Abstract
Background
People with cystic fibrosis (CF) and pancreatic insufficiency are at risk of a deficiency in fat‐soluble vitamins, including vitamin A. Vitamin A deficiency predominantly causes eye and skin problems, while excessive levels of vitamin A can harm the respiratory and skeletal systems in children and interfere with the metabolism of other fat‐soluble vitamins. Most CF centres administer vitamin A as supplements to reduce the frequency of vitamin A deficiency in people with CF and to improve clinical outcomes such as growth, although the recommended dose varies between different guidelines. Thus, a systematic review on vitamin A and vitamin A‐like supplementation (carotenes or other retinoids) in people with CF would help guide clinical practice. This is an update of an earlier Cochrane Review.
Objectives
To determine if supplementation with vitamin A, carotenes or other retinoid supplements in children and adults with CF reduces the frequency of vitamin A deficiency disorders, improves general and respiratory health and affects the frequency of vitamin A toxicity.
Search methods
We searched the Cochrane Cystic Fibrosis and Genetic Disorders Group Cystic Fibrosis Trials Register compiled from electronic database searches and handsearching of journals and conference abstract books. Additionally we searched several ongoing trials registries, including ClinicalTrials.gov, the WHO International Clinical Trials Registry Platform and the International Standard Randomised Controlled Trial Number Registry.
Most recent database searches: 01 June 2018.
Selection criteria
All randomised or quasi‐randomised controlled studies comparing all preparations of oral vitamin A, carotenes or retinoids (or in combination), used as a supplement compared to placebo at any dose, for at least three months, in people with CF (diagnosed by sweat tests or genetic testing) with and without pancreatic insufficiency.
Data collection and analysis
Two authors individually assessed study quality and extracted data on outcome measures. The authors assessed the quality of the evidence using the GRADE system. Investigators were contacted to retrieve missing quantitative data.
Main results
No studies of vitamin A or other retinoid supplementation were eligible for inclusion. However, one randomised study of beta (β)‐carotene supplementation involving 24 people with CF who were receiving pancreatic enzyme substitution was included. The study compared successive β‐carotene supplementation periods (high dose followed by low dose) compared to placebo. The results for the low‐dose supplementation period should be interpreted with caution, due to the lack of a wash‐out period after the high‐dose supplementation.
The included study did not report on two of the review's primary outcomes (vitamin A deficiency disorders and mortality); results for our third primary outcome of growth and nutritional status (reported as z score for height) showed no difference between supplementation and placebo, mean difference (MD) ‐0.23 (95% confidence interval (CI) ‐0.89 to 0.43) (low‐quality evidence). With regards to secondary outcomes, supplementation with high‐dose β‐carotene for three months led to significantly fewer days of systemic antibiotics required to treat pulmonary exacerbations, compared to controls, MD ‐15 days (95% CI ‐27.60 to ‐2.40); however, this was not maintained in the second three‐month section of the study when the level of β‐carotene supplementation was reduced, MD ‐8 days (95% CI ‐18.80 to 2.80) (low‐quality evidence). There were no statistically significant effects between groups in lung function (low‐quality evidence) and no adverse events were observed (low‐quality evidence). Supplementation affected levels of β‐carotene in plasma, but not vitamin A levels. The study did not report on quality of life or toxicity.
Authors' conclusions
Since no randomised or quasi‐randomised controlled studies on retinoid supplementation were identified, no conclusion on the supplementation of vitamin A in people with CF can be drawn. Additionally, due to methodological limitations in the included study, also reflected in the low‐quality evidence judged following the specific evidence grading system (GRADE), no clear conclusions on β‐carotene supplementation can be drawn. Until further data are available, country‐ or region‐specific guidelines regarding these practices should be followed.
Plain language summary
The use of regular vitamin A or vitamin A‐like preparations for children and adults with cystic fibrosis
Review question
We reviewed the evidence regarding the effect of regular vitamin A or vitamin A‐like (carotenes or other retinoids) supplements in children and adults with cystic fibrosis.
Background
In people with cystic fibrosis only a small proportion of some vitamins, such as vitamin A, may be absorbed by the body and lead to problems caused by vitamin deficiency. A lack of vitamin A (vitamin A deficiency) can cause eye and skin problems and is associated with poorer general and respiratory health. Therefore, people with cystic fibrosis are usually supplemented with regular vitamin A preparations from a very young age. However, too much vitamin A can cause bone and liver problems. Excessive carotene levels are known to cause carotenaemia, a harmless, reversible yellowing of the skin, whilst a lack of carotene is not known to cause adverse manifestations in individuals with normal vitamin A levels.
Search date
The evidence is current to: 01 June 2018.
Study characteristics
No studies comparing vitamin A or other retinoid supplements to placebo (dummy drug containing no vitamin A) were included, but we did find one study comparing beta‐carotene supplementation (a precursor of vitamin A) to placebo. A total of 24 people with cystic fibrosis (aged 6.7 to 27.7 years) were put into groups at random and treated either with β‐carotene capsules (at a high dose for three months followed by a low dose for a further three months) or with placebo (for six months).
Key results
No studies on vitamin A supplementation were included in this review.
The single included study revealed that high‐dose beta‐carotene supplementation for three months led to fewer days on which people with CF required antibiotics compared to placebo, but this was not the case in the following three‐month section of the study when low‐dose beta‐carotene supplementation was compared to placebo. Other clinical outcome measures (growth, nutritional status and lung function) showed no statistical significant differences between treatment and placebo groups. No side effects were observed. The other outcomes in this review, such as vitamin A deficiency symptoms, mortality, toxicity and quality of life, were not reported.
Quality of the evidence
We could only include one study in this review and that study had several limitations. This is reflected in the assessment of low‐quality evidence, judged using the specific evidence grading system (GRADE). So, we feel that the strength of evidence is low. Not all outcome measures were reported after each supplementation dose and results should be viewed with some caution as some beta‐carotene from the high‐dose period was probably still present in the blood during the low‐dose supplementation period.
Conclusions
Since no studies on vitamin A supplementation were included in the review, no conclusions can be drawn regarding the routine use of vitamin A supplements. Due to limitations of the included study of beta‐carotene supplementation, no definitive conclusions regarding its use can be drawn either. Until further evidence is available, local guidelines should be followed regarding supplementation.
Summary of findings
Summary of findings 1. Summary of findings.
| β‐carotene supplementationcompared to placebo in children and adults with CF | ||||||
|
Patient or population: children and adults with CF Settings: outpatient Intervention: β‐carotene supplementation (month 1 to 3: high‐dose (1 mg/kg/day (max 50 mg/day); month 4 to 6: low‐dose (10 mg/day)) Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) |
Relative effect (95% CI) |
No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | β‐carotene supplementation | |||||
|
Vitamin A deficiency disorders Follow‐up: NA |
Outcome not reported | NA | NA | We planned to assess visual impairment, any other ocular dysfunction and skin manifestations, but the included study did not report any of these. | ||
|
Growth and nutritional status:
z‐score for height Follow‐up: At 6 months (low‐dose) |
The mean (SD) z score for height at 6 months was ‐0.81 (0.63) in the placebo group. | The mean z score for height was 0.23 lower (0.89 lower to 0.43 higher) in the supplementation group. |
NA | 24 (1 study) |
⊕⊕⊝⊝ Low1,2 | We planned to assess weight (kg and z score), height (cm and z score) and BMI. No separate analysable weight data were reported, height was only reported as a z score and the authors stated no differences between groups for BMI. |
|
Mortality Follow‐up: NA |
Outcome not reported | NA | NA | |||
|
Respiratory outcomes: FEV1 (% predicted): Follow‐up: At 3 months (high‐dose) Follow‐up: At 6 months (low‐dose) |
At 3 months mean (SD) FEV1 (% predicted) was 82.2% (15.1) in the placebo group. At 6 months mean (SD) FEV1 (% predicted) was 80.3% (19.1) in the placebo group. |
At 3 months mean FEV1 (% predicted) was 10.6% lower (31.1% lower to 9.9% higher) in the supplementation group. At 6 months mean FEV1 (% predicted) was 10.3% lower (31.6% lower to 11.0% higher) in the supplementation group. |
NA | 24 (1 study) |
⊕⊕⊝⊝ Low1,2 | |
|
Respiratory outcomes: Antibiotic days per patient in past 3 months Follow‐up: At 3 months (high‐dose) Follow‐up: At 6 months (low‐dose) |
At 3 months the mean (SD) number of antibiotic days was 24.8 (19.1) days in the placebo group. At 6 months the mean (SD) number of antibiotic days was 18.5 (15.8) days in the placebo group. |
At 3 months the mean number of antibiotic days was 15.0 days lower (27.6 lower to 2.4 lower) in the supplementation group. At 6 months the mean number of antibiotic days was 8.0 days lower (18.8 days lower to 2.8 days higher) in the supplementation group. |
NA | 24 (1 study) |
⊕⊕⊝⊝ Low1,2 | |
|
Adverse events Follow‐up: At 6 months (low‐dose) |
No adverse events reported. | No adverse events reported. | NA | 24 (1 study) | ⊕⊕⊕⊝ Low1,3 | Authors only mentioned that no adverse events were observed, without specification. |
| *The basis for the assumed risk is the event rate in the control group across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CF: cystic fibrosis; CI: confidence interval; FEV1: forced expiratory volume in 1 second; NA: Not applicable; SD: standard deviation. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
1. Downgraded once due risk of bias: unclear information relating to methodology such method of generation of random sequence, allocation concealment and blinding. Also due to the lack of an adequate wash‐out period post high‐dose supplementation, results post low‐dose supplementation might not be fully representative, increasing the risk of bias due to study design.
2. Downgraded once due to imprecision: The CI crosses no difference and due to the wide CI minor differences are not ruled out.
3. Downgraded once as no data are provided, only narrative.
Background
Description of the condition
Cystic fibrosis (CF) is a genetic disorder that affects multiple organs. Pancreatic insufficiency affects up to 90% of people with CF, whereby fat malabsorption occurs and pancreatic enzyme replacement is required to prevent steatorrhoea and malnutrition (Dodge 2006). Fat soluble vitamins (A, D, E and K) are co‐absorbed with fat and thus deficiency of these vitamins may occur (Dodge 2006). Most CF centres now routinely administer these vitamins as supplements from the neonatal period, but the recommendations differ among the major CF centres (Li 2016). In the past, a few centres have administered them only later in life or when deficiencies are detected clinically or on routine monitoring. While deficiencies may occur from the disease process of CF and insufficient supplementation, vitamin toxicity may also occur from excess supplementation. Both deficiency and excess of these vitamins may lead to specific medical problems (Dodge 2006; Hammond 2013; Sethuraman 2006). Current guidelines judged the available evidence for routine vitamin A supplementation as insufficient to guide practice, their recommendations are, however, based on non‐randomised trials and expert opinion (Royal Brompton Hospital 2017; Saxby 2017).
Vitamin A is an essential nutrient for epithelial cell maintenance and repair in the respiratory, urinary and intestinal tract, immune response, and bone growth (Saxby 2017). Dietary vitamin A (retinol or retinol esters) is found in liver, beef, eggs, fish, the fat of dairy products and vitamin A fortified margarine. Both alpha (α)‐ and beta (β)‐carotene can act as precursors for the synthesis of vitamin A. The dietary carotenoid (β‐carotene) is found in red, orange, yellow and leafy green vegetables (e.g. carrots, sweet potato and silverbeet) and red and orange fruit (e.g. mangos and oranges). Like vitamin A, β‐carotene is an antioxidant, which plays a role in coping with the oxidative stress that results from inflammatory and infectious processes in CF (Cantin 2007).
Vitamin A may be obtained from dietary sources by multiple pathways, either in its direct form as retinol‐esters, or indirectly as β‐carotene, which is partly converted to retinol (Harrison 2012). In the direct pathway, the long‐chain fatty acids of retinol are hydrolysed by pancreatic enzymes and enzymes released by intestinal cells (Harrison 2012). Since up to 90% of people with CF suffer from pancreatic insufficiency (Dodge 2006), fat uptake, and thereby also the uptake of fat‐soluble vitamins including vitamin A, is restrained. Absorption of β‐carotene and its conversion to retinol are not withheld by a decreased pancreas function, β‐carotene uptake is partly converted to retinol, a precursor of other forms of vitamin A, which can be reduced to retinol (Paik 2001). Although β‐carotene absorption is theoretically not impaired in people with CF, it is unknown whether β‐carotene supplementation improves vitamin A serum concentrations.
Vitamin A deficiency can be defined as a serum retinol (SROL) concentration less than 0.70 µmol/L (less than 20 µg/dl) (West 2003). However, SROL levels may be influenced by albumin and retinol binding protein (RBP) as well as acute illnesses with infection and inflammation (Napoli 1996; Stephensen 1994). Levels of SROL should be measured while individuals are clinically stable (Borowitz 2002; Saxby 2017). Carotene deficiency has no defined serum concentrations (CDC 2012), although some studies define β‐carotene reference values based on the 95% confidence interval (CI) of β‐carotene serum concentrations in healthy individuals (Olmedilla 2001; Socha 2010).
The major consequence of vitamin A deficiency is ocular dysfunction with abnormal dark adaptation (night blindness), conjunctival and corneal xerosis (thickening) which can lead to blindness (Saxby 2017; West 2003). Another consequence of vitamin A deficiency is the skin condition phrynoderma (a form of follicular hyperkeratosis associated with some micronutrient deficiencies). Vitamin A deficiency has also been linked to impaired mechanisms of host resistance to infection, poor growth and increased mortality in a study of mothers and children (West 2003). On the other hand, hypervitaminosis A (excess levels of vitamin A) is associated with hepatotoxicity and bone problems (Penniston 2006). Also, cross‐sectional studies have reported that up to 25% of children with CF do not require vitamin A supplementation as sufficient amounts were already available though their diet (Brei 2013; Graham‐Maar 2006).
Carotenes, including β‐carotene, are known to be effective in preventing radical‐ or oxidative stress initiated damage (Krinsky 2005). However, as long as vitamin A levels are normal, adverse clinical manifestations of β‐carotene deficiency are unknown (Cantin 2007). Excessive intake of β‐carotene is known to cause carotenaemia, a harmless, reversible yellowing of the skin (Lascari 1981). In general, most authors consider excessive intake of β‐carotene as nontoxic (Cantin 2007; Galli 2012; Hammond 2013), although a meta‐analysis conducted by Bjelkovic and colleagues revealed that a daily intake of β‐carotene supplementation in a dose higher than the recommended daily allowances (β‐carotene equivalent to a dose of vitamin A of 800 µg = 9.6 mg β‐carotene) increased mortality amongst adults in the general population (Bjelakovic 2013). Furthermore, β‐carotene supplementation in smokers and asbestos workers is associated with an increased risk of lung and gastric cancer (Druesne 2010).
Description of the intervention
Vitamin A is available as a sole supplement as well as in combination form with other vitamins as multivitamins (either as a liquid or a tablet). The availability of different formulations differ in different health services (Graham‐Maar 2006). Vitamin A is usually administered as a daily dose, but the recommended doses vary in different guidelines. For example, the USA guidelines recommend daily supplementation of 10,000 IU from the age of eight years (Borowitz 2002); whereas the Australian guidelines recommend a daily supplementation dose of 2500 IU to 5000 IU for older children, adolescents and adults (Saxby 2017). Supplements of β‐carotene are available solely or in combination with other carotenoids or vitamins, or both; although β‐carotene supplementation is currently not recommended in CF (Saxby 2017).
How the intervention might work
Normalisation of vitamin A levels may avoid the afore‐mentioned problems. However supplementation of these vitamins to excessive levels may cause harm to the skeletal system (osteoporosis and fractures) and liver abnormality in children with and without CF (Graham‐Maar 2006; Penniston 2006; Sethuraman 2006).
Why it is important to do this review
Fat‐soluble vitamin supplementation varies between CF centres with differing guidelines and no uniform approach, both within regions and internationally. While vitamin A deficiency may be a problem, excess supplementation causing chronic hypervitaminosis A may also occur. Furthermore, it is not known whether there is a beneficial or harmful effect of carotene supplementation in people with CF. Thus a systematic review on the efficacy of vitamins A, D, E, K and antioxidant supplementation in children and adults with CF in preventing effects of the deficiency of these micronutrients would help guide clinical practice. Supplementation of vitamins D, E and K and other antioxidants has been addressed in other Cochrane Reviews (Ciofu 2014; Ferguson 2014; Jagannath 2017; Okebukola 2017). This review will evaluate vitamin A, carotene and other retinoid supplementation in children and adults with CF. This version of the review is an update of previous versions (Bonifant 2012; Bonifant 2014; O'Neil 2008).
Objectives
To determine if, in children and adults with CF, vitamin A, carotene and other retinoid supplementation:
reduces the frequency of vitamin A deficiency disorders;
improves general and respiratory health;
affects the frequency of vitamin A toxicity.
Methods
Criteria for considering studies for this review
Types of studies
Randomised (RCTs) and quasi‐RCTs. We will assess cross‐over trials on a case‐by‐case basis and inclusion will depend on the data available given the potential for carry‐over effects of treatment.
Types of participants
Children or adults with CF (defined by sweat tests or genetic testing) with and without pancreatic insufficiency.
Types of interventions
All preparations of oral vitamin A, carotene or other retinoids used as a supplement compared to either no supplementation or placebo at any dose for at least three months.
Types of outcome measures
Primary outcomes
-
Vitamin A deficiency disorders
visual impairment
any other ocular dysfunction
skin manifestations
-
Growth and nutritional status
weight (kg and z score)
height (cm and z score)
body mass index (BMI)
Mortality
Secondary outcomes
-
Respiratory outcomes
bronchiectasis severity control (Likert scale, visual analogue scale or radiological score (Marchant 2001))
-
lung function indices
forced expiratory volume in one second (FEV1)
forced vital capacity (FVC)
proportions of participants who had respiratory exacerbations or hospitalisations or both
total number of hospitalised days or days off work or school
Quality of life
Adverse events (including vomiting, loss of appetite, osteoporosis, fractures and any other adverse event noted)
Possible toxicity events
Measured levels of vitamin A, carotenes or other retinoids
We planned to evaluate outcomes based on:
short term (12 months or less); and
medium to long term (longer than one year).
Search methods for identification of studies
We searched for all relevant published and unpublished trials without restrictions on language, year or publication status.
Electronic searches
Previous versions of this review did not include carotene in the search terms (Bonifant 2012; Bonifant 2012; O'Neil 2008). In this updated review, we identified relevant studies from the Group's Cystic Fibrosis Trials Register using the terms: Vitamin A OR *carotene OR retin*.
The Cystic Fibrosis Trials Register is compiled from electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL) (updated each new issue of the Cochrane Library), weekly searches of MEDLINE, a search of Embase to 1995 and the prospective handsearching of two journals ‐ Pediatric Pulmonology and the Journal of Cystic Fibrosis. Unpublished work is identified by searching through the abstract books of three major cystic fibrosis conferences: the International Cystic Fibrosis Conference; the European Cystic Fibrosis Conference and the North American Cystic Fibrosis Conference. For full details of all searching activities for the register, please see the relevant sections of the Cystic Fibrosis and Genetic Disorders Group website.
Date of the most recent search of the Group’s Cystic Fibrosis Trials Register: 01 June 2018.
We also searched the following trials registries:
US National Institutes of Health Ongoing Trials Register Clinicaltrials.gov (www.clinicaltrials.gov; searched 09 June 2018);
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (apps.who.int/trialsearch; 09 June 2018);
International Standard Randomised Controlled Trial Number (ISRCTN) Registry (www.isrctn.com; searched 09 June 2018).
For details of our search strategies, please see Appendix 1.
Searching other resources
We checked the bibliographies of included studies and any relevant systematic reviews identified for further references to relevant trials.
Data collection and analysis
The authors applied the process described below for data collection and analysis:
Selection of studies
From the title and abstract, two authors (JdV, JM) independently reviewed results of the literature searches to identify studies potentially relevant for further assessment. From these studies, the same two authors independently examined the papers in further detail in order to select studies for inclusion using the criteria stated above. The authors resolved disagreement by third party adjudication by another review author (AC).
Data extraction and management
The authors (JdV, JM) reviewed studies that satisfied the inclusion criteria and independently extracted data on the outcomes described as follows: study setting; year of study; source of funding; participant recruitment details (including number of eligible participants); inclusion and exclusion criteria; randomisation and allocation concealment method; numbers of participants randomised; blinding (masking) of participants, care providers and outcome assessors; dose and type of intervention; duration of therapy; co‐interventions; numbers of participants not followed up; reasons for withdrawals from study protocol (clinical, side effects, refusal and other); side effects of therapy; and whether intention‐to‐treat analyses were possible.
The authors planned to evaluate outcomes based on short term (12 months or less) and medium to long term (longer than one year), but due to data availability actually presented data at three months and six months.
If, in future updates of this review, we extract data from studies on various supplements, outcome measures from different types of supplementation (vitamin A, carotenes and other retinoids) we will analyse these separately.
Assessment of risk of bias in included studies
Two review authors (JdV, JM) independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We planned to resolve any disagreements by discussion or by involving another review author (AC). The review authors assessed the risk of bias according to the following domains:
random sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting; and
other bias.
The review authors graded each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for the judgment in the 'Risk of bias' (RoB) table. We then summarised the risk of bias judgements across different studies for each of the domains listed. We planned to blind separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality may be very different than for a patient‐reported pain scale). Where information on risk of bias related to unpublished data or correspondence with a study author, we noted this in the 'Risk of bias' table.
When considering treatment effects, the review authors took into account the risk of bias for the studies that contributed to that outcome.
Measures of treatment effect
The review authors planned to analyse continuous outcomes (growth and nutritional status, respiratory outcomes, quality of life scores, and levels of vitamin A, carotenes or other retinoids) as the mean relative change from baseline for each group or mean post‐treatment or post‐intervention values and standard deviation (SD). We were only able to analyse the post intervention values in this version of the review. We then calculated a pooled estimate of treatment effect by the mean difference and 95% confidence intervals (CIs) using RevMan software (RevMan 2014).
No data were available for dichotomous outcomes (vitamin A deficiency disorders, mortality, adverse events and toxicity events). If such data becomes available in future updates of the review, the review authors will calculate the odds ratio (OR) and 95% CIs using a modified ITT analysis, i.e. if the original investigators did not use ITT analysis, they will consider dropouts to be failures. The authors will calculate numbers‐needed‐to‐treat (NNT) and their 95% CIs from the pooled OR and its 95% CIs for a specific baseline risk, which is the sum of all the events in the control groups (in all studies on that type of supplementation) divided by the total participant numbers in control groups in all studies on that type of supplementation using an online calculator (Cates 2003).
Unit of analysis issues
We will assess cross‐over trials on a case‐by‐case basis and inclusion will depend on the data available given the potential for carry‐over effects of treatment. Cross‐over trials with dichotomous outcomes require more complicated analysis methods and for this the authors will consult with a statistician (Elbourne 2002).
Dealing with missing data
We requested further information from the primary investigators (where required).
Assessment of heterogeneity
Since only one study was included, no heterogeneity between studies could be assessed. When more studies are added to future versions of this review, we will describe any heterogeneity between study results and test this to see if it reaches statistical significance using a Chi² test. We will consider heterogeneity to be significant when the P value is less than 0.10 (Higgins 2011). The authors also plan to use the I² statistic to measure heterogeneity among the trials in each analysis, where heterogeneity is categorised such that a value of under 25% is considered low, around 50% is considered moderate and over 75% is considered a high degree of heterogeneity (Higgins 2003).
Data synthesis
We analysed the data using a fixed‐effect model. However, in future updates of the review we will use the random‐effects model whenever there are concerns about statistical heterogeneity.
Subgroup analysis and investigation of heterogeneity
We had planned to perform the following subgroup analyses to investigate any heterogeneity identified but were unable to do so as only one study was included:
children (aged 18 years or less) and adults (over 18 years);
formulations of the vitamin (single or multivitamin);
vitamin A and vitamin A‐like (carotenes or other retinoids) supplementation;
presence of pancreatic insufficiency.
Sensitivity analysis
The review authors also planned to use sensitivity analyses to evaluate treatment effect by excluding trials with an high risk of bias (either as judged overall or for the specific domains of selection bias and blinding).
Summary of findings table
In a post hoc change, we created a 'Summary of findings' table with the following outcomes included (Table 1).
Vitamin A deficiency disorders
Growth and nutritional status
Mortality
FEV1 (% predicted)
Antibiotic days per participant in past three months
Adverse events
Based on the GRADE approach, we assessed the following factors influencing the quality level of the body of evidence of the included study.
Limitations in the design and implementation
Indirectness of evidence
Unexplained heterogeneity or inconsistency of results
Imprecision of results
High probability of publication bias
We justified all decisions to upgrade or downgrade the assessed quality of the currently only included study in footnotes. Since we were not able to include any studies comparing vitamin A supplementation with placebo in people with CF, we did not generate a summary of findings table for this comparison.
Results
Description of studies
Results of the search
The conducted search returned 14 references to six studies (Cobanoglu 2002; Garić 2015; Homnick 1995; NCT01859390; Rust 1998; Wood 2003). Full‐text papers were available for four studies. One study had only been published in the form of three abstracts; however, the authors kindly provided their unpublished manuscript including supplemental material (Garić 2015). The flow of studies through the screening process of the review is presented in a flow diagram (Figure 1).
1.
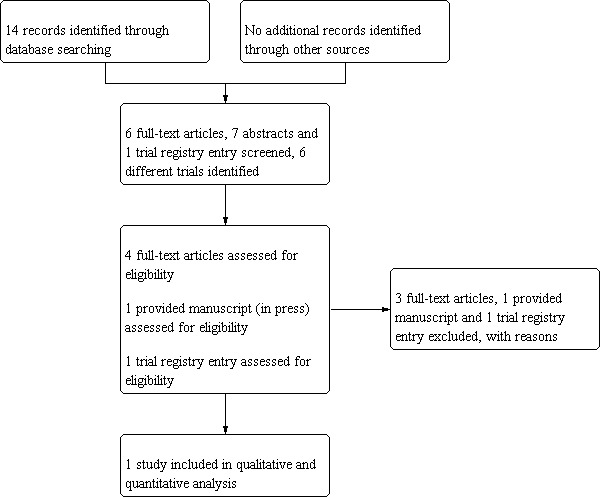
Study flow diagram
Included studies
Please see Characteristics of included studies.
No studies of vitamin A or other retinoid supplementation that fulfilled the inclusion criteria were identified. One study on β‐carotene supplementation was included in this review (Rust 1998).
Trial design
The included study was conducted in a single centre in Vienna, Austria with a duration of six months.
Participants
The study randomised 24 people (adults and children) with CF and included a cohort of 14 age‐matched healthy controls (data for this cohort not included in this review). The age of participants ranged from 6.7 years to 27.7 years; 25% of participants were male.
Interventions
Rust and colleagues compared β‐carotene supplementation to placebo. The β‐carotene supplementation group received a high‐dose supplementation of 1 mg/kg/day β‐carotene (maximum 50 mg/day) for 12 weeks, followed by a weight‐independent low‐dose supplementation of 10 mg/day β‐carotene for a further 12 weeks. The placebo group received starch‐containing placebo capsules of identical appearance as the β‐carotene supplementation capsules for 24 weeks. All participants remained on any regular daily supplementation with multivitamins and pancreatic enzymes during the study period.
Outcomes
Relevant data reported for this review were anthropometric outcome measures, respiratory outcome measures, adverse events and plasma concentrations of vitamin A and β‐carotene.
Excluded studies
Please see Characteristics of excluded studies.
Five studies were excluded (Cobanoglu 2002; Garić 2015; Homnick 1995; NCT01859390; Wood 2003). One study was excluded since β‐carotene supplementation doses were individually adjusted based on β‐carotene plasma concentrations and no placebo supplementation was described (Homnick 1995). A second study was excluded due to the lack of an appropriate control group as all children with CF received the same intervention (Cobanoglu 2002). Furthermore, in two studies participants received combined supplements rather than just vitamin A (NCT01859390; Wood 2003). The double‐blind placebo‐controlled study of fenretinide supplementation (an escalating daily dose schedule versus placebo) was excluded since the duration of supplementation at each dose level was only three weeks (outside our inclusion criteria) (Garić 2015).
Risk of bias in included studies
The only included study was judged as having a unclear risk of bias overall (Rust 1998). Further details regarding different domains of bias are described under the subheadings below, in the risk of bias summary (Figure 2) and in the risk of bias table below the 'Characteristics of included studies' table.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for the included study.
Allocation
The risk of allocation bias is determined to be unclear, as neither the method of generation of the randomisation sequence, nor the method of allocation concealment were described in the included study (Rust 1998).
Blinding
The risk associated with participant blinding was deemed to be low since the capsules for both supplements and placebo were identical. However, the risk of detection bias due to inadequate blinding was considered to be unclear, as it was not stated if the outcome assessor was blinded (Rust 1998).
Incomplete outcome data
The included study was assessed as having a unclear risk of attrition bias, as the authors did not mention explicitly how they dealt with dropouts. However, 24 participants were analysed at baseline and post‐intervention; hence, although details on compliance were not provided, the study either used an intention‐to‐treat analysis or had no dropouts. (Rust 1998).
Selective reporting
The risk of reporting bias was considered high in the included study, since not all outcome measures are reported at each endpoint (growth and nutritional status not reported post high‐dose supplementation) (Rust 1998). The authors specifically define pulmonary exacerbations and symptoms, but the prevalence of those exacerbations and symptoms is only reported indirectly, reflected in the amount of days on which systemic antibiotics were prescribed. Furthemore, modified Shwachmann‐Kulczycki scores were measured on a monthly basis but only baseline values were reported, although the authors did mention there were no statistical significant differences. Also, differences in the data for some outcome measures were identified in various manuscripts reporting the same study and same study population.
Other potential sources of bias
The risk of other potential bias was judged as high. Besides a typical history of CF and sweat chloride levels over 60 mEq/L, no further inclusion or exclusion criteria were stated; it was also not stated whether participants were immunocompetent or if any were post‐transplant (potential for selection bias). The investigators measured the Shwachmann‐Kulczycki score without its included radiographical assessment as a clinical outcome measure; this is a modified version of the instrument that has not been validated.
With regards to study design, the sample size in the included study is small and no power calculations were mentioned. Furthermore, the included study had a multi‐dose design with no washout period after the high‐dose supplementation and before the low‐dose supplementation and it is unclear whether this introduced any bias to the results. Since the half‐time of β‐carotene in plasma in healthy individuals is at least a week (Burri 2001; Dueker 2000; Thürmann 2002; Wise 2009), the entire low‐dose supplementation period would be expected to be influenced by previous high‐dose supplementation and results should be interpreted with caution.
Finally, no declaration of interest was stated, nor any details about funding, thus there is an unclear risk of bias due to these issues.
Effects of interventions
See: Table 1
Vitamin A supplementation
The authors did not find any eligible studies on vitamin A supplementation that fulfilled the inclusion criteria.
Carotene supplementation
One study (24 participants) on carotene supplementation was eligible for inclusion (Rust 1998). Data were limited and we contacted the investigators for additional information; unfortunately, although a reply was received, no further information could be provided. We judged the study to have an unclear risk of bias due to its design. Since no adequate washout period prior to low‐dose supplementation was implemented, outcome measures at the endpoint directly post low‐dose supplementation should be interpreted with caution (see Data and analyses; Table 1).
Primary outcomes
1. Vitamin A deficiency disorders
The only included study did not report on any vitamin A deficiency disorders (Rust 1998).
2. Growth and nutritional status
a. weight
No separate analysable weight data were reported.
b. height
After 24 weeks of β‐carotene supplementation (12 weeks at a high dose followed by 12 weeks at a low dose), there was no statistical significant difference in the z score for height between the supplementation and the placebo groups, MD ‐0.23 (95% CI ‐0.89 to 0.43) (low‐quality evidence) (Analysis 1.1).
1.1. Analysis.

Comparison 1: β‐carotene supplementation versus placebo, Outcome 1: Growth and nutritional status: z score for height
c. BMI
Additionally, the authors reported no significant group differences or time‐trends for measurements of BMI. No data were reported post high‐dose supplementation. Quantitative data on BMI were requested but not available.
3. Mortality
The included study did not report on mortality (Rust 1998).
Secondary outcomes
1. Respiratory outcomes
a. Bronchiectasis severity control
The included study did not report on bronchiectasis severity control (Rust 1998).
b. Lung function indices
i. FEV1
No statistical significant difference in FEV1 (% predicted) was observed between the β‐carotene supplementation and the placebo groups at either three months (post high dose), MD ‐10.6% (95% CI ‐31.1 to 9.9) or six months (post low dose), MD ‐10.3% (95%CI ‐31.6 to 110.0), both results judged to be low‐quality evidence (Analysis 1.2).
1.2. Analysis.

Comparison 1: β‐carotene supplementation versus placebo, Outcome 2: Respiratory outcomes: FEV1 (% predicted)
ii. FVC
The included study did not report on FVC (Rust 1998).
c. Proportions of participants who had respiratory exacerbations or hospitalisations or both
The included study measured this outcome in terms of the number of days per person on which systemic antibiotics were used in three‐month blocks (three months prior to baseline, baseline to three months and three months to six months). At three months (post high dose β‐carotene supplementation) a statistical significant difference was observed between the supplementation group and the placebo group, MD ‐15.00 days (95% CI ‐27.60 to ‐2.40) (low‐quality evidence) (Analysis 1.3). This effect was not maintained during the low‐dose supplementation, as seen at the six‐month time‐point, which should be interpreted carefully since for this outcome a carry‐over effect would have been present, MD ‐8.00 days (95% CI ‐18.80 to 2.80) (low‐quality evidence).
1.3. Analysis.

Comparison 1: β‐carotene supplementation versus placebo, Outcome 3: Respiratory outcomes: antibiotic days per patient in past 3 months
d. Total number of hospitalised days or days off work or school
The included study did not report on the number of hospitalised days or days off work or school (Rust 1998).
2. Quality of life
The included study did not report on quality of life (Rust 1998).
3. Adverse events
In the included study, the authors reported that no adverse events were observed (low‐quality evidence) (Rust 1998).
4. Possible toxicity events
The included study did not report on any toxicity events, although the authors stated that no risk of vitamin A toxicity could be detected since vitamin A plasma levels stayed in the lower normal range during the entire study (Rust 1998).
5. Measured levels of vitamin A, carotenes or other retinoids (or both)
Data showed that β‐carotene supplementation did not seem to affect vitamin A plasma levels post high‐dose supplementation, MD ‐0.10 µmol/L (95% CI ‐0.31 to 0.11) and minimal post low‐dose supplementation, MD 0.20 µmol/L (95% 0.04 to 0.36) (Analysis 1.4). Plasma levels of β‐carotene were significantly higher following high‐dose β‐carotene supplementation compared to levels in the placebo group, MD 0.49 µmol/L (95% CI 0.28 to 0.70) (Analysis 1.5). This effect was partly sustained at the end of the following three‐month low‐dose supplementation, MD 0.26 µmol/L (95% CI 0.15 to 0.37) (Analysis 1.5). Although discrepancies between the different papers from this study on the reported β‐carotene plasma levels after four weeks have been identified, no discrepancies in measured levels at the endpoints were observed.
1.4. Analysis.

Comparison 1: β‐carotene supplementation versus placebo, Outcome 4: Plasma concentrations: vitamin A [µmol/L]
1.5. Analysis.

Comparison 1: β‐carotene supplementation versus placebo, Outcome 5: Plasma concentrations: β‐carotene [µmol/L]
Other retinoid supplementation
No studies on other retinoid supplementation were eligible for inclusion.
Discussion
Summary of main results
In this updated review, there were no studies on vitamin A or other retinoid supplementation for people with CF eligible for inclusion. A single study on β‐carotene supplementation included at the 2018 update showed positive effects on some of the defined outcome measures for this review (Rust 1998). However, the strength of evidence for this included study is considered low (Table 1) (Figure 2), mainly due to study design, unclear description of methods and outcome reporting, and small study population. Nevertheless, the study found that with high‐dose β‐carotene supplementation significantly fewer days of systemic antibiotics were required for treating pulmonary exacerbations compared to controls, a finding that was not sustained during low‐dose supplementation. In addition, as one would expect, β‐carotene supplementation resulted in higher β‐carotene plasma levels. No statistically significant effect on any other clinical outcome measures was shown.
Overall completeness and applicability of evidence
It is well accepted that people with CF and pancreatic insufficiency are at risk of vitamin A deficiency. However, this is now a rare occurrence (Brei 2013). It is also biologically plausible that currently, with improved pancreatic replacement therapies and attention to macronutrition and caloric supplements, the majority of people with CF are vitamin A sufficient and may not require daily vitamin A supplementation. Despite this, daily vitamin A supplementation is almost universally recommended for people with CF who are pancreatic insufficient (Graham‐Maar 2006; Royal Brompton Hospital 2017; Saxby 2017). Whether or not there is a beneficial or harmful effect of this vitamin A supplementation in people with CF remains unknown. Since no studies of vitamin A supplementation were included in this review, no conclusions regarding vitamin A supplementation can be made.
Supplementation with β‐carotene is currently not recommended in people with CF (Saxby 2017); no convincing evidence of clinical benefit from β‐carotene supplementation in people with CF was demonstrated; a conclusion shared by Ciofu and colleagues, who reviewed antioxidant supplementation, including β‐carotene supplementation, in people with CF (Ciofu 2014). Although the authors of the included study recommend routine β‐carotene supplementation in people with CF, the results of our data analysis do not convincingly support this. It has been shown that β‐carotene supplementation is effective in correcting imbalance of markers of oxidative stress in people with CF, yet the clinical benefit of this correction has not been proven (Galli 2012).
Since no studies of other retinoid supplementation were included in this review, no conclusions regarding these supplements can be made.
A potential limitation is the fact that oxidative stress parameters are not included in the outcome measures (see Types of outcome measures). Although β‐carotene supplementation, a known antioxidant, is included, other oxidative stress markers (e.g. lipid peroxidation products and trolox equivalent antioxidative capacity) are not included. This decision was deliberate as plasma antioxidant status, and hence oxidative stress markers, are not directly related to improvement in clinical important outcome measures in CF (Ciofu 2014; Galli 2012).
In summary, this updated Cochrane Review has added results from one small single‐centre study (Rust 1998). There is an unclear risk of potential bias within the data, particularly for outcomes post low‐dose supplementation due to the study design. Hence, although data analysis partly supports supplementation in terms of need for antibiotics and plasma levels of β‐carotene, this review provides only limited evidence that β‐carotene supplementation in people with CF may be beneficial.
Quality of the evidence
With no studies on vitamin A or other retinoid supplementation eligible for inclusion and only one small study (n = 24) on β‐carotene supplementation included, the overall quality of the evidence is considered low. As described above in more detail, the included study was not free of bias, mainly due to its design and the unclear description of methods and outcome reporting. This is also reflected in the quality assessments for the evidence presented in the included study using the GRADE approach (Table 1). Since the overall quality of the evidence is considered low, the ability to draw any robust conclusions on β‐carotene supplementation is limited.
Potential biases in the review process
To reduce potential biases, two authors (JM, JdV) assessed all potentially eligible studies individually. The data extraction and risk of bias assessments were also independently undertaken by the same two authors and when disagreement existed, an independent third author adjudicated (AC). No external potential sources of bias exist for any authors.
Agreements and disagreements with other studies or reviews
While vitamin A deficiency causes eye and skin disorders, excess vitamin A can also cause problems (Griffiths 2000; Penniston 2006). Indeed, increasingly data on micronutrients have shown that micronutrient supplementation is only beneficial in states of deficiency and harmful when no deficiency exists (Chang 2006; Shenkin 2006). For vitamin A, Griffiths has termed this the 'vitamin A paradox' as vitamin A supplementation is likely to be "protective against pneumonia in malnourished children (who are likely to be vitamin A‐deficient) and is paradoxically detrimental for adequately nourished children" (Griffiths 2000). Vitamin A supplementation following current regimens leads to adequate intake levels of vitamin A, but levels exceeding the recommended upper level are not uncommon (Brei 2013; Graham‐Maar 2006; Li 2016; Maqbool 2008). Thus, some have called for individualised supplementation based on annual measurements rather than a fixed dosage, as is currently recommended in most CF guidelines (Borowitz 2002; Royal Brompton Hospital 2017; Saxby 2017).
Current guidelines do not specify whether the water‐soluble or the fat‐soluble form of retinol should be administered, but water‐soluble preparations present more risks of excess vitamin A levels to people with CF with pancreatic insufficiency, due to the easier absorption of the water‐soluble preparations compared to the fat‐soluble preparations (Brei 2013). Unfortunately, since no randomised clinical studies on vitamin A supplementation in CF were identified, the authors cannot draw any conclusions about the benefits of vitamin A supplementation in CF, nor whether supplementation should be administered as an individualised or a fixed dosage and whether this should be fat‐ or water‐soluble preparations.
There is currently no recommendation for β‐carotene supplementation in people with CF (Saxby 2017). A β‐carotene deficiency (either in CF or the general population) has not been defined, although it has been reported that children with CF display 9% to 24% of the normal serum carotenoid concentration and increased markers of oxidative stress (Cantin 2007). The authors of a systematic review on antioxidant supplementation in CF, which also includes non‐randomised studies, concluded that normalizing β‐carotene concentrations is effective in correcting oxidative stress markers and is associated with minor clinical improvements (Galli 2012). The Cochrane Review of antioxidant supplementation in CF found no positive treatment effect of any of the antioxidant micronutrients on any clinical outcomes (Ciofu 2014). As they did not look at β‐carotene supplementation alone, no conclusions about its use can be made.
Finally, it is not known whether supplementation with other retinoids is beneficial in children with CF or not. A randomised study showed that fenretinide supplementation corrects the inflammatory‐related imbalance between long chain and very long chain ceramides in CF compared to healthy controls within two weeks (Garić 2015). So far no clinical outcomes have been reported, hence further research into fenretinide supplementation is needed to determine any clinical benefits.
Authors' conclusions
Implications for practice.
As there were no randomised or quasi‐randomised controlled studies on vitamin A or retinoid supplementation included, we cannot draw any conclusions on the benefits (or otherwise) of regular administration of these supplements in people with cystic fibrosis (CF). In addition, although beta (β)‐carotene supplementation was beneficial in one clinical outcome measure (need for antibiotics), interpretation should be cautious due to methodological limitations, restraining the ability to draw clear conclusions. Until further data are available, country‐ or region‐specific guidelines (e.g. UK CF Trust Nutrition Guidelines (CF Trust 2016)) on the use and monitoring of vitamin A, carotenes or other retinoids in people with CF should be followed.
Implications for research.
There is an obvious need for a well‐designed, adequately‐powered, multicentre, parallel, randomised controlled study to assess if vitamin A or vitamin A‐like (carotenes or other retinoids) supplementation, in children and adults with CF is beneficial or otherwise. The study should examine if the administered supplementations positively or negatively influence the frequency of symptoms of vitamin A deficiency or general and respiratory outcomes. The possible negative effects should be examined in light of recent data showing possible harm when micronutrients are used in people who are not micronutrient‐deficient. Safety monitoring during such a study would be important as the current practice is to use supplementation of vitamin A in people with CF. Vitamin A levels should be measured before and during the studies when clinically stable and related to serum albumin and retinol binding protein. Studies involving both children and adults are required and results should be related to nutritional status and pancreatic status. Data relating to appropriate dose, frequency of supplementation and type of formulation of vitamin A, retinoids or carotenes are also needed. However, it is unlikely that well‐designed, randomised studies will be conducted in near future, given the costs involved and current CF research priorities. Furthermore, current widespread practice is to prescribe multivitamin preparations to people with CF, raising logistical problems for future studies to administer solely preparations of vitamin A. Thus, to examine the effect of vitamin A, retinoid or carotene supplementation in people with CF, evidence may come inevitably from studies with different designs (pro‐ and retrospective cohort studies) leading to less robust quality evidence.
What's new
| Date | Event | Description |
|---|---|---|
| 12 May 2020 | Amended | The authors of the review are not aware of any further research in this field and will not be updating this review at this time. They plan to revisit their decision in two years time (2022). |
History
Protocol first published: Issue 4, 2007 Review first published: Issue 1, 2008
| Date | Event | Description |
|---|---|---|
| 17 July 2018 | New search has been performed | Placebo‐controlled studies of carotenes or retinoids other than vitamin A are now also eligible for inclusion. A new search with extended search terms of the Cystic Fibrosis and Genetic Disorders Review Group's Cystic Fibrosis Trials Register identified 13 references to five studies. An additional search of trials registries identified one ongoing study. One study with seven references has been included in this review (Rust 1998) and the remaining studies have been excluded (Cobanoglu 2002; Garić 2015; Homnick 1995; NCT01859390; Wood 2003). The format of the plain language summary has been updated in line with current guidance and a summary of findings table has been added. |
| 17 July 2018 | New citation required and conclusions have changed | While our original conclusions on vitamin A supplementation have not changed, new conclusions on the use of carotenes or retinoids supplementation have been drawn. The author team has been expanded with two new authors, Jorrit de Vries and Julie Marchant. |
| 6 May 2014 | New search has been performed | A search of the Group's Cystic Fibrosis Trials Register did not identify any new studies potentially eligible for inclusion in this review. |
| 6 May 2014 | New citation required but conclusions have not changed | No new studies were included so the conclusions of the review have not changed. |
| 7 June 2012 | New citation required but conclusions have not changed | No new studies were included so the conclusions of the review have not changed. |
| 7 June 2012 | New search has been performed | A search of the Group's Cystic Fibrosis Trials Register did not identify any new references potentially eligible for inclusion in this review. |
| 1 December 2009 | New search has been performed | A search of the Group's Cystic Fibrosis Trials Register identified a single reference which was excluded (Wood 2003). |
| 12 August 2009 | Amended | Contact details updated. |
| 10 April 2008 | New search has been performed | A search of the Group's Cystic Fibrosis Trials Register did not identify any trials which might be eligible for inclusion in this review. |
| 10 April 2008 | Amended | Converted to new review format. |
Acknowledgements
We thank Nikki Jahnke, Dr Gerard Ryan and Dr Karen Robinson from the Cochrane Cystic Fibrosis and Genetic Disorders Group for their advice, supportive role and comments to the protocol and review and to Natalie Hall for help with the searches.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Cystic Fibrosis and Genetic Disorders Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Electronic searches
| Database/ Resource | Strategy |
| Clinicaltrials.gov (Clinicaltrials.gov) |
Vitamin A OR *carotene OR retin* |
| WHO ICTRP (apps.who.int/trialsearch/) |
Vitamin A OR *carotene OR retin* |
| ISRCTN Registry (www.isrctn.com/) |
Vitamin A OR *carotene OR retin* |
Data and analyses
Comparison 1. β‐carotene supplementation versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Growth and nutritional status: z score for height | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1.1 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2 Respiratory outcomes: FEV1 (% predicted) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.1 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.2 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3 Respiratory outcomes: antibiotic days per patient in past 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.1 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.2 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4 Plasma concentrations: vitamin A [µmol/L] | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4.1 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4.2 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.5 Plasma concentrations: β‐carotene [µmol/L] | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.5.1 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.5.2 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Rust 1998.
| Study characteristics | ||
| Methods | Randomised placebo‐controlled clinical study. Parallel design. Duration: 6 months. Location: single‐centre pilot study conducted in Vienna, Austria. |
|
| Participants |
Total cohort (n = 24) Age (mean (SD)): 12.8 (6.3) years (range: 6.7 to 27.7 years). Gender split: 25% male. Supplementation group (n = 13) Age (mean (SD)): 14.6 (7.7) years. Gender split: 30.7% male. Placebo group (n = 11) Age (mean (SD)): 10.5 (4.0) years. Gender split: 18.2% male. |
|
| Interventions |
Supplementation group: weeks 1 ‐ 12: 1x daily 1 mg/kg β‐carotene (maximum 50 mg/day) (high dose); weeks 13 ‐ 24: 1x daily 10 mg β‐carotene (low dose). Placebo group: weeks 1 ‐ 24: starch‐containing capsules of identical appearance as β‐carotene capsules. Participants continued taking previous daily supplementation with multivitamins (1 mg ‐ 2 mg retinol, 50 mg ‐ 200 mg ascorbate, 110 mg ‐ 400 mg α‐tocopherol) and pancreatic enzymes during the study period. |
|
| Outcomes | ‐ Growth and nutritional status (z score for height, body mass index (no quantitative data post intervention)). ‐ Respiratory outcomes (FEV1 (% predicted), frequency of pulmonary exacerbations: number of days per person on which systemic antibiotics were used in previous 3‐month block). ‐ adverse events. ‐ plasma concentrations of vitamin A and β‐carotene. Furthermore, total antioxidative capacity, several plasma concentrations (α‐carotene, cholesterol adjusted α‐tocopherol, lycopene, γ‐tocopherol, urate, bilirubin, albumin, glutathione and malondialdehyde) and Shwachmann‐Kulczycki score without X‐ray (measured monthly, but only reported at baseline) were reported. |
|
| Funding source | No declaration of interest stated, nor any details about funding. | |
| Notes | Since there was no adequate washout period after high dose supplementation (1 mg/kg/day β‐carotene), outcomes post low‐dose supplementation (1x daily 10 mg β‐carotene) should be interpreted very cautiously. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated, authors only state: "Thirteen patients … were randomised to receive β‐carotene supplementation". |
| Allocation concealment (selection bias) | Unclear risk | Concealment method for sequence allocation not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Authors state: "To conceal treatment all patients received capsules of identical appearance". Whether or not personnel were blinded is not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is not stated whether or not outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The authors did not mention explicitly if there were any dropouts or whether an intention‐to‐treat analysis has been used. 24 participants were analysed at baseline and post‐intervention, but, although assessed, details on compliance were not provided |
| Selective reporting (reporting bias) | High risk | Not all outcome measures reported at each endpoint (growth and nutritional status not reported post high‐dose supplementation). Furthemore, for monthly measured modified Shwachmann‐Kulczycki scores, only baseline values were reported, although the authors mentioned there were no statistical significant differences. The authors specifically define pulmonary exacerbations and its symptoms, but the prevalence of those exacerbations and symptoms is not reported, only indirect measurements by the amount of days on which systemic antibiotics were prescribed. There are discrepancies in the reporting different data for some outcome measures by various manuscripts reporting on the same study and study population. For example, in the first paper published by Rust in 1998, mean (SD) β‐carotene plasma levels are reported to be 0.6 (0.3) µmol/L, which is presented in a later paper by Renner in 2001 as 0.51 (0.30) µmol/L. |
| Other bias | High risk |
Unclear risk Besides a typical history of CF and sweat chloride levels > 60 mEq/L, no further inclusion or exclusion criteria were stated. Not stated whether participants were immunocompetent or if any were post‐transplant. Also, no declaration of interest or details of funding source stated. The sample size is small and no power calculations were described, therefore, the risk of bias due to a lack of power is considered unclear. High risk The authors monthly measured the Shwachmann‐Kulczycki score without radiographical assessment as a clinical outcome measure; a modified version of this instrument, that has not been validated. There was no washout period used after the high‐dose period and before the low‐dose period, but data were only reported at the end of the study compared to baseline leading to a risk of bias from the study design and outcome measures post low‐dose supplementation should be interpreted very cautiously. |
CF: cystic fibrosis FEV1: forced expiratory volume in one second SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cobanoglu 2002 | Open study which examined the outcomes of several blood markers (inflammatory and antioxidant) and pulmonary function indices in 15 children with CF and 12 children with non‐CF bronchiectasis, receiving oral β‐carotene supplementation (3x daily mean (SD) 0.69 (0.19) mg/kg). All children with CF received the same intervention, there was no relevant control group. |
| Garić 2015 | Phase 1b trial examining the safety of a novel oral solid dosage form of fenretinide in people with CF (n = 15) (escalating daily dose schedule versus placebo), but of insufficient duration (3 weeks at each dose level). |
| Homnick 1995 | Open study measuring several anthropometric and laboratory outcomes for β‐carotene supplementation in 13 people with CF, either assigned to a supplementation group (n = 5) or control group (n = 8). Participants did not receive a constant level of supplementation: initially the level was 2x daily 30 mg β‐carotene which was then individually and periodically increased up to 240 mg/day in order to achieve β‐carotene plasma concentrations of 0.37 to 0.74 µmol/L; no placebo supplementation in control group described. |
| NCT01859390 | Comparison of the effects of a modified formulation of AquADEKs (a multivitamin supplement) versus a traditional AquaDEKs, but not solely vitamin A or β‐carotene. |
| Wood 2003 | Intervention not relevant. Randomised controlled study of 46 people with CF comparing a low dose of a combined supplement (10 mg vitamin E and 500 µg vitamin A)) to a high dose of a different combined supplement (200 mg vitamin E, 300 mg vitamin C, 25 mg β‐carotene, 90 µg Se, and 500 µg vitamin A). |
CF: cystic fibrosis SD: standard deviation
Differences between protocol and review
A post hoc decision was made to add β‐carotene and retinoids (other than vitamin A) into the review, since those are considered a form of vitamin A.
Contributions of authors
Protocol: CB and AC wrote the protocol. ES reviewed the protocol.
Original review: When any studies are identified, CB and AC will select relevant studies, perform data extraction and analysis and write the review. ES will contribute to writing of the review.
Updated reviews: JdV and JM selected relevant studies, performed data extraction and analysis for the updated review. JdV, JM and AC wrote the updated reviews.
Sources of support
Internal sources
Royal Children's Hospital Foundation, Brisbane, Australia
External sources
National Health and Medical Research Council, Australia
-
National Institute for Health Research, UK
This systematic review was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Cystic Fibrosis and Genetic Disorders Group.
Declarations of interest
Catherine Bonifant has no potential conflict of interest.
Anne Chang declares the receipt of a grant provided by GSK, which is, however, unrelated to this topic.
Elizabeth Shevill has no potential conflict of interest.
Jorrit de Vries has no potential conflict of interest.
Julie Marchant has no potential conflict of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Rust 1998 {published data only}
- Engl B, Rust P, Eichler I, Renner S, Elmadfa I. Bioavailability of therapeutic Beta-Carotine (BC) in patients with cystic fibrosis (CF) and effects on anthropometrical parameters over 6 months [Bioverfugbarkeit einer therapeutischen Beta-Carotin (BC) Gabe bei Patienten mit zystischer Fibrose (CF) und Auswirkungen auf anthropometrische Parameter uber eine Versuchsdauer von 6 Monaten]. Monatsschrift fur Kinderheilkunde 1997; 145:S 134. [CENTRAL: 336058] [CFGD REGISTER: GN69g] [Google Scholar]
- Renner S, Rath R, Rust P, Lehr S, Frischer T, Elmadfa I, et al. Effects of beta-carotene supplementation for six months on clinical and laboratory parameters in patients with cystic fibrosis. Thorax 2001; 56(1):48-52. [CENTRAL: 329478] [CFGD REGISTER: GN69f] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renner S, Wojnarowski C, Koller DY, Rust P, Elmadfa I, Eichler I. Patients with cystic fibrosis (CF) benefit from β-carotene supplementation for 6 months. Pediatric Pulmonology 1997; Suppl 14:314. [CENTRAL: 794966] [CFGD REGISTER: GN69a] [Google Scholar]
- Renner S, Wojnarowski C, Koller DY, Rust P, Elmadfa I, Eichler I. Patients with cystic fibrosis (CF) benefit from beta-Carotene supplementation for 6 months. In: 22nd European Cystic Fibrosis Conference; 1998 June 13-19; Berlin, Germany. 1998:97. [CENTRAL: 794967] [CFGD REGISTER: GN69b]
- Rust P, Eichler I, Elmadfa I. Influence of an oral beta-carotine-supplementation on the antioxidant status of patients with cystic fibrosis [Einfluss einer oralen beta-Karotin-Supplementierung auf den Antioxidantienstatus von Patienten mit zystischer Fibrose]. Atemwegs und Lungenkrankheiten 1997; 23:51. [CENTRAL: 255854] [CFGD REGISTER: GN69d] [Google Scholar]
- Rust P, Eichler I, Renner S, Elmadfa I. Effects of long-term oral beta-carotene supplementation on lipid peroxidation in patients with cystic fibrosis. International Journal for Vitamin and Nutrition Research 1998; 68(2):83-7. [CENTRAL: 208549] [CFGD REGISTER: GN69c] [PMID: ] [PubMed] [Google Scholar]
- Rust P, Eichler I, Renner S, Elmadfa I. Long-term oral beta-carotene supplementation in patients with cystic fibrosis - effects on antioxidative status and pulmonary function. Annals of Nutrition & Metabolism 2000; 44(1):30-7. [CENTRAL: 297191] [CFGD REGISTER: GN69e] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Cobanoglu 2002 {published data only}
- Cobanoğlu N, Ozçelik U, Göçmen A, Kiper N, Doğru D. Antioxidant effect of beta-carotene in cystic fibrosis and bronchiectasis: clinical and laboratory parameters of a pilot study. Acta Paediatrica 2002; 91(7):793-8. [CFGD REGISTER: GN99] [PMID: ] [DOI] [PubMed] [Google Scholar]
Garić 2015 {published and unpublished data}
- Garić D, De Sanctis J, Wojewodka G, Houle D, Cupri S, Hajduch M, et al. Fenretinide differentially modulates the levels of long- and very long-chain ceramides by downregulating Cers5 enzyme: evidence from bench to bedside. Journal of Molecular Medicine (Berlin, Germany) 2017; 95(10):1053-64. [DOI] [PubMed] [Google Scholar]
- Garic D, Wojewodka G, De Sanctis JB, Hajduch M, Kopriva F, Pislariu R, et al. Fenretinide treatment increases long chain ceramide C24:0 and decreases short chain ceramide C16:0 levels in patients with cystic fibrosis (phase IB clinical trial). Pediatric pulmonology 2015; 50 Suppl 41:291. [ABSTRACT NO: 264] [CFGD REGISTER: GN253b] [Google Scholar]
- Radzioch D, Wojewodka G, Cupri S, Colin P, Pislariu R, Garić D, et al. A novel oral formulation of fenretinide demonstrates safety and tolerability in a phase 1B dose-ascending trial involving adult cystic fibrosis patients. Pediatric Pulmonology 2015; 50 Suppl 41:290. [ABSTRACT NO: 261 ] [CFGD REGISTER: GN253c] [Google Scholar]
- Wojewodka G, Matouk E, De Sanctis JB, Pislariu R, Colin P, Matin C, et al. The cystic fibrosis associated fatty acid imbalance is corrected by a novel formulation of fenretinide in a phase 1B clinical trial. Pediatric Pulmonology 2015; 50 Suppl 41:289. [ABSTRACT NO: 260 ] [CFGD REGISTER: GN253a] [Google Scholar]
Homnick 1995 {published data only}
- Homnick DN, Spillers CR, Cox SR, Cox JH, Yelton LA, De Loof MJ, et al. Single- and multiple-dose response relationships of beta-carotene in cystic fibrosis. Journal of Pediatrics 1995; 127(3):491-4. [CFGD REGISTER: GN68] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT01859390 {published data only}
- NCT01859390. Effects of an antioxidant-enriched multivitamin supplement on inflammation and oxidative stress in cystic fibrosis (AquADEKs-2) [A multi-center, randomized, controlled, double-blind study of the effects of an antioxidant-enriched multivitamin supplement on inflammation and oxidative stress in cystic fibrosis patients]. clinicaltrials.gov/ct2/show/NCT01859390 (first received 21 May 2013).
Wood 2003 {published data only}
- Wood LG, Fitzgerald DA, Lee AK, Garg ML. Improved antioxidant and fatty acid status of patients with cystic fibrosis after antioxidant supplementation is linked to improved lung function. American Journal of Clinical Nutrition 2003; 77(1):150-9. [CFGD REGISTER: GN98] [PMID: ] [DOI] [PubMed] [Google Scholar]
Additional references
Bjelakovic 2013
- Bjelakovic G, Nikolova D, Gluud C. Meta-regression analyses, meta-analyses, and trial sequential analyses of the effects of supplementation with beta-carotene, vitamin A, and vitamin E singly or in different combinations on all-cause mortality: do we have evidence for lack of harm? PloS one 2013; 8(9):e74558. [DOI: 10.1371/journal.pone.0074558] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Borowitz 2002
- Borowitz D, Baker RD, Stallings V. Consensus report on nutrition for pediatric patients with cystic fibrosis. Journal of Pediatric Gastroenterology and Nutrition 2002; 35(3):246-59. [PMID: ] [DOI] [PubMed] [Google Scholar]
Brei 2013
- Brei C, Simon A, Krawinkel MB, Naehrlich L. Individualized vitamin A supplementation for patients with cystic fibrosis. Clinical Nutrition (Edinburgh, Scotland) 2013; 32(5):805-10. [DOI: 10.1016/j.clnu.2013.01.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Burri 2001
- Burri BJ, Neidlinger TR, Clifford AJ. Serum carotenoid depletion follows first-order kinetics in healthy adult women fed naturally low carotenoid diets. Journal of nutrition 2001; 131(8):2096-100. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cantin 2007
- Cantin AM, White TB, Cross CE, Forman HJ, Sokol RJ, Borowitz D. Antioxidants in cystic fibrosis. Conclusions from the CF Antioxidant Workshop, Bethesda, Maryland, November 11-12, 2003. Free Radical Biology and Medicine 2007; 42(1):15-31. [DOI: 10.1016/j.freeradbiomed.2006.09.022] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cates 2003 [Computer program]
- Visual Rx. Online NNT Calculator. Version 4. Cates C, 2016.Available at www.nntonline.net/.
CDC 2012
- Centers for Disease Control and Prevention. Second national report on biochemical indicators of diet and nutrition in the U.S. population 2012; 2012 April. www.cdc.gov/nutritionreport/report.html (accessed prior to 08 November 2017). [https://www.cdc.gov/nutritionreport/report.html]
CF Trust 2016
- UK Cystic Fibrosis Trust Nutrition Working Group. Nutritional management of cystic fibrosis. UK Cystic Fibrosis Trust Consensus Document on Nutritional Management 2016.
Chang 2006
- Chang AB, Torzillo PJ, Boyce NC, White AV, Stewart PA, Wheaton GR, et al. Zinc and vitamin A supplementation in Indigenous Australian children hospitalised with lower respiratory tract infection: a randomised controlled trial. Medical Journal of Australia 2006; 184(3):107-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ciofu 2014
- Ciofu O, Lykkesfeldt J. Antioxidant supplementation for lung disease in cystic fibrosis. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD007020.pub3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dodge 2006
- Dodge JA, Turck D. Cystic fibrosis: nutritional consequences and management. Best Practice & Research. Clinical Gastroenterology 2006; 20(3):531-46. [DOI: 10.1016/j.bpg.2005.11.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Druesne 2010
- Druesne-Pecollo N, Latino-Martel P, Norat T, Barrandon E, Bertrais S, Galan P, et al. Beta-carotene supplementation and cancer risk: a systematic review and meta-analysis of randomized controlled trials. International Journal of Cancer 2010; 127(1):172-84. [DOI: 10.1002/ijc.25008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dueker 2000
- Dueker SR, Lin Y, Buchholz BA, Schneider PD, Lamé MW, Segall HJ, et al. Long-term kinetic study of beta-carotene, using accelerator mass spectrometry in an adult volunteer. Journal of Lipid Research 2000; 41(11):1790-800. [PMID: ] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002; 31(1):140-9. [PMID: 11914310] [DOI] [PubMed] [Google Scholar]
Ferguson 2014
- Ferguson JH, Chang AB. Vitamin D supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD007298.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Galli 2012
- Galli F, Battistoni A, Gambari R, Pompella A, Bragonzi A, Pilolli F, et al. Oxidative stress and antioxidant therapy in cystic fibrosis. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 2012; 1822(5):690-713. [DOI: 10.1016/j.bbadis.2011.12.012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Graham‐Maar 2006
- Graham-Maar RC, Schall JI, Stettler N, Zemel BS, Stallings VA. Elevated vitamin A intake and serum retinol in preadolescent children with cystic fibrosis. American Journal of Clinical Nutrition 2006; 84(1):174-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
Griffiths 2000
- Griffiths JK. The vitamin A paradox. Journal of Pediatrics 2000; 137(5):604-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hammond 2013
- Hammond BR Jr, Renzi LM. Carotenoids. Advances in Nutrition 2013; 4(4):474-6. [DOI: 10.3945/an.113.004028] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrison 2012
- Harrison E. Mechanisms involved in the intestinal absorption of dietary vitamin A and provitamin A carotenoids. Biochimica et biophysica acta 2012; 1821(1):70-7. [DOI: 10.1016/j.bbalip.2011.06.002] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327(7414):557-60. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions 5.1 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jagannath 2017
- Jagannath VA, Thaker V, Chang AB, Price AI. Vitamin K supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2017, Issue 8. [DOI: 10.1002/14651858.CD008482.pub5] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krinsky 2005
- Krinsky NI, Johnson EJ. Carotenoid actions and their relation to health and disease. Molecular Aspects of Medicine 2005; 26(6):459-516. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lascari 1981
- Lascari AD. Carotenemia. A review. Clinical Pediatrics 1981; 20(1):25-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2016
- Li L, Somerset S. Dietary intake and nutritional status of micronutrients in adults with cystic fibrosis in relation to current recommendations. Clinical Nutrition 2016; 35(4):775-82. [DOI: 10.1016/j.clnu.2015.06.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Maqbool 2008
- Maqbool A, Graham-Maar RC, Schall JI, Zemel BS, Stallings VA. Vitamin A intake and elevated serum retinol levels in children and young adults with cystic fibrosis. Journal of Cystic Fibrosis 2008; 7(2):137-41. [DOI: 10.1016/j.jcf.2007.07.002] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marchant 2001
- Marchant JM, Masel JP, Dickinson FL, Masters IB, Chang AB. Application of chest high-resolution computer tomography in young children with cystic fibrosis. Pediatric Pulmonology 2001; 31(1):24-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Napoli 1996
- Napoli JL. Retinoic acid biosynthesis and metabolism. The FASEB journal : official publication of the Federation of American Societies for Experimental Biology 1996; 10(9):993-1001. [PMID: ] [DOI] [PubMed] [Google Scholar]
Okebukola 2017
- Okebukola PO, Kansra S, Barrett J. Vitamin E supplementation in people with cystic fibrosis. Cochrane Database of Systematic Reviews 2017, Issue 3. [DOI: 10.1002/14651858.CD009422.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olmedilla 2001
- Olmedilla B, Granado F, Southon S, Wright AJA, Blanco I, Gil-Martinez E, et al. Serum concentrations of carotenoids and vitamins A, E, and C in control subjects from five European countries. British Journal of Nutrition 2001; 85(2):227-38. [DOI: 10.1079/BJN2000248] [PMID: ] [DOI] [PubMed] [Google Scholar]
Paik 2001
- Paik J, During A, Harrison EH, Mendelsohn CL, Lai K, Blaner WS. Expression and characterization of a murine enzyme able to cleave beta-carotene. The formation of retinoids. The Journal of biological chemistry 2001; 276(34):32160-8. [DOI: 10.1074/jbc.M010086200] [PMID: ] [DOI] [PubMed] [Google Scholar]
Penniston 2006
- Penniston KL, Tanumihardjo SA. The acute and chronic toxic effects of vitamin A. American Journal of Clinical Nutrition 2006; 83(2):191-201. [PMID: ] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Royal Brompton Hospital 2017
- Clinical Guidelines: Care of Children with Cystic Fibrosis: Royal Brompton Hospital (7th edition) 2017. www.rbht.nhs.uk/childrencf (accessed 07 February 2017).
Saxby 2017
Sethuraman 2006
- Sethuraman U. Vitamins. Pediatric Review 2006; 27(2):44-55. [PMID: ] [DOI] [PubMed] [Google Scholar]
Shenkin 2006
- Shenkin A. The key role of micronutrients. Clinical Nutrition 2006; 25(1):1-13. [DOI: 10.1016/j.clnu.2005.11.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Socha 2010
- Socha P, Skorupa E, Pawlowska J, Wierzbicka A, Dhawan A, Jankowska I, et al. Beta-carotene deficiency in cholestatic liver disease of childhood is caused by beta-carotene malabsorption. Journal of Pediatric Gastroenterology and Nutrition 2010; 51(1):106-9. [DOI: 10.1097/MPG.0b013e3181d1afff] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stephensen 1994
- Stephensen CB, Alvarez JO, Kohatsu J, Hardmeier R, Kennedy JI Jr, Gammon RB Jr. Vitamin A is excreted in the urine during acute infection. American Journal of Clinical Nutrition 1994; 60(3):388-92. [PMID: ] [DOI] [PubMed] [Google Scholar]
Thürmann 2002
- Thürmann PA, Steffen J, Zwernemann C, Aebischer CP, Cohn W, Wendt G, et al. Plasma concentration response to drinks containing beta-carotene as carrot juice or formulated as a water dispersible powder. European Journal of Nutrition 2002; 41(5):228-35. [DOI: 10.1007/s00394-002-0381-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
West 2003
- West KP Jr. Vitamin A deficiency disorders in children and women. Food and Nutrition Bulletin 2003; 24(4 Suppl):S78-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wise 2009
- Wise JA, Kaats GR, Preuss HG, Morin RJ. beta-Carotene and alpha-tocopherol in healthy overweight adults; depletion kinetics are correlated with adiposity. International Journal of Food Sciences and Nutrition 2009; 60(Suppl 3):65-75. [DOI: 10.1080/09637480902852553] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Bonifant 2012
- Bonifant CM, Shevill E, Chang AB. Vitamin A supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD006751.pub3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bonifant 2014
- Bonifant CM, Shevill E, Chang AB. Vitamin A supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD006751.pub4] [PMID: ] [DOI] [PubMed] [Google Scholar]
O'Neil 2008
- O'Neil CM, Shevill E, Chang AB. Vitamin A supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD006751.pub2] [PMID: ] [DOI] [PubMed] [Google Scholar]


