Abstract
Background
Researchers have suggested that omega‐3 polyunsaturated fatty acids from oily fish (long‐chain omega‐3 (LCn3), including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)), as well as from plants (alpha‐linolenic acid (ALA)) benefit cardiovascular health. Guidelines recommend increasing omega‐3‐rich foods, and sometimes supplementation, but recent trials have not confirmed this.
Objectives
To assess effects of increased intake of fish‐ and plant‐based omega‐3 for all‐cause mortality, cardiovascular (CVD) events, adiposity and lipids.
Search methods
We searched CENTRAL, MEDLINE and Embase to April 2017, plus ClinicalTrials.gov and World Health Organization International Clinical Trials Registry to September 2016, with no language restrictions. We handsearched systematic review references and bibliographies and contacted authors.
Selection criteria
We included randomised controlled trials (RCTs) that lasted at least 12 months and compared supplementation and/or advice to increase LCn3 or ALA intake versus usual or lower intake.
Data collection and analysis
Two review authors independently assessed studies for inclusion, extracted data and assessed validity. We performed separate random‐effects meta‐analysis for ALA and LCn3 interventions, and assessed dose‐response relationships through meta‐regression.
Main results
We included 79 RCTs (112,059 participants) in this review update and found that 25 were at low summary risk of bias. Trials were of 12 to 72 months' duration and included adults at varying cardiovascular risk, mainly in high‐income countries. Most studies assessed LCn3 supplementation with capsules, but some used LCn3‐ or ALA‐rich or enriched foods or dietary advice compared to placebo or usual diet.
Meta‐analysis and sensitivity analyses suggested little or no effect of increasing LCn3 on all‐cause mortality (RR 0.98, 95% CI 0.90 to 1.03, 92,653 participants; 8189 deaths in 39 trials, high‐quality evidence), cardiovascular mortality (RR 0.95, 95% CI 0.87 to 1.03, 67,772 participants; 4544 CVD deaths in 25 RCTs), cardiovascular events (RR 0.99, 95% CI 0.94 to 1.04, 90,378 participants; 14,737 people experienced events in 38 trials, high‐quality evidence), coronary heart disease (CHD) mortality (RR 0.93, 95% CI 0.79 to 1.09, 73,491 participants; 1596 CHD deaths in 21 RCTs), stroke (RR 1.06, 95% CI 0.96 to 1.16, 89,358 participants; 1822 strokes in 28 trials) or arrhythmia (RR 0.97, 95% CI 0.90 to 1.05, 53,796 participants; 3788 people experienced arrhythmia in 28 RCTs). There was a suggestion that LCn3 reduced CHD events (RR 0.93, 95% CI 0.88 to 0.97, 84,301 participants; 5469 people experienced CHD events in 28 RCTs); however, this was not maintained in sensitivity analyses – LCn3 probably makes little or no difference to CHD event risk. All evidence was of moderate GRADE quality, except as noted.
Increasing ALA intake probably makes little or no difference to all‐cause mortality (RR 1.01, 95% CI 0.84 to 1.20, 19,327 participants; 459 deaths, 5 RCTs),cardiovascular mortality (RR 0.96, 95% CI 0.74 to 1.25, 18,619 participants; 219 cardiovascular deaths, 4 RCTs), and it may make little or no difference to CHD events (RR 1.00, 95% CI 0.80 to 1.22, 19,061 participants, 397 CHD events, 4 RCTs, low‐quality evidence). However, increased ALA may slightly reduce risk of cardiovascular events (from 4.8% to 4.7%, RR 0.95, 95% CI 0.83 to 1.07, 19,327 participants; 884 CVD events, 5 RCTs, low‐quality evidence), and probably reduces risk of CHD mortality (1.1% to 1.0%, RR 0.95, 95% CI 0.72 to 1.26, 18,353 participants; 193 CHD deaths, 3 RCTs), and arrhythmia (3.3% to 2.6%, RR 0.79, 95% CI 0.57 to 1.10, 4,837 participants; 141 events, 1 RCT). Effects on stroke are unclear.
Sensitivity analysis retaining only trials at low summary risk of bias moved effect sizes towards the null (RR 1.0) for all LCn3 primary outcomes except arrhythmias, but for most ALA outcomes, effect sizes moved to suggest protection. LCn3 funnel plots suggested that adding in missing studies/results would move effect sizes towards null for most primary outcomes. There were no dose or duration effects in subgrouping or meta‐regression.
There was no evidence that increasing LCn3 or ALA altered serious adverse events, adiposity or lipids, although LCn3 slightly reduced triglycerides and increased HDL. ALA probably reduces HDL (high‐ or moderate‐quality evidence).
Authors' conclusions
This is the most extensive systematic assessment of effects of omega‐3 fats on cardiovascular health to date. Moderate‐ and high‐quality evidence suggests that increasing EPA and DHA has little or no effect on mortality or cardiovascular health (evidence mainly from supplement trials). Previous suggestions of benefits from EPA and DHA supplements appear to spring from trials with higher risk of bias. Low‐quality evidence suggests ALA may slightly reduce CVD event risk, CHD mortality and arrhythmia.
Keywords: Adult; Humans; Dietary Supplements; Cardiovascular Diseases; Cardiovascular Diseases/diet therapy; Cardiovascular Diseases/mortality; Cardiovascular Diseases/prevention & control; Cause of Death; Docosahexaenoic Acids; Docosahexaenoic Acids/therapeutic use; Eicosapentaenoic Acid; Eicosapentaenoic Acid/therapeutic use; Fatty Acids, Omega‐3; Fatty Acids, Omega‐3/adverse effects; Fatty Acids, Omega‐3/therapeutic use; Primary Prevention; Randomized Controlled Trials as Topic; Secondary Prevention; Treatment Outcome; alpha‐Linolenic Acid; alpha‐Linolenic Acid/therapeutic use
Omega‐3 intake for cardiovascular disease
Review question
We reviewed randomised trials (where participants have an equal chance of being assigned to either treatment) examining effects of increasing fish‐ and plant‐based omega‐3 fats on heart and circulatory disease (called cardiovascular diseases, CVD, which include heart attacks and stroke), fatness and blood fats (lipids, including cholesterol, triglycerides, high‐density lipoprotein (HDL – 'good' cholesterol) and low‐density lipoprotein (LDL – 'bad' cholesterol)).
Background
Omega‐3 fats are essential – to stay healthy we must obtain some from food. The main types of omega‐3 fats are alpha‐linolenic acid (ALA), a fat found in plant foods, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), both found in fish. There is a common belief that eating more fish or taking omega‐3 supplements reduces our risk of heart disease, stroke and death.
Study characteristics
The evidence is current to April 2017. The review included 79 trials involving over 112,000 people. These studies assessed effects of greater omega‐3 intake versus lower or no omega‐3 intake for heart and circulatory disease. Twenty‐five studies were very trustworthy (well‐designed so as not to give biased results). Participants were adults, some with existing illness and some healthy, living in North America, Europe, Australia and Asia. Participants increased omega‐3 fats, or maintained their usual fats for at least a year. Most EPA and DHA trials provided capsules, few gave oily fish.
Key results
Increasing EPA and DHA has little or no effect on all‐cause deaths and cardiovascular events (high‐quality evidence) and probably makes little or no difference to cardiovascular death, coronary deaths or events, stroke, or heart irregularities (moderate‐quality evidence, coronary events are illnesses of the arteries which supply the heart). EPA and DHA slightly reduce serum triglycerides and raise HDL (high‐quality evidence).
Eating more ALA (for example, by increasing walnuts or enriched margarine) probably makes little or no difference to all‐cause or cardiovascular deaths or coronary events but probably slightly reduce cardiovascular events, coronary mortality and heart irregularities (moderate/low‐quality evidence). Effects of ALA on stroke are unclear as the evidence was of very low quality.
There is evidence that taking omega‐3 capsules does not reduce heart disease, stroke or death. There is little evidence of effects of eating fish. Although EPA and DHA reduce triglycerides, supplementary omega‐3 fats are probably not useful for preventing or treating heart and circulatory diseases. However, increasing plant‐based ALA may be slightly protective for some heart and circulatory diseases.
Summary of findings
Summary of findings for the main comparison.
High versus low LCn3 for preventing cardiovascular disease and mortality (primary outcomes)
| High versus low LCn3 for preventing cardiovascular disease and mortality (primary outcomes) | ||||||
|
Patient or population: adults with or without existing CVD Setting: participants were living at home for most or all of the duration of their trials. Most studies were carried out in high‐income economies (World Bank 2018), but four trials were carried out in upper‐middle income countries (Argentina, Iran, Turkey and China). No studies took place in low‐ or low‐middle income countries. Intervention: higher intake of long‐chain omega‐3 fats Comparison: lower intake of long‐chain omega‐3 fats The intervention was dietary supplementation, a provided diet or advice on diet. Supplementation may have been in oil or capsule form or as foodstuffs provided, to be consumed by mouth (excluding enteral and parenteral feeds and enemas). The foodstuffs or supplements must have been: oily fish or fish oils as a food, oil, made into a spreading fat or supplementing another food (such as bread or eggs). Refined eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) or concentrated fish or algal oils, were also accepted. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with lower LCn3 | Risk with higher LCn3 | |||||
|
All‐cause mortality – deaths Assessed with: number of participants dying of any cause, whether reported as an outcome or a reason for dropout Duration: range 12 to 72 months |
90 per 1,000 | 88 per 1,000 (83 to 92) | RR 0.98 (0.93 to 1.03) | 92,653 (39 RCTs) | ⊕⊕⊕⊕ Higha | Meta‐analysis and indications of bias suggest risk reduction of less than 2%. Long‐chain omega‐3 fat intake makes little or no difference to all‐cause mortality. |
|
Cardiovascular mortality – cardiovascular deaths Assessed with: deaths from any cardiovascular cause. Where this was not available, cardiac death was used instead where known. Duration: range 12 to 72 months |
69 per 1,000 | 66 per 1,000 (60 to 71) | RR 0.95 (0.87 to 1.03) | 67,772 (25 RCTs) | ⊕⊕⊕⊝ Moderateb | Meta‐analysis and indications of bias suggest risk reduction of less than 5%. Long‐chain omega‐3 fat intake probably makes little or no difference to cardiovascular deaths. |
|
Cardiovascular events – cardiovascular events Assessed with: number of participants experiencing any cardiovascular event Duration: range 12 to 72 months |
165 per 1,000 | 164 per 1,000 (155 to 172) | RR 0.99 (0.94 to 1.04) | 90,378 (38 RCTs) | ⊕⊕⊕⊕ Highc | Meta‐analysis and indications of bias suggest risk reduction of less than 1%. Long‐chain omega‐3 fat intake makes little or no difference to risk of cardiovascular events. |
|
Coronary heart disease mortality – CHD deaths Assessed with: coronary deaths, or where these were not reported, IHD death, fatal MI or cardiac death (in that order) Duration: range 12 to 72 months |
22 per 1,000 | 21 per 1,000 (18 to 24) | RR 0.93 (0.79 to 1.09) | 73,491 (21 RCTs) | ⊕⊕⊕⊝ Moderated | Meta‐analysis and indications of bias suggest risk reduction of less than 7%. Long‐chain omega‐3 fat intake probably makes little or no difference to coronary heart mortality. |
|
Coronary heart disease events – CHD events Assessed with: number of participants experiencing the first outcome in this list reported for each trial: CHD or coronary events; total MI; acute coronary syndrome; or angina (stable and unstable) Duration: range 12 to 72 months |
68 per 1,000 | 63 per 1,000 (59 to 65) | RR 0.93 (0.88 to 0.97) | 84,301 (28 RCTs) | ⊕⊕⊕⊝ Moderatee | Meta‐analysis and indications of bias suggest risk reduction of less than 7%. Long‐chain omega‐3 fat intake probably makes little or no difference to risk of coronary heart events. |
|
Stroke Assessed with: number of participants experiencing at least one fatal or non‐fatal, ischaemic or haemorrhagic stroke Duration: range 12 to 72 months |
20 per 1,000 | 21 per 1,000 (19 to 23) | RR 1.06 (0.96 to 1.16) | 89,358 (28 RCTs) | ⊕⊕⊕⊝ Moderatef | Meta‐analysis and indications of bias suggest increased risk of less than 6%. Long‐chain omega‐3 fat intake probably makes little or no difference to risk of experiencing a stroke. |
|
Arrhythmias Assessed with: number of participants experiencing fatal or nonfatal, new or recurrent arrhythmia, including atrial fibrillation, ventricular tachycardia and ventricular fibrillation. Duration: range 12 to 72 months |
68 per 1,000 | 66 per 1,000 (62 to 72) | RR 0.97 (0.90 to 1.05) | 53,796 (28 RCTs) | ⊕⊕⊕⊝ Moderateg | Meta‐analysis and indications of bias suggest risk reduction of less than 3%. Long‐chain omega‐3 fat intake probably makes little or no difference to risk of arrhythmia. |
|
Harms: bleeding Assessed with: number of participants experiencing bleeding events. Duration: range 12 to 72 months |
8 per 1,000 | 8 per 1,000 (5 to 11) | RR 1.06 (0.73 to 1.52) | 45,562 (8 RCTs) | ⊕⊝⊝⊝ Very lowh | The effect of long‐chain omega‐3 fat intake on bleeding is unclear as the evidence is of very low quality. |
|
Harms: pulmonary embolus or DVT Assessed with: number of participants experiencing pulmonary embolus or deep vein thrombosis Duration: range 18 to 36 months |
5 per 1,000 | 6 per 1,000 (2 to 18) | RR 1.25 (0.41 to 3.78) | 3,011 (4 RCTs) | ⊕⊝⊝⊝ Very lowi | The effect of long‐chain omega‐3 fat intake on pulmonary embolus or DVT is unclear as the evidence is of very low quality. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CHD: coronary heart disease; CI: confidence interval; DVT: deep vein thrombosis; IHD: ischaemic heart disease; MI: myocardial infarction; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aAll‐cause mortality, LCn3
- Risk of bias: effect size moved closer to no effect (RR 1.0) when analysis was limited to studies at low summary risk of bias and low risk of compliance bias (adding weight to the suggestion of little or no effect) but did not alter with fixed‐effect meta‐analysis or results in the analysis limited to larger studies. It was further noted by the WHO NUGAG Subgroup on Diet and Health that although many of the RCTs had issues with blinding, the tendency for lack of blinding is an overestimation of effect. This is less of a concern for this outcome, as the pooled effect was approaching null and not statistically significant. Not downgraded.
- Inconsistency: I2 was < 60% and I2 reduced when analysis was limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries were represented but underrepresented. Not downgraded.
- Imprecision: tight confidence intervals, very large numbers of participants have taken part in RCTs in long‐term studies with consistent results. Given the lack of a statistically significant effect in this very large set of participants, any effect appears too small to be individually relevant. Not downgraded.
- Publication bias: the funnel plot suggested that some small studies with higher numbers of events in the intervention group might be missing. If such missing studies were added back in, the RR would rise. This adds weight to the suggestion of little or no effect. Not downgraded.
bCardiovascular mortality, LCn3
- Risk of bias: effect size moved closer to no effect (RR 1.0) when analysis was limited to studies at low summary risk of bias and low risk of compliance bias (adding weight to the suggestion of little or no effect) but did not alter with fixed‐effect meta‐analysis or results in the analysis limited to larger studies. It was further noted by the WHO NUGAG Subgroup on Diet and Health that although many of the RCTs had issues with blinding, the tendency for lack of blinding is an overestimation of effect. This is less of a concern for this outcome, as the pooled effect was approaching null and not statistically significant. Not downgraded.
- Inconsistency: I2 was < 60% and I2 reduced when analysis was limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: Although very large numbers of participants have taken part in RCTs in long‐term studies, with consistent results, the 95% CI includes the null. Given the lack of a statistically significant effect in this very large set of participants, any effect appears too small to be individually relevant. However, as 95% confidence intervals do not exclude important benefits or harms. Downgraded once.
- Publication bias: the funnel plot suggested that some small studies with higher numbers of events in the intervention group might be missing. If such missing studies were added back in, the RR would rise. This adds weight to the suggestion of little or no effect. Not downgraded.
cCardiovascular events, LCn3
- Risk of bias: effect size moved closer to no effect (RR 1.0) when analysis was limited to studies at low summary risk of bias and low risk of compliance bias (adding weight to the suggestion of little or no effect) but did not alter with fixed‐effect meta‐analysis or results in the analysis limited to larger studies. It was further noted by the WHO NUGAG Subgroup on Diet and Health that although many of the RCTs had issues with blinding, the tendency for lack of blinding is an overestimation of effect. This is less of a concern for this outcome, as the pooled effect was approaching null and not statistically significant. Not downgraded.
- Inconsistency: I2 was < 60% and I2 reduced when analysis was limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries were represented but underrepresented. Not downgraded.
- Imprecision: very large numbers of participants have taken part in RCTs in long‐term studies with consistent results. Given the lack of an important effect in this very large set of participants, any effect appears too small to be individually relevant. However, as 95% confidence intervals do not exclude important benefits or harms, we downgraded once.
- Publication bias: the funnel plot suggested that some small studies with higher numbers of events in the intervention group might be missing. If such missing studies were added back in, the RR would rise. This adds weight to the suggestion of little or no effect. Not downgraded.
dCoronary heart disease mortality, LCn3
- Risk of bias: effect size moved closer to no effect (RR 1.0) when analysis was limited to studies at low summary risk of bias and low risk of compliance bias (adding weight to the suggestion of little or no effect) but did not alter with fixed‐effect meta‐analysis or results in the analysis limited to larger studies. It was further noted by the WHO NUGAG Subgroup on Diet and Health that although many of the RCTs had issues with blinding, the tendency for lack of blinding is an overestimation of effect. This is less of a concern for this outcome, as the pooled effect was approaching null and not statistically significant. Not downgraded.
- Inconsistency: I2 was < 60% and I2 reduced when analysis was limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: very large numbers of participants have taken part in RCTs in long‐term studies with consistent results. Given the lack of a statistically significant effect in this very large set of participants, any effect appears too small to be individually relevant. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded once.
- Publication bias: the funnel plot suggested that some small studies with higher numbers of events in the intervention group might be missing. If such missing studies were added back in the RR would rise. This adds weight to the suggestion of little or no effect. Not downgraded.
eCoronary heart disease events, LCn3
- Risk of bias: effect size moved closer to no effect (RR 1.0) when was analysis limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. However, effect size did not alter with fixed‐effect meta‐analysis or limiting to studies at low risk of compliance bias or larger trials. It was further noted by the WHO NUGAG Subgroup on Diet and Health that there was a significant effect observed in main analysis but the effect moved closer to a non‐significant, null effect when analysis was limited to studies at low summary risk of bias. Downgraded once.
- Inconsistency: I2 was < 60% and I2 reduced when analysis was limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries were represented but underrepresented. Not downgraded.
- Imprecision: 95% CI did not include the null. Not downgraded.
- Publication bias: the funnel plot suggested that some small studies with higher numbers of events in the intervention group might be missing. If such missing studies were added back in, the RR would rise. This adds weight to the suggestion of little or no effect. Not downgraded.
fStroke, LCn3
- Risk of bias: effect size moved closer to no effect (RR 1.0) when analysis limited to studies at low summary risk of bias (adding weight to the suggestion of little or no effect), but did not alter with fixed‐effect meta‐analysis or limiting to larger studies. Limiting to studies at low risk of compliance problems resulted in the suggestion of greater harm. It was further noted by the WHO NUGAG Subgroup on Diet and Health that although many of the RCTs had issues with blinding, the tendency for lack of blinding is an overestimation of effect. This is less of a concern for this outcome, as the pooled effect was approaching null and not statistically significant. Not downgraded.
- Inconsistency: I2 was < 60%. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries were represented but underrepresented. Not downgraded.
- Imprecision: very large numbers of participants have taken part in RCTs in long‐term studies with consistent results. Given the lack of a statistically significant effect in this very large set of participants any effect appears too small to be individually relevant. However, as 95% confidence intervals do not exclude important benefits or harms, we downgraded once.
- Publication bias: the funnel plot did not suggest any small study bias. Not downgraded.
gArrhythmias, LCn3
- Risk of bias: effect size remained similar in most sensitivity analyses, but moved closer to no effect (RR 1.01) when analysis used fixed‐effect meta‐analysis (adding weight to the suggestion of little or no effect) and suggested harm when limited to studies at low summary risk of bias. Not downgraded.
- Inconsistency: I2 was < 60% and I2 reduced when analysis was limited to studies at low summary risk of bias. This adds weight to the suggestion of little or no effect. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries were represented but underrepresented. Not downgraded.
- Imprecision: As 95% confidence intervals do not exclude important benefits we downgraded once.
- Publication bias: funnel plot not interpretable as studies all of a similar size and weight. Not downgraded.
hBleeding, LCn3
- Risk of bias: effect size changed direction (from harmful to protective) when analysis limited to studies at low summary risk of bias. Downgraded once.
- Inconsistency: I2 was < 60%. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries not represented. Not downgraded.
- Imprecision: 95% confidence intervals do not exclude large and important benefits or harms. Downgraded twice.
- Publication bias: insufficient studies for funnel plot. Not downgraded.
iPulmonary embolus or DVD, LCn3
- Risk of bias: effect size suggested greater harm when analysis limited to studies at low summary risk of bias. Downgraded once.
- Inconsistency: I2 was < 60%. Not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. Low‐ and middle‐income countries not represented. Not downgraded.
- Imprecision: 95% confidence intervals do not exclude large benefits or large harms. Downgraded twice.
- Publication bias: insufficient studies for funnel plot. Not downgraded.
Summary of findings 2.
High versus low ALA omega‐3 fats for preventing cardiovascular disease (primary outcomes)
| High versus low ALA omega‐3 fats for preventing cardiovascular disease (primary outcomes) | ||||||
|
Patient or population: adults with or without existing CVD Setting: participants were living at home for most or all of the duration of their trials. Most studies were carried out in high‐income economies (World Bank 2018), but four trials were carried out in upper‐middle income countries (Argentina, Iran, Turkey and China). No studies took place in low‐ or low‐middle income countries. Intervention: higher intake of ALA Comparison: lower intake of ALA The intervention was dietary supplementation, a provided diet or advice on diet. Supplementation may have been in oil or capsule form or as foodstuffs provided, to be consumed by mouth (excluding enteral and parenteral feeds and enemas). The foodstuffs or supplements must have been: refined ALA, linseed (flax), canola (rapeseed), perilla, purslane, mustard seed, candlenut, stillingia or walnut as a food, oil, made into a spreading fat or supplementing another food (such as bread or eggs). For ALA sources the product consumed had to have an omega‐3 fat content of at least 10% of the total fat content. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with lower ALA | Risk with higher ALA | |||||
|
All‐cause mortality – deaths Assessed with: number of participants dying of any cause, whether reported as an outcome or a reason for dropout Duration: range 12 to 40 months |
25 per 1000 | 25 per 1000 (21 to 29) | RR 1.01 (0.84 to 1.20) | 19327 (5 RCTs) | ⊕⊕⊕⊝ Moderatea | Meta‐analysis and sensitivity analyses suggest risk increase of less than 1%. ALA intake probably makes little or no difference to all‐cause mortality. |
|
Cardiovascular mortality – cardiovascular deaths Assessed with: deaths from any cardiovascular cause. Where this was not available cardiac death was used instead where known. Duration: range 12 to 40 months |
12 per 1000 | 12 per 1000 (9 to 15) | RR 0.96 (0.74 to 1.25) | 18619 (4 RCTs) | ⊕⊕⊕⊝ Moderateb | Meta‐analysis and sensitivity analyses suggest risk reduction of less than 5%. ALA intake probably makes little or no difference to cardiovascular mortality. |
|
Cardiovascular events – cardiovascular events Assessed with: number of participants experiencing any cardiovascular event Duration: range 12 to 40 months |
48 per 1000 | 47 per 1000 (39 to 57) | RR 0.95 (0.83 to 1.07) | 19327 (5 RCTs) | ⊕⊕⊝⊝ Lowc | Meta‐analysis and sensitivity analyses suggest risk reduction of 5% to 10%. ALA intake may reduce the risk of cardiovascular events but by a very small amount (from 4.8 to 4.7%). One thousand people would need to consume more ALA to prevent a single person experiencing a CVD event (NNT=1000). |
|
Coronary heart mortality – CHD deaths Assessed with: Coronary deaths, or where these were not reported, IHD death, fatal MI or cardiac death (in that order) Duration: range 12 to 40 months |
11 per 1000 | 10 per 1000 (8 to 14) | RR 0.95 (0.72 to 1.26) | 18353 (3 RCTs) | ⊕⊕⊕⊝ Moderated | Meta‐analysis and sensitivity analyses suggest risk reduction of 5% to 8%. ALA intake probably reduces risk of CHD mortality but by a very small amount (from 1.1 to 1.0%). One thousand people would need to consume more ALA to prevent a single person experiencing a CHD death (NNT=1000). |
|
Coronary Heart Disease – CHD events Assessed with: number of participants experiencing the first outcome in this list reported for each trial: CHD or coronary events; total MI; acute coronary syndrome; or angina (stable and unstable) Duration: range 12 to 40 months |
22 per 1000 | 22 per 1000 (17 to 28) | RR 1.00 (0.82 to 1.22) | 19061 (4 RCTs) | ⊕⊕⊝⊝ Lowe | Meta‐analysis and sensitivity analyses suggest risk reduction of 0% to 9%. ALA intake may make little or no difference to CHD events. |
|
Stroke Assessed with: number of participants experiencing at least one fatal or non‐fatal, ischaemic or haemorrhagic stroke Duration: range 12 to 40 months |
2 per 1000 | 3 per 1000 (2 to 5) | RR 1.15 (0.66 to 2.01) | 19327 (5 RCTs) | ⊕⊝⊝⊝ Very lowf | Meta‐analysis and sensitivity analyses suggest risk increase of −15% to 23%. The effect of ALA intake on stroke is unclear as the evidence is of very low quality. |
|
Arrhythmias – AF, VT, VF Assessed with: number of participants experiencing fatal or nonfatal, new or recurrent arrhythmia, including atrial fibrillation, ventricular tachycardia and ventricular fibrillation Duration: 1 trial of 40 months |
33 per 1000 | 26 per 1000 (19 to 36) | RR 0.79 (0.57 to 1.10) | 4837 (1 RCT) | ⊕⊕⊕⊝ Moderateg | Meta‐analysis and sensitivity analyses suggest risk reduction of 21%. ALA intake probably reduces the risk of arrhythmias a small amount (from 3.3 to 2.6%). 143 people would need to consume more ALA to prevent a single person experiencing an arrhythmic event (NNT=143). |
|
Harms: bleeding Assessed with: number of participants experiencing bleeding events |
The effect of ALA intake on bleeding is unclear as no studies reported this outcome. | |||||
|
Harms: pulmonary embolus or DVT Assessed with: number of participants experiencing pulmonary embolus or deep vein thrombosis Duration: range 24 months |
3 per 1000 | 1 per 1000 (0 to 23) | RR 0.32 (0.01 to 7.80) | 708 (1 study) | ⊕⊝⊝⊝ Very lowh | The effect of ALA intake on pulmonary embolus or DVT is unclear as the evidence is of very low quality. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ALA: alpha‐linolenic acid; CHD: coronary heart disease; CI: confidence interval; DVT: deep vein thrombosis; IHD: ischaemic heart disease; MI: myocardial infarction; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aAll‐cause mortality, ALA
- Risk of bias: there was little or no effect in the main meta‐analysis or when data were limited to RCTs at low summary risk of bias, low risk of compliance problems or larger trials, though a suggestion of increased risk of death with fixed‐effect meta‐analyses. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
bCardiovascular mortality, ALA
- Risk of bias: there was little or no effect in the main analysis, or when data were limited to RCTs at low summary risk of bias, larger trials or fixed‐effect meta‐analysis, though a small benefit was suggested when studies were limited to trials with low risk of compliance bias. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
cCardiovascular events, ALA
- Risk of bias: there was a small effect in the main analysis, with larger trials and in fixed‐effect analysis, and a larger effect when data were limited to RCTs at low summary risk of bias or at low risk from compliance problems. Downgraded once.
- Inconsistency: I2 was <60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
dCoronary heart disease mortality, ALA
- Risk of bias: while ALA reduced CHD mortality by 5% in the main analysis, fixed‐effect analysis and in larger trials, limiting data to RCTs at low summary risk of bias and low risk of compliance problems resulted in 7%‐8% reductions. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded. Downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
eCoronary heart disease events, ALA
- Risk of bias: there was little or no effect in the main analyses, in fixed‐effect meta‐analysis, or in larger studies, but some risk reduction (8 to 9%) when data were limited to RCTs at low summary risk of bias or low risk of compliance bias. Downgraded once.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded. Downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
fStroke, ALA
- Risk of bias: the main analysis, fixed‐effect analysis, and larger trials suggest increased risk of stroke with more ALA, but there was little or no effect when data were limited to RCTs at low summary risk of bias, and a suggestion of benefit when limited to trials with low risk of compliance problems. Downgraded twice.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with CVD risk factors or previous CVD as well as non‐CVD health problems. All studies were conducted in high‐income countries. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies, but only 49 participants experienced strokes. 95% confidence intervals do not exclude important benefits or harms, downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
gArrhythmias, ALA
- Risk of bias: there was a 21% reduction in risk of arrhythmia in the main analysis, when data were limited to RCTs at low summary risk of bias, in larger trials and when data were limited to trials at low risk from compliance. Not downgraded.
- Inconsistency: only one trial, no inconsistency. Not downgraded.
- Indirectness: a single trial, which included adults with previous MI in a high‐income country and only assessed new arrhythmia. Not downgraded.
- Imprecision: large numbers of participants have taken part in this long term study. However, as 95% confidence intervals do not exclude important benefits or harms we downgraded once.
- Publication bias: funnel plot not useful as fewer than 10 trials included. Not downgraded.
hPulmonary embolus or DVD, ALA
- Risk of bias: the single trial was not at low summary risk of bias. Downgraded once.
- Inconsistency: with one trial no inconsistency. Not downgraded.
- Indirectness: healthy men and women, no participants with CVD risk factors or previous CVD; low‐ and middle‐income countries not represented. Not downgraded.
- Imprecision: only one event included in a single trial. Downgraded twice.
- Publication bias: insufficient studies for funnel plot. Not downgraded.
Summary of findings 3.
High versus low omega‐3 fats for modification of CVD risk factors (adiposity and lipids): key outcomes
| High versus low omega‐3 fats for modification of CVD risk factors (adiposity and lipids) | |||||
|
Patient or population: adults with or without existing CVD Setting: participants were living at home for most or all of the duration of their trials. Most studies were carried out in high‐income economies (World Bank 2018), but four trials were carried out in upper‐middle income countries. No studies took place in low‐ or low‐middle income countries. Intervention: higher omega‐3 intake (LCn3 or ALA) Comparison: lower omega‐3 intake (LCn3 or ALA) The intervention was dietary supplementation, a provided diet or advice on diet. Supplementation may have been in oil or capsule form or as foodstuffs provided, to be consumed by mouth (excluding enteral and parenteral feeds and enemas). The foodstuffs or supplements must have been: oily fish; fish oils; linseed (flax), canola (rapeseed), perilla, purslane, mustard seed, candlenut, stillingia or walnut as a food, oil, made into a spreading fat or supplementing another food (such as bread or eggs). For ALA sources the product consumed had to have an omega‐3 fat content of at least 10% of the total fat content. Refined eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) or alpha‐linolenic acids, or concentrated fish or algal oils, were also accepted. | |||||
|
Outcomes All in trials of 12 to 72 months' duration |
Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with low omega‐3 | Risk with high omega‐3 | ||||
| Measures of adiposity – LCn3 – Weight, kg | Mean body weight was 81.2 kg | MD 0.01 kg lower (0.84 lower to 0.82 higher) | 15812 (12 RCTs) | ⊕⊕⊕⊕ Higha | LCn3 intake makes little or no difference to body weight. |
| Measures of adiposity – LCn3 – BMI, kg/m2 | Mean BMI was 27.3 kg/m2 | MD 0.04 higher (0.16 lower to 0.24 higher) | 15234 (14 RCTs) | ⊕⊕⊕⊕ Highb | LCn3 intake makes little or no difference to BMI. |
| Serum total cholesterol – LCn3 – TC, mmol/L | Mean TC was 5.61 mmol/L | MD 0.01 lower (0.05 lower to 0.04 higher) | 37281 (28 RCTs) | ⊕⊕⊕⊝ Moderatec | LCn3 intake probably makes little or no difference to serum total cholesterol. |
| Serum triglyceride, fasting – LCn3 – TG, mmol/L | Mean TG was 1.59 mmol/L | MD 0.24 lower (0.32 lower to 0.17 lower) | 35534 (24 RCTs) | ⊕⊕⊕⊕ Highd | Increasing LCn3 intake reduces serum triglyceride. |
| Serum high density lipoprotein – LCn3 – HDL, mmol/L | Mean HDL was 1.32 mmol/L | MD 0.02 higher (0 to 0.04 higher) | 37237 (27 RCTs) | ⊕⊕⊕⊕ Highe | Increasing LCn3 intake increases serum HDL. |
| Serum low density lipoprotein – LCn3 – LDL, mmol/L | Mean LDL was 3.27 mmol/L | MD 0.01 higher (0.01 lower to 0.03 higher) | 35035 (23 RCTs) | ⊕⊕⊕⊝ Moderatef | LCn3 intake probably makes little or no difference to serum LDL. |
| Measures of adiposity – ALA – Weight, kg | Mean weight was 80.9 kg | MD 0.17 higher (0.61 lower to 0.96 higher) | 664 (4 RCTs) | ⊕⊝⊝⊝ Very lowg | The effect of ALA intake on body weight is unclear as the evidence is of very low quality. |
| Measures of adiposity – ALA – BMI, kg/m2 | Mean BMI was 27.4 kg/m2 | MD 0.12 higher (0.06 lower to 0.3 higher) | 1581 (3 RCTs) | ⊕⊕⊝⊝ Lowh | ALA intake may make little or no difference to BMI. |
| Serum total cholesterol – ALA – TC, mmol/L | Mean TC was 5.02 mmol/L | MD 0.09 lower (0.23 lower to 0.05 higher) | 2164 (6 RCTs) | ⊕⊕⊝⊝ Lowi | ALA intake may make little or no difference to serum total cholesterol (low‐quality/certainty evidence). |
| Serum Triglyceride, fasting – ALA – TG, mmol/L | Mean TG was 1.48 mmol/L | MD 0.03 lower (0.11 lower to 0.05 higher) | 1776 (6 RCTs) | ⊕⊕⊕⊝ Moderatej | ALA intake probably makes little or no difference to serum triglycerides (moderate‐quality/certainty evidence). |
| Serum high density lipoprotein – ALA – HDL, mmol/L | Mean HDL was 1.49 mmol/L | MD 0.02 lower (0.08 lower to 0.03 higher) | 1776 (6 RCTs) | ⊕⊕⊕⊝ Moderatek | ALA intake probably reduces serum HDL. |
| Serum low density lipoprotein – ALA – LDL, mmol/L | Mean LDL was 2.88 mmol/L | MD 0.05 lower (0.15 lower to 0.04 higher) | 2201 (7 RCTs) | ⊕⊕⊝⊝ Lowl | ALA intake may make little or no difference to serum LDL. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BMI: body mass index; CI: confidence interval; HDL: high‐density lipoprotein; LCn3: long‐chain omega‐3 fatty acids; LDL: low‐density lipoprotein; MD: mean difference; RCT: randomised controlled trial; TC: total cholesterol; TG: triglycerides. | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
aMeasures of adiposity, weight, LCn3
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were underrepresented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals exclude important benefits or harms. Not downgraded.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
bMeasures of adiposity, BMI, LCn3
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were underrepresented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals exclude important benefits or harms. Not downgraded.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included. Not downgraded.
cLipids, serum total cholesterol, LCn3
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: when we ran fixed‐effect analysis, a statistically significant effect was suggested. The 95% CI included null but excluded important benefits or harms. Downgraded once..
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
dLipids, serum triglycerides, LCn3
- Risk of bias: there was a statistically significant effect overall and in all sensitivity analyses, including when data were limited to RCTs at low summary risk of bias. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals exclude harms. Not downgraded.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
eLipids, HDL, LCn3
- Risk of bias: the suggested increase in HDL with increased LCn3 was apparent in all sensitivity analyses. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals exclude harms. Not downgraded.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
fLipids, LDL, LCn3
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals included the null but excluded important benefits or harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
gMeasures of adiposity, weight, ALA
- Risk of bias: no included trials were at low summary risk of bias. Downgraded once.
- Inconsistency: I2 was > 60%, downgraded once.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals include some benefits or harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
hMeasures of adiposity, BMI, ALA
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was > 60%, downgraded once.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% confidence intervals include some benefits and harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
iLipids, serum total cholesterol, ALA
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was > 60%. Downgraded once.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: when we ran fixed‐effect analysis a statistically significant effect was suggested, but main analysis includes some benefits and harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
jLipids, serum triglycerides, ALA
- Risk of bias: there was little or no effect in the main analysis or in any sensitivity analysis. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% include benefits and harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
kLipids, HDL, ALA
- Risk of bias: there was a statistically significant effect with fixed effects analysis and when data were limited to RCTs at low summary risk of bias, but the main analysis and other sensitivity analyses also suggested reductions om HDL. Not downgraded.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: large numbers of participants have taken part in RCTs in long‐term studies with consistent results. 95% CI includes benefits and harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
lLipids, LDL, ALA
- Risk of bias: apparent effect altered from slight benefit to slight harm when data were limited to RCTs at low summary risk of bias. Downgraded once.
- Inconsistency: I2 was < 60%; not downgraded.
- Indirectness: representative, generalisable adult population including men and women, including healthy participants and participants with previous CVD. However, low‐ and middle‐income countries were not represented. Not downgraded.
- Imprecision: when we ran fixed‐effect analysis a statistically significant effect was suggested. For main analysis 95% CI included benefits and harms. Downgraded once.
- Publication bias: funnel plot was not interpretable, no clear small study bias. However, we are aware of several studies whose data could not be included; not downgraded.
Background
Description of the condition
Cardiovascular diseases (CVDs) are disorders of the heart and blood vessels. They include cerebrovascular disease (including stroke and transient ischaemic attack), coronary heart disease (including heart attack or myocardial infarction and angina), peripheral arterial disease (diseases of the blood vessels to the arms and legs), deep vein thrombosis and pulmonary embolism (blood clots formed in the legs which can move to the heart and lungs), as well as rheumatic and congenital heart disease (WHO 2017); these last two are not discussed in this review. Globally, 31% of all global deaths are due to CVD, more than from any other cause (WHO 2017). Of the 17.7 million people who died from CVDs in 2015, 7.4 million were due to coronary heart disease and 6.7 million due to stroke. Of 17 million premature deaths in 2015 caused by non‐communicable diseases, 82% were in low‐ and middle‐income countries, and 37% were caused by CVDs (WHO 2017).
Description of the intervention
Omega‐3 fats (also called Ω3 or n‐3 fats) from fish sources include eicosapentaenoic acid (EPA, or 20:5), docosahexaenoic acid (DHA, 22:6) and docosapentaenoic acid (DPA, 22:5), the longer chain omega‐3 fats (LCn3). Alpha‐linolenic acid (ALA or α‐linolenic, 18:3) is the shorter chain omega‐3 fat found in plants and grass‐fed, which is partially converted to longer chain omega‐3 fatty acids within our bodies. There is some debate about the effectiveness of this conversion, which may differ depending on whether it is assessed over the short or long term as well as on other dietary factors (Li 1999; Pawlosky 2001). For this reason the effectiveness of ALA may differ from that of the longer chain omega‐3 fats.
Since Bang and colleagues first suggested that the abundance of omega‐3 fatty acids in the diet of the Greenland Inuit people was responsible for their low mortality from ischaemic heart disease (Bang 1972; Bang 1976), there has been considerable interest in the protective role and possible mechanism of action of marine unsaturated fats. This interest has spread to encompass plant seeds and oils rich in omega‐3 fatty acids, including chia seed, flax (linseed) and rapeseed (canola) oils (Nettleton 1991), their derivatives (e.g. margarines), purslane leaves (Simopoulos 1992), and nuts (especially walnuts).
How the intervention might work
Proposed mechanisms for the protective role of omega‐3 fats against cardiovascular diseases include: lowering the blood pressure; altering the lipid profile, especially reduced serum triglyceride concentration; modulating arterial lipoprotein lipase levels; reducing thrombotic tendency; producing anti‐inflammatory effects and anti‐arrhythmic effects; improving vascular endothelial function and insulin sensitivity; and increasing plaque stability and paraoxonase levels (Bhatnagar 2003; BNF 1999; Calabresi 2004; Chang 2013; Geelen 2004).
Given that most omega‐3 fats are ingested in the form of oily fish or fish oil (often fish liver) capsules, reports of high levels of various toxic compounds such as mercury, dioxins and polychlorinated biphenyls (PCBs) in oily fish and fish oils are concerning (FSA 2000; Liem 1997; MAFF 1998A; USFDA 1995). These are all fat soluble and accumulate over time in the body, so harms may be exhibited only after long‐term fish consumption or supplementation with fish oils. Animal intervention studies and human cohorts who have suffered accidental exposure to dioxins and PCBs suggest that pre‐natal exposure may cause sub‐fertility problems, and adult exposures may lead to an excess of total cancers (JECFA 2001). Human cohorts exposed to high levels of mercury exhibit neurological problems (USFDA 1995). As many people eat oily fish once or twice a week or take fish oil supplements, it is important to explore the potentially harmful effects of fish‐associated omega‐3 intake. It is also possible that omega‐3 fats themselves may exhibit harm, for example through extension of bleeding times or suppression of normal immune responses (USFDA 2000).
Cardiovascular effects of eating more oily fish may differ from those of taking a fish oil supplement because fish (not fish oil) is a rich source of nutrients including selenium, iodine, zinc, calcium and protein. Fish in the diet may also displace a variety of other foods including sources of saturated or trans fats, so it could alter CVD in other ways.
Why it is important to do this review
There is a great deal of public belief in the cardiovascular benefits of omega‐3 fats. Analysis of US National Health and Nutrition Examination Survey data from 2003 to 2008 suggests that in the USA, adults' mean long‐chain omega‐3 intakes were greater from dietary supplements (0.72 g/d EPA and DHA) than from foods (0.41 g/d, Papanikolaou 2014). But public health advice differs across countries. For example, the National Institute for Health and Clinical Excellence in the UK now encourages fish intake but discourages supplementation: "people with or at high risk of CVD should be advised to consume at least 2 portions of fish per week, including a portion of oily fish". However, it advises that omega‐3 fatty acid compounds "should not be offered for primary or secondary prevention of CVD" (NICE 2016). The American Heart Association (AHA) also "recommends eating fish (particularly fatty fish) at least two times (two servings) a week". Although the AHA suggests that omega‐3 intake via foods is preferable, the AHA is more positive about omega‐3 supplements: "those with coronary artery disease may not get enough omega‐3 by diet alone. These people may want to talk to their doctor about supplements. And for those with high triglycerides, even larger doses could help" (AHA 2016). These recommendations are balanced with a warning about potential excessive bleeding in those taking doses of > 3 g/d omega‐3 fatty acids (presumably long‐chain omega‐3 fats). Such recommendations, and resulting increased fish consumption, have potentially negative long‐term consequences for our marine ecosystems (Brunner 2009).
Epidemiological studies have supported the relationship between high omega‐3 intake and lower cardiovascular disease (CVD) rates (Ballard‐Barbash 1987; Burr 1993; Kris‐Etherton 2002). However, these associations could be due to some other characteristic of people who choose to eat fish. In many societies eating fish is associated with better social status and a health‐conscientious life view (Cade 2007), so eating fish is highly confounded by dietary quality, socioeconomic status and other markers of healthy lifestyles. As an example, the global attributable burden of eating a diet low in seafood omega‐3 fats was estimated as 1.1% of global disability‐adjusted life‐years (DALYs; 95% CI 0.8 to 1.5), "with 22% of ischaemic heart disease DALYs attributable to low seafood intake" (Engell 2013). The data sources are not described, but when the estimate was derived from RCTs alone, rather than cohort studies and RCTs combined, the estimated global attributable burden was much smaller, 0.5% (95% CI −0.5 to 1.4). Information concerning cause and effect is more reliably supplied by intervention trials in which participants are randomly allocated to receive fish oil or advice to eat more fish.
Systematic reviews of randomised controlled trials (RCTs) have had various findings. An earlier version of this review found no effects for omega‐3 fats on all‐cause mortality or cardiovascular outcomes in trials of at least six months' duration (which included > 36,000 participants) (Hooper 2004). Since Hooper 2004 was published, several other systematic reviews have suggested a lack of effect for omega‐3 fats on all‐cause mortality or a variety of CVDs (Campbell 2013; Chowdhury 2012; Khoueiry 2013; Kotwal 2012; Kwak 2012; Mariani 2013; Rizos 2012; Zheng 2014). However, others have highlighted particular outcomes or circumstances in which CVD prevention was evident: after heart surgery (He 2013), for preventing sudden cardiac death (Zhao 2009), for reducing CVD mortality and sudden cardiac death (although with no effect on all‐cause mortality) (Trikalinos 2012), for CVD mortality (Sethi 2016), and for reducing the risk of stroke in women (albeit with no effect on stroke overall) (Larsson 2012). Kwak 2012 reported marginal effects on cardiovascular death, though these were lost when a poor‐quality trial was removed, and a few others have reported only positive effects in their abstracts (reductions in cardiovascular events, cardiac death and coronary events) (Delgado‐Lista 2012). These disparate findings have fuelled both debate and confusion. A recent extensive Agency for Healthcare Research and Quality review meta‐analysed risk factors extensively but suggested there was only limited RCT data to assess the effects of omega‐3 fats on clinical CVD outcomes (Balk 2016).
This systematic review and meta‐analysis aimed to assess the evidence on the effects of omega‐3 fats (long‐chain and ALA separately) on all‐cause mortality and CVDs. It also aimed to assess potentially harmful effects of omega‐3 fats or compounds associated with consuming long‐chain omega‐3 fats such as excessive bleeding. A related review has formally systematically reviewed potential harms such as excessive cancers, rather than simply examining studies included in this review for cancer outcomes (Hanson 2017b). We assessed mechanisms of action such as lipid and body weight changes and antiarrhythmic effects as primary or secondary outcomes in this review, and we have systematically reviewed these outcomes in a formal way by including trials that assessed adiposity, lipids and arrhythmic events even where no CVD events occurred or were reported. Sister systematic reviews have assessed anti‐inflammatory effects and effects on inflammatory bowel disease (Thorpe 2017), as well as effects on insulin sensitivity and glucose metabolism (Brown 2017).
The World Health Organization (WHO) is currently updating its guidance on polyunsaturated fatty acid intake in adults and children. The update and expansion of this review was commissioned by WHO in order to inform and contribute to the development of updated WHO recommendations. The results of this review including GRADE assessments were discussed and reviewed by the WHO Nutrition Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health as part of WHO’s guideline development process.
Objectives
To assess the effects of increased intake of fish‐ and plant‐based omega‐3 for all‐cause mortality, cardiovascular (CVD) events, adiposity and lipids.
The primary review question was, 'Do long‐chain omega‐3 (LCn3, fish‐based omega‐3 fats) or ALA (plant‐based omega‐3 fats) fats alter risk of all‐cause mortality, cardiovascular deaths, cardiovascular events, coronary heart disease deaths, coronary heart disease events, stroke, arrhythmia, adiposity and lipids?'
Secondary questions include the following.
-
If omega‐3 fatty acids confer protection:
does protection occur equally in those at low and at high risk of cardiovascular disease?
does protection depend on the dose of omega‐3 fats taken per day?
do effects differ between dietary and supplemental omega‐3 sources?
does protection depend on study summary risk of bias?
Is protection or harm stronger with longer trial duration?
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled clinical trials that included diet advice or dietary supplementation to promote omega‐3 fatty acid intake versus placebo, no supplementation, usual diet or lower dose omega‐3. One of our outcomes had to be measured and available (through publications or contact with authors), and trials had to follow participants for at least 12 months (52 weeks or 360 days) for mortality and cardiovascular outcomes. For advice trials, follow‐up must have been at least 12 months following advice, and for trials where participants received food or supplementation, provision must have continued for at least 12 months). We accepted randomisation of individuals or of clusters as long as there were at least six clusters randomised.
Careful work by Browning suggests that supplements of EPA and DHA equivalent to one weekly portion of oily fish results in 95% of maximal incorporation by 5 days for EPA in plasma phosphatidylcholine (95% CI 0 to 18 days) to 273 days for DHA into blood mononuclear cells (95% CI 0 to 670 days) (FISH 2012). While this suggests individual variability, on average all compartments except blood mononuclear cells had equilibrated by 117 days (both EPA and DHA into plasma phosphatidylcholine, plasma cholesteryl esters, plasma nonesterified fatty acids, plasma triglycerides, erythrocytes and platelets). The authors stated "EPA and DHA reached a maximum in platelets in 3–4 weeks and 1–2 months, respectively, and in blood mononuclear cells in 6–9 months". For this reason we chose 12 months as the minimum duration of intervention, as it allows equilibration of most body compartments with EPA and DHA as well as time for this change in body composition to have some effect on cardiovascular risk or mortality.
In previous reviews of dietary effects on cardiovascular outcomes, we limited trials to at least two years' duration (Hooper 2015), as the proposed mechanism of effects was via LDL cholesterol, atherosclerosis and its sequelae, and this takes time to develop. The 4S trial showed separation of the survival curves at around two years (Scandinavian Simvastatin Survival Study Group 1994). Potential mechanisms for effects of polyunsaturated fatty acids (PUFAs) are broader, including what could be rapid effects on arrhythmias or inflammation, so we decided to include trials of at least 12 months to ensure we did not miss these effects.
Types of participants
Studies in adults (18 years or older, men and/or women) at any risk of cardiovascular disease (with or without existing cardiovascular disease) were eligible, including those in participants with increased risk of cancer, those undergoing or who have undergone coronary artery bypass grafting or angioplasty, and those with current or previous cardiovascular disease, nephritis in systemic lupus erythematosus, breast cysts, diabetes mellitus, rheumatoid arthritis, multiple sclerosis, psoriasis, hay fever, asthma or ulcerative colitis. Including these populations allows us to understand both development and progression of cardiovascular disease (primary and secondary prevention). We excluded participants who were pregnant or acutely ill (with acute‐stage cancer, undergoing heart or renal transplantation, with HIV or AIDS, on haemodialysis, with IgA glomerulonephritis, or any other renal problem except in diabetes).
Types of interventions
The intervention must have been dietary supplementation, a provided diet or advice on diet. The foodstuffs or supplements must have been: oily fish (including mackerel, dogfish, salmon, herring, trout, tuna, sturgeon, stablefish, anchovy, sprat, coho, capelin, sardines, swordfish, sild, pilchard, brisling, menhaden, bloater, whitebait, crab and conger eel); fish oils (made from any of the above or a mixture of fish, or cod liver oil); linseed (flax), canola (rapeseed), perilla, purslane, mustard seed, candlenut, stillingia or walnut as a food, capsule, oil, made into a spreading fat or supplementing another food (such as bread or eggs). For ALA sources the product consumed had to have an omega‐3 fat content of at least 10% of the total fat content. Refined eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) or alpha‐linolenic acids, or concentrated fish or algal oils, were also accepted. Supplementation may have been in oil or capsule form or as foodstuffs provided to be consumed by mouth (excluding enteral and parenteral feeds and enemas).
We excluded studies using multiple risk factor interventions on lifestyle factors (such as weight reduction, smoking or physical activity goals), or differential dietary interventions not involving dietary fats, except where that other intervention was a direct replacement for polyunsaturated fats or the effect of diet or supplementation could be separated out from the other interventions.
Studies were eligible if they compared the effect of dietary advice or supplementation to increase omega‐3 fats with the usual diet, no advice, no supplementation, placebo or lower dose omega‐3.
Types of outcome measures
Primary outcomes
Primary outcomes included numbers of participants experiencing:
all‐cause mortality (deaths);
cardiovascular mortality (cardiovascular deaths);
cardiovascular events (cardiovascular events);
coronary heart disease mortality (CHD deaths);
coronary heart disease events (CHD events);
stroke; and
arrhythmia (atrial fibrillation).
We analysed coronary heart disease using the first of the following to be reported: number of participants experiencing CHD or coronary events, total myocardial infarction (MI), acute coronary syndrome or angina (stable and unstable). This meant that if trialists reported CHD events, we used these in analysis and ignored the other outcomes; where trials did not report CHD events but did report total MI, we used that (and so on). Combined cardiovascular events included fatal and non‐fatal myocardial infarction, angina, stroke, heart failure, peripheral arterial disease, sudden death and non‐scheduled cardiovascular interventions – coronary artery bypass surgery or angioplasty. We included all available outcomes where we could be sure that the same participant was not being counted twice.
At the request of WHO NUGAG Subgroup on Diet and Health, we added CHD mortality post hoc as a primary outcome. Data used were the first of the following list reported: coronary death, ischaemic heart disease (IHD) death, fatal MI, cardiac death. We only used cardiac death when no other outcomes in this category were available, and we ran a sensitivity analysis omitting cardiac death. The reason for excluding cardiac death in sensitivity analysis was that it goes slightly outside our area of interest, including other causes of death in addition to CHD, such as cardiomyopathies and congenital and valvular heart diseases. We wanted to include cardiac death in the main analysis as we felt that otherwise we would be missing some important cases of coronary heart mortality, but we decided to exclude it in sensitivity analysis as we were potentially including a few outcomes that CHD mortality did not encompass.
Secondary outcomes
Secondary outcomes included:
major adverse cerebrovascular or cardiovascular events (MACCEs) or individual cardiovascular events (total, fatal or non‐fatal MI, sudden cardiac death, angina, heart failure, revascularisation, peripheral arterial disease or acute coronary syndrome);
body weight and other measures of adiposity; and
lipids (total, LDL or HDL cholesterol and triglycerides).
We defined MACCEs as participants experiencing MI, unstable angina, stroke or death. We did not consider studies that did not provide data on all these health events for this outcome.
The review included studies if any of their participants experienced or were assessed for any primary or secondary outcome. These could have been reported in publications (as outcomes or reasons for dropout or adverse events), supplied by study authors, or which clearly happened even if exact numbers were not available. However, as almost all trials note if a death or cardiovascular event occurs in a study participant (so ALL trials assess for our primary outcomes) we only included trials where at least one event occurred, or where a continuous outcome was measured.
Tertiary outcomes
We extracted the following outcomes where available within included studies.
Blood pressure.
Serious adverse events (any other reported illnesses).
Side effects.
Dropouts.
Quality of life measures.
Economic costs.
We originally intended to assess type 2 diabetes diagnoses, measures of glucose metabolism, cancers, breast cancer, neurocognitive outcomes such as dementia, depression and anxiety within included studies. However, as part of the larger set of reviews we formally systematically reviewed effects of omega‐3 fats on type 2 diabetes diagnoses and measures of glucose metabolism (Brown 2017), cancers including breast cancer (Hanson 2017b), neurocognitive outcomes such as dementia (Jimoh 2017), irritable bowel disease (IBD) and inflammatory factors (Thorpe 2017), depression and anxiety (Hanson 2017a), and functional outcomes (Abdelhamid 2017), so a partial assessment within this review would be unhelpful and potentially misleading. For this reason we exclude these specific outcomes from our reporting of serious adverse events.
Key outcomes
When the World Health Organization (WHO) Nutrition Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health requested this review update they named the following as key outcomes to inform their planned dietary guidance.
All‐cause mortality.
CVD mortality.
CVD events.
CHD mortality.
CHD events.
Stroke.
Arrhythmia (atrial fibrillation).
Serum lipids including total cholesterol (TC), fasting triglycerides (TG), high‐density lipoprotein (HDL) and low‐density lipoprotein (LDL).
Measures of adiposity (body weight and body mass index).
We were not able to make all of these outcomes into primary outcomes. However, because WHO NUGAG Subgroup on Diet and Health will use these outcomes to underpin guidance, we carried out sensitivity analyses, subgroup analyses and GRADE assessment of quality of evidence for them, even when they were not primary outcomes.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases on 27 April 2017 to identify reports of relevant randomised clinical trials.
Cochrane Central Register of Controlled Trials (CENTRAL; 2017; Issue 3) in the Cochrane Library.
Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, MEDLINE Daily and MEDLINE (Ovid, 1946 to 27 April 2017).
Embase Classic and Embase (Ovid, 1947 to 2017 week 17).
We applied date limits to the terms from the original strategies so that the search included only new records, but we did not apply any date limits to newly added terms. Appendix 1 shows the MEDLINE search strategy for the original version of this review, and Appendix 2 shows the updated searches. We de‐duplicated the results against each other. The RCT filter for MEDLINE was the Cochrane sensitivity and precision‐maximising RCT filter, and for Embase, we applied the terms as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
As we were also running searches for a new systematic review of the effects of polyunsaturated fats on cardiovascular disease (Abdelhamid 2018), as well as updating and extending a Cochrane Review of the effects of omega‐6 polyunsaturated fats on health outcomes (Hooper 2018), we also ran searches for these reviews using the same RCT filters (Appendix 3). The results of these searches were de‐duplicated against the omega‐3 searches, and all the titles and abstracts assessed as a single set for all three reviews. We created a dataset of RCTs that lasted at least six months and compared higher versus lower omega‐6, omega‐3 or total polyunsaturated fatty acids (PUFA) in adults. We used this dataset as the wider study pool from which we selected included studies for all reviews (Abdelhamid 2018; Abdelhamid 2017; Hooper 2018; Brown 2017; Hanson 2017a; Hanson 2017b; Jimoh 2017; Thorpe 2017; Hooper 2004).
We searched two trials registers, ClinicalTrials.gov (clinicaltrials.gov) and the WHO International Clinical Trials Registry Platform (ICTRP, www.who.int/ictrp/en) on 23 September 2016 for registry entries for relevant completed and ongoing studies.
Searching other resources
We assessed titles and abstracts retrieved during these electronic searches for relevant RCTs and also relevant systematic reviews. We handsearched the included studies in all relevant systematic reviews for new trials and additional publications of included trials.
We contacted authors of all large included studies (at least 100 participants) and some smaller trials for further study data, methodological details and references to studies not yet identified, including published, unpublished or ongoing studies.
Data collection and analysis
Selection of studies
At least two reviewers independently assessed titles and abstracts resulting from the electronic and bibliographic searches. We combined the search results for this review and two others, Abdelhamid 2018and Hooper 2018, de‐duplicating and assessing them at the same time. We rejected titles and abstracts on initial screen only if the reviewer could determine from the title and abstract that the article was not a report of a randomised controlled trial; did not address omega‐3 intake (or total polyunsaturated fat or omega‐6 fat for the other two reviews); were exclusively in children or young adults (less than 18 years old), pregnant women or the critically ill; were of less than 12 months' duration; or if the intervention was multi‐factorial and we could not separate out the effect of dietary fat.
We rejected studies only when it was certain that no primary or secondary outcome events occurred, and none of the secondary outcome risk factors were measured. When we could not reject a title/abstract with certainty, we obtained the full text of the article for further evaluation. We made attempts to obtain full‐text translations and/or evaluations of all potentially relevant non‐English articles.
We used an in/out form to assess full‐text papers and studies for inclusion (or otherwise) into the review. We contacted the authors of all potentially included RCTs for further information on trial methodology and outcomes. Two assessors independently decided on inclusion of full‐text RCTs, resolving any differences by discussion and, when necessary, in consultation with the review team.
Data extraction and management
We designed a data extraction form for this review, which each of the reviewers tested on a common 'training' study (SCIMO 1999), and we adapted it as appropriate. We extracted data concerning participants, interventions, and outcomes, as described above in the selection criteria section. We extracted dichotomous data from dietary advice studies at the latest point available in the trial (regardless of the amount of reinforcement of the original dietary message), while for supplement studies, we extracted dichotomous data to the point that supplementation or the trial ended, whichever was earlier. We extracted continuous data at the nearest time point to 12 months and also the latest point available in fixed‐term trials, but in studies where participants were followed up for varying durations (aside from dropouts), we extracted the participants' data from the first time point following the mean trial duration. We never used data from periods following the end of a trial in meta‐analysis.
We also extracted data on risk of bias, assessed using the Cochrane 'Risk of bias' tool, along with data on potential effect modifiers, including existing cardiovascular disease (primary or secondary prevention), trial duration, intensity of intervention (dietary advice, diet provided, supplemental foods, supplements (capsules) and any combination), long‐chain omega‐3 fats or ALA and dose, replacement, medications used (including statins, antihypertensive, antiarrhythmic or antithrombotic medication), fatty acid data (from plasma, platelets or adipose tissue) and smoking status.
For primary and secondary dichotomous outcomes, we extracted numbers of participants experiencing an outcome and total numbers of participants randomised (or in whom the outcome was assessed where known) for each study arm. For continuous outcomes, we extracted the number of participants assessed, means and standard deviations of the final readings in each treatment arm; we calculated standard deviations from other variance data where appropriate. Where data were available on both change and final readings, we used data on change.
Two reviewers independently extracted original reports of trial results. We resolved differences between reviewers' results by discussion and, when necessary, in consultation with a third reviewer or the review team.
Assessment of risk of bias in included studies
Two reviewers independently assessed risk of bias for each included study, using Cochrane criteria (Higgins 2011), including in the domains of sequence generation; allocation concealment; blinding of participants and personnel, blinding of outcome assessors; incomplete outcome data; and selective outcome reporting. Additional review‐specific criteria included similarity of type and intensity of intervention in both arms (attention) and evidence of appropriate moderate to high compliance (to establish that the intervention group were receiving a different intake of omega‐3 fats than the control group). Table 10 presents specific details of how we interpreted these criteria for this review.
Table 1.
Risk of bias assessment methods in greater detail
| Risk of bias element | Criteria for low risk of bias | Criteria for unclear | Criteria for high risk of bias |
| Selection bias: random sequence generation | The study authors needed to have described the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups. For example "the randomisation sequence was computer generated". We allowed that a good method of randomisation was strongly implied if the authors discussed stratification and/or blocking. Therefore, if the authors were not explicit about their randomisation method but did describe stratification or blocking we assessed this as corresponding to low risk. | The study authors have not described their method in sufficient detail for the assessment of whether it would produce comparable groups. For example, the authors state "the trial was randomised" and provide no further information. | The randomisation method was assessed as not truly random, and may not produce comparable groups. |
| Selection bias: allocation concealment | The study authors needed to have described the method used to conceal allocation sequence in sufficient detail to determine whether the allocations could have been foreseen in advance of, or during, enrolment. Good methods included putting allocation codes in opaque sealed envelopes (ideally prepared by someone outside the treatment or assessment teams and sequentially numbered), using a telephone allocation system after the participants had consented to participate or providing a random number that links to a specific set of capsules prepared and distributed centrally or by an arms‐length pharmacist. | The authors gave insufficient detail as to method. | The allocation was known in advance of participants consenting to take part in the study. |
| Performance bias: blinding of participants and personnel | The study authors needed to have described all measures used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. Ideally, they should also have provided information relating to whether the intended blinding was effective. For example, the authors could say "both the intervention and placebo capsules looked and tasted the same." However, if the study authors did not provide information on whether the blinding was effective, but sufficient detail was given on a good method of blinding, then it was assumed that the blinding was effective and the risk of bias was low. | Insufficient methodological details were provided e.g. "the study was blinded." | The study was unblinded or where blinding was broken, e.g. "the capsules were visually identical but the participants reported a strong fishy flavour in the intervention group only." |
| Detection bias: blinding of outcome assessment | Study authors needed to have described measures used, if any, to blind outcome assessors from knowledge of which intervention a participant received. Ideally, they should also have provided information relating to whether the intended blinding was effective. For example, the authors could say "the outcome assessors had no knowledge of the group allocation, and both the intervention and placebo capsules looked and tasted the same so the self‐assessment scales were also blinded." However if the study authors did not provide information on whether the blinding was effective, but sufficient detail was given on a good method of blinding of the assessors, then it was assumed that the blinding was effective and the risk of bias is low. All biochemical assessment (lipids, glucose, CRP, insulin, PSA, etc.) were considered at low risk of detection bias if outcome assessor blinding or double blinding was stated. | Insufficient methodological details were provided e.g. "the study was blinded." | The study was unblinded or blinding was broken, e.g. for a self‐assessment measure "the capsules were visually identical but the participants reported a strong fishy flavour in the intervention group only." Because the level of blinding could vary by outcome assessment of risk of bias was based on blinding of the review's primary outcome(s). Where primary outcomes had different assessments we opted for the higher risk of bias but noted that that risk of bias was lower for other outcomes. |
| Attrition bias: incomplete outcome data | The study authors needed to describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. They needed to report the number of attrition/exclusions, the numbers in each group at each time point, reasons for attrition/exclusion and any re‐inclusions in analyses. Ideally, they would report how they imputed any missing data e.g. last observation carried forward. There needed to be a reasonable balance of attrition/exclusions between study arms and ≤ 20% of the sample should be lost over a year. | The authors didn't state reasons for attrition/exclusion, or were unclear about the numbers lost to attrition/exclusion in each study arm. | The authors demonstrated a substantial difference in the rates of attrition/exclusions between the study arms and/or > 20% of the baseline sample was lost over a year (> 10% over 6 months). |
| Reporting bias: selective outcome reporting | The study authors needed to have published their trial protocol or trials registry entry before the end of the study's recruitment period i.e. prospectively. They needed to have reported on all of the primary and secondary outcomes listed in the protocol/registry entry. Reporting additional secondary outcomes in the results paper(s), although not ideal, was deemed to still be low risk. | No trial protocol or trials registry entry was found, it was registered retrospectively, or the dates of registration and participant recruitment were unclear. | The study authors did not report at least one primary or secondary outcome listed in the protocol/registry entry or the results paper(s) reported a primary outcome that was not listed at all in the protocol or not listed as a primary outcome in the protocol. |
| Other sources of bias: attention bias | The study authors needed to have reported that participants in all study arms received the same amount of attention and time from researchers and clinical teams. For example, "All participants attended the clinic for a baseline assessment which took 2 hours. They were then followed with monthly telephone calls, and finally attended for a 6 month assessment at the clinic which took 1 hour." If the study only differed by the content of the capsules, and the assessment schedule was not stated to differ between the two arms, it was assumed to be at low risk. | The authors did not state the attention each arm received. | Participants in different arms received different amounts of attention. For example "the intervention group only attended for additional assessments at months 2, 4, and 6" or "the rates of relapse differed substantially between the groups which led to differing amounts of treatment time and attention," or "the intervention group received a 40 minute dietary education session." |
| Other sources of bias: limited compliance | The study authors needed to have reported on the level of compliance in all arms in sufficient detail to determine whether the study results were robust. We followed a flow chart to make this determination. A statistically significant difference between the intervention and control groups in a body measure of at least 50% of the text fatty acids. Where no body measures were reported then estimated compliance needed to be greater than 64% (proportion complying multiplied by compliance threshold). | Compliance not reported or not in a way that could be interpreted. | Measures of compliance were reported but fell below the appropriate thresholds. |
| Other sources of bias: other | In the absence of any additional issues this item was coded "low risk of bias" | — | If fraud concerns had been raised and the paper had been withdrawn, or the author had been found guilty of fraud by a legal or medical entity the paper was excluded from the review. However if fraud concerns were raised, but the journal had not withdrawn the paper, and the author had not been formally sanctioned; then the study was included in the review, but concerns were raised here, and the risk of bias for this item was high. |
CRP: C‐reactive protein; PSA: prostate specific antigen.
We considered a study to be at low risk of attention bias when participants were given the same amount of time and attention from study staff and health professionals whether they were in the intervention or control arms, and at low risk of compliance bias when adherence was assessed, results of that assessment were clearly reported for both intervention and control arms, and where most participants appeared to have taken at least 75% of the intended PUFA dose.
Summary risk of bias
Schulz 1995 found that poorly concealed allocation was associated with a 40% greater effect size, so randomisation and allocation concealment are core issues for all trials. Lack of blinding is associated with bias, though smaller levels of bias than lack of allocation concealment (Savovic 2012), especially in studies with objectively measured outcomes (Wood 2008), such as those we primarily used in our review. Although we originally planned to assess summary risk of bias for all included trials in the same way across this review, the omega‐3 review and the total PUFA review (Abdelhamid 2018; Hooper 2018; Hooper 2004), we adopted a different approach after discussing the different nature of supplement trials compared to dietary advice or food provision trials with the WHO NUGAG Subgroup on Diet and Health.
We considered supplement or capsule type trials to be at low summary risk of bias where we judged randomisation, allocation concealment, blinding of participants and personnel, and blinding of outcome assessors to be adequate. We considered all other trials to be at moderate or high risk of bias (a single category).
We considered dietary advice or all‐food‐provided type trials to be at low summary risk of bias where we judged randomisation, allocation concealment, and blinding of outcome assessors to be adequate. We considered all other trials to be at moderate or high risk of bias (a single category).
Measures of treatment effect
We pooled dichotomous data using risk ratios (RR) to describe effect sizes and continuous data using mean differences (MD). Where effects were described by different but comparable measures or scales in different studies, we combined them using standardised mean difference (SMD).
Unit of analysis issues
We considered that we could reduce patient numbers in cluster‐randomised trials to an effective sample size, as described by Hauck 1991; however, we identified no such trials. For combined outcomes (e.g. combined cardiovascular events), we made attempts to add numbers of individuals experiencing specific outcomes within studies, but only where we could be certain that we were not counting individual participants more than once within any one of our review outcome categories.
For studies with intervention arms providing different omega‐3 doses, we combined data for the intervention groups for binary outcomes and used data on higher dose data versus control for continuous outcomes. We used arms with different doses separately when subgrouping by dose. Where factorial trials ran more than one intervention included in this review (AlphaOmega ‐ ALA 2010; AlphaOmega ‐ EPA+DHA 2010), we did not pool both comparisons in the same meta‐analysis.
Dealing with missing data
We sought trials registry entries and study protocols to help us assess which studies measured each outcome. Where trials appeared to have collected – but did not report – data, we wrote to study authors to ask for information. We wrote to authors of all studies that randomised at least 100 participants as well as to those of many smaller studies (although not to all due to limited resources), prioritising our efforts on larger studies that would tend to provide more information to the review. For larger studies where we found no trials registry entry or protocol, we wrote to study authors to ask whether they had collected information on any outcomes of interest that we had not yet located. Where it was clear that data existed but could not be located to use within the review, we noted this and assessed the potential effect of this missing data on effect sizes narratively.
Assessment of heterogeneity
We assessed heterogeneity using the I2 test and assumed it to be important when I2 was more than 60% (Higgins 2003).
Assessment of reporting biases
We used funnel plots to assess for evidence of bias for primary outcomes where at least 10 studies contributed to the meta‐analysis (Egger 1997).
Data synthesis
Primary measures of interest were effects of dietary advice or supplementation of fish‐based (long‐chain, LCn3) omega‐3 fats, and alpha linolenic acid (ALA), on primary outcomes. We separated out effects of LCn3 and ALA in all analyses and thus present two separate sets of results: one for ALA and one for LCn3.
We combined treatment/control differences in the outcomes across studies using relative risks (RR) or mean differences (MD) in random‐effects meta‐analysis. For combined outcomes (e.g. combined cardiovascular events), we made attempts to add numbers of individuals experiencing specific outcomes within studies, but only where we were certain that we were not counting individual participants more than once within any one of our review outcome categories. However, individuals may have been counted for more than one of the review outcomes (in separate forest plots).
Subgroup analysis and investigation of heterogeneity
We explored the effects of LCn3 and ALA separately on all primary review outcomes and also on key review outcomes where these were secondary outcomes in our review and included at least six studies by subgrouping. The planned subgroup analyses were:
type of intervention – dietary advice, supplemental foods (for example margarine fortified with rapeseed, tins of sardines or oils to use in cooking) provided by the study, supplements (capsules or oils) provided to take as medicine or any combination;
replacement of saturated fatty acids (SFA), mono‐unsaturated fatty acids (MUFA), omega‐6 fats, fat mixture, carbohydrates or sugars, non‐fat or no placebo, or unclear, with LCn3 or ALA;
primary prevention versus secondary prevention of CVD;
LCn3 dose: at least 150 mg/d, 250 mg/d, 400 mg/d from all sources including supplements (above or below each threshold) – low dose 0.4 g/d to 2.4 g/d, medium dose 2.5 g/d to 4.4 g/d, and high dose ≥ 4.5 g/d of combined long‐chain omega‐3 fats,
ALA dose: higher versus lower levels of intake (≥ 5 g/d versus < 5 g/d);
trial duration – studies with medium follow‐up (12 to 23 months), medium follow‐up (24 to 47 months) and long follow‐up (≥ 48 months);
statin use (< 50% of control group on statins, ≥ 50% of control group on statins, use of statins unclear);
baseline long‐chain omega‐3 intake, and baseline ALA intake.
There were insufficient data on baseline omega three intake (or intake in control groups which could have been used as a proxy) to subgroup by baseline omega‐3 intake.
Meta‐regression
We used meta‐regression to further explore effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose (looking for evidence of dose response for each), duration, primary or secondary prevention, food or capsule intervention (food included dietary advice and supplemental foods), and risk of bias (summary risk of bias low or moderate to high) on primary outcomes. We performed random‐effects meta‐regression using the STATA command metareg (Berkley 1995; Sharp 1998): log(e) relative risk versus (dose or primary/secondary prevention or type of intervention or risk of bias or duration), weighted by the standard error of the log(e) relative risk. Where there were no events in one arm, we added 0.1 to the numbers for both groups (so a trial with 10 people experiencing stroke in one arm but none in the other arm would be entered as 10.1 and 0.1). We analysed all included trials (of at least 12 months' duration) that reported each outcome from this review and its sister reviews (omega‐3 trials from this review, omega‐6 trials from the update of Hooper 2018, and total PUFA trials from Abdelhamid 2018). We carried out meta‐regression of each variable singly, then a multivariate meta‐regression of the three variables with lowest P values in single regression for each outcome. Given that we generally included data from around 35 trials and there were some missing data for some trials, we did not run meta‐regressions with more than three variables at one time.
Sensitivity analysis
We carried out sensitivity analyses on all primary outcomes (regardless of the number of included trials) and on key outcomes that were secondary outcomes in this review.
We used sensitivity analyses to assess robustness of results to:
trial quality (removing trials at moderate or high summary risk of bias);
study size (retaining only trials that randomised at least 100 participants across all study arms);
fixed‐effect analysis; and
compliance (retaining only trials where we assessed compliance as conferring low risk of bias).
We tabulated the type and frequency of side effects and adverse effects (with the other extracted data on adverse effects) and compared between different studies and designs.
'Summary of findings' tables
Outcome data were interpreted as follows:
Is there an effect? (options were ‘increased risk’, ‘decreased risk’, or ‘little or no effect’). Our main outcome measure was RR so we decided on existence of an effect using RR. RR < 8% (RR < 0.92 or > 1.08) for the highest quality evidence suggested increased or decreased risk (otherwise little or no effect). The presence or not of an effect was decided on the RR for the main analysis and sensitivity analyses.
Quality of evidence was assessed using GRADE assessment (GRADE Working Group 2004) for key outcomes. We used the five GRADE considerations (risk of bias, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence as it related to the studies that contributed data to the meta‐analyses for the prespecified outcomes. We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), plus GRADEpro GDT software (GRADEpro GDT 2015). We justified all decisions to downgrade the quality of studies using footnotes and made comments to aid reader's understanding of the review.
Where there was a suggested effect the size of effect was assessed using the NNT or ARR.
We included three 'Summary of findings' tables: for effects of LCn3 on primary outcomes, effects of ALA on primary outcomes, and for key outcomes that were not included in the review primary outcomes (measures of adiposity and serum lipids).
Results
Description of studies
Results of the search
The electronic searches for the full set of reviews (populating the dataset of all trials that assessed effects of higher versus lower omega‐6, omega‐3 or PUFA over at least 6 months) generated 37,810 titles and abstracts, which we de‐duplicated to 19,772 hits. We assessed these along with 53 studies previously included from Hooper 2018 and Hooper 2004, to reassess for inclusion; 986 potentially relevant trials registry entries; and 35 new references gained from systematic review reference lists. In total, we assessed 20,846 titles and abstracts in duplicate to decide whether to retrieve full texts. We ultimately assessed 2155 full‐text reports, of which 226 were systematic reviews. Two review authors independently assessed the remaining 1929 papers for inclusion and grouped them into studies. Of these, we included 208 RCTs in a wider set of trials that underpinned the full set of reviews (this review and several others including Abdelhamid 2018; Abdelhamid 2017; Hooper 2018; Brown 2017; Hanson 2017a; Hanson 2017b; Jimoh 2017; Thorpe 2017). This wider set of trials included RCTs of omega‐3, omega‐6 or total polyunsaturated fatty acids (PUFA) interventions with a duration of at least six months (Figure 1) and comprised 730 reports.
Figure 1.
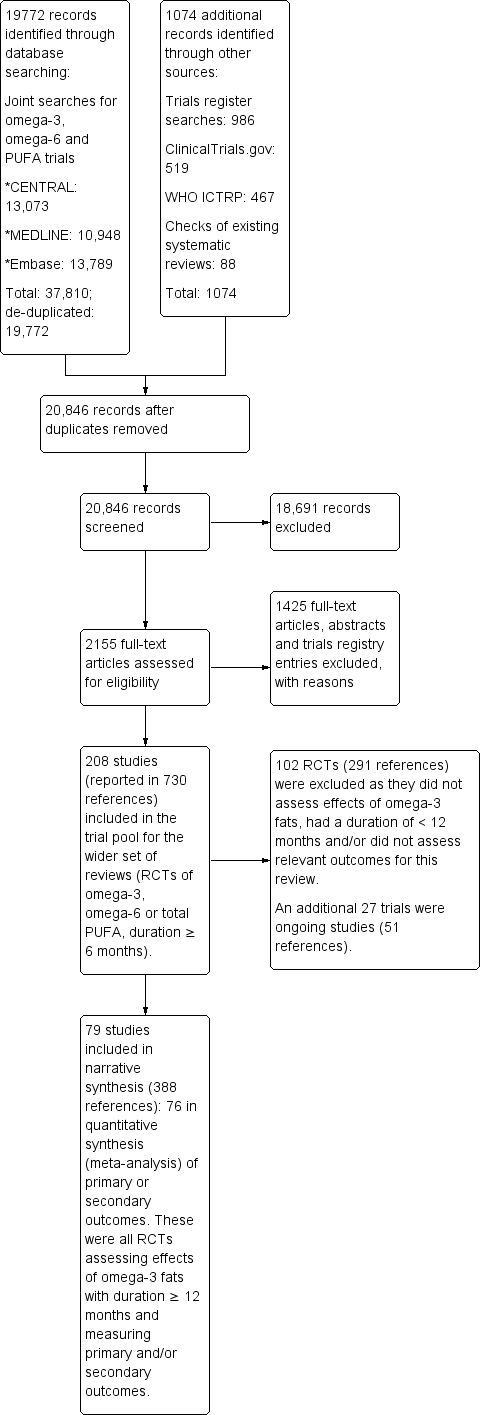
Study flow diagram.
Of these 208 RCTs:
27 RCTs (51 documents) assessed effects of omega‐3 fats over at least one year but were ongoing (without published outcome data);
102 RCTs (291 documents) did not assess effects of omega‐3 fats or had a duration of less than one year, so we excluded them; and
79 RCTs (388 documents) were eligible for inclusion in this review.
Of these 79 RCTs, 76 were included in meta‐analyses. Three trials clearly collected relevant data but did not report them in a format that could be used in meta‐analyses (Gill 2012; Ramirez‐Ramirez 2013; Reed 2014; Figure 1).
Included studies
The 79 included RCTs randomised 112,059 participants, tripling the number of participants in the original version of this review (36,913 participants, some of whom were followed for only six months). The number of participants in included studies ranged from 11 to 18,645. Twelve trials randomised at least 1000 participants (AlphaOmega ‐ ALA 2010; AlphaOmega ‐ EPA+DHA 2010; AREDS2 2014; DART2 2003; DART 1989; GISSI‐HF 2008; GISSI‐P 1999; JELIS 2007; Norwegian 1968; OMEGA 2009; ORIGIN 2012; Risk & Prevention 2013; SU.FOL.OM3 2010), of which one was a 2 × 2 factorial trial where both interventions were included (AlphaOmega ‐ ALA 2010; AlphaOmega ‐ EPA+DHA 2010). Most of these larger trials assessed effects of longer chain omega‐3 fats, but two studies/arms assessed effects of ALA (AlphaOmega ‐ ALA 2010; Norwegian 1968).
Participants had cardiovascular disease at baseline in 33 of the trials (secondary prevention), and the remaining 46 trials were of primary prevention.
Most studies assessed effects of long‐chain omega‐3 fats.
Sixty‐two studies increased LCn3 intake using supplementary capsules or medicinal oils (ADCS 2010; AFFORD 2013; Ahn 2016; AREDS2 2014; Baldassarre 2006; Bates 1989; Berson 2004; Brox 2001; Caldwell 2011; Derosa 2016; Deslypere 1992; Doi 2014; DO IT 2010; EPE‐A 2014 (as two different doses); EPIC‐1 2008; EPIC‐2 2008; EPOCH 2014; Erdogan 2007; FAAT 2005; FORWARD 2013; Franzen 1993; Gill 2012; GISSI‐HF 2008; GISSI‐P 1999; HARP 1995; JELIS 2007; Kumar 2012; Kumar 2013; Lorenz‐Meyer 1996; MAPT 2017; MARINA 2011; Mita 2007; NAT2 2013; Nodari 2011 AF; Nodari 2011 HF; Norouzi 2014; Nutristroke 2009; Nye 1990; OFAMI 2001; OMEGA 2009; OPAL 2010; ORIGIN 2012; ORL 2013; Özaydin 2011; Proudman 2015; Puri 2005; Raitt 2005; Ramirez‐Ramirez 2013; Reed 2014; Risk & Prevention 2013; Rossing 1996; Sandhu 2016; SCIMO 1999; Shinto 2014; SHOT 1996; Sianni 2013; SOFA 2006; Sofi 2010; SU.FOL.OM3 2010; Tande 2016; WELCOME 2015; Zhang 2017).
Two trials used supplemented or supplemental foods, such as enriched margarine or juice to increase LCn3 (AlphaOmega ‐ EPA+DHA 2010; FOSTAR 2016).
Four increased LCn3 fats using dietary advice (DART2 2003; DART 1989; DISAF 2003; THIS DIET 2008).
Three provided some combination of these interventions to increase LCn3 (DIPP 2015; SMART 2013; Weinstock‐Guttman 2005).
Fewer studies assessed the effects of ALA on health outcomes.
One trial used supplementary capsules or medicinal oils to increase ALA (Norwegian 1968).
Six increased ALA using supplemented or supplemental foods, such as enriched margarine, bread, walnuts or other enriched food products (AlphaOmega ‐ ALA 2010; Dodin 2005; FLAX‐PAD 2013; HERO 2009; MARGARIN 2002; WAHA 2016).
One used a combination of these to increase ALA (MENU 2016).
One trial provided an intervention combining LCn3 and ALA as capsules (DIPP 2015). However, trialists did not state the ALA dose, so we treated the study as an LCn3 intervention.
Control groups received olive, corn, sunflower oils, other types of fats (including medium‐chain triglycerides and fat replicating the composition of an average European diet), other 'inert' or ill‐defined substances (liquid paraffin, aluminium hydroxide, 'placebo' not described), different dietary advice or foods without the omega‐3 enrichment, or no treatment/no placebo.
The main study outcome was cardiovascular in 48 studies. Eighteen studies (19 comparisons) aimed to measure death or cardiovascular events (AlphaOmega ‐ ALA 2010; AlphaOmega ‐ EPA+DHA 2010; DART2 2003; DART 1989; Doi 2014; FAAT 2005; FLAX‐PAD 2013; GISSI‐HF 2008; GISSI‐P 1999; JELIS 2007; Norwegian 1968; Nye 1990; OFAMI 2001; OMEGA 2009; ORIGIN 2012; Risk & Prevention 2013; SOFA 2006; SU.FOL.OM3 2010; THIS DIET 2008).
Thirty studies aimed to measure various cardiovascular risk factors or progression of cardiovascular health.
Atrial fibrillation recurrence or sinus rhythm (AFFORD 2013; DISAF 2003; Erdogan 2007; FAAT 2005; FORWARD 2013; Kumar 2012; Kumar 2013; Nodari 2011 AF; Özaydin 2011; Raitt 2005; Sianni 2013).
Atherosclerosis progression/regression (Ahn 2016; DO IT 2010; HARP 1995; SCIMO 1999).
Left ventricular function (Nodari 2011 HF).
CABG graft patency (SHOT 1996).
Lipids and other CVD risk factors (Brox 2001; Deslypere 1992; Franzen 1993; MARGARIN 2002).
Diabetes, insulin or glucose‐based outcomes (Derosa 2016; Rossing 1996).
Endothelial function or carotid intima‐media thickness (IMT) (Baldassarre 2006; Gill 2012; MARINA 2011; Mita 2007).
Body weight and adiposity (HERO 2009; MENU 2016; SMART 2013).
Thirty‐one RCTs assessed effects on other health states.
Cognitive measures (ADCS 2010; EPOCH 2014; MAPT 2017; OPAL 2010; Shinto 2014; WAHA 2016; Zhang 2017).
Eye health (AREDS2 2014; Berson 2004; NAT2 2013).
Multiple sclerosis outcomes (Bates 1989; Weinstock‐Guttman 2005).
Cancer or pre‐cancer outcomes (DIPP 2015).
Bone health (Dodin 2005).
Liver health (Caldwell 2011; EPE‐A 2014; Sofi 2010; WELCOME 2015).
Gastrointestinal health (Crohn's EPIC‐1 2008; EPIC‐2 2008; Lorenz‐Meyer 1996).
Arthritis outcomes (FOSTAR 2016; Proudman 2015; Reed 2014).
Functional status (Nutristroke 2009).
Neurological function after spinal injury or in Huntington's disease (Norouzi 2014; Puri 2005).
Safety outcomes and adverse events (ORL 2013; Tande 2016).
Breast health (Sandhu 2016).
Inflammatory markers (Ramirez‐Ramirez 2013).
Most studies took place in high‐income economies (World Bank 2018), but four were in upper‐middle‐income countries: Argentina (FORWARD 2013), Iran (Norouzi 2014), Turkey (Özaydin 2011), and China (Zhang 2017). No studies took place in low‐ or low‐middle income countries.
We identified a further 27 ongoing trials, which we describe in the table of Characteristics of ongoing studies. At the time of writing this review, all of these trials were unpublished, and some were recruiting or delivering interventions or had recently been completed, and trialists were presumably analysing data and writing up results. Others appear overdue for publication, and their status is unclear – they may constitute missing data.
Excluded studies
We read full texts of over 1000 papers, so the full list of excluded studies is too extensive to add to this review. The main reason for exclusion of full‐text papers was duration of less than 12 months (this was often unclear in abstracts, so we collected full‐text papers to check).
We initially included several studies into our wider data set (Singh 1992; Singh 1997a; Singh 1997b; Singh 2002), but we later excluded them due to expressions of concern published by the BMJ and The Lancet (BMJ 2005; Horton 2005; White 2005). These expressions of concern followed extensive examination of the conduct, results and publication of these studies and questioned the veracity of data behind several studies published by RB Singh. Another trial was retracted and so not included (Matsuyama 2005).
Risk of bias in included studies
We assessed summary risk of bias as low in 25 RCTs (26 comparisons: ADCS 2010; AlphaOmega ‐ ALA 2010; AlphaOmega ‐ EPA+DHA 2010; AREDS2 2014; Berson 2004; Caldwell 2011; Derosa 2016; EPOCH 2014; FLAX‐PAD 2013; FORWARD 2013; FOSTAR 2016; Lorenz‐Meyer 1996; MAPT 2017; MARGARIN 2002; MARINA 2011; NAT2 2013; OMEGA 2009; OPAL 2010; ORIGIN 2012; Proudman 2015; Puri 2005; Reed 2014; SCIMO 1999; SOFA 2006; SU.FOL.OM3 2010; WELCOME 2015), and we deemed it to be moderate to high in the remainder. Our definition of low summary risk of bias is in the section Assessment of risk of bias in included studies. Figure 2 itemises risk of bias by domain and study.
Figure 2.
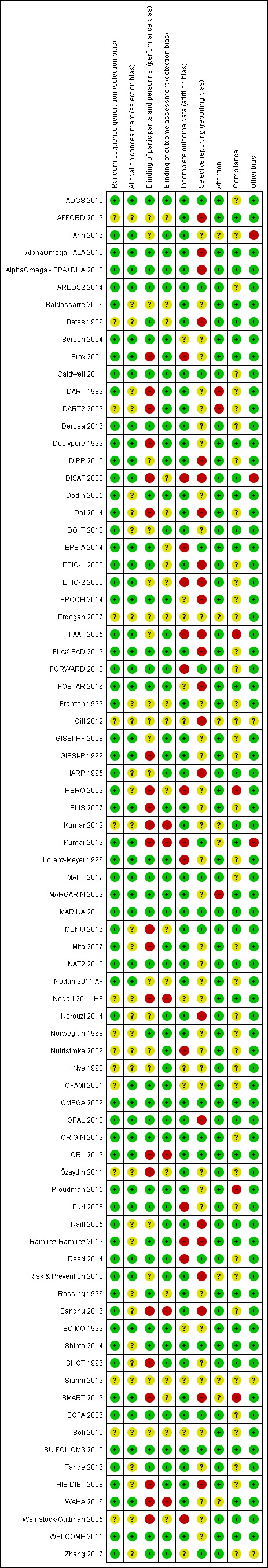
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Of the 79 RCT arms described in the 'Risk of bias' summary (Figure 2), 64 studies described randomisation well enough to merit an assessment of low risk (the remainder were unclear), and 45 study arms described adequate allocation concealment (the remaining 34 were unclear).
Blinding
We considered blinding of participants and personnel to be at low risk of bias in 37 of the 79 comparisons (Figure 2). Lack of blinding of participants put 22 trials at high risk of bias while the remaining 20 arms were at unclear risk. Blinding of outcome assessors put trials at low risk of detection bias in 53 studies and at high risk in 6 trials; this aspect was unclear in the remainder. We found that 33 studies were at low risk of both performance and detection bias.
Incomplete outcome data
We found that 53 trials were at low risk of attrition bias, 14 at high risk, and the remaining 12 at unclear risk.
Selective reporting
We determined that 17 trials had a pre‐published trials registry entry or protocol and reported all planned outcomes appropriately so were considered at low risk of selective reporting. Twenty‐three trials were at high risk of selective reporting omitting reports on either pre‐stated outcomes or time points. We judged the remaining 39 trials to be at unclear risk of reporting bias as we could not find any protocol or prospective trial registry entry (often trials were published prior to trial registration availability).
Other potential sources of bias
We assessed risk of bias from lack of compliance and attention bias and also noted other sources of bias. We found four studies to be at high risk of compliance bias (FAAT 2005; HERO 2009; Proudman 2015; SMART 2013), while 34 studies provided evidence of good compliance, and the remaining 41 studies were unclear. We noted a high risk of attention bias in three studies where intervention participants potentially had more dedicated time for dietary advice or follow‐up (DART2 2003; DART 1989; MARGARIN 2002). Nine trials did not provide enough details to assess so we considered them to be at unclear risk of attention bias (Ahn 2016; Erdogan 2007; Gill 2012; Kumar 2012; Kumar 2013; Risk & Prevention 2013; Sianni 2013; SMART 2013; WAHA 2016), while we thought the remaining 67 were at low risk of attention bias. We judged three studies to be at high risk of other potential biases: Ahn 2016 because it is unclear whether it was placebo‐controlled, and there was concern over reported standard deviations, DISAF 2003 because the study stopped early, and Kumar 2013 due to concerns over design. Three studies were at unclear risk due to insufficient methodological detail being provided (Gill 2012; Sianni 2013; Zhang 2017).
Effects of interventions
See: Table 1; Table 2; Table 3
Primary outcomes
See Table 1 for a GRADE summary of our evidence on effects of long‐chain omega‐3 (LCn3) fats (including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and docosapentaenoic acid (DPA)) on our primary outcomes.
Effects of long‐chain omega‐3 fats on primary health outcomes
All‐cause mortality (LCn3)
High‐quality evidence showed little or no effect of LCn3 on all‐cause mortality.
There was little or no effect of increasing long‐chain omega‐3 fats on all‐cause mortality, despite 8189 deaths in > 92,000 participants (RR 0.98, 95% CI 0.93 to 1.03, I2 = 12%, Analysis 1.1). The funnel plot suggested that some small studies with higher numbers of deaths in the intervention group might be missing (Figure 3), indicating small study bias. If such missing studies were added back in the RR would rise (towards the null value of 1.0).
Analysis 1.1.
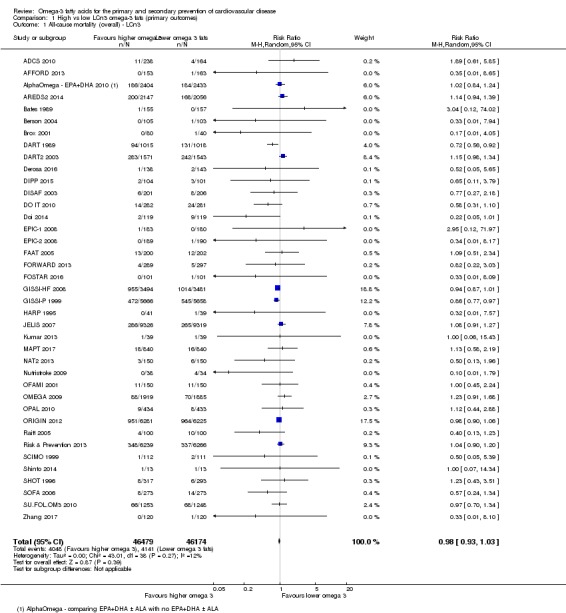
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 1 All‐cause mortality (overall) ‐ LCn3.
Figure 3.
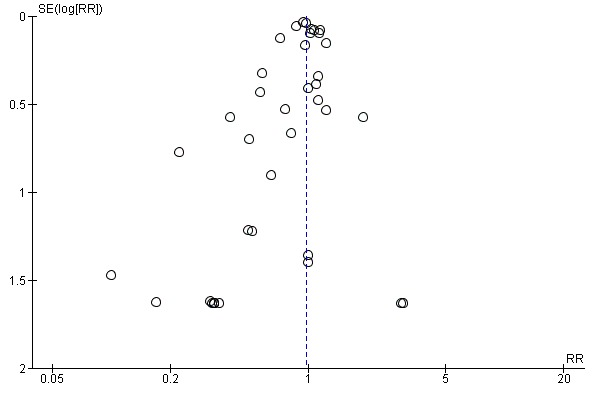
Funnel plot of comparison: 1 High vs low LCn3 omega‐3 fats (primary outcomes), outcome: 1.1 Aall‐cause mortality (overall) – LCn3.
Sensitivity analyses using fixed‐effect meta‐analysis did not alter the lack of effect on all‐cause mortality (RR 0.97, 95% CI 0.93 to 1.01, Analysis 1.2). Removing RCTs not at low summary risk of bias left us with 15 RCTs involving over 33,000 participants, 3059 of whom died, suggesting no effect of LCn3 on mortality (RR 1.01, 95% CI 0.94 to 1.08, I2 = 0%, Analysis 1.3). This lack of effect was also evident in sensitivity analyses limited to studies at low risk of compliance bias and to larger studies (Analysis 1.4).
Analysis 1.2.
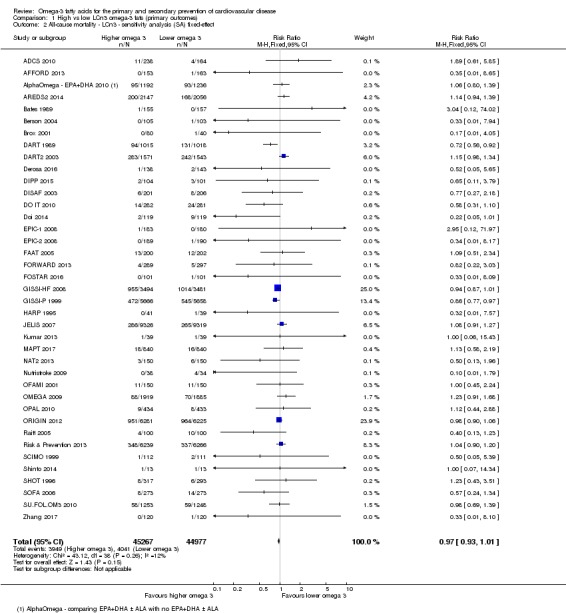
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 2 All‐cause mortality ‐ LCn3 ‐ sensitivity analysis (SA) fixed‐effect.
Analysis 1.3.
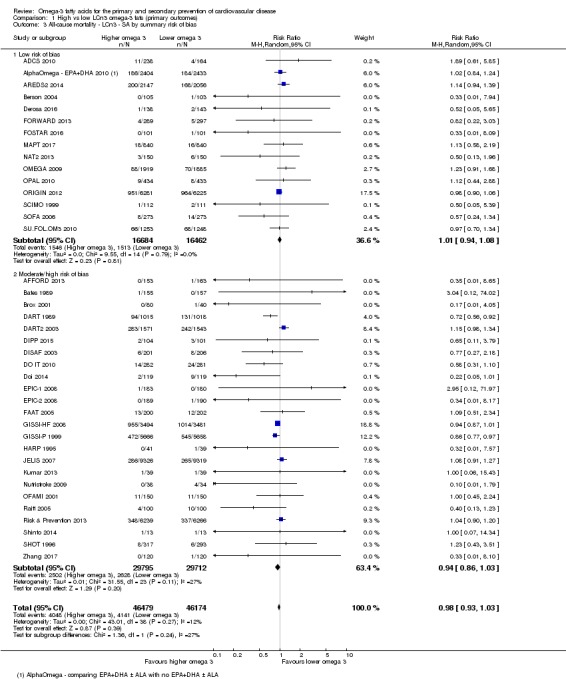
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 3 All‐cause mortality ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.4.
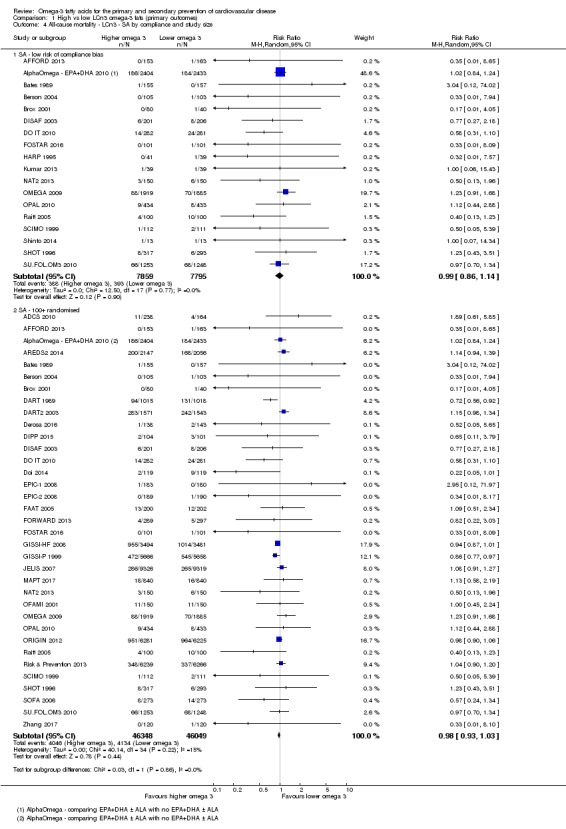
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 4 All‐cause mortality ‐ LCn3 ‐ SA by compliance and study size.
The lack of effect for LCn3 on mortality did not differ by replacement with mono‐unsaturated fatty acids (MUFA), omega‐3 fats or other types of placebo compounds (Analysis 1.6). There was no suggestion of any dose effect for long‐chain omega‐3 fats on mortality (Analysis 1.5), and subgroups with RRs further away from 1.00 had wider 95% confidence intervals. The lack of effect did not differ by primary versus secondary prevention (Analysis 1.9) or mode of intervention (dietary advice, supplemental foods, or capsules, Analysis 1.7). While there was some suggestion of a small risk reduction in total mortality with LCn3 in studies with medium to long duration (2 to < 4 years, RR 0.91, 95% CI 0.86 to 0.96) and this subgroup was clearly different from other durations (test for subgroup differences P = 0.007), the effect was not evident in shorter (1 to < 2 years) or longer studies (≥ 4 years, RR 1.03, 95% CI 0.98 to 1.09). Because of the lack of effect in longer studies, we did not assume any duration effects (Analysis 1.8).
Analysis 1.6.
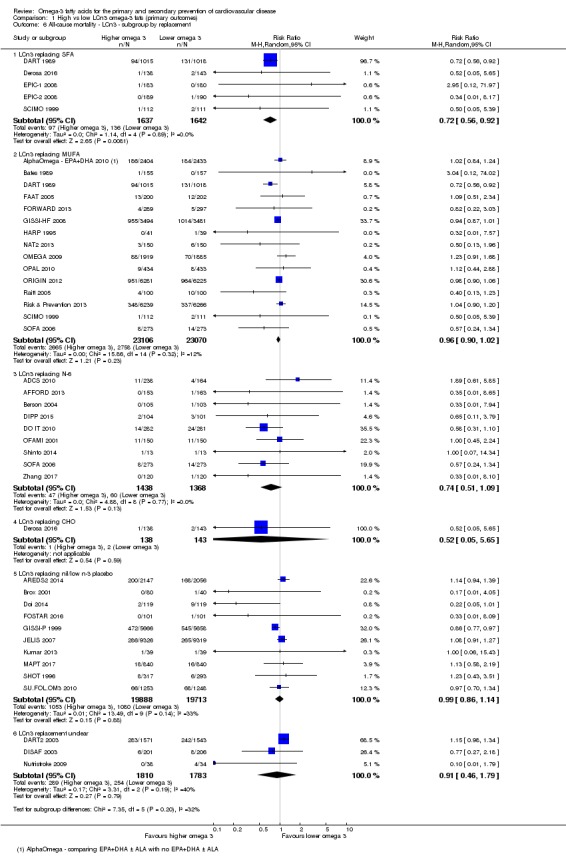
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 6 All‐cause mortality ‐ LCn3 ‐ subgroup by replacement.
Analysis 1.5.
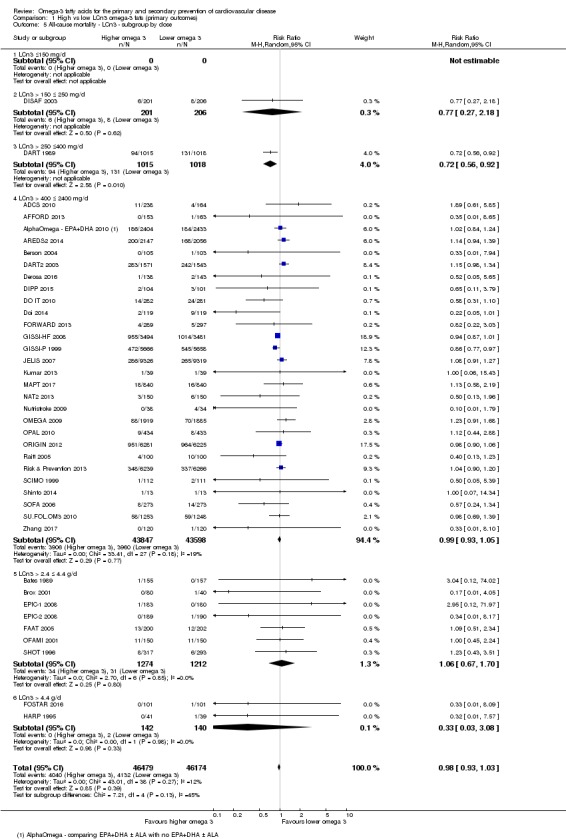
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 5 All‐cause mortality ‐ LCn3 ‐ subgroup by dose.
Analysis 1.9.
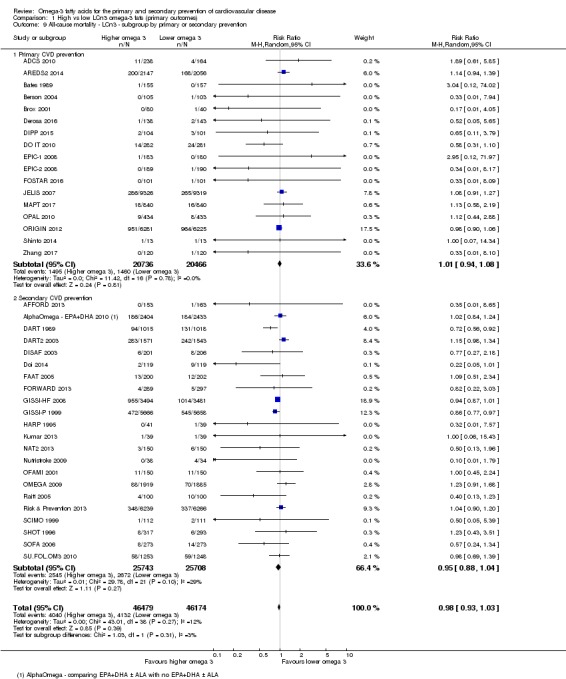
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 9 All‐cause mortality ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 1.7.
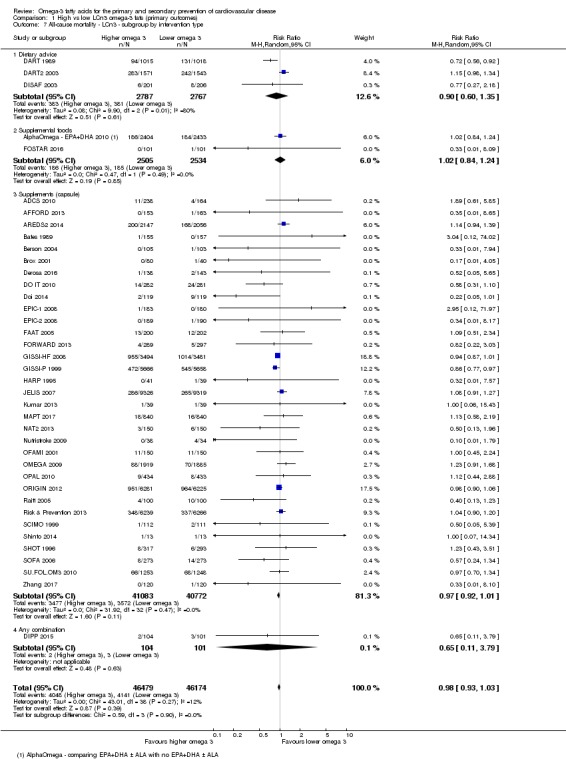
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 7 All‐cause mortality ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.8.
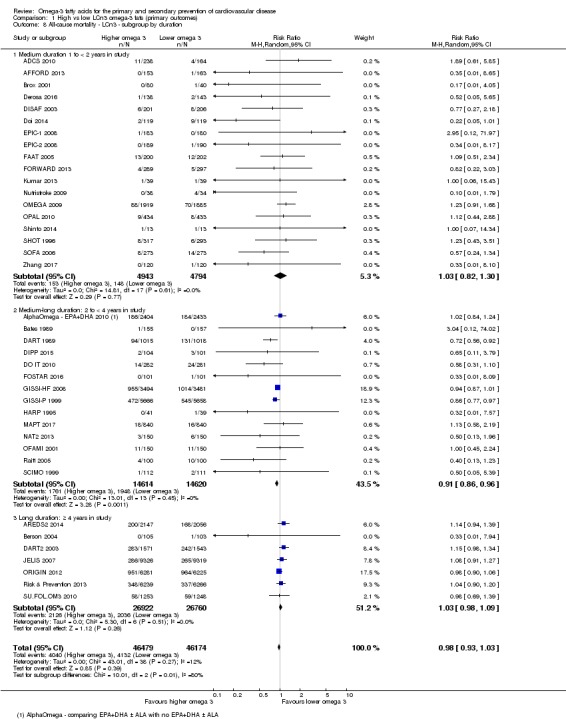
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 8 All‐cause mortality ‐ LCn3 ‐ subgroup by duration.
As there was no suggestion of any effect of LCn3 fats on all‐cause mortality, we did not carry out meta‐regression.
GRADE assessment suggested that the finding of little or no effect of LCn3 on all‐cause mortality was supported by high‐quality evidence (not downgraded, Table 1).
Cardiovascular mortality (LCn3)
Moderate‐quality evidence suggests that long‐chain omega‐3 fat intake probably makes little or no difference to cardiovascular deaths.
Twenty‐five trials in at least 67,000 participants, 4544 of whom died of CVD, reported on cardiovascular mortality (RR 0.95, 95% CI 0.87 to 1.03, I2 = 24%, Analysis 1.11). The funnel plot suggested that some smaller studies with more cardiovascular deaths in the intervention group were missing (some small study bias, Figure 4) – if this were the case then adding the missing studies would increase the relative risk towards the null (no effect).
Analysis 1.11.
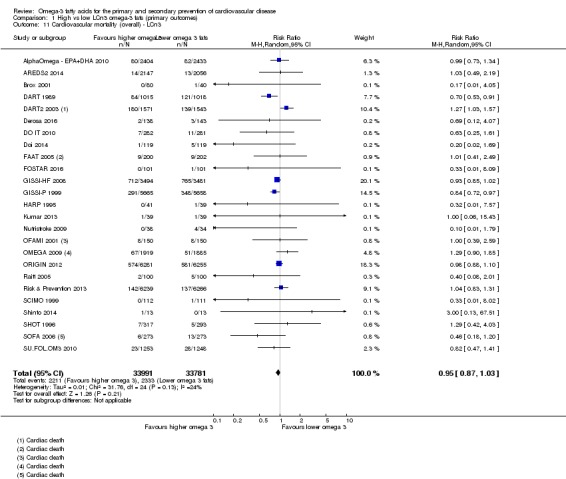
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 11 Cardiovascular mortality (overall) ‐ LCn3.
Figure 4.
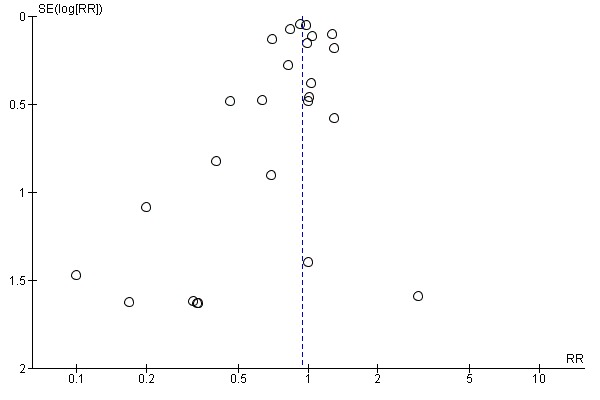
Funnel plot of comparison: 1 High vs low LCn3 omega‐3 fats (primary outcomes), outcome: 1.11 Cardiovascular mortality (overall) – LCn3.
Fixed‐effect meta‐analysis suggested a 6% reduction in CVD mortality risk (RR 0.94, 95% CI 0.89 to 1.00, Analysis 1.12). However, sensitivity analyses removing RCTs not at low summary risk of bias left nine RCTs in over 29,000 participants, 1539 of whom died, suggesting little or no effect of LCn3 on CVD mortality (RR 0.99, 95% CI 0.90 to 1.09, I2 = 0%, Analysis 1.13). Removing trials not at low risk of compliance bias had a similar effect (Analysis 1.14).
Analysis 1.12.
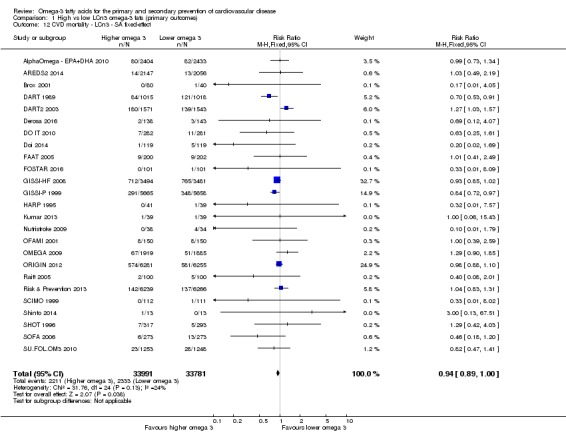
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 12 CVD mortality ‐ LCn3 ‐ SA fixed‐effect.
Analysis 1.13.
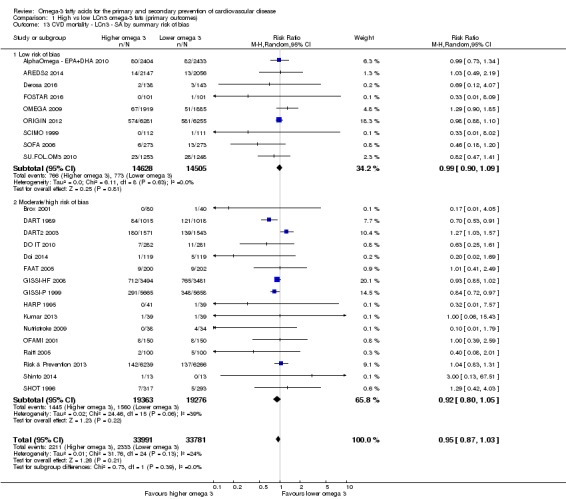
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 13 CVD mortality ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.14.
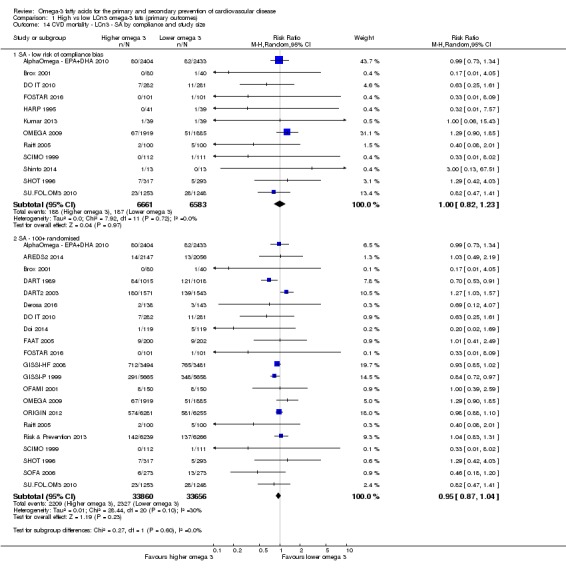
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 14 CVD mortality ‐ LCn3 ‐ SA by compliance and study size.
There were no statistically significant differences between subgroups and no differential effects by replacement (Analysis 1.16), mode of intervention (Analysis 1.17), duration (marginally significant difference between subgroups, P = 0.06; effects seen only in medium‐ to long‐term trials and not in shorter or longer studies, Analysis 1.18), primary or secondary prevention (Analysis 1.19), statin use (Analysis 1.20) or omega‐3 dose (Analysis 1.15). There was no suggestion of a dose‐response effect.
Analysis 1.16.
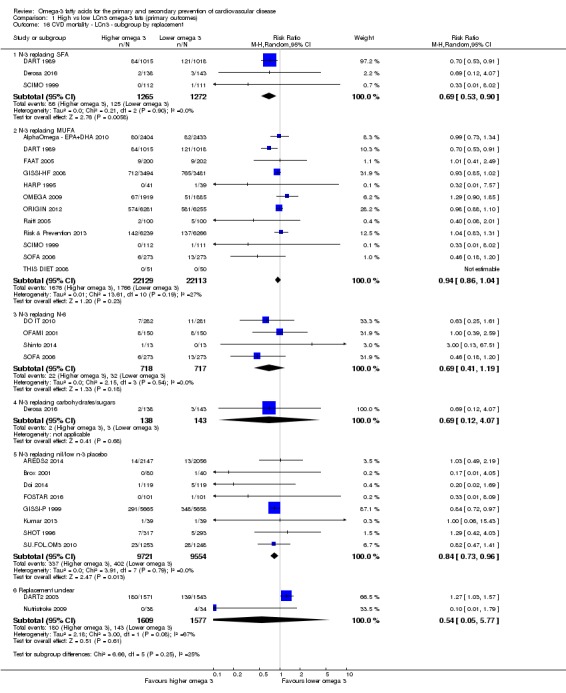
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 16 CVD mortality ‐ LCn3 ‐ subgroup by replacement.
Analysis 1.17.
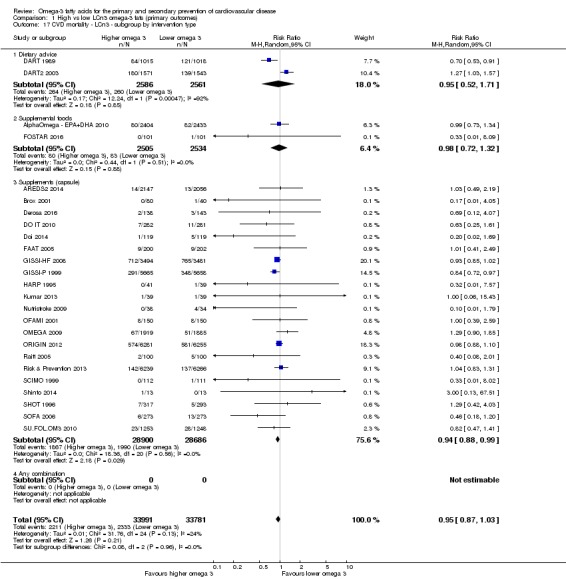
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 17 CVD mortality ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.18.
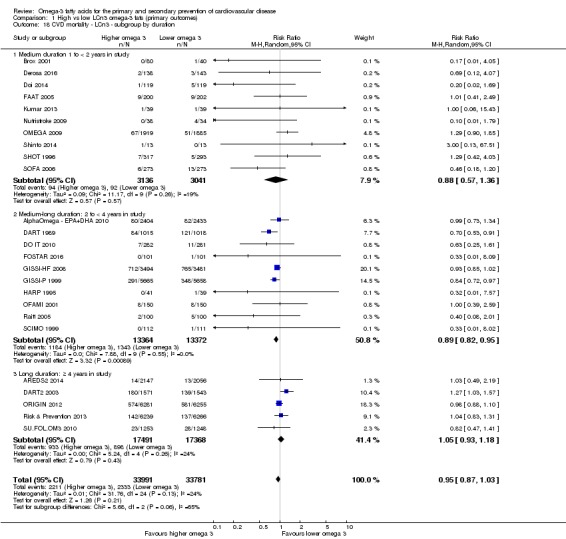
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 18 CVD mortality ‐ LCn3 ‐ subgroup by duration.
Analysis 1.19.
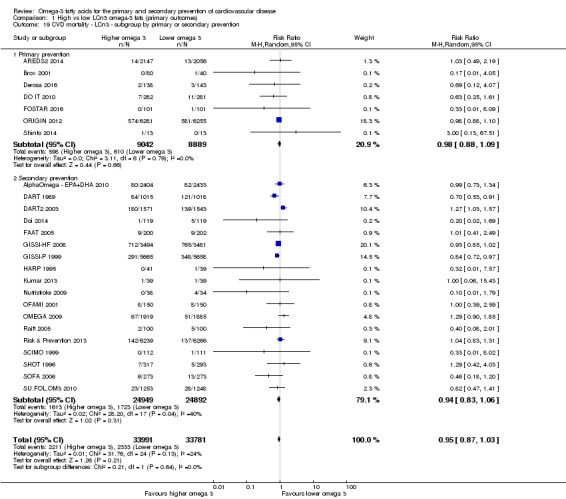
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 19 CVD mortality ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 1.20.
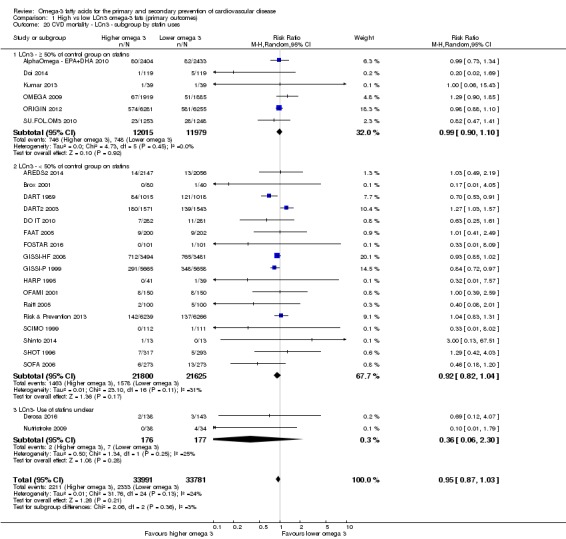
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 20 CVD mortality ‐ LCn3 ‐ subgroup by statin uses.
Analysis 1.15.
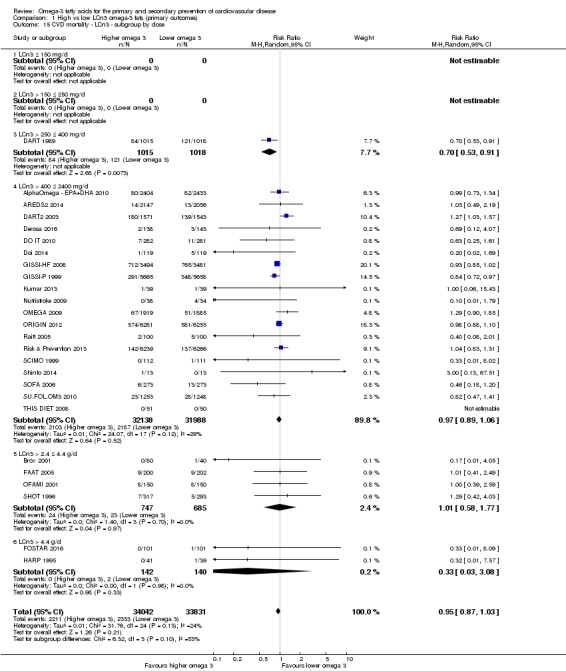
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 15 CVD mortality ‐ LCn3 ‐ subgroup by dose.
Meta‐regression to assess effects of LCn3 dose (or alpha‐linolenic acid (ALA), omega‐6 or total poly‐unsaturated fatty acid (PUFA) dose), duration, intervention type, primary or secondary prevention and risk of bias (as well as a single multiple regression of the three factors with the smallest P value) showed no association between these factors and risk of cardiovascular mortality (all P values were > 0.60, Table 11). We saw no suggestion of dose‐response or duration effects.
Table 2.
Meta‐regression results for cardiovascular mortalitya
| Variable assessed | P value |
| LCn3 dose | 0.61 |
| ALA dose | 0.91 |
| Omega‐6 dose | 0.81 |
| Total PUFA dose | 0.82 |
| Duration, months | 0.68 |
| Primary or secondary CVD prevention | 0.88 |
| Food or capsule | 0.54 |
| Risk of bias | 0.94 |
| Food or capsule + LCn3 dose + duration |
0.70 0.96 0.69 |
ALA: alpha‐linolenic acid; CVD: cardiovascular disease; LCn3: long‐chain omega‐3 fatty acids; PUFA: poly‐unsaturated fatty acids.
aRandom‐effects meta‐regression exploring effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose, study duration, primary or secondary prevention, food or capsule intervention, and summary risk of bias (low or moderate to high) on cardiovascular mortality. We ran the meta‐regression using all included trials that reported this outcome in this review, and its sister reviews (update of Hooper 2018, and Abdelhamid 2018). For each variable the P value presented represents probability that the relationship was due to chance (as we had limited power we assumed a true relationship when P < 0.10). Meta‐regression was of each variable singly, plus a multivariate meta‐regression of the 3 single variables with lowest P values. See methods for further information.
The suggestion of a protective effect disappeared in studies at low summary risk of bias and at low risk of compliance problems. The funnel plot suggests that the true risk ratio is higher than the main estimate, and there was no suggestion of dose or duration effects; thus we summarised the evidence as showing little or no effect of LCn3 on CVD mortality. GRADE assessment suggested moderate‐quality evidence that long‐chain omega‐3 fat intake probably makes little or no difference to cardiovascular deaths (moderate‐quality/certainty evidence, downgraded once for imprecision).
Combined cardiovascular events (LCn3)
High‐quality evidence suggests that LCn3 intake makes little or no difference to risk of cardiovascular events.
There was little or no effect of increasing LCn3 fats on cardiovascular events (RR 0.99, 95% CI 0.94 to 1.04, I2 = 37%, Analysis 1.21). Analyses included 14,737 participants with cardiovascular events in more than 90,000 participants in 38 trials. The funnel plot suggested that some smaller studies with more participants experiencing cardiovascular events in the intervention group were missing (some small study bias, not shown) – if this were the case then adding the missing studies would increase the relative risk.
Analysis 1.21.
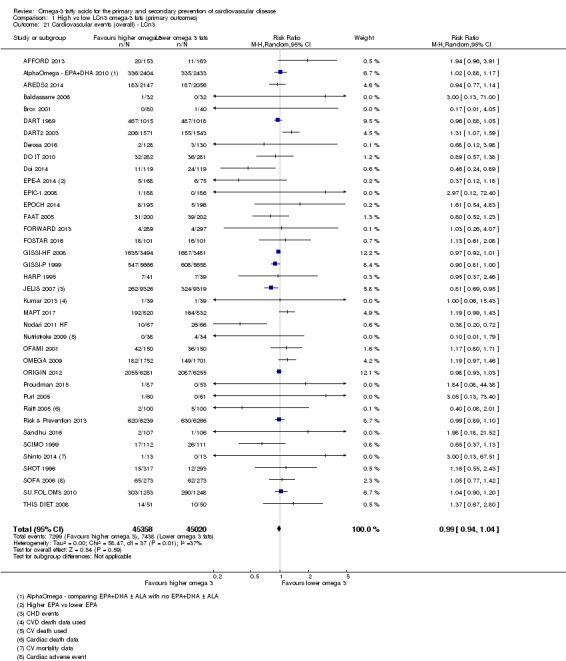
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 21 Cardiovascular events (overall) ‐ LCn3.
Sensitivity analyses removing trials at moderate to high risk of bias left 14 trials, including more than 31,000 participants, 6695 of whom had CVD events, with no suggestion of any effect of LCn3 fats (RR 1.00, 95% CI 0.96 to 1.05, I2 = 0%, Analysis 1.23). Sensitivity analyses including studies at low risk of compliance bias, at low risk of small study bias and using fixed‐effect meta‐analysis did not suggest any effect of LCn3 on CVD events (Analysis 1.22; Analysis 1.24).
Analysis 1.23.
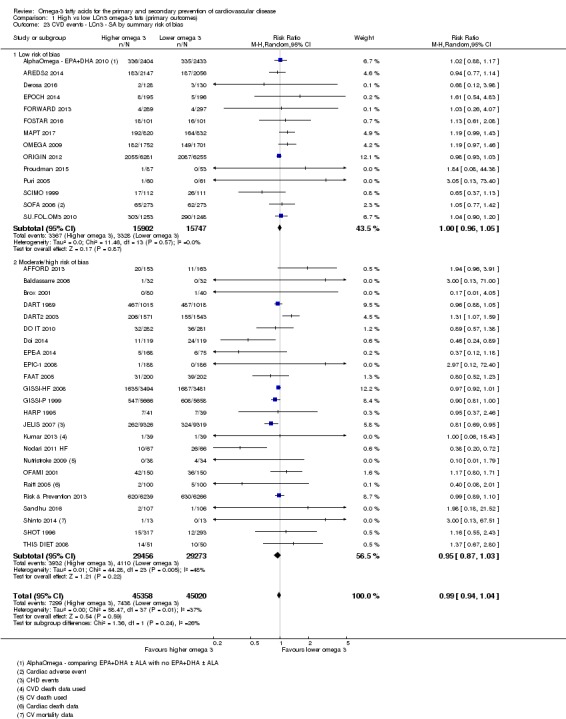
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 23 CVD events ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.22.
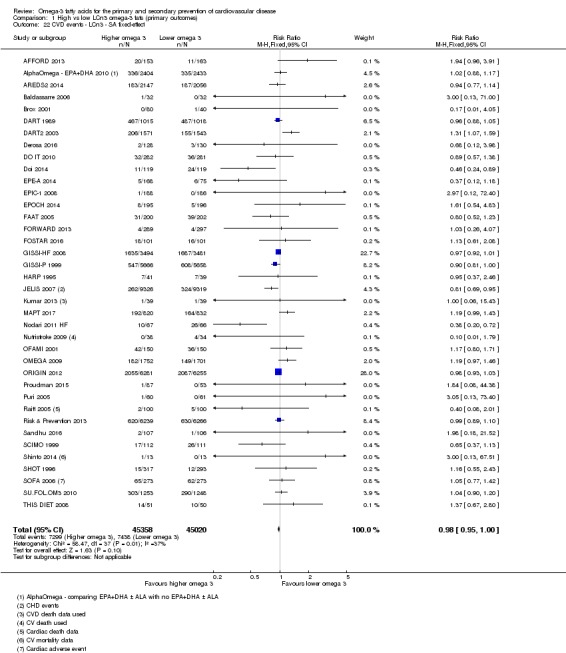
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 22 CVD events ‐ LCn3 ‐ SA fixed‐effect.
Analysis 1.24.
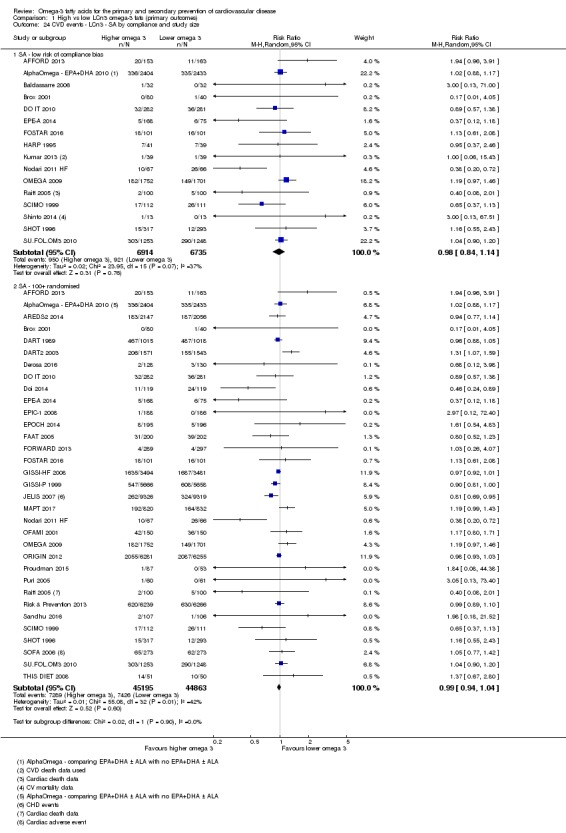
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 24 CVD events ‐ LCn3 ‐ SA by compliance and study size.
In subgroup analysis, there was no suggestion of a dose‐response effect (Analysis 1.25). Effects did not differ by replacement (Analysis 1.26), baseline CVD risk (Analysis 1.29), type of intervention (Analysis 1.27), statin use (Analysis 1.30), LCn3 dose (Analysis 1.25) or study duration (Analysis 1.28), and there were no important differences between subgroups.
Analysis 1.25.
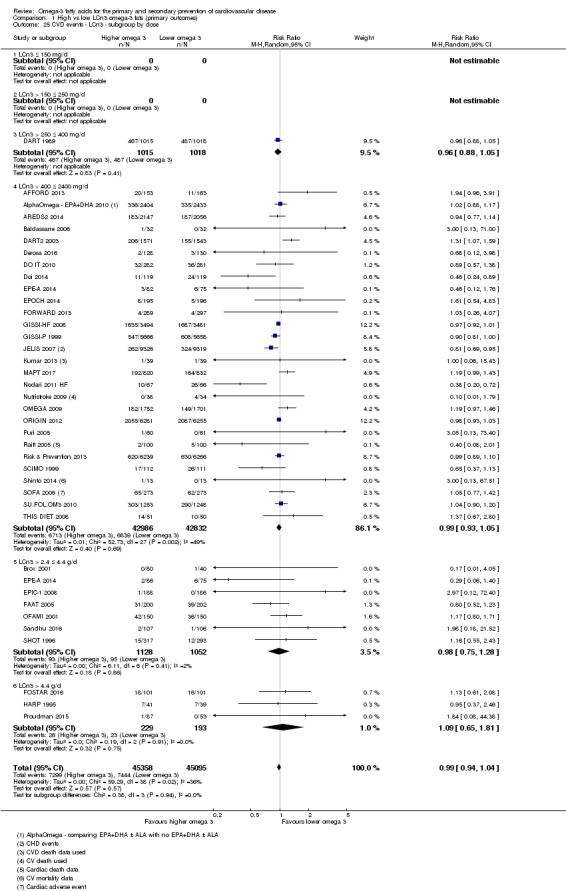
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 25 CVD events ‐ LCn3 ‐ subgroup by dose.
Analysis 1.26.
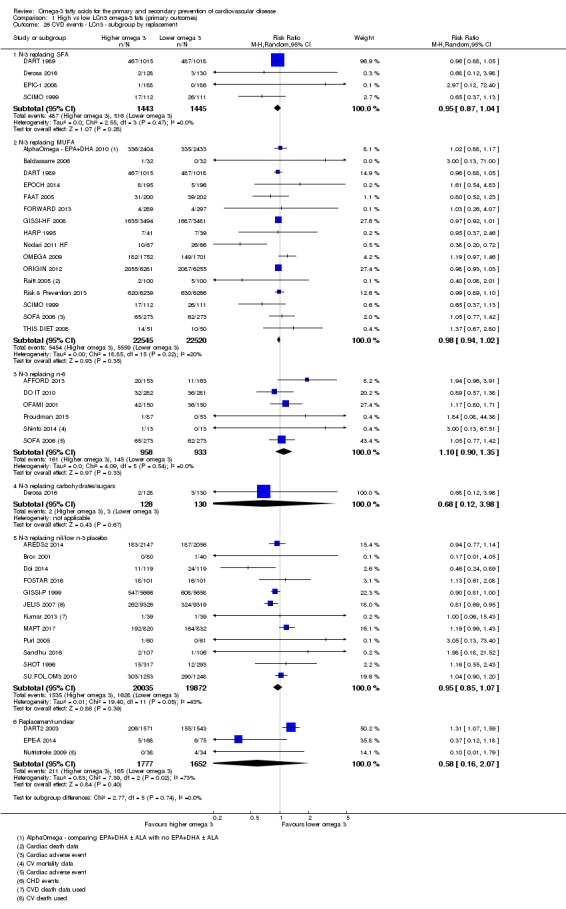
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 26 CVD events ‐ LCn3 ‐ subgroup by replacement.
Analysis 1.29.
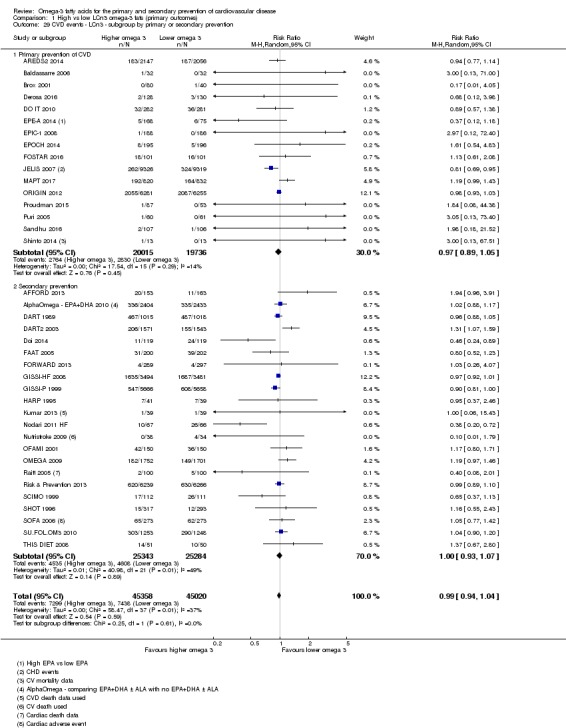
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 29 CVD events ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 1.27.
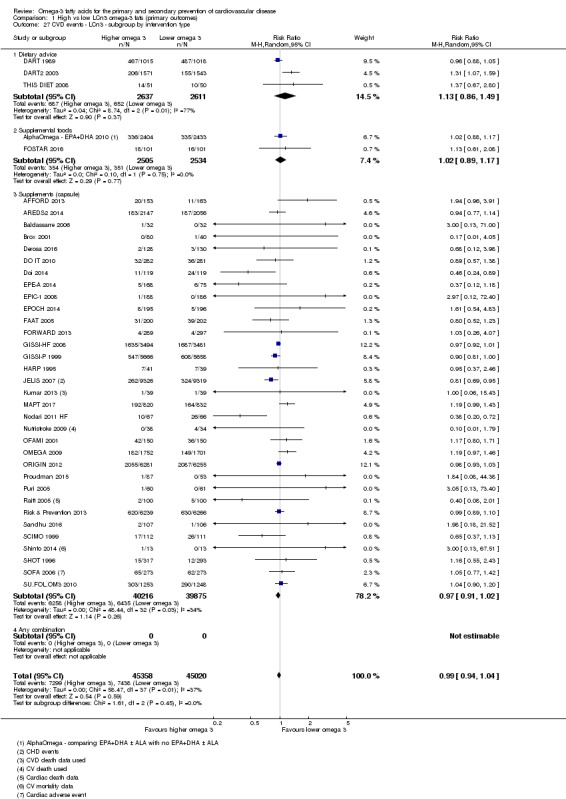
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 27 CVD events ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.30.
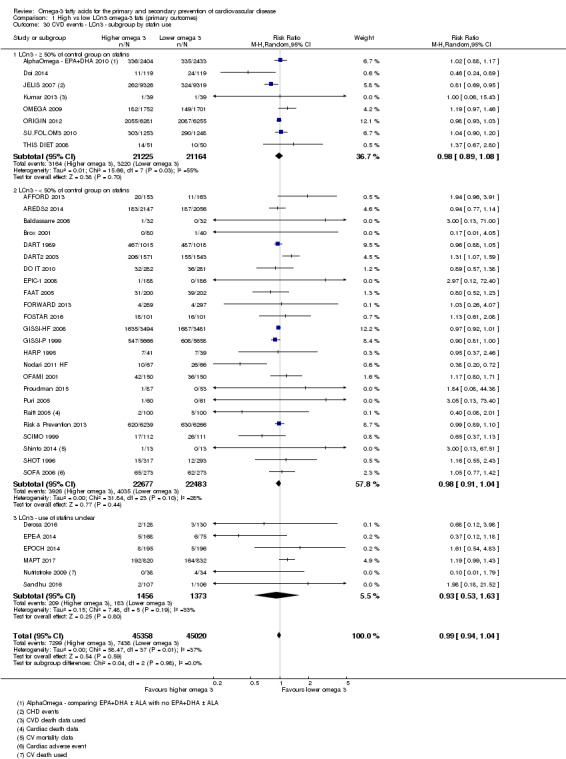
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 30 CVD events ‐ LCn3 ‐ subgroup by statin use.
Analysis 1.28.
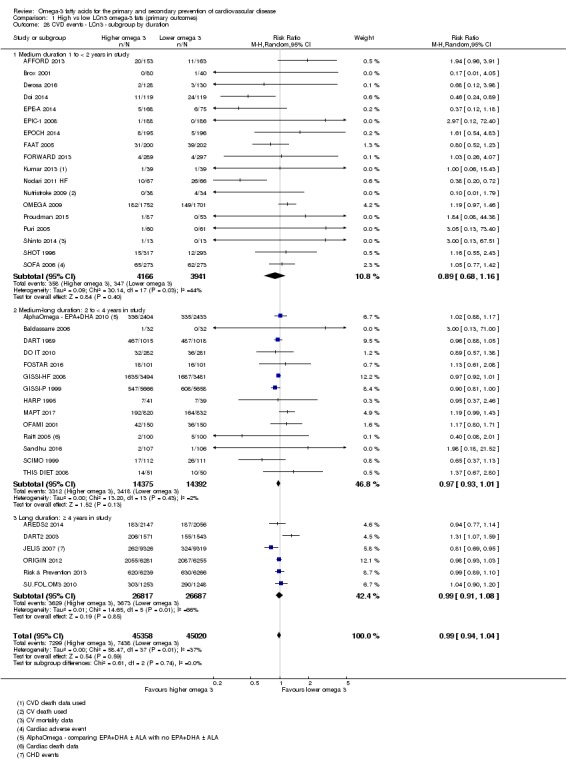
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 28 CVD events ‐ LCn3 ‐ subgroup by duration.
Meta‐regression to assess effects of LCn3 dose (or doses of ALA, omega‐6 and total PUFA), duration, intervention type, primary or secondary prevention and risk of bias (as well as a single multiple regression of the three factors with the smallest P value) showed no association between these factors and risk of cardiovascular events (all P values were ≥ 0.24, Table 12). We saw no suggestion of dose or duration effects.
Table 3.
Meta‐regression results for cardiovascular eventsa
| Variable assessed | P value |
| LCn3 dose | 0.91 |
| ALA dose | 0.70 |
| omega‐6 dose | 0.34 |
| Total PUFA dose | 0.34 |
| Duration, months | 0.62 |
| Primary or secondary CVD prevention | 0.78 |
| Food or capsule | 0.83 |
| Risk of bias | 0.24 |
| Risk of bias + PUFA dose + Omega‐6 dose |
0.25 0.87 0.83 |
ALA: alpha‐linolenic acid; CVD: cardiovascular disease; LCn3: long‐chain omega‐3 fatty acids; PUFA: poly‐unsaturated fatty acids.
aRandom‐effects meta‐regression exploring effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose, study duration, primary or secondary prevention, food or capsule intervention, and summary risk of bias (low or moderate to high) on cardiovascular events. We ran the meta‐regression using all included trials that reported this outcome in this review, and its sister reviews (update of Hooper 2018, and Abdelhamid 2018). For each variable the P value presented represents probability that the relationship was due to chance (as we had limited power we assumed a true relationship when P < 0.10). Meta‐regression was of each variable singly, plus a multivariate meta‐regression of the 3 single variables with lowest P values. See methods for further information.
GRADE assessment suggested high‐quality evidence that LCn3 intake makes little or no difference to risk of cardiovascular events (high‐quality/certainty evidence).
Coronary heart mortality (LCn3)
Moderate‐quality evidence suggests that long‐chain omega‐3 fat intake probably makes little or no difference to coronary heart mortality.
There was a suggestion that increasing LCn3 fats reduced the risk of coronary heart mortality by 7% (RR 0.93, 95% CI 0.79 to 1.09, I2 = 35%) in 21 trials reporting 1596 events in more than 73,000 participants (Analysis 1.31). Sensitivity analyses using a fixed‐effect model suggested a 6% reduction in CHD mortality (Analysis 1.32).
Analysis 1.31.
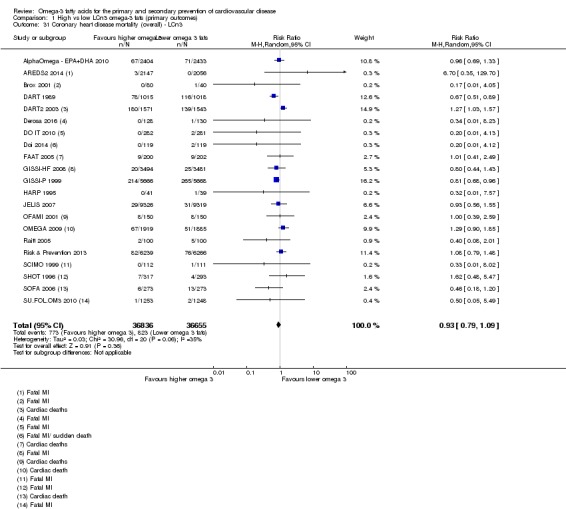
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 31 Coronary heart disease mortality (overall) ‐ LCn3.
Analysis 1.32.
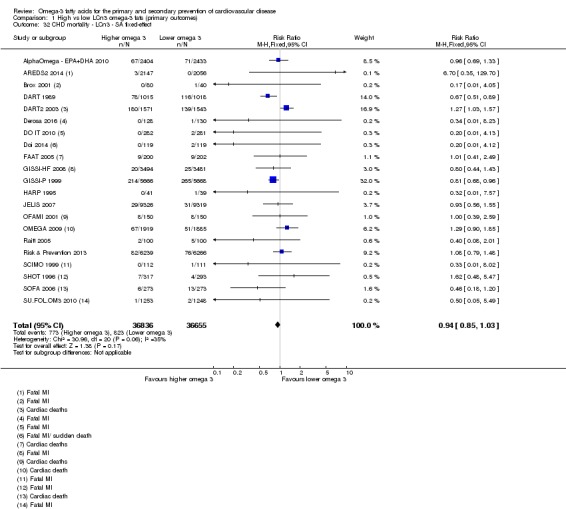
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 32 CHD mortality ‐ LCn3 ‐ SA fixed‐effect.
However, retaining only RCTs at low summary risk of bias, meta‐analysis of seven trials with more than 16,000 participants and 283 CHD deaths suggested no effect of LCn3 fats on CHD deaths (RR 1.00, 95% CI 0.72 to 1.37, I2 = 18%, Analysis 1.33). Sensitivity analyses retaining only trials with low risk of compliance bias suggested a 5% increase in risk with LCn3, but retaining only larger trials suggested a 7% reduction (Analysis 1.34). The funnel plot suggested that some smaller studies with higher RRs were missing (Figure 5), and if added back these would increase the RR.
Analysis 1.33.
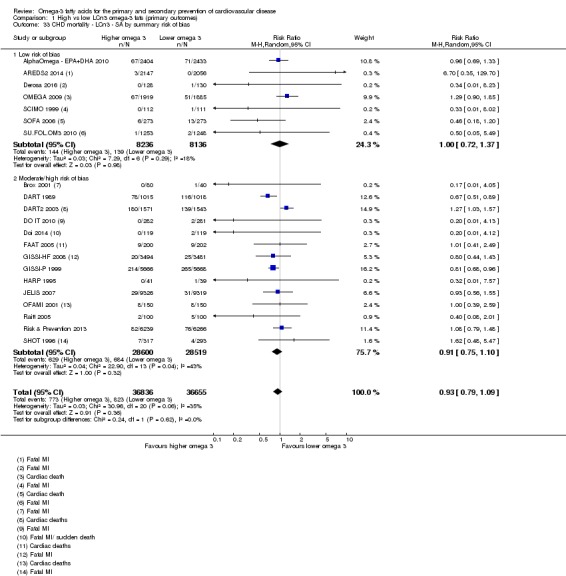
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 33 CHD mortality ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.34.
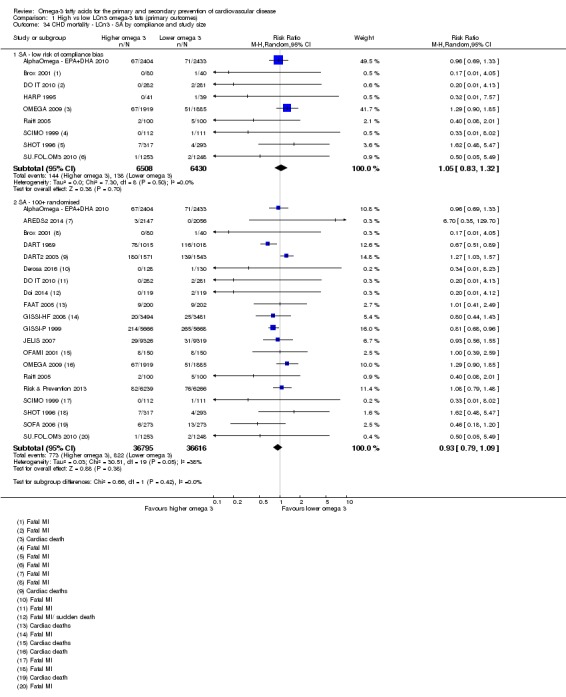
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 34 CHD mortality ‐ LCn3 ‐ SA by compliance and study size.
Figure 5.
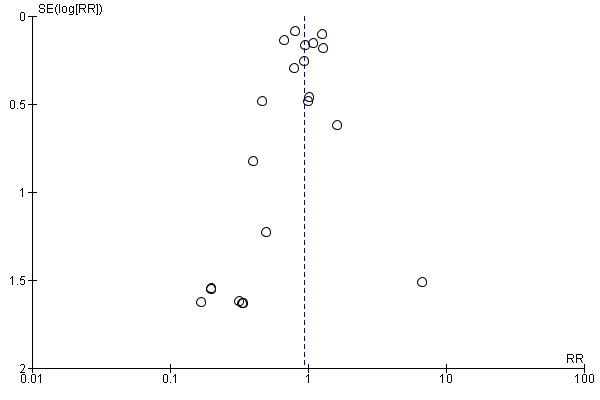
Funnel plot of comparison: 1 High vs low LCn3 omega‐3 fats (primary outcomes), outcome: 1.31 Coronary heart disease mortality (overall) – LCn3.
When we added this outcome we had pre‐specified that we would use the first of the following list reported in any trial: coronary death, ischaemic heart disease (IHD) death, fatal MI and cardiac death. We used cardiac death only when no other outcomes in this category were available, and we ran a sensitivity analysis omitting cardiac death as it potentially includes other causes of death in addition to CHD, such as cardiomyopathies and congenital and valvular heart diseases (though numbers are likely to be small). Omitting cardiac death resulted in a 17% reduction in CHD deaths with LCn3 (RR 0.83, 95% CI 0.74 to 0.94, I2 = 0%, 16 trials including 65,325 participants, Analysis 1.35).
Analysis 1.35.
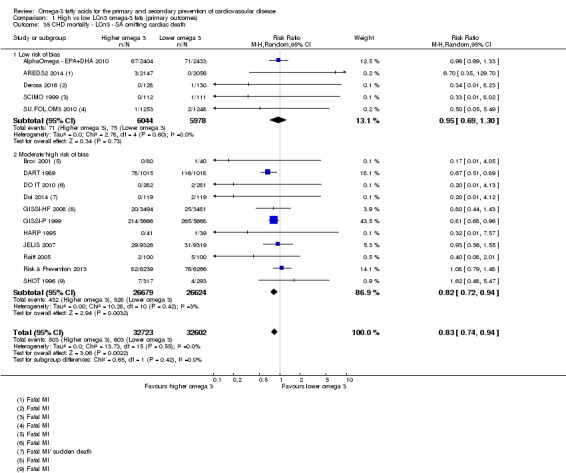
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 35 CHD mortality ‐ LCn3 ‐ SA omitting cardiac death.
There were no statistically significant differences between subgroups for type of intervention (Analysis 1.38), dose (Analysis 1.36), baseline CVD risk (Analysis 1.40), statin use (Analysis 1.41) or baseline coronary artery disease status (Analysis 1.42). There were important differences between subgroups for study duration, with no effect in shorter trials (1 to < 2 years), a significant protective effect of LCn3 fats in medium‐ to long‐term trials (2 to < 4 years) and an almost statistically significant harmful effect in long trials (≥ 4 years, Analysis 1.39), so we did not assume any differential effect by duration. The differences between subgroups for replacement disappeared when we omitted the 'replacement unclear' category (altering the test for subgroup differences to P = 0.46, Analysis 1.37).
Analysis 1.38.
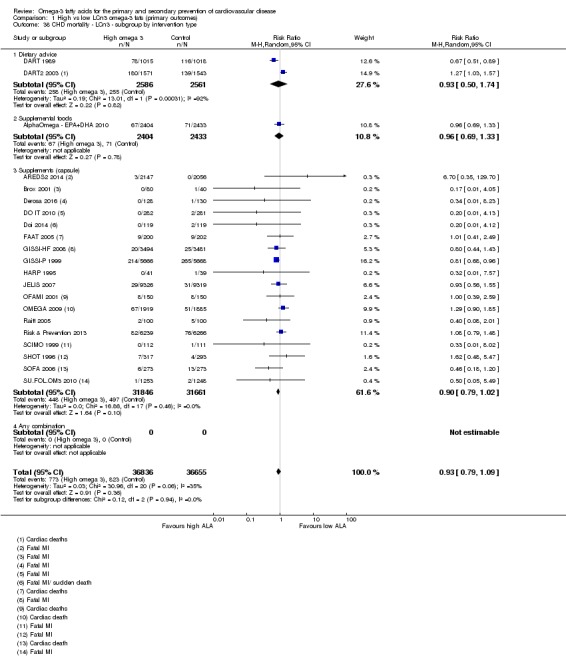
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 38 CHD mortality ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.36.
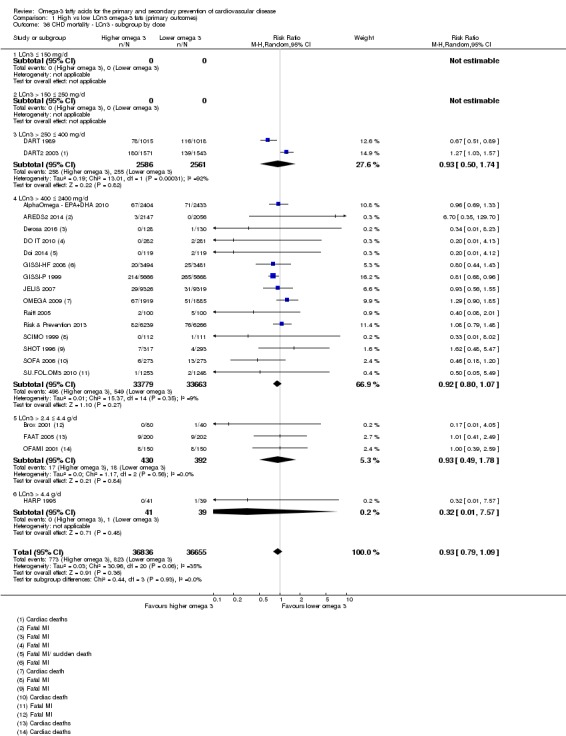
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 36 CHD mortality ‐ LCn3 ‐ subgroup by dose.
Analysis 1.40.
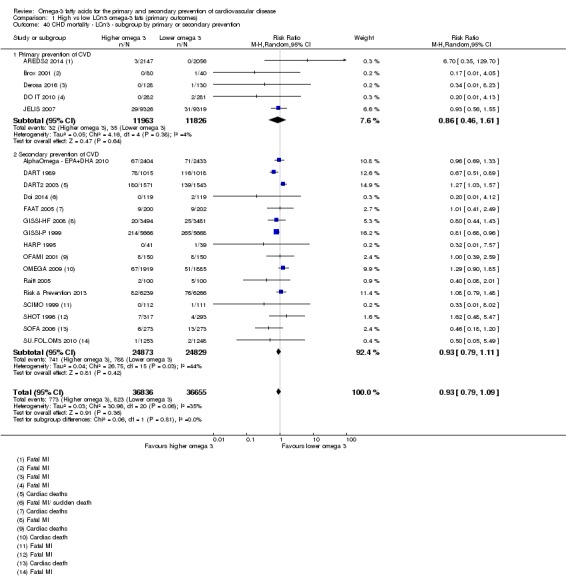
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 40 CHD mortality ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 1.41.
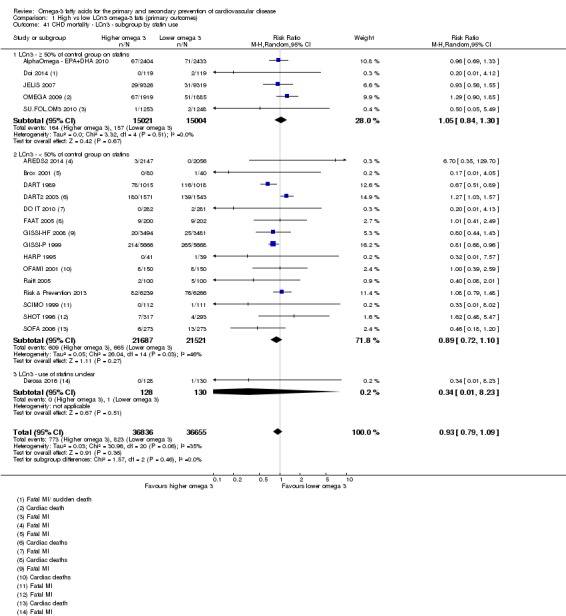
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 41 CHD mortality ‐ LCn3 ‐ subgroup by statin use.
Analysis 1.42.
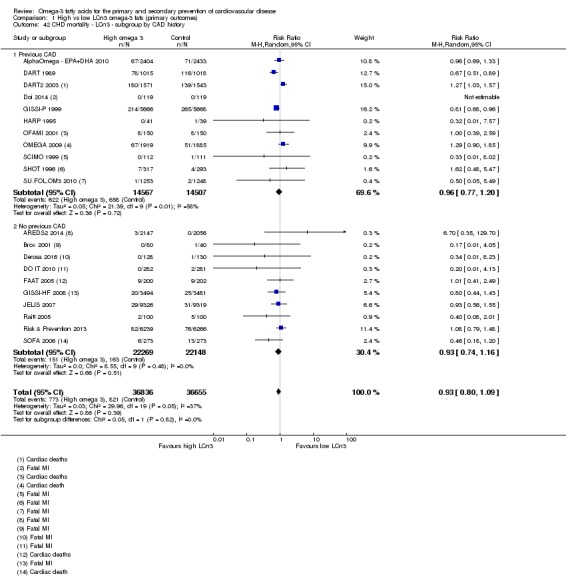
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 42 CHD mortality ‐ LCn3 ‐ subgroup by CAD history.
Analysis 1.39.
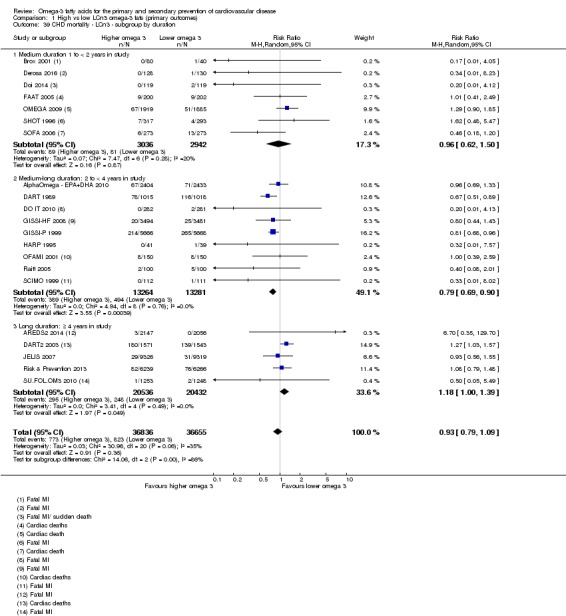
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 39 CHD mortality ‐ LCn3 ‐ subgroup by duration.
Analysis 1.37.
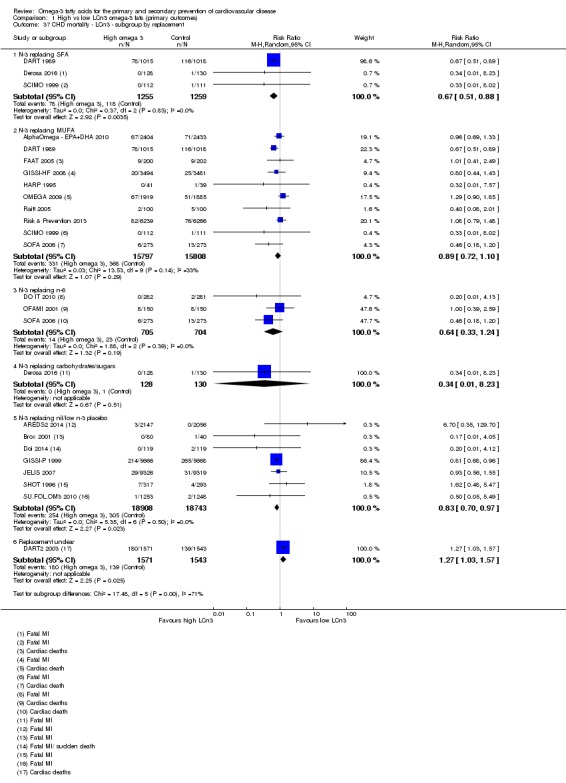
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 37 CHD mortality ‐ LCn3 ‐ subgroup by replacement.
Meta‐regression to assess effects of LCn3 dose on CHD mortality found no relationship (P = 0.94, Table 13). Similarly we saw no relationships between ALA dose, omega‐6 dose, total PUFA dose, duration, intervention type, primary or secondary prevention or risk of bias and CHD deaths (all P values were > 0.40, Table 13). Multiple regression of the three factors with the smallest P value found no factors associated with risk of CHD deaths. We saw no suggestion of dose or duration effects.
Table 4.
Meta‐regression results for CHD deathsa
| Variable assessed | P value |
| LCn3 dose | 0.94 |
| ALA dose | 0.93 |
| Omega‐6 dose | 0.66 |
| Total PUFA dose | 0.64 |
| Duration, months | 0.41 |
| Primary or secondary CVD prevention | 0.63 |
| Food or capsule | 0.78 |
| Risk of bias | 0.89 |
| Duration + Primary or secondary prevention + PUFA dose |
0.73 0.90 0.76 |
ALA: alpha‐linolenic acid; CVD: cardiovascular disease; LCn3: long‐chain omega‐3 fatty acids; PUFA: poly‐unsaturated fatty acids.
aRandom‐effects meta‐regression exploring effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose, study duration, primary or secondary prevention, food or capsule intervention, and summary risk of bias (low or moderate to high) on CHD mortality. We ran the meta‐regression using all included trials that reported this outcome in this review, and its sister reviews (update of Hooper 2018, and Abdelhamid 2018). For each variable the P value presented represents probability that the relationship was due to chance (as we had limited power we assumed a true relationship when P < 0.10). Meta‐regression was of each variable singly, plus a multivariate meta‐regression of the 3 single variables with lowest P values. See methods for further information.
The suggestion of a protective effect disappeared in studies at low summary risk of bias, the funnel plot suggests that the true risk ratio is higher than the main estimate, and there was no suggestion of dose or duration effects, so we summarised the evidence by assuming little or no effect of LCn3 on CHD mortality. GRADE assessment suggested moderate‐quality evidence that long‐chain omega‐3 fat intake probably makes little or no difference to coronary heart mortality (moderate‐quality/certainty evidence, downgraded once for imprecision).
Coronary heart disease events (LCn3)
Moderate‐quality evidence suggests that long‐chain omega‐3 fat intake probably makes little or no difference to risk of coronary heart events.
The main meta‐analysis suggested a 7% reduction in people experiencing CHD events with higher intake of LCn3 fats (RR 0.93, 95% CI 0.88 to 0.97, I2 = 0%, 5469 events, > 84,000 participants, Analysis 1.43). The funnel plot suggested that some smaller studies with more cardiovascular deaths in the intervention group were missing (some small study bias, Figure 6) – if this were the case then adding the missing studies would increase the relative risk.
Analysis 1.43.
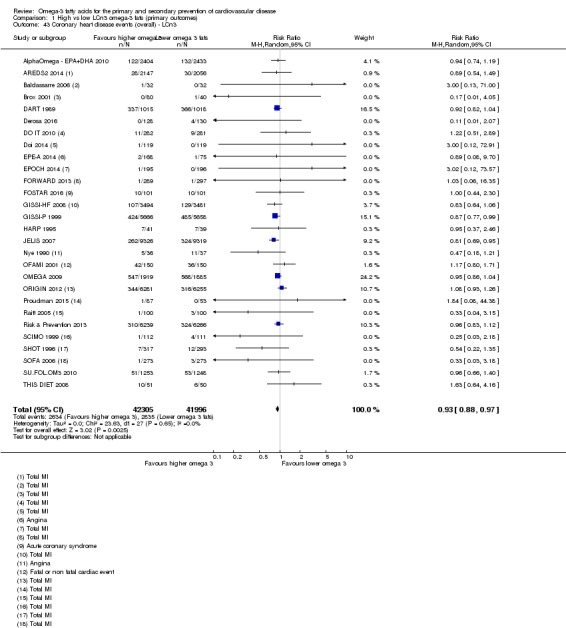
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 43 Coronary heart disease events (overall) ‐ LCn3.
Figure 6.
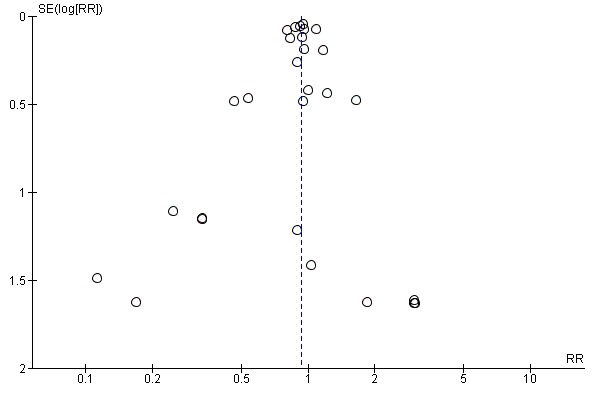
Funnel plot of comparison: 1 High vs low LCn3 omega‐3 fats (primary outcomes), outcome: 1.43 Coronary heart disease events (overall) – LCn3.
Sensitivity analyses using a fixed‐effect model did not alter the results (RR 0.92, 95% CI 0.88 to 0.97, Analysis 1.44). The protective effect was lost in studies at low summary risk of bias (Analysis 1.45), and the effect was smaller when studies were limited to those with good compliance and to larger studies (Analysis 1.46). Removing RCTs not at low summary risk of bias left 12 trials with more than 30,000 participants, 2228 of whom developed CHD (RR 0.97, 95% CI 0.90 to 1.05, I2 = 0%, Analysis 1.45).
Analysis 1.44.
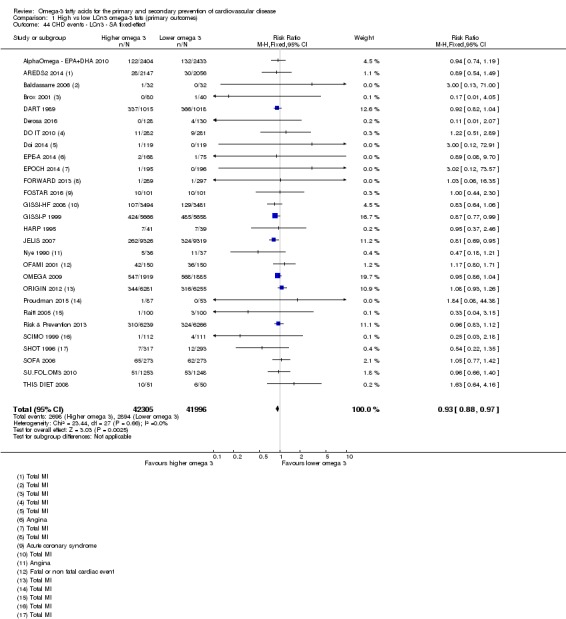
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 44 CHD events ‐ LCn3 ‐ SA fixed‐effect.
Analysis 1.45.
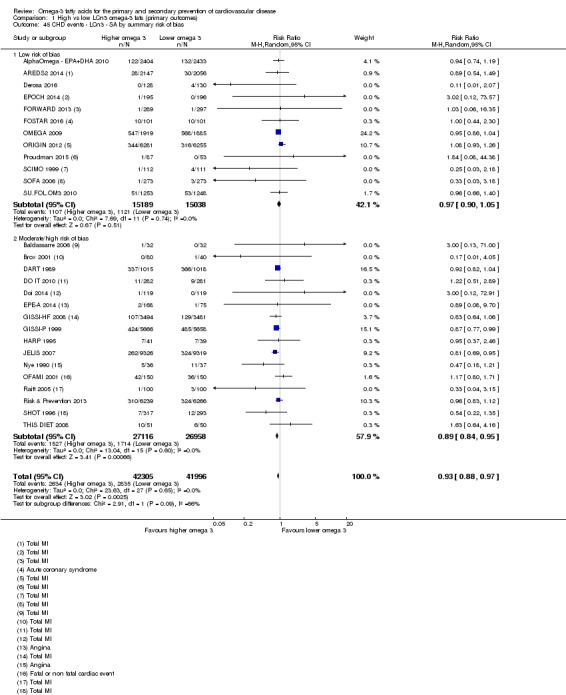
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 45 CHD events ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.46.
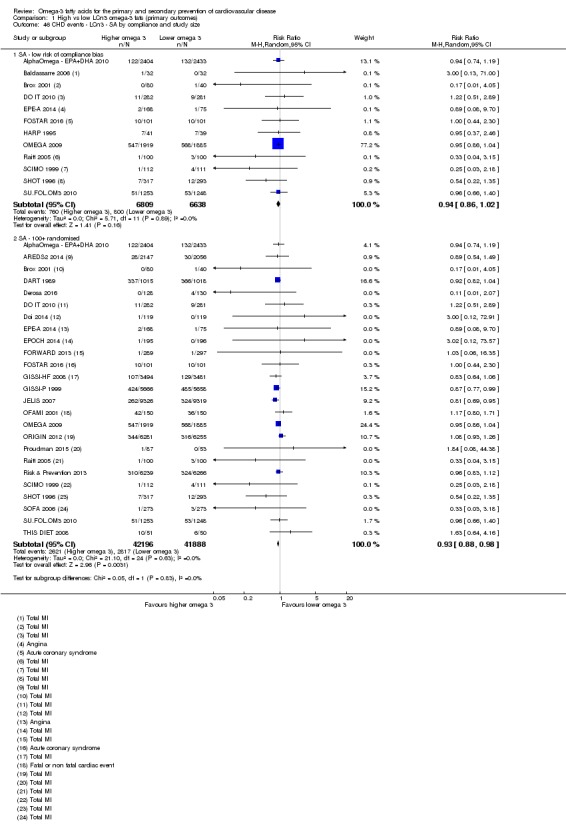
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 46 CHD events ‐ LCn3 ‐ SA by compliance and study size.
There were no statistically significant differences between subgroups (Analysis 1.47; Analysis 1.48; Analysis 1.49; Analysis 1.50; Analysis 1.51; Analysis 1.52; Analysis 1.53).
Analysis 1.47.
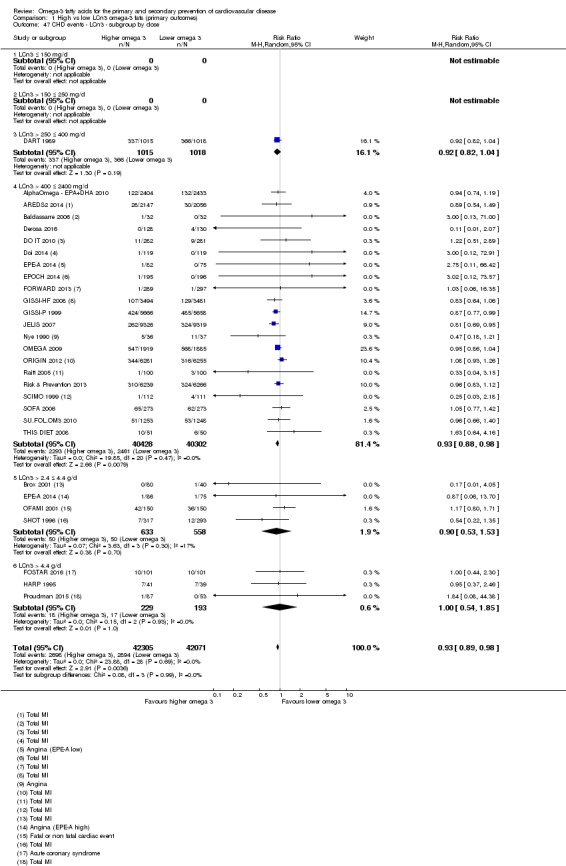
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 47 CHD events ‐ LCn3 ‐ subgroup by dose.
Analysis 1.48.
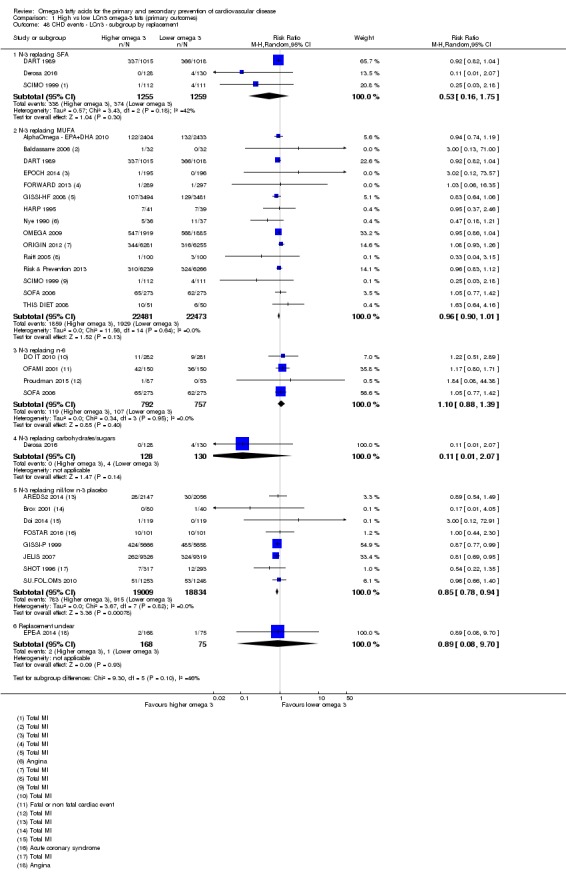
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 48 CHD events ‐ LCn3 ‐ subgroup by replacement.
Analysis 1.49.
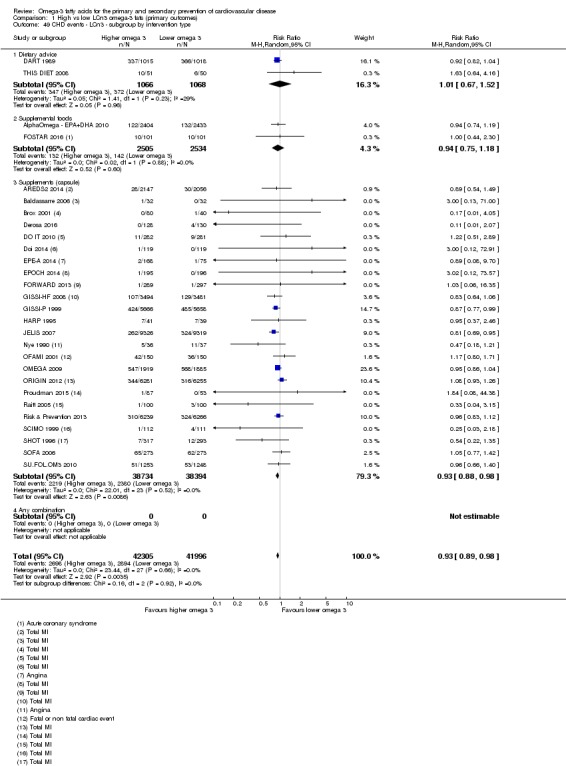
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 49 CHD events ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.50.
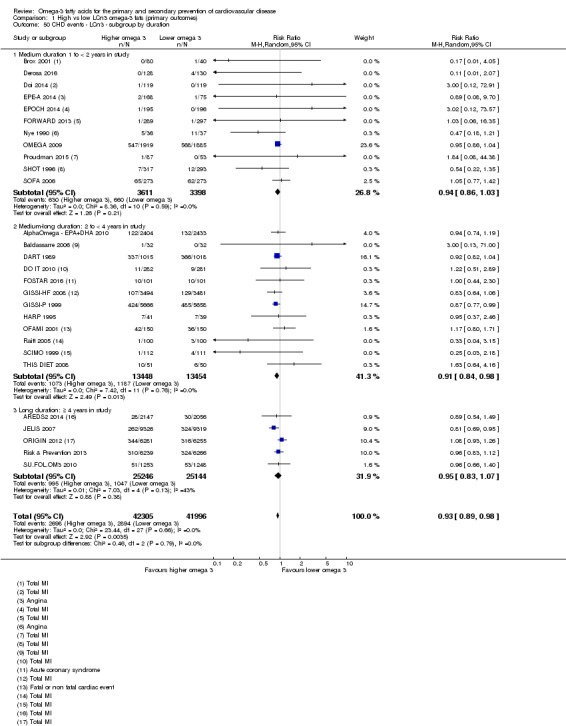
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 50 CHD events ‐ LCn3 ‐ subgroup by duration.
Analysis 1.51.
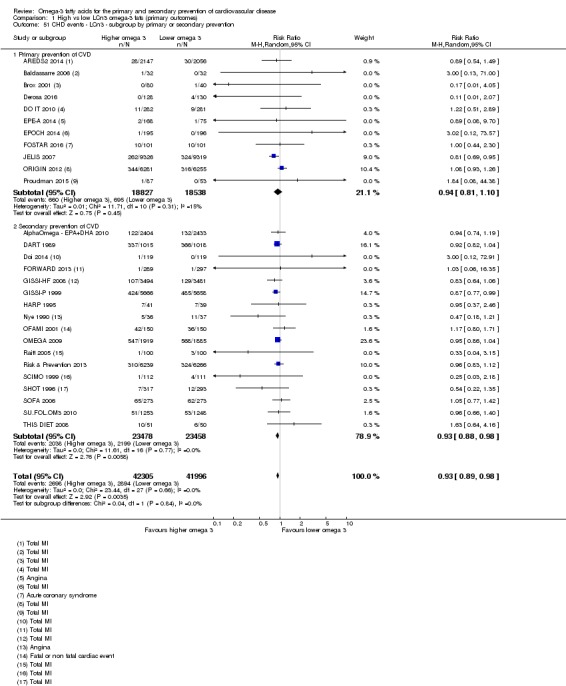
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 51 CHD events ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 1.52.
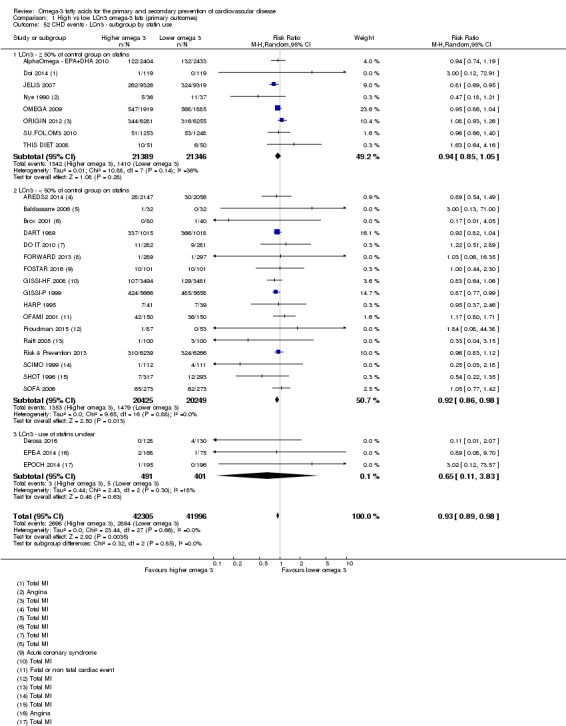
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 52 CHD events ‐ LCn3 ‐ subgroup by statin use.
Analysis 1.53.
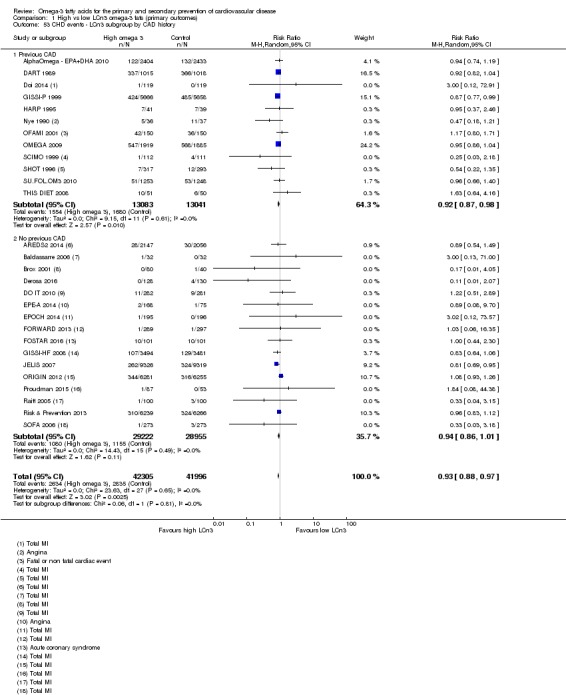
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 53 CHD events ‐ LCn3 subgroup by CAD history.
Meta‐regression to assess effects of LCn3, ALA, omega‐6, total PUFA dose and duration, intervention type, primary or secondary prevention, and risk of bias (as well as a single multiple regression of the three factors with the smallest P value) showed no association between these factors and the risk of CHD events (all P values were > 0.20, Table 14). We saw no suggestion of dose‐response or duration effects.
Table 5.
Metaregression results for CHD eventsa
| Variable assessed | P value |
| LCn3 dose | 0.68 |
| ALA dose | 0.23 |
| Omega‐6 dose | 0.84 |
| Total PUFA dose | 0.79 |
| Duration, months | 0.87 |
| Primary or secondary CVD prevention | 0.42 |
| Food or capsule | 0.91 |
| Risk of bias | 0.98 |
| ALA dose + Prim or sec prev + LCn3 dose |
0.32 0.46 0.86 |
ALA: alpha‐linolenic acid; CVD: cardiovascular disease; LCn3: long‐chain omega‐3 fatty acids; PUFA: poly‐unsaturated fatty acids.
aRandom‐effects meta‐regression exploring effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose, study duration, primary or secondary prevention, food or capsule intervention, and summary risk of bias (low or moderate to high) on CHD events. We ran the meta‐regression using all included trials that reported this outcome in this review, and its sister reviews (update of Hooper 2018, and Abdelhamid 2018). For each variable the P value presented represents probability that the relationship was due to chance (as we had limited power we assumed a true relationship when P < 0.10). Meta‐regression was of each variable singly, plus a multivariate meta‐regression of the 3 single variables with lowest P values. See methods for further information.
Because a protective effect was only apparent in studies at higher risk of bias, we were concerned that the reduction in CHD events is residual and arises from methodological weaknesses in some of the studies (there was a marginally significant difference between the group of studies at low risk of bias, and those at moderate to high risk of bias, P = 0.09, Analysis 1.45). GRADE assessment suggested moderate‐quality evidence that long‐chain omega‐3 fat intake probably makes little or no difference to risk of coronary heart events (moderate‐quality/certainty evidence, downgraded once for risk of bias).
Stroke (LCn3)
Moderate‐quality evidence suggests that long‐chain omega‐3 fat intake probably makes little or no difference to risk of experiencing a stroke.
There was a suggestion that increasing intake of LCn3 results in a 6% higher risk of stroke (RR 1.06, 95% CI 0.96 to 1.16, I2 = 0%, 1822 reported strokes, Analysis 1.54), and the funnel plot did not suggest any small study bias (not shown).
Analysis 1.54.
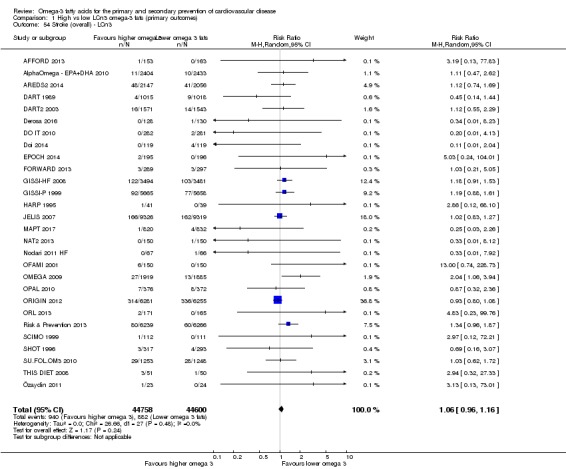
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 54 Stroke (overall) ‐ LCn3.
Sensitivity analyses removing trials not at low summary risk of bias left 12 trials with 888 participants experiencing strokes, suggesting little or no effect of LCn3 fats on stroke (RR 0.98, 95% CI 0.86 to 1.12, I2 = 0%, Analysis 1.56). Using fixed‐effect meta‐analysis also suggested a 6% increase in risk (Analysis 1.55), while sensitivity analysis removing trials with risk from poor compliance and smaller trials suggested there may be harm from increased LCn3 (Analysis 1.57).
Analysis 1.56.
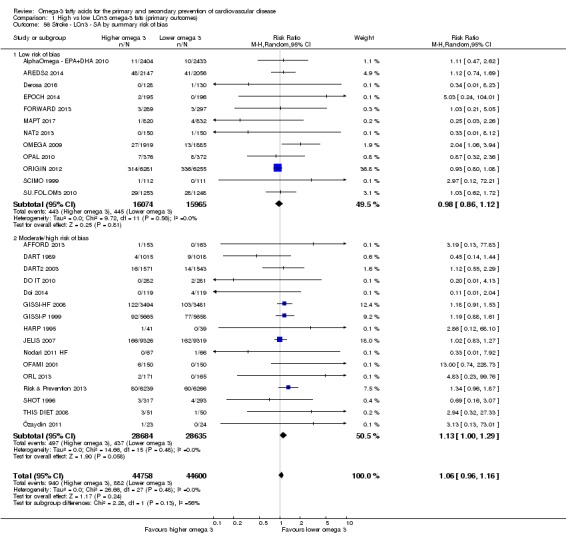
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 56 Stroke ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.55.
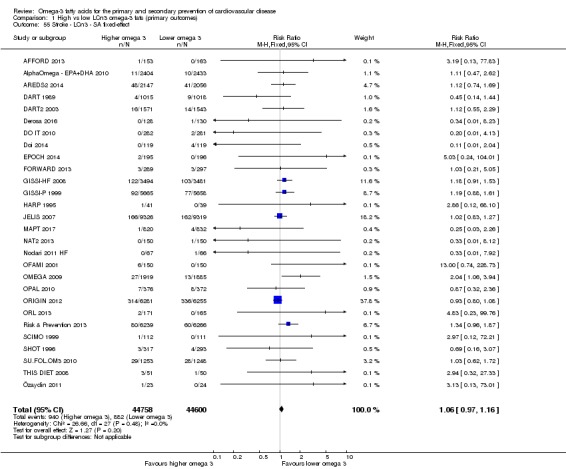
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 55 Stroke ‐ LCn3 ‐ SA fixed‐effect.
Analysis 1.57.
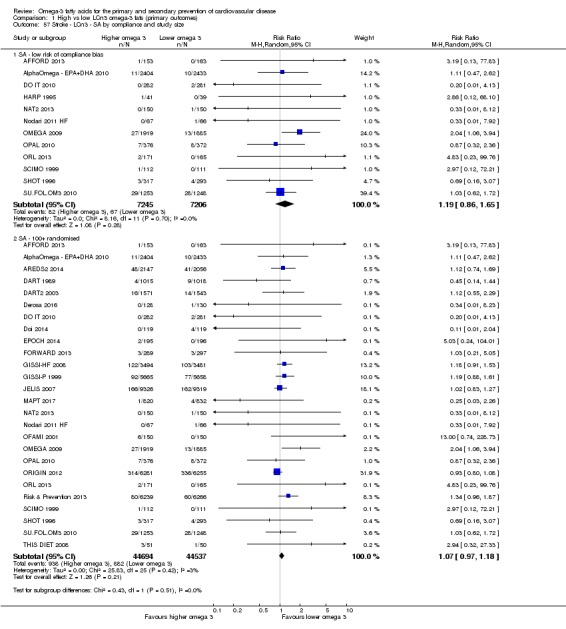
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 57 Stroke ‐ LCn3 ‐ SA by compliance and study size.
When studies reported stroke type separately, the risk of both haemorrhagic (RR 1.20, 95% CI 0.85 to 1.69, I2 = 0%, 130 participants with events) and ischaemic stroke were increased (RR 1.09, 95% CI 0.89 to 1.33, I2 = 13%, 556 people with events, in 8 trials each, Analysis 1.58). Five trials reported only 40 participants experiencing transient ischaemic attack (TIA), suggesting a 26% reduction in risk but with very wide confidence intervals (TIAs were not included in any other stroke categories, Analysis 1.58). Subgrouping did not suggest important differences by intervention type, replacement, statin use, trial duration or dose (Analysis 1.59; Analysis 1.60; Analysis 1.61; Analysis 1.62; Analysis 1.64). There was a suggestion of increased stroke risk in people with CVD at baseline (RR 1.21, 95% CI 1.05 to 1.40, I2 = 0%, with differences in effect size between subgroups by primary or secondary prevention, P = 0.02, Analysis 1.63).
Analysis 1.58.
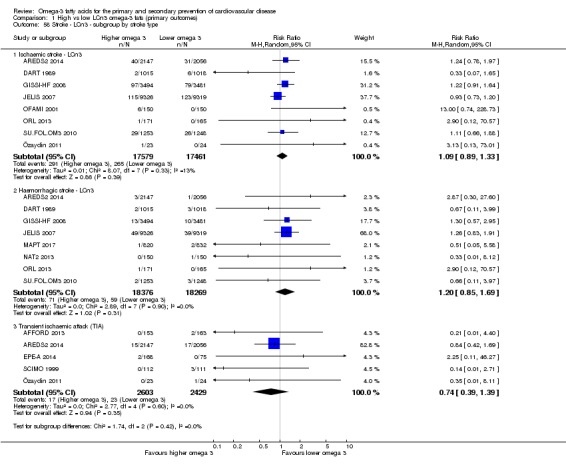
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 58 Stroke ‐ LCn3 ‐ subgroup by stroke type.
Analysis 1.59.
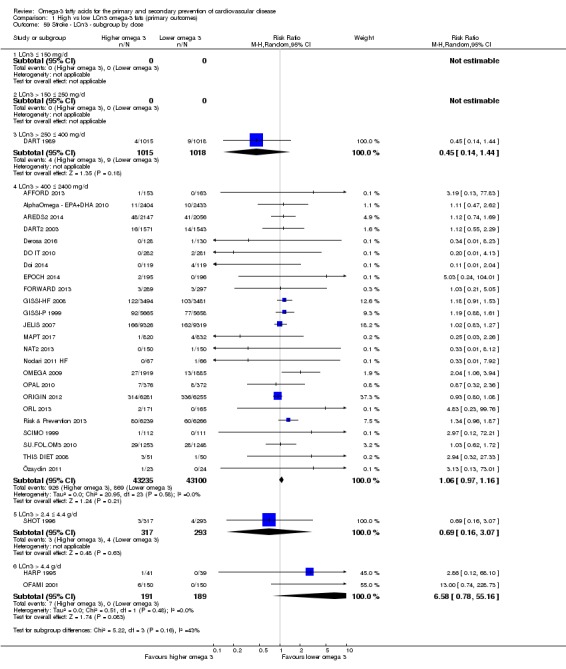
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 59 Stroke ‐ LCn3 ‐ subgroup by dose.
Analysis 1.60.
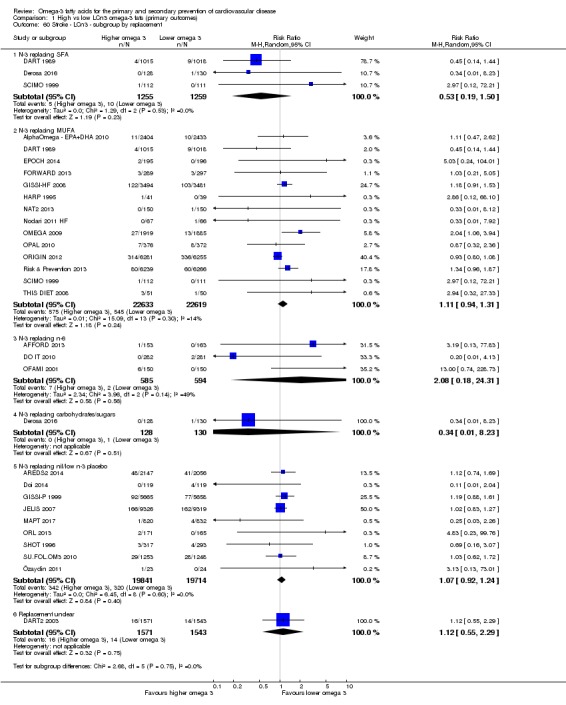
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 60 Stroke ‐ LCn3 ‐ subgroup by replacement.
Analysis 1.61.
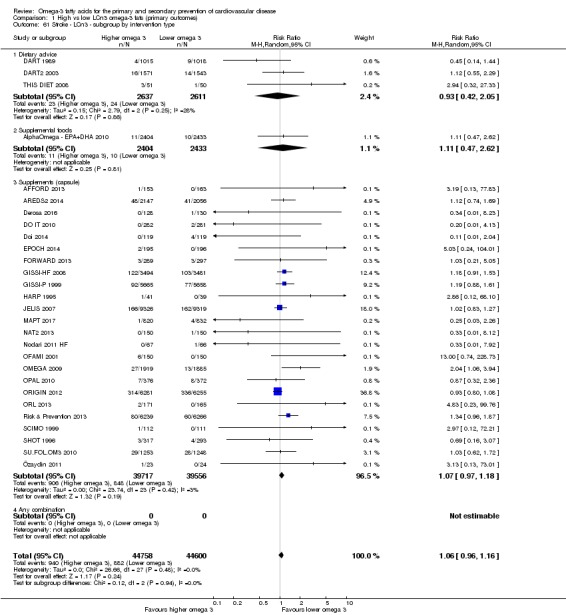
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 61 Stroke ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.62.
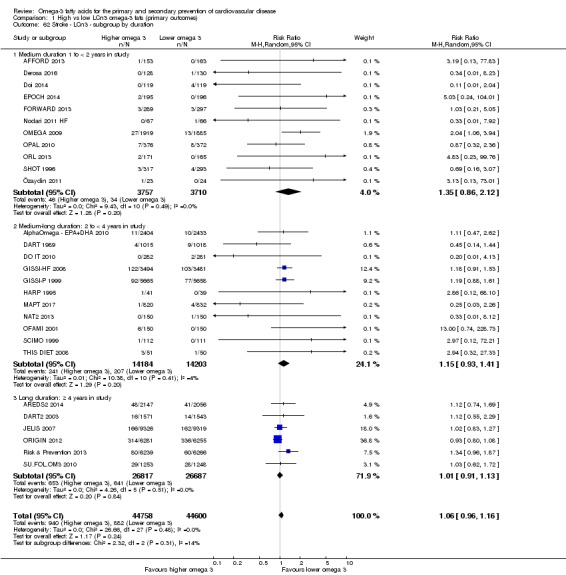
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 62 Stroke ‐ LCn3 ‐ subgroup by duration.
Analysis 1.64.
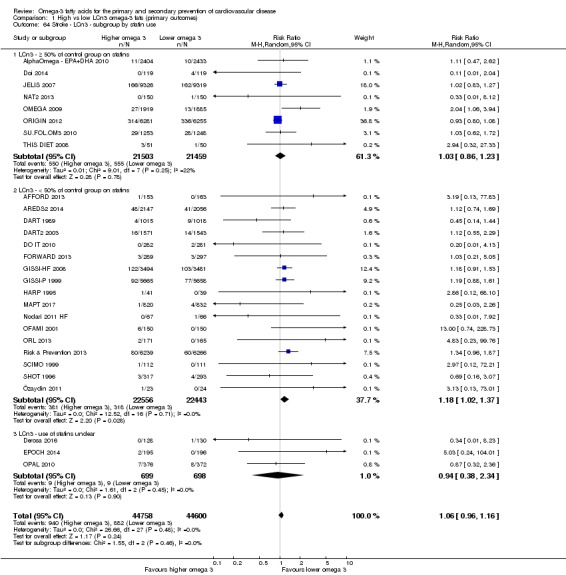
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 64 Stroke ‐ LCn3 ‐ subgroup by statin use.
Analysis 1.63.
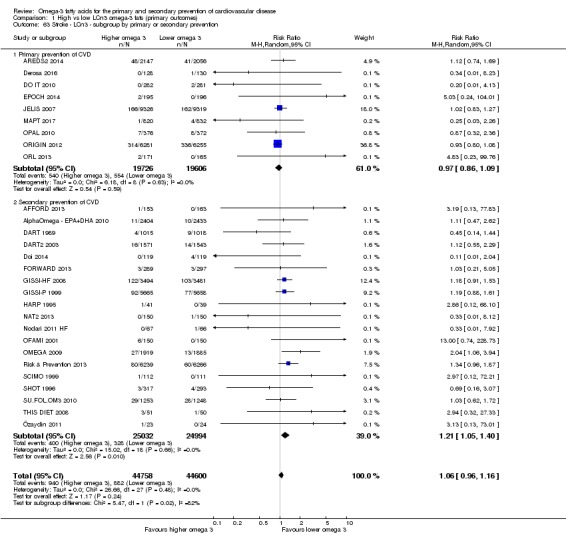
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 63 Stroke ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Meta‐regression to assess effects of LCn3 dose did not find any clear dose response on risk of stroke (P = 0.42, Table 15). Univariate meta‐regression suggested that trials of shorter duration showed a greater effect on reducing stroke (P = 0.012) and that LCn3 fats may be more protective against stroke in secondary prevention than primary (P = 0.04, Table 15). There were no clear relationships between dose of any PUFA type, risk of bias, or use of food or capsules, and no significant relationships in multivariate meta‐regression.
Table 6.
Metaregression results for strokea
| Variable assessed | P value | Coefficient sign where P < 0.10 |
| LCn3 dose | 0.42 | — |
| ALA dose | 0.81 | — |
| Omega‐6 dose | 0.19 | — |
| Total PUFA dose | 0.21 | — |
| Duration, months | 0.012 | Negative (greater effect with shorter duration) |
| Primary or secondary CVD prevention | 0.04 | Positive (greater effect with secondary prevention) |
| Food or capsule | 0.21 | — |
| Risk of bias | 0.25 | — |
| Duration + primary or secondary prevention + omega‐6 |
0.21 0.67 0.38 |
— |
ALA: alpha‐linolenic acid; CVD: cardiovascular disease; LCn3: long‐chain omega‐3 fatty acids; PUFA: poly‐unsaturated fatty acids.
aRandom‐effects meta‐regression exploring effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose, study duration, primary or secondary prevention, food or capsule intervention, and summary risk of bias (low or moderate to high) on stroke. We ran the meta‐regression using all included trials that reported this outcome in this review, and its sister reviews (update of Hooper 2018, and Abdelhamid 2018). For each variable the P value presented represents probability that the relationship was due to chance (as we had limited power we assumed a true relationship when P < 0.10). Meta‐regression was of each variable singly, plus a multivariate meta‐regression of the 3 single variables with lowest P values. See methods for further information.
Given that studies at low summary risk of bias suggested little or no effect of LCn3 on stroke risk, and there were no dose‐response or duration relationships, we assumed little or no true effect. GRADE assessment suggests moderate‐quality evidence that long‐chain omega‐3 fat intake probably makes little or no difference to risk of experiencing a stroke (moderate‐quality/certainty evidence, downgraded once for imprecision).
Arrhythmia (LCn3)
Moderate‐quality evidence suggests that long‐chain omega‐3 fat intake probably makes little or no difference to risk of arrhythmia.
There was no effect of LCn3 fats on incidence of new or recurrent (fatal and non‐fatal) arrhythmias (RR 0.97, 95% CI 0.90 to 1.05, I2 = 43%, 3788 events in > 53,000 participants, Analysis 1.65). The funnel plot was not interpretable as studies were clustered (not shown).
Analysis 1.65.
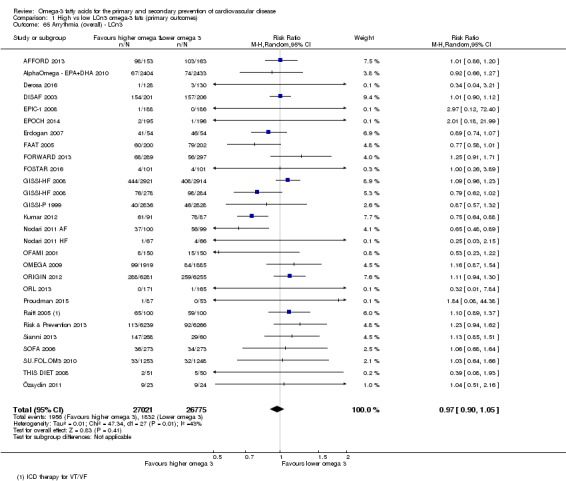
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 65 Arrythmia (overall) ‐ LCn3.
Sensitivity analyses removing trials not at low summary risk of bias left 10 trials with 1146 events (> 25,000 participants), suggesting a 10% increase in risk of arrhythmia with increased LCn3 (RR 1.10, 95% CI 0.98 to 1.23, I2 = 0%, Analysis 1.67). Restricting the analysis to studies at low summary risk of bias removed heterogeneity, and there was a statistically significant difference in effect size between subgroups at low versus moderate to high risk of bias (P = 0.03, Analysis 1.67). Using fixed‐effect methodology did not alter the apparent lack of effect of LCn3 on arrhythmia (Analysis 1.66), and sensitivity analysis by compliance and study size also suggested little or no effect of LCn3 on arrhythmia (Analysis 1.68).
Analysis 1.67.
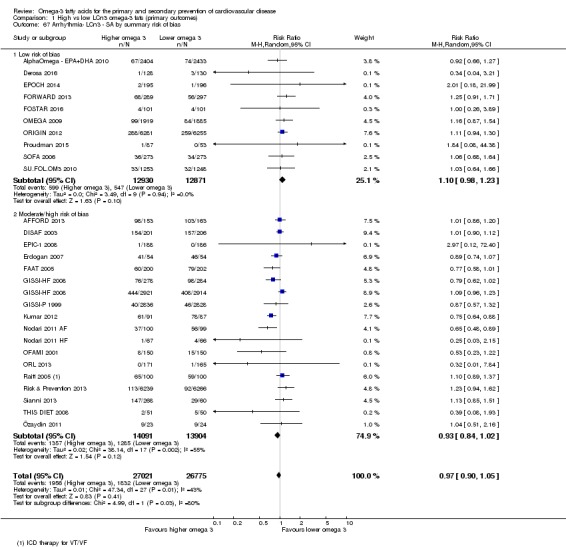
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 67 Arrhythmia‐ LCn3 ‐ SA by summary risk of bias.
Analysis 1.66.
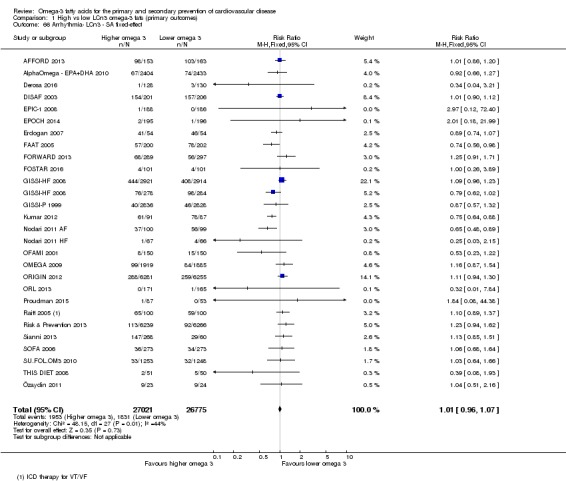
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 66 Arrhythmia‐ LCn3 ‐ SA fixed‐effect.
Analysis 1.68.
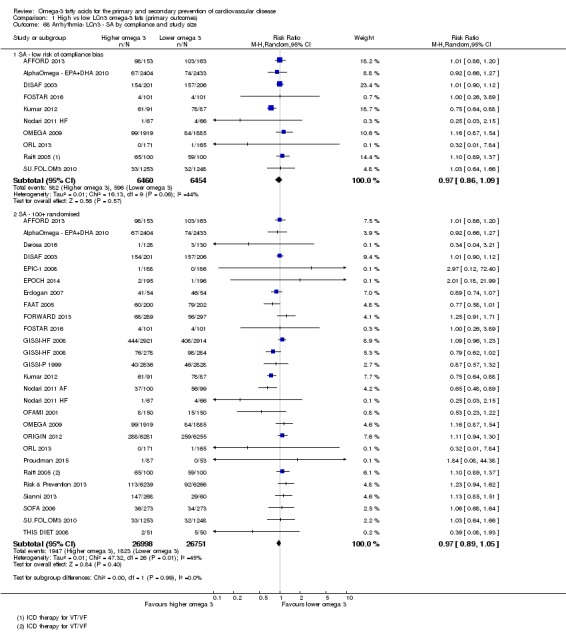
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 68 Arrhythmia‐ LCn3 ‐ SA by compliance and study size.
Subgrouping by new or recurrent arrhythmias suggested differences between subgroups, with LCn3 increasing the risk of new arrhythmias and reducing the risk of recurrent arrhythmia (Analysis 1.69). There were also statistically significant differences between subgroups by fatality, with a suggestion that LCn3 increased the risk of fatal arrhythmias but reduced the risk of non‐fatal arrhythmias (Analysis 1.70). Subgroup analyses by type of intervention, replacement, baseline CVD risk, statin use, dose and study duration did not suggest any statistically significant differences between subgroups (Analysis 1.71; Analysis 1.72; Analysis 1.73; Analysis 1.74; Analysis 1.75; Analysis 1.76).
Analysis 1.69.
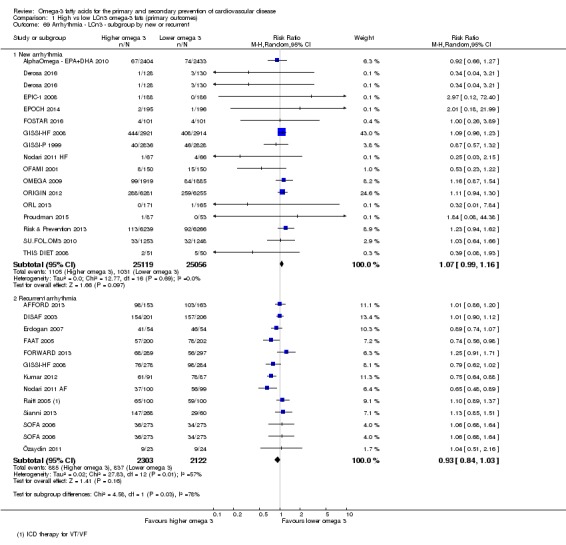
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 69 Arrhythmia ‐ LCn3 ‐ subgroup by new or recurrent.
Analysis 1.70.
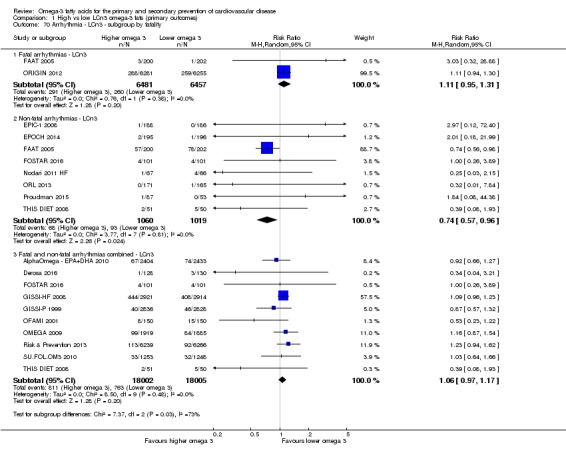
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 70 Arrhythmia ‐ LCn3 ‐ subgroup by fatality.
Analysis 1.71.
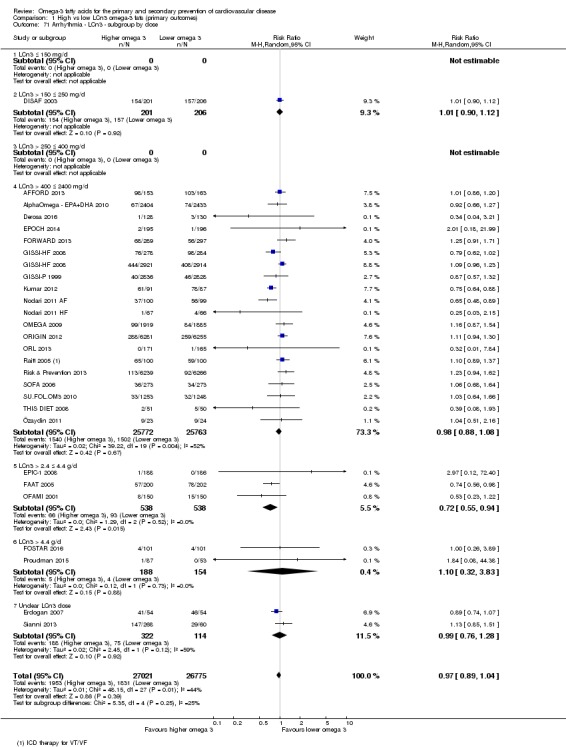
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 71 Arrhythmia ‐ LCn3 ‐ subgroup by dose.
Analysis 1.72.
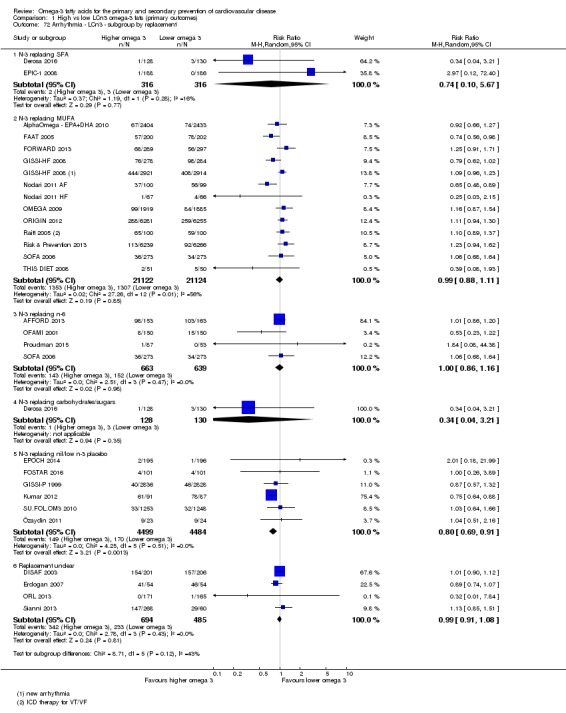
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 72 Arrhythmia ‐ LCn3 ‐ subgroup by replacement.
Analysis 1.73.
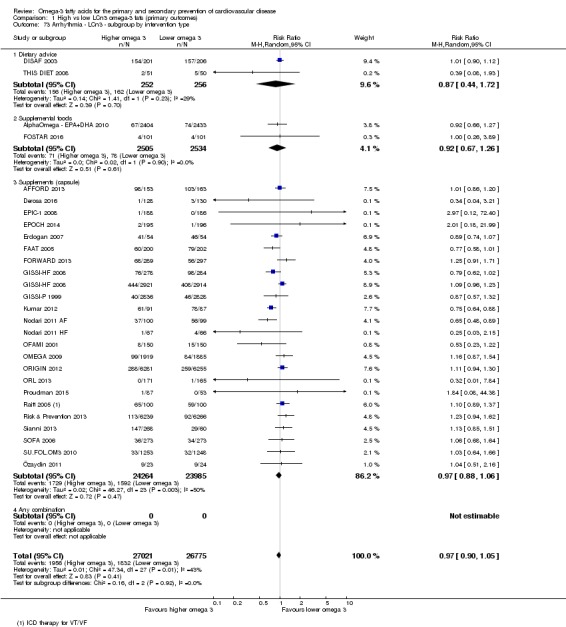
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 73 Arrhythmia ‐ LCn3 ‐ subgroup by intervention type.
Analysis 1.74.
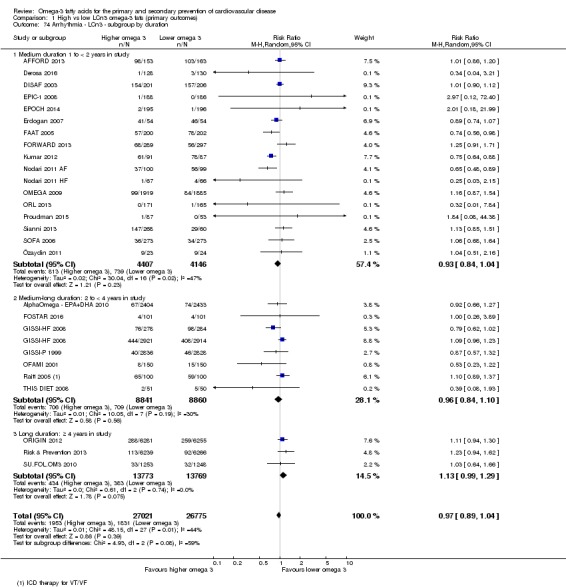
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 74 Arrhythmia ‐ LCn3 ‐ subgroup by duration.
Analysis 1.75.
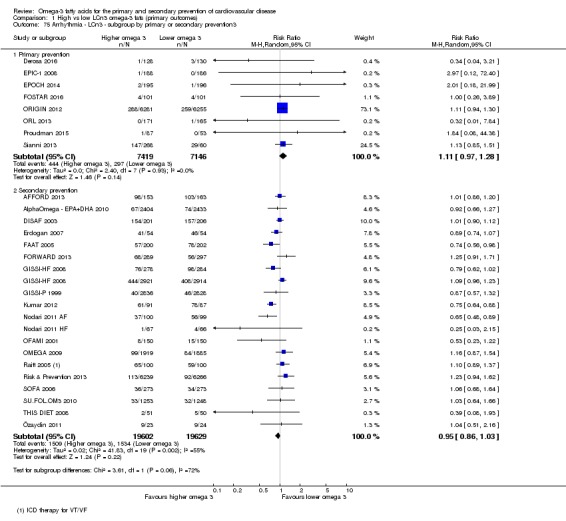
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 75 Arrhythmia ‐ LCn3 ‐ subgroup by primary or secondary prevention3.
Analysis 1.76.
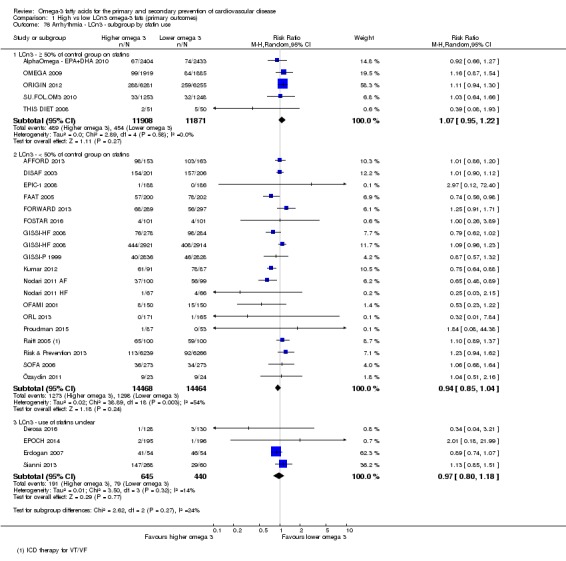
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 76 Arrhythmia ‐ LCn3 ‐ subgroup by statin use.
Meta‐regression suggested a marginally significant negative dose‐response relationship with LCn3 fats, such that lower dose was associated with lower risk of arrhythmia (P = 0.06, Table 16). The effect remained marginally significant when we controlled for primary or secondary prevention and study duration (P = 0.09). Because of the negative direction of this apparent dose‐response relationship, we assumed it was likely to be a chance occurrence resulting from running a large number of statistical tests. There was also a marginally significant relationship for arrhythmia with primary versus secondary prevention, suggesting greater reduction in arrhythmia risk in primary prevention (P = 0.07, Table 16). There were no other suggested relationships.
Table 7.
Meta‐regression results for arrhythmiasa
| Variable assessed | P value | Coefficient sign where P < 0.10 |
| LCn3 dose | 0.06 | Negative (greater effect at lower dose) |
| ALA dose | 0.67 | — |
| Omega‐6 dose | 0.59 | — |
| Total PUFA dose | 0.54 | — |
| Duration, months | 0.16 | — |
| Primary or secondary CVD prevention | 0.07 | Negative (greater effect with primary prevention) |
| Food or capsule | 0.82 | — |
| Risk of bias | 0.51 | — |
| LCn3 dose + Primary secondary prevention + duration |
0.09 0.12 0.46 |
— |
ALA: alpha‐linolenic acid; CVD: cardiovascular disease; LCn3: long‐chain omega‐3 fatty acids; PUFA: poly‐unsaturated fatty acids.
aRandom‐effects meta‐regression exploring effects of LCn3 dose, ALA dose, omega‐6 dose, total PUFA dose, study duration, primary or secondary prevention, food or capsule intervention, and summary risk of bias (low or moderate to high) on arrhythmia. We ran the meta‐regression using all included trials that reported this outcome in this review, and its sister reviews (update of Hooper 2018, and Abdelhamid 2018). For each variable the P value presented represents probability that the relationship was due to chance (as we had limited power we assumed a true relationship when P < 0.10). Meta‐regression was of each variable singly, plus a multivariate meta‐regression of the 3 single variables with lowest P values. See methods for further information.
GRADE assessment suggested moderate‐quality evidence that long‐chain omega‐3 fat intake probably makes little or no difference to risk of arrhythmia (moderate‐quality/certainty evidence, downgraded once for imprecision).
Effects of ALA on primary health outcomes
See Table 2 for a summary of our evidence on effects of ALA on our primary outcomes.
As there were fewer than 10 studies for all ALA analyses we did not use funnel plots, though we did run sensitivity analyses and subgroups. We assessed ALA dose‐response and duration effects in meta‐regression of all included LCn3, ALA, omega‐6 and total PUFA trials (but not of ALA trials alone as there were too few studies to carry out meta‐regression with any reliability).
All‐cause mortality (ALA)
Moderate‐quality evidence suggests that ALA intake probably makes little or no difference to all‐cause mortality.
There was little or no effect of increasing ALA omega‐3 fats on all‐cause mortality, with 458 deaths in more than 18,000 participants involved in four studies (RR 1.01, 95% CI 0.84 to 1.20, I2 = 0%, Analysis 4.1).
Analysis 4.1.
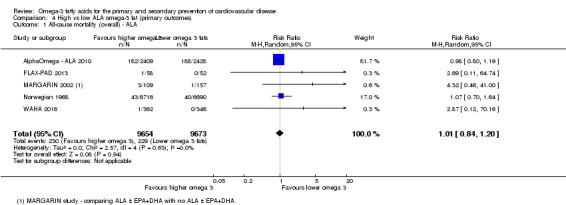
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 1 All‐cause mortality (overall) ‐ ALA.
Sensitivity analyses removing RCTs not at low summary risk of bias left three trials with 375 deaths, again suggesting little or no effect (RR 1.02, 95% CI 0.72 to 1.45, I2 = 3%, Analysis 4.3). Using fixed‐effect meta‐analysis suggested a 6% increase in risk of all‐cause mortality with increased ALA (RR 1.06, 95% CI 0.84 to 1.34, Analysis 4.2), while limiting the analysis to studies at low risk of compliance problems showed a 5% increase, and including only larger trials showed little or no effect (Analysis 4.4).
Analysis 4.3.
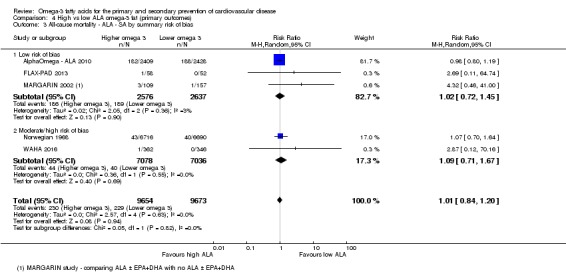
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 3 All‐cause mortality ‐ ALA ‐ SA by summary risk of bias.
Analysis 4.2.
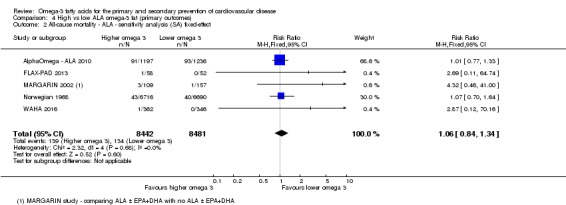
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 2 All‐cause mortality ‐ ALA ‐ sensitivity analysis (SA) fixed‐effect.
Analysis 4.4.
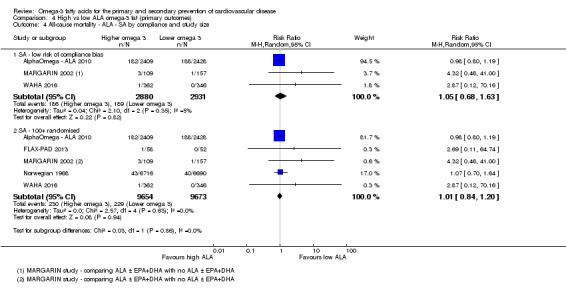
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 4 All‐cause mortality ‐ ALA ‐ SA by compliance and study size.
Subgrouping by ALA dose, trial duration, statin use, replacement, primary or secondary prevention, or intervention type did not result in any significant differences between subgroups (Analysis 4.5; Analysis 4.6; Analysis 4.7; Analysis 4.8; Analysis 4.9; Analysis 4.10). As there was no suggestion of effect in any subgroup, we did not carry out meta‐regression.
Analysis 4.5.
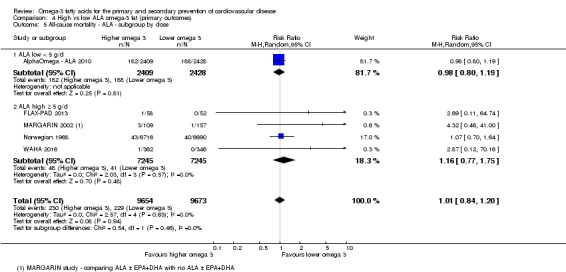
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 5 All‐cause mortality ‐ ALA ‐ subgroup by dose.
Analysis 4.6.
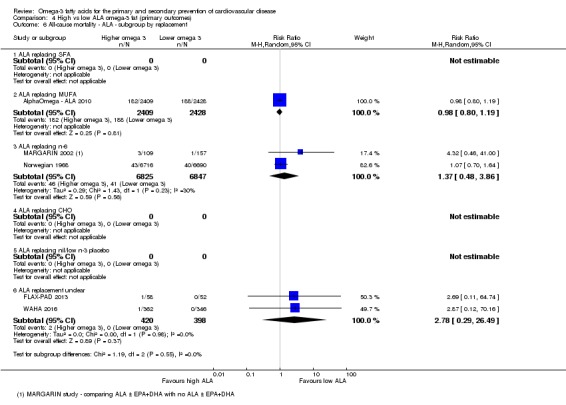
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 6 All‐cause mortality ‐ ALA ‐ subgroup by replacement.
Analysis 4.7.
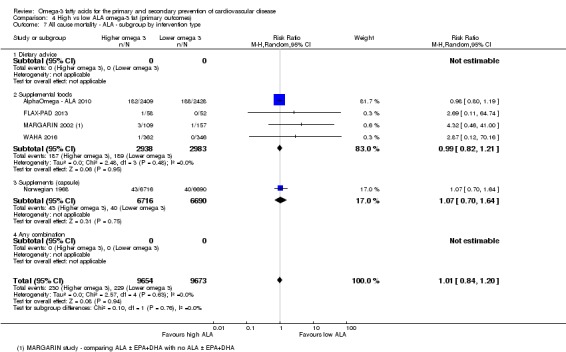
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 7 All cause mortality ‐ ALA ‐ subgroup by intervention type.
Analysis 4.8.
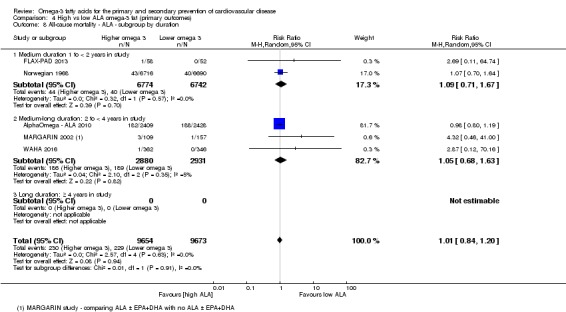
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 8 All‐cause mortality ‐ ALA ‐ subgroup by duration.
Analysis 4.9.
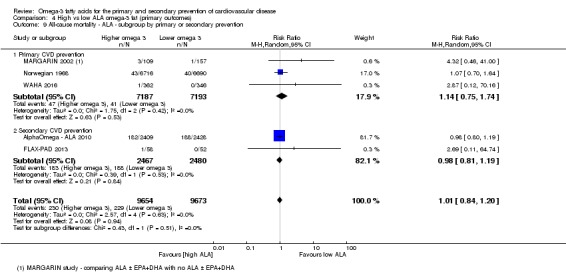
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 9 All‐cause mortality ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 4.10.
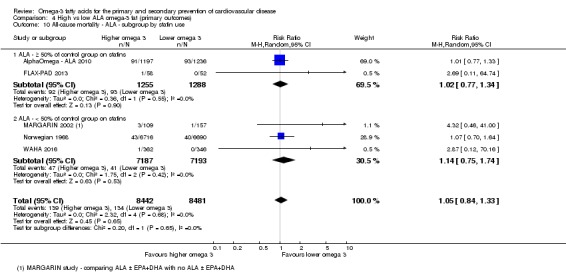
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 10 All‐cause mortality ‐ ALA ‐ subgroup by statin use.
GRADE assessment suggested that ALA intake probably makes little or no difference to all‐cause mortality (moderate‐quality/certainty evidence, downgraded once for imprecision).
Cardiovascular mortality (ALA)
Moderate‐quality evidence suggests that increasing ALA intake probably has little or no effect on cardiovascular mortality.
Four studies contributed data to this outcome. There was little or no effect of increasing ALA omega‐3 fats on cardiovascular mortality (RR 0.96, 95% CI 0.74 to 1.25, I2 = 0%, Analysis 4.11), but confidence intervals were very wide. Analyses included 219 CVD deaths in > 18,000 participants.
Analysis 4.11.
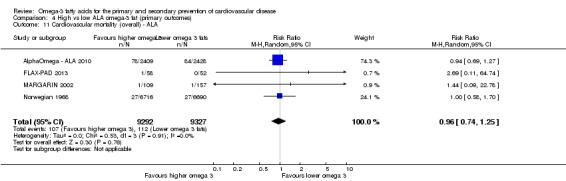
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 11 Cardiovascular mortality (overall) ‐ ALA.
Sensitivity analyses using fixed‐effect meta‐analysis did alter the lack of effect (RR 0.96, 95% CI 0.74 to 1.25, Analysis 4.12). Removing studies not at low risk of bias left three trials with 165 cardiovascular deaths, suggesting a 5% reduction of cardiovascular death risk with higher ALA (RR 0.95, 95% CI 0.70 to 1.28, Analysis 4.13). Sensitivity analysis by compliance or study size again suggested 6% and 4% reductions, respectively, in CVD mortality risk (Analysis 4.14).
Analysis 4.12.
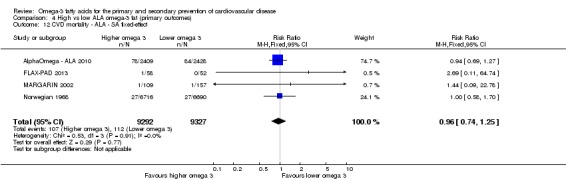
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 12 CVD mortality ‐ ALA ‐ SA fixed‐effect.
Analysis 4.13.
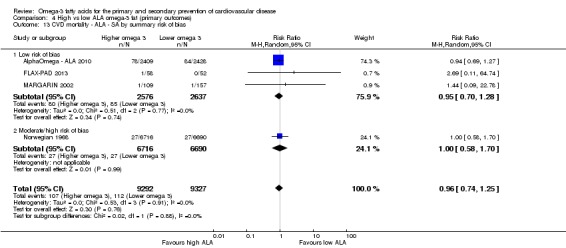
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 13 CVD mortality ‐ ALA ‐ SA by summary risk of bias.
Analysis 4.14.
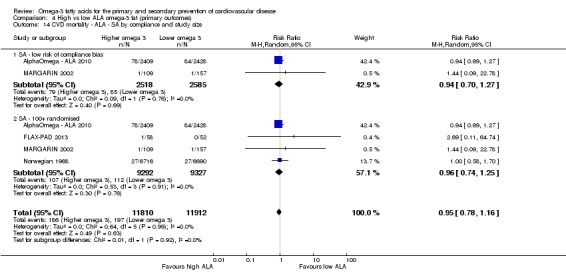
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 14 CVD mortality ‐ ALA ‐ SA by compliance and study size.
Subgrouping by ALA dose, study duration, replacement, intervention type, statin use or primary/secondary prevention did not suggest important differences between subgroups (Analysis 4.15; Analysis 4.16; Analysis 4.17; Analysis 4.18; Analysis 4.19; Analysis 4.20). Meta‐regression to assess for effects of ALA dose on cardiovascular mortality did not suggest dose effects (P = 0.91, Table 11).
Analysis 4.15.
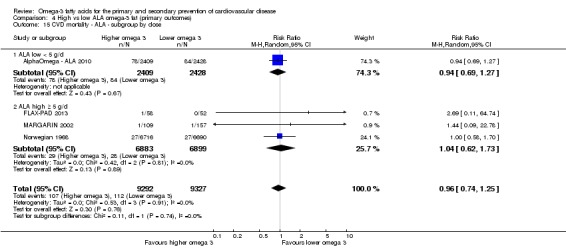
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 15 CVD mortality ‐ ALA ‐ subgroup by dose.
Analysis 4.16.
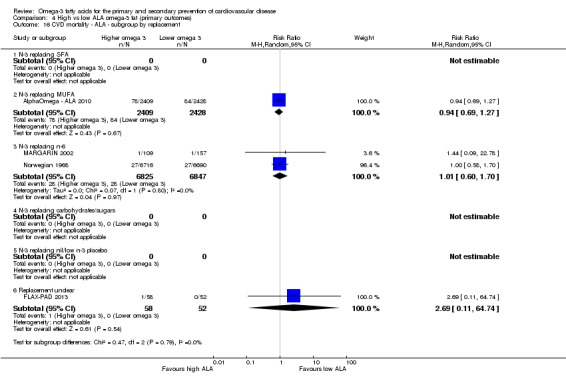
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 16 CVD mortality ‐ ALA ‐ subgroup by replacement.
Analysis 4.17.
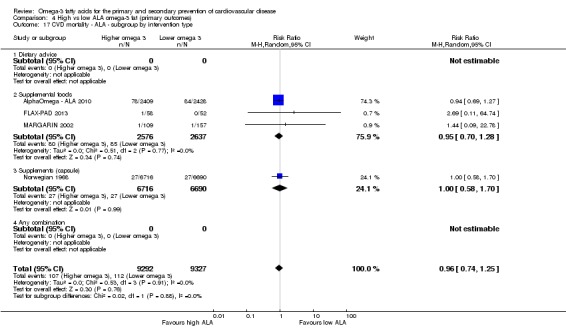
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 17 CVD mortality ‐ ALA ‐ subgroup by intervention type.
Analysis 4.18.
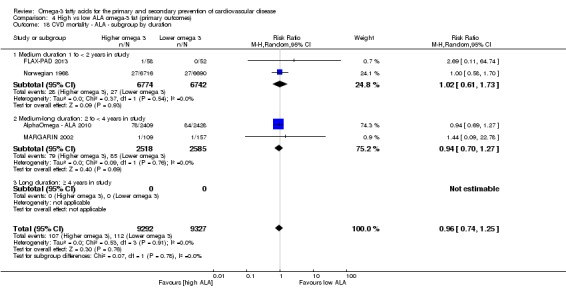
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 18 CVD mortality ‐ ALA ‐ subgroup by duration.
Analysis 4.19.
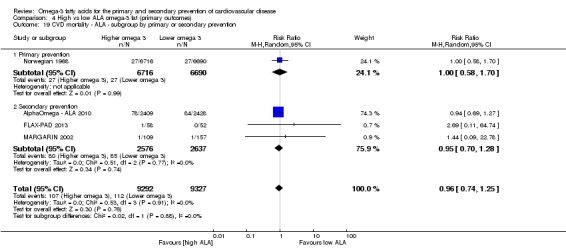
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 19 CVD mortality ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 4.20.
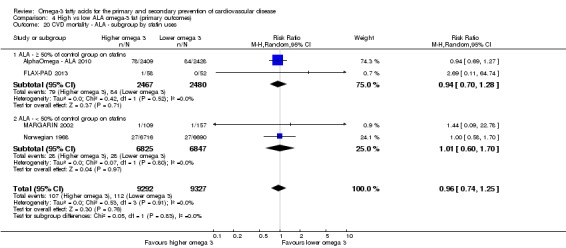
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 20 CVD mortality ‐ ALA ‐ subgroup by statin uses.
GRADE assessment suggested that increasing ALA intake probably has little or no effect on cardiovascular mortality (moderate‐quality/certainty evidence, downgraded once for imprecision).
Cardiovascular events (ALA)
GRADE assessment suggested that increasing ALA intake may reduce the risk of cardiovascular events by a small amount.
There was a 5% reduction in risk of cardiovascular events in five trials with increased ALA intake (RR 0.95, 95% CI 0.83 to 1.07, I2 = 0%, 884 out of > 19,000 participants experienced at least one cardiovascular event, Analysis 4.21).
Analysis 4.21.
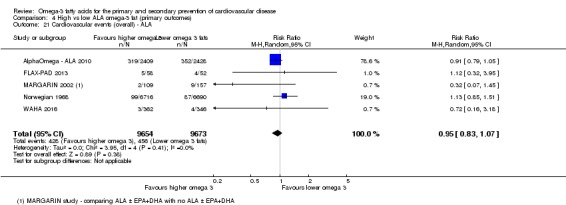
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 21 Cardiovascular events (overall) ‐ ALA.
Sensitivity analyses removing studies at moderate to high risk of bias left three trials in which 691 of > 5,000 enrolled participants experienced at least one cardiovascular event, suggesting a 9% reduction in risk of CVD events with higher ALA (RR 0.91, 95% CI 0.79 to 1.04, I2 = 0%, Analysis 4.23). Fixed‐effect analysis suggested a 5% reduction in risk (Analysis 4.22), while studies at low risk of compliance bias suggested a 10% reduction in risk, and larger studies a 5% reduction (Analysis 4.24).
Analysis 4.23.
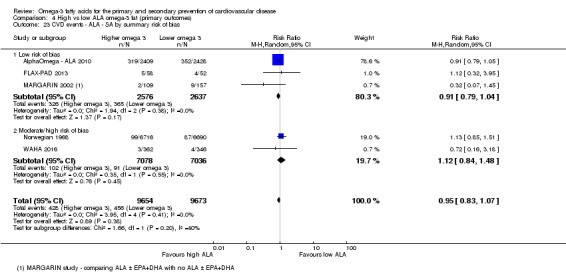
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 23 CVD events ‐ ALA ‐ SA by summary risk of bias.
Analysis 4.22.
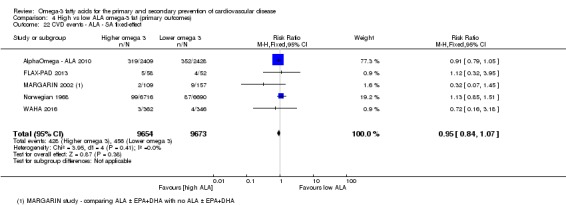
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 22 CVD events ‐ ALA ‐ SA fixed‐effect.
Analysis 4.24.
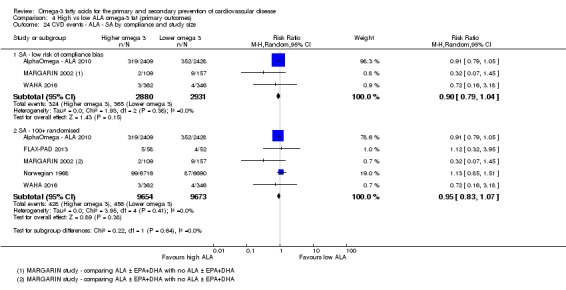
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 24 CVD events ‐ ALA ‐ SA by compliance and study size.
Subgrouping by ALA dose, study duration, replacement, intervention type, statin use or primary/secondary prevention did not suggest significant differences between subgroups (Analysis 4.25; Analysis 4.26; Analysis 4.27; Analysis 4.28; Analysis 4.29; Analysis 4.30). Meta‐regression to assess for effects of ALA dose on cardiovascular events did not suggest any dose effects (P = 0.70, Table 12).
Analysis 4.25.
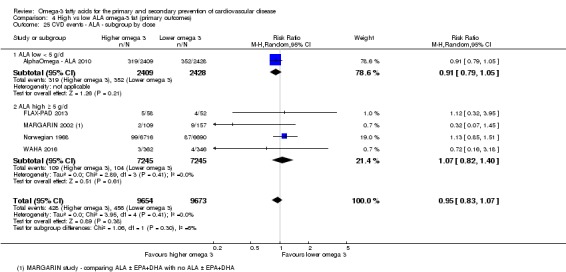
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 25 CVD events ‐ ALA ‐ subgroup by dose.
Analysis 4.26.
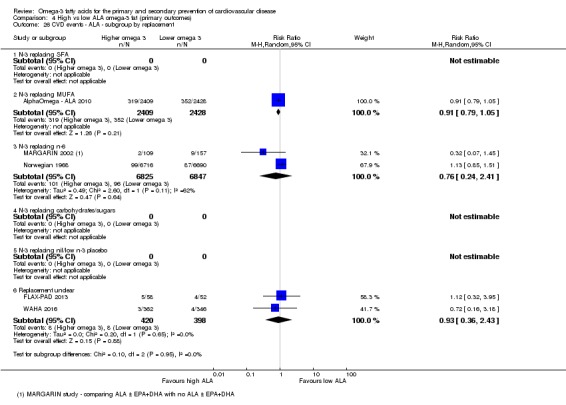
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 26 CVD events ‐ ALA ‐ subgroup by replacement.
Analysis 4.27.
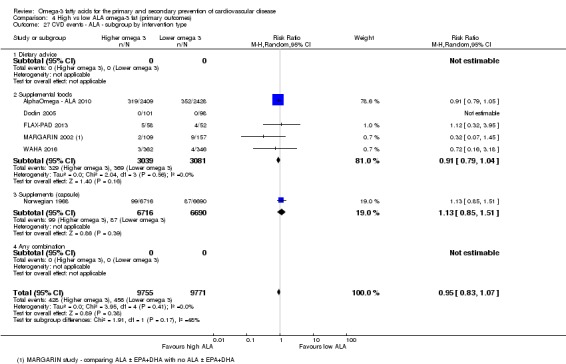
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 27 CVD events ‐ ALA ‐ subgroup by intervention type.
Analysis 4.28.
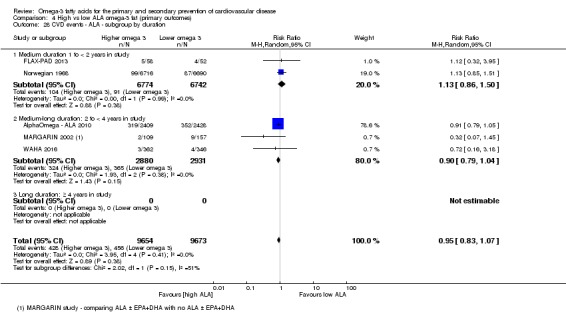
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 28 CVD events ‐ ALA ‐ subgroup by duration.
Analysis 4.29.
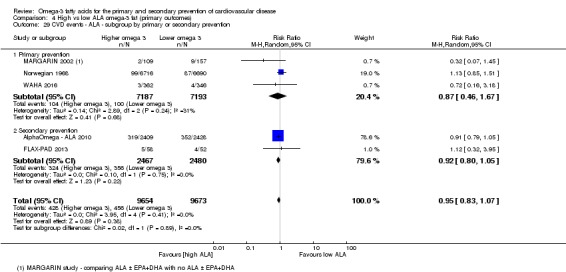
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 29 CVD events ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 4.30.
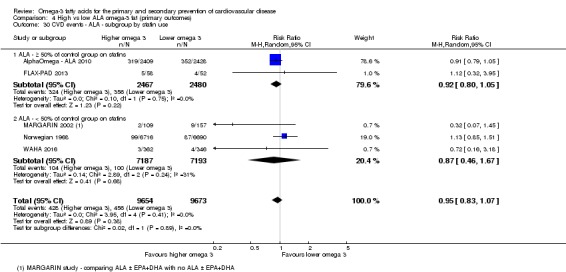
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 30 CVD events ‐ ALA ‐ subgroup by statin use.
GRADE assessment suggested that increasing ALA intake may reduce the risk of cardiovascular events by a small amount (low‐quality/certainty evidence, downgraded once for risk of bias and once for imprecision).
Coronary heart disease mortality (ALA)
GRADE assessment suggested that increasing ALA intake probably reduces the risk of CHD mortality a little.
Three studies reported 193 CHD deaths in > 18,000 participants, suggesting a 5% reduction in CHD mortality with increased ALA (RR 0.95, 95% CI 0.72 to 1.26, I2 = 0%, Analysis 4.31).
Analysis 4.31.
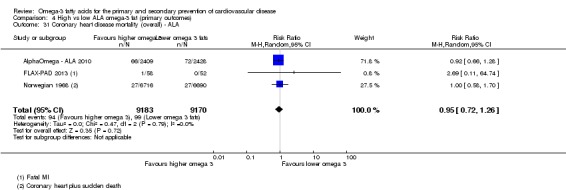
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 31 Coronary heart disease mortality (overall) ‐ ALA.
Sensitivity analyses using fixed‐effect meta‐analysis did not alter the effect (RR 0.95, 95% CI 0.72 to 1.26, Analysis 4.32). Studies at low summary risk of bias suggested a 7% reduction in risk of CHD mortality (including 2 trials with 4947 participants, RR 0.93, 95% CI 0.67 to 1.30, I2 = 0%, Analysis 4.33), with similar effects in studies at low risk of compliance bias, or low risk of small study bias (Analysis 4.34).
Analysis 4.32.
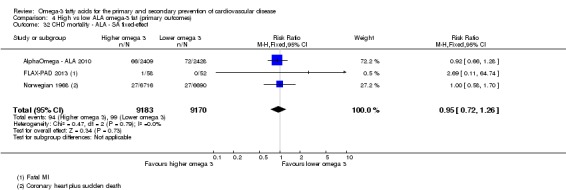
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 32 CHD mortality ‐ ALA ‐ SA fixed‐effect.
Analysis 4.33.
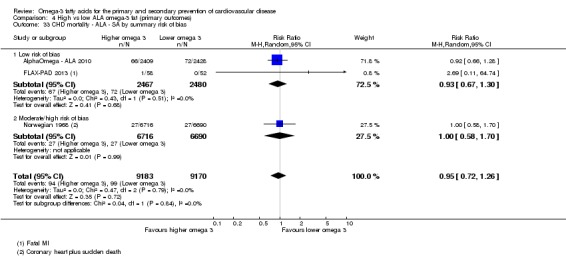
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 33 CHD mortality ‐ ALA ‐ SA by summary risk of bias.
Analysis 4.34.
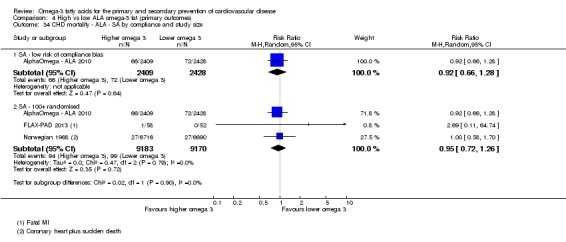
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 34 CHD mortality ‐ ALA ‐ SA by compliance and study size.
Subgrouping by ALA dose, study duration, replacement, intervention type, statin use, primary/secondary prevention or previous history of coronary artery disease did not suggest important differences between subgroups (Analysis 4.35; Analysis 4.36; Analysis 4.37; Analysis 4.38; Analysis 4.39; Analysis 4.40; Analysis 4.41). Meta‐regression to assess for effects of ALA dose on CHD deaths did not suggest any dose effects (P = 0.93, Table 13).
Analysis 4.35.
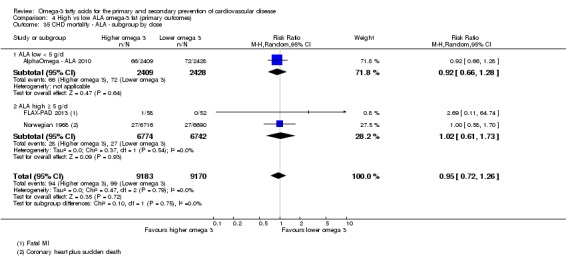
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 35 CHD mortality ‐ ALA ‐ subgroup by dose.
Analysis 4.36.
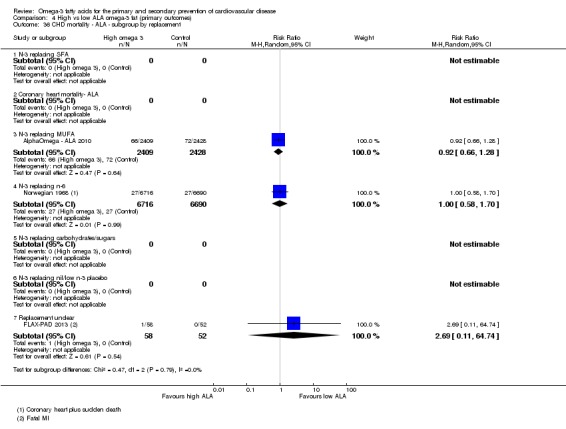
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 36 CHD mortality ‐ ALA ‐ subgroup by replacement.
Analysis 4.37.
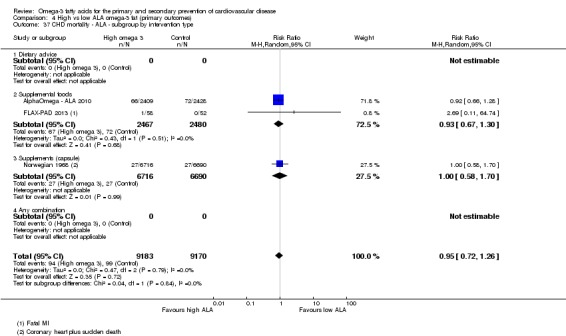
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 37 CHD mortality ‐ ALA ‐ subgroup by intervention type.
Analysis 4.38.
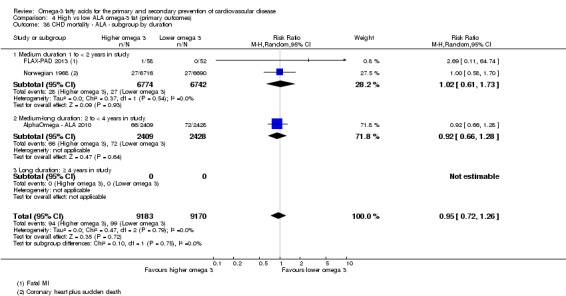
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 38 CHD mortality ‐ ALA ‐ subgroup by duration.
Analysis 4.39.
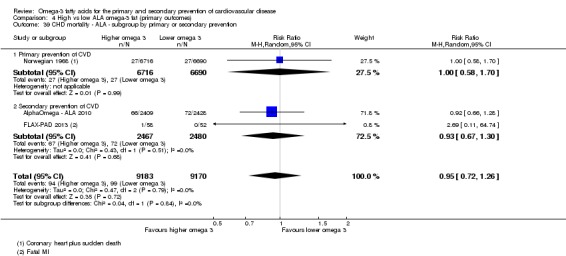
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 39 CHD mortality ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 4.40.
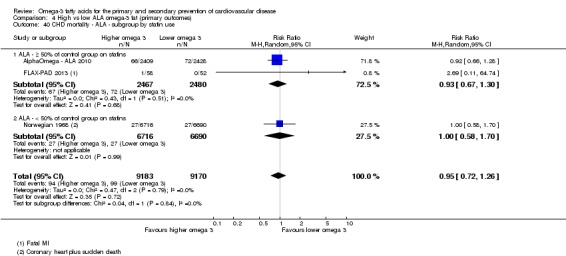
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 40 CHD mortality ‐ ALA ‐ subgroup by statin use.
Analysis 4.41.
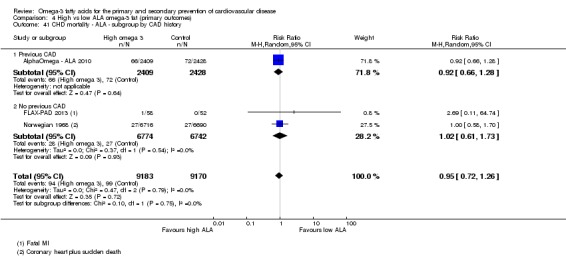
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 41 CHD mortality ‐ ALA ‐ subgroup by CAD history.
GRADE assessment suggested that increasing ALA intake probably reduces the risk of CHD mortality a little (moderate‐quality/certainty evidence, downgraded once for imprecision).
Coronary heart disease events (ALA)
Low‐quality evidence suggests that ALA intake may make little or no difference to CHD events.
Three studies contributed data to this outcome, with 396 out of over 18,000 participants experiencing at least one CHD event. There was little or no effect on CHD risk with increased ALA (RR 1.00, 95% CI 0.82 to 1.22, I2 = 2%, Analysis 4.42).
Analysis 4.42.
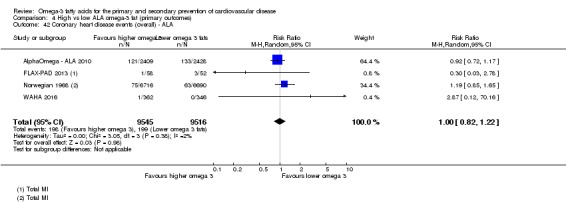
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 42 Coronary heart disease events (overall) ‐ ALA.
Sensitivity analyses using fixed‐effect meta‐analysis did not alter the lack of effect (RR 1.00, 95% CI 0.82 to 1.21, Analysis 4.43). Removing studies not at low summary risk of bias left two studies with almost 5000 participants, suggesting a 9% reduction in risk of a CHD event (RR 0.91, 95% CI 0.71 to 1.15, Analysis 4.44), similar to sensitivity analysis omitting studies with potential compliance problems (Analysis 4.45), though no effects were seen when restricting analysis to larger trials (Analysis 4.45).
Analysis 4.43.
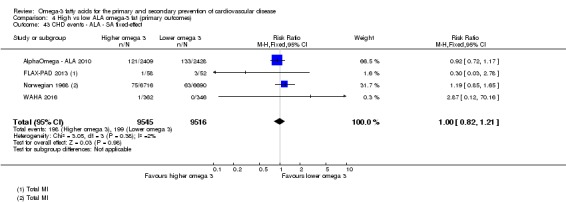
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 43 CHD events ‐ ALA ‐ SA fixed‐effect.
Analysis 4.44.
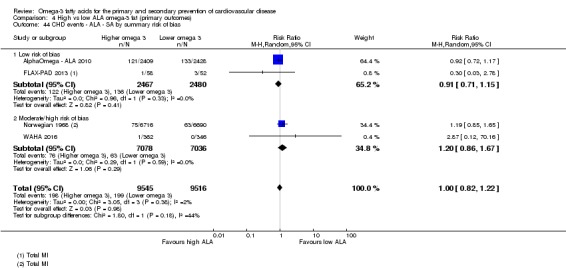
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 44 CHD events ‐ ALA ‐ SA by summary risk of bias.
Analysis 4.45.
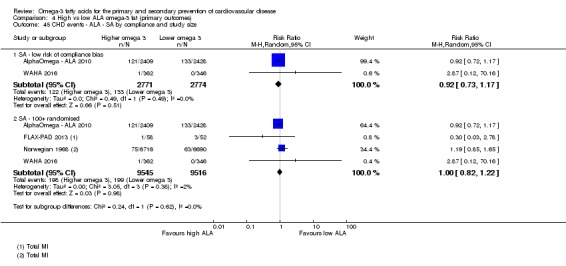
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 45 CHD events ‐ ALA ‐ SA by compliance and study size.
Subgrouping by ALA dose, study duration, replacement, intervention type, statin use, primary/secondary prevention or previous history of coronary artery disease did not suggest important differences between subgroups (Analysis 4.46; Analysis 4.47; Analysis 4.48; Analysis 4.49; Analysis 4.50; Analysis 4.51; Analysis 4.52). Meta‐regression did not suggest that there was a direct relationship between ALA dose and CHD events (Table 14).
Analysis 4.46.
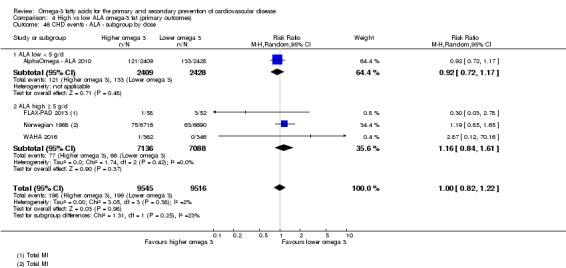
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 46 CHD events ‐ ALA ‐ subgroup by dose.
Analysis 4.47.
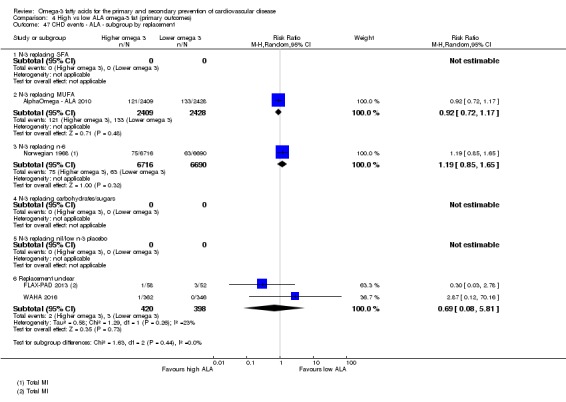
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 47 CHD events ‐ ALA ‐ subgroup by replacement.
Analysis 4.48.
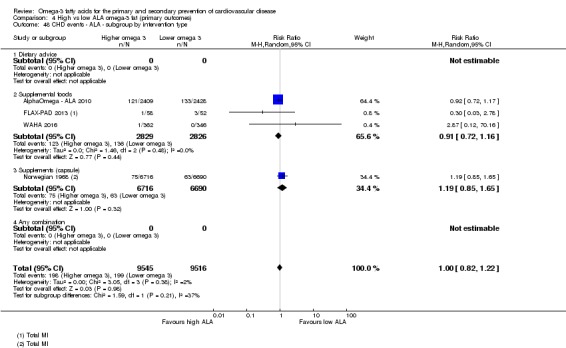
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 48 CHD events ‐ ALA ‐ subgroup by intervention type.
Analysis 4.49.
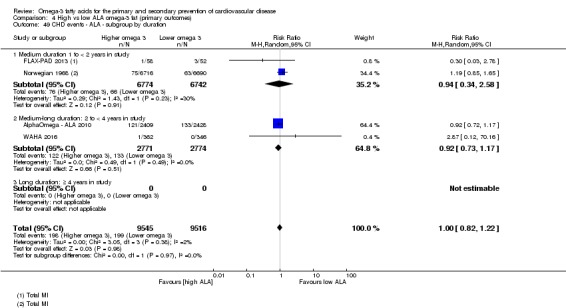
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 49 CHD events ‐ ALA ‐ subgroup by duration.
Analysis 4.50.
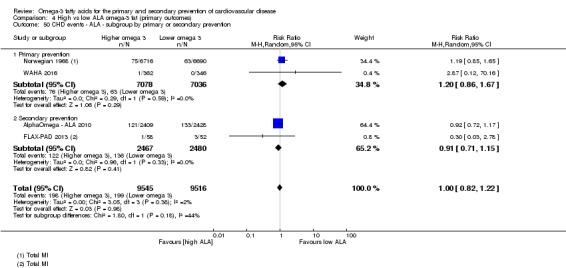
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 50 CHD events ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 4.51.
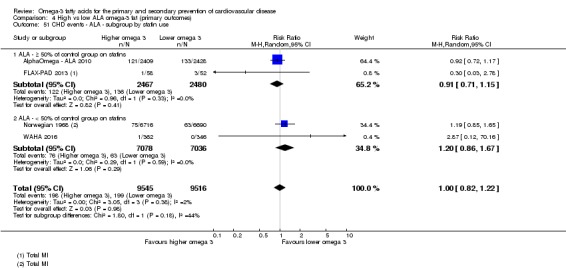
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 51 CHD events ‐ ALA ‐ subgroup by statin use.
Analysis 4.52.
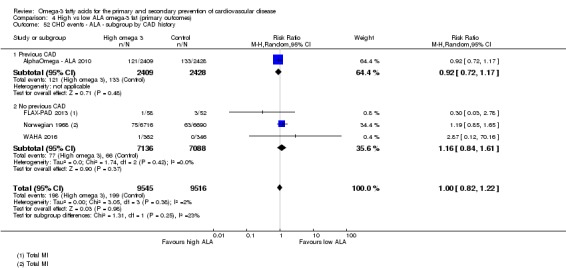
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 52 CHD events ‐ ALA ‐ subgroup by CAD history.
Given the differences in sensitivity analyses, GRADE assessment suggested that ALA intake may make little or no difference to CHD events (low‐quality/certainty evidence, downgraded once for risk of bias and once for imprecision).
Stroke (ALA)
The effect of ALA intake on stroke is unclear, as the evidence is of very low quality.
Five RCTs involved 51 people out of more than 18,000 participants experiencing a stroke, suggesting a 15% increase in stroke risk with increased ALA (RR1.15, 95% CI 0.66 to 2.01, I2 = 0%, Analysis 4.53). Sensitivity analyses removing studies not at low summary risk of bias left three studies with 27 stroke events and no suggestion of effect (Analysis 4.55). Using a fixed‐effect model suggested a 23% increased risk of stroke (Analysis 4.54), while removing studies at high risk of bias due to compliance suggested a 15% reduction in stroke risk, while larger studies suggested a 15% greater stroke risk (Analysis 4.56).
Analysis 4.53.
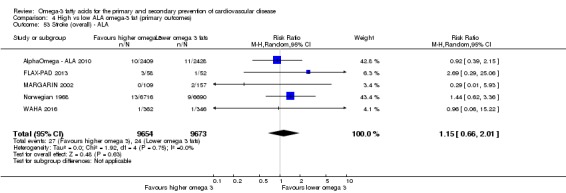
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 53 Stroke (overall) ‐ ALA.
Analysis 4.55.
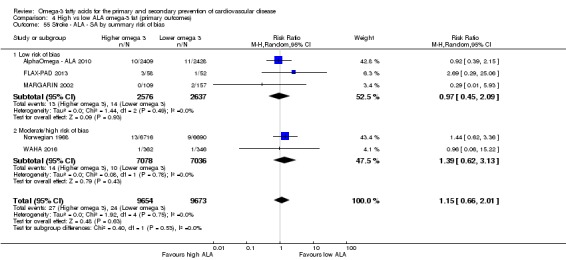
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 55 Stroke ‐ ALA ‐ SA by summary risk of bias.
Analysis 4.54.
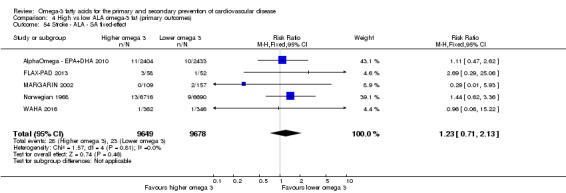
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 54 Stroke ‐ ALA ‐ SA fixed‐effect.
Analysis 4.56.
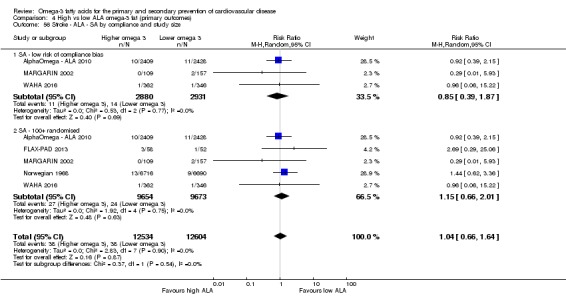
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 56 Stroke ‐ ALA ‐ SA by compliance and study size.
Subgrouping by ALA dose, study duration, replacement, intervention type, statin use or primary/secondary prevention did not result in significant differences between subgroups (Analysis 4.57; Analysis 4.58; Analysis 4.59; Analysis 4.60; Analysis 4.61; Analysis 4.62). When examining data reported by type of stroke, only three studies reported on 28 ischaemic strokes, with no clear effects, and no studies reported on haemorrhagic stroke (Analysis 4.63). Meta‐regression did not suggest any relationship between ALA dose and risk of stroke (Table 15).
Analysis 4.57.
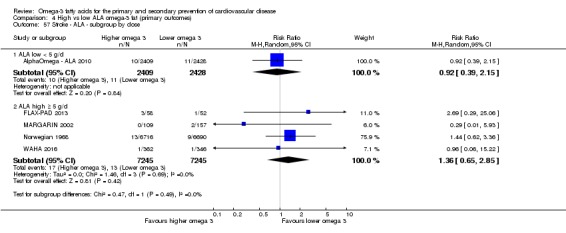
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 57 Stroke ‐ ALA ‐ subgroup by dose.
Analysis 4.58.
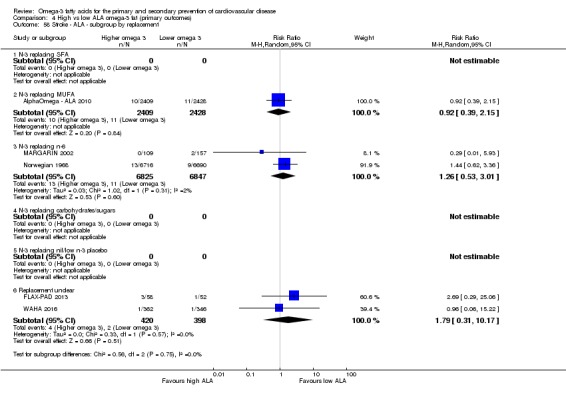
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 58 Stroke ‐ ALA ‐ subgroup by replacement.
Analysis 4.59.
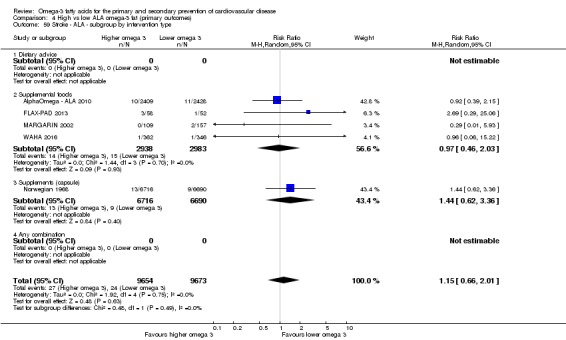
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 59 Stroke ‐ ALA ‐ subgroup by intervention type.
Analysis 4.60.
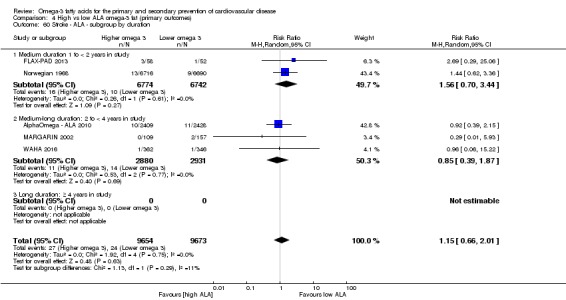
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 60 Stroke ‐ ALA ‐ subgroup by duration.
Analysis 4.61.
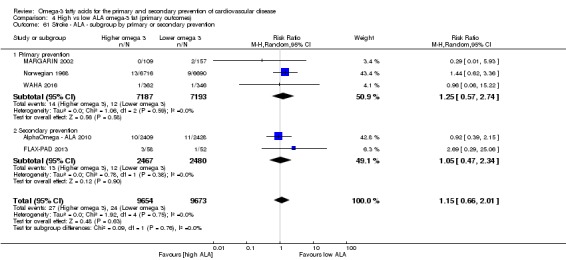
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 61 Stroke ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 4.62.
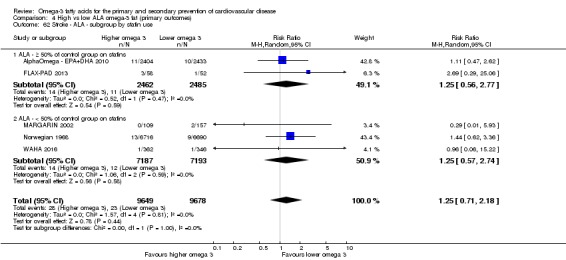
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 62 Stroke ‐ ALA ‐ subgroup by statin use.
Analysis 4.63.
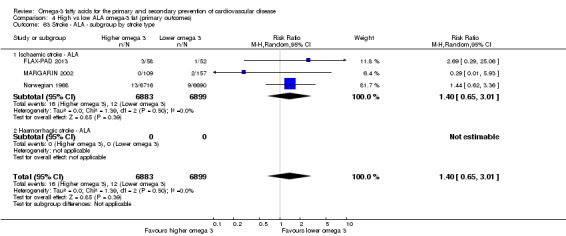
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 63 Stroke ‐ ALA ‐ subgroup by stroke type.
The effect of ALA on stroke is unclear as the evidence is of very low quality (downgraded twice for risk of bias and once for imprecision).
Arrhythmia (ALA)
Moderate‐quality evidence suggested that ALA intake probably reduces the risk of arrhythmias.
Only one study reported effects of ALA on arrhythmia, with 141 new arrhythmias in 4837 participants, suggesting a 21% reduction in arrhythmia but with wide confidence intervals (RR 0.79, 95% CI 0.57 to 1.10, Analysis 4.64). The results were identical when sensitivity analysis retained only studies at low summary risk of bias (as we judged the single included study to be at low risk of bias, Analysis 4.65). As there was only one trial, we did not carry out further sensitivity analyses or subgrouping. There was no suggestion of a dose‐response relationship between ALA and arrhythmia risk in meta‐regression (P = 0.67, Table 16).
Analysis 4.64.
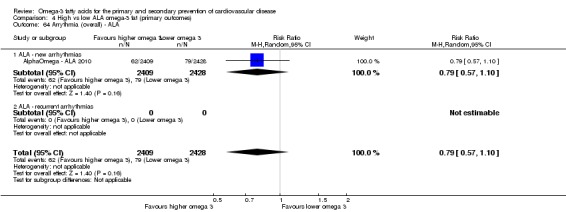
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 64 Arrythmia (overall) ‐ ALA.
Analysis 4.65.
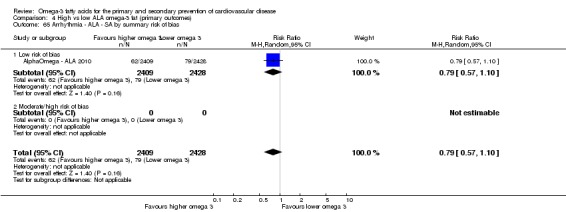
Comparison 4 High vs low ALA omega‐3 fat (primary outcomes), Outcome 65 Arrhythmia ‐ ALA ‐ SA by summary risk of bias.
GRADE assessment suggested that ALA intake probably reduces the risk of arrhythmias (moderate‐quality/certainty evidence, downgraded once for imprecision).
Secondary outcomes
See Table 3 for a summary of our evidence on effects of long‐chain omega‐3 fats and ALA on serum lipids and measures of adiposity.
Effects of long‐chain omega‐3 fats (EPA, DHA and DPA) on secondary health outcomes
We did not carry out sensitivity analyses or subgrouping on secondary outcomes, except for adiposity and lipids (which were key outcomes). We did carry out some post hoc sensitivity analyses to further assess effects of LCn3 on MI, to ascertain whether the suggested protection was stable to sensitivity analyses.
Major adverse cerebrovascular or cardiovascular events (LCn3)
Five trials reported on major adverse cerebrovascular or cardiovascular events (MACCEs) in more than 34,000 participants, 4232 of whom suffered from a MACCE, suggesting little or no effect of LCn3 fats (RR 1.03, 95% CI 0.97 to 1.09, I2 = 0%, Analysis 2.1).
Analysis 2.1.
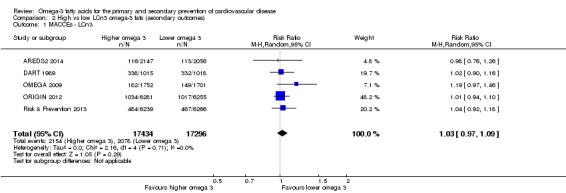
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 1 MACCEs ‐ LCn3.
Myocardial infarction (LCn3)
Twenty‐three studies (> 72,000 participants) reported on total (fatal and non‐fatal) myocardial infarction (MI). Meta‐analyses suggested that increasing LCn3 fats resulted in a small reduction in total MI (RR 0.95, 95% CI 0.88 to 1.03, I2 = 0%, 2200 MI events, Analysis 2.2). This was confirmed in sensitivity analyses limited to studies without compliance problems and to studies that randomised at least 100 participants (Analysis 2.4), but analyses limited to studies at low summary risk of bias suggest little or no effect of LCn3 on MI (RR 1.03, 95% CI 0.92 to 1.15, I2 = 0%, > 30,000 participants in 11 trials, and reporting on 1154 people experiencing at least one MI, Analysis 2.3). This suggests little or no true effect of LCn3 on MI.
Analysis 2.2.
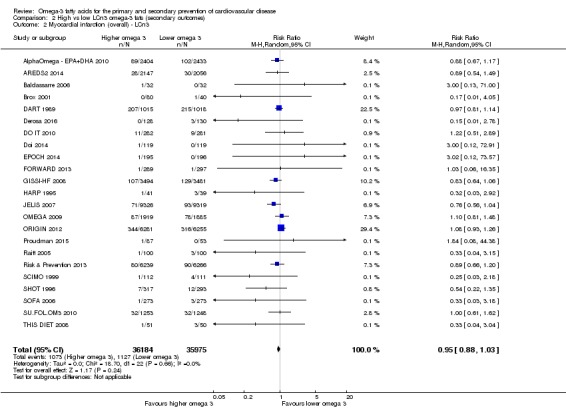
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 2 Myocardial infarction (overall) ‐ LCn3.
Analysis 2.4.
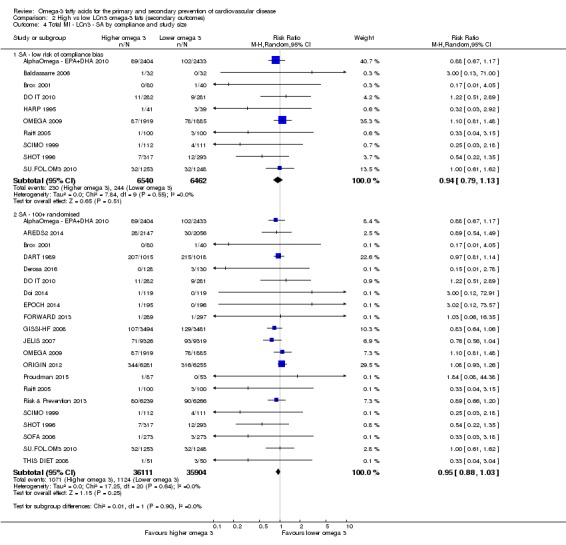
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 4 Total MI ‐ LCn3 ‐ SA by compliance and study size.
Analysis 2.3.
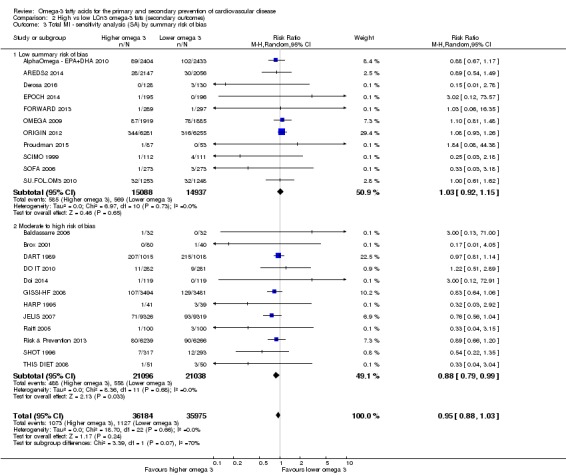
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 3 Total MI ‐ sensitivity analysis (SA) by summary risk of bias.
We ran subgroup analyses by fatality at the request of the WHO NUGAG Subgroup on Diet and Health, finding no significant difference between fatal and non‐fatal MI subgroups (P = 0.23, Analysis 2.5).
Analysis 2.5.
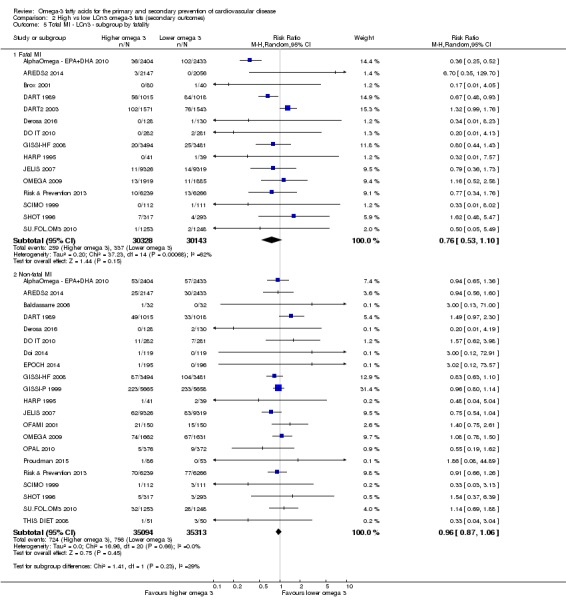
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 5 Total MI ‐ LCn3 ‐ subgroup by fatality.
Sudden cardiac death (LCn3)
There was little or no effect of LCn3 fats on sudden cardiac death (RR 0.97, 95% CI 0.80 to 1.18, I2 = 38%, 1274 deaths, 14 studies in > 65,000 people, Analysis 2.6).
Analysis 2.6.
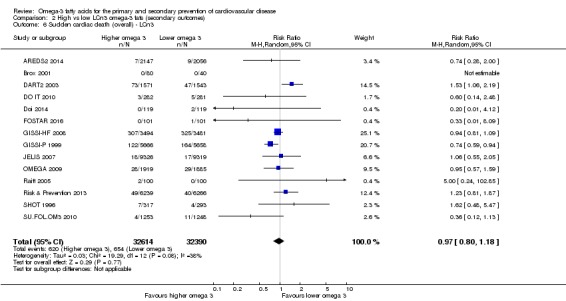
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 6 Sudden cardiac death (overall) ‐ LCn3.
Angina (LCn3)
Meta‐analysis of 11 studies involving more than 39,000 participants, 2418 of whom reported new or worsening angina, suggested little or no effect of increasing LCn3 fats (RR 0.99, 95% CI 0.92 to 1.07, I2 = 0%, Analysis 2.7).
Analysis 2.7.
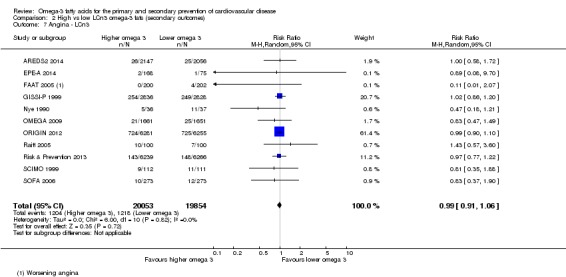
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 7 Angina ‐ LCn3.
Heart failure (LCn3)
Meta‐analysis suggested a small effect for LCn3 fatty acids on heart failure diagnosis in 15 trials with 4098 people experiencing events (RR 0.93, 95% CI 0.85 to 1.03, I2 = 31%, Analysis 2.8). Because of this suggested effectiveness, we ran a sensitivity analysis limited to the six studies at low summary risk of bias, which suggested little effect (RR 0.97, 95% CI 0.89 to 1.06, I2 = 0%, 1809 participants experiencing heart failure). For this reason we concluded that there was little or no effect of LCn3 on risk of heart failure.
Analysis 2.8.
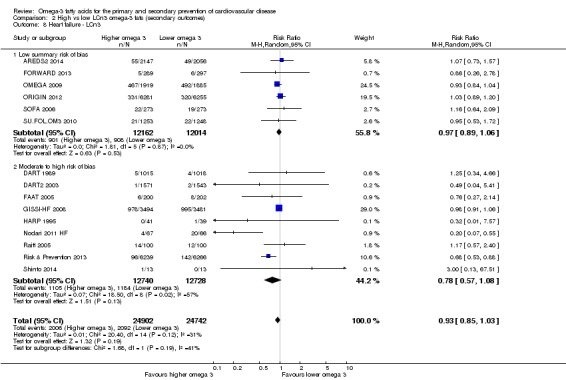
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 8 Heart failure ‐ LCn3.
Revascularisation (LCn3)
Meta‐analysis suggested little or no effect of LCn3 fats on revascularisation (all types combined, RR 0.98, 95% CI 0.94 to 1.03, 6558 participants experiencing revascularisation, I2 = 0%, Analysis 2.9). Data on angioplasty alone were similar (RR 0.96, 95% CI 0.74 to 1.24, 215 events), and there were insufficient reported CABGs to give meaningful results (9 events, Analysis 2.9).
Analysis 2.9.
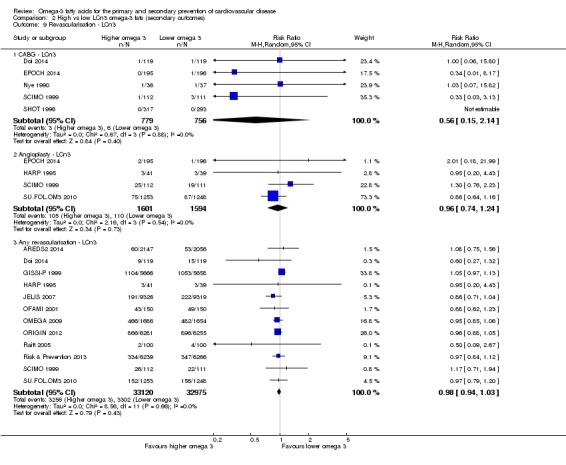
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 9 Revascularisation ‐ LCn3.
Peripheral arterial disease (LCn3)
Meta‐analysis suggested that LCn3 reduced the risk of peripheral arterial disease (PAD) by 7% (RR 0.93, 95% CI 0.74 to 1.18, I2 = 0%, 282 events in > 49,000 participants, 7 trials, Analysis 2.10). All relevant studies had randomised at least 100 participants, so this sensitivity analysis did not alter the effect, but limiting the analysis to studies at low risk of compliance bias suggested little or no effect of LCn3 on PAD, and limiting analyses to studies at low summary risk of bias suggested an increase in PAD with increased LCn3 (Analysis 2.11; Analysis 2.12). The effect of LCn3 on peripheral arterial disease is unclear – there may be increased, decreased or no effect.
Analysis 2.10.
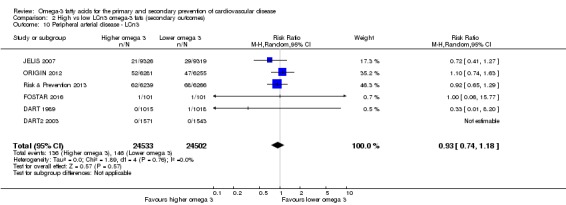
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 10 Peripheral arterial disease ‐ LCn3.
Analysis 2.11.
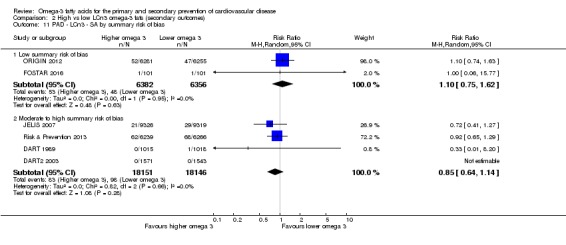
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 11 PAD ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.12.
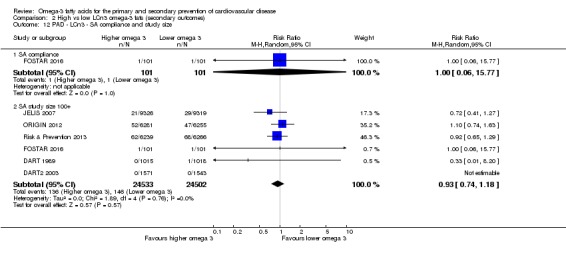
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 12 PAD ‐ LCn3 ‐ SA compliance and study size.
Acute coronary syndrome (LCn3)
There were limited data on effects of increasing LCn3 fats on acute coronary syndrome (RR 1.19, 95% CI 0.71 to 2.00, I2 = 0%, 55 events in > 2000 participants, 2 trials, Analysis 2.13).
Analysis 2.13.
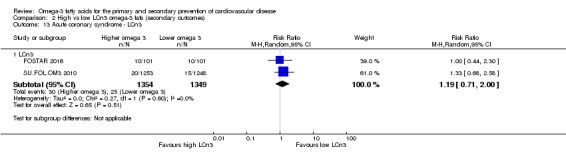
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 13 Acute coronary syndrome ‐ LCn3.
Body weight, body mass index (BMI) and other measures of adiposity (LCn3)
Body weight
High‐quality evidence shows that LCn3 intake makes little or no difference to body weight.
Twelve studies, 11 of which were included in meta‐analysis, reported on the effect of increasing LCn3 on body weight, suggesting little or no effect in > 15,000 participants (mean difference (MD) −0.01 kg, 95% CI −0.84 to 0.82, I2 = 49%, Analysis 2.14). Sensitivity analysis limited to studies at low summary risk of bias, low risk from compliance, larger trials or fixed‐effect analysis (not shown) did not alter this lack of effect (Analysis 2.15; Analysis 2.16).
Analysis 2.14.
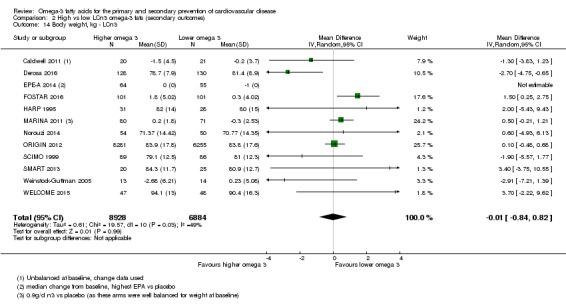
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 14 Body weight, kg ‐ LCn3.
Analysis 2.15.
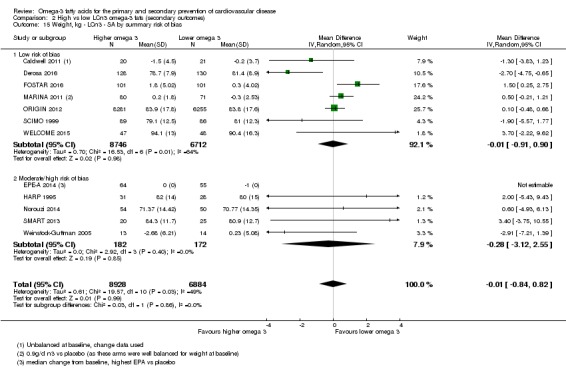
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 15 Weight, kg ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.16.
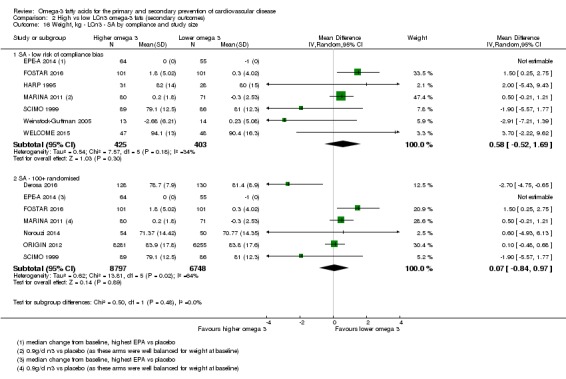
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 16 Weight, kg ‐ LCn3 ‐ SA by compliance and study size.
Subgroup analysis by intervention type, primary or secondary prevention, statin use and trial duration did not suggest important differences between subgroups (Analysis 2.19; Analysis 2.20; Analysis 2.21; Analysis 2.22). There was a marginally significant difference between dose subgroups (P = 0.06, Analysis 2.17) and increased body weight when participants received very high LCn3 doses (> 4.4 g/d LCn3, MD 1.51 kg, 95% CI 0.28 to 2.75, I2 = 0%, 2 trials including 261 participants, Analysis 2.17). Subgrouping by replacement suggested differences between subgroups (P < 0.001, Analysis 2.18, with reduced body weight when LCn3 replaced saturated fatty acids (SFA) or carbohydrates but increased weight when LCn3 replaced nil or low LCn3 (Analysis 2.18).
Analysis 2.19.
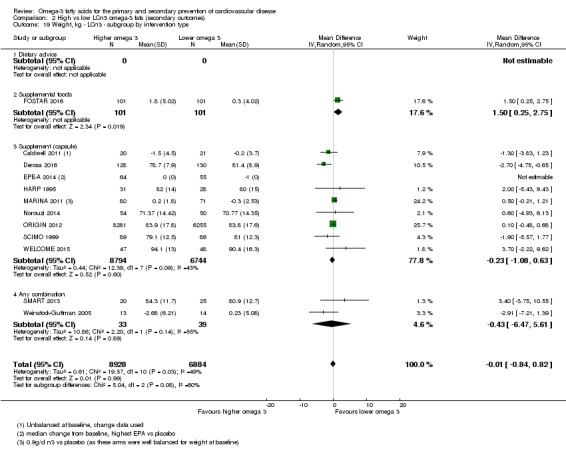
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 19 Weight, kg ‐ LCn3 ‐ subgroup by intervention type.
Analysis 2.20.
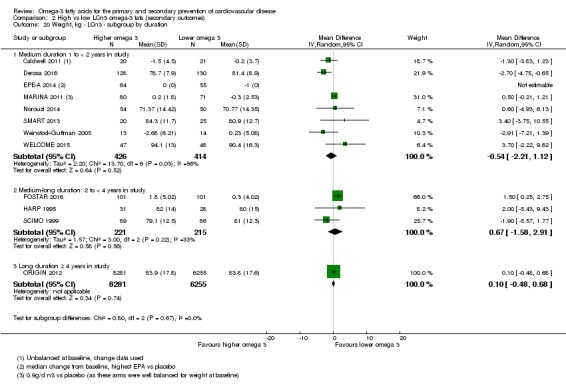
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 20 Weight, kg ‐ LCn3 ‐ subgroup by duration.
Analysis 2.21.
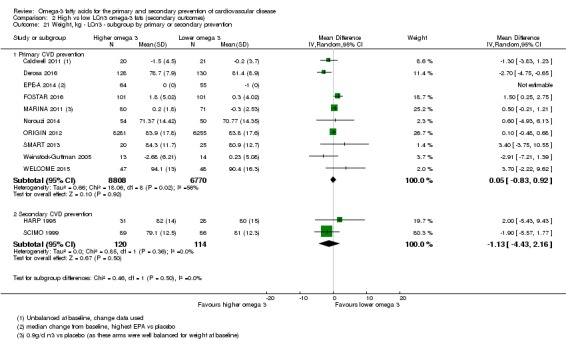
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 21 Weight, kg ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 2.22.
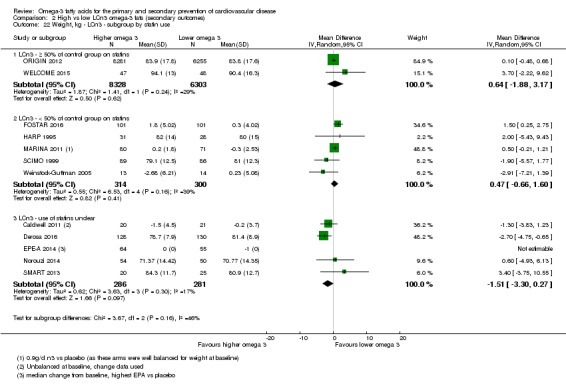
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 22 Weight, kg ‐ LCn3 ‐ subgroup by statin use.
Analysis 2.17.
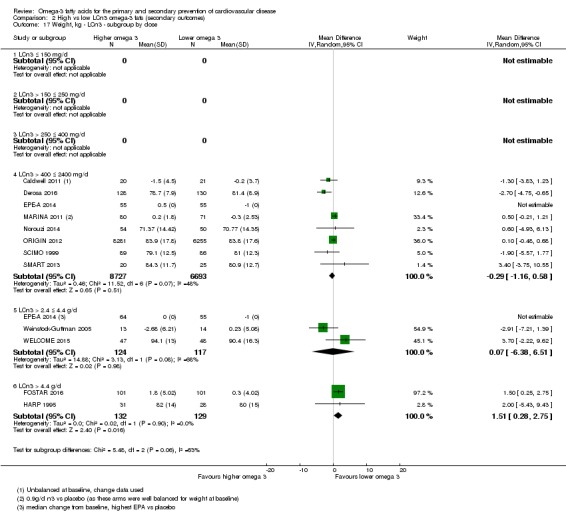
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 17 Weight, kg ‐ LCn3 ‐ subgroup by dose.
Analysis 2.18.
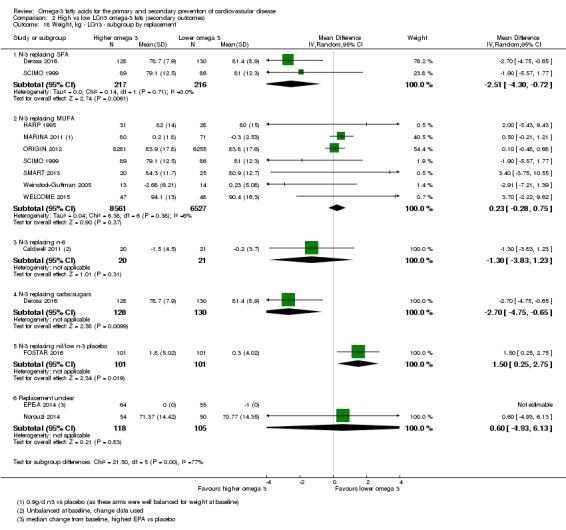
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 18 Weight, kg ‐ LCn3 ‐ subgroup by replacement.
Several studies clearly measured body weight but did not report it in a useable way (Baldassarre 2006; Caldwell 2011; Deslypere 1992; EPE‐A 2014; MARINA 2011; Nutristroke 2009). Body weight is commonly measured in healthcare settings, so there may be considerably more missing data than these.
GRADE evidence suggests high‐quality evidence that LCn3 intake makes little or no difference to body weight (high‐quality/certainty evidence).
BMI
High‐quality evidence shows that LCn3 intake makes little or no difference to BMI.
Fourteen trials, 12 of which were included in meta‐analysis, reported on BMI, suggesting little or no effect of LCn3 on BMI (MD 0.04 kg/m2, 95% CI −0.16 to 0.24, I2 = 40%, > 15,000 participants, Analysis 2.23). This lack of effect was also apparent in sensitivity analyses limited to studies at low summary risk of bias (Analysis 2.24), with good compliance or with large study size (Analysis 2.25), as well as fixed‐effect analysis (not shown). Subgroup analyses by primary or secondary prevention, LCn3 dose, intervention type, statin use and trial duration did not suggest important differences between subgroups (Analysis 2.26; Analysis 2.28; Analysis 2.29; Analysis 2.30; Analysis 2.31). There were significant differences between subgroups when subgrouped by replacement, suggesting lower BMI when LCn3 was replaced by SFA and carbohydrate, but increased BMI with LCn3 in other replacements (P = 0.04, Analysis 2.27).
Analysis 2.23.
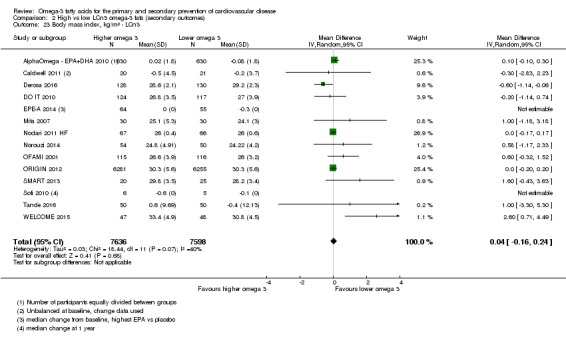
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 23 Body mass index, kg/m² ‐ LCn3.
Analysis 2.24.
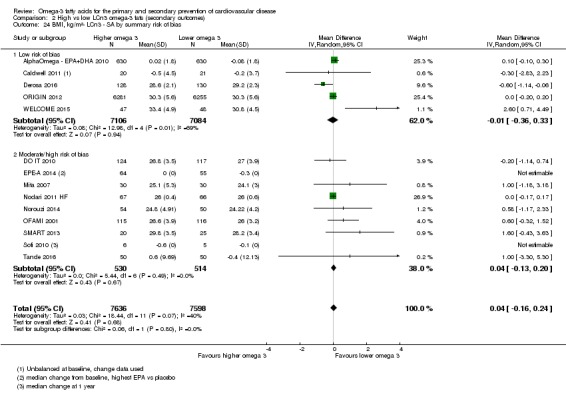
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 24 BMI, kg/m²‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.25.
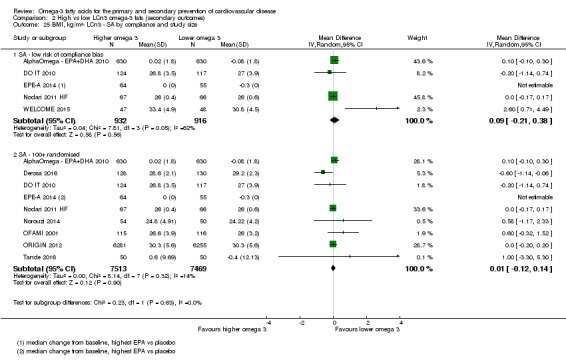
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 25 BMI, kg/m²‐ LCn3 ‐ SA by compliance and study size.
Analysis 2.26.
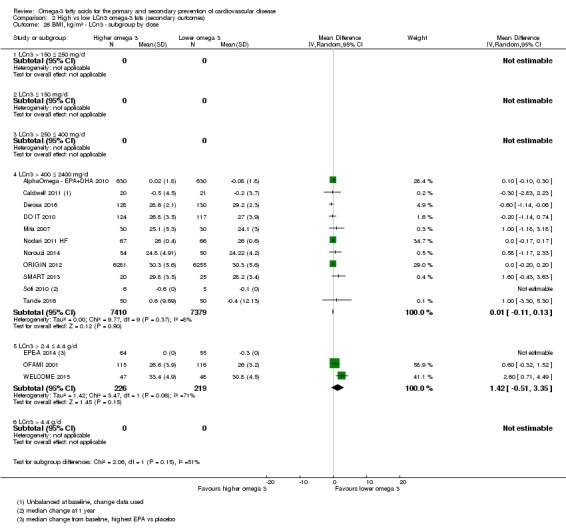
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 26 BMI, kg/m² ‐ LCn3 ‐ subgroup by dose.
Analysis 2.28.
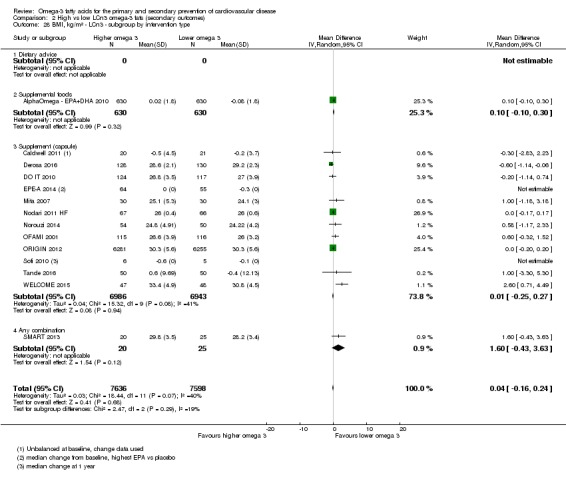
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 28 BMI, kg/m² ‐ LCn3 ‐ subgroup by intervention type.
Analysis 2.29.
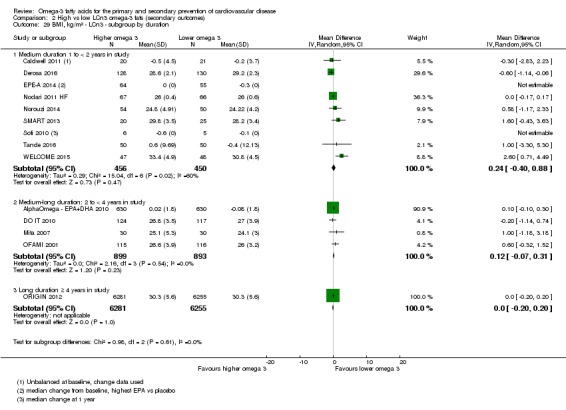
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 29 BMI, kg/m² ‐ LCn3 ‐ subgroup by duration.
Analysis 2.30.
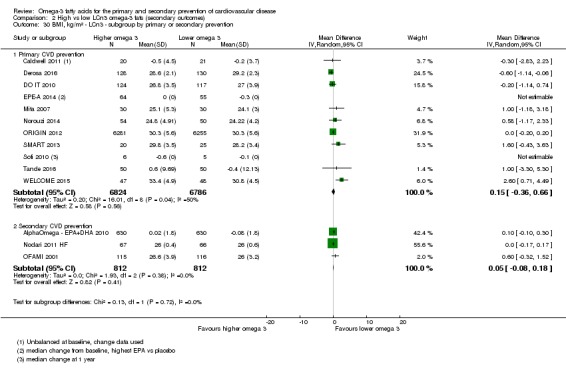
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 30 BMI, kg/m² ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 2.31.
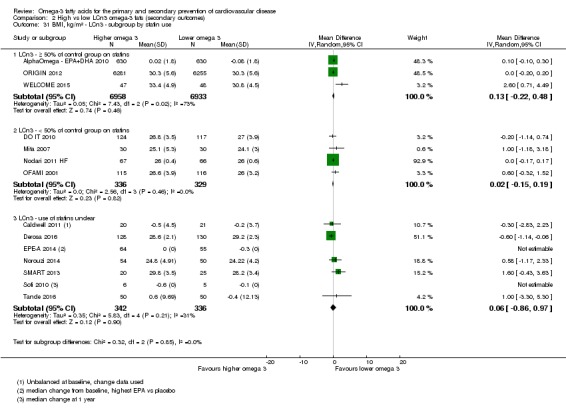
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 31 BMI, kg/m² ‐ LCn3 ‐ subgroup by statin use.
Analysis 2.27.
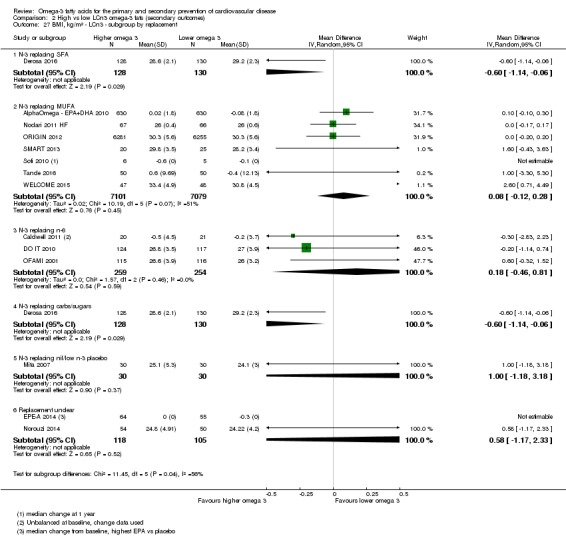
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 27 BMI, kg/m² ‐ LCn3 ‐ subgroup by replacement.
Several studies clearly measured BMI but did not report it in a useable way (Caldwell 2011; EPE‐A 2014; Nutristroke 2009; Ramirez‐Ramirez 2013;Sofi 2010), suggesting that missing data may be an issue with this outcome.
GRADE evidence suggests high‐quality evidence that LCn3 intake makes little or no difference to BMI (high‐quality/certainty evidence).
Other measures of adiposity
Few studies reported on other measures of adiposity (percentage body fat, percentage visceral fat, waist circumference, waist/hip ratio, abdominal circumference and hip circumference) with some suggesting higher adiposity and some lower adiposity in groups with more LCn3 (Analysis 2.32).
Analysis 2.32.
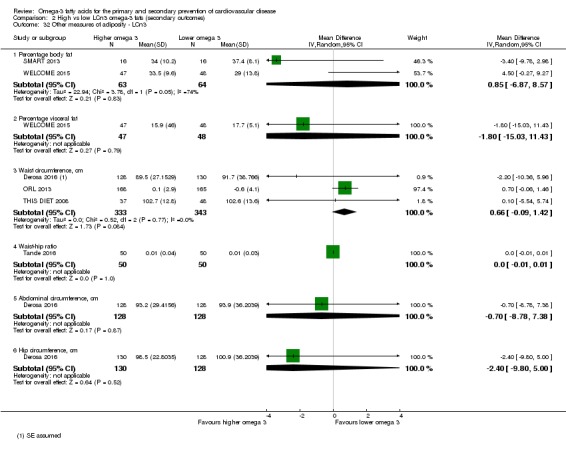
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 32 Other measures of adiposity ‐ LCn3.
Serum lipids (LCn3)
Several studies clearly measured lipids but did not report them in a way that we could include in our meta‐analyses. These generally included Baldassarre 2006, Gill 2012,Ramirez‐Ramirez 2013 and Reed 2014, plus Ahn 2016,Caldwell 2011,Franzen 1993 and Rossing 1996, which assessed but did not report triglycerides, and Franzen 1993, which measured but did not provide useable data for HDL and LDL cholesterol. For this reason missing data may potentially bias these outcomes.
Serum total cholesterol
Moderate‐quality evidence shows that LCn3 intake probably makes little or no difference to serum total cholesterol.
Twenty‐eight trials provided data on long‐term effects of LCn3 fats on serum total cholesterol, suggesting little or no effect in more than 37,000 participants (MD −0.01 mmol/L, 95% CI −0.5 to 0.04, I2 = 19%, Analysis 2.33). Sensitivity analyses limited to trials at low summary risk of bias, low risk of compliance issues, and larger trials also suggested little or no effect of LCn3 on serum total cholesterol (Analysis 2.34; Analysis 2.35), but fixed‐effect meta‐analysis suggested that LCn3 reduced serum total cholesterol (MD −0.04 mmol/L, 95% CI −0.06 to −0.02, I2 = 19%, not shown). Subgrouping by duration did not suggest any differential effects of LCn3 (Analysis 2.39). There were significant differences between subgroups by dose but no logical sequence suggesting a true dose‐response effect (P = 0.03, Analysis 2.36). There were also subgroup differences for replacement and intervention type (Analysis 2.37; Analysis 2.38), with reductions in serum total cholesterol when supplemental capsules were used and when LCn3 replaced carbohydrates (Analysis 2.36; Analysis 2.37; Analysis 2.38).
Analysis 2.33.
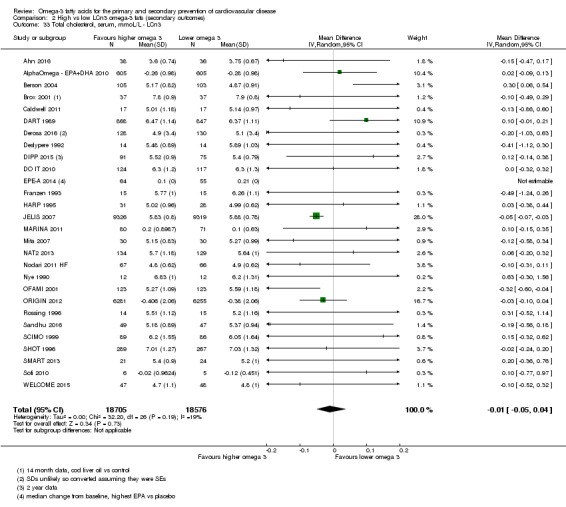
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 33 Total cholesterol, serum, mmoL/L ‐ LCn3.
Analysis 2.34.
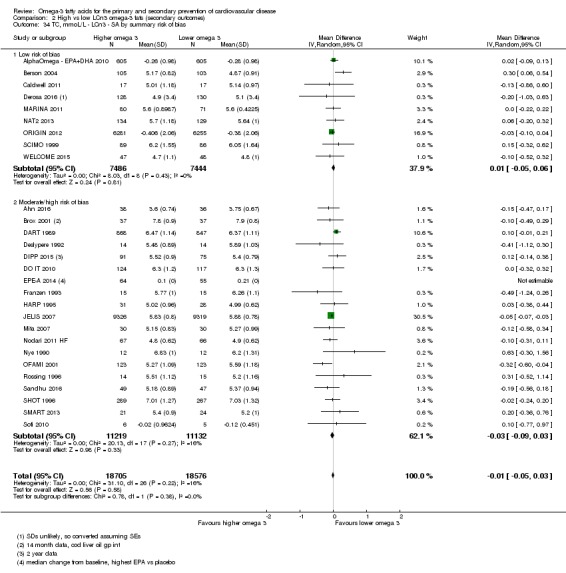
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 34 TC, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.35.
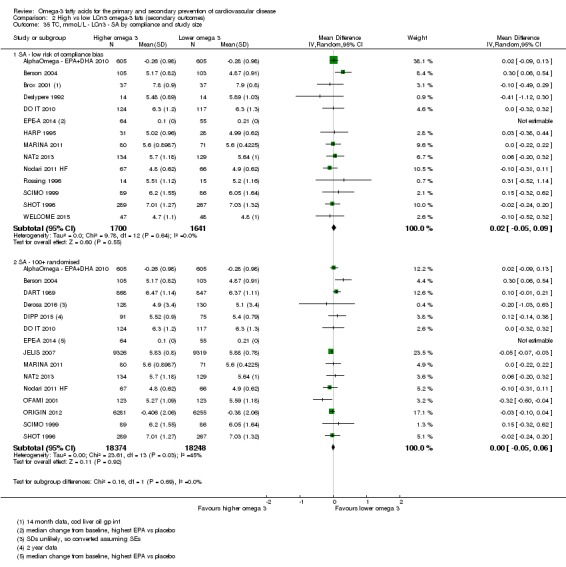
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 35 TC, mmoL/L ‐ LCn3 ‐ SA by compliance and study size.
Analysis 2.39.
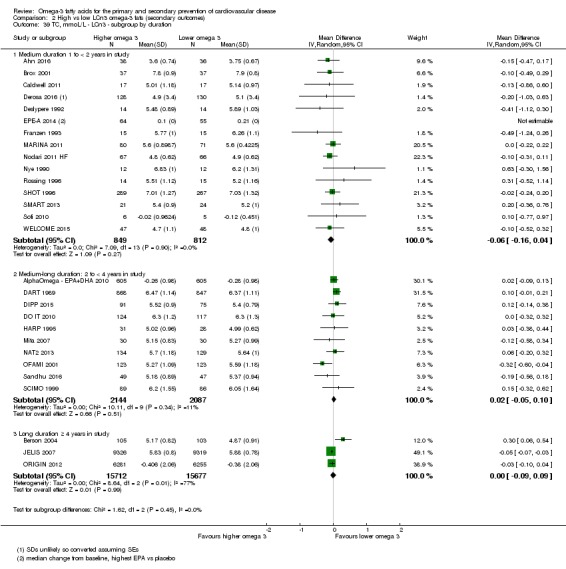
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 39 TC, mmoL/L ‐ LCn3 ‐ subgroup by duration.
Analysis 2.36.
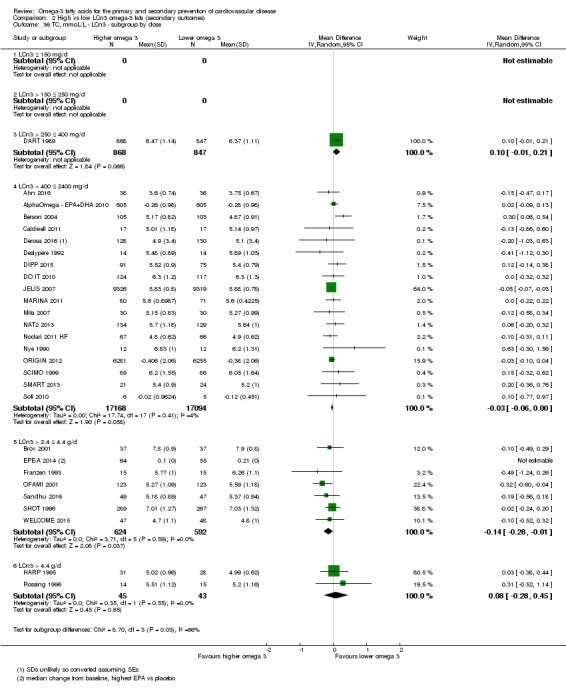
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 36 TC, mmoL/L ‐ LCn3 ‐ subgroup by dose.
Analysis 2.37.
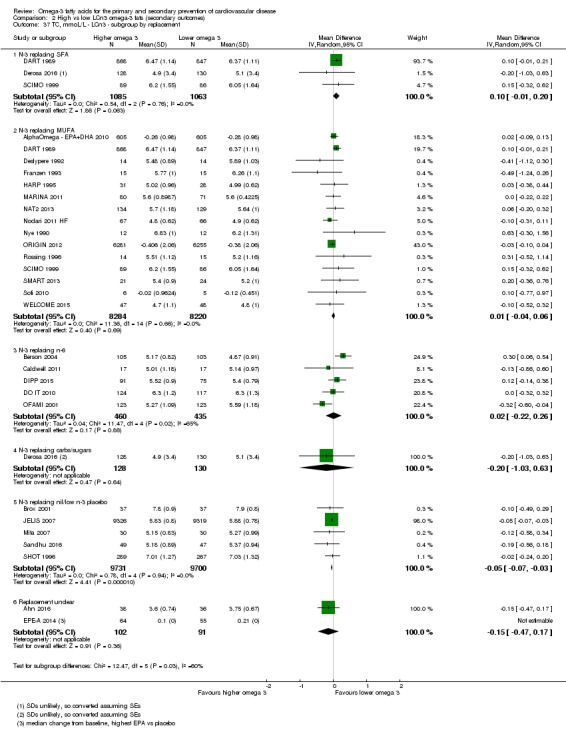
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 37 TC, mmoL/L ‐ LCn3 ‐ subgroup by replacement.
Analysis 2.38.
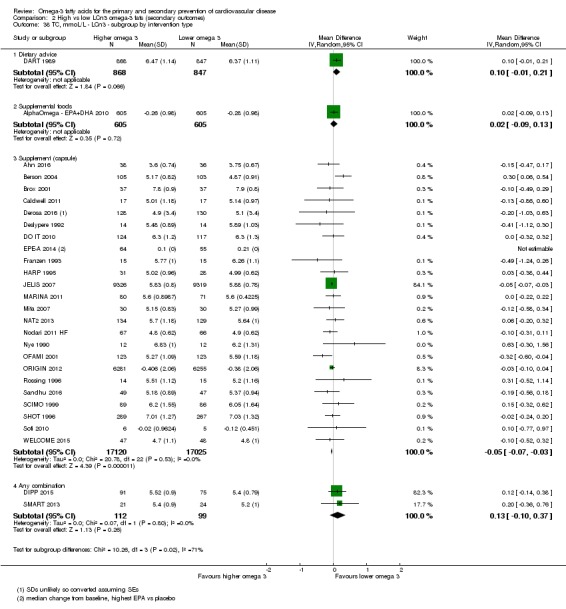
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 38 TC, mmoL/L ‐ LCn3 ‐ subgroup by intervention type.
GRADE assessment suggests moderate‐quality evidence that LCn3 intake probably makes little or no difference to serum total cholesterol (moderate‐quality/certainty evidence, downgraded once for imprecision).
Serum triglycerides
High‐quality evidence suggests that LCn3 intake reduces serum triglycerides in a dose‐dependent manner.
LCn3 fats significantly reduced serum triglycerides in > 35,000 participants in 23 trials (MD −0.24 mmol/L, 95% CI −0.31 to −0.16, I2 = 48%, Analysis 2.42). This effect was not lost in sensitivity analysis excluding studies at moderate to high risk of bias, those without clear compliance or small studies (Analysis 2.43; Analysis 2.44), or using fixed‐effect analysis (not shown). Subgrouping suggested that the reduction of serum triglycerides did not differ between subgroups by primary or secondary prevention, statin use, replacement, intervention type or trial duration ( Analysis 2.46; Analysis 2.47; Analysis 2.48; Analysis 2.49; Analysis 2.50). There was a suggestion of a dose‐response relationship with greater reductions in triglycerides at higher LCn3 doses, with significant differences between subgroups (P = 0.04, Analysis 2.45).
Analysis 2.42.
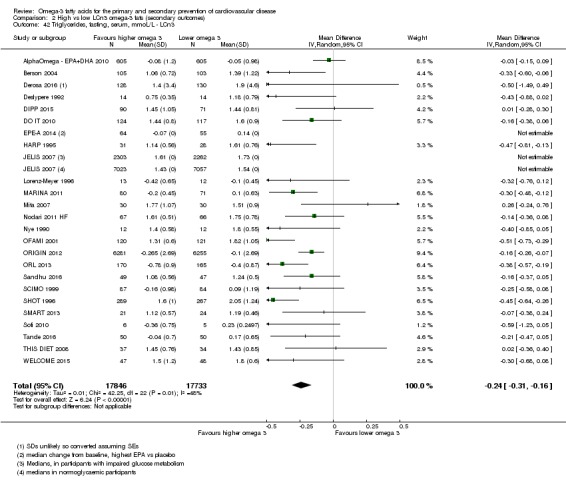
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 42 Triglycerides, fasting, serum, mmoL/L ‐ LCn3.
Analysis 2.43.
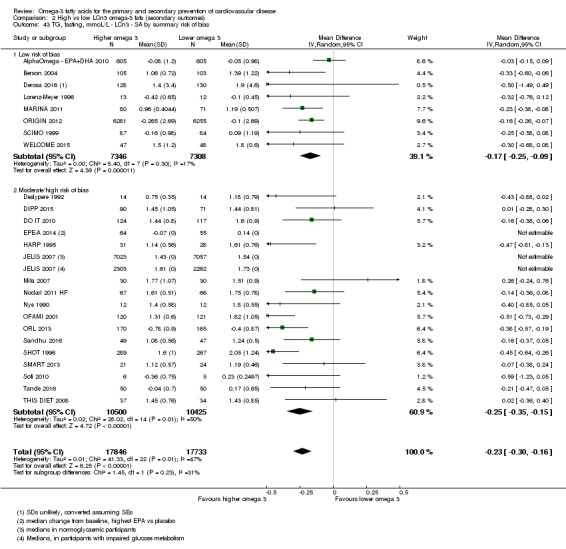
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 43 TG, fasting, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.44.
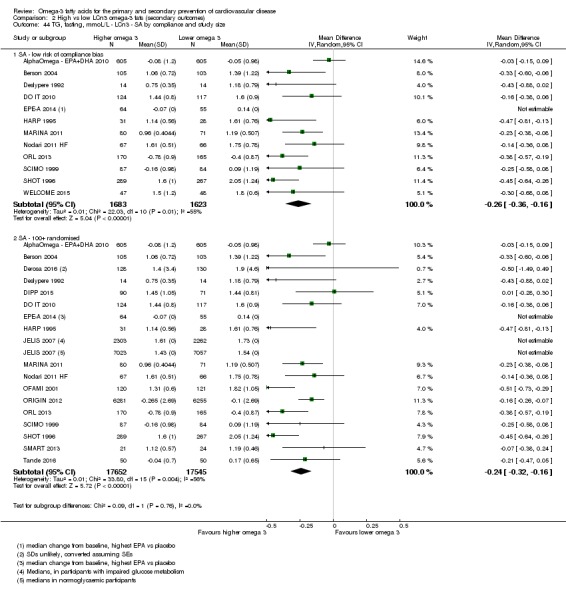
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 44 TG, fasting, mmoL/L ‐ LCn3 ‐ SA by compliance and study size.
Analysis 2.46.
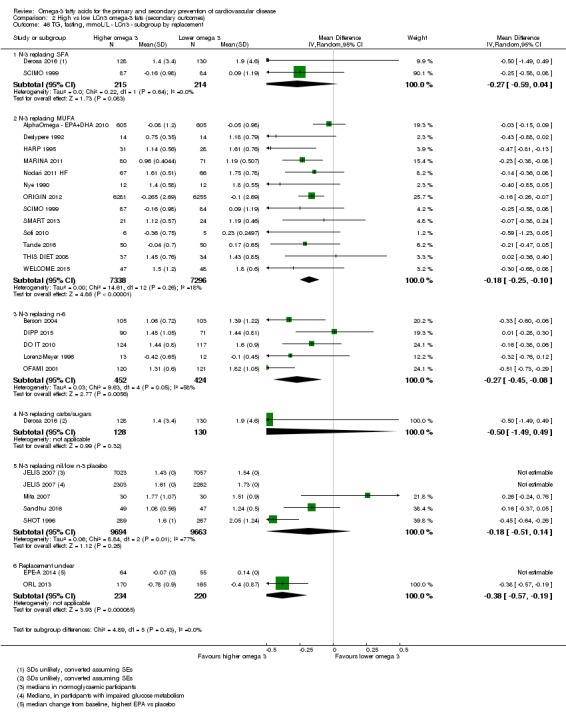
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 46 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by replacement.
Analysis 2.47.
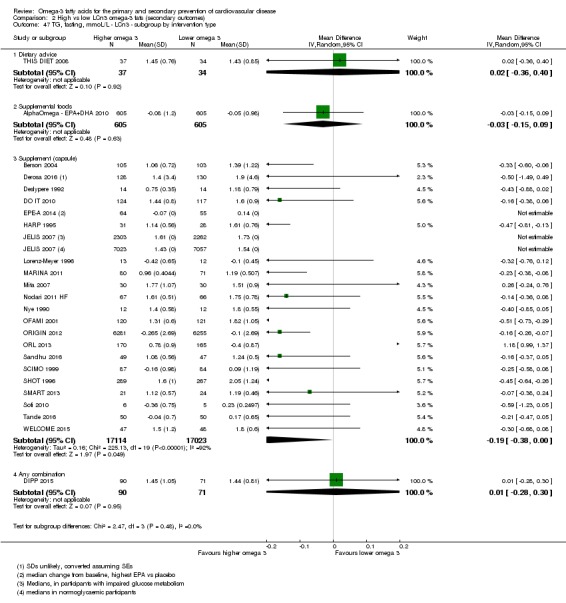
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 47 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by intervention type.
Analysis 2.48.
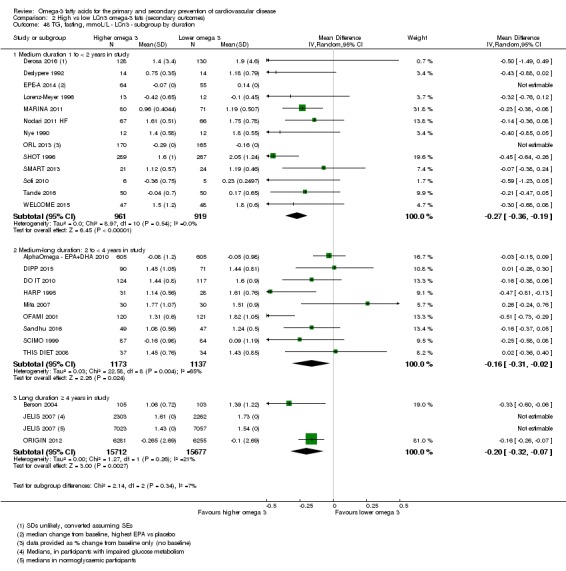
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 48 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by duration.
Analysis 2.49.
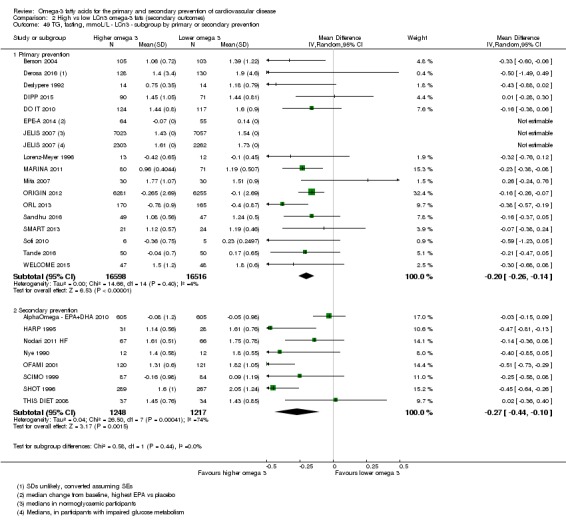
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 49 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 2.50.
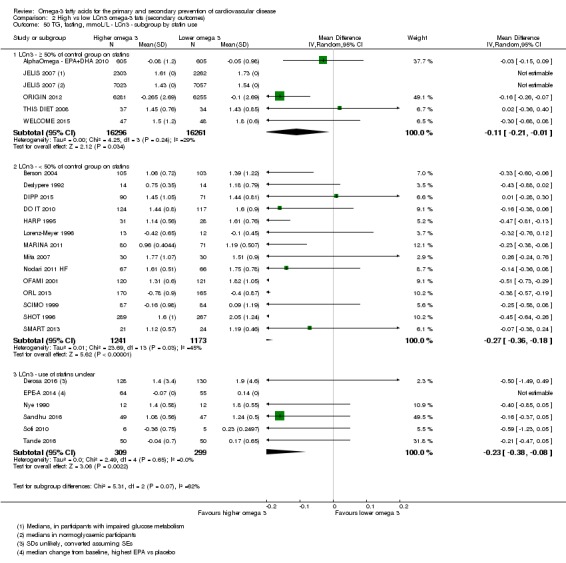
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 50 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by statin use.
Analysis 2.45.
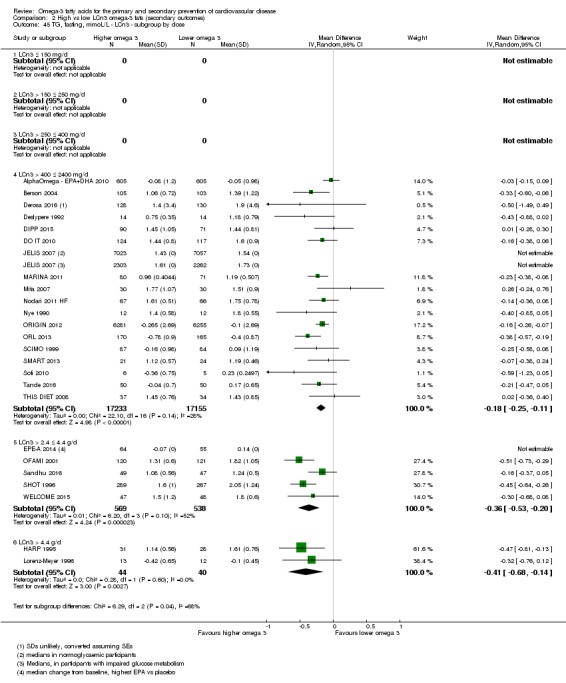
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 45 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by dose.
GRADE evidence suggests high‐quality evidence that LCn3 intake reduces serum triglycerides in a dose‐dependent manner (not downgraded).
HDL cholesterol
High‐quality evidence suggests that LCn3 intake increases HDL cholesterol a small amount.
Twenty‐seven trials including more than 37,000 participants suggested an increase in serum HDL cholesterol with increased LCn3 (MD 0.02 mmol/L, 95% CI 0.00 to 0.04, P = 0.03, I2 = 48%, Analysis 2.51). There was still a suggestion of a small HDL increase when we limited analysis to the eight studies at low summary risk of bias (MD 0.03 mmol/L, 95% CI −0.01 to 0.07, I2 = 66%, > 14,000 participants, Analysis 2.52) where heterogeneity was very high. Limiting analyses by compliance and study size (Analysis 2.53) and in fixed‐effect analysis (not shown), results suggested increases in HDL with LCn3. There were no significant differences between subgroups in any analysis except by duration, where shorter trials suggested HDL increases, with no effect in longer trials (P = 0.05, Analysis 2.57). There were no important differences between other subgroups and no suggestion of a dose‐response relationship (Analysis 2.54; Analysis 2.55; Analysis 2.56; Analysis 2.58; Analysis 2.59).
Analysis 2.51.
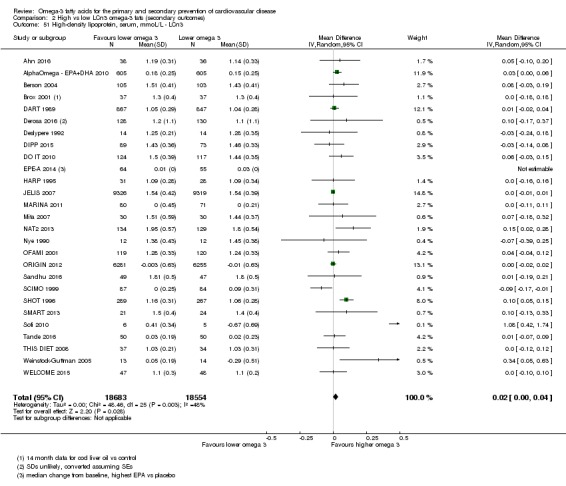
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 51 High‐density lipoprotein, serum, mmoL/L ‐ LCn3.
Analysis 2.52.
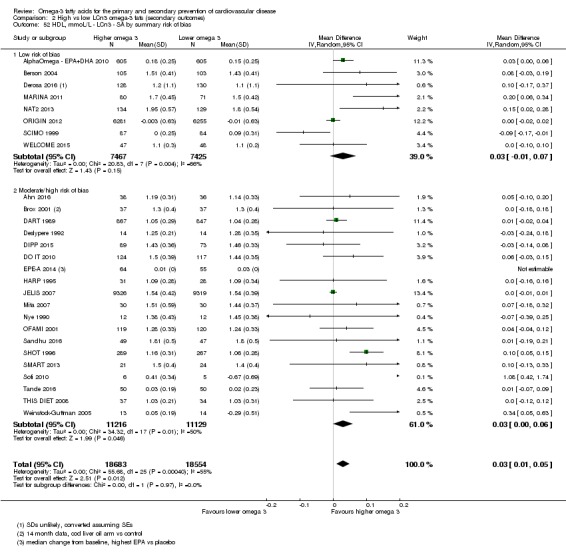
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 52 HDL, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.53.
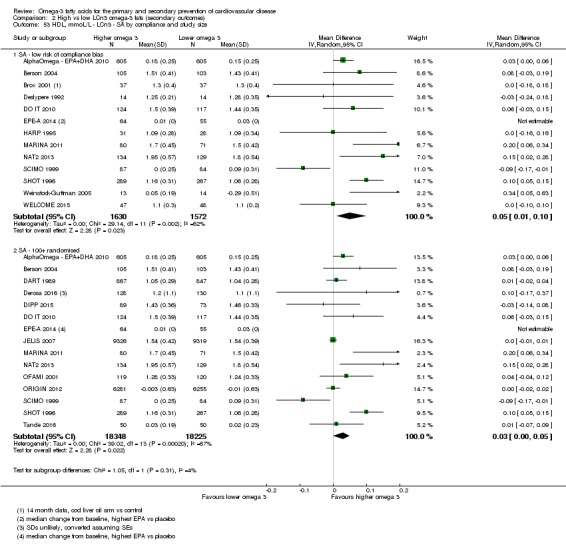
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 53 HDL, mmoL/L ‐ LCn3 ‐ SA by compliance and study size.
Analysis 2.57.
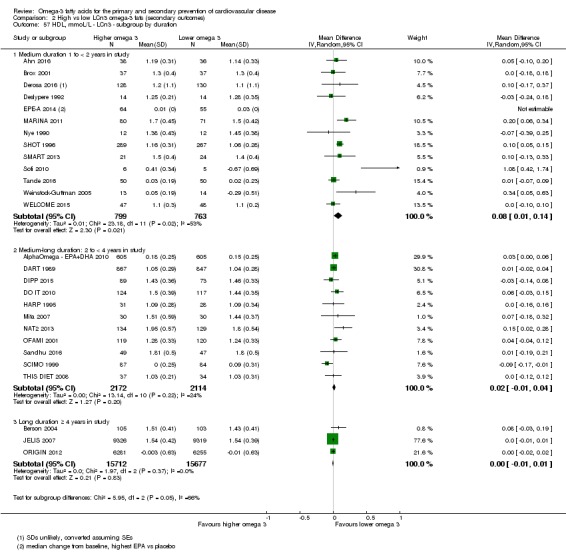
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 57 HDL, mmoL/L ‐ LCn3 ‐ subgroup by duration.
Analysis 2.54.
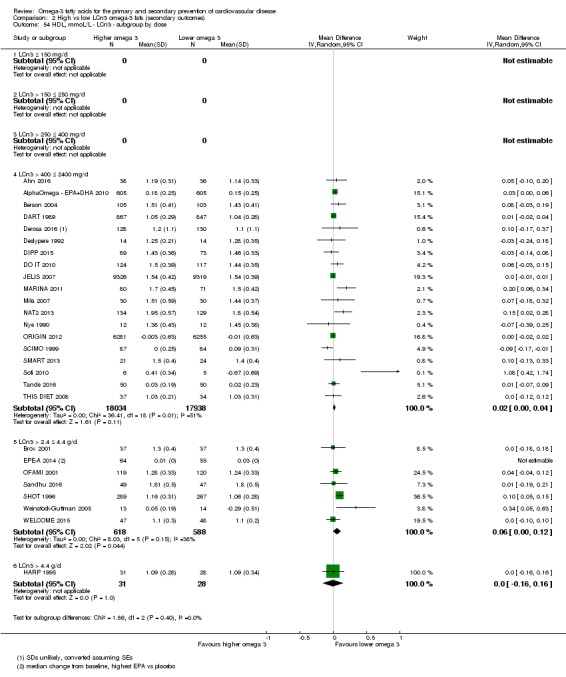
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 54 HDL, mmoL/L ‐ LCn3 ‐ subgroup by dose.
Analysis 2.55.
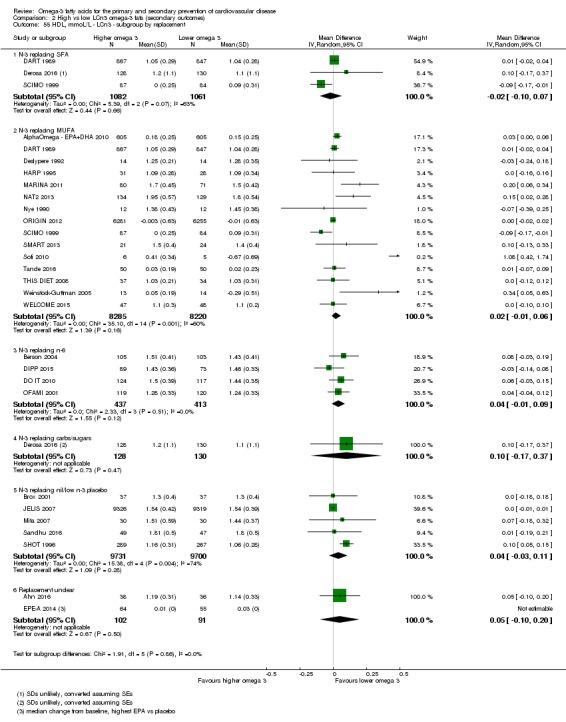
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 55 HDL, mmoL/L ‐ LCn3 ‐ subgroup by replacement.
Analysis 2.56.
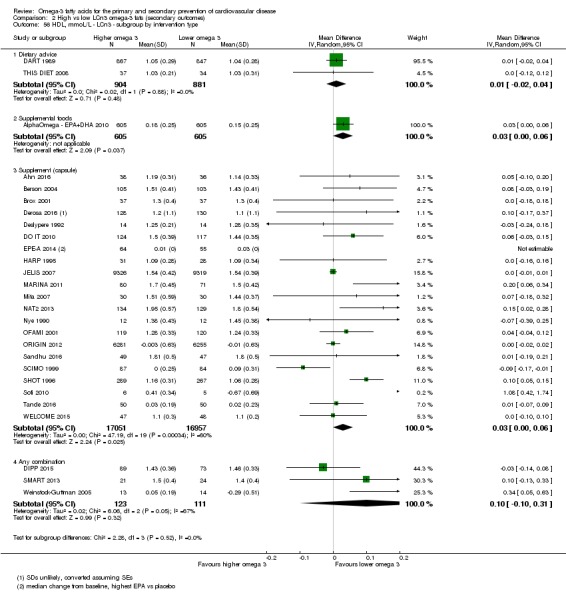
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 56 HDL, mmoL/L ‐ LCn3 ‐ subgroup by intervention type.
Analysis 2.58.
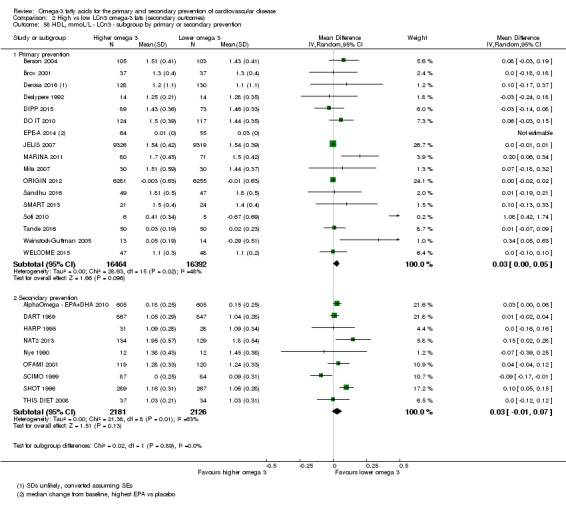
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 58 HDL, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 2.59.
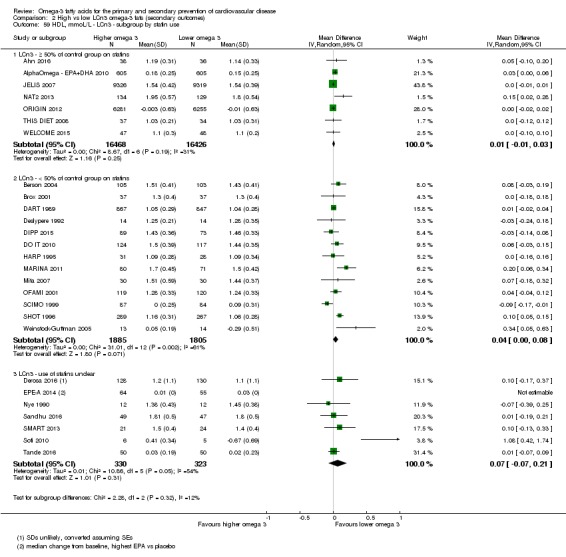
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 59 HDL, mmoL/L ‐ LCn3 ‐ subgroup by statin use.
GRADE assessment suggests high‐quality evidence that LCn3 intake increases HDL cholesterol a little (not downgraded).
LDL cholesterol
GRADE assessment suggests moderate‐quality evidence that LCn3 intake probably makes little or no difference to LDL cholesterol.
There was little or no effect of increasing LCn3 on serum LDL cholesterol in over 35,000 participants from 23 trials (MD 0.01 mmol/L, 95% CI −0.01 to 0.03, I2 = 0%, Analysis 2.60). This lack of effect did not alter in sensitivity analyses limited to trials at low summary risk of bias, to trials with good evidence of compliance (Analysis 2.61) , larger studies (Analysis 2.62) or in fixed‐effect meta‐analysis (not shown). We saw no statistically significant differences between subgroups except for with regard to statin use, where there was an increase in LDL cholesterol in nine trials where statin use was low (Analysis 2.63; Analysis 2.64; Analysis 2.65; Analysis 2.66; Analysis 2.67; Analysis 2.68).
Analysis 2.60.
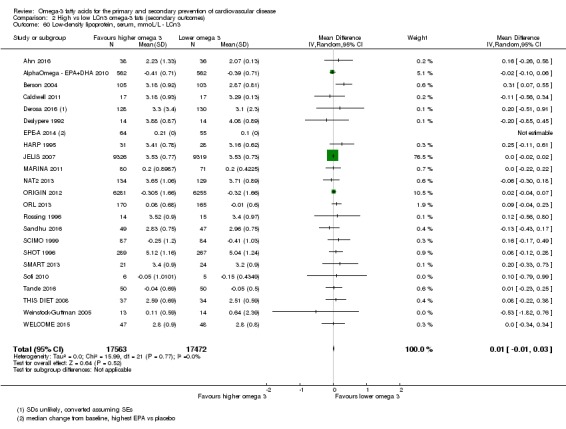
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 60 Low‐density lipoprotein, serum, mmoL/L ‐ LCn3.
Analysis 2.61.
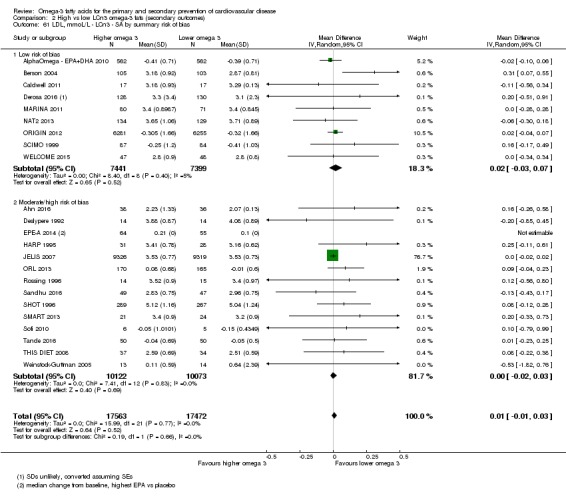
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 61 LDL, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias.
Analysis 2.62.
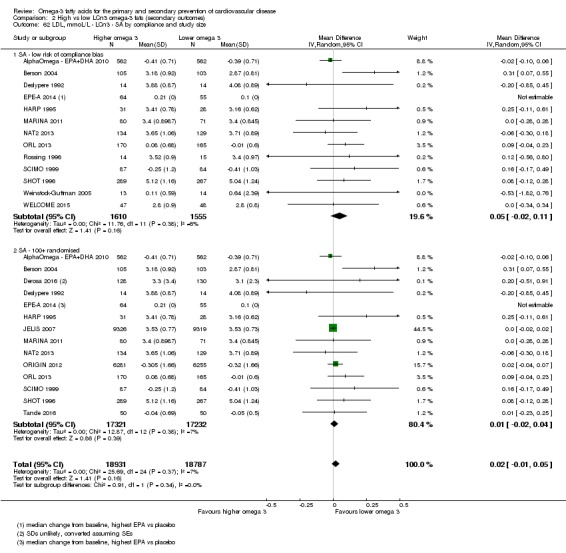
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 62 LDL, mmoL/L ‐ LCn3 ‐ SA by compliance and study size.
Analysis 2.63.
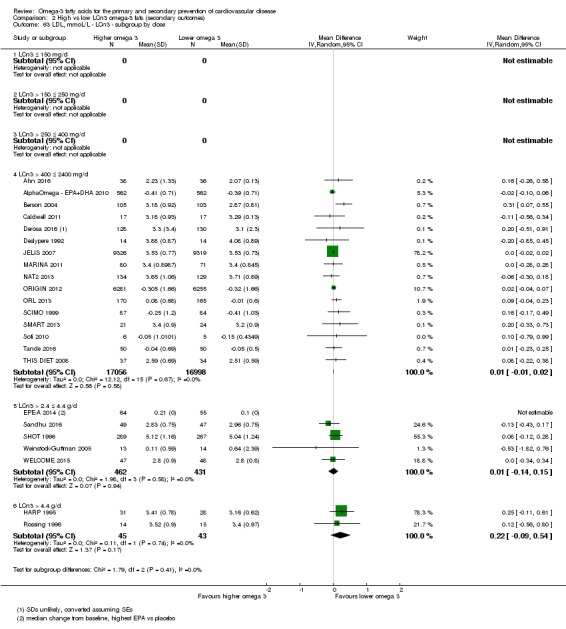
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 63 LDL, mmoL/L ‐ LCn3 ‐ subgroup by dose.
Analysis 2.64.
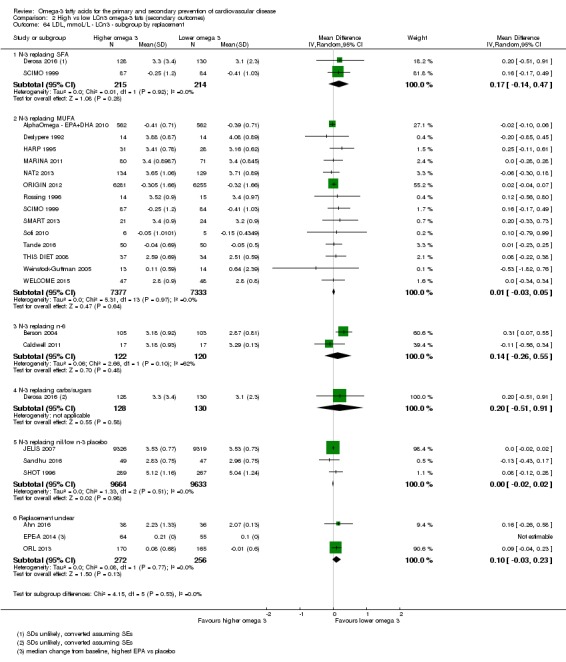
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 64 LDL, mmoL/L ‐ LCn3 ‐ subgroup by replacement.
Analysis 2.65.
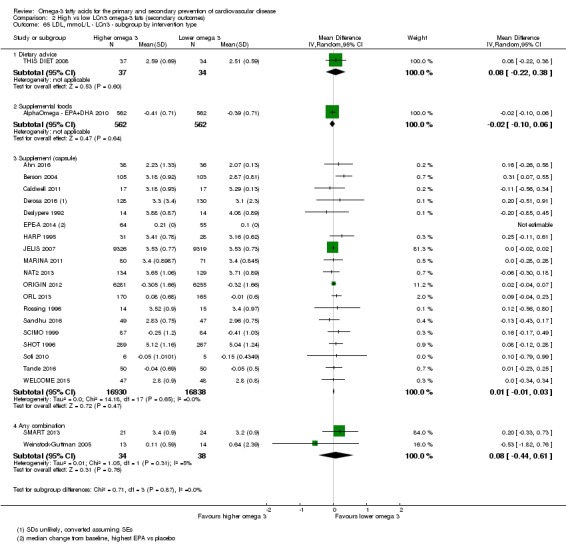
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 65 LDL, mmoL/L ‐ LCn3 ‐ subgroup by intervention type.
Analysis 2.66.
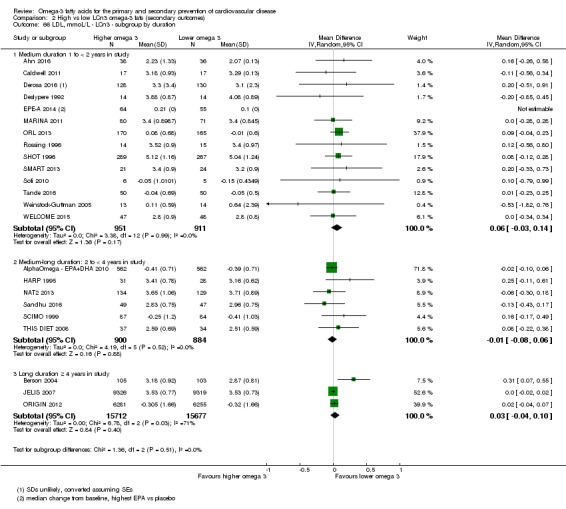
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 66 LDL, mmoL/L ‐ LCn3 ‐ subgroup by duration.
Analysis 2.67.
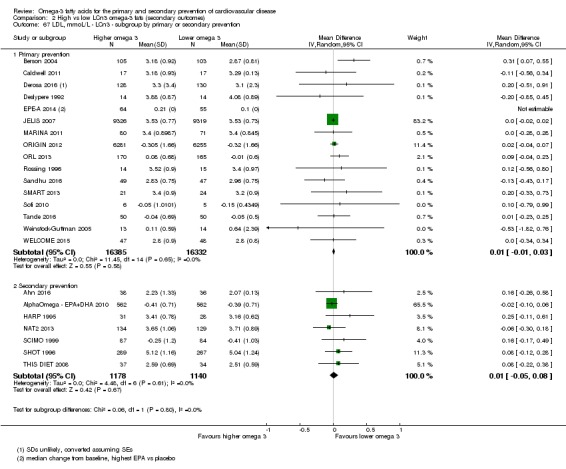
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 67 LDL, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 2.68.
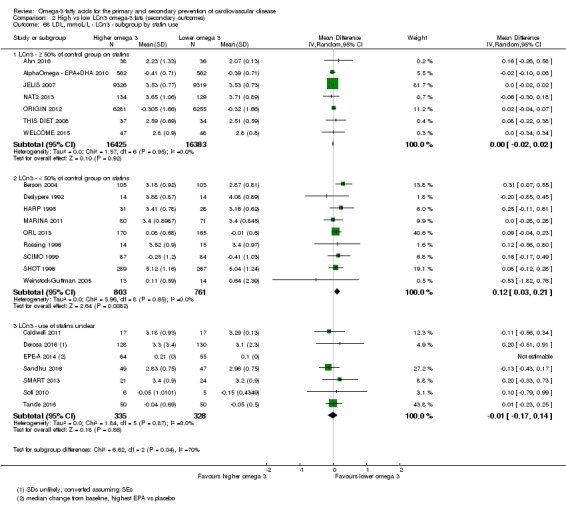
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 68 LDL, mmoL/L ‐ LCn3 ‐ subgroup by statin use.
GRADE assessment suggests moderate‐quality evidence that LCn3 intake probably makes little or no difference to LDL cholesterol (moderate‐quality/certainty evidence, downgraded once for imprecision).
Effects of ALA on secondary health outcomes
We did not plan any sensitivity or subgroup analyses on secondary outcomes, except for adiposity and lipids (key outcomes). As fewer than 10 ALA trials were available for these outcomes, we carried out only sensitivity analyses.
Major adverse cerebrovascular or cardiovascular events (ALA)
One trial reported on MACCEs in 110 participants, 9 of whom experienced an event. There were insufficient data to suggest any effect of ALA on MACCEs (RR 1.12, 95% CI 0.32 to 3.95, Analysis 5.1).
Analysis 5.1.
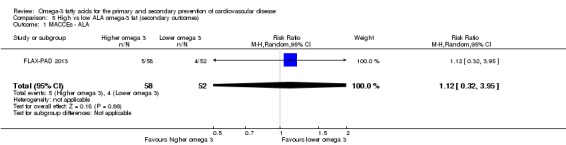
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 1 MACCEs ‐ ALA.
Myocardial infarction (ALA)
Three studies reported that 333 out of more than 18,000 participants experienced a fatal or non‐fatal MI, suggesting little or no effect of ALA on MI (RR 1.00, 95% CI 0.76 to 1.32, I2 = 26%, Analysis 5.2).
Analysis 5.2.
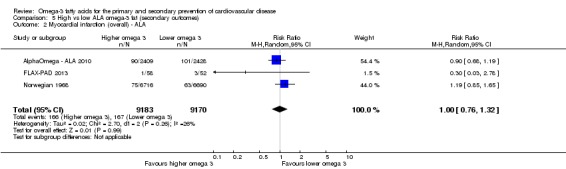
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 2 Myocardial infarction (overall) ‐ ALA.
We carried out subgroup analyses by fatality at the request of the WHO NUGAG Subgroup on Diet and Health, and these suggested no significant differences between fatal and non‐fatal MI subgroups (P = 0.36, Analysis 5.3).
Analysis 5.3.
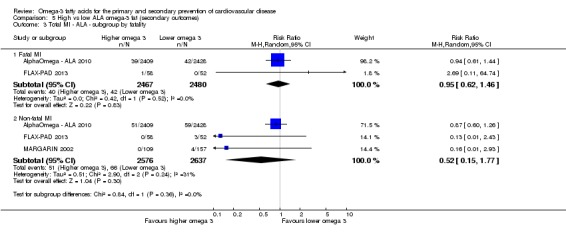
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 3 Total MI ‐ ALA ‐ subgroup by fatality.
Sudden cardiac death (ALA)
No studies assessed effects of ALA on sudden cardiac death.
Angina (ALA)
Two trials assessed the effects of increasing ALA on diagnosis of new or worsening angina (39 of > 13,000 participants experienced this). There were insufficient data to suggest any effect of ALA on angina (RR1.41, 95% CI 0.75 to 2.64, I2 = 0%, Analysis 5.4).
Analysis 5.4.
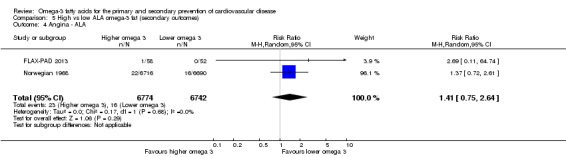
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 4 Angina ‐ ALA.
Heart failure (ALA)
No studies assessed effects of ALA on heart failure.
Revascularisation (ALA)
Only one trial (3 events in 266 participants) reported on the effects of increased ALA on revascularisation (RR 0.72, 95% CI 0.07 to 7.84, 3 events, Analysis 5.5) or CABG specifically (RR 0.29, 95% CI 0.01 to 5.93, 2 events, Analysis 5.5). There were insufficient data to suggest any effect of ALA on revascularisation.
Analysis 5.5.
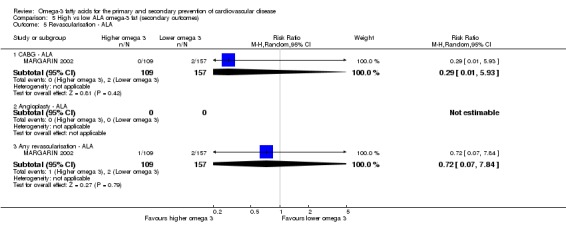
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 5 Revascularisation ‐ ALA.
Peripheral arterial disease (ALA)
Meta‐analysis suggested no clear effect of ALA on PAD in a single study (RR 0.25, 95% CI 0.05 to 1.17, 10 of the > 13,000 participants experienced PAD, Analysis 5.6). There were insufficient data to suggest any effect of ALA on the outcome.
Analysis 5.6.
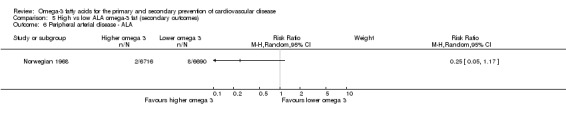
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 6 Peripheral arterial disease ‐ ALA.
Acute coronary syndrome (ALA)
There were no trials assessing effects of ALA on acute coronary syndrome.
Body weight, BMI and other measures of adiposity (ALA)
Low‐quality evidence suggests that ALA intake may make little or no difference to BMI, but the effect of LCn3 intake on body weight is unclear as the evidence is of very low quality.
Four studies reported on the effect of ALA on body weight in 664 participants, suggesting some weight reduction in those taking more ALA but with extremely high heterogeneity (MD −1.49 kg, 95% CI −4.17 to 1.18, I2 = 73%, Analysis 5.7). Sensitivity analysis using fixed‐effect meta‐analysis suggested a slight increase in body weight with ALA (Analysis 5.8), while no studies were at low summary risk of bias (Analysis 5.9). Retaining only trials at low risk for compliance bias or only larger trials suggested weight reduction with ALA (Analysis 5.10). There were no significant differences between subgroups by intervention type, dose, duration, replacement, statin use, or primary or secondary prevention of CVD (Analysis 5.11; Analysis 5.12; Analysis 5.13; Analysis 5.14; Analysis 5.15; Analysis 5.16). GRADE assessment suggests that the effect of ALA intake on body weight is unclear, as the evidence is of very low quality (downgraded once each for risk of bias, inconsistency and imprecision).
Analysis 5.7.
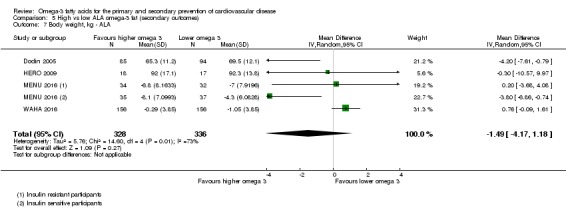
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 7 Body weight, kg ‐ ALA.
Analysis 5.8.
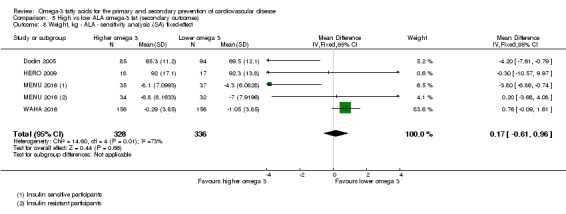
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 8 Weight, kg ‐ ALA ‐ sensitivity analysis (SA) fixed‐effect.
Analysis 5.9.
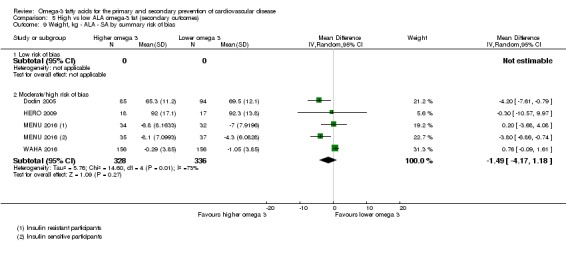
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 9 Weight, kg ‐ ALA ‐ SA by summary risk of bias.
Analysis 5.10.
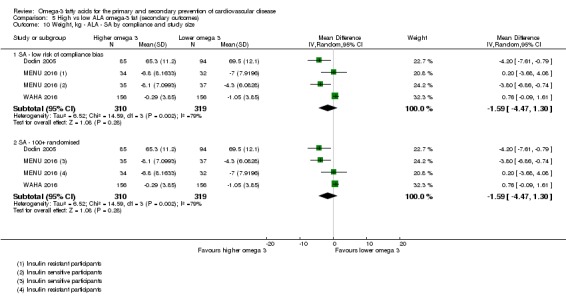
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 10 Weight, kg ‐ ALA ‐ SA by compliance and study size.
Analysis 5.11.
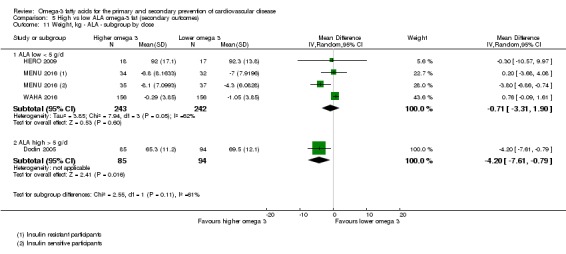
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 11 Weight, kg ‐ ALA ‐ subgroup by dose.
Analysis 5.12.
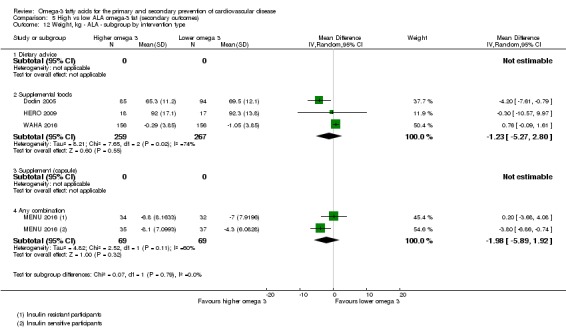
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 12 Weight, kg ‐ ALA ‐ subgroup by intervention type.
Analysis 5.13.
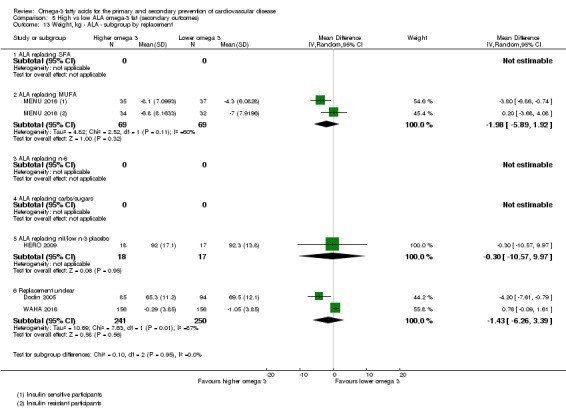
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 13 Weight, kg ‐ ALA ‐ subgroup by replacement.
Analysis 5.14.
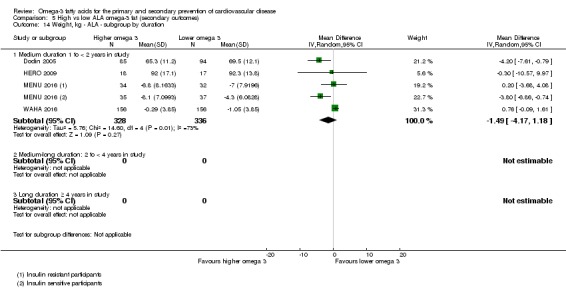
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 14 Weight, kg ‐ ALA ‐ subgroup by duration.
Analysis 5.15.
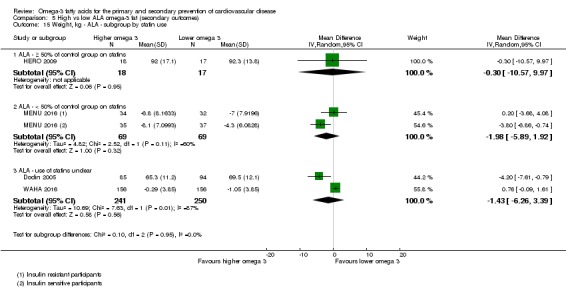
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 15 Weight, kg ‐ ALA ‐ subgroup by statin use.
Analysis 5.16.
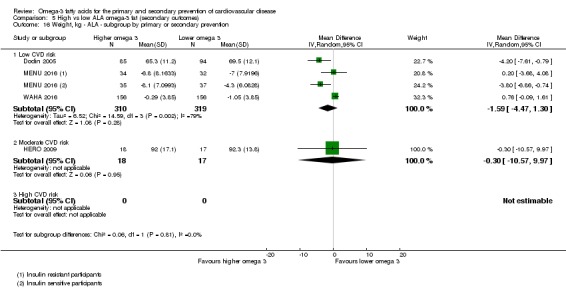
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 16 Weight, kg ‐ ALA ‐ subgroup by primary or secondary prevention.
Three trials reported on BMI, suggesting a reduction in BMI with increased ALA (MD −0.42 kg/m2, 95% CI −1.53 to 0.69, I2 = 65%, 1581 participants, Analysis 5.17), again with high heterogeneity. Sensitivity analyses using fixed‐effect analysis or only retaining studies at low summary risk of bias suggested a small increase in BMI with ALA (Analysis 5.18; Analysis 5.19), while limiting to studies at low risk of compliance bias or eliminating smaller studies suggested a small reduction in BMI with increased ALA (Analysis 5.20). There were no statistically significant differences between subgroups differentiated by replacement or statin use (Analysis 5.23; Analysis 5.25), but there were differences by dose – subgrouping by dose suggested greater reduction of BMI in studies giving more ALA (P = 0.03, Analysis 5.21). All included studies gave supplemental foods (Analysis 5.22). There were greater reductions in BMI in shorter studies (P = 0.02, Analysis 5.24) and in primary prevention studies (P = 0.03, Analysis 5.26), but the inclusion of Dodin 2005 in any subgroup tended to differentiate that group from the others. GRADE assessment suggests low‐quality evidence that ALA intake may make little or no difference to BMI (low‐quality/certainty evidence, downgraded once each for imprecision and inconsistency).
Analysis 5.17.
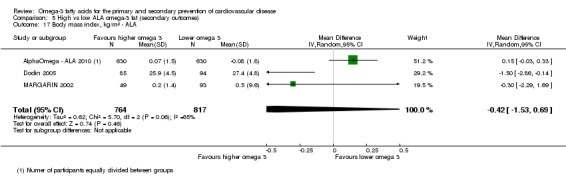
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 17 Body mass index, kg/m² ‐ ALA.
Analysis 5.18.
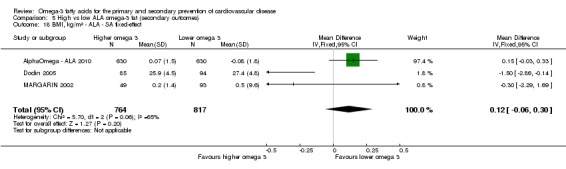
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 18 BMI, kg/m² ‐ ALA ‐ SA fixed‐effect.
Analysis 5.19.
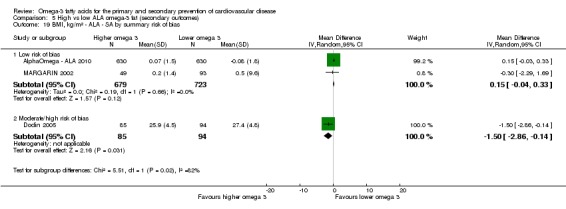
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 19 BMI, kg/m² ‐ ALA ‐ SA by summary risk of bias.
Analysis 5.20.
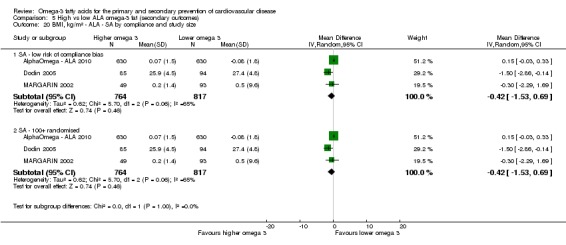
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 20 BMI, kg/m² ‐ ALA ‐ SA by compliance and study size.
Analysis 5.23.
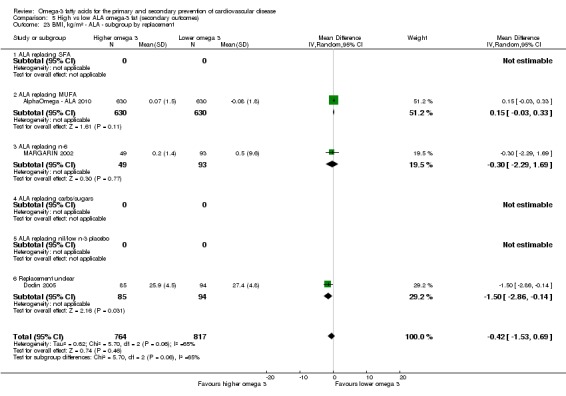
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 23 BMI, kg/m² ‐ ALA ‐ subgroup by replacement.
Analysis 5.25.
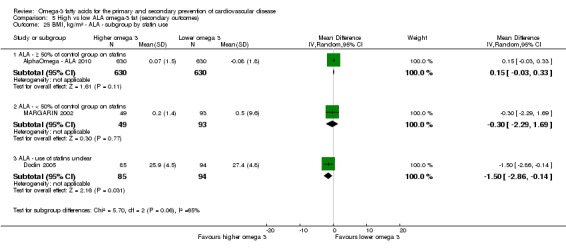
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 25 BMI, kg/m² ‐ ALA ‐ subgroup by statin use.
Analysis 5.21.
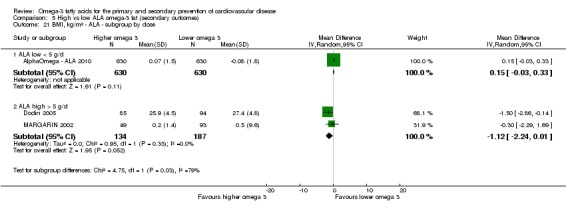
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 21 BMI, kg/m² ‐ ALA ‐ subgroup by dose.
Analysis 5.22.
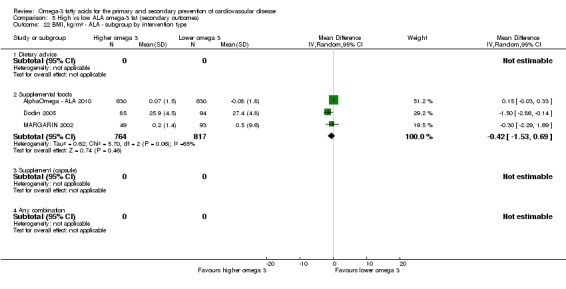
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 22 BMI, kg/m² ‐ ALA ‐ subgroup by intervention type.
Analysis 5.24.
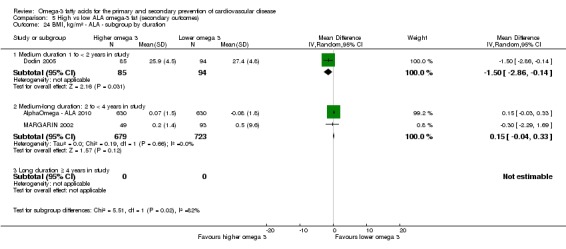
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 24 BMI, kg/m² ‐ ALA ‐ subgroup by duration.
Analysis 5.26.
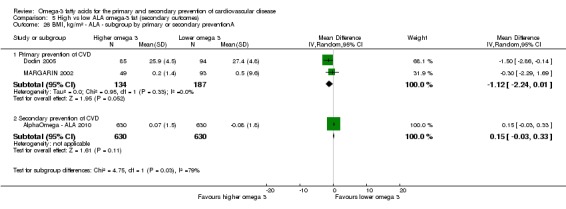
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 26 BMI, kg/m² ‐ ALA ‐ subgroup by primary or secondary preventionA.
One study reported on visceral adipose tissue, suggesting no clear effect, but three trials reported on waist circumference. Meta‐analysis of two of these suggested that increasing ALA resulted in reduced weight circumference (MD −1.59 cm, 95% CI −3.10 to −0.07, I2 = 0%, Analysis 5.27). However, the single trial that we could not include in the meta‐analysis due to lack of information on variance suggested effects in the opposite direction. Sensitivity analyses (only retaining studies at low summary risk of bias, not shown) removed all trials.
Analysis 5.27.
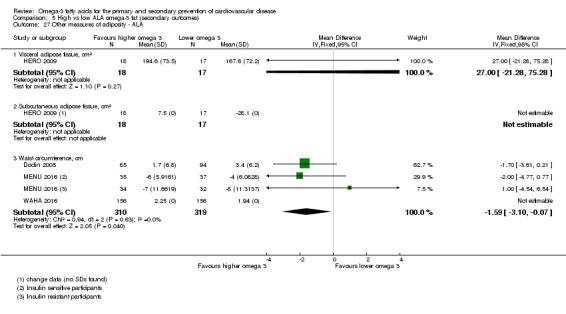
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 27 Other measures of adiposity ‐ ALA.
Serum lipids (ALA)
Serum total cholesterol
Low‐quality evidence suggests that ALA intake may make little or no difference to serum total cholesterol.
Six trials provided data on the long‐term effects of ALA on serum total cholesterol, suggesting that increased ALA intake leads to a small reduction in total cholesterol, but with high heterogeneity (MD −0.09 mmol/L, 95% CI −0.23 to 0.05, I2 = 63%, in > 2000 participants, Analysis 5.28). Restricting analyses to studies at low summary risk of bias suggested no effect of ALA (Analysis 5.30), but fixed‐effect analysis suggested that the intervention led to a reduction (Analysis 5.29), as did sensitivity analyses limited to studies at low risk of compliance bias or larger studies (Analysis 5.31). All studies provided food supplements (Analysis 5.33), but subgroup analyses suggested greater reductions in total cholesterol in shorter duration studies (P = 0.02, Analysis 5.35). Other differences between subgroups resulted from effects groups where ALA replacement or statin use was 'unclear' (Analysis 5.34; Analysis 5.36), or there were no differences (Analysis 5.32; Analysis 5.37). GRADE assessment suggests low‐quality evidence that ALA intake may make little or no difference to serum total cholesterol (downgraded once each for imprecision and inconsistency).
Analysis 5.28.
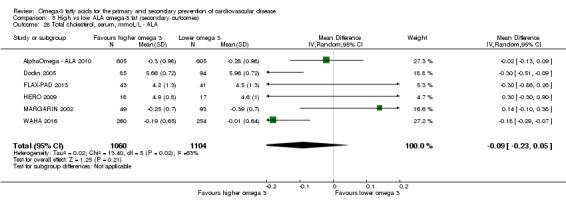
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 28 Total cholesterol, serum, mmoL/L ‐ ALA.
Analysis 5.30.
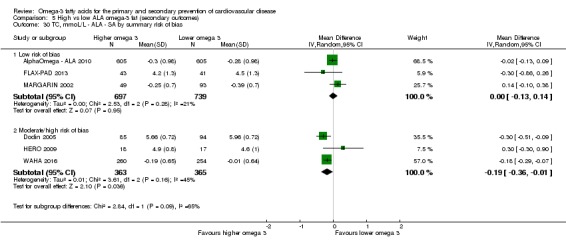
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 30 TC, mmoL/L ‐ ALA ‐ SA by summary risk of bias.
Analysis 5.29.
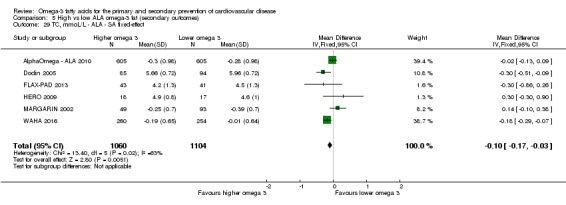
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 29 TC, mmoL/L ‐ ALA ‐ SA fixed‐effect.
Analysis 5.31.
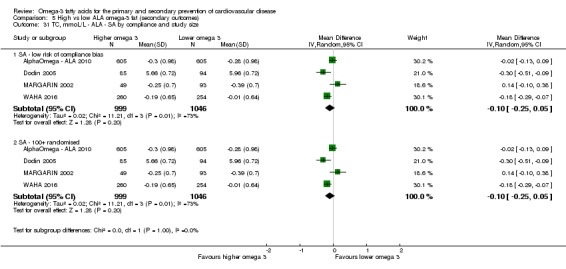
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 31 TC, mmoL/L ‐ ALA ‐ SA by compliance and study size.
Analysis 5.33.
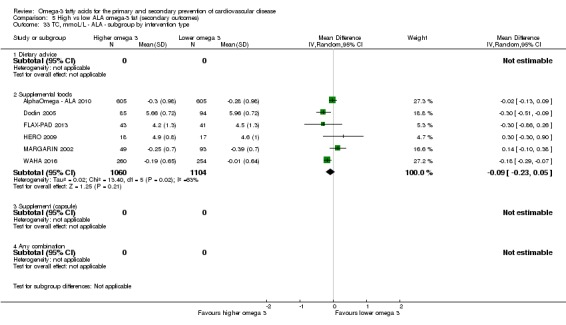
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 33 TC, mmoL/L ‐ ALA ‐ subgroup by intervention type.
Analysis 5.35.
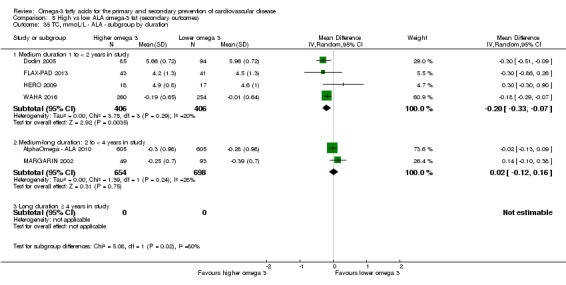
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 35 TC, mmoL/L ‐ ALA ‐ subgroup by duration.
Analysis 5.34.
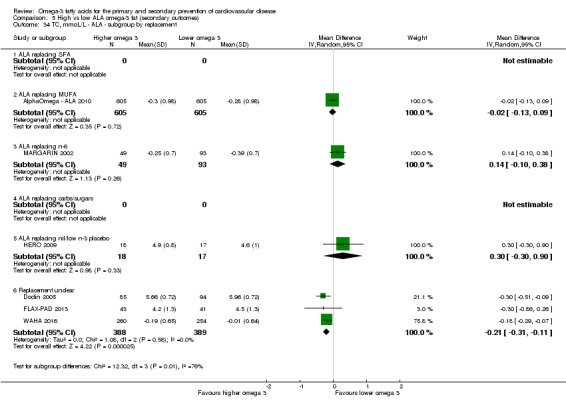
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 34 TC, mmoL/L ‐ ALA ‐ subgroup by replacement.
Analysis 5.36.
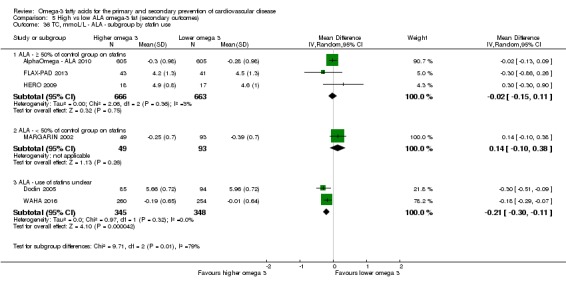
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 36 TC, mmoL/L ‐ ALA ‐ subgroup by statin use.
Analysis 5.32.
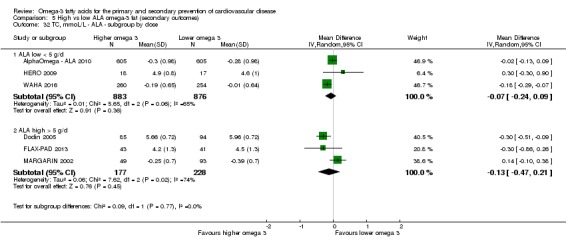
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 32 TC, mmoL/L ‐ ALA ‐ subgroup by dose.
Analysis 5.37.
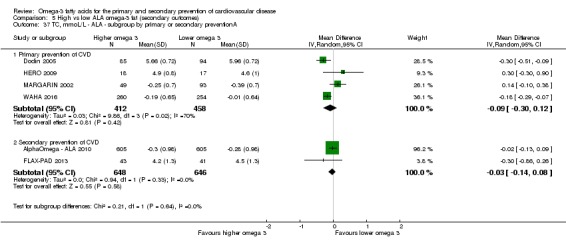
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 37 TC, mmoL/L ‐ ALA ‐ subgroup by primary or secondary preventionA.
Serum triglycerides
Moderate‐quality evidence suggests that ALA intake probably makes little or no difference to serum triglycerides.
There was little or no effect of ALA on serum triglycerides in 1776 participants in six trials (MD −0.03 mmol/L, 95% CI −0.11 to 0.05, I2 = 0%, Analysis 5.38). There was little or no effect of ALA in sensitivity analysis removing trials of moderate to high risk of bias (Analysis 5.40), in fixed‐effect meta‐analysis (Analysis 5.39), or limiting by compliance bias or study size (Analysis 5.41). Subgrouping suggested no important differential effects by dose, duration, replacement, intervention type, statin use, or primary or secondary prevention (Analysis 5.42; Analysis 5.43; Analysis 5.44; Analysis 5.45; Analysis 5.46; Analysis 5.47). GRADE assessment suggests moderate‐quality evidence that ALA intake probably makes little or no difference to serum triglycerides (downgraded once for imprecision).
Analysis 5.38.
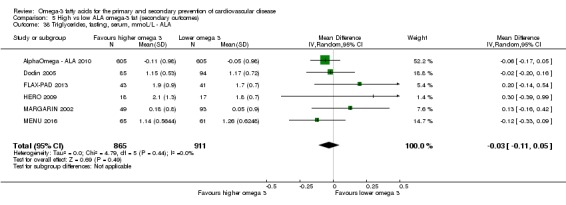
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 38 Triglycerides, fasting, serum, mmoL/L ‐ ALA.
Analysis 5.40.
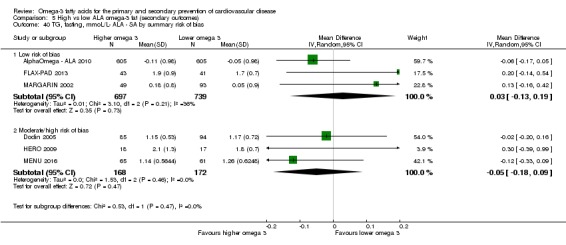
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 40 TG, fasting, mmoL/L‐ ALA ‐ SA by summary risk of bias.
Analysis 5.39.
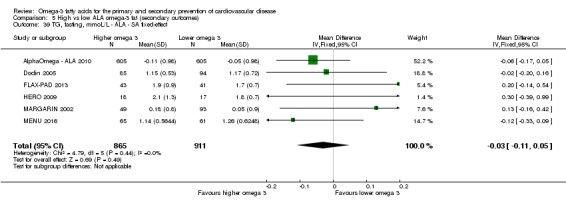
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 39 TG, fasting, mmoL/L ‐ ALA ‐ SA fixed‐effect.
Analysis 5.41.
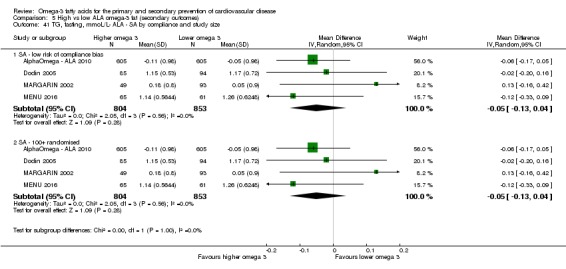
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 41 TG, fasting, mmoL/L‐ ALA ‐ SA by compliance and study size.
Analysis 5.42.
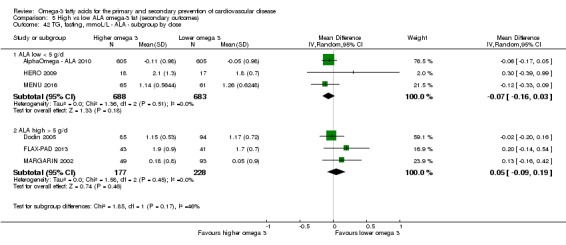
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 42 TG, fasting, mmoL/L ‐ ALA ‐ subgroup by dose.
Analysis 5.43.
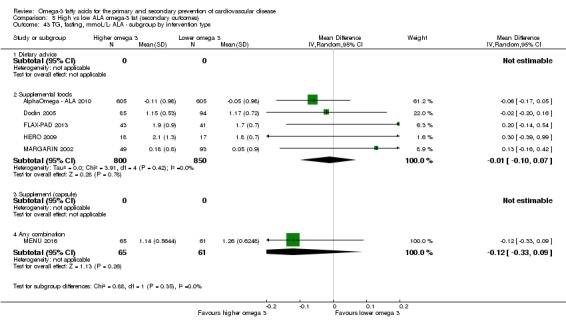
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 43 TG, fasting, mmoL/L‐ ALA ‐ subgroup by intervention type.
Analysis 5.44.
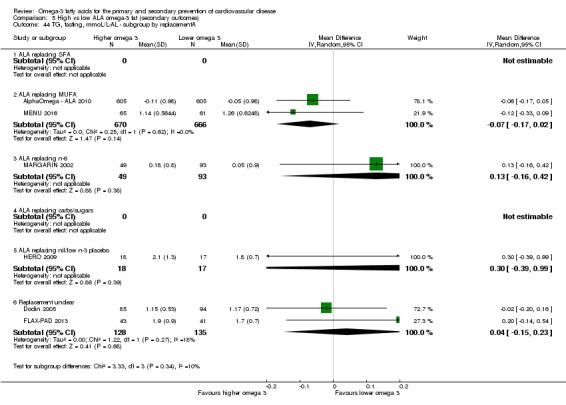
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 44 TG, fasting, mmoL/L‐AL ‐ subgroup by replacementA.
Analysis 5.45.
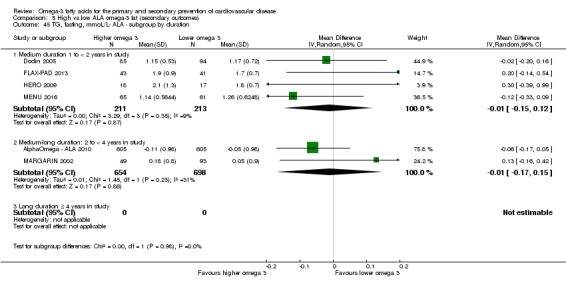
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 45 TG, fasting, mmoL/L‐ ALA ‐ subgroup by duration.
Analysis 5.46.
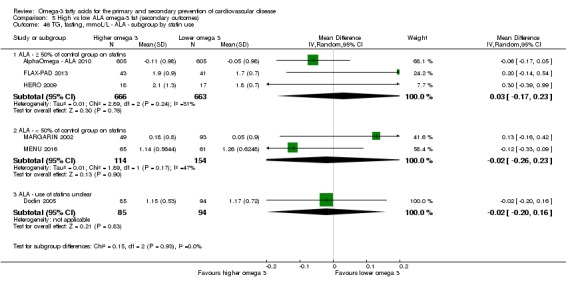
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 46 TG, fasting, mmoL/L ‐ ALA ‐ subgroup by statin use.
Analysis 5.47.
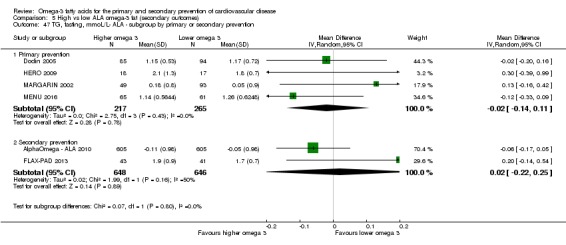
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 47 TG, fasting, mmoL/L‐ ALA ‐ subgroup by primary or secondary prevention.
HDL cholesterol
Moderate‐quality evidence suggests that ALA probably reduces HDL cholesterol.
There was little or no effect of ALA on HDL cholesterol in 1776 participants of 6 trials (MD −0.02 mmol/L, 95% CI −0.08 to 0.03, I2 = 53%, Analysis 5.48), although there were reductions of HDL in both analyses by risk of bias and using fixed‐effect meta‐analysis (Analysis 5.49; Analysis 5.50) with similar effects in studies with good compliance and in larger trials (Analysis 5.51). A further trial, WAHA 2016, also measured HDL but did not provide data in a useable format for meta‐analysis. There was a suggestion of greater HDL reduction with greater ALA dose (P = 0.09, Analysis 5.52), but no other subgrouping effects were evident (Analysis 5.53; Analysis 5.54; Analysis 5.55; Analysis 5.56; Analysis 5.57). GRADE assessment suggests moderate‐quality evidence that ALA probably reduces HDL cholesterol (downgraded for imprecision).
Analysis 5.48.
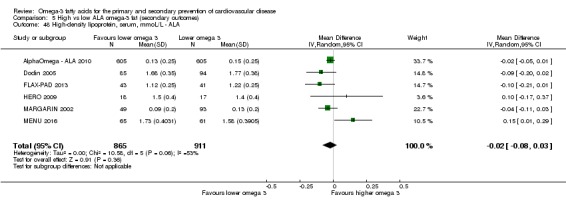
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 48 High‐density lipoprotein, serum, mmoL/L ‐ ALA.
Analysis 5.49.
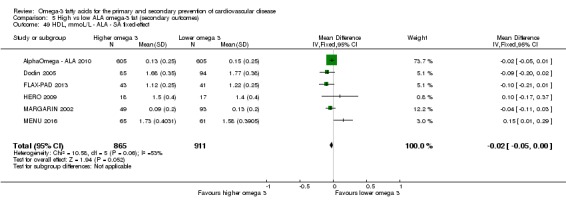
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 49 HDL, mmoL/L ‐ ALA ‐ SA fixed‐effect.
Analysis 5.50.
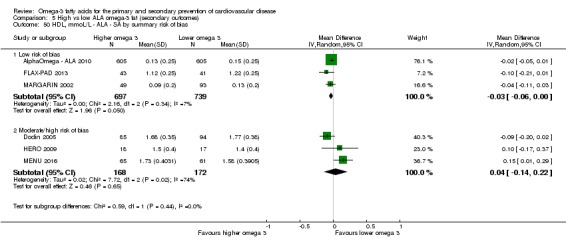
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 50 HDL, mmoL/L ‐ ALA ‐ SA by summary risk of bias.
Analysis 5.51.
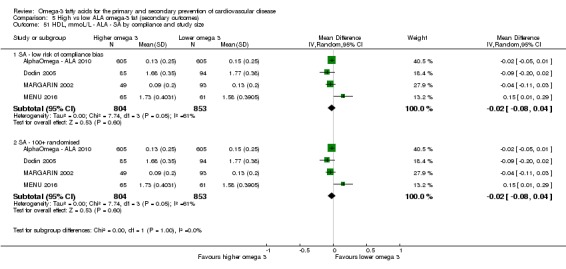
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 51 HDL, mmoL/L ‐ ALA ‐ SA by compliance and study size.
Analysis 5.52.
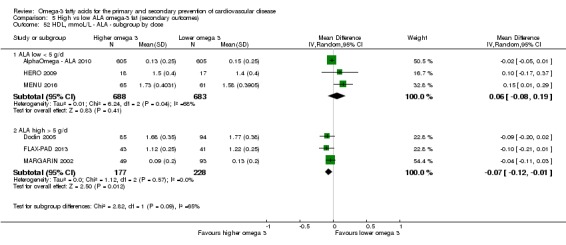
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 52 HDL, mmoL/L ‐ ALA ‐ subgroup by dose.
Analysis 5.53.
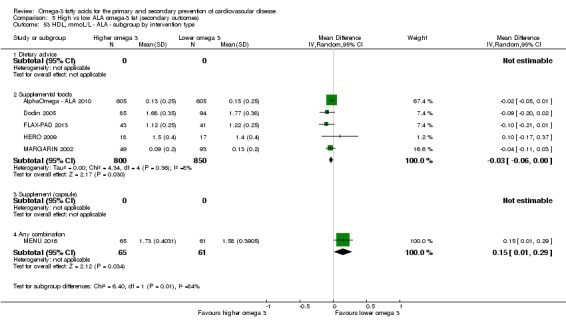
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 53 HDL, mmoL/L ‐ ALA ‐ subgroup by intervention type.
Analysis 5.54.
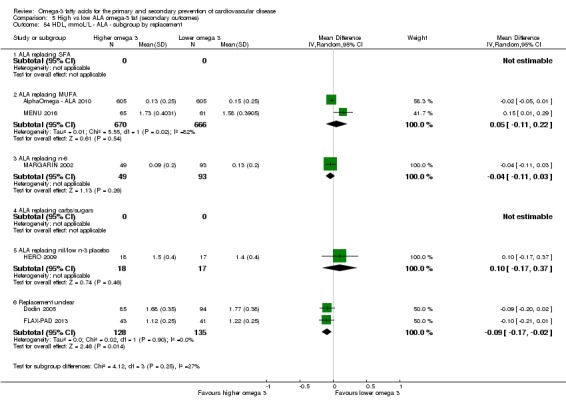
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 54 HDL, mmoL/L ‐ ALA ‐ subgroup by replacement.
Analysis 5.55.
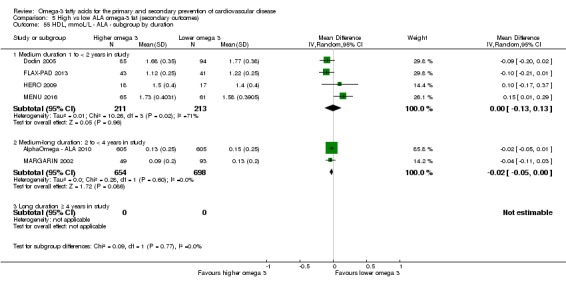
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 55 HDL, mmoL/L ‐ ALA ‐ subgroup by duration.
Analysis 5.56.
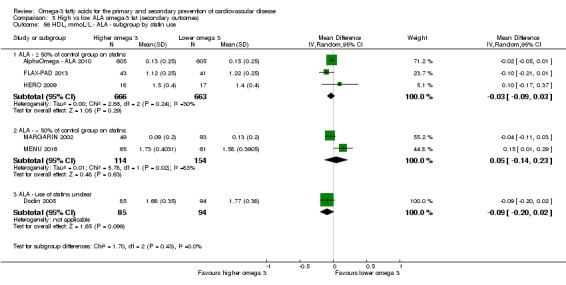
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 56 HDL, mmoL/L ‐ ALA ‐ subgroup by statin use.
Analysis 5.57.
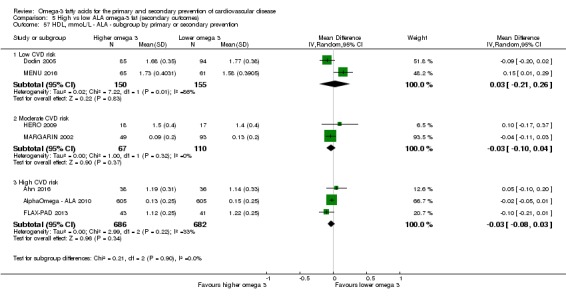
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 57 HDL, mmoL/L ‐ ALA ‐ subgroup by primary or secondary prevention.
LDL cholesterol
Low‐quality evidence suggests that ALA intake may make little or no difference to LDL cholesterol.
There was a small reduction of LDL cholesterol with ALA in 2201 participants of 7 trials (MD −0.05 mmol/L, 95% CI −0.15 to 0.04, I2 = 46%, Analysis 5.58), with similar effects in studies with good compliance and in larger trials (Analysis 5.61). While fixed‐effect analysis suggested marginal statistical significance of this reduction (P = 0.06, Analysis 5.59), there were no effects when we limited analyses to studies at low summary risk of bias (MD 0.02 mmol/L, 95% CI −0.05 to 0.10, I2 = 0%, Analysis 5.60). Subgrouping suggested no differences in effect by ALA dose or primary or secondary prevention (Analysis 5.62; Analysis 5.67), but shorter studies, those with unclear replacement and unclear statin use suggested reductions in LDL with ALA (Analysis 5.64; Analysis 5.65; Analysis 5.66). All studies provided supplemental foods (Analysis 5.63). GRADE assessment suggests low‐quality evidence that ALA intake may make little or no difference to LDL cholesterol (downgraded once each for risk of bias and imprecision).
Analysis 5.58.
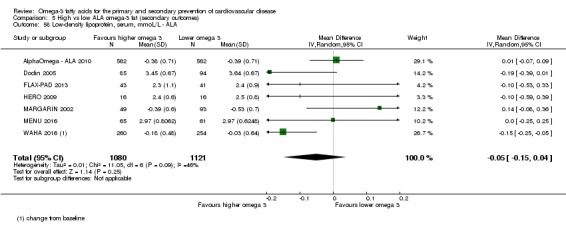
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 58 Low‐density lipoprotein, serum, mmoL/L ‐ ALA.
Analysis 5.61.
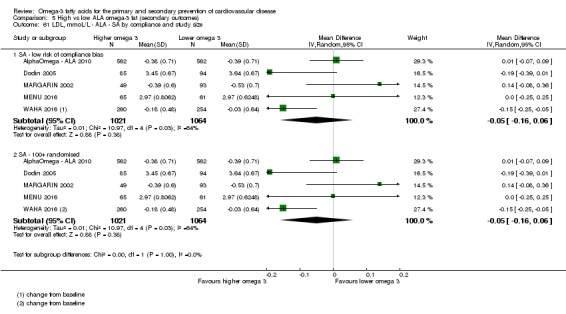
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 61 LDL, mmoL/L ‐ ALA ‐ SA by compliance and study size.
Analysis 5.59.
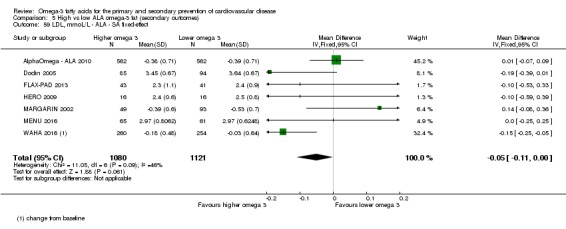
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 59 LDL, mmoL/L ‐ ALA ‐ SA fixed‐effect.
Analysis 5.60.
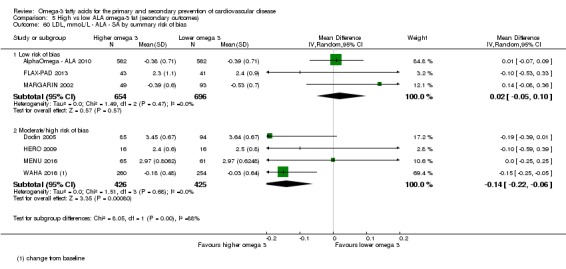
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 60 LDL, mmoL/L ‐ ALA ‐ SA by summary risk of bias.
Analysis 5.62.
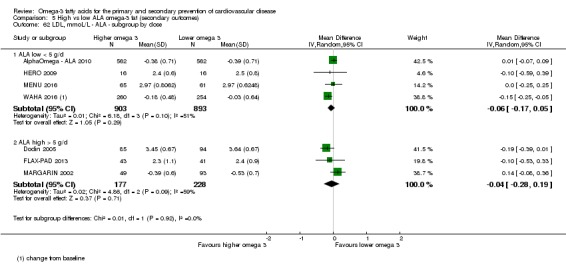
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 62 LDL, mmoL/L ‐ ALA ‐ subgroup by dose.
Analysis 5.67.
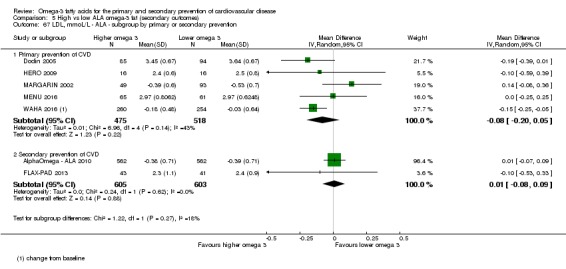
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 67 LDL, mmoL/L ‐ ALA ‐ subgroup by primary or secondary prevention.
Analysis 5.64.
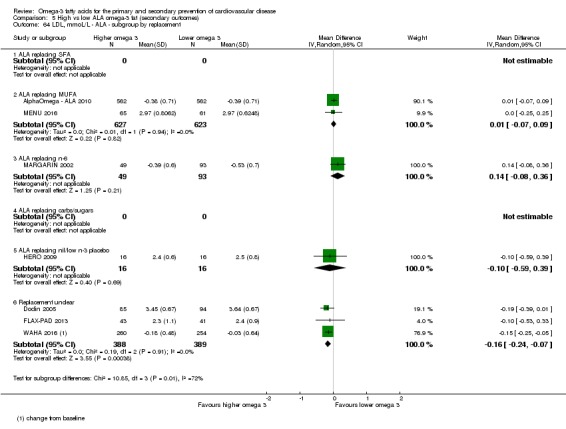
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 64 LDL, mmoL/L ‐ ALA ‐ subgroup by replacement.
Analysis 5.65.
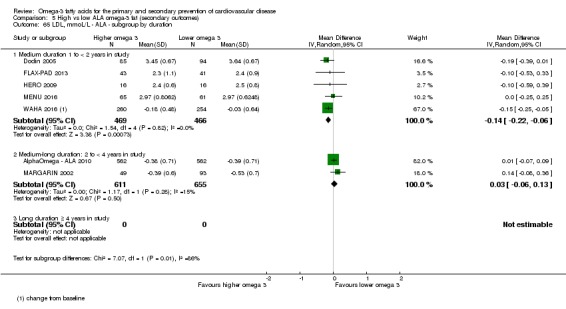
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 65 LDL, mmoL/L ‐ ALA ‐ subgroup by duration.
Analysis 5.66.
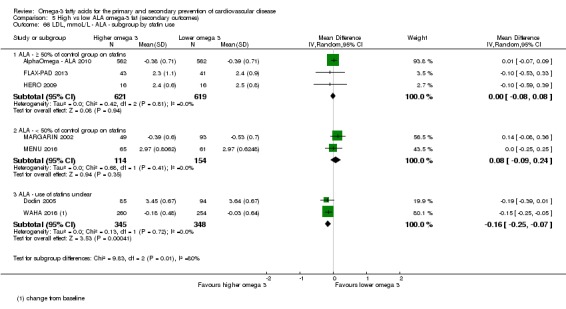
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 66 LDL, mmoL/L ‐ ALA ‐ subgroup by statin use.
Analysis 5.63.
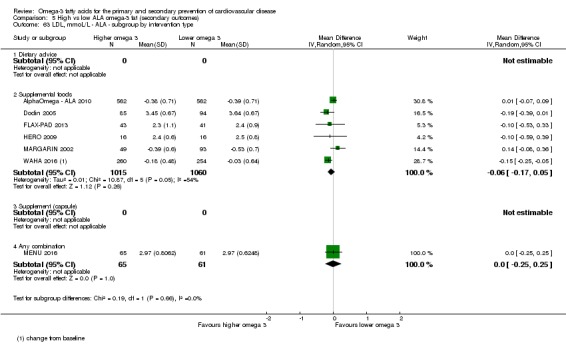
Comparison 5 High vs low ALA omega‐3 fat (secondary outcomes), Outcome 63 LDL, mmoL/L ‐ ALA ‐ subgroup by intervention type.
Tertiary outcomes
Effects of long‐chain omega‐3 fats (EPA, DHA and DPA) on tertiary health outcomes
We extracted these outcomes from studies that we included for other outcomes, so we did not assess them completely or systematically. We did not carry out sensitivity analyses or subgrouping for these outcomes. We are aware of missing data for some of these outcomes, including blood pressure in Ramirez‐Ramirez 2013.
Blood pressure (LCn3)
Fifteen included trials (> 34,000 participants) contributed data on effects of LCn3 fats on blood pressure. Meta‐analysis suggested little or no effect of LCn3 on systolic (MD 0.02 mmHg, 95% CI −0.32 to 0.35, I2 = 0%, Analysis 3.1) or diastolic (MD −0.02 mmHg, 95% CI −0.22 to 0.17, I2 = 0%, Analysis 3.1) blood pressure in trials of at least one year.
Analysis 3.1.
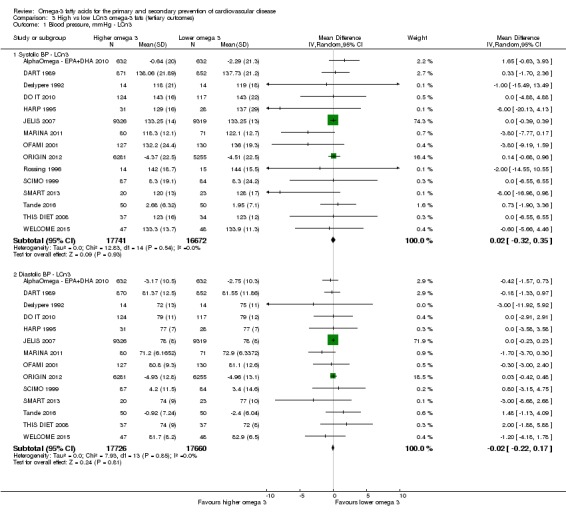
Comparison 3 High vs low LCn3 omega‐3 fats (tertiary outcomes), Outcome 1 Blood pressure, mmHg ‐ LCn3.
Serious adverse effects (LCn3)
As part of the larger set of reviews we formally systematically reviewed effects of omega‐3 fats on type 2 diabetes diagnoses, measures of glucose metabolism (Brown 2017), cancers including breast cancer (Hanson 2017b), neurocognitive outcomes such as dementia (Jimoh 2017), irritable bowel disease (IBD) and inflammatory factors (Thorpe 2017), depression and anxiety (Hanson 2017a), and functional outcomes (Abdelhamid 2017), so we do not present these outcomes here.
We did collect data on the following potentially important health outcomes (Analysis 3.2).
Analysis 3.2.
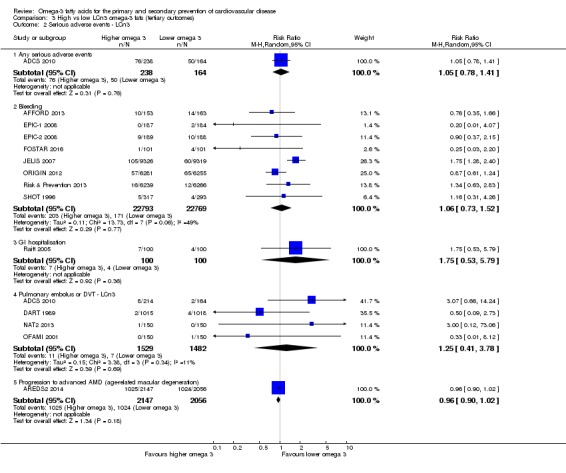
Comparison 3 High vs low LCn3 omega‐3 fats (tertiary outcomes), Outcome 2 Serious adverse events ‐ LCn3.
Any serious adverse event (RR 1.05, 95% CI 0.78 to 1.41, I2 NA, 126 events in > 400 participants in 1 trial).
Bleeding (RR 1.06, 95% CI 0.73 to 1.52, I2 = 49%, 374 events in > 45,000 participants in 8 trials).
Gastrointestinal hospitalisation (RR 1.75, 95% CI 0.53 to 5.79, I2 NA, 11 events in 200 participants in 1 trial).
Pulmonary embolus or DVT (RR 1.25, 95% CI 0.41 to 3.78, I2 = 11%, 18 events in > 3000 participants in 4 trials).
Progression to advanced age‐related macular degeneration (RR 0.96, 95% CI 0.90 to 1.02, I2 NA, 2049 events in > 4000 participants in 1 trial).
Thrombophlebitis: no data identified.
Urolithiasis: no data identified.
Side effects (non‐serious, LCn3)
To assess side effects we collected data on the following potential side effects (Analysis 3.3).
Analysis 3.3.
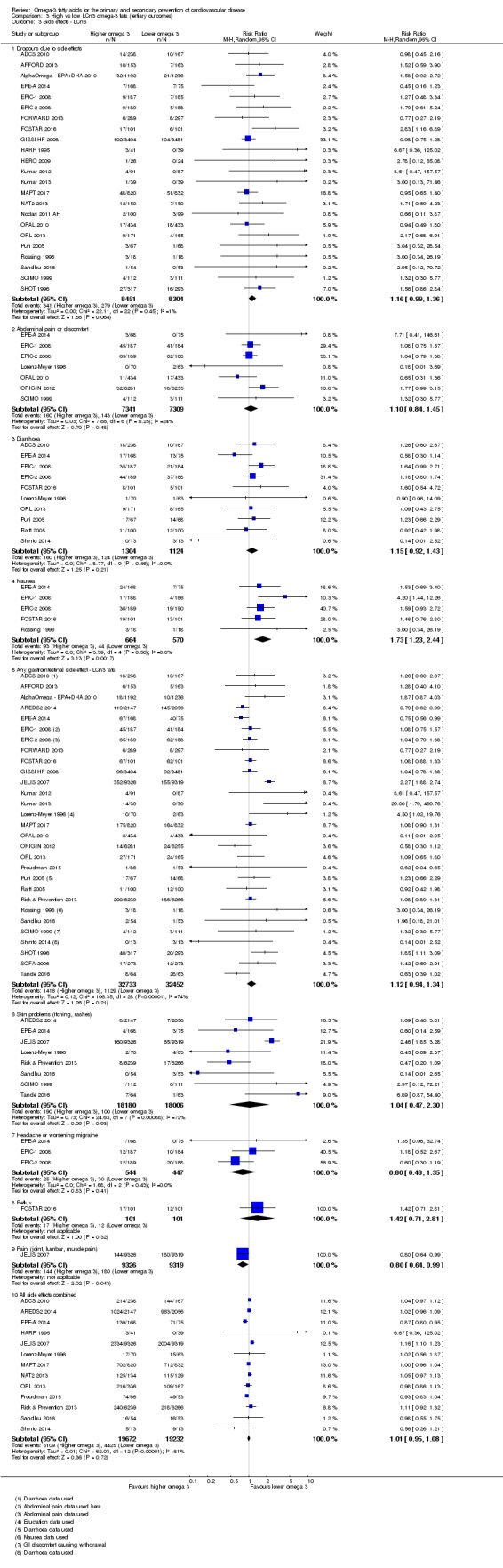
Comparison 3 High vs low LCn3 omega‐3 fats (tertiary outcomes), Outcome 3 Side effects ‐ LCn3.
Withdrawal: the data suggest more participants taking LCn3 fats dropped out because of side effects (RR 1.16, 95% CI 0.99 to 1.36, I2 = 1%, 620 dropouts in > 16,000 participants, 23 trials).
Increased abdominal pain or discomfort: data suggest an association with higher LCn3 (RR 1.10, 95% CI 0.84 to 1.45, I2 = 24%, 303 events in > 14,000 participants, 7 trials).
Diarrhoea: the data suggested an increased risk with increased LCn3 (RR 1.15, 95% CI 0.92 to 1.43, I2 = 0%, 284 events in > 2000 participants, 10 trials).
Nausea: risk increased with LCn3 (RR 1.76, 95% CI 1.25 to 2.48, I2 = 0%, 140 events in > 1000 participants, 6 trials).
Any gastrointestinal side effect: risk also appeared to increase with LCn3, albeit with very high heterogeneity (RR 1.12, 95% CI 0.94 to 1.34, I2 = 74%, 2545 events in > 65,000 participants, 29 trials).
Skin problems, including itching or rashes: these were not affected by LCn3 in a meta‐analysis with high heterogeneity (RR 1.04, 95% CI 0.47 to 2.30, I2 = 72%, 290 events in > 36,000 participants, 8 trials).
Headache or worsening migraine: there were limited data on this outcome (RR 0.81, 95% CI 0.48 to 1.36, I2 = 0%, 55 events in 996 participants, 3 trials).
Reflux: there were limited data (RR 1.42, 95% CI 0.71 to 2.81, I2 NA, 29 events in 202 participants, 1 trial).
Joint lumbar and muscle pain: one study provided data suggesting that LCn3 reduced the risk of such pain (RR 0.80, 95% CI 0.64 to 0.99, 324 out of > 18,000 participants experiencing pain).
All adverse effects: there was no suggestion that LCn3 increased or decreased all side effects combined in a meta‐analysis with very high heterogeneity (RR 1.01, 95% CI 0.95 to 1.08, I2 = 81%, 9534 people with at least one side effect in > 38,000 participants, 13 trials).
Dropouts (LCn3)
Included studies reported 5515 dropouts over > 31,000 participants in 30 trials, suggesting no difference in dropout rates between intervention and control arms (RR 1.02, 95% CI 0.95 to 1.09, I2 = 11%, Analysis 3.4).
Analysis 3.4.
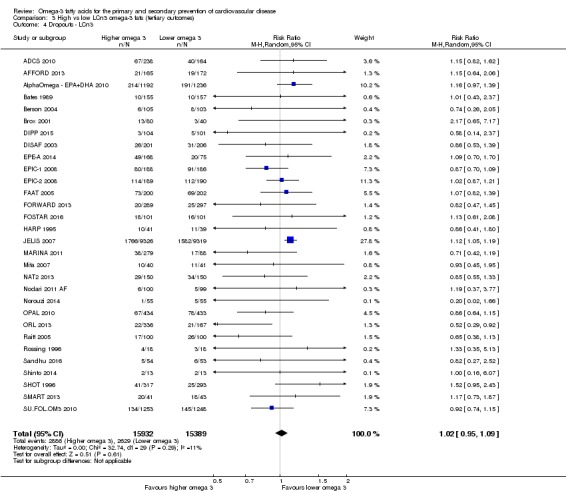
Comparison 3 High vs low LCn3 omega‐3 fats (tertiary outcomes), Outcome 4 Dropouts ‐ LCn3.
Quality of life, economic costs (LCn3)
We found no data on quality of life outcomes or economic costs.
Effects of ALA on tertiary health outcomes
We extracted these outcomes from studies that we included for other outcomes, so we did not assess them completely or systematically. We did not carry out sensitivity analyses or subgrouping for these outcomes.
Blood pressure (ALA)
Four included trials (1671 participants) contributed data on effects of ALA on blood pressure. Meta‐analysis suggested little or no effect of ALA on systolic (MD −0.87 mmHg, 95% CI −4.48 to 2.75, I2 = 58%, Analysis 6.1) or diastolic (MD −1.42 mmHg, 95% CI −4.40 to 1.57, I2 = 74%, Analysis 6.1) blood pressure in trials of at least one year. The heterogeneity in these results reflect a single trial, FLAX‐PAD 2013, that showed large diastolic and systolic blood pressure effects. The other (larger) trials did not suggest such effects.
Analysis 6.1.
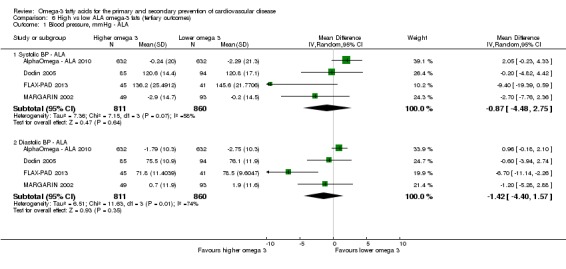
Comparison 6 High vs low ALA omega‐3 fats (tertiary outcomes), Outcome 1 Blood pressure, mmHg ‐ ALA.
Serious adverse effects (ALA)
As part of the larger set of reviews we formally systematically reviewed effects of omega‐3 fats on type 2 diabetes diagnoses and measures of glucose metabolism (Brown 2017), cancers including breast cancer (Hanson 2017b), neurocognitive outcomes such as dementia (Jimoh 2017), irritable bowel disease (IBD) and inflammatory factors (Thorpe 2017), depression and anxiety (Hanson 2017a), and functional outcomes (Abdelhamid 2017), so we do not present these outcomes here.
We did collect data on the following potentially important health outcomes (Analysis 6.2).
Analysis 6.2.
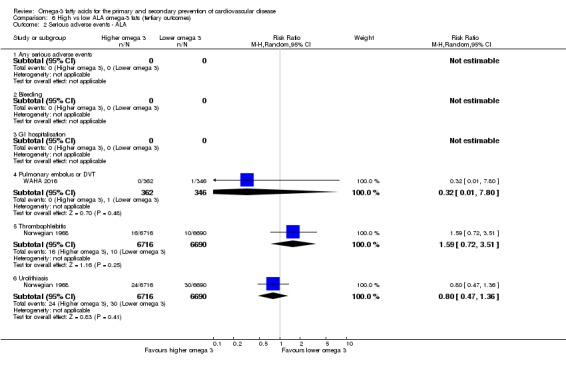
Comparison 6 High vs low ALA omega‐3 fats (tertiary outcomes), Outcome 2 Serious adverse events ‐ ALA.
Any serious adverse event: no data identified.
Bleeding: no data identified.
Gastrointestinal hospitalisation: no data identified.
Pulmonary embolus or DVT: only one event was identified in a single study, so there were insufficient data to assess effects
Progression to advanced age‐related macular degeneration: no data identified.
Thrombophlebitis: there were insufficient data to assess effects (RR 1.59, 95% CI 0.72 to 3.51, I2 NA, 26 events, > 13,000 participants, 1 trial).
Urolithiasis: there were insufficient data to assess effects (RR 0.80, 95% CI 0.47 to 1.36, I2 NA, 54 events, > 13,000 participants, 1 trial).
Side effects (non‐serious, ALA)
To assess potential side effects, we collected data on the following (Analysis 6.3).
Analysis 6.3.
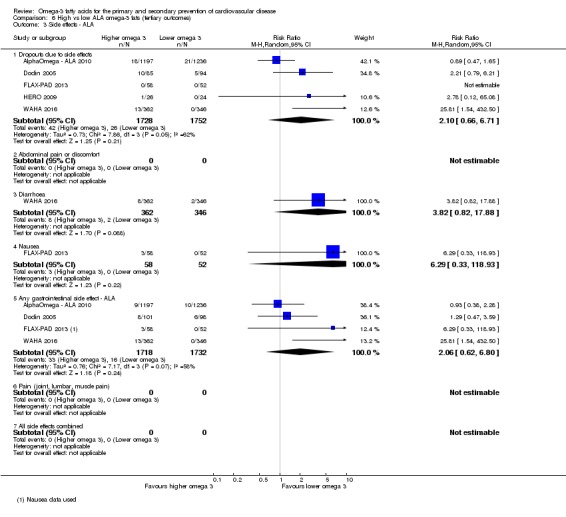
Comparison 6 High vs low ALA omega‐3 fats (tertiary outcomes), Outcome 3 Side effects ‐ ALA.
Dropouts due to side effects: data suggested that ALA increased the risk of withdrawal, although there was high heterogeneity (RR 2.10, 95% CI 0.66 to 6.71, I2 = 62%, 68 events, > 3000 participants, 5 trials).
Abdominal pain or discomfort: no data identified.
Diarrhoea: a single study identified 10 participants with diarrhoea, suggesting a higher risk of diarrhoea with greater ALA intake (RR 3.82, 95% CI 0.82 to 17.88).
Nausea: there were insufficient data to assess effects of ALA (RR 6.29, 95% CI 0.33 to 118.93, I2 NA, 3 events, 110 participants, 1 trial).
Any gastrointestinal side effect: there were insufficient data to assess effects of ALA (RR 1.79, 95% CI 0.48 to 6.69, I2 = 69%, 46 events, > 3000 participants, 3 trials). The very high heterogeneity suggests that gastrointestinal side effects may be collected in different ways in different trials.
Skin problems, including itching or rashes: no data identified.
Headache or worsening migraine: no data identified.
Reflux: no data identified.
All side effects combined: no data identified.
Dropouts (ALA)
Included studies reported 558 dropouts over > 3000 participants in 6 trials, suggesting slightly higher dropout rates in participants taking higher ALA (RR 1.08, 95% CI 0.92 to 1.25, I2 = 0%, Analysis 6.4).
Analysis 6.4.
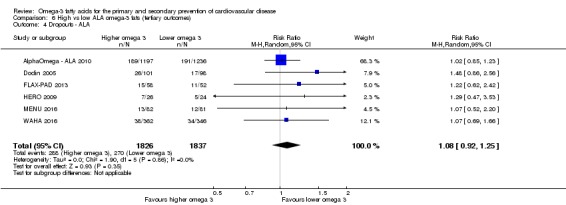
Comparison 6 High vs low ALA omega‐3 fats (tertiary outcomes), Outcome 4 Dropouts ‐ ALA.
Quality of life, economic costs (ALA)
We found no data on quality of life outcomes or economic costs.
Discussion
Summary of main results
We included 79 randomised controlled trials (112,059 participants), of which 25 were at low summary risk of bias (randomisation, allocation concealment, selection and detection bias all at low risk for supplementation trials; randomisation, allocation concealment and detection bias all at low risk for dietary advice trials). Trials of 12 to 72 months' duration included adults at varying levels of cardiovascular risk, mainly in high‐income countries. Most studies assessed LCn3 supplementation with capsules, but some used LCn3‐ or ALA‐rich or enriched foods or dietary advice compared to placebo or usual diet.
Pooled trial results suggested there is probably little or no effect of increasing long‐chain omega‐3 fats on risk of our primary outcomes: all‐cause mortality, cardiovascular deaths, cardiovascular events, coronary heart disease deaths, coronary heart disease events, stroke or arrhythmias (moderate and high‐quality evidence). For all of these outcomes except arrhythmia, limiting LCn3 analyses to trials at low summary risk of bias moved the effect size towards 1.0 (the null value) whether initial analyses suggested a protective effect (for example, for CHD mortality, whose effect size moved from RR 0.93 to RR 1.00) or a harmful effect (for example, stroke, whose effect size moved from RR 1.06 to RR 0.98). We found no suggestion of dose response (in subgrouping or meta‐regression), or important effects regardless of sensitivity analysis, subgrouping or meta‐regression. These results apply to supplemental LCn3 intake. We did not see important differences in LCn3 trials between those providing oily fish (dietary source) or EPA/DHA capsules (supplemental source), but as few trials provided whole fish health effects may differ.
On the other hand we found moderate‐quality evidence that increasing ALA probably reduces risk of CHD mortality a very small amount (from 1.1% to 1.0%) and arrhythmia (from 3.3% to 2.6%), and low‐quality evidence that increasing ALA may reduce risk of CVD events a little (from 4.8% to 4.7%). However, there is probably little or no effect on all‐cause or cardiovascular mortality or coronary heart disease events (low and moderate‐quality evidence), and effects on stroke are unclear. For ALA, limiting analyses to studies at low summary risk of bias tended to reduce the RR, or increase the suggested protection. Data were more limited than for LCn3, and there were too few studies for informative funnel plots or subgroup analyses. These suggested benefits of ALA need to be considered with caution, as effects were small, and few trials (though often at low summary risk of bias) addressed the outcomes.
Meta‐analyses suggested little or no effect of long‐chain omega‐3 fats or ALA intake on secondary outcomes: major adverse cerebrovascular or cardiovascular events, fatal and/or non‐fatal myocardial infarction, sudden cardiac death, new or worsening angina, heart failure, revascularisation, peripheral arterial disease or acute coronary syndrome.
There was no evidence for effects of LCn3 or ALA on measures of adiposity, but LCn3 did reduce serum triglycerides and increase HDL cholesterol a little. We did not see these effects in trials of ALA, and no omega‐3 fats altered total or LDL cholesterol in these long‐term trials. Within the included studies we assessed effects on blood pressure, serious adverse effects, side effects and dropouts. There was no suggestion that blood pressure or risk of adverse events such as bleeding differed by LCn3 or ALA intake. Thus, proposed mechanisms for omega‐3 activity, including lowering of blood pressure, reduced thrombotic tendency and anti‐arrhythmic effects are not apparent in adult humans, but LCn3 does lower serum triglyceride levels.
The review has provided some answers for its secondary questions.
-
If omega‐3 fatty acids confer protection:
does protection occur equally in those at low and at high risk of cardiovascular disease? There is no evidence of differential effects on mortality or cardiovascular health by primary or secondary CVD prevention.
does protection depend on the dose of omega‐3 fats taken per day? We ran subgroup analyses for primary and key outcomes and meta‐regression for primary outcomes but found no evidence of differential effects by LCn3 or ALA dose on any outcomes except LCn3 on serum triglycerides, where there was a statistically significant difference between different dose subgroups and greater effects with higher dose.
do effects differ between dietary and supplemental omega‐3 sources? We assessed this question by looking for statistically significant differences between subgroups but found no evidence of differential effects by dietary or supplemental LCn3 or ALA sources. However, few of the LCn3 trials advised or gave fish, most gave supplemental fish oils, so our ability to assess effects of eating more oily whole fish are limited.
does protection depend on study summary risk of bias? Some analyses suggested a protective effect of LCn3 fats, but these effects disappeared when analyses were limited to studies at low summary risk of bias. The stronger studies with higher internal validity suggested few or no effects of LCn3 on mortality or CVD outcomes. On the other hand, for most primary cardiovascular outcomes, ALA trials at low summary risk of bias suggested greater protection with higher ALA than in the main analysis (including trials of all levels of summary risk of bias).
Is protection or harm stronger with longer trial duration? In subgroup analyses for primary and key outcomes and in meta‐regression for primary outcomes, there was no evidence that longer trials increased the effect of LCn3 or ALA.
Overall completeness and applicability of evidence
We searched very carefully to find all studies relevant to this review and located 79 trials randomising 112,059 participants to higher and lower omega‐3 fats (LCn3 or ALA) for at least 12 months.
To reduce selection bias, we contacted authors of trials that appeared to have randomised appropriate participants to appropriate intervention and comparator but may not have published relevant outcomes. If trialists had assessed any of our outcomes, we requested data and included the study. This enabled us to include several additional trials. We also contacted authors of all included trials that randomised at least 100 participants (and most smaller trials) to request data on any further outcomes (as well as on methodological issues) that may have been recorded but not reported. We tried to contact 72 of the 79 included studies (all except Baldassarre 2006; HERO 2009; Mita 2007; Nutristroke 2009; Özaydin 2011; Shinto 2014; Sofi 2010). This allowed us to collect useful additional data on outcomes such as deaths and cardiovascular events that we would not have had access to otherwise.
We identified 27 trials that appeared to be unpublished at the time of writing (Characteristics of ongoing studies). We have labelled these trials as ongoing, although some appear overdue for publication, and their status is unclear – they may constitute missing data. We tried to contact authors of all 'overdue' ongoing studies, and some stated that publications are forthcoming; others did not reply. We suspect that if trialists have not published outcomes, it is likely that any protective health effects did not reach statistical significance. Given that existing studies suggest no effects of omega‐3 fats on cardiovascular health outcomes, any missing data may not affect outcomes greatly; however, for completeness we would prefer to include all available data.
Post hoc, we followed advice to assess differences in effects between EPA and DHA within the review. However, most LCn3 trials provided or advised changes resulting in increased intakes of both EPA and DHA (as in natural fish oil), though in different ratios. Only three trials provided data on DHA only (ADCS 2010; Berson 2004; Zhang 2017), and five provided data on EPA only (Doi 2014; JELIS 2007; Mita 2007; Nye 1990; Puri 2005). Unfortunately for any single outcome only two or three of these trials were represented, so our ability to assess differential effects of the DHA‐only and EPA‐only interventions was very limited, and we have not presented these analyses or attempted to draw any information from them.
Quality of the evidence
Figure 2 displays risk of bias of included studies. Of the 79 RCTs, 25 were at low summary risk of bias (at low risk of selection bias, performance bias and detection bias, plus low risk of performance bias in supplemental trials). We assessed the validity of evidence in meta‐analyses by running sensitivity analyses that removed trials not at low summary risk of bias. When sensitivity analyses removed LCn3 trials at moderate to high summary risk of bias, effect sizes moved closer to no effect (RR 1.0) for all primary outcomes except arrhythmias, where the RR rose to 1.10. Funnel plots for LCn3 trials suggested that there may be missing studies for all primary outcomes except stroke and arrhythmia, and in all cases adding such studies back in would move effect sizes closer to no effect (RR 1.0). This lack of effect in the studies at lowest risk of bias (with suggestions of effect in studies at moderate to high risk of bias) was an important finding from this review and supported our interpretation of lack of effect of long‐chain omega‐3 fats on our primary outcomes.
As there were fewer ALA trials, funnel plots were not useful, but sensitivity analyses retaining only trials at low summary risk of bias were more variable, often suggesting lower risk of a cardiovascular outcome.
Potential biases in the review process
Potential adverse effects include cancers and neurological problems associated with polychlorinated biphenyls (PCBs) or mercury in fish oils, and bleeds associated with reductions in clotting (see How the intervention might work). Any data on bleeds, including haemorrhagic stroke, have been collated in this review, though we did not ask authors specifically for additional data on these outcomes. Unfortunately there were insufficient data on serious harms (bleeding and pulmonary embolism or deep vein thrombosis) to assess these potential harms. We have not collated data on cancers and neurological problems within this review but have formally systematically reviewed them elsewhere (Hanson 2017b; Jimoh 2017). This approach is preferable to including data on these outcomes from within included studies, which would be incomplete and potentially underpowered to show important effects.
One problem with CVD outcomes is that they are collected together in a variety of ways, depending on the study. For example, in assessing CHD mortality, we pre‐specified that we would include the first of the following list reported in any trial: coronary death, ischaemic heart disease death, fatal myocardial infarction, cardiac death. Each included trial includes outcome data in its own way, so we had to adapt to this in our analysis. One way to get around this problem would be to use individual patient data, as in one recent meta‐analysis that included fewer trials than this review but was able to formulate their outcome data to match precisely between trials (Aung 2018). The next section discusses similarities and differences between this review and Aung 2018, but their findings were highly similar. For CHD mortality, our meta‐analytic estimate of effect of LCn3 was RR 0.93, (95% CI 0.79 to 1.09, I2 = 35%) in 21 trials reporting 1596 CHD deaths, while theirs was RR 0.93 (95% CI 0.83 to 1.03) in 10 trials reporting 2695 CHD deaths.
While we tried hard to locate all available trials and collect additional outcome data where possible, there was evidence from funnel plots of some small study bias. Some smaller studies showing increased risk of CVD outcomes with omega‐3 fats may be missing from some of the meta‐analyses. If these studies were replaced they would tend to increase risk ratios. This suggests that there is some underlying small study bias within the review.
Given that the many LCn3 studies at moderate to high risk of bias appear to be inflating any protective effects, and that small study bias is also inflating any protective effects, it is justified to view with skepticism the occasional suggestion of a protective effect. Given the very large number of subgroup analyses we carried out, it is also important to treat the occasional subgroup analysis that throws up a statistically significant difference between subgroups very cautiously.
A secondary question asked by this review was about differential effects of dietary and supplemental LCn3 fats. LCn3 interventions included dietary advice (advice to eat more oily fish), supplemental foods (LCn3 fats incorporated into other foods such as margarine) and supplements or capsules (by far the greatest proportion of studies). Dietary fish is likely to have different health effects, as it may take the place of less healthy foods in the diet (leading to reduced saturated fat intake, for example) and provides many nutrients in addition to omega‐3 fats (such as protein, selenium, iodine, calcium, magnesium, etc.). There were only four LCn3 dietary advice trials with event data (DART 1989; DART2 2003; DISAF 2003; THIS DIET 2008), and two of these also provided fish oil capsules when participants did not want to eat more fish (DART 1989; DART2 2003). We found no statistically significant differences between dietary advice subgroups and supplemental foods or capsule subgroups for primary outcomes. This may mean that health effects between the two types of intervention are not different, but It is likely that our analysis was underpowered to see any such differences if they exist.
Population LCn3 status varies widely across the world, from over 8% of fatty acids in Japan, Scandinavia and other areas with non‐Westernised dietary patterns to less than 4% in North, South and Central America; Europe; the Middle East; Southeast Asia; and Africa (Stark 2016). We hypothesised that additional LCn3 might have greater health effects in people whose usual LCn3 intake was relatively low, but unfortunately we were not able to ascertain baseline LCn3 intake or status for most of our included trials. However, most of the included studies were carried out in areas of the world with lower LCn3 status, so we would expect to see effects of increasing LCn3 in most included trials if such effects exist – the fact that we did not see them suggests that any such effects may not be important in the populations included in this review.
Agreements and disagreements with other studies or reviews
One potential difference between the findings of this review and some other trials and reviews is our running sensitivity analyses assessing effects exclusively in studies at low summary risk of bias. This clarified the lack of effect of LCn3 fats on CHD mortality, CHD events and heart failure, which otherwise appeared slightly protective, and on stroke, which otherwise appeared slightly harmful. On the other hand, these sensitivity analyses suggested some protective effects for ALA (on CVD events, CHD mortality, CHD events and arrhythmia), though these were small and evidence limited.
The effect of LCn3 on arrhythmias was unclear. There was a suggestion that LCn3 was harmful regarding development of new arrhythmia (where trials were not set up with arrhythmia as a primary outcome), but protective of recurrent arrhythmia. However, trials at low summary risk of bias suggested harm, and other trials (at moderate to high risk of bias) suggested benefit. Eight of the 10 included studies at low summary risk of bias were trials assessing new arrhythmia. It is possible that the apparent difference between effects on new and recurrent arrhythmia are related to summary risk of bias.
There was no suggestion that blood pressure or risk of adverse events such as bleeding differed by LCn3 or ALA intake. This suggests that possible mechanisms for omega‐3 activity, including lowering of blood pressure, reduced thrombotic tendency and anti‐arrhythmic effects are not important in most adult humans, though LCn3 does appear to lower serum triglyceride levels. We did not systematically review blood pressure data so may have missed a few long‐term studies (though not many) – missing data from included studies is likely to be a bigger issues. Of the 15 included trials that reported blood pressure outcomes, nine reported numbers of hypertensive participants at baseline, ranging from 5% in MARINA 2011 to 79% of participants in ORIGIN 2012. Effects did not differ by proportions of hypertensive participants (I2 was 0% for both systolic and diastolic blood pressure, Analysis 3.1).
Nearly 20 years ago, the GISSI‐P 1999 trial suggested that LCn3 had its primary effects in reducing sudden cardiac death. However, the forest plot clearly shows that subsequent trials have not seen this effect individually or in aggregate (Analysis 2.6).
The scope of this review is similar to that of the extensive Agency for Healthcare Research and Quality review (Balk 2016), so we have compared our results with theirs. Given that our review included 79 RCTs randomising more than 112,000 participants, who experienced over 8000 deaths and upwards of 4000 CVD deaths, we were surprised to read that Balk and colleagues characterised the body of evidence as having "limited data ... from RCTs on the effect of n‐3 FA on clinical CVD outcomes" (Balk 2016). This appears to be because the Balk review excluded RCTs of people with non‐CVD and non‐diabetes related diseases at baseline, while we included them. While Balk 2016 excluded some studies we included, it did not include any studies providing all‐cause mortality data that we excluded. This meant that in analysing effects on all‐cause mortality, Balk 2016 included 18 RCTs randomising 81,027 participants experiencing 8480 deaths, while we included 112,059 participants randomised to high or low LCn3 or ALA experiencing 8648 deaths. Balk 2016 excluded studies that we included, such as AREDS2 2014, a high‐quality trial with 368 deaths in more than 4000 participants with age‐related macular degeneration. This sort of population appeared ideal to us for assessment of omega‐3 fats on primary prevention of CVD, as these people tend to be elderly but there is no clear reason why omega‐3 fats would affect CVD differently in this population than in other older adults at usual CVD risk.
Despite these slight differences in approach, we obtained very similar effect estimates to Balk 2016. We meta‐analysed effects of LCn3 and ALA trials, finding an RR for all‐cause mortality of 0.98 (95% CI 0.93 to 1.03, I2 = 6%), compared to a pooled RR for all‐cause mortality of 0.97 (95% CI 0.92 to 1.03) in Balk 2016. While that review seldom pooled their results, we can compare our results with theirs where they did. Despite our slightly different inclusion criteria, our results are very comparable (Table 17).
Table 8.
Comparison of the results of this review with Balk 2016 and Aung 2018a
| Balk 2016 | Aung 2018 | This review | ||||
| Number of people experiencing events | RR (95% CI) | Number of people experiencing events | RR (95% CI) | No of people experiencing events | RR (95% CI) | |
| All‐cause mortality | 8480 | 0.97 (0.92 to 1.03) | — | Not assessed | 8647 | 0.98 (0.93 to 1.03) |
| Cardiovascular deaths | 3799 | 0.92 (0.82 to 1.02) | — | Not assessed | 4763 | 0.95 (0.87 to 1.03) |
| CVD events (MACCEs in Balk 2016) | 8085 | 0.96 (0.91 to 1.02) | 12001 | 0.97 (0.93 to 1.01) | 15614 | 0.99 (0.94 to 1.04) |
| CHD deaths | — | Not pooled | 2695 | 0.93, (0.83 to 1.03) | 1791 | 0.93 (0.79 to 1.09) |
| CHD events | — | Not assessed | 6273 | 0.96, (0.90 to 1.01) | 5865 | 0.93 (0.88 to 0.97) |
| Stroke | 1467 | 0.98 (0.88 to 1.09) | 1713 | 1.03 (0.93 to 1.13) | 1871 | 1.06 (0.96, 1.16) |
| Arrhythmia | — | Not pooled | — | Not assessed | 3788 | 0.97 (0.90 to 1.05) |
CHD: coronary heart disease; CI: confidence interval; CVD: cardiovascular disease; MACCE: major adverse cerebrovascular or cardiovascular event; RR: risk ratio.
aMeta‐analysis of effects of LCn3 in Balk 2016 and Aung 2018 systematic reviews, comparing their findings with our findings for our primary outcomes.
A recent individual meta‐analysis of 10 large trials in almost 78,000 people at high risk of CVD found no associations of LCn3 with CHD mortality (RR 0.93, 99% CI 0.83 to 1.03), nonfatal MI (RR 0.97, 99% CI 0.87 to 1.08), CHD events (RR 0.96, 95% CI 0.90 to 1.01) or major vascular events (RR 0.97, 95% CI 0.93 to 1.01, Aung 2018). Aung 2018 included individual patient data from the participants of large, long trials (randomising at least 500 participants and following them for at least one year) (AlphaOmega ‐ EPA+DHA 2010; AREDS2 2014; DO IT 2010; GISSI‐HF 2008; GISSI‐P 1999; JELIS 2007; OMEGA 2009; ORIGIN 2012; Risk & Prevention 2013; SU.FOL.OM3 2010), and this review includes all their trials. Their review had the advantage of being able to ensure that they had complete and equivalent data for all of their key outcomes from all the trials, reducing the risk of publication bias, but the disadvantage of missing all the data from many large LCn3 trials such as DART2 2003,DART 1989,FORWARD 2013,MAPT 2017,SHOT 1996 and SOFA 2006 (all LCn3 trials randomising at least 500 participants). It also missed large trials of LCn3 in lower risk participants such as OPAL 2010, and large trials of ALA such as MARGARIN 2002, Norwegian 1968 and WAHA 2016, as well as all the smaller trials. However, though taking different approaches, the results of this review and Aung 2018 are also very similar (Table 17). LCn3 has little or no effect on major cardiovascular outcomes. This review, Balk 2016 and Aung 2018 addressed the analysis of the data in slightly different ways, creating sensitivity analyses for each other. The fact that they came to the same conclusions reassures us that our conclusions are solidly based.
Our results, suggesting high‐quality evidence of no clinically useful cardiovascular health effects of either LCn3 or ALA, are consistent with many further high‐quality recent systematic reviews (Campbell 2013; Chowdhury 2012; Enns 2014; He 2013; Khoueiry 2013; Kotwal 2012; Kwak 2012; Mariani 2013; Rizos 2012; Zheng 2014), and they confirm and expand on the findings of earlier versions of this review (Hooper 2004; Hooper 2006).
Authors' conclusions
We found high‐quality evidence that long‐chain omega‐3 fats do not have important positive or negative effects on mortality or CVD events and moderate‐quality evidence that they have little or no effect on other measures of cardiovascular health in primary or secondary prevention. Most evidence on long‐chain omega‐3 fats came from trials of capsules of fish oil or EPA/DHA mixtures. While we did not see important differences between trials of supplemental capsules and trials of oily fish, there were few trials of oily fish.
We found moderate‐quality evidence that increasing ALA probably slightly reduces risk of CHD mortality and arrhythmia, and may slightly reduce risk of CVD events. However, there is probably little or no effect on all‐cause or cardiovascular mortality or coronary heart disease events (low and moderate‐quality evidence). Effects of ALA were very small ‐ 143 people would need to increase their ALA intake to prevent one person developing arrhythmia, and 1000 would need to take more ALA to prevent one person experiencing a CVD event or dying from CHD. Trials of ALA gave ALA‐rich or enriched foods such as walnuts or enriched margarine.
Supplemental long‐chain omega‐3 fats are probably not useful for preventing or treating cardiovascular disease, although long‐chain omega‐3 fats can help to reduce serum triglycerides and raise HDL a little. Fish and seafood are nutrient‐dense and rich in a variety of other nutrients (such as vitamin D, calcium, iodine, selenium) so are useful foods even without cardiovascular benefits. In light of the evidence in this review it would be appropriate to review official recommendations supporting supplemental LCn3 fatty acid intake.
ALA is an essential fatty acid, an important part of a mixed diet, and increasing intakes may be very slightly beneficial for prevention or treatment of cardiovascular disease.
There are several large ongoing trials of supplemental long‐chain omega‐3 fats (see Characteristics of ongoing studies). We suggest that given the lack of convincing effects suggested for omega‐3 fats in the large number of trials to date, no further trials should be initiated until the ongoing trials have reported. Further large and high‐quality trials of ALA carried out in lower and higher income countries and that assess baseline ALA intake and use biomarkers to assess compliance would be helpful to clarify the cardiovascular effects of ALA. Similarly trials of dietary fish would be helpful.
Feedback
Interpretation of effect estimates, 18 July 2018
Summary
I am not clear how the quoted RRs and CIs in the abstract support statements of no effect in one part but statements of effect in another part. It seems that throughout the CIs comprehensively span unity. For example, how is a statement of 'probably reduces risk of CHD mortality' supported by the metrics '(1.1% to 1.0%, RR 0.95, 95% CI 0.72 to 1.26, 18,353 participants; 193 CHD deaths, 3 RCTs'? That seems like an entirely null result.
Contributors
Feedback submitted by: Bruce Neal
Dosing and conclusions, 19 July 2018
Summary
Most of the CVD OR ranges listed for lcN3 data showed zones of significant OR benefit. No dosing information was included. I question the study's "conclusions", and believe that a more sensitive analysis of the data could easily show benefit in terms of CVD risk reduction.
Reply
Feedback submitted by: TR Morris
Acknowledgements
The wider set of reviews, including this one, were carried out by the Polyunsaturated Fats and Health (PUFAH) group. PUFAH includes Asmaa Abdelhamid, Zoya Ahmed, Sarah MA Ajabnoor, Fai K AlAbdulghafoor, Lena Al‐Khudairy, Priti Biswas, Julii Suzanne Brainard, Charlene Bridges, Tracey J Brown, Katherine HO Deane, Daisy H Donaldson, Sarah Hanson, Lee Hooper, Oluseyi F Jimoh, Nicole Martin, Katie Maas, Helen J Moore, Alex T O’Brien, Karen Rees, Ruksana Sivakaran, Fujian Song, Carolyn D Summerbell,, Gabrielle C Thorpe, Xia Wang , Ailsa Welch, Lauren Winstanley, and Helen V Worthington.
The review authors thank all of the authors of primary studies who kindly provided us with the best set of data available, including: D Kromhout, Wageningen University (AlphaOmega ‐ ALA 2010; AlphaOmega ‐ EPA+DHA 2010); Emily Chew, NIH (AREDS2 2014); J Brox, University Hospital of North Norway (Brox 2001); C Argo, University of Virginia (Caldwell 2011); ML Burr, University of Wales and A Ness, University of Bristol (DART 1989; DART2 2003); G Derosa and P Maffioli, University of Pavia (Derosa 2016); PNM Demacker, University Hospital Nijmegen (Deslypere 1992); S Tokudome, National Institue of Health and Nutrition, Japan (DIPP 2015); R Harrison, University of Manchester, UK (DISAF 2003); G Einvik, Akershus University Hospital and H Arnesen, Oslo University Hospital (DO IT 2010); S Dodin, Universite Laval (Dodin 2005); D Schoenfeld, Harvard Medical School (FAAT 2005); A Macchia, Fundacio'n GESICA (FORWARD 2013); C Hill, the Queen Elizabeth Hospital (FOSTAR 2016); D Franzen, Universitat zu Koln (Franzen 1993); P Bauer, Medical University of Vienna (Lorenz‐Meyer 1996); WJ Bemelmans, National Institute for Public Health and the Environment, Bilthoven (MARGARIN 2002); T Sanders, King's College, London (MARINA 2011); E Souied, Hôpital intercommunal de Créteil, France (NAT2 2013); D Nilsen, University of Bergen, Norway (OFAMI 2001); S Schneider, Institut für Herzinfarktforschung, Germany (OMEGA 2009); A Dangour, London School of Hygiene & Tropical Medicine (OPAL 2010); M James, Royal Adelaide Hospital, Australia (Proudman 2015); R Zurier, University of Massachusetts Medical School (Reed 2014); C Roncaglioni and I Marzona, IRCCS‐Istituto di Ricerche Farmacologiche Mario Negri, Italy (Risk & Prevention 2013); A Manni, Penn State College of Medicine, USA (Sandhu 2016); C von Schacky, Ludwig Maximilians University, Munich, Germany (SCIMO 1999); L Tapsell, M Batterham and E Neale, University of Wollongong, Australia (SMART 2013); P Galan, Université Paris (SU.FOL.OM3 2010); K Tande, Calanus AS, Norway (Tande 2016); K Tuttle, Sacred Heart Medical Center, Spokane (THIS DIET 2008); J Sabaté, Loma Linda University, California (WAHA 2016); E Scorletti, University of Southampton, UK (WELCOME 2015).
Thanks also to the authors who replied but were not able to provide further details or confirmed no relevant outcomes, including: S Jebb, University of Oxford (FISH 2012); R Holman, University of Oxford (AFORRD 2010); J Quinn, Oregon Health & Science University (ADCS 2010); D Bates, Royal Victoria Infirmary, Newcastle on Tyne and R Dworkin, University of Rochester, UK (Bates 1989); E Berson, Harvard Medical School, USA (Berson 2004); A Sanyal, Virginia Commonwealth University, USA (EPE‐A 2014); G Pierce, St. Boniface Hospital Research Centre, Canada (FLAX‐PAD 2013); H Gerstein, McMaster University, Canada (ORIGIN 2012); B Puri, Imperial College London (Puri 2005); M Raitt, Oregon Health & Science University, USA (Raitt 2005); J Eritsland, Oslo University Hospital, Norway (SHOT 1996); and I Brouwer, Vrije Universiteit Amsterdam, the Netherlands (SOFA 2006).
Warm thanks and appreciation to the authors of the first review who did not continue as authors in the review update, including Roger A Harrison, Andrew Ness, Nigel E Capps, George Davey Smith, Shah BJ Ebrahim and Rudolph A Riemersma. Acknowledgements for the earlier version of this systematic review, which we have built on to create the current review: our thanks to Julian Higgins, who was involved in the design of the review, along with Theresa Moore and Margaret Burke from the Cochrane Heart Group. Also to Charlotte C Hammer for help with German translation for Franzen 1993.
Appendices
Appendix 1. Medline (Ovid) search strategy run in 2002 for the previous version of this review.
1 exp Fish Oils/ 2 exp Linseed Oil/ 3 linolenic acids/ or exp alpha‐linolenic acid/ 4 exp Fatty Acids, Omega‐3/ 5 (fish adj5 (diet$ or nutrit$ or oil$ or supplement$)).tw. 6 (oil$ adj3 (cod$ or marin$ or rapeseed$ or canola$)).tw. 7 (omega‐3 or omega3).tw. 8 (eicosapentaen$ or icosapentaen$).tw. 9 docosahexaen$.tw. 10 (Linolen$ or alpha‐linolen$ or alphalinolen$).tw. 11 (maxepa$ or omacor$).tw. 12 (trout or kipper$ or salmon or mackerel$ or tuna or tunafish or sardine$ or pilchard$ or herring$).tw. 13 flax$.tw. 14 rapeseed$.tw. 15 canola$.tw. 16 alphalinolen$.tw. 17 perilla$.tw. 18 linolen$.tw. 19 linseed$.tw. 20 maxepa$.tw. 21 (oil$ adj3 colza).tw. 22 (marin$ adj3 (lipid$ or oil$)).tw. 23 naudicelle$.tw. 24 sild.tw. 25 (clupe$ adj3 hareng$).tw. 26 whitebait$.tw. 27 sprat$.tw. 28 brisling$.tw. 29 (salmo adj3 trut$).tw. 30 bloater.tw. 31 scomb$.tw. 32 conger$.tw. 33 tunny.tw. 34 tuna‐fish.tw. 35 thunnus$.tw. 36 swordfish$.tw. 37 xiphias$.tw. 38 dogfish.tw. 39 scyliorhinus$.tw. 40 (crab or crabs).tw. 41 (cancer adj3 pagurus).tw. 42 (laks or lax).tw. 43 exp Flax/ 44 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 45 randomized controlled trial.pt. 46 controlled clinical trial.pt. 47 randomized.ab. 48 placebo.ab. 49 clinical trials as topic.sh. 50 randomly.ab. 51 trial.ti. 52 50 or 47 or 51 or 46 or 45 or 48 or 49 53 (animals not (human and animals)).sh. 54 52 not 53 55 44 and 54 56 (20$ not (2000$ or 2001$)).ed. 57 55 and 56
Appendix 2. Searches run in July 2016 to update the omega‐3 review
CENTRAL
#1 MeSH descriptor: [Fish Oils] explode all trees
#2 MeSH descriptor: [Linseed Oil] this term only
#3 MeSH descriptor: [Linolenic Acids] this term only
#4 MeSH descriptor: [Fatty Acids, Omega‐3] explode all trees
#5 (fish near/3 oil*)
#6 (oil* near/3 (cod* or marin*))
#7 (omega‐3 or omega3 or (omega* near/5 fat*))
#8 eicosapentaen*
#9 docosahexaen*
#10 (oil* near/3 (flax* or rapeseed* or canola*))
#11 (Linolen* or alpha‐linolen* or alphalinolen*)
#12 (perilla* or linseed* or maxepa*)
#13 (oil* near/3 (rape or colza))
#14 (marin* near/3 lipid*)
#15 (naudicelle* or herring* or sild)
#16 (clupe* near/3 hareng*)
#17 (whitebait or sardine* or sardina* or pilchard* or sprat* or brisling*)
#18 (salmo* near/3 trut*)
#19 (trout or bloater or kipper* or salmon or mackerel* or scomb* or conger* or tuna or tunny or tunafish or tuna‐fish)
#20 (thunnus* or swordfish* or xiphias* or dogfish or scyliorrhinus*)
#21 (crab or crabs or (cancer pagarus))
#22 (DHA or EPA)
#23 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 Publication Year from 2002 to 2016
#24 MeSH descriptor: [Salmoniformes] explode all trees
#25 MeSH descriptor: [Tuna] this term only
#26 MeSH descriptor: [alpha‐Linolenic Acid] this term only
#27 MeSH descriptor: [Flax] this term only
#28 (fish near/3 (diet* or capsul* or nutrit* or supplement*))
#29 (icosapentaen* or docosapentaen*)
#30 (oil* near/3 (purslane or mustard* or candlenut* or stillingia or walnut*))
#31 (laks or lax)
#32 (ALA or DPA)
#33 (algal near oil*)
#34 #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33
#35 #23 or #34
MEDLINE Ovid
1. exp Fish Oils/
2. Linseed Oil/
3. linolenic acids/ or alpha‐linolenic acid/
4. Flax/
5. exp Fatty Acids, Omega‐3/
6. (fish adj3 (diet* or nutrit* or oil* or supplement*)).ti,ab.
7. (oil* adj3 (cod* or marin*)).ti,ab.
8. (omega‐3 or omega3 or (omega* adj5 fat*)).ti,ab.
9. eicosapentaen*.ti,ab.
10. docosahexaen*.ti,ab.
11. (oil* adj3 (flax* or rapeseed* or canola*)).ti,ab.
12. (Linolen* or alpha‐linolen* or alphalinolen*).ti,ab.
13. (perilla* or linseed* or maxepa*).ti,ab.
14. (oil* adj3 (rape or colza)).ti,ab.
15. (marin* adj3 lipid*).ti,ab.
16. (naudicelle* or herring* or sild).ti,ab.
17. (clupe* adj3 hareng*).ti,ab.
18. (whitebait or sardine* or sardina* or pilchard* or sprat* or brisling*).ti,ab.
19. (salmo* adj3 trut*).ti,ab.
20. (trout or bloater or kipper* or salmon or mackerel* or scomb* or conger* or tuna or tunny or tunafish or tuna‐fish).ti,ab.
21. (thunnus* or swordfish* or xiphias* or dogfish or scyliorrhinus* or laks or lax).ti,ab.
22. (crab or crabs or cancer pagarus).ti,ab.
23. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
24. randomized controlled trial.pt.
25. controlled clinical trial.pt.
26. randomized.ab.
27. placebo.ab.
28. clinical trials as topic.sh.
29. randomly.ab.
30. trial.ti.
31. 24 or 25 or 26 or 27 or 28 or 29 or 30
32. exp animals/ not humans.sh.
33. 31 not 32
34. 23 and 33
35. limit 34 to ed=20020201‐20160721
36. exp salmoniformes/ or tuna/
37. (fish adj3 capsul*).ti,ab.
38. icosapentaen*.ti,ab.
39. docosapentaen*.ti,ab.
40. (oil* adj3 (purslane or mustard* or candlenut* or stillingia or walnut*)).ti,ab.
41. 36 or 37 or 38 or 39 or 40
42. 33 and 41
43. 35 or 42
Embase Ovid
1. exp salmoniformes/ or tuna/
2. fish oil/
3. linseed oil/
4. linolenic acid/
5. Flax/
6. omega 3 fatty acid/
7. (fish adj3 (diet* or nutrit* or oil* or supplement*)).ti,ab.
8. (oil* adj3 (cod* or marin*)).ti,ab.
9. (omega‐3 or omega3 or (omega* adj5 fat*)).ti,ab.
10. (eicosapentaen* or icosapentaen*).ti,ab.
11. docosahexaen*.ti,ab.
12. (oil* adj3 (flax* or rapeseed* or canola*)).ti,ab.
13. (Linolen* or alpha‐linolen* or alphalinolen*).ti,ab.
14. (perilla* or linseed* or maxepa*).ti,ab.
15. (marin* adj3 lipid*).ti,ab.
16. (naudicelle* or herring* or sild).ti,ab.
17. (clupe* adj3 hareng*).ti,ab.
18. (whitebait or sardine* or sardina* or pilchard* or sprat* or brisling*).ti,ab.
19. (salmo* adj3 trut*).ti,ab.
20. (trout or bloater or kipper* or salmon or mackerel* or scomb* or conger* or tuna or tunny or tunafish or tuna‐fish).ti,ab.
21. (thunnus* or swordfish* or xiphias* or dogfish or scyliorrhinus* or laks or lax).ti,ab.
22. (crab or crabs or (cancer adj3 pagarus)).ti,ab.
23. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
24. random$.tw.
25. placebo$.tw.
26. (doubl$ adj blind$).tw.
27. (singl$ adj blind$).tw.
28. double blind procedure/
29. randomized controlled trial/
30. single blind procedure/
31. 24 or 25 or 26 or 27 or 28 or 29 or 30
32. (animal/ or nonhuman/) not human/
33. 31 not 32
34. 23 and 33
35. (2002* or 2003* or 2004* or 2005* or 2006* or 2007* or 2008* or 2009* or 2010* or 2011* or 2012* or 2013* or 2014* or 2015* or 2016*).dd,em.
36. 34 and 35
37. exp salmonine/
38. (fish adj3 capsul*).ti,ab.
39. docosapentaen*.ti,ab.
40. (ALA or DHA or DPA or EPA).ti,ab.
41. (algal adj oil*).ti,ab.
42. 37 or 38 or 39 or 40 or 41
43. 33 and 42
44. 36 or 43
Appendix 3. Searches run in April 2017 for allied reviews
These searches were developed and run to collect relevant trials for the systematic reviews on omega‐6 fats (the update of Hooper 2018) and on total PUFA fats (Abdelhamid 2018) on health. They are shown here as these searches were run with the searches for this review, the identified titles and abstracts de‐duplicated and combined, so that we assessed titles and abstracts for all three reviews together. These searches were each run from database inception, due to the widening of the inclusion criteria, then de‐duplicated with each other. The RCT filter for MEDLINE is the Cochrane sensitivity and precision‐maximising RCT filter, and for Embase, terms as recommended in the Cochrane Handbook have been applied (Lefebvre 2011).
CENTRAL
#1 MeSH descriptor: [Fatty Acids, Essential] explode all trees
#2 MeSH descriptor: [Fatty Acids, Unsaturated] this term only
#3 ((polyunsaturat* or poly‐unsaturat*) near/3 fat*)
#4 (poly* adj4 unsat* near/4 fatty acid*)
#5 PUFA
#6 MeSH descriptor: [Fatty Acids, Omega‐6] explode all trees
#7 omega‐6
#8 (n‐6 near/4 acid*) or ("n 6" near/4 acid*)
#9 linoleic acid*
#10 MeSH descriptor: [Corn Oil] this term only
#11 MeSH descriptor: [Cottonseed Oil] this term only
#12 MeSH descriptor: [Olive Oil] this term only
#13 MeSH descriptor: [Safflower Oil] this term only
#14 MeSH descriptor: [Sesame Oil] this term only
#15 MeSH descriptor: [Soybean Oil] this term only
#16 ((corn or maize or mazola) near/4 oil*)
#17 (cottonseed* or (cotton next seed*))
#18 (olive near/4 oil*)
#19 (safflower near/4 oil*)
#20 (sesame near/4 oil*)
#21 ((soy bean or soybean) near/4 (oil* or fat*))
#22 (so?a near/4 oil*)
#23 so?aoil*
#24 (soy near/4 oil*)
#25 (sunflower near/4 oil*)
#26 helianth*
#27 (grapeseed near/4 oil*)
#28 (canola near/4 oil*)
#29 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28
MEDLINE Ovid
1. exp fatty acids, essential/
2. fatty acids, unsaturated/
3. ((polyunsaturat* or poly‐unsaturat*) adj3 fat*).ti,ab.
4. (poly* adj4 unsat* adj4 fatty acid*).ti,ab.
5. PUFA.ti,ab.
6. exp fatty acids, omega‐6/
7. omega‐6.ti,ab.
8. (n‐6 adj4 acid*).ti,ab.
9. linoleic acid*.ti,ab.
10. corn oil/ or cottonseed oil/ or olive oil/ or safflower oil/ or sesame oil/ or soybean oil/
11. ((corn or maize or mazola) adj4 oil*).ti,ab.
12. (cottonseed* or (cotton adj seed*)).ti,ab.
13. (olive adj4 oil*).ti,ab.
14. (safflower adj4 oil*).ti,ab.
15. (sesame adj4 oil*).ti,ab.
16. ((soy bean or soybean) adj4 (oil* or fat*)).ti,ab.
17. (so?a adj4 oil*).ti,ab.
18. so?aoil*.ti,ab.
19. (soy adj4 oil*).ti,ab.
20. (sunflower adj4 oil*).ti,ab.
21. helianth*.ti,ab.
22. (grapeseed adj4 oil*).ti,ab.
23. (canola adj4 oil*).ti,ab.
24. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
25. randomized controlled trial.pt.
26. controlled clinical trial.pt.
27. randomized.ab.
28. placebo.ab.
29. clinical trials as topic.sh.
30. randomly.ab.
31. trial.ti.
32. 25 or 26 or 27 or 28 or 29 or 30 or 31
33. exp animals/ not humans.sh.
34. 32 not 33
35. 24 and 34
Embase Ovid
1. exp essential fatty acid/
2. unsaturated fatty acid/ or docosapentaenoic acid/ or omega 6 fatty acid/ or polyunsaturated fatty acid/
3. ((polyunsaturat* or poly‐unsaturat*) adj3 fat*).ti,ab.
4. (poly* adj4 unsat* adj4 fatty acid*).ti,ab.
5. PUFA.ti,ab.
6. omega‐6.ti,ab.
7. (n‐6 adj4 acid*).ti,ab.
8. linoleic acid*.ti,ab.
9. edible oil/ or canola oil/ or corn oil/ or cotton seed oil/ or olive oil/ or safflower oil/ or safflower oil plus soybean oil/ or sesame seed oil/ or soybean oil/ or sunflower oil/
10. ((corn or maize or mazola) adj4 oil*).ti,ab.
11. (cottonseed* or (cotton adj seed*)).ti,ab.
12. (olive adj4 oil*).ti,ab.
13. (safflower adj4 oil*).ti,ab.
14. (sesame adj4 oil*).ti,ab.
15. ((soy bean or soybean) adj4 (oil* or fat*)).ti,ab.
16. (so?a adj4 oil*).ti,ab.
17. so?aoil*.ti,ab.
18. (soy adj4 oil*).ti,ab.
19. (sunflower adj4 oil*).ti,ab.
20. helianth*.ti,ab.
21. (grapeseed adj4 oil*).ti,ab.
22. (canola adj4 oil*).ti,ab.
23. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
24. double blind procedure/
25. single blind procedure/
26. randomized controlled trial/
27. ((double* or single*) adj blind*).ti,ab.
28. (random* or placebo*).ti,ab.
29. 24 or 25 or 26 or 27 or 28
30. (animal/ or nonhuman/) not human/
31. 29 not 30
32. 23 and 31
Data and analyses
Comparison 1.
High vs low LCn3 omega‐3 fats (primary outcomes)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All‐cause mortality (overall) ‐ LCn3 | 39 | 92653 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 2 All‐cause mortality ‐ LCn3 ‐ sensitivity analysis (SA) fixed‐effect | 39 | 90244 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.93, 1.01] |
| 3 All‐cause mortality ‐ LCn3 ‐ SA by summary risk of bias | 39 | 92653 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 3.1 Low risk of bias | 15 | 33146 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.08] |
| 3.2 Moderate/high risk of bias | 24 | 59507 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.86, 1.03] |
| 4 All‐cause mortality ‐ LCn3 ‐ SA by compliance and study size | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 SA ‐ low risk of compliance bias | 18 | 15654 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.86, 1.14] |
| 4.2 SA ‐ 100+ randomised | 35 | 92397 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 5 All‐cause mortality ‐ LCn3 ‐ subgroup by dose | 39 | 92653 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 5.1 LCn3 ≤150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 LCn3 > 150 ≤ 250 mg/d | 1 | 407 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.27, 2.18] |
| 5.3 LCn3 > 250 ≤400 mg/d | 1 | 2033 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.56, 0.92] |
| 5.4 LCn3 > 400 ≤ 2400 mg/d | 28 | 87445 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 5.5 LCn3 > 2.4 ≤ 4.4 g/d | 7 | 2486 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.67, 1.70] |
| 5.6 LCn3 > 4.4 g/d | 2 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.03, 3.08] |
| 6 All‐cause mortality ‐ LCn3 ‐ subgroup by replacement | 39 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 LCn3 replacing SFA | 5 | 3279 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.56, 0.92] |
| 6.2 LCn3 replacing MUFA | 15 | 46176 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.90, 1.02] |
| 6.3 LCn3 replacing N‐6 | 9 | 2806 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.51, 1.09] |
| 6.4 LCn3 replacing CHO | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.05, 5.65] |
| 6.5 LCn3 replacing nil/low n‐3 placebo | 10 | 39601 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.86, 1.14] |
| 6.6 LCn3 replacement unclear | 3 | 3593 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.46, 1.79] |
| 7 All‐cause mortality ‐ LCn3 ‐ subgroup by intervention type | 39 | 92653 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 7.1 Dietary advice | 3 | 5554 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.60, 1.35] |
| 7.2 Supplemental foods | 2 | 5039 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.84, 1.24] |
| 7.3 Supplements (capsule) | 33 | 81855 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.92, 1.01] |
| 7.4 Any combination | 1 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.11, 3.79] |
| 8 All‐cause mortality ‐ LCn3 ‐ subgroup by duration | 39 | 92653 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 8.1 Medium duration 1 to < 2 years in study | 18 | 9737 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.82, 1.30] |
| 8.2 Medium‐long duration: 2 to < 4 years in study | 14 | 29234 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.86, 0.96] |
| 8.3 Long duration: ≥ 4 years in study | 7 | 53682 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.98, 1.09] |
| 9 All‐cause mortality ‐ LCn3 ‐ subgroup by primary or secondary prevention | 39 | 92653 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.03] |
| 9.1 Primary CVD prevention | 17 | 41202 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.08] |
| 9.2 Secondary CVD prevention | 22 | 51451 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.04] |
| 10 All‐cause mortality ‐ LCn3 ‐ subgroup by statin use | 39 | 90244 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.92, 1.03] |
| 10.1 LCn3 ‐ ≥50% of control group on statins | 8 | 40500 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.93, 1.11] |
| 10.2 LCn3 ‐ < 50% of control group on statins | 26 | 46604 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.03] |
| 10.3 LCn3 ‐ use of statins unclear | 5 | 3140 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.58, 1.63] |
| 11 Cardiovascular mortality (overall) ‐ LCn3 | 25 | 67772 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 12 CVD mortality ‐ LCn3 ‐ SA fixed‐effect | 25 | 67772 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.89, 1.00] |
| 13 CVD mortality ‐ LCn3 ‐ SA by summary risk of bias | 25 | 67772 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 13.1 Low risk of bias | 9 | 29133 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.90, 1.09] |
| 13.2 Moderate/high risk of bias | 16 | 38639 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.05] |
| 14 CVD mortality ‐ LCn3 ‐ SA by compliance and study size | 24 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 14.1 SA ‐ low risk of compliance bias | 12 | 13244 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.23] |
| 14.2 SA ‐ 100+ randomised | 21 | 67516 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.04] |
| 15 CVD mortality ‐ LCn3 ‐ subgroup by dose | 26 | 67873 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 15.1 LCn3 ≤ 150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 LCn3 > 250 ≤ 400 mg/d | 1 | 2033 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.53, 0.91] |
| 15.4 LCn3 > 400 ≤ 2400 mg/d | 19 | 64126 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.06] |
| 15.5 LCn3 > 2.4 ≤ 4.4 g/d | 4 | 1432 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.58, 1.77] |
| 15.6 LCn3 > 4.4 g/d | 2 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.03, 3.08] |
| 16 CVD mortality ‐ LCn3 ‐ subgroup by replacement | 26 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 16.1 N‐3 replacing SFA | 3 | 2537 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.53, 0.90] |
| 16.2 N‐3 replacing MUFA | 12 | 44242 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.86, 1.04] |
| 16.3 N‐3 replacing N‐6 | 4 | 1435 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.41, 1.19] |
| 16.4 N‐3 replacing carbohydrates/sugars | 1 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.12, 4.07] |
| 16.5 N‐3 replacing nil/low n‐3 placebo | 8 | 19275 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.73, 0.96] |
| 16.6 Replacement unclear | 2 | 3186 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.05, 5.77] |
| 17 CVD mortality ‐ LCn3 ‐ subgroup by intervention type | 25 | 67772 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 17.1 Dietary advice | 2 | 5147 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.52, 1.71] |
| 17.2 Supplemental foods | 2 | 5039 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.72, 1.32] |
| 17.3 Supplements (capsule) | 21 | 57586 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.88, 0.99] |
| 17.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 CVD mortality ‐ LCn3 ‐ subgroup by duration | 25 | 67772 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 18.1 Medium duration 1 to < 2 years in study | 10 | 6177 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.57, 1.36] |
| 18.2 Medium‐long duration: 2 to < 4 years in study | 10 | 26736 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.82, 0.95] |
| 18.3 Long duration: ≥ 4 years in study | 5 | 34859 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.93, 1.18] |
| 19 CVD mortality ‐ LCn3 ‐ subgroup by primary or secondary prevention | 25 | 67772 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 19.1 Primary prevention | 7 | 17931 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.88, 1.09] |
| 19.2 Secondary prevention | 18 | 49841 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.83, 1.06] |
| 20 CVD mortality ‐ LCn3 ‐ subgroup by statin uses | 25 | 67772 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 20.1 LCn3 ‐ ≥ 50% of control group on statins | 6 | 23994 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.90, 1.10] |
| 20.2 LCn3 ‐ < 50% of control group on statins | 17 | 43425 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.82, 1.04] |
| 20.3 LCn3‐ Use of statins unclear | 2 | 353 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.06, 2.30] |
| 21 Cardiovascular events (overall) ‐ LCn3 | 38 | 90378 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 22 CVD events ‐ LCn3 ‐ SA fixed‐effect | 38 | 90378 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.95, 1.00] |
| 23 CVD events ‐ LCn3 ‐ SA by summary risk of bias | 38 | 90378 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 23.1 Low risk of bias | 14 | 31649 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.96, 1.05] |
| 23.2 Moderate/high risk of bias | 24 | 58729 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.03] |
| 24 CVD events ‐ LCn3 ‐ SA by compliance and study size | 37 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 24.1 SA ‐ low risk of compliance bias | 16 | 13649 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.84, 1.14] |
| 24.2 SA ‐ 100+ randomised | 33 | 90058 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 25 CVD events ‐ LCn3 ‐ subgroup by dose | 38 | 90453 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 25.1 LCn3 ≤ 150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.3 LCn3 > 250 ≤ 400 mg/d | 1 | 2033 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.88, 1.05] |
| 25.4 LCn3 > 400 ≤ 2400 mg/d | 28 | 85818 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 25.5 LCn3 > 2.4 ≤ 4.4 g/d | 7 | 2180 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.75, 1.28] |
| 25.6 LCn3 > 4.4 g/d | 3 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.65, 1.81] |
| 26 CVD events ‐ LCn3 ‐ subgroup by replacement | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 26.1 N‐3 replacing SFA | 4 | 2888 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.04] |
| 26.2 N‐3 replacing MUFA | 16 | 45065 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.94, 1.02] |
| 26.3 N‐3 replacing n‐6 | 6 | 1891 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.90, 1.35] |
| 26.4 N‐3 replacing carbohydrates/sugars | 1 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.12, 3.98] |
| 26.5 N‐3 replacing nil/low n‐3 placebo | 12 | 39907 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.85, 1.07] |
| 26.6 Replacement unclear | 3 | 3429 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.16, 2.07] |
| 27 CVD events ‐ LCn3 ‐ subgroup by intervention type | 38 | 90378 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 27.1 Dietary advice | 3 | 5248 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.86, 1.49] |
| 27.2 Supplemental foods | 2 | 5039 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.89, 1.17] |
| 27.3 Supplements (capsule) | 33 | 80091 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.91, 1.02] |
| 27.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 CVD events ‐ LCn3 ‐ subgroup by duration | 38 | 90378 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 28.1 Medium duration 1 to < 2 years in study | 18 | 8107 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.68, 1.16] |
| 28.2 Medium‐long duration: 2 to < 4 years in study | 14 | 28767 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.93, 1.01] |
| 28.3 Long duration: ≥ 4 years in study | 6 | 53504 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.91, 1.08] |
| 29 CVD events ‐ LCn3 ‐ subgroup by primary or secondary prevention | 38 | 90378 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 29.1 Primary prevention of CVD | 16 | 39751 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.05] |
| 29.2 Secondary prevention | 22 | 50627 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.93, 1.07] |
| 30 CVD events ‐ LCn3 ‐ subgroup by statin use | 38 | 90378 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.04] |
| 30.1 LCn3 ‐ ≥ 50% of control group on statins | 8 | 42389 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.89, 1.08] |
| 30.2 LCn3 ‐ < 50% of control group on statins | 24 | 45160 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.91, 1.04] |
| 30.3 LCn3 ‐ use of statins unclear | 6 | 2829 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.53, 1.63] |
| 31 Coronary heart disease mortality (overall) ‐ LCn3 | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 32 CHD mortality ‐ LCn3 ‐ SA fixed‐effect | 21 | 73491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.85, 1.03] |
| 33 CHD mortality ‐ LCn3 ‐ SA by summary risk of bias | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 33.1 Low risk of bias | 7 | 16372 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.72, 1.37] |
| 33.2 Moderate/high risk of bias | 14 | 57119 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.75, 1.10] |
| 34 CHD mortality ‐ LCn3 ‐ SA by compliance and study size | 21 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 34.1 SA ‐ low risk of compliance bias | 9 | 12938 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.83, 1.32] |
| 34.2 SA ‐ 100+ randomised | 20 | 73411 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 35 CHD mortality ‐ LCn3 ‐ SA omitting cardiac death | 16 | 65325 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.74, 0.94] |
| 35.1 Low risk of bias | 5 | 12022 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.69, 1.30] |
| 35.2 Moderate/high risk of bias | 11 | 53303 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.72, 0.94] |
| 36 CHD mortality ‐ LCn3 ‐ subgroup by dose | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 36.1 LCn3 ≤ 150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.3 LCn3 > 250 ≤ 400 mg/d | 2 | 5147 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.50, 1.74] |
| 36.4 LCn3 > 400 ≤ 2400 mg/d | 15 | 67442 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.07] |
| 36.5 LCn3 > 2.4 ≤ 4.4 g/d | 3 | 822 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.49, 1.78] |
| 36.6 LCn3 > 4.4 g/d | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 7.57] |
| 37 CHD mortality ‐ LCn3 ‐ subgroup by replacement | 21 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 37.1 N‐3 replacing SFA | 3 | 2514 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.51, 0.88] |
| 37.2 N‐3 replacing MUFA | 10 | 31605 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.72, 1.10] |
| 37.3 N‐3 replacing n‐6 | 3 | 1409 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.33, 1.24] |
| 37.4 N‐3 replacing carbohydrates/sugars | 1 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.01, 8.23] |
| 37.5 N‐3 replacing nil/low n‐3 placebo | 7 | 37651 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.70, 0.97] |
| 37.6 Replacement unclear | 1 | 3114 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.03, 1.57] |
| 38 CHD mortality ‐ LCn3 ‐ subgroup by intervention type | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 38.1 Dietary advice | 2 | 5147 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.50, 1.74] |
| 38.2 Supplemental foods | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.69, 1.33] |
| 38.3 Supplements (capsule) | 18 | 63507 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.79, 1.02] |
| 38.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 CHD mortality ‐ LCn3 ‐ subgroup by duration | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 39.1 Medium duration 1 to < 2 years in study | 7 | 5978 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.62, 1.50] |
| 39.2 Medium‐long duration: 2 to < 4 years in study | 9 | 26545 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.69, 0.90] |
| 39.3 Long duration: ≥ 4 years in study | 5 | 40968 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.00, 1.39] |
| 40 CHD mortality ‐ LCn3 ‐ subgroup by primary or secondary prevention | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 40.1 Primary prevention of CVD | 5 | 23789 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.46, 1.61] |
| 40.2 Secondary prevention of CVD | 16 | 49702 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.11] |
| 41 CHD mortality ‐ LCn3 ‐ subgroup by statin use | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.79, 1.09] |
| 41.1 LCn3 ‐ ≥ 50% of control group on statins | 5 | 30025 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.84, 1.30] |
| 41.2 LCn3 ‐ < 50% of control group on statins | 15 | 43208 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.72, 1.10] |
| 41.3 LCn3 ‐ use of statins unclear | 1 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.01, 8.23] |
| 42 CHD mortality ‐ LCn3 ‐ subgroup by CAD history | 21 | 73491 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.80, 1.09] |
| 42.1 Previous CAD | 11 | 29074 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.77, 1.20] |
| 42.2 No previous CAD | 10 | 44417 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.74, 1.16] |
| 43 Coronary heart disease events (overall) ‐ LCn3 | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.97] |
| 44 CHD events ‐ LCn3 ‐ SA fixed‐effect | 28 | 84301 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.88, 0.97] |
| 45 CHD events ‐ LCn3 ‐ SA by summary risk of bias | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.97] |
| 45.1 Low risk of bias | 12 | 30227 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.90, 1.05] |
| 45.2 Moderate/high risk of bias | 16 | 54074 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.84, 0.95] |
| 46 CHD events ‐ LCn3 ‐ SA by compliance and study size | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 46.1 SA ‐ low risk of compliance bias | 12 | 13447 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.86, 1.02] |
| 46.2 SA ‐ 100+ randomised | 25 | 84084 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.98] |
| 47 CHD events ‐ LCn3 ‐ subgroup by dose | 28 | 84376 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 47.1 LCn3 ≤ 150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 47.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 47.3 LCn3 > 250 ≤ 400 mg/d | 1 | 2033 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.82, 1.04] |
| 47.4 LCn3 > 400 ≤ 2400 mg/d | 21 | 80730 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.98] |
| 47.5 LCn3 > 2.4 ≤ 4.4 g/d | 4 | 1191 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.53, 1.53] |
| 47.6 LCn3 > 4.4 g/d | 3 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.54, 1.85] |
| 48 CHD events ‐ LCn3 ‐ subgroup by replacement | 28 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 48.1 N‐3 replacing SFA | 3 | 2514 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.16, 1.75] |
| 48.2 N‐3 replacing MUFA | 15 | 44954 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.90, 1.01] |
| 48.3 N‐3 replacing n‐6 | 4 | 1549 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.88, 1.39] |
| 48.4 N‐3 replacing carbohydrates/sugars | 1 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.11 [0.01, 2.07] |
| 48.5 N‐3 replacing nil/low n‐3 placebo | 8 | 37843 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.78, 0.94] |
| 48.6 Replacement unclear | 1 | 243 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.08, 9.70] |
| 49 CHD events ‐ LCn3 ‐ subgroup by intervention type | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 49.1 Dietary advice | 2 | 2134 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.67, 1.52] |
| 49.2 Supplemental foods | 2 | 5039 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.75, 1.18] |
| 49.3 Supplements (capsule) | 24 | 77128 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.98] |
| 49.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 50 CHD events ‐ LCn3 ‐ subgroup by duration | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 50.1 Medium duration 1 to < 2 years in study | 11 | 7009 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.86, 1.03] |
| 50.2 Medium‐long duration: 2 to < 4 years in study | 12 | 26902 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.84, 0.98] |
| 50.3 Long duration: ≥ 4 years in study | 5 | 50390 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 51 CHD events ‐ LCn3 ‐ subgroup by primary or secondary prevention | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 51.1 Primary prevention of CVD | 11 | 37365 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.81, 1.10] |
| 51.2 Secondary prevention of CVD | 17 | 46936 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.98] |
| 52 CHD events ‐ LCn3 ‐ subgroup by statin use | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 52.1 LCn3 ‐ ≥ 50% of control group on statins | 8 | 42735 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.85, 1.05] |
| 52.2 LCn3 ‐ < 50% of control group on statins | 17 | 40674 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.86, 0.98] |
| 52.3 LCn3 ‐ use of statins unclear | 3 | 892 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.11, 3.83] |
| 53 CHD events ‐ LCn3 subgroup by CAD history | 28 | 84301 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.97] |
| 53.1 Previous CAD | 12 | 26124 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.87, 0.98] |
| 53.2 No previous CAD | 16 | 58177 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.86, 1.01] |
| 54 Stroke (overall) ‐ LCn3 | 28 | 89358 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.16] |
| 55 Stroke ‐ LCn3 ‐ SA fixed‐effect | 28 | 89358 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.97, 1.16] |
| 56 Stroke ‐ LCn3 ‐ SA by summary risk of bias | 28 | 89358 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.16] |
| 56.1 Low risk of bias | 12 | 32039 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 56.2 Moderate/high risk of bias | 16 | 57319 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [1.00, 1.29] |
| 57 Stroke ‐ LCn3 ‐ SA by compliance and study size | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 57.1 SA ‐ low risk of compliance bias | 12 | 14451 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.86, 1.65] |
| 57.2 SA ‐ 100+ randomised | 26 | 89231 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.97, 1.18] |
| 58 Stroke ‐ LCn3 ‐ subgroup by stroke type | 13 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 58.1 Ischaemic stroke ‐ LCn3 | 8 | 35040 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.89, 1.33] |
| 58.2 Haemorrhagic stroke ‐ LCn3 | 8 | 36645 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.85, 1.69] |
| 58.3 Transient ischaemic attack (TIA) | 5 | 5032 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.39, 1.39] |
| 59 Stroke ‐ LCn3 ‐ subgroup by dose | 28 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 59.1 LCn3 ≤ 150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 59.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 59.3 LCn3 > 250 ≤ 400 mg/d | 1 | 2033 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.14, 1.44] |
| 59.4 LCn3 > 400 ≤ 2400 mg/d | 24 | 86335 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.16] |
| 59.5 LCn3 > 2.4 ≤ 4.4 g/d | 1 | 610 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.16, 3.07] |
| 59.6 LCn3 > 4.4 g/d | 2 | 380 | Risk Ratio (M‐H, Random, 95% CI) | 6.58 [0.78, 55.16] |
| 60 Stroke ‐ LCn3 ‐ subgroup by replacement | 28 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 60.1 N‐3 replacing SFA | 3 | 2514 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.19, 1.50] |
| 60.2 N‐3 replacing MUFA | 14 | 45252 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.94, 1.31] |
| 60.3 N‐3 replacing n‐6 | 3 | 1179 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [0.18, 24.31] |
| 60.4 N‐3 replacing carbohydrates/sugars | 1 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.01, 8.23] |
| 60.5 N‐3 replacing nil/low n‐3 placebo | 9 | 39555 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.92, 1.24] |
| 60.6 Replacement unclear | 1 | 3114 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.55, 2.29] |
| 61 Stroke ‐ LCn3 ‐ subgroup by intervention type | 28 | 89358 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.16] |
| 61.1 Dietary advice | 3 | 5248 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.42, 2.05] |
| 61.2 Supplemental foods | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.47, 2.62] |
| 61.3 Supplements (capsule) | 24 | 79273 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.97, 1.18] |
| 61.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 62 Stroke ‐ LCn3 ‐ subgroup by duration | 28 | 89358 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.16] |
| 62.1 Medium duration 1 to < 2 years in study | 11 | 7467 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.86, 2.12] |
| 62.2 Medium‐long duration: 2 to < 4 years in study | 11 | 28387 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.93, 1.41] |
| 62.3 Long duration: ≥ 4 years in study | 6 | 53504 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.91, 1.13] |
| 63 Stroke ‐ LCn3 ‐ subgroup by primary or secondary prevention | 28 | 89358 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.16] |
| 63.1 Primary prevention of CVD | 9 | 39332 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.09] |
| 63.2 Secondary prevention of CVD | 19 | 50026 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.05, 1.40] |
| 64 Stroke ‐ LCn3 ‐ subgroup by statin use | 28 | 89358 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.16] |
| 64.1 LCn3 ‐ ≥ 50% of control group on statins | 8 | 42962 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.86, 1.23] |
| 64.2 LCn3 ‐ < 50% of control group on statins | 17 | 44999 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.02, 1.37] |
| 64.3 LCn3 ‐ use of statins unclear | 3 | 1397 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.38, 2.34] |
| 65 Arrythmia (overall) ‐ LCn3 | 27 | 53796 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.90, 1.05] |
| 66 Arrhythmia‐ LCn3 ‐ SA fixed‐effect | 27 | 53796 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.96, 1.07] |
| 67 Arrhythmia‐ LCn3 ‐ SA by summary risk of bias | 27 | 53796 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.90, 1.05] |
| 67.1 Low risk of bias | 10 | 25801 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.98, 1.23] |
| 67.2 Moderate/high risk of bias | 17 | 27995 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.02] |
| 68 Arrhythmia‐ LCn3 ‐ SA by compliance and study size | 26 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 68.1 SA ‐ low risk of compliance bias | 10 | 12914 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.09] |
| 68.2 SA ‐ 100+ randomised | 26 | 53749 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.05] |
| 69 Arrhythmia ‐ LCn3 ‐ subgroup by new or recurrent | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 69.1 New arrhythmia | 16 | 50175 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.99, 1.16] |
| 69.2 Recurrent arrhythmia | 12 | 4425 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 70 Arrhythmia ‐ LCn3 ‐ subgroup by fatality | 17 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 70.1 Fatal arrhythmias ‐ LCn3 | 2 | 12938 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.95, 1.31] |
| 70.2 Non‐fatal arrhythmias ‐ LCn3 | 8 | 2079 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.57, 0.96] |
| 70.3 Fatal and non‐fatal arrhythmias combined ‐ LCn3 | 10 | 36007 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.17] |
| 71 Arrhythmia ‐ LCn3 ‐ subgroup by dose | 27 | 53796 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.04] |
| 71.1 LCn3 ≤ 150 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 71.2 LCn3 > 150 ≤ 250 mg/d | 1 | 407 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.90, 1.12] |
| 71.3 LCn3 > 250 ≤ 400 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 71.4 LCn3 > 400 ≤ 2400 mg/d | 19 | 51535 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.88, 1.08] |
| 71.5 LCn3 > 2.4 ≤ 4.4 g/d | 3 | 1076 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.55, 0.94] |
| 71.6 LCn3 > 4.4 g/d | 2 | 342 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.32, 3.83] |
| 71.7 Unclear LCn3 dose | 2 | 436 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.76, 1.28] |
| 72 Arrhythmia ‐ LCn3 ‐ subgroup by replacement | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 72.1 N‐3 replacing SFA | 2 | 632 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.10, 5.67] |
| 72.2 N‐3 replacing MUFA | 12 | 42246 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.88, 1.11] |
| 72.3 N‐3 replacing n‐6 | 4 | 1302 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.86, 1.16] |
| 72.4 N‐3 replacing carbohydrates/sugars | 1 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.04, 3.21] |
| 72.5 N‐3 replacing nil/low n‐3 placebo | 6 | 8983 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.69, 0.91] |
| 72.6 Replacement unclear | 4 | 1179 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.91, 1.08] |
| 73 Arrhythmia ‐ LCn3 ‐ subgroup by intervention type | 27 | 53796 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.90, 1.05] |
| 73.1 Dietary advice | 2 | 508 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.44, 1.72] |
| 73.2 Supplemental foods | 2 | 5039 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.67, 1.26] |
| 73.3 Supplements (capsule) | 23 | 48249 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.88, 1.06] |
| 73.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 74 Arrhythmia ‐ LCn3 ‐ subgroup by duration | 27 | 53796 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.04] |
| 74.1 Medium duration 1 to < 2 years in study | 17 | 8553 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.04] |
| 74.2 Medium‐long duration: 2 to < 4 years in study | 7 | 17701 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.84, 1.10] |
| 74.3 Long duration: ≥ 4 years in study | 3 | 27542 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.99, 1.29] |
| 75 Arrhythmia ‐ LCn3 ‐ subgroup by primary or secondary prevention3 | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 75.1 Primary prevention | 8 | 14565 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.97, 1.28] |
| 75.2 Secondary prevention | 19 | 39231 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.86, 1.03] |
| 76 Arrhythmia ‐ LCn3 ‐ subgroup by statin use | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 76.1 LCn3 ‐ ≥ 50% of control group on statins | 5 | 23779 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.95, 1.22] |
| 76.2 LCn3 ‐ < 50% of control group on statins | 18 | 28932 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.85, 1.04] |
| 76.3 LCn3 ‐ use of statins unclear | 4 | 1085 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.80, 1.18] |
Analysis 1.10.
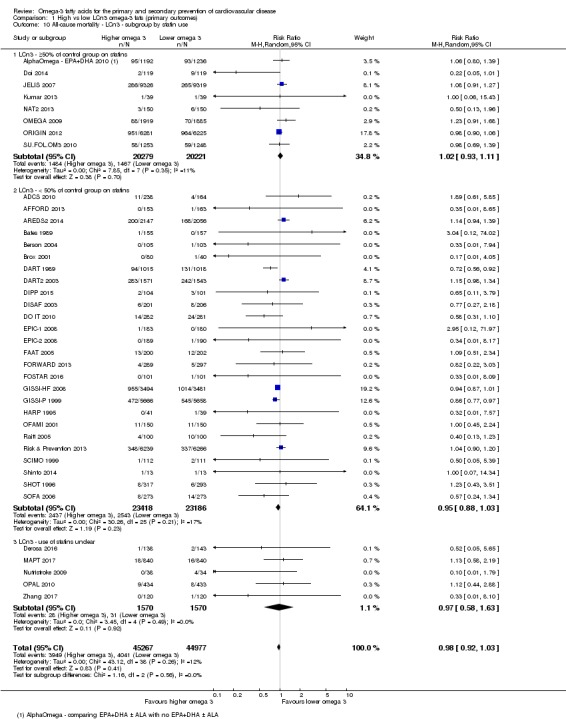
Comparison 1 High vs low LCn3 omega‐3 fats (primary outcomes), Outcome 10 All‐cause mortality ‐ LCn3 ‐ subgroup by statin use.
Comparison 2.
High vs low LCn3 omega‐3 fats (secondary outcomes)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 MACCEs ‐ LCn3 | 5 | 34730 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.97, 1.09] |
| 2 Myocardial infarction (overall) ‐ LCn3 | 23 | 72159 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.03] |
| 3 Total MI ‐ sensitivity analysis (SA) by summary risk of bias | 23 | 72159 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.03] |
| 3.1 Low summary risk of bias | 11 | 30025 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.92, 1.15] |
| 3.2 Moderate to high risk of bias | 12 | 42134 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.79, 0.99] |
| 4 Total MI ‐ LCn3 ‐ SA by compliance and study size | 23 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 SA ‐ low risk of compliance bias | 10 | 13002 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.79, 1.13] |
| 4.2 SA ‐ 100+ randomised | 21 | 72015 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.88, 1.03] |
| 5 Total MI ‐ LCn3 ‐ subgroup by fatality | 23 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Fatal MI | 15 | 60471 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.53, 1.10] |
| 5.2 Non‐fatal MI | 21 | 70407 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.87, 1.06] |
| 6 Sudden cardiac death (overall) ‐ LCn3 | 14 | 65004 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.80, 1.18] |
| 7 Angina ‐ LCn3 | 11 | 39907 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.91, 1.06] |
| 8 Heart failure ‐ LCn3 | 15 | 49644 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.85, 1.03] |
| 8.1 Low summary risk of bias | 6 | 24176 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.06] |
| 8.2 Moderate to high risk of bias | 9 | 25468 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.57, 1.08] |
| 9 Revascularisation ‐ LCn3 | 15 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 CABG ‐ LCn3 | 5 | 1535 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.15, 2.14] |
| 9.2 Angioplasty ‐ LCn3 | 4 | 3195 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.24] |
| 9.3 Any revascularisation ‐ LCn3 | 12 | 66095 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.94, 1.03] |
| 10 Peripheral arterial disease ‐ LCn3 | 6 | 49035 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.74, 1.18] |
| 11 PAD ‐ LCn3 ‐ SA by summary risk of bias | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Low summary risk of bias | 2 | 12738 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.75, 1.62] |
| 11.2 Moderate to high summary risk of bias | 4 | 36297 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.64, 1.14] |
| 12 PAD ‐ LCn3 ‐ SA compliance and study size | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 SA compliance | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.06, 15.77] |
| 12.2 SA study size 100+ | 6 | 49035 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.74, 1.18] |
| 13 Acute coronary syndrome ‐ LCn3 | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 LCn3 | 2 | 2703 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.71, 2.00] |
| 14 Body weight, kg ‐ LCn3 | 12 | 15812 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.84, 0.82] |
| 15 Weight, kg ‐ LCn3 ‐ SA by summary risk of bias | 12 | 15812 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.84, 0.82] |
| 15.1 Low risk of bias | 7 | 15458 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.91, 0.90] |
| 15.2 Moderate/high risk of bias | 5 | 354 | Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐3.12, 2.55] |
| 16 Weight, kg ‐ LCn3 ‐ SA by compliance and study size | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 SA ‐ low risk of compliance bias | 7 | 828 | Mean Difference (IV, Random, 95% CI) | 0.58 [‐0.52, 1.69] |
| 16.2 SA ‐ 100+ randomised | 7 | 15545 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.84, 0.97] |
| 17 Weight, kg ‐ LCn3 ‐ subgroup by dose | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 17.1 LCn3 ≤ 150 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 LCn3 > 250 ≤ 400 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.4 LCn3 > 400 ≤ 2400 mg/d | 8 | 15420 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐1.16, 0.58] |
| 17.5 LCn3 > 2.4 ≤ 4.4 g/d | 3 | 241 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐6.38, 6.51] |
| 17.6 LCn3 > 4.4 g/d | 2 | 261 | Mean Difference (IV, Random, 95% CI) | 1.51 [0.28, 2.75] |
| 18 Weight, kg ‐ LCn3 ‐ subgroup by replacement | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 18.1 N‐3 replacing SFA | 2 | 433 | Mean Difference (IV, Random, 95% CI) | ‐2.51 [‐4.30, ‐0.72] |
| 18.2 N‐3 replacing MUFA | 7 | 15088 | Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.28, 0.75] |
| 18.3 N‐3 replacing n‐6 | 1 | 41 | Mean Difference (IV, Random, 95% CI) | ‐1.3 [‐3.83, 1.23] |
| 18.4 N‐3 replacing carbs/sugars | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐2.70 [‐4.75, ‐0.65] |
| 18.5 N‐3 replacing nil/low n‐3 placebo | 1 | 202 | Mean Difference (IV, Random, 95% CI) | 1.5 [0.25, 2.75] |
| 18.6 Replacement unclear | 2 | 223 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐4.93, 6.13] |
| 19 Weight, kg ‐ LCn3 ‐ subgroup by intervention type | 12 | 15812 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.84, 0.82] |
| 19.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.2 Supplemental foods | 1 | 202 | Mean Difference (IV, Random, 95% CI) | 1.5 [0.25, 2.75] |
| 19.3 Supplement (capsule) | 9 | 15538 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.08, 0.63] |
| 19.4 Any combination | 2 | 72 | Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐6.47, 5.61] |
| 20 Weight, kg ‐ LCn3 ‐ subgroup by duration | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 20.1 Medium duration 1 to < 2 years in study | 8 | 840 | Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐2.21, 1.12] |
| 20.2 Medium‐long duration: 2 to < 4 years in study | 3 | 436 | Mean Difference (IV, Random, 95% CI) | 0.67 [‐1.58, 2.91] |
| 20.3 Long duration ≥ 4 years in study | 1 | 14536 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.48, 0.68] |
| 21 Weight, kg ‐ LCn3 ‐ subgroup by primary or secondary prevention | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 21.1 Primary CVD prevention | 10 | 15578 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.83, 0.92] |
| 21.2 Secondary CVD prevention | 2 | 234 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐4.43, 2.16] |
| 22 Weight, kg ‐ LCn3 ‐ subgroup by statin use | 12 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 22.1 LCn3 ‐ ≥ 50% of control group on statins | 2 | 14631 | Mean Difference (IV, Random, 95% CI) | 0.64 [‐1.88, 3.17] |
| 22.2 LCn3 ‐ < 50% of control group on statins | 5 | 614 | Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.66, 1.60] |
| 22.3 LCn3 ‐ use of statins unclear | 5 | 567 | Mean Difference (IV, Random, 95% CI) | ‐1.51 [‐3.30, 0.27] |
| 23 Body mass index, kg/m² ‐ LCn3 | 14 | 15234 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.16, 0.24] |
| 24 BMI, kg/m²‐ LCn3 ‐ SA by summary risk of bias | 14 | 15234 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.16, 0.24] |
| 24.1 Low risk of bias | 5 | 14190 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.36, 0.33] |
| 24.2 Moderate/high risk of bias | 9 | 1044 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.13, 0.20] |
| 25 BMI, kg/m²‐ LCn3 ‐ SA by compliance and study size | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 25.1 SA ‐ low risk of compliance bias | 5 | 1848 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.21, 0.38] |
| 25.2 SA ‐ 100+ randomised | 9 | 14982 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.12, 0.14] |
| 26 BMI, kg/m² ‐ LCn3 ‐ subgroup by dose | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 26.1 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 LCn3 ≤ 150 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.3 LCn3 > 250 ≤ 400 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.4 LCn3 > 400 ≤ 2400 mg/d | 11 | 14789 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.11, 0.13] |
| 26.5 LCn3 > 2.4 ≤ 4.4 g/d | 3 | 445 | Mean Difference (IV, Random, 95% CI) | 1.42 [‐0.51, 3.35] |
| 26.6 LCn3 > 4.4 g/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 BMI, kg/m² ‐ LCn3 ‐ subgroup by replacement | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 27.1 N‐3 replacing SFA | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.14, ‐0.06] |
| 27.2 N‐3 replacing MUFA | 7 | 14180 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.12, 0.28] |
| 27.3 N‐3 replacing n‐6 | 3 | 513 | Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.46, 0.81] |
| 27.4 N‐3 replacing carbs/sugars | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.14, ‐0.06] |
| 27.5 N‐3 replacing nil/low n‐3 placebo | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.0 [‐1.18, 3.18] |
| 27.6 Replacement unclear | 2 | 223 | Mean Difference (IV, Random, 95% CI) | 0.58 [‐1.17, 2.33] |
| 28 BMI, kg/m² ‐ LCn3 ‐ subgroup by intervention type | 14 | 15234 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.16, 0.24] |
| 28.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 Supplemental foods | 1 | 1260 | Mean Difference (IV, Random, 95% CI) | 0.1 [‐0.10, 0.30] |
| 28.3 Supplement (capsule) | 12 | 13929 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.25, 0.27] |
| 28.4 Any combination | 1 | 45 | Mean Difference (IV, Random, 95% CI) | 1.60 [‐0.43, 3.63] |
| 29 BMI, kg/m² ‐ LCn3 ‐ subgroup by duration | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 29.1 Medium duration 1 to < 2 years in study | 9 | 906 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.40, 0.88] |
| 29.2 Medium‐long duration: 2 to < 4 years in study | 4 | 1792 | Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.07, 0.31] |
| 29.3 Long duration ≥ 4 years in study | 1 | 12536 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.20, 0.20] |
| 30 BMI, kg/m² ‐ LCn3 ‐ subgroup by primary or secondary prevention | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 30.1 Primary CVD prevention | 11 | 13610 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.36, 0.66] |
| 30.2 Secondary CVD prevention | 3 | 1624 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.08, 0.18] |
| 31 BMI, kg/m² ‐ LCn3 ‐ subgroup by statin use | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 31.1 LCn3 ‐ ≥ 50% of control group on statins | 3 | 13891 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.22, 0.48] |
| 31.2 LCn3 ‐ < 50% of control group on statins | 4 | 665 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.15, 0.19] |
| 31.3 LCn3 ‐ use of statins unclear | 7 | 678 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.86, 0.97] |
| 32 Other measures of adiposity ‐ LCn3 | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 32.1 Percentage body fat | 2 | 127 | Mean Difference (IV, Random, 95% CI) | 0.85 [‐6.87, 8.57] |
| 32.2 Percentage visceral fat | 1 | 95 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐15.03, 11.43] |
| 32.3 Waist circumference, cm | 3 | 676 | Mean Difference (IV, Random, 95% CI) | 0.66 [‐0.09, 1.42] |
| 32.4 Waist‐hip ratio | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.01, 0.01] |
| 32.5 Abdominal circumference, cm | 1 | 256 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐8.78, 7.38] |
| 32.6 Hip circumference, cm | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐9.80, 5.00] |
| 33 Total cholesterol, serum, mmoL/L ‐ LCn3 | 28 | 37281 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.05, 0.04] |
| 34 TC, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias | 28 | 37281 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.05, 0.03] |
| 34.1 Low risk of bias | 9 | 14930 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.05, 0.06] |
| 34.2 Moderate/high risk of bias | 19 | 22351 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| 35 TC, mmoL/L ‐ LCn3 ‐ SA by compliance and study size | 20 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 35.1 SA ‐ low risk of compliance bias | 14 | 3341 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.05, 0.09] |
| 35.2 SA ‐ 100+ randomised | 15 | 36622 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.05, 0.06] |
| 36 TC, mmoL/L ‐ LCn3 ‐ subgroup by dose | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 36.1 LCn3 ≤ 150 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.3 LCn3 > 250 ≤ 400 mg/d | 1 | 1715 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.01, 0.21] |
| 36.4 LCn3 > 400 ≤ 2400 mg/d | 18 | 34262 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.06, 0.00] |
| 36.5 LCn3 > 2.4 ≤ 4.4 g/d | 7 | 1216 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.28, ‐0.01] |
| 36.6 LCn3 > 4.4 g/d | 2 | 88 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.28, 0.45] |
| 37 TC, mmoL/L ‐ LCn3 ‐ subgroup by replacement | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 37.1 N‐3 replacing SFA | 3 | 2148 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.01, 0.20] |
| 37.2 N‐3 replacing MUFA | 15 | 16504 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.04, 0.06] |
| 37.3 N‐3 replacing n‐6 | 5 | 895 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.22, 0.26] |
| 37.4 N‐3 replacing carbs/sugars | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.03, 0.63] |
| 37.5 N‐3 replacing nil/low n‐3 placebo | 5 | 19431 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.07, ‐0.03] |
| 37.6 Replacement unclear | 2 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.47, 0.17] |
| 38 TC, mmoL/L ‐ LCn3 ‐ subgroup by intervention type | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 38.1 Dietary advice | 1 | 1715 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.01, 0.21] |
| 38.2 Supplemental foods | 1 | 1210 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.09, 0.13] |
| 38.3 Supplement (capsule) | 24 | 34145 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.07, ‐0.03] |
| 38.4 Any combination | 2 | 211 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.10, 0.37] |
| 39 TC, mmoL/L ‐ LCn3 ‐ subgroup by duration | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 39.1 Medium duration 1 to < 2 years in study | 15 | 1661 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.16, 0.04] |
| 39.2 Medium‐long duration: 2 to < 4 years in study | 10 | 4231 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.05, 0.10] |
| 39.3 Long duration ≥ 4 years in study | 3 | 31389 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.09, 0.09] |
| 40 TC, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 40.1 Primary prevention | 17 | 32796 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.07, ‐0.02] |
| 40.2 Secondary prevention | 11 | 4485 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.09, 0.08] |
| 41 TC, mmoL/L ‐ LCn3 ‐ subgroup by statin use | 28 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 41.1 LCn3 ‐ ≥ 50% of control group on statins | 6 | 32823 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.07, ‐0.02] |
| 41.2 LCn3 ‐ < 50% of control group on statins | 15 | 3871 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.08, 0.10] |
| 41.3 LCn3 ‐ use of statins unclear | 7 | 587 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.27, 0.22] |
| 42 Triglycerides, fasting, serum, mmoL/L ‐ LCn3 | 25 | 35579 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.31, ‐0.16] |
| 43 TG, fasting, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias | 25 | 35579 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.30, ‐0.16] |
| 43.1 Low risk of bias | 8 | 14654 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.25, ‐0.09] |
| 43.2 Moderate/high risk of bias | 17 | 20925 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.35, ‐0.15] |
| 44 TG, fasting, mmoL/L ‐ LCn3 ‐ SA by compliance and study size | 19 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 44.1 SA ‐ low risk of compliance bias | 12 | 3306 | Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.36, ‐0.16] |
| 44.2 SA ‐ 100+ randomised | 18 | 35197 | Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.32, ‐0.16] |
| 45 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by dose | 25 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 45.1 LCn3 ≤ 150 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 45.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 45.3 LCn3 > 250 ≤ 400 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 45.4 LCn3 > 400 ≤ 2400 mg/d | 18 | 34388 | Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.25, ‐0.11] |
| 45.5 LCn3 > 2.4 ≤ 4.4 g/d | 5 | 1107 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.53, ‐0.20] |
| 45.6 LCn3 > 4.4 g/d | 2 | 84 | Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.68, ‐0.14] |
| 46 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by replacement | 25 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 46.1 N‐3 replacing SFA | 2 | 429 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.59, 0.04] |
| 46.2 N‐3 replacing MUFA | 13 | 14634 | Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.25, ‐0.10] |
| 46.3 N‐3 replacing n‐6 | 5 | 876 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.45, ‐0.08] |
| 46.4 N‐3 replacing carbs/sugars | 1 | 258 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐1.49, 0.49] |
| 46.5 N‐3 replacing nil/low n‐3 placebo | 4 | 19357 | Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.51, 0.14] |
| 46.6 Replacement unclear | 2 | 454 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.57, ‐0.19] |
| 47 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by intervention type | 25 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 47.1 Dietary advice | 1 | 71 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.36, 0.40] |
| 47.2 Supplemental foods | 1 | 1210 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.15, 0.09] |
| 47.3 Supplement (capsule) | 22 | 34137 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.38, ‐0.00] |
| 47.4 Any combination | 1 | 161 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.28, 0.30] |
| 48 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by duration | 25 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 48.1 Medium duration 1 to < 2 years in study | 13 | 1880 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.36, ‐0.19] |
| 48.2 Medium‐long duration: 2 to < 4 years in study | 9 | 2310 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.31, ‐0.02] |
| 48.3 Long duration ≥ 4 years in study | 3 | 31389 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.32, ‐0.07] |
| 49 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention | 25 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 49.1 Primary prevention | 17 | 33114 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.26, ‐0.14] |
| 49.2 Secondary prevention | 8 | 2465 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.44, ‐0.10] |
| 50 TG, fasting, mmoL/L ‐ LCn3 ‐ subgroup by statin use | 25 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 50.1 LCn3 ‐ ≥ 50% of control group on statins | 5 | 32557 | Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.21, ‐0.01] |
| 50.2 LCn3 ‐ < 50% of control group on statins | 14 | 2414 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.36, ‐0.18] |
| 50.3 LCn3 ‐ use of statins unclear | 6 | 608 | Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.38, ‐0.08] |
| 51 High‐density lipoprotein, serum, mmoL/L ‐ LCn3 | 27 | 37237 | Mean Difference (IV, Random, 95% CI) | 0.02 [0.00, 0.04] |
| 52 HDL, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias | 27 | 37237 | Mean Difference (IV, Random, 95% CI) | 0.03 [0.01, 0.05] |
| 52.1 Low risk of bias | 8 | 14892 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.01, 0.07] |
| 52.2 Moderate/high risk of bias | 19 | 22345 | Mean Difference (IV, Random, 95% CI) | 0.03 [0.00, 0.06] |
| 53 HDL, mmoL/L ‐ LCn3 ‐ SA by compliance and study size | 20 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 53.1 SA ‐ low risk of compliance bias | 13 | 3202 | Mean Difference (IV, Random, 95% CI) | 0.05 [0.01, 0.10] |
| 53.2 SA ‐ 100+ randomised | 15 | 36573 | Mean Difference (IV, Random, 95% CI) | 0.03 [0.00, 0.05] |
| 54 HDL, mmoL/L ‐ LCn3 ‐ subgroup by dose | 27 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 54.1 LCn3 ≤ 150 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 54.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 54.3 LCn3 > 250 ≤ 400 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 54.4 LCn3 > 400 ≤ 2400 mg/d | 19 | 35972 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.00, 0.04] |
| 54.5 LCn3 > 2.4 ≤ 4.4 g/d | 7 | 1206 | Mean Difference (IV, Random, 95% CI) | 0.06 [0.00, 0.12] |
| 54.6 LCn3 > 4.4 g/d | 1 | 59 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.16, 0.16] |
| 55 HDL, mmoL/L ‐ LCn3 ‐ subgroup by replacement | 27 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 55.1 N‐3 replacing SFA | 3 | 2143 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.10, 0.07] |
| 55.2 N‐3 replacing MUFA | 15 | 16505 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.01, 0.06] |
| 55.3 N‐3 replacing n‐6 | 4 | 850 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.01, 0.09] |
| 55.4 N‐3 replacing carbs/sugars | 1 | 258 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.17, 0.37] |
| 55.5 N‐3 replacing nil/low n‐3 placebo | 5 | 19431 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.03, 0.11] |
| 55.6 Replacement unclear | 2 | 193 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.10, 0.20] |
| 56 HDL, mmoL/L ‐ LCn3 ‐ subgroup by intervention type | 27 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 56.1 Dietary advice | 2 | 1785 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.02, 0.04] |
| 56.2 Supplemental foods | 1 | 1210 | Mean Difference (IV, Random, 95% CI) | 0.03 [0.00, 0.06] |
| 56.3 Supplement (capsule) | 21 | 34008 | Mean Difference (IV, Random, 95% CI) | 0.03 [0.00, 0.06] |
| 56.4 Any combination | 3 | 234 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.10, 0.31] |
| 57 HDL, mmoL/L ‐ LCn3 ‐ subgroup by duration | 27 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 57.1 Medium duration 1 to < 2 years in study | 13 | 1562 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.01, 0.14] |
| 57.2 Medium‐long duration: 2 to < 4 years in study | 11 | 4286 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.01, 0.04] |
| 57.3 Long duration ≥ 4 years in study | 3 | 31389 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.01, 0.01] |
| 58 HDL, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention | 26 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 58.1 Primary prevention | 17 | 32856 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.00, 0.05] |
| 58.2 Secondary prevention | 9 | 4307 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.01, 0.07] |
| 59 HDL, mmoL/L ‐ LCn3 ‐ subgroup by statin use | 27 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 59.1 LCn3 ‐ ≥ 50% of control group on statins | 7 | 32894 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
| 59.2 LCn3 ‐ < 50% of control group on statins | 13 | 3690 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.00, 0.08] |
| 59.3 LCn3 ‐ use of statins unclear | 7 | 653 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.07, 0.21] |
| 60 Low‐density lipoprotein, serum, mmoL/L ‐ LCn3 | 23 | 35035 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
| 61 LDL, mmoL/L ‐ LCn3 ‐ SA by summary risk of bias | 23 | 35035 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
| 61.1 Low risk of bias | 9 | 14840 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.03, 0.07] |
| 61.2 Moderate/high risk of bias | 14 | 20195 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.02, 0.03] |
| 62 LDL, mmoL/L ‐ LCn3 ‐ SA by compliance and study size | 17 | 37718 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.01, 0.05] |
| 62.1 SA ‐ low risk of compliance bias | 13 | 3165 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.02, 0.11] |
| 62.2 SA ‐ 100+ randomised | 14 | 34553 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.02, 0.04] |
| 63 LDL, mmoL/L ‐ LCn3 ‐ subgroup by dose | 23 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 63.1 LCn3 ≤ 150 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63.2 LCn3 > 150 ≤ 250 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63.3 LCn3 > 250 ≤ 400 mg/d | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63.4 LCn3 > 400 ≤ 2400 mg/d | 16 | 34054 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.01, 0.02] |
| 63.5 LCn3 > 2.4 ≤ 4.4 g/d | 5 | 893 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.14, 0.15] |
| 63.6 LCn3 > 4.4 g/d | 2 | 88 | Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.09, 0.54] |
| 64 LDL, mmoL/L ‐ LCn3 ‐ subgroup by replacement | 23 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 64.1 N‐3 replacing SFA | 2 | 429 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.14, 0.47] |
| 64.2 N‐3 replacing MUFA | 14 | 14710 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 64.3 N‐3 replacing n‐6 | 2 | 242 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.26, 0.55] |
| 64.4 N‐3 replacing carbs/sugars | 1 | 258 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.51, 0.91] |
| 64.5 N‐3 replacing nil/low n‐3 placebo | 3 | 19297 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.02, 0.02] |
| 64.6 Replacement unclear | 3 | 528 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.03, 0.23] |
| 65 LDL, mmoL/L ‐ LCn3 ‐ subgroup by intervention type | 23 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 65.1 Dietary advice | 1 | 71 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.22, 0.38] |
| 65.2 Supplemental foods | 1 | 1124 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.10, 0.06] |
| 65.3 Supplement (capsule) | 19 | 33768 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
| 65.4 Any combination | 2 | 72 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.44, 0.61] |
| 66 LDL, mmoL/L ‐ LCn3 ‐ subgroup by duration | 23 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 66.1 Medium duration 1 to < 2 years in study | 14 | 1862 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.03, 0.14] |
| 66.2 Medium‐long duration: 2 to < 4 years in study | 6 | 1784 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.08, 0.06] |
| 66.3 Long duration ≥ 4 years in study | 3 | 31389 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.04, 0.10] |
| 67 LDL, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention | 23 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 67.1 Primary prevention | 16 | 32717 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
| 67.2 Secondary prevention | 7 | 2318 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.05, 0.08] |
| 68 LDL, mmoL/L ‐ LCn3 ‐ subgroup by statin use | 23 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 68.1 LCn3 ‐ ≥ 50% of control group on statins | 7 | 32808 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.02, 0.02] |
| 68.2 LCn3 ‐ < 50% of control group on statins | 9 | 1564 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.03, 0.21] |
| 68.3 LCn3 ‐ use of statins unclear | 7 | 663 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.17, 0.14] |
Analysis 2.40.
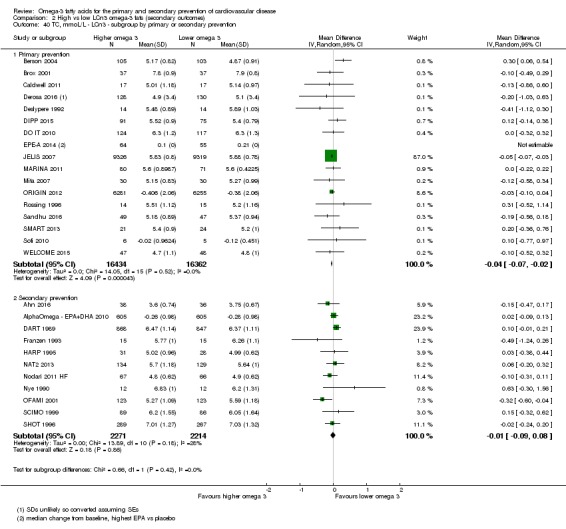
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 40 TC, mmoL/L ‐ LCn3 ‐ subgroup by primary or secondary prevention.
Analysis 2.41.
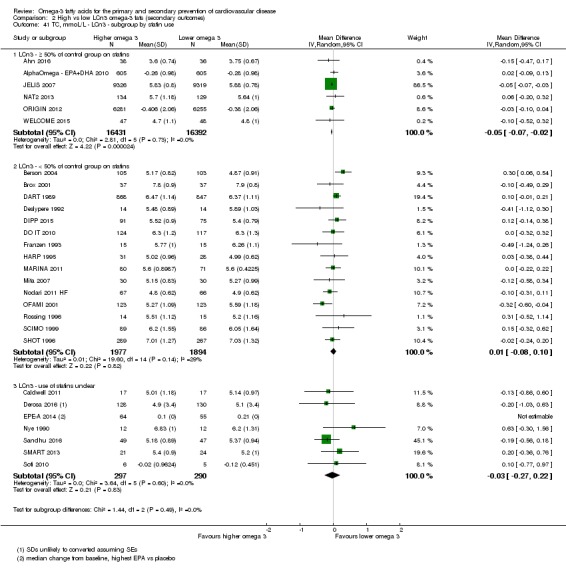
Comparison 2 High vs low LCn3 omega‐3 fats (secondary outcomes), Outcome 41 TC, mmoL/L ‐ LCn3 ‐ subgroup by statin use.
Comparison 3.
High vs low LCn3 omega‐3 fats (tertiary outcomes)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Blood pressure, mmHg ‐ LCn3 | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Systolic BP ‐ LCn3 | 15 | 34413 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.32, 0.35] |
| 1.2 Diastolic BP ‐ LCn3 | 14 | 35386 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.22, 0.17] |
| 2 Serious adverse events ‐ LCn3 | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Any serious adverse events | 1 | 402 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.78, 1.41] |
| 2.2 Bleeding | 8 | 45562 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.73, 1.52] |
| 2.3 GI hospitalisation | 1 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.53, 5.79] |
| 2.4 Pulmonary embolus or DVT ‐ LCn3 | 4 | 3011 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.41, 3.78] |
| 2.5 Progression to advanced AMD (age‐related macular degeneration) | 1 | 4203 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.90, 1.02] |
| 3 Side effects ‐ LCn3 | 33 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Dropouts due to side effects | 23 | 16755 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.99, 1.36] |
| 3.2 Abdominal pain or discomfort | 7 | 14650 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.84, 1.45] |
| 3.3 Diarrhoea | 10 | 2428 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.92, 1.43] |
| 3.4 Nausea | 5 | 1234 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.23, 2.44] |
| 3.5 Any gastrointestinal side effect ‐ LCn3 fats | 29 | 65185 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.94, 1.34] |
| 3.6 Skin problems (itching, rashes) | 8 | 36186 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.47, 2.30] |
| 3.7 Headache or worsening migraine | 3 | 991 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.48, 1.35] |
| 3.8 Reflux | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.71, 2.81] |
| 3.9 Pain (joint, lumbar, muscle pain) | 1 | 18645 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.64, 0.99] |
| 3.10 All side effects combined | 13 | 38904 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.95, 1.08] |
| 4 Dropouts ‐ LCn3 | 30 | 31321 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.95, 1.09] |
Comparison 4.
High vs low ALA omega‐3 fat (primary outcomes)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All‐cause mortality (overall) ‐ ALA | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 2 All‐cause mortality ‐ ALA ‐ sensitivity analysis (SA) fixed‐effect | 5 | 16923 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.84, 1.34] |
| 3 All‐cause mortality ‐ ALA ‐ SA by summary risk of bias | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 3.1 Low risk of bias | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.72, 1.45] |
| 3.2 Moderate/high risk of bias | 2 | 14114 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.71, 1.67] |
| 4 All‐cause mortality ‐ ALA ‐ SA by compliance and study size | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 SA ‐ low risk of compliance bias | 3 | 5811 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.68, 1.63] |
| 4.2 SA ‐ 100+ randomised | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 5 All‐cause mortality ‐ ALA ‐ subgroup by dose | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 5.1 ALA low < 5 g/d | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.80, 1.19] |
| 5.2 ALA high ≥ 5 g/d | 4 | 14490 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.77, 1.75] |
| 6 All‐cause mortality ‐ ALA ‐ subgroup by replacement | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 ALA replacing SFA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 ALA replacing MUFA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.80, 1.19] |
| 6.3 ALA replacing n‐6 | 2 | 13672 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.48, 3.86] |
| 6.4 ALA replacing CHO | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.5 ALA replacing nil/low n‐3 placebo | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.6 ALA replacement unclear | 2 | 818 | Risk Ratio (M‐H, Random, 95% CI) | 2.78 [0.29, 26.49] |
| 7 All cause mortality ‐ ALA ‐ subgroup by intervention type | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 7.1 Dietary advice | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Supplemental foods | 4 | 5921 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.82, 1.21] |
| 7.3 Supplements (capsule) | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.70, 1.64] |
| 7.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 All‐cause mortality ‐ ALA ‐ subgroup by duration | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 8.1 Medium duration 1 to < 2 years in study | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.71, 1.67] |
| 8.2 Medium‐long duration: 2 to < 4 years in study | 3 | 5811 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.68, 1.63] |
| 8.3 Long duration: ≥ 4 years in study | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 All‐cause mortality ‐ ALA ‐ subgroup by primary or secondary prevention | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.20] |
| 9.1 Primary CVD prevention | 3 | 14380 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.75, 1.74] |
| 9.2 Secondary CVD prevention | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.81, 1.19] |
| 10 All‐cause mortality ‐ ALA ‐ subgroup by statin use | 5 | 16923 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.84, 1.33] |
| 10.1 ALA ‐ ≥ 50% of control group on statins | 2 | 2543 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.77, 1.34] |
| 10.2 ALA ‐ < 50% of control group on statins | 3 | 14380 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.75, 1.74] |
| 11 Cardiovascular mortality (overall) ‐ ALA | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 12 CVD mortality ‐ ALA ‐ SA fixed‐effect | 4 | 18619 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.74, 1.25] |
| 13 CVD mortality ‐ ALA ‐ SA by summary risk of bias | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 13.1 Low risk of bias | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.70, 1.28] |
| 13.2 Moderate/high risk of bias | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 14 CVD mortality ‐ ALA ‐ SA by compliance and study size | 4 | 23722 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.78, 1.16] |
| 14.1 SA ‐ low risk of compliance bias | 2 | 5103 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.70, 1.27] |
| 14.2 SA ‐ 100+ randomised | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 15 CVD mortality ‐ ALA ‐ subgroup by dose | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 15.1 ALA low < 5 g/d | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.69, 1.27] |
| 15.2 ALA high ≥ 5 g/d | 3 | 13782 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.62, 1.73] |
| 16 CVD mortality ‐ ALA ‐ subgroup by replacement | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 16.1 N‐3 replacing SFA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 N‐3 replacing MUFA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.69, 1.27] |
| 16.3 N‐3 replacing n‐6 | 2 | 13672 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.60, 1.70] |
| 16.4 N‐3 replacing carbohydrates/sugars | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.5 N‐3 replacing nil/low n‐3 placebo | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.6 Replacement unclear | 1 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 2.69 [0.11, 64.74] |
| 17 CVD mortality ‐ ALA ‐ subgroup by intervention type | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 17.1 Dietary advice | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Supplemental foods | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.70, 1.28] |
| 17.3 Supplements (capsule) | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 17.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 CVD mortality ‐ ALA ‐ subgroup by duration | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 18.1 Medium duration 1 to < 2 years in study | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.61, 1.73] |
| 18.2 Medium‐long duration: 2 to < 4 years in study | 2 | 5103 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.70, 1.27] |
| 18.3 Long duration: ≥ 4 years in study | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 CVD mortality ‐ ALA ‐ subgroup by primary or secondary prevention | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 19.1 Primary prevention | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 19.2 Secondary prevention | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.70, 1.28] |
| 20 CVD mortality ‐ ALA ‐ subgroup by statin uses | 4 | 18619 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.74, 1.25] |
| 20.1 ALA ‐ ≥ 50% of control group on statins | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.70, 1.28] |
| 20.2 ALA ‐ < 50% of control group on statins | 2 | 13672 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.60, 1.70] |
| 21 Cardiovascular events (overall) ‐ ALA | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 22 CVD events ‐ ALA ‐ SA fixed‐effect | 5 | 19327 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.84, 1.07] |
| 23 CVD events ‐ ALA ‐ SA by summary risk of bias | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 23.1 Low risk of bias | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.79, 1.04] |
| 23.2 Moderate/high risk of bias | 2 | 14114 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.84, 1.48] |
| 24 CVD events ‐ ALA ‐ SA by compliance and study size | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 24.1 SA ‐ low risk of compliance bias | 3 | 5811 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.79, 1.04] |
| 24.2 SA ‐ 100+ randomised | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 25 CVD events ‐ ALA ‐ subgroup by dose | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 25.1 ALA low < 5 g/d | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.79, 1.05] |
| 25.2 ALA high ≥ 5 g/d | 4 | 14490 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.82, 1.40] |
| 26 CVD events ‐ ALA ‐ subgroup by replacement | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 26.1 N‐3 replacing SFA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 N‐3 replacing MUFA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.79, 1.05] |
| 26.3 N‐3 replacing n‐6 | 2 | 13672 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.24, 2.41] |
| 26.4 N‐3 replacing carbohydrates/sugars | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.5 N‐3 replacing nil/low n‐3 placebo | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.6 Replacement unclear | 2 | 818 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.36, 2.43] |
| 27 CVD events ‐ ALA ‐ subgroup by intervention type | 6 | 19526 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 27.1 Dietary advice | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 Supplemental foods | 5 | 6120 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.79, 1.04] |
| 27.3 Supplements (capsule) | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.85, 1.51] |
| 27.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 CVD events ‐ ALA ‐ subgroup by duration | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 28.1 Medium duration 1 to < 2 years in study | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.86, 1.50] |
| 28.2 Medium‐long duration: 2 to < 4 years in study | 3 | 5811 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.79, 1.04] |
| 28.3 Long duration: ≥ 4 years in study | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 CVD events ‐ ALA ‐ subgroup by primary or secondary prevention | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 29.1 Primary prevention | 3 | 14380 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.46, 1.67] |
| 29.2 Secondary prevention | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.05] |
| 30 CVD events ‐ ALA ‐ subgroup by statin use | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.07] |
| 30.1 ALA ‐ ≥ 50% of control group on statins | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.05] |
| 30.2 ALA ‐ < 50% of control group on statins | 3 | 14380 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.46, 1.67] |
| 31 Coronary heart disease mortality (overall) ‐ ALA | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 32 CHD mortality ‐ ALA ‐ SA fixed‐effect | 3 | 18353 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.72, 1.26] |
| 33 CHD mortality ‐ ALA ‐ SA by summary risk of bias | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 33.1 Low risk of bias | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.67, 1.30] |
| 33.2 Moderate/high risk of bias | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 34 CHD mortality ‐ ALA ‐ SA by compliance and study size | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 34.1 SA ‐ low risk of compliance bias | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.66, 1.28] |
| 34.2 SA ‐ 100+ randomised | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 35 CHD mortality ‐ ALA ‐ subgroup by dose | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 35.1 ALA low < 5 g/d | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.66, 1.28] |
| 35.2 ALA high ≥ 5 g/d | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.61, 1.73] |
| 36 CHD mortality ‐ ALA ‐ subgroup by replacement | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 36.1 N‐3 replacing SFA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Coronary heart mortality‐ ALA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.3 N‐3 replacing MUFA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.66, 1.28] |
| 36.4 N‐3 replacing n‐6 | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 36.5 N‐3 replacing carbohydrates/sugars | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.6 N‐3 replacing nil/low n‐3 placebo | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.7 Replacement unclear | 1 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 2.69 [0.11, 64.74] |
| 37 CHD mortality ‐ ALA ‐ subgroup by intervention type | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 37.1 Dietary advice | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37.2 Supplemental foods | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.67, 1.30] |
| 37.3 Supplements (capsule) | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 37.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 CHD mortality ‐ ALA ‐ subgroup by duration | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 38.1 Medium duration 1 to < 2 years in study | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.61, 1.73] |
| 38.2 Medium‐long duration: 2 to < 4 years in study | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.66, 1.28] |
| 38.3 Long duration: ≥ 4 years in study | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 CHD mortality ‐ ALA ‐ subgroup by primary or secondary prevention | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 39.1 Primary prevention of CVD | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 39.2 Secondary prevention of CVD | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.67, 1.30] |
| 40 CHD mortality ‐ ALA ‐ subgroup by statin use | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 40.1 ALA ‐ ≥ 50% of control group on statins | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.67, 1.30] |
| 40.2 ALA ‐ < 50% of control group on statins | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.58, 1.70] |
| 41 CHD mortality ‐ ALA ‐ subgroup by CAD history | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.72, 1.26] |
| 41.1 Previous CAD | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.66, 1.28] |
| 41.2 No previous CAD | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.61, 1.73] |
| 42 Coronary heart disease events (overall) ‐ ALA | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 43 CHD events ‐ ALA ‐ SA fixed‐effect | 4 | 19061 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.82, 1.21] |
| 44 CHD events ‐ ALA ‐ SA by summary risk of bias | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 44.1 Low risk of bias | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.15] |
| 44.2 Moderate/high risk of bias | 2 | 14114 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.86, 1.67] |
| 45 CHD events ‐ ALA ‐ SA by compliance and study size | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 45.1 SA ‐ low risk of compliance bias | 2 | 5545 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.73, 1.17] |
| 45.2 SA ‐ 100+ randomised | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 46 CHD events ‐ ALA ‐ subgroup by dose | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 46.1 ALA low < 5 g/d | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.72, 1.17] |
| 46.2 ALA high ≥ 5 g/d | 3 | 14224 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.84, 1.61] |
| 47 CHD events ‐ ALA ‐ subgroup by replacement | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 47.1 N‐3 replacing SFA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 47.2 N‐3 replacing MUFA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.72, 1.17] |
| 47.3 N‐3 replacing n‐6 | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.85, 1.65] |
| 47.4 N‐3 replacing carbohydrates/sugars | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 47.5 N‐3 replacing nil/low n‐3 placebo | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 47.6 Replacement unclear | 2 | 818 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.08, 5.81] |
| 48 CHD events ‐ ALA ‐ subgroup by intervention type | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 48.1 Dietary advice | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 48.2 Supplemental foods | 3 | 5655 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.72, 1.16] |
| 48.3 Supplements (capsule) | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.85, 1.65] |
| 48.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 49 CHD events ‐ ALA ‐ subgroup by duration | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 49.1 Medium duration 1 to < 2 years in study | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.34, 2.58] |
| 49.2 Medium‐long duration: 2 to < 4 years in study | 2 | 5545 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.73, 1.17] |
| 49.3 Long duration: ≥ 4 years in study | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 50 CHD events ‐ ALA ‐ subgroup by primary or secondary prevention | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 50.1 Primary prevention | 2 | 14114 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.86, 1.67] |
| 50.2 Secondary prevention | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.15] |
| 51 CHD events ‐ ALA ‐ subgroup by statin use | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 51.1 ALA ‐ ≥ 50% of control group on statins | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.15] |
| 51.2 ALA ‐ < 50% of control group on statins | 2 | 14114 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.86, 1.67] |
| 52 CHD events ‐ ALA ‐ subgroup by CAD history | 4 | 19061 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.82, 1.22] |
| 52.1 Previous CAD | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.72, 1.17] |
| 52.2 No previous CAD | 3 | 14224 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.84, 1.61] |
| 53 Stroke (overall) ‐ ALA | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.66, 2.01] |
| 54 Stroke ‐ ALA ‐ SA fixed‐effect | 5 | 19327 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.71, 2.13] |
| 55 Stroke ‐ ALA ‐ SA by summary risk of bias | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.66, 2.01] |
| 55.1 Low risk of bias | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.45, 2.09] |
| 55.2 Moderate/high risk of bias | 2 | 14114 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.62, 3.13] |
| 56 Stroke ‐ ALA ‐ SA by compliance and study size | 5 | 25138 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.66, 1.64] |
| 56.1 SA ‐ low risk of compliance bias | 3 | 5811 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.39, 1.87] |
| 56.2 SA ‐ 100+ randomised | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.66, 2.01] |
| 57 Stroke ‐ ALA ‐ subgroup by dose | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 57.1 ALA low < 5 g/d | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.39, 2.15] |
| 57.2 ALA high ≥ 5 g/d | 4 | 14490 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.65, 2.85] |
| 58 Stroke ‐ ALA ‐ subgroup by replacement | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 58.1 N‐3 replacing SFA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 58.2 N‐3 replacing MUFA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.39, 2.15] |
| 58.3 N‐3 replacing n‐6 | 2 | 13672 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.53, 3.01] |
| 58.4 N‐3 replacing carbohydrates/sugars | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 58.5 N‐3 replacing nil/low n‐3 placebo | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 58.6 Replacement unclear | 2 | 818 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.31, 10.17] |
| 59 Stroke ‐ ALA ‐ subgroup by intervention type | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.66, 2.01] |
| 59.1 Dietary advice | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 59.2 Supplemental foods | 4 | 5921 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.46, 2.03] |
| 59.3 Supplements (capsule) | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.62, 3.36] |
| 59.4 Any combination | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 60 Stroke ‐ ALA ‐ subgroup by duration | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.66, 2.01] |
| 60.1 Medium duration 1 to < 2 years in study | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.70, 3.44] |
| 60.2 Medium‐long duration: 2 to < 4 years in study | 3 | 5811 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.39, 1.87] |
| 60.3 Long duration: ≥ 4 years in study | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 61 Stroke ‐ ALA ‐ subgroup by primary or secondary prevention | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.66, 2.01] |
| 61.1 Primary prevention | 3 | 14380 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.57, 2.74] |
| 61.2 Secondary prevention | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.47, 2.34] |
| 62 Stroke ‐ ALA ‐ subgroup by statin use | 5 | 19327 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.71, 2.18] |
| 62.1 ALA ‐ ≥ 50% of control group on statins | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.56, 2.77] |
| 62.2 ALA ‐ < 50% of control group on statins | 3 | 14380 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.57, 2.74] |
| 63 Stroke ‐ ALA ‐ subgroup by stroke type | 3 | 13782 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.65, 3.01] |
| 63.1 Ischaemic stroke ‐ ALA | 3 | 13782 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.65, 3.01] |
| 63.2 Haemorrhagic stroke ‐ ALA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 64 Arrythmia (overall) ‐ ALA | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.57, 1.10] |
| 64.1 ALA ‐ new arrhythmias | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.57, 1.10] |
| 64.2 ALA ‐ recurrent arrhythmias | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 65 Arrhythmia ‐ ALA ‐ SA by summary risk of bias | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.57, 1.10] |
| 65.1 Low risk of bias | 1 | 4837 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.57, 1.10] |
| 65.2 Moderate/high risk of bias | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5.
High vs low ALA omega‐3 fat (secondary outcomes)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 MACCEs ‐ ALA | 1 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.32, 3.95] |
| 2 Myocardial infarction (overall) ‐ ALA | 3 | 18353 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.76, 1.32] |
| 3 Total MI ‐ ALA ‐ subgroup by fatality | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Fatal MI | 2 | 4947 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.62, 1.46] |
| 3.2 Non‐fatal MI | 3 | 5213 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.15, 1.77] |
| 4 Angina ‐ ALA | 2 | 13516 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [0.75, 2.64] |
| 5 Revascularisation ‐ ALA | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 CABG ‐ ALA | 1 | 266 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.01, 5.93] |
| 5.2 Angioplasty ‐ ALA | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 Any revascularisation ‐ ALA | 1 | 266 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.07, 7.84] |
| 6 Peripheral arterial disease ‐ ALA | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7 Body weight, kg ‐ ALA | 4 | 664 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐4.17, 1.18] |
| 8 Weight, kg ‐ ALA ‐ sensitivity analysis (SA) fixed‐effect | 4 | 664 | Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.61, 0.96] |
| 9 Weight, kg ‐ ALA ‐ SA by summary risk of bias | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Low risk of bias | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Moderate/high risk of bias | 4 | 664 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐4.17, 1.18] |
| 10 Weight, kg ‐ ALA ‐ SA by compliance and study size | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 SA ‐ low risk of compliance bias | 3 | 629 | Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐4.47, 1.30] |
| 10.2 SA ‐ 100+ randomised | 3 | 629 | Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐4.47, 1.30] |
| 11 Weight, kg ‐ ALA ‐ subgroup by dose | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 ALA low < 5 g/d | 3 | 485 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐3.31, 1.90] |
| 11.2 ALA high > 5 g/d | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐4.20 [‐7.61, ‐0.79] |
| 12 Weight, kg ‐ ALA ‐ subgroup by intervention type | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Supplemental foods | 3 | 526 | Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐5.27, 2.80] |
| 12.3 Supplement (capsule) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.4 Any combination | 1 | 138 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐5.89, 1.92] |
| 13 Weight, kg ‐ ALA ‐ subgroup by replacement | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 ALA replacing SFA | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 ALA replacing MUFA | 1 | 138 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐5.89, 1.92] |
| 13.3 ALA replacing n‐6 | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.4 ALA replacing carbs/sugars | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.5 ALA replacing nil/low n‐3 placebo | 1 | 35 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐10.57, 9.97] |
| 13.6 Replacement unclear | 2 | 491 | Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐6.26, 3.39] |
| 14 Weight, kg ‐ ALA ‐ subgroup by duration | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 Medium duration 1 to < 2 years in study | 4 | 664 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐4.17, 1.18] |
| 14.2 Medium‐long duration: 2 to < 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Long duration ≥ 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Weight, kg ‐ ALA ‐ subgroup by statin use | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 ALA ‐ ≥ 50% of control group on statins | 1 | 35 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐10.57, 9.97] |
| 15.2 ALA ‐ < 50% of control group on statins | 1 | 138 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐5.89, 1.92] |
| 15.3 ALA ‐ use of statins unclear | 2 | 491 | Mean Difference (IV, Random, 95% CI) | ‐1.43 [‐6.26, 3.39] |
| 16 Weight, kg ‐ ALA ‐ subgroup by primary or secondary prevention | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Low CVD risk | 3 | 629 | Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐4.47, 1.30] |
| 16.2 Moderate CVD risk | 1 | 35 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐10.57, 9.97] |
| 16.3 High CVD risk | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Body mass index, kg/m² ‐ ALA | 3 | 1581 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐1.53, 0.69] |
| 18 BMI, kg/m² ‐ ALA ‐ SA fixed‐effect | 3 | 1581 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.06, 0.30] |
| 19 BMI, kg/m² ‐ ALA ‐ SA by summary risk of bias | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 19.1 Low risk of bias | 2 | 1402 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.04, 0.33] |
| 19.2 Moderate/high risk of bias | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐2.86, ‐0.14] |
| 20 BMI, kg/m² ‐ ALA ‐ SA by compliance and study size | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 20.1 SA ‐ low risk of compliance bias | 3 | 1581 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐1.53, 0.69] |
| 20.2 SA ‐ 100+ randomised | 3 | 1581 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐1.53, 0.69] |
| 21 BMI, kg/m² ‐ ALA ‐ subgroup by dose | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 21.1 ALA low < 5 g/d | 1 | 1260 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.03, 0.33] |
| 21.2 ALA high > 5 g/d | 2 | 321 | Mean Difference (IV, Random, 95% CI) | ‐1.12 [‐2.24, 0.01] |
| 22 BMI, kg/m² ‐ ALA ‐ subgroup by intervention type | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 22.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.2 Supplemental foods | 3 | 1581 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐1.53, 0.69] |
| 22.3 Supplement (capsule) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.4 Any combination | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 BMI, kg/m² ‐ ALA ‐ subgroup by replacement | 3 | 1581 | Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐1.53, 0.69] |
| 23.1 ALA replacing SFA | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 ALA replacing MUFA | 1 | 1260 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.03, 0.33] |
| 23.3 ALA replacing n‐6 | 1 | 142 | Mean Difference (IV, Random, 95% CI) | ‐0.3 [‐2.29, 1.69] |
| 23.4 ALA replacing carbs/sugars | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.5 ALA replacing nil/low n‐3 placebo | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.6 Replacement unclear | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐2.86, ‐0.14] |
| 24 BMI, kg/m² ‐ ALA ‐ subgroup by duration | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 24.1 Medium duration 1 to < 2 years in study | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐2.86, ‐0.14] |
| 24.2 Medium‐long duration: 2 to < 4 years in study | 2 | 1402 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.04, 0.33] |
| 24.3 Long duration ≥ 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 BMI, kg/m² ‐ ALA ‐ subgroup by statin use | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 25.1 ALA ‐ ≥ 50% of control group on statins | 1 | 1260 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.03, 0.33] |
| 25.2 ALA ‐ < 50% of control group on statins | 1 | 142 | Mean Difference (IV, Random, 95% CI) | ‐0.3 [‐2.29, 1.69] |
| 25.3 ALA ‐ use of statins unclear | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐2.86, ‐0.14] |
| 26 BMI, kg/m² ‐ ALA ‐ subgroup by primary or secondary preventionA | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 26.1 Primary prevention of CVD | 2 | 321 | Mean Difference (IV, Random, 95% CI) | ‐1.12 [‐2.24, 0.01] |
| 26.2 Secondary prevention of CVD | 1 | 1260 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.03, 0.33] |
| 27 Other measures of adiposity ‐ ALA | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 27.1 Visceral adipose tissue, cm² | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 27.0 [‐21.28, 75.28] |
| 27.2 Subcutaneous adipose tissue, cm² | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 27.3 Waist circumference, cm | 3 | 629 | Mean Difference (IV, Fixed, 95% CI) | ‐1.59 [‐3.10, ‐0.07] |
| 28 Total cholesterol, serum, mmoL/L ‐ ALA | 6 | 2164 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.23, 0.05] |
| 29 TC, mmoL/L ‐ ALA ‐ SA fixed‐effect | 6 | 2164 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.17, ‐0.03] |
| 30 TC, mmoL/L ‐ ALA ‐ SA by summary risk of bias | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 30.1 Low risk of bias | 3 | 1436 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.13, 0.14] |
| 30.2 Moderate/high risk of bias | 3 | 728 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.36, ‐0.01] |
| 31 TC, mmoL/L ‐ ALA ‐ SA by compliance and study size | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 31.1 SA ‐ low risk of compliance bias | 4 | 2045 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.25, 0.05] |
| 31.2 SA ‐ 100+ randomised | 4 | 2045 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.25, 0.05] |
| 32 TC, mmoL/L ‐ ALA ‐ subgroup by dose | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 32.1 ALA low < 5 g/d | 3 | 1759 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.24, 0.09] |
| 32.2 ALA high > 5 g/d | 3 | 405 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.47, 0.21] |
| 33 TC, mmoL/L ‐ ALA ‐ subgroup by intervention type | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 33.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Supplemental foods | 6 | 2164 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.23, 0.05] |
| 33.3 Supplement (capsule) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.4 Any combination | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 TC, mmoL/L ‐ ALA ‐ subgroup by replacement | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 34.1 ALA replacing SFA | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.2 ALA replacing MUFA | 1 | 1210 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.13, 0.09] |
| 34.3 ALA replacing n‐6 | 1 | 142 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.10, 0.38] |
| 34.4 ALA replacing carbs/sugars | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34.5 ALA replacing nil/low n‐3 placebo | 1 | 35 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.30, 0.90] |
| 34.6 Replacement unclear | 3 | 777 | Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.31, ‐0.11] |
| 35 TC, mmoL/L ‐ ALA ‐ subgroup by duration | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 35.1 Medium duration 1 to < 2 years in study | 4 | 812 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.33, ‐0.07] |
| 35.2 Medium‐long duration: 2 to < 4 years in study | 2 | 1352 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.12, 0.16] |
| 35.3 Long duration ≥ 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36 TC, mmoL/L ‐ ALA ‐ subgroup by statin use | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 36.1 ALA ‐ ≥ 50% of control group on statins | 3 | 1329 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.15, 0.11] |
| 36.2 ALA ‐ < 50% of control group on statins | 1 | 142 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.10, 0.38] |
| 36.3 ALA ‐ use of statins unclear | 2 | 693 | Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.30, ‐0.11] |
| 37 TC, mmoL/L ‐ ALA ‐ subgroup by primary or secondary preventionA | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 37.1 Primary prevention of CVD | 4 | 870 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.30, 0.12] |
| 37.2 Secondary prevention of CVD | 2 | 1294 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.14, 0.08] |
| 38 Triglycerides, fasting, serum, mmoL/L ‐ ALA | 6 | 1776 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.11, 0.05] |
| 39 TG, fasting, mmoL/L ‐ ALA ‐ SA fixed‐effect | 6 | 1776 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.11, 0.05] |
| 40 TG, fasting, mmoL/L‐ ALA ‐ SA by summary risk of bias | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 40.1 Low risk of bias | 3 | 1436 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.13, 0.19] |
| 40.2 Moderate/high risk of bias | 3 | 340 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.18, 0.09] |
| 41 TG, fasting, mmoL/L‐ ALA ‐ SA by compliance and study size | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 41.1 SA ‐ low risk of compliance bias | 4 | 1657 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.13, 0.04] |
| 41.2 SA ‐ 100+ randomised | 4 | 1657 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.13, 0.04] |
| 42 TG, fasting, mmoL/L ‐ ALA ‐ subgroup by dose | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 42.1 ALA low < 5 g/d | 3 | 1371 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.16, 0.03] |
| 42.2 ALA high > 5 g/d | 3 | 405 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.09, 0.19] |
| 43 TG, fasting, mmoL/L‐ ALA ‐ subgroup by intervention type | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 43.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 43.2 Supplemental foods | 5 | 1650 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.10, 0.07] |
| 43.3 Supplement (capsule) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 43.4 Any combination | 1 | 126 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.33, 0.09] |
| 44 TG, fasting, mmoL/L‐AL ‐ subgroup by replacementA | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 44.1 ALA replacing SFA | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 44.2 ALA replacing MUFA | 2 | 1336 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.17, 0.02] |
| 44.3 ALA replacing n‐6 | 1 | 142 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.16, 0.42] |
| 44.4 ALA replacing carbs/sugars | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 44.5 ALA replacing nil/low n‐3 placebo | 1 | 35 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.39, 0.99] |
| 44.6 Replacement unclear | 2 | 263 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.15, 0.23] |
| 45 TG, fasting, mmoL/L‐ ALA ‐ subgroup by duration | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 45.1 Medium duration 1 to < 2 years in study | 4 | 424 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.15, 0.12] |
| 45.2 Medium‐long duration: 2 to < 4 years in study | 2 | 1352 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.17, 0.15] |
| 45.3 Long duration ≥ 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 46 TG, fasting, mmoL/L ‐ ALA ‐ subgroup by statin use | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 46.1 ALA ‐ ≥ 50% of control group on statins | 3 | 1329 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.17, 0.23] |
| 46.2 ALA ‐ < 50% of control group on statins | 2 | 268 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.26, 0.23] |
| 46.3 ALA ‐ use of statins unclear | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.20, 0.16] |
| 47 TG, fasting, mmoL/L‐ ALA ‐ subgroup by primary or secondary prevention | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 47.1 Primary prevention | 4 | 482 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.14, 0.11] |
| 47.2 Secondary prevention | 2 | 1294 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.22, 0.25] |
| 48 High‐density lipoprotein, serum, mmoL/L ‐ ALA | 6 | 1776 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.08, 0.03] |
| 49 HDL, mmoL/L ‐ ALA ‐ SA fixed‐effect | 6 | 1776 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.00] |
| 50 HDL, mmoL/L ‐ ALA ‐ SA by summary risk of bias | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 50.1 Low risk of bias | 3 | 1436 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.06, 0.00] |
| 50.2 Moderate/high risk of bias | 3 | 340 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.14, 0.22] |
| 51 HDL, mmoL/L ‐ ALA ‐ SA by compliance and study size | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 51.1 SA ‐ low risk of compliance bias | 4 | 1657 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.08, 0.04] |
| 51.2 SA ‐ 100+ randomised | 4 | 1657 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.08, 0.04] |
| 52 HDL, mmoL/L ‐ ALA ‐ subgroup by dose | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 52.1 ALA low < 5 g/d | 3 | 1371 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.08, 0.19] |
| 52.2 ALA high > 5 g/d | 3 | 405 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.12, ‐0.01] |
| 53 HDL, mmoL/L ‐ ALA ‐ subgroup by intervention type | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 53.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 53.2 Supplemental foods | 5 | 1650 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.06, ‐0.00] |
| 53.3 Supplement (capsule) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 53.4 Any combination | 1 | 126 | Mean Difference (IV, Random, 95% CI) | 0.15 [0.01, 0.29] |
| 54 HDL, mmoL/L ‐ ALA ‐ subgroup by replacement | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 54.1 ALA replacing SFA | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 54.2 ALA replacing MUFA | 2 | 1336 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.11, 0.22] |
| 54.3 ALA replacing n‐6 | 1 | 142 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.11, 0.03] |
| 54.4 ALA replacing carbs/sugars | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 54.5 ALA replacing nil/low n‐3 placebo | 1 | 35 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.17, 0.37] |
| 54.6 Replacement unclear | 2 | 263 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.17, ‐0.02] |
| 55 HDL, mmoL/L ‐ ALA ‐ subgroup by duration | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 55.1 Medium duration 1 to < 2 years in study | 4 | 424 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.13, 0.13] |
| 55.2 Medium‐long duration: 2 to < 4 years in study | 2 | 1352 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.05, 0.00] |
| 55.3 Long duration ≥ 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 56 HDL, mmoL/L ‐ ALA ‐ subgroup by statin use | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 56.1 ALA ‐ ≥ 50% of control group on statins | 3 | 1329 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| 56.2 ALA ‐ < 50% of control group on statins | 2 | 268 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.14, 0.23] |
| 56.3 ALA ‐ use of statins unclear | 1 | 179 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.20, 0.02] |
| 57 HDL, mmoL/L ‐ ALA ‐ subgroup by primary or secondary prevention | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 57.1 Low CVD risk | 2 | 305 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.21, 0.26] |
| 57.2 Moderate CVD risk | 2 | 177 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.10, 0.04] |
| 57.3 High CVD risk | 3 | 1368 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.08, 0.03] |
| 58 Low‐density lipoprotein, serum, mmoL/L ‐ ALA | 7 | 2201 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.15, 0.04] |
| 59 LDL, mmoL/L ‐ ALA ‐ SA fixed‐effect | 7 | 2201 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.11, 0.00] |
| 60 LDL, mmoL/L ‐ ALA ‐ SA by summary risk of bias | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 60.1 Low risk of bias | 3 | 1350 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.05, 0.10] |
| 60.2 Moderate/high risk of bias | 4 | 851 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.22, ‐0.06] |
| 61 LDL, mmoL/L ‐ ALA ‐ SA by compliance and study size | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 61.1 SA ‐ low risk of compliance bias | 5 | 2085 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.16, 0.06] |
| 61.2 SA ‐ 100+ randomised | 5 | 2085 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.16, 0.06] |
| 62 LDL, mmoL/L ‐ ALA ‐ subgroup by dose | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 62.1 ALA low < 5 g/d | 4 | 1796 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.17, 0.05] |
| 62.2 ALA high > 5 g/d | 3 | 405 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.28, 0.19] |
| 63 LDL, mmoL/L ‐ ALA ‐ subgroup by intervention type | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 63.1 Dietary advice | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63.2 Supplemental foods | 6 | 2075 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.17, 0.05] |
| 63.3 Supplement (capsule) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63.4 Any combination | 1 | 126 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.25, 0.25] |
| 64 LDL, mmoL/L ‐ ALA ‐ subgroup by replacement | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 64.1 ALA replacing SFA | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 64.2 ALA replacing MUFA | 2 | 1250 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.07, 0.09] |
| 64.3 ALA replacing n‐6 | 1 | 142 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.08, 0.36] |
| 64.4 ALA replacing carbs/sugars | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 64.5 ALA replacing nil/low n‐3 placebo | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.59, 0.39] |
| 64.6 Replacement unclear | 3 | 777 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.24, ‐0.07] |
| 65 LDL, mmoL/L ‐ ALA ‐ subgroup by duration | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 65.1 Medium duration 1 to < 2 years in study | 5 | 935 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.22, ‐0.06] |
| 65.2 Medium‐long duration: 2 to < 4 years in study | 2 | 1266 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.06, 0.13] |
| 65.3 Long duration ≥ 4 years in study | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 66 LDL, mmoL/L ‐ ALA ‐ subgroup by statin use | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 66.1 ALA ‐ ≥ 50% of control group on statins | 3 | 1240 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.08, 0.08] |
| 66.2 ALA ‐ < 50% of control group on statins | 2 | 268 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.09, 0.24] |
| 66.3 ALA ‐ use of statins unclear | 2 | 693 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.25, ‐0.07] |
| 67 LDL, mmoL/L ‐ ALA ‐ subgroup by primary or secondary prevention | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 67.1 Primary prevention of CVD | 5 | 993 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.20, 0.05] |
| 67.2 Secondary prevention of CVD | 2 | 1208 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.08, 0.09] |
Comparison 6.
High vs low ALA omega‐3 fats (tertiary outcomes)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Blood pressure, mmHg ‐ ALA | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Systolic BP ‐ ALA | 4 | 1671 | Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐4.48, 2.75] |
| 1.2 Diastolic BP ‐ ALA | 4 | 1671 | Mean Difference (IV, Random, 95% CI) | ‐1.42 [‐4.40, 1.57] |
| 2 Serious adverse events ‐ ALA | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Any serious adverse events | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Bleeding | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 GI hospitalisation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.4 Pulmonary embolus or DVT | 1 | 708 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 7.80] |
| 2.5 Thrombophleibitis | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.72, 3.51] |
| 2.6 Urolithiasis | 1 | 13406 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.47, 1.36] |
| 3 Side effects ‐ ALA | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Dropouts due to side effects | 5 | 3480 | Risk Ratio (M‐H, Random, 95% CI) | 2.10 [0.66, 6.71] |
| 3.2 Abdominal pain or discomfort | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 Diarrhoea | 1 | 708 | Risk Ratio (M‐H, Random, 95% CI) | 3.82 [0.82, 17.88] |
| 3.4 Nausea | 1 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 6.29 [0.33, 118.93] |
| 3.5 Any gastrointestinal side effect ‐ ALA | 4 | 3450 | Risk Ratio (M‐H, Random, 95% CI) | 2.06 [0.62, 6.80] |
| 3.6 Pain (joint, lumbar, muscle pain) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.7 All side effects combined | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Dropouts ‐ ALA | 6 | 3663 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.92, 1.25] |
What's new
| Date | Event | Description |
|---|---|---|
| 28 November 2018 | Amended | Feedback has been received and added to the review |
History
Protocol first published: Issue 2, 1999 Review first published: Issue 4, 2004
| Date | Event | Description |
|---|---|---|
| 13 March 2018 | New citation required and conclusions have changed | This update now reports arrhythmia (atrial fibrillation) and cardiovascular mortality data. Data now included from 79 RCTs (112,059 participants) lasting at least one year, of which 25 were at low summary risk of bias. We added the following outcomes to the list of primary outcomes upon the request of World Health Organization (WHO) Nutrition Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health.
We altered inclusion criteria to include only RCTs of at least 12 months' duration (rather than 6 months as previously), and we excluded cohort studies. We are assessing effects of long‐chain omega‐3 fats separately from effects of alpha‐linolenic acid (as planned in the previously published version). |
| 27 April 2017 | New search has been performed | Electronic searches updated to 27 April 2017 |
| 14 March 2012 | Amended | Additional tables re‐numbered |
| 16 October 2011 | New search has been performed | Searches updated to July 2011. Cohort studies not included in this update, and previously included cohort studies and related text have been removed. Previously included trials where we know that no deaths or primary or secondary health events occurred were removed. New secondary outcomes added (fatal and non‐fatal arrhythmias, and diabetes) Cardiovascular mortality added as a primary outcome. |
| 9 September 2008 | Amended | Converted to new review format. |
| 1 August 2004 | New citation required and conclusions have changed | Substantive amendment |
Differences between protocol and review
Differences between the previous version of this review (2004) and this update (2018):
Authors altered. The Acknowledgments recognise authors of the previous version who chose not to participate in this update.
Background updated.
Objectives: primary objective altered from 'Do dietary or supplemental omega‐3 fatty acids alter total mortality, cardiovascular events, cancers or other adverse events?' to 'Do long‐chain omega‐3 (LCn3, fish‐based omega‐3 fats) or ALA (plant‐based omega‐3 fats) fats alter risk of all‐cause mortality, cardiovascular deaths, cardiovascular events, coronary heart disease deaths, coronary heart disease events, stroke, arrhythmia, adiposity and lipids?' This change in emphasis, which we anticipated in the original review, focuses on long‐chain omega‐3 fats (EPA, DHA, DPA) and ALA separately. We discuss changes in outcomes assessed below.
Secondary questions: we added assessment of effects of omega‐3 fats (including both LCn3 and ALA) as a secondary question.
Types of studies included: included RCTs had to be at least one year in duration in the update (the limit was six months in the original review). We excluded cohort studies from the update.
Types of outcomes: primary outcomes assessed were updated, removing cancers and adverse events as primary outcomes and adding cardiovascular deaths, coronary heart disease deaths and events, stroke and arrhythmia (atrial fibrillation) as primary outcomes. Adiposity and lipids were added as key secondary outcomes. Cancer outcomes and other non‐cardiovascular outcomes, including diabetes, were assessed in separate reviews (Abdelhamid 2018; Abdelhamid 2017; Brown 2017; Hanson 2017a; Hanson 2017b; Jimoh 2017; Thorpe 2017).
Secondary outcomes: we added new secondary outcomes (major adverse cardiac or cerebrovascular events (MACCEs), myocardial infarction, sudden cardiac death, angina, heart failure, peripheral arterial disease, re‐vascularisation and acute coronary syndrome). Blood pressure (a secondary outcome in the original review) became a tertiary outcome in the update. We dropped urinary thromboxane and participant fatty acid data as secondary outcomes but collected fatty acid data to help assess compliance.
Risk of bias: we updated this review to incorporate the Cochrane 'Risk of bias' tool (for all included studies). We slightly updated our assessment of summary risk of bias from low summary risk when "allocation concealment was adequate, and participant, provider and outcome assessor blinding were all coded 'yes'" to low summary risk for a supplement or capsule type trial where "we judged randomisation, allocation concealment, blinding of participants and personnel, and blinding of outcome assessors to be adequate" and for a dietary advice or all‐food provided type trial where "we judged randomisation, allocation concealment, and blinding of outcome assessors to be adequate".
-
Subgroup analyses: in the update we carried out separate subgroup analyses for LCn3 and ALA studies. Subgrouping in the update was as in the original review (by dose, dietary or supplemental source and trial duration), with the addition of some new subgroups. We added new subgroup analyses at the request of the WHO NUGAG Subgroup on Diet and Health.
Replacement of SFA, MUFA, omega‐6 fats, fat mixture, carbohydrates or sugars, non‐fat or no placebo (or unclear) by LCn3 or ALA.
Primary prevention versus secondary prevention of CVD.
Statin use (< 50% of control group on statins, ≥ 50% of control group on statins, use of statins unclear).
Baseline LCn3 or ALA intake.
Sensitivity analyses: updated for this review. Limiting analyses to studies at low summary risk of bias was continued in the update from the original review, and we added sensitivity analyses by study size (retaining only trials that randomised at least 100 participants across all study arms), fixed‐effect meta‐analysis and compliance (retaining only studies at low risk of compliance bias, this latter at the request of WHO NUGAG Subgroup on Diet and Health).
Heterogeneity: the original review used Cochran's test while the update used I2. This reflects current best methodology.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Alzheimer's Disease Cooperative Study (ADCS) RCT, parallel, (n‐3 DHA vs n‐6 LA), 18 months Summary risk of bias: low |
|
| Participants | Individuals with mild to moderate Alzheimer's disease N: 238 intervention, 164 control Level of risk for CVD: low Men: 52.9% intervention, 40.2% control Mean age in years (SD): 76 (9.3) intervention, 76 (7.8) control Age range: unclear Smokers: 24.4% intervention, 21.9% control Hypertension: not reported Medications taken by at least 50% of those in the control group: cholinesterase inhibitor, memantine Medications taken by 20%‐49% of those in the control group: none Medications taken by some, but less than 20% of the control group: none Location: USA Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: DHA vs omega 6 Intervention: 2 × 1 g algal‐derived DHA capsules (Neuromins) per day for a total daily dose of 2 g, each capsule contain 45% to 55% of DHA and does not contain EPA (950 mg soft‐gel capsules which contain approximately 510 mg DHA). Dose: +DHA 1.02 g/d. Control: 2 × 1 g placebo capsules per day (made up of corn or soy oil) Compliance: measured by pill counts at every visit Length of intervention: 18 months |
|
| Outcomes | Main study outcome: change in the cognitive subscale of the Alzheimer's Disease Assessment Scale (ADAS‐cog) and change in the Clinical Dementia Rating (CDR) Dropouts: 67 intervention, 40 control (discontinued treatment but included in main analyses) Available outcomes: mortality, measures of cognition, baseline & change in plasma DHA, adverse events Response to contact: no data provided |
|
| Notes | Study funding; quote: "grant UO1‐AG10483 from the National Institute on Aging. The National Institute on Aging was not otherwise involved in the design and conduct of the study, or in the analysis of data or preparation of the manuscript". "The placebo and DHA study drugs were provided by Martek Biosciences. Martek also provided plasma and cerebrospinal fluid measurements of fatty acids, as well as partial financial support for the magnetic resonance imaging sub study. (Martek Biosciences produces nutritional supplements from cultivated fungi and microalgae). Martek employees participated in design of the study and in revision of the manuscript, but were not involved in data management or data analysis." (Quinn 2010, p. 1910). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was achieved with a centralised interactive voice response system, using a block design with a block size of 5 (3 in the DHA group and 2 in the placebo group. |
| Allocation concealment (selection bias) | Low risk | Randomisation was achieved with a centralised interactive voice response system, using a block design with a block size of 5 (3 in the DHA group and 2 in the placebo group. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo capsules (made up of corn or soy oil) were identical in appearance. The adequacy of blinding was assessed by questionnaires completed by caregivers, study coordinators, and site physicians. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The adequacy of blinding was assessed by questionnaires completed by caregivers, study coordinators, and site physicians with results showing no difference between groups and the majority did not know. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis. At 12 months data were available for > 80% (ITT analysis) |
| Selective reporting (reporting bias) | Low risk | Prospectively registered February 2007, study started February 2007, completed May 2009. Primary outcomes were rate of change in ADAS‐Cog11 and CDR‐SOB, which are both reported in main report. NPI and ADL were secondary outcomes also reported. |
| Attention | Low risk | Both study arms had the same follow‐up and care. |
| Compliance | Unclear risk | Measured by pill count at every visit. 28% intervention and 24% control discontinued supplement with a minority discontinuing due to adverse events. A further 8% were excluded for < 80% compliance in both intervention and control arms. |
| Other bias | Low risk | None noted |
| Methods | Multi‐center study to evaluate the effect of n‐3 fatty acids on arrhythmia recurrence in atrial fibrillation (AFFORD) RCT, parallel, (n‐3 EPA + DHA vs n‐6), 12 months Summary risk of bias: moderate or high |
|
| Participants | People with symptomatic paroxysmal or persistent AF N: 165 intervention, 172 control. (analysed, intervention: 153 control: 163) Level of risk for CVD: high Men: 69% intervention, 65% control Mean age in years (SD): 60 (12) intervention, 62 (13) control Age range: not reported Smokers: not reported Hypertension: 45% intervention, 42% control Medications taken by at least 50% of those in the control group: oral anticoagulant Medications taken by 20%‐49%: beta‐blockers, angiotensin‐converting enzyme inhibitors, angiotensin receptor blockers Medications taken by some, but < 20%: none Location: Canada Ethnicity: not reported |
|
| Interventions | Type: supplement (fish oil) Comparison: EPA + DHA vs omega 6 safflower oil Intervention: 4 × 1 g enteric‐coated fish oil capsules/d (1.6 g/d EPA + 0.8 g/d DHA, Genuine Health, Toronto, Ontario, Canada). Dose: +2.4 g/d EPA + DHA, Control: 4 ×1 g matching placebo capsules, 4 g/d safflower oil Compliance: omega‐3 index increased in intervention group, but not control, over the study Duration of intervention: 6 to 16 months |
|
| Outcomes | Main study outcome: AF recurrence Dropouts: 21 intervention, 19 control Available outcomes: all‐cause mortality, stroke, AF recurrence,TIA, CV events, CRP (not usable) Response to contact: no |
|
| Notes | Authors contacted about QoL, resource use and dietary habits Study funding: Canadian Institutes for Health Research and the Heart and Stroke Foundation of Quebec |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "[R]andomised" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Described as double‐blind, but blinding not described or tested |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | An independent events committee adjudicated AF recurrences, bleeding, strokes, transient ischemic attacks, and deaths, but unclear if blinded to allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participant flow well described. ITT analysis |
| Selective reporting (reporting bias) | High risk | NCT01235130 registered July 2010, recruitment March 2009‐March 2012, follow‐up finished December 2012. Results published 2014, but no data on quality of life, resource utilisation, or dietary habits (stated in registry) found |
| Attention | Low risk | No problem with attention bias |
| Compliance | Low risk | Omega‐3 index measured |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (EPA + DHA + statins vs statins), 12 months Summary risk of bias: moderate to high |
|
| Participants | Statin treated CAD patients undergoing PCI N: 38 intervention, 36 control Level of risk for CVD: high Men: 63.2% intervention, 72.2% control Mean age in years (SD): 59.6 (9.1) intervention, 60.7 (0.8) [sic] control Age range: unclear Smokers: 36.8% intervention, 58.3% control Hypertension: 50% in both groups Medications taken by at least 50% of those in the control group: aspirin, clopidogrel, ACE inhibitors/ARB, beta‐blockers, atorvastatin Medications taken by 20%‐49% of those in the control group: cilostazol Medications taken by some, but less than 20% of the control group: rosuvastatin, nitrates, calcium antagonists Location: South Korea Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs unclear (nil) Intervention: 3 g of ω‐3 PUFA containing 1395 mg of EPA and 1125 mg of DHA per day. No further details. Dose: +2.52 g/d EPA + DHA Control: unclear whether control group were given placebo or only statins Compliance: unclear how it was measured but reported good compliance with no numbers Length of intervention: 12 months |
|
| Outcomes | Main study outcome: change in atherosclerotic burden Dropouts: none Available outcomes: lipids (TG reported as median, IQR so not used), atheroma volume, neointimal volume index Response to contact: no |
|
| Notes | Study funding: the study was supported by clinical research grant from Pusan National University Hospital | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation was carried out using random number tables to assign each participant to the intervention or control group |
| Allocation concealment (selection bias) | Low risk | Participants were assigned randomisation numbers sequentially on recruitment to the study, and the randomisation codes were retained by the clinical research coordinator. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No details |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The personnel responsible for randomisation as well as those performing laboratory measurements were blinded to the randomisation assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial register entry found |
| Attention | Unclear risk | No details |
| Compliance | Unclear risk | No details on how it was measured and no fatty acid levels reported |
| Other bias | High risk | It's unclear whether the study was placebo controlled or the control group had no intervention. Also, some of the SDs appear to be incorrectly reported. |
| Methods | RCT, (n‐3 ALA vs MUFA), 40 months Summary risk of bias: low |
|
| Participants | 60‐80 year‐olds with previous MI N: 1197 ALA intervention, 1236 control (1212 ALA + EPA/DHA intervention group) Level of risk for CVD: high Men: 77.9% intervention, 78.7% control Mean age in years (SD): 69.0 (5.6) intervention, 68.9 (5.6) control Age range: 60‐80 years Smokers: 17.4% intervention, 18% control Hypertension: unclear Medications taken by at least 50% of those in the control group: lipid lowering medication, antihypertensives, antithrombotics Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: antiarrythmic drugs, antidiabetic drugs Location: the Netherlands Ethnicty: not reported |
|
| Interventions | Type: supplementary margarine Comparsion: ALA vs MUFA Intervention 20 g of enriched margarine per day incorporating: 2 g ALA. 8 × 250 g margarine tubs delivered every 12 weeks. Dose: average achieved +1.9 g/d ALA Control: 20 g of margarine per day. No additional n‐3 PUFAs. Identical margarine (oleic acid) placebo. Compliance: unused margarine tubs were returned‐ daily intakes of margarine and n‐3 fatty acids were calculated on the basis of the amount unused. Adherence was measured by levels of fatty acids in plasma cholesteryl esters, margarine and questionnaires. 90.5% of patients adhered to the protocol and consumed 20.6 (SD 2.8) g of margarine/d. Length of intervention: 40 months |
|
| Outcomes | Main study outcome: cardiovascular disease events Dropouts: 91 died, 98 discontinued intervention, 93 died, 93 discontinued control Available outcomes: deaths, MI, cardiovascular events, ventricular arrhythmia, Incident cardiovascular disease Response to contact: yes (data provided) |
|
| Notes | The study has 3 intervention arms (ALA margarine, EPA/DHA margarine, mixture of the two interventions). This table represents the ALA only intervention. Outcome data is used for the ALA group where reported separately or for the combined (ALA arm, ALA + EPA/DHA arm) Study funding: Netherlands Heart Foundation, National Institutes of Health and Unilever R&D (latter provided unrestricted grant for distribution of trial margarines) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | On the computer by a random number generator before the start of the trial |
| Allocation concealment (selection bias) | Low risk | Author confirmed allocation was concealed from clinicians/ researchers |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The 4 types of margarine were "similar in taste, texture and colour". A trained test panel did not perceive a fishy taste or odour. Randomisation tables were stored safely under supervision. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Randomisation tables were stored safely under supervision. There was an independent statistician for data analysis. Quote: "Events were coded by three members of the end‐point adjudication committee who were unaware of the identity of the patient, the identity of the treating physician and the patients assigned study group". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients were followed up for events computerised linkage with municipal registries. 2531 patients were only followed up for baseline anthropometric and medical measurements. |
| Selective reporting (reporting bias) | High risk | Sudden cardiac death endpoint omitted. Registered in August 2005, recruitment was from 2002 to 2006. Outcomes papers published in 2010 |
| Attention | Low risk | All participants appear to have had similar frequency and quantity of attention and follow‐up |
| Compliance | Low risk | Unused margarine tubs were returned; daily intakes of margarine and n‐3 fatty acids were calculated on the basis of the amount unused. Adherence was measured by levels of fatty acids in plasma cholesteryl esters, margarine and questionnaires. 90.5% of patients adhered to the protocol and consumed 20.6 (SD 2.8) g of margarine/d |
| Other bias | Low risk | None noted |
| Methods | RCT, (EPA + DHA vs MUFA), 40 months Summary risk of bias: low |
|
| Participants | 60‐80 year‐olds with previous MI N: 1192 EPA/DHA intervention, 1236 control (1212 ALA + EPA/DHA intervention group) Level of risk for CVD: high Men: 78.1% intervention, 78.7% control Mean age in years (SD): 69.1 (5.6) intervention, 68.9 (5.6) control Age range: 60‐80 years Smokers: 16.8%, intervention, 18% control Hypertension: unclear Medications taken by at least 50% of those in the control group: lipid‐lowering medication, antihypertensives, antithrombotics Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: antiarrythmic drugs, antidiabetic drugs Location: the Netherlands Ethnicty: not reported |
|
| Interventions | Type: supplementary margarine Comparison 1: EPA + DHA vs MUFA Intervention: 20 g of enriched margarine per day incorporating 400 mg EPA‐DHA (240 mg EPA and 160 mg DHA). Dose: average achieved 376 mg/d EPA + DHA Control: 20 g of margarine per day. No additional n‐3 PUFAs. Identical margarine (oleic acid) placebo Compliance: unused margarine tubs were returned; daily intakes of margarine and n‐3 fatty acids were calculated on the basis of the amount unused. Adherence was measured by levels of fatty acids in plasma cholesteryl esters, margarine and questionnaires. 90.5% of patients adhered to the protocol. Length of intervention: 40 months |
|
| Outcomes | Main study outcome: cardiovascular disease events Dropouts: 95 died, 119 discontinued intervention, 93 died, 93 discontinued control Available outcomes: deaths, MI, cardiovascular events, ventricular arrhythmia, incident cardiovascular disease Response to contact: yes (data provided) | |
| Notes | The study has three intervention arms (ALA margarine, EPA/DHA margarine, mixture of the two interventions). This table represents theEPA/DHA only intervention. Outcome data is used for the EPA/DHA group where available or for the combined (EPA/DHA arm, EPA/DHA + ALA arm) Study funding: Netherlands Heart Foundation, National Institutes of Health and Unilever R&D (latter provided unrestricted grant for distribution of trial margarines) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | On the computer by a random number generator before the start of the trial |
| Allocation concealment (selection bias) | Low risk | Author confirmed allocation was concealed from clinicians/ researchers |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The 4 types of margarine were "similar in taste, texture and colour". A trained test panel did not perceive a fishy taste or odour. Randomisation tables were stored safely under supervision. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Randomisation tables were stored safely under supervision. There was an independent statistician for data analysis. Quote: "Events were coded by three members of the end‐point adjudication committee who were unaware of the identity of the patient, the identity of the treating physician and the patients assigned study group". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients were followed up for events computerised linkage with municipal registries. 2531 patients were only followed up for baseline anthropometric and medical measurements. |
| Selective reporting (reporting bias) | High risk | Sudden cardiac death endpoint omitted. Registered from August 2005, recruitment was from 2002 to 2006. Outcomes papers published in 2010 |
| Attention | Low risk | All participants appear to have had similar frequency and quantity of attention and follow‐up |
| Compliance | Low risk | Unused margarine tubs were returned; daily intakes of margarine and n‐3 fatty acids were calculated on the basis of the amount unused. Adherence was measured by levels of fatty acids in plasma cholesteryl esters, margarine and questionnaires. 90.5% of patients adhered to the protocol and consumed 20.6 (SD 2.8) g of margarine/d |
| Other bias | Low risk | None noted |
| Methods | Age‐Related Eye Disease Study 2 (AREDS2) RCT, parallel, 2 × 2 factorial (n‐3 EPA + DHA vs nil) also randomised to lutein and zeaxanthin vs nil), 5 years Summary risk of bias: low |
|
| Participants | People aged 50‐85 years at high risk of progression to advanced age‐related macular degeneration (AMD) N: 2147 intervention (1068 DHA/EPA, 1079 DHA/EPA + lutein/zeaxanthin), 2056 control (1012 placebo, 1044 lutein/zeaxanthin) Level of risk for CVD: low (however ˜20% had previous CV event) Men: intervention 42.1%, control 44.4% Age in years: intervention median 74.6 (IQR 11.1), control median 74 (IQR 11.1) Age range: 68‐79 years Smokers: intervention 6.3%, control 7.2% Hypertension: unclear Medications taken by at least 50% of those in the control group: multivitamins Medications taken by 20%‐49% of those in the control group: cholesterol lowering drugs, aspirin Medications taken by some, but less than 20% of the control group: NSAID, paracetamol Location: USA Ethnicty: white 96.5% intervention, 96.6% control; Hispanic: 2.6 intervention, 1.3 control |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs nil Intervention 350 mg/d DHA plus 650 mg/d EPA added to the standard AREDS supplement of Vitamin C (500 mg/d), Vitamin E (440 IU/d), beta‐carotene (15 mg/d), zinc oxide (80 mg/d) and cupric oxide (2 mg/d). Dose: +1 g/d EPA + DHA Control: standard AREDS supplement of Vitamin C (500 mg/d), Vitamin E (400IU/d), beta‐carotene (15 mg/d), zinc oxide (80 mg/d) and cupric oxide (2 mg/d). Compliance: assessed by pill count – 84% of participants in each group took at least 75% of study medications Length of intervention: 60 months |
|
| Outcomes | Main study outcome: development of advanced AMD Dropouts: intervention 200 died, 165 discontinued, 80 were lost to follow‐up; control 168 died, 140 discontinued, 61 were lost to follow‐up Available outcomes: deaths, cardiovascular death, MI, stroke, angina, heart failure, revascularisation, cognition, eye health, (authors provided data on diabetes diagnosis, depression diagnosis, breast cancer) Response to contact: yes (data provided) |
|
| Notes | Study funding: National Eye Institute/National Institutes of Health, Department of Health and Human Services | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random block design was implemented using the AREDS2 Advantage Electronic Data Capture system by the AREDS2 Coordinating Center" |
| Allocation concealment (selection bias) | Low risk | Each treatment was assigned 5 bottle numbers. Bottle numbers were issued via an electronic randomisation system for each participant once study eligibility was verified. The assigned bottle number was used to distribute the study treatment(s). AREDS2 Coordinating centre personnel involved in creating the randomisation system had access to the bottle number/treatment assignments. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Participants, investigators, study coordinators, and all other study personnel are masked to treatment assignment". However, no information was given regarding the taste, smell, or appearance of the active or placebo capsules. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The coordinating centre randomly assigned the event to a study adjudicator, who made the final determination of these study endpoints through review of the medical records and applying the endpoint criterion defined a priori. All adjudicators were masked to study assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | < 20% attrition over 5 years, balanced reasons for dropouts |
| Selective reporting (reporting bias) | Low risk | Outcomes in trials registry entry appear to all be reported (NCT00345176). Entry received June 2006, recruitment September 2006 – October 2012 |
| Attention | Low risk | Participants, investigators, study coordinators, and all other study personnel are masked to treatment assignment, so attention bias not feasible |
| Compliance | Unclear risk | Assessed by pill count – 84% of participants in each group took at least 75% of study medications |
| Other bias | Low risk | None noted |
| Methods | RCT, (n‐3 EPA + DHA vs MUFA), 24 months Summary risk of bias: moderate or high |
|
| Participants | 45‐70 year olds with combined hyperlipoproteinaemia N: 32 intervention, 32 control Level of risk for CVD: moderate Men: 29% intervention, 29% control Mean age in years (SD): 53.7 (7.2) intervention, 53.7 (6.9) control Age range: 45‐70 years (inclusion) Smokers: 28.1% intervention, 28.1% control Hypertension: none (exclusion criteria) Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported (patients on HRT, anti‐hypertensive drugs, lipid lowering drugs, or who smoked > 10 cigarettes were excluded) Location: Italy Ethnicty: not reported |
|
| Interventions | Type: capsules Comparsion: LCn3 vs MUFA Intervention: 1 g × 6 soft gelatin capsules/d of fatty acid mixture (19% EPA), 13% DHA, 19% palmitic acid, 18% oleic acid, 2% LA and 29% other minor components) providing 1.08 g/d EPA, 0.72 g/d DHA, 0.01 g/d tocopherol acetate, divided to three doses. Dose: 1.8 g/d EPA + DHA Control: 1 g × 6 opaque identical soft gelatin capsules/d of olive oil divided in 3 doses. Compliance: assessed by counting returned capsules at each visit and by measuring EPA and DHA levels at month 24 Length of intervention: 24 months |
|
| Outcomes | Main study outcome: carotid atherosclerosis measures Dropouts: 2 intervention, 5 control Available outcomes: deaths (nil), MI (lipids, weight, BP and heart rate reported but not in a usable format; lipid data were presented at various times without clear numerical data, suggesting falls in TGs in the intervention but not control arms, and rises in LDL and HDL cholesterol in intervention but not control arms. For the other outcomes the text states "a rise in body weight (+ 3%, P < 0.01) was observed at the end of the study in both groups. Blood pressure and heart rate were unchanged". Effects on IMT and platelets also reported but not used) Response to contact: not yet attempted |
|
| Notes | Study funding: supported by Institut De Recherche Pierre Fabre, Departement Recherche Clinique | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An appropriate software was used to obtain 2 groups balanced for sex, age and smoking |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double‐blind and placebo capsules were opaque and identical looking to intervention. However no information provided on capsules taste or smell |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All dropouts are accounted for. "One patient left the study after 3 months because he moved to another city and was therefore excluded from statistical analyses. Two patients were excluded because of major deviation from the protocol during the follow‐up (anti‐hypertensive assumption) and four because of non‐compliance on the basis of returning capsules (compliance < 70%). The final analysed group included 57 patients (30 on active treatment)." |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial register record |
| Attention | Low risk | Both groups had the same contact and number of visits. |
| Compliance | Low risk | Pill count, we know they excluded 4/64 who returned > 70% of capsules. So 60/64 had > 70% compliance with significant increase in serum EPA and DHA in the intervention group. |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (n‐3 EPA + DHA vs MUFA), 24 months Summary risk of bias: moderate or high |
|
| Participants | People with multiple sclerosis N: 155 intervention, 157 control. (analysed, intervention: 145 control: 147) Level of risk for CVD: low Men: 34.2% intervention, 30.6% control Mean age in years (SD): 34.0 (6.6) intervention, 33.7 (6.3) control Age range: not reported but 16‐45 years inclusion criteria Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49%: not reported Medications taken by some, but < 20%: not reported Location: UK Ethnicity: not reported |
|
| Interventions | Type: supplement (fish oil capsule) Comparison: EPA + DHA vs MUFA Intervention: 20 × 0.5 g/d capsules MaxEPA fish body oil (10 g/d fish oil providing 1.71 g/d EPA +1.14 g/d DHA +10 IU/d vitamin E), plus all advised to reduce animal fat and ensure plentiful omega‐6 fats. Dose: +2.85 g/d EPA + DHA Control: 20 × 0.5 g/d capsules olive oil (10 g/d olive oil), plus all advised to reduce animal fat and ensure plentiful omega‐6 fats. All capsules contained 0.5 IU vit E and 100 ppm dodecyl gallate to minimise peroxide formation Compliance: serum EPA and DHA rose in intervention group but fell in controls Duration of intervention: 24 months (5 years mentioned but outcomes not reported) |
|
| Outcomes | Main study outcome: multiple sclerosis progress Dropouts: 10 intervention, 10 control Available outcomes: all‐cause mortality, progress of MS, rate of MS relapse Response to contact: yes (no data provided) |
|
| Notes | Study funding: Multiple Sclerosis Society of Great Britain and Northern Ireland, but Marfleet Refining provided fish oil and placebo capsules | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomised" |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Paper states research was "double blind" and control capsules "had the same appearance and flavour as the fish oil capsules and were packed and dispensed in identical fashion" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low risk at reported time points |
| Selective reporting (reporting bias) | High risk | No protocol or trials registration entries found. Study was intended to run for 5 years, but outcomes only appear to be reported for the first 2 years. |
| Attention | Low risk | Unlikely as each had capsules |
| Compliance | Low risk | Serum EPA and DHA rose in intervention group but fell in controls |
| Other bias | Low risk | Not noted |
| Methods | RCT, parallel, (n‐3 DHA vs n‐6 LA), 48 months Summary risk of bias: low |
|
| Participants | People with retinitis pigmentosa aged 18‐55 years N: 221 randomised overall, analysed 105 intervention, 103 control Level of risk for CVD: low Men: 48% intervention, 54% control Mean age in years (SD): 37.8 (6.5) intervention, 36.0 (7.2) control Age range: unclear (18‐55 inclusion criterion) Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: vitamin A Medications taken by 20%‐49% of those in the control group: multivitamins Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: unclear (6% of the study population were minorities) |
|
| Interventions | Type: supplement (DHA capsules) Comparison: DHA vs omega 6 Intervention: 6 × 500 mg capsules/d of DHA (1.2 g/d DHA plus 1.8 g vegetable oil) plus < 0.0006 mg/d tocopherols plus 15,000 IU retinyl palmitate (vitamin A). Dose: +1.2 g/d DHA Control: 6 × 500 mg capsules/d of soy and corn oils (half each) with 120 mg/d ALA, plus < 0.0006 mg/d tocopherols plus 15000 IU retinyl palmitate (vitamin A) Compliance: 92% of capsules taken by both intervention and control groups (assessed by monthly calendars), Plasma DHA much higher in intervention than control Length of intervention: 48 months |
|
| Outcomes | Main study outcome: retinal degeneration Dropouts: 5 or 6 intervention, 7 or 8 control Available outcomes: mortality, cancer diagnoses, lipids, eyesight Response to contact: yes (no data provided) |
|
| Notes | Study funding: National Eye Institute and Foundation Fighting Blindness | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Random numbers available only to programmer who provided assignments to data manager, all staff in contact with patients were masked to group assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | States that all staff in contact with participants were masked to group assignment, as were participants. However no information was provided regarding the taste, smell and appearance of the active and placebo capsules |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All assessments were performed blind to study allocation. Each ocular examination was performed without review of previous records. All serum samples were analysed without knowledge of treatment group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers of dropouts and reasons for dropouts not stated. 221 participants randomised, data presented on 208 participants |
| Selective reporting (reporting bias) | Unclear risk | No trials registry entry or protocol found. |
| Attention | Low risk | Staff in contact with patients were masked, so unable to bias time, etc. |
| Compliance | Low risk | 92% of capsules taken by both intervention and control groups (assessed by monthly calendars), Plasma DHA much higher in intervention than control |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, 3 arms (n‐3 EPA + DHA from cod liver vs n‐3 EPA + DHA from seal oil vs nil), 14 months Summary risk of bias: moderate or high | |
| Participants | Subjects with moderate hypercholesterolaemia N: 40 seal oil (SO), 40 cod liver oil (CLO), 40 control (numbers analysed vary by outcome) Level of risk for CVD: moderate (dyslipidaemia) Men: 53% seal oil, 50% cod liver oil, 48% control Mean age in years: 53.2 seal oil, 55.0 cod liver oil, 55.8 control Age range: 43‐66 years Smokers: unclear Hypertension: unclear Medications taken by at least 50% of those in the control group: none allowed Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Norway Ethnicity: not reported |
|
| Interventions | Type: supplement (oil) Comparison: EPA + DHA vs nil Intervention: Intervention: seal oil – 15 mL/d (2.6 g, 1.1 g/d EPA + 1.5/d DHA) (total n‐3 3.9 g/d, total PUFA 4.2 g/d): SO dose: EPA + DHA 2.6 g/d Cod liver oil – 15 mL/d (3.3 g, 1.5 g /d EPA + 1.8 g/d DHA) (total n‐3 4.1 g/d, total PUFA 4.35 g/d): CLO dose: EPA + DHA 3.3 g/d Control: nil, no supplement Compliance: serum omega‐3 fatty acids, rose from around 1 mmoL/L to 2.4 (seal oil), 2.1 (cod liver oil) and 1.2 mmoL/L (control) Length of intervention: 14 months |
|
| Outcomes | Main study outcome: serum lipids Dropouts: 8 seal oil, 2 cod liver oil, 1 control Available outcomes: total and cardiovascular deaths, MI, combined CV events, lipids, adverse events Response to contact: yes (author provided methodological details) |
|
| Notes | Data of two intervention groups combined for dichotomous outcomes and CLO vs control data used for continuous outcomes Study funding: the study was supported by the programme Medical Research in Finnmark County, University of Tromsø |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | J Brox stated (personal communication, January 2017): "The randomization of the 120 participants was done by first generating 3 groups (seal oil, cod liver oil, control), then giving each participant a number (1‐120), "'putting all the numbers into the same hat' and blindly drawing one number at the time from the hat. The first 40 numbers (1‐40) were allocated to the seal oil group, the next 40 numbers (41‐80) to the cod liver oil group and the rest (81‐120) were allocated to the control group." |
| Allocation concealment (selection bias) | Low risk | J Brox stated (personal communication, January 2017): "The researcher/clinician who invited the participants had no knowledge of to which group the participants would be allocated." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "controls were aware – not given a supplement" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | J Brox stated (personal communication, 2003): "All the persons involved in the drawing & analysing of blood were unaware of treatment. The technicians analysing the blood did not have any personal contact with the participants except K. Olaussen who did the FA analysis … she only had access to the sample numbers not names and code. The participants did not know their number (says elsewhere that K Olaussen did not know allocations). The only outcome assessor was J Brox who did not have personal contact with participants, randomising, collecting results or analysing process." "The only assessor was J Brox who did not have any personal contact with the participants, had nothing to do with the randomising or analysing process, or the collecting of results." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Control group 3 dropouts, seal oil group 10 dropouts, cod liver oil 3 dropouts. So substantial differences in rates of dropouts between the groups |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trials register entry was found |
| Attention | Low risk | No suggestion of differential attention |
| Compliance | Low risk | Serum omega‐3 fatty acids, rose from around 1 mmoL/L to 2.4 (seal oil), 2.1 (cod liver oil) and 1.2 mmoL/L (control) |
| Other bias | Low risk | No further bias noted |
| Methods | RCT, parallel, (n‐3 EPA + DHA vs n‐6 LA), 12 months Summary risk of bias: low |
|
| Participants | Participants with non‐cirrhotic NASH (non‐alcoholic steatohepatitis) N: 20 intervention, 21 control (analysed 17 intervention, 17 control) Level of risk for CVD: moderate Men: 35.3% intervention, 41.2% control Mean age in years (SD): 46.4 (12.1) intervention, 47.2 (12) control Age range: 25‐72 years Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: intervention, 100% white, control 94.% white, 5.9% other |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs omega 6 Intervention: 3 × 1 g fish oil capsules/d (Nordic Natural) for a total 2.1 g/d n‐3, each capsule contained 70% of n‐3 (1050 mg EPA, 750 mg DHA + 300 mg other n‐3). Dose: 1.8 g/d EPA + DHA Control: 3 × 1 g identical placebo (soybean) capsules per day containing 8% fish oils Both groups had dietary counselling on caloric intake and physical activity Compliance: unclear (measured n‐6‐n‐3 ratio due to its link to hepatic lipid composition) Length of intervention: 12 months |
|
| Outcomes | Main study outcome: NASH activity score Dropouts: 3 intervention, 3 control Available outcomes: lipids (TG too unbalanced at baseline to use), measures of adiposity (weight, BMI, visceral fat – all unbalanced at baseline so not used), fasting glucose, insulin, HOMA‐IR, QUICKI (also NASH progression, hepatic fat, ALT, VO2 max, activity level, markers of cell injury, adiponectin not used) Response to contact: yes, change data supplied for BMI and body weight, confirmed no deaths, cardiovascular events, diabetes, depression, breast cancer or IBD diagnoses |
|
| Notes | Data on; BMI, weight, visceral fat, TG and glucose were not used as they were different between groups at baseline. Study funding: study was supported by NIH NCCAM Grant 5R21AT2901–2 and 5 M01 RR00847. Study medication and identical appearing placebo was provided at no charge by Nordic Natural. RBC phospholipid profile was performed by Metametrix (www.metametrix.com). M30, M65, adiponectin, and IGFBP‐1 electro chemiluminescence assays were performed by Wellstat Diagnostics (www.wellstatdiagnostics.com). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to n‐3 or placebo using a stratified block 1:1 randomisation scheme. An independent biostatistician generated the randomisation list which was confidentially forwarded to the Investigational pharmacy |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All staff and subjects were blinded to therapy assignment throughout the study period. Both capsules were identical. However no information provided on capsules taste or smell |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded for main outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 15% dropouts explained and equal in both groups |
| Selective reporting (reporting bias) | Low risk | The trial was prospectively registered |
| Attention | Low risk | Both groups had the same attention |
| Compliance | Unclear risk | No details on compliance measurement |
| Other bias | Low risk | None noted |
| Methods | Diet And Reinfarction Trial (DART) – oily fish advice (or capsule) arm RCT – parallel, 2 × 2 × 2 factorial (n‐3 EPA + DHA vs nil or fat advice vs not, oily fish advice (or capsule) vs not, dietary fibre advice vs not)), 2 years Summary risk of bias: moderate or high |
|
| Participants | Men recovering from myocardial infarction N: 1015 intervention, 1018 Level of risk for CVD: high (post‐MI) Men: 100% Mean age, SD: 56.7 intervention, 56.4 control (SDs not stated) Age range: unclear Smokers: 61.7% intervention, 62.2% control Hypertension: 22.7% intervention, 24.6% control Medications taken by at least 50% of those in the control group: none reported Medications taken by 20%‐49%: beta‐blockers, other antihypertensives, antianginals Medications taken by some, but < 20%: anticoagulant, aspirin/antiplatelet, digoxin/antiarrhythmic Location: UK Ethnicity: not stated |
|
| Interventions | Type: dietary advice (to eat more oily fish) Comparison: EPA + DHA vs SFA + MUFA (by dietary achievement below) Intervention: advised to eat at least 2 weekly portions of 200‐400 g fatty fish (mackerel, herring, kipper, pilchard, sardine, salmon, trout). If this was not possible, given MaxEPA capsules, 3/d (0.5 g EPA/d). 191/883 participants were taking MaxEPA at 2 years. Advice was reinforced 3‐monthly. Dose: aimed for 0.5 g/d EPA Control: No such dietary advice or capsules Compliance: 7 day weighed food diary of a random sub‐sample indicated intake of 2.5 g/week EPA intervention, 0.8 g/week EPA control Dietary achievements Total fat intake, %E (through study): control 35 (SD 6), intervention 31 (SD 7) (MD −4.00, 95% CI −4.57 to −3.43); significant reduction Saturated fat intake, %E (through study): control 15 (SD 3), intervention 11 (SD 3), (MD −4.00, 95% CI −4.26 to −3.74); significant reduction PUFA intake (through study), %E⁑: control 7 (SD unclear), intervention 9 (SD unclear), (MD 2.00, 95% CI 1.57 to 2.43 assuming SDs of 5) significant increase PUFA n‐3 intake: EPA, control 0.6 (SD 0.7) g/week, intervention 2.4 (SD 1.4) g/week PUFA n‐6 intake: not reported MUFA intake (through study), %E⁑: control 13 (SD unclear), intervention 11 (SD unclear) (MD −2.00, 95% CI −2.43 to −1.57 assuming SDs of 5); significant reduction CHO intake (through study), %E: control 44 (SD 6),intervention 46 (SD 7) (MD 2.00, 95% CI 1.43 to 2.57); significant increase Protein intake (through study), %E: control 17(SD 4), intervention 18 (SD 4) (MD 1.00, 95% CI 0.65 to 1.35); significant increase Trans fat intake: not reported Length of intervention: 24 months |
|
| Outcomes | Main study outcome: total mortality, reinfarction, CHD death Dropouts: none for mortality Available outcomes: total and CV deaths, MI, CHD events, lipids, blood pressure, cancer deaths Response to contact: yes (data provided) |
|
| Notes | Some of each group were also advised on low fat and high PUFA and/or high fibre diets, all participants who smoked were advised to stop and all with a BMI > 30 kg/m2 were given weight reduction advice, regardless of randomisation arm. The low fat high PUFA comparison was included in the omega‐6 review. Study funding: by the Welsh Scheme for the Development of Health and Social Research, the Welsh Heart Foundation and the Health Promotion, Research Trust. Seven Seas Health Care and Duncan Flockhart provided Maxepa capsules |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomised" confirmed by author |
| Allocation concealment (selection bias) | Unclear risk | Pre‐prepared sequentially numbered enveloped opened by dietitian (unclear if envelopes were opaque) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of dietary advice (or lack of it) is not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were not aware of study allocation (Prof Burr stated he did not know assignments) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Hospital notes and death registers were flagged to catch all outcome data |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trials register entry was found |
| Attention | High risk | More attention was paid to those given dietary advice |
| Compliance | Unclear risk | 7 day weighed food diary of a random sub‐sample indicated intake of 2.5 g/week EPA intervention, 0.8 g/week EPA control |
| Other bias | Low risk | None noted |
| Methods | Diet and Angina Randomised Trial (DART2) RCT, 2 × 2, (oily fish or capsulesn‐3 EPA + DHA vs nil, also no specific advice, also fruit, vegetables and oats vs no specific advice), 3‐9 years Summary risk of bias: moderate or high |
|
| Participants | Men treated for angina N: 1571 intervention, 1543 control (all analysed for events) Control level of risk for CVD: high Men: 100% Mean age in years (SD): 61.1 (NR) intervention, 61.1 (NR) control Age range: unclear Smokers: 25% intervention, 23% control Hypertension: 49% intervention, 47% control Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49%: lipid lowering, beta‐blockers Medications taken by some, but less than 20% of the control group: not reported Location: UK Ethnicity: not reported |
|
| Interventions | Type: dietary advice (to eat more oily fish or take fish oil capsules) Comparison: EPA + DHA vs unclear (not total fat, SFA or alcohol, presumably CHO and/or protein but not clear) Intervention: most (1109) advised to eat at least 2 weekly portions of fatty fish OR take MaxEPA capsules, 3/d (0.5 g EPA/d). But 462 participants were sub‐randomised to receive only fish oil capsules, not dietary fish advice. Dose: aimed for 0.5 g/d EPA. Control: none specific sensible eating advice that did not include either of the interventions. Compliance: postal dietary questionnaire suggested dietary EPA intake increased by 2.4 g /week intervention, 0.2 g /week control Dietary achievements Total fat intake, (change from baseline to 6 months): control −8.6 g/d (SD 20.9), intervention −5.2 (g/d SD 21.4) (MD 3.4 g/d) Saturated fat intake, (change from baseline to 6 months): control −3.5 g/d (SD 9.3), intervention −2.8 g/d (SD 9.4), (MD 0.7 g/d) PUFA intake (change from baseline to 6 months): control −1.6 g/d (SD 5.4), intervention −0.1 g/d (SD 5.8) (MD 1.5 g/d) PUFA n‐3 intake (change from baseline to 6 months): EPA, control 0.12 g/week (SD 0.73), intervention 2.65 g/week (SD 1.35) (MD 2.53 g/week) PUFA n‐6 intake: not reported MUFA intake: not reported CHO intake: not reported Protein intake: not reported Trans fat intake: not reported Duration of intervention: 36 to 108 months |
|
| Outcomes | Main study outcome: total mortality Dropouts: none for mortality Available outcomes: total and CV deaths, sudden death, stroke, heart failure, cancer deaths Response to contact: yes (data provided) | |
| Notes | Some of each group were also advised on high fruit, vegetables and oat diets, and those who received neither fish nor fruit advice received 'non‐specific' dietary advice. All those whose BMI > 30 kg/m2 in both groups received weight reduction advice. Study funding: probably British Heart Foundation, Seven Seas Ltd, Novex Pharma Ltd and the Fish Foundation (these were acknowledged) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly allocated" |
| Allocation concealment (selection bias) | Unclear risk | Pre‐prepared sequentially numbered enveloped opened by dietitian (unclear if envelopes were opaque) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Dietary advice, so not possible for participants to be blinded to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were not aware of study allocation (Prof Burr stated he did not know assignments) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Hospital notes and death registers were flagged to catch all outcome data |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was found, or trials registry entry |
| Attention | High risk | More attention was paid to those given dietary advice |
| Compliance | Unclear risk | Postal dietary questionnaire suggested dietary EPA intake increased by 2.4 g/week intervention, 0.2 g/week control |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (n‐3 PUFA capsules vs placebo), 18 months Summary risk of bias: low |
|
| Participants | White overweight/obese patients with impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) N: 138 intervention, 143 control (analysed 128 intervention, 130 control) Level of risk for CVD: low Men: 50.72% intervention, 48.95% control Mean age in years (SD): 53.4 (11.2) intervention, 54.8 (12.1) control Age range: unclear Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Italy Ethnicity: white |
|
| Interventions | Type: capsule (n‐3 PUFA) Comparison: EPA + DHA vs CHO + SFA Intervention: 3 ×1 g capsule/ day n‐3 PUFAs (ethylic esters, each 1‐g capsule of n‐3 PUFAs contains highly concentrated ethyl esters of omega‐3 fatty acids, primarily EPA, and DHA in the proportion of 0.9–1.5). Dose: unclear (approx 2‐3 g/d) Control: placebo (a capsule containing sucrose, mannitol and mineral salts, magnesium stearate (a saturated fat) and silicon dioxide, used as anti‐caking agents) Both groups were given diet advice to follow a controlled‐energy diet based on AHA recommendations (50% of calories from carbohydrates, 30% from fat (6% saturated), and 20% from proteins, with a maximum cholesterol content of 300 mg/day and 35 g/day of fibre). Individuals were also encouraged to increase their physical activity by walking briskly for 20 to 30 min, 3 to 5 times per week, or by cycling Compliance: measured by counting the number of pills returned at the time of specified clinic visits Length of intervention: 18 months |
|
| Outcomes | Main study outcome: insulin resistance Dropouts: 23 across arms (no details on groups but stated that there were no difference between groups) Available outcomes: mortality, CV mortality, CHD event, stroke, combined CVD events, MI, AF, weight, BMI, lipids, diabetes mellitus Response to contact: yes (data provided) |
|
| Notes | Study funding: "The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done using a drawing of envelopes containing randomisation codes prepared by a statistician. |
| Allocation concealment (selection bias) | Low risk | Author stated that allocation was concealed from clinicians and researchers, but no methodology provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both n‐3 PUFAs and placebo were supplied as identical, opaque, white capsules in coded bottles to ensure the blind status of the study. However no information provided on capsules taste or smell |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A copy of the code was provided only to the person performing the statistical analysis |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | An intention‐to‐treat analysis was conducted for patients who received 1 dose of study medication |
| Selective reporting (reporting bias) | Unclear risk | No trial registry or protocol found |
| Attention | Low risk | No difference reported |
| Compliance | Unclear risk | Measured by counting the number of pills returned at the time of specified clinic visits |
| Other bias | Low risk | None noted |
| Methods | RCT 4 arms, ( n‐3 EPA + DHA (3 different doses) vs MUFA), 12 months Summary risk of bias: moderate or high |
|
| Participants | Healthy monks N: 14 high, 15 medium, 15 low dose intervention, 14 control Level of risk for CVD: low Men: 100% Mean age in years (SD): 56.2 (16.5) (not reported by arm) Age range: 21‐87 Smokers: none Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported (no medications influencing lipid metabolism or non‐steroidal anti‐inflammatory drugs were allowed) Location: the Netherlands Ethnicity: not reported |
|
| Interventions | Type: capsules Comparsion: LCn3 vs MUFA Intervention 9 capsules (9 g vol.) per day, of which 3, 6 or 9 were fish oil (Labaz, Brussels, Belgium) and any remainder were placebo (providing respectively 1.12; 2.24 or 3.37 g n‐3 FA/day). Dose: 1.12 g/d; 2.24 g/d or 3.37 g/d EPA + DHA) Control: 9 placebo capsules made up of olive oil (Puget Marseille, France) and Palmoil (Loders‐Kroklaan Wormerveen, the Netherlands) with the same SFA, cholesterol and vitamin E as the fish oil capsules. Compliance: assessed by counting remaining capsules every 2 months and by measuring EPA concentration. Excellent compliance reported and shown by the EPA concentration results Length of intervention: 12 months |
|
| Outcomes | Main study outcome: effect on coronary risk factors Dropouts: none Available outcomes: deaths (nil), CVD events (nil), lipids, BP, HbA1c, weight (measured but only text suggests "no significant changes in the anthropometric parameters (weight, length, waist, hip and thigh circumferences) during the study"), IL‐6, TNF‐alpha and several IL‐1s (IL‐6 reported as below detection range, for the others there was "no significant difference between the two treatment groups at any point in time") Response to contact: yes |
|
| Notes | Study funding: capsules supplied by Labaz (Brussels Belgium). The placebo capsules contained olive oil (Puget) and palm oil (Loders‐Kroklaan, Wormerveer). Financial support by Sanofi‐Labaz. Data entered for high fish oil versus placebo groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (author correspondence): "The manufacturer provided envelopes containing numbers corresponding with boxes of capsules. For each enrolled subject, random envelope was opened." |
| Allocation concealment (selection bias) | Low risk | Allocation concealed from all this way |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Although double blind, the fishy taste of the active treatment was not matched (author states that the fishy taste was clear in the intervention capsules) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Authors confirmed outcome assessors were unaware until afterwards. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registry record |
| Attention | Low risk | No difference between groups |
| Compliance | Low risk | Significant difference in EPA concentration |
| Other bias | Low risk | None noted |
| Methods | Dietary Intervention for Patients Polypectomized for tumours of the colorectum (DIPP) RCT, parallel, 2 arms (n‐3 EPA + DHA + n‐3 ALA vs nil), 24 months Summary risk of bias: moderate or high |
|
| Participants | Patients previously polypectomised for colorectal tumours N: 104 intervention, 101 control Level of risk for CVD: low Men: 73.1% intervention, 74.3% control Mean age in years (SD): 58.3 (9.5) intervention, 59.7 (8.9) control Age range: 35‐75 Smokers: 65.4% intervention, 61.4% control Hypertension: not reported Medications taken by at least 50% of those in the control group: supplements Medications taken by 20%‐49% of those in the control group: none Medications taken by some, but less than 20% of the control group: oral contraceptive pills Location: Japan Ethnicity: not reported |
|
| Interventions | Type: advice + supplement (fish oil capsules) Comparison: EPA + DHA + ALA vs omega‐6 Intervention: advice to reduce total fat intake, decrease consumption of n‐6 PUFAs, increase intake of n‐3 PUFAs from fish/marine foods, increase intake of n‐3 PUFAs from perilla oil rich in ALA, take 8 capsules of fish oil/day (equivalent to 96 mg/day of EPA and 360 mg/day of DHA). Dose: 456mg/d EPA + DHA and unknown dose of ALA Control: advice to decrease intake of fats/oils as a whole Compliance: measured via semi‐quantitative food frequency questionnaire, plasma fatty acid concentrations, fatty acid compositions in the membranes of red blood cells and the sigmoid colon. Reported satisfactorily high compliance with protocol in both groups but no figures provided. Length of intervention: 24 months |
|
| Outcomes | Main study outcome: number and size of colorectal tumours Dropouts: 3 intervention, 5 control Available outcomes: all cause mortality, dietary intake, plasma fatty acids, lipids, side effects, glucose Response to contact: yes (methodological details provided) |
|
| Notes | Study funding: all were either government or charity grants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly allocated using random digit number for allocation of participants |
| Allocation concealment (selection bias) | Low risk | Author confirmed "Allocation information was blinded to clinicians and researchers" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | From the 2015 paper, "The attending physicians as well as the participants were blinded to the assignment information". However in the discussion section they say "complete participant blinding could not have been achieved because free living participants might have exchanged information on their dietary intervention, say in the hospital waiting room". Author confirmed blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "physicians, including colonoscopists, a scientist who conducted blood and specimen analyses, and pathologists were blinded" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All those randomised were accounted for |
| Selective reporting (reporting bias) | High risk | The researchers chose not to report data on the number, size and pathological type of the colorectal tumours as they said they would in the trials register. They reported more outcomes in the paper than initially stated. UMIN000000461 Registered 3 August 2006, recruitment completed 1 March 2007 |
| Attention | Low risk | Participants were given equal follow‐up |
| Compliance | Unclear risk | Reported satisfactorily high compliance with protocol was noted in both groups but no figures |
| Other bias | Low risk | None noted |
| Methods | Dietary Intervention Study for AF (DISAF) RCT, parallel, 2 arms (n‐3 EPA + DHA vs nil), 12 months Summary risk of bias: moderate or high |
|
| Participants | People presenting for first treatment of acute/persistent atrial fibrillation or flutter, confirmed by ECG N: intervention 201, control 206 Level of risk for CVD: high (patients with atrial fibrillation) Men: intervention 64.7%, control 63.6% Mean age in years (SD): intervention 67.7 (9.4), control 68.7 (9.5) Age range: unclear Smokers: intervention 10.9%, control 12.1% Hypertension: intervention 48.2%, control 40.8% Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: antiarrythmics, antithrombotics Medications taken by some, but less than 20% of the control group: not reported Location: UK Ethnicity: white British |
|
| Interventions | Type: dietary advice Comparison: EPA + DHA vs unclear Intervention: dietary assistants gave advice and support to eat 2 to 3 portions of oily fish per week (providing up to 10 g LCn3/ week), plus 2 to 3 portions of fruit and vegetables per day. Dose: 1.4 g/d EPA + DHA. Control: dietary assistants gave advice and support to eat 2 to 3 portions of fruit and vegetables per day. No other health/lifestyle given as part of the trial Compliance: assessed red blood cell fatty acids and found some increases in EPA and DHA in intervention compared to control (no further intake data) Length of intervention: 12 months |
|
| Outcomes | Main study outcome: sinus rhythm after 12 months Dropouts: unclear Available outcomes: deaths, AF recurrence Response to contact: yes (data provided) |
|
| Notes | Study funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was by phone to an independent randomisation office, which used pre‐printed random number tables |
| Allocation concealment (selection bias) | Low risk | Randomisation was by phone to an independent randomisation office, which used pre‐printed random number tables |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Dietary advice was clear, so allocation known by participants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Some discrepancies between papers, reasons unclear |
| Selective reporting (reporting bias) | High risk | ISRCTN16448451 registered 23 January 2004, recruitment from 1 July 1998 to 1 July 2002; some secondary outcomes were not reported |
| Attention | Low risk | Intervention (advice to eat more oil‐rich fish, fruit and vegetables) and control (advice to eat more fruit and vegetables) groups appeared to be given equivalent time and attention. |
| Compliance | Low risk | Assessed red blood cell fatty acids and found some increases in EPA and DHA in intervention compared to control |
| Other bias | High risk | The trial was stopped early |
| Methods | Diet and Omega 3 Intervention Trial on Atherosclerosis (DO IT) Randomisation: RCT, parallel, 2 × 2 factorial, (n‐3 DHA + EPA vs n‐6 LA also dietary advice intervention), 36 months Summary risk of bias: moderate or high |
|
| Participants | Elderly men with longstanding dyslipidaemia or hypertension (a subset of Oslo Diet heart study) N: intervention 282 (140 n‐3 capsules + 142 n‐3 capsules and dietary advice), control 281 (142 placebo capsules + 139 placebo capsules and dietary advice) Level of risk for CVD: moderate Men: intervention 100%, control 100% Mean age in years (SD): intervention 70.4 (2.9), control 69.7 (3.0) years Age range: 64‐76 years Smokers: intervention 35%, control 33% Hypertension: intervention 29%, control 27% Medications taken by at least 50% of those in the control group: none Medications taken by 20%‐49% of those in the control group: statins and acetylsalicylic acid Medications taken by some, but less than 20% of the control group: β‐blockers, ACE inhibitors and nitrates Location: Norway Ethnicity: not reported |
|
| Interventions | Type: supplement/ capsule (also dietary advice as the factorial intervention) Comparison: EPA + DHA vs omega‐6 Intervention: 2 × 2 capsules/d incl 2.4 g/d of omega‐3 PUFA (Pikasol, 0.84 g/d EPA plus 0.48 g/d DHA plus 8.4 mg/d tocopherols). Dose: 1.32 g/d EPA + DHA Control: 2 × 2 capsules/d inc 4 g/d corn oil (2.24 g/d linoleic, 1.28 g/d oleic acid, 16 mg/d tocopherols) Compliance: pharmacy records suggested that > 90% of supplements were taken, and plasma EPA and DHA were raised in intervention compared to control participants. Duration of intervention: 36 months |
|
| Outcomes | Main study outcome: atherosclerosis progression. Dropouts: intervention 14 died, 20 others discontinued, control 24 died, 18 others discontinued Available outcomes: mortality, cardiovascular deaths, CHD events, CV events, MI, stroke, diabetes, glucose, lipids, cancer diagnosis, cancer deaths, sudden death, BMI (waist circumference reported as median, IQR) Response to contact: yes (data provided) |
|
| Notes | The other 2 × 2 intervention was dietary counselling to increase both omega‐3 and omega‐6 fats as well as fruit and vegetables. Study funding: Norwegian Cardiovascular Council, Norwegian retail company RIMI, vegetable oil and margarine supplied by the Norwegian food company Mills DA and placebo capsules by LUBE |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block randomisation, no clear mechanism provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Capsules of fish oil or placebo taken, but unclear whether blinded and if so, how well or successfully |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Mortality data were supplied from the Norwegian Cause of Death Registry, and all clinical events were confirmed by hospital records and verified by an independent cardiologist" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition as deaths and events collected from centralised register |
| Selective reporting (reporting bias) | Unclear risk | Trials registry entry submitted after the outcomes papers were published. |
| Attention | Low risk | No suggestion of attention bias between verum and placebo supplement arms |
| Compliance | Low risk | Pharmacy records suggested that > 90% of supplements were taken, and plasma EPA and DHA were raised in intervention compared to control participants |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (n‐3 ALA vs n‐6 LA), 12 months Summary risk of bias: moderate or high |
|
| Participants | Healthy menopausal women N: 101 intervention, 98 control. (analysed, intervention: 85 control: 94) Level of risk for CVD: low Men: 0% intervention, 0% control Mean age in years (SD): 54.0 (4.0) intervention, 55.4 (4.5) control Age range: 49‐65 Smokers: 8% intervention, 6% control Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Canada Ethnicity: French Canadian |
|
| Interventions | Type: food supplement (flaxseed) Comparison: ALA vs unclear (probably includes lipids, CHO and protein, but not clear) Intervention: 40 g/d flaxseed incorporated into diets (providing 21,071 g total lignans, 180 calories, 16 g lipids (57% ALA), and 11 g total dietary fibre). Dose: 9.1 g/d ALA Control: 40 g/d wheat germ incorporated into diets (providing 196 g total lignans, 144 calories, 4 g lipids (6.9% ALA), and 6 g total dietary fibre Compliance: first morning urine collection was performed at randomisation and at month 12 to measure urinary lignin levels. In addition, study participants recorded their daily intake of seeds on diary cards and were asked to return unused bread and packages of seeds at each visit. Good compliance reported Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: bone mineral density Dropouts: 26 intervention, 17 control (but 13/17 had an endpoint evaluation) Available outcomes: weight, BMI, QoL, blood pressure, lipids, glucose, adverse events, dietary intake, plasma fatty acids Response to contact: yes |
|
| Notes | Auhors replied to tell us that there were no deaths or CV events during the study Study funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule was prepared by the clinical unit of the research centre using computer generated randomisation in blocks of 4‐8 |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, investigators, staff, and statisticians were blinded to dietary assignments for the duration of the study. Quote: "a local baker prepared loaves of bread. Each week, the loaves of bread were delivered in sealed, opaque unmarked wrappers to the Department of Food and Nutrition Sciences at Laval University. The seeds were ground up and vacuum‐packed in the same laboratory. The Department of Food and Nutrition Sciences was responsible for labelling the bags of bread and packages of seeds with the subject's randomization number. Bread and packages of seeds were provided on a 3‐month basis. The foods that both groups received was similar in appearance and packaging and was kept frozen until consumption to avoid essential fatty acid |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, investigators, staff, and statisticians were blinded to dietary assignments for the duration of the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis. Loss to follow‐up 10%, reasons given |
| Selective reporting (reporting bias) | Unclear risk | No protocol or clinical trial registry entry found |
| Attention | Low risk | All participants had same number of visits |
| Compliance | Low risk | First morning urine collection was performed at randomisation and at month 12 to measure urinary lignin levels. In addition, study participants recorded their daily intake of seeds on diary cards and were asked to return unused bread and packages of seeds at each visit. Good compliance reported |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (n‐3 EPA vs nil), 12 months Summary risk of bias: moderate or high |
|
| Participants | Patients having PCI after acute MI N: 119 intervention, 119 control analysed Level of risk for CVD: high Men: 77% intervention, 76% control Mean age in years (SD): 70 (11) intervention, 71 (12) control Age range: unclear Smokers: 28% intervention, 32% control Hypertension: 71% intervention, 69% control Medications taken by at least 50% of those in the control group: aspirin, ticlopidine, beta‐blockers, statins (as part of treatment) Medications taken by 20%‐49% of those in the control group: ARB/ACE inhibitors Medications taken by some, but less than 20% of the control group: none Location: Japan Ethnicity: not reported |
|
| Interventions | Type: supplement (EPA) Comparison: EPA vs nil Intervention: purified EPA ethyl esters (> 98%) 1800 mg EPA/day within 24 hours after PCI plus statins. Dose: 1.8 g/d EPA Control: statins with no EPA Compliance: not reported Length of intervention: 12 months |
|
| Outcomes | Main study outcome: cardiovascular events Dropouts: 1 intervention, 2 control Available outcomes: mortality, stroke, MI, sudden death, CV death, revascularisation Response to contact: no |
|
| Notes | Study funding: trial registry state "self‐funded". The authors received honoraria from Mochida Pharmaceutical Co. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated, randomisation plan, which included stratification by age and sex |
| Allocation concealment (selection bias) | Unclear risk | Carried out by research technician but unclear |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label but blind endpoint |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Data on outcomes were collected from clinical charts. Unclear if blinded. Diagnoses were confirmed by investigator blind to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 3 dropouts, similar rates between the groups and reasons given |
| Selective reporting (reporting bias) | High risk | Data collection completed before trial registry entry. Only 1% dropouts |
| Attention | Low risk | Timing of follow‐up similar |
| Compliance | Unclear risk | Not reported |
| Other bias | Low risk | None observed |
| Methods | EPE‐A RCT, parallel, 3 arms (n‐3 EPA, low dose vs high dose vs unclear placebo), 12 months Summary risk of bias: moderate or high |
|
| Participants | People with non‐alcoholic steatohepatitis (NASH) and non‐alcoholic fatty liver disease (NAFLD) N: 86 intervention‐high, 82 int low, 75 control (analysed 64, 55, 55 respectively, ITT analysis for primary outcomes) Level of risk for CVD: low (although 35% had type II diabetes) Men: 33.7% intervention‐high, 41.5% intervention‐low, 42.7% control Mean age in years (SD): 47.8 (11.1) intervention‐high, 47.8 (12.5) intervention‐low, 50.5 (12.5) control Age range: not reported Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: white intervention‐low: 94%, intervention‐high: 87%, control: 90.7% African American intervention‐low: 3.7%, intervention‐high: 2.3%, control: 4.0% Others intervention‐low: 2.4%, intervention‐high: 10.5%, control: 5.3% |
|
| Interventions | Type: supplement (omega 3 capsule) Comparison 1: high EPA vs low EPA (unclear what replaced EPA) Comparison 2: EPA vs unclear (placebo contents not reported) Intervention‐high: EPA‐E 2.7 g/d, 3 × EPA‐E 300 mg capsules. Dose: 2.7 g/d EPA + DHA Intervention‐low: EPA‐E 1.8 g/d, 2 × EPA‐E 300 mg capsules + 1 placebo capsule Dose: 1.8 g/d EPA + DHA Control: 3 × placebo capsules. The pills were identical with respect to size, colour and smell Compliance: estimated by pill count and measuring the ratio of serum EPA to arachidonic acid. compliance rates for the 3 groups (placebo vs EPA‐E 1800 mg/d vs EPA‐E 2700 mg/d) were 89.5% (6.8%), 90.3% (5.7%) and 89.5% (5.3%), respectively Length of intervention: 12 months |
|
| Outcomes | Main study outcome: histological response in standardised scoring of liver biopsies and change in ALT level Dropouts: 22 intervention‐high, 27 intervention‐low, 20 control Available outcomes: cardiac events, deaths (none), angina, adverse events (weight, BMI, lipids, glucose, HbA1c, HOMA, hsCRP all reported as medians so not useable in meta‐analyses) Response to contact: yes (provided methodological details) |
|
| Notes | Data combined for the 2 intervention groups for binary outcomes and higher dose data vs control used for continuous outcomes Study funding: supported entirely by Mochida Pharmaceuticals |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation using an interactive voice‐response system to assign subjects in a 1:1:1 ratio between the 2 arms for each site separately. Participants were stratified by the presence of type 2 diabetes. The total fraction of such individuals was capped at 40% of the study cohort |
| Allocation concealment (selection bias) | Low risk | As above (remote computer‐generated randomisation) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind stated, but no further details. Author confirmed researchers and outcome assessors were blinded to treatment allocation and pills were identical with respect to size, colour and smell |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number and characteristics of participants lost to follow‐up similar across arms, however < 80% provided outcome data relevant to this systematic review |
| Selective reporting (reporting bias) | Low risk | Registered June 2010, study started June 2010, completed October 2012. All outcomes in trials registry entry were also reported in the trials registry. Secondary outcomes reported were not planned (compared with first version of clinicaltrials.gov entry) |
| Attention | Low risk | All participants had same follow‐up visits. |
| Compliance | Low risk | Compliance was estimated by pill count and measuring the ratio of serum EPA to arachidonic acid. Compliance rates for the 3 groups (placebo vs EPA‐E 1800 mg/d vs EPA‐E 2700 mg/d) were 89.5% (6.8%), 90.3% (5.7%) and 89.5% (5.3%) respectively |
| Other bias | Low risk | None noted |
| Methods | EPANOVA in Crohn's disease, study 1 (EPIC‐1) RCT, parallel, 2‐arm (omega 3 vs MCT), 52 weeks Summary risk of bias: moderate or high |
|
| Participants | Adults with quiescent Crohn's disease (CDAI) score < 150 N: 188 intervention, 186 control Level of risk for CVD: low Men: 48.1% intervention, 41.1% control Mean age in years (SD): 40.5 (15.2) intervention, 38.2 (13.1) control Age range: 18‐70 years Smokers: 30.6% intervention, 34.4% control Hypertension: unclear Medications taken by at least 50% of those in the control group: oral 5‐ASA therapy, Systemic corticosteroids – prednisolone, budesonide Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: antibiotic therapy, topical rectal therapy, immune‐modifying agents, immune modifiers/biologics Location: Canada, Europe, Israel, USA Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs SFA (medium chain triglycerides of short SFAs) Intervention: 2 × 2 1 g gelatin capsules omega‐3 free fatty acids (Epanova‐ 2.2 g EPA, 0.8 g DHA). Dose: 3 g/d EPA + DHA Control: 4 x1 g capsules medium chain triglycerides Compliance: pill counts, 79.2% adhered intervention, 75.6% adhered control Length of intervention: mean 52 weeks |
|
| Outcomes | Main study outcome: Crohns relapse‐free time Dropouts: 80 intervention, 91 control Available outcomes: total deaths, non‐fatal arrhythmias, cancer diagnoses, cancer deaths, adverse events Response to contact: yes (data provided) |
|
| Notes | Study funding: Tillotts Pharma, authors had extensive financial disclosures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by number generator. Used a centralised randomisation procedure via interactive voice recognition system. |
| Allocation concealment (selection bias) | Low risk | Centralised randomisation (see above) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blinding stated, identical capsule (slow‐release capsules). Neither investigator nor participant knew the allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study states double‐blind but does not state that outcome assessors were blinded or provide a mechanism for this |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number of dropouts and reasons provided. 171 of 187 in intervention group and 174 of 184 in control group provided data for primary outcome, (7% dropout), though 80 in the intervention group and 91 in the control group terminated early. |
| Selective reporting (reporting bias) | High risk | Trials registration (NCT00613197) first received in 2008, but study started in 2003 and was published in 2008 |
| Attention | Low risk | As investigators were blinded attention bias was not possible. |
| Compliance | Unclear risk | Pill counts, 79.2% adhered intervention, 75.6% adhered control |
| Other bias | Low risk | No further bias noted |
| Methods | EPANOVA in Crohn's Disease, Study 2 (EPIC‐2) RCT, parallel, 2 arms (omega 3 vs MCT), 58 weeks Summary risk of bias: moderate or high |
|
| Participants | Adults with a confirmed diagnosis of Crohn's Disease and a Crohn's Disease Activity Index (CDAI) score < 150 who are responding to steroid induction therapy N: intervention, 189, control 190 (187 intervention, 188 control analysed) Level of risk for CVD: low (people with quiescent Crohn's disease) Men: 48.1% intervention, 41.1% control Mean age in years (SD): 38.5 (13.8) intervention, 40.0 (13.6) years control Age range: > 16 years Smokers: 25.1% intervention, 37.2% control Hypertension: unclear Medications taken by at least 50% of those in the control group: systemic corticosteroids – prednisolone, budesonide (but tapered and discontinued during the study) Medications taken by 20%‐49% of those in the control group: only reported for prior 12 months Medications taken by some, but less than 20% of the control group: only reported for prior 12 months Location: Canada, Europe, Israel, USA Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs SFA (medium chain triglycerides of short SFAs) Intervention: 2 × 2 1 g gelatin capsules omega‐3 free fatty acids (Epanova) providing total dose ˜2.2 g/d EPA, 0.8 g/d DHA. Dose: ˜3.0 g/d EPA + DHA Control: 2 × 2 1 g capsules medium chain triglyceride oil Compliance: measured by patient interviews and pill counts, 75.4% adhered intervention, 81.4% adhered control Length of intervention: mean 58 weeks |
|
| Outcomes | Main study outcome: maintain Crohns symptomatic remission Dropouts: 114 intervention, 112 control Available outcomes: mortality, CV events (nil), cancer diagnoses, adverse events Response to contact: yes (data provided) | |
| Notes | Study funding: Tillotts Pharma, authors had extensive financial disclosures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by number generator. Used a centralised randomisation procedure via interactive voice recognition system |
| Allocation concealment (selection bias) | Low risk | Centralised randomisation (see above) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double blinding stated, identical capsule (slow‐release capsules). Neither investigator nor participant knew the allocation. However no information provided on capsules taste or smell |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study states double‐blind but does not state that outcome assessors were blinded or provide a mechanism for this |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Number of dropouts and reasons provided, however 114 of 189 in intervention group and 112 of 190 in control group terminated early. |
| Selective reporting (reporting bias) | High risk | NCT00074542. First received 2003, study start 2002. Published 2008. Some outcomes, such as quality of life, stated in trials registry but not in published papers |
| Attention | Low risk | As investigators were blinded, attention bias was not possible. |
| Compliance | Unclear risk | Measured by patient interviews and pill counts, 75.4% adhered intervention, 81.4% adhered control |
| Other bias | Low risk | No further bias noted |
| Methods | Older People, Omega‐3 and Cognitive Health (EPOCH) RCT, parallel (n‐3 EPA + DHA vs MUFA), 18 months Summary risk of bias: low |
|
| Participants | Healthy older adults with no cognitive impairment N: 195 intervention, 196 control (reported by author) Level of risk for CVD: low Men: not reported Mean age in years (SD): not reported Age range: not reported, but 65‐90 recruited Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Australia Ethnicity: not reported |
|
| Interventions | Type: supplement (fish oil capsules) Comparison: EPA + DHA vs MUFA Intervention: 4 capsules/d (1.72 g/d DHA and 0.60 g/d EPA). Dose: 2.32 g/d EPA + DHA Control: 4 capsules/d (3.960 g/d olive oil and 40 mg/d fish oil) Compliance: count of all unused supplements returned at three‐monthly intervals, plus self‐report calendars, mailed back on a monthly basis. If compliance fell below 85% (re calendars), they were contacted by a researcher who noted the reasons. Compliance also assessed by erythrocyte membrane n‐3 LC PUFA status Length of intervention: 18 months |
|
| Outcomes | Main study outcome: change in cognitive performance Dropouts: not reported Available outcomes: mortality (nil), MI, stroke, revascularisation, arrhythmias, CV events Response to contact: yes (data provided) |
|
| Notes | Authors reported some events, but don't appear to be published. Study funding: EPAX donated the Omega‐3 concentrate and Blackmores Pty Ltd donated the placebo and packaging of the Omega‐3 concentrate. The trial was supported by the Brailsford Robertson Award 2007‐2008 (University of Adelaide and CSIRO Food and Nutritional Sciences), and is funded by a National Health and Medical Research Project Grant (#578800). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Age‐stratified, permuted‐block randomisation, with mixed block‐sizes (2‐8, size unknown to study investigators), 1:1 allocation. Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Low risk | An independent researcher prepared allocation to treatment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The researchers, project staff, and participants remained blinded to treatment allocation until the trial was completed and the database locked. However, no information provided on capsules appearance, taste or smell |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data for each group presented, and no attrition data presented |
| Selective reporting (reporting bias) | High risk | Only cognitive functions reported for whole population (not by arm). No secondary outcomes reported (MMSE; perceived health status, depressive symptoms, positive and negative affect, life satisfaction, self‐reported cognitive functioning, and functional capacity; blood pressure; biomarkers of glucose, glycated haemoglobin, triglycerides, total cholesterol, HDL, LDL, homocysteine, CRP, MDA, and telomere length) |
| Attention | Low risk | All had the same contact and attention |
| Compliance | Unclear risk | Count of all unused supplements returned at 3‐monthly intervals, plus self‐report calendars, mailed back on a monthly basis. If compliance fell below 85% (re calendars), they were contacted by a researcher who noted the reasons. Compliance also assessed by erythrocyte membrane n‐3 LC PUFA status but results not reported |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel (n‐3 EPA + DHA vs unclear), 12 months Summary risk of bias: moderate to high |
|
| Participants | People with successful external cardioversion N: unclear intervention, unclear control (54 analysed intervention, 54 control) Level of risk for CVD: high Men: 70% intervention, 74% control Mean age in years (SD): 65.0 (mean for whole group, SD not reported) Age range: not reported Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Germany Ethnicity: not reported |
|
| Interventions | Type: supplement (probably, not described) Comparison: high EPA + DHA vs unclear placebo Intervention: described only as "PUFA" but included in systematic review (Mariani 2013) by Erdogan et al on effects of n‐3 PUFA. Dose: unclear Control: described only as "placebo" Compliance: not reported Length of intervention: 12 months |
|
| Outcomes | Main study outcome: atrial fibrillation relapse Dropouts: not reported Available outcomes: recurrent AF (reported in Mariani 2013), mortality (none) Response to contact: no reply to date |
|
| Notes | Funding source: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Described as triple blind, but no further details provided (only an abstract with some details in a related trial publication and some in a systematic review by the same author) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described, but analysis appears to have been carried out blind to intervention/control status |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number randomised not described |
| Selective reporting (reporting bias) | Unclear risk | Unclear, no trial registry entry or protocol found |
| Attention | Unclear risk | Not described |
| Compliance | Unclear risk | Not described |
| Other bias | Low risk | None noted |
| Methods | Fatty Acid Antiarrhythmia Trial – FAAT Randomisation: RCT, parallel, 2 arms, (n‐3 EPA + DHA vs MUFA), 12 months Summary risk of bias: moderate or high |
|
| Participants | People with implanted cardioverter defibrillators (ICDs) N: intervention 200, control 202 Level of risk for CVD: high (patients with ICDs). Men: intervention 84.5%, control 81.7% Mean age in years (SD): intervention 65.7 (11.6), control 65.3 (11.7) Age range: unclear Smokers: intervention 15%, control 11.4% Hypertension: unclear Medications taken by at least 50% of those in the control group: ACE inhibitors, beta‐blockers Medications taken by 20% ‐ 49%: diuretics Medications taken by some, but < 20%: calcium channel blockers, amiodarone, sotalol, type 1 antiarrhythmics Location: USA Ethnicity: intervention 95.5% white, control 96.5% white |
|
| Interventions | Type: supplement/capsule Comparison: EPA + DHA vs MUFA Intervention: 4 ×1 g/d fish oil gelatin capsules, 2.6 g/d EPA + DHA (Pronova Biocare, quantities of EPA + DHA unclear). Dose: 2.6 g/d EPA + DHA Control: 4 ×1 g/d olive oil capsules, 4 g/d (in identical gelatin capsules, < 0.06 g/d EPA and < 0.06 g/d DHA) All were advised to use olive oil rather than the common plant seed oils for cooking, dressings, and sauces Compliance: pill counts and platelet phospholipid data suggested greater omega 3 intake in intervention participants. 35% were non‐compliers (36.5% intervention, 34.2% control) Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: fatal ventricular arrhythmias Dropouts: intervention 13 deaths, unclear no. of dropouts, control 12 deaths, dropouts unclear Available outcomes: deaths, cardiovascular deaths, CVD events, deaths from heart failure, fatal arrhythmias, MI, angina Response to contact: yes (data provided) |
|
| Notes | Study funding: the study was supported in part by a grant from the NHLBI, NIH (HL62154) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation tables for each collaborating site, stratified by site |
| Allocation concealment (selection bias) | Low risk | Author confirmed allocation was concealed from investigators |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study referred to as "double blind" and gelatin capsules (verum and placebo) were stated as being of identical appearance but no discussion of taste or smell. Author confirmed that investigators and patients were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | VT and VF events were assessed blinded to allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large numbers dropped out so some deaths, etc. may have been missed, 35% discontinued early due to non‐compliance but were assessed at study end, data censored for some participants |
| Selective reporting (reporting bias) | High risk | Trials registry data received September 2005, paper published November 2005 |
| Attention | Low risk | Time and attention appeared similar between the 2 arms |
| Compliance | High risk | Pill counts and platelet phospholipid data suggested greater omega 3 intake in intervention participants. 35% were non‐compliers (36.5% intervention, 34.2% control) |
| Other bias | Low risk | None noted |
| Methods | Effects of Dietary Flaxseed on Symptoms of Cardiovascular Disease in Patients With Peripheral Arterial Disease (FLAX PAD) RCT, parallel, (n‐3 ALA vs mixed fat), 12 months Summary risk of bias: low |
|
| Participants | Patients with peripheral artery disease, over 40 years old N: 58 intervention, 52 control Level of risk for CVD: high (all had peripheral artery disease, 80% had hyperlipidaemia) Men: 74.1% intervention, 73.1% control Mean age in years (SD): 67.4 (8.06) intervention, 65.3 (9.4) control Age range: unclear Smokers: 19.2% intervention, 34.6% control Hypertension: 81% intervention, 69.2% control Medications taken by at least 50% of those in the control group: lipid lowering medication, antihypertensives, antithrombotics Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: insulin or blood sugar‐lowering drugs Location: Canada Ethnicity: unclear |
|
| Interventions | Type: food supplement (milled flaxseed) Comparison: ALA vs unclear (mix of wheat, wheat germ and mixed dietary oils) Intervention: food products (i.e. bagels, muffins, bars, pasta, buns, and milled seeds) containing 30 g of milled flaxseed daily. Dose: ˜6.8 g/d ALA (calculated based on 30 g milled flaxseed/d) Control: placebo food products (i.e. bagels, muffins, bars, pasta, buns, and milled seeds) containing a mixture of wheat, wheat bran, and mixed dietary oils to replace the flaxseed daily Compliance: plasma levels of enterolignans and the n‐3 fatty acid ALA were used as markers of dietary compliancy Length of intervention: 12 months |
|
| Outcomes | Main study outcome: all‐cause mortality, cardiovascular mortality, stroke, and myocardial infarctions Dropouts: 15 intervention, 11 control Available outcomes: blood pressure, lipids, adverse events, plasma ALA Response to contact: yes (but no data provided) |
|
| Notes | Different intervention dropout figures reported in two publications (13 or 15) Study funding: funded by government organisations but foods created and provided by a company |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly selected by a computer programme |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed. The person who determined if a participant was eligible for inclusion in the trial was unaware, when this decision was made, of which group the subject would be allocated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Product colour and texture were similar to disguise the composition of the product. Participants, personnel administering the intervention and those assessing the outcomes were blinded to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All personnel that collected or analysed data were blinded to the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised accounted for in main outcomes |
| Selective reporting (reporting bias) | High risk | Prospectively registered October 2008, study start October 2008, primary outcome data completed March 2011, end date December 2017. Cardiovascular mortality and measures of adiposity not reported in a useable way |
| Attention | Low risk | Both groups had the same care |
| Compliance | Unclear risk | 12 in intervention group and 8 in placebo group unwilling to comply with diet |
| Other bias | Low risk | None noted |
| Methods | Randomized trial to assess efficacy of PUFA for the maintenance of sinus rhythm in persistent atrial fibrillation (FORWARD) RCT, parallel, (n‐3 EPA + DHA vs MUFA), 12 months Summary risk of bias: low |
|
| Participants | Patients with paroxysmal atrial fibrillation N: 289 intervention, 297 control Level of risk for CVD: high Men: 57.8% intervention, 51.9% control Mean age in years (SD): 66.3 (12) intervention, 65.9 (10.5) control Age range: > 21 Smokers: 9% intervention, 6.2% control Hypertension: 92.2% intervention, 90.8% control Medications taken by at least 50% of those in the control group: aspirin, amiodarone, 'any antithrombotic treatment', beta‐blockers Medications taken by 20%‐49% of those in the control group: anticoagulants Medications taken by some, but less than 20% of the control group: none reported Location: Argentina Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs MUFA Intervention: one capsule/ day containing 1 g of n‐3 PUFA (Societá Prodotti Antibiotici and SigmaTau, Italy) (provided 850 mg to 882 mg EPA/DHA). Dose: 0.85 g/d EPA + DHA Control: identical placebo capsule containing olive oil Compliance: not reported. Length of intervention: 12 months |
|
| Outcomes | Main study outcome: survival free of atrial fibrillation Dropouts: 20 intervention, 25 control Available outcomes: mortality, MI, AF, heart failure, stroke, hospitalisation, side effects. Authors supplied further info on CVD events and methodology Response to contact: yes |
|
| Notes | Study funding: through unrestricted grants provided by companies that supplied study drugs, however "these companies did not have representatives on the Steering Committee" who terminated the trial after 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were centrally assigned to receive either 1 g of n‐3 PUFA or placebo in a ratio of 1:1" – computer generated in blocks of 4 and 6 stratified by study location |
| Allocation concealment (selection bias) | Low risk | As above, centrally allocated. Communication from authors was ambiguous, stated that the person recruiting was aware of which arm the individual would be allocated to, but that the "study was double‐blind, placebo‐controlled." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Each study site will be supplied with study drug and placebo in identically appearing packaging". "Both placebo and active treatment have the same odour and produce a comparable degree of fishy aftertaste" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Patients, investigator staff, persons performing the assessments, and data analysts will remain blind to the identity of the treatment from the time of randomisation until database lock" "The adjudication committee members are unaware of participant allocation and assess all available data and documentation with reference to pre‐established criteria". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "the study was cut short by the trial steering committee due to 'a slower‐than‐expected recruitment rate and lower event rates'. This 'resulted in an underpowered clinical trial unable to verify its hypothesis'. Therefore the outcome data were not as complete as they were initially meant to be". |
| Selective reporting (reporting bias) | Low risk | Prospectively registered January 2008, study start January 2008, completion August 2011. All outcomes in trials registry appear to have been reported. |
| Attention | Low risk | Both intervention and control given the same exposure to research personnel. 2013 paper: "Clinical outcomes, adherence, and adverse events were assessed 2, 4, 8, and 12 months after randomization" |
| Compliance | Unclear risk | Not reported |
| Other bias | Low risk | None noted |
| Methods | Fish Oil in knee OSTeoARthritis (FOSTAR) RCT, parallel, (n‐3 EPA + DHA vs low n‐3), 24 months Summary risk of bias: low |
|
| Participants | Adults aged 40+ years with knee osteoarthritis N: 101 intervention, 101 control Level of risk for CVD: low Men: 41% intervention, 60% control Mean age in years (SD): 60.8 (10) intervention, 61.1 (10) control Age range: > 40 Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: none reported Medications taken by 20%‐49% of those in the control group: not reported at baseline, but 'during' includes Vit. D ˜ 32% Medications taken by some, but less than 20% of the control group: not reported at baseline, but 'during' includes Glucocorticoid, HRT/anti‐resorptive, both ˜ 10% Location: Australia Ethnicity: not reported |
|
| Interventions | Type: supplementary food (enriched orange juice) Comparison: high EPA + DHA vs low EPA + DHA plus ALA (replacement unclear, but low omega 3) Intervention: 1‐3 × a day drink of fruit juice mixed with day total = 15 mL of fish oil supplement (18% EPA, 12% DHA, 4.5 g/day total omega 3). Dose: 4.5 g/d EPA + DHA Control: liquid oral oil 15 mL sunola oil/day (which contains fish oil 2 mL plus 13 mL canola oil) (total omega‐3 fat: ≥ 0.45 g EPA + DHA from 15 mL) Compliance: assessed by measuring the oil volume in returned bottles, compliance was > 80% in both groups. Both groups had increases from baseline in plasma EPA and DHA with the high‐dose group having substantially larger increases, consistent with compliance with study oil Length of intervention: 24 months |
|
| Outcomes | Main study outcome: change in pain scale of WOMAC index Dropouts: 18 intervention, 16 control Available outcomes: mortality, CVD events, adverse events, analgesic use, bone marrow density, weight gain and serum fatty acids Response to contact: yes |
|
| Notes | Data on quality of life and pain score are presented in a figure and not in a usable format Study funding: government funding |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random allocation sequence |
| Allocation concealment (selection bias) | Low risk | A security‐protected central automated allocation procedure was used to allocate participants to one of the 2 treatment arms. This was performed centrally at one pharmacy and then used to allocate and administer the oil at each site |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Citrus flavouring was added to both oils to achieve comparable taste and optimise masking. Both were provided in identical dark 500‐mL bottles with similar labelling. At the end of the study, 52% of participants were unsure which group to which they had been allocated (50% high dose, 50% low dose). Of the remaining who thought they knew which group they were allocated, only 57% answered correctly, suggesting that blinding had been well maintained |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants and staff involved in patient care and assessment of BMD remained blinded throughout the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Oil intolerance in 1st year differed, others appear similar, but numbers confused |
| Selective reporting (reporting bias) | High risk | Prospectively registered August 2007, recruitment started July 2007, outcomes published 2016. Variety of outcomes such as quality of life stated in trials registry but not published. |
| Attention | Low risk | Same contact and instruction schedule for all participants. |
| Compliance | Low risk | Assessed by measuring the oil volume in returned bottles, compliance was > 80% in both groups. Both groups had increases from baseline in plasma EPA and DHA with the high‐dose group having substantially larger increases, consistent with compliance with study oil |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel (n‐3 EPA + DHA vs MUFA), 12 months Summary risk of bias: moderate to high |
|
| Participants | Adults with documented coronary heart disease N: 15 intervention, 15 control Level of risk for CVD: high Men: unclear Mean age in years (SD): 52 (9) intervention, 54 (7) control Age range: not reported Smokers: 87% intervention, 100% control Hypertension: not reported Medications taken by at least 50% of those in the control group: aspirin, beta‐blockers Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Lipid lowering medications were not allowed Location: Germany Ethnicity: not reported |
|
| Interventions | Type: fish oil capsules Comparison: EPA + DHA vs MUFA Intervention: 9 × 1 g capsules/day of fish oils (20% EPA, 15% DHA, 3.15 g/day total omega 3). Dose: 3.15 g/d EPA + DHA Control: 9 × 1 g capsules/day olive oil (which contains 6.3 g/day MUFA, 1.35 g/day SFA, 1.35 g/d total omega 6 fat) Compliance: assessed by pill counts and FA in body tissue analysis Length of intervention: 12 months |
|
| Outcomes | Main study outcome: blood lipids and FA in body tissues Dropouts: 0 intervention, 0 control Available outcomes: mortality (nil death), CVD events (nil), lipids (only TC used as the others were different at baseline), adverse events, serum fatty acids Response to contact: yes |
|
| Notes | Study funding: unclear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Unclear risk | No details. They received their initial allocation in a sealed box in person; subsequent doses arrived in the post |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No further details beyond stating "double blind" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Unclear risk | No trial register or protocol found |
| Attention | Low risk | No difference between groups |
| Compliance | Unclear risk | Measured but no results |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (EPA + DHA vs unclear), 24 months Summary risk of bias: moderate or high |
|
| Participants | Adults with Metabolic syndrome N: unclear, total randomised 101 Level of risk for CVD: low Men: 47% total, no details by group Mean age in years (SD): 55 (10) total Age range: 18‐75 years Smokers: 0% intervention, 0% control Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: unclear |
|
| Interventions | Type: supplement (fish oil capsules) Comparison: EPA + DHA vs placebo (unclear what) Intervention: fO3FA capsules 1.8 g of EPA + DHA daily. Dose: 1.8 g/d EPA + DHA Control: matching placebo supplement Compliance: not reported Length of intervention: 12 months |
|
| Outcomes | Main study outcome: change in carotid IMT Dropouts: unclear Available outcomes: lipids, insulin and glucose are stated as secondary outcomes but no usable data published Response to contact: no |
|
| Notes | Results cannot be used as numbers are not reported by study arm. Study funding: unclear, but mentions that Pfizer, NIH and "Northwest Lipids Clinic" are partners |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No data |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No data |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data |
| Selective reporting (reporting bias) | High risk | Inadequate detail in reporting as no full text publication found; Gill 2014 does give detail on carotid IMT, but not on other primary or secondary outcomes. The trial was prospectively registered (registered July 2006, unclear when recruitment started, final data collection 2011, first data published 2012). |
| Attention | Unclear risk | No data |
| Compliance | Unclear risk | No data |
| Other bias | Unclear risk | No data |
| Methods | Gruppo Italiano per la Sperimentazione della Streptochinasi nell'Infarto Miocardico – Heart Failure (GISSI‐HF) RCT, parallel, 2 arms (n‐3 EPA + DHA vs MUFA), 3.9 years Summary risk of bias: moderate or high |
|
| Participants | Patients with chronic heart failure N: 3494 intervention, 3481 control Level of risk for CVD: high Men: 77.8% intervention, 78.8% control Mean age: 67 (11) intervention,67 (11) control Age range: 18+ years Smokers: 14.4% intervention, 13.9% control Hypertension: 54.0% intervention, 55.2% control Medications taken by at least 50% of those in the control group: ACE inhibitors, beta‐blockers, diuretics Medications taken by 20%‐49% of those in the control group: spironolactone, digitalis, oral anticoagulants, aspirin, nitrates, statin Medications taken by some, but less than 20% of the control group: ARBs, other antiplatelets, calcium channel blockers, amiodarone Location: Italy Ethnicity: unclear |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs MUFA Intervention:1 capsule per day of 1 g n‐3 mainly EPA and DHA as ethyl esters in the average ratio of 1:1.2. Dose: ˜0.866 g/d EPA + DHA Control: 1 g/d matching olive oil placebo capsule Compliance: unclear Length of intervention: median 3.9 years |
|
| Outcomes | Main study outcome: time to death or admission to hospital for cardiovascular reasons Dropouts: 34 intervention, 46 control (1004 intervention and 1029 control stopped study treatment) Available outcomes: mortality, CV mortality, MI, stroke, new heart failure, incident AF, resumed arrhythmia gatalitis Response to contact: yes (no data provided) |
|
| Notes | Study funding: funders included Pfizer, AstraZeneca and others | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned (with stratification by site) to treatment groups |
| Allocation concealment (selection bias) | Low risk | Randomly assigned (with stratification by site) to treatment groups by a concealed computerised telephone randomisation system |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Double blinding stated, but taste not reported as masked and blinding of participants not checked |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All events "adjudicated blindly by an ad‐hoc committee on the basis of pre‐agreed definitions and procedures" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for attrition and exclusion were stated and addressed. Numbers in each intervention compared to numbers were similar. |
| Selective reporting (reporting bias) | Unclear risk | Published rationale and design (Tavazzi 2004) suggested primary outcomes were deaths and death or CV hospitalisation (published). Secondary outcomes not stated and no trials registry entry found |
| Attention | Low risk | Scheduled clinic visits at 1, 3, 6 months then 6 monthly until the end of the trial (for both arms) |
| Compliance | Unclear risk | No details |
| Other bias | Low risk | No further bias noted |
| Methods | Gruppo Italiano per la Sperimentazione della Streptochinasi nell'Infarto Miocardico – Prevention (GISSI‐P) RCT, 2 × 2 (n‐3 EPA + DHA vs nil), 42 months Summary risk of bias: moderate or high |
|
| Participants | People with recent (≤ 3 months) myocardial infarction N: 5666 intervention, 5658 control (99.9% follow‐up at study end) Level of risk for CVD: high Men: 85.7% intervention, 84.9% control Mean age in years (SD): 59.3 (10.6) intervention, 59.5 (10.5) years control Age range: < 50 to > 80 Smokers: 42.6% intervention, 42.3% control Hypertension: 36.2% intervention, 34.9% control Medications taken by at least 50% of those in the control group: anti‐platelet Medications taken by 20%‐49% of those in the control group: ACE inhibitors, beta‐blockers Medications taken by some, but less than 20% of the control group: lipid lowering Location: Italy Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs nil Intervention: gelatin capsules of omega‐3‐acid ethyl esters 90 (Omacor), 1/d (850‐882 mg/d EPA + DHA daily, ratio 1:2) Dose: ˜0.866 g/d EPA + DHA Control: nil (no placebo) Compliance: capsule counts, 11.6% had stopped taking Omacor by 12 months, 28.5% by the end of the study Duration of intervention: median follow‐up 40 months |
|
| Outcomes | Main study outcome: all cause mortality, CV mortality, stroke, MI Dropouts: unclear (however, all randomised were included in analyses) Available outcomes: total, sudden and CV deaths, MI, stroke, angioplasty or CABG, angina, CHD, cancer diagnosis, cancer death, combined CV events, side effects Response to contact: no |
|
| Notes | Numbers are slightly different in different publications (Lancet 1999 paper used as main source). Half of both groups were on vitamin E supplements (300 mg/d synthetic α‐tocopherol) as this was the other 2 × 2 intervention. Study funding: Bristol Meyers Squibb, Pharmacia Upjohn, Societa Produtti Antibiotici, Pfizer |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Telephone/computer network, stratified by hospital, based on a biased coin algorithm |
| Allocation concealment (selection bias) | Low risk | Randomisation by telephone with the coordinating centre |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo intervention (capsule vs nil) so participants not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "validation of clinical events ... was assured by an ad‐hoc committee of expert cardiologists and neurologists blinded to patients treatment assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Clearly described, good follow‐up (< 28% dropped out over 3.5 years) |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trials registry entry was found |
| Attention | Low risk | Slight as no placebo, otherwise similar |
| Compliance | Unclear risk | Capsule counts, 11.6% had stopped taking Omacor by 12 months, 28.5% by the end of the study |
| Other bias | Low risk | No further bias noted |
| Methods | Harvard Atherosclerosis Reversibility Project (HARP) RCT, (n‐3 EPA + DHA vs MUFA), 24 months Summary risk of bias: moderate or high |
|
| Participants | Patients with coronary heart disease N: 41 intervention, 39 control (99.9% follow‐up at study end) Level of risk for CVD: high Men: 93.5% intervention, 92.9 % control Mean age in years (SD): 62 (7) intervention, 62 (7) years control Age range: 30‐75 Smokers: 0% (exclusion criteria) Hypertension: 48% intervention, 36% control Medications taken by at least 50% of those in the control group: beta blockers, antiplatelet agents Medications taken by 20%‐49% of those in the control group: calcium channel blockers, nitrates Medications taken by some, but less than 20% of the control group: ACE inhibitors, oral hypoglycaemic drugs Location: USA Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: LCn3 vs MUFA Intervention: 12 fish oil capsules/day (Promega, Parke‐Davis) in divided doses, preferably after meals. Each fish oil capsule contained 500 mg of n‐3 polyunsaturated fatty acids composed of EPA (240 mg), DHA (160 mg) and other (100 mg) (mainly DPA) providing total daily dose of 6 g of n‐3 fatty acids. Dose: 6 g/d LCn3 Control: olive oil capsules identical in appearance to the fish oil capsules. Compliance: capsule counts and serum level measurements. Adherence averaged 80% intervention, and 90% control with significant levels of adipose n‐3 fatty acids in the fish oil group. Duration of intervention: average 28 months |
|
| Outcomes | Main study outcome: regression of coronary artery lesions Dropouts: 10 intervention, 11 control Available outcomes: all‐cause and CV deaths, fatal and non‐fatal MI, stroke, angioplasty or CABG, unstable angina, CHD, cancer diagnosis, combined CV events, side effects Response to contact: yes | |
| Notes | Study funding: National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health, Bethesda, Maryland, Warner Lambert‐Parke Davis, East Hanover, New Jersey; and by an Established Investigator Award to Dr Sacks from the American Heart Association, Dallas, Texas | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization" stratified by clinical management regime and total/HDL cholesterol ratio |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "patients and personnel responsible for lab measurements, cardiac catheterization, and analysis of angiography films were blinded to the treatment assignment". Although capsules were identical in appearance, no information on their taste and smell |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "patients and personnel responsible for lab measurements, cardiac catheterization, and analysis of angiography films were blinded to the treatment assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate over 28 months and all reasons are well documented |
| Selective reporting (reporting bias) | High risk | Trial registered retrospectively after publication |
| Attention | Low risk | Nothing in description implies the arms were treated differently |
| Compliance | Low risk | Very clear (P < 0.001) differences between arms for the 3 main n‐3 components in the fish oil |
| Other bias | Low risk | None noted |
| Methods | Healthy Eating to Reduce Overweight in people with type 2 diabetes (HERO) RCT, parallel, (n‐3 ALA vs low n‐3), 12 months Summary risk of bias: moderate or high |
|
| Participants | Overweight adults with non‐insulin treated diabetes N: 26 intervention, 24 control (analysed, intervention: 18 control: 17) Level of risk for CVD: moderate Male %: not reported Mean age in years (SD): 54 (8.7), not reported by arm Age range: 33‐70 years Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: lipid lowering drugs, oral hypoglycemics Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Australia Ethnicity: not reported |
|
| Interventions | Type: food supplement (walnuts) Comparison: ALA vs nil Intervention: 30 g/d snack portions of walnuts (provided 10% MUFA, 10% E PUFA, and a P/S ratio of 1.0) and advised not to take fish oil supplements. ALA dose not reported. Dose: ˜3 g/d ALA based on 30 g/d intake of walnuts Control: no supplements Both groups were given low‐fat isocaloric dietary advice (30% E fat (10% E SFA, 15% E MUFA; 5% E PUFA, P/S ratio of 0.5), 20% E protein and 50% E CHO) plus advice to brisk walk 30 min × 3 times/week Compliance: measured by erythrocyte membrane fatty acid levels which were similar in both groups Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: change in body weight and % body fat Dropouts: 8 intervention, 5 control Available outcomes: all cause mortality (nil deaths), weight, visceral adipose tissue, lipids, glucose, insulin, HbA1c (body fat % and subcutaneous adipose tissue measured but too different at baseline to use) Response to contact: not yet attempted |
|
| Notes | Body fat % was too different between groups at baseline hence data not used Study funding: California Walnuts Commission |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted using a computerised random number generator by a researcher independent of the subject interface. |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Subjects, but not dietitians, were blinded to the type of overall diet (a prepackaged 30 g snack portion of walnuts was given to the walnut group unbeknown to the controls)". However, there was no placebo supplement, so blinding easily broken |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Paper states "code was concealed from the researchers collecting data, as well as from subjects." However as participants could not be blinded outcome assessors may not have been (problem for measures of adiposity, not for biochemical measures) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout rate 35 of 50 analysed (30% attrition rate) |
| Selective reporting (reporting bias) | Unclear risk | Trial was registered postanalysis |
| Attention | Low risk | Both groups appear to have had same level of attention |
| Compliance | High risk | ALA levels almost exactly the same in intervention and control |
| Other bias | Low risk | None noted |
| Methods | Japan Eicosapentaenoic acid Lipid Intervention Study (JELIS) RCT, parallel, 2‐arm (EPA capsule vs nil), 5 years Summary risk of bias: moderate or high |
|
| Participants | People with hypercholesterolaemia N: intervention, 9326, control 9319 (analysed intervention 9326, control 9319) Level of risk for CVD: moderate (Patients with hypercholesterolaemia) Men: 32% intervention, 31% control Mean age in years (SD): 61 (8) intervention 61 (9) control Age range: 40‐75 years Smokers: 20% intervention, 18% control Hypertension: 36% intervention, 35% control Medications taken by at least 50% of those in the control group: statins Medications taken by 20%‐49% of those in the control group: calcium channel blockers, other antihypertensives Medications taken by some, but less than 20% of the control group: beta‐blockers, antiplatelet, hypoglycemics, nitrates Location: Japan Ethnicity: Japanese |
|
| Interventions | Type: supplement (EPA capsule) Comparison 1: EPA vs nil Intervention: 3 × 2 × 300 mg capsules/d EPA ethyl ester (total dose of 1.8 g/d EPA), after meals. Dose: 1.8 g/d EPA Control: nothing (though all in both groups received "appropriate" dietary advice). All patients in both groups were on statins. Compliance: monitored by local physicians and measuring plasma fatty acids concentrations. Study drug regimens, 71% adhered EPA intervention, 73% adhered EPA control, 74% adhered statin Duration of intervention: maximum 5 years, mean 4.7 (1.1) years |
|
| Outcomes | Main study outcome: major coronary events Dropouts: 1766 intervention, 1582 control (but all had endpoint evaluation) Available outcomes: major coronary events: sudden cardiac death, fatal or non‐fatal MI, unstable angina, angioplasty or CABG. Also all‐cause mortality, stroke, peripheral artery disease, cancer, lipids, rise in blood sugar, fasting glucose, HbA1c Response to contact: no |
|
| Notes | Study funding: Mochida Pharmaceutical Company | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Statistical co‐ordination centre: "permitted block randomisation with a block size of 4" |
| Allocation concealment (selection bias) | Low risk | Centralised. Statistical coordinating centre (see above) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded as there was no placebo. Quote: "[o]pen label blinded end point" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Clinical endpoints ... reported by local physicians were checked by members of a regional organizing committee in a blinded fashion. Then an endpoints adjudication committee ... confirmed them once a year without knowledge of the treatment allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Well documented, dropout numbers low |
| Selective reporting (reporting bias) | Unclear risk | NCT00231738 registered October 2005, recruitment November 1996 to November 1999, main results published 2007. Rationale and design paper published in 2003 (reported baseline characteristics, so before completed follow‐up, but after data collection began). All reported outcomes appear to have been published. |
| Attention | Low risk | Slight, as no placebo provided to control group, but only capsules to intervention group. Otherwise 2 groups appeared to be treated equally |
| Compliance | Unclear risk | Monitored by local physicians and measuring plasma fatty acids concentrations. Study drug regimens,71% adhered EPA intervention, 73% adhered EPA control, 74% adhered statin |
| Other bias | Low risk | No further bias noted |
| Methods | RCT, parallel, (fish oil vs nil), 12 months Summary risk of bias: moderate or high |
|
| Participants | Patients with persistent atrial fibrillation (AF) on warfarin N: 92 intervention, 90 control (91 and 87 analysed ITT) Level of risk for CVD: high Male %: 82.4 intervention, 72.4 control Mean age in years (SD): 63 (10) intervention, 61(13) control Age range: 18‐85 years (inclusion criteria) Smokers: 22.2% intervention, 11.5% control Hypertension: 45.6% intervention, 58.6% control Medications taken by at least 50% of those in the control group: anti‐arrhythmic drugs, renin‐angiotensin system inhibitors Medications taken by 20%‐49% of those in the control group: statins Medications taken by some, but less than 20% of the control group: not reported Location: Australia Ethnicity: not reported |
|
| Interventions | Type: fish oil capsule Comparison: EPA + DHA vs nil Intervention: 6 capsules/day of a fish oil preparation containing a total dose of 1.02 g of EPA and 0.72 g DHA. Participants in the omega‐3 group were asked to continue fish oils till a maximum of 1 year or till return of persistent AF. Dose: 1.7 g/d EPA + DHA Control: no supplements. Patients were advised not to take any fish oil supplements. All patients underwent cardioversion following randomisation. Compliance: was monitored on a weekly basis via telephone and during follow‐up by using a pill count plus serum EPA and DHA levels which were significantly increased Duration of intervention: 1 year (or AF recurrence) |
|
| Outcomes | Main study outcome: atrial fibrillation recurrence Dropouts: 4 intervention, 0 control Available outcomes: all‐cause mortality (nil death), AF recurrence, time to AF recurrence, adverse events Response to contact: contact not yet established |
|
| Notes | Study funding: the study was funded in part by the National Heart Foundation of Australia and the Pfizer Cardiovascular Lipid Research Grant. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were randomised to a control or an omega‐3 group in a 1:1 fashion (no details of method) |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label with no placebo control |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open label |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis was conducted |
| Selective reporting (reporting bias) | Unclear risk | Trial registered 2005 but data collection started 2003 |
| Attention | Unclear risk | Intervention group had capsules, while control group did not. Potential for greater contact and checking with intervention group on this basis, although otherwise both groups seem to have had the same care. |
| Compliance | Low risk | EPA and DHA levels were significantly higher in intervention group |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (fish oil vs nil), 12 months Summary risk of bias: moderate or high |
|
| Participants | Patients > 60 years with sinoatrial node disease and dual chamber pacemakers N: 39 intervention, 39 control randomised (18 intervention vs 39 control at 12 months) Level of risk for CVD: moderate/high Male %: 46% intervention, 56% control Mean age in years (SD): 78 (7) intervention, 77(8) control Age range: not reported Smokers: not reported Hypertension: 72% Medications taken by at least 50% of those in the control group: statin, renin‐angiotensin system inhibitors Medications taken by 20%‐49% of those in the control group: anti‐arrhythmic drugs Medications taken by some, but less than 20% of the control group: not reported Location: Australia Ethnicity: not reported |
|
| Interventions | Type: omega 3 capsule Comparison: EPA + DHA vs nil Intervention: a triglyceride preparation containing a total of 6 g/day of omega‐3 polyunsaturated fatty acids of which 1.8 g/day were n‐3 (1.02 g EPA and 0.72 g DHA). Dose: 1.8 g/d EPA + DHA Control: no supplements Compliance: measured by weekly dietary history and pill count. Fatty acid status measured at randomisation and between 1‐3 months post randomisation (blood samples). Duration of intervention: median 378 days |
|
| Outcomes | Main study outcome: atrial fibrillation burden Dropouts: 1 intervention, 0 control Available outcomes: all cause mortality, CV mortality, AF (frequency and duration but not recurrence so not used), adverse events Response to contact: written but no contact yet |
|
| Notes | Study funding: unclear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using sequentially numbered, opaque, sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label design |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "At each visit, stored AT/AF diagnostic data were retrieved in an un‐blinded fashion" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 1 lost, and reason explained. 21 of the 39 randomised to the intervention were crossed over to control at 6 months so 12‐month outcomes are reported for 17/18 intervention while baseline characteristics are reported for the 39 patients. |
| Selective reporting (reporting bias) | Low risk | Trial prospectively registered and outcomes stated were reported |
| Attention | Unclear risk | As only the intervention group had supplements there was potential for attention differences. Other contact appears the same. |
| Compliance | Low risk | EPA was 3‐fold higher and DHA 1.8 fold higher compared with controls. EPA and DHA did not change significantly in controls upon repeat testing |
| Other bias | High risk | Odd design – 21 of the 39 randomised to the intervention were crossed over to control at 6 months |
| Methods | RCT‐ parallel, 2 arms (omega 3 vs corn oil), 12 months Summary risk of bias: low |
|
| Participants | People with Crohn's disease in remission (but with a recent relapse) N: 70 intervention, 63 control Level of risk for CVD: low Men: 35.7% intervention, 27.0% control Mean age in years (SD): 29.5 (9.6) intervention, 31.8 (10.9) control Age range: 17‐62 years intervention, 17‐65 years control Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: methylprednisolone (all for 1st 8 weeks) Medications taken by 20%‐49%: not reported Medications taken by some, but < 20%: not reported Location: Germany Ethnicity: not reported |
|
| Interventions | Type: supplement (fish oil) Comparison: EPA + DHA vs omega 6 Intervention: 2 × 3 1 g gelatin capsules/d of ethylester fish oil concentrate (3.3 g/d EPA + 1.8 g/d DHA). Dose: 5.1 g/d EPA + DHA Control: 2 × 3 1 g gelatin capsules/d of corn oil Compliance: pill count, 5 non‐compliant patients, among compliant patients, 18 were censored (for not using the medication for 3 continuous weeks) Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: Crohn's disease duration of remission Dropouts: unclear Available outcomes: mortality (nil), Crohn's disease activity and relapses, serum triglycerides Response to contact: yes (methodological details provided) |
|
| Notes | There was a third arm of dietary advice (for low CHO diet) Study funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised within the centres in blocks of six (block size blinded to the centres) |
| Allocation concealment (selection bias) | Low risk | Author reported allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Double blind conditions were intended for the verum‐placebo comparisons". Author stated that capsules were identical in appearance (taste not mentioned). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Primary outcome was relapses "classified in a blind fashion by a primary end‐point committee" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants were accounted for based on the main outcome of the study (relapses), however 20% omitted from analyses and numbers confusing |
| Selective reporting (reporting bias) | Unclear risk | No trials registry entry or protocol found |
| Attention | Low risk | All patients were seen by their physician in the respective centre after regular time intervals (1, 2, 3, 6, 9 and 12 months). |
| Compliance | Unclear risk | Pill count, 5 non‐compliant patients, among compliant patients, 18 were censored (for not using the medication for three continuous weeks). 23 of 133 non‐compliant |
| Other bias | Low risk | None noted |
| Methods | Multidomain Alzheimer Preventive Trial (MAPT) 4 arms RCT, parallel, (n‐3 ± multidomain intervention vs placebo ± multidomain intervention), 36 months Summary risk of bias: low |
|
| Participants | Population: people aged at least 70 years without dementia but with memory complaint, IADL limitation or slow gait speed N: 840 intervention (arms 1 and 3), 840 control (arms 2 and 4) randomised. Numbers analysed differ by outcome. Level of risk for CVD: low Men: 37.2% intervention, 34.5% control. (combined groups) Mean age in years (SD): 75.6 (4.7) and 74.4 (4.4) intervention, 75.1 (4.3) and 75 (4.1) control Age range: not reported Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: France and Monaco Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs paraffin oil (non‐fat) Intervention Arm 1: omega‐3 (V0137 CA 800 mg/d DHA; 225 mg/d EPA in soft caps). Dose for arms 1 and 3: 1.025 g/d EPA + DHA Arm 3: omega 3 (V0137 CA 800 mg/d DHA; 225 mg/d EPA in soft caps) plus multi‐domain intervention (nutrition, physical exercise, cognitive stimulation, social activities) Control: Arm 2: placebo capsules containing flavoured paraffin oil. All capsules were supplied by Pierre Fabre Médicament (Castres, France) Arm 4: placebo capsules plus multi‐domain intervention (nutrition, physical exercise, cognitive stimulation, social activities) Compliance: adherence to study interventions was assessed every 6 months. For supplementation, adherence was assessed by counting the number of capsules returned by participants (or based on treatment dates if the number of capsules was missing). Furthermore, biological samples were obtained at baseline and after 12 months to assess concentrations of DHA and EPA in red blood cell membranes. Duration of intervention: 36 months |
|
| Outcomes | Main study outcome: change in cognitive function ) Dropouts: 200 intervention, 194 control Available outcomes: mortality, CVD events, haemorrhagic stroke, adverse events, functional capacity, other cognitive functions, safety and tolerability Response to contact: no |
|
| Notes | Study funding: Gérontopôle of Toulouse, the French Ministry of Health (PHRC 2008, 2009), the Pierre Fabre Research Institute (manufacturer of the polyunsaturated fatty acid supplement), Exhonit Therapeutics, and Avid Radiopharmaceuticals | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned (1:1:1:1) to the combined intervention (i.e. the multidomain intervention plus polyunsaturated fatty acids), the multidomain intervention plus placebo, polyunsaturated fatty acids only, or placebo only. A computer‐generated randomisation procedure (done by ClinInfo, a subcontractor) was used with block sizes of 8 and stratification by centre. |
| Allocation concealment (selection bias) | Low risk | A clinical research assistant, who was not involved in the assessment of participants, used a centralised interactive voice response system to identify which group to allocate the participant to, and which lot number to administer. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All participants and study staff were blinded to polyunsaturated fatty acid or placebo assignment – both sets of capsules looked and tasted identical. In view of the nature of the multidomain intervention, the study was unblinded for this component, but the independent neuropsychologists who were trained to assess cognitive outcomes were blinded to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All participants and study staff were blinded to polyunsaturated fatty acid or placebo assignment—both sets of capsules looked and tasted identical. In view of the nature of the multidomain intervention, the study was unblinded for this component, but the independent neuropsychologists who were trained to assess cognitive outcomes were blinded to group assignment. Data analysts were not blinded to group assignment, but two data managers, one statistician (CC) and two physicians (SA and BV) did a blinded data review. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1680 participants were enrolled and randomly allocated, the modified intention‐to‐treat population (N = 1525), i.e. 155 excluded (9% over 3 years) |
| Selective reporting (reporting bias) | Low risk | Protocol registered ClinicalTrials.gov (NCT00672685) – outcomes match report. Because of advances in the field since our trial was designed in 2007, we decided to modify the primary outcome from one cognitive test to a composite cognitive score, which is now thought to be a better endpoint. This protocol amendment was submitted to the local ethical committee on 2 February 2015 and was subsequently approved |
| Attention | Low risk | Both groups assessed at baseline, 6, 12, 24, 36 months. Groups 1 and 2 only differed by content of capsules. |
| Compliance | Unclear risk | Adherence to study interventions was assessed every 6 months, by counting the number of capsules returned (or based on treatment dates if the number of capsules was missing). Biological samples were obtained at baseline and after 12 months to assess concentrations of DHA and EPA in red blood cell membranes, but outcomes not reported. |
| Other bias | Low risk | None noted |
| Methods | Mediterranean alpha‐linolenic enriched Groningen dietary intervention study (MARGARIN) RCT, factorial 2 × 2 (ALA rich margarine vs LA rich margarine, also nutrition education vs no education but this is not included), 2 years Summary risk of bias: low |
|
| Participants | Hypercholestrolemic adults with 2 or more CVD risk factors N: total 282 randomised; 114 intervention (51 with nutrition education, 58 without NE) 157 control (52 with NE, 105 without NE) Level of risk for CVD: moderate (multiple cardiovascular risk factors, 10‐year IHD risk ˜20%) Men: 41.9% intervention, 45.7% control Mean age in years (SD): 54.4 (9.5) intervention, 53.9 (9.8) control Age range: 30‐70 Smokers: 49.1% intervention, 49.3% control Hypertension: 52.9% intervention, 45.3% control (on anti‐hypertensives) Medications taken by at least 50% of those in the control group: antihypertensives Medications taken by 20%‐49%: not reported Medications taken by some, but < 20%: not reported Location: the Netherlands Ethnicity: not reported |
|
| Interventions | Type: supplementary food (ALA enriched margarine) Intervention: provided with ALA rich margarine (80% fat of which 15% was ALA and 46% LA) to be eaten ad libitum. Dose: average intake 6.3 g/d ALA (was also 1 g/d ALA in the control group). Control: provided with linoleic rich margarine (80% fat of which 0.3% was ALA and 58% LA), identical in taste and packaging. Both margarines contained 0.66 mg vit E/g, 9 micro‐g vit A/g and 0.023 micro‐g vit D/g Comparison: ALA vs omega 6 Compliance: serum fatty acids used to assess, ALA rose by 0.47 mol % (SD 0.04) and 0.36 mol% (SD 0.04) intervention arms (with and without NE) and fell by 0.06 mol % (SD 0.04) and 0.11 mol % (SD 0.03) control arms (with and without NE), significantly different. Duration of intervention: 24 months |
|
| Outcomes | Main study outcome: cardiovascular risk factors and IHD risk Dropouts: unclear Available outcomes: total and CV deaths, non‐fatal MI, stroke, CABG and angioplasty, BMI, lipids, BP Response to contact: yes | |
| Notes | Study funding: Prevent fund and Unilever Research Other intervention (2 × 2) was educational, teaching a multifactorial dietary intervention. It was excluded as multifactorial. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random allocation, allocated by an independent trial coordination centre that organised masked distribution of margarines |
| Allocation concealment (selection bias) | Low risk | Allocated by an independent trial coordination centre which organised masked distribution of margarines |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind; the 2 margarines are described as identical as to taste and packaging (though not reported as checked) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | 2 independent physicians, a cardiologist and a general practitioner validated and classified results in a blinded fashion |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The number randomised to each arm was unclear, but one publication clarifies (55 randomised to each arm, 51 intervention and 52 control analysed). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trials registry entry was found. |
| Attention | High risk | There was no difference in attention between margarine types, but the dietary advice group spent more time with study staff than the control group, and some (not quite randomly allocated) were sent individual motivational letters (Siero 2000). |
| Compliance | Low risk | Serum fatty acids used to assess, ALA rose by 0.47 mol% (SD 0.04) and 0.36 mol % (SD 0.04) intervention arms (with and without NE) and fell by 0.06 mol % (SD 0.04) and 0.11 mol % (SD 0.03) control arms (with and without NE), Significantly different |
| Other bias | Low risk | No further bias noted |
| Methods | Modulation of Atherosclerosis Risk by Increasing dose of n‐3 fatty Acids (MARINA) RCT, parallel, 4 arms (n‐3 PUFA 3 different doses or olive oil placebo), 12 months Summary risk of bias: low |
|
| Participants | Non‐smoking men and women aged 45‐70 years N: intervention. 279 in 3 groups (G1 0.45 g/d n = 94, G2 0.9 g/d n = 93, G3 1.8 g/d n = 92); control: 88 (analysed G1 0.45 g/d n = 81, G2 0.9 g/d n = 80, G3 1.8 g/d n = 80, control 71) Level of risk for CVD: low Men: 38.7% intervention, 38.6% control Mean age in years (CI): G1: 55 (53, 56), G2: 55 (54, 56), G3: 55 (54, 57) intervention 55 (54,57) control Age range: 45‐70 Smokers: 0% intervention, 0% control Hypertension: 5.4% intervention, 5% control Medications taken by at least 50% of those in the control group: none Medications taken by 20%‐49% of those in the control group: none Medications taken by some, but less than 20% of the control group: statins, antihypertensives, HRT, thyroxine Location: UK Ethnicity: G1: white 80.9%, black 4.3%, Asian 6.4%, East Asian 4.3%, other 4.3% G2: white 78.5%, black 6.5%, Asian 10.8%, East Asian 0%, other 4.3% G3: white 85.9%, black 1.1%, Asian 2.2%, East Asian 4.3%, other 6.5% Control: white 77.3%, black 10.2%, Asian 6.8%, East Asian 2.3%, other 3.4% |
|
| Interventions | Type: supplement (fish oil capsules) Comparison 1: EPA + DHA vs MUFA Comparison 2: high EPA + DHA vs low EPA + DHA Intervention: 3 × 1 g oil gelatin capsule/day consisting of blend of EPA concentrate, DHA concentrate, refined olive oil and 0.1% peppermint oil. Providing a daily dose of: 0.45 g, 0.9 g, or 1.8 g per day (all with EPA/DHA ratio of 1.51). Dose: 1.8 g/d EPA + DHA (G3 used for outcomes) Control: 3 gelatin capsules/ day containing refined olive oil + 0.1% peppermint oil Compliance: measured by capsule counting and erythrocyte lipids for proportion of EPA/DHA @ baseline, 6 months, 12 months. 88.5% of participants consumed > 90% of capsules provided. EPA and DHA in erythrocyte lipids increased in dose‐dependent manner compared with placebo, indicating long‐term compliance with intervention. Length of intervention: 12 months |
|
| Outcomes | Main study outcome: endothelial function, arterial stiffness Dropouts: 38 intervention (13,13,12), 17 control Available outcomes: lipids, dietary intake, CRP, BP (supine and ambulatory – numeric data not provided, but study states that there were no significant differences between arms). Weight data not used as baseline is different between groups (FMD, arterials stiffness, carotid intima media thickness, heart rate variability, heart rate, endothelial progenitor cells reported but not used) Contact with authors: yes (many outcomes above provided in end of study report from authors) |
|
| Notes | Outcome data used G3 (highest dose) vs placebo for continuous outcomes and combined the 3 intervention groups vs placebo for dichotomous outcomes Study funding: Food Standards Agency |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the random allocation sequence was generated with a computer program by using the process of minimisation to balance age, sex and ethnicity between treatment groups." |
| Allocation concealment (selection bias) | Low risk | Quote: "We enrolled eligible participants and the study database program allocated a serious of capsules to the participant. The treatments associated with the capsule codes were concealed from all investigators and associated clinical staff until the data analysis was complete. The code breaker was an employee of MedSciNet who constructed the trial database." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "We enrolled eligible participants and the study database program allocated a serious of capsules to the participant. The treatments associated with the capsule codes were concealed from all investigators and associated clinical staff until the data analysis was complete. The code breaker was an employee of MedSciNet who constructed the trial database." "blends of the test fat with 0.1% peppermint oil to disguise the fish taste of the EPA and DHA" (peppermint oil in both intervention and control capsules) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "We enrolled eligible participants and the study database program allocated a serious of capsules to the participant. The treatments associated with the capsule codes were concealed from all investigators and associated clinical staff until the data analysis was complete. The code breaker was an employee of MedSciNet who constructed the trial database." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 15% withdrawal, reasons for attrition reported |
| Selective reporting (reporting bias) | Low risk | Outcomes published match trials register. Registered September 2008, trial started June 2008, ended December 2010, main publication 2011 |
| Attention | Low risk | No difference between groups |
| Compliance | Low risk | Statistically significant difference in erythrocyte omega 3 fats at 12 months between different arms |
| Other bias | Low risk | None noted |
| Methods | Metabolism, Exercise and Nutrition at UCSD (MENU) RCT, parallel, (walnut rich moderate fat diet vs moderate fat diet), 12 months Summary risk of bias: moderate or high |
|
| Participants | Overweight and obese women, of whom half were insulin resistant N: 82 intervention, 81 control (analysed, intervention: 65 control: 61) Level of risk for CVD: low Men: 0% intervention, 0% control Mean age (SD) years: 51 (NR) intervention, 50 (NR) control Age range: 22‐67 years intervention, 25‐72 years control Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: 10% were on cholesterol medications Location: USA Ethnicity: Hispanic 18% intervention, 14% control; black 9% intervention, 3% control; Asian American 1% intervention, 4% control; white non‐Hispanic 71% intervention, 78% control. |
|
| Interventions | Type: food and advice Comparison: walnut rich moderate fat diet (ALA) vs moderate fat diet (MUFA) Intervention: advice to follow walnut‐rich higher fat diet (35%E fat with limited SFA, MUFA encouraged, including 42 g/d walnuts (provided by study), 45%E CHO, 20%E protein). Participants given print materials on diet and exercise, attended group sessions weekly for 1st 4 months, biweekly for next 2 months, then monthly to 1 year), provided web‐based tracking for dietary constituents, scale, pedometer, measuring cups and exercise videos. Regular dietetic and group leader support. Clinic visits were at 0, 6 and 12 months. Dose: ˜4.2 g/d ALA (calculated based on 42 g/d intake of walnuts) Control: exactly as intervention for goals, materials and support except higher fat diet did not include walnuts (35% E fat with limited SFA, MUFA encouraged, 45%E CHO, 20%E protein) Compliance: walnut consumption reported on form and nuts provided. Red blood cell ALA significantly higher in intervention at 12 months than control Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: body weight Dropouts: 13 of 82 intervention, 12 of 81 control Available outcomes: weight, waist circumference, HDL and LDL cholesterol, triglycerides, insulin, glucose, HOMA‐IR, HOMA‐beta, CRP and IL‐6 (estradiol, SHBG, nutrient gene interactions, physical activity and heart rate also presented) Response to contact: no reply received to date |
|
| Notes | Study funding: National Cancer Institute and California Walnut Commission | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation stratified by age and insulin resistance |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open study, participants were advised on their diets extensively |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not mentioned, so unclear for their primary outcome, weight |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Paper states ITT analysis but 25 dropouts (15%) not included in 1 year data, but dropout reasons clear |
| Selective reporting (reporting bias) | Low risk | Pre‐registered, all mentioned outcomes reported at 12 months |
| Attention | Low risk | Appear very equal |
| Compliance | Low risk | Statistically significant difference between intervention and control arms for ALA in blood cell membranes at 12 months |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (EPA capsules vs nil), 2 years Summary risk of bias: moderate to high |
|
| Participants | Japanese type 2 diabetics N: intervention. 40, control: 41 (analysed 30, 30) Level of risk for CVD: moderate Men: 53% intervention, 67% control Mean age in years (SD): 59 (11.2) intervention 61.2 (8.4) control Age range: not reported Smokers: 40% intervention, 43% control Hypertension: not reported Medications taken by at least 50% of those in the control group: oral hypoglycemics Medications taken by 20%‐49% of those in the control group: insulin, lipid lowering drugs, antihypertensives Medications taken by some, but less than 20% of the control group: antithrombotics Location: Japan Ethnicity: 100% Japanese |
|
| Interventions | Type: supplement (EPA oil capsules) Comparison: EPA vs nil Intervention: 1800 mg/d EPA EPADEL capsules (Mochida Pharmaceutical Co Ltd Japan)‐ 98% pure ethyl‐ester EPA (unclear how many caps). Dose: ˜1.8 g/d EPA Control: no intervention Compliance: checked during 3 month reviews throughout trial and 5 participants were excluded for poor compliance but no details on method or results Length of intervention: mean 2.1 (0.2) years |
|
| Outcomes | Main study outcome: progression of diabetic macroangiopathy measured by carotid intima‐media thickness and brachial‐ankle pulse wave velocity Dropouts: 10 intervention, 11 control Available outcomes: BMI, lipids, BP, HbA1c, cancer diagnosis Response to contact: not yet attempted |
|
| Notes | Blood pressure data not used as groups are different at baseline Study funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients randomly divided into 2 groups matched for age and gender |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors of main study outcomes were blinded to the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate (26%) over 2 years. All dropouts explained, however, 5 were excluded for poor compliance but no clear predefined protocol for exclusion |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Attention | Low risk | All participants had the same contact |
| Compliance | Unclear risk | Compliance measured but no clear methods or reported results |
| Other bias | Low risk | None noted |
| Methods | Nutritional AMD Treatment‐2 (NAT2) RCT, parallel, (EPA + DHA vs MUFA), 36 months Summary risk of bias: low |
|
| Participants | Patients with early age related macular degeneration N: 150 intervention, 150 control Level of risk for CVD: high (92.5% intervention and 79.8 controls had past CVD) Men: 31.3% intervention, 39.5% control Mean age in years (SD): 73.9 (6.6) intervention, 73.2 (6.8) control Age range: 55‐85 Smokers: 6.7% intervention, 8.5% control Hypertension: 58% total (not reported by study arm) Medications taken by at least 50% of those in the control group: lipid‐lowering medication Medications taken by 20%‐49% of those in the control group: agents acting on renin‐angiotensin system, anti‐inflammatory and anti‐rheumatic products Medications taken by some, but less than 20% of the control group: insulin or blood sugar lowering drugs Location: France Ethnicity: unclear |
|
| Interventions | Type: supplement (fish oil capsule) Comparison: EPA + DHA vs MUFA Intervention: 3 daily fish oil capsules containing 1110 total n‐3 FAs (EPA: 270 mg/day DHA: 840 mg/day) and vit E: 6 mg/day. Dose: 1.1 g/d EPA + DHA Control: 3 × 602 mg olive oil capsules a day containing 0.2 g total PUFA and vit E: 0.09 g/d Compliance: assessed during visits from unused capsules and serum PUFA levels. Overall compliance over the 3 years; 69.4% intervention, 70.5% control Length of intervention: 36 months |
|
| Outcomes | Main study outcome: time to occurrence of choroidal new vessels (CNV) in the study eye from prospective assessment of fluorescein angiography Dropouts: 29 intervention, 34 control Available outcomes: all cause mortality, plasma lipids, adverse events, serum FAs Response to contact: yes (no added data) |
|
| Notes | TG data not used as presented as median (5th‐95th percentile) Study funding: Laboratoire Chauvin, Bausch & Lomb Inc |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | QL Ranclin software was used to generate the randomisation list before enrolment. The patients and the study personnel both were blinded to the treatment assignment |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The capsules had the same appearance, the same size, and the same weight (602 mg) in both DHA and placebo groups. No masking flavour was added to the capsules, which were otherwise odourless |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Author confirmed blinding of outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Any temporary discontinuation of the treatment was considered to be a deviation from the study protocol. Discontinuation for more than 5 months was considered to be a major deviation from the study protocol. Participants who dropped out were taken in account in the survival analysis and occurrence of CNV and were counted at last angiography performed. |
| Selective reporting (reporting bias) | Unclear risk | ISRCTN98246501. Retrospectively registered May 2007, recruitment started December 2003, completed November 2008, key publication 2013 |
| Attention | Low risk | Same amount of time spend with both study arms |
| Compliance | Low risk | Assessed during visits from unused capsules and serum PUFA levels. Overall compliance over the 3 years; 69.4% intervention, 70.5% control |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (DHA + EPA vs MUFA), 12 months Summary risk of bias: moderate or high |
|
| Participants | Patients with persistent atrial fibrillation with at least 1 relapse after cardioversion N: 102 intervention, 103 control. (analysed, intervention: 94 control: 94) Level of risk for CVD: high Men: 70% intervention, 63% control Mean age in years (SD): 70 (6) intervention, 69 (9) control Age range: not reported (18‐80 inclusion criteria) Smokers: 10% intervention, 9.1% control Hypertension: 47% intervention, 40% control Medications taken by at least 50% of those in the control group: beta‐blockers, ACE inhibitors, anticoagulant therapy, amiodarone Medications taken by 20%‐49% of those in the control group: diuretics, antiplatelet, statins Medications taken by some, but less than 20% of the control group: calcium channel blockers Location: Italy Ethnicity: not reported |
|
| Interventions | Type: supplement (omega‐3‐acid ethyl esters 90: Omacor) Comparison: EPA + DHA vs MUFA Intervention: 2 × 1 g/d Omacor (total 1.7 g/d EPA + DHA at a ratio of 0.9 to 1.5). Dose: 1.7 g/d EPA + DHA Control: 2 × 1 g/d olive oil (gelatin capsules identical in appearance to Omacor) Compliance: no details Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: probability of maintenance of sinus rhythm Dropouts: 6 intervention, 5 control Available outcomes: adverse events, AF recurrence (nil death) Response to contact: no |
|
| Notes | Study funding: 'Centro per lo Studio ed il Trattamento dello Scompenso Cardiaco' of the University of Brescia, Brescia, Italy. The work of Dr Campia was supported by National Institutes of Health grant K12 HL083790‐01a1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment followed a computer‐generated randomisation list obtained using blocks of size 4 |
| Allocation concealment (selection bias) | Low risk | The randomisation schedule was kept in the research pharmacy area and was available only to unblinded pharmacy personnel until after the database was locked. At that time, the unblinded patient treatment information was made available to the investigators. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo gelatin capsules identical in appearance to Omacor. However no information provided as to their smell and taste. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised were accounted for. ITT analysis for main outcomes |
| Selective reporting (reporting bias) | Unclear risk | NCT01198275. Registered retrospectively in September 2010, study started January 2006, completed May 2008, main publication 2011 |
| Attention | Low risk | No difference between groups |
| Compliance | Unclear risk | No details |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (DHA + EPA vs MUFA), 12 months Summary risk of bias: moderate or high |
|
| Participants | People with heart failure (non‐ischaemic dilated cardiomyopathy) N: 67 intervention, 66 control. (analysed, intervention: 67 control: 66) Level of risk for CVD: high Men: 95.5% intervention, 84.9% control Mean age in years (SD): 61 (11) intervention, 64 (9) control Age range: not reported (18‐75 inclusion criteria) Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: beta‐blockers, ACE inhibitors, furosemide, amiodarone, aldosterone blockers Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: statins, ARB Location: Italy Ethnicity: not reported |
|
| Interventions | Type: supplement (Omacor) Comparison: EPA + DHA vs MUFA Intervention: 2 × 1 g/d Omacor (1.7 g/d EPA + DHA at a ratio of 0.9 to 1.5) Control: 2 × 1 g/d olive oil (gelatin capsules identical in appearance to Omacor) Compliance: pill counts – participants were withdrawn if < 80% capsules taken (none were withdrawn). Fatty acid EPA + DHA 0.83% in intervention group, 0.41% in control group. Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: left ventricular function and functional capacity Dropouts: 0 intervention, 0 control Available outcomes: mortality (nil death), combined CVD events, AF, BMI, hospitalisation for cardiovascular reasons, hospitalisation for worsening heart failure, lipids, blood glucose (but too different at baseline to use), serum cytokine Response to contact: yes |
|
| Notes | Study funding: Centro per lo Studio ed il Trattamento dello Scompenso Cardiaco, one author was a consultant for 8 pharmaceutical companies | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomised" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Paper states that placebo and verum were identical and that the study was double blind, but blinding of participants not checked. Author confirmed investigators not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Author confirmed assessors not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear whether all participants were assessed for all outcomes (e.g. hospitalisation), but some outcomes report no attrition |
| Selective reporting (reporting bias) | Unclear risk | NCT01223703 – study registration October 2010, recruitment November 2007 to June 2009. Retrospective |
| Attention | Low risk | No suggestion of this, and investigators appeared blinded (so could not differ in attention provided by allocation) |
| Compliance | Low risk | See characteristics table |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (MorDHA capsules vs unclear placebo), 14 months Summary risk of bias: moderate or high |
|
| Participants | Patients with chronic traumatic spinal cord injury N: 55 intervention, 55 control. (analysed, intervention: 54 control: 50) Level of risk for CVD: low Men: 81.5% intervention, 82% control Mean age in years (SD): 51.15 (13.43) intervention, 54.12 (11.76) control Age range: 15‐74 years intervention, 30‐74 years control Smokers: 0% (exclusion criteria) Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Iran Ethnicity: not reported |
|
| Interventions | Type: supplement (n‐3 capsules) Comparison: EPA + DHA vs placebo (unclear what) Intervention: 2 MorDHA capsules (providing 870 mg DHA and 130 mg EPA) per day. Dose: 1 g/d DHA + EPA Control: 2 placebo capsules per day. Both capsules were similar in colour, shape, and taste. Both groups received one calcium capsules per day consisting of 1000 mg calcium and 400 IU vitamin D. Compliance: pill counts – compliance averaged 80% in both groups Duration of intervention: 14 months |
|
| Outcomes | Main study outcome: professionals evaluation of neurological function Dropouts: 1 intervention, 5 control Available outcomes: functional measures (total and sub‐scales), BMI, leptin and adiponectin concentration. Response to contact: no |
|
| Notes | Study funding: PhD university funding. Omega 3 capsules were provided by Minami Nutrition Co (Aartselaar, Belgium) and placebo capsules were supplied by Zahravi Pharmaceutical Co. (Tabriz, Iran). Calcium capsules were provided by Darou Pakhsh Pharm Co. (Tehran, Iran) Data were collected at the beginning of the study and after 14 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using permuted balanced block randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No further detail on allocation |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Stated as double blind but content of placebo not stated and no report of attempt to mask n‐3 FA taste. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Unclear, few details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was 1 in intervention group, 5 in control group, so minor. "the two most common reasons for dropouts were experiencing GI side effects or difficulty to maintain scheduled clinic visits" |
| Selective reporting (reporting bias) | High risk | Some of the outcomes stated in the trial register are not reported. Registered March 2011, study start November 2010, completion April 2012 |
| Attention | Low risk | No difference between groups |
| Compliance | Unclear risk | Pill counts – compliance averaged 80% in both groups |
| Other bias | Low risk | None noted |
| Methods | Norwegian Vegetable Oil Experiment of 1965‐6 RCT, parallel, 2 arms (ALA linseed oil vs omega 6 sunflower oil), 1 year Risk of bias: moderate or high |
|
| Participants | Men working in Norwegian companies aged 50‐59 years N: 6716 intervention, 6690 control Level of risk for CVD: low (working men, though a few had had a previous MI or angina) Men: 100% Mean age in years (SD): unclear Age range: 50‐59 years Smokers: unclear (˜48% non‐smokers) Hypertension: unclear Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Norway Ethnicity: unclear |
|
| Interventions | Type: supplementary food (oil) Comparison: ALA vs omega 6 Intervention: linseed oil, 10 mL/d (55% ALA), 5.5 g/d ALA, 1.5 g/d linoleic. Dose: 5.5 g/d ALA Control: sunflower oil, 10 mL/d (1.4% ALA), 0.1 g/d ALA, 6.3 g/d linoleic. Vitamin E was added to both oils. Compliance: 73% were still taking the linseed oil at 1 year, 72% were still taking their sunflower oil at 1 year (unclear how this was ascertained) Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: morbidity and mortality Dropouts: survival status was traced for all but 4 included men, health status was missing for about 80 men in total or 0.6%. Available outcomes: total and CV deaths, MI, angina, stroke, peripheral vascular disease, combined CV events, total cholesterol (subgroup) Response to contact: no |
|
| Notes | Study funding: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Paper states "simple randomisation" without clarification |
| Allocation concealment (selection bias) | Unclear risk | Few details provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Paper states that the workplace doctors who administered the trial locally were sent bottles for each participant marked only with their trial number, and that "appearance and taste of the products were so similar that most participants were unable to identify the type" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Company physicians recorded health status, and were also blinded to intervention (as above) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Detailed description, and those who left employment during the study were followed up for survival and morbidity via the main health system |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trials registration found |
| Attention | Low risk | As company physicians administered oils and assessed outcomes but were blind to treatment arm there could not be attention bias |
| Compliance | Unclear risk | 73% were still taking the linseed oil at 1 year, 72% were still taking their sunflower oil at 1 year (unclear how this was ascertained) |
| Other bias | Low risk | No further bias noted |
| Methods | Nutristroke RCT, parallel, (diet rich in vitamins and omega 3 plus omega 3 supplement vs diet rich in vitamins and omega 3), 12 months Summary risk of bias: moderate or high |
|
| Participants | People in a rehabilitation unit who had survived a stroke N: 38 intervention, 34 control. (analysed, intervention: 32 control: 20) Level of risk for CVD: high Men: 74% intervention, 56% control Mean age in years (SD): 61.3 (13.6) n‐3, 66.3 (11.4) n‐3 + antioxidant intervention, 68.4 (12.6) placebo, 65.1 (12.8) antioxidant – control Age range: not reported Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Italy Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: fish oil vs unclear placebo Intervention: fish oil gelatin capsules including 250 mg DHA + 250 mg EPA. Dose: 0.5 g/d EPA + DHA Control: "identical to supplement but contained no antioxidants or polyunsaturated fatty acids" Compliance: appears to have been assessed at meetings or on the phone monthly, but results unclear Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: functional status in stroke survivors Dropouts: 6 intervention, 14 control Available outcomes: mortality and cardiovascular mortality, lipids (6 months), albumin and lymphocyte counts (6 months), Barthel Index (functional status), neurological impairment (not reported by intervention group), mobility, adiposity (no numerical data presented; quote: "there were no statistically significant differences in body weight, BMI, arm circumference and triceps skin fold at the different time points") Response to contact: not yet attempted |
|
| Notes | 2 × 2 study that also had an antioxidant supplementary focus (supplementary vitamins C and E, beta carotene and polyphenols) Study funding: Italian Ministry of Health, Sigma‐Tau Health Science provided omega 3 capsules |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized by means of a specific list" |
| Allocation concealment (selection bias) | Unclear risk | Randomisation methodology not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "the placebo was identical to the supplement but contained no antioxidants or polyunsaturated fatty acids; no patient, research assistant, investigator or any other medical or nursing staff could distinguish the placebo from the supplements during the study". However, only one placebo discussed and unclear whether it was a placebo capsule (for omega 3) or pill (for antioxidants) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "assays were quality control checked by internal standard and calibration curve in a random and double blind way" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rates of dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trials registry entry found |
| Attention | Low risk | All assessments and treatments appear equal across the intervention groups |
| Compliance | Unclear risk | Appears to have been assessed at meetings or on the phone monthly, but results unclear |
| Other bias | Low risk | None noted |
| Methods | Randomisation: parallel, 3 groups (omega 3 vs olive oil vs aspirin and dipyridamole), 1 year Risk of bias: moderate or high |
|
| Participants | People undergoing PTCA N: 36 intervention, 37 control (also 35 allocated to arm 3, aspirin and dipyridamole) Level of risk for CVD: high (people undergoing angioplasty) Men: 78% intervention, 76% control Mean age in years (SD): 54 (8) intervention, 55 (8) control years Age range: unclear Smokers: unclear Hypertension: unclear Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: New Zealand Ethnicity: unclear |
|
| Interventions | Type: supplement (capsules) Comparison: EPA vs MUFA Intervention: MaxEPA capsules 12/d (2.2 g EPA). Dose: 2.2 g/d EPA Control: olive oil capsules, 12/d, identical to MaxEPA. Both capsules included vitamin E Compliance: no data Length of intervention: 12 months |
|
| Outcomes | Main study outcome: angina, restenosis Dropouts: none Available outcomes: angina, interventions, lipids (Nil death) Response to contact: no |
|
| Notes | Study funding: Medical Research Council of New Zealand and Scherer Ltd (who supplied MaxEPA and the olive oil capsules) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided without exclusions into 3 groups" |
| Allocation concealment (selection bias) | Unclear risk | Unclear, no further info |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | States that placebo capsules were identical to the MaxEPA, and "neither the patient nor the attending cardiologist knew which capsules were being used" (but no masking of taste was reported, and participant guesses as to allocation were not reported) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "neither the patient, nor the attending cardiologist knew which capsules were being used" ... "Angioplasty was repeated electively at one year or before where symptoms recurred, and assessed without knowledge of the patient's treatment group." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some participants were lost to follow‐up and reasons for this were unclear |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trials registration found |
| Attention | Low risk | No suggestion of attention bias, symptomatic patients were reviewed between scheduled visits, otherwise all on the same schedule |
| Compliance | Unclear risk | No data |
| Other bias | Low risk | No further bias noted |
| Methods | Omacor Following Acute Myocardial Infarction (OFAMI) RCT, parallel, 2 arms (omega 3 vs corn oil), 2 years Summary risk of bias: moderate or high |
|
| Participants | Patients recruited 4‐8 days after confirmed MI N: 150 intervention, 150 control Level of risk for CVD: high Men: 77% intervention, 82% control Mean age in years (SD): 64.4 intervention, 63.6 control (no SD) Age range: 28‐86 years intervention, 29‐87 years control Smokers: 39% intervention, 38% control Hypertension: 29% intervention, 23% control Medications taken by at least 50% of those in the control group: b‐blockers, aspirin Medications taken by 20%‐49% of those in the control group: statins, ACE inhibitors Medications taken by some, but less than 20% of the control group: diuretics, warfarin Location: Norway Ethnicity: unclear |
|
| Interventions | Type: supplement (capsules) Comparison: EPA + DHA vs omega 6 Intervention: 4 gelatin capsules of omega‐3‐acid ethyl esters 90 (Omacor, Pronova A/S, Oslo, Norway), each is 1 g containing 850‐882 mg EPA and DHA as concentrated ethylesters Dose ˜3.4‐ 3.5 g/d EPA + DHA Control: corn oil capsules, 4/d, each contains 1 g of corn oil Compliance: assessed by questionnaire and capsule count, 82% intervention group had complete compliance after 6 weeks, 86% of controls Length of intervention: 24 months |
|
| Outcomes | Main study outcome: CV events Dropouts: unclear Available outcomes: total and CV deaths, MI, unstable angina, interventions, combined CV events, BMI, lipids, BP (authors provided additional data on glucose, AF, stroke) Response to contact: yes |
|
| Notes | Study funding: Pharmacia‐Upjohn and Pronova | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" – Pharmacia was responsible for randomisation. Author response: participants were randomised in blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Author confirmed allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical capsules containing either Omacor or corn oil. Double blinding stated, but taste not reported as masked and blinding of participants not checked |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Author stated: all later analyses performed without the knowledge of outcome |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of dropouts was unclear |
| Selective reporting (reporting bias) | Unclear risk | Trials registry NCT01422317. Outcomes reported in trials registry appear to have been published, but registration was retrospective. |
| Attention | Low risk | All participants appear to have been reviewed at the same intervals |
| Compliance | Unclear risk | Assessed by questionnaire and capsule count, 82% intervention group had complete compliance after 6 weeks, 86% of controls |
| Other bias | Low risk | No further bias noted |
| Methods | Effect of Omega 3 fatty acids on reduction of sudden cardiac death after MI (OMEGA) 2 arm, parallel RCT (omega 3 vs olive oil), 12 months Summary risk of bias: low |
|
| Participants | People who have had an acute myocardial infarction N: 1940 intervention,1911 control (analysed for primary endpoints 1919 intervention, 1885 control) Level of risk for CVD: high Men: 75.1% intervention, 73.7% control Age (median): 64.0 years, intervention, 64.0 years control Age range: unclear (upper and lower quartiles 54‐72) Smokers: 35.9% intervention, 37.5% control Hypertension: 66.9% intervention, 66.1% control Medications taken by at least 50% of those in the control group: statins, ACE inhibitors, beta‐blockers, clopidogrel, aspirin Medications taken by 20%‐49%: diuretics Medications taken by some, but < 20%: AT1 receptor blockers, vit K antagonist, calcium channel blockers, digitalis, amiodarone, oral antidiabetics, insulin Location: Germany Ethnicity: not reported |
|
| Interventions | Type: supplement (capsules) Comparison: EPA + DHA vs MUFA Intervention: 1 × 1 g/d Pronova BiCare soft gelatin capsule 'zodin' omega‐3 acid ethyl esters (460 mg/d EPA and 386 mg/d DHA). Dose: 0.85 g/d EPA + DHA Control: 1 × 1 g/d olive oil capsule identical to intervention Compliance: 93.1% of intervention group and 93.2% of control participants took > 70% of capsules Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: sudden cardiac death, cardiac arrest Dropouts: Control: 26 (8‐lost to follow‐up, 2‐withdrew before allocation, 16‐excluded.) intervention: 21 Available outcomes: deaths, CV mortality, MACCE, MI, arrhythmias, heart failure, stroke, revascularisation, lipids, authors supplied information on angina, depression, cancers, AF Response to contact: yes |
|
| Notes | Study funding: Tromsdorff Arzneimittel commissioned the research | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation code generated by alpha med PHARBIL, done in blocks of 8. Randomisation was stratified by centre. |
| Allocation concealment (selection bias) | Low risk | Appearance of the drugs or the drug containers did not allow patients and physicians to deduce the study arm. 4‐digit number on a concealed container |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Capsules for placebo and intervention looked the same, randomisation code unknown to investigator (taste and smell not mentioned) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Classification of adverse events blinded to allocation, and there was a blinded endpoint committee for all pre‐specified outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All events were documented by the investigators and reported to the assigned clinical research organisation and the sponsor. The data safety monitoring board judged any imbalances between the study arms. |
| Selective reporting (reporting bias) | Low risk | NCT00251134 registered in 2005. Study start date: 2003, Completed: 2008, study design: 2006, Published paper: 2010. All trials registry primary and secondary outcomes reported |
| Attention | Low risk | Capsules for both arms |
| Compliance | Low risk | 93.1% of intervention group and 93.2% of control participants took > 70% of capsules. EAIC 0.65 intervention, and control |
| Other bias | Low risk | None noted |
| Methods | Older People And n‐3 Long‐chain polyunsaturated fatty acid (OPAL) 2 arm, parallel, RCT, 12 months Summary risk of bias: low |
|
| Participants | Healthy cognitively normal adults aged 70‐79 years N: 434 intervention, 433 control (analysed 376 intervention, 372 control) Level of risk for CVD: low Men: 53.4% intervention, 56.6% control Mean age in years (SD): 74.7 (2.5) intervention, 74.6 (2.7) control Age range: 70‐79 years Smokers: not reported Hypertension: 54.9% intervention, 56.9% control Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49%: not reported Medications taken by some, but < 20%: not reported Location: England and Wales Ethnicity: not reported |
|
| Interventions | Type: supplement (capsules) Comparison: EPA + DHA vs MUFA Intervention: 2 × 650 mg capsule/d Ocean Nutrition vanilla flavoured soft gelatin capsule (total daily dose of 200 mg EPA and 500 mg DHA). Dose: 0.7 g/d EPA + DHA Control: 2 × 650 mg olive oil capsule identical to intervention Compliance: count returned capsules. Capsules not returned:
Fasting serum fatty acids, mg/L, mean (SD)
Length of intervention: 24 months |
|
| Outcomes | Main study outcome: delayed onset of cognitive decline Dropouts: control: 78 (8 died, 53 withdrew, 17 discontinued intervention but provided data); intervention: 67 (9 died, 49 withdrew, 9 discontinued intervention but provided data) Available outcomes: deaths, MI, arrhythmias, stroke, diabetes, lipids Response to contact: yes |
|
| Notes | Study funding: UK Food Standards Agency, NHS R&D provided support costs | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were "selected in random blocks". "Research nurses telephoned a central computerized randomization service to obtain treatment allocation codes". |
| Allocation concealment (selection bias) | Low risk | Central allocation via telephone |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Identical capsules (vanilla‐flavoured, dark‐brown coloured). Supplements packaged into identical pots, each containing 180 capsules, labelled by staff not involved in the study. All project staff were unaware of group assignments until after data analysis. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All project staff were unaware of group assignments until after data analysis. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants who discontinued the supplements invited to an interview at 24 months. Dropouts explained and similar in both arms (intervention 49 withdrew, control 53 withdrew) |
| Selective reporting (reporting bias) | High risk | ISRCTN72331636. Trial registered 2004, before study began. Protocol published 2006. Publication of first results 2010. Many outcomes, such as depression and BP were stated in trials registry entry but not reported. |
| Attention | Low risk | All participants had the same review schedule, and staff were unaware of assignments |
| Compliance | Low risk | Count returned capsules. Capsules not returned (intervention ‐ median: 0.95; IQR: 0.82, 1.00; control ‐ median: 0.95; IQR: 0.81, 1.00). Fasting serum fatty acids, mg/L, mean (SD): EPA, intervention 49.9 (2.7); control 39.1 (3.1). DHA, intervention 95.6 (3.1); control 70.7 (2.9). α‐linoleic: intervention 21.5 (0.8); control 22.0 (0.9) |
| Other bias | Low risk | No further bias noted |
| Methods | Outcome Reduction With Initial Glargine Intervention (ORIGIN) RCT, 2 × 2 factorial, (capsule of n‐3 fatty acids or placebo), 72 months Summary risk of bias: low |
|
| Participants | People at high risk of CV events with impaired fasting glucose, impaired glucose tolerance or diabetes N: 6319 intervention, 6292 control. (analysed, intervention: 6281 control: 6255) Level of risk for CVD: moderate Men: 65.4% intervention, 64.7% control Mean age in years (SD): 63.5 (7.8) intervention, 63.6 (7.9) control Age range: unclear, eligible if aged ≥ 50 years Smokers: current smokers 12.1% intervention, 12.6% control Hypertension: 78.7% intervention, 80.3% control Medications taken by at least 50% of those in the control group: ACE inhibitor or ARB, aspirin or other antiplatelet, beta‐blocker, statin, glucose‐lowering drug Medications taken by 20%‐49%: calcium‐channel blocker Medications taken by some, but less than 20%: thiazide diuretics, anticoagulant Location: 40 study locations in Europe and the Americas Ethnicity: unclear |
|
| Interventions | Type: supplement capsule (Omacor) Comparison: EPA + DHA vs MUFA Intervention: 1 gelatin capsule/d Omacor containing at least 900 mg ethyl esters of n‐3 fats (465 mg EPA + 375 mg DHA). Dose: 0.84 g/d EPA + DHA Control: 1 × 1 g gelatin capsule/d olive oil Compliance: methods of assessment unclear, but reported that "rates of adherence to the study‐drug regimen were similar in the two groups with 96% of patients continuing to receive the study drug at 1 year ... and 88% at the end of the study". Length of intervention: 74 months mean follow‐up (median 6.2 years) |
|
| Outcomes | Main study outcome: composite of the First Occurrence of Cardiovascular (CV) Death, Nonfatal Myocardial Infarction (MI) or Nonfatal Stroke Dropouts: 38 intervention, 37 control (some of the remainder did not have final outcome status, were lost or withdrew consent, but were included in analysis) Available outcomes: mortality, CV mortality, fatal arrhythmia, MI, stroke, heart failure, angina, revascularisation, breast cancer, cancer diagnoses and cancer deaths, BP, lipids (HbA1c given as medians only) Response to contact: yes but no data provided |
|
| Notes | The other 2 × 2 assignment was to insulin glargine versus standard care, and is not discussed here. Results are reported here for the trial duration and not the follow‐up post trial (the ORIGIN and Legacy Effects, ORIGINALE). Study funding: Sanofi Aventis, Omacor provided by Pronova Biocare |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomized by an automated telephone randomization system (using randomly varying block sizes)" |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study described as "double blind" and placebo described as identical. Blinding of patients, investigators, local and central trials personnel described. However, no information provided as to the capsule's smell and taste |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "all primary and secondary outcomes were adjudicated with the use of prespecified definitions by a committee whose members were unaware of study‐group assignments" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Almost all participants were included in outcomes |
| Selective reporting (reporting bias) | Low risk | NCT00069784 – registered October 2003, study started August 2003, final data collection December 2011. Most outcomes appear to have been reported in various publications (cardiovascular events only reported by glargine randomisation). |
| Attention | Low risk | No suggestion of differences between groups |
| Compliance | Unclear risk | Methods of assessment unclear, but reported that "rates of adherence to the study‐drug regimen were similar in the two groups with 96% of patients continuing to receive the study drug at 1 year ... and 88% at the end of the study" |
| Other bias | Low risk | None noted |
| Methods | Omega‐3 fatty acids randomised long‐term (ORL) RCT‐ parallel, 3 arms (TAK‐085 2 g, TAK‐085 4 g, and EPA‐E 1.8 g), 12 months Summary risk of bias: moderate or high |
|
| Participants | Population: Japanese adults with hypertriglyceridaemia N: 171 intervention (4 g TAK), 165 control (2 g TAK) Level of risk for CVD: moderate Men: 70.8% intervention, 71.5% control Mean age in years (SD): 55.9 (10.12) intervention, 56 (10.95) control Age range: 20‐74 Smokers (current): 27.5% intervention, 31.5% control Hypertension: 66.7% intervention, 67.3% control Medications taken by at least 50% of those in the control group: HMG‐CoA reductase inhibitor Medications taken by 20%‐49%: statin Medications taken by some, but less than 20%: not reported Location: Japan Ethnicity: unclear |
|
| Interventions | Type: supplement (TAK‐085 capsules) Comparison: EPA + DHA higher vs lower dose Intervention: 1 × 2/d capsule each containing 2 g of TAK‐085 (1 g of fatty acid in TAK‐085 capsules contains approximately 465 mg of EPA‐E plus 375 mg of DHA‐E). Total dose of 1.86 g/d EPA + 1.5 g/d DHA. Dose: ˜3.4 g/d EPA + DHA) (difference of +1.7 g/d from control arm) Control: 1 capsule/d containing 2 g of TAK‐085 (1 g of fatty acid in TAK‐085 capsules contains approximately 465 mg of EPA‐E plus 375 mg of DHA‐E). Total dose of 0.93 g/d EPA + 0.75 g/d DHA. Dose: 1.7 g/d EPA + DHA Compliance: monitored every 4 weeks, mean rate of compliance reported as > 96% in each group Length of intervention: 12 months |
|
| Outcomes | Main study outcome: safety outcomes and adverse events Dropouts: group 1: 8, group 2: 14, group 3 (not analysed): 21 Available outcomes: adverse events (including CVD events, cancers), CRP, waist circumference, weight, blood pressure (nil death), lipids provided as % change from baseline, but no baseline data available, so not used in meta‐analyses Response to contact: no |
|
| Notes | A third arm of EPA‐E 1.8 g supplementation is not used here. Outcome data used TAK‐4 vs TAK‐2 Study funding: Takeda Pharmaceutical Company |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was stratified according to statin use and performed by an independent registration centre |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open label |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for and analysed for main outcomes |
| Selective reporting (reporting bias) | Low risk | Trials registry entry May 2011, study start date November 2009, completion November 2011, so partially retrospective. However, entry appears to reflect reported outcomes. |
| Attention | Low risk | Capsules, appears similar |
| Compliance | Low risk | Monitored every 4 weeks, mean rate of compliance reported as > 96% in each group |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (EPA + DHA fish oil vs omega 6 sunola oil), 12 months Summary risk of bias: low |
|
| Participants | Patients with rheumatoid arthritis < 12 months' duration, DMARD‐naive N: 87 intervention, 53 control. (analysed, intervention: 75 control: 47) Level of risk for CVD: low Men: 29% intervention, 25% control Mean age in years (SD): 56.1 (15.9) intervention, 55.5 (14.1) control Age range: unclear Smokers: 65.1% intervention, 54.7% control (includes current and previous smokers) Hypertension: not reported Medications taken by at least 50% of those in the control group: triple DMARD therapy (SSZ 0.5 g/d, HCQ 200 mg twice/day and MTX 10 mg once per week) Medications taken by 20%‐49% of those in the control group: NSAIDS Medications taken by some, but less than 20% of the control group: oral or parenteral steroids Location: Australia Ethnicity: not reported |
|
| Interventions | Type: supplement (fish oil) Comparison: high EPA + DHA vs omega 6 (low EPA + DHA with sunola oil) Intervention: 10 mL/d fish oil concentrate (BLT Incromega TG3525) providing 5.5 g/day (3.2 EPA + 2.3 DHA). Dose: 5.5 g/d EPA + DHA Control: 10 mL/d sunola oil:capelin oil (2:1) providing 0.21 g EPA + 0.19 g DHA/d as TAG (0.40 g/day EPA + DHA). Compliance: consumption checked at each visit. 100% compliance would be consumption of 3650 mL oil at 12 months. The fish oil group was less compliant than the control group with median intakes of 2482 mL and 3248 mL, respectively (P = 0.015, Mann‐Whitney U test). This provided an average daily intake of EPA + DHA of 3.7 g and 0.36 g in the fish oil and control groups, respectively. Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: disease‐modifying anti‐rheumatic drugs (DMARD) failure and remission Dropouts: 11 intervention, 6 control Available outcomes: mortality (nil death), adverse events including CVD, DAS score, diabetes, authors supplied methodology data plus BMI change Response to contact: yes |
|
| Notes | DAS scores are reported as median and IQR in Proudman 2012 abstract Study funding: National Health Medical Research Council of Australia and Royal Adelaide Hospital Research Committee. Melrose Health provided support for ongoing studies. The oil was made by the Royal Adelaide Hospital Pharmacy |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation schedule was prepared using an online random number generator and involved randomly permuted blocks of size six." |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was performed by the RAH pharmacy, which also prepared and provided the study oils in 500 mL identical dark brown bottles labelled with consecutive study numbers" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Both participants and investigators/assessors were blinded to the group allocation. Although the control oil was paler in colour than the fish oil, this was not evident in the brown bottles. The 'fishy' odour of each oil was similar." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Both participants and investigators/assessors were blinded to the group allocation. Quote: "Investigators and subjects remained blinded for all withdrawals." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The flow of all study participants shown in FIGURE 2 |
| Selective reporting (reporting bias) | Unclear risk | Outcomes reported in trial register matched with the outcomes reported in publications. However, the study was retrospectively registered – registered in 2013, recruitment began in 2001 |
| Attention | Low risk | No difference between groups |
| Compliance | High risk | Consumption checked at each visit. 100% compliance would be consumption of 3650 mL oil at 12 months. The fish oil group was less compliant than the control group with median intakes of 2482 mL (68%) and 3248 mL (89%), respectively (P = 0.015, Mann‐Whitney U test). This provided an average daily intake of EPA + DHA of 3.7 g and 0.36 g in the fish oil and control groups, respectively |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel (ethyl‐EPA vs paraffin), 2 arm, 12 months Summary risk of bias: low |
|
| Participants | People with Huntington's Disease N: 67 intervention, 68 control (analysed, intervention: 39 control: 44) Level of risk for CVD: low Men: 57% intervention, 44% control Mean age in years (SD): 50 (9.3) intervention, 49 (9.0) control Age range: not reported Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: antidepressants Medications taken by some, but < 20%: neuroleptics Location: UK, USA, Canada, Australia Ethnicity: intervention: 94% white, 4% black, 1% Asian; control: 97%, 3%, 0%, respectively |
|
| Interventions | Type: supplement (ethyl‐EPA) Comparison: EPA vs paraffin (non‐fat) Intervention: 2 × 2 × 500 mg capsules/d, total dose of 2 g/day ethyl‐EPA (code name LAX‐101, purity 95%). Dose: 1.9 g/d EPA Control: 2 × 2 × 500 mg capsules/d liquid paraffin Compliance: 38 were excluded for protocol violations, 4 intervention and 16 control were non‐compliant with capsules Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: functional status in Huntington's Disease Dropouts: 7 intervention, 7 control Available outcomes: measures of functional capacity, CV events, cancers (nil deaths) Response to contact: yes (no additional data provided) |
|
| Notes | Study funding: Amarin Neuroscience Ltd. (formerly known as Laxdale Ltd.), provided organisation, funding and salaries | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After screening and acceptance... patients were assigned to treatment by receiving a numbered pack supplied by a clinical trials packaging organization ... independent of all other aspects of the trial. Randomization was stratified in a block size of four, with the appropriate number of blocks allocated to each center. PCI Clinical Services held the randomization code until the database had been closed and all patients had been assigned" |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "[p]lacebo and ethyl‐EPA capsules were of identical appearance" (though taste and smell not reported). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Randomisation described as "double‐blind", "neither the patients nor the participating medical staff had access to this code during the course of the study" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Clearly reported and complete, however > 20% attrition |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trials registry entry identified |
| Attention | Low risk | Unlikely |
| Compliance | Unclear risk | 38 were excluded for protocol violations, 4 intervention and 16 control were non‐compliant with capsules |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (fish oil or olive oil), 24 months Summary risk of bias: moderate or high |
|
| Participants | People with implantable cardioverter defibrillators and recent sustained ventricular tachycardia or ventricular fibrillation (VT/VF) N: 100 intervention, 100 control Level of risk for CVD: high Men: 86% intervention, 86% control Mean age in years (SD): 63 (13) intervention, 62 (13) control Age range: not reported but 18‐75 inclusion criteria Smokers: not reported Hypertension: 46% intervention, 55% control Medications taken by at least 50% of those in the control group: diuretic, beta blockers, ACE inhibitors Medications taken by 20%‐49% of those in the control group: digoxin, statins Medications taken by some, but less than 20% of the control group: calcium channel blocker Location: USA Ethnicity: 94% white in intervention group, 97% in control group |
|
| Interventions | Type: supplement (fish oil capsules vs olive oil capsules) Comparison: EPA + DHA vs MUFA Intervention: 1.8 g/d fish oil capsules (Hoffman LaRoche, including ethyl esters of EPA and DHA, 0.76 g/d EPA, 0.54 g/d DHA). Dose: 1.3 g/d EPA + DHA Control: 1.8 g/d olive oil capsules (Hoffman LaRoche, 73% oleic acid) Compliance: while control group plasma and platelet DHA and EPA did not change, there were increases of 2%‐8.3% in the intervention group Duration of intervention: 24 months (median 718 days) |
|
| Outcomes | Main study outcome: time to first episode of VT/VF Dropouts: 17 intervention, 26 control Available outcomes: deaths, CV death, MI, angina, revascularisation, arrhythmias, sudden cardiac death, cancer Response to contact: yes but no data provided |
|
| Notes | Study funding: NIH and Hoffman LaRoche | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer generated block randomisation scheme" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participant blinding unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | ICD traces were viewed by researchers blinded to allocation, "double blind placebo‐controlled" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Almost all participants were included in outcome assessment, well described |
| Selective reporting (reporting bias) | High risk | NCT registered in February 2000, study carried out from February 1999 to January 2004. Most outcomes stated in registry entry reported, but quality of life missing |
| Attention | Low risk | Capsules were the only different interventions between arms, little opportunity for attention bias |
| Compliance | Low risk | While control group plasma and platelet DHA and EPA did not change, there were increases of 2%‐8.3% in the intervention group |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (fish oil vs sunflower oil), 12 months Summary risk of bias: moderate or high |
|
| Participants | People with relapsing remitting multiple sclerosis N: 25 intervention, 25 control. (analysed, intervention: 20 control: 19) Level of risk for CVD: low Men: 83% intervention, 82% control (but these appear unlikely) Mean age (SD) years: 35.1 (7.6) intervention, 34.9 (7.8) control Age range: not reported but 18‐55 years were inclusion criteria Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: 100% treated with interferon beta1b for at least 1 year before the trial began Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Mexico Ethnicity: not reported |
|
| Interventions | Type: supplement Comparison: DHA + EPA vs sunflower oil Intervention: 4 g/d omega Rx capsules (Dr Sears zone diet, with excipient of glycerin, water, tocopherol, sunflower oil, titanium dioxide, includes 0.8 g/d EPA plus 1.6 g/d DHA). Dose: 2.4 g/d EPA + DHA Control: excipient only (Perfect Source Natural Products, glycerin, water, tocopherol, sunflower oil, titanium dioxide) Compliance: consumption diary plus pills returned at each visit, adherence calculated (correct formula?? pills consumed × 100/pills returned), optimal adherence was considered to be > 80%, 1 intervention and 3 control were excluded due to compliance < 80%. Blood DHA and EPA were significantly different at 12 months. Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: TNF‐alpha Dropouts: 5 of 25 intervention, 6 of 25 control Available outcomes: TNF‐alpha, IL‐6, IL‐1 beta, nitric oxide catabolites, MS relapse, disability EDSS, liver and renal function tests, haemoglobin, leucocytes, platelets, oxidative outcomes (glucose and lipids data collected but not reported, for BMI and BP paper reports "no difference through study") Response to contact: not yet attempted |
|
| Notes | Study funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence (blocks of 4) |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "capsules were identical in appearance, packaging and labelling", "physicians and patients were blind to the intervention", and there was a rosemary flavour to mask. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "an independent physician evaluated the EDSS score and collected samples at each clinic visit" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss of 11/50 over 1 year, 22% loss |
| Selective reporting (reporting bias) | High risk | Paper reports analysis of glucose and lipids but these are not reported |
| Attention | Low risk | Appeared similar, reviewed every 3 months |
| Compliance | Low risk | Blood DHA and EPA were significantly different at 12 months |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, 3 arms (fish oil or borage oil), 18 months Summary risk of bias: low |
|
| Participants | Adults with rheumatoid arthritis N: 53 intervention, 52 control (28 intervention, 24 control analysed) Level of risk for CVD: low Men: 13.2% intervention, 23.1% control Mean age in years (SD): 57.3 (12.3) intervention, 60.3 (9.2) control Age range: not reported but 18‐85 inclusion criteria Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: methotrexate, DMARDs, and TNF blockers Medications taken by 20%‐49% of those in the control group: corticosteroids and TNF blockers Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: black/African‐American: intervention (fish oil): 7.8% control (borage oil): 7.8% |
|
| Interventions | Type: supplement (fish oil vs borage oil) Comparison: EPA + DHA vs Omega 6 Intervention: 7 fish oil (2.1 gm EPA:1.4 gm DHA) capsules and 6 sunflower seed oil capsules daily = 13 capsules divided doses. Dose: 3.5 g/d EPA + DHA Control: 6 borage seed oil (1.8 g GLA) capsules plus 7 sunflower seed oil capsules daily Compliance: assessed by capsule counts and patient report. Patient report, indicates that 45% of patients reported ever missing a dose (borage: 42%, fish 48%). Median total capsules missed (excluding those with 0) were 182 (borage: 164, fish 169) Duration of intervention: 18 months |
|
| Outcomes | Main study outcome: RA modified disease activity score Dropouts: 25 intervention, 28 control Available outcomes: mortality (nil death), CVD events (nil), DAS score, CDAI score. Authors suggested that LDL and total cholesterol were reduced in the intervention group at 18 months, and HDL was increased in both intervention and control at 18 months, while diastolic BP was reduced in the intervention group at 18 months, but no numbers provided. CRP and ESR data were provided combined for the intervention and control arms in the author response, so not useable Response to contact: yes, authors supplied details of methodology but no usable outcome data |
|
| Notes | A third arm (45 participants) were given a combination of both oils but not discussed here. Study funding: National Institutes of Health Grant RO1‐AT000309 from the National Center for Complementary and Alternative Medicine |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Author stated "stratified random block, stratified by site using random blocks of 3 & 6" |
| Allocation concealment (selection bias) | Low risk | No methodology provided in the paper, but the author suggested concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, all capsules were identical in appearance and colour, they were shipped in opaque plastic bottles to the University of Massachusetts University Hospital pharmacy, from where they were distributed to participating centres. However no information provided as to their smell and taste. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Author confirmed outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Authors mention intention‐to‐treat analysis but shows completers analysis. Numbers of participants are not provided for all outcomes measured. Provide results for the overall group (69 participants table 3a) while the flow diagram states there are 74 completers. 51% dropped out. |
| Selective reporting (reporting bias) | Low risk | Study prospectively registered in 2003, estimated study completion November 2008, published in 2014. Both outcomes reported in registry are reported in the publication. |
| Attention | Low risk | All patients were evaluated at 3‐month intervals, by the same examiner. |
| Compliance | Unclear risk | Assessed by capsule counts and patient report. Patient report, indicates that 45% of patients reported ever missing a dose (borage: 42%, fish 48%). Median total capsules missed (excluding those with 0) were 182 (borage: 164, fish 169) |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (n‐3 vs olive oil), 60 months Summary risk of bias: moderate or high |
|
| Participants | Patients with multiple cardiovascular risk factors N: 6244 intervention, 6269 control (analysed, intervention: 6239 control: 6266) Level of risk for CVD: high Men: 62.3% intervention, 60.6% control Mean age in years (SD): 63.9 (9.3) intervention, 64.0 (9.6) control Age range: not reported Smokers: 22.1% intervention, 21.4% control. Hypertension: 84.6% intervention, 84.5% control Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: ACE inhibitor; ARB; diuretic agent; calcium‐channel blocker; beta‐blocker; oral hypoglycaemic drug; statin; antiplatelet agent Medications taken by some, but less than 20% of the control group: insulin Location: Italy Ethnicity: not reported |
|
| Interventions | Type: supplement (n‐3 capsules) Comparison: EPA + DHA vs MUFA Intervention: 1 g/d n‐3 capsules polyunsaturated fatty acid ethyl esters (EPA and DHA content 850‐882 mg with an average ratio of 1.0 to 1.2). Dose: ˜0.87 g/d EPA + DHA Control: 1 g/d olive oil capsules Compliance: measured by self‐report during follow‐up visits but no results reported Duration of intervention: 60 months |
|
| Outcomes | Main study outcome: composite of time to death from cardiovascular causes or hospital admission for cardiovascular causes Dropouts: intervention: 5 withdrew consent before baseline, 43 lost to follow‐up, 1115 stopped treatment. 6239 analysed. Control: 3 (withdrew consent before baseline), 39 lost to follow‐up, 1218 stopped treatment. 6266 analysed Available outcomes: mortality, CV mortality, CV events, coronary related events and mortality, MI, AF, heart failure, side effects, stroke, cancer diagnosis, cancer death. Authors provided data on diabetes diagnosis, glucose and HbA1c. Response to contact: yes |
|
| Notes | All continuous outcomes change data are reported as least squares mean hence not used. Study funding, quote: "The steering committee had the full and sole responsibility for planning and coordinating the study, analyzing and interpreting the data, and preparing the manuscript and submitting it for publication. Società Prodotti Antibiotici, Pfizer, and Sigma Tau funded the trial but had no role in the study design, planning, conduct, or analysis or in the interpretation or reporting of the results" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Treatment was centrally assigned by means of telephone on the basis of a concealed, computer‐generated randomization list, stratified according to general practitioner." |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Patients, general practitioners, coordination and statistical staff, and outcome assessors were unaware of the study assignments until the final analyses were completed." However, there was no mention of placebo appearance or other methods of blinding, so unclear. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Patients, general practitioners, coordination and statistical staff, and outcome assessors were unaware of the study assignments until the final analyses were completed." Quote: "All events included in the primary efficacy end point were documented with the use of a narrative summary and supporting documentation and were adjudicated on the basis of prespecified criteria by an ad hoc committee consisting of a cardiologist, an internist, and a neurologist who were unaware of the study assignments" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Analyses were performed in the intention‐to‐treat population, except for a prespecified per protocol analysis of the primary end point in patients with no major protocol violations who did not permanently stop treatment." Figures differ in Visentin 2008: (p. i73)"At the end of March 2006, 12 521 patients have been Randomized"; "After 1‐year of follow‐up, 2.5% of the patients withdrawn from the trial and 5% of the patients discontinued treatment. The reasons for drug discontinuation were 1.7% for side effects (mainly gastrointestinal) and 3.3% others (clinical or patient's refusal)… After 1‐year of follow‐up, 1.0% had CV death and 3.4% hospitalisation for CV events (primary end point)" |
| Selective reporting (reporting bias) | High risk | Primary endpoint was amended part way through study. Differences in groupings of cardiovascular events in tables 2; S4 and S5. For hospital admissions notes each patient could have more than one cardiovascular cause |
| Attention | Unclear risk | Does not state attention differs or is the same between groups‐ regularly see GP for follow‐up and blinding not clear |
| Compliance | Unclear risk | No results |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (fish oil vs olive oil), 12 months Summary risk of bias: moderate or high |
|
| Participants | Adults with insulin‐dependant diabetes mellitus, diabetic nephropathy and normal BP N: 18 intervention, 18 control (analysed, 17 intervention, 15 control) Level of risk for CVD: moderate Men: 64% intervention, 67% control Mean age (SD) years: 32 (7) intervention, 34 (10) control Age range: 18‐55 years Smokers: 50% intervention, 47% control Hypertension: not reported Medications taken by at least 50% of those in the control group: insulin Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Denmark Ethnicity: not reported |
|
| Interventions | Type: supplement Comparison: EPA + DHA vs MUFA Intervention: cod‐liver oil emulsion (Pharma‐Vinci A/S Denmark). EPA 2 g, DHA 2.6 g, total PUFA 4.6 g/day. Dose: 4.6 g/d EPA + DHA Control: olive oil emulsion (Pharma‐Vinci A/S Denmark) Compliance: assessed through omega 3 incorporation in platelets, and the paper reports significantly higher omega 3 levels in platelets at 12 months Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: diabetic nephropathy Dropouts: 1 intervention, 3 control (though 3 further intervention participants are not included in all data) Available outcomes: mortality (nil), breast cancer, total and LDL cholesterol, sBP (TGs reported as medians so not used, albuminurea, fractional albumin clearance, transcapillary escape rate of albumin, prothrombin fragment reported as geometric means or medians, HbA1c, HDL and diastolic BP too different at baseline to include, GFR, PAI1, TPA, fibrinogen, etc. not relevant) Response to contact: yes |
|
| Notes | Study funding: the Danish Heart Association. Eskisol Fish oil and placebo oil emulsions were provided by Pharma‐Vinci A/S, Frederiksvaerk, Denmark | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomised using concealed randomisation to receive either fish oil or olive oil in blocks of 4 according to their glomerular filtration rate." |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Active and placebo (olive oil) were given as emulsions with orange flavour. At the end patients were allowed to guess about treatment and ˜50% were right" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts similar between groups although relatively high for small sample size. 3 dropouts from fish oil and 1 from control due to side effects. Intention‐to‐treat analysis appears to have been given for albuminuria only |
| Selective reporting (reporting bias) | Unclear risk | No trials registry entry or protocol found |
| Attention | Low risk | Time and attention appear to be the same. All patients were given dietary advice. |
| Compliance | Low risk | Reports significantly higher omega 3 levels in platelets at 12 months for the intervention group |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel 5 arms (combined groups 4 and 5 omega‐3‐acid ethyl esters (Lovaza) n‐3 ± raloxifene vs control groups 1 and 3 ± raloxifene), 24 months Summary risk of bias: moderate or high |
|
| Participants | Healthy postmenopausal women (50% normal weight, 30% overweight, 20% obese) with high breast density detected on their routine screening mammograms N: 54 + 53 intervention, 53 + 53 control Level of risk for CVD: low Men: 0% intervention, 0% control Mean age in years (SD): 56.56 (6.9) + 57.85 (5.1) intervention, 57.11 (5.9) + 57.68 (5.1) control Age range: not reported Smokers: 0% intervention, 0% control Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: not reported |
|
| Interventions | Type: supplement (n‐3 capsules) Comparison: EPA + DHA vs nil Intervention: group 4, Lovaza 4 g per day. Lovaza is the FDA‐approved n‐3 FA formulation containing 465 mg of EPA + 375 mg of DHA per gram, total dose; 1860 mg/d EPA, 1500 mg/d DHA. Group 5 as group 4 plus 30 mg raloxifene/d. Dose: 3.36 g/d EPA + DHA Control: group 1, no treatment; group 3, 30 mg raloxifene/d Compliance: measured by pill count, recorded at follow‐up visits and further verified by serum fatty acids monitoring. Compliance was 94% (SE 2%) at 6 months and 97% (SE 2%) at 12 months. Only 2 participants had a compliance < 85% (84% and 81%). Duration of intervention: 24 months |
|
| Outcomes | Main study outcome: change in breast density Dropouts: 5 intervention, 6 control Available outcomes: cardiovascular events, breast cancer, lipids, dietary intake, plasma FAs, adverse events (including one incidence of hyperglycaemia) Response to contact: yes |
|
| Notes | The study had 5 arms: group 1, no treatment, control; group 2, raloxifene 60 mg orally daily; group 3, raloxifene 30 mg orally daily; group 4, Lovaza 4 g orally daily; and group 5, Lovaza 4 g/d plus raloxifene 30 mg orally daily. Data here is combined for groups 4 and 5 vs 1 and 3 for binary outcomes and group 1 vs 4 used for continuous outcomes Study funding: GlaxoSmith Kline and Eli Lilly provided Lovaza and raloxifene, respectively. Funded by Susan G Komen for the Cure, KG081632 (A Manni) and pilot funds from the Penn State Hershey Cancer Institute (K El‐Bayoumy) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sandhu 2016 pg 276: "each study participant was randomly assigned with equal probability to one of the following five groups. A block randomization scheme was used to ensure balance treatment allocation during the course of enrolment." |
| Allocation concealment (selection bias) | Unclear risk | No description of concealment of allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open label |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open label |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | < 20% lost over 2 years, detailed reasons provided, no suggestion these are unbalanced |
| Selective reporting (reporting bias) | High risk | Biomarkers of oxidative stress (Urinary 8‐(isoprostane) F‐2α and 8OHdG, Lymphocyte 8‐OHdG, DNA etheno adducts), Urinary 2‐OHE1, 4‐OHE1, and 16α‐OHE1, Serum level of C‐reactive protein and IL‐6, Serum level of IGF‐I and IGFBP‐3, complete blood count mentioned in trial registry but not reported in Sandhu 2016. (More outcomes reported than in registry – diet, physical activity levels, adverse events) |
| Attention | Low risk | Participants assessed at baseline, 1‐year and 2‐year follow‐up |
| Compliance | Unclear risk | Measured by pill count, recorded at follow‐up visits and further verified by serum fatty acids monitoring. Compliance was 94% (SE 2%) at 6 months and 97% (SE 2%) at 12 months. Only 2 participants had a compliance < 85% (84% and 81%) |
| Other bias | Low risk | None noted |
| Methods | Study on prevention of Coronary atherosclerosis with Marine Omega 3 fatty acids (SCIMO) RCT, parallel (omega 3 vs average European fats), 2 years Summary risk of bias: low |
|
| Participants | People with angiographically proven coronary artery disease N: 112 intervention, 111 control (analysed 82 intervention, 80 control) Level of risk for CVD: high Men: 82% intervention, 78.6% control Mean age in years (SD): 57.8 (9.7) intervention, 58.9 (8.1) control Age range: unclear (18‐75 inclusion criteria) Smokers: 16.2% intervention, 22.3% control Hypertension: 53.1% intervention, 45.5% control (history of high blood pressure) Medications taken by at least 50% of those in the control group: platelet inhibitors, beta‐blockers Medications taken by 20%‐49% of those in the control group: long‐term nitrate therapy, lipid‐lowering agents, ACE inhibitors, diuretics, calcium antagonists, other antihypertensive agents and digitalis. Medications taken by some, but less than 20% of the control group: nitrates only on demand Location: Germany Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs SFA + MUFA (average European fat composition) Intervention: concentrated fish oil capsules, 6x 1 g capsules/d for first 3 months, 3 × 1 g/d for rest of study (4 g/d EPA +DHA + DPA + ALA for first 3 months, then 2 g/d). Dose: ˜2 g/d LCn3 Control: capsules containing fat which replicated the fat composition of the average European diet, 6/d for first 3 months, 3/d for rest of study, opaque soft gelatin capsules identical to fish capsules in identical screw‐top containers Compliance: capsule count, overall 2284 (SD 313) capsules taken of 2460 prescribed for each person, erythrocyte phospholipids rose from 4.6% to 11.8% at 24 months in intervention, and didn't alter from baseline in controls Length of intervention: 24 months |
|
| Outcomes | Main study outcome: changes in stenosis on angiography Dropouts: unclear Available outcomes: mortality, MI, CV events, revascularisation, angina, stroke, cancer diagnosis, weight, lipids, BP, side effects Response to contact: yes |
|
| Notes | Asked participants to guess treatment allocation, of those in intervention 63/90 were unsure, 5/90 guessed placebo and 22/90 guessed fish oil; of those in control 66/85 were unsure, 9/85 guessed placebo and 10/85 guessed fish oil Study funding: Pronova provided capsules and funds for study monitoring but it was stated that the funders played no part in analysis or publication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified, and for the resulting 9 strata "a random sequence of study group assignments was computer generated by the trial monitor" |
| Allocation concealment (selection bias) | Low risk | Sealed, sequential numbered envelopes used (opaque not stated, but provided only a random number which linked to a specific container of capsules). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo and fish oil capsules "looked identical and were made of soft opaque gelatin and each contained 1 g of a fatty acid mixture". These were provided in identical containers with identical labels with a randomisation number. Patients were told that capsules differed in composition but not in taste. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding is described and is very strong for angiographic outcomes, but there is no description of how cardiovascular events were assessed or recorded. However outcomes assessors were probably the same assessors and so blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear for how many participants clinical events were assessed (though described in detail for angiographic outcomes), so trial flow unclear |
| Selective reporting (reporting bias) | Unclear risk | No study trials register entry or protocol was found |
| Attention | Low risk | As study personnel were unaware of assignments bias in attention was not possible |
| Compliance | Low risk | Capsule count, overall 2284 (SD 313) capsules taken of 2460 prescribed for each person, erythrocyte phospholipids rose from 4.6% to 11.8% at 24 months in intervention and didn't alter from baseline in controls |
| Other bias | Low risk | No further bias noted |
| Methods | RCT, parallel (fish oil capsule vs soybean oil capsule), 12 months Summary risk of bias: moderate to high |
|
| Participants | Patients aged 55 or more with probable Alzheimer dementia diagnosis N: 13 intervention, 13 control Level of risk for CVD: low Men: 61% intervention 46% control Mean age in years (SD): 75.9 (8.1) intervention, 75.2 (10.8) control Age range: 55+ (inclusion criteria) Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: anti‐cholinesterases or memantine Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Lipid‐lowering medications and many other drugs were not allowed Location: USA Ethnicity: 100% white |
|
| Interventions | Type: fish oil capsules Comparison: EPA + DHA vs n‐6 Intervention: 3 × 1 g capsules/day of fish oils (975 mg EPA, 675 mg DHA per day). Dose: 1.65 g/d EPA + DHA Control: 3 × 1 g capsules/day soybean oil (which contains 5% fish oil) Both groups had a placebo lipoic acid tablet and lemon‐flavoured capsules Compliance: assessed by pill counts and FA in red blood cell membranes. Results showed increased EPA + DHA levels in the intervention group. Length of intervention: 12 months |
|
| Outcomes | Main study outcome: F2‐isoprostane levels (oxidative stress measure) Dropouts: 2 intervention, 2 control Available outcomes: mortality, CVD events, adverse events, serum fatty acids, measures of cognition (ADAS Cog and MMSE), ADL, IADL (also F2 isoprostane) Response to contact: not attempted |
|
| Notes | Study funding: National Institutes of Health/National Institute of Aging (NIH/NIA) and NIH General Clinical Research | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised by a computer‐generated scheme that was stratified by smoking status |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Capsules matched for taste and flavour. Blinding assessed at the end and majority of staff and participants were unaware of treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 15% dropouts explained and included |
| Selective reporting (reporting bias) | Low risk | NCT00090402 first received: 25 August 2004, study start date April 2004. More secondary outcomes reported than included in the trial register entry |
| Attention | Low risk | Both arms seem to have had the same contact |
| Compliance | Low risk | Compliance measured and FAs levels reported. Results showed increased EPA + DHA levels in the intervention group |
| Other bias | Low risk | None noted |
| Methods | SHunt Occlusion Trial (SHOT) RCT, parallel (omega 3 vs nil), 4 arms, 1 year Summary risk of bias: moderate or high |
|
| Participants | People admitted for coronary bypass grafting N: 317 intervention, 293 control Level of risk for CVD: high Men: 86% intervention, 88% control Mean age in years (SD): 59.9 (8.7) intervention, 59.4 (8.8) control Age range: unclear Smokers: 19% intervention, 20% control Hypertension: 20% intervention, 25% control Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: antihypertensives Medications taken by some, but less than 20% of the control group: not reported Location: Norway Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs nil Intervention: 4 fish‐oil concentrate soft gelatin capsules/d (Omacor; Pronova AS, Oslo,Norway) containing 51% EPA and 32% DHA ethyl esters and 3.7 mg vitamin E as an antioxidant. Dose: 3.3 g/d EPA + DHA Control: no treatment Compliance: capsule count, 88% taken, serum EPA + DHA rose in the intervention group (176 to 257 mg/L at 9 months) and fell in the control group (170 to 169 mg/L at 9 months) Length of intervention: 12 months |
|
| Outcomes | Main study outcome: CABG graft patency Dropouts: 15 intervention, 14 control Available outcomes: deaths, CV deaths, MI, stroke, repeat CABG, combined CV events, lipids, side effects Response to contact: yes | |
| Notes | The study had 4 arms; aspirin; warfarin; fish oil + aspirin; and warfarin + fish oil. The first 2 groups are combined as the control and the last two combined as intervention. Dietary assessment suggested total diet plus supplement intakes as follows: 2.7 g/d EPA + DHA at baseline, 5.5 g/d at 9 months intervention, 2.5 g/d at baseline, 2.2 g/d at 9 months control group Study funding: in part by Pronova and Nycomed Pharma |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were provided in consecutively sealed envelopes generated centrally |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not reported as opaque |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open trial, no blinding apart from outcome assessors so participants and study personnel were aware of assignments. However, author suggested in personal communication that participants were not aware of their assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors (radiologists) reported as blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for attrition and exclusions stated, numbers clear, dropouts < 20% per year |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trials register entry was found |
| Attention | Low risk | Appeared equivalent between arms |
| Compliance | Low risk | Capsule count, 88% taken, serum EPA + DHA rose in the intervention group (176 to 257 mg/L at 9 months) and fell in the control group (170 to 169 mg/L at 9 months) |
| Other bias | Low risk | No further bias noted |
| Methods | RCT, parallel, (fish oil vs placebo), 12 months Summary risk of bias: moderate or high |
|
| Participants | Patients with hypertension and paroxysmal or persistent atrial fibrillation (AF) N: 268 intervention, 60 control Level of risk for CVD: moderate Men: not reported Mean age (SD) years: 62 (6), not reported by arm Age range: not reported Smokers: not reported Hypertension: 100% Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Greece Ethnicity: not reported |
|
| Interventions | Type: supplement Comparison: fish oil vs unclear placebo Intervention: omega‐3 fatty acids with no further details. Dose: 4 g/d omega Control: placebo, no further details Compliance: no details Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: AF recurrence and BP Dropouts: no details Available outcomes: new AF episodes, BP (not in a usable format) Response to contact: no |
|
| Notes | Study funding: unclear The study's only publication was a conference abstract. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details, probably randomised but unclear |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No details |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial register record found |
| Attention | Unclear risk | No details |
| Compliance | Unclear risk | No details |
| Other bias | Unclear risk | No details |
| Methods | SMART trial (from the Smart Foods Centre) RCT, 3‐arm parallel, (Fish + S: hypocaloric diet plus fish plus fish oil capsules vs Fish: hypocaloric diet plus fish plus olive oil capsules vs control: hypocaloric diet plus olive oil capsules), 12 months Summary risk of bias: moderate or high |
|
| Participants | Overweight adults N: fish + S intervention 41, fish 43, control 42. (analysed, fish + S intervention 21, fish 25, control 18) Level of risk for CVD: low Men: 27% fish + S intervention, 23% fish intervention, 28% control Mean age (SD) years: unclear by arm, overall 45.1 (8.4) Age range: not reported but 18‐60 years eligible Smokers: not reported but 5.9% overall Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Australia Ethnicity: not reported |
|
| Interventions | Type: supplement and food Comparison: EPA + DHA vs MUFA (Fish plus fish oil supplements vs Fish plus olive oil supplements vs olive oil supplements) Intervention, Fish + S: hypocaloric diet aiming at 30% E from fat, 25% E from protein, 45% E from CHO, plus 180 g fish/week plus capsules including 420 mg/d EPA + 210 mg/d DHA (Blackmores Promega Heart). Dose: 0.63 g/d EPA + DHA Intervention, fish: hypocaloric diet aiming at 30% E from fat, 25% E from protein, 45% E from CHO, plus 180 g fish/week plus capsules including 1 g olive oil/d Control: hypocaloric diet aiming at 30% E from fat, 25% E from protein, 45% E from CHO, plus capsules including 1 g olive oil/d Compliance: assessed through diet histories (fish) and erythrocyte fatty acid supplements (capsules), but results not reported Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: total % body fat Dropouts: fish + supplement intervention 20, fish intervention 18, control 24 Available outcomes: weight, BMI, lipids, BP, fasting glucose, fasting insulin, % body fat (leptin also reported), no deaths or cardiovascular events occurred (authors report) Response to contact: authors provided data on CVD events (none) and mean/SD data for TGs and fasting insulin |
|
| Notes | To assess effects of omega 3 fats the best comparison in this study is fish + S vs fish, so numerical data reflect this comparison. Study funding: Australian National Health and Medical Research Council, fish and olive oil capsules were provided free by Blackmores Australia |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A researcher independent of the subject interface undertook the randomisation of participants into diet groups (stratified by sex and block randomised...)" |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was performed centrally, off‐site and the holder of the allocation schedule provided the codes to a single researcher who was independent to the subject interface. The placebo and active ingredient capsules were coded off‐site . The codes were kept from the researchers collecting dietary data and delivering treatment. Allocation concealment was maintained as the persons responsible for screening eligible participants for inclusion in the trial was unaware to which supplement group the subject would be allocated. Different dietitians collected the dietary data and provided dietary advice" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | As above, but impossible to blind participants to the fish advice |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Very high levels of attrition, though intention‐to‐treat analyses carried out |
| Selective reporting (reporting bias) | High risk | We were unable to find data on 24 hour energy expenditure, oxidation or heart rate which were stated as primary and secondary outcomes in the trials registry. |
| Attention | Unclear risk | While dietary education was for 1 hour then 6 further half hour follow‐ups plus written materials and monthly newsletters plus dietary interviews it is not clear whether this was in all arms or only some of them. |
| Compliance | High risk | Quote: "Of the 12 months completers, 57% were judged to be compliant, 39% (n = 7) for the control group who reported < 180 g fish/week, 48% (n = 12) for the Fish group who reported ≥180 g fish/week, and 85% (n = 17) for the Fish + S group who reported ≥180 g fish/week or ≥90% supplements". However, erythrocyte (EPA + DHA)/total fatty acids × 100 was significantly different for the fish oil supplemented group compared to the two others – but it was only measured in around half of the participants as the others dropped out, so presumably were non‐compliant. |
| Other bias | Low risk | None noted |
| Methods | Study on Omega‐3 Fatty Acids and Ventricular Arrhythmia (SOFA) 2 arm, parallel RCT (n‐3 EPA + DHA vs MUFA), 12 months Summary risk of bias: low |
|
| Participants | People with previous ventricular arrhythmias and implantable cardioverter defibrillators N: 273 intervention, 273 control (273 intervention, 273 control analysed) Level of risk for CVD: high Men: 84% intervention, 85 % control Mean age in years (SD): 60.5 (12.8) intervention, 62.4 (11.4) control Age range: unclear (18 years and older) Smokers: 16% intervention, 8% control Hypertension: 53% intervention, 49% control Medications taken by at least 50% of those in the control group: beta‐blockers Medications taken by 20%‐49% of those in the control group: lipid lowering, antiarrythmic medications (combined) Medications taken by some, but less than 20% of the control group: amiodarone, sotalol Location: 8 countries in Europe Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs MUFA + omega 6 Intervention: 2 g/d (4 capsules) purified fish oil. 961 mg n‐3 PUFAS (464 mg EPA + 335 mg DHA and 162 mg other n‐3 PUFAs) daily. 3000 ppm vitamin E (Loders Croklann, Wormeveer). Dose: 0.8 g/d EPA + DHA Control: 2 g/d high‐oleic acid sunflower oil. 3000 ppm vitamin E (Loders Croklann, Wormeveer) Compliance: daily diary, checked by research nurses every 4 months. Judging by capsule count, 207 patients in the fish oil group and 218 in the placebo took more than 80% of their capsules. N‐3 fatty acid composition in serum cholesterol levels was measured at baseline and the end of the trial. The EPA concentration in serum cholesterol esters increased in the expected range. No data provided Length of intervention: 12 months |
|
| Outcomes | Main study outcome: spontaneous ventricular tachyarrhythmias and all‐cause mortality Dropouts: 33 intervention (23 partial follow‐up), 33 control (14 partial follow‐up) Available outcomes: deaths, MI, new angina, new heart failure, no fatal arrhythmias, cancer, cardiovascular events, side effects Response to contact: yes but no data provided |
|
| Notes | Study funding: Wageningen Centre for Food Sciences (alliance of major Dutch food industries and others) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients using beta‐blockers were separately randomised in blocks of 2. A computer randomisation programme randomly took the first treatment of a block. The second patient in a block of 2 always received the opposite treatment. |
| Allocation concealment (selection bias) | Low risk | Treatments (blinded medication numbers) were centrally assigned by a telephone allocation service. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blinding. Bottles containing capsules labelled with medication numbers that are unidentifiable for patients as well as investigators. Fish oil and placebo capsules have identical appearance. Difference can't be tasted if swallowed with water (as suggested) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "blinded endpoint adjudication committee" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis. Did a partial follow‐up on some patients who dropped out due to non‐compliance. |
| Selective reporting (reporting bias) | Low risk | NCT00110838, trial registered in May 2005, end of trial January 2005, trial results published in 2006. However, rationale and design paper (stating outcomes) published in 2003. Outcomes in the 2006 paper appear to be the same as in Rationale paper. |
| Attention | Low risk | Unlikely as intervention blinded to investigators and only intervention was capsules |
| Compliance | Unclear risk | Daily diary, checked by research nurses every 4 months. Judging by capsule count, 207 patients in the fish oil group and 218 in the placebo took more than 80% of their capsules. N‐3 fatty acid composition in serum cholesterol levels was measured at baseline and the end of the trial. The EPA concentration in serum cholesterol esters increased in the expected range. No data provided |
| Other bias | Low risk | No further bias noted |
| Methods | 2‐arm, parallel RCT (enriched olive oil vs olive oil), 12 months Summary risk of bias: moderate or high |
|
| Participants | Non‐alcoholic fatty liver disease patients N: 6 intervention, 5 control Level of risk for CVD: low Men: 66.7% intervention, 100% control Median age: 55 intervention, 54 control Age range: 30‐41 intervention, 42‐70 control Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Italy Ethnicity: not reported |
|
| Interventions | Type: supplement (oil) Comparison: EPA + DHA vs MUFA Intervention: 6.5 mL/d olive oil enriched with n‐3 (t‐Omega 3, tFarma srl, Italy) containing 0.47 g EPA, 0.24 g DHA plus dietary recommendations. Dose: 0.83 g/d EPA + DHA Control: 6.5 mL/d olive oil plus dietary recommendations Compliance: was verified by counting the empty boxes on return but no data reported Length of intervention: 12 months |
|
| Outcomes | Main study outcome: fatty liver status Dropouts: unclear Available outcomes: lipids, glucose, insulin, HOMA, (BMI not in usable format, also LFTs, oxidative markers, adiponectin, fatty liver and steatosis outcomes) Response to contact: not yet attempted |
|
| Notes | Study funding: oil supplied by tFarma and funding not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomized into two groups" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No details |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers analysed for liver health are for those randomised. Numbers analysed for other outcomes not stated. No mention of dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration |
| Attention | Low risk | Both groups received same contact |
| Compliance | Unclear risk | Measured but no results reported |
| Other bias | Low risk | None noted |
| Methods | Supplementation en Folates et Omega 3 (SU.FOL.OM3) RCT, 2 × 2 factorial (LCn3 omega 3 vs placebo, also B vitamin comparison), 4 years Summary risk of bias: low |
|
| Participants | People with a history of MI, unstable angina or ischemic stroke N: control: 1248, intervention: 1253 Level of risk for CVD: high Men: 80.85% intervention, 78.25% control Mean age in years (SD): 61.1 (8.8) intervention, 60.8 (8.7) control Age range: 53‐68 years intervention, 54‐68 years control Smokers: 11.1% intervention, 10.4% control Hypertension: not reported Medications taken by at least 50% of those in the control group: beta‐blockers, aspirin or antiplatelets, lipid lowering, ACE inhibitors Medications taken by 20%‐49%: not reported Medications taken by some, but < 20%: calcium channel blocker, angiotensin II receptor blockers Location: France Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs non fat placebo Intervention: 2 gelatin capsules Pierre Fabre omega 3 (400 mg/d EPA and 200 mg/d DHA) Control: 2 gelatin capsules/d placebo (liquid paraffin with fish flavour) Compliance: tested by questionnaire, response rate was on average 96%. Out of this, 86% complied Duration of intervention: 4 years |
|
| Outcomes | Main study outcome: composite of myocardial infarction, cerebral vascular ischemic accident or cardiovascular deaths Dropouts: control: 145 (66 withdrew, 11 lost to follow‐up, 68 deaths), intervention: 134 (61 withdrew, 7 lost to follow‐up, 66 deaths) Available outcomes: deaths, cardiovascular death, non fatal MI, stroke, CV events, coronary events, cancer events, Geriatric Depression Scale score, authors provided additional information on outcomes and methodology Response to contact: yes (data provided) |
|
| Notes | The other factorial intervention was B‐vitamins (560 µg methyl‐terahydrofolate, 3 mg B‐6, 20 µg B12) vs placebo Study funding: French Ministry of Research, Ministry of Health, Sodexo, Candia, Unilever, Danone, Roche, Merck |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Used computerized block randomisation with stratification by sex, age, prior CVD, and city of residence". "Permuted block randomisation (with a block size randomly selected as 8) was used". |
| Allocation concealment (selection bias) | Low risk | Allocation of participants was programmed by the statistical coordinating centre, who sent participants sufficient treatment capsules for 1 year in an appropriately labelled package |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All subjects and investigators were blinded to treatment allocation", and placebo capsules looked and tasted "identical to the active supplementation". Fish oil flavour was used in placebos. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome investigators were blinded to allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attritions and exclusions were well described. Only 10% loss over 4 years, well balanced |
| Selective reporting (reporting bias) | Low risk | ISRCTN41926726 registered 2005, 2003 publication on background and rationale, recruitment started April 2003, 2008 protocol, recruitment ended June 2009, 2010 results published. Outcomes in registry entry appear to have been published. |
| Attention | Low risk | Not likely as capsules used |
| Compliance | Low risk | Quote: "Allocation to omega 3 fatty acids increased plasma concentrations of omega 3 fatty acids by 37% compared with placebo" (appears statistically significantly different, though not explicitly stated) … "The overall response rate for return of completed questionnaires was 99%, 96%, 94%, and 95% at 6, 12, and 24 months and at the end of the trial, respectively. About 86% of those who returned a questionnaire reported that they were compliant with the study treatment and compliance was similar in all four groups" |
| Other bias | Low risk | No further bias noted |
| Methods | 2 arm, parallel RCT (calanus (marine) oil vs olive oil), 12 months Summary risk of bias: moderate to high |
|
| Participants | Healthy male and female volunteers with BMI 25‐35 kg/m2 N: 64 intervention, 63 control (50 intervention, 50 control analysed) Level of risk for CVD: low Men: 42% intervention, 43 % control Mean age in years (SD): 50.7 (7.7) intervention, 49 (9.4) control Age range: unclear (18 years and older) Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Norway Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: EPA + DHA vs MUFA Intervention: 2 × 500 mg Calanus oil capsules twice daily to provide a daily dose of 2 g. Supplements were provided by Ayanda AS (Norway) as blister packs of 60 capsules each. The Calanus oil contained approximately 85% wax ester with a sum of neutral lipids > 90%. Dose: 2 g/d EPA + DHA Control: identical capsules of olive oil. Compositional analysis indicated that the fatty acid content of the olive oil was primarily oleic acid (76.9%), palmitic acid (10.2%), and linoleic acid (7.7%). Compliance: assessed through the return of unused capsules. Compliance rate reported for both intervention and placebo groups was good (86‐88%) Length of intervention: 12 months |
|
| Outcomes | Main study outcome: safety of Calanus oil consumption Dropouts: 14 intervention, 13 control Available outcomes: BMI, waist‐hip ratio, BP, pulse, HbA1c, ESR, CRP, lipids, glucose tolerance, insulin, clinical chemistry parameters, adverse events (no CVD events, deaths or other major health outcomes occurred according to author reply) Response to contact: author replied with methodological and event information |
|
| Notes | Study funding: Calanus AS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization of the study subjects into the intervention group or the placebo group was performed by the University Hospital of North Norway clinical research unit and was stratified by gender." Author reply stated that "[r]andomization was performed by competent people at the drugstore affiliated to the University Hospital, with no interconnection, formally or materially with the research department from where the study was managed. Randomization was performed prior to recruiting subjects." |
| Allocation concealment (selection bias) | Unclear risk | As above, unclear. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants in the placebo group received identical capsules at similar daily doses as the intervention group. However, no information provided as to their smell and taste. Also unclear if investigators were blinded. Author reply stated "Each study subject was given a randomization number, which carried the name of the person, date of birth and treatment information (intervention or control). The randomization number was the only information made available to the study personnel, and the code was managed by personnel outside the research department. This code was broken after the completion of all analysis with all primary data processed." Blinding of participants only possible for fish plus supplementation vs fish plus placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All dropouts (˜20%) are explained |
| Selective reporting (reporting bias) | Unclear risk | No trials registry entry or protocol found |
| Attention | Low risk | Appear to be similar in both groups |
| Compliance | Unclear risk | Quote: "levels of DHA and EPA in the blood were generally higher in the Calanus oil group over baseline values relative to the placebo controls" but no data provided |
| Other bias | Low risk | None noted |
| Methods | The Heart Institute of Spokane Diet Study (THIS‐DIET) RCT‐ parallel, 24 months Summary risk of bias: moderate or high |
|
| Participants | Recent survivors of first myocardial infarction (within < 6 weeks) N: 51 intervention, 50 control Level of CVD risk: high Men: 80% intervention, 68% control Mean age in years (SD): 58 (10) intervention, 58 (9) control Age range: unclear Smokers: 25% intervention, 30% control Hypertension: 43% intervention, 50% control (uncontrolled or secondary hypertension excluded) Medications taken by at least 50% of those in the control group: aspirin, statins, beta‐blockers, and ACE inhibitors or angiotensin receptor blockers. Medications taken by 20%‐49%: not reported Medications taken by some, but < 20%: not reported Location: USA Ethnicity: intervention 98% white; control 94% white |
|
| Interventions | Type: dietary advice (to follow a Mediterranean style diet high in n‐3) Comparison: EPA + DHA vs MUFA (biggest dietary change) Intervention: Mediterranean style diet high in n‐3. Dietary counselling group sessions; two in first month then at months 3, 6, 12 and 24. Sessions focused on behaviour modification and practical aspects of assigned diet including recipes, shopping and dining out. Aim to increase omega 3 fat intake to > 0.75% kcal. Dose: ˜1.5 g/d omega 3 fat, or 0.31% E by intake assessment. Control: dietary advice (to follow the American Heart Association Step II diet). Same number of group sessions as intervention. The 2 diets were low in saturated fat (< 7% kcal) and cholesterol (< 200 mg/day); the Mediterranean‐style diet was distinguished by greater omega‐3 fat intake (> 0.75% kcal). Compliance: participants were required to attend six sessions and only invited but not required to attend extra sessions. 3‐day food diaries were reviewed with dietitians. Compliance results not stated. Dietary achievements: Total fat intake, % E (at 24 months): control 29.7 (SD 9.3), intervention 29.1 (SD 8.6) Saturated fat intake, % E (at 24 months): control 8.0 (SD 2.9), intervention 7.9 (SD 3.2) PUFA intake, % E (at 24 months): control 5.7 (SD 3.1), intervention 5.7 (SD 2.4) PUFA n‐3 intake, % E: control 0.46 (SD 0.38), intervention 0.67 (SD 0.35) g/week PUFA n‐6 intake: not reported MUFA intake, % E (at 24 months): control 10.3 (SD 5.1), intervention 9.7 (SD 3.6) CHO intake, % E (at 24 months): control 54 (SD 11), intervention 54 (SD 10) Protein intake, % E (at 24 months): control 17 (SD 2), intervention 18 (SD 3) Trans fat intake: not reported Length of intervention: 24 months |
|
| Outcomes | Main study outcome: a composite of endpoints including all‐cause and cardiac death, MI, hospital admissions for heart failure, unstable angina, or stroke Dropouts: none for primary outcomes Available outcomes: total and CVD deaths (nil deaths), CV events, stroke, MI, diagnosis of diabetes mellitus, BMI and weight (different at baseline hence not used), waist circum, lipids, blood pressure, albuminuria, CRP, creatinine and dietary intake (authors supplied further data on newly diagnosed DM, glucose and insulin data, cancers, depression, atrial fibrillation) Response to contact: yes further data supplied as above |
|
| Notes | The study compared the 2 intervention groups to a non‐randomised usual care control group (not reported here) Study funding: no funding details is provided but some reported conflict of interests for an author. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed envelopes concealing the allocation sequence were prepared by a research coordinator. Assignment was stratified by diabetes mellitus status using 10‐envelope blocks. Envelopes were selected in the prepared order from a locked drawer by a study dietitian to assign interventions |
| Allocation concealment (selection bias) | Unclear risk | As above but opacity of envelopes is not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither the intervention team nor participants could be blinded to dietary assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The PI was blinded for the purpose of adjudicating clinical end points and adverse events by the removal of identifiers from records used for review. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Primary outcomes data provided for all randomised |
| Selective reporting (reporting bias) | High risk | NCT00269425. Trial was registered in 2005, data collection started in October 2000, January 2008 (final data collection date for primary outcome measure), publication 2008. A number of the outcomes from the registration were not reported e.g. cardiovascular revascularisation, peripheral revascularisation or amputation, doubling of serum creatinine, dialysis, or kidney transplant, new hypertension. Also numerous secondary measures were reported that were not in the original registration. |
| Attention | Low risk | Both arms had the same contact and attention |
| Compliance | Unclear risk | No details |
| Other bias | Low risk | None noted |
| Methods | The Walnut and Healthy Aging Study (WAHA) 2‐arm, parallel RCT (usual diet plus walnuts vs usual diet), 2 years Summary risk of bias: moderate to high |
|
| Participants | Middle‐aged healthy adults N: 362 intervention, 346 control (only preliminary data on 312 participants from one of the two centres is available) Level of risk for CVD: low Men: 32.6% intervention, 31.5% control Mean age in years (SD): 69.4 (3.8) intervention, 68.9 (3.5) control Age range: 63‐79 (inclusion criteria) Smokers: 4.4% intervention, 1.2% control Hypertension: 52.8% intervention, 52.9% control Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: Spain and USA Ethnicity: not reported |
|
| Interventions | Type: supplement (food) Comparison: ALA vs unclear Intervention: 15% of daily energy intake as walnuts. The estimated amount of walnuts ranged from about 30–60 g/day (1‐2 ounces). Sachets for daily consumption containing 30 g, 45 g, or 60 g of raw, pieced walnuts were provided as 8‐week allotments to be eaten daily, preferably as the raw product, either as a snack or by incorporating them into shakes, yogurts, cereals, or salads. To improve participants' compliance, 1‐kg extra walnut allowances were provided every 2 months to take into account family needs. Dose: ˜5 g/d ALA Control: usual diet without walnut Compliance: assessed by dietitians through FFQs, recount of empty packages, and changes in FAs concentrations. 95% consumed at least 30 g/d. The proportion of α‐linolenic acid in red blood cells increased in the walnut group by 0.16% (95% CI 0.14 to 0.18) and in the control group by 0.02% (95% CI −0.01 to 0.04; P < 0.001). No data on dietary intake provided. Length of intervention: 2 years (only 1 year results have partly been published) |
|
| Outcomes | Main study outcome: change in cognitive decline (results not yet published) Dropouts: 36 intervention, 21 control (after 1 year) Available outcomes: lipids (for TG and HDL only data states "no between diet differences were observed"), weight (waist circumference was provided but without variance, abstract stated that "there were no significant changes in body fat and waist‐to‐hip ratio over time and between the two groups"). Authors provided data on mortality, CVD events, cancer deaths and diagnoses, IBD diagnosis (no CVD deaths). Cognitive, ophthalmological, inflammatory markers, glycaemic status and other outcomes are not yet available. Response to contact: authors provided additional outcome and methodology data. |
|
| Notes | Study funding: Calfornia Walnut Commission The 2‐year results as well the full 1‐year results are yet to be published. Outcome data reported are for only for participants from one centre (USA) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomized to either the control or walnut group using a computerized random number table with stratification by center, sex, and age range. Couples entering the study were treated as one number and were randomized into the same group". |
| Allocation concealment (selection bias) | Low risk | Author reply states, "Baseline subject data was collected before randomization. Randomization was done by the clinician, pressing the key on the computer. Since this was a dual center (Barcelona and Loma Linda) trial, a single computer software randomized participants for both the centers." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Single blind. "An unavoidable limitation of the study is not being able to blind participants to the intervention since it consists of a whole food" Rajaram 2017. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Author reply states "Study personnel not in contact with the subjects were blind to the treatment assignment. So (lab technicians, ophthalmology technician, neuro cognitive testers) were not aware of the treatment assignment. Of course clinicians who were visited by subjects every two months, knew the treatment assignment". This suggests that allocation was known by physicians, so high risk for event data |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 38/362 dropouts in intervention group = 10.5%. 34/346 dropouts in control group = 9.8%. Similar dropout in groups over 2 years. |
| Selective reporting (reporting bias) | Unclear risk | Although prospectively registered, no full results paper published – results from conference abstracts only report some secondary outcomes |
| Attention | Unclear risk | Not enough details |
| Compliance | Low risk | ALA levels were significantly higher in the intervention group |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (low fat diet (15% fat) with n‐3 fish oils vs AHA Step I diet (fat ≤ 30%) with olive oil supplements), 12 months Summary risk of bias: moderate or high |
|
| Participants | Population: adults with multiple sclerosis N: 15 intervention, 16 control (analysed, intervention: 13, control: 14) Level of risk for CVD: low Men: 15.4% intervention, 14.3% control Mean age in years (SD): 39.9 (10.0) intervention, 45.1 (7.7) control Age range: not reported Smokers: not reported Hypertension: not reported Medications taken by at least 50% of those in the control group: all patients received 400 units of vitamin E, one multivitamin tablet (not containing any PUFA) and at least 500 mg calcium per day Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: USA Ethnicity: not reported |
|
| Interventions | Type: dietary advice plus supplement Comparison: EPA + DHA vs MUFA (low fat diet (15% fat) with n‐3 fish oils vs AHA Step I diet (fat ≤ 30%) with olive oil supplements) Intervention: 1.98 g/d EPA, 1.32 g/d DHA supplements (EPAX 5500 EE, Tishcon Corp) + low fat diet (< 15% total calories). Dose: 3.3 g/d EPA + DHA Control: one 1 g olive oil placebo capsules 6 times daily, moderate fat diet (< 30% total calories) (American Heart Association Step 1 diet) Compliance: assessed by individual food records; intervention 69.2% control 66.7% compliance; also at 12 months there was a significant difference between the fatty acid status of the intervention and control groups in terms of EPA (P = 0.027), as described in table 3 of the main paper Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: physical component scale (PCS) Dropouts: 3 intervention, 7 control Available outcomes: Mental Health Inventory, Modified Fatigue Impact Scale, weight change, HDL and LDL cholesterol, adverse events (MS relapse, TNF‐alpha, ICAM‐1, VCAM‐1 and other inflammatory markers, SF‐36 not used) Response to contact: no |
|
| Notes | Study funding: National Multiple Sclerosis Society (PP0620T), Mellen Center Foundation and ''The Jog for the Jake'' grant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States "randomly assigned", no further details |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Patients knew the percentage of dietary fat but did not know the assignment of capsules oil supplementation." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Discrepancy in numbers of participants discontinued and numbers analysed. Per protocol analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trials register entry found |
| Attention | Low risk | Treated equally |
| Compliance | Low risk | Assessed by individual food records; intervention 69.2% control 66.7% compliance. At 12 months there was a significant difference between the EPA status of the intervention and control groups (P = 0.027). |
| Other bias | Low risk | None noted |
| Methods | Wessex Evaluation of Fatty Liver and Cardiovascular Markers in NAFLD with Omacor Therapy (WELCOME) RCT, parallel, (Omacor or placebo), 15‐18 months Summary risk of bias: low |
|
| Participants | Patients with NAFLD N: 51 intervention, 52 control (analysed, 47 intervention, 48 control) Level of risk for CVD: moderate Men: 49% intervention, 67% control Mean age in years (SD): 48.6 (11.1) intervention, 54 (9.6) control Age range: not reported (18‐75 years inclusion criteria) Smokers: 14.3% intervention, 11.8% control Hypertension: not reported Medications taken by at least 50% of those in the control group: lipid lowering drugs Medications taken by 20%‐49% of those in the control group: antihypertensives, metformin (data not provided by group) Medications taken by some, but less than 20% of the control group: none reported Location: UK Ethnicity: not reported |
|
| Interventions | Type: supplement (Omacor capsules) Comparison: DHA + EPA vs MUFA Intervention: 4 g OMACOR per day (providing 1.84 g EPA, 1.52 g DHA as ethyl esters)]. Dose: 3.36 g/d EPA + DHA Control: 4 g olive oil capsules/ day (providing; ALA1%, oleic acid 67%, palmitic acid 15%, stearic acid 2%, n‐6 fat: 15%) Compliance: was assessed by recording the returned unused capsules and quantification of erthrocyte EPA + DHA enrichment (a prespecified threshold of 2% for DHA & threshold of 0.7% for EPA enrichment) Duration of intervention: 15‐18 months |
|
| Outcomes | Main study outcome: changes in mean liver fat %, changes in 2 liver fibrosis scores, change in serum biomarkers Dropouts: 4 intervention, 4 control Available outcomes: weight, BMI, lipids, blood pressure, glucose, insulin sensitivity, body fat measures, liver enzymes, HbA1c, serum n‐3 FAs, authors provided details of diabetes diagnoses, % body fat, BP and carotid intima media thickness Response to contact: yes |
|
| Notes | Study funding: National Institute for Health Research (NIHR) Southampton Biomedical Research Unit grant and by a Diabetes UK allied health research training fellowship awarded to KGM (Diabetes UK. BDA 09/ 0003937). CDB, PCC and ES are supported in part by the NIHR Southampton Biomedical Research Centre. Omacor and placebo were provided by Pronova Biopharma through Abbott Laboratories, Southampton, UK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were block randomised by an independent clinical trials pharmacist to treatment with identical capsules by mouth of either n‐3 fatty acid ethyl esters (4 g/d Omacor; Pronova, Sandefjord, Norway) or placebo (4 g/d olive oil) for a minimum of 15 months and a maximum of 18 months (McCormick‐2015, p2). Patients were randomised according to standardised procedures (computerised block randomisation) by a research pharmacist at University Hospital Southampton NHS Foundation Trust. Simple randomisation in blocks of 4, either to trial medication or placebo was used. (Scorletti‐2014, p 2) |
| Allocation concealment (selection bias) | Low risk | Participants were block randomised by an independent clinical trials pharmacist to treatment with identical capsules by mouth of either n‐3 fatty acid ethyl esters (4 g/d Omacor; Pronova, Sandefjord, Norway) or placebo (4 g/d olive oil) for a minimum of 15 months and a maximum of 18 months (McCormick‐2015, p2). Only the clinical trials pharmacist was unblinded, and randomisation group allocation was concealed from all study members throughout the trial. (McCormick‐2015, p 2). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Paper states that only the clinical trials pharmacist was unblinded, and randomisation group allocation was concealed from all study members throughout the trial. However, the trial register record states "single blind (investigator)". Although the capsules were identical, no information provided as to their smell and taste |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The ITT analysis included all patients randomised who had complete data (baseline and end‐of‐study measurements), regardless of whether they were later found to be ineligible, a protocol violator, given the wrong treatment allocation, or never treated) (Scorletti 2014, p 4) |
| Selective reporting (reporting bias) | Unclear risk | Prospectively registered September 2008, study start September 2009, end February 2017. Outcome data for cardiac function not yet published, though other cardiovascular measures reported – take as ongoing as recent end date |
| Attention | Low risk | Both groups had the same attention |
| Compliance | Low risk | Assessed by recording the returned unused capsules and quantification of erthrocyte EPA + DHA enrichment (a prespecified threshold of 2% for DHA and threshold of 0.7% for EPA enrichment). Quote: "Enrichment was highly variable in the DHA+EPA group and 5 and 6 participants in the DHA+EPA group did not reach the prespecified threshold for EPA and DHA enrichment, respectively. In the placebo group, we expected no enrichment between baseline and end of study in all participants in this group, but 3 and 4 participants reached the thresholds set for the DHA+EPA group, for EPA and DHA, respectively. One participant in the placebo group admitted to taking cod liver oil during the study and another markedly increased consumption of fish." 10 of 95 non‐compliant |
| Other bias | Low risk | None noted |
| Methods | RCT, parallel, (n‐3 DHA vs n‐6 LA), 12 months Summary risk of bias: moderate to high |
|
| Participants | Otherwise healthy elderly people with mild cognitive impairment. N: 120 intervention, 120 control (analysed, intervention: 110 control: 109) Level of risk for CVD: low Men: 35.8% intervention, 34.2% control Mean age in years (SD): 74.5 (2.65) intervention, 74.6 (3.31) control Age range: eligibility criteria were age 65‐85 years at trial start Smokers: 59.17% intervention, 61.67% control Hypertension: 9.17% intervention, 7.50% control Medications taken by at least 50% of those in the control group: not reported Medications taken by 20%‐49% of those in the control group: not reported Medications taken by some, but less than 20% of the control group: not reported Location: China Ethnicity: assumed Chinese |
|
| Interventions | Type: supplement (capsule) Comparison: DHA vs corn oil (n‐6) Intervention: 1 capsule twice a day, with meals, including 2 g algal DHA (45‐55% DHA by weight). Martek Biosciences, Columbia, MD. Dose: ˜1 g/d DHA Control: corn oil, orange‐flavoured and orange colour to protect the study blind Compliance: participants were asked to return any remaining tablets. Compliance was defined as a ratio (actually taken/should have taken). Achieved 97% for intervention, 95% for control. Serum levels of DHA also measured, DHA at 6 months barely higher in intervention than in controls Duration of intervention: 12 months |
|
| Outcomes | Main study outcome: cognitive function and hippocampal volume Dropouts: 10 intervention, 11 control Available outcomes: mortality, cognitive outcomes and cerebral volume measurements Response to contact: no reply to date |
|
| Notes | Study funding: Chinese Nutrition Society (CNS) Nutrition Research Foundation‐ DSM Research Fund | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated, also statistics analyst ignorant to this study used random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo capsules … identical in appearance. All capsules were orange‐flavoured and orange colour to protect the study blind . Packaged into identical pots, each containing 180 capsules, and labelled by staff who were not involved in the study. A blinding key linked each participant to his or her assigned treatment. This key was kept by an investigator not involved in any data collection or analyses, in a secure electronic file. The code was revealed at the completion of the trial following analyses of the main study aims. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All project staff were unaware of group assignments until the completion of the trial and after data analysis |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | They did not describe how they imputed missing data (lost contact with patients, but called this an ITT analysis). Overall well matched and not high attrition. |
| Selective reporting (reporting bias) | Low risk | Registered trial prospectively. Outcomes match protocol |
| Attention | Low risk | "Adherence was encouraged and monitored throughout the trial by telephone assessment at 15 time points, and by blood assay at baseline" 6 months and 12 months. This and assessments were described as same for both arms. |
| Compliance | Unclear risk | Quote: "participants were requested to return any remaining tablets in order to measure compliance, together with the replenishment of capsules for the following month." Compliance … defined "as a ratio = actually taken/should have taken". "Adherence was encouraged and monitored throughout the trial by telephone assessment at 15 time points, and by blood assay at baseline" 6 months and 12 months On compliance tree, leads to "No, because no P values were supplied" therefore risk of compliance bias unclear |
| Other bias | Unclear risk | Although the register says single blind, the publication very clearly describes a double‐blind RCT |
| Methods | RCT, parallel, (n‐3 fish oil + amiodarone vs amiodarone), 12 months Summary risk of bias: moderate or high |
|
| Participants | Patients with persistent atrial fibrillation (AF) referred to cardioversion N: 23 intervention, 24 control Level of risk for CVD: high Men: 47.8% intervention, 37.5% control Mean age in years (SD): 62 (12) intervention, 61 (11) control Age range: 37‐81 Smokers: not reported Hypertension: 56.5% intervention, 50% control Medications taken by at least 50% of those in the control group: all patients received amiodarone (an antiarrhythmic medication) Medications taken by 20%‐49% of those in the control group: beta‐blockers, statins, ACE inhibitors and ARBs Medications taken by some, but less than 20% of the control group: calcium antagonists Location: Turkey Ethnicity: not reported |
|
| Interventions | Type: supplement (capsule) Comparison: LCn3 vs nil Intervention: 2 g/d n‐3 PUFA (Marincap, Kocak, Turkey). 4 × 500 mg capsules providing EPA 18% (360 mg/d); DHA 12% (240 mg/d). Dose: 0.6 g/d EPA + DHA Control: no placebo. Amiodarone was given to both groups. Compliance: no details Duration of intervention: 12 months or AF recurrence |
|
| Outcomes | Main study outcome: AF recurrence(endpoint) Dropouts: no details Available outcomes: all cause mortality (nil death), stroke, TIA, AF recurrence (hyperthyroidism diagnosis, hospitalisation) Response to contact: not yet attempted |
|
| Notes | Study funding: unclear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomised"; no further details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All were accounted for |
| Selective reporting (reporting bias) | Unclear risk | No trial registry entry or protocol found |
| Attention | Low risk | Both groups seem to have the same care |
| Compliance | Unclear risk | No information |
| Other bias | Low risk | None noted |
ACE: angiotensin‐converting enzyme; ADAS: Alzheimer's Disease Assessment Scale; ADL: activities of daily living; AF: atrial fibrillation; AHA: American Heart Association; BMI: body mass index; ALT: alanine transaminase; ARB: angiotensin‐receptor blocker; BMD: bone mineral density; BMI: body mass index; BP: blood pressure; CABG: coronary artery bypass grafting; CDAI: Clinical Disease Activity Index; CHD: coronary heart disease; CHO: carbohydrate; CV: cardiovascular;CRP: C‐reactive protein; CVD: cardiovascular disease; DAS: Disease Activity Score; DBP: diastolic blood pressure; DHA: docosahexaenoic acid; DM: diabetes mellitus; DMARD: disease‐modifying antirheumatic drugs; DPA: docosapentaenoic acid; E: dietary energy; ECG: electrocardiogram; EDSS: Expanded Disability Status Scale; EPA: eicosapentaenoic acid; ESR: erythrocyte sedimentation rate; FA: fatty acid; FFQ: food frequency questionnaire; FH: family history; FMD: flow‐mediated dilation; GFR: glomular filtration rate; GLA: gamma linolenic acid; HbA1c: glycated haemoglobin; HCQ: hydroxychloroquine; HDL: high‐density lipoprotein; H/O: personal history of; HOMA‐IR: homeostatic model assessment of insulin resistance; HRT: hormone replacement therapy; HT: hypertension; IBD: inflammatory bowel disease; IADL: instrumental activities of daily living; ICAM‐1: intercellular adhesion molecule 1; IL: interleukin;IMT: immune‐mediated thrombocytopenia; IQR: interquartile range; LCn3: long‐chain omega‐3 fatty acids; LDL: low‐density lipoprotein; MD: mean difference; MDA: malondialdehyde; MI: myocardial infarction; MMSE: Mini–Mental State Examination; MS: multiple sclerosis; MUFA: mono‐unsaturated fatty acids; MXT: methotrexate;n‐3: omega‐3; NASH: non‐alcoholic steatohepatitis; NSAID: non‐steroidal anti‐inflammatory drug; PAI1: plasminogen activator inhibitor‐1; PI: principal investigator;PUFA: poly‐unsaturated fatty acids; PTCA: percutaneous transluminal coronary angioplasty; P/S: poly‐unsaturated/saturated fat ratio; QoL: quality of life; QUICKI: quantitative insulin sensitivity check index; RA: rheumatoid arthritis; RCT: randomised controlled trial; SBP: systolic blood pressure; SD: standard deviation;SE: standard error; RCT: randomised controlled trial; SFA: saturated fatty acids; SSZ: sulfasalazine; TAG: triacylglycerol; TG: serum triglycerides; TIA: transient ischaemic attack; TNF: tumour necrosis factor; VCAM‐1: vascular cell adhesion molecule 1; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alekseeva 2000 | Study not randomised |
| Baleztena 2015 | No relevant outcomes measured |
| Belch 1988 | No relevant outcomes measured |
| Belluzzi 1996 | Authors confirmed no relevant outcomes measured |
| Berthoux 1992 | Participants not adult humans, or participants unwell at baseline |
| Borchgrevink 1966 | Mean duration of intervention 10 months (range 3 to 16 months) |
| Busnach 1998 | Participants not adult humans, or participants unwell at baseline |
| CANN 2015 | Intervention is multifactorial (FA/flavanoid blend) |
| Cappelli 1997 | Participants not adult humans, or participants unwell at baseline |
| CARES 2015 | Multisupplement intervention |
| Cheng 1990a | No appropriate control group |
| Cheng 1990b | No appropriate control group |
| Clark 1993 | No relevant outcomes measured |
| Clark 1994 | Participants not adult humans, or participants unwell at baseline |
| Clark 2001 | Participants not adult humans, or participants unwell at baseline |
| Clausen 1989 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| Diskin 1990 | No omega‐3 supplementation or dietary advice |
| Donadio 1994 | Participants not adult humans, or participants unwell at baseline |
| Doyle 2001 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| Dry 1991 | No relevant outcomes measured |
| Ezaki 1999 | Study not randomised |
| Feher 2005 | Intervention is multifactorial (omega 3 given with coenzyme Q and other compounds vs placebo) |
| FISH 2012 | No clinical outcomes collected (confirmed by corresponding author, 30 November 2016) |
| Fonolla 2009 | Intervention was milk enriched with EPA and DHA but also other vitamins and minerals ‐ multifactorial dietary intervention |
| Fonolla‐Joya 2016 | Intervention was milk enriched with EPA and DHA but also other vitamins and minerals ‐ multifactorial dietary intervention |
| Franzen 1989 | Study not randomised |
| Galarraga 2008 | 9‐month intervention period |
| Gapparova 2000 | Study not randomised |
| Gazso 1992 | No omega‐3 supplementation or dietary advice |
| Geusens 1994 | No relevant outcomes measured |
| Gogos 1998 | Participants not adult humans, or participants unwell at baseline |
| Greatrex 2000 | Study not randomised |
| Griffin 1999 | Study not randomised |
| Hamazaki 1984 | Participants not adult humans, or participants unwell at baseline |
| Hansen 1996 | Multi‐factorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| Harris 1991 | No appropriate control group |
| Hashimoto 2012 | No relevant outcomes measured |
| Hashimoto 2016 | No relevant outcomes measured |
| Hawthorne 1992 | Authors confirmed no relevant outcomes measured |
| HEARTS 2015 | Intervention included intensive behavioural changes including exercise and nutrition counselling geared towards weight loss |
| Hogg 1995 | Participants not adult humans, or participants unwell at baseline |
| HOPE epilepsy 2012 | Trial recruitment was suspended due to lack of funding |
| Huang 1996 | No relevant outcomes measured |
| Huang 2008 | Intervention was 9 months and no relevant outcomes |
| ISRCTN38354847 | The proposed one‐year study was never conducted |
| Junker 1990 | Follow‐up not at least a year |
| Kachorovskii 1977 | No omega‐3 supplementation or dietary advice |
| Kanorskii 2007 | LCn3 compared to sotalol (group 1), sotalol & perindopril (group 2), sotalol, perindopril & rosuvastatin (group 3), so no useful control group |
| Karlsson 1998 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| Kaul 1992 | Intervention duration 6 months |
| Khan 2003 | Intervention was 8 months |
| Konya 2000 | Study not randomised |
| Kremer 1995 | < 1 year duration |
| Kruger 1998 | No relevant outcomes measured |
| Kurabayashi 2000 | < 1 year duration |
| Lau 1993 | Authors confirmed no relevant outcomes |
| Leaf 1995 | Study not randomised |
| Lee 2010 | Authors confirmed no relevant outcomes measured |
| Leng 1998 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| LipiDiDiet 2016 | Multifactorial dietary intervention that included omega 3 fats but many other nutrition components |
| Loeschke 1996 | No relevant outcomes measured |
| LUTEGA 2013 | Multisupplement intervention |
| Lyon Diet Heart 1994 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary interventions) |
| Maachi 1995 | Participants not adult humans, or participants unwell at baseline |
| Macsai 2008 | No relevant outcomes measured |
| Mansel 1990 | Not an omega‐3 intervention |
| Mantzaris 1996 | No relevant outcomes measured |
| Mate‐Jimenez 1991 | Authors confirmed no relevant outcomes |
| Matsuyama 2005 | Publication retracted (fraudulent) |
| Middleton 2002 | Unbalanced intervention as the intervention arm contains additional GLA |
| MoodFOOD 2016 | Multisupplement intervention |
| NAYAB 2017 | No planned relevant outcomes. Follow‐up < 12 months |
| NCT01235533 | 48 weeks intervention planned in trials register entry |
| NU‐AGE 2014 | Multifactorial dietary intervention |
| NutriMEMO 2014 | Mutlisupplement intervention |
| OFAMS 2012 | No relevant outcomes measured |
| Okuda 1996 | No appropriate control group |
| OLIVE 1998 | Study was not funded and did not achieve full recruitment (info provided by co‐author) |
| Oslo DIET HEART 1970 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| Pogozheva 1997 | Study not randomised |
| Pogozheva 2000 | Study not randomised |
| Puri 2008 | Authors confirmed no relevant outcomes |
| Quazi 1994 | Study not randomised, < 1 year intervention |
| Sacks 1994 | < 1 year intervention |
| Saynor 1988 | Study not randomised |
| Saynor 1992 | No appropriate control group |
| Selvais 1995 | Intervention was < 1 year |
| Shimizu 1995 | Authors confirmed no relevant outcomes |
| Singh 1992 | Expressions of concern issued by the BMJ and The Lancet regarding research by this first author (BMJ 2005; Horton 2005) |
| Singh 1997a | Expressions of concern issued by theBMJ and The Lancet regarding research by this first author (BMJ 2005; Horton 2005) |
| Singh 1997b | Expressions of concern issued by the BMJ and The Lancet regarding research by this first author (BMJ 2005; Horton 2005) |
| Singh 2002 | Expressions of concern issued by the BMJ and The Lancet regarding research by this first author (BMJ 2005; Horton 2005) |
| Tariq 1989 | Participants not adult humans, or participants unwell at baseline and intervention is < 1 year |
| Terano 1999 | Authors confirmed no relevant outcomes during trial |
| Tomer 2001 | No relevant outcomes. Measured lipids but unclear baseline and endpoint is probably 4 weeks |
| Torjesen 1997 | Multifactorial intervention (cannot separate effects of omega‐3 fats from those of other dietary, behavioural or drug interventions) |
| VSDR 2015 | The supplement (Nutrof Omega) contained DHA, Vit C, E, B1, B2, B3, B6, B9, B12, Zn, Mn, Se, Cu, lutein and zeaxanthin (multifactorial dietary intervention) |
| Wheaton 2010 | Participants were not a minimum of 18 years old |
| Yasui 2001 | No appropriate control group |
| Zinger 1987 | Study not randomised |
DHA: docosahexaenoic acid; EPA: eicosapentaenoic acid; FA: fatty acid; GLA: gamma linolenic acid.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Aboriginal Cardiovascular Omega‐3 randomised controlled trial (AC Omega3) |
| Methods | RCT |
| Participants | Indigenous Australian adults with stable coronary artery disease |
| Interventions | Each for 12 months: Arm 1: omega‐3 (1800 mg/d AlaskOmega: 3 capsules/d: 400 mg EPA and 200 mg DHA) Arm 2: placebo mixed oil capsules (1000 mg/d: 3 capsules/d containing palm oil, gelatin, glycerol, sunflower oil, rapeseed oil, mixed tocopherols, and a "small amount" of fish oil (for taste to aid blinding) |
| Outcomes | Primary: serum non‐HDL‐C Secondary: triglycerides, total cholesterol, LDL cholesterol, HDL cholesterol, lipid functionality by cholesterol efflux and CETP, heart rate variability, platelet function and thrombosis markers, inflammation markers, cumulative combined rate of major adverse cardiac events (including death, non‐fatal MI, unstable angina, non‐fatal stroke, revascularisation and cardiac related hospital admissions) |
| Starting date | Registered on trials registry: 10 July 2014 Study start date: 1 October 2014 Estimated study completion date: unclear |
| Contact information | Alex Brown (PI), Wardliparingga Aboriginal Unit, Adelaide, Australia, alex.brown@sahmri.com |
| Notes | ACTRN12614000732684 Alex Brown contacted in 2016: confirmed study is actively recruiting |
| Trial name or title | Atorvastatin in Factorial with Omega‐3 fatty acid Risk Reduction in Diabetes (AFORRD) |
| Methods | RCT |
| Participants | Patients with type 2 diabetes with no known CVD and not taking lipid‐lowering therapy, adults (> 18 years) N: intervention 397, control 403 (analysed intervention 371, control 361) |
| Interventions | Each for 12 months: Arm 1: atorvastatin (Lipitor 20 mg/d) and olive oil placebo (2 g/d) Arm 2: omega‐3 (Omacor 2 g/d: 46% EPA, 38% DHA) and placebo tablets for atorvastatin Arm 3: atorvastatin (Lipitor 20 mg/d) and Omega‐3 (Omacor 2 g/d: 46% EPA, 38% DHA) Arm 4: placebo tablets for atorvastatin and olive oil placebo (2 g/d) |
| Outcomes | Primary: lipid profiles Secondary: phytosterol changes, HbA1c, estimated CVD risk using the UK Prospective Diabetes Study risk engine |
| Starting date | Registered on trials registry: 4 April 2004 Study start date: 1 November 2004 Estimated study completion date: 31 July 2006 |
| Contact information | Rury Holman, Oxford Centre for Diabetes |
| Notes | ISRCTN76737502 Rury Holman contacted in 2016: confirmed results are not yet published, but planned |
| Trial name or title | A Study of Cardiovascular Events iN Diabetes (ASCEND) |
| Methods | RCT |
| Participants | Patients with diabetes, without vascular disease |
| Interventions | Each for 7 years: Arm 1: omega‐3 (1 g/d: 0.41 g EPA, 0.34 g DHA) and placebo tablets for aspirin Arm 2: aspirin (100 mg/d) and olive oil placebo capsule Arm 3: omega‐3 (1 g/d) and aspirin (100 mg/d) Arm 4: olive oil placebo and placebo tablets for aspirin |
| Outcomes | Primary: cardiovascular events Secondary: mortality, hospitalisations, cancer |
| Starting date | Registered on trials registry: 24 August 2005 Study start date: March 2005 Estimated study completion date: September 2017 |
| Contact information | Jane Armitage (PI), University of Oxford Clinical Trial Service Unit |
| Notes |
NCT00135226 Trial website: ascend.medsci.ox.ac.uk; rum.ctsu.ox.ac.uk/ascend |
| Trial name or title | Clinical efficacy of fish oil as adjunct therapy for patients with chronic periodontitis |
| Methods | RCT |
| Participants | Patients (25‐80 years, non‐smokers) with newly diagnosed severe but non‐aggressive periodontitis |
| Interventions | Each for 13 months: Arm 1: fish oil rich in EPA (6 × 500 mg capsules/d: 277 mg EPA; 27 mg DHA) and standard periodontal treatment (scaling and debridement) Arm 2: fish oil rich in DHA (6 × 500 mg capsules/d: 66 mg EPA; 258 mg DHA) and standard periodontal treatment Arm 3: soya oil placebo (6 × 500 mg capsules/d) and standard periodontal treatment |
| Outcomes | Primary: probing pocket depth, clinical attachment level (CAL) Secondary: inflammatory biomarkers in gingival crevicular fluid, erythrocyte omega‐3, C‐reactive protein |
| Starting date | Registered on trials registry: 23 July 2010 Study start date: July 2010 Estimated study completion date: unclear |
| Contact information | Mark Bartold, University of Adelaide, mark.bartold@adelaide.edu.au |
| Notes | ACTRN12610000594022 PhD, Boram Park, available giving 4 month outcome data for pilot study N = 33 participants Mark Bartold written to in 2016. Confirmed preparing full publications for submission |
| Trial name or title | Beyond Ageing Project phase 2: a selective prevention trial using novel pharmacotherapies in an older age cohort at risk for depression |
| Methods | RCT |
| Participants | Older adults (60+ years) at risk of depression (K‐10 score ranging from 16‐29) who initially participated in the first Beyond Ageing Project |
| Interventions | Each for 12 months: Arm 1: omega‐3 (4 capsules, total 2 g/d: 1200 mg EPA and 800 mg DHA) and placebo microcrystalline cellulose (1 capsule) Arm 2: paraffin oil placebo (4 capsules) and sertraline hydrochloride (1 capsule, 50 mg) Arm 3: paraffin oil placebo (4 capsules) and placebo microcrystalline cellulose (1 capsule) |
| Outcomes | Primary: depressive symptoms (PHQ‐9, patient health questionnaire 9) Secondary: cognitive decline, MMSE, brain metabolism, hippocampal volume, anxiety (assessed using GAD‐7), disability (WHODAS‐II), sleeping problems (PSQI, Pittsburgh Sleep Quality Index), exercise (Active Australian Survey) |
| Starting date | Registered on trials registry: 12 January 2010 Study start date: June 2011 Estimated study completion date: main results expected in 2017 |
| Contact information | Ian Hickie (PI), Brain and Mind Centre, University of Sydney, ian.hickie@sydney.adu.au |
| Notes | ACTRN12610000032055 |
| Trial name or title | Long‐term effects of a reduced fat diet intervention in pre‐diabetes |
| Methods | RCT |
| Participants | Participants with pre‐diabetes, impaired fasting glucose (IFG) or impaired glucose tolerance (IGT), 201 participants discussed in one abstract, 134 in a later abstract |
| Interventions | Each for 3 years: Arm 1: reduced fat diet (fat content at or below 20% total energy, ratio of PUFA/SFA 0.8 to 1.0) Arm 2: normal/control diet |
| Outcomes | Incidence of diabetes, BMI, lipids, insulin, plasma glucose, HbA1c, blood pressure, nutritional intake |
| Starting date | Registered on trials registry: no registration found Study start date: not stated Estimated study completion date: not stated |
| Contact information | Chandrakala Galla, chandrakala.galla@gmail.com; Arpana Gaddam, dr.arpanag@gmail.com |
| Notes | Authors written to in 2016: Dr Gaddam confirmed work submitted as a PhD but not published in full. Requested copy of PhD thesis, but no reply to date. Funding: DiabetOmics India |
| Trial name or title | Influence of different sources of n‐3 fatty acid on plasma lipid in moderately hypercholesterolaemic subjects |
| Methods | RCT |
| Participants | Adults (40‐65 years) with mild to moderate hypercholesterolaemia |
| Interventions | Arm 1: EPA/DHA 1.8 g/d Arm 2: EPA/DHA 3.6 g/d Arm 3: ALA 4 g/d Arm 4: placebo |
| Outcomes | Fatty acids, lipids, cytokines (IL‐6, IL‐1a) |
| Starting date | Registered on trials registry: 13 March 2012 Study start date: unclear Estimated study completion date: unclear |
| Contact information | Su Yixiang, Sun‐Yat Sen University, China, suyx@mail.sysu.edu.cn; Zhou Quan, Guangzhou Medical University, joan_zq@126.com |
| Notes | ChiCTR‐TRC−12002014 Su Yixiang and Zhou Quan contacted in 2016: no response |
| Trial name or title | Vitamin D3‐ omega3‐ home exercise‐ healthy ageing and longevity trial (DO‐HEALTH) |
| Methods | RCT |
| Participants | Community dwelling adults 70 years and older, 50% of seniors enrolled based on a fall in the year before enrolment |
| Interventions | Each for 3 years: Arm 1: omega‐3 (1 g/d, ratio EPA:DHA = 1:2) and vitamin D3 (2000 IU/d) capsules and strength home exercise (3 × 30 min/week) Arm 2: omega‐3 (1 g/d, ratio EPA:DHA = 1:2) and vitamin D3 (2000 IU/d) capsules and flexibility home exercise (3 × 30 min/week) Arm 3: omega‐3 (1 g/d, ratio EPA:DHA = 1:2) and placebo capsules and strength home exercise (3 × 30 min/week) Arm 4: omega‐3 (1 g/d, ratio EPA:DHA = 1:2) and placebo capsules and flexibility home exercise (3 × 30 min/week) Arm 5: placebo and vitamin D3 (2000 IU/d) capsules and strength home exercise (3 × 30 min/week) Arm 6: placebo and vitamin D3 (2000 IU/d) capsules and flexibility home exercise (3 × 30 min/week) Arm 7: placebo and placebo capsules and strength home exercise (3 × 30 min/week) Arm 8: placebo and placebo capsules and flexibility home exercise (3 × 30 min/week) |
| Outcomes | Primary: non‐vertebral fractures, functional decline, blood pressure, cognitive decline, rate of any infection Secondary: other fractures, falls, pain in knee osteoarthritis, musculoskeletal changes, gastro‐intestinal symptoms, mental and oral health, quality of life, life‐expectancy, cardiovascular events, cancer, glucose measures, cost‐benefit. All endpoints supported by a DO‐HEALTH biomarker study |
| Starting date | Registered on trials registry: 6 December 2012 Study start date: December 2012 Estimated study completion date: November 2017 |
| Contact information | Heike Bischoff‐Ferrari (PI), Centre on Aging and Mobility, University of Zurich |
| Notes |
NCT01745263 EudraCT: 2012−001249‐41 www.do‐health.eu |
| Trial name or title | DRy Eye Assessment and Management study (DREAM) |
| Methods | RCT |
| Participants | Adults with dry eye |
| Interventions | Each for 2 years Arm 1: omega‐3 supplements (2000 mg EPA + 1000 mgDHA/d as 5 gel caps) Arm 2: olive oil supplements (5 gel caps) |
| Outcomes | Primary: OSDI score (ocular surface disease index) Secondary: other eye health measures, SF‐36, healthcare utilisation costs, cost‐effectiveness |
| Starting date | Registered on Trials Registry 28 April 2014 Study start date: November 2014 Estimated study completion date: July 2017 |
| Contact information | Penny Asbell, Mount Sinai Icahn School of Medicine (Study Chair), Maureen Maguire, University of Pennsylvania (PI) |
| Notes | NCT02128763 |
| Trial name or title | ENabling Reduction of low‐Grade Inflammation in SEniors (ENRGISE) |
| Methods | RCT |
| Participants | People aged 70+ years with self‐reported walking or stair‐climbing difficulty |
| Interventions | Each for 1 year Arm 1: omega‐3 fish oil (1.4 g/d for 6 months, possibly increasing to 2.8 g/d) Arm 2: losartan 25 mg/d Arm 3: placebo corn oil (for omega‐3) plus placebo cellulose (for losartan) Arm 4: omega‐3 plus losartan Arm 5: placebo corn oil (for omega‐3) Arm 6: placebo cellulose (for losartan) |
| Outcomes | Primary: IL‐6, 400 meter walk test Secondary: short physical performance battery, frailty, hand grip strength, knee dynamometry, SF‐36 |
| Starting date | Registered on Trials Registry 3 February 2016 Study start date: February 2016 Estimated study completion date: March 2018 |
| Contact information | Jane Lu janelu@ufl.edu Michael Stancil mstancil@ufl.edu |
| Notes | NCT02676466 |
| Trial name or title | Intervention of testosterone and fish oil for the prevention of Alzheimer's Disease: InTrePad |
| Methods | RCT |
| Participants | PiB‐PET (Pittsburgh compound B) positive men aged 60 years and over with subjective memory complaints |
| Interventions | Each for 56 weeks: Arm 1: DHA capsules (1720 mg/d) and testosterone undecanoate (intramuscular injection 1000 mg/4 mL every 8 weeks) Arm 2: placebo DHA and testosterone undecanoate (intramuscular injection 1000 mg/4 mL every 8 weeks) Arm 3: placebo DHA and placebo testosterone |
| Outcomes | Primary: PiB score Secondary: neuropsychological, mood and daily functioning questionnaires, beta amyloid levels, fluorodeoxyglucose to assess brain glucose metabolism, inflammatory and oxidative biomarkers, hippocampal volume, quality of life, safety and tolerability of treatment |
| Starting date | Registered on trials registry: 14 January 2013 Study start date: 28 February 2013 Estimated study completion date: not stated |
| Contact information | Ralph Martins (PI), Sir James McCusker Alzheimer's Disease Research Unit, Hollywood Medical Centre, Nedlands, Australia, r.martins@ecu.edu.au |
| Notes | ACTRN12613000034730 Ralph Martins written to in 2016‐ no response |
| Trial name or title | Long‐term effects of interventional strategies to prevent cognitive decline in elderly (MAPT PLUS) |
| Methods | RCT – extension of MAPT trial |
| Participants | Participants of MAPT trial |
| Interventions | Follow‐up 2 year extension of patients in MAPT, after completion of MAPT interventions |
| Outcomes | Primary: cognitive and functional status (Grober and Buschke test) Secondary: markers of cerebral atrophy, cost‐effectiveness |
| Starting date | Registered on trials registry: 30 December 2011 Study start date: December 2011 Estimated study completion date: November 2016 |
| Contact information | Bruno Vellas (PI), University Hospital, Toulouse, vellas.b@chu‐toulouse.fr |
| Notes |
NCT01513252 Bruno Vellas written to in 2016‐ no response |
| Trial name or title | Omega 3 fatty acids in bipolar disorder prophylaxis |
| Methods | RCT |
| Participants | People aged 18 to 65 with bipolar disorder |
| Interventions | Each for 12 months: Arm 1: omega‐3 Arm 2: placebo |
| Outcomes | Prophylactic efficacy |
| Starting date | Trial Registration entry: 2 February 2001 Trial start date: July 2000 Estimated study completion: July 2004 |
| Contact information | Andrew Stoll, Mclean Hospital |
| Notes |
NCT00010868 The PI, Andrew Stoll, appears to have been struck off the medical register in Massachusetts in 2011 (Commonwealth of Massachusetts Board of Registration in Medicine, Adjudicatory Case number 2011−026) so it has not been possible to contact him and no publication of results has been found |
| Trial name or title | Studies of serum PSA (prostate specific antigen) to help resolve the current implication of alpha‐linolenic acid and prostate cancer |
| Methods | RCT |
| Participants | Adults 18‐77 years |
| Interventions | Arm 1: ALA rich diet Arm 2: control (not detailed) |
| Outcomes | Prostate specific antigen, atrial fibrillation |
| Starting date | Registered on trials registry: 29 March 2006 Study start date: unclear Estimated study completion date: unclear |
| Contact information | David Jenkins, University of Toronnto, nutritionproject@smh.toronto.on.ca |
| Notes |
NCT00309439 David Jenkins written to in 2016: confirmed not published in full and data incomplete |
| Trial name or title | Arrhythmia prevention with an alpha‐linolenic enriched diet |
| Methods | RCT, parallel, 2 arm, 12 months |
| Participants | 98 people with successful atrial fibrillation electrical cardioversion |
| Interventions | Canola margarine and oil, rich in ALA, versus a conventional diet (control), for 1 year |
| Outcomes | Length of time to first recurrence of AF |
| Starting date | June 1999, expected finish date June 2003, registered December 2006 so appears to have been carried out |
| Contact information | Principal Investigator: Jean‐Paul Broustet, MD, PhD, Universitary Hospital Haut‐Lévêque Bordeaux France |
| Notes | NCT00410020, registered December 2006, no publication found |
| Trial name or title | Dietary energy restriction and omega‐3 fatty acids on mammary tissue |
| Methods | RCT |
| Participants | Overweight women (30‐55 years) with increased breast cancer risk |
| Interventions | For 1 year: Arm 1: lovaza (omega‐3‐acid ethyl esters) Arm 2: lovaza and dietary energy restriction Arm 3: placebo Arm 4: placebo and dietary energy restriction |
| Outcomes | Ki67 expression at 1 year |
| Starting date | Registered on trials registry: 31 January 2013 Study start date: March 2013 Estimated study completion date: March 2018 |
| Contact information | Andrea Manni, Hershey Medical Centre, amanni@hmc.psu.edu (PI) or Cynthia DuBrock, cdubrock@hmc.psu.edu |
| Notes | NCT01784042. Trials register states "Withdrawn (no funding)" |
| Trial name or title | Investigating a phosphatidylserine based dietary approach for the management of mild cognitive impairment |
| Methods | RCT |
| Participants | People with mild cognitive impairment (MCI) aged 65‐85 years |
| Interventions | Each for 24 months: Arm 1: phosphatidylserine omega‐3 (DHA enriched) Arm 2: placebo cellulose capsules |
| Outcomes | Primary: selective reminding test (SRT) Secondary: mini mental state examination (MMSE), neurological battery test (NBT), dementia (DSM‐4 criteria), mini sleep questionnaire (MSQ), Hamilton Anxiety rating scale (HAM‐A), safety and adverse events |
| Starting date | Registered on trials registry: 6 August 2014 Study start date: September 2014 Estimated study completion date: September 2019 |
| Contact information | Nadia Niemerzyanski, nadiaN@enzymotec.com; Yael Richter, yaelr@enzymotec.com |
| Notes | NCT02211560 |
| Trial name or title | Omega 3 fatty acids and ERPR(‐)HER2(±) breast cancer prevention |
| Methods | RCT |
| Participants | Women at risk for recurrent breast cancer‐ with prior diagnosis of stage 0 to III breast cancer and completion of surgery, chemotherapy or trastuzumab or radiation therapy |
| Interventions | Each for 12 months: Arm 1: omega‐3 high dose capsules (5 g/d EPA + DHA) Arm 2: omega‐3 low dose capsules (0.9 g/d EPA + DHA) |
| Outcomes | Primary: breast adipose tissue metabolites Secondary: cytomorphology or cell proliferation of mammary epithelial cells, DNA promoter methylation and pro‐inflammatory gene expression in mammary epithelial and adipose tissue |
| Starting date | Registered on trials registry: 14 October 2014 Study start date: August 2014 Estimated study completion date: January 2019 |
| Contact information | Anitra Sumbry, anitra.sumbry@osumc.edu; Lisa Yee (PI), Ohio State University |
| Notes | NCT02295059 |
| Trial name or title | Impact of icosapent ethyl on Alzheimer's disease (AD) biomarkers in preclinical adults |
| Methods | RCT |
| Participants | Cognitively healthy adults aged 50 to 70 years whose parents had AD |
| Interventions | Each for 18 months: Arm 1: Icosapent ethyl EPA (Vascepa) 4 g/d gel cap Arm 2: matching gel cap placebo |
| Outcomes | Primary: cerebral blood flow by MRI (magnetic resonance imaging) Secondary: CSF biomarkers of AD, cognitive performance (preclinical Alzheimer's cognitive composite, PACC) |
| Starting date | Registered on trials registry: 21 March 2016 Study start date: December 2016 Estimated study completion date: November 2021 |
| Contact information | Cynthia Carlsson, cynthia.carlsson@va.gov; Elena Beckman, elena.beckman@va.gov |
| Notes | NCT02719327 |
| Trial name or title | OMega‐3 fatty acids in Elderly patients with Myocardial Infarction study (OMEMI) |
| Methods | RCT |
| Participants | Elderly patients (70‐82 years) with acute MI |
| Interventions | Each for 24 months: Arm 1: omega‐3 capsules, 3/d (Pikasol, total of 1.8 g/d EPA + DHA) and standard therapy Arm 2: corn oil placebo, 3/d and standard therapy |
| Outcomes | Primary: composite of total mortality, first non‐fatal recurring AMI, stroke and revascularisation Secondary: new onset atrial fibrillation, adipose tissue, serum fatty acids, makers of endothelial function, inflammation, coagulation and fibrinolytic activity, genes associated with atherothrombosis |
| Starting date | Registered on trials registry: 16 April 2013 Study start date: November 2012 Estimated study completion date: November 2019 |
| Contact information | Svein Solheim, Center for Clinical Heart Research, Oslo University Hospital, arnljot.tveit@vestreviken.no |
| Notes | NCT01841944 |
| Trial name or title | Reduction of cardiovascular events with EPA‐intervention trial (REDUCE‐IT) |
| Methods | RCT |
| Participants | Patients (45 years or over) with hypertriglyceridaemia, with cardiovascular disease or at high risk for cardiovascular disease, and on statin |
| Interventions | Each for 4‐6 years: Arm 1: EPA ethyl ester (AMR101 4 g/d) Arm 2: placebo |
| Outcomes | Primary: composite of cardiovascular death, MI, stroke, coronary revascularisation and hospitalisation for unstable angina Secondary: incidence of additional cardiovascular events, lipid and lipoprotein levels |
| Starting date | Registered on trials registry: 13 December 2011 Study start date: November 2011 Estimated study completion date: December 2017 |
| Contact information | Deepak Bhatt (PI), Brigham and Women's Hospital |
| Notes | NCT01492361 |
| Trial name or title | The seAFOod (systematic evaluation of Aspirin and Fish Oil) Polyp Prevention Trial |
| Methods | RCT |
| Participants | NHS Bowel Cancer Screening Programme patients (55‐73 years) identified as "high risk" (5 or more small adenomas; or 3 or more adenomas with at least one being 10 mm or more in diameter) after their 1st screening colonoscopy |
| Interventions | Each for 12 months: Arm 1: EPA (ALFA capsules: 2 × 500 mg twice daily = 2 g/d) and aspirin placebo (1/d) Arm 2: EPA placebo (capric and capryllic acid triglycerides: 2/d) and aspirin (1/d = 300 mg/d) Arm 3: EPA (ALFA capsules: 2 × 500 mg twice daily = 2 g/d) and aspirin (1/d = 300 mg/d) Arm 4: EPA placebo (cparic and capryllic acid triglycerides: 2/d) and aspirin placebo (1/d) |
| Outcomes | Primary: number of patients with one or more adenomas at 12 months Secondary: adverse events, number of "advanced" adenomas per patients, number of "high risk" patients re‐classified as "intermediate risk", number patients with one or more advanced adenomas, adenoma region in the colorectum, total number of adenomas per patient, number of patients with colorectal cancer, levels of bioactive lipid mediators e.g. omega‐3 |
| Starting date | Trial Registration entry: 6 May 2011 Trial start date: 30 May 2011 Estimated study completion: 31 July 2017 |
| Contact information | Mark Hull, Leeds Institute of Molecular Medicine, m.a.hull@leeds.ac.uk |
| Notes | ISRCTN05926847 EudraCT 2010−020943−10 www.seafood‐trial.co.uk |
| Trial name or title | N‐3 PUFA for vascular cognitive aging |
| Methods | RCT |
| Participants | Older adults (80 years and older) at high risk for cognitive decline and dementia of Alzheimer's type |
| Interventions | Each for 3 years: Arm 1: omega‐3 fish oil (1.65 g/d EPA + DHA) Arm 2: soybean oil placebo (1.65 g/d) |
| Outcomes | Primary: total cerebral white matter volume Secondary: biomarkers of endothelial health, total brain atrophy, medial temporal lobe atrophy, ventricular expansion, trail making test part B, digit symbol WAIS‐R, cerebral blood flow, fractional anisotropy within frontal gyri |
| Starting date | Registered on trials registry: 24 September 2013 Study start date: May 2014 Estimated study completion date: March 2019 |
| Contact information | Alena Borgatti, borgatti@ohsu.edu; James Dursch, dursch@ohsu.edu; Gene Bowman and Lynne Shinto (PIs), Oregon Health and Science University |
| Notes | NCT01953705 |
| Trial name or title | A long‐term outcomes study to assess statin residual risk reduction with EpaNova in high cardiovascular risk patients with hypertriglyceridemia (STRENGTH) |
| Methods | RCT |
| Participants | Adult patients with hypertriglyceridaemia and low HDL and high risk for CVD |
| Interventions | Each for 3‐5 years: Arm 1: omega‐3 carboxylic acid capsule (Epanova, not less than 800 mg/g) and statin (once daily) Arm 2: corn oil placebo capsule and statin (once daily) |
| Outcomes | Primary: time to first occurrence of any component of the composite MACE (cardiovascular death, nonfatal MI, nonfatal stroke, emergent/elective coronary revascularisation, hospitalisation for unstable angina) Secondary: composite measure of cardiovascular events that include the first occurrence of cardiovascular death, nonfatal MI and non‐fatal stroke; composite measure of coronary events that include the first occurrence of cardiac death; first occurrence of individual components of MACE; time to cardiovascular death. Other measures include: all cause mortality, new atrial fibrillation, thrombotic events, heart failure events |
| Starting date | Trial Registration entry: 2 April 2014 Trial start date: October 2014 Estimated study completion: November 2019 |
| Contact information | AstraZeneca Clinical Study Information Centre, information.center@astrazeneca.com. PIs Steven Nissen (Cleveland Clinic), Michael Lincoff (Cleveland Clinic) Stephen Nicholls (Adelaide Clinical Research) |
| Notes |
NCT02104817 EudraCT: 2014−001069−28 |
| Trial name or title | Improving the results of heart bypass surgery using new approaches to surgery and medication (SUPERIORSVG) |
| Methods | RCT |
| Participants | Adults having coronary artery bypass graft (CABG) using saphenous vein graft (SVG) |
| Interventions | Each for 12 months: Arm 1: fish oil supplements (2 × 1 g/d Ocean Nutrition capsules: 55% fish oils EPA:DHA 33%:22%) and SVG conventionally harvested Arm 2: placebo and SVG conventionally harvested Arm 3: fish oil supplements (2 × 1 g/d Ocean Nutrition capsules: 55% fish oils EPA:DHA 33%:22%) and SVG no‐touch harvest Arm 4: placebo and SVG no‐touch harvest |
| Outcomes | Primary: proportion of grafts occluded Secondary: significant stenosis, adverse SVG harvesting events, composite outcome of all‐cause mortality, non‐fatal MI and repeat revascularisation |
| Starting date | Registered on trials registry: 12 January 2010 Study start date: July 2011 Estimated study completion date: December 2016 |
| Contact information | Stephen Fremes, Sunnybrook Health Sciences Centre (PI) |
| Notes | NCT01047449 |
| Trial name or title | Effect of PUFA on vascular healing process in hypercholesterolemic patients with ACS |
| Methods | RCT |
| Participants | Hypercholesterolemic patients (20‐80 years) with acute coronary syndrome who have received successful OCT‐guided PCI (optical coherence tomography‐guided percutaneous coronary intervention) |
| Interventions | Each for 12 months: Arm 1: intensive lipid lowering therapy with both statin and EPA + DHA Arm 2: intensive lipid lowering therapy with both statin and EPA Arm 3: standard lipid lowering therapy with statins |
| Outcomes | Primary: changes in OCT parameter Secondary: lipids, serum plasma profile, inflammatory parameters, adverse cardiovascular events |
| Starting date | Registered on trials registry: 1 February 2014 Study start date: 1 February 2014 Estimated study completion date: 30 June 2019 |
| Contact information | Shiro Uemura (PI), Nara Medical University, Japan, suemura@naramed‐u.ac.jp |
| Notes | UMIN000012825 |
| Trial name or title | VITamin D and omegA‐3 triaL (VITAL) |
| Methods | RCT |
| Participants | Multi‐ethnic population of > 25,000 apparently healthy adults (men 50 years plus, women 55 years plus) without cancer or CVD at baseline |
| Interventions | Each for mean 5 years: Arm 1: omega‐3 (Omacor fish oil, EPA + DHA 1 g/d: 465 mg EPA; 375 mg DHA) and placebo Arm 2: placebo and vitamin D3 (1/d, 2,000IU) Arm 3: omega‐3 (Omacor fish oil, EPA + DHA 1 g/d: 465 mg EPA; 375 mg DHA) and vitamin D3 (1/d, 2000 IU) Arm 4: placebo and placebo |
| Outcomes | Primary: reduction in risk for total cancer and CVD events (a composite of MI, stroke, and cardiovascular mortality) Secondary: lowered risk for expanded composite cardiovascular endpoint (MI, stroke, cardiovascular mortality, coronary revascularisation), the individual components of the primary endpoint, site specific cancers, mortality, diabetes, hypertension, cognitive decline, autoimmune conditions, infections, chronic respiratory disease, depression, bone health, fractures, chronic knee pain, body composition, physical disability, falls, plasma biomarker measures |
| Starting date | Registered on trials registry: 13 January 2010 Study start date: July 2010 Estimated study completion date: December 2017 |
| Contact information | JoAnn Manson or Julie Buring (PIs), Brigham and Women's Hospital, Boston and Harvard School of Public Health, Boston, vitalstudy@rics.bwh.harvard.edu |
| Notes |
NCT01169259 www.vitalstudy.org |
ACS: acute coronary syndrome; AD: Alzheimer's disease; AF: atrial fibrillation; BMI: body mass index; BMI: body mass index; CABG: coronary artery bypass graft; CETP: cholesteryl ester transfer protein; CHD: coronary heart disease; CVD: cardiovascular disease; DHA: docosahexaenoic acid; EPA: eicosapentaenoic acid; GAD‐7: generalised anxiety disorder 7; HbA1c: glycated haemoglobin; HDL: high‐density lipoprotein; IFG: impaired fasting glucose; IGT: impaired glucose tolerance; IL: interleukin; LDL: low‐density lipoprotein; MACE: major adverse coronary event; MI: myocardial infarction; MRI: magentic resonance imaging; OCT: optical coherence tomography; OSDI: ocular surface disease index; PCI: percutaneous coronary intervention; PHQ‐9: patient health questionnaire 9; PI: principal investigator; PSA: prostate specific antigen; PSQI: Pittsburgh Sleep Quality Index; PUFA: poly‐unsaturated fatty acids; RCT: randomised controlled trial; RCT: randomised controlled trial; SFA: saturated fatty acids; SVG: saphenous vein graft.
Contributions of authors
LH and CDS conceived and led the original version of this review; LH, CDS, HM and HVW were authors of the original version of this review. LH designed the searches, and CB developed, refined, ran and de‐duplicated them. ASA, TJB, JSB, PB, GCT, KHOD, HVW, FS and LH screened titles and abstracts; ASA, JSB, PB, GCT and LH assessed full‐text papers for inclusion; LH, PB and JSB searched trials registers and assessed entries for inclusion; LH and ASA located full texts, managed assessment and collection of titles, abstracts and full texts, data extraction and risk of bias assessment. All authors carried out data extraction and assessed risk of bias. LH, KHOD and JSB designed risk of bias assessment; JSB, KHOD, TJB, ASA and LH wrote to study authors; LH, KHOD, JSB, TJB and ASA carried out data checks; JSB, TJB, LH and ASA tabulated intake and status data. FS, KHOD, JSB, HVW, CDS and LH provided methodological support. ASA, FKA and LH entered data into RevMan and ran meta‐analyses, ASA and LH carried out sensitivity and subgroup analyses, and LH the meta‐regression. ASA wrote the first draft of the review and LH the WHO NUGAG Subgroup on Diet and Health report; both carried out GRADE assessment and interpretation. All authors critically read and commented on the final draft and agreed on it for submission.
Sources of support
Internal sources
University of East Anglia, UK.
-
Cochrane Heart Group, UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Heart Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health, UK
External sources
-
World Health Organization nutrition guidance expert advisory group (NUGAG), Not specified.
WHO NUGAG Subgroup on Diet and Health requested and funded the update and extension of this review.
Declarations of interest
ASA: none known. TJB: none known. JSB: none known. PB: none known. GCT: none known. HJM: none known. KHOD: none known. FKA: none known. CDS: none known. HVW: none known. FS: none known. LH: none known.
Edited (no change to conclusions)
References
References to studies included in this review
- Quinn JF, Raman R, Thomas RG, Yurko‐Mauro K, Nelson EB, Dyck C, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trial. JAMA 2010;304(17):1903‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigam A, Talajic M, Roy D, Nattel S, Lambert J, Nozza A, et al. Fish oil for the reduction of atrial fibrillation recurrence, inflammation, and oxidative stress. Journal of the American College of Cardiology 2014;64(14):1441‐8. [DOI] [PubMed] [Google Scholar]; Nigam A, Talajic M, Roy D, Nattel S, Lambert J, Nozza A, et al. Multicentre trial of fish oil for the reduction of atrial fibrillation recurrence, inflammation and oxidative stress: the atrial fibrillation fish oil research study. Canadian Journal of Cardiology 2013;1:S383. [DOI] [PubMed] [Google Scholar]
- Ahn J, Park SK, Park TS, Kim JH, Yun E, Kim SP, et al. Effect of n‐3 polyunsaturated fatty acids on regression of coronary atherosclerosis in statin treated patients undergoing percutaneous coronary intervention. Korean Circulation Journal 2016;46(4):481‐9. [PUBMED: 27482256] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer IA, Geleijnse JM, Klaasen VM, Smit LA, Giltay EJ, Goede J, et al. Effect of alpha linolenic acid supplementation on serum prostate specific antigen (PSA): results from the alpha omega trial. PLOS ONE 2013;8(12):e81519. [DOI] [PMC free article] [PubMed] [Google Scholar]; Eussen SR, Geleijnse JM, Giltay EJ, Rompelberg CJ, Klungel OH, Kromhout D. Effects of n‐3 fatty acids on major cardiovascular events in statin users and non‐users with a history of myocardial infarction. European Heart Journal 2012;33(13):1582‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]; Geleijnse J, Giltay E, Kromhout D. Effects of n‐3 fatty acids on cognitive decline: a randomized double‐blind, placebo‐controlled trial in stable myocardial infarction patients. Alzheimer's & Dementia 2011;1:S512. [DOI] [PubMed] [Google Scholar]; Geleijnse JM, Giltay EJ, Kromhout D. Effects of n‐3 fatty acids on cognitive decline: a randomized, double‐blind, placebo‐controlled trial in stable myocardial infarction patients. Alzheimer's & Dementia 2012;8(4):278‐87. [DOI] [PubMed] [Google Scholar]; Geleijnse JM, Giltay EJ, Schouten EG, Goede J, Oude Griep LM, Teitsma‐Jansen AM, et al. Effect of low doses of n‐3 fatty acids on cardiovascular diseases in 4,837 post‐myocardial infarction patients: design and baseline characteristics of the Alpha Omega Trial. American Heart Journal 2010;159(4):539‐46. [DOI: 10/1016/j.ahj.2009.12.033] [DOI] [PubMed] [Google Scholar]; Giltay EJ, Geleijnse JM, Heijboer AC, Goede J, Oude Griep LM, Blankenstein MA, et al. No effects of n‐3 fatty acid supplementation on serum total testosterone levels in older men: the Alpha Omega Trial. International Journal of Andrology 2012;35(5):680‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Giltay EJ, Geleijnse JM, Kromhout D. Effects of n‐3 fatty acids on depressive symptoms and dispositional optimism after myocardial infarction. American Journal of Clinical Nutrition 2011;94(6):1442‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hoogeveen E, Gemen E, Geleijnse M, Kusters R, Kromhout D, Giltay E. Effects of N‐3 fatty acids on decline of kidney function after myocardial infarction: Alpha Omega Trial. Nephrology Dialysis Transplantation 2012;27:ii64. [Google Scholar]; Hoogeveen EK, Geleijnse JM, Kromhout D, Giltay EJ. No effect of n‐3 fatty acids on high‐sensitivity C‐reactive protein after myocardial infarction: the Alpha Omega Trial. European Journal of Preventive Cardiology 2014;21(11):1429‐36. [DOI] [PubMed] [Google Scholar]; Hoogeveen EK, Geleijnse JM, Kromhout D, Stijnen T, Gemen EF, Kusters R, et al. Effect of omega‐3 fatty acids on kidney function after myocardial infarction: the Alpha Omega Trial. Clinical Journal of The American Society of Nephrology: CJASN 2014;9(10):1676‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kromhout D, Geleijnse JM, Goede J, Oude Griep LM, Mulder BJ, Boer MJ, et al. N‐3 fatty acids, ventricular arrhythmia‐related events, and fatal myocardial infarction in post myocardial infarction patients with diabetes. Diabetes Care 2011;34(12):2515‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kromhout D, Giltay EJ, Geleijnse JM, Alpha Omega Trial Group. N‐3 fatty acids and cardiovascular events after myocardial infarction. New England Journal of Medicine 2010;363(18):2015‐26. [DOI] [PubMed] [Google Scholar]
- Brouwer IA, Geleijnse JM, Klaasen VM, Smit LA, Giltay EJ, Goede J, et al. Effect of alpha linolenic acid supplementation on serum prostate specific antigen (PSA): results from the alpha omega trial. PLOS ONE 2013;8(12):e81519. [DOI] [PMC free article] [PubMed] [Google Scholar]; Eussen SR, Geleijnse JM, Giltay EJ, Rompelberg CJ, Klungel OH, Kromhout D. Effects of n‐3 fatty acids on major cardiovascular events in statin users and non‐users with a history of myocardial infarction. European Heart Journal 2012;33(13):1582‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]; Geleijnse J, Giltay E, Kromhout D. Effects of n‐3 fatty acids on cognitive decline: A randomized double‐blind, placebo‐controlled trial in stable myocardial infarction patients. Alzheimer's & Dementia 2011;1:S512. [DOI] [PubMed] [Google Scholar]; Geleijnse JM, Giltay EJ, Kromhout D. Effects of n‐3 fatty acids on cognitive decline: a randomized, double‐blind, placebo‐controlled trial in stable myocardial infarction patients. Alzheimer's & Dementia 2012;8(4):278‐87. [DOI] [PubMed] [Google Scholar]; Geleijnse JM, Giltay EJ, Schouten EG, Goede J, Oude Griep LM, Teitsma‐Jansen AM, et al. Effect of low doses of n‐3 fatty acids on cardiovascular diseases in 4,837 post‐myocardial infarction patients: design and baseline characteristics of the Alpha Omega Trial. American Heart Journal 2010;159(4):539‐46. [DOI: 10/1016/j.ahj.2009.12.033] [DOI] [PubMed] [Google Scholar]; Giltay EJ, Geleijnse JM, Heijboer AC, Goede J, Oude Griep LM, Blankenstein MA, et al. No effects of n‐3 fatty acid supplementation on serum total testosterone levels in older men: the Alpha Omega Trial. International Journal of Andrology 2012;35(5):680‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Giltay EJ, Geleijnse JM, Kromhout D. Effects of n‐3 fatty acids on depressive symptoms and dispositional optimism after myocardial infarction. American Journal of Clinical Nutrition 2011;94(6):1442‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]; Hoogeveen E, Gemen E, Geleijnse M, Kusters R, Kromhout D, Giltay E. Effects of N‐3 fatty acids on decline of kidney function after myocardial infarction: Alpha Omega Trial. Nephrology Dialysis Transplantation 2012;27:ii64. [Google Scholar]; Hoogeveen EK, Geleijnse JM, Kromhout D, Giltay EJ. No effect of n‐3 fatty acids on high‐sensitivity C‐reactive protein after myocardial infarction: the Alpha Omega Trial. European Journal of Preventive Cardiology 2014;21(11):1429‐36. [DOI] [PubMed] [Google Scholar]; Hoogeveen EK, Geleijnse JM, Kromhout D, Stijnen T, Gemen EF, Kusters R, et al. Effect of omega‐3 fatty acids on kidney function after myocardial infarction: the Alpha Omega Trial. Clinical Journal of The American Society of Nephrology: CJASN 2014;9(10):1676‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kromhout D, Geleijnse JM, Goede J, Oude Griep LM, Mulder BJ, Boer MJ, et al. N‐3 fatty acids, ventricular arrhythmia‐related events, and fatal myocardial infarction in post myocardial infarction patients with diabetes. Diabetes Care 2011;34(12):2515‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kromhout D, Giltay EJ, Geleijnse JM, Alpha Omega Trial Group. N‐3 fatty acids and cardiovascular events after myocardial infarction. New England Journal of Medicine 2010;363(18):2015‐26. [DOI] [PubMed] [Google Scholar]
- Age‐Related Eye Disease Study 2(AREDS2) Research Group. Lutein + zeaxanthin and omega‐3 fatty acids for age‐related macular degeneration: the Age‐Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA 2013;309(19):2005‐15. [PUBMED: 23644932] [DOI] [PubMed] [Google Scholar]; Age‐Related Eye Disease Study, Chew EY, Clemons TE, SanGiovanni JP, Danis RP, Ferris FL 3rd, et al. Secondary analyses of the effects of lutein/zeaxanthin on age‐related macular degeneration progression: AREDS2 report No. 3. JAMA Ophthalmology 2014;132(2):142‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]; Age‐Related Eye Disease Study, Chew EY, SanGiovanni JP, Ferris FL, Wong WT, Agron E, et al. Lutein/zeaxanthin for the treatment of age‐related cataract: AREDS2 randomized trial report no. 4. JAMA Ophthalmology 2013;131(7):843‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]; Age‐Related Eye Disease Study, Huynh N, Nicholson BP, Agron E, Clemons TE, Bressler SB, et al. Visual acuity after cataract surgery in patients with age‐related macular degeneration: age‐related eye disease study 2 report number 5. Ophthalmology 2014;121(6):1229‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bonds DE, Harrington M, Worrall BB, Bertoni AG, Eaton CB, et al. Writing Group for the AREDS Research Group. Effect of long‐chain omega‐3 fatty acids and lutein + zeaxanthin supplements on cardiovascular outcomes: results of the Age‐Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA Internal Medicine 2014;174(5):763‐71. [DOI] [PubMed] [Google Scholar]; Chew EY, Clemons T, SanGiovanni JP, Danis R, Domalpally A, et al. Group Areds Research. The Age‐Related Eye Disease Study 2 (AREDS2): study design and baseline characteristics (AREDS2 report number 1). Ophthalmology 2012;119(11):2282‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chew EY, Clemons TE. In reply: Making sense of the evidence from the age‐related eye disease study 2 randomized clinical trial. JAMA Ophthalmology 2014;132(8):1031‐2. [DOI] [PubMed] [Google Scholar]; Chew EY, Clemons TE, Agron E, Launer LJ, Grodstein F, Bernstein PS, et al. Effect of omega‐3 fatty acids, lutein/zeaxanthin, or other nutrient supplementation on cognitive function: the AREDS2 randomized clinical trial. JAMA 2015;314(8):791‐801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldassarre D, Amato M, Eligini S, Barbieri SS, Mussoni L, Frigerio B, et al. Effect of n‐3 fatty acids on carotid atherosclerosis and haemostasis in patients with combined hyperlipoproteinemia: a double‐blind pilot study in primary prevention. Annals of Medicine 2006;38(5):367‐75. [DOI: 10.1080/07853890600852880] [DOI] [PubMed] [Google Scholar]
- Bates D, Cartlidge NE, French JM, Jackson MJ, Nightingale S, Shaw DA, et al. A double‐blind controlled trial of long chain n‐3 polyunsaturated fatty acids in the treatment of multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry 1989;52(1):18‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berson EL, Rosner B, Sandberg MA, Weigel‐DiFranco C, Moser A, Brockhurst RJ, et al. Clinical trial of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment. Archives of Ophthalmology 2004;122(9):1297‐305. [DOI] [PubMed] [Google Scholar]; Berson EL, Rosner B, Sandberg MA, Weigel‐DiFranco C, Moser A, Brockhurst RJ, et al. Further evaluation of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment: subgroup analyses. Archives of Ophthalmology 2004;122(9):1306‐14. [DOI] [PubMed] [Google Scholar]
- Brox J, Olaussen K, Osterud B, Elvevoll EO, Bjornstad E, Brattebog G, et al. A long‐term seal‐ and cod‐liver‐oil supplementation in hypercholesterolemic subjects. Lipids 2001;36(1):7‐13. [DOI] [PubMed] [Google Scholar]
- Argo CK, Patrie JT, Lackner C, Henry TD, Lange EE, Weltman AL, et al. Effects of n‐3 fish oil on metabolic and histological parameters in NASH: a double‐blind, randomized, placebo‐controlled trial. Journal of Hepatology 2015;62(1):190‐7. [PUBMED: 25195547] [DOI] [PMC free article] [PubMed] [Google Scholar]; Caldwell SH, Argo CK, Henry TD, Lackner C, Pramoonjago P, Weltman AL, et al. Dissociated histological and metabolic effects of omega‐3 (3000 mg/d) versus placebo with both exercise and diet in a double‐blind randomized controlled trial of NASH. Journal of Hepatology2011; Vol. 54, issue Supplement 1:S8.
- Burr ML, Fehily AM. Fatty fish and heart disease: a randomized controlled trial. World Review of Nutrition and Dietetics 1991;66:306‐12. [DOI] [PubMed] [Google Scholar]; Burr ML, Fehily AM. Fish and the heart. Lancet 1989;ii:1451‐2. [Google Scholar]; Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet 1989;2(8666):757‐61. [DOI] [PubMed] [Google Scholar]; Burr ML, Fehily AM, Rogers S, Welsby E, King S, Sandham S. Diet and reinfarction trial (DART): design, recruitment, and compliance. European Heart Journal 1989;10(6):558‐67. [DOI] [PubMed] [Google Scholar]; Burr ML, Holliday RM, Fehily AM, Whitehead PJ. Haematological prognostic indices after myocardial infarction: evidence from the diet and reinfarction trial (DART). European Heart Journal 1992;13(2):166‐70. [DOI] [PubMed] [Google Scholar]; Burr ML, Sweetham PM, Fehily AM. Diet and reinfarction. European Heart Journal 1994;15(8):1152‐3. [DOI] [PubMed] [Google Scholar]; Fehily AM, Vaughan‐Williams E, Shiels K, Williams AH, Horner M, Bingham G, et al. Factors influencing compliance with dietary advice: the Diet and Reinfarction Trial (DART). Journal of Human Nutrition and Dietetics 1991;4:33‐42. [Google Scholar]; Fehily AM, Vaughan‐Williams E, Shiels K, Williams AH, Horner M, Bingham G, et al. The effect of dietary advice on nutrient intakes: evidence from the diet and reinfarction trial (DART). Journal of Human Nutrition & Dietetics 1989;2:4235. [Google Scholar]; Ness AR, Hughes J, Elwood PC, Whitley E, Smith GD, Burr ML. The long‐term effect of dietary advice in men with coronary disease: follow‐up of the Diet and Reinfarction Trial (DART). European Journal of Clinical Nutrition 2002;56(6):512‐8. [DOI] [PubMed] [Google Scholar]; Ness AR, Whitley E, Burr ML, Elwood PC, Smith GD, Ebrahim S. The long‐term effect of advice to eat more fish on blood pressure in men with coronary disease: results from the diet and reinfarction trial. Journal of Human Hypertension 1999;13(11):729‐33. [DOI] [PubMed] [Google Scholar]
- Burr ML. Secondary prevention of CHD in UK men: the diet and reinfarction trial and its sequel. Proceedings of the Nutrition Society 2007;66(1):9‐15. [PUBMED: 17343767] [DOI] [PubMed] [Google Scholar]; Burr ML, Ashfield‐Watt PA, Dunstan FD, Fehily AM, Breay P, Ashton T, et al. Lack of benefit of dietary advice to men with angina: results of a controlled trial. European Journal of Clinical Nutrition 2003;57(2):193‐200. [DOI] [PubMed] [Google Scholar]; Burr ML, Dunstan FD, George CH. Is fish oil good or bad for heart disease? Two trials with apparently conflicting results. Journal of Membrane Biology 2005;206(2):155‐63. [PUBMED: 16456725] [DOI] [PubMed] [Google Scholar]; Ness AR, Ashfield‐Watt PAL, Whiting JM, Smith GD, Hughes J, Burr ML. The long‐term effect of dietary advice on the diet of men with angina: the diet and angina randomized trial. Journal of Human Nutrition and Dietetics 2004;17:1‐3. [DOI] [PubMed] [Google Scholar]; Ness AR, Gallacher JE, Bennett PD, Gunnell DJ, Rogers PJ, Kessler D, et al. Advice to eat fish and mood: a randomised controlled trial in men with angina. Nutritional Neuroscience 2003;6(1):63‐5. [DOI] [PubMed] [Google Scholar]
- Derosa G, Cicero AF, D'Angelo A, Borghi C, Maffioli P. Effects of n‐3 PUFAs on fasting plasma glucose and insulin resistance in patients with impaired fasting glucose or impaired glucose tolerance. BioFactors (Oxford, England) 2016;42(3):316‐22. [PUBMED: 27040503] [DOI] [PubMed] [Google Scholar]
- Blok WL, Deslypere JP, Demacker PN, Ven‐Jongekrijg J, Hectors MP, Meer JW, et al. Pro‐ and anti‐inflammatory cytokines in healthy volunteers fed various doses of fish oil for 1 year. European Journal of Clinical Investigation 1997;27(12):1003‐8. [PUBMED: 9466128] [DOI] [PubMed] [Google Scholar]; Deslypere JP. Influence of supplementation with n‐3 fatty acids on different coronary risk factors in men: a placebo controlled study. Verhandelingen ‐ Koninklijke Academie voor Geneeskunde van Belgie 1992;54(3):189‐216. [PUBMED: 1413984] [PubMed] [Google Scholar]; Katan MB, Deslypere JP, Birgelen AP, Penders M, Zegwaard M. Kinetics of the incorporation of dietary fatty acids into serum cholesteryl esters, erythrocyte membranes, and adipose tissue: an 18‐month controlled study. Journal of Lipid Research 1997;38(10):2012‐22. [PUBMED: 9374124] [PubMed] [Google Scholar]
- Tokudome S, Kuriki K, Yokoyama Y, Sasaki M, Joh T, Kamiya T, et al. Dietary n‐3/long‐chain n‐3 polyunsaturated fatty acids for prevention of sporadic colorectal tumors: a randomized controlled trial in polypectomized participants. Prostaglandins Leukotrienes and Essential Fatty Acids 2015;94:1‐11. [PUBMED: 25451556] [DOI] [PubMed] [Google Scholar]; Tokudome S, Yokoyama Y, Kamiya T, Seno K, Okuyama H, Kuriki K, et al. Rationale and study design of dietary intervention in patients polypectomized for tumors of the colorectum. Japanese Journal of Clinical Oncology 2002;32(12):550‐3. [PUBMED: 12578906] [DOI] [PubMed] [Google Scholar]
- Harrison RA. Dietary Intervention for Maintaining Sinus Rhythm Following Cardioversion for Atrial Fibrillation: a Randomised Controlled Trial [PhD thesis]. Manchester (UK): Faculty of Medicine, Dentistry, Nursing and Pharmacy, 2005. [Google Scholar]; Harrison RA, Elton P. From pies to pilchards: dietary assistants increase consumption of oil rich fish. Journal of Epidemiology and Community Health 2000;Suppl:6. [Google Scholar]; Harrison RA, Elton PJ. Can an oil‐rich fish diet improve treatment outcomes following cardioversion for atrial fibrillation? A randomised controlled trial. Study design and compliance. International Society for the Study of Fatty Acids and Lipids (ISSFAL); 2002 May; Montreal, Canada. 2002. [Google Scholar]; Harrison RA, Elton PJ. Is there a role for long‐chain omega3 or oil‐rich fish in the treatment of atrial fibrillation?. Medical Hypotheses 2005;64(1):59‐63. [PUBMED: 15533612] [DOI] [PubMed] [Google Scholar]; Harrison RA, Purnell P, Elton PJ. Using community‐based dietary assistants to increase the intake of oil‐rich fish among older people. European Journal of Public Health 2003;13(Suppl 1):105. 12803407 [Google Scholar]; Harrison RA, Suresh V, Purnell B, Roberts C, Houghton P, Miller J, et al. Can oil‐rich fish sustain normal sinus rhythm after cardioversion for atrial fibrillation? An RCT (DISAF). Author supplied data 29 September 2010.
- Dodin S, Cunnane SC, Masse B, Lemay A, Jacques H, Asselin G, et al. Flaxseed on cardiovascular disease markers in healthy menopausal women: a randomized, double‐blind, placebo‐controlled trial. Nutrition (Burbank, CA) 2008;24(1):23‐30. [PUBMED: 17981439] [DOI] [PubMed] [Google Scholar]; Dodin S, Lemay A, Jacques H, Legare F, Forest JC, Masse B. The effects of flaxseed dietary supplement on lipid profile, bone mineral density, and symptoms in menopausal women: a randomized, double‐blind, wheat germ placebo‐controlled clinical trial. Journal of Clinical Endocrinology and Metabolism 2005;90(3):1390‐7. [PUBMED: 15613422] [DOI] [PubMed] [Google Scholar]
- Doi M, Nosaka K, Miyoshi T, Iwamoto M, Kajiya M, Okawa K, et al. Clinical outcomes of early initiation of pure eicosapentaenoic acid supplement after percutaneous coronary intervention in patients with acute coronary syndrome. European Heart Journal 2014;35(Abstract Suppl):1156. [Google Scholar]; Doi M, Nosaka K, Miyoshi T, Iwamoto M, Kajiya M, Okawa K, et al. Early eicosapentaenoic acid treatment after percutaneous coronary intervention reduces acute inflammatory responses and ventricular arrhythmias in patients with acute myocardial infarction: a randomized, controlled study. International Journal of Cardiology 2014;176(3):577‐82. [PUBMED: 25305703] [DOI] [PubMed] [Google Scholar]; Nosaka K, Miyoshi T, Iwamoto M, Kajiya M, Okawa K, Tsukuda S, et al. Early initiation of eicosapentaenoic acid and statin treatment is associated with better clinical outcomes than statin alone in patients with acute coronary syndromes: 1‐year outcomes of a randomized controlled study. International Journal of Cardiology 2017;228:173‐9. [DOI: 10.1016/j.ijcard.2016.11.105] [DOI] [PubMed] [Google Scholar]; Nosaka K, Miyoshi T, Okawa K, Tsukuda S, Sogo M, Nishibe T, et al. Early initiation of eicosapentaenoic acid and statin treatment is associated with better clinical outcomes than statin alone in patients with acute coronary syndromes: 1‐year outcomes of a randomized controlled study. Journal of the American College of Cardiology. 2016; Vol. 67:573. [DOI] [PubMed] [Google Scholar]
- Berstad P, Seljeflot I, Veierod MB, Hjerkinn EM, Arnesen H, Pedersen JI. Supplementation with fish oil affects the association between very long‐chain n‐3 polyunsaturated fatty acids in serum non‐esterified fatty acids and soluble vascular cell adhesion molecule‐1. Clinical Science 2003;105(1):13‐20. [DOI] [PubMed] [Google Scholar]; Eid HM, Arnesen H, Hjerkinn EM, Lyberg T, Ellingsen I, Seljeflot I. Effect of diet and omega‐3 fatty acid intervention on asymmetric dimethylarginine. Nutrition & Metabolism 2006;3:4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Eid HMA, Arnesen H, Hjerkinn EM, Lyberg T, Ellingsen I, Seljeflot I. Effect of diet and omega‐3 fatty acid intervention on asymmetric dimethylarginine. Nutrition and Metabolism 2006;3:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]; Einvik G, Ekeberg O, Klemsdal TO, Sandvik L, Hjerkinn EM. Physical distress is associated with cardiovascular events in a high risk population of elderly men. BMC Cardiovascular Disorders 2009;9:14. [PUBMED: 19331677] [DOI] [PMC free article] [PubMed] [Google Scholar]; Einvik G, Ekeberg O, Lavik JG, Ellingsen I, Klemsdal TO, Hjerkinn EM. The influence of long‐term awareness of hyperlipidemia and of 3 years of dietary counselling on depression, anxiety, and quality of life. Journal of Psychosomatic Research 2010;68(6):567‐72. [DOI] [PubMed] [Google Scholar]; Einvik G, Klemsdal TO, Sandvik L, Hjerkinn EM. A randomized clinical trial on n‐3 polyunsaturated fatty acids supplementation and all‐cause mortality in elderly men at high cardiovascular risk. European Journal of Cardiovascular Prevention & Rehabilitation 2010;17(5):588‐92. [DOI] [PubMed] [Google Scholar]; Ellingsen I, Hjerkinn EM, Arnesen H, Seljeflot I, Hjermann I, Tonstad S. Follow‐up of diet and cardiovascular risk factors 20 years after cessation of intervention in the Oslo Diet and Antismoking study. European Journal of Clinical Nutrition 2006;60(3):378‐85. [DOI] [PubMed] [Google Scholar]; Furenes EB, Seljeflot I, Solheim S, Hjerkinn EM, Arnesen H, Furenes EB. Long‐term influence of diet and/or omega‐3 fatty acids on matrix metalloproteinase‐9 and pregnancy‐associated plasma protein‐A in men at high risk of coronary heart disease. Scandinavian Journal of Clinical and Laboratory Investigation 2008;68(3):177‐84. [DOI] [PubMed] [Google Scholar]; Hjerkinn EM, Abdelnoor M, Breivik L, Bergengen L, Ellingsen I, Seljeflot I, et al. Effect of diet or very long chain omega‐3 fatty acids on progression of atherosclerosis, evaluated by carotid plaques, intima‐media thickness and by pulse wave propagation in elderly men with hypercholesterolaemia. European Journal of Cardiovascular Prevention & Rehabilitation 2006;13(3):325‐33. [DOI] [PubMed] [Google Scholar]; Hjerkinn EM, Seljeflot I, Ellingsen I, Berstad P, Hjermann I, Sandvik L, et al. Influence of long‐term intervention with dietary counselling, long‐chain n‐3 fatty acid supplements, or both on circulating markers of endothelial activation in men with long‐standing hyperlipidemia. American Journal of Clinical Nutrition 2005;81(3):583‐9. [DOI] [PubMed] [Google Scholar]; Lindman AS, Pedersen JI, Hjerkinn EM, Arnesen H, Veierod MB, Ellingsen I, et al. The effects of long‐term diet and omega‐3 fatty acid supplementation on coagulation factor VII and serum phospholipids with special emphasis on the R353Q polymorphism of the FVII gene. Thrombosis & Haemostasis 2004;91(6):1097‐104. [DOI] [PubMed] [Google Scholar]; Troseid M, Arnesen H, Hjerkinn EM, Seljeflot I. Serum levels of interleukin‐18 are reduced by diet and n‐3 fatty acid intervention in elderly high‐risk men. Metabolism: Clinical & Experimental 2009;58(11):1543‐9. [DOI] [PubMed] [Google Scholar]; Troseid M, Seljeflot I, Weiss TW, Klemsdal TO, Hjerkinn EM, Arnesen H. Arterial stiffness is independently associated with interleukin‐18 and components of the metabolic syndrome. Atherosclerosis 2010;209(2):337‐9. [DOI] [PubMed] [Google Scholar]
- Sanyal AJ, Abdelmalek MF, Suzuki A, Cummings OW, Chojkier M. No significant effects of ethyl‐eicosapentanoic acid on histologic features of nonalcoholic steatohepatitis in a phase 2 trial. Gastroenterology 2014;147(2):377‐84.e1. [PUBMED: 24818764] [DOI] [PubMed] [Google Scholar]
- Feagan BG, Sandborn WJ, Mittmann U, Bar‐Meir S, D'Haens G, Bradette M, et al. Omega‐3 free fatty acids for the maintenance of remission in Crohn disease: the EPIC randomized controlled trials. JAMA 2008;299(14):1690‐7. [DOI] [PubMed] [Google Scholar]
- Feagan BG, Sandborn WJ, Mittmann U, Bar‐Meir S, D'Haens G, Bradette M, et al. Omega‐3 free fatty acids for the maintenance of remission in Crohn disease: the EPIC randomized controlled trials. JAMA 2008;229(14):1690‐7. [DOI] [PubMed] [Google Scholar]
- Danthiir V, Burns NR, Nettelbeck T, Wilson C, Wittert G. The older people, omega‐3, and cognitive health (EPOCH) trial design and methodology: a randomised, double‐blind, controlled trial investigating the effect of long‐chain omega‐3 fatty acids on cognitive ageing and wellbeing in cognitively healthy older adults. Nutrition Journal 2011;10:117. [PUBMED: 22011460] [DOI] [PMC free article] [PubMed] [Google Scholar]; Danthiir V, Hosking D, Burns NR, Wilson C, Nettelbeck T, Calvaresi E, et al. Cognitive performance in older adults is inversely associated with fish consumption but not erythrocyte membrane n‐3 fatty acids. Journal of Nutrition 2014;144(3):311‐20. [PUBMED: 24353345] [DOI] [PubMed] [Google Scholar]
- Erdogan A, Bayer M, Kollath D, Greiss H, Voss R, Neumann T, et al. Omega AF study: polyunsaturated fatty acids (PUFA) for prevention of atrial fibrillation relapse after successful external cardioversion. Heart Rhythm 2007;4(5):S185‐6. [Google Scholar]; Heidt MC, Vician M, Stracke SKH, Stadlbauer T, Grebe MT, Boening A, et al. Beneficial effects of intravenously administered n‐3 fatty acids for the prevention of atrial fibrillation after coronary artery bypass surgery: a prospective randomized study. Thoracic and Cardiovascular Surgeon 2009;57:276‐80. [DOI: 10.1055/s-0029-1185301] [DOI] [PubMed] [Google Scholar]; Mariani J, Doval HC, Nul D, Varini S, Grancelli H, Ferrante D, et al. N‐3 polyunsaturated fatty acids to prevent atrial fibrillation: updated systematic review and meta‐analysis of randomized controlled trials. Journal of the American Heart Association 2013;2(1):e005033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leaf A, Albert CM, Josephson M, Steinhaus D, Kluger J, Kang JX, et al. Prevention of fatal arrhythmias in high‐risk subjects by fish oil n‐3 fatty acid intake. Circulation 2005;112(18):2762‐8. [DOI] [PubMed] [Google Scholar]
- Caligiuri SP, Aukema HM, Ravandi A, Guzman R, Dibrov E, Pierce GN. Flaxseed consumption reduces blood pressure in patients with hypertension by altering circulating oxylipins via an alpha‐linolenic acid‐induced inhibition of soluble epoxide hydrolase. Hypertension 2014;64(1):53‐9. [PUBMED: 24777981] [DOI] [PubMed] [Google Scholar]; Caligiuri SP, Rodriguez‐Leyva D, Aukema HM, Ravandi A, Weighell W, Guzman R, et al. Dietary flaxseed reduces central aortic blood pressure without cardiac involvement but through changes in plasma oxylipins. Hypertension 2016;68(4):1031‐8. [PUBMED: 27528063] [DOI] [PubMed] [Google Scholar]; Edel A, Rodriguez‐Leyva D, Weighell W, Vallee R, Aliani M, Guzman R, et al. Flaxseed lignan metabolites elicit antihypertensive effects in pad patients in the flax‐pad trial. Annals of Nutrition and Metabolism 2013;63:1339. [Google Scholar]; Edel AL, Rodriguez‐Leyva D, Maddaford TG, Caligiuri SP, Austria JA, Weighell W, et al. Dietary flaxseed independently lowers circulating cholesterol and lowers it beyond the effects of cholesterol‐lowering medications alone in patients with peripheral artery disease. Journal of Nutrition 2015;145(4):749‐57. [PUBMED: 25694068] [DOI] [PubMed] [Google Scholar]; Leyva DR, Zahradka P, Ramjiawan B, Guzman R, Aliani M, Pierce GN. The effect of dietary flaxseed on improving symptoms of cardiovascular disease in patients with peripheral artery disease: rationale and design of the FLAX‐PAD randomized controlled trial. Contemporary Clinical Trials 2011;32(5):724‐30. [PUBMED: 21616170] [DOI] [PubMed] [Google Scholar]; Pierce GN, Edel AL, LaVallee R, Caligiuri S, Aukema H, Ravandi A, et al. The use of dietary flaxseed to promote cardiovascular health. Acta Physiologica 2014;211:15. [Google Scholar]; Pierce GN, Rodriguez‐Leyva D, Edel A, Guzman R, Aliani M. The clinical use of flaxseed as a powerful nutritional intervention to treat cardiovascular disease. Cardiology (Switzerland) 2013;126:201. [Google Scholar]; Rodriguez‐Leyva D, Weighell W, Edel AL, LaVallee R, Dibrov E, Pinneker R, et al. Potent antihypertensive action of dietary flaxseed in hypertensive patients. Hypertension 2013;62(6):1081‐9. [PUBMED: 24126178] [DOI] [PubMed] [Google Scholar]
- Macchia A, Grancelli H, Varini S, Nul D, Ferrante D, Mariani J, et al. Late‐breaking clinical trials: treatments for prevention of cardiovascular events: a population perspective. Circulation. 2012; Vol. 126:2780‐1. [Google Scholar]; Macchia A, Grancelli H, Varini S, Nul D, Laffaye N, Mariani J, et al. Omega‐3 fatty acids for the prevention of recurrent symptomatic atrial fibrillation: results of the FORWARD (randomized trial to assess efficacy of PUFA for the maintenance of sinus rhythm in persistent atrial fibrillation) trial. Journal of the American College of Cardiology 2013;61(4):463‐8. [PUBMED: 23265344] [DOI] [PubMed] [Google Scholar]; Macchia A, Varini S, Grancelli H, Nul D, Laffaye N, Ferrante D, et al. The rationale and design of the FORomegaARD trial: a randomized, double‐blind, placebo‐controlled, independent study to test the efficacy of n‐3 PUFA for the maintenance of normal sinus rhythm in patients with previous atrial fibrillation. American Heart Journal 2009;157(3):423‐7. [PUBMED: 19249410] [DOI] [PubMed] [Google Scholar]
- Chen JS, Hill CL, Lester S, Ruediger CD, Battersby R, Jones G, et al. Supplementation with omega‐3 fish oil has no effect on bone mineral density in adults with knee osteoarthritis: a 2‐year randomized controlled trial. Osteoporosis International 2016;27(5):1897‐905. [PUBMED: 26694596] [DOI] [PubMed] [Google Scholar]; Hill C, Lester SE, Jones G. Response to 'Low‐dose versus high‐dose fish oil for pain reduction and function improvement in patients with knee osteoarthritis' by Chen et al. Annals of the Rheumatic Diseases2016; Vol. 75, issue 1:e8. [PUBMED: 26662278] [DOI] [PubMed]; Hill CL, March LM, Aitken D, Lester SE, Battersby R, Hynes K, et al. Fish oil in knee osteoarthritis: a randomised clinical trial of low dose versus high dose. Annals of the Rheumatic Diseases 2016;75(1):23‐9. [PUBMED: 26353789] [DOI] [PubMed] [Google Scholar]
- Franzen D. A prospective, randomized, and double‐blind trial on the effect of fish oil on the incidence of restenosis following ptca. Catheterization and Cardiovascular Diagnosis 1993;28(4):301‐10. [DOI] [PubMed] [Google Scholar]; Franzen D, Geisel J, Hopp HW, Oette K, Hilger HH. Long‐term effects of low dosage fish oil on serum lipids and lipoproteins [Langzeiteffekte von niedrigdosiertem Fischol auf Serumlipide und Lipoproteine]. Medizinische Klinik 1993;88(3):134‐8. [PubMed] [Google Scholar]
- Gill EA, Chen MA, Paramsothy P, Fish B, Isquith D, Thirumalai A, et al. Omega‐3 fatty acids effects on carotid IMT in metabolic syndrome. Circulation 2014;130:A1269. Abstract no. 12697. [Google Scholar]; Gill EA, Chen MA, Thirumalai A, Fish B, Paramsothy P. Omega‐3 fatty acids improve dyslipidemia but not inflammatory markers in metabolic syndrome. Journal of Clinical Lipidology 2012;6:278‐9. [Google Scholar]
- Aleksova A, Masson S, Maggioni AP, Lucci D, Fabbri G, Beretta L, et al. N‐3 polyunsaturated fatty acids and atrial fibrillation in patients with chronic heart failure: the GISSI‐HF trial. European Journal of Heart Failure 2013;15(11):1289‐95. [DOI] [PubMed] [Google Scholar]; Canepa M, Temporelli PL, Rossi A, Gonzini L, Nicolosi GL, Staszewsky L, et al. Prevalence and prognostic impact of chronic obstructive pulmonary disease in patients with chronic heart failure. Data from the GISSI‐Heart Failure trial. European Journal of Heart Failure 2016;18:442‐3. [DOI] [PubMed] [Google Scholar]; Cowie MR, Cure S, Bianic F, McGuire A, Goodall G, Tavazzi L. Cost‐effectiveness of highly purified omega‐3 polyunsaturated fatty acid ethyl esters in the treatment of chronic heart failure: results of Markov modelling in a UK setting. European Journal of Heart Failure 2011;13(6):681‐9. [DOI: 10.1093/eurjhf/hfr023] [DOI] [PubMed] [Google Scholar]; Finzi A, Barlera S, Serra DM, Rossi MG, Ruggeri A, Mezzani A, et al. Antiarrhythmic effects of n‐3 PUFA in patients with heart failure and an implantable cardioverter defibrillator in the GISSI‐HF trial. European Heart Journal 2009;30:279. [Google Scholar]; Finzi AA, Latini R, Barlera S, Rossi MG, Ruggeri A, Mezzani A, et al. Effects of n‐3 polyunsaturated fatty acids on malignant ventricular arrhythmias in patients with chronic heart failure and implantable cardioverter‐defibrillators: A substudy of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Insufficienza Cardiaca (GISSI‐HF) trial. American Heart Journal 2011;161(2):338‐43. [DOI: 10.1016/j.ahj.2010.10.032] [DOI] [PubMed] [Google Scholar]; Ghio S, Scelsi L, Latini R, Masson S, Eleuteri E, Palvarini M, et al. Effects of n‐3 polyunsaturated fatty acids and of rosuvastatin on left ventricular function in chronic heart failure: a substudy of GISSI‐HF trial. European Journal of Heart Failure 2010;12(12):1345‐53. [DOI] [PubMed] [Google Scholar]; Gissi‐HF Investigators, Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, et al. Effect of n‐3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI‐HF trial): a randomised, double‐blind, placebo‐controlled trial. Lancet 2008;372(9645):1223‐30. [DOI: 10.1016/S01406736(08)61239-8] [DOI] [PubMed] [Google Scholar]; Rovere MT, Barlera S, Staszewsky L, Mezzani A, Midi P, Marchioli R, et al. Effect of n‐3PUFA on heart rate variability. Data from the GISSI‐HF holter substudy. Circulation 2011;124(21 Suppl 1):A14829. [Google Scholar]; Rovere MT, Pinna GD, Maestri R, Barlera S, Bernardinangeli M, Veniani M, et al. Autonomic markers and cardiovascular and arrhythmic events in heart failure patients: still a place in prognostication? Data from the GISSI‐HF trial. European Journal of Heart Failure 2012;14(12):1410‐9. [DOI] [PubMed] [Google Scholar]; Rovere MT, Staszewsky L, Barlera S, Maestri R, Mezzani A, Midi P, et al. n‐3PUFA and Holter‐derived autonomic variables in patients with heart failure: data from the Gruppo Italiano per lo Studio della Sopravvivenza nell'Insufficienza Cardiaca (GISSI‐HF) Holter substudy. Heart Rhythm 2013;10(2):226‐32. [DOI] [PubMed] [Google Scholar]; Latini R, Masson S, Tacconi M, Bernasconi R, Dragani L, Milani V, et al. Circulating levels of n‐3 polyunsaturated fatty acids in patients with chronic heart failure. Data from the GISSI‐HF trial. European Heart Journal 2011;32:919. [Google Scholar]; Maggioni AP, Fabbri G, Lucci D, Marchioli R, Franzosi MG, Latini R, et al. Effects of rosuvastatin on atrial fibrillation occurrence: ancillary results of the GISSI‐HF trial. Eupropean Heart Journal 2009;30(19):232736. [DOI] [PubMed] [Google Scholar]; Marchioli R, Aldegheri MP, Borghese L, Franzosi MG, Latini R, Marfisi RM, et al. Time course analysis of the effect of n‐3 PUFA on fatal and non fatal arrhythmias in heart failure: secondary results of the GISSI‐HF trial. European Heart Journal 2009;30:165. [Google Scholar]; Marchioli R, Cucchi G, Gualco A, Franzosi MG, Levantesi G, Maggioni AP, et al. Time course analysis of the effect of n‐3 PUFA on fatal and non fatal heart failure: secondary results of the GISSI‐HF trial. European Heart Journal 2009;30:432. [Google Scholar]; Marchioli R, Franzosi MG, Latini R, Maggioni AP, Marfisi RM, Minneci C, et al. Prognostic ability of a Mediterranean dietary score in heart failure: preliminary analysis of the GISSI‐Heart failure Trial. European Heart Journal 2009;30:1026. [Google Scholar]; Marchioli R, Franzosi MG, Latini R, Maggioni AP, Marfisi RM, Nicolosi GL, et al. Effect of n‐3 PUFA in heart failure patients with different dietary habits: preliminary results of the GISSI‐heart failure trial. European Heart Journal 2009;30:426. 19174428 [Google Scholar]; Marchioli R, Franzosi MG, Levantesi G, Marfisi RM, Maggioni AP, Nicolosi GL, et al. Effect of n‐3 PUFA according to fish intake: preliminary results of GISSI‐Heart Failure. European Heart Journal 2009;30:707. [Google Scholar]; Marchioli R, Levantesi G, Silletta MG, Barlera S, Bernardinangeli M, Carbonieri E, et al. Effect of n‐3 polyunsaturated fatty acids and rosuvastatin in patients with heart failure: results of the GISSI‐HF trial. Expert Reviews Cardiovascular Therapys 2009;7(7):735‐48. [DOI] [PubMed] [Google Scholar]; Masson S, Latini R, Milani V, Moretti L, Rossi MG, Carbonieri E, et al. Prevalence and prognostic value of elevated urinary albumin excretion in patients with chronic heart failure: data from the GISSI‐Heart Failure trial. Circulation: Heart Failure 2010;3(1):65‐72. [DOI] [PubMed] [Google Scholar]; Masson S, Marchioli R, Mozaffarian D, Bernasconi R, Milani V, Dragani L, et al. Plasma n‐3 polyunsaturated fatty acids in chronic heart failure in the GISSI‐Heart Failure Trial: relation with fish intake, circulating biomarkers, and mortality. American Heart Journal 2013;165(2):208‐15. [DOI] [PubMed] [Google Scholar]; Røysland R, Masson S, Omland T, Milani V, Bjerre M, Flyvbjerg A, et al. Prognostic value of osteoprotegerin in chronic heart failure: the GISSI‐HF trial. American Heart Journal 2010;160(2):286‐93. [DOI: 10.1016/j.ahj.2010.05.015] [DOI] [PubMed] [Google Scholar]; Tavazzi L, Tognoni G, Franzosi MG, Latini R, Maggioni AP, Marchioli R, et al. Rationale and design of the GISSI heart failure trial: a large trial to assess the effects of n‐3 polyunsaturated fatty acids and rosuvastatin in symptomatic congestive heart failure. European Journal of Heart Failure 2004;6(5):635‐41. [DOI: 10.1016/j.ejheart.2004.03.001] [DOI] [PubMed] [Google Scholar]
- Franzosi MG, Brunetti M, Marchioli R, Marfisi RM, Tognoni G, Valagussa F, GISSI‐Prevenzione I. Cost‐effectiveness analysis of n‐3 polyunsaturated fatty acids (PUFA) after myocardial infarction: results from Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto (GISSI)‐Prevenzione Trial. Pharmacoeconomics 2001;19(4):411‐20. [DOI] [PubMed] [Google Scholar]; GISSI‐Prevenzione Investigators. Dietary supplementation with n‐3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI‐Prevenzione trial. Lancet 1999;354:447‐55. [PubMed] [Google Scholar]; Marchioli R. Treatment with n‐3 polyunsaturated fatty acids after myocardial infarction: results of GISSI‐Prevenzione Trial. European Heart Journal Supplements 2001;3(Suppl D):D85‐D97. [DOI] [PubMed] [Google Scholar]; Marchioli R, Barzi F, Bomba E, Chieffo C, Gregorio DDMR, Franzosi MG, et al. Early protection against sudden death by n‐3 polyunsaturated fatty acids after myocardial infarction: time course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)‐Prevenzione. Circulation 2002;105:1897‐903. [DOI] [PubMed] [Google Scholar]; Marchioli R, Pasquale A. The biochemical, pharmacological and epidemiological reference picture of the GISSI‐Prevention. The Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico. Giornale Italiano di Cardiologia 1993;23(9):933‐64. [PubMed] [Google Scholar]; Marchioli R, Valagussa F. The results of the GISSI‐Prevenzione trial in the general framework of secondary prevention. European Heart Journal 2000;21(12):949‐52. [DOI] [PubMed] [Google Scholar]
- Pasternak RC, Brown LE, Stone PH, Silverman DI, Gibson CM, Sacks FM. Effect of combination therapy with lipid‐reducing drugs in patients with coronary heart disease and "normal" cholesterol levels. A randomized, placebo‐controlled trial. Annals of Internal Medicine 1996;125(7):529‐40. [PUBMED: 8815751] [DOI] [PubMed] [Google Scholar]; Sacks FM, Pasternak RC, Gibson CM, Rosner B, Stone PH. Effect on coronary atherosclerosis of decrease in plasma cholesterol concentrations in normocholesterolaemic patients. Lancet 1994;344(8931):1182‐6. [PUBMED: 7934538] [DOI] [PubMed] [Google Scholar]; Sacks FM, Stone PH, Gibson CM, Silverman DI, Rosner B, Pasternak RC. Controlled trial of fish oil for regression of human coronary atherosclerosis. Journal of the American College of Cardiology 1995;25(7):1492‐8. [DOI] [PubMed] [Google Scholar]
- Tan SY. Dietary Manipulation and Weight Management [PhD thesis]. Wollongong, Australia: University of Wollonong, 2010. [Google Scholar]; Tapsell LC, Batterham MJ, Teuss G, Tan SY, Dalton S, Quick CJ, et al. Long‐term effects of increased dietary polyunsaturated fat from walnuts on metabolic parameters in type II diabetes. European Journal of Clinical Nutrition 2009;63(8):1008‐15. [PUBMED: 19352378] [DOI] [PubMed] [Google Scholar]
- Cleland JG, Freemantle N, Coletta AP, Clark AL. Clinical trials update from the American Heart Association: REPAIR‐AMI, ASTAMI, JELIS, MEGA, REVIVE‐II, SURVIVE, and PROACTIVE. European Journal of Heart Failure 2006;8(1):105‐10. [DOI: 10.1016/j.ejheart.2005.12.003] [DOI] [PubMed] [Google Scholar]; Ishikawa Y, Yokoyama M, Saito Y, Matsuzaki M, Origasa H, Oikawa S, et al. Preventive effects of eicosapentaenoic acid on coronary artery disease in patients with peripheral artery disease. Circulation Journal 2010;74(7):1451‐7. [DOI: 10.1253/circj.CJ-09-0520] [DOI] [PubMed] [Google Scholar]; Itakura H, Yokoyama M, Matsuzaki M, Saito Y, Origasa H, Ishikawa Y, et al. Relationships between plasma fatty acid composition and coronary artery disease. Journal of Atherosclerosis and Thrombosis 2011;18(2):99‐107. [PUBMED: 21099130] [DOI] [PubMed] [Google Scholar]; Itakura H, Yokoyama M, Matsuzaki M, Saito Y, Origasa H, Ishikawa Y, et al. The change in low‐density lipoprotein cholesterol concentration is positively related to plasma docosahexaenoic acid but not eicosapentaenoic acid. Journal of Atherosclerosis and Thrombosis 2012;19(7):673‐9. [PUBMED: 22653220] [DOI] [PubMed] [Google Scholar]; Matsuzaki M, Yokoyama M, Saito Y, Origasa H, Ishikawa Y, Oikawa S, et al. Incremental effects of eicosapentaenoic acid on cardiovascular events in statin‐treated patients with coronary artery disease. Secondary prevention analysis from JELIS. Circulation Journal 2009;73(7):1283‐90. [DOI] [PubMed] [Google Scholar]; Oikawa S, Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, et al. Suppressive effect of EPA on the incidence of coronary events in hypercholesterolemia with impaired glucose metabolism: sub‐analysis of the Japan EPA Lipid Intervention Study (JELIS). Atherosclerosis 2009;206(2):535‐9. [DOI: 10.1016/j.atherosclerosis.2009.03.029] [DOI] [PubMed] [Google Scholar]; Origasa H, Yokoyama M, Matsuzaki M, Saito Y, Matsuzawa Y, JELIS Investigators. Clinical importance of adherence to treatment with eicosapentaenoic acid by patients with hypercholesterolemia. Circulation Journal 2010;74(3):510‐7. [DOI: 10.1253/circj.CJ-09-0746] [DOI] [PubMed] [Google Scholar]; Saito Y, Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Ishikawa Y, et al. Effects of EPA on coronary artery disease in hypercholesterolemic patients with multiple risk factors: sub‐analysis of primary prevention cases from the Japan EPA Lipid Intervention Study (JELIS). Atherosclerosis 2008;200(1):135‐40. [DOI: 10.1016/j.atherosclerosis.2008.06.003] [DOI] [PubMed] [Google Scholar]; Tanaka K, Ishikawa Y, Yokoyama M, Origasa H, Matsuzaki M, Saito Y, et al. Reduction in the recurrence of stroke by eicosapentaenoic acid for hypercholesterolemic patients: subanalysis of the JELIS trial. Stroke 2008;39(8):2052‐8. [DOI: 10.1161/STROKEAHA.107.509455] [DOI] [PubMed] [Google Scholar]; Yamanouchi D, Komori K. Eicosapentaenoic acid as the gold standard for patients with peripheral artery disease? Subanalysis of the JELIS trial. Circulation Journal 2010;74(7):1298‐9. [DOI: 10.1253/circj.CJ-10-0449] [DOI] [PubMed] [Google Scholar]; Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open‐label, blinded endpoint analysis. Lancet 2007;369(9567):1090‐8. [DOI] [PubMed] [Google Scholar]; Yokoyama M, Origasa H, for the JELIS Investigators. Effects of eicosapentaenoic acid on cardiovascular events in Japanese patients with hypercholesterolaemia: rationale, design, and baseline characteristics of the Japan EPA Lipid Intervention Study (JELIS). American Heart Journal 2003;146:613‐20. [DOI] [PubMed] [Google Scholar]
- Kumar S, Sutherland F, Morton JB, Lee G, Morgan J, Wong J, et al. Long‐term omega‐3 polyunsaturated fatty acid supplementation reduces the recurrence of persistent atrial fibrillation after electrical cardioversion. Heart Rhythm 2012;9(4):483‐91. [DOI: 10.1016/j.hrthm.2011.11.034] [DOI] [PubMed] [Google Scholar]
- Kumar S, Sutherland F, Stevenson I, Lee JM, Garg ML, Sparks PB. Effects of long‐term omega‐3 polyunsaturated fatty acid supplementation on paroxysmal atrial tachyarrhythmia burden in patients with implanted pacemakers: results from a prospective randomised study. International Journal of Cardiology 2013;168(4):3812‐7. [PUBMED: 23890856] [DOI] [PubMed] [Google Scholar]
- Lorenz‐Meyer H, Bauer P, Nicolay C, Schulz B, Purrmann J, Fleig WE, et al. Omega‐3 fatty acids and low carbohydrate diet for maintenance of remission in Crohn's disease. A randomized controlled multicenter trial. Scandinavian Journal of Gastroenterology 1996;31(8):778‐85. [DOI] [PubMed] [Google Scholar]
- Andrieu S, Guyonnet S, Coley N, Cantet C, Bonnefoy M, Bordes S, et al. Effect of long‐term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): a randomised, placebo‐controlled trial. Lancet Neurology 2017;16:377‐89. [DOI: 10.1016/S1474-4422(17)30040-6] [DOI] [PubMed] [Google Scholar]; Carrie I, Kan GA, Gillette‐Guyonnet S, Andrieu S, Dartigues JF, Touchon J, et al. Recruitment strategies for preventive trials. The MAPT study (MultiDomain Alzheimer Preventive Trial). Journal of Nutrition, Health & Aging 2012;16(4):355‐9. [DOI] [PubMed] [Google Scholar]; Delrieu J, Andrieu S, Pahor M, Cantet C, Cesari M, Ousset PJ, et al. Neuropsychological profile of "cognitive frailty" subjects in MAPT study. Journal of Prevention of Alzheimer's Disease 2016;3(3):151‐9. [DOI: 10.14283/jpad.2016.94] [DOI] [PMC free article] [PubMed] [Google Scholar]; Delrieu J, Payoux P, Hitzel A, Peiffer S, Abellan Van Kan G, Gillette S, et al. Multidomain alzheimer's disease preventive trial: florbetapir ancillary study. Alzheimer's and Dementia 2011;1:S419. [Google Scholar]; Fougere B, Barreto PD, Goisser S, Soriano G, Guyonnet S, Andrieu S, et al. Red blood cell membrane omega‐3 fatty acid levels and physical performance: cross‐sectional data from the MAPT study. Clinical Nutrition 2017 Apr 12 [Epub ahead of print]:1‐4. [DOI: 10.1016/j.clnu.2017.04.005] [DOI] [PubMed]; Gillette S. The multidomain Alzheimer preventive trial (MAPT): a new approach for the prevention of Alzheimer's disease. Alzheimer's & Dementia 2009;S4‐02‐05:145. [Google Scholar]; Gillette‐Guyonnet S, Andrieu S, Dantoine T, Dartigues JF, Touchon J, Vellas B, et al. Commentary on "A roadmap for the prevention of dementia II. Leon Thal Symposium 2008." The Multidomain Alzheimer Preventive Trial (MAPT): a new approach to the prevention of Alzheimer's disease. Alzheimer's & Dementia 2009;5(2):114‐21. [DOI] [PubMed] [Google Scholar]; Gillette‐Guyonnet S, Vellas B, Sandrine A, Charlotte D, Isabelle C. MAPT study: a 3‐year randomized trial of omega 3 and/or multidomain intervention for the prevention of cognitive decline in frail elderly subjects‐rationale, design and baseline data. Alzheimer's & Dementia 2011;1:S97‐8. [Google Scholar]; Vellas B, Carrie I, Gillette‐Guyonnet S, Touchon J, Dantoine T, Dartigues JF, et al. MAPT Study: a multidomain approach for preventing ALzheimer's disease: design and baseline data. Journal of Prevention of Alzheimers Disease 2014;1(1):13‐22. [PMC free article] [PubMed] [Google Scholar]; Vellas B, Carrie I, Guyonnet S, Touchon J, Dantoine T, Dartigues JF, et al. MAPT (multi‐domain Alzheimer's prevention trial): Results at 36 months. Alzheimer's & Dementia 2015;1:331. [Google Scholar]; Vellas B, Touchon J, Weiner M. MAPT (multidomain Alzheimer preventive trial) imaging (MRI, FDG‐PET, amyloid‐PET) data. Journal of Nutrition, Health and Aging 2012;16(9):812‐5. [DOI] [PubMed] [Google Scholar]
- Bemelmans WJ, Broer J, Feskens EJ, Smit AJ, Muskiet AJ, Lefrandt JD, et al. Effect of an increased intake of alpha‐linolenic acid and group nutritional education on cardiovascular risk factors: the Mediterranean alpha‐linolenic enriched Groningen dietary intervention (MARGARIN) study. American Journal of Clinical Nutrition 2002;75:221‐7. [DOI] [PubMed] [Google Scholar]; Bemelmans WJ, Broer J, Vries JH, Hulshof KF, May JF, Meyboom‐De Jong B. Impact of Mediterranean diet education versus posted leaflet on dietary habits and serum cholesterol in a high risk population for cardiovascular disease. Public Health Nutrition 2000;3(3):273‐83. [DOI] [PubMed] [Google Scholar]; Bemelmans WJ, Lefrandt JD, Feskens EJ, Broer J, Tervaert JW, May JF, et al. Change in saturated fat intake is associated with progression of carotid and femoral intima‐media thickness, and with levels of soluble intercellular adhesion molecule‐1. Atherosclerosis 2002;163(1):113‐20. [DOI] [PubMed] [Google Scholar]; Bemelmans WJ, Lefrandt JD, Feskens EJ, Haelst PL, Broer J, Meyboom‐de Jong B, et al. Increased alpha‐linolenic acid intake lowers C‐reactive protein, but has no effect on markers of atherosclerosis. European Journal of Clinical Nutrition 2004;58(7):1083‐9. [DOI] [PubMed] [Google Scholar]; Bemelmans WJ, Muskiet FA, Feskens EJ, Vries JH, Broer J, May JF, et al. Associations of alpha‐linolenic acid and linoleic acid with risk factors for coronary heart disease. European Journal of Clinical Nutrition 2000;54(12):865‐71. [DOI] [PubMed] [Google Scholar]; Siero FW, Broer J, Bemelmans WJ, Meyboom‐de Jong BM. Impact of group nutrition education and surplus value of Prochaska based stage‐matched information on health‐related cognitions and on Mediterranean nutrition behaviour. Health Education Research 2000;15(5):635‐47. [DOI] [PubMed] [Google Scholar]
- Al‐Hilal M, Alsaleh A, Maniou Z, Lewis FJ, Hall WL, Sanders TA, et al. Genetic variation at the FADS1‐FADS2 gene locus influences delta‐5 desaturase activity and LC‐PUFA proportions after fish oil supplement. Journal of Lipid Research 2013;54(2):542‐51. [PUBMED: 23160180] [DOI] [PMC free article] [PubMed] [Google Scholar]; AlSaleh A, Maniou Z, Lewis FJ, Hall WL, Sanders TA, O'Dell SD. Interaction between a CSK gene variant and fish oil intake influences blood pressure in healthy adults. Journal of Nutrition 2014;144(3):267‐72. [PUBMED: 24401815] [DOI] [PubMed] [Google Scholar]; Alsaleh A, Crepostnaia D, Maniou Z, Lewis FJ, Hall WL, Sanders TA, et al. Adiponectin gene variant interacts with fish oil supplementation to influence serum adiponectin in older individuals. Journal of Nutrition 2013;143(7):1021‐7. [PUBMED: 23658423] [DOI] [PubMed] [Google Scholar]; Hall WL, Hay G, Maniou Z, Seed PT, Chowienczyk PJ, Sanders TA. Effect of low doses of long chain n‐3 polyunsaturated fatty acids on sleep‐time heart rate variability: a randomized, controlled trial. International Journal of Cardiology 2013;168:4439‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]; Pinto AM, Hall WL, Sanders TAB. Effect of low doses of long chain n‐3 PUFA intake on daytime heart rate variability: results from the MARINA study. European Journal of Preventive Cardiology 2015;1:S146. [Google Scholar]; Sanders TA, Hall WL, Maniou Z, Lewis F, Seed PT, Chowienczyk PJ. Effect of low doses of long‐chain n‐3 PUFAs on endothelial function and arterial stiffness: a randomized controlled trial. American Journal of Clinical Nutrition 2011;94(4):973‐80. [PUBMED: 21865334] [DOI] [PubMed] [Google Scholar]; Sanders TAB, Chowienczyk PJ, Hall W, Lewis F, Seed P, Maniou Z, et al. The influences of increasing intakes of EPA and DHA on vascular function and risk factors for cardiovascular disease. Food Standards Agency Project N02041. Final Report2011.
- Le T, Flatt SW, Natarajan L, Pakiz B, Quintana EL, Heath DD, et al. Effects of diet composition and insulin resistance status on plasma lipid levels in a weight loss intervention in women. Journal of the American Heart Association 2016;5(1):e002771. [DOI: 10.1161/JAHA.115.002771] [DOI] [PMC free article] [PubMed] [Google Scholar]; Rock CL, Flatt SW, Pakiz B, Quintana EL, Heath DD, Rana BK, et al. Effects of diet composition on weight loss, metabolic factors and biomarkers in a 1‐year weight loss intervention in obese women examined by baseline insulin resistance status. Metabolism 2016;65(11):1605‐13. [DOI: 10.1016/j.metabol.2016.07.008] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mita T, Watada H, Ogihara T, Nomiyama T, Ogawa O, Kinoshita J, et al. Eicosapentaenoic acid reduces the progression of carotid intima‐media thickness in patients with type 2 diabetes. Atherosclerosis 2007;191(1):162‐7. [DOI] [PubMed] [Google Scholar]
- Merle BM, Benlian P, Puche N, Bassols A, Delcourt C, Souied EH. Circulating omega‐3 fatty acids and neovascular age‐related macular degeneration. Investigative Ophthalmology & Visual Science 2014;55(3):2010‐9. [PUBMED: 24557349] [DOI] [PubMed] [Google Scholar]; Merle BM, Richard F, Benlian P, Puche N, Delcourt C, Souied EH. CFH Y402H and ARMS2 A69S polymorphisms and oral supplementation with docosahexaenoic acid in neovascular age‐related macular degeneration patients: the NAT2 study. PLOS ONE 2015;10(7):e0130816. [PUBMED: 26132079] [DOI] [PMC free article] [PubMed] [Google Scholar]; Querques G, Merle BM, Pumariega NM, Benlian P, Delcourt C, Zourdani A, et al. Dynamic drusen remodelling in participants of the nutritional AMD treatment‐2 (NAT‐2) randomized trial. PLOS ONE 2016;11(2):e0149219. [PUBMED: 26901353] [DOI] [PMC free article] [PubMed] [Google Scholar]; Souied EH, Delcourt C, Querques G, Bassols A, Merle B, Zourdani A, et al. Oral docosahexaenoic acid in the prevention of exudative age‐related macular degeneration: the nutritional AMD treatment 2 study. Ophthalmology 2013;120(8):1619‐31. [PUBMED: 23395546] [DOI] [PubMed] [Google Scholar]
- Nodari S, Triggiani M, Campia U, Manerba A, Milesi G, Cesana BM, et al. N‐3 polyunsaturated fatty acids in the prevention of atrial fibrillation recurrences after electrical cardioversion: a prospective, randomized study. Circulation 2011;124(10):1100‐6. [PUBMED: 21844082] [DOI] [PubMed] [Google Scholar]
- NCT01223703. PUFAs and left ventricular function in heart failure (CS‐PUFA‐02) [Effects of n‐3 Polyunsaturated Fatty Acids (PUFAs) on Left Ventricular Function and Functional Capacity in Patients With Dilated Cardiomyopathy]. https://clinicaltrials.gov/ct2/show/NCT01223703 (first received 19 October 2010). ; Nodari S, Triggiani M, Berlinghieri N, Milesi G, Foresti A, Gheorghiade M, et al. Effects of n‐3 polyunsaturated fatty acids on left ventricular function and functional capacity in heart failure patients. European Heart Journal 2010;31:850. [Google Scholar]; Nodari S, Triggiani M, Campia U, Manerba A, Milesi G, Cesana BM, et al. Effects of n‐3 polyunsaturated fatty acids on left ventricular function and functional capacity in patients with dilated cardiomyopathy. Journal of the American College of Cardiology 2011;57(7):870‐9. [DOI] [PubMed] [Google Scholar]; Nodari S, Triggiani M, Campia U, Zhao L, Manerba A, Milesi G, et al. Plasma levels of n‐3 polyunsaturated fatty acids and risk of hospitalization in patients with non‐ischemic cardiomyopathy. Circulation. Conference: American Heart Association 2012;126(21 Suppl 1):A17431. [Google Scholar]
- Norouzi Javidan A, Sabour H, Latifi S, Abrishamkar M, Soltani Z, Shidfar F, et al. Does consumption of polyunsaturated fatty acids influence on neurorehabilitation in traumatic spinal cord‐injured individuals? A double‐blinded clinical trial. Spinal Cord 2014;52(5):378‐82. [PUBMED: 24637568] [DOI] [PubMed] [Google Scholar]; Sabour H, Norouzi Javidan A, Latifi S, Shidfar F, Heshmat R, Emami Razavi SH, et al. Omega‐3 fatty acids' effect on leptin and adiponectin concentrations in patients with spinal cord injury: a double‐blinded randomized clinical trial. Journal of Spinal Cord Medicine 2015;38(5):599‐606. [PUBMED: 25096818] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natvig H. The effect of unsaturated fatty acids on the incidence of coronary infarction, etc [Effekten av umettede fettsyrer hyppigheten av hjerteinfarkt M.M.]. Tidsskrift for Den Norske Laegeforening 1967;87(11):1033‐41. [PubMed] [Google Scholar]; Natvig H, Borchgrevink CF, Dedichen J, Owren PA, Schiotz EH, Westlund K. A controlled trial of the effect of linolenic acid on incidence of coronary heart disease. The Norwegian vegetable oil experiment of 1965‐66. Scandinavian Journal of Clinical & Laboratory Investigation 1968;105(Suppl):1‐20. [PubMed] [Google Scholar]
- Garbagnati F, Cairella G, Martino A, Multari M, Scognamiglio U, Venturiero V, et al. Is antioxidant and n‐3 supplementation able to improve functional status in post‐stroke patients? Results from the Nutristroke Trial. Cerebrovascular Diseases 2009;27(4):375‐83. [DOI: 10.1159/000207441] [DOI] [PubMed] [Google Scholar]
- Ilsey CDJ, Nye ER, Sutherland W, Ram J, Ablett MB. Randomised placebo controlled trial of MAXEPA and aspirin/persantin after successful coronary angioplasty. Australian & New Zealand Journal of Medicine 1987;17:559. [Google Scholar]; Nye ER, Ablett MB, Robertson MC, Ilsley CD, Sutherland WH. Effect of eicosapentaenoic acid on restenosis rate, clinical course and blood lipids in patients after percutaneous transluminal coronary angioplasty. Australian and New Zealand Journal of Medicine 1990;20(4):549‐52. [DOI] [PubMed] [Google Scholar]
- Aarsetoy H, Brugger‐Andersen T, Hetland O, Grundt H, Nilsen DW. Long term influence of regular intake of high dose n‐3 fatty acids on CD40‐ligand, pregnancy‐associated plasma protein A and matrix metalloproteinase‐9 following acute myocardial infarction. Thrombosis & Haemostasis 2006;95(2):329‐36. [DOI] [PubMed] [Google Scholar]; Grundt H, Hetland O, Nilsen DW. Changes in tissue factor and activated factor XII following an acute myocardial infarction were uninfluenced by high doses of n‐3 polyunsaturated fatty acids. Thrombosis & Haemostasis 2003;89(4):752‐9. [PubMed] [Google Scholar]; Grundt H, Nilsen DW, Hetland O, Mansoor MA. Clinical outcome and atherothrombogenic risk profile after prolonged wash‐out following long‐term treatment with high doses of n‐3 PUFAs in patients with an acute myocardial infarction. Clinical Nutrition 2004;23(4):491‐500. [DOI] [PubMed] [Google Scholar]; Grundt H, Nilsen DW, Mansoor MA, Hetland O, Nordoy A. Reduction in homocysteine by n‐3 polyunsaturated fatty acids after 1 year in a randomised double‐blind study following an acute myocardial infarction: no effect on endothelial adhesion properties. Pathophysiology of Haemostasis & Thrombosis 2003;33(2):88‐95. [DOI] [PubMed] [Google Scholar]; Grundt H, Nilsen DW, Mansoor MA, Nordoy A. Increased lipid peroxidation during long‐term intervention with high doses of n‐3 fatty acids (PUFAs) following an acute myocardial infarction. European Journal of Clinical Nutrition 2003;57(6):793‐800. [DOI] [PubMed] [Google Scholar]; Naesgaard PA, Grundt H, Brede C, Nilsen DW. The effect on vitamin D levels of long‐term high‐dose treatment with a concentrated omega‐3 compound (Omacor/Lovaza) in patients hospitalized with a myocardial infarction. Circulation 2014;130(Suppl 2):A17245. [Google Scholar]; Nilsen DW, Albrektsen G, Landmark K, Moen S, Aarsland T, Woie L. Effects of a high‐dose concentrate of n‐3 fatty acids or corn oil introduced early after an acute myocardial infarction on serum triacylglycerol and HDL cholesterol. American Journal of Clinical Nutrition 2001;74(1):50‐6. [DOI] [PubMed] [Google Scholar]; Poenitz V, Grundt H, Bottazzi B, Cuccovillo I, Mantovani A, Nilsen DW. Pentraxin 3 is uninfluenced by high doses of concentrated omega‐3 fatty acids administered for 12 months following an acute myocardial infarction. Circulation. Conference: American Heart Association 2012;126(21 Suppl 1):A13464. [Google Scholar]
- Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, et al. OMEGA, a randomized, placebo‐controlled trial to test the effect of highly purified omega‐3 fatty acids on top of modern guideline‐adjusted therapy after myocardial infarction. Circulation 2010;122(21):2152‐9. [DOI: 10.1161/CIRCULATIONAHA.110.948562] [DOI] [PubMed] [Google Scholar]; Rauch B, Schiele R, Schneider S, Gohlke H, Diller F, Gottwik M, et al. Highly purified omega‐3 fatty acids for secondary prevention of sudden cardiac death after myocardial infarction‐aims and methods of the OMEGA‐study. Cardiovascular Drugs Therapy 2006;20(5):365‐75. [DOI: 10.1007/s10557-006-0495-6] [DOI] [PubMed] [Google Scholar]; Zimmer R, Riemer T, Rauch B, Schneider S, Schiele R, Gohlke H, et al. Effects of 1‐year treatment with highly purified omega‐3 fatty acids on depression after myocardial infarction: results from the OMEGA trial. Journal of Clinical Psychiatry 2013;74(11):e1037‐45. [PUBMED: 24330904] [DOI] [PubMed] [Google Scholar]
- Dangour AD, Allen E, Elbourne D, Fasey N, Fletcher AE, Hardy P, et al. Effect of 2‐y n‐3 long‐chain polyunsaturated fatty acid supplementation on cognitive function in older people: a randomized, double‐blind, controlled trial. American Journal of Clinical Nutrition 2010;91(6):1725‐32. [DOI] [PubMed] [Google Scholar]; Dangour AD, Allen E, Elbourne D, Fletcher A, Richards M, Uauy R. Fish consumption and cognitive function among older people in the UK: baseline data from the OPAL study. Journal of Nutrition, Health & Aging 2009;13(3):198‐202. [DOI] [PubMed] [Google Scholar]; Dangour AD, Allen E, Elbourne D, Fletcher AE, Neveu MM, Uauy R, Holder G. N‐3 fatty acids and retinal function. Ophthalmology 2013;120(3):643. [DOI: 10.1016/j.ophtha.2012.09.043] [DOI] [PubMed] [Google Scholar]; Dangour AD, Clemens F, Elbourne D, Fasey N, Fletcher AE, Hardy P, et al. A randomised controlled trial investigating the effect of n‐3 long‐chain polyunsaturated fatty acid supplementation on cognitive and retinal function in cognitively healthy older people: the Older People And n‐3 Long‐chain polyunsaturated fatty acids (OPAL) study protocol [ISRCTN72331636]. Nutrition Journal 2006;5:20. [DOI] [PMC free article] [PubMed] [Google Scholar]; ISRCTN72331636. The OPAL Study: Older People And n‐3 Long‐chain polyunsaturated fatty acids. http://www.isrctn.com/ISRCTN72331636 (first received 27 April 2004). [ISRCTN72331636]
- Bordeleau L, Yakubovich N, Dagenais G, Rosenstock J, Ryden LE, Spinas G, et al. Cancer outcomes in patients with dysglycemia on basal insulin: results of the Origin trial. Diabetes 2013;62:A72. [Google Scholar]; Bordeleau L, Yakubovich N, Dagenais GR, Rosenstock J, Probstfield J, Chang Yu P, et al. The association of basal insulin glargine and/or n‐3 fatty acids with incident cancers in patients with dysglycemia. Diabetes Care 2014;37(5):1360‐6. [DOI] [PubMed] [Google Scholar]; Lonn EM, Bosch J, Diaz R, Lopez‐Jaramillo P, Ramachandran A, Hancu N, et al. Effect of insulin glargine and n‐3FA on carotid intima‐media thickness in people with dysglycemia at high risk for cardiovascular events: the glucose reduction and atherosclerosis continuing evaluation study (ORIGIN‐GRACE). Diabetes Care 2013;36(9):2466‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]; Maggioni AP, Fabbri G, Bosch J, Dyal L, Ryden LE, Gerstein HC, et al. Effects of n‐3 fatty acids on long‐term outcomes of high risk patients with type 2 diabetes mellitus or IGF/IGT with a recent myocardial infarction. European Heart Journal 2013;34:352. [Google Scholar]; Origin Trial Investigators, Bosch J, Gerstein HC, Dagenais GR, Diaz R, Dyal L, et al. N‐3 fatty acids and cardiovascular outcomes in patients with dysglycemia. New England Journal of Medicine 2012;367(4):309‐18. [DOI] [PubMed] [Google Scholar]; Origin Trial Investigators, Gerstein H, Yusuf S, Riddle MC, Ryden L, Bosch J. Rationale, design, and baseline characteristics for a large international trial of cardiovascular disease prevention in people with dysglycemia: the ORIGIN Trial (Outcome Reduction with an Initial Glargine Intervention). American Heart Journal 2008;155(1):26‐32, 32. [DOI] [PubMed] [Google Scholar]; Origin Trial Investigators, Gerstein HC, Bosch J, Dagenais GR, Diaz R, Jung H, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. New England Journal of Medicine 2012;367(4):319‐28. [DOI] [PubMed] [Google Scholar]; Punthakee Z, Gerstein HC, Bosch J, Tyrwhitt J, Jung H, Lee SF, et al. Cardiovascular and other outcomes postintervention with insulin glargine and omega‐3 fatty acids (ORIGINALE). Diabetes Care 2016;39(5):709‐16. [DOI] [PubMed] [Google Scholar]
- Tatsuno I, Saito Y, Kudou K, Ootake J. Long‐term safety and efficacy of TAK‐085 in Japanese subjects with hypertriglyceridemia undergoing lifestyle modification: the omega‐3 fatty acids randomized long‐term (ORL) study. Journal of Clinical Lipidology 2013;7(6):615‐25. [PUBMED: 24314359] [DOI] [PubMed] [Google Scholar]; Tatsuno IT, Saito YS, Kudou KK, Otake JO, Minamide YM. Effects of long‐term treatment with omega‐3 polyunsaturated fatty acids (Lotriga) on atherogenic lipoproteins in hypertriglyceridemia:results from a phase 3 randomized, open‐label, 1‐year study. European Heart Journal 2013;34:768. [Google Scholar]
- Özaydin M, Erdoğan D, Tayyar S, Uysal BA, Doğan A, Içli A, et al. N‐3 polyunsaturated fatty acids administration does not reduce the recurrence rates of atrial fibrillation and inflammation after electrical cardioversion: a prospective randomized study. Anadolu Kardiyoloji Dergisi 2011;11(4):305‐9. [DOI: 10.5152/akd.2011.080] [DOI] [PubMed] [Google Scholar]
- Proudman S, Spargo L, Hall C, McWilliams L, Lee A, Maureen R, et al. Fish oil in rheumatoid arthritis: a randomised, double blind trial comparing high dose with low dose. Internal Medicine Journal 2012;42(Suppl 1):2‐3. [Google Scholar]; Proudman SM, Cleland LG, Metcalf RG, Sullivan TR, Spargo LD, James MJ. Plasma n‐3 fatty acids and clinical outcomes in recent‐onset rheumatoid arthritis. British Journal of Nutrition 2015;114(6):885‐90. [PUBMED: 26283657] [DOI] [PubMed] [Google Scholar]; Proudman SM, James MJ, Spargo LD, Metcalf RG, Sullivan TR, Rischmueller M, et al. Fish oil in recent onset rheumatoid arthritis: a randomised, double‐blind controlled trial within algorithm‐based drug use. Annals of the Rheumatic Diseases 2015;74(1):89‐95. [PUBMED: 24081439] [DOI] [PubMed] [Google Scholar]
- Puri BK, Leavitt BR, Hayden MR, Ross CA, Rosenblatt A, Greenamyre JT, et al. Ethyl‐EPA in Huntington disease: a double‐blind, randomized, placebo‐controlled trial. Neurology 2005;65(2):286‐92. [DOI] [PubMed] [Google Scholar]
- Raitt MH, Connor WE, Morris C, Kron J, Halperin B, Chugh SS, et al. Fish oil supplementation and risk of ventricular tachycardia and ventricular fibrillation in patients with implantable defibrillators: a randomized controlled trial. JAMA 2005;293(23):2884‐91. [DOI] [PubMed] [Google Scholar]
- Ramirez‐Ramirez V, Macias‐Islas MA, Ortiz GG, Pacheco‐Moises F, Torres‐Sanchez ED, Sorto‐Gomez TE, et al. Efficacy of fish oil on serum of TNF α , IL‐1 β , and IL‐6 oxidative stress markers in multiple sclerosis treated with interferon beta‐1b. Oxidative Medicine and Cellular Longevity 2013;2013:709493. [DOI: 10.1155/2013/709493] [DOI] [PMC free article] [PubMed] [Google Scholar]; Sorto‐Gomez TE, Ortiz GG, Pacheco‐Moises FP, Torres‐Sanchez ED, Ramirez‐Ramirez V, Macias‐Islas MA, et al. Effect of fish oil on glutathione redox system in multiple sclerosis. American Journal of Neurodegenerative Disease 2016;5(2):145‐51. [PMC free article] [PubMed] [Google Scholar]
- Olendzki BC, Leung K, Buskirk S, Reed G, Zurier RB. Treatment of rheumatoid arthritis with marine and botanical oils: influence on serum lipids. Evidence‐Based Complementary & Alternative Medicine: eCAM 2011;2011:827286. [DOI] [PMC free article] [PubMed] [Google Scholar]; Reed GW, Leung K, Rossetti RG, Vanbuskirk S, Sharp JT, Zurier RB. Treatment of rheumatoid arthritis with marine and botanical oils: an 18‐month, randomized, and double‐blind trial. Evidence‐Based Complementary & Alternative Medicine: eCAM 2014;2014:857456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rischio and Prevenzione Investigators. Efficacy of n‐3 polyunsaturated fatty acids and feasibility of optimizing preventive strategies in patients at high cardiovascular risk: rationale, design and baseline characteristics of the Rischio and Prevenzione study, a large randomised trial in general practice. Trials 2010;11(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]; Risk and Prevention Study Collaborative Group, Roncaglioni MC, Tombesi M, Avanzini F, Barlera S, Caimi V, et al. N‐3 fatty acids in patients with multiple cardiovascular risk factors. New England Journal of Medicine 2013;368(19):1800‐8. [DOI] [PubMed] [Google Scholar]; Visentin G, Risk & Prevention Study Grp. Towards evidence‐based practice via practice‐based evidence: the Italian experience. Family Practice 2008;25(Suppl 1):i71‐4. [DOI] [PubMed] [Google Scholar]
- Myrup B, Rossing P, Jensen T, Parving H‐H, Holmer G, Gram J, et al. Lack of effect of fish oil supplementation on coagulation and transcapillary escape rate of albumin in insulin‐dependent diabetic patients with diabetic nephropathy. Scandinavian Journal of Clinical & Laboratory Investigation 2001;61(5):349‐56. [DOI] [PubMed] [Google Scholar]; Rossing P, Hansen BV, Nielsen FS, Myrup B, Holmer G, Parving HH. Fish oil in diabetic nephropathy. Diabetes Care 1996;19(11):1214‐9. [DOI] [PubMed] [Google Scholar]
- Sandhu N, Schetter SE, Liao J, Hartman TJ, Richie JP, McGinley J, et al. Influence of obesity on breast density reduction by omega‐3 fatty acids: evidence from a randomized clinical trial. Cancer Prevention Research 2016;9(4):275‐82. [PUBMED: 26714774] [DOI] [PubMed] [Google Scholar]; Signori C, DuBrock C, Richie JP, Prokopczyk B, Demers LM, Hamilton C, et al. Administration of omega‐3 fatty acids and Raloxifene to women at high risk of breast cancer: interim feasibility and biomarkers analysis from a clinical trial. European Journal of Clinical Nutrition 2012;66(8):878‐84. [PUBMED: 22669332] [DOI] [PubMed] [Google Scholar]
- Angerer P, Kothny W, Stork S, Schacky C. Effect of dietary supplementation with omega‐3 fatty acids on progression of atherosclerosis in carotid arteries. Cardiovascular Research 2002;54(1):183‐90. [DOI] [PubMed] [Google Scholar]; Schacky C, Angerer P, Kothny W, Theisen K, Mudra H. The effect of dietary omega‐3 fatty acids on coronary atherosclerosis. A randomized, double‐blind, placebo‐controlled trial. Annals of Internal Medicine 1999;130(7):554‐62. [DOI] [PubMed] [Google Scholar]; Schacky C, Baumann K, Angerer P. The effect of n‐3 fatty acids on coronary atherosclerosis: results from SCIMO, an angiographic study, background and implications. Lipids 2001;36(Suppl):S99‐102. [DOI] [PubMed] [Google Scholar]
- NCT00090402. Fish oil and alpha lipoic acid in treating Alzheimer's Disease [Fish Oil and Alpha Lipoic Acid in Mild Alzheimer's Disease]. https://clinicaltrials.gov/ct2/show/NCT00090402 (first received 24 August 2004). [CENTRAL: NCT00090402]; Shinto L, Quinn J, Montine T, Dodge HH, Woodward W, Baldauf‐Wagner S, et al. A randomized placebo‐controlled pilot trial of omega‐3 fatty acids and alpha lipoic acid in Alzheimer's disease. Journal of Alzheimer's Disease: JAD 2014;38(1):111‐20. [PUBMED: 24077434] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eritsland J, Arnesen H, Berg K, Seljeflot I, Abdelnoor M. Serum Lp(a) lipoprotein levels in patients with coronary artery disease and the influence of long‐term n‐3 fatty acid supplementation. Scandinavian Journal of Clinical and Laboratory Investigation 1995;55(4):295‐300. [DOI] [PubMed] [Google Scholar]; Eritsland J, Arnesen H, Gronseth K, Fjeld NB, Abdelnoor M. Effect of dietary supplementation with n‐3 fatty acids on coronary artery bypass graft patency. American Journal of Cardiology 1996;77(1):31‐6. [DOI] [PubMed] [Google Scholar]; Eritsland J, Arnesen H, Gronseth K, Fjeld NB, Abdelnoor M. Effect of supplementation with n‐3 fatty acids on graft patency in patients undergoing coronary artery bypass operation. Results from SHOT study. European Heart Journal 1994;15:29. [Google Scholar]; Eritsland J, Arnesen H, Seljeflot I, Hostmark AT. Long‐term metabolic effects of n‐3 polyunsaturated fatty acids in patients with coronary artery disease. American Journal of Clinical Nutrition 1995;61(4):831‐6. [DOI] [PubMed] [Google Scholar]; Eritsland J, Arnesen H, Seljeflot I, Kierulf P. Long‐term effects of n‐3 polyunsaturated fatty acids on haemostatic variables and bleeding episodes in patients with coronary artery disease. Blood Coagulation & Fibrinolysis 1995;6(1):17‐22. [DOI] [PubMed] [Google Scholar]; Eritsland J, Seljeflot I, Abdelnoor M, Arnesen H. Long‐term influence of omega‐3 fatty acids on fibrinolysis, fibrinogen, and serum lipids. Fibrinolysis 1994;8(2):120‐5. [Google Scholar]; Eritsland J, Seljeflot I, Abdelnoor M, Arnesen H, Torjesen PA. Long‐term effects of n‐3 fatty acids on serum lipids and glycaemic control. Scandinavian Journal of Clinical and Laboratory Investigation 1994;54(4):273‐80. [DOI] [PubMed] [Google Scholar]; Eritsland J, Seljeflot I, Arnesen H, Abdelnoor M. Long‐term effects of fish oil supplementation in patients with coronary artery disease: influence on lipoproteins, coagulation and fibrinolysis. Thrombosis Research 1992;65:75. [Google Scholar]; Eritsland J, Seljeflot I, Arnesen H, Abdelnoor M. Long‐term influence of omega‐3 fatty acids on fibrinolysis, fibrinogen, and serum lipids. Thrombosis and Haemostasis 1993;69:1065. [Google Scholar]; Eritsland J, Seljeflot I, Arnesen H, Westvik AB, Kierulf P. Effect of long‐term, moderate‐dose supplementation with omega‐3 fatty acids on monocyte procoagulant activity and release of interleukin‐6 in patients with coronary artery disease. Thrombosis Research 1995;77(4):337‐46. [DOI] [PubMed] [Google Scholar]
- Sianni A, Matsoukis I, Ganotopoulou A, Paraskevas P, Asimis A, Tsivilis N, et al. Effect of omega 3 fatty acids in patients with hypertension and atrial fibrillation. Clinical Nutrition 2013;32:S70‐1. [Google Scholar]
- Anil S, Charlton KE, Tapsell LC, Probst Y, Ndanuko R, Batterham MJ. Identification of dietary patterns associated with blood pressure in a sample of overweight Australians. Journal of Human Hypertension 2016;30(11):672‐8. [DOI: 10.1038/jhh.2016.10] [DOI] [PubMed] [Google Scholar]; Tapsell LC, Batterham MJ, Charlton KE. Effect of dietary restriction and n‐3 PUFA supplementation on insulin resistance in obese adults. FASEB Journal 2010;24:733.9. [Google Scholar]; Tapsell LC, Batterham MJ, Charlton KE, Neale EP, Probst YC, O'Shea JE, et al. Foods, nutrients or whole diets: effects of targeting fish and LCn3PUFA consumption in a 12mo weight loss trial. BMC Public Health 2013;13:1231. [PUBMED: 24369765] [DOI] [PMC free article] [PubMed] [Google Scholar]; Zhang Q, O'Shea JE, Thorne RL, Tapsell LC, Batterham M, Charlton KE. Baseline characteristics of volunteers in the smart clinical trial: associations between habitual physical activity and lifestyle disease risk factors.. Nutrition and Dietetics 2010;67(Suppl 1):67‐8. [Google Scholar]
- Brouwer IA, Katan MB, Schouten EG, Camm AJ, Hauer RNW, Wever EFD, et al. Rationale and design of a clinical trial on n‐3 fatty acids and cardiac arrhythmia (SOFA). Annals of Nutrition & Metabolism 2001;45(Suppl 1):79. [Google Scholar]; Brouwer IA, Raitt MH, Dullemeijer C, Kraemer DF, Zock PL, Morris C, et al. Effect of fish oil on ventricular tachyarrhythmia in three studies in patients with implantable cardioverter defibrillators. European Heart Journal 2009;30(7):820‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Brouwer IA, Zock PL, Camm AJ, Böcker D, Hauer RN, Wever EF, et al. Effect of fish oil on ventricular tachyarrhythmia and death in patients with implantable cardioverter defibrillators: the study on omega‐3 fatty acids and ventricular arrhythmia (SOFA) randomized trial. JAMA 2006;295(22):2613‐9. [DOI] [PubMed] [Google Scholar]; Brouwer IA, Zock PL, Wever EFD, Hauer RNW, Camm AJ, Bocker D, et al. Rationale and design of a randomised controlled clinical trial on supplemental intake of n‐3 fatty acids and incidence of cardiac arrhythmia: SOFA. European Journal of Clinical Nutrition 2003;57:1323‐30. [DOI] [PubMed] [Google Scholar]
- Sofi F, Giangrandi I, Cesari F, Corsani I, Abbate R, Gensini GF, et al. Effects of a 1‐year dietary intervention with n‐3 polyunsaturated fatty acid‐enriched olive oil on non‐alcoholic fatty liver disease patients: a preliminary study. International Journal of Food Sciences and Nutrition 2010;61(8):792‐802. [PUBMED: 20465434] [DOI] [PubMed] [Google Scholar]
- Ahluwalia N, Blacher J, Szabo De Edelenyi F, Faure P, Julia C, Hercberg S, et al. Prognostic value of multiple emerging biomarkers in cardiovascular risk prediction in patients with stable cardiovascular disease. Atherosclerosis 2013;228(2):478‐84. [DOI] [PubMed] [Google Scholar]; Andreeva VA, Galan P, Torres M, Julia C, Hercberg S, Kesse‐Guyot E. Supplementation with B vitamins or n‐3 fatty acids and depressive symptoms in cardiovascular disease survivors: ancillary findings from the SUpplementation with FOLate, vitamins B‐6 and B‐12 and/or OMega‐3 fatty acids (SU.FOL.OM3) randomized trial. American Journal of Clinical Nutrition 2012;96(1):208‐14. [DOI] [PubMed] [Google Scholar]; Andreeva VA, Kesse‐Guyot E, Barberger‐Gateau P, Fezeu L, Hercberg S, Galan P. Cognitive function after supplementation with B vitamins and long‐chain omega‐3 fatty acids: ancillary findings from the SU.FOL.OM3 randomized trial. American Journal of Clinical Nutrition 2011;94(1):278‐86. [DOI] [PubMed] [Google Scholar]; Andreeva VA, Latarche C, Hercberg S, Briancon S, Galan P, Kesse‐Guyot E. B vitamin and/or n‐3 fatty acid supplementation and health‐related quality of life: ancillary findings from the SU.FOL.OM3 randomized trial. PLOS ONE 2014;9(1):e84844. [DOI] [PMC free article] [PubMed] [Google Scholar]; Andreeva VA, Touvier M, Kesse‐Guyot E, Julia C, Galan P, Hercberg S. B vitamin and/or omega‐3 fatty acid supplementation and cancer: ancillary findings from the supplementation with folate, vitamins B6 and B12, and/or omega‐3 fatty acids (SU.FOL.OM3) randomized trial. Archives of Internal Medicine 2012;172(7):540‐7. [DOI] [PubMed] [Google Scholar]; Blacher J, Czernichow S, Paillard F, Ducimetiere P, Hercberg S, Galan P, et al. Cardiovascular effects of B‐vitamins and/or n‐3 fatty acids: the SU.FOL.OM3 trial. International Journal of Cardiology 2013;167(2):508‐13. [DOI] [PubMed] [Google Scholar]; Blacher J, Safar ME, Ly C, Szabo De Edelenyi F, Hercberg S, Galan P. Blood pressure variability: cardiovascular risk integrator or independent risk factor. Journal of Human Hypertension 2015;29(2):122‐6. [DOI] [PubMed] [Google Scholar]; Fezeu LK, Laporte F, Kesse‐Guyot E, Andreeva VA, Blacher J, Hercberg S, et al. Baseline plasma fatty acids profile and incident cardiovascular events in the SU.FOL.OM3 trial: the evidence revisited. PLOS ONE 2014;9(4):e92548. [DOI] [PMC free article] [PubMed] [Google Scholar]; Galan P, Briancon S, Blacher J, Czernichow S, Hercberg S. The SU.FOL.OM3 Study: a secondary prevention trial testing the impact of supplementation with folate and B‐vitamins and/or Omega‐3 PUFA on fatal and non fatal cardiovascular events, design, methods and participants characteristics. Trials 2008;9:35. [DOI: 10.1186/1745-6215-9-35] [DOI] [PMC free article] [PubMed] [Google Scholar]; Galan P, Briancon S, Blacher J, Czernichow S, Hercberg S. The SU.FOL.OM3 Study: a secondary prevention trial testing the impact of supplementation with folate and B‐vitamins and/or Omega‐3 PUFA on fatal and non fatal cardiovascular events, design, methods and participants characteristics. Trials 2008;9:35. [DOI] [PMC free article] [PubMed] [Google Scholar]; Galan P, Briancon S, Blacher J, Czernichow S, Hercberg S. The scientific basis of the SU.FOL.OM3 study: a secondary intervention trial of folate, B6 and B12 vitamins and/or omega3 fatty acid supplements in the prevention of recurrent ischemic events. Sang Thrombose Vaisseaux 2009;21(4):207‐13. [Google Scholar]; Galan P, Briançon S, Blacher J, Czernichow S, Hercberg S. The scientific basis of the SU.FOL.OM3 study: a secondary intervention trial of folate, B6 and B12 vitamins and/or omega3 fatty acid supplements in the prevention of recurrent ischemic events [Bases scientifiques de l'étude SUFOLOM3: essai de prévention secondaire visant à tester l'impact d'une supplémentation en folates, vitamines B6 et B12 et/ ou acides gras oméga‐3 dans la prévention de la récidive de pathologies ischémiques]. Sang Thrombose Vaisseaux 2009;21(4):207‐13. [Google Scholar]; Galan P, Kesse‐Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S, SU.FOL.OM3 Collaborative Group. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ 2010;341:c6273. [DOI: 10.1136/bmj.c6273] [DOI] [PMC free article] [PubMed] [Google Scholar]; Galan P, Bree A, Mennen L, Potier de Courcy G, Preziozi P, Bertrais S, Castetbon K, Hercberg S. Background and rationale of the SU.FOL.OM3 study: double‐blind randomized placebo‐controlled secondary prevention trial to test the impact of supplementation with folate, vitamin B6 and B12 and/or omega‐3 fatty acids on the prevention of recurrent ischemic events in subjects with atherosclerosis in the coronary or cerebral arteries. Journal of Nutrition, Health and Aging 2003;7(6):428‐35. [PubMed] [Google Scholar]; Kesse‐Guyot E, Peneau S, Hercberg S, Galan P, Vogt L, Escande M, et al. Thirteen‐year prospective study between fish consumption, long‐chain N‐3 fatty acids intakes and cognitive function. Journal of Nutrition, Health and Aging 2011;15(2):115‐20. [DOI] [PubMed] [Google Scholar]; Szabo De Edelenyi F, Vergnaud AC, Ahluwalia N, Julia C, Hercberg S, Blacher J, et al. Effect of B‐vitamins and n‐3 PUFA supplementation for 5 years on blood pressure in patients with CVD. British Journal of Nutrition 2012;107(6):921‐7. [DOI] [PubMed] [Google Scholar]; Vesin C, Galan P, Gautier B, Czernichow S, Hercberg S, Blacher J. Control of baseline cardiovascular risk factors in the SU‐FOL‐OM3 study cohort: does the localization of the arterial event matter?. European Journal of Cardiovascular Prevention & Rehabilitation 2010;17(5):541‐8. [DOI] [PubMed] [Google Scholar]; Bree A, Mennen LI, Hercberg S, Galan P. Evidence for a protective (synergistic?) effect of B‐vitamins and omega‐3 fatty acids on cardiovascular diseases. European Journal of Clinical Nutrition 2004;58(5):732‐44. [DOI] [PubMed] [Google Scholar]
- Tande KS, Vo TD, Lynch BS. Clinical safety evaluation of marine oil derived from Calanus finmarchicus. Regulatory Toxicology and Pharmacology: RTP 2016;80:25‐31. [PUBMED: 27233921] [DOI] [PubMed] [Google Scholar]
- Packard DP, Milton JE, Shuler LA, Short RA, Tuttle KR. Implications of chronic kidney disease for dietary treatment of cardiovascular disease. Journal of Renal Nutrition 2006;16(3):259‐68. [DOI] [PubMed] [Google Scholar]; Tuttle KR, Shuler LA, Packard DP, Milton JE, Daratha KB, Bibus DM, et al. Comparison of low‐fat versus Mediterranean‐style dietary intervention after first myocardial infarction (from The Heart Institute of Spokane Diet Intervention and Evaluation Trial). American Journal of Cardiology 2008;101(11):1523‐30. [PUBMED: 18489927] [DOI] [PubMed] [Google Scholar]
- Bitok E, Jaceldo‐Siegl K, Rajaram S, Serra‐Mir M, Roth I, Feitas‐Simoes T, et al. Favourable nutrient intake and displacement with long‐term walnut supplementation among elderly: results of a randomised trial. British Journal of Nutrition 2017;118(3):201‐9. [DOI: 10.1017/S0007114517001957] [DOI] [PubMed] [Google Scholar]; Bitok E, Rajaram S, Ros E. Does a daily walnut supplement given for a year result in body weight gain?. FASEB Journal2016; Vol. 30:1157.5. ; Huey L, Bitok E, Kazzi N. Dietary compliance of walnut or no walnut intake in a 1‐year randomized intervention trial among free‐living elderly in the Walnuts and Healthy Aging Study (WAHA). FASEB Journal2016; Vol. 30:1157.10. ; Rajaram S, Valls‐Pedret C, Cofan M, Sabate J, Serra‐Mir M, Perez‐Heras AM, et al. The Walnuts and Healthy Aging Study (WAHA): protocol for a nutritional intervention trial with walnuts on brain aging. Frontiers in Aging Neuroscience 2016;8:333. [PUBMED: 28119602] [DOI] [PMC free article] [PubMed] [Google Scholar]; Ros, Emilio, Rajaram, Sujatha, Sala‐Vila, Aleix, et al. Effect of a 1‐year walnut supplementation on blood lipids among older individuals: findings from the Walnuts and Healthy Aging (WAHA) study. FASEB Journal2016; Vol. 30, issue 1 Suppl:293.4.
- Weinstock‐Guttman B, Baier M, Park Y, Feichter J, Lee‐Kwen P, Gallagher E, et al. Low fat dietary intervention with n‐3 fatty acid supplementation in multiple sclerosis patients. Prostaglandins, Leukotrienes and Essential Fatty Acids 2005;73:397‐404. [DOI: 10.1016/j.plefa.2005.05.024] [DOI] [PubMed] [Google Scholar]
- Bhatia L, Scorletti E, Curzen N, Clough GF, Calder PC, Byrne CD. Improvement in non‐alcoholic fatty liver disease severity is associated with a reduction in carotid intima‐media thickness progression. Atherosclerosis 2016;246:13‐20. [PUBMED: 26748347] [DOI] [PubMed] [Google Scholar]; Byrne CD, Targher G. Ectopic fat, insulin resistance, and nonalcoholic fatty liver disease: implications for cardiovascular disease. Arteriosclerosis, Thrombosis, and Vascular Biology 2014;34(6):1155‐61. [PUBMED: 24743428] [DOI] [PubMed] [Google Scholar]; Byrne CD, Targher G. Time to replace assessment of liver histology with MR‐based imaging tests to assess efficacy of interventions for nonalcoholic fatty liver disease. Gastroenterology2016; Vol. 150, issue 1:7‐10. [PUBMED: 26602219] [DOI] [PubMed]; Clough GF, McCormick KG, Scorletti E, Bhatia L, Calder PC, Griffin MJ, et al. Higher body fat percentage is associated with enhanced temperature perception in NAFLD: results from the randomised Wessex evaluation of fatty liver and cardiovascular markers in NAFLD with omacor therapy trial (WELCOME) trial. Diabetologia 2016;59(7):1422‐9. [PUBMED: 27106721] [DOI] [PubMed] [Google Scholar]; Hodson L, Bhatia L, Scorletti E, Smith DE, Jackson NC, Shojaee‐Moradie F, et al. Docosahexaenoic acid enrichment in NAFLD is associated with improvements in hepatic metabolism and hepatic insulin sensitivity: a pilot study. European Journal of Clinical Nutrition 2017;71(8):973‐9. [PUBMED: 28294174] [DOI] [PMC free article] [PubMed] [Google Scholar]; McCormick KG, Scorletti E, Bhatia L, Calder PC, Griffin MJ, Clough GF, et al. Impact of high dose n‐3 polyunsaturated fatty acid treatment on measures of microvascular function and vibration perception in non‐alcoholic fatty liver disease: results from the randomised WELCOME trial. Diabetologia 2015;58(8):1916‐25. [PUBMED: 26021488] [DOI] [PubMed] [Google Scholar]; McCormick KG, Scorletti ES, Bhatia L, Calder PC, Griffin MJ, Clough GF, et al. Peripheral sensory nerve function is independently associated with microvascular function, but neither are improved by n‐3 fatty acids. Diabetic Medicine 2015;32(S1):99. [Google Scholar]; Scorletti E, Bhatia B, McCormick KG, Clough GF, Nash K, Hodson L, et al. Potential benefits of purified long chainomega‐3 fatty acid treatment in non‐alcoholic fatty liver disease (NAFLD): a potential treatment for early NAFLD in metabolic syndrome and type 2 diabetes? Results from the WELCOME study. Diabetic Medicine 2014;31:1. [Google Scholar]; Scorletti E, Bhatia L, McCormick KG, Clough GF, Nash K, Calder PC, et al. Design and rationale of the WELCOME trial: A randomised, placebo controlled study to test the efficacy of purified long chainomega‐3 fatty acid treatment in non‐alcoholic fatty liver disease [corrected]. Contemporary Clinical Trials 2014;37(2):301‐11. [PUBMED: 24556343] [DOI] [PubMed] [Google Scholar]; Scorletti E, Bhatia L, McCormick KG, Clough GF, Nash K, Calder PC, et al. Design and rationale of the WELCOME trial: a randomised, placebo controlled study to test the efficacy of purified long chain omega‐3 fatty treatment in non‐alcoholic fatty liver disease. Contemporary Clinical Trials 2014;38(1):156. [DOI] [PubMed] [Google Scholar]; Scorletti E, Bhatia L, McCormick KG, Clough GF, Nash K, Hodson L, et al. Effects of purified eicosapentaenoic and docosahexaenoic acids in nonalcoholic fatty liver disease: results from the Welcome* study. Hepatology (Baltimore, MD) 2014;60(4):1211‐21. [PUBMED: 25043514] [DOI] [PubMed] [Google Scholar]; Scorletti E, West AL, Bhatia L, Hoile SP, McCormick KG, Burdge GC, et al. Treating liver fat and serum triglyceride levels in NAFLD, effects of PNPLA3 and TM6SF2 genotypes: results from the WELCOME trial. Journal of Hepatology 2015;63(6):1476‐83. [PUBMED: 26272871] [DOI] [PubMed] [Google Scholar]; Targher G, Byrne CD. Clinical review: nonalcoholic fatty liver disease: a novel cardiometabolic risk factor for type 2 diabetes and its complications. Journal of Clinical Endocrinology and Metabolism 2013;98(2):483‐95. [PUBMED: 23293330] [DOI] [PubMed] [Google Scholar]
- Zhang Y‐P, Rujuan M, Qing L, Wu T, Ma F. Effects of DHA supplementation on hippocampal volume and cognitive function in older adults with mild cognitive impairment: a 12‐month randomized, double‐blind, placebo‐controlled trial. Journal of Alzheimer's Disease 2016;55(2):497‐507. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Alekseeva RI, Sharafetdinov K, Plotnikova OA, Meshcheriakova VA, Mal'tsev GI, Kulakova SN. Effects of a diet including linseed oil on clinical and metabolic parameters in patients with type 2 diabetes mellitus. Voprosy Pitaniia 2000;69(6):32‐5. [PubMed] [Google Scholar]
- Baleztena Gurrea J, Ruiz‐Canela M, Pardo M, Castellanos MC, Gozalo MJ, Añorbe T, et al. Utility of heavy food supplement in omega‐3 fatty acids in the prevention of dementia, in relation to the basal nutritional level, in people of advanced age: randomized multicenter study. Revista Española de Geriatría y Gerontología 2015;50:1‐49. 25443787 [Google Scholar]; Bes‐Rastrollo M, Baleztena J, Aguirre I, Ruiz‐Canela M. Utility of a rich food supplement Omega‐3 fatty acids in the prevention of dementia, in relation to baseline nutritional level, in people with advanced age: multicentre randomised study [Complemento alimenticio rico en ácidos grasos omega‐3 en la prevención de la demencia: estudio aleatorizado multicéntrico]. Nutrición Clínica en Medicina 2015;9(1):38. [Google Scholar]
- Belch JJ, Ansell D, Madhok R, O'Dowd A, Sturrock RD. Effects of altering dietary essential fatty acids on requirements for non‐steroidal anti‐inflammatory drugs in patients with rheumatoid arthritis: a double blind placebo controlled study. Annals of the Rheumatic Diseases 1988;47(2):96‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belluzzi A, Brignola C, Campieri M, Pera A, Boschi S, Miglioli M. Effect of an enteric‐coated fish‐oil preparation on relapses in Crohn's disease. New England Journal of Medicine 13‐6‐1996;334(24):1557‐60. [DOI] [PubMed] [Google Scholar]
- Berthoux FC, Guerin C, Burgard G, Berthoux P, Alamartine E. One‐year randomized controlled trial with omega‐3 fatty acid‐fish oil in clinical renal transplantation. Transplantation Proceedings 1992;24(6):2578‐82. [PubMed] [Google Scholar]
- Borchgrevink CF, Berg KJ, Skaga E, Skjaeggestad O, Stormorken H. Effect of linseed oil on platelet adhesiveness and bleeding time in patients with coronary heart disease. Lancet 1965;ii:980‐2. [DOI] [PubMed] [Google Scholar]; Borchgrevink CF, Skaga E, Berg KJ, Skjaeggestad O. Absence of prophylactic effect of linolenic acid in patients with coronary heart disease. Lancet 1966;2(456):187‐9. [DOI] [PubMed] [Google Scholar]
- Busnach G, Straglioto E, Minetti E, Perego A, Brando B, Broggi ML, et al. Effect of N‐3 polyunsaturated fatty acids on cyclosporine pharmacokinetics in kidney graft recipients: a randomized placebo‐controlled study. Journal of Nephrology 1998;11(2):87‐93. [PubMed] [Google Scholar]
- NCT02525198. The cognitive ageing nutrition and neurogenesis trial (CANN) [A randomised controlled trial in 'at risk' humans investigating the cognitive benefits of a combined flavonoid/fatty acid intervention and underlying mechanisms of action: the Cognitive Aging Nutrition and Neurogenesis 8CANN) trial]. clinicaltrials.gov/ct2/show/NCT02525198 (first received 17 August 2015).
- Cappelli P, Di LL, Stuard S, Ballone E, Albertazzi A. N‐3 polyunsaturated fatty acid supplementation in chronic progressive renal disease. Journal of Nephrology 1997;10(3):157‐62. [PubMed] [Google Scholar]
- ISRCTN10431469. Changes in brain function among individuals with a mild memory impairment (CARES). www.isrctn.com/ISRCTN10431469 (first received 21 December 2015). [ISRCTN10431469]
- Cheng A, Bustami M, Norell MS, Mitchell AG, Ilsey CDJ. The effect of omega‐3 fatty acids on restenosis after coronary angioplasty. European Heart Journal 1990;11:368. 2139611 [Google Scholar]
- Cheng IKP, Chan PCK, Chan MK. The effect of fish oil dietary supplement on the progression of mesangial IgA glomerulonephritis. Nephrology, Dialysis, Transplantation 1990;5:241‐16. [DOI] [PubMed] [Google Scholar]
- Clark WF, Parbtani A, Naylor CD, Levinton CM, Muirhead N, Spanner E, et al. Fish oil in lupus nephritis: clinical findings and methodological implications. Kindney International 1993;44(1):75‐86. [DOI] [PubMed] [Google Scholar]
- Clark WF, Parbtani A. Omega‐3 fatty acid supplementation in clinical and experimental lupus nephritis. American Journal of Kidney Diseases 1994;23(5):644‐7. [DOI] [PubMed] [Google Scholar]
- Clark WF, Kortas C, Heidenheim AP, Garland J, Spanner E, Parbtani A. Flaxseed in lupus nephritis: a two‐year nonplacebo‐controlled crossover study. Journal of the American College of Nutrition 2001;20(2 Suppl):143‐8. [PUBMED: 11349937] [DOI] [PubMed] [Google Scholar]
- Clausen J, Nielsen SA, Kristensen M. Biochemical and clinical effects of an antioxidative supplementation of geriatric patients. A double blind study. Biological Trace Element Research 1989;20(1‐2):135‐51. [DOI] [PubMed] [Google Scholar]
- Diskin CJ, Thomas CE, Zellner CP, Lock S, Tanja J. Fish oil to prevent intimal hyperplasia and access thrombosis. Nephron 1990;55(4):445‐7. [DOI] [PubMed] [Google Scholar]
- Donadio JJ, Bergstralh EJ, Offord KP, Spencer DC, Holley KE. A controlled trial of fish oil in IgA nephropathy. Mayo Nephrology Collaborative Group. New England Journal of Medicine 1994;331:1194‐9. [DOI] [PubMed] [Google Scholar]
- Doyle W, Srivastava A, Crawford MA, Bhatti R, Brooke Z, Costeloe KL. Inter‐pregnancy folate and iron status of women in an inner‐city population. British Journal of Nutrition 2001;86(1):81‐7. [DOI] [PubMed] [Google Scholar]
- Dry J, Vincent D. Effect of a fish oil diet on asthma: results of a 1‐year double‐blind study. International Archives of Allergy and Applied Immunology 1991;95(2‐3):156‐7. [DOI] [PubMed] [Google Scholar]
- Ezaki O, Takahashi M, Shigematsu T, Shimamura K, Kimura J, Ezaki H, et al. Long‐term effects of dietary alpha‐linolenic acid from perilla oil on serum fatty acids composition and on the risk factors of coronary heart disease in Japanese elderly subjects. Journal of Nutritional Science & Vitaminology 1999;45(6):759‐72. [DOI] [PubMed] [Google Scholar]
- Feher J, Kovacs B, Kovacs I, Schveoller M, Papale A, Balacco Gabrieli C. Improvement of visual functions and fundus alterations in early age‐related macular degeneration treated with a combination of acetyl‐L‐carnitine, n‐3 fatty acids, and coenzyme Q10. Ophthalmologica 2005;219(3):154‐66. [PUBMED: 15947501] [DOI] [PubMed] [Google Scholar]
- Browning LM, Walker CG, Mander AP, West AL, Madden J, Gambell JM, et al. Incorporation of eicosapentaenoic and docosahexaenoic acids into lipid pools when given as supplements providing doses equivalent to typical intakes of oily fish. American Journal of Clinical Nutrition 2012;96(4):748‐58. [PUBMED: 22932281] [DOI] [PMC free article] [PubMed] [Google Scholar]; Walker CG, Browning LM, Mander AP, Madden J, West AL, Calder PC, et al. Age and sex differences in the incorporation of EPA and DHA into plasma fractions, cells and adipose tissue in humans. British Journal of Nutrition 2014;111(4):679‐89. [PUBMED: 24063767] [DOI] [PMC free article] [PubMed] [Google Scholar]; Walker CG, Browning LM, Stecher L, West AL, Madden J, Jebb SA, et al. Fatty acid profile of plasma NEFA does not reflect adipose tissue fatty acid profile. British Journal of Nutrition 2015;114(5):756‐62. [PUBMED: 26205910] [DOI] [PubMed] [Google Scholar]; Walker CG, West AL, Browning LM, Madden J, Gambell JM, Jebb SA, et al. The pattern of fatty acids displaced by EPA and DHA following 12 months supplementation varies between blood cell and plasma fractions. Nutrients 2015;7(8):6281‐93. [PUBMED: 26247960] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonolla J, Lopez‐Huertas E, Machado FJ, Molina D, Alvarez I, Marmol E, et al. Milk enriched with "healthy fatty acids" improves cardiovascular risk markers and nutritional status in human volunteers. Nutrition 2009;25(4):408‐14. [PUBMED: 19084376] [DOI] [PubMed] [Google Scholar]
- Fonolla J, Diaz‐Ropero M, Geerlings A, Marti J, Lopez‐Huertas E. Daily intake of a dairy drink enriched with omega‐3 (EPA+DHA) and oleic acid improves cardiovascular markers in healthy postmenopausal women. Atherosclerosis Supplements 2010;11(2):58. [Google Scholar]; Fonolla J, Diaz‐Ropero P, Marti JL, Rodriguez‐Martinez C, Lopez‐Huertas E. Daily intake of a low lactose dairy drink enriched with omega‐3 (EPA+DHA), oleic acid and calcium improves nutritional and bone status in healthy postmenopausal women. Clinical Nutrition 2011;6(1):86. [Google Scholar]; Fonolla‐Joya J, Reyes‐García R, García‐Martín A, López‐Huertas E, Muñoz‐Torres M. Daily intake of milk enriched with n‐3 fatty acids, oleic acid, and calcium improves metabolic and bone biomarkers in postmenopausal women. Journal of the American College of Nutrition 2016;35(6):529‐36. [DOI: 10.1080/07315724.2014] [DOI] [PubMed] [Google Scholar]
- Franzen D, Hopp HW, Schanwell M, Hilger HH. Long‐term effect of fish oil and olive oil on plasma lipids in patients with CHD. Zeitschrift fur Kardiologie 1989;78(Suppl 4):28. 2530710 [Google Scholar]
- Galarraga B, Ho M, Youssef HM, Hill A, McMahon H, Hall C, et al. Cod liver oil (n‐3 fatty acids) as an non‐steroidal anti‐inflammatory drug sparing agent in rheumatoid arthritis. Rheumatology 2008;47(5):665‐9. [DOI: 10.1093/rheumatology/ken024] [DOI] [PubMed] [Google Scholar]
- Gapparova KM, Pogozheva AV, Kulakova SN, Tutel'ian VA. Effects of omega‐3 polyunsaturated fatty acids of vegetable and animal origin on clinical and metabolic indicators and the intensity of lipid peroxidation in patients with ischemic heart disease and impaired carbohydrate tolerance. Voprosy Pitaniia 2000;69(1‐2):46‐9. [PubMed] [Google Scholar]
- Gazso A, Horrobin D, Sinzinger H. Influence of omega‐3 fatty acids on the prostaglandin‐metabolism in healthy volunteers and patients suffering from PVD. Agents and Actions. Supplements 1992;37:151‐6. [DOI] [PubMed] [Google Scholar]
- Geusens P, Wouters C, Nijs J, Jiang Y, Dequeker J. Long‐term effect of omega‐3 fatty acid supplementation in active rheumatoid arthritis. A 12‐month, double‐blind, controlled study. Arthritis and Rheumatism 1994;37(6):824‐9. [DOI] [PubMed] [Google Scholar]
- Gogos CA, Ginopoulos P, Salsa B, Apostolidou E, Zoumbos NC, Kalfarentzos F. Dietary omega‐3 polyunsaturated fatty acids plus vitamin E restore immunodeficiency and prolong survival for severely ill patients with generalized malignancy: a randomized control trial. Cancer 1998;82(2):395‐402. [DOI] [PubMed] [Google Scholar]
- Greatrex JC, Drasdo N, Dresser K. Scotopic sensitivity in dyslexia and requirements for DHA supplementation. Lancet 2000;355(9213):1429‐30. [DOI] [PubMed] [Google Scholar]
- Griffin BA, Minihane AM, Furlonger N, Chapman C, Murphy M, Williams D, et al. Inter‐relationships between small, dense low‐density lipoprotein (LDL), plasma triacylglycerol and LDL apoprotein B in an atherogenic lipoprotein phenotype in free‐living subjects. Clinical Science 1999;97(3):269‐76. [PubMed] [Google Scholar]
- Hamazaki T, Tateno S, Shishido H. Eicosapentaenoic acid and IgA nephropathy. Lancet 1984;1(8384):1017‐8. [DOI] [PubMed] [Google Scholar]
- Hansen GV, Nielsen L, Kluger E, Thysen M, Emmertsen H, Stengaard PK, et al. Nutritional status of Danish rheumatoid arthritis patients and effects of a diet adjusted in energy intake, fish‐meal, and antioxidants. Scandinavian Journal of Rheumatology 1996;25(5):325‐30. [DOI] [PubMed] [Google Scholar]
- Harris WS, Windsor SL, Dujovne CA. Effects of four doses of n‐3 fatty acids given to hyperlipidemic patients for six months. Journal of the American College of Nutrition 1991;10(3):220‐7. [DOI] [PubMed] [Google Scholar]
- Hashimoto M, Yamashita K, Kato S, Tamai T, Matsumoto I, Tanabe Y, et al. Beneficial effects of dietary docosahexaenoic acid intervention on cognitive function in elderly people with very mild dementia in Japan. Alzheimer's and Dementia 2011;1:S610‐1. [Google Scholar]; Hashimoto M, Yamashita K, Kato S, Tamai T, Tanabe Y, Mitarai M, et al. Beneficial effects of daily dietary omega‐3 polyunsaturated fatty acid supplementation on age related cognitive decline in elderly Japanese with very mild dementia: a 2‐year randomized,double‐blind, placebo‐controlled trial. Journal of Aging Research & Clinical Practice 2012;1(3):193‐201. [Google Scholar]
- Hashimoto M, Kato S, Tanabe Y, Katakura M, Mamun AA, Ohno M, et al. Beneficial effects of dietary docosahexaenoic acid intervention on cognitive function and mental health of the oldest elderly in Japanese care facilities and nursing homes. Geriatrics & Gerontology International 2017;17(2):330‐7. [PUBMED: 26822516] [DOI] [PubMed] [Google Scholar]
- Hawthorne AB, Daneshmend TK, Hawkey CJ, Belluzzi A, Everitt SJ, Holmes GK, et al. Treatment of ulcerative colitis with fish oil supplementation: a prospective 12 month randomised controlled trial. Gut 1992;33(7):922‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakshminarayan DK, Elajami TK, Soliman M, Alfaddagh A, Welty FK. Omega‐3 fatty acids supplementation attenuates the progression of microalbuminuria in diabetics with coronary artery disease. Circulation 2015;132:A15530. [Google Scholar]
- Hogg RJ. A randomized, placebo‐controlled, multicenter trial evaluating alternate‐day prednisone and fish oil supplements in young patients with immunoglobulin A nephropathy. American Journal of Kidney Diseases 1995;26(5):792‐6. [DOI] [PubMed] [Google Scholar]
- NCT01744275. High dose omega 3 fatty acids supplementation in patients with epilepsy: the HOPE‐Epilepsy trial. clinicaltrials.gov/ct2/show/NCT01744275 (first received 6 December 2012).
- Huang YC, Jessup JM, Forse RA, Flickner S, Pleskow D, Anastopoulos HT, et al. N‐3 fatty acids decrease colonic epithelial cell proliferation in high‐risk bowel mucosa. Lipids 1996;31:S313‐7. [DOI] [PubMed] [Google Scholar]
- Huang LL, Coleman HR, Kim J, Monasterio F, Wong WT, Schleicher RL, et al. Oral supplementation of lutein/zeaxanthin and omega‐3 long chain polyunsaturated fatty acids in persons aged 60 years or older, with or without AMD. Investigative Ophthalmology & Visual Science 2008;49(9):3864‐9. [DOI] [PubMed] [Google Scholar]
- ISRCTN38354847. A multicentre, double‐blind, randomised, parallel group, placebo‐controlled trial of LAX‐101 (ethyl eicosapentaenoate [EPA]) as adjunct therapy in patients who remain depressed following treatment with standard antidepressant therapy. www.isrctn.com/ISRCTN38354847 (first received 3 February 2003).
- Junker L, Engel S, Berger I, Barleben H. Serum enzymes in grade I hypertensive patients before and following a change in nutrition in relation to polyene acid and electrolyte content. Zeitschrift fur die Gesamte Innere Medizin und Ihre Grenzgebiete 1990;45(11):323‐4. [PubMed] [Google Scholar]
- Kachorovskii BV, Zhoglo FA, Zaverbnyi MI. Total lipid content in the blood after using fish oil in natural and emulsified forms. Farmatsiia 1977;26(5):86. [PubMed] [Google Scholar]
- Kanorskii SG, Bodrikova VV, Kanorskaia Iu S. Influence of perindopril, rosuvastatin, or omega‐3 polyunsaturated fatty acids on efficacy of antirecurrence therapy with sotalol in patients with persistent atrial fibrillation. Kardiologiia 2007;47(12):39‐44. [PubMed] [Google Scholar]
- Karlsson J, Hesselius G, Nygard B, Ronneberg R. Plasma omega‐3 fatty acids before and after nutritional therapy. Journal of Nutritional & Environmental Medicine 1998;8(1):25‐34. [Google Scholar]
- Kaul U, Sanghvi S, Bahl VK, Dev V, Wasir HS. Fish oil supplements for prevention of restenosis after coronary angioplasty. International Journal of Cardiology 1992;35(1):87‐93. [DOI] [PubMed] [Google Scholar]
- Khan F, Elherik K, Bolton‐Smith C, Barr R, Hill A, Murrie I, Belch JJF. The effects of dietary fatty acid supplementation on endothelial function and vascular tone in healthy subjects. Cardiovascular Research 2003;59(4):955‐62. [DOI] [PubMed] [Google Scholar]
- Konya E, Tsuji H, Umekawa T, Kurita T, Iguchi M. Effect of ethyl icosapentate on urinary calcium and oxalate excretion. International Journal of Urology 2000;7(10):361‐5. [DOI] [PubMed] [Google Scholar]
- Kremer JM, Lawrence DA, Petrillo GF, Litts LL, Mullaly PM, Rynes RI, et al. Effects of high‐dose fish oil on rheumatoid arthritis after stopping nonsteroidal antiinflammatory drugs. Clinical and immune correlates. Arthritis and Rheumatism 1995;38(8):1107‐14. [DOI] [PubMed] [Google Scholar]
- Kruger MC, Coetzer H, Winter R, Gericke G, Papendorp DH. Calcium, gamma‐linolenic acid and eicosapentaenoic acid supplementation in senile osteoporosis. Aging (Milano) 1998;10(5):385‐94. [DOI] [PubMed] [Google Scholar]
- Kurabayashi T, Okada M, Tanaka K. Eicosapentaenoic acid effect on hyperlipidemia in menopausal Japanese women. The Niigata Epadel Study Group. Obstetrics & Gynecology 2000;96(4):521‐8. [DOI] [PubMed] [Google Scholar]
- Lau CS, McMahon H, Morley KD, Belch JJF. Effects of Maxepa on non‐steroidal anti‐inflammatory drug useage in patients with mild rheumatoid arthritis. British Journal of Rheumatology 1991;30:137. [DOI] [PubMed] [Google Scholar]; Lau CS, Morley KD, Belch JJ. Effects of fish oil supplementation on non‐steroidal anti‐inflammatory drug requirement in patients with mild rheumatoid arthritis: a double‐blind placebo controlled study. British Journal of Rheumatology 1993;32(11):982‐9. [DOI] [PubMed] [Google Scholar]
- Leaf DA, Connor WE, Barstad L, Sexton G. Incorporation of dietary n‐3 fatty acids into the fatty acids of human adipose tissue and plasma lipid classes. American Journal of Clinical Nutrition 1995;62(1):68‐73. [DOI] [PubMed] [Google Scholar]
- Lee TKM, Clandinin MT, Hébert M, MacDonald IM. Effect of docosahexaenoic acid supplementation on the macular function of patients with Best vitelliform macular dystrophy: randomized clinical trial. Canadian Journal of Ophthalmology 2010;45(5):514‐9. [DOI] [PubMed] [Google Scholar]
- Leng GC, Lee AJ, Fowkes FG, Jepson RG, Lowe GD, Skinner ER, et al. Randomized controlled trial of gamma‐linolenic acid and eicosapentaenoic acid in peripheral arterial disease. Clinical Nutrition 1998;17(6):265‐71. [DOI] [PubMed] [Google Scholar]; Leng GC, Lee AJ, Fowkes FGR, Jepson RG, Horrobin D, Lowe GDO, et al. Randomised controlled trial of y‐linolenic and eicosapentaenoic acid in peripheral vascular disease. Prostaglandins, Leukotrienes and Essential Fatty Acids 1997;57(2):218. [Google Scholar]
- Freund‐Levi Y, Visser PJ, Kivipelto M, Wieggers RL, Hartmann T, Soininen H. The Lipididiet study: rationale and study design. Alzheimer's & Dementia 2012;1:602. [Google Scholar]; Soininen H, Visser PJ, Kivipelto M, Hees A, Rouws C, Hartmann T. A clinical trial investigating the effects of Souvenaid in prodromal Alzheimer's disease: progress and baseline characteristics of the Lipididiet study. Neurobiology of Aging 2014;35:S20. 24952993 [Google Scholar]; Visser PJ, Soininen H, Kivipelto M, Freund‐Levi Y, Kamphuis P, Wieggers RL, et al. A randomized controlled trial investigating the effects of Souvenaid in prodromal Alzheimer's disease: baseline characteristics of the LipiDiDiet study. Alzheimer's & Dementia 2013;9(4 Suppl):669‐70. [DOI: 10.1016/j.jalz.2013.05.1381] [DOI] [Google Scholar]
- Loeschke K, Ueberschaer B, Pietsch A, Gruber E, Ewe K, Wiebecke B, et al. N‐3 fatty acids only delay early relapse of ulcerative colitis in remission. Digestive Diseases and Sciences 1996;41(10):2087‐94. [DOI] [PubMed] [Google Scholar]
- Arnold C, Winter L, Frohlich K, Jentsch S, Dawczynski J, Jahreis G, et al. Macular xanthophylls and omega‐3 long‐chain polyunsaturated fatty acids in age‐related macular degeneration: a randomized trial. JAMA Ophthalmology 2013;131(5):564‐72. [PUBMED: 23519529] [DOI] [PubMed] [Google Scholar]; Dawczynski J, Jentsch S, Schweitzer D, Hammer M, Lang GE, Strobel J. Long term effects of lutein, zeaxanthin and omega‐3‐LCPUFAs supplementation on optical density of macular pigment in AMD patients: the LUTEGA study. Graefe's Archive for Clinical and Experimental Ophthalmology 2013;251(12):2711‐23. [PUBMED: 23695657] [DOI] [PubMed] [Google Scholar]
- Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, et al. Mediterranean alpha‐linolenic acid‐rich diet in secondary prevention of coronary heart disease. [Erratum appears in Lancet 1995 Mar 18;345(8951):738]. Lancet 1994;343(8911):1454‐9. [DOI: 10.1016/S0140-6736(94)92580-1] [DOI] [PubMed] [Google Scholar]; Lorgeril M, Salen P, Caillat‐Vallet E, Hanauer MT, Barthelemy JC, Mamelle N. Control of bias in dietary trial to prevent coronary recurrences: the Lyon Diet Heart Study. European Journal of Clinical Nutrition 1997;51(2):116‐22. [DOI] [PubMed] [Google Scholar]; Lorgeril M, Salen P, Martin JL, Mamelle N, Monjaud I, Touboul P, et al. Effect of a Mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease. Insights into the cardioprotective effect of certain nutriments. Journal of the American College of Cardiology 1996;28(5):1103‐8. [DOI] [PubMed] [Google Scholar]; Lorgeril M, Salen P, Martin JL, Monjaud I, Boucher P, Mamelle N. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Archives of Internal Medicine 1998;158(11):1181‐7. [DOI] [PubMed] [Google Scholar]; Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 1999;99(6):779‐85. [DOI] [PubMed] [Google Scholar]; Lorgeril M, Salen P, Spodick DH. Does a Mediterranean dietary pattern prolong survival?. Cardiology Review 1999;16(12):30‐4. [Google Scholar]; Renaud S, Lorgeril M, Delaye J, Guidollet J, Jacquard F, Mamelle N, et al. Cretan Mediterranean diet for prevention of coronary heart disease. American Journal of Clinical Nutrition 1995;61(6 Suppl):1360S‐7S. [DOI] [PubMed] [Google Scholar]
- Maachi K, Berthoux P, Burgard G, Alamartine E, Berthoux F. Results of a 1‐year randomized controlled trial with omega‐3 fatty acid fish oil in renal transplantation under triple immunosuppressive therapy. Transplantation Proceedings 1995;27(1):846‐9. [PubMed] [Google Scholar]
- Macsai MS. The role of omega‐3 dietary supplementation in blepharitis and meibomian gland dysfunction (an AOS thesis). Transactions of the American Ophthalmological Society 2008;106:336‐56. [PUBMED: 19277245] [PMC free article] [PubMed] [Google Scholar]
- Mansel RE, Harrison BJ, Melhuish J, Sheridan W, Pye JK, Pritchard G, et al. A randomized trial of dietary intervention with essential fatty acids in patients with categorized cysts. Annals of the New York Academy of Sciences 1990;586:288‐94. [DOI] [PubMed] [Google Scholar]
- Mantzaris GJ, Archavlis E, Zografos C, Petraki K, Spiliades C, Triantafyllou G. A prospective, randomized, placebo‐controlled study of fish oil in ulcerative colitis. Hellenic Journal of Gastroenterology 1996;9(2):138‐41. [Google Scholar]
- Mate J, Castanos R, Garcia‐Semaniego J, Pajares JM. Does dietary fish oil maintain the remission of Crohn's disease: a study case control. Gastroenterology 1991;100:A228. [Google Scholar]
- Matsuyama W, Mitsuyama H, Watanabe M, Oonakahara K, Higashimoto I, Osame M, et al. Effects of omega‐3 polyunsaturated fatty acids on inflammatory markers in COPD. Chest 2005;128(6):3817‐27. [DOI] [PubMed] [Google Scholar]
- Middleton SJ, Naylor S, Woolner J, Hunter JO. A double‐blind, randomized, placebo‐controlled trial of essential fatty acid supplementation in the maintenance of remission of ulcerative colitis. Alimentary Pharmacology & Therapeutics 2002;16(6):1131‐5. [PUBMED: 12030955] [DOI] [PubMed] [Google Scholar]
- Roca M, Kohls E, Gili M, Watkins E, Owens M, Hegerl U, et al. Prevention of depression through nutritional strategies in high‐risk persons: rationale and design of the MooDFOOD prevention trial. BMC Psychiatry 2016;16(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qurashi I, Chaudhry IB, Khoso AB, Farooque S, Lane S, Husain MO, et al. A randomised, double‐blind, placebo‐controlled trial of minocycline and/or omega‐3 fatty acids added to treatment as usual for at‐risk mental states (NAYAB): study protocol. Trials 2017;18(1):524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01235533. Fish oil supplementation in late‐life depression. clinicaltrials.gov/ct2/show/NCT01235533 (first received 5 November 2010).
- Berendsen A, Santoro A, Pini E, Cevenini E, Ostan R, Pietruszka B, et al. Reprint of: a parallel randomized trial on the effect of a healthful diet on inflammageing and its consequences in European elderly people: design of the NU‐AGE dietary intervention study. Mechanisms of Ageing and Development 2014;136:14‐21. [DOI] [PubMed] [Google Scholar]; Santoro A, Pini E, Scurti M, Palmas G, Berendsen A, Brzozowska A, et al. Combating inflammaging through a Mediterranean whole diet approach: the NU‐AGE project's conceptual framework and design. Mechanisms of Ageing and Development 2014;136‐137:3‐13. [DOI] [PubMed] [Google Scholar]
- Laake K, Myhre P, Nordby LM, Seljeflot I, Abdelnoor M, Smith P, et al. Effects of omega3 supplementation in elderly patients with acute myocardial infarction: design of a prospective randomized placebo controlled study. BMC Geriatrics 2014;14:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torkildsen O, Wergeland S, Bakke S, Beiske AG, Bjerve KS, Hovdal H, et al. Omega‐3 fatty acid treatment in multiple sclerosis (OFAMS Study): a randomized, double‐blind, placebo‐controlled trial. Archives of Neurology 2012;69(8):1044‐51. [PUBMED: 22507886] [DOI] [PubMed] [Google Scholar]
- Okuda Y, Mizutani M, Ogawa M, Sone H, Asano M, Asakura Y, et al. Long‐term effects of eicosapentaenoic acid on diabetic peripheral neuropathy and serum lipids in patients with type II diabetes mellitus. Journal of Diabetes and its Complications 1996;10(5):280‐7. [DOI] [PubMed] [Google Scholar]
- Colquhoun DM, Hicks BJ, Somerset S. Rationale and design of the "OLIVE" study (comparison of an olive oil enriched to a low fat diet intervention study using vascular endpoints). Atheroscerosis 1997;134(1‐2):326‐27. [Google Scholar]; Colquhoun DM, Somerset S, Glasziou PP, Richards D, Weyers J. Comparison of an olive oil enriched diet to a low fat diet intervention study using vascular endpoints: assessed by repeat quantitative angiography (OLIVE study). Australian Journal of Nutrition and Dietetics 1998;55(Suppl 4):S24‐9. [Google Scholar]
- Leren P. The Oslo diet‐heart study. Eleven year report. Circulation 1970;42:935‐42. [DOI] [PubMed] [Google Scholar]; Leren P. The effect of a cholesterol lowering diet in male survivors of myocardial infarction. (A controlled clinical trial). Nordisk Medicin 1967;77(21):658‐61. [PubMed] [Google Scholar]; Leren P. The effect of plasma cholesterol lowering diet in male survivors of myocardial infarction. A controlled clinical trial. Acta Medica Scandinavica 1966;466(Suppl):1‐92. [PubMed] [Google Scholar]; Leren P. The effect of plasma‐cholesterol‐lowering diet in male survivors of myocardial infarction. A controlled clinical trial. Bulletin of the New York Academy of Medicine 1968;44:1012‐20. [PMC free article] [PubMed] [Google Scholar]
- Pogozheva AV, Rozanova IA, Sorokovoi KV, Karagodina ZV, Levachev MM. Lipid peroxidation in patients with ischemic heart disease, hyperlipidemia and/or hypertension while polyunsaturated omega‐3 fatty acids of plant and animal origin were in their diet. Voprosy Pitaniia 1997;4:32‐5. [PubMed] [Google Scholar]
- Pogozheva AV, Tutel'ian VA, Gapparova KM, Trushina EN, Miagkova MA. The effect of an antiatherosclerotic diet including omega‐3 polyunsaturated fatty acids of marine and plant origins on the indices of cellular and humoral immunity in patients with ischemic heart disease and a disordered carbohydrate tolerance. Voprosy Pitaniia 2000;69(4):33‐5. [PubMed] [Google Scholar]
- Moher D, Weeks L, Ocampo M, Seely D, Sampson M, Altman DG, et al. Describing reporting guidelines for health research: a systematic review. Journal of Clinical Epidemiology 2011;64(7):718‐42. [DOI: 10.1016/j.jclinepi.2010.09.013] [DOI] [PubMed] [Google Scholar]; Puri BK, Bydder GM, Manku MS, Clarke A, Waldman AD, Beckmann CF. Reduction in cerebral atrophy associated with ethyl‐eicosapentaenoic acid treatment in patients with Huntington's disease. Journal of International Medical Research 2008;36:896‐905. [DOI] [PubMed] [Google Scholar]
- Quazi S, Mohiduzzaman M, Mostafizur RM, Keramat AS. Effect of hilsa (Tenualosa ilisha) fish in hypercholesterolemic subjects. Bangladesh Medical Research Council Bulletin 1994;20(1):1‐7. [PubMed] [Google Scholar]
- He J, Klag MJ, Appel LJ, Charleston J, Whelton PK. Seven‐year incidence of hypertension in a cohort of middle‐aged African Americans and whites. Hypertension 1998;31(5):1130‐5. [DOI] [PubMed] [Google Scholar]; Meilahn EN, Kuller LH, Kiss JE, Sacks FM. Coagulation parameters among healthy adults taking fish oil versus placebo. Arteriosclerosis 1990;10:916A. [Google Scholar]; Sacks FM, Hebert P, Appel LJ, Borhani NO, Applegate WB, Cohen JD, et al. Short report: the effect of fish oil on blood pressure and high‐density lipoprotein‐cholesterol levels in phase I of the Trials of Hypertension Prevention. Journal of Hypertension 1994;12(2):209‐13. [PubMed] [Google Scholar]; Sacks FM, Hebert P, Appel LJ, Borhani NO, Applegate WB, Cohen JD, et al. The effect of fish oil on blood pressure and high‐density lipoprotein‐cholesterol levels in phase I of the trials of hypertension prevention. Journal of Hypertension. Supplement 1994;12(7):S23‐31. [PubMed] [Google Scholar]; Satterfield S, Borhani NO, Whelton P, Goodwin L, Brinkmann C, Charleston J, et al. Recruitment for phase I of the Trials of Hypertension Prevention. American Journal of Preventive Medicine 1993;9(4):237‐43. [PubMed] [Google Scholar]; Trials of Hypertension Prevention Collaborative Research Group. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, phase I. JAMA 1992;267(9):1213‐20. [DOI] [PubMed] [Google Scholar]; Whelton PK, Kumanyika SK, Cook NR, Cutler JA, Borhani NO, Hennekens CH, et al. Efficacy of nonpharmacologic interventions in adults with high‐normal blood pressure: results from phase 1 of the Trials of Hypertension Prevention. American Journal of Clinical Nutrition 1997;65(2 Suppl):652S‐60S. [DOI] [PubMed] [Google Scholar]
- Saynor R, Gillott T. Fish oil and plasma fibrinogen. BMJ 1988;297:1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saynor R, Gillott T. Changes in blood lipids and fibrinogen with a note on safety in a long term study on the effects of n‐3 fatty acids in subjects receiving fish oil supplements and followed for seven years. Lipids 1992;27(7):533‐8. [DOI] [PubMed] [Google Scholar]
- Selvais PL, Ketelslegers JM, Buysschaert M, Hermans MP. Plasma endothelin‐1 immunoreactivity is increased following long‐term dietary supplementation with omega‐3 fatty acids in microalbuminuric IDDM patients. Diabetologia 1995;38:253. [DOI] [PubMed] [Google Scholar]
- Shimizu H, Ohtani K, Tanaka Y, Sato N, Mori M, Shimomura Y. Long‐term effect of eicosapentaenoic acid ethyl (EPA‐E) on albuminuria of non‐insulin dependent diabetic patients. Diabetes Research and Clinical Practice 1995;28(1):35‐40. [DOI] [PubMed] [Google Scholar]
- Singh RB, Fedacko J, Vargova V, Pella D, Niaz MA, Ghosh S. Effect of low W‐6/W‐3 fatty acid ratio Paleolithic style diet in patients with acute coronary syndromes: a randomized, single blind, controlled trial. World Heart Journal 2012;4(1):71‐84. [Google Scholar]; Singh RB, Rastogi SS, Verma R, Laxmi B, Singh R, Ghosh S, et al. Randomised controlled trial of cardioprotective diet in patients with recent acute myocardial infarction: results of one year follow up. BMJ 1992;304:1015‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh RB, Niaz MA, Sharma JP, Kumar R, Rastogi V, Moshiri M. Randomized, double‐blind, placebo‐controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival 4. Cardiovascular Drugs and Therapy 1997;11(3):485‐91. [DOI] [PubMed] [Google Scholar]
- Singh RB, Niaz MA, Sharma JP, Kumar R, Rastogi V, Moshiri M. Randomized, double‐blind, placebo‐controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival 4. Cardiovascular Drugs and Therapy 1997;11(3):485‐91. [DOI] [PubMed] [Google Scholar]
- Pella D, Dubnov G, Singh RB, Sharma R, Berry EM, Manor O. Effects of an Indo‐Mediterranean diet on the omega‐6/omega‐3 ratio in patients at high risk of coronary artery disease: the Indian paradox. World Review of Nutrition and Dietetics 2003;92:74‐80. [DOI] [PubMed] [Google Scholar]; Singh RB, Dubnov G, Niaz MA, Ghosh S, Singh R, Rastogi SS, et al. Effect of an Indo‐Mediterranean diet on progression of coronary artery disease in high risk patients (Indo‐Mediterranean Diet Heart Study): a randomised single‐blind trial. Lancet 2002;360(9344):1455‐61. [DOI] [PubMed] [Google Scholar]
- Tariq T, Close C, Dodds R, Viberti GC, Lee T, Vergani D. The effect of fish‐oil on the remission of type 1 (insulin‐dependent) diabetes in newly diagnosed patients. Diabetologia 1989;32(10):765. [DOI] [PubMed] [Google Scholar]
- Terano T, Fujishiro S, Ban T, Yamamoto K, Tanaka T, Noguchi Y, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids 1999;34:S345‐6. [DOI] [PubMed] [Google Scholar]
- Tomer A, Kasey S, Connor WE, Clark S, Harker LA, Eckman JR. Reduction of pain episodes and prothrombotic activity in sickle cell disease by dietary n‐3 fatty acids. Thrombosis & Haemostasis 2001;85(6):966‐74. [PubMed] [Google Scholar]
- Torjesen PA, Birkeland KI, Anderssen SA, Hjermann I, Holme I, Urdal P. Lifestyle changes may reverse development of the insulin resistance syndrome. The Oslo Diet and Exercise Study: a randomized trial. Diabetes Care 1997;20(1):26‐31. [DOI] [PubMed] [Google Scholar]
- Roig‐Revert MJ, Lleo‐Perez A, Zanon‐Moreno V, Vivar‐Llopis B, Marin‐Montiel J, Dolz‐Marco R, et al. Enhanced oxidative stress and other potential biomarkers for retinopathy in type 2 diabetics: beneficial effects of the nutraceutic supplements. BioMed Research International 2015;2015:408180. [PUBMED: 26618168] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton DH, Hoffman DR, Locke KG, Watkins RB, Birch DG. Biological safety assessment of docosahexaenoic acid supplementation in a randomized clinical trial for X‐linked retinitis pigmentosa. Archives of Ophthalmology 2010;121(9):1269‐78. [DOI] [PubMed] [Google Scholar]
- Yasui T, Tanaka H, Fujita K, Iguchi M, Kohri K. Effects of eicosapentaenoic acid on urinary calcium excretion in calcium stone formers. European Urology 2001;39(5):580‐5. [DOI] [PubMed] [Google Scholar]
- Zinger P, Berger I, Liuk K, Taube K, Naumann E. Changes in arterial pressure, serum lipids and thromboxane B2 after using a diet with various levels of eicosapentaenoic acid in patients with hypertension. Klinicheskaia Meditsina 1987;65(1):62‐4. [PubMed] [Google Scholar]
References to ongoing studies
- ACTRN12614000732684. The Aboriginal cardiovascular omega‐3 randomised controlled trial [The effect of omega‐3 supplementation on adverse cardiovascular (CV) events among Indigenous Australians with stable coronary artery disease: A randomized controlled trial Query!]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366337 (first received 10 July 2014).
- Holman RR, Paul S, Farmer A, Tucker L, Stratton IM, Neil HA, et al. Atorvastatin in factorial with omega‐3 EE90 risk reduction in diabetes (AFORRD): a randomised controlled trial. Diabetologia 2009;52(1):50‐9. [DOI] [PubMed] [Google Scholar]; Neil HA, Ceglarek U, Thiery J, Paul S, Farmer A, Holman RR. Impact of atorvastatin and omega‐3 ethyl esters 90 on plasma plant sterol concentrations and cholesterol synthesis in type 2 diabetes: a randomised placebo controlled factorial trial. Atherosclerosis 2010;213(2):512‐7. [DOI] [PubMed] [Google Scholar]
- Bowman L, Aung T, Haynes R, Armitage J. ASCEND: design and baseline characteristics of a large randomised trial in diabetes. Diabetes 2012;61:A556‐7. [Google Scholar]; NCT00135226. ASCEND: A Study of Cardiovascular Events iN Diabetes [A Study of Cardiovascular Events iN Diabetes ‐ A Randomized 2x2 Factorial Study of Aspirin Versus Placebo, and of Omega‐3 Fatty Acid Supplementation Versus Placebo, for Primary Prevention of Cardiovascular Events in People With Diabetes]. https://clinicaltrials.gov/ct2/show/NCT00135226 (first received 25 August 2005).
- ACTRN12610000594022. Fish oil as adjunct therapy for periodontitis [Clinical efficacy of fish oil as adjunct therapy for patients with chronic periodontitis]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=335470 (first received 23 July 2010).
- ACTRN12610000032055. The Beyond Ageing Project: A selective prevention trial using novel pharmacotherapies in an older age cohort at risk for depression Query! [In older adults (60+ years) at risk for depression, can sertraline and/or omega‐3 fatty acids compared with a placebo, reduce or prevent depressive symptoms, incidence of new cases of depression and/or cognitive decline]. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=308413 (first received 22 October 2009). ; Cockayne NL, Duffy SL, Bonomally R, English A, Amminger PG, Mackinnon A, et al. The Beyond Ageing Project Phase 2: a double‐blind, selective prevention, randomised, placebo‐controlled trial of omega‐3 fatty acids and sertraline in an older age cohort at risk for depression: study protocol for a randomized controlled trial. Trials 2015;16:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrakala G, Arpana G, Rao PV. Long‐term effects of a reduced fat diet intervention in pre‐diabetes. 70th Scientific Sessions of the American Diabetes Association; 25‐29 June 2010; Orlando (FL). 2010; Vol. professional.diabetes.org/meeting/scientific‐sessions/70th‐scientific‐sessions‐2010:195‐PO. [Google Scholar]; Chandrakala G, Arpana G, Sreenivas T, Rao PV. Low‐fat (< 20%) diets prevent type 2 diabetes mellitus. Diabetes 2012;61:A190. [Google Scholar]
- ChiCTR‐TRC‐12002014. Influence of different source of n‐3 fatty acid on plasma lipid in moderately hypercholesterolemia subject and the valid dosage. www.chictr.org.cn/hvshowproject.aspx?id=2374 (first received 3 May 2015).
- Do‐Health. DO‐HEALTH trial web site. do‐health.eu/wordpress (accessed prior to 10 May 2018). ; NCT01745263. DO‐HEALTH / Vitamin D3 ‐ Omega3 ‐ Home Exercise ‐ Healthy Ageing and Longevity Trial (DO‐HEALTH). https://clinicaltrials.gov/ct2/show/NCT01745263 (first received 10 December 2012).
- NCT02128763. Dry eye assessment and management study (DREAM). clinicaltrials.gov/ct2/show/NCT02128763 (first received 1 May 2014).
- NCT02676466. The ENRGISE pilot study (ENRGISE) [The ENRGISE (ENabling Reduction of Low‐Grade Inflammation in SEniors) Pilot Study]. clinicaltrials.gov/ct2/show/NCT02676466 (first received 8 February 2016).
- ACTRN12613000034730. Intervention of testosterone & fish oil as a possible strategy for the prevention of Alzheimer's disease. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=363372 (first received 14 January 2013).
- NCT01513252. Long‐term effects of interventional strategies to prevent cognitive decline in elderly (MAPT‐PLUS). clinicaltrials.gov/ct2/show/NCT01513252 (first received 20 January 2012).
- NCT00010868. Omega‐3 fatty acids in bipolar disorder [Omega‐3 Fatty Acids in Bipolar Disorder Prophylaxis]. clinicaltrials.gov/ct2/show/NCT00010868 (first received 5 February 2001).
- NCT00309439. ALA and prostate cancer [Studies of Serum PSA to Help Resolve the Current Implication of Alpha‐linolenic Acid (ALA) and Prostate Cancer]. clinicaltrials.gov/ct2/show/NCT00309439 (first received 31 March 2006).
- NCT00410020. Arrhythmia prevention with an alpha‐linolenic enriched diet [Secondary Prevention of Atrial Fibrillation With an Alpha‐Linolenic Enriched Diet : a Randomized Study]. clinicaltrials.gov/ct2/show/NCT00410020 (first received 12 December 2006).
- NCT01784042. Dietary energy restriction and omega‐3 fatty acids on mammary tissue [Effect of Dietary Energy Restriction and Omega‐3 Fatty Acids on Mammary Tissue and Systemic Biomarkers of Breast Cancer Risk]. clinicaltrials.gov/ct2/show/NCT01784042 (first received 5 February 2013).
- NCT02211560. Investigating a phosphatidylserine based dietary approach for the management of mild cognitive impairment [A, Multi‐center, Double‐blind, Randomized, Placebo‐controlled Study for the Efficacy of Phosphatidylserine in Mild Cognitive Impairment (MCI)]. clinicaltrials.gov/ct2/show/NCT02211560 (first received 7 August 2014).
- NCT02295059. Omega 3 fatty acids and ERPR(‐)HER2(+/‐) breast cancer prevention [Omega‐3 Fatty Acids and ERPR(‐) and HER‐2/Neu(+/‐) Breast Cancer Prevention]. clinicaltrials.gov/ct2/show/NCT02295059 (first received 20 November 2014).
- NCT02719327. Brain amyloid and vascular effects of eicosapentaenoic acid (BRAVE‐EPA) [Impact of Icosapent Ethyl on Alzheimers Disease Biomarkers in Preclinical Adults]. clinicaltrials.gov/ct2/show/NCT02719327 (first received 25 March 2016).
- Laake K, Myhre P, Nordby LM, Seljeflot I, Abdelnoor M, Smith P, et al. Effects of omega 3 supplementation in elderly patients with acute myocardial infarction: design of a prospective randomized placebo controlled study. BMC Geriatrics 2014;14:74. [DOI] [PMC free article] [PubMed] [Google Scholar]; Laake K, Seljeflot I, Schmidt EB, Myhre P, Tveit A, Arnesen H, et al. Serum fatty acids, traditional risk factors, and comorbidity as related to myocardial injury in an elderly population with acute myocardial infarction. Journal of Lipids 2016;2016:4945720. [dx.doi.org/10.1155/2016/4945720] [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT01841944. Omega‐3 Fatty Acids in Elderly Patients With Acute Myocardial Infarction (OMEMI) [Giving Omega‐3 Fatty Acids to Elderly Patients Diagnosed With Acute Myocardial Infarction to Investigate the Effect on Cardiovascular Morbidity and Mortality]. https://clinicaltrials.gov/ct2/show/NCT01841944 (first received 29 April 2013).
- NCT01492361. A study of AMR101 to evaluate its ability to reduce cardiovascular events in high risk patients with hypertriglyceridemia and on statin. The primary objective is to evaluate the effect of 4 g/day AMR101 for preventing the occurrence of a first major cardiovascular event (REDUCE‐IT). clinicaltrials.gov/ct2/show/NCT01492361 (first received 15 December 2011).
- Hull MA, Sandell AC, Montgomery AA, Logan RF, Clifford GM, Rees CJ, et al. A randomized controlled trial of eicosapentaenoic acid and/or aspirin for colorectal adenoma prevention during colonoscopic surveillance in the NHS Bowel Cancer Screening Programme (The seAFOod Polyp Prevention Trial): study protocol for a randomized controlled trial. Trials 2013;14:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01953705. n‐3 PUFA for Vascular Cognitive Aging [Omega 3 PUFA for the Vascular Component of Age‐related Cognitive Decline]. https://clinicaltrials.gov/ct2/show/NCT01953705 (first received 1 October 2013). ; Shinto L, Silbert LC, Dodge HH, Quinn JF, Howieson D, Kaye J, et al. Omega 3 fatty acids for the prevention of vascular cognitive aging: methods and rationale for a phase II trial. Alzheimer's & Dementia 2015;11(7):610. [Google Scholar]
- EudraCT 2014‐001069‐28. A long‐term outcomes study to assess statin residual risk reduction with EpaNova in high cardiovascular risk patients with hypertriglyceridemia (STRENGTH). www.clinicaltrialsregister.eu/ctr‐search/search?query=2014‐001069‐28 (first received 10 February 2015).
- NCT01047449. Improving the results of heart bypass surgery using new approaches to surgery and medication (SUPERIORSVG) [Surgical and Pharmacological Novel Interventions to Improve Overall Results of Saphenous Vein Graft Patency in Coronary Artery Bypass Grafting Surgery: An International Multi‐Center Randomized Controlled Clinical Trial]. clinicaltrials.gov/ct2/show/NCT01047449 (first received 13 January 2010).
- UMIN000012825. Effect of polyunsaturated fatty acids on vascular healing process in hyper‐cholesterolemic patients with acute coronary syndrome. upload.umin.ac.jp/cgi‐open‐bin/ctr_e/ctr_view.cgi?recptno=R000014981 (first received 1 February 2015).
- Bassuk SS, Manson JE, Lee IM, Cook NR, Christen WG, Bubes VY, et al. Baseline characteristics of participants in the VITamin D and OmegA‐3 TriaL (VITAL). Contemporary Clinical Trials 2016;47:235‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gold DR, Litonjua AA, Carey VJ, Manson JE, Buring JE, Lee IM, et al. Lung VITAL: rationale, design, and baseline characteristics of an ancillary study evaluating the effects of vitamin D and/or marine omega‐3 fatty acid supplements on acute exacerbations of chronic respiratory disease, asthma control, pneumonia and lung function in adults. Contemporary Clinical Trials 2016;47:185‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gold DR, Luttmann‐Gibson H, Litonjua AA, Friedenberg G, Gordon D, Lee IM, et al. Baseline chronic obstructive pulmonary disease in the lung vitamin D and omega‐3 trial. American Journal of Respiratory and Critical Care Medicine 2014;189:D44 COPD. [Google Scholar]; Kang JH, Grodstein F, Manson JAE. Cognitive substudy of the vitamin d and omega‐3 trial (vital‐cog): design of a large randomized trial of omega‐3 and vitamin d supplements in relation to cognitive change. Alzheimer's & Dementia 2015;1:608. [Google Scholar]; LeBoff MS, Yue AY, Copeland T, Cook NR, Buring JE, Manson JE. VITAL‐Bone Health: rationale and design of two ancillary studies evaluating the effects of vitamin D and/or omega‐3 fatty acid supplements on incident fractures and bone health outcomes in the VITamin D and OmegA‐3 TriaL (VITAL). Contemporary Clinical Trials 2015;41:259‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]; Manson JAE. Vitamin D and cancer and cardiovascular disease: ready for prime time?. Menopause 2010;17(6):1215. [Google Scholar]; Manson JE. Vitamin D and the heart: why we need large‐scale clinical trials. Cleveland Clinic Journal of Medicine 2010;77(12):903‐10. [DOI] [PubMed] [Google Scholar]; Manson JE, Bassuk SS, Lee IM, Cook NR, Albert MA, Gordon D, et al. The VITamin D and OmegA‐3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega‐3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemporary Clinical Trials 2012;33(1):159‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT01169259. Vitamin D and Omega‐3 Trial (VITAL) (VITAL). https://clinicaltrials.gov/ct2/show/record/NCT01169259 (first received 26 July 2010). ; Pradhan AD, Manson JE. Update on the Vitamin D and OmegA‐3 trial (VITAL). Journal of Steroid Biochemistry & Molecular Biology 2016;155(Pt B):252‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
- Abdelhamid A, Hooper L, Welch A. Polyunsaturated fatty acids for musculoskeletal health and functional status in older adults. PROSPERO 2017;www.crd.york.ac.uk/prospero/display_record.php?RecordID=79211:CRD42017079211. [Google Scholar]
- Abdelhamid AS, Martin N, Bridges C, Brainard JS, Wang X, Brown TJ, et al. Polyunsaturated fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews 2018, Issue 6. [DOI: 10.1002/14651858.CD012345.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Heart Association. Fish and Omega‐3 Fatty Acids. www.heart.org/HEARTORG/HealthyLiving/HealthyEating/HealthyDietGoals/Fish‐and‐Omega‐3‐Fatty‐Acids_UCM_303248_Article.jsp#.WhfuRzenzIU (accessed 24 November 2017).
- Aung T, Halsey J, Kromhout D, Gerstein HC, Marchioli R, Tavazzi L, et al. Associations of omega‐3 fatty acid supplement use with cardiovascular disease risks: meta‐analysis of 10 trials involving 77 917 individuals. JAMA Cardiology 2018;3(3):225‐34. [DOI: 10.1001/jamacardio.2017.5205] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balk EM, Adam GP, Langberg V, Halladay C, Chung M, Lin L, et al. Omega‐3 fatty acids and cardiovascular disease: an updated systematic review. Rockville (MD): Agency for Healthcare Research and Quality; 2016. Evidence report/technology assessment no. 223. AHRQ Publication No. 16‐E002‐EF. www.effectivehealthcare.ahrq.gov/reports/final.cfm. [DOI: 10.23970/AHRQEPCERTA223] [DOI] [PubMed]
- Ballard‐Barbash R, Callaway CW. Marine fish oils: role in prevention of coronary artery disease. Mayo Clinic Proceedings 1987;62:113‐8. [DOI] [PubMed] [Google Scholar]
- Bang HO, Dyerberg J. Plasma lipids and lipoproteins in Greenlandic west coast eskimos. Acta Medica Scandinavica 1972;192:85‐94. [DOI] [PubMed] [Google Scholar]
- Bang HO, Dyerberg J, Hjorne N. The composition of food consumed by Greenland Eskimos. Acta Medica Scandinavica 1976;200:69‐73. [DOI] [PubMed] [Google Scholar]
- Berkley CS, Hoaglin DC, Mosteller F, Colditz GA. A random‐effects regression model for meta‐analysis. Statistics in Medicine 1995;14:395‐411. [DOI] [PubMed] [Google Scholar]
- Bhatnagar D, Durrington PN. Omega‐3 fatty acids: their role in the prevention and treatment of atherosclerosis related risk factors and complications. International Journal of Clinical Practice 2003;57(4):305‐14. [PubMed] [Google Scholar]
- BMJ editors. Expression of concern. BMJ 2005;331:266. [DOI: 10.1136/bmj.331.7511.266] [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Nutrition Foundation. N‐3 fatty acids and health. London: British Nutrition Foundation; 1999. Briefing paper.
- Brown T, Song F, Wang X, Brainard J, Hooper L. Dietary polyunsaturated fat for prevention and treatment of type 2 diabetes mellitus. PROSPERO 2017;www.crd.york.ac.uk/prospero/display_record.php?RecordID=64110:CRD42017064110. [Google Scholar]
- Brunner EJ, Jones PJ, Friel S, Bartley M. Fish, human health and marine ecosystem health: policies in collision. International Journal of Epidemiology 2009;38(1):93‐100. [DOI: 10.1093/ije/dyn157] [DOI] [PubMed] [Google Scholar]
- Burr ML. Fish and ischaemic heart disease. World Review of Nutrition and Dietetics 1993;72:49‐60. [DOI] [PubMed] [Google Scholar]
- Cade JE, Burley VJ, Greenwood DC, UK Women's Cohort Study Steering Group. The UK Women's Cohort Study: comparison of vegetarians, fish‐eaters and meat‐eaters. Public Health Nutrition 2007;7(7):871‐8. [DOI: 10.1079/PHN2004620] [DOI] [PubMed] [Google Scholar]
- Calabresi L, Villa B, Canavesi M, Sirtori CR, James RW, Bernini F, et al. An omega‐3 polyunsaturated fatty acid concentrate increases plasma high‐density lipoprotein 2 cholesterol and paraoxonase levels in patients with familial combined hyperlipidemia. Metabolism 2004;53(2):153‐8. [DOI] [PubMed] [Google Scholar]
- Campbell A, Price J, Hiatt WR. Omega‐3 fatty acids for intermittent claudication. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD003833.pub4] [DOI] [PubMed] [Google Scholar]
- Chang CL, Deckelbaum RJ. Omega‐3 fatty acids: mechanisms underlying "protective effects" in atherosclerosis. Current Opinion in Lipidology 2013;24(4):345‐50. [DOI: 10.1097/MOL.0b013e3283616364] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury R, Stevens S, Gorman D, Pan A, Warnakula S, Chowdhury S, et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta‐analysis. BMJ 2012;345(7881):e6698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado‐Lista J, Perez‐Martinez P, Lopez‐Miranda J, Perez‐Jimenez F. Long chain omega‐3 fatty acids and cardiovascular disease: a systematic review. British Journal of Nutrition 2012;107(Suppl 2):S201‐13. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engell RE, Sanman E, Lim SS, Mozaffarian D. Seafood omega‐3 intake and risk of coronary heart disease death: an updated meta‐analysis with implications for attributable burden. Lancet 2013;381(Special Issue):S45. [DOI: 10.1016/S0140-6736(13)61299-4] [DOI] [Google Scholar]
- Enns JE, Yeganeh A, Zarychanski R, Abou‐Setta AM, Friesen C, Zahradka P, et al. The impact of omega‐3 polyunsaturated fatty acid supplementation on the incidence of cardiovascular events and complications in peripheral arterial disease: a systematic review and meta‐analysis. BMC Cardiovascular Disorders 2014;14:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food Standards Agency UK. Dioxins and PCBs in the UK diet: 1997 Total diet study samples. Food Surveillance Information Sheet. Number 4/00; 2000. [FSIS 4/00]
- Geelen A, Brouwer IA, Zock PL, Katan MB. Antiarrhythmic effects of n‐3 fatty acids: evidence from human studies. Current Opinion in Lipidology 2004;15:25‐30. [DOI] [PubMed] [Google Scholar]
- GRADE Working Group. Grading quality of evidence and strength of recommendations. British Medical Journal 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMaster University (developed by Evidence Prime, Inc). GRADEpro GDT. Version accessed 30 Sept 2017. Hamilton (ON): McMaster University (developed by Evidence Prime, Inc), 2015.
- Hanson S, Biswas P, Jimoh OF, O'Brien A, Hooper L, Abdelhamid A, et al. Dietary polyunsaturated fat for prevention and treatment of depression and anxiety. PROSPERO 2017;www.crd.york.ac.uk/prospero/display_record.php?RecordID=56092:CRD42017056092. [Google Scholar]
- Hanson S, Thorpe G, Winstanley L, Abdelhamid A, Hooper L. Effects of supplementary dietary polyunsaturated fat on cancer incidence. PROSPERO 2017;www.crd.york.ac.uk/prospero/display_record.php?RecordID=56109:CRD42017056109. [Google Scholar]
- Hauck WW, Gilliss CL, Donner A, Gortner S. Randomisation by cluster. Nursing Research 1991;40(6):356‐8. [PubMed] [Google Scholar]
- He Z, Yang L, Tian J, Yang K, Wu J, Yao Y. Efficacy and safety of omega‐3 fatty acids for the prevention of atrial fibrillation: a meta‐analysis. Canadian Journal of Cardiology 2013;29(2):196‐203. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Sterne JAC, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Hooper L, Martin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database of Systematic Reviews 2015, Issue 6. [DOI: 10.1002/14651858.CD011737] [DOI] [PubMed] [Google Scholar]
- Hooper L, Al‐Khudairy L, Abdelhamid AS, Rees K, Brainard JS, Brown TJ, et al. Omega‐6 fats for the prevention and treatment of cardiovascular disease. Cochrane Database of Systematic Reviews 2018, Issue 6. [DOI: 10.1002/14651858.CD011094.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton R. Expression of concern: Indo‐Mediterranean Diet Heart Study. Lancet 2005;366(9483):354‐6. [DOI: 10.1016/S0140-6736(05)67006-7] [DOI] [PubMed] [Google Scholar]
- Joint FAO/WHO Expert Committee on Food Additives. Summary of the fifty‐seventh meeting of JEFCA, 2001. http://apps.who.int/iris/bitstream/handle/10665/42578/WHO_TRS_909.pdf?sequence=1.
- Jimoh OF, Brainard J, Deane KA, Biswas P, Donaldson D, Hooper L. Dietary polyunsaturated fat for prevention and treatment of neurocognitive disorders. PROSPERO 2017;www.crd.york.ac.uk/prospero/display_record.php?RecordID=19049:CRD42017019049. [Google Scholar]
- Khoueiry G, Abi Rafeh N, Sullivan E, Saiful F, Jaffery Z, Kenigsberg DN, et al. Do omega‐3 polyunsaturated fatty acids reduce risk of sudden cardiac death and ventricular arrhythmias? A meta‐analysis of randomized trials. Heart & Lung 2013;42(4):251‐6. [DOI] [PubMed] [Google Scholar]
- Kotwal S, Jun M, Sullivan D, Perkovic V, Neal B. Omega 3 Fatty acids and cardiovascular outcomes: systematic review and meta‐analysis. Circulation. Cardiovascular Quality & Outcomes 2012;5(6):808‐18. [DOI] [PubMed] [Google Scholar]
- Kris‐Etherton PM, Harris WS, Appel LJ for the Nutrition Committee of the American Heart Association. Fish consumption, fish oil, omega 3 fatty acids, and cardiovascular disease. Circulation 2002;106:2747‐57. [DOI] [PubMed] [Google Scholar]
- Kwak SM, Myung SK, Lee YJ, Seo HG. Efficacy of omega‐3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta‐analysis of randomized, double‐blind, placebo‐controlled trials. Archives of Internal Medicine 2012;172(9):686‐94. [DOI] [PubMed] [Google Scholar]
- Larsson SC, Orsini N, Wolk A. Long‐chain omega‐3 polyunsaturated fatty acids and risk of stroke: a meta‐analysis. European Journal of Epidemiology 2012;27(12):895‐901. [DOI] [PubMed] [Google Scholar]
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Li D, Sinclair A, Wilson A, Nakkote S, Kelly F, Abedin L, et al. Effect of dietary alpha‐linolenic acid on thrombotic risk factors in vegetarian men. American Journal of Clinical Nutrition 1999;69:872‐82. [DOI] [PubMed] [Google Scholar]
- Liem AKD, Theelen RMC. Dioxins: Chemical Analysis, Exposure and Risk Assessment. Utrecht: Universiteit Utrecht, 1997. [ISBN 90 393 2012 8] [Google Scholar]
- MAFF UK. Concentrations of metals and other elements in marine fish and shellfish. Food Surveillance Information Sheet no.151; 1998. [FSIS 151]
- Mariani J, Doval HC, Nul D, Varini S, Grancelli H, Ferrante D, et al. N‐3 polyunsaturated fatty acids to prevent atrial fibrillation: updated systematic review and meta‐analysis of randomized controlled trials. Journal of the American Heart Association 2013;2(1):e005033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nettleton JA. Omega‐3 fatty acids: comparison of plant and seafood sources in human nutrition. Journal of the American Dietetic Association 1991;91:331‐7. [PubMed] [Google Scholar]
- NICE. Cardiovascular disease: risk assessment and reduction, including lipid modification Clinical guideline [CG181]. www.nice.org.uk/guidance/cg181 July 2014, last updated September 2016.
- Papanikolaou Y, Brooks J, Reider C, Fulgoni VL. U.S. adults are not meeting recommended levels for fish and omega‐3 fatty acid intake: results of an analysis using observational data from NHANES 2003–2008. Nutrition Journal 2014;13:31. [DOI: 10.1186/1475-2891-13-31] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlosky RJ, Hibbeln JR, Novotny JA, Salem N Jr. Physiological compartmental analysis of alpha‐linolenic acid metabolism in adult humans. Journal of Lipid Research 2001;42:1257‐65. [PubMed] [Google Scholar]
- Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS. Association between omega‐3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta‐analysis. JAMA 2012;308(10):1024‐33. [DOI] [PubMed] [Google Scholar]
- Savovic J, Jones H, Altman D, Harris R, Jüni P, Pildal J, et al. Influence of reported study design characteristics on intervention effect estimates from randomised controlled trials: combined analysis of meta‐epidemiological studies. Health Technology Assessment 2012;16:1‐82. [DOI] [PubMed] [Google Scholar]
- Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344(8934):1383‐9. [PubMed] [Google Scholar]
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
- Sethi A, Bajaj A, Khosla S, Arora RR. Statin use mitigate the benefit of omega‐3 fatty acids supplementation: a meta‐regression of randomized trials. American Journal of Therapeutics 2016;23(3):e737‐48. [DOI] [PubMed] [Google Scholar]
- Sharp S. Meta‐analysis regression. Stata Technical Bulletin 1998;42:16‐22. [Google Scholar]
- Simopoulos AP, Norman HA, Gillaspy JE, Duke JA. Common purslane: a source of omega‐3 fatty acids and antioxidants. Journal of the American College of Nutrition 1992;11(4):374‐82. [DOI] [PubMed] [Google Scholar]
- Stark KD, Elswyk ME. Higgins R, Weatherford CA, Salem N Jr. Global survey of the omega‐3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Progress in Lipid Research 2016;63:132‐52. [DOI: 10.1016/j.plipres.2016.05.001] [DOI] [PubMed] [Google Scholar]
- Thorpe G, Ajabnoor S, Ahmed Z, Abdelhamid A, Hooper L. Dietary polyunsaturated fat for prevention and treatment of inflammatory bowel disease. PROSPERO 2017;www.crd.york.ac.uk/prospero/display_record.php?RecordID=68704:CRD42017068704. [Google Scholar]
- Trikalinos TA, Moorthy D, Chung M, Yu WW, Lee J, Lichtenstein AH, et al. Concordance of randomized and nonrandomized studies was unrelated to translational patterns of two nutrient‐disease associations. Journal of Clinical Epidemiology 2012;65(1):16‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Food, Drug Administration. What You Need to Know About Mercury in Fish and Shellfish. www.fda.gov/food/foodborneillnesscontaminants/metals/ucm351781.htm(accessed May 2018).
- U. S. Food, Drug Administration. Center for Food Safety and Applied Nutrition, Office of Nutritional Products. Labeling, and Dietary Supplements: Letter Regarding Dietary Supplement Health Claim for Omega‐3 Fatty Acids and Coronary Heart Disease (Docket No. 91N‐0103). www.fda.gov/Food/LabelingNutrition/ucm073992.htm#cardio2004.
- White C. Suspected research fraud: difficulties of getting at the truth. BMJ 2005;331(7511):281‐8. [DOI: 10.1136/bmj.331.7511.281] [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Cardiovascular Diseases (CVDs).. Fact sheets; May 2017. www.who.int/mediacentre/factsheets/fs317/en (accessed 24 November 2017).
- Wood L, Egger M, Gluud LL, Schulz K, Jüni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta‐epidemiological study. BMJ 2008;336:601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. World Bank Country and Lending Groups ‐ country classification. datahelpdesk.worldbank.org/knowledgebase/articles/906519‐world‐bank‐country‐and‐lending‐groups (accessed 3 April 2018).
- Zhao YT, Chen Q, Sun YX, Li XB, Zhang P, Xu Y, et al. Prevention of sudden cardiac death with omega‐3 fatty acids in patients with coronary heart disease: a meta‐analysis of randomized controlled trials. Annals of Medicine 2009;41(4):301‐10. [DOI] [PubMed] [Google Scholar]
- Zheng T, Zhao J, Wang Y, Liu W, Wang Z, Shang Y, et al. The limited effect of omega‐3 polyunsaturated fatty acids on cardiovascular risk in patients with impaired glucose metabolism: a meta‐analysis. Clinical Biochemistry 2014;47(6):369‐77. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Hooper L, Harrison RA, Summerbell CD, Moore H, Worthington HV, Ness A, et al. Omega 3 fatty acids for prevention and treatment of cardiovascular disease. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD003177.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper L, Thompson RL, Harrison RA, Summerbell CD, Ness AR, Moore HJ, et al. Risks and benefits of omega 3 fats for mortality, cardiovascular disease, and cancer: systematic review. BMJ 2006;322:752. [DOI: 10.1136/bmj.38755.366331.2F] [DOI] [PMC free article] [PubMed] [Google Scholar]


