Carew 2001 {published data only}
- Carew LB, Chamberlain VM. Interdisciplinary update nutrition course offered to educators through interactive television. Journal of Nutrition Education 2001;33(6):352‐3. [DOI] [PubMed] [Google Scholar]
Cobia 1995 {published data only}
- Cobia DC, Center H, Buckhalt JA, Meadows ME. An interprofessional model for serving youth at risk for substance abuse: the team case study. Journal of Drug Education 1995;25(2):99‐109. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Coggrave 2001 {published data only}
- Coggrave M. Care of the ventilator dependent spinal cord‐injured patient. British Journal of Therapy & Rehabilitation 2001;8(4):146‐9. [Google Scholar]
Connolly 1995 {published data only}
- Connolly PM. Transdisciplinary collaboration of academia and practice in the area of serious mental illness. Australian & New Zealand Journal of Mental Health Nursing 1995;4(4):168‐80. [MEDLINE: ] [PubMed] [Google Scholar]
Cooper 2005 {published data only}
- Cooper H, Spencer‐Dawe E, McLean E. Beginning the process of teamwork: design, implementation and evaluation of an inter‐professional education intervention for first year undergraduate students. Journal of Interprofessional Care 2005;19(5):492‐508. [DOI] [PubMed] [Google Scholar]
Corso 2006 {published data only}
- Corso R, Brekken L, Ducey C, KnappPhilo J. Professional development strategies to support the inclusion of infants and toddlers with disabilities in infant‐family programs. Zero to Three 2006;26(3):36‐42. [Google Scholar]
Crutcher 2004 {published data only}
- Crutcher RA, Then K, Edwards A, Taylor K, Norton P. Multi‐professional education in diabetes. Medical Teacher 2004;26(5):435‐43. [DOI] [PubMed] [Google Scholar]
Dacey 2010 {published data only}
- Dacey M, Murphy JI, Anderson DC, McCloskey WW. An interprofessional service‐learning course: uniting students across educational levels and promoting patient‐centered care. Journal of Nursing Education 2010;49(12):696‐9. [DOI] [PubMed] [Google Scholar]
Dalton 1999 {published data only}
- Dalton JA, Blau W, Lindley C, Carlson J, Youngblood R, Greer SM. Changing acute pain management to improve patient outcomes: an educational approach. Journal of Pain and Symptom Management 1999;17(4):277‐87. [DOI] [PubMed] [Google Scholar]
DeVita 2005 {published data only}
- DeVita, Schaefer J, Lutz J, Wang H, Dongilli T. Improving medical emergency team (MET) performance using a novel curriculum and a computerized human patient stimulator. Quality & Safety in Health Care 2005;14(5):326‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dienst 1981 {published data only}
- Dienst ER, Byl N. Evaluation of an educational program in health care teams. Journal of Community Health 1981;6(4):282‐98. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dobson 2002 {published data only}
- Dobson S, Upadhyaya S, Stanley B. Using an interdisciplinary approach to training to develop the quality of communication with adults with profound learning disabilities by care staff. International Journal of Language & Communication Disorders 2002;37(1):41‐57. [DOI] [PubMed] [Google Scholar]
Falconer 1993 {published data only}
- Falconer JA, Roth EJ, Sutin JA, Strasser DC, Chang RW. The critical path method in stroke rehabilitation: lessons from an experiment in cost containment and outcome improvement. Quality Review Bulletin 1993;19(1):8‐16. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fields 2005 {published data only}
- Fields M, Peterman J. Intravenous medication safety system averts high‐risk medication errors and provides actionable data. Nursing Administration Quarterly 2005;29(1):78‐87. [DOI] [PubMed] [Google Scholar]
Gandara 2010 {published data only}
- Gandara E, Ungar J, Lee J, Chan‐Macrae M, O'Malley T, Schnipper JL. Discharge documentation of patients discharged to subacute facilities: a three‐year quality improvement process across an integrated health care system. Joint Commission Journal on Quality & Patient Safety 2010;36(6):243‐51. [DOI] [PubMed] [Google Scholar]
Hanson 2005 {published data only}
- Hanson LC, Reynolds KS, Henderson M, Pickard CG. A quality improvement intervention to increase palliative care in nursing homes. Journal of Palliative Medicine 2005;8(3):576‐84. [DOI] [PubMed] [Google Scholar]
Harmon 1998 {published data only}
- Harmon RL, Sheehy LM, Davis DM. The utility of external performance measurement tools in program evaluation. Rahabilitation Nursing 1998;23(1):8‐11. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hayward 1996 {published data only}
- Hayward KS, Powell LT, McRoberts J. Changes in student perceptions of interdisciplinary practice in the rural setting. Journal of Allied Health 1996;25(4):315‐27. [MEDLINE: ] [PubMed] [Google Scholar]
Hien 2008 {published data only}
- Hien le TT, Takano T, Seino K, Ohnishi M, Nakamura K. Effectiveness of a capacity‐building program for community leaders in a healthy living environment: a randomized community‐based intervention in rural Vietnam. Health Promotion International 2008;23(4):354‐64. [DOI] [PubMed] [Google Scholar]
Hook 2003 {published data only}
- Hook AD, Lawson‐Porter A. The development and evaluation of a fieldwork educator's training programme for allied health professionals. Medical Teacher 2003;25(5):527‐36. [DOI] [PubMed] [Google Scholar]
Hope 2005 {published data only}
- Hope JM, Lugassy D, Meyer R, Jeanty F, Myers S, Jones S, et al. Bringing interdisciplinary and multicultural team building to health care education: the downstate team‐building initiative. Academic Medicine 2005;80(1):74‐83. [DOI] [PubMed] [Google Scholar]
Horbar 2001 {published data only}
- Horbar JD, Rogowski J, Plsek PE, Delmore P, Edwards WH, Hocker J, et al. Collaborative quality improvement for neonatal intensive care. NIC/Q project investigators of the Vermont Oxford Network. Pediatrics 2001;107(1383):14‐22. [DOI] [PubMed] [Google Scholar]
Hughes 2000 {published data only}
- Hughes TL, Medina Walpole AM. Implementation of an interdisciplinary behavior management program. Journal of the American Geriatrics Society 2000;48(5):581‐7. [PubMed] [Google Scholar]
James 2005 {published data only}
- James R, Barker J. Evaluation of a model of interprofessional education. Nursing Times 2005;101(40):34‐6. [PubMed] [Google Scholar]
Jones 2006 {published data only}
- Jones D, Bates S, Warrillow S, Goldsmith D, Kattula A, Way M, et al. Effect of an education programme on the utilization of a medical emergency team in a teaching hospital. Internal Medicine Journal 2006;36(4):231‐6. [DOI] [PubMed] [Google Scholar]
Jordan‐Marsh 2004 {published data only}
- Jordan‐Marsh M, Hubbard J, Watson R, Deon Hall R, Miller P, Mohan O. The social ecology of changing pain management: do I have to cry?. Journal of Pediatric Nursing 2004;19(3):193‐203. [DOI] [PubMed] [Google Scholar]
Kenward 2009 {published data only}
- Kenward L, Stiles M. Intermediate care: an interprofessional education opportunity in primary care. Journal of Interprofessional Care 2009;23(6):668‐71. [DOI] [PubMed] [Google Scholar]
Ketola 2000 {published data only}
- Ketola E, Sipil R, M'kel M, Klockars M. Quality improvement programme for cardiovascular disease risk factor recording in primary care. Quality in Health Care 2000;9(3257):175‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kwan 2006 {published data only}
- Kwan D, Barker KK, Austin Z, Chatalalsingh C, Grdisa V, Langlois S, et al. Effectiveness of a faculty development program on interprofessional education: a randomized controlled trial. Journal of Interprofessional Care 2006;20(3):314‐6. [DOI] [PubMed] [Google Scholar]
Landon 2004 {published data only}
- Landon BE, Wilson IB, McInnes K, Landrum MB, Hirschhorn L, Marsden PV, et al. Improving patient care: effects of a quality improvement collaborative on the outcome of care of patients with HIV infection: the EQHIV study. Annals of Internal Medicine 2004;140(11):887‐96. [DOI] [PubMed] [Google Scholar]
Lawrence 2002 {published data only}
- Lawrence SJ, Shadel BN, Leet TL, Hall JB, Mundy LM. An intervention to improve antibiotic delivery and sputum procurement in patients hospitalized with community‐acquired pneumonia. Chest 2002;122(3):913‐9. [DOI] [PubMed] [Google Scholar]
Lia‐Hoagberg 1997 {published data only}
- Lia‐Hoagberg B, Nelson P, Chase RA. An interdisciplinary health team training program for school staff in Minnesota. Journal of School Health 1997;67(3):94‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Llewellyn‐Jones 1999 {published data only}
- Llewellyn‐Jones RH, Baikie KA, Smithers H, Cohen J, Snowdon J, Tennant CC. Multifaceted shared care intervention for late life depression in residential care: randomised controlled trial. BMJ 1999;319(7211174):676‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
McBride 2000 {published data only}
- McBride P, Underbakke G, Plane MB, Massoth K, Brown R, Solberg LI, et al. Improving prevention systems in primary care practices: the health education and research trial (HEART). Journal of Family Practice 2000;49(2707):115‐25. [PubMed] [Google Scholar]
Monette 2008 {published data only}
- Monette J, Champoux N, Monette M, Fournier L, Wolfson C, du Fort GG, et al. Effect of an interdisciplinary educational program on antipsychotic prescribing among nursing home residents with dementia. International Journal of Geriatric Psychiatry 2008;23(6):574‐9. [DOI] [PubMed] [Google Scholar]
Nash 1993 {published data only}
- Nash A, Hoy A. Terminal care in the community ‐ an evaluation of residential workshops for general practitioner/district nurse teams. Palliative Medicine 1993;7(1):5‐17. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
O'Boyle 1995 {published data only}
- O'Boyle M, Paniagua FA, Wassef A, Hoizer C. Training health professionals in the recognition and treatment of depression. Psychiatric Services 1995;46(6):616‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Olivecrona 2010 {published data only}
- Olivecrona C, Karrlander S, Hylin U, Tornkvist H, Jonsson C, Svensen C. [A successful educational program for medical and nursing students. Interprofessional learning gives insights and strengthens team work]. Lakartidningen 2010;107(3):113‐5. [PubMed] [Google Scholar]
Ouslander 2001 {published data only}
- Ouslander JG, Maloney C, Grasela TH, Rogers L, Walawander CA. Implementation of a nursing home urinary incontinence management program with and without tolterodine. Journal of the American Medical Directors Association 2001;2(5):207‐14. [PubMed] [Google Scholar]
Phillips 2002 {published data only}
- Phillips M, Givens C, Schreiner B. Put into practice: impact of a multidisciplinary education program for children and adolescents with type 2 diabetes. Diabetes Educator 2002;28(3):400‐2. [PubMed] [Google Scholar]
Price 2005 {published data only}
- Price D, Howard M, Shaw E, Zazulak J, Waters H, Chan D. Family medicine obstetrics: collaborative interdisciplinary program for a declining resource. Canadian Family Physician 2005;51:68‐74. [PMC free article] [PubMed] [Google Scholar]
Rogowski 2001 {published data only}
- Rogowski JA, Horbar JD, Plsek PE, Baker LS, Deterding J, Edwards WH, et al. Economic implications of neonatal intensive care unit collaborative quality improvement. Pediatrics 2001;107(1384):23‐9. [DOI] [PubMed] [Google Scholar]
Rubenstein 1999 {published data only}
- Rubenstein LV, Jackson‐Triche M, Unutzer J, Miranda J, Minnium K, Pearson ML, et al. Evidence‐based care for depression in managed primary care practices. Health Affairs 1999;18(5439):89‐105. [DOI] [PubMed] [Google Scholar]
Ryan 2002 {published data only}
- Ryan A, Carter J, Lucas J, Berger J. You need not make the journey alone: overcoming impediments to providing palliative care in a public urban teaching hospital. American Journal of Hospice and Palliative Care 2002;19(3):171‐80. [DOI] [PubMed] [Google Scholar]
Sauer 2010 {published data only}
- Sauer J, Darioly A, Mast MS, Schmid PC, Bischof N. A multi‐level approach of evaluating crew resource management training: a laboratory‐based study examining communication skills as a function of team congruence. Ergonomics 2010;53(11):1311‐24. [DOI] [PubMed] [Google Scholar]
Smarr 2003 {published data only}
- Smarr KL. The effects of arthritis professional continuing education in vocational rehabilitation [unpublished Ph.D.]. University of Missouri, Columbia 2003.
Smith 2005 {published data only}
- Smith C, Rebeck S, Schaag H, Kleinbeck S, Moore JM, Bleich MR. A model for evaluating systemic change: measuring outcomes of hospital discharge education redesign. Journal of Nursing Administration 2005;35(2):67‐73. [PubMed] [Google Scholar]
Stewart 2010 {published data only}
- Stewart EE, Nutting PA, Crabtree BF, Stange KC, Miller WL, Jaen CR. Implementing the patient‐centered medical home: observation and description of the national demonstration project. Annals of Family Medicine 2010;8 Suppl 1:S21‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2002 {published data only}
- Taylor BL, Smith GB. Trainees' views of a multidisciplinary training programme in intensive care medicine. Care of the Critically Ill 2002;18(5):148‐51. [Google Scholar]
Thomas 2007 {published data only}
- Thomas EJ, Taggart B, Crandell S, Lasky RE, Williams AL, Love LJ, et al. Teaching teamwork during the Neonatal Resuscitation Program: a randomized trial. Journal of Perinatology 2007;27(7):409‐14. [DOI] [PubMed] [Google Scholar]
Trummer 2006 {published data only}
- Trummer UF, Mueller UO, Nowak P, Stidl T, Pelikan JM. Does physician‐patient communication that aims at empowering patients improve clinical outcome? A case study. Patient Education & Counseling 2006;61(2):299‐306. [DOI] [PubMed] [Google Scholar]
Tschopp 2005 {published data only}
- Tschopp JM, Frey JG, Janssens JP, Burrus C, Garrone S, Pernet R, et al. Asthma outpatient education by multiple implementation strategy: outcome of a programme using a personal notebook. Respiratory Medicine 2005;99(3):355‐62. [DOI] [PubMed] [Google Scholar]
Umble 2003 {published data only}
- Umble KE, Shay S, Sollecito W. An interdisciplinary MPH via distance learning: meeting the educational needs of practitioners. Journal of Public Health Management and Practice 2003;9(2):123‐35. [DOI] [PubMed] [Google Scholar]
Unutzer 2001 {published data only}
- Unutzer J, Rubenstein L, Katon WJ, Tang L, Duan N, Lagomasino IT, et al. Two‐year effects of quality improvement programs on medication management for depression. Archives of General Psychiatry 2001;58(10233):935‐42. [DOI] [PubMed] [Google Scholar]
Ward 2004 {published data only}
- Ward C, Wright M. Fast‐track palliative care training to bridge the theory‐practice gap. Nursing Times 2004;100(12):38‐40. [PubMed] [Google Scholar]
Wells 2000 {published data only}
- Wells K, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 2000;283(2176):212‐20. [DOI] [PubMed] [Google Scholar]
Westfelt 2010 {published data only}
- Westfelt P, Hedskold M, Pukk‐Harenstam K, Svensson R M, Wallin C J. [Efficient training in cooperation within your own emergency department. With patient simulation and skilled trainers]. Lakartidningen 2010;107(10):685‐9. [PubMed] [Google Scholar]
Wisborg 2009 {published data only}
- Wisborg T, Brattebo G, Brinchmann‐Hansen A, Hansen K S. Mannequin or standardized patient: participants' assessment of two training modalities in trauma team simulation. Scandinavian Journal of Trauma, Resuscitation & Emergency Medicine 2009;17:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Barr 2005
- Barr H, Koppel I, Reeves S, Hammick M, Freeth D. Effective interprofessional education: assumption, argument and evidence. London: Blackwell, 2005. [Google Scholar]
Berridge 2010
- Berridge EJ, Mackintosh N, Freeth D. Supporting patient safety: examining communication within delivery suite teams through contrasting approaches to research observation. Midwifery 2010;26:512‐9. [DOI] [PubMed] [Google Scholar]
Charles Campion‐Smith 2011
- Campion‐Smith C, Austin H, Criswick S, Dowling B, Francis G. Can sharing stories change practice? A qualitative study of an interprofessional narrative‐based palliative care course. Journal of Interprofessional Care 2011;25:105–11. [DOI] [PubMed] [Google Scholar]
CIHC 2010
- Canadian Interprofessional Health Collaboration. A national interprofessional competency framework, 2010. www.cihc.ca/files/CIHC_IPCompetencies_Feb1210.pdf. Vancouver, B.C.: Canadian Interprofessional Health Collaboration, (accessed 18 February 2013).
Craig 2008
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, Guidance, MRC. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frenk 2010
- Frenk J, Chen L, Bhutta Z, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet 2010;376(9756):1923‐58. [DOI: 10.1016/S0140-6736(10)61854-5] [DOI] [PubMed] [Google Scholar]
Interprofessional Educ Collab Expert Panel 2011
- Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: Report of an expert panel, 2011. www.aacp.org/resources/education/Documents/10‐242IPECFullReportfinal.pdf. Washington, D.C.: Interprofessional Education Collaborative, (accessed 18 February 2013).
Makowsky 2009
- Makowsky M, Schindel T, Rosenthal M, Campbell K, Tsuyuki R, Madill H. Collaboration between pharmacists, physicians and nurse practitioners: a qualitative investigation of working relationships in the inpatient medical setting. Journal of Interprofessional Care 2009;23(2):169‐84. [DOI] [PubMed] [Google Scholar]
Reeves 2008
- Reeves S, Zwarenstein M, Goldman J, Barr H, Freeth D, Hammick M, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD002213.pub2] [DOI] [PubMed] [Google Scholar]
Reeves 2010
- Reeves S, Lewin S, Espin S, Zwarenstein M. Interprofessional Teamwork for Health and Social Care. London: Blackwell‐Wiley, 2010. [Google Scholar]
Sargeant 2011
- Sargeant J, MacLeod T, Murray A. An interprofessional approach to teaching communication skills. Journal of Continuing Education in the Health Professions 2011;31(4):265‐7. [DOI: 10.1002/chp.20139] [DOI] [PubMed] [Google Scholar]
Suter 2012
- Suter E, Deutschlander S, Mickelson G, Nurani Z, Lait J, Harrison L, et al. Can interprofessional collaboration provide health human resources solutions? A knowledge synthesis. Journal of Interprofessional Care 2012;26(4):261‐8. [DOI: ] [DOI] [PubMed] [Google Scholar]
WHO 2010
- World Health Organization. Framework for action on interprofessional education and collaborative practice, 2010. whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf (accessed 18 February 2013). [WHO reference number: WHO/HRH/HPN/10.3.]
References to other published versions of this review
Zwarenstein 2000
- Zwarenstein M, Reeves S, Barr H, Hammick M, Koppel I, Atkins J. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD002213] [DOI] [PubMed] [Google Scholar]
Zwarenstein 2009
- Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD000072.pub2] [DOI] [PubMed] [Google Scholar]


