Abstract
Background
Couple therapy for depression has the twofold aim of modifying negative interaction patterns and increasing mutually supportive aspects of intimate relationships, changing the interpersonal context of depression. Couple therapy is included in several guidelines among the suggested treatments for depression.
Objectives
1. The main objective was to examine the effects of couple therapy compared to individual psychotherapy for depression. 2. Secondary objectives were to examine the effects of couple therapy compared to drug therapy and no/minimal treatment for depression.
Search methods
The Cochrane Common Mental Disorders Group Controlled Trials Register (CCMDCTR), the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (Ovid), Embase (Ovid) and PsycINFO (Ovid) were searched to 19 February 2018. Relevant journals and reference lists were checked.
Selection criteria
Randomised and quasi‐randomised controlled trials examining the effects of couple therapy versus individual psychotherapy, drug therapy, or no treatment/minimal treatment for depression were included in the review.
Data collection and analysis
We considered as primary outcomes the depressive symptom level, the depression persistence, and the dropouts; the relationship distress level was a secondary outcome. We extracted data using a standardised spreadsheet. Where data were not included in published papers, we tried to obtain the data from the authors. We synthesised data using Review Manager software version 5.3. We pooled dichotomous data using the relative risk (RR), and continuous data calculating the standardised mean difference (SMD), together with 95% confidence intervals (CIs). We employed the random‐effects model for all comparisons and also calculated a formal test for heterogeneity, the natural approximate Chi2 test.
Main results
We included fourteen studies from Europe, North America, and Israel, with 651 participants. Eighty per cent of participants were Caucasian. Therefore, the findings cannot be considered as applicable to non‐Western countries or to other ethnic groups in Western countries. On average, participants had moderate depression, preventing the extension of results to severely depressed patients. Almost all participants were aged between 36 and 47 years.
There was no evidence of difference in effect at the end of treatment between couple therapy and individual psychotherapy, either for the continuous outcome of depressive symptoms, based on nine studies with 304 participants (SMD −0.17, 95% CI −0.44 to 0.10, low‐quality evidence), or the proportion of participants remaining depressed, based on six studies with 237 participants (RR 0.94, 95% CI 0.72 to 1.22, low‐quality evidence). Findings from studies with 6‐month or longer follow‐up confirmed the lack of difference between the two conditions.
No trial gave information on harmful effects. However, we considered rates of treatment discontinuation for any reason as a proxy indicator of adverse outcomes. There was no evidence of difference for dropout rates between couple therapy and individual psychotherapy, based on eight studies with 316 participants (RR 0.85, 95% CI 0.51 to 1.41, low‐quality evidence).
Few data were available for the comparison with drug therapy. Data from a small study with 12 participants showed no difference for the continuous outcome of depressive symptoms at end of treatment (SMD −0.51, 95% CI −1.69 to 0.66, very low‐quality evidence) and at 6‐month follow‐up (SMD −1.07, 95% CI ‐2.45 to 0.31, very low‐quality evidence). Data on dropouts from two studies with 95 participants showed a clear advantage for couple therapy (RR 0.31, 95% CI 0.15 to 0.61, very low‐quality evidence). However, this finding was heavily influenced by a single study, probably affected by a selection bias favouring couple therapy.
The comparison between couple therapy plus drug therapy and drug therapy alone showed no difference in depressive symptom level, based on two studies with 34 participants (SMD −1.04, 95% CI ‐3.97 to 1.89, very low‐quality evidence) and on dropouts, based on two studies with 45 participants (RR 1.03, 95% CI 0.07 to 15.52, very low‐quality evidence).
The comparison with no/minimal treatment showed a large significant effect favouring couple therapy both for depressive symptom level, based on three studies with 90 participants: (SMD −0.95, 95% CI −1.59 to −0.32, very low‐quality evidence) and persistence of depression, based on two studies with 65 participants (RR 0.48, 95% CI 0.32 to 0.70, very low‐quality evidence). No data were available for dropouts for this comparison.
Concerning relationship distress, the comparison with individual psychotherapy showed that couple therapy appeared more effective in reducing distress level at the end of treatment, based on six studies with 187 participants (SMD −0.50, CI −0.97 to −0.02, very low‐quality evidence) and the persistence of distress, based on two studies with 81 participants (RR 0.71, 95% CI 0.51 to 0.98, very low‐quality evidence). The quality of evidence was heavily affected by substantial heterogeneity (I2 = 59%). In the analysis restricted to studies including only distressed couples, no heterogeneity was found and the effect in distress level at the end of treatment was larger (SMD −1.10, 95% CI −1.59 to −0.61). Very few data on this outcome were available for other comparisons.
We assessed the certainty of the evidence using the GRADE system. The results were weakened by the low quality of evidence related to the effects on depressive symptoms, in comparison with individual psychotherapy, and by very low quality evidence for all other comparisons and for the effects on relationship distress. Most studies were affected by problems such as the small number of cases, performance bias, assessment bias due to the non‐blinding outcome assessment, incomplete outcome reporting and the allegiance bias of investigators. Heterogeneity was, in particular, a problem for data about relationship distress.
Authors' conclusions
Although there is suggestion that couple therapy is as effective as individual psychotherapy in improving depressive symptoms and more effective in improving relations in distressed couples, the low or very low quality of the evidence seriously limits the possibility of drawing firm conclusions. Very few data were available for comparisons with no/minimal treatment and drug therapy. Future trials of high quality should test in large samples with a long follow‐up of the effects of couple therapy in comparison to other interventions in discordant couples with a depressed partner, considering the role of relationship quality as a potential effect mediator in the improvement of depression.
Keywords: Adult, Humans, Middle Aged, Interpersonal Relations, Marital Therapy, Antidepressive Agents, Antidepressive Agents/therapeutic use, Depression, Depression/epidemiology, Depression/therapy, Patient Dropouts, Patient Dropouts/statistics & numerical data, Randomized Controlled Trials as Topic, Sex Factors
Plain language summary
Couple therapy for depression
Why is this review important?
Depression is a common mental disorder characterised by sadness, loss of pleasure in most activities, feelings of worthlessness or guilt, thoughts of death or suicide. Couple therapy has been suggested as a treatment for couples with a depressed partner on the basis of the association between depressive symptoms and relationship distress, the role of relational negative factors in onset and maintenance of depression, and the buffering effect of intimacy and interpersonal support. Couple therapy works by modifying negative interactional patterns and increasing mutually supportive aspects of relationships. It is important to know whether couple therapy can help people with depression.
Who will be interested in this review?
This review will be of interest to people with depression, their partners, and people involved in their care.
What questions does this review aim to answer?
This review aimed to assess evidence about the effects of couple therapy for couples with a depressed partner.
Which studies were included in the review?
We considered studies of couple therapy delivered in outpatient settings to couples in which a partner had a clinical diagnosis of depressive disorder. We included 14 studies with 651 participants .Thirteen of the studies were randomised controlled trials, where participants were assigned by chance alone to the couple therapy treatment group or usual care. However, one study was not completely randomised due to therapist availability.
What does the evidence from the review tell us?
There was low‐quality evidence to suggest that couple therapy is as effective as individual psychotherapy in improving depression. People with depression might do better when receiving couple therapy compared with no treatment, but we are very uncertain about this effect because of the very low quality of studies. In comparison with treatment with antidepressant medication, limited data was available. Although data on few dropouts favour couple therapy, the very low quality of data seriously weakens this finding. The comparison between couple therapy plus antidpressant medication and antidepressants alone showed no difference in depressive symptom level, but the results were based on two small studies. Couple therapy was more effective in reducing relationship distress than individual psychotherapy and this effect was enhanced when distressed couples were considered separately. However, this result has to be considered with great caution, because of the very low quality of studies. Most studies were affected by small sample sizes, unclear sample representativeness, loss of participants at follow‐up, and investigators' allegiance bias. Moreover, there were few follow‐ups that went beyond 6 months post‐treatment. Only one study tested whether improvements in couple relationships led to improvement in depression, finding supporting evidence for that. However, the small sample of this study and the lack of other studies which investigated this hypothesis means we could not test in this review if this finding was supported. Although it is difficult to draw conclusions with any confidence on differences between couple therapy and other treatments for depression, the possibility of improvement in couple relationships may favour its choice when relationship distress is a major problem.
What should happen next?
We need good quality trials, testing in large samples with long follow‐up of the effects of couple therapy in comparison to other interventions, especially in distressed couples.
Summary of findings
Summary of findings for the main comparison. Summary of findings for the comparison with individual psychotherapy.
| Couple therapy compared with individual psychotherapy for depression | ||||||
|
Patient or population: heterosexual adult couples aged > 18 with a partner having a clinical diagnosis of depressive disorder Settings: outpatient Intervention: couple therapy Comparison: individual psychotherapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Individual psychotherapy | Couple therapy | |||||
|
Depressive symptoms at end of treatment Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HDRS). BDI is a self‐report inventory including 21 questions, each answer being scored from 0 to 3 with the total score ranging from 0 to 63. HDRS is an expert‐rated questionnaire including 17 items scored from 0 to 2 or 5 depending on the item, with the total score ranging from 0 to 50. In both scales, higher scores indicate more severe depression |
The mean depression level at post‐treatment in the intervention group was 0.17 standard deviations lower than in the control group (0.44 lower to 0.10 higher) |
304 (9 studies) |
Lowa ⊕⊕⊝⊝ |
This is a small effect. No evidence that couple therapy reduced depression in participants, compared to individual psychotherapy. | ||
|
Persistence of depression at end of treatment Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HDRS) |
Study population | RR 0.94 (0.72 to 1.22) |
237 (6 studies) |
Lowb ⊕⊕⊝⊝ |
No evidence that couple therapy reduced the rates of people remaining depressed, compared to individual psychotherapy. | |
| 568 per 1000 |
532 per 1000 (445 to 617) |
|||||
| Dropouts | Study population | RR 0.85 (0.51 to 1.41) |
364 (9 studies) |
Lowc ⊕⊕⊝⊝ |
No evidence that couple therapy reduced the dropout risk, compared to individual psychotherapy. | |
| 223 per 1000 |
190 per 1000 (141 to 252) |
|||||
|
Relationship distress at end of treatment Dyadic Adjustment Scale (DAS) or Maudsley Marital Questionnaire (MMQ). DAS is a self‐report inventory with 32 items, with the total score ranging from 0 to 151. Higher scores indicate less distress. MMQ is a self‐report questionnaire including 15 items covering relational and sexual adjustment, with the total score ranging from 0 to 120. Higher scores indicate more distress. |
The mean relationship distress level at post‐treatment in the intervention group was 0.50 standard deviations lower than in the control group (0.97 to 0.02 lower) |
187 (6 studies) |
Very lowd ⊕⊝⊝⊝ |
This is a moderate effect. Couple therapy appeared to be more effective than individual psychotherapy in reducing relationship distress, but studies were of poor quality. | ||
| *The basis for the assumed risk is the control group risk. The corresponding risk is based on the assumed risk in the treatment group and the relative effect of intervention. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the standardised mean difference of the intervention (and its 95% CI). CI: Confidence interval; SMD: Standardised mean difference; RR; Risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
a High risk of bias in all trials due to lack of blinding of participants and in seven trials due to lack of blinding in outcome assessment. Conflict of interest raising the possibility of allegiance bias in three trials. Possible indirectness of evidence due to recruitment of populations to some extent not representative of clinical practice in four studies. Quality of evidence downgraded by two levels. The overall judgement about biases is likely to seriously affect the interpretation of results.
bHigh risk of bias in all trials due to lack of blinding of participants and in five trials due to lack of blinding in outcome assessment. Conflict of interest raising the possibility of allegiance bias in three trials. Possible indirectness of evidence due to recruitment of populations to some extent not representative of clinical practice in two studies. Quality of evidence downgraded by two levels. The overall judgement about biases is likely to seriously affect the interpretation of results.
c High risk of bias in all trials due to lack of blinding of participants and conflict of interest raising the possibility of allegiance bias. Possible indirectness of evidence due to recruitment of populations to some extent not representative of clinical practice in two studies. Very wide confidence interval. Quality of evidence downgraded by two levels.The overall judgement about biases is likely to seriously affect the interpretation of results.
d High risk of bias in all trials due to lack of blinding of participants and lack of blinding in outcome assessment. Conflict of interest raising the possibility of allegiance bias in two trials. Possible indirectness of evidence due to recruitment of populations to some extent not representative of clinical practice in two studies. Substantial statistical heterogeneity. Quality of evidence downgraded by three levels. The overall judgement about biases is likely to very seriously affect the interpretation of results.
Summary of findings 2. Summary of findings for the comparison with drug therapy.
| Couple therapy compared with drug therapy for depression | ||||||
|
Patient or population: heterosexual adult couples aged >18 with a partner having a clinical diagnosis of depressive disorder Settings: outpatient Intervention: couple therapy Comparison: drug therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Drug therapy | Couple therapy | |||||
|
Depressive symptoms at end of treatment Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HDRS). BDI is a self‐report inventory including 21 questions, each answer being scored from 0 to 3 with the total score ranging from 0 to 63. HDRS is an expert‐rated questionnaire including 17 items scored from 0 to 2 or 5 depending on the item, with the total score ranging from 0 to 50. In both scales, higher scores indicate more severe depression. |
The mean depression level at post‐treatment in the intervention group was 0.51 standard deviations lower than in the control group (1.69 lower to 0.66 higher) |
12 (1 study) |
Very lowa ⊕⊝⊝⊝ |
No evidence that couple therapy reduced depression in participants, compared to drug therapy. | ||
| Persistence of depression at end of treatment | No data available | |||||
| Dropouts | Study population | RR 0.31 (0.15 to 0.61) |
95 (2 studies) |
Very lowb ⊕⊝⊝⊝ |
Couple therapy appeared to be more effective than drug therapy in reducing dropout risk, but studies were of very poor quality. | |
| 543 per 1000 |
163 per 1000 (85 to 290) |
|||||
|
Relationship distress at post‐treatment Dyadic Adjustment Scale (DAS) or Maudsley Marital Questionnaire (MMQ). DAS is a self‐report inventory with 32 items, with the total score ranging from 0 to 151. Higher scores indicate less distress. MMQ is a self‐report questionnaire including 15 items covering relational and sexual adjustment, with the total score ranging from 0 to 120. Higher scores indicate more distress. |
The mean relationship distress level at post‐treatment in the intervention group was 0.47 standard deviations lower than in the control group (1.64 lower to 0.70 higher) |
12 (1 study) |
Very lowa ⊕⊝⊝⊝ |
No evidence that couple therapy reduced relationship distress in participants, compared to drug therapy. | ||
| *The basis for the assumed risk is the control group risk. The corresponding risk is based on the assumed risk in the treatment group and the relative effect of intervention. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the standardised mean difference of the intervention (and its 95% CI). CI: Confidence interval; SMD: Standardised mean difference; RR; Risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
a High risk of bias due to lack of blinding of participants. Conflict of interest raising the possibility of allegiance bias. A single trial with very few participants. Indirectness of evidence due to recruitment of a population possibly not representative of clinical practice. Quality of evidence downgraded by three levels. The overall judgement about biases is likely to very seriously affect the interpretation of results.
b High risk of bias due to lack of blinding of participants. Conflict of interest raising the possibility of allegiance bias. Two trials. Results heavily influenced by a single trial at high risk of bias showing indirectness of evidence due to recruitment of a population not representative of clinical practice. Quality of evidence downgraded by three levels. The overall judgement about biases is likely to very seriously affect the interpretation of results.
Summary of findings 3. Summary of findings for the comparison with no/minimal treatment.
| Couple therapy compared with no/minimal treatment for depression | ||||||
|
Patient or population: heterosexual adult couples aged > 18 with a partner having a clinical diagnosis of depressive disorder Settings: outpatient Intervention: couple therapy Comparison: no/minimal therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No/minimal treatment | Couple therapy | |||||
|
Depressive symptoms at the end of treatment Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HDRS). BDI is a self‐report inventory including 21 questions, each answer being scored from 0 to 3 with the total score ranging from 0 to 63. HDRS is an expert‐rated questionnaire including 17 items scored from 0 to 2 or 5 depending on the item, with the total score ranging from 0 to 50. In both scales, higher scores indicate more severe depression. |
The mean depression level at post‐treatment in the intervention group was 0.95 standard deviations lower than in the control group (1.59 to 0.32 lower) |
90 (3 studies) |
Very lowa ⊕⊝⊝⊝ |
This is a large effect. Couple therapy appeared to be more effective than no/minimal treatment in reducing depression, but studies were of very poor quality. |
||
|
Persistence of depression at the end of treatment Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HDRS) |
Study population | RR 0.48 (0.32 to 0.70) | 65 (2 studies) |
Very lowb ⊕⊝⊝⊝ |
Couple therapy appeared to be more effective than no/minimal treatment in reducing the rates of people remaining depressed, but studies were of very poor quality. | |
| 935 per 1000 | 441 per 1000 (289 to 606) | |||||
| Dropouts | No data available | |||||
|
Relationship distress at the end of treatment Dyadic Adjustment Scale (DAS) or Maudsley Marital Questionnaire (MMQ). DAS is a self‐report inventory with 32 items, with the total score ranging from 0 to 151. Higher scores indicate less distress. MMQ is a self‐report questionnaire including 15 items covering relational and sexual adjustment, with the total score ranging from 0 to 120. Higher scores indicate more distress. |
The mean relationship distress level at post‐treatment in the intervention group was 0.80 standard deviations lower than in the control group (1.64 lower to 0.04 higher) |
60 (2 studies) |
Very lowc ⊕⊝⊝⊝ |
No evidence that couple therapy reduced relationship distress in participants, compared to no/minimal treatment. | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
a High risk of bias due to lack of blinding of participants and of outcome assessment. Two out of three studies with high risk of conflict of interest raising the possibility of allegiance bias. Very wide confidence interval. Quality of evidence downgraded by three levels. The overall judgement about biases is likely to very seriously affect the interpretation of results.
b High risk of bias due to lack of blinding of participants and of outcome assessment. One study with high risk of conflict of interest raising the possibility of allegiance bias. One study reported incomplete outcome data. Quality of evidence downgraded by three levels. The overall judgement about biases is likely to very seriously affect the interpretation of results.
c High risk of bias due to lack of blinding of participants and of outcome assessment. Two out of three studies with high risk of conflict of interest raising the possibility of allegiance bias. Very wide confidence interval. Quality of evidence downgraded by three levels.The overall judgement about biases is likely to very seriously affect the interpretation of results.
Summary of findings 4. Summary of findings for the comparison between couple therapy plus drug therapy and drug therapy alone.
| Couple therapy plus drug therapy compared with drug therapy alone for depression | ||||||
|
Patient or population: heterosexual adult couples aged > 18 with a partner having a clinical diagnosis of depressive disorder Settings: outpatient Intervention: couple therapy plus drug therapy Comparison: drug therapy alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Drug therapy alone | Couple therapy plus drug therapy | |||||
|
Depressive symptoms at the end of treatment Beck Depression Inventory (BDI) or Hamilton Depression Rating Scale (HDRS). BDI is a self‐report inventory including 21 questions, each answer being scored from 0 to 3 with the total score ranging from 0 to 63. HDRS is an expert‐rated questionnaire including 17 items scored from 0 to 2 or 5 depending on the item, with the total score ranging from 0 to 50. In both scales, higher scores indicate more severe depression |
The mean depression level at post‐treatment in the intervention group was 1.04 standard deviations lower than in the control group (3.97 lower to 1.89 higher) |
34 (2 studies) |
Very lowa ⊕⊝⊝⊝ |
No evidence that couple therapy plus drug therapy reduced depression in participants, compared to drug therapy alone. | ||
| Persistence of depression at the end of treatment | No data available | |||||
| Dropouts | Study population | RR 1.03 (0.07 to 15.52) | 45 (2 studies) |
Very lowa ⊕⊝⊝⊝ |
No evidence that couple therapy plus drug therapy reduced droput risk in participants, compared to drug therapy alone. | |
| 158 per 1000 | 231 per 1000 (110 to 420) | |||||
|
Relationship distress at the end of treatment Dyadic Adjustment Scale (DAS) or Quality of Marriage Index ‐ QMI. DAS is a self‐report inventory with 32 items, with the total score ranging from 0 to 151. Higher scores indicate less distress. QMI is a six‐item self‐rated inventory. Respondents answer the first five items on a 7‐point scale ranging from 1 (strongly disagree) to 7 (strongly agree). The sixth item is answered on a 10‐point scale ranging from 1 (extremely low) to 10 (extremely high). Lower scores represent lower relational quality. A score of 28 or less corresponds to the cut‐off of DAS considered as a criterion for relationship distress. |
The mean relationship distress level at post‐treatment in the intervention group was 0.60 standard deviations lower than in the control group (1.35 lower to 0.14 higher) |
34 (2 studies) |
Very lowa ⊕⊝⊝⊝ |
No evidence that couple therapy plus drug therapy reduced relationship distress in participants, compared to drug therapy alone. | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
a Data from two studies with small samples at high risk of bias. Very wide confidence interval. Substantial statistical heterogeneity. Quality of evidence downgraded by three levels. The overall judgement about biases is likely to very seriously affect the interpretation of results.
Background
Description of the condition
Depression is a common mental disorder primarily characterised by pervasive sadness with loss of interest or pleasure in most activities. It is often associated with changes in appetite, sleeping patterns, agitation or retardation, decreased energy, feelings of worthlessness or guilt, impairment in concentration, and recurrent thoughts of death or suicide. It is generally agreed that, according to current diagnostic criteria, depressive disorders can be ranged along a continuum by levels of symptom severity, number of mental or physical symptoms, and duration (APA 2000; WHO 1992).
Depression is present in all countries and all age groups. Its distribution is nonetheless different across countries, age groups and genders, probably reflecting cultural differences or variations in risk factors. In Western countries, one‐year prevalence rates of major depression in adults cluster around 5% and lifetime rates around 15% (Hasin 2005; Üstün 2004). Less reliable data are available for minor depressive disorders. However, recent estimates show a one‐year prevalence of chronic minor depression at about 2% (Waraich 2004). In many low and middle‐income countries, rates are even higher (Kessler 2013). One main feature of depression is the different distribution in the two genders. Depression in women is about twice as prevalent as it is in men (Üstün 2004). Although depression is often short‐lasting or self‐limiting, in a substantial number of cases, it follows a chronic, relapsing, or recurrent course. Recovery following a major depressive episode occurs within one year in about 50% of cases (Bland 1997). Moreover, about 60% of people who have recovered from a first episode of major depression will experience further depressive symptoms in the following five years (Mueller 1999).
Depression carries an overall increased mortality risk, with a high risk of suicide compared to the general population. A Canadian study observed a twofold standardised mortality rate for all causes (Newman 1991). A meta‐analysis estimated the lifetime suicide risk in depressed people at around 2% (Bostwick 2000). Depression can be a very disabling illness. Its symptoms interfere with daily functioning, social role performance, work productivity, and physical wellbeing. According to recent estimates (Vos 2000), the disability‐adjusted life years (DALYs) rates per 1000 population for depression were 5.3 in males and 7.7 in females. Depression in 2010 has been estimated as the second most important cause of years lived with disability worldwide (Ferrari 2013).
Depression and other affective disorders impose a substantial economic burden on both developed and developing countries. In the United States, in 1998, it was estimated to cost around USD 65 billion (Berto 2000). In Europe, the annual cost of depression was estimated at EUR 118 billion in 2004 (Sobocki 2006). Direct costs alone totaled EUR 42 billion and indirect costs due to morbidity and mortality were estimated at EUR 76 billion. This makes depression the most costly among mental and neurological disorders in Europe, accounting for 33% of the total cost. The cost of depression corresponds to 1% of the total economy of Europe (Sobocki 2006). Hidden social and emotional costs, which are much more difficult to estimate, are relevant for patients, family members and caregivers (Goodman 1999).
Risk factors for depressive disorders are manifold, ranging from genetically‐based biological vulnerability to social and interpersonal factors. Childhood events, adverse life circumstances, and stressful relationships play a relevant role in the onset and maintenance of depression (Kendler 1999).
Description of the intervention
In addition to antidepressant drug therapy, a number of psychological interventions have shown to be effective as treatment for depression (Cuijpers 2008a). Psychological and pharmacological treatments are considered equally effective (Cristea 2017). Moreover, psychological treatments are increasingly becoming a focus of interest as a consequence of various factors, such as lower dropout rates, contraindications and side effects of medications, failure of many patients to comply with maintenance drug therapy, and patients' preference (Chilvers 2001; Cuijpers 2008b). Although the best evidence is available for cognitive‐behavioural therapies, other treatment models, such as interpersonal therapy, psychodynamic therapy based on psychoanalytical concepts, non‐directive counselling, and couple therapy have been included in most guidelines as possibly effective interventions (Malhi 2009; NICE 2009).
Couple therapy has been first suggested more than forty years ago as an approach for couples with a depressed spouse (Friedman 1975). It is a form of psychological intervention involving the presence of both partners of a committed relationship in sessions led by a trained therapist, with the twofold aim of modifying negative interactional patterns and promoting supportive aspects of a close relationship. The main focus of intervention is always on mutual relationship aspects (Lebow 2012).
A large body of evidence supports a close link between relationship variables and depression (Denton 2003). Community‐based epidemiological studies and surveys using self‐report questionnaires show a strong cross‐sectional association between depressive symptoms and marital dissatisfaction (Whisman 2001). Longitudinal studies show the reciprocal influence of depression and couple problems: either depressive symptoms predict later marital dissatisfaction or marital dissatisfaction predicts onset of depressive episodes (Kronmüller 2011); stressful relational events, such as partner infidelity or threats of disruption of a romantic relationship can precipitate or exacerbate depressive symptoms (Cano 2000); interactions in couples with one depressed partner are often characterized by criticism, hostility and overprotection, i.e. a highly expressed emotional style, known to be among the most important stressors involved in the causal chain leading to relapse of depressive episodes (Hooley 2007); by contrast, interpersonal support, enhanced intimacy, and help by a partner in implementing coping strategies have a buffering effect on depressive symptoms, thus facilitating recovery (Beach 1998).
A number of partly overlapping theories have been advanced to conceptualise the role of the relational processes in onset and maintenance of depression. Recent integrative approaches suggest that depressed mood and conflict in couples may be mutually influential: relationship dissatisfaction leads to depression by reducing social support and increasing stress and hostility, while behaviour of depressed individuals may elicit rejection from a partner and increase subjective and objective indicators of interpersonal stress, thus creating a vicious cycle in which disruptive interactional aspects and depression reinforce each other (Rehman 2008).
Such findings provide the logical foundation for the assumption that couple‐focused therapy should be more effective than an individual‐based treatment for patients with depression living with a regular partner, especially if there is a significant relationship distress.
How the intervention might work
Couple therapy, mainly based on social learning and systemic theories, has the twofold aim of modifying negative interactional patterns and increasing mutually supportive aspects of couple relationships. Although a variety of treatment models have been used, a number of common principles underlie all interventions: (a) altering the couple's view of the presenting problem to be more objective, contextualised, and related to the couple interactions ; (b) decreasing emotion‐driven, dysfunctional behaviour; (c) eliciting emotion‐based behaviour; (d) increasing constructive communication patterns; and (e) emphasising strengths and reinforcing gains (Benson 2012).
Why it is important to do this review
A number of controlled clinical trials examining the effectiveness of couple therapy for depression have been conducted. A number of authors have concluded that several forms of couple therapy can effectively treat depression (Baucom 1998). However, although some narrative reviews have been published (Denton 2006; Gilliam 2005; Gupta 2003; Hollon 2012; Whisman 2012), data from clinical trials have never been subjected to quantitative analyses. This review aimed at filling this gap, by appraising and summarising evidence from all the available studies, to provide an overall assessment of the role of couple therapy among psychosocial treatments for depression. The publication of new trials on this topic made it necessary to update the first edition of this review.
Objectives
1. The main objective was to examine the effects of couple therapy compared to individual psychotherapy for depression. 2. Secondary objectives were to examine the effects of couple therapy compared to drug therapy and no/minimal treatment for depression.
Methods
Criteria for considering studies for this review
Types of studies
Wer considered for this review randomised controlled trials, including cluster trials, and quasi‐randomised controlled trials, in which treatment assignment was decided through methods such as alternation, rotation, or randomisation restricted by therapist availability, which has been used used in psychotherapy research (Cristea 2017). We did not consider naturalistic and observational studies.
Types of participants
Participant characteristics
Heterosexual adult couples aged 18 years or more with a partner having a clinical diagnosis of depressive disorder. We included studies adopting any standardised and validated diagnostic criteria to define depressive disorder.
Diagnosis
Depressive disorder diagnosed by any of the following diagnostic systems: Research Diagnostic Criteria (Spitzer 1978), criteria of the Present State Examination (Wing 1974), Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM‐III) (APA 1980), DSM‐III‐Revised (R) (APA 1987), DSM‐Fourth Edition (IV) (APA 1994), DSM‐IV‐Text Revision (TR) (APA 2000), DSM‐5 (APA 2013), and International Classification of Diseases, Tenth Edition (ICD−10) (WHO 1992).
Comorbidities
We included trials whether or not comorbidities were present in the sample.
Setting
We included studies conducted in any outpatient setting either in primary care or specialist services. We excluded studies conducted in inpatient settings. However, we included studies recruiting participants during inpatient admission if most of the intervention was delivered after discharge.
Types of interventions
Experimental interventions
Couple therapy, for the purpose of this review was defined as a structured psychological intervention in which a trained therapist meets both partners of a committed relationship, in regular face‐to‐face sessions, with the explicit aim of modifying dysfunctional patterns of interaction and enhancing positive relationships. Any treatment model delivered to couples was considered for inclusion. In addition to couple therapy alone, the combination of couple therapy and antidepressant drug therapy was also considered.
Excluded interventions
1. Studies that focused on family therapy, where the treatment was delivered to the whole family unit, including children.
2. Studies that were targeted to postnatal depression.
Comparator interventions
The main comparison was with individual psychotherapy. Any intervention defined by the authors as 'individual psychotherapy', irrespective of the treatment model, was included under this heading. We considered as suitable all models supported by evidence of efficacy in treatment of depression: cognitive, behavioural, interpersonal, psychodynamic, supportive, problem‐solving (Cuijpers 2008a).
Secondary comparisons were with antidepressant drug therapy and with no/minimal treatment. In accordance with the recent guidelines (Bauer 2013), the following drug categories were considered as suitable: tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin‐norepinephrine reuptake inhibitors, norepinephrine‐dopamine reuptake inhibitors, monoamine oxidase inhibitors, and atypical antidepressants. No/minimal treatment in psychotherapy research usually includes waiting lists or unspecific contacts. All studies included in this review providing comparison with no/minimal treatment used waiting list as a control condition.
Types of outcome measures
Primary outcomes
1. Efficacy outcome. Depressive symptom level, presented as continuous (means and standard deviations) or dichotomous (persistence of depression versus remission or clinically significant improvement) data, measured through use of self‐rated questionnaires, such as Beck Depression Inventory (BDI) (Beck 1961), or clinician‐rated scales, such as the Hamilton Rating Scales for Depression (HRSD) (Hamilton 1960), and the Inventory of Depressive Symptomatology (IDS‐C30) (Rush 1996).
2. Adverse events outcome. Proportion of dropouts or participants who discontinued treatment for any reason. This outcome was not considered in studies providing comparison with waitlist, because discontinuation of treatment does not make any sense in a no‐treatment condition.
Secondary outcomes
3. Relationship distress. Since modification of dysfunctional patterns of interaction is an aim of couple therapy, we considered measures of relationship distress according to standardised instruments. In couple therapy research, the most commonly used is by far the Dyadic Adjustment Scale (DAS) (MacIntosh 2014; Spanier 1976). We assessed relationship distress in two ways: as continuous (means and standard deviations) and dichotomous (significant versus not significant clinical improvement) data.
Timing of outcome assessment
We decided to assess end of treatment outcomes, short‐term and long‐term outcomes. After an examination of outcome research in psychotherapy of depression (Cuijpers 2008a), we decided to consider 6‐month follow‐up as 'short‐term' and 15 or more months follow‐up as 'long‐term'.
Hierarchy of outcome measures
Primary outcomes
Depressive symptoms
Although the BDI (Beck 1961) is the most often used in psychotherapy research, we considered that this self‐report measure would carry a high risk of bias because, in all studies included in this review, the participants were aware of the assigned intervention. Therefore, when more than one scale was used, we preferred as a first choice the expert‐rated HRSD (Hamilton 1960), provided it was used by blind assessors. If assessment by HRSD was not blind, thus carrying a high risk of bias as well, we preferred BDI. Although operational criteria for remission have been suggested for both scales, through the identification of cut‐offs derived from studies on normative samples discriminating between mental health and psychopathology (Grundy 1996; Ogles 1995), there is no agreement on the exact definition of such cut‐offs. Therefore, we accepted the criteria indicated by the authors to define remission or clinical significant improvement.
We list below the main scales that provided data on this outcome:
Beck Depression Inventory ‐ BDI
The Beck Depression Inventory (BDI, BDI‐II) is a 21‐question multiple‐choice self‐report inventory, one of the most widely used instruments for measuring the severity of major depression (Beck 1961; Beck 1996). Both the BDI and the BDI‐II contain 21 questions, each answer being scored on a scale value of 0 to 3. Higher total scores indicate more severe depressive symptoms. The cut‐offs used in recent research are: 0 to 13: minimal depression; 14 to 19: mild depression; 20 to 28: moderate depression; and 29 to 63: severe depression. Depression can be thought of as having two components: the affective component (e.g. mood) and the physical or 'somatic' component (e.g. loss of appetite). The BDI‐II reflects this and can be separated into two subscales. The affective subscale contains eight items: pessimism, past failures, guilt feelings, punishment feelings, self‐dislike, self‐criticism, suicidal thoughts or wishes, and worthlessness. The somatic subscale consists of the other thirteen items: sadness, loss of pleasure, crying, agitation, loss of interest, indecisiveness, loss of energy, change in sleep patterns, irritability, change in appetite, concentration difficulties, tiredness and/or fatigue, and loss of interest in sex.
Hamilton Rating Scale for Depression ‐ HRSD
The Hamilton Rating Scale for Depression (HRSD) is a multiple item clinician‐rated questionnaire used to provide an indication of depression severity to evaluate treatment outcome (Hamilton 1960; Hamilton 1980). The original version contains 17 items to be rated (HRSD−17) (Hamilton 1980). Each item of the questionnaire is scored on a 3 or 5 point scale, depending on the item, and the total score is compared to the corresponding descriptor. A score of 0 to 7 is considered to be normal. Scores of 20 or higher indicate moderate, severe, or very severe depression, and are usually required for entry into a clinical trial. Questions 18 to 21 may be recorded to give further information about the depression (such as whether diurnal variation or paranoid symptoms are present), but are not part of the scale.
Inventory of Depressive Symptomatology‐IDS 30
The Inventory of Depressive Symptomatology‐IDS 30 (Rush 1996), is a multiple item clinician‐rated inventory used to differentiate depression from euthymic states, to assess the depression severity and to evaluate change over time. It comprises 30 items scored on a 4 point scale. A score below 12 is considered to be normal, between 12 and 23 indicates mild depression, 24 to 36 moderate depression, 37 to 46 moderate to severe, and more than 46, severe depression.
Secondary outcomes
Relationship distress
If there were several measures used, we considered as a first choice the widely used DAS (Dyadic Adjustment Scale) (Spanier 1976), then the instrument with the more robust psychometric properties.
We list below the scales that provided data on this outcome:
Dyadic Adjustment Scale ‐ DAS
The Dyadic Adjustment Scale (Spanier 1976), is currently the most widely utilized self‐report measure of relationship adjustment in the social and behavioural sciences. It is a 32‐item measure developed for couples in stable committed relationships. DAS often serves as a dependent measure of couple satisfaction or to classify 'distressed' versus 'nondistressed' couples in interaction task research. Scores range from 0 to 151, with higher scores indicating better adjustment. Scores below 95 are usually considered as indicators of relationship distress. In Spanier 1976, original factor analysis of the DAS identified four subscales, which he advised could each be used independently: Dyadic Consensus, Dyadic Satisfaction, Dyadic Cohesion, and Affectional Expression. Locke‐Wallace Marital Adjustment Scale ‐ LWMAS
The Locke Wallace Marital Adjustment Scale is a 15‐item self‐rated scale that assesses couple satisfaction (Locke 1976). The test has been widely used for the assessment of relational quality over the last forty years. The test consists of 15 items and it is quick to administer and score despite unequal weights for different items. For each item, there is an algorithm leading to one of three acuity ranges (i.e. Very Unhappy, Happy, Perfectly Happy). The logic for the user receiving specific feedback is included in the algorithms below each item. Total score is the sum of all items, with possible range from 2 to 158. For the total score, the following cut‐offs are proposed: 100 to 158 for high satisfaction; 85 to 99 for moderate satisfaction; 2 to 84 for low satisfaction. Maudsley Marital Questionnaire ‐ MMQ
The Maudsley Marital Questionnaire is a standardised and validated self‐rated questionnaire with 15 items relating to relational and sexual adjustment, with a nine‐point (0 to 8) scale appended to each question (Arrindell 1983). The MMQ defines satisfaction as the subjective evaluation of the emotional connection and the sexual relationship with the partner. Two subscales of the MMQ were identified: couple satisfaction (ten items) and sexual satisfaction (five items). Respondents are usually asked to indicate which point on the scale best described their situation over the previous 2 weeks. Items in each subscale are summed. Scores on the relational satisfaction subscale could range from 0 to 80 and on the sexual satisfaction subscale from 0 to 40, with a higher score indicating less satisfaction.
Quality of Marriage Index ‐ QMI
The Quality of Marriage Index is a standardised and validated six‐item self‐rated measure of marital satisfaction (Norton 1983). Respondents answer the first five items on a 7‐point scale ranging from 1 (strongly disagree) to 7 (strongly agree). The sixth item is answered on a 10‐point scale ranging from 1 (extremely low) to 10 (extremely high). Lower scores represent lower relational quality. A score of 28 or less corresponds to the cut‐off of DAS considered as a criterion for relationship distress.
Search methods for identification of studies
Electronic searches
For the earlier version of this review, the Cochrane Common Mental Disorder's information specialist searched the specialised register (the CCMDCTR) in September 2005, using the following strategy:
Diagnosis = (Depressi* or Dysthymi*) and Intervention = ('Marital Therapy' or Couples or Family)
Details of the Group's specialised register can be found in Appendix 1.
The information specialist repeated the search in March 2010, using the same strategy, but ran additional searches on MEDLINE (Ovid), Embase (Ovid) and PsycINFO (Ovid) (Appendix 2), as the register had fallen out of date at this time, due to the change over of staff at the editorial base.
Further update searches were performed on the Group's (up‐to‐date) specialised register in September 2014, May 2015 and February 2016 using the following search terms (across both the studies and references register):
#1 (depress* or dysthymi* or 'affective disorder*' or 'affective symptom*' or mood*):ti,ab,kw,ky,emt,mh,mc #2 ((marital or marriage) NEAR relations*):ti,ab,kw,ky,emt,mh,mc #3 ((*therap* or counsel* or treat* or intervention*) NEAR (marital or marriage or couple* or spouse* or partner*)):ti,ab,kw,ky,emt,mh,mc #4 ((*therap* or counsel* or treat* or intervention*) and (partners near patients)):ti,ab,kw,ky,emt,mh,mc #5 ('marital disput*' or 'conjoint therapy'):ti,ab,kw,ky,emt,mh,mc #6 (#1 and (#2 or #3 or #4 or #5))
[Key to field tags. ti:title; ab:abstract; kw:keywords; ky:other keywords; mh:MeSH headings; mc:MeSH check words; emt:EMTREE headings]
The searches were further updated in February 2018. The Cochrane Common Mental Disorders Controlled Trials Register (CCMDCTR ‒ both Studies and References), the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (Ovid), Embase (Ovid) and PsycINFO (Ovid) were searched on February 19th 2018. The search strategies are reported in Appendix 3.
No restrictions on date, language, or publication status were applied to the searches. The date of the latest search (results incorporated): 19 February 2018
The information specialist also searched ClinicalTrials.gov and the WHO's trials portal (ICTRP) (all years to 19 February 2018).
Searching other resources
Handsearching
We handsearched and examined psychiatric and psychological journals identified as potentially including contributions relevant for this review. We checked all issues of the following journals between 1986 and February 2018:Psychotherapy and Psychosomatics, Behavior Modification, Behaviour Therapy, Journal of Consulting and Clinical Psychology, Journal of Sex and Marital Therapy, Family Process, Journal of Marital and Family Therapy, Clinical Psychology Review, American Journal of Family Therapy, Journal of Family Therapy, Australian and New Zealand Journal of Family Therapy, Contemporary Family Therapy, Journal of Couple and Relationship Therapy, Couple and Family Psychology: Research and Practice.
Reference lists
We checked the database of randomised controlled and comparative studies examining the effects of psychotherapy for adult depression run by the Department of Psychology of VU University Amsterdam (http://www.evidencebasedpsychotherapies.org). Moreover, we examined references from the text of reports of relevant trials and reviews for further trials not otherwise identified. We searched relevant books and chapters identified through reviews, trial bibliographies and electronic databases to identify trials published in books rather than journals.
Correspondence
We tried to obtain data not included in some of the published papers. We contacted the first author of the report with a standard letter, explaining the purposes of the review and the reasons for requesting additional data. In case of no answer in one month, we made an additional attempt. If no usable information was supplied, we excluded the study from the analysis related to the missing data.
Data collection and analysis
Selection of studies
One reviewer (AB) screened the abstracts of all publications obtained by the search strategy, in order to identify the eligible studies. A first list of potentially eligible studies was drafted, and was cross‐checked by the second and third reviewer (BD, AP). We decided by mutual consensus on a final list of trials. No disagreement between reviewers was found about the trials to be included. We obtained and inspected all papers to assess their relevance to this review. We identified any additional report related to the trials, to search for data not found in the primary paper. All relevant papers are included in the reference to studies list (Included studies).
Data extraction and management
Two review authors (AB and BD) independently evaluated trials for data extraction. Any discrepancy was resolved by resorting to the opinion of the third author (AP).
We used a data collection form to extract study characteristics and outcome data which had been piloted on at least one study in the review. Two review authors (AB and BD) extracted study characteristics and outcome data from the included studies. We considered the following study characteristics:
Methods: Study design, total duration of study, number of study centres and location, study setting, unit of allocation, withdrawals;
Participants: Number, mean age, age range, gender, ethnicity, severity of condition, diagnostic criteria, inclusion and exclusion criteria, social and demographic characteristics;
Interventions: Experimental and comparison treatments, duration of treatment;
Outcomes: Primary and secondary outcomes specified and collected, and time points reported;
Notes: Characteristics of therapists, treatment integrity assessment, notable conflicts of interest of trial authors.
The 'Characteristics of included studies' tables report if outcome data were not provided in a usable way. We resolved any disagreement by consensus. One review author (AB) transferred data into the Review Manager (RevMan 2014). We double‐checked data by comparing the data presented in the systematic review with the study reports. A second review author (BD) spot‐checked study characteristics for accuracy against the trial reports.
Main comparisons
1. Couple therapy versus individual psychotherapy.
2. Couple therapy versus antidepressant drug therapy;
3. Couple therapy versus no/minimal treatment;
4. Couple therapy plus drug therapy versus antidepressant drug therapy alone.
Assessment of risk of bias in included studies
We assessed the risk of bias by using the criteria described in the version 5.1.0 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The three review authors independently assessed the risk of bias for each study. Any disagreement was resolved by discussion.
The following domains were considered:
Random sequence generation;
Allocation concealment;
Blinding of participants and personnel;
Blinding of outcome assessment;
Incomplete outcome data;
Selective outcome reporting;
Other potential sources of bias.
We judged each potential source of bias as high, low or unclear, providing support for judgment in the 'Risk of bias' table. We summarised the risk of bias across different studies for each of the domains listed. We considered blinding separately for outcomes, where necessary. Where information on risk of bias came from unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
Measures of treatment effect
Dichotomous data
We combined dichotomous data by calculating the risk ratio (RR), with its 95% confidence interval (CI).
Continuous data
We pooled continuous data by calculating the standardised mean difference (SMD), together with 95% CI. We used the SMD to combine different scales for measuring depressive symptoms or relationship distress across studies.
Unit of analysis issues
We did not find any cluster randomised or cross‐over trials.
Studies with multiple treatment groups
In five out of 14 studies, couple therapy was compared with two control conditions (Beach 1992; Bodenmann 2008a; Jacobson 1991; Lemmens 2009; Teichman 1995). We first identified the control conditions relevant to our analysis, then for the two studies, Beach 1992 and Teichman 1995, in which two control conditions fulfilled our inclusion criteria, we performed two pairwise independent comparisons of couple therapy and each control condition.
Dealing with missing data
We checked for each study whether an intention‐to treat‐analysis was performed. If not, we checked the possibility of acceptable reasons for missing data. In the absence of any acceptable reason, we noted the risk of bias from incomplete outcome data in the 'risk of bias' table.
Assessment of heterogeneity
We estimated heterogeneity through the Chi2 test and the I2 statistic, to have an estimate of the percentage of variability not due to chance alone. We followed the guidelines of the Cochrane Handbook, in which a rough guide to interpretation of I2 values is presented (Higgins 2011):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: may represent considerable heterogeneity.
Moreover, we took into account that the importance of the observed value of I2 statistic depends on (i) magnitude and direction of effects and (ii) strength of evidence for heterogeneity (e.g. P value from the chi2 test). If important heterogeneity emerged, we considered the investigation of the sources.
Assessment of reporting biases
We assessed the studies to identify selective outcome reporting. This has been considered as a source of bias and noted in the 'risk of bias' table.Concerning publication bias, we first considered performing an inspection of funnel plots, but the small number of studies available prevented us from using tests for funnel plot asymmetry.
Data synthesis
We used the random‐effects model to compute SMD and RR. The estimates produced through random‐effects models provide a conservative estimate of the average treatment effect, in contrast with fixed‐effect models, which provide the best estimate of the treatment effect (DerSimonian 1986). As we suspected heterogeneity among studies, we used the random‐effects model.
Subgroup analysis and investigation of heterogeneity
As previously mentioned, there is a consistent finding that relationship distress is a risk factor for depression and it has been suggested that reduction of relationship distress works as a mediator for improvement of depression. Therefore, our aim was to perform subgroup analyses by investigating separately the effects of couple therapy in distressed and nondistressed couples. However, we have not been able to conduct the planned analyses due to the lack of sufficient data.
We addressed and identified heterogeneity. When we found results showing substantial or considerable heterogeneity (i.e. substantial 50‐90%, considerable 75‐100%), we investigated whether heterogeneity substantially altered the results. If yes, we commented on this in the text.
Sensitivity analysis
The earlier version of this analysis did not include any sensitivity analysis. However, in this update we decided to perform two sensitivity analyses according to the following criteria:
1. Randomisation: Removal of the only quasi‐randomised study (Teichman 1995)
2. Eligibility: Removal of the studies in which the presence of relationship distress was not an inclusion criterion.
Summary of findings table
The first author (AB) prepared the 'Summary of findings' table for all comparisons, addressing the primary and secondary outcomes of depressive symptoms, persistence of depression, dropout rates and relationship distress. We rated the quality according to the GRADE Working Group grades of evidence (Higgins 2011). In the table, the primary and secondary outcomes are included. We calculated the assumed risk on the basis of the control groups' risk.
Results
Description of studies
See the Characteristics of included studies and the Excluded studies tables.
Results of the search
We conducted the first search for the first edition of this review in September 2005 and five further searches in March 2010, September 2014, May 2015, February 2016 and February 2018. After removing duplicates, we identified 400 records potentially relevant for our review. We excluded 370 records on the basis of information provided by titles and abstracts. We read the full text of 30 studies to assess their eligibility. We judged a total of 14 studies with 651 participants as eligible (Figure 1), adding six studies to those included in the earlier version.
1.
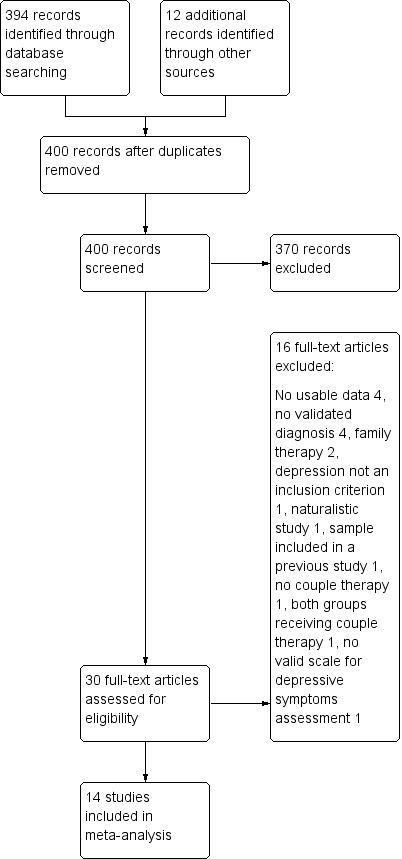
Study flow diagram
We sought information about unpublished or unclear data from the authors of the following studies: Beach 1992, Bodenmann 2008a, Dessaulles 2003, Emanuels 1996, Emanuels 1997, Jacobson 1991, Leff 2000, Seikkula 2012 and Teichman 1995. Beach 1992, Bodenmann 2008a, Seikkula 2012 and Teichman 1995 provided the requested information.
Included studies
Study design
All studies used a parallel group design. Thirteen of the included studies were randomised controlled trials. Teichman 1995 reported that assignment to treatment groups was random but restricted by therapist availability. Therefore, we considered this study as a quasi‐randomised trial.
Sample size
Fourteen studies randomised a total of 651 participants, ranging from 18 in Dessaulles 2003 and Foley 1989 to 83 in Lemmens 2009. The number of participants in each arm ranged between nine and 40.
Setting
All studies were conducted in outpatient mental health settings, although in Lemmens 2009, the treatment started during inpatient admission in some cases. Teichman 1995 was carried out in Israel, Leff 2000 in the United Kingdom, Bodenmann 2008a in Switzerland, Lemmens 2009 in Belgium, Seikkula 2012 in Finland, Dessaulles 2003 in Canada, two studies came from The Netherlands (Emanuels 1996; Emanuels 1997), and six studies came from the USA (Beach 1992; Cohen 2010; Denton 2012; Foley 1989; Jacobson 1991; Compton 2008).
Duration of follow‐up
In all studies, assessment was done at the end of the treatment. In addition, ten studies carried out follow‐up ranging from three months in Cohen 2010 and Dessaulles 2003 to two years (Leff 2000; Seikkula 2012). In four studies, follow‐up was longer than one year (Bodenmann 2008a; Leff 2000; Lemmens 2009; Seikkula 2012). However, in two studies it was not possible to ascertain whether the follow‐up period was intended after the end of treatment or did include the treatment itself (Lemmens 2009; Seikkula 2012). According to our definition, three studies (Bodenmann 2008a, Dessaulles 2003, Teichman 1995) provided data for short‐term follow‐up (6 months) and three studies (Bodenmann 2008a, Lemmens 2009, Seikkula 2012) provided data for long‐term follow‐up (15‐24 months).
Participants
Gender
Five studies included depressed women only in both experimental and control groups (Beach 1992; Cohen 2010; Denton 2012; Dessaulles 2003; Jacobson 1991). Eight studies included both men and women with depression (Bodenmann 2008a; Emanuels 1996; Emanuels 1997; Foley 1989; Leff 2000; Lemmens 2009; Seikkula 2012; Teichman 1995). In four studies, the proportion of women in the experimental group ranged from 50% (Bodenmann 2008a), to 64% (Lemmens 2009). In four studies, the proportion of women was reported for the full sample, without indicating the distribution by gender between the experimental and control groups. The proportion of women ranged from 53% (Emanuels 1996; Teichman 1995), to 72% (Foley 1989). Compton 2008 included couples with a depressed spouse, without giving any information on distribution by gender.
Age
The mean age of the participants was between 34 and 48 years, with the exception of the study by Compton 2008, which targeted older adults with a mean age of 68 years.
Diagnosis
Twelve studies included cases meeting criteria for major depressive disorder according to DSM‐III or DSM‐IV (Beach 1992; Bodenmann 2008a; Cohen 2010; Denton 2012; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Jacobson 1991; Lemmens 2009; Compton 2008; Seikkula 2012; Teichman 1995). Among them, four studies included also participants with dysthymia (Beach 1992; Bodenmann 2008a; Cohen 2010; Teichman 1995). The study by Foley 1989 used the Research Diagnostic Criteria definition of depression (Spitzer 1978), and the study by Leff 2000 used the Present State Examination (Wing 1974).
Relationship distress
In seven studies, relationship distress was an inclusion criterion (Beach 1992; Denton 2012; Dessaulles 2003; Emanuels 1996; Foley 1989; Leff 2000; Compton 2008). In three studies that included either couples with and without relationship distress, the authors did not show the distribution according to this variable (Bodenmann 2008a; Cohen 2010; Lemmens 2009; Seikkula 2012). In the study by Jacobson 1991, in the treatment group 42% of couples showed relationship distress. In Emanuels 1997, couples were selected as showing no distress. In the study by Teichman 1995, the couples' status about relationship distress was not specified.
Recruitment
In five studies, the population was identified through a mix of newspaper advertisement and referral by general practitioners or mental health clinics (Dessaulles 2003; Emanuels 1996; Emanuels 1997; Jacobson 1991; Leff 2000); five studies recruited the participants from among those who sought treatment in mental health clinics (Cohen 2010; Foley 1989; Compton 2008; Seikkula 2012; Teichman 1995), two studies recruited participants from private practices (Bodenmann 2008a; Denton 2012). Lemmens 2009 included referrals to a psychiatric department of a university hospital and Beach 1992 relied on newspaper advertisements only.
Interventions
Intervention group
Although not all the papers described the treatment condition thoroughly, treatment models were defined as cognitive‐behavioural (Beach 1992; Bodenmann 2008a; Cohen 2010; Emanuels 1996; Emanuels 1997; Jacobson 1991; Compton 2008; Teichman 1995), emotion focused, based on integration of systemic and experiential approaches (Denton 2012; Dessaulles 2003), interpersonal (Foley 1989), and systemic (Leff 2000; Lemmens 2009; Seikkula 2012). The therapies in the Leff, Bodenmann and Denton studies were described according to manuals (Bodenmann 2004; Johnson 2004; Jones 1999). Denton assessed the therapists' adherence to the manual by using a fidelity scale (Denton 2009). The study by Emanuels 1997 was included, although the experimental treatment was defined by the authors as ‘spouse‐aided therapy’, not as couple therapy. However, spouse‐aided therapy is based on the concept of marital homeostasis and it has been defined as a form of couple therapy, because it was designed to enable spouses to identify and stop their contribution to the patient’s disorder (Hafner 1983). Moreover, papers on spouse‐aided therapy have been usually included in reviews of couple therapy (Denton 2003). Therefore, we concluded that this study met our inclusion criteria. In the study by Lemmens 2009, the experimental treatment was labelled as 'single family therapy'. However, a close examination of the paper showed that actually the intervention was couple therapy.
The treatment was delivered in weekly sessions, ranging between 15 and 20 in six studies (Beach 1992; Denton 2012; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Teichman 1995). The study by Jacobson 1991 reported the number of 20 sessions, without specifying the interval between sessions. In the study by Compton 2008, the treatment was delivered in 26 weekly sessions, in the study by Bodenmann 2008a, in 10 biweekly sessions, in the study by Lemmens 2009, in six biweekly sessions plus one session after three months, in the study by Cohen 2010, in five weekly sessions. One study did not set up a fixed treatment length (Seikkula 2012), but set the minimum number of five sessions and reported that an average number of 11 sessions was delivered to the couple therapy group (range 5 to 33). The study by Leff 2000 reported a number of 12 to 20 sessions, without specifying the treatment length.
All studies reported that sessions were conducted by well‐trained expert therapists. Four studies assessed the treatment fidelity (Cohen 2010; Denton 2012; Dessaulles 2003; Jacobson 1991).
Control group
The control treatments were described as individual cognitive‐behavioural therapy in seven studies (Beach 1992; Bodenmann 2008a; Emanuels 1996; Emanuels 1997; Jacobson 1991; Lemmens 2009; Teichman 1995), and as interpersonal individual psychotherapy in the Foley 1989 study. Seikkula 2012 did not specify the individual psychotherapy model, but information from other papers by his research group led to the identification of a psychodynamic model. Two studies included, in addition to the individual therapy group, a no treatment/waiting list condition (Beach 1992; Teichman 1995). Three studies compared couple therapy with antidepressant drug therapy (Denton 2012; Dessaulles 2003; Leff 2000). The study by Denton was an augmentation study in which the couple therapy did receive antidepressant drugs as well. Cohen 2010 randomised the control group to the waiting list condition. Three studies also included an additional control condition not relevant to our analysis (Bodenmann 2008a; Jacobson 1991; Lemmens 2009).
In almost all studies, the number of sessions and treatment length were the same in the control group and in the intervention group. The only exception was the study by Bodenmann 2008a, in which the individual cognitive‐behavioural therapy was delivered in 20 weekly sessions, by contrast with 10 biweekly sessions of couple therapy.
All studies reported that individual therapy sessions were conducted by well‐trained expert therapists. Treatment fidelity was assessed in one study (Jacobson 1991).
Outcomes
We were able to extract data on mental health (i.e. depressive symptoms and persistence of depression), on study retention (i.e. dropouts), and on relationship distress.
For depression, seven studies used self‐rated questionnaires, i.e. the BDI (Beach 1992; Cohen 2010; Emanuels 1996; Emanuels 1997; Lemmens 2009; Teichman 1995), and the IDD (Dessaulles 2003). Three studies used clinician‐rated scales: Foley 1989 and Compton 2008 used the HRSD, and Denton 2012 the IDS‐C30. Four studies used both a self‐report (BDI) and a clinician rated (HRSD) scale (Bodenmann 2008a; Jacobson 1991; Leff 2000; Seikkula 2012). Three studies used recovery from depression as an outcome criterion (Beach 1998; Jacobson 1993; Teichman 1995), setting slightly different thresholds on BDI to define a participant as recovered. As far as relationship distress is concerned, the DAS was used in six studies (Beach 1992; Cohen 2010; Dessaulles 2003; Jacobson 1991; Compton 2008; Seikkula 2012). Foley 1989 used both the DAS and the LWMAS, but did not present usable data on the DAS global score. Therefore, we used data from the LWMAS for this analysis. Emanuels 1996 and Emanuels 1997 used the MMQ. Denton 2012 used the QMI. Lemmens 2009 assessed relationship distress by DAS in the study sample at baseline only. Leff 2000 included changes in relationship distress as an outcome criterion, but did not present data about this issue. Although values on relationship distress were usually presented as continuous, Beach 1992 and Jacobson 1991 computed a threshold to identify the full resolution of marital distress, thus allowing analyses of dichotomous data. Bodenmann 2008a used three measures to assess relational quality: Partnership Questionnaire (Hahlweg 1996), Dyadic Coping Inventory (Bodenmann 2008b) and Five‐Minute Speech Sample (Magaña 1986), failing to produce usable data for analysis.
Excluded studies
We excluded sixteen studies: one because the mothers' depression was part of a wider problem related to the presence of a disruptive child and the experimental group was treated by family therapy (Sanders 2000); three, reported by the same author (Waring 1990; Waring 1994; Waring 1995), because they did not give enough information to extract any data. We excluded the study by Jacobson 1993 because it reported a follow‐up of the sub‐sample of recovered participants already included in a previous clinical trial. We excluded the study by Friedman 1975 because primary diagnosis of depressive disorder was not settled according to an internationally validated diagnostic system, and it provided only poor description of the couple therapy offered. In the study of Dick‐Grace 1995, the intervention was cognitive therapy offered according to three modalities: individual, couple, and family, but useful data could not be extracted. Tilden 2010 used a naturalistic prospective design and the intervention was delivered during inpatient admission. The Swanson study tested an intervention entirely focused on the meaning of experience of miscarriage and did not adopt principles and methods of couple therapy (Swanson 2009). In Noorbala 2008, the intervention was cognitive therapy plus supportive therapy for infertility aiming at resolving symptoms in women undergoing infertility treatment. The comparison was between psychological treatment offered before and during infertility treatment. In Miller 2005, the experimental group was treated by family therapy in an inpatient setting. Moreover, data were given according to matching and mismatching of the assigned treatment to the clinicians' evaluation of the participants' needs and not according to randomisation. In four studies, no formal diagnosis of depression was made (Kröger 2012, Hajiheidari 2013; Hashemi 2017; Soltani 2014). In Shahverdi 2015, the primary outcome was improvement of general mental health, not depressive symptom level.
Ongoing studies
We did not identify any ongoing study.
Studies awaiting classification
We did not identify any study awaiting classification.
Risk of bias in included studies
See the Risk of Bias Table of each study in the Characteristics of included studies table and the summaries of the results in Figure 2 and Figure 3.
2.
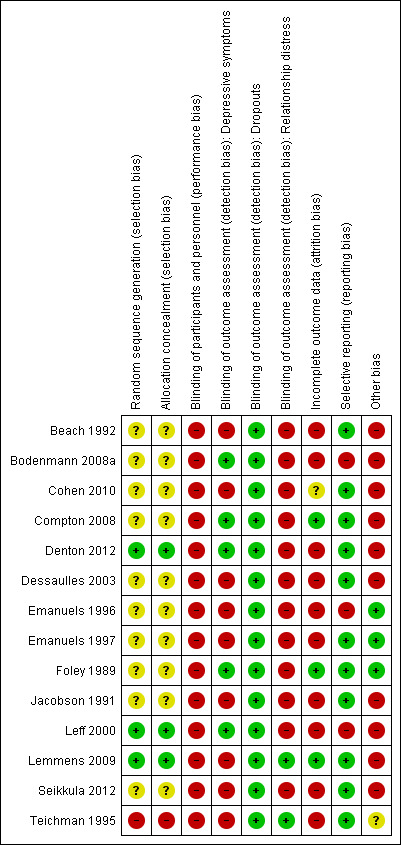
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
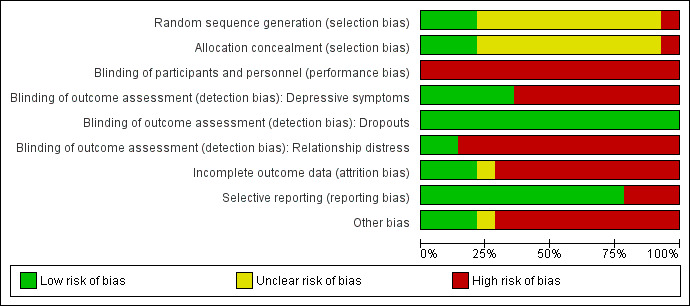
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
We assessed random sequence generation and allocation concealment separately. We judged ten studies to be at unclear risk of selection bias for not providing adequate information on both aspects (Beach 1992; Bodenmann 2008a; Cohen 2010; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Foley 1989; Jacobson 1991; Compton 2008; Seikkula 2012). We judged three studies to be at low risk of selection bias as they clearly reported a satisfactory randomisation procedure (Denton 2012; Leff 2000; Lemmens 2009). In Teichman 1995, the author, when giving us information about unpublished data, specified that allocation was randomised restricted by therapist availability. Participants who were screened and received a diagnosis of depression were assigned to the first available therapist and each therapist practiced only one type of treatment. Morever, no details about allocation concealment were provided. Therefore, we classified this study at high risk of selection bias.
Blinding
Blinding of patients and personnel
Blinding of participants and clinicians is not feasible in studies of psychological interventions, therefore failure to meet this criterion led us to consider all studies at high risk of performance bias.
Blinding of outcome assessment: depressive symptoms
Depressive symptoms were assessed in seven studies by self‐report measures only (Beach 1992; Cohen 2010; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Lemmens 2009; Teichman 1995). Since participants were always aware of the treatment they received, we considered studies using self‐report measures were at high risk of detection bias. We considered free of detection bias two studies reporting blind assessment of depression by expert‐rated measures, in addition to self‐rating by participants (Bodenmann 2008a; Leff 2000). In three studies, expert‐rated measures only were used and blindness was achieved (Denton 2012; Foley 1989; Compton 2008). We judged to be at unclear risk of detection bias two studies, because the authors, although using expert‐rated measures, did not provide adequate information on blindness (Jacobson 1991; Seikkula 2012).
Blinding of outcome assessment: dropouts
In all studies reporting this outcome we judged dropout rates assessment at low risk of bias (Beach 1992; Bodenmann 2008a; Compton 2008; Denton 2012; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Foley 1989; Jacobson 1991; Leff 2000; Lemmens 2009; Seikkula 2012; Teichman 1995).
Blinding of outcome assessment: relationship distress
Assessment of relationship distress was done in twelve studies by self‐report measures, thus carrying a high risk of detection bias (Beach 1992; Bodenmann 2008a; Cohen 2010; Denton 2012; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Foley 1989; Jacobson 1991; Leff 2000; Compton 2008; Seikkula 2012). The remaining studies did not assess this outcome.
Incomplete outcome data
In ten studies, the analysis was conducted on completers only or failed to include all dropouts or cases lost to follow‐up (Beach 1992; Bodenmann 2008a; Denton 2012; Dessaulles 2003; Emanuels 1996; Emanuels 1997; Jacobson 1991; Leff 2000; Seikkula 2012; Teichman 1995). Therefore, we judged these studies to be at high risk of attrition bias. We judged at low risk of attrition bias three studies that either conducted an intention‐to treat analysis or reported no missing data (Foley 1989; Lemmens 2009; Compton 2008). We assumed that an intention‐to‐treat analysis was performed when a) trial participants were analysed in the groups in which they were randomised, regardless of how long they were actually treated, and b) all participants were included regardless of whether their outcomes were actually collected. In one study, analyses were conducted using hierarchical linear modelling (Cohen 2010). This is appropriate for handling missing data, but no usable data were presented according to this analysis. Therefore, we judged the risk of attrition bias in this study to be unclear.
One study used a likelihood approach in order to allow for dropouts and to produce valid parameter estimates and standard errors, as long as the dropouts were not informative (Leff 2000). Moreover, in this same study, the one‐year follow‐up was comprised only of those who completed treatment, whereas in the two‐year follow‐up, some participants who had dropped out of treatment were also evaluated and included in the analysis.
Selective reporting
We found full reports of all outcomes in nine studies (Beach 1992; Cohen 2010; Dessaulles 2003; Emanuels 1997; Jacobson 1991; Lemmens 2009; Compton 2008; Seikkula 2012; Teichman 1995), and these studies were judged to be at low risk of reporting bias. We judged the risk of reporting bias to be high in five studies that failed to report data on all prespecified outcomes (Bodenmann 2008a; Denton 2012; Emanuels 1996; Foley 1989; Leff 2000).
Other potential sources of bias
In five studies, the principal investigator was strongly involved in the development of the experimental treatment or was among the clinicians providing the treatment, thus raising the possibility of allegiance bias or conflict of interest (Beach 1992; Cohen 2010; Denton 2012; Dessaulles 2003; Jacobson 1991). We considered these studies to be at high risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Comparison 1. Couple therapy versus individual psychotherapy
Nine studies, including 364 participants, contributed data to this comparison. See Table 1 and Table 2.
Primary outcomes
1.1 Depressive symptom level
a) Continuous data
Compared with individual psychotherapy, there was low‐quality evidence from nine studies with 304 participants showing no evidence of difference in the level of depressive symptoms at the end of treatment (SMD −0.17, 95% confidence interval (CI) −0.44 to 0.10; Analysis 1.1). No relevant heterogeneity was found. Compared with individual psychotherapy, there was low‐quality evidence from two studies with 59 participants showing no evidence of difference in the level of depressive symptoms at 6‐month follow‐up (SMD −0.25, 95% CI −0.77 to 0.27; Analysis 1.2). We did not find relevant heterogeneity. Compared with individual psychotherapy, there was low‐quality evidence from three studies with 117 participants showing no evidence of difference in the level of depressive symptoms at 15/24‐month follow‐up (SMD −0.34, 95% CI −0.78 to 0.10; Analysis 1.3). No relevant heterogeneity was found.
1.1. Analysis.
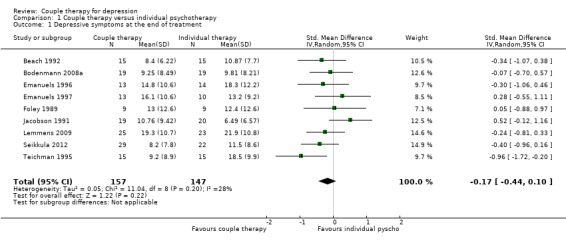
Comparison 1 Couple therapy versus individual psychotherapy, Outcome 1 Depressive symptoms at the end of treatment.
1.2. Analysis.
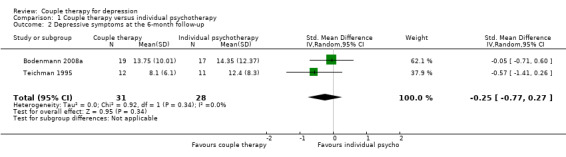
Comparison 1 Couple therapy versus individual psychotherapy, Outcome 2 Depressive symptoms at the 6‐month follow‐up.
1.3. Analysis.
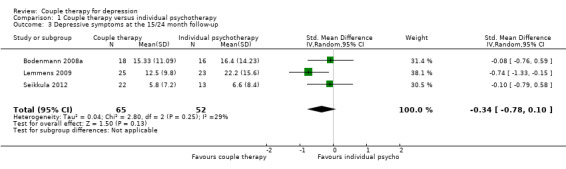
Comparison 1 Couple therapy versus individual psychotherapy, Outcome 3 Depressive symptoms at the 15/24 month follow‐up.
b) Dichotomous data (persistence of depression)
Compared with individual psychotherapy, there was low‐quality evidence from six studies with 237 participants showing no evidence of difference in persistence of depression at the end of treatment (RR 0.94, 95% CI 0.72 to 1.22; Analysis 1.4). We did not find relevant heterogeneity. Compared with individual psychotherapy, there was very low‐quality evidence from a single study with 23 participants showing no evidence of difference in persistence of depression at 6‐month follow‐up (RR 0.76, 95% CI 0.32 to 1.80; Analysis 1.5). No data were available for this outcome at 15/24 month follow‐up.
1.4. Analysis.
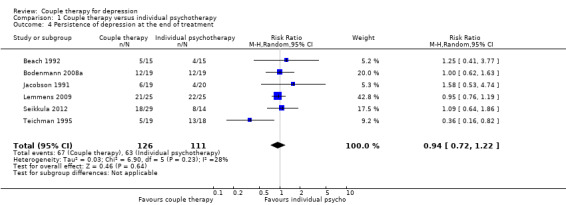
Comparison 1 Couple therapy versus individual psychotherapy, Outcome 4 Persistence of depression at the end of treatment.
1.5. Analysis.

Comparison 1 Couple therapy versus individual psychotherapy, Outcome 5 Persistence of depression at 6‐month follow‐up.
1.2 Dropouts
Compared with individual psychotherapy, there was low‐quality evidence from nine studies with 364 participants showing no difference in dropout rates at the end of treatment (RR 0.85, 95% CI 0.51 to 1.41; Analysis 1.6). We did not find relevant heterogeneity. This outcome was not applicable at 6‐month and 15/24‐month follow‐up.
1.6. Analysis.

Comparison 1 Couple therapy versus individual psychotherapy, Outcome 6 Dropouts.
Secondary outcomes
1.3 Relationship distress
a) Continuous data
Compared with individual psychotherapy, there was very low‐quality evidence from six studies with 187 participants showing that couple therapy appeared to be more effective in reducing the level of distress assessed at the end of treatment (SMD −0.50, 95% CI −0.97 to −0.02; Analysis 1.7). However, this finding is weakened by a substantial heterogeneity (I2 = 59%). No data were available for this outcome at 6‐month follow‐up. Compared with individual psychotherapy, there was very low‐quality evidence from a single study with 34 participants showing no difference in level of distress assessed at 15/24‐month follow‐up (SMD 0.12, 95% CI −0.59 to 0.82; Analysis 1.8)
1.7. Analysis.
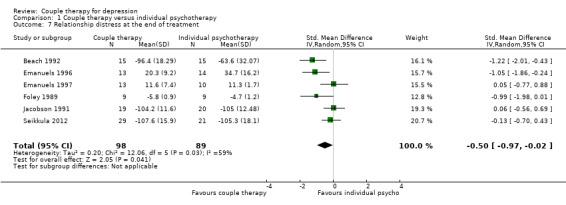
Comparison 1 Couple therapy versus individual psychotherapy, Outcome 7 Relationship distress at the end of treatment.
1.8. Analysis.
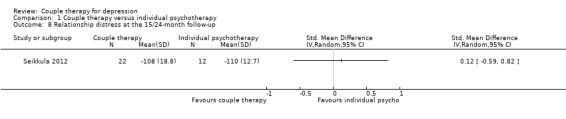
Comparison 1 Couple therapy versus individual psychotherapy, Outcome 8 Relationship distress at the 15/24‐month follow‐up.
b) Dichotomous data (persistence of relationship distress)
Compared with individual psychotherapy, there was very low‐quality evidence from two studies with 81 participants showing a difference favouring couple therapy (RR 0.71, 95% CI 0.51 to 0.98; Analysis 1.9). We did not find relevant heterogeneity. No data were available for this outcome at 6‐month or 15/24‐month follow‐up.
1.9. Analysis.

Comparison 1 Couple therapy versus individual psychotherapy, Outcome 9 Persistence of relationship distress at the end of treatment.
Comparison 2. Couple therapy versus drug therapy
Two studies including 95 participants contributed data to this comparison (Dessaulles 2003; Leff 2000).
Primary outcomes
2.1 Depressive symptom level
a) Continuous data
Compared with drug therapy, there was very low‐quality evidence from a single study with 12 participants showing no evidence of difference in the level of depressive symptoms at the end of treatment (standard mean difference (SMD −0.51, 95% confidence interval (CI) −1.69 to 0.66; Analysis 2.1). Compared with drug therapy, there was very low‐quality evidence from a single study with 12 participants showing no evidence of difference in the level of depressive symptoms at 6‐month follow‐up (SMD −1.07, 95% CI ‐2.45 to 0.31: Analysis 2.2).
2.1. Analysis.
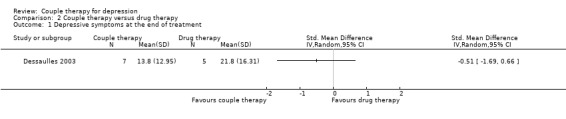
Comparison 2 Couple therapy versus drug therapy, Outcome 1 Depressive symptoms at the end of treatment.
2.2. Analysis.
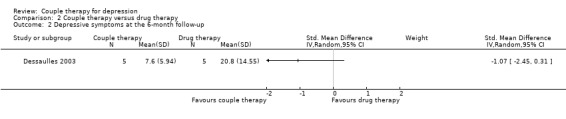
Comparison 2 Couple therapy versus drug therapy, Outcome 2 Depressive symptoms at the 6‐month follow‐up.
2.2 Dropouts
Compared with drug therapy, there was very low‐quality evidence from two studies with 95 participants showing a difference favouring couple therapy in dropout rates at the end of treatment (RR 0.31, 95% CI 0.15 to 0.61; Analysis 2.3). We did not find relevant heterogeneity.
2.3. Analysis.
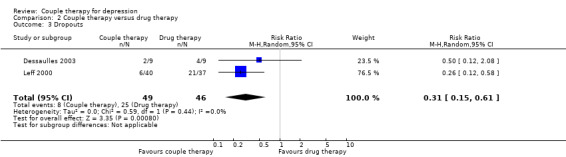
Comparison 2 Couple therapy versus drug therapy, Outcome 3 Dropouts.
Secondary outcomes
2.3 Relationship distress
a) Continuous data
Compared with drug therapy, there was very low‐quality evidence from a single study with 12 participants showing no evidence of difference in the level of distress assessed at the end of treatment (SMD −0.47, 95% confidence interval (CI) −1.64 to 0.70: Analysis 2.4). Compared with drug therapy, there was very low‐quality evidence from a single study with 12 participants showing no evidence of difference in the level of depressive symptoms at 6‐month follow‐up (SMD −0.99, 95% CI ‐2.35 to 0.37: Analysis 2.5). No data were available for this outcome at 15/24‐month follow‐up.
2.4. Analysis.
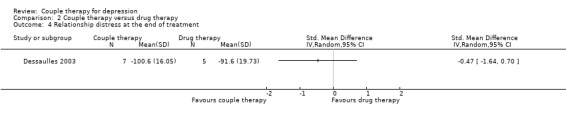
Comparison 2 Couple therapy versus drug therapy, Outcome 4 Relationship distress at the end of treatment.
2.5. Analysis.

Comparison 2 Couple therapy versus drug therapy, Outcome 5 Relationship distress at the 6‐month follow‐up.
b) Dichotomous data (persistence of relationship distress)
No data were available.
Comparison 3. Couple therapy versus no/minimal treatment
Three studies including 90 participants contributed data to this comparison (Beach 1992; Cohen 2010; Teichman 1995).
Primary outcomes
3.1 Depressive symptom level
a) Continuous data
Compared with no/minimal treatment, there was very low‐quality evidence from three studies with 90 participants showing that couple therapy appeared more effective in reducing the level of depressive symptoms at the end of treatment (SMD −0.95, 95% CI −1.59 to −0.32: Analysis 3.1). However, we are very uncertain about this finding, due to the small number of studies contributing data to this comparison and the substantial heterogeneity (I2 = 50%) identified. No data were available for this outcome at 6‐month and 15/24‐month follow‐up.
3.1. Analysis.

Comparison 3 Couple therapy versus no/minimal treatment, Outcome 1 Depressive symptoms at the end of treatment.
b) Dichotomous data (persistence of depression)
Compared with no/minimal treatment, there was very low‐quality evidence from two studies with 65 participants favouring couple therapy in reducing the persistence of depression at the end of treatment (RR 0.48, 95% CI 0.32 to 0.70: Analysis 3.2). We did not find relevant heterogeneity.
3.2. Analysis.

Comparison 3 Couple therapy versus no/minimal treatment, Outcome 2 Persistence of depression at the end of treatment.
3.2. Dropouts
No data were available.
Secondary outcomes
3.3. Relationship distress
a) Continuous data
Compared with no/minimal treatment, there was very low‐quality evidence from two studies with 60 participants showing no difference in the level of distress assessed at the end of treatment (SMD −0.80, 95% CI −1.64 to 0.04; Analysis 3.3). However, we are very uncertain about this finding, due to the small number of studies contributing data to this comparison and the substantial heterogeneity (I2 = 59%) identified. No data were available for this outcome at 6‐month and 15/24‐month follow‐up.
3.3. Analysis.
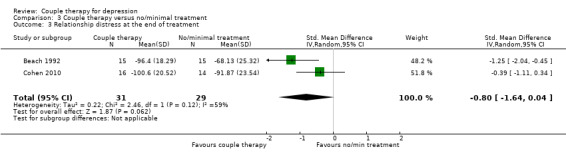
Comparison 3 Couple therapy versus no/minimal treatment, Outcome 3 Relationship distress at the end of treatment.
b) Dichotomous data (persistence of relationship distress)
No data were available.
Comparison 4. Couple therapy plus drug therapy versus drug therapy alone
Two studies, including 45 participants, contributed data to this comparison (Denton 2012; Compton 2008).
Primary outcomes
4.1 Depressive symptom level
a) Continuous data
In couple therapy plus drug therapy compared with drug therapy alone, there was very low‐quality evidence from two studies with 34 participants showing no evidence of difference in the level of depressive symptoms at the end of treatment (SMD −1.04, 95% CI ‐3.97 to 1.89: Analysis 4.1). However, we are very uncertain about this finding, due to the small number of studies contributing data to this comparison and the considerable heterogeneity (I2 = 89%) identified. No data were available for this outcome at 6‐month and 15/24‐month follow‐up.
4.1. Analysis.
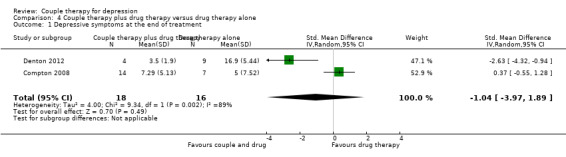
Comparison 4 Couple therapy plus drug therapy versus drug therapy alone, Outcome 1 Depressive symptoms at the end of treatment.
b) Dichotomous data (persistence of depression)
No data were available.
4.2 Dropouts
In couple therapy plus drug therapy compared with drug therapy alone, there was very low‐quality evidence from two studies with 45 participants showing no difference in dropout rates at the end of treatment (RR 1.03, 95% CI 0.07 to 15.52; Analysis 4.2). However, we are very uncertain about this finding, due to the small number of studies contributing data to this comparison and the substantial heterogeneity (I2 = 63%) identified.
4.2. Analysis.

Comparison 4 Couple therapy plus drug therapy versus drug therapy alone, Outcome 2 Dropouts.
Secondary outcomes
4.3 Relationship distress
a) Continuous data
In couple therapy plus drug therapy compared with drug therapy alone, there was very low‐quality evidence from two studies with 34 participants showing no evidence of difference in the level of relationship quality at the end of treatment (SMD −0.60, 95% CI −1.35 to 0.14; Analysis 4.3). No heterogeneity was found.
4.3. Analysis.

Comparison 4 Couple therapy plus drug therapy versus drug therapy alone, Outcome 3 Relationship distress at the end of treatment.
b) Dichotomous data (persistence of relationship distress)
No data were available.
Sensitivity analysis
The removal of the quasi‐randomised trial by Teichman 1995 did not materially change the results of the main comparison between couple therapy and individual therapy in relation to the level of depressive symptoms. No evidence of difference was found (SMD −0.09, 95% CI −0.38 to 0.15).
The removal of the studies where the presence of relationship distress was not an inclusion criterion did not materially change the results of the main comparison between couple therapy and individual therapy in relation to the level of depressive symptoms. No evidence of difference was found (SMD −0.23, 95% CI −0.69 to 0.22). By contrast, in relation to the level of relationship distress, data showed a large difference favouring couple therapy (SMD −1.10, 95% CI −1.59 to −0.61). We did not find any heterogeneity, thus raising the possibility that the inclusion of both distressed and non‐distressed couples in most studies was a source of heterogeneity for the relationship distress outcome.
However, these results should be considered with great caution, because they are weakened by the low number of studies and participants (three studies with 75 participants).
Discussion
Summary of main results
1 Couple therapy vs individual psychotherapy
Low‐quality evidence suggests that there is no difference between couple therapy and individual psychotherapy as a treatment targeted to depressive symptoms. We found no difference at the end of treatment, at 6‐month and 15/24‐month follow‐up either considering continuous (depressive symptoms) or dichotomous (persistence of depression) outcome measures. Only in one study (Teichman 1995), couple therapy was more effective in improving depression. However, this study had the highest risk of bias for a variety of reasons. Even by removing the studies where couple discord was not an inclusion criterion, no evidence of difference was found. Actually, couple therapy and individual psychotherapy were both effective in reducing the depressive symptoms and, to a lesser extent, in inducing remission from depression.
None of the trials considered adverse effect outcomes. However, we considered dropout rates or rates of treatment discontinuation for any reason as a proxy indicator of adverse outcomes. We did not find any difference in effect for dropout rates between couple therapy and individual psychotherapy, based on eight low‐quality studies with 316 participants.
Concerning relationship distress, very low‐quality evidence supported the efficacy of couple therapy. We found relevant heterogeneity among the studies providing data for this analysis. In two studies (Beach 1992; Emanuels 1996), a strong effect favouring couple therapy was found, whereas other studies showed no difference (Emanuels 1997; Foley 1989; Jacobson 1991; Seikkula 2012). However, only three studies restricted the inclusion to distressed couples (Beach 1992; Emanuels 1996; Foley 1989). One study selected non‐distressed couples (Emanuels 1997), and the remaining studies included both distressed and non distressed couples. Therefore, the effect was weakened by the presence in the samples of a number of non‐discordant couples. The sensitivity analysis, done by removing the studies where relationship distress was not an inclusion criterion, actually showed a large effect favouring the couple therapy, with no heterogeneity.
The hypothesis assumed by the main models of couple therapy (Gupta 2003), i.e. that the improvement in the couple relationship works as a mediator for the improvement of depression, was not adequately tested. An attempt in this direction was made in one study (Beach 1992). The authors used multiple regression to show that change in marital satisfaction was a mediator of change in depression, because the coefficient for change in level of depression became non‐significant when change in couple adjustment was added in the regression model. However, this result was derived from the analysis of a very small subsample of 13 participants.
2 Couple therapy vs drug therapy
Data on depressive symptoms and relationship distress from a single small study providing very low‐quality evidence showed no difference. Data on dropouts from two studies showed a clear advantage for couple therapy. However, the quality of evidence was very low, because this positive result was strongly influenced by a single study (Leff 2000), where a large effect favouring couple therapy was found. In this study, there was a strong suggestion of a selection bias, possibly leading to the inclusion of participants seeking an alternative to drug treatment.
3 Couple therapy vs no/minimal treatment
All three studies providing data for this analysis used waiting lists as a control condition. Very low‐quality evidence showed a large effect of couple therapy in reducing depressive symptoms. Data favouring couple therapy on full remission of depression come from only two small studies. Very low‐quality evidence showed no difference in reduction of relationship distress. Out of the two small studies providing data for this outcome, one did not use relationship distress as an inclusion criterion.
4 Couple therapy plus drug therapy vs drug therapy alone
Two small studies provided data on the comparison between couple therapy alone versus couple therapy plus drug treatment. Very low‐quality evidence showed no difference in depressive symptoms, dropouts, and relationship distress.
Overall completeness and applicability of evidence
The conclusions of this meta‐analysis are mainly applicable to the comparison of couple versus individual psychotherapy for depression and relationship outcomes. The treatment modalities of couple therapy presented in the trials met the common features of couple therapy as described in the clinical literature (Benson 2012). Both couple therapy and individual psychotherapy were delivered by competent therapists.
The very low‐quality of evidence for other comparisons limits our ability to make confident conclusions about the efficacy of couple therapy versus drug therapy (two studies with 95 participants); no/minimal treatment (three studies with 90 participants) and on the comparison between couple therapy plus drug therapy and drug therapy alone (two studies with 45 participants).
The studies reviewed came from Europe, North America, and Israel. The ethnic background of participants was reported only in four studies, showing an overwhelming majority of more than 80% of Caucasians. Therefore, the findings cannot be considered applicable to non‐Western countries and not even to ethnic minorities in the Western world. The depressed partner was a woman in 70% of cases. However, this higher percentage was mainly due to five studies with 194 participants restricting the recruitment to couples with a depressed woman. Studies not using this inclusion criterion showed a more balanced gender distribution (54% women vs 46% men). Overall, the results can be applied to both sexes. Mean scores of scales assessing depressive symptoms of study participants at baseline showed moderate depression severity (BDI scores ranging from 22 to 27). Therefore, most study participants had moderate depression and the results cannot be extended to severely depressed patients. Mean age of included participants was between 36 and 47 years in all studies, with the exception of the study by Compton 2008, targeted to older adults over 65 years. Therefore, the findings cannot be applied to people over 50 years.
Six studies recruited all or some of the participants through newspaper or radio advertisements (Beach 1992; Denton 2012; Emanuels 1996; Emanuels 1997; Jacobson 1991; Leff 2000). This method may lead to the inclusion of a population not fully representative of people seeking help for mental health problems, thus limiting the findings applicability to current clinical practice.
Quality of the evidence
We did not find any study was fully free of risk of bias. A major source of bias was the researcher allegiance found in most studies, whereby investigators were strongly involved in the development of the experimental treatment, thus raising the issue of conflict of interest. This is a serious problem, because recent systematic reviews confirmed that researcher allegiance is a relevant factor influencing outcome in psychotherapy research (Munder 2013). The failure to ensure blind outcome assessment was a major issue as well. We are aware that blinding of participants and clinicians is impossible in psychotherapy research, by contrast with drug therapy trials (Carroll 1994). However, the combination of knowledge of the assigned treatment by participants and providers with the use of self‐report or unblinded expert‐rated measures produced a high risk of bias in all but five studies for the primary outcome of depression and in all but one study for the relationship distress outcome. Additional relevant problems were: statistical heterogeneity, incomplete outcome data, and selective reporting, due to the failure in most studies to include dropouts in the analysis and to provide usable data on all outcomes in some studies.
See Figure 2 and Figure 3 for more information.
As previously mentioned, the small number of studies available prevented us from inspecting funnel plots for asymmetry. However, some problem in this area could be suspected from the strong allegiance of almost all researchers.
Seven studies were of small size, including fewer than fifty participants. Very wide confidence intervals in most analyses for both RRs and SMDs led to considerable imprecision.
We considered the overall quality of evidence as low for the main comparison in relation to the primary outcomes (depressive symptoms and dropouts) and very low for the secondary outcome of relationship distress. Quality was uniformly very low for all secondary comparisons. See Table 1 and Table 2. No improvement in quality was found in recent studies in comparison with the older ones.
Potential biases in the review process
Despite all efforts, it was not possible to gather full information from a number of studies showing incomplete outcome data. It is worth noting that unpublished data obtained from one author (Seikkula 2012) led to results neither presented nor commented on in published papers.
The low‐quality assessment assigned to some studies was often due to limitations in data reporting, rather than shortcomings in study design or conduction, therefore, it could have been modified if full data were made available by the authors.
Agreements and disagreements with other studies or reviews
No systematic reviews of the effect of couple therapy in depression have been performed either before or after the first version of this review. The earlier narrative review by Gupta 2003 concluded that couple‐based approaches to the treatment of depression showed considerable promise, but had substantial room for improvement in terms of efficacy and applicability, leaving a number of questions unanswered, as suggested also by Gilliam 2005.
Three further narrative reviews have been published in the last years (Denton 2006; Hollon 2012; Whisman 2012). The review by Denton 2006, without examining in detail the available trials, concluded that couple therapy was as effective in treating depression as individual therapy in discordant couples, but only couple therapy improved relationship functioning. The authors stated that the only situation where couple therapy was less effective than individual therapy was when depression was not associated with relationship distress and they considered emotion‐focused therapy as the best suited model to address depression. Hollon 2012 focused on research supporting the view of depression as an interpersonal process and referred to the first version of this meta‐analysis, reaching the same conclusion on efficacy of couple therapy as Denton 2006, but, by contrast, the authors endorsed behavioural couple therapy as the model of choice. Whisman 2012 reviewed ten trials included in this meta‐analysis and concluded that couple therapy was effective in reducing depression and relationship discord in distressed couples and depression in individuals in nondiscordant relationships. The authors noted that additional research was needed to identify mediators of the effect of couple therapy.
Overall, the main conclusions of the last narrative reviews are in agreement with ours, although they tend to overstate the effects of couple therapy. However, all authors, except for Denton 2006, failed to compare couple therapy with individual psychotherapy. All authors did not assess the quality of studies and therefore they did not consider the low quality of evidence supporting the results. Concerning the differences between couple therapy models, we have to point out that the studies included in this meta‐analysis did not provide enough data for a thorough investigation of this issue.
Authors' conclusions
Implications for practice.
This review sought to determine whether couple therapy was as effective and acceptable as individual psychotherapy, drug therapy, or no/minimal treatment in improving depressive symptoms and relationship distress. The available evidence suggests that there is no reason to consider couple therapy as more or less effective than individual psychotherapy as a treatment for depression. This holds true even when depression is associated with relationship distress. In most studies the outcome was assessed at end of treatment or at 6‐month follow‐up. Results from the few studies with a longer follow‐up did not show a better long‐term outcome for couple therapy, as suggested by some naturalistic studies (Lundblad 2006). This possibility however warrants further investigations through studies with long follow‐up.
An improvement in the relationship of discordant couples might be expected from couple therapy. Therefore, the choice of couple therapy could be justified when relationship distress is a major problem or attention to the quality of the relationship is warranted. However, the low or very low quality of evidence base limits the ability to draw firm conclusions on this issue.
Lastly, the available data cannot be applied to the elderly and to people with severe depression, because the samples studied included mostly young to middle age adults with moderate depression.
Implications for research.
Given the inclusion of couple therapy in most guidelines for treatment of depression, this review draws attention to the low or very low quality of available evidence and the need for further good quality studies. The pitfalls found in almost all studies should be addressed to produce more conclusive findings. In particular: a) researchers need to consider allegiance bias and implement studies in such a way that the allegiance bias is minimised or removed. This means that researchers should be encouraged to test interventions that are not their own interventions and to have project investigators not involved in the development of the intervention; b) clinical trials should have higher numbers of randomised participants drawn from a clinically representative practice, thus improving external validity and applicability of the findings; c) intention‐to‐treat analysis should be performed, at least for dichotomous outcomes; d) follow‐up periods should be at least one year; e) better strategies should be implemented to reduce the number of participants lost at follow‐up; f) assessment of outcome indicators should be blind; g) treatment fidelity should be assessed. The role of change in relational quality as a mediating variable in treatment of depression is relevant to understanding the specific action of couple therapy, and it needs to be better investigated through more adequate research designs and data analysis. To answer the question about superiority of couple therapy compared to individual therapy in distressed couples, the samples should be limited to couples showing relationship distress. Lastly, evidence from recent systematic reviews that the combination of individual or group psychotherapy and drug treatment is more effective in major depression than the two treatments given separately should be taken into account (Cuijpers 2009; Cuijpers 2014). Therefore, the efficacy of couple therapy in addition to drug therapy should also be investigated.
What's new
| Date | Event | Description |
|---|---|---|
| 13 April 2018 | New search has been performed | The review has been updated |
| 8 September 2016 | New citation required and conclusions have changed | The title of the review has been changed and the conclusions have been changed as a result of new searches adding six studies to those included in the earlier review |
History
Protocol first published: Issue 2, 2004 Review first published: Issue 1, 2006
| Date | Event | Description |
|---|---|---|
| 3 June 2010 | Amended | Protocol amended |
Notes
None.
Acknowledgements
The review authors wish to thank the Common Mental Disorder Group Information Specialist for assistance in developing the search strategy.
CRG Funding Acknowledgement The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Common Mental Disorders Group.
Disclaimer The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the NIHR, the NHS, or the Department of Health.
Appendices
Appendix 1. Cochrane Specialised Register
Specialised Register of the Cochrane Common Mental Disorders Group
The Cochrane Common Mental Disorders Group (CCMD) maintains two archived clinical trials registers at its editorial base in York, UK: a references register and a studies‐based register. The CCMDCTR‐References Register contains over 40,000 reports of RCTs in depression, anxiety and neurosis. Approximately 50% of these references have been tagged as individual, coded trials. The coded trials are held in the CCMDCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual, using a controlled vocabulary (please contact the CCMD Information Specialists for further details). Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950 to 2016), Embase (1974 to 2016) and PsycINFO (1967 to 2016); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review‐specific searches of additional databases. Reports of trials are also sourced from international trial registers via the World Health Organization's trials portal (the International Clinical Trials Registry Platform (ICTRP)), pharmaceutical companies, the handsearching of key journals, conference proceedings, and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCMD's generic search strategies (used to identify RCTs) can be found on the Group's website. The Group’s Specialised Register had fallen out of date with the Editorial Group’s move from Bristol to York in the summer of 2016.
[Please note, as of October 2015, the Group has changed its name to: Cochrane Common Mental Disorders, and their specialised register is now known as the CCMDCTR, to reflect this change.]
Appendix 2. Other database search strategies (Oct 2010)
Cochrane Central Register of Contolled Trials (CENTRAL) #1 MeSH descriptor MARITAL THERAPY, this term only #2 MeSH descriptor MARRIAGE explode all trees #3 MeSH descriptor SPOUSES explode all trees #4 MeSH descriptor PSYCHOTHERAPY explode all trees #5 (( #2 OR #3 ) AND #4) #6 ((therap* or psychotherap*) NEAR/7 (marital or marriage or couple* or spouse* or partner*)) #7 (#1 OR #5 OR #6) #8 MeSH descriptor DEPRESSION, this term only #9 MeSH descriptor DEPRESSIVE DISORDER, MAJOR, this term only #10 MeSH descriptor DYSTHYMIC DISORDER, this term only #11 (depression or depressive or dysthymi*) #12 (#8 OR #9 OR #10 OR #11) #13 (#7 AND #12) #14 SR‐DEPRESSN #15 HS‐DEPRESSN #16 (#14 OR #15) #17 (#13 AND NOT #16) #18 (#17), from 2005 to 2010
OVID MEDLINE 1. MARITAL THERAPY/ 2. MARRIAGE/ 3. SPOUSES/ 4. exp PSYCHOTHERAPY/ 5. (2 or 3) and 4 6. ((therap$ or psychotherap$) adj7 (marital or marriage or couple$ or spouse$ or partner$)).tw. 7. 1 or 5 or 6 8. DEPRESSION/ 9. DEPRESSIVE DISORDER, MAJOR/ 10. DYSTHYMIC DISORDER/ 11. (depression or depressive or dysthymi$).tw. 12. or/8−11 13. 7 and 12 14. randomized controlled trial.pt. 15. controlled clinical trial.pt. 16. randomly.ab. 17. randomi#ed.ab. 18. (control* adj3 (trial* or study or studies)).tw. 19. placebo$.ab. 20. trial.ab. 21. groups.ab. 22. or/14‐21 23. 13 and 22 24. ("2005" or "2006" or "2007" or "2008" or "2009" or "2010").yr. 25. (2006$ or 2007$ or 2008$ or 2009$ or 2010$).ed. 26. or/23‐24 27. 23 and 26
OVID EMBASE 1. MARITAL THERAPY/ 2. MARRIAGE/ 3. SPOUSE/ 4. exp PSYCHOTHERAPY/ 5. (2 or 3) and 4 6. ((therap$ or psychotherap$) adj7 (marital or marriage or couple$ or spouse$ or partner$)).tw. 7. (1 or 5 or 6) 8. exp DEPRESSION 9. (depression or depressive or dysthymi$).tw. 10. 8 or 9 11. 7 and 10 12. randomized controlled trial/ 13. major clinical study/ 14. controlled study/ 15. randomi#ed.ti,ab. 16. randomly.ab. 17. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 18. (control$ adj3 (trial$ or study or studies$)).tw. 19. trial.ti,ab. 20. placebo$.tw. 21. or/12‐20 22. 11 and 21 23. ("2005" or "2006" or "2007" or "2008" or "2009" or "2010").yr. 24. (2006$ or 2007$ or 2008$ or 2009$ or 2010$).em. 25. or/23‐24 26. 22 and 25
OVID PsycINFO 1.MARRIAGE COUNSELING/ 2.COUPLES THERAPY/ 3.MARITAL RELATIONS/ 4.MARRIAGE/ 5.COUPLES/ 6.SPOUSES/ 7. exp PSYCHOTHERAPY/ 8.(3 or 4 or 5 or 6) and 7 9.((therap$ or psychotherap$ or counsel$) adj7 (marital or marriage or couple$ or spouse$ or partner$)).tw. 10.1 or 2 or 8 or 9 11.exp MAJOR DEPRESSION/ 12.ATYPICAL DEPRESSION/ 13.(depression or depressive or dysthymi$).tw. 14.or/11−13 15.10 and 14 16.clinical trials.de. 17.placebo.de. 18.treatment effectiveness evaluation.de. 19.mental health program evaluation.de. 20.followup studies.de. 21."2000".md. [method=treatment outcome clinical trial] 22.random$.tw. 23.placebo$.tw. 24.trial.tw. 25.(control$ adj3 (study or studies)).tw. 26.control$ group$.tw. 27.comparative stud$.tw. 28.((singl$ or doubl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 29.or/16‐28 30.15 and 29 31.("2005" or "2006" or "2007" or "2008" or "2009" or "2010").yr. 32.(2006$ or 2007$ or 2008$ or 2009$ or 2010$).up. 33.(2006$ or 2007$ or 2008$ or 2009$ or 2010$).an. 34.or/31‐33 35.30 and 34
Appendix 3. Database search strategies (Feb 2018)
Database: CENTRAL
Host: Wiley
Data Parameters: Issue 1 of 12, January 2018
Date searched: Monday, February 19th 2018
Searched by: Chris Cooper
Hits: 0
Search strategy:
ID Search Hits
#1 MeSH descriptor: [Marital Therapy] this term only 128
#2 MeSH descriptor: [Marriage] this term only 268
#3 MeSH descriptor: [Spouses] this term only 304
#4 MeSH descriptor: [Psychotherapy] explode all trees 21833
#5 (#2 or #3) and 4 191
#6 ((therap* or psychotherap*) near/7 (marital or marriage or couple* or spouse* or partner*)) 1406
#7 #1 or #5 or #6 1521
#8 MeSH descriptor: [Depressive Disorder, Major] explode all trees 3359
#9 MeSH descriptor: [Depression] this term only 7658
#10 MeSH descriptor: [Dysthymic Disorder] this term only 158
#11 (depression or depressive or dysthymi*) 55359
#12 #8 or #9 or #10 or #11 55359
#13 #7 and #12 Online Publication Date from Jan 2016 to Feb 2018 25
Notes: CENTRAL only = 0 records in date range 2016‐current
File: N/A
Databases: Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)
Host: OVID
Data Parameters: 1946 to Present
Date Searched: Monday, February 19th 2018
Searched by: Chris
Hits: 24
Search strategy:
Database(s): 1946 to Present Search Strategy:
| # | Searches | Results |
| 1 | MARITAL THERAPY/ | 1488 |
| 2 | MARRIAGE/ | 22211 |
| 3 | SPOUSE/ | 8674 |
| 4 | exp PSYCHOTHERAPY/ | 177924 |
| 5 | (2 or 3) and 4 | 1916 |
| 6 | ((therap$ or psychotherap$) adj7 (marital or marriage or couple$ or spouse$ or partner$)).ti,ab,kf. | 5220 |
| 7 | 1 or 5 or 6 | 7078 |
| 8 | DEPRESSIVE DISORDER, MAJOR/ | 25332 |
| 9 | DEPRESSION/ | 99309 |
| 10 | DYSTHYMIC DISORDER/ | 1093 |
| 11 | (depression or depressive or dysthymi$).ti,ab,kf. | 325105 |
| 12 | 8 or 9 or 10 or 11 | 351599 |
| 13 | 7 and 12 | 531 |
| 14 | randomized controlled trial.pt. | 453811 |
| 15 | controlled clinical trial.pt. | 92162 |
| 16 | randomly.ab. | 285193 |
| 17 | (randomized or randomised).ab. | 482173 |
| 18 | (control* adj3 (trial* or study or studies)).ti,ab,kf. | 439107 |
| 19 | placebo$.ab. | 187134 |
| 20 | trial.ab. | 418580 |
| 21 | groups.ab. | 1764677 |
| 22 | 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 | 2702546 |
| 23 | 13 and 22 | 170 |
| 24 | (2016* or 2017* or 2018*).yr,dt,ed,ep. | 3354952 |
| 25 | 23 and 24 | 24 |
Notes: N/A
File: HO2MEDLINE24.txt
Database: Embase
Host: OVID
Data Parameters: 1974 to 2018 February 16
Date searched: Monday, February 19th 2018
Searched by: Chris Cooper
Hits: 65
Search strategy:
Search Strategy:
| # | Searches | Results |
| 1 | MARITAL THERAPY/ | 2939 |
| 2 | MARRIAGE/ | 51076 |
| 3 | SPOUSE/ | 13599 |
| 4 | exp PSYCHOTHERAPY/ | 234469 |
| 5 | (2 or 3) and 4 | 2983 |
| 6 | ((therap$ or psychotherap$) adj7 (marital or marriage or couple$ or spouse$ or partner$)).tw. | 7814 |
| 7 | 1 or 5 or 6 | 11174 |
| 8 | exp DEPRESSION/ | 404425 |
| 9 | (depression or depressive or dysthymi$).tw. | 434869 |
| 10 | 8 or 9 | 585771 |
| 11 | 7 and 10 | 1304 |
| 12 | randomized controlled trial/ | 487494 |
| 13 | major clinical study/ | 3002641 |
| 14 | controlled study/ | 5777541 |
| 15 | (randomized or randomised).ti,ab. | 728848 |
| 16 | randomly.ab. | 369989 |
| 17 | ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. | 270122 |
| 18 | (control$ adj3 (trial$ or study or studies$)).tw. | 579278 |
| 19 | trial.ti,ab. | 694693 |
| 20 | placebo$.tw. | 268426 |
| 21 | 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 | 8303795 |
| 22 | 11 and 21 | 480 |
| 23 | (2016* or 2017* or 2018*).yr,dc. | 3804066 |
| 24 | 22 and 23 | 65 |
Notes: N/A
File: HO2Embase65.txt
Database: PscyINFO
Host: OVID
Data Parameters: 1806 to February Week 1 2018
Date searched: Monday, February 19th 2018
Searched by: Chris Cooper
Hits: 16
Search Strategy:
| # | Searches | Results |
| 1 | exp Marriage Counseling/ | 5128 |
| 2 | exp MARRIAGE/ | 10952 |
| 3 | exp SPOUSES/ | 15189 |
| 4 | exp PSYCHOTHERAPY/ | 205279 |
| 5 | (2 or 3) and 4 | 1288 |
| 6 | ((therap$ or psychotherap$) adj7 (marital or marriage or couple$ or spouse$ or partner$)).ti,ab. | 11799 |
| 7 | 1 or 5 or 6 | 14271 |
| 8 | exp Major Depression/ | 116740 |
| 9 | exp "DEPRESSION (EMOTION)"/ | 24174 |
| 10 | DYSTHYMIC DISORDER/ | 1456 |
| 11 | (depression or depressive or dysthymi$).ti,ab. | 251440 |
| 12 | 8 or 9 or 10 or 11 | 261819 |
| 13 | 7 and 12 | 898 |
| 14 | randomly.ab. | 64977 |
| 15 | (randomized or randomised).ti,ab. | 69748 |
| 16 | (control* adj3 (trial* or study or studies)).ti,ab. | 71249 |
| 17 | placebo$.ab. | 36757 |
| 18 | trial.ab. | 83237 |
| 19 | groups.ab. | 446298 |
| 20 | 14 or 15 or 16 or 17 or 18 or 19 | 615592 |
| 21 | 13 and 20 | 181 |
| 22 | (2016* or 2017* or 2018*).yr,dc,mo. | 380262 |
| 23 | 21 and 22 | 16 |
Notes: N/A
File: HS02 PsycINFO16.txt
Data and analyses
Comparison 1. Couple therapy versus individual psychotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depressive symptoms at the end of treatment | 9 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.44, 0.10] |
| 2 Depressive symptoms at the 6‐month follow‐up | 2 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.77, 0.27] |
| 3 Depressive symptoms at the 15/24 month follow‐up | 3 | 117 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.78, 0.10] |
| 4 Persistence of depression at the end of treatment | 6 | 237 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.72, 1.22] |
| 5 Persistence of depression at 6‐month follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Dropouts | 9 | 364 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.51, 1.41] |
| 7 Relationship distress at the end of treatment | 6 | 187 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.97, ‐0.02] |
| 8 Relationship distress at the 15/24‐month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Persistence of relationship distress at the end of treatment | 2 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.51, 0.98] |
Comparison 2. Couple therapy versus drug therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depressive symptoms at the end of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Depressive symptoms at the 6‐month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Dropouts | 2 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.15, 0.61] |
| 4 Relationship distress at the end of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Relationship distress at the 6‐month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. Couple therapy versus no/minimal treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depressive symptoms at the end of treatment | 3 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.59, ‐0.32] |
| 2 Persistence of depression at the end of treatment | 2 | 65 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.32, 0.70] |
| 3 Relationship distress at the end of treatment | 2 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.64, 0.04] |
Comparison 4. Couple therapy plus drug therapy versus drug therapy alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depressive symptoms at the end of treatment | 2 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.04 [‐3.97, 1.89] |
| 2 Dropouts | 2 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.07, 15.52] |
| 3 Relationship distress at the end of treatment | 2 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.35, 0.14] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beach 1992.
| Methods | Parallel group randomised controlled trial | |
| Participants |
Participants: depressed women in discordant couples with DSM‐III major depression and/or dysthymia Sex: women (n = 45) Age: mean age: 39.14 (range 28 to 59) years Unit of allocation: individual participant Number randomised: 54 Number completing: 45 Setting: Marital Clinic at Stony Brook University, New York (USA) Inclusion criteria:
Exclusion criteria:
Ethnicity: not specified Baseline characteristics: Women mean age = 39.14 (range = 28 to 59) years mean educational level = 14.20 years mean DAS = 69.93 years Men mean age = 42.29 (range = 30 to 69) years mean educational level = 14.16 years mean DAS = 85.22 years Couples mean household income = 37,700 USD per year mean number of children = 2.42 (range 0 to 7) mean length of marriage = 14 years |
|
| Interventions |
Three conditions: Behavioural marital therapy (BMT); cognitive‐behavioural therapy (CBT); wait list. BMT: Aimed at increasing positive affectional and decreasing adversative behaviours, improving problem solving and communicative skills, setting reasonable expectations of spouses, understanding reasons for the development of discord, based on the approach described by Beach 1990. CBT: Individual therapy aimed at modifying dysfunctional cognitions and problematic behaviour, based on Beck 1979. Duration of intervention: 15 to 20 weekly sessions for BMT and CBT, 15 weeks for wait list. Length of follow‐up: Assessment at post‐treatment and 1 year. |
|
| Outcomes |
Depression: Self‐assessment by BDI Dropouts Relationship distress: Self‐assessment by DAS (For wives: BDI and DAS. For husbands: DAS.) |
|
| Notes | Both treatments provided by 4 well‐trained therapists (2 doctoral level psychologists, 2 advanced graduate students). Treatment integrity assessed. No statistical power was reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information about the sequence generation process |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Number and timing of dropouts are reported |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 54 participants randomised, 6 dropped out of treatment before five sessions, 3 excluded for protocol violations. Data for these participants were not included in the paper. No missing data were reported. No intention‐to‐treat analysis was performed. |
| Selective reporting (reporting bias) | Low risk | Data reported for all mentioned endpoints |
| Other bias | High risk | The principal investigator was a leading figure in behavioural couple therapy, raising the possibility of allegiance bias. |
Bodenmann 2008a.
| Methods | Three‐arm parallel group randomised controlled trial | |
| Participants |
Participants: outpatients meeting Research Diagnostic Criteria for major depressive disorder or dysthymia Sex: both men (n = 25) and women (n = 35) Age: adults. Mean (SD) age reported separately for the three intervention groups: CBT 44.35 (11.31) years, IPT 47.33 (10.60) years, COCT 44.35 (10.20) years Unit of allocation: individual participant Number randomised: 60 Number completing: 57 Setting: outpatient private practices in five major Swiss cities (Basel, Bern, Fribourg, Luzern, Zurich) Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported. German‐speaking Baseline characteristics Low/medium education n = 33, High education n = 27; Low income n = 21, medium income n = 29, high income n = 10; Mean length of relationship (SD): CBT 18.23 (11.66) years, IPT 17.6 (10.78) years, COCT 14.39 (10.30) years: On antidepressant medications n = 34. |
|
| Interventions |
Three conditions: Individual cognitive behavioural therapy (CBT), Individual interpersonal therapy (IPT), Coping‐oriented couples therapy (COCT) . CBT according to the guidelines by Beck 1979: IPT: based on approach by Klerman 1984, in one to three sessions (the partner could be invited). COCT according to a manual by Bodenmann 2004. Duration of intervention: 20 weekly sessions for CBT and IPT, 10 biweekly sessions for COCT Length of follow‐up: Assessments at 2 weeks, 6 months, 1 year, 1.5 years. |
|
| Outcomes |
Depression: Self‐assessment by BDI Clinician assessment of depressive symptoms by HRSD. Rates of recovery from depression and relapse calculated on operationalised criteria. Dropouts Relationship distress: Self‐assessment of relational quality by Partnership Questionnaire (Hahlweg 1996), self‐assessment of mutual support by Dyadic Coping Inventory (Bodenmann 2008b), expert assessment of open criticism from the partner to the participants by Five Minutes Speech Sample (Magaña 1986). However, the last measure cannot be considered as a valid measure of relationship distress. |
|
| Notes | No calculation of statistical power. Treatments provided by 19 experienced therapists (9 for CBT, 6 for IPT, 4 for COCT). Treatment fidelity assessed and was found to be medium/high for all three treatment conditions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators defined the study as a quote: “randomised clinical trial” but did not report details about method of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Investigators defined the study as a quote: “randomised clinical trial” but did not report details about allocation concealment. Clarification about allocation concealment was requested from the principal investigator, who specified that quote: “allocation was concealed”, without giving further details. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | Low risk | Outcome was assessed by both a self‐report and an expert‐rated measure. The authors did not report details about assessors blinding for the expert‐rated measure (HRSD). Clarirification about this issue was requested from the principal investigator, who specified that Quote: "the assessors were blinded with regard to treatment conditions and time of measurement (pre, post, follow‐ups). Furthermore, they did not have any information about the participant and his or her partner". Review authors judged that blinding of assessment was ensured. |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Number and timing of dropouts are shown in a flow‐chart. Reasons for dropouts are provided in the text |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Investigators reported that 60 participants were randomised, 57 completed the study, 56 were assessed at post‐test, 54 at 6‐month follow‐up, 50 at 1‐year follow‐up, 52 at 1.5‐year follow‐up. No intention‐to treat analysis was performed. |
| Selective reporting (reporting bias) | High risk | Concerning the relationship measures, the investigators reported summary statements without providing full data |
| Other bias | High risk | The principal investigator was the developer of the couple therapy model used in the experimental condition, raising the possibility of allegiance bias. |
Cohen 2010.
| Methods | Parallel group randomised controlled trial. | |
| Participants |
Participants: depressed women Sex: women (n = 35) Age: Adults. Mean (SD) age reported separately for the intervention and the control group. Intervention: 42.72 (11.60) years. Wait list: 43.69 (9.81) years Unit of allocation: individual participant Number randomised: 35 Number completing: 30 Setting: Marital Clinic at Stony Brook University, New York (USA) Inclusion criteria:
Exclusion criteria:
Ethnicity:
Baseline characteristics: Treatment (n = 18) Age: women, mean 42.72 (11.60) years; men, mean 44.75 (9.17) years Married: 94.1% Years married: 17.00 (13.08) Education Level
Employment
Yearly family income: 71,667 USD (27,356) Diagnosis
Age at onset: 35.50 (17.30) Lifetime no. of episodes 1: 35.7% 2: 14.3% 3 to 4: 28.5% > 5: 21.4% Weeks in current episode: 16.20 (12.28) Wait list (n = 17) Age: women, 43.69 (9.81); men, 45.39 (12.23) Married: 94.4% Years married: 13.43 (10.55) Education Level
Employment
Yearly family income: mean 100,091 USD (39,267) Diagnosis
Age at onset: 27.57 (14.39) years Lifetime no. of episodes 1: 13.3% 2: 26.7% 3 to 4: 20% > 5: 40% Weeks in current episode: 25.10 (60.10) |
|
| Interventions |
Two conditions: Brief problem‐focused Couple Therapy (BCT) for depression; Wait list. Manualised BCT aimed at promoting an increased understanding of depression as an illness, to reduce negative attitudes and behaviours toward depression, and increase empathy and mutual support: 5 2‐hr weekly sessions. Four major areas: psychoeducation, communication, empathy‐building, and support‐building. Wait list: at study entry, participants were informed of the possibility of waiting 4 months for treatment. Duration of intervention: 5 weeks Length of follow‐up: Assessments at post‐treatment and 3 months. |
|
| Outcomes |
Depression: Self‐assessment by BDI‐II Clinician‐rated assessment by HRSD Recovery: Defined by a score > 11 on BDI‐II Global symptomatology: Self‐assessment by Symptom Checklist‐90 (SCL‐90) (Derogatis 1983). Relationship distress: Self‐assessment by DAS. |
|
| Notes | Treatments provided by four advanced clinical psychology doctoral students. Treatment integrity assessed for the four major areas of the targeted intervention. Therapists received high adherence ratings across all scales. No statistical power was reported and no primary outcomes were specified. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators defined the study as a quote: “randomised clinical trial” but did not report details about method of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Investigators did not report details about method of sequence generation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Outcome not assessed |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 14% of the total data were missing at post‐test analysis for continuous measures and 23% for dichotomous measures. The loss was unbalanced across groups for dichotomous data. Although analyses were conducted using hierarchical linear modelling, which is appropriate for handling missing data, no usable data were presented according to this analysis. |
| Selective reporting (reporting bias) | Low risk | The study protocol was available and all of the study’s prespecified outcomes that are of interest for the review were reported |
| Other bias | High risk | The principal investigator was also the therapist in half of the cases in the experimental condition, raising the possibility of conflict of interest. |
Compton 2008.
| Methods | Parallel group randomised controlled trial. | |
| Participants |
Participants Distressed couples older than 60 years with a spouse meeting diagnostic criteria for major depressive disorder Sex No information on distribution by sex of the depressed spouses Age Treatment: mean (SD) 67.2 (7.5) years Control: mean (SD) 71.2 (6.0) years Unit of allocation: Individual participant Number randomised: 21 Number completing: 20 Setting: Outpatient clinic, Duke University Child and Family Study Center, Durham, USA. Inclusion criteria:
Exclusion criteria:
Ethnicity: Not specified Baseline characteristics: No information other than age and sex reported |
|
| Interventions |
Two conditions: Antidepressant medication plus weekly behavioural marital therapy (BMT) Weekly antidepressant medication management. No details provided about BMT. Duration of intervention: 6 months. Length of follow‐up. Assessment at post‐treatment and 6 months |
|
| Outcomes |
Depression: Clinician‐assessed depressive symptomatology by HRSD Dropouts Relationship distress: Self‐assessment by DAS |
|
| Notes | No indications of therapists' characteristics. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators defined the study as quote: “randomised clinical trial” but did not report details about method of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Investigators defined the study as quote: “randomised clinical trial” but did not report details about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | Low risk | Expert‐rated outcome measure assessed by blind assessors |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | The number of dropouts is reported in a table. |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | All outcomes for primary endpoints were reported according to the protocol |
| Other bias | High risk | No description of sample baseline characteristics was provided. |
Denton 2012.
| Methods | Parallel group randomised controlled trial. | |
| Participants |
Participants: outpatients meeting criteria for a DSM‐IV major depressive episode assessed by the SCID Sex: women (n = 24) Age: Mean (SD) age reported separately for the couple therapy plus medication and the medication group. Couple therapy plus medication: 34 (11.5) years, medication: 31.7 (8.7) years Unit of allocation: individual participant Number randomised: 24 Number completing: 16 Setting: Three private practices in Dallas area and the University of Dallas Family Studies Center, USA Inclusion criteria:
Exclusion criteria:
Ethnicity: intervention group: 83% white, Control group: 67% white Baseline characteristics Couple therapy plus medication: Education mean 14.8 years Income 58% < USD 50,000/year Medication: Education mean 14.6 years Income 42% < USD 50,000/year |
|
| Interventions |
Two conditions: Emotion‐Focused Couple Therapy (EFT) plus Medication Management; Medication Management alone. Manualised EFT, described as a synthesis of family systems and experiential approaches, carried out in nine steps across three stages of treatment. 50‐min sessions. 10 weekly sessions plus five biweekly Medication Management consisting of one of the following antidepressant medications: Sertraline, Escitalopram, Buproprion XL, Venlafaxine XR, delivered by a certified psychiatrist according to the MDD treatment algorithm of the Texas Medication Agorithm Project (Suehs 2008). Duration of intervention: 6 months. Length of follow‐up: Assessments at post‐treatment, 3 months and 6 months. |
|
| Outcomes |
Depression Clinician‐assessed depressive symptomatology by IDS‐C30 Dropouts Relationship quality Quality of relationship self‐assessed by QMI (Norton 1983). |
|
| Notes | EFT delivered by 4 therapists licensed as marriage and family therapists experienced in EFT, with a score of at least 40 on the Emotion Focused Therapy‐Therapist Fidelity Scale (Denton 2009). Weekly supervision by an expert EFT supervisor. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation schedule prior to start the study enrolment. Stratification based on whether the male partner met criteria for major depression episode. |
| Allocation concealment (selection bias) | Low risk | Allocation by slips of paper sealed in numbered opaque envelopes opened by a research assistant in sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | Low risk | Expert‐rated measure administered by trained blind assessors. Quality of rating evaluated through control of audiorecorded interviews. |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Detailed information on number and timing of dropouts and reasons for dropouts is provided. |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 12 participants randomised in each group, 2 interrupted treatment in the control group, and 6 interrupted EFT treatment in the experimental group. Lost at follow‐up were 3 at 6‐month, and 7 at 9‐ and 12‐month follow‐up in the control group, and 4, 3 and 4 at 6‐, 9‐ and 12‐month follow‐up in the experimental group. Procedures were used to include respondents with missing data, but no intention‐to‐treat analysis was mentioned |
| Selective reporting (reporting bias) | Low risk | All outcomes for primary endpoints were reported according to the protocol. |
| Other bias | High risk | The clinicians responsible for manualising the experimental condition were members of the research team, raising the possibility of allegiance bias. |
Dessaulles 2003.
| Methods | Parallel group randomised controlled trial. | |
| Participants |
Participants: outpatients meeting criteria for a major depressive episode on the Diagnostic Interview Schedule Sex: women (n = 18) Age: adults. Mean age 36 years Unit of allocation: individual participant. Number randomised: 18 Number completing: 12 Setting: Clinic attached to the Center for Psychological Services at the University of Ottawa (Canada). Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported Baseline characteristics: on average cohabiting for 11 years, with two children. Mean income of CAN 45,000. Mean age of male partners 38 years |
|
| Interventions |
Two conditions: Emotion‐focused couples therapy (EFT) and drug therapy. EFT: 14 weekly conjoint sessions Drug therapy: either desimipramine or trimipramine (125 to 225 mg/day) or trazodone (250 to 450 mg/day). Duration of intervention: 16 weeks, 14 weekly conjoint sessions plus one individual session for each partner. Length of follow‐up: assessments at post‐treatment, 3 and 6 months. |
|
| Outcomes |
Depression: self‐assessment by IDD. Dropouts Relationship distress: self‐assessment by DAS |
|
| Notes | No calculation of statistical power. Treatments provided by 6 doctoral interns in clinical psychology. Treatment fidelity assessed and found adequate. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators reported that “subjects were randomly assigned to receive either EFT or pharmacotherapy”, but did not report further details. We requested clarification about method of sequence generation from the principal investigator. We received no answer. |
| Allocation concealment (selection bias) | Unclear risk | Investigators reported that Quote: “subjects were randomly assigned to receive either EFT or pharmacotherapy”, but did not report further details. Clarification about allocation concealment was requested from the principal investigator. We received no answer. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information on number of dropouts provided |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Investigators reported that 18 participants were randomised, 12 completed the study, 12 were assessed at post‐test, 12 at 3‐month follow‐up, 10 at 6‐month follow‐up. No intention‐to treat analysis was performed. |
| Selective reporting (reporting bias) | Low risk | All outcomes for primary endpoints were reported according to the protocol. |
| Other bias | High risk | The clinicians responsible for manualising the experimental condition were members of the research team, raising the possibility of allegiance bias. Drug therapy in the control group was discontinued after 16 weeks, which is not adequate according to the current guidelines. |
Emanuels 1996.
| Methods | Parallel group randomised controlled trial. | |
| Participants |
Participants: outpatients recruited by advertisements in newspapers, referred by general practitioners and mental health services. 135 were identified, of whom 116 received a diagnosis of depression. Sex: both men (n = 17) and women (n = 19) Age: mean age 38.4 years in completers and 38.8 years in dropouts Unit of allocation: individual participant Number randomised: 36 Number completing: 27 Setting: outpatient clinics of Department of Psychology, University of Groningen and of Dennenoord (The Netherlands) Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported Baseline characteristics: depressive complaints present 1 month to 40 years, 36 also experienced marital distress, mean length of relationship 13.8 years, mean BDI 21.6, mean MMQ participant 31.4, mean MMQ spouse 26.5 |
|
| Interventions |
Two conditions: BMT based on approach by Beach 1992 and communication training by Emmelkamp 1984, Individual behavioural‐cognitive therapy based on Beck 1979 approach. Both interventions manual‐guided Duration of intervention: Both interventions 16 1‐hour weekly sessions Length of follow‐up: Assessment at post‐treatment |
|
| Outcomes |
Depression Self‐assessment by BDI Dropouts Couple satisfaction Self‐assessment by Maudsley Marital Questionnaire (MMQ) |
|
| Notes | No power calculation made. Both treatments delivered by well‐trained expert therapists. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Patients were randomly assigned to behavioural marital therapy or individual behavioural‐cognitive therapy” and investigators did not report further details. |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Patients were randomly assigned to behavioural marital therapy or individual behavioural‐cognitive therapy” and investigators did not report further details. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information on number of dropouts provided |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analyses conducted on the completers only. No intention‐to treat analysis was performed. |
| Selective reporting (reporting bias) | High risk | BDI data were not presented as a categorical variable. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Emanuels 1997.
| Methods | Parallel group randomised controlled trial. | |
| Participants |
Participants: outpatients with a diagnosis of depression, without relationship distress, recruited by advertisements in newspapers (83%), referred by practitioners, and mental health services Sex: both men (n = 12) women (n = 19) Age: mean age 42.2 years in the completers, 41.3 years in the dropouts Unit of allocation: individual participant Number randomised: 32 (1 excluded for protocol violation). Number completing: 23 Setting: Outpatient clinics of Department of Psychology, University of Groningen and of Dennenoord (The Netherlands). Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported Baseline characteristics: depressive complaints present 1 month to 40 years, mean length of relationship 15.8, mean BDI 23.5, mean MMQ‐M (a subscale on quality of the relationship with the spouse) participant 11.3, mean MMQ‐M spouse 10.6 |
|
| Interventions |
Two conditions Spouse‐aided therapy with the same content of individual behavioural‐cognitive therapy but a conjoint format, Individual behavioural‐cognitive therapy based on Beck 1979 approach Both interventions were manual‐guided Duration of intervention: Both interventions 16 1‐hour weekly sessions Length of follow‐up: Assessment at post‐treatment |
|
| Outcomes |
Depression Self‐assessment by BDI Dropouts Couple satisfaction Self‐assessment by MMQ |
|
| Notes | No power calculation made. Both treatments delivered by well‐trained expert therapists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Patients were randomly assigned to behavioural marital therapy or individual behavioural‐cognitive therapy” and investigators did not report further details. |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Patients were randomly assigned to behavioural marital therapy or individual behavioural‐cognitive therapy” and investigators did not report further details. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions. |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information on number of dropouts and reasons for dropouts is provided |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analyses conducted on the completers only. No intention‐to treat analysis was performed |
| Selective reporting (reporting bias) | Low risk | BDI data were not presented as a categorical variable |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Foley 1989.
| Methods | Parallel group randomised trial. | |
| Participants |
Participants: married outpatients meeting Research Diagnostic Criteria for a current episode of major depressive disorder assessed by SADS‐L diagnostic interview Sex: both men (n = 5) and women (n = 13) Age: adults. Mean age 40 years Unit of allocation: individual participant Number randomised: 18 Number completing: 15 Setting: not specified Inclusion criteria:
Exclusion criteria: serious suicide risk Ethnicity: white 94% Baseline characteristics: mean marriage length 15 years. 39% social class III, 33% social class IV. 61% catholic. 78% of partners had a lifetime history of mental disorder, 50% previous episodes of major depression, 12% current episode of major depression |
|
| Interventions |
Two conditions: Conjoint marital interpersonal psychotherapy (IPT‐CM), Individual interpersonal psychotherapy (IPT). Both therapies based on the approach described by Klerman 1984. Duration of intervention: 16 weekly sessions Length of follow‐up: Assessment at post‐treatment |
|
| Outcomes |
Depression: Clinician‐rated depressive symptoms by HRSD Dropouts Couple adjustment: Self‐assessment by DAS Participant satisfaction: Self‐report by an ad hoc questionnaire. |
|
| Notes | No calculation of statistical power. Treatments provided by 3 therapists for IPT (a psychiatrist, a psychologist and a social worker) and 3 therapists (social workers) for IPT‐CM. All therapists with extensive prior experience. Quality of therapy monitored. All therapists judged to be competent by expert raters. Drug therapy not allowed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators reported their study as a quote: “randomised clinical trial”, but did not report further details |
| Allocation concealment (selection bias) | Unclear risk | See above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | Low risk | Outcome assessed by an expert‐rated measure. The authors reported that quote: "depression and social functioning were assessed by blind trained evaluators" |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information on number of dropouts and reasons for dropouts is provided |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Investigators reported that 18 participants were randomised and 15 completed the study. Intention‐to‐treat analysis was performed. |
| Selective reporting (reporting bias) | Low risk | Data reported for all mentioned endpoints |
| Other bias | Low risk | The study was free from other biases. |
Jacobson 1991.
| Methods | Parallel group randomised trial | |
| Participants |
Participants: depressed married women with compliant partners Sex: women (n = 72) Age: Adults. Mean age 38.5 years. No significant differences between intervention and control group Unit of allocation: individual participant Number randomised: 72 Number completing: 60 Setting: not specified Inclusion criteria:
Exclusion criteria:
Ethnicity: not specified Baseline characteristics: not specified |
|
| Interventions |
Three conditions: BMT based on approach by Jacobson 1986, Individual CBT, Combined treatment with BMT plus CBT Duration of intervention: 20 sessions, time interval between sessions not specified Length of follow‐up: assessment at post‐treatment |
|
| Outcomes |
Depression: Self‐assessment by BDI and clinician‐rated depressive symptoms by HRSD Dropouts Relationship distress: Self‐assessment by DAS |
|
| Notes | Separate analyis for distressed and non‐distressed couples. Treatments provided by 3 licensed psychologists, one psychiatric social worker with an ACSW degree, and two advanced clinical psychology graduate students. For BMT and CT, all went through a year of training and treating pilot cases before participation. For BMT, all therapists were trained and supervised until they scored consistently above 40 on the Cognitive Therapy Scale (Dobson 1985). Treatment integrity assessed through an ad hoc developed scale consisting of 51 items. 17 items represented behaviours supposed to occur in CT, 17 in BMT and 17 unspecific clinical skills. 3 graduate students blind to treatment condition served as raters. Treatment integrity wss considered as achieved in 85% of the sessions. A chi‐square test for differential dropout rate across groups was not significant. Additional analyses led the investigators to conclude that attrition did not distort the findings. No statistical power was reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information about the sequence generation process |
| Allocation concealment (selection bias) | Unclear risk | Method of concealment not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by both a self‐report and an expert‐rated measure. Blinding not feasible for self‐report measures. No information given about assessment by the expert‐rated measure. |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information on number of dropouts is provided |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 14% of the subject did not complete the treatment. The number of dropouts was unbalanced across groups. The analysis was conducted on completers only. The authors reported that outcomes were available also for dropouts, but did not report the data. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes that are of interest to this review were reported |
| Other bias | High risk | The principal investigator was a leading figure in behavioural couple therapy, raising the possibility of allegiance bias. |
Leff 2000.
| Methods | Parallel group randomised trial. | |
| Participants |
Participants: outpatients with primary diagnosis of depression according to Present State Examination (Wing 1974), recruited through professional contacts (General Practitioners, psychiatric outpatient services and emergency departments), and newspaper advertisements Sex: both men (n = 10) and women (n = 27) in the drug treatment group. Both men (n = 23) and women (n = 17) in the couple therapy group Age: mean age 38.6 years and 39.7 years in the drug treatment and couple therapy groups, respectively Unit of allocation: individual participant Number randomised: 77 Number completing: 50 Setting: Outpatient clinic, Maudsley Hospital, London, United Kingdom. Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported Baseline characteristics: mean length of relationship 10.8 years in the couple therapy group and 10.1 years in the drug treatment group; mean DAS 87.3 and 96.5, respectively; partner’s critical comments 8.3 and 8.8; mean age at first depression episode: 29.8 years and 28.6 years; mean HRSD 18.1 and 18.7; mean BDI 25.4 and 28.1 |
|
| Interventions |
Two conditions Systemic couple therapy, drug therapy Systemic couple therapy: Aimed at helping participant and partner to gain new perspectives on problems, attach different meanings to depressive behaviours, and experiment with new ways of relating, based on a manual (Jones 1999). Drug therapy: Best available clinical regimen defined as desipramine gradually increased over a few weeks. Compliance assessed through serum levels assessment. If no response at 6 weeks with therapeutic serum levels of 125 μg/ml or side effects, trazodone or fluvoxamine were tried, then continued for 4 months and then gradually reduced. Duration of intervention: 12 to 20 sessions of couple therapy, time interval between sessions not specified, drug therapy for one year Length of follow‐up: Assessment at 1 and 2 years |
|
| Outcomes |
Depression: Self‐assessment by BDI and clinician‐rated depressive symptoms assessed by HRSD Relationship distress: Self‐assessment by DAS |
|
| Notes | The trial initially included an arm of cognitive therapy which was discontinued because of the high number of dropouts. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | Low risk | Outcome assessed by both a self‐report and an expert‐rated measure. Blinding not feasible for self‐report measures. Expert‐rated measure assessed by blind assessors. |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Details about the number, the timing and the reasons for dropouts is provided |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The investigators wrote that intention‐to‐treat analysis was performed, including any data available from dropouts. However, they failed to retrieve data from all dropouts. The difference in dropout rates between the experimental group (15%) and the control group (57%) was highly significant. |
| Selective reporting (reporting bias) | High risk | Outcome variables were described with a graph for the BDI, and no figures were given. HRSD data were not shown and in the results authors wrote quote: “... there was no significant advantage for couple therapy over medication.” Data on relationship distress were not shown. The authors wrote quote: "changes in the CFI and the Dyadic Adjustment Scale will be presented in another paper". However, no further paper reporting these data has been found. |
| Other bias | High risk | A payment was used to induce dropouts to return for the 2‐year follow‐up assessment, High number of dropouts in the drug therapy group. The great number of dropouts in the drug treatment group could be due to the fact that participants were recruited to participate in a study on marital therapy, therefore selecting people not interested in drug treatment. |
Lemmens 2009.
| Methods | Three arm parallel randomised trial | |
| Participants |
Participants: consecutive referrals to Anxiety and Depression Unit of the University Hospital, admitted to hospital or day‐hospital, with a DSM‐IV diagnosis of major depressive disorder Sex: both men (n = 23) and women (n = 60) Age: mean 43.9 years in multiple family therapy (MFT), 43.2 years in treatment as usual (TAU), 40.2 years in couple therapy (CT) Unit of allocation: individual participant Number randomised: 83 Number completing: 74 Setting: Day Hospital and Outpatient Clinic of the Anxiety and Depression Unit of the University Hospital of Leuven (Belgium). Participants treated mostly in outpatient setting. Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported Baseline characteristics: mean duration of relationship 18.7 years in MFT, 18.1 years in TAU, 14.8 years in CT, mean DAS was 98.5 in MFT, 98.1 in TAU, 104.9 in CT, mean HRSD was 17.9, 17.9 and 18.0, respectively, mean BDI was 26.6, 27.3 and 26.2, respectively, and mean duration of the index admission 11.3 weeks, 12,6 and 12.4 respectively ; 74.3% in MFT, 65.2% in TAU and 80% in CT had recurrent depression. |
|
| Interventions |
Three conditions: Treatment as usual (TAU) plus 60‐minute 7 Couple Therapy sessions, TAU plus 60‐minute 7 Multiple Family therapy sessions, TAU only. Couple therapy sessions followed a protocol based on systemic couple therapy for depression manual (Jones 1999), incorporating social constructionist and narrative concepts, and the family systems‐illness model. Multiple Family Therapy conceptually similar to couple therapy; the group consisted of 4 to 7 families and was used as a resource for problem solving, following a model by Lemmens 2007. Treatment as usual a mix of various psychological interventions, mainly based on a cognitive‐behavioural model, non‐verbal therapies, and antidepressant drug therapy. Duration of intervention: Couple Therapy and Multiple Family Therapy 6 sessions in 3 months plus 1 session after 3 months more, TAU 3 months Length of follow‐up: assessments at 3 and 15 months. |
|
| Outcomes |
Depression Self‐assessment by BDI. Response to treatment for depression was defined as a > 50% improvement in the BDI, and remission as BDI < 9. Hospitalisation Rehospitalisation rates Psychiatric Consultation Psychiatric consultation rates Antidepressant medication Rates of participants not using antidepressant medications |
|
| Notes | A majority of cases (number not reported) was initially admitted to hospital, although treatments were mostly delivered in outpatient clinics. The three samples have different sizes (35 in MFT, 23 in TAU, 25 in SFT). Study power and sample sizes not calculated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The patients were randomised in blocks of 4‐7, using a random number table and sealed envelopes” |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | The description of patients' progress through the trial provides information on number and timing of dropouts |
| Blinding of outcome assessment (detection bias) Relationship distress | Low risk | Outcome not assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis, likelihood approach |
| Selective reporting (reporting bias) | Low risk | Full data were reported thoroughly |
| Other bias | High risk | Probable contamination between TAU and the two experimental conditions. No information was given about the therapists' experience and the possibility of allegiance bias. The three samples had different sizes (35 in MFT, 23 in TAU, 25 in SFT). The authors gave no explanation for this finding. |
Seikkula 2012.
| Methods | Parallel group randomised trial | |
| Participants |
Participants: married outpatients meeting DSM‐IV diagnostic criteria for unipolar depression, assessed by an unspecified structured diagnostic interview Sex: both men and women. Distribution by gender reported only for completers: men n = 27, women n = 24 Age: adults. Distribution by age reported only for completers. Mean age 41.2 years in experimental group and 43.5 years in control group Unit of allocation: individual participant Number randomised: 66 Number completing: 51 Setting: three mental health outpatient clinics attached to three departments of psychiatry in Finland Inclusion criteria:
Exclusion criteria: none Ethnicity: not reported Baseline characteristics: data reported on completers only. Mean duration of unemployment 3.6 (SD 7.5) months (experimental group); 0.9 (SD 0.2) months (control group). Mean number of children under school age 0.2 (SD 0.5) (experimental group); 0.09 (SD 0.43) (control group) Mean duration of current illness 38 (SD 56.3) months (experimental group); 45 (SD 63.7) months (control group). |
|
| Interventions |
Two conditions: Systemic Couple Therapy, TAU. Systemic Couple Therapy delivered by two co‐therapists, focused on dialogue and narrative psychotherapy (n = 35). TAU mainly based on individual psychodynamic psychotherapy (n = 31). Drug therapy was allowed in both treatment groups For couple therapy group, 5 minimum sessions, no fixed number of sessions. Need‐adapted treatment Duration of intervention: Systemic Couple Therapy, mean 11 sessions, minimum 5 sessions. Time interval between sessions not specified, TAU duration not specified. Length of follow‐up: Assessments at 6, 12, 18 and 24 months. |
|
| Outcomes |
Depression: Self‐assessment by BDI, clinician‐rated depressive symptoms by HRSD. Recovery status was assessed by using an unspecified score. General psychopathology: Clinician‐rated psychiatric symptomatology by SCL‐90 (Derogatis 1983) Global functioning: Clinician‐rated global functioning by Global Assessment of Functioning Dropouts Alcohol use: Clinician‐rated alcohol use by Alcohol Use Disorder Identification Test (AUDIT) Relationship distress: Self‐assessment by DAS |
|
| Notes | Systemic couple therapy provided by 30 qualified family therapists (mean age 51 years) with extensive prior experience. Individual psychotherapy to the control group was provided by expert therapists. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators reported their study as, quote: “randomised clinical trial”, but did not report further details |
| Allocation concealment (selection bias) | Unclear risk | No details about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by both a self‐report and an expert‐rated measure. Blinding not feasible for self‐report measures. Expert‐rated measure administered by unblinded researchers. |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information on droputs reported in a flow‐chart indicating the number of dropouts throughout the phases of treatment |
| Blinding of outcome assessment (detection bias) Relationship distress | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Investigators reported that 66 participants were randomised and 51 completed the study. Intention‐to‐treat analysis was not performed. |
| Selective reporting (reporting bias) | Low risk | Full data reported for primary and secondary endpoints |
| Other bias | High risk | 10 cases in the couple therapy group had some sessions of individual therapy and 7 cases in the TAU group had some sessions of individual therapy. Therefore, contamination between the two conditions occurred to some extent. |
Teichman 1995.
| Methods | Three arm parallel group quasi‐randomised trial (randomisation restricted by therapists' availability). The groups were matched for medication and diagnosis. | |
| Participants |
Participants: married outpatients meeting DSM‐III‐R criteria for major depressive disorder or dysthymia Sex: both men and women. Distribution reported only for completers. Men: n = 21 and women: n = 24 Age: adults. Mean age 47.86 years for participants (range 28 to 65) and 47 years for their partners (range 22 to 66) Unit of allocation: individual participant Number randomised: 56 Number completing: 45 Setting: clinic attached to a mental hospital in Israel Inclusion criteria:
Exclusion criteria:
Ethnicity: not reported Baseline characteristics: Mean marriage length 16.53 years; mean income USD 45,000 |
|
| Interventions |
Three conditions: Cognitive Marital Therapy (CMT), individual Cognitive Behavioural Therapy (CBT), Wait list. CMT as described by Teichman 1990. Individual Cognitive Behavioural Therapy based on the approach by Beck 1979. Number of participants in groups was given for completers only (15 in each group). Drug therapy allowed in all groups. Duration of intervention: 15 weekly sessions. Mean 13.4 sessions for CMT, 12.5 sessions for CBT. In the wait list group, participants remained for 3 months. Length of follow‐up: assessment at post‐treatment and 6 months. Wait‐list group assessed at 3 months only |
|
| Outcomes |
Depression: self‐assessment by BDI. Recovery defined as score ≤ 10 Dropouts Level of functioning by Clinician‐rated Patient Evaluation Questionnaire (Goldstein 1971). Participant’s and partner’s satisfaction Self‐assessment by one‐item scale ranged from 1 (lowest satisfaction) to 7 (highest satisfaction). |
|
| Notes | No calculation of statistical power. Treatments provided by 19 therapists (4 psychiatrists, 5 psychologists, 10 social workers) with a mean of 10.2 years of experience in CMT group and 9.7 years in CBT group. Treatment fidelity not assessed. Six participants in each group received antidepressant medications (details of medications not reported). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Investigators reported that, quote: “assignment to treatment groups was random restricted only by therapist availability” |
| Allocation concealment (selection bias) | High risk | Investigators reported that, quote: “assignment to treatment groups was random restricted only by therapist availability”. No information provided on allocation concealment, but we judged that, since the randomisation method relied on the availability of therapists, allocation concealment could not have been undertaken. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel not feasible in clinical trials of psychological interventions |
| Blinding of outcome assessment (detection bias) Depressive symptoms | High risk | Outcome assessed by a self‐report measure. Blinding not feasible |
| Blinding of outcome assessment (detection bias) Dropouts | Low risk | Information is provided on number and timing of dropouts and reasons for dropouts |
| Blinding of outcome assessment (detection bias) Relationship distress | Low risk | Outcome not assessed |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Investigators reported that 56 participants were randomised, and 11 from the two treatment groups dropped out before completing 7 sessions (number in the two groups not reported). The participants who participated in at least 7 sessions were considered as completers. For the primary endpoint, 45 participants were assessed after treatment, and 23 were assessed at follow‐up. No intention‐to treat analysis was performed. |
| Selective reporting (reporting bias) | Low risk | Full data reported for primary and secondary endpoints |
| Other bias | Unclear risk | No information on differences between groups on exposure to drug therapies. |
List of abbreviations:
ACSW = Academy of Certified Social Workers
AUDIT = Alcohol Use Disorder Identification Test
BCT = Brief Problem‐Focused Couple Therapy
BDI = Beck Depression Inventory
BMT = Behavioural Marital Therapy
CBT = Cognitive Behavioural Therapy
CFI = Camberwell Family Interview
CMT = Cognitive Marital Therapy
COCT = Coping‐Oriented Couples Therapy
CT = Couple Therapy
DAS = Dyadic Adjustment Scale
DSM‐III = Diagnostic and Statistical Manual of Mental Disorders‐3d edition
DSM‐III‐R = Diagnostic and Statistical Manual of Mental Disorders‐3d edition, revised
DSM‐IV = Diagnostic and Statistical Manual of Mental Disorders‐4th edition
ECT = Electroconvulsive therapy
EFT = Emotion‐Focused Couple Therapy
HRSD = Hamilton Rating Scale for Depression
IDD = Inventory to Diagnose Depression
IDS‐C30 = Inventory of Depressive Symptomatology
IPT = Individual Interpersonal Therapy
IPT‐CM = Conjoint Marital Interpersonal Psychotherapy
MDD = Major Depressive Disorder
MMD = Maudsley Marital Questionnaire
MMQ‐M = Maudsley Marital Questionnaire‐Marital Satisfaction
MFT = Multiple Family Therapy
QMI = Quality of Marriage Index
SADS‐L = Schedule for Affective Disorders and Schizophrenia‐Lifetime Version
SCID = Structured Clinical Interview for DSM
SCL‐90 = Symptom Checklist 90
SD = Standard Deviation
TAU = Treatment as Usual
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Dick‐Grace 1995 | The intervention was cognitive therapy offered according to three modalities: individual, couple, and family, but useful data could not be extracted |
| Friedman 1975 | Primary diagnosis of depressive disorder was not settled according to an internationally validated diagnostic system, and it provided only poor description of the couple therapy offered |
| Hajiheidari 2013 | No formal diagnosis of depression was made |
| Hashemi 2017 | No formal diagnosis of depression was made |
| Jacobson 1993 | Reported a follow‐up of the sub‐sample of recovered participants already included in a previous clinical trial |
| Kröger 2012 | No formal diagnosis of depression was made |
| Miller 2005 | The experimental group was treated by family therapy in an inpatient setting. Moreover, data were given according to matching and mismatching of the assigned treatment to the clinicians' evaluation of the participants' needs and not according to randomisation |
| Noorbala 2008 | The intervention was cognitive therapy plus supportive therapy for infertility aiming at resolving symptoms in women undergoing infertility treatment. The comparison was between psychological treatment offered before and during infertility treatment. |
| Sanders 2000 | Mothers' depression was part of a wider problem related to the presence of a disruptive child and the experimental group was treated by family therapy |
| Shahverdi 2015 | Primary outcome was improvement of general mental health, not depressive symptom level |
| Soltani 2014 | No formal diagnosis of depression was made |
| Swanson 2009 | Tested an intervention entirely focused on the meaning of the experience of miscarriage and did not adopt principles and methods of couple therapy |
| Tilden 2010 | Naturalistic prospective design and the intervention was delivered during inpatient admission |
| Waring 1990 | Not enough information was provided to extract data |
| Waring 1994 | Not enough information was provided to extract data |
| Waring 1995 | Not enough information was provided to extract data |
Differences between protocol and review
The following points have been changed from the earlier version of this review:
1. The terminology has been changed from 'marital therapy' to 'couple therapy', to take into account the recent practice of considering as the target of intervention any couple in a committed relationship, and not just married couples.
2. In the first version of this review, one objective was to identify mediating variables through which marital therapy was effective. In this new version, we decided to restrict our focus on the effects of therapy, leaving aside the analysis of mediating variables, which would require a specific study design.
3. The age limit has been changed from 16 years to 18 years because 18 years usually defines the age at which people become adults. Couple therapy is conceived for an adult population and therefore we deemed it more appropriate to select such a population.
4. A close examination of the study by Lemmens 2009 led the authors of this review to update the definition of 'outpatient setting' by including treatments started during inpatient admission provided that the majority of couple therapy sessions were delivered after discharge. Actually, this was the case for a subgroup of participants in the Lemmens 2009 study.
4. It has been specified that 'waiting list', as is usual in psychotherapy research, is considered equivalent to 'no/minimal treatment'.
5. In the first version of this review, outcomes were assessed at the the end of treatment and at 6‐month follow‐up. This was changed to add assessment at longer follow‐up (15 months or more), taking into account the importance of more than one year follow‐up assessment in psychotherapy research (Cuijpers 2008a).
6. The methods have been brought up‐to‐date to comply with the MECIR standards, especially with regard with the assessment of risk of bias and the use of the GRADE approach for the evaluation of evidence quality, as indicated in RevMan 2014 and in the Cochrane Handbook by Higgins 2011.
7. It was specified in the previous version of this review (Barbato 2006) that the inclusion of the quasi‐randomised study by Teichman 1995 was a post‐hoc decision. When the earlier protocol of this review was revised in 2010, we decided to amend the protocol by including both randomised and quasi‐randomised studies. Therefore, we checked the results of the original search performed in 2005 to look for other quasi‐randomised studies to be included in the review. We used the same criterion when screening the electronic search results from 2010 onwards and handsearching the journals and reference lists. We did not find other quasi‐randomised studies. It is worth noting that the study by Teichman 1995 was included among the randomised clinical trials examining the effects of psychotherapy for adult depression in the database run by the Department of Psychology of VU University Amsterdam (http://www.evidencebasedpsychotherapies.org). However, the authors of this review confirmed the decision to consider this paper as a quasi randomised study.
Contributions of authors
All review authors contributed equally to the review.
Sources of support
Internal sources
IRCCS‐Istituto di Ricerche Farmacologiche Mario Negri, Italy.
External sources
No sources of support supplied
Declarations of interest
None.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Beach 1992 {published and unpublished data}
- Beach SR. Information on our trial [personal communication]. E‐mail to: A Barbato 6 December 2005.
- Beach SR, O'Leary K. Treating depression in the context of marital discord: outcome and predictors of response of marital therapy versus cognitive therapy. Behavior Therapy 1992;23(4):507‐28. [Google Scholar]
Bodenmann 2008a {published and unpublished data}
- Bodenmann G. Re: Cochrane review of couple therapy [personal communication]. E‐mail to: A Barbato 10 February 2011.
- Bodenmann G, Plancherel B, Beach SRH, Widmer K, Gabriel B, Meuwly N, et al. Effects of coping‐oriented couples therapy on depression: a randomized clinical trial. Journal of Consulting and Clinical Psychology 2008;76(6):944‐54. [DOI] [PubMed] [Google Scholar]
- Gabriel B, Bodenmann G, Widmer K, Charvoz L, Schramm E, Hautzinger M. Effects of cognitive behavior therapy, interpersonal psychotherapy, and coping‐oriented couple therapy for the treatment of depression on the observed dyadic coping behavior [Auswirkungen der kognitiven verhaltenstherapie, der interpersonellen psychotherapie sowie der bewältigungsorientierten paartherapie zur behandlung von depressionen auf das beobachtete dyadische copingverhalten]. Zeitschrift für Klinische Psychologie und Psychotherapie 2008;37(3):179‐89. [Google Scholar]
- Gabriel B, Bodenmann G, Widmer K, Charvoz L, Schramm E, Hautzinger M. Effects of different therapeutical approaches for the treatment of depression on the observed dyadic conflict behavior [Auswirkungen verschiedener therapeutischer Ansätze zur behandlung von depressionen auf das beobachtete partnerschaftliche konfliktverhalten]. Zeitschrift für Psychiatrie, Psychologie und Psychotherapie 2009;57(1):43‐54. [Google Scholar]
Cohen 2010 {published data only}
- Cohen S. Development of a brief couples therapy for depression: targeting illness‐related attitudes and behaviors, empathy, and support [PhD thesis]. New York: University of Stony Brook, 2007. [Google Scholar]
- Cohen S, O'Leary KD, Foran H. A randomized clinical trial of a brief, problem‐focused couple therapy for depression. Behavior Therapy 2010;41(4):433‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, O'Leary KD, Foran HM, Kliem S. Mechanisms of change in brief couple therapy for depression. Behavior Therapy 2014;45(3):402‐17. [DOI] [PubMed] [Google Scholar]
Compton 2008 {published data only (unpublished sought but not used)}
- Compton J. Adapting marital therapy in older adults with depression. clinicaltrialsgov/ct2/show/NCT00612807 (first received 12 February 2008).
Denton 2012 {published data only}
- Denton WH, Wittenborn AK, Golden RM. Augmenting antidepressant medication treatment of depressed women with emotionally focused therapy for couples: a randomized pilot study. Journal of Marital and Family Therapy 2012;38(1):23‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dessaulles 2003 {published data only}
- Dessaulles A. The Treatment of Clinical Depression in the Context of Marital Distress [Thesis]. Ottawa: Canadian Theses Service, National Library of Canada, 1991. [Google Scholar]
- Dessaulles A, Johnson SM, Denton WH. Emotion focused therapy for couples in treatment of depression: a pilot study. American Journal of Family Therapy 2003;31(5):345‐53. [Google Scholar]
Emanuels 1996 {published data only}
- Emanuels‐Zuurveen L, Emmelkamp PM. Individual behavioural‐cognitive therapy v marital therapy for depression in marital distressed couples. British Journal of Psychiatry 1996;169(2):181‐8. [DOI] [PubMed] [Google Scholar]
Emanuels 1997 {published data only}
- Emanuels‐Zuurveen L, Emmelkamp PM. Spouse‐aided therapy with depressed patients. Behavior Modification 1997;21(1):62‐77. [DOI] [PubMed] [Google Scholar]
Foley 1989 {published data only}
- Foley SH, Rounsaville BJ, Weissman MM, Sholomskas D, Chevron E. Individual versus conjoint interpersonal psychotherapy for depressed patients with marital disputes. International Journal of Family Psychiatry 1989;10(1):29‐42. [Google Scholar]
Jacobson 1991 {published data only}
- Jacobson NS, Dobson K, Fruzzetti AE, Schmaling KB. Marital therapy as a treatment for depression. Journal of Consulting and Clinical Psychology 1991;59(4):547‐57. [DOI] [PubMed] [Google Scholar]
Leff 2000 {published data only}
- Leff J, Alexander B, Asen E, Brewin CR, Dayson D, Vearnals S, et al. Mode of action of family interventions in depression and schizophrenia: the same or different?. Journal of Family Therapy 2003;25(4):357‐70. [Google Scholar]
- Leff J, Vearnals S, Brewin CR, Wolff G, Alexander B, Asen E, et al. The London Depression Intervention trial. Randomised controlled trial of antidepressants v couple therapy in the treatment and maintenance of people with depression living with the partner: clinical outcome and costs. British Journal of Psychiatry 2000;177(2):95‐100. [DOI] [PubMed] [Google Scholar]
Lemmens 2009 {published data only}
- Lemmens GMD, Eisler I, Buysse A, Heene E, Demyttenaere K. The effects on mood of adjunctive single‐family and multi‐family group therapy in the treatment of hospital patients with major depression. Psychotherapy and Psychosomatics 2009;78(2):98‐105. [DOI] [PubMed] [Google Scholar]
Seikkula 2012 {published and unpublished data}
- Kuhlman I, Toivanen A, Seikkula J. Couple therapy for depression within a naturalistic setting in Finland: factors related to change in the patient and the spouse. Contemporary Family Therapy 2013;35(4):656‐72. [Google Scholar]
- Seikkula J. Cochrane review couple therapy [personal communication]. E‐mail to: A Barbato 22 April 2013.
- Seikkula J, Aaltonen J, Kalla O, Saarinen P, Tolvanen A. Couple therapy for depression in a naturalistic setting in Finland: a 2‐year randomized trial. Journal of Family Therapy 2012;35(3):281‐302. [Google Scholar]
Teichman 1995 {published and unpublished data}
- Teichman Y. Randomization method [personal communication]. E‐mail to: A Barbato 10 December 2005.
- Teichman Y, Bar‐El Z, Shor H, Sirota P, Elizur A. A comparison of two modalities of cognitive therapy (individual and marital) in treating depression. Psychiatry 1995;58(2):136‐48. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Dick‐Grace 1995 {published data only}
- Dick‐Grace JE. Cognitive Therapy with Depressed, Female Outpatients in Individual, Couple, and Group Treatment Modalities: an Evaluation [Doctoral thesis]. Tallahassee: School of Social Work, Florida State University, 1995. [Google Scholar]
Friedman 1975 {published data only}
- Friedman AS. Interaction of drug therapy with marital therapy in depressive patients. Archives of General Psychiatry 1975;32(5):619‐37. [DOI] [PubMed] [Google Scholar]
Hajiheidari 2013 {published data only}
- Hajiheidari M, Sharifi M, Khorvash F. The effect of interpersonal psychotherapy on marriage adaptive and postpartum depression in Isfahan. International Journal of Preventive Medicine 2013;4 suppl 2:S256‐61. [PMC free article] [PubMed] [Google Scholar]
Hashemi 2017 {published data only}
- Hashemi SF, Kimiaei SA. The effectiveness of emotion‐focused cognitive therapy in decreasing depression due to marital relationship problems. Universal Journal of Psychology 2017;5(4):196‐203. [Google Scholar]
Jacobson 1993 {published data only}
- Jacobson NS, Fruzzetti AE, Dobson K, Whisman M, Hops H. Couple therapy as a treatment for depression: II. The effects of relationship quality and therapy on depressive relapse. Journal of Consulting and Clinical Psychology 1993;61(3):516‐9. [DOI] [PubMed] [Google Scholar]
Kröger 2012 {published data only}
- Kröger C, Reissner T, Vasterling I, Schütz K, Kliem S. Therapy for couples after an affair: a randomized controlled trial. Behaviour Research and Therapy 2012;50(12):786‐96. [DOI] [PubMed] [Google Scholar]
Miller 2005 {published data only}
- Miller IW, Keitner G, Ryan CE, Solomon DA, Cardemil EV, Beevers CG. Treatment matching in the post hospital care of depressed patients. American Journal of Psychiatry 2005;162(11):2131‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Noorbala 2008 {published data only}
- Noorbala AA, Ramazanzadeh F, Malekafzali H, Abediania N, Forooshani AR, Shariat M, et al. Effects of a psychological intervention on depression in infertile couples. International Journal of Gynecology and Obstetrics 2008;101(3):248‐52. [DOI] [PubMed] [Google Scholar]
Sanders 2000 {published data only}
- Sanders MR, McFarland M. Treatment of depressed mothers with disruptive children: a controlled evaluation of cognitive behavioural family intervention. Behavior Therapy 2000;31(1):89‐112. [Google Scholar]
Shahverdi 2015 {published data only}
- Shahverdi JA, Ahmadi SM, Rezaei M, Bakhtiari M. Effectiveness of behavioral couple therapy on improve mental health and reduction of marital conflict among infertile couples who referred to the Motazedi infertility center in Kermanshah. IRHRC Annual Meeting Reproductive and Infertility Updates. 2015.
Soltani 2014 {published data only}
- Soltani M, Shairi MR, Roshan R, Rahimi C. The impact of emotionally focused therapy on emotional distress in infertile couples. International Journal of Fertility and Sterility 2014;7(4):337‐44. [PMC free article] [PubMed] [Google Scholar]
Swanson 2009 {published data only}
- Swanson KM, Chen HT, Graham JC, Wojnar DM, Petras A. Resolution of depression and grief during the first year after miscarriage: a randomized controlled clinical trial of couples‐focused interventions. Journal of Women's Health 2009;18(8):1245‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tilden 2010 {published data only}
- Tilden T, Gude T, Hoffart A. The course of dyadic adjustment and depressive symptoms during and after couples therapy: a prospective follow‐up study of inpatient treatment. Journal of Marital and Family Therapy 2010;36(1):43‐58. [DOI] [PubMed] [Google Scholar]
Waring 1990 {published data only}
- Waring EM, Carver C, Stalker CA, Fry R, Schaefer B. A randomized clinical trial of cognitive marital therapy. Journal of Sex and Marital Therapy 1990;16(3):165‐80. [DOI] [PubMed] [Google Scholar]
Waring 1994 {published data only}
- Waring EM. The role of marital therapy in the treatment of depressed married women. Canadian Journal of Psychiatry 1994;39(9):568‐71. [DOI] [PubMed] [Google Scholar]
Waring 1995 {published data only}
- Waring EM, Chamberlaine CH, Carver CM, Stalker CA, Schaefer B. A pilot study of marital therapy as a treatment for depression. American Journal of Family Therapy 1995;23(1):3‐9. [Google Scholar]
Additional references
APA 1980
- American Psychiatric Association. Diagnostical and Statistical Manual of Mental Disorders (DSM‐III). 3rd Edition. Washington: American Psychiatric Association, 1980. [Google Scholar]
APA 1987
- American Psychiatric Association. Diagnostical and Statistical Manual of Mental Disorders (DSM‐III‐R). 3rd Edition. Washington: American Psychiatric Association, 1987. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostical and Statistical Manual of Mental Disorders (DSM‐IV). 4th Edition. Washington: American Psychiatric Association, 1994. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV‐TR). Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
APA 2013
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐5). 5th Edition. Washington DC: American Psychiatric Association, 2013. [Google Scholar]
Arrindell 1983
- Arrindell WA, Boelens W, Lambert H. On the psychometric properties of the Maudsley Questionnaire (MMQ): evaluation of self‐ratings in distressed and "normal" volunteer couples based on the Dutch version. Personality and Individual Differences 1983;4(3):293‐306. [Google Scholar]
Barbato 2006
- Barbato A, D'Avanzo B. Marital therapy for depression. Cochrane Database of Systematic Reviews 2006, Issue 2.. [DOI: 10.1002/14651858.CD004188.pub2] [DOI] [PubMed] [Google Scholar]
Baucom 1998
- Baucom DH, Shoham V, Mueser KT, Daiuto AD, Stickle TL. Empirically supported couple and family interventions for marital distress and adult mental health problems. Journal of Consulting and Clinical Psychology 1998;66(1):53‐88. [DOI] [PubMed] [Google Scholar]
Bauer 2013
- Bauer M, Pfennig A, Severus E, Whybrow PC, Angst J, Möller HJ. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. The World Journal of Biological Psychiatry 2013;14(5):334‐85. [DOI] [PubMed] [Google Scholar]
Beach 1990
- Beach SRH, Sandeen EE, O'Leary KD. Depression in Marriage. New York: Guilford, 1990. [Google Scholar]
Beach 1998
- Beach SRH, Fincham FD. Marital processes and depression. Family psychopathology. The relational roots of dysfunctional behavior. New York, NY: Guilford Press, 1998. [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Medelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4(6):561‐71. [DOI] [PubMed] [Google Scholar]
Beck 1979
- Beck AT, Rush AJ, Shaw BL, Emery G. Cognitive Therapy of Depression. New York: Guilford Press, 1979. [Google Scholar]
Beck 1996
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories ‐IA and ‐II in psychiatric outpatients. Journal of Personality Assessment 1996;67(3):588‐97. [DOI] [PubMed] [Google Scholar]
Benson 2012
- Benson LA, McGinn MM, Christensen A. Common principles of couple therapy. Behavior Therapy 2012;43(1):23‐35. [DOI] [PubMed] [Google Scholar]
Berto 2000
- Berto P, D'Ilario D, Ruffo P, Virgilio R, Rizzo F. Depression: cost‐of‐illness studies in the international literature, a review. Journal of Mental Health Policy and Economics 2000;3(1):3‐10. [DOI] [PubMed] [Google Scholar]
Bland 1997
- Bland RC, Newman SC, Orn H. Age and remission of psychiatric disorders. Canadian Journal of Psychiatry 1997;42(7):722‐9. [DOI] [PubMed] [Google Scholar]
Bodenmann 2004
- Bodenmann G. Verhaltenstherapie mit Paaren. Bern: Huber, 2004. [Google Scholar]
Bodenmann 2008b
- Bodenmann G. Dyadic Coping Inventar: Manual. Bern: Huber, 2008. [Google Scholar]
Bostwick 2000
- Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. American Journal of Psychiatry 2000;157(12):1925‐32. [DOI] [PubMed] [Google Scholar]
Cano 2000
- Cano A, O'Leary KD. Infidelity and separations precipitate major depressive episodes and symptoms of nonspecific depression and anxiety. Journal of Consulting and Clinical Psychology 2000;68(5):774‐81. [PubMed] [Google Scholar]
Carroll 1994
- Carroll KM, Rounsaville BJ, Nich C. Blind man's bluff: effectiveness and significance of psychotherapy and pharmacotherapy blinding procedures in a clinical trial. Journal of Consulting and Clinical Psychology 1994;62(2):276‐80. [DOI] [PubMed] [Google Scholar]
Chilvers 2001
- Chilvers C, Dewey M, Fielding C, Gretton V, Miller P, Palmer B, et al. Antidepressant drugs and generic counselling for treatment of major depression in primary care: randomised trial with patient preference arms. BMJ 2001;322(7289):772‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cristea 2017
- Cristea IA, Gentili C, Pietrini P, Cuijpers P. Sponsorship bias in the comparative efficacy of psychotherapy and pharmacotherapy for adult depression: meta‐analysis. British Journal of Psychiatry 2017;210(1):16‐23. [DOI] [PubMed] [Google Scholar]
Cuijpers 2008a
- Cujpers P, Straten A, Andersson G, Oppen P. Psychotherapy for depression in adults: a meta‐analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology 2008;76:909‐22. [DOI] [PubMed] [Google Scholar]
Cuijpers 2008b
- Cuijpers P, Straten A, Oppen P, Andersson G. Are psychological and pharmacologic interventions equally effective in the treatment of adult depressive disorders? A meta‐analysis of comparative studies. Journal of Clinical Psychiatry 2008;69(11):1675‐85. [DOI] [PubMed] [Google Scholar]
Cuijpers 2009
- Cuijpers P, Straten A, Warmerdam L, Andersson G. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta‐analysis. Depression and Anxiety 2009;26(3):279–88. [DOI] [PubMed] [Google Scholar]
Cuijpers 2014
- Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta‐analysis. World Psychiatry 2014;13(1):56‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Denton 2003
- Denton WH, Golden RN. Depression, marital discord and couple therapy. Current Opinion in Psychiatry 2003;16(1):29‐34. [Google Scholar]
Denton 2006
- Denton WH, Burwell SR. Systemic couple intervention for depression in women. Journal of Systemic Therapies 2006;25(1):43‐57. [Google Scholar]
Denton 2009
- Denton WH, Johnson SM, Burleson BR. Emotion‐focused therapy‐therapist fidelity scale (EFT‐TFS): conceptual development and content validity. Journal of Couple and Relationship Therapy 2009;8(3):226‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Derogatis 1983
- Derogatis LR. The SCL‐90: Administration, Scoring and Procedures for the SCL‐90. Baltimore: Clinical Psychometris Research, 1983. [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Dobson 1985
- Dobson KS, Shaw BF, Vallis TM. Reliability of a measure of the quality of cognitive therapy. British Journal of Clinical Psychology 1985;24(4):295‐300. [DOI] [PubMed] [Google Scholar]
Emmelkamp 1984
- Emmelkamp PMG, Helm M, MacGillavry D, Zanten B. Marital therapy with clinically distressed couples: a comparative evaluation of system theoretic, contingency contracting and communication skills approaches. In: Hahlweg K, Jacobson N editor(s). Marital Interaction Analysis and Modification. New York: Guilford, 1984. [Google Scholar]
Ferrari 2013
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJL, et al. Burden of depressive disorders by country, sex, age and year: findings from the global burden of disease study 2010. PLOS Medicine 2013;10(11):e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
Folstein 1975
- Folstein MF, Folstein SE, McHugh PR. Mini‐mental state. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 1975;12(3):189‐98. [DOI] [PubMed] [Google Scholar]
Gilliam 2005
- Gilliam CM, Cottone RR. Couple or individual therapy for the treatment of depression? An update of the empirical literature. American Journal of Family Therapy 2005;33(3):265‐72. [Google Scholar]
Goldstein 1971
- Goldstein AP. Psychotherapeutic Relationship. 1st Edition. New York (NY): Pergamon Press, 1971. [Google Scholar]
Goodman 1999
- Goodman SH, Gotlib IH. Risk of psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychological Review 1999;106(3):458‐90. [DOI] [PubMed] [Google Scholar]
Grundy 1996
- Grundy CT, Lambert MJ, Grundy EM. Assessing clinical significance: application to the Hamilton Rating Scale for Depression. Journal of Mental Health 1996;5(1):25‐33. [Google Scholar]
Gupta 2003
- Gupta M, Coyne JC, Beach SR. Couples treatment for major depression: critique of the literature and suggestions for some different directions. Journal of Family Therapy 2003;25(4):317‐46. [Google Scholar]
Hafner 1983
- Hafner RJ, Badenoch A, Fisher J, Swift H. Spouse‐aided versus individual therapy in persisting psychiatric disorders: a systematic comparison. Family Process 1983;22(3):385–90. [DOI] [PubMed] [Google Scholar]
Hahlweg 1996
- Hahlweg K. Fragebogen zur Partnerschaftsdiagnostik (FPD). Göttingen (GER): Hogrefe, 1996. [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 1960;23(1):56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 1980
- Hamilton M. Rating depressive patients. Journal of Clinical Psychiatry 1980;41(1):21‐4. [PubMed] [Google Scholar]
Hasin 2005
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder. Results from the National Epidemiologic Survey on alcoholism and related conditions. Archives of General Psychiatry 2005;62(10):1097‐106. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hollon 2012
- Hollon SD, Sexton TL. Determining what works in depression treatment: translating research to relational practice using treatment guidelines. Couple and Family Psychology: Research and Practice 2012;1(3):199‐212. [Google Scholar]
Hooley 2007
- Hooley JM. Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology 2007;3(1):329‐52. [DOI] [PubMed] [Google Scholar]
Jacobson 1986
- Jacobson NS, Holtzworth‐Munroe A. Marital therapy: a social learning/cognitive perspective. In: Jacobson NS, Gurman AS editor(s). Clinical Handbook of Marital Therapy. New York (NY): Guilford, 1986:29‐70. [Google Scholar]
Johnson 2004
- Johnson SM. The Practice of Emotionally Focused Therapy: Creating Connection. 2nd Edition. London (UK): Brunner‐Routledge, 2004. [Google Scholar]
Jones 1999
- Jones E, Asen E. Systemic Couple Therapy and Depression. 1st Edition. London (UK): Karnac, 1999. [Google Scholar]
Kendler 1999
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry 1999;156(6):1243–51. [DOI] [PubMed] [Google Scholar]
Kessler 2013
- Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annual Review of Public Health 2013;34(1):119‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klerman 1984
- Klerman G, Weissman MM, Rounsaville BJ, Chevron E. The Theory and Practice of Interpersonal Psychotherapy for Depression. 1st Edition. New York (NY): Basic Books, 1984. [Google Scholar]
Kronmüller 2011
- Kronmüller KT, Backenstrass M, Victor D, Postelnicu I, Schenkenbach C, Joest K, et al. Quality of marital relationship and depression: results of a 10‐year prospective follow‐up study. Journal of Affective Disorders 2011;128(1‐2):64‐71. [DOI] [PubMed] [Google Scholar]
Lebow 2012
- Lebow J, Chambers AL, Chistensen A, Johnson SM. Research on the treatment of couple distress. Journal of Marital and Family Therapy 2012;38(1):145‐68. [DOI] [PubMed] [Google Scholar]
Lemmens 2007
- Lemmens GMD, Eisler I, Migerode L, Heireman M, Demyttenaere K. Family discussion group therapy for major depression: the brief systemic multi‐family group intervention for hospitalised patients and their family members. Journal of Family Therapy 2007;29(1):49‐68. [Google Scholar]
Locke 1976
- Locke HJ, Wallace KM. Short‐term marital adjustment and prediction tests: their reliability and validity. Journal of Marriage and Family 1976;38(1):15‐28. [Google Scholar]
Lundblad 2006
- Lundblad AM, Hansson K. Couples therapy: effectiveness of treatment and long‐term follow‐up. Journal of Family Therapy 2006;28(2):136‐52. [Google Scholar]
MacIntosh 2014
- MacIntosh HB, Butters M. Measuring outcomes in couple therapy: a systematic review and critical discussion. Journal of Couple and Relationship Therapy: Innovations in Clinical and Educational Interventions 2014;13(1):44‐62. [Google Scholar]
Magaña 1986
- Magaña AB. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Research 1986;17(3):203‐12. [DOI] [PubMed] [Google Scholar]
Malhi 2009
- Malhi GS, Adams D, Porter R, Wignall A, Lampe L, O’Connor N, et al. Clinical practice recommendations for depression. Acta Psychiatrica Scandinavica 2009;119(1):8–26. [DOI] [PubMed] [Google Scholar]
Mueller 1999
- Mueller TL, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow‐up. American Journal of Psychiatry 1999;156(7):1000‐6. [DOI] [PubMed] [Google Scholar]
Munder 2013
- Munder T, Brütsch O, Leonhart R, Gerger H, Barth J. Researcher allegiance in psychotherapy outcome research: an overview of reviews. Clinical Psychology Review 2013;33(4):501‐11. [DOI] [PubMed] [Google Scholar]
Newman 1991
- Newman SC, Bland RC. Suicide risk varies by subtype of affective disorder. Acta Psychiatrica Scandinavica 1991;83(6):420‐6. [DOI] [PubMed] [Google Scholar]
NICE 2009
- National Institute for Health and Clinical Excellence (NICE). Depression in adults: recognition and management (CG90). www.nice.org.uk/guidance/cg90/resources/depression‐in‐adults‐recognition‐and‐management‐pdf‐975742638037 2009 (updated April 2018). [PubMed]
Norton 1983
- Norton R. Measuring marital quality: a critical look at the dependent variable. Journal of Marriage and the Family 1983;45(1):141‐51. [Google Scholar]
Ogles 1995
- Ogles BM, Lambert MJ, Sawyer JD. Clinical significance of the National Institute of Mental Health Treatment of Depression Collaborative Research Program data. Journal of Consulting and Clinical Psychology 1995;63(2):321‐26. [DOI] [PubMed] [Google Scholar]
Raskin 1967
- Raskin A, Schulterbrandt J, Reatig N, Rice CA. Factors of psychopathology in interview, ward behavior, and self‐report ratings of hospitalized depressives. Journal of Consulting and Clinical Psychology 1967;31(3):270‐8. [DOI] [PubMed] [Google Scholar]
Rehman 2008
- Rehman US, Gollan J, Mortimer AR. The marital context of depression: research, limitations, and new directions. Clinical Psychology Review 2008;28(2):179‐98. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rush 1996
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The inventory of depressive symptomatology (IDS): psychometric properties. Psychological Medicine 1996;26(3):477‐86. [DOI] [PubMed] [Google Scholar]
Sobocki 2006
- Sobocki P, Jönsson B, Angst J, Rehnberg C. Cost of depression in Europe. Journal of Mental Health Policy and Economics 2006;9(2):87‐98. [PubMed] [Google Scholar]
Spanier 1976
- Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriages and similar dyads. Journal of Marriage and the Family 1976;38(1):15‐28. [Google Scholar]
Spitzer 1978
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry 1978;35(6):773‐85. [DOI] [PubMed] [Google Scholar]
Suehs 2008
- Suehs B, Argo TR, Bendele SD, Crismon ML, Trivedi MH, Kurian B. Texas medication algorithm procedural manual: major depressive disorder algorithms. www.dshs.state.tx.us/mhprograms/pdf/TIMA_MDD_Manual_080608.pdf (accessed prior to 15 May 2018).
Teichman 1990
- Teichman Y, Teichman M. Interpersonal view of depression: review and integration. Journal of Family Psychology 1990;3(4):349‐67. [Google Scholar]
Vaughn 1976b
- Vaughn C, Leff JP. The measurement of expressed emotion in families of psychiatric patients. British Journal of Social and Clinical Psychology 1976;15(2):157‐65. [DOI] [PubMed] [Google Scholar]
Vos 2000
- Vos T, Mathers CD. The burden of mental disorders: a comparison of methods between the Australian Burden of Disease Studies and the Global Burden of Disease Study. Bulletin of the World Health Organization 2000;78(4):427‐38. [PMC free article] [PubMed] [Google Scholar]
Waraich 2004
- Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Canadian Journal of Psychiatry 2004;49(2):124‐38. [DOI] [PubMed] [Google Scholar]
Whisman 2001
- Whisman MA. The association between depression and marital dissatisfaction. Marital and Family Processes in Depression: A Scientific Foundation for Clinical Practice. Washington (DC): American Psychological Association, 2001. [Google Scholar]
Whisman 2012
- Whisman MA, Johnson DP, Be D, Li A. Couple‐based interventions for depression. Couple and Family Psychology: Research and Practice 2012;1(3):185‐98. [Google Scholar]
WHO 1992
- World Health Organization. The ICD‐10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. [Google Scholar]
Wing 1974
- Wing JK, Cooper JE, Sartorius N. The Measurement and Classification of Psychiatric Symptoms. Cambridge (UK): Cambridge University Press, 1974. [Google Scholar]
Zimmerman 1986
- Zimmerman M, Coryell W, Corenthal C, Wison S. A self‐report scale to diagnose major depressive disorder. Archives of General Psychiatry 1986;43(11):1076‐81. [DOI] [PubMed] [Google Scholar]
Üstün 2004
- Üstün TB, Ayuso‐Mateos JL, Chatterji S, Mathers C, Murray CJL. Global burden of depressive disorders in the year 2000. British Journal of Psychiatry 2004;184(5):386‐92. [DOI] [PubMed] [Google Scholar]


