Abstract
Background
Caesarean section rates are increasing globally. The factors contributing to this increase are complex, and identifying interventions to address them is challenging. Non‐clinical interventions are applied independently of a clinical encounter between a health provider and a patient. Such interventions may target women, health professionals or organisations. They address the determinants of caesarean births and could have a role in reducing unnecessary caesarean sections. This review was first published in 2011. This review update will inform a new WHO guideline, and the scope of the update was informed by WHO’s Guideline Development Group for this guideline.
Objectives
To evaluate the effectiveness and safety of non‐clinical interventions intended to reduce unnecessary caesarean section.
Search methods
We searched CENTRAL, MEDLINE, Embase, CINAHL and two trials registers in March 2018. We also searched websites of relevant organisations and reference lists of related reviews.
Selection criteria
Randomised trials, non‐randomised trials, controlled before‐after studies, interrupted time series studies and repeated measures studies were eligible for inclusion. The primary outcome measures were: caesarean section, spontaneous vaginal birth and instrumental birth.
Data collection and analysis
We followed standard methodological procedures recommended by Cochrane. We narratively described results of individual studies (drawing summarised evidence from single studies assessing distinct interventions).
Main results
We included 29 studies in this review (19 randomised trials, 1 controlled before‐after study and 9 interrupted time series studies). Most of the studies (20 studies) were conducted in high‐income countries and none took place in low‐income countries. The studies enrolled a mixed population of pregnant women, including nulliparous women, multiparous women, women with a fear of childbirth, women with high levels of anxiety and women having undergone a previous caesarean section.
Overall, we found low‐, moderate‐ or high‐certainty evidence that the following interventions have a beneficial effect on at least one primary outcome measure and no moderate‐ or high‐certainty evidence of adverse effects.
Interventions targeted at women or families
Childbirth training workshops for mothers alone may reduce caesarean section (risk ratio (RR) 0.55, 95% confidence interval (CI) 0.33 to 0.89) and may increase spontaneous vaginal birth (RR 2.25, 95% CI 1.16 to 4.36). Childbirth training workshops for couples may reduce caesarean section (RR 0.59, 95% CI 0.37 to 0.94) and may increase spontaneous vaginal birth (RR 2.13, 95% CI 1.09 to 4.16). We judged this one study with 60 participants to have low‐certainty evidence for the outcomes above.
Nurse‐led applied relaxation training programmes (RR 0.22, 95% CI 0.11 to 0.43; 104 participants, low‐certainty evidence) and psychosocial couple‐based prevention programmes (RR 0.53, 95% CI 0.32 to 0.90; 147 participants, low‐certainty evidence) may reduce caesarean section. Psychoeducation may increase spontaneous vaginal birth (RR 1.33, 95% CI 1.11 to 1.61; 371 participants, low‐certainty evidence). The control group received routine maternity care in all studies.
There were insufficient data on the effect of the four interventions on maternal and neonatal mortality or morbidity.
Interventions targeted at healthcare professionals
Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication slightly reduces the risk of overall caesarean section (mean difference in rate change ‐1.9%, 95% CI ‐3.8 to ‐0.1; 149,223 participants). Implementation of clinical practice guidelines combined with audit and feedback also slightly reduces the risk of caesarean section (risk difference (RD) ‐1.8%, 95% CI ‐3.8 to ‐0.2; 105,351 participants). Physician education by local opinion leader (obstetrician‐gynaecologist) reduced the risk of elective caesarean section to 53.7% from 66.8% (opinion leader education: 53.7%, 95% CI 46.5 to 61.0%; control: 66.8%, 95% CI 61.7 to 72.0%; 2496 participants). Healthcare professionals in the control groups received routine care in the studies. There was little or no difference in maternal and neonatal mortality or morbidity between study groups. We judged the certainty of evidence to be high.
Interventions targeted at healthcare organisations or facilities
Collaborative midwifery‐labourist care (in which the obstetrician provides in‐house labour and delivery coverage, 24 hours a day, without competing clinical duties), versus a private practice model of care, may reduce the primary caesarean section rate. In one interrupted time series study, the caesarean section rate decreased by 7% in the year after the intervention, and by 1.7% per year thereafter (1722 participants); the vaginal birth rate after caesarean section increased from 13.3% before to 22.4% after the intervention (684 participants). Maternal and neonatal mortality were not reported. We judged the certainty of evidence to be low.
We studied the following interventions, and they either made little or no difference to caesarean section rates or had uncertain effects.
Moderate‐certainty evidence suggests little or no difference in caesarean section rates between usual care and: antenatal education programmes for physiologic childbirth; antenatal education on natural childbirth preparation with training in breathing and relaxation techniques; computer‐based decision aids; individualised prenatal education and support programmes (versus written information in pamphlet).
Low‐certainty evidence suggests little or no difference in caesarean section rates between usual care and: psychoeducation; pelvic floor muscle training exercises with telephone follow‐up (versus pelvic floor muscle training without telephone follow‐up); intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy); education of public health nurses on childbirth classes; role play (versus standard education using lectures); interactive decision aids (versus educational brochures); labourist model of obstetric care (versus traditional model of obstetric care).
We are very uncertain as to the effect of other interventions identified on caesarean section rates as the certainty of the evidence is very low.
Authors' conclusions
We evaluated a wide range of non‐clinical interventions to reduce unnecessary caesarean section, mostly in high‐income settings. Few interventions with moderate‐ or high‐certainty evidence, mainly targeting healthcare professionals (implementation of guidelines combined with mandatory second opinion, implementation of guidelines combined with audit and feedback, physician education by local opinion leader) have been shown to safely reduce caesarean section rates. There are uncertainties in existing evidence related to very‐low or low‐certainty evidence, applicability of interventions and lack of studies, particularly around interventions targeted at women or families and healthcare organisations or facilities.
Plain language summary
Non‐clinical interventions for reducing unnecessary caesarean section
What is the aim of this review?
The aim of this Cochrane Review was to find out whether non‐clinical interventions, which aim to reduce unnecessary caesarean sections, such as providing education to healthcare workers and mothers, are safe and effective. This review was first published in 2011. This review update will inform a new WHO guideline, and the scope of the update was informed by WHO’s Guideline Development Group for this guideline.
Key messages
We studied a wide range of non‐clinical interventions that aim to reduce unnecessary caesarean sections, mostly in high‐income countries. Based on high‐quality evidence, few interventions have been shown to reduce caesarean section rates without adverse effects on maternal or neonatal outcomes. These interventions are mainly aimed at healthcare professionals (nurses, midwives, physicians) and involve using: clinical guidelines combined with mandatory second opinion for caesarean section indication; clinical guidelines combined with audit and feedback about caesarean section practices; and opinion leaders (obstetrician/gynaecologist) to provide education to healthcare professionals.
What was studied in this review?
Caesarean section is an operation used to prevent and reduce complications of childbirth. While it can be a life‐saving procedure for both the mother and baby, caesarean section is not without harm and should only be carried out when necessary. Caesarean sections increase the likelihood of bleeding, maternal infections and infant breathing problems, among other complications. The number of caesarean sections performed has been increasing worldwide. Whilst there may be medical reasons for this increase, other factors, such as clinician convenience and maternal fears, may also be responsible.
What are the main results of the review?
We included 29 studies in this review. Most of the studies (20 studies) were conducted in high‐income countries; none in low‐income countries.
We rated the quality of the evidence from studies using four levels: very low, low, moderate, or high. Very low‐quality means that we are very uncertain about the results. High‐quality evidence means that we are very confident in the results.
Overall, we found eight of the 29 interventions included in the review to have a beneficial effect on at least one of our main outcomes with low‐, moderate‐ or high‐quality evidence, and no moderate‐ or high‐quality evidence of harm:
Interventions aimed at women or families: providing childbirth training workshops for mothers and couples; relaxation training programmes led by nurses; psychosocial couple‐based prevention programmes; and psychoeducation. The interventions were compared to routine practice. The quality of evidence from the studies was low.
Interventions aimed at healthcare professionals: using clinical guidelines combined with mandatory second opinion for caesarean section indication; using clinical guidelines combined with audit and feedback about caesarean section practices; and having opinion leaders (obstetrician/gynaecologist) provide education to healthcare professionals. The interventions were compared to routine practice. The quality of evidence was high.
Interventions aimed at healthcare organisations or facilities: collaborative midwifery‐labourist model of care (in which the obstetrician provides in‐house labour and delivery coverage, 24 hours a day, without competing clinical duties) compared to a private model of care. The quality of evidence was low.
We studied a number of other interventions and they either made little or no difference to caesarean section rates, or had uncertain effects.
Limited data were available on possible harms associated with the interventions examined in this review.
How up‐to‐date is this review?
The evidence is current to March 2018.
Summary of findings
Background
This is the first update of the original review (Khunpradit 2011).
Description of the condition
Caesarean section is an intervention to reduce complications associated with childbirth. While it can be a life‐saving procedure for both the mother and the baby, there is no evidence showing the benefits of caesarean delivery for women or babies who do not require the procedure. As with any surgery, caesarean sections are associated with short‐ and long‐term risks which can extend many years beyond the current delivery and affect the health of the woman, baby and future pregnancies. Maternal risks include infections, haemorrhage, other organ injury, and complications related to use of anaesthesia or blood transfusion (Cook 2013; Marshall 2011). There is also a higher risk of complications in subsequent pregnancies, such as uterine rupture, placental implantation problems and need for hysterectomy (Keag 2018; Timor‐Tritsch 2012). Infant risks include respiratory problems, asthma and obesity in childhood (Keag 2018).
Given the balance of risks and benefits, national clinical societies recommend that in the absence of maternal or foetal indications for caesarean section, a plan for vaginal delivery is safe and recommended (ACOG 2013). The National Institute for Health and Care Excellence (NICE) in its 2013 evidence update "recommends that if a woman requests a CS [caesarean section] when there is no other indication; discuss the overall risks and benefits of CS compared with vaginal birth. If necessary, a discussion should be held with other members of the obstetric team (including the obstetrician, midwife and anaesthetist) if necessary to explore the reasons for the request, and ensure the woman has accurate information. If after discussion and offer of support (including perinatal mental health support for women with anxiety about childbirth), a vaginal birth is still not an acceptable option, offer a planned CS." (NICE 2013).
Worldwide, reported caesarean section rates vary widely, especially between high‐ and low‐income countries. However, the rise in caesarean section rates is a global phenomenon. From 1990 to 2014, the global average caesarean section rate increased three‐fold from 6.7% to 19.1%, with an average rate increase of 4.4% per year. On average, caesarean section rates increased from 22.8% to 42.2% in Latin American and the Caribbean, 18.5% to 32.6% in Oceania, 22.3% to 32.3% in North America, 11.2% to 25% in Europe, 4.4% to 19.5% in Asia, and 2.9% to 7.4% in Africa (Betrán 2016a).
In 1985, the World Health Organization (WHO) issued a consensus statement suggesting there were unlikely to be any additional health benefits associated with caesarean section rates above 10% to 15% (WHO 1985). More recently in 2015, the WHO published the results of a systematic review of population‐based studies to help determine an ideal caesarean section rate at a population level (Betrán 2016b). Based on this review, the WHO found that while caesarean sections are effective in saving maternal and infant lives and should be provided for medically indicated reasons, caesarean rates greater than 10% at a population level are not associated with reductions in maternal and newborn mortality. The result of this systematic review was confirmed by a complementary global longitudinal ecological study (Ye 2015).
The factors affecting the rate of caesarean section births are complex, and identifying interventions to reduce this rate is challenging. The decision to perform a caesarean section may be made before conception, earlier in pregnancy or during a perinatal emergency. The decision may be made by a doctor or the mother, and may be affected by a range of other factors. Factors independently associated with caesarean births include: maternal age, body weight (NCC‐WCH 2011), women increasingly wanting to determine how and when their child is born (Lo 2003), cultural beliefs about the birthing process that make caesarean sections more or less attractive (Hsu 2008), beliefs about the impact of caesarean section (Dweik 2014), primiparity (Pang 2008), generational shifts in work and family responsibilities (Scioscia 2008), physician and organisational factors (Hoxha 2017; Ji 2015; Lin 2004; Luthy 2003; Mi 2014; Thomas 2001; Zwecker 2011). Indeed, some have argued that simple policy options are unlikely to effectively address the many different factors involved (Scioscia 2008), and that multicomponent interventions that address a range of determinants are desired.
Description of the intervention
Clinical interventions that could help to reduce caesarean section rates have been assessed in a number of systematic reviews and include: active management in labour (Brown 2013; Catling‐Paull 2011b; Hartmann 2012), use of a partogram with a four‐hour action line in labour, foetal blood sampling before caesarean section for abnormal cardiotocograph in labour, and support for women who choose vaginal birth after caesarean section (NICE 2013), improved and standardised foetal heart rate interpretation and management, external cephalic version for breech presentation after 36 weeks (NICE 2013), and a trial of labour for women with twin gestations when the first twin is in cephalic presentation (ACOG SMFM 2014). These are clinical decisions and are not included in this review.
This review examines non‐clinical interventions (i.e. interventions applied independent of a clinical encounter between a healthcare provider and a patient in the context of patient care) to reduce unnecessary caesarean section rates (i.e. those performed in the absence of medical indications (Kabir 2004; Koroukian 1998)). These interventions may target women (e.g. birth preparation classes), healthcare professionals (e.g. implementation of clinical practice guidelines) or healthcare organisations (e.g. different payment systems for caesarean section) (Table 5).
1. Classification of non‐clinical interventions.
| Intervention | Examples of interventions |
| Interventions targeted at women, the community, or the general public | |
|
|
|
Dissemination of information or advocacy with support or campaigns from local or international opinion leaders
|
|
|
| Interventions targeted at healthcare professionals | |
|
|
|
|
|
|
| Interventions targeted at healthcare organisations or facilities | |
|
Different types of nurse/midwife staffing models
Different types of physician staffing models
|
|
|
|
|
|
|
|
|
|
|
AML: active management of labour; ANC: antenatal care; CS: caesarean section; VBAC: vaginal birth after caesarean; VD: vaginal delivery; TOLAC: trial of labour after caesarean
How the intervention might work
The different interventions intended to reduce caesarean section births might work by addressing determinants of caesarean births. Table 6 shows examples of interventions targeting healthcare recipients, healthcare professionals, or healthcare organisations that contribute to increasing caesarean section rates.
2. Examples of determinants of caesarean section births and interventions targeted at the determinants.
| Level | Determinants | Interventions |
| Healthcare recipients (women, families) |
|
|
|
|
|
| Healthcare professionals |
|
|
|
|
|
| Healthcare organisations or facilities |
|
|
|
|
|
|
|
CS: caesarean section; VD: vaginal delivery
Why it is important to do this review
A reliable synthesis of the evidence will help determine the effectiveness and safety of existing interventions that aim to reduce unnecessary caesarean sections, and help decision makers select the most appropriate interventions to implement. In 2011, we found evidence from 16 studies that non‐clinical interventions may have a role in reducing unnecessary caesarean sections (Khunpradit 2011). As the prevention of unnecessary caesarean sections continues to be a global priority and the body of evidence continues to increase, an update of this review is warranted to provide up‐to‐date evidence to guide policy and practice decisions to reduce caesarean births. This review update will inform a new WHO guideline, and the scope of the update was informed by WHO’s Guideline Development Group for this guideline.
Objectives
To determine the effectiveness and safety of non‐clinical interventions intended to reduce unnecessary caesarean section.
Methods
Criteria for considering studies for this review
Types of studies
The following studies were eligible for inclusion (EPOC 2017).
Randomised trials.
Non‐randomised trials.
Controlled before‐after studies (with at least two intervention sites and two control sites).
Interrupted time series studies (where the time of intervention is clearly defined and there are at least three data points before and three after the intervention).
Repeated measures studies (an interrupted time series study where measurements are made in the same individuals at each time point).
Types of participants
Studies involving the following groups of participants were eligible for inclusion.
Pregnant women seeking maternity care during pregnancy, labour and delivery.
Families of pregnant women.
Healthcare providers who work with pregnant women (nurses, midwives, physicians).
Healthcare facilities that provide maternity care to pregnant women.
Communities and advocacy groups involved in maternity care.
Types of interventions
Studies involving the following interventions were eligible for inclusion (Table 5).
Interventions targeted at women, the community or the general public (e.g. birth preparation classes).
Interventions targeted at healthcare professionals (e.g. implementation of clinical practice guidelines).
Interventions targeted at healthcare organisations or facilities (e.g. different payment systems for caesarean section).
We compared the interventions above to the following.
No intervention.
Usual care or practice in accordance with local protocols.
Another intervention, as reported in the studies.
In order to avoid duplication, we have not included other related interventions addressed in related reviews: midwife‐led continuity of care (Sandall 2016); continuous labour support (Bohren 2017); physical activity‐based interventions (i‐WIP 2017); alternative institutional birth environment (Hodnett 2012); and planned hospital birth versus planned home birth (Olsen 2012). Furthermore, we only included non‐clinical interventions specifically designed to reduce caesarean section rates. Interventions not specifically designed to reduce caesarean section rates are not included, even if they may incidentally reduce caesarean section rates.
As noted above, this review update will inform a new WHO guideline, and the scope of the update was informed by WHO’s Guideline Development Group for this guideline.
Types of outcome measures
Primary outcomes
Caesarean section
Spontaneous vaginal birth
Instrumental vaginal birth
Secondary outcomes
Maternal mortality and morbidity
Neonatal mortality and morbidity
Maternal birth experience
Healthcare resource utilisation
Details of the outcome measures are summarised in Table 7. We excluded studies that only reported secondary outcomes without data on primary outcomes.
3. Primary and secondary outcome measures.
|
Maternal mortality and morbidity 1. Maternal death 2. Maternal morbidity Perineal or vaginal trauma
Maternal morbidity
Serious maternal morbidity
Long‐term maternal outcomes
Neonatal mortality and morbidity 1. Neonatal death 2. Neonatal morbidity Birth trauma
Perinatal asphyxia
Long‐term infant outcomes
|
Search methods for identification of studies
Electronic searches
We searched the following databases (Appendix 1):
The Cochrane Pregnancy and Childbirth Group specialised register (March 2010 to August 2014) (searched August 2014)
Cochrane Central Register of Controlled Trials (CENTRAL;2018, Issue 2) in the Cochrane Library (searched 8 March 2018)
MEDLINE Ovid (including Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Versions) (to 7 March 2018) (searched 8 March 2018)
EMBASE Ovid (to 7 March 2018) (searched 8 March 2018)
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; to 8 March 2018) (searched 8 March 2018)
Search strategies are comprised of keywords and controlled vocabulary terms. We applied no language limits. Searches for this update aimed to retrieve material published since 2010; the date of the searches in the previous version of the review. The search terms were revised to increase specificity by analysing the titles, abstracts and MEDLINE index terms of the included studies from the previous version of the review using various text analysis tools (TerMine; Voyant Tools; Yale MeSH Analyzer).
Prior to the above, we ran updated searches in August 2014 (Appendix 2) and February 2017 (Appendix 3). The February 2017 searches were supplementary searches run in MEDLINE and Embase for interventions relating to environmental modifications (i.e. physical or sensory environment of labour or delivery room), organisational goals (i.e. setting predetermined caesarean section rates) and organisational change (i.e. strategies to change organisational culture).
Searching other resources
Grey literature
Since the Cochrane Pregnancy and Childbirth Group Specialised Register includes extensive handsearching of journals and conference proceedings, we did not perform additional handsearching of journals or conference proceedings. We searched reference lists of trials and related reviews, websites of relevant organisations, and contacted authors for additional articles.
Trials registries
We searched the following two clinical trials registries for ongoing trials or completed trials that have not been published on 8 March 2018:
International Clinical Trials Registry Platform (ICTRP), Word Health Organization (WHO) (www.who.int/ictrp/en/).
ClinicalTrials.gov, US National Institutes of Health (NIH) (clinicaltrials.gov/).
Data collection and analysis
Selection of studies
We entered the identified records into Covidence after removing duplicates (www.covidence.org). Seven review authors, working in pairs, independently screened titles, abstracts and full texts of identified records and selected studies meeting review inclusion criteria. We resolved disagreements by discussion.
Data extraction and management
Five review authors, working in pairs, independently extracted data on the following aspects from the included studies. We entered data into a pilot‐tested data extraction form. We resolved disagreements by discussion.
Study design and unit of allocation.
Study setting (e.g. community, hospital, single or multicentre).
Participants (e.g. parity, gestational age).
Intervention and control (e.g. duration and frequency of training).
Outcome measures (e.g. caesarean section).
Assessment of risk of bias in included studies
Five review authors, working in pairs, independently assessed study risk of bias using the Cochrane EPOC 'Risk of bias' criteria for randomised trials, non‐randomised trials, controlled before‐after studies and interrupted time series studies (EPOC 2017). We classified findings into three categories: low ‐ low risk of bias for key quality domains; high ‐ high risk of bias for one or more of the key domains; or unclear ‐ unclear risk of bias for one or more of the key domains. We resolved disagreements by discussion.
Measures of treatment effect
For dichotomous outcomes, we assessed the effect of interventions using risk ratios (RRs), odds ratios (ORs) or risk differences (RDs). We used the mean difference (MD) measure for continuous outcomes. For interrupted time series studies, we used two effect sizes to measure the intervention effect: change in level (also called 'step change') and change in trend (also called 'change in slope') before and after the intervention (Bernal 2017). Change in level is the difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; change in trend is the difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in the event. Where these effect measures were not estimable (e.g. owing to insufficient data), we reported results in natural units as reported in the studies.
Unit of analysis issues
We checked whether appropriate analysis was conducted to adjust for clustering in cluster‐randomised trials. If there was a unit of analysis error and reanalysis was not possible, we reported only the point estimate without a measure of variance (such as confidence intervals (CIs)).
Three of the included studies had three arms and therefore contributed multiple comparisons (Lomas 1991; Montgomery 2007; Valiani 2014). A unit of analysis error did not arise from these studies as we did not pool effect estimates from the studies.
Dealing with missing data
We contacted authors of included studies where needed data were missing, or where we required further clarification on the reported data. Where data were not available from the authors, we reported the data as missing and analysed only the available data. We did not impute or extrapolate values for missing data.
Assessment of heterogeneity
We did not conduct statistical tests for heterogeneity (differences in study designs and interventions precluded meta‐analysis).
Assessment of reporting biases
We assessed potential reporting bias due to selective outcome reporting as one component of 'Risk of bias' assessment. In addition, we checked whether prespecified outcomes were reported, based on the information provided in trials registry records or protocols, where these were available.
Data synthesis
We grouped interventions into four categories and prepared evidence tables for each category.
Interventions targeted at women or families (Table 8; Table 9).
Interventions targeted at healthcare professionals (Table 10; Table 11).
Interventions targeted at healthcare organisations or facilities (Table 12; Table 13).
'Cross‐cutting' interventions (i.e. multifaceted interventions with components targeted at women, healthcare professionals or healthcare organisations) (Table 14; Table 15).
4. Interventions targeted at women or families.
| Study | Intervention | Details |
| Bastani 2006 | Nurse‐led applied relaxation training programme |
|
| Bergstrom 2009 | Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques |
|
| Eden 2014 | Computerised decision aid versus educational brochures |
Computerised decision aid
Educational brochures
|
| Feinberg 2015 | Psychosocial couple‐based prevention programme |
|
| Fenwick 2015 | Psychoeducation by telephone |
|
| Fraser 1997 | Individualised prenatal education and support programme versus written information in pamphlet |
Prenatal education and support programme
First contact, duration (minutes ± SD): stratum 1 (low motivation), 57 ± 20; stratum 2 (high motivation): 54 ± 20; second contact, duration (minutes ± SD): stratum 1: 54 ± 22, stratum 2: 54 ± 20. Pamphlet group
|
| Masoumi 2016 | Antenatal education programme for physiologic childbirth (birth preparation training) |
|
| Montgomery 2007 | Computer decision aids versus usual care |
Two computer‐based interventions delivered using a laptop computer, usually in the women's own home.
Usual care: this comprised the usual level of care given by the obstetric and midwifery team. Women in the two intervention groups also received usual care. |
| Navaee 2015 | Role play education versus standard education using lectures |
Role‐playing group
Standard education (lecture group)
|
| Rouhe 2013 | Psychoeducation |
|
| Saisto 2001 | Intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy) |
|
| Sharifirad 2013 | Prenatal education for husbands |
|
| Shorten 2005 | Decision‐aid booklet |
|
| Valiani 2014 | Childbirth training workshop |
|
| Wang 2014 | PFMT with telephone follow‐up |
|
ACOG: American College of Obstetricians and Gynecologists; CS: caesarean section; PFMT: pelvic floor muscle training; SD: standard deviation; VBAC: vaginal birth after caesarean
5. Effects of interventions targeted at women or families.
| Study | Quality assessment | Outcome | Intervention | Control | Effect (95% CI) or P value |
Certainty (GRADE)* |
|||||
| Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | ||||||
| Bastani 2006 | RT | Seriousa | Single study | Not serious | Seriousb | None | CS | 8/52 (15.4%) | 21/52 (40.4%) | RR 0.22 (0.11 to 0.43) |
㊉㊉㊀㊀ LOWa,b |
| Instrumental delivery (forceps and vacuum extraction) | 11/52 (21.2%) | 25/52 (48.1%) | RR 0.44 (0.24 to 0.80) | ||||||||
| Bergstrom 2009 | RT | Not serious | Single study | Not serious | Seriousc | None | Elective CS | 29/484 (6.0%) | 31/493 (6.3%) | RR 0.95 (0.58 to 1.56) |
㊉㊉㊉㊀ MODERATEc |
| Emergency CS | 67/484 (13.8%) | 75/493 (15.2%) | RR 0.91 (0.67 to 1.23) | ||||||||
| SVD | 321/484 (66.3%) | 327/493 (66.3%) | RR 1.00 (0.91 to 1.09) | ||||||||
| Instrumental delivery | 67/484 (13.8%) | 60/493 (12.2%) | RR 1.14 (0.82 to 1.57) | ||||||||
| Experience of childbirth (W‐DEQ B): mean (SD) | 49.6 ± 26 (number of participants unclear) |
50.1 ± 25 (number of participants unclear) |
MD ‐0.5 (‐3.2 to 4.1) | ||||||||
| Eden 2014 | RT | Seriousa | Single study | Not serious | Seriousb | None | Decisional conflict (overall, women in third trimester) | Mean score: Baseline: 19.4 (12.7 to 26.1) Follow‐up: 10.7 (5.6 to 15.9) n = 35 |
Mean score: Baseline: 16.5 (9.5 to 23.5) Follow‐up: 14.1 (8.7 to 19.4) n = 32 |
MD: ‐0.32, P = 0.003 |
㊉㊉㊀㊀ LOWa,b |
| VBAC | 41% (number of events/participants unclear) | 37% (number of events/participants unclear) | P = 0.72 | ||||||||
| Feinberg 2015 | RT | Seriousa | Single study | Not serious | Seriousb | None | CS | 21% (n = 76) (number of events unclear) |
40% (n = 71) (number of events unclear) |
OR 0.36 (0.15 to 0.86) |
㊉㊉㊀㊀ LOWa,b |
| Maternity length of stay (days) (mean, SD) | 3.11 ± 2.09 (n = 76) | 3.36 ± 2.50 (n = 71) | MD ‐0.25 (‐1.00 to 0.50) | ||||||||
| Newborn length of stay (days) (mean, SD) | 2.67 ± 1.04 (n = 76) | 2.89 ± 1.17 (n = 71) | MD ‐0.22 (‐0.58 to 0.14) | ||||||||
| Fenwick 2015 | RT | Seriousa | Single study | Seriousd | Seriousb | None | Overall CS | 31/91 (34.1%) | 39/93 (41.9%) | RR 0.81 (0.56 to 1.18) |
㊉㊀㊀㊀ VERY LOWa,b,c |
| Emergency CS | 16/91 (17.6%) | 23/91 (24.7%) | RR 0.70 (0.39 to 1.23) | ||||||||
| SVD | 44/91 (48.4%) | 39/93 (41.9%) | RR 1.15 (0.84 to 1.59) | ||||||||
| Forceps and vacuum delivery | 16/91 (17.6%) | 15/93 (16.1%) | RR 1.09 (0.57 to 2.07) | ||||||||
| Nursery admission | 16/91 (17.6%) | 18/91 (19.4%) | RR 0.89 (0.48 to 1.63) | ||||||||
| Maternal readmission | 3/91 (3.3%) | 5/91 (5.4%) | RR 0.60 (0.15 to 2.44) | ||||||||
| Baby readmission | 8/91 (8.8%) | 6/91 (6.5%) | RR 1.33 (0.48 to 3.69) | ||||||||
| Breastfeeding at 6 months | 76/91 (83.5%) | 73/91 (78.5%) | RR 1.04 (0.91 to 1.19) | ||||||||
| Satisfaction with mode of birth | 53/91 (58.2%) | 61/91 (65.6%) | RR 0.87 (0.69 to 1.09) | ||||||||
| Fraser 1997 | RT | Not serious | Single study | Not serious | Seriousb | None | Overall CS | 302/641 (47.1%) | 324/634 (51.1%) | RR 0.92 (0.82 to 1.03) |
㊉㊉㊉㊀ MODERATEb |
| Scheduled CS | 137/641 (21.4%) | 150/634 (23.7%) | RR 0.90 (0.74 to 1.11) | ||||||||
| Urgent CS | 39/641 (6.1%) | 44/634 (6.9%) | RR 0.88 (0.58 to 1.33) | ||||||||
| VBAC | 339/641 (53%) | 310/634 (49%) | RR 1.08 (0.97 to 1.21) | ||||||||
| Birth experience | Mean score, SD: 75.2 ± 20.7 | Mean score, SD: 74.2 ± 21.8 | P = 0.59 | ||||||||
| Maternal morbidity and neonatal outcomes | Rates of maternal morbidity and neonatal outcomes were similar in the study groups (maternal–uterine rupture or dehiscence, hysterectomy, blood transfusion; neonatal–perinatal deaths, Apgar score less than 7 at 5 minutes, admission to NICU) | ||||||||||
| Masoumi 2016 | RT | Not serious | Single study | Not serious | Seriousb | None | CS | 33/75 (44%) | 32/75 (43.7%) | RR 1.03 (0.72 to 1.49) |
㊉㊉㊉㊀ MODERATEb |
| Physiologic birth | 6/75 (8%) | 0/75 (0%) | Not estimable | ||||||||
| Normal vaginal birth | 36/75 (48%) | 43/75 (57%) | RR 0.84 (0.62 to 1.14) | ||||||||
| Montgomery 2007 | RT | Not serious | Single study | Not serious | Seriousc | None | Information group versus usual care group: elective CS | 117/240 (48.8%) | 118/238 (49.6%) | RR 0.98 (0.82 to 1.18) |
㊉㊉㊉㊀ MODERATEc |
| Decision analysis group versus usual care group: elective CS | 97/235 (41.3%) | 118/238 (49.6%) | RR 0.83 (0.68 to 1.02) | ||||||||
| Information group versus usual care group: emergency CS | 53/240 (22.1%) | 48/238 (20.2%) | RR 1.09 (0.77 to 1.55) | ||||||||
| Decision analysis group versus usual care group: emergency CS | 50/235 (21.3%) | 48/238 (20.2%) | RR 1.05 (0.74 to 1.50) | ||||||||
| Decision analysis versus usual care group: vaginal birth | 88/235 (37.5%) | 72/238 (30.3%) | RR 1.24 (0.96 to 1.60) | ||||||||
| Information group versus usual care group: vaginal birth | 70/240 (29.2%) | 72/238 (30.3%) | RR 0.96 (0.73 to 1.27) | ||||||||
| Navaee 2015 | RT | Seriousa | Single study | Not serious | Seriousb | None | CS | 13/35 (37.1%) | 18/32 (56.2%) | RR 0.66 (0.39 to 1.12) |
㊉㊉㊀㊀ LOWa,b |
| Rouhe 2013 | RT | Seriousa | Single study | Not serious | Seriousb | None | Overall CS | 30/131 (22.9%) | 78/240 (32.5%) | RR 0.70 (0.49 to 1.01) |
㊉㊉㊀㊀ LOWa,b |
| Elective CS | 14/131 (10.1%) | 31/240 (12.9%) | RR 0.83 (0.46 to 1.50) | ||||||||
| Emergency CS | 16/131 (12.2%) | 47/240 (19.6%) | RR 0.62 (0.37 to 1.06) | ||||||||
| SVD | 83/131 (63.4%) | 114/240 (47.5%) | RR 1.33 (1.11 to 1.61) | ||||||||
| Positive delivery experience, >75th percentile of the DSS | 30/77 (36.1%) | 31/124 (22.8%) | RR 1.56 (1.03 to 2.36) | ||||||||
| Saisto 2001 | RT | Seriousa | Single study | Not serious | Seriousb | None | CS | 37/85 (43.5%) | 44/91 (48.4%) | RR 0.90 (0.65 to 1.24) |
㊉㊉㊀㊀ LOWa,b |
| CS for psychosocial reasons | 20/85 (23.5%) | 26/91 (28.6%) | RR 0.82 (0.50 to 1.36) | ||||||||
| Satisfaction with childbirth (scale: from 1 to 5) |
Mean score, SD: 3.7 ± 1.4 | Mean score, SD: 4.0 ± 1.3 | NS | ||||||||
| Sharifirad 2013 | RT | Seriousa | Single study | Seriousd | Seriousb | None | CS | 29.5% (n = 44) (number of events unclear) |
50.0% (n = 44) (number of events unclear) |
P < 0.05 |
㊉㊀㊀㊀ VERY LOWa,b,c |
| Shorten 2005 | RT | Not serious | Single study | Not serious | Seriousb | None | Elective repeat CS | Baseline: 29.6% Follow‐up: 52.2% (n = 115) |
Baseline: 23.2% Follow‐up: 49.4% (n = 112) |
Absolute change from baseline: 26.2% versus 22.6% Difference in absolute change from baseline: ‐3.6% (NS) |
㊉㊉㊉㊀ MODERATEb |
| Decisional conflict scores | Baseline: 2.34 Follow‐up: 1.94 Change in score: ‐0.40 (‐0.51 to ‐0.29); n = 99 |
Baseline: 2.26 Follow‐up: 2.18 Change in score: ‐0.08 (‐0.22 to 0.06); n = 88 |
P < 0.05 | ||||||||
| Satisfaction with birth experience (scale: 1 to 10) | Mean satisfaction rating: 7.70 | Mean satisfaction rating: 7.90 | NS | ||||||||
| Valiani 2014 | RT | Seriousa | Single study | Not serious | Seriousb | None | Mothers alone versus control: CS | 12/30 (40%) | 22/30 (73.3%) | RR 0.55 (0.33 to 0.89) |
㊉㊉㊀㊀ LOWa,b |
| Couple versus control: CS | 13/30 (43.3%) | 22/30 (73.3%) | RR 0.59 (0.37 to 0.94) | ||||||||
| Mothers alone versus control: vaginal delivery | 18/30 (60%) | 8/30 (26.7%) | RR 2.25 (1.16 to 4.36) | ||||||||
| Couple versus control: vaginal delivery | 17/30 (56.7%) | 8/30 (26.7%) | RR 2.13 (1.09 to 4.16) | ||||||||
| Wang 2014 | RT | Seriousa | Single study | Not serious | Seriousb | None | Overall CS | 16/35 (31.4%) | 27/55 (49.1%) | RR 0.87 (0.37 to 2.04) |
㊉㊉㊀㊀ LOWa,b |
| Episiotomy | 47.1% (number of events/participants unclear) | 47.3% (number of events/participants unclear) | P = 0.35 | ||||||||
| Perineal laceration | 7.8% (number of events/participants unclear) | 3.6% (number of events/participants unclear) | P = 0.98 | ||||||||
| Couple versus control: CS | 13/30 (43.3%) | 22/30 (73.3%) | RR 0.59 (0.37 to 0.94) | ||||||||
| Mothers alone versus control: vaginal delivery | 18/30 (60%) | 8/30 (26.7%) | RR 2.25 (1.16 to 4.36) | ||||||||
| Couple versus control: vaginal delivery | 17/30 (56.7%) | 8/30 (26.7%) | RR 2.13 (1.09 to 4.16) | ||||||||
| About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as 'quality of evidence' or 'confidence in the estimate' †Substantially different = a large enough difference that it might affect a decision | |||||||||||
| DSS: delivery satisfaction scale; MD: mean difference; NICU: neonatal intensive care unit; NS: not significant; OR: odds ratio; RR: risk ratio; RT: randomised trial; SD: standard deviation; SVD: spontaneous vaginal delivery; VBAC: vaginal birth after cesarean; W‐DEQ B Wijma Delivery Expectancy/Experience Questionnaire–Version B. aDowngraded one level for serious risk of bias (due to flaws in randomisation procedures). bDowngraded one level for serious imprecision (due to small sample size and few events). cDowngraded one level due to serious imprecision (95% CI includes appreciable benefit and harm). dDowngraded one level for serious indirectness (follow‐up analyses, not described in the trial report, indicated that the impact on caesarean sections was due to reduced birth complications arising from fetal position (e.g. breech birth) and labor progression). | |||||||||||
6. Interventions targeted at healthcare professionals.
| Study | Intervention | Details |
| Althabe 2004 | Evidence‐based guidelines plus mandatory second opinion |
|
| Chaillet 2015 | Evidence‐based guidelines plus audit and feedback |
|
| Hemminki 2008 | Education of public health nurses on childbirth classes |
|
| Liang 2004 | Peer review plus mandatory second opinion |
|
| Lomas 1991 | Audit and feedback plus local opinion leader education |
|
| Mohammadi 2012 | Audit and feedback plus financial incentive |
|
| Poma 1998 | Audit and feedback plus 24‐hour in‐house coverage by dedicated physician |
|
| Scarella 2011 | Audit and feedback using the Robson classification (Robson 2001) |
|
7. Effects of interventions targeted at healthcare professionals.
| Study | Quality assessment | Outcome | Intervention | Control | Effect | Certainty (GRADE) | |||||||
| Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Relative (95% CIa) or P value | |||||||
| Althabe 2004 | RT | Not serious | Single study | Not serious | Not serious | None | All CS | Mean baseline rate (34,735 women): 26.3 Mean follow‐up rate (35,675): 24.7 Mean rate change: ‐1.6 |
Mean baseline rate (39,175 women): 24.6 Mean follow‐up rate (39,638): 24.9 Mean rate change: 0.3 |
Mean difference in rate change: ‐1.9 (‐3.8 to ‐0.1) |
㊉㊉㊉㊉ HIGH |
||
| Elective CS | Mean baseline rate (34,735 women): 8.9 Mean follow‐up rate (35,675): 9.1 Mean rate change: 0.1 |
Mean baseline rate (39,175 women): 9.1 Mean follow‐up rate (39,638): 9.0 Mean rate change: ‐0.1 |
Mean difference in rate change: 0.2 (‐1.4 to 1.8) | ||||||||||
| Intrapartum CS | Mean baseline rate (34,735 women): 17.4 Mean follow‐up rate (35,675): 15.6 Mean rate change: ‐1.8 |
Mean baseline rate (39,175 women): 15.4 Mean follow‐up rate (39,638): 15.9 Mean rate change: 0.4 |
Mean difference in rate change: ‐2.2 (‐4.3 to ‐0.1) | ||||||||||
| Maternal mortality | Mean baseline rate per 10,000 livebirths (34,735 women): 3.2 Mean follow‐up rate per 10,000 livebirths (35,675 women): 4.3 |
Mean baseline rate per 10,000 livebirths (39,175 women): 5.9 Mean follow‐up rate per 10,000 livebirths (39,638 women): 7.5 |
Mean difference in rate change: 0.66 (‐0.4 to 5.3) (re‐analysed) |
||||||||||
| Neonatal mortality | Mean baseline rate (34,735 women): 1.1 Mean follow‐up rate per 10,000 livebirths (35 675 women): 0.9 |
Mean baseline rate (39,175 women): 1.1 Mean follow‐up rate (39,638 women): 1.0 |
Mean difference in rate change (95% CI): ‐0.1 (‐0.4 to 0.3) |
||||||||||
| Neonatal morbidity | NR | ‐ | ‐ | ‐ | |||||||||
| Chaillet 2015 | Cluster‐RT | Not serious | Single study | Not serious | Not serious | None | Overall CS | Baseline: 5484/24,388 (22.5%) Post‐intervention: 5128/23,484 (21.8%) |
Baseline: 6671/28,698 (23.2%) Post‐intervention: 6767/28,781 (23.5%) |
OR 0.90 (0.80 to 0.99)b RD ‐1.8% (‐3.8 to ‐0.2)b |
㊉㊉㊉㊉ HIGH |
||
| Elective repeat caesarean section | Baseline: 1995/24,388 (8.2%) Post‐intervention: 1931/23,484 (8.2%) |
Baseline: 2404/28,698 (8.4%) Post‐intervention: 2598/28,781 (9.0%) |
RD – 0.6% | ||||||||||
| Low risk group: CS | Baseline: 971/11478 (8.5%) Post‐intervention: 763/10067 (7.6%) |
Baseline: 1256/14717 (8.5%) Post‐intervention: 1172/13019 (9.0%) |
RD ‐1.7% (‐3.0 to ‐0.3) | ||||||||||
| Hemminki 2008 | Cluster‐RT | Seriousc | Single study | Not serious | Seriousd | None | CS | 166/845 (19%) | 116/723 (16%) | OR 1.29 (0.99 to 1.67) |
㊉㊉㊀㊀ LOWc,d |
||
| Liang 2004 | ITS | Seriouse | Single study | Not serious | Not serious | None | CS | Change in level of total caesarean deliveries at 12 monthsf: ‐2.4% (‐11.4% to 6.7%) Change in slopef: 1.34% (‐2.5% to 5.2%) |
㊉㊀㊀㊀ VERY LOWe |
||||
| Lomas 1991 | Cluster‐RT | Not serious | Single study | Not serious | Not serious | None | Audit and feedback | Opinion leader education | Control |
㊉㊉㊉㊉ HIGH |
|||
| Elective CS | 69.7% (62.4 to 77.0%) | 53.7% (46.5 to 61.0%) | 66.8% (61.7 to 72.0%) | ||||||||||
| Unscheduled CS | 18.6% (13.9 to 23.2% | 21.4% (16.8 to 26.1%) | 18.7% (15.4 to 22.1%) | ||||||||||
| Trial of labour rates (%) | 21.4% (13.9 to 29.0%) | 38.2% (30.6 to 45.7%) | 28.3% (23.0 to 33.7%) | ||||||||||
| Vaginal births (%) | 11.8% (5.8 to 17.7%) | 25.3% (19.3 to 31.2%) | 14.5% (10.3 to 18.7%) | ||||||||||
| Low Apgar score < 7 at 5 mins (%) | 5.9 (4.2 to 7.6) | 0.9 (0.0 to 2.6) | 1.2 (0.0 to 2.4) | ||||||||||
| Duration of hospital stay (%) | < 6 days: 27.9 6 days: 29.9 > 6 days: 42.2 |
< 6 days: 46.6 6 days: 31.4 > 6 days: 22.0 |
< 6 days: 32.2 6 days: 31.1 > 6 days: 36.7 |
||||||||||
| Mohammadi 2012 | CBA (reanalysed as ITS) |
Seriouse | Single study | Not serious | Not serious | None | CS | Change in level of caesarean deliveries during the intervention: ‐14.6% (‐24.4% to ‐4.8%), P = 0.02 Change in slope ‐0.07% (‐1.5% to 1.3%), NS |
㊉㊀㊀㊀ VERY LOWe |
||||
| Poma 1998 | ITS | Seriouse | Single study | Not serious | Not serious | None | CS | Change in level of total caesarean deliveries (primary and repeat caesarean sections) at 24 months: ‐6.6% (‐10.1 to ‐3.2); change in slope: ‐0.11% (‐0.25 to 0.02) (data reanalysed) |
㊉㊀㊀㊀ VERY LOWe |
||||
| Scarella 2011 | ITS | Seriouse | Single study | Not serious | Not serious | None | CS | Change in level of caesarean deliveries during intervention: ‐11% (‐23.2 to 1.2%), NS Change in slope: ‐1.1% (‐6.4 to 4.2%), NS Change in level of caesarean deliveries in the immediate post‐intervention period compared with the intervention period: 8.6% (2.1 to 15.2%), P = 0.022 Change in slope: ‐0.3% (‐1.6 to 0.9%), NS |
㊉㊀㊀㊀ VERY LOWe |
||||
| About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as 'quality of evidence' or 'confidence in the estimate' †Substantially different = a large enough difference that it might affect a decision | |||||||||||||
| CBA: controlled before‐after study; CS: caesarean section; ITS: interrupted time series; NR: not reported; NS: not significant; OR: odds ratio; RD: risk difference; RR: risk ratio; RT: randomised trial. aNumbers in parentheses are 95% confidence limits. bDowngraded one level for serious imprecision (confidence interval includes null effects) cAdjusted in between‐group comparison of the change from the preintervention period to the post‐intervention period (adjusted for hospital and patient characteristics). dDowngraded one level for serious risk of bias (pilot study with no sample size calculation; unit of analysis error). eDowngraded one level for possible confounding (unclear whether the intervention occurred independently of other changes over time). fTwo standardised effect sizes are obtained from ITS analysis: change in level (also called 'step change') and change in trend (also called 'change in slope') before and after the intervention. Change in level = difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; change in trend = difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in caesarean section rate. | |||||||||||||
8. Interventions targeted at healthcare organisations or facilities.
| Study | Intervention | Details |
| Financial interventions targeted at healthcare professionals | ||
| Keeler 1996 | Equalising physician fees for vaginal and caesarean section delivery | Revision to fee schedule for obstetric and other procedures including equalising the fees for vaginal and caesarean sections. |
| Lo 2008 |
|
National Health Insurance Taiwan equalised the fee for VBAC to that of a caesarean in April 2003. In May 2005, the fee for vaginal birth was raised to the equivalent of that of a caesarean section. |
| Staffing model interventions | ||
| Rosenstein 2015 | Expanded access to collaborative 24‐hour midwifery‐labourist care model | Expansion of a labourist model that includes 24‐hour in‐hospital midwifery coverage to privately insured patients ('labourist', generally designates an obstetrician who provides in‐house labour and delivery coverage without competing clinical duties). One midwife and one labourist present in‐house, 24 hours a day, working collaboratively to provide primary labour management for all private and public patients. |
| Srinivas 2016 | Labourist model of obstetric care | Labourist model of obstetric care: presence of a labour and delivery provider for a set period of time, whose sole focus is on the labour and delivery unit without other competing clinical duties. The labourist model was based on the internal medicine hospitalist model where physicians spend > 25% of their time caring for inpatients. |
VBAC: vaginal birth after caesarean
9. Effects of interventions targeted at healthcare organisations or facilities.
| Study | Quality assessment | Outcome | Intervention | Control | Relative effect (95% CI) |
Certainty (GRADE) |
|||||
| Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | ||||||
| Effects of financial strategies targeted at healthcare professionals | |||||||||||
| Keeler 1996 | ITS | Seriousa | Single study | Not serious | Not serious | None | CS | CS rates for non‐breech deliveries decreased by 1.2% (22.5% before reform versus 21.3% after reform) |
㊉㊀㊀㊀ VERY LOWa |
||
| Lo 2008 | ITS | Seriousa | Single study | Not serious | Not serious | None | CS | The change in the level of total CS rates following the rise in VBAC fees was ‐1.68 (95% CI ‐2.3 to ‐1.07); the change in slope was ‐0.004 (95% CI ‐0.05 to 0.04)b The change in the level of total CS rates (for all indications and order of birth) following the rise in vaginal birth fees was 1.19 (95% CI ‐0.01 to 2.40) and the change in slope was ‐0.43 (95% CI ‐0.78 to ‐0.09)b |
㊉㊀㊀㊀ VERY LOWa |
||
| Effects of different staffing models of care | |||||||||||
| Rosenstein 2015 | Cohort (with ITS analysis) | Not serious | Single study | Not serious | Not serious | None | Primary CS | Before expansion: 381/1201 (31.7%) | After expansion: 130/521 (25.0%) | OR 0.56 (0.39 to 0.81) |
㊉㊉㊀㊀ LOWc |
| VBAC | Before expansion: 60/452 (13.3%) | After expansion: 52/232 (22.4%) |
OR 2.03 (1.08 to 3.80) | ||||||||
| Srinivas 2016 | CBA | Not serious | Single study | Not serious | Not serious | None | CS | Labourist before, % (N): 32.6 (47,206) Labourist after, % (N): 33.6 (35,210) |
Non‐labourist before, % (N): 28.5 (46,486) Non‐labourist after, % (N): 31.8 (42,348) |
OR 1.02 (0.97 to 1.1) | ㊉㊉㊀㊀ LOWc |
| Labourist before, % (N): 3.8 (5549) Labourist after, % (N): 3.5 (3814) |
Non‐labourist before, % (N): 6.2 (10,018) Non‐labourist before, % (N): 4.8 (6339) |
OR 1.07 (0.88 to 1.30) | |||||||||
| Low Apgar (less than 7) at 5 minutes | Labourist before, % (N): 0.2 (216) Labourist after, % (N): 0.2 (223) |
Non‐labourist before, % (N): 0.4 (557) Non‐labourist after, % (N): 0.4 (476) |
OR 1.09 (0.69 to 1.72) | ||||||||
| Birth asphyxia | Labourist before, % (N): 0.2 (310) Labourist after, % (N): 0.2 (171) |
Non‐labourist before, % (N): 0.3 (398) Non‐labourist after, % (N): 0.2 (247) |
OR 0.75 (0.48 to 1.18) | ||||||||
| Maternal prolonged length of stay | Labourist before, % (N): 21.4 (31,002) Labourist after, % (N): 21.5 (22,512) |
Non‐labourist before, % (N): 24.2 (39,354) Non‐labourist after, % (N): 26.2 (34,876) |
OR 0.99 (0.87 to 1.14) | ||||||||
| About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as 'quality of evidence' or 'confidence in the estimate' †Substantially different = a large enough difference that it might affect a decision | |||||||||||
| CBA: controlled before‐after; CS: caesarean section; CI: confidence interval; ITS: interrupted time series; OR: odds ratio; VBAC: vaginal birth after caesarean. aDowngraded one level for serious risk of bias (due to possible confounding of outcome, unclear whether the intervention occurred independently of other changes over time). bTwo standardised effect sizes are obtained from ITS analysis: a change in level (also called ‘step change’) and a change in trend (also called ‘change in slope’) before and after the intervention. Change in level = difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; change in trend = difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in CS rate. cObservational study which start at low certainty evidence according to GRADE (we did not downgrade or upgrade the certainty of evidence) | |||||||||||
10. 'Cross‐cutting' interventions.
| Study | Intervention | Details |
| Ayres‐De‐Campos 2015 | Transmission of information and training of healthcare professionals, together with the inclusion of CS rates as a criterion for hospital funding | Concerted action to reduce CS
|
| Runmei 2012 | Continuous quality improvement programme (educational programme for hospital staff and women, auditing surgeon practices, public health education, monitoring caesarean section rates and neonatal outcomes) | Continuous quality improvement programme Stage 1: January 2005 to December 2006
Stage 2 (January to June 2007)
Stage 3 (Jan 2005‐Dec 2011)
|
CS: caesarean section
11. Effects of 'cross‐cutting' interventions.
| Study | Quality assessment | Outcome | No of participants |
Relative effect (95% CI) or P value |
Certainty (GRADE) |
||||||
| Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Intervention | Control | ||||
| Ayres‐De‐Campos 2015 | ITS | Seriousa | Single study | Not serious | Not serious | None | In the period between 2009 and 2014, representing the possible influence of the concerted action: the CS rate in the study region decreased by 20.0% (from 36.0 to 28.8%, time trend P < 0.001)b; rates of instrumental vaginal delivery increased by 33.1% (from 13.7 to 18.2%, time trend P < 0.001), VBAC increased by 99.8% (from 16.4 to 32.8%, time trend P < 0.001), while perineal lacerations increased by 45.2% (from 0.42 to 0.61%, time trend P < 0.001)b; the incidence of hypoxia‐related complications decreased by 14.1% (from 0.71 to 0.61%, time trend P < 0.001)b |
㊉㊀㊀㊀ VERY LOWa |
|||
| Runmei 2012 | CBA (reanalysed as ITS) |
Seriousa | Single study | Not serious | Not serious | None | CS | Change in level of caesarean deliveries during intervention: ‐13.4% (95% CI ‐19.6% to ‐7.1%)b; change in slope of caesarean deliveries: ‐0.72% (95% CI ‐3% to 1.5%)b |
㊉㊀㊀㊀ VERY LOWa |
||
| Maternal morbidity | "We found a significant increase in the incidence of all obstetric complications, with the exception of placental abruption, after 2004..." | ||||||||||
| Neonatal morbidity | "The incidence of birth asphyxia did not increase after 2004 (P = 0.303)" | ||||||||||
| About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as 'quality of evidence' or 'confidence in the estimate' †Substantially different = a large enough difference that it might affect a decision | |||||||||||
| CBA: controlled before‐after; CI: confidence interval; CS: caesarean section; ITS: interrupted time series; VBAC: vaginal birth after caesarean. aDowngraded one level for serious risk of bias (due to possible confounding of outcome, unclear whether the intervention occurred independently of other changes over time). bTwo standardised effect sizes are obtained from interrupted time series analysis: a change in level (also called ‘step change’) and a change in trend (also called ‘change in slope’) before and after the intervention. Change in level = difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; change in trend = difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in caesarean section rate. | |||||||||||
GRADE and summary of findings
We assessed the certainty of evidence (confidence in the estimate of effect) using GRADE (Guyatt 2008). The GRADE assessments were conducted by one review author (NO) and checked by at least one other review author.
According to GRADE, evidence from randomised trials starts at high certainty while that from observational studies starts at low certainty. We downgraded certainty of evidence from randomised trials in consideration of five factors: risk of bias or study limitations, directness, consistency of results, precision of effect estimates and publication bias. Quality of evidence from observational studies can be upgraded in consideration of three factors: magnitude of effect, dose‐response gradient and influence of residual plausible confounding. We did not upgrade the quality of evidence from any of the included observational studies as none met the upgrading criteria.
We prepared four 'Summary of findings' tables (one each for the four intervention categories) summarising effects of the interventions on the primary outcome measures (caesarean section, spontaneous vaginal birth, and instrumental vaginal birth) and adverse effects (maternal and neonatal mortality or morbidity).
Subgroup analysis and investigation of heterogeneity
We did not conduct a subgroup analysis to explore if effects of interventions varied by factors such as parity, socioeconomic status or geographical regions (there was insufficient data for these analyses).
Sensitivity analysis
We did not conduct a sensitivity analysis as we did not pooled the data.
Results
Description of studies
Results of the search
Details of the search results are presented in Figure 1. We identified 12,155 records from electronic databases, clinical trials registries and other resources. We excluded 12,015 records following a review of titles and abstracts. We retrieved the full texts of the remaining 140 records for detailed eligibility assessment. We excluded 113 records; two studies are awaiting classification and will be considered for inclusion in the next update of this review (Characteristics of studies awaiting classification), and eight trials are ongoing (Characteristics of ongoing studies).
1.

aSearches run in March 2018 (Appendix 1).
bSearches run in August 2014 (Appendix 2) and February 2017 (Appendix 3).
Overall, 29 studies fulfilled the review inclusion criteria (17 new studies and 12 studies from the original review (Khunpradit 2011)).
Included studies
The 29 included studies form the basis of the findings summarised in this review (Characteristics of included studies).
These studies were conducted in 18 different countries.
North America (7 studies in USA; 2 studies in Canada).
Europe (3 studies in Finland; 1 study each in UK, Portugal, Sweden).
Latin America (1 study in Chile; 1 multicentre study in Argentina, Brazil, Cuba, Guatemala, Mexico).
Western Asia (6 studies in Iran).
East Asia (2 studies in China; 2 studies in Taiwan).
Oceania (2 studies in Australia).
Caesarean section rates in the control groups (or prior to intervention in other study designs) ranged from 12% in Hemminki 2008 to 73.3% in Valiani 2014.
Eight studies included only nulliparous women (Bastani 2006; Bergstrom 2009; Feinberg 2015; Navaee 2015; Rouhe 2013; Sharifirad 2013; Valiani 2014; Wang 2014). Five studies included only women having undergone a previous caesarean section (Eden 2014; Fraser 1997; Lomas 1991; Montgomery 2007; Shorten 2005); the remaining 16 studies included a mixed population of women.
Twenty‐three studies were supported by grants from various funding agencies (international funding agencies, national research councils, universities, among others); two studies received no specific financial support. No information about funding was available from four studies.
1. Interventions targeted at women or families
Fifteen studies (4459 participants) were included in this category: 12 studies compared specific educational interventions to routine maternity care (Bastani 2006; Bergstrom 2009; Feinberg 2015; Fenwick 2015; Masoumi 2016; Montgomery 2007; Rouhe 2013; Saisto 2001; Sharifirad 2013; Shorten 2005; Valiani 2014; Wang 2014). Three studies compared different formats of educational interventions (Eden 2014; Fraser 1997; Navaee 2015). All of the studies were randomised trials.
Participants in the included studies comprised: women with a fear of childbirth (Fenwick 2015; Navaee 2015; Rouhe 2013; Saisto 2001); women with high levels of anxiety (Bastani 2006); husbands of pregnant women (Sharifirad 2013); pregnant women and couples (Valiani 2014); and pregnant women with no particular health condition in the remaining studies.
The majority of studies were conducted in high‐income countries: USA (Eden 2014; Feinberg 2015; Fraser 1997); UK (Montgomery 2007); Australia (Fenwick 2015; Shorten 2005); Canada (Fraser 1997); Sweden (Bergstrom 2009); and Finland (Rouhe 2013; Saisto 2001). Six studies were conducted in middle‐income countries: China (Wang 2014); Iran (Bastani 2006; Masoumi 2016; Navaee 2015; Sharifirad 2013; Valiani 2014). No studies were carried out in low‐income countries.
The specific educational interventions assessed were the following.
Antenatal education programme for physiologic childbirth (birth preparation training) (Masoumi 2016).
Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques (Bergstrom 2009).
Childbirth training workshop (Valiani 2014)
Prenatal education for husbands of pregnant women (Sharifirad 2013).
Pelvic floor muscle training exercises with telephone follow‐up (Wang 2014).
Nurse‐led applied relaxation training programme (Bastani 2006).
Psychosocial couple‐based prevention programme (Feinberg 2015).
Psychoeducation by telephone (Fenwick 2015).
Psychoeducation (Rouhe 2013).
Two computer‐based decision aids (information programme, decision analysis) (Montgomery 2007).
Intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy) (Saisto 2001).
Decision aid booklet (Shorten 2005).
Women in the control group received routine maternity care. Pelvic floor muscle training with telephone follow‐up was compared to Pelvic floor muscle training without telephone follow‐up.
The different formats of educational interventions assessed were the following.
Role play education versus standard education using lectures (Navaee 2015).
Interactive decision aid versus educational brochures (Eden 2014).
Individualised prenatal education and support programme versus written information in pamphlets (Fraser 1997).
Details of the interventions are summarised in Table 8.
2. Interventions targeted at healthcare professionals
We included eight studies in this category (Althabe 2004; Chaillet 2015; Hemminki 2008; Liang 2004; Lomas 1991; Mohammadi 2012;Poma 1998; Scarella 2011). Study designs were varied: cluster‐randomised trials (Althabe 2004; Chaillet 2015; Hemminki 2008; Lomas 1991); controlled before‐after studies (reanalysed using interrupted time series methods) (Mohammadi 2012); and interrupted time series studies (Liang 2004; Poma 1998; Scarella 2011).
Six studies were conducted in high‐income countries: USA (Poma 1998); Canada (Chaillet 2015; Lomas 1991); Finland (Hemminki 2008); Chile (Scarella 2011); and Taiwan (Liang 2004). Two studies were conducted in middle‐income countries: Iran (Mohammadi 2012); multicountry ‐ Mexico, Argentina, Brazil, Cuba, Guatemala and Mexico (Althabe 2004). No studies were carried out in low‐income countries.
Health professionals studied were: physicians (obstetrician‐gynaecologist) (Althabe 2004; Liang 2004; Lomas 1991; Mohammadi 2012; Poma 1998); physicians and nurses (Chaillet 2015; Scarella 2011); and public health nurses (Hemminki 2008).
The interventions assessed were the following.
Education of public health nurses on childbirth classes (Hemminki 2008).
Peer review plus mandatory second opinion (Liang 2004).
Evidence‐based guidelines plus mandatory second opinion (Althabe 2004).
Evidence‐based guidelines plus audit and feedback (Chaillet 2015).
Audit and feedback using Robson classification (Scarella 2011).
Audit and feedback plus financial incentive (Mohammadi 2012).
Audit and feedback plus 24‐hour in‐house physician coverage (Poma 1998).
Audit and feedback plus local opinion leader education (Lomas 1991).
Details of the interventions are summarised in Table 10.
3. Interventions targeted at healthcare organisations or facilities
3.1 Financial interventions targeted at healthcare professionals
We included two interrupted time series studies in this category (Keeler 1996; Lo 2008). The studies were conducted in the USA (Keeler 1996), and Taiwan (Lo 2008). Both assessed insurance reforms equalising physician fees for vaginal births and caesarean sections. Details of the interventions are summarised in Table 12.
3.2 Different staffing models of care
We included two studies in this category. The interventions assessed were the following.
Labourist model of obstetric care versus routine delivery care (Srinivas 2016). ('Labourist' generally refers to an obstetrician who provides in‐house labour and delivery coverage without competing clinical duties).
Midwifery‐labourist model of care versus private practice care model (Rosenstein 2015).
Details of the interventions are summarised in Table 12.
Study designs were varied: controlled before‐after study (Srinivas 2016); interrupted time series study (Rosenstein 2015). Both studies were conducted in the USA.
4. 'Cross‐cutting' interventions
We included the following two interventions in this category.
Multifaceted programme comprising an education programme for hospital staff and women, audit of surgeon practices, public health campaign, monitoring rates of caesarean section and neonatal outcomes (Runmei 2012).
Multifaceted programme comprising transmission of information on caesarean section to health professionals, training of health workers on best obstetric practices and inclusion of caesarean section rates as a criterion for hospital funding (Ayres‐De‐Campos 2015).
Details of the interventions are summarised in Table 14.
Study design and settings were varied: interrupted time series study (Ayres‐De‐Campos 2015); controlled before‐after study (Runmei 2012). Ayres‐De‐Campos 2015 was conducted in Portugal, while Runmei 2012 was conducted in China.
Excluded studies
We excluded 52 studies because of ineligible study designs, interventions and outcome measures (see Characteristics of excluded studies).
Risk of bias in included studies
Randomised trials, non‐randomised trials and controlled before‐after studies (20 studies)
Allocation
We judged random sequence generation and allocation concealment to be adequate (indicating low risk of selection bias) in eight trials (Althabe 2004; Chaillet 2015; Eden 2014; Fenwick 2015; Fraser 1997; Masoumi 2016; Montgomery 2007; Shorten 2005). We judged Srinivas 2016 to be at high risk of selection bias. The risk of selection bias in the remaining trials was unclear (insufficient information was available regarding allocation concealment).
Blinding
We judged blinding of study participants and personnel to be adequate (indicating low risk of performance bias) in four trials (Althabe 2004; Chaillet 2015; Eden 2014; Fenwick 2015). The risk of performance bias was unclear in the remaining trials. Blinding of primary outcome measures was not feasible (caesarean and vaginal births are objective outcomes).
Incomplete outcome data
We judged the risk of attrition bias (due to incomplete outcome data) to be low in 14 trials, high in one trial (Hemminki 2008), and unclear in five trials (Feinberg 2015; Lomas 1991; Navaee 2015; Valiani 2014; Wang 2014).
Selective reporting
We judged all trials to be at low risk of reporting bias (due to selective reporting), except in one trial (Hemminki 2008), where the likelihood of reporting bias was unclear.
Other potential sources of bias
We judged three trials to be at risk of other biases due to unit of analysis issues (Bergstrom 2009; Lomas 1991), and lack of a priori sample size calculation (Hemminki 2008).
Details of the risk of bias judgements are summarised in Characteristics of included studies and Figure 2.
2.
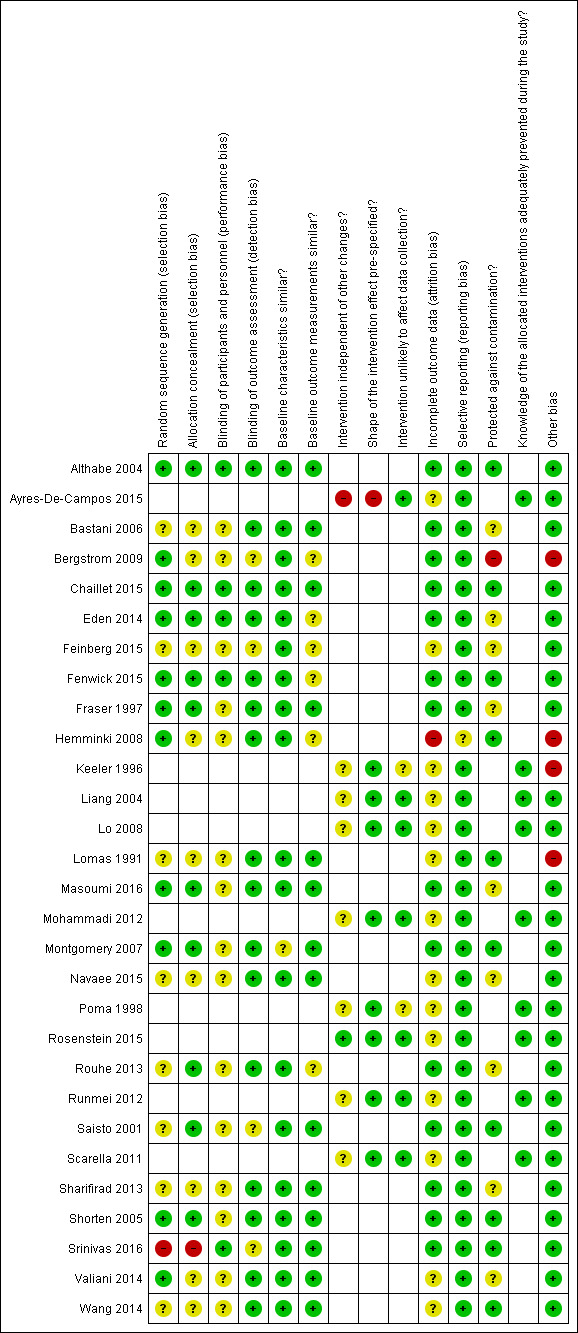
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Interrupted time series studies (9 studies)
We judged all of the interrupted time series studies to be at unclear risk of attrition bias and free of reporting bias. The shape of the intervention effect was prespecified in all except two studies (Ayres‐De‐Campos 2015; Poma 1998). It was not clear if the intervention was independent of other changes in all except one study (Rosenstein 2015). The intervention seemed unlikely to affect data collection in all except two studies (Keeler 1996; Poma 1998). We considered knowledge of the allocated interventions to be adequately prevented in all studies (main outcomes of interests are objective). We judged one study to be at high risk of other bias (due to inadequate analysis) (Keeler 1996).
Details of the risk of bias judgements are summarised in Characteristics of included studies and Figure 2.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Interventions targeted at women or families.
| Patients or population: mixed population (women with a fear of childbirth; women with high levels of anxiety; husbands of pregnant women; pregnant women and couples; and pregnant women with no particular health condition) | ||||||
| Intervention | Primary outcome measure | Plain language summary | Absolute effectǂ |
Relative effect (95% CI) |
Certainty (GRADE) | |
| with control |
with intervention (95% CI) |
|||||
| Education, birth preparation classes and support programmes | ||||||
|
Childbirth training workshop (Iran) (Valiani 2014, randomised trial) |
Caesarean section | Childbirth training workshop may reduce the caesarean section rate compared to routine maternity care | 73 per 100 | 40 per 100 (24 to 65) |
Mothers alone versus control: RR 0.55 (0.33 to 0.89) (1 study, 60 women) |
㊉㊉㊀㊀ LOWa,b |
| 73 per 100 | 43 per 100 (27 to 69) |
Couple versus control: RR 0.59 (0.37 to 0.94) (1 study, 60 women) |
||||
| Spontaneous vaginal birth | Childbirth training workshop may increase spontaneous vaginal birth compared to routine maternity care | 27 per 100 | 61 per 100 (31 to 118) |
Mothers alone versus control: RR 2.25 (1.16 to 4.36) (1 study, 60 women) |
||
| 27 per 100 | 58 per 100 (29 to 112) |
Couple versus control: RR 2.13 (1.09 to 4.16) (1 study, 60 women) |
||||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Nurse‐led applied relaxation training programme (Iran) (Bastani 2006, randomised trial) |
Caesarean section | Nurse‐led applied relaxation training programme may reduce caesarean section rate compared to routine maternity care | 404 per 1000 | 89 per 1000 (44 to 174) |
RR 0.22 (0.11 to 0.43) (1 study, 104 women) |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | Nurse‐led applied relaxation training programme may reduce instrumental vaginal births compared to routine maternity care | 481 per 1000 | 212 per 1000 (115 to 385) |
RR 0.44 (0.24 to 0.80) (1 study, 104 women) |
㊉㊉㊀㊀ LOWa,b |
|
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Psychosocial couple‐based prevention programme (USA) (Feinberg 2015, randomised trial) |
Caesarean section | Psychosocial couple‐based prevention programme may reduce caesarean section rate compared to routine maternity care | 394 per 1000c | 209 per 1000 (126 to 355) |
RR 0.53 (0.32 to 0.90)c (1 study, 147 women) |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Psychoeducation (Finland) (Rouhe 2013, randomised trial) |
Caesarean section | Psychoeducation may lead to little or no difference in caesarean section rate compared to routine maternity care | 325 per 1000 | 228 per 1000 (159 to 328) |
RR 0.70 (0.49 to 1.01) (1 study, 371 women) |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | Psychoeducation may increase spontaneous vaginal birth compared to routine maternity care | 475 per 1000 | 632 per 1000 (527 to 765) |
RR 1.33 (1.11 to 1.61) (1 study, 371 women) |
||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Antenatal education programme for physiologic childbirth (Iran) (Masoumi 2016, randomised trial) |
Caesarean section | Antenatal education programme for physiologic childbirth probably leads to little or no difference in caesarean section rate compared to routine maternity care | 437 per 1000 | 450 per 1000 (315 to 651) |
RR 1.03 (0.72 to 1.49) (1 study, 150 women) |
㊉㊉㊉㊀ MODERATEa |
| Spontaneous vaginal birth – physiologic birth | Antenatal education programme for physiologic childbirth probably increases rates of physiologic birth compared to routine maternity care | 0 per 1000 | 80 per 1000 (CI not estimable) |
Relative effect not estimable (1 study, 150 women) |
||
| Spontaneous vaginal birth – normal vaginal birth | Antenatal education programme for physiologic childbirth probably leads to little or no difference in normal vaginal birth compared to routine maternity care | 570 per 1000 | 479 per 1000 (353 to 650) |
RR 0.84 (0.62 to 1.14) (1 study, 150 women) |
||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Pelvic floor muscle training exercises (China) (Wang 2014, randomised trial) |
Caesarean section | Pelvic floor muscle training exercises with telephone follow‐up may lead to little or no difference in caesarean section rate compared to pelvic floor muscle training without telephone follow‐up | 49 per 100 | 43 per 100 (18 to 100) |
RR 0.87 (0.37 to 2.04) (1 study, 90 women) |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques (Sweden) (Bergstrom 2009, randomised trial) |
Caesarean section – elective | Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques probably leads to little or no difference in elective caesarean section rate compared to routine maternity care | 630 per 1000 | 599 per 1000 (365 to 983) |
RR 0.95 (0.58 to 1.56) (1 study, 977 women) |
㊉㊉㊉㊀ MODERATEd |
| Caesarean section – emergency | Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques probably leads to little or no difference in emergency caesarean section rate compared to routine maternity care | 152 per 1000 | 138 per 1000 (102 to 187) |
RR 0.91 (0.67 to 1.23) (1 study, 977 women) |
||
| Spontaneous vaginal birth | Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques probably leads to little or no difference in spontaneous vaginal birth rate compared to routine maternity care | 663 per 1000 | 663 per 1000 (603 to 723) |
RR 1.00 (0.91 to 1.09) (1 study, 977 women) |
||
| Instrumental vaginal birth | Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques probably leads to little or no difference in instrumental vaginal birth rate compared to routine maternity care | 122 per 1000 | 139 per 1000 (100 to 192) |
RR 1.14 (0.82 to 1.57) (1 study, 977 women) |
||
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Computer‐based decision aids (information programme, decision analysis) (UK) (Montgomery 2007, randomised trial) |
Caesarean section – elective | Information group versus usual care: computer‐based decision aids (information programme) probably leads to little or no difference in elective caesarean section rate compared to usual care | 496 per 1000 | 486 per 1000 (407 to 585) |
RR 0.98 (0.82 to 1.18) (1 study, 478 women) |
㊉㊉㊉㊀ MODERATEd |
| Caesarean section – elective | Decision analysis group versus usual care: computer‐based decision aids (decision analysis) probably leads to little or no difference in elective caesarean section rate compared to usual care | 496 per 1000 | 412 per 1000 (337 to 506) |
RR 0.83 (0.68 to 1.02) (1 study, 478 women) |
||
| Caesarean section – emergency | Information group versus usual care: computer‐based decision aids (information programme) probably leads to little or no difference in emergency caesarean section rate compared to usual care | 202 per 1000 | 220 per 1000 (156 to 313) |
RR 1.09 (0.77 to 1.55) (1 study, 478 women) |
||
| Caesarean section – emergency | Decision analysis group versus usual care: computer‐based decision aids (decision analysis) probably leads to little or no difference in emergency caesarean section rate compared to usual care | 202 per 1000 | 212 per 1000 (150 to 303 |
RR 1.05 (0.74 to 1.50) (1 study, 478 women) |
||
| Spontaneous vaginal birth | Decision analysis versus usual care: computer‐based decision aids (decision analysis) probably leads to little or no difference in spontaneous vaginal birth rate compared to usual care | 303 per 1000 | 376 per 1000 (291 to 485) |
RR 1.24 (0.96 to 1.60) (1 study, 478 women) |
||
| Spontaneous vaginal birth | Information group versus usual care: computer‐based decision aids (information programme) probably leads to little or no difference in spontaneous vaginal birth rate compared to usual care | 303 per 1000 | 291 per 1000 (221 to 385) |
RR 0.96 (0.73 to 1.27) (1 study, 478 women) |
||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Decision aid booklet (Australia) (Shorten 2005, randomised trial) |
Caesarean section – elective repeat | Decision aid booklet probably leads to little or no difference in elective repeat caesarean section compared to routine maternity care | Baseline: 23.2% Follow‐up: 49.4% Change from baseline: 26.2% |
Baseline: 29.6% Follow‐up: 52.2% Change from baseline: 22.6% |
Relative effect not reported Difference in absolute change from baseline: ‐3.6% (NS) (1 study, 227 women) |
㊉㊉㊉㊀ MODERATEa |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy) (Finland) (Saisto 2001, randomised trial) |
Caesarean section | Intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy) may lead to little or no difference in caesarean section rate compared to routine maternity care | 484 per 1000 | 436 per 1000 (315 to 600) |
RR 0.90 (0.65 to 1.24) (1 study, 176 women) |
㊉㊉㊀㊀ LOWa,b |
| Caesarean section – for psychological reasons | Intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy) may lead to little or no difference in caesarean section rate for psychological reasons compared to routine maternity care | 286 per 1000 | 235 per 1000 (143 to 389) |
RR 0.82 (0.50 to 1.36) (1 study, 176 women) |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Psychoeducation sessions by telephone (Australia) (Fenwick 2015, randomised trial) |
Caesarean section – overall | The effect of psychoeducation sessions by telephone (compared to routine maternity care) on overall caesarean section rate is uncertain | 419 per 1000 | 339 per 1000 (235 to 494) |
RR 0.81 (0.56 to 1.18) (1 study, 184 women) |
㊉㊀㊀㊀ VERY LOWa,b,e |
| Caesarean section – emergency | The effect of psychoeducation sessions by telephone (compared to routine maternity care) on emergency caesarean section rate is uncertain | 247 per 1000 | 173 per 1000 (96 to 304) |
RR 0.70 (0.39 to 1.23) (1 study, 182 women) |
||
| Spontaneous vaginal birth | The effect of psychoeducation sessions by telephone (compared to routine maternity care) on spontaneous vaginal birth rate is uncertain | 419 per 1000 | 482 per 1000 (352 to 666) |
RR 1.15 (0.84 to 1.59) (1 study, 184 women) |
||
| Instrumental vaginal birth | The effect of psychoeducation sessions by telephone (compared to routine maternity care) on instrumental vaginal birth rate is uncertain | 161 per 1000 | 176 per 1000 (92 to 333) |
RR 1.09 (0.57 to 2.07) (1 study, 184 women) |
||
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Prenatal education for husbands of pregnant women (Iran) (Sharifirad 2013, randomised trial) |
Caesarean section | The effect of prenatal education for husbands of pregnant women (compared to routine maternity care) on caesarean section rate is uncertain | 50.0% (number of events not reported) |
29.5% (number of events not reported) |
Relative effect not reported P < 0.05 (1 study, 88 women) |
㊉㊀㊀㊀ VERY LOWb,c,f |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Different formats of educational interventions | ||||||
|
Role play versus standard education using lectures (Iran) (Navaee 2015, randomised trial) |
Caesarean section | Role play may lead to little or no difference in caesarean section rate compared to education using lectures | 56 per 100 | 37 per 100 (22 to 63) |
RR 0.66 (0.39 to 1.12) (1 study, 67 women) |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Interactive decision aid versus educational brochures (USA) (Eden 2014, randomised trial) |
Caesarean section – VBAC | Interactive decision aid may lead to little or no difference in VBAC rate compared to educational brochures | 37% Number of events unclear |
41% Number of events unclear |
P = 0.72 Number of participants unclear |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Individualised prenatal education and support programme versus written information in pamphlet (Canada, USA) (Fraser 1997, randomised trial) |
Caesarean section – scheduled | Individualised prenatal education and support programme probably leads to little or no difference in scheduled caesarean section rate compared to written information in pamphlet | 237 per 1000 | 213 per 1000 (175 to 263) |
RR 0.90 (0.74 to 1.11) (1 study, 1275 women) |
㊉㊉㊉㊀ MODERATEa |
| Caesarean section – urgent | Individualised prenatal education and support programme probably leads to little or no difference in urgent caesarean section rate compared to written information in pamphlet | 690 per 1000 | 607 per 1000 (400 to 918) |
RR 0.88 (0.58 to 1.33) (1 study, 1275 women) |
||
| Caesarean section – VBAC | Individualised prenatal education and support programme probably leads to little or no difference in VBAC rate compared to written information in pamphlet | 490 per 1000 | 529 per 1000 (475 to 593) |
RR 1.08 (0.97 to 1.21) (1 study, 1275 women) |
||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal morbidity, neonatal morbidity or mortality | Individualised prenatal education and support programme probably leads to little or no difference in maternal morbidity, neonatal morbidity or mortality compared to written information in pamphlet | Rates of maternal morbidity and neonatal outcomes were similar in the study groups (maternal–uterine rupture or dehiscence, hysterectomy, blood transfusion; neonatal–perinatal deaths, Apgar score less than 7 at 5 minutes, admission to NICU) | ㊉㊉㊉㊀ MODERATEa |
|||
| ǂThe corresponding risk (absolute effect with intervention) (and its 95% confidence interval) is based on the assumed risk in the comparison group ((i.e. risk with control) and the relative effect of the intervention (and its 95% CI). About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as ‘quality of evidence’ or ‘confidence in the estimate’ †Substantially different = a large enough difference that it might affect a decision. CI: confidence interval; NICU: neonatal intensive care unit; NR: not reported; NS; not significant; RR: risk ratio; VBAC: vaginal birth after caesarean. | ||||||
|
aDowngraded one level for serious risk of bias (due to inadequate randomisation processes). bDowngraded one level for serious imprecision (due to small sample size and few events). cReanalysed, based on: control event rate (40%, n = 71); intervention event rate (21%, n = 76); odds ratio (OR) 0.36, 95% CI 0.15 to 0.86). dDowngraded one level due to serious imprecision (95% CI includes appreciable benefit and harm). eDowngraded one level for serious indirectness (follow‐up analyses, not described in the trial report, indicated that the impact on caesarean sections was due to reduced birth complications arising from foetal position (e.g. breech birth) and labour progression). fDowngraded two levels for very serious risk of bias (due to inadequate randomisation processes and reporting issues). | ||||||
Summary of findings 2. Interventions targeted at healthcare professionals.
| Patients or population: nurses, midwives, physicians | ||||||
| Intervention | Primary outcome measure | Plain language summary | Absolute effectǂ |
Relative effect (95% CI) |
Certainty (GRADE) | |
| with control |
with intervention (95% CI) |
|||||
|
Implementation of clinical practice guidelines combined with mandatory second opinion (Argentina, Brazil, Cuba, Guatemala and Mexico) (Althabe 2004, cluster‐randomised trial) |
Caesarean section – all | Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication slightly reduces the caesarean section rate compared to routine maternity care | Mean baseline rate: 24.6 (39,175 women) Mean follow‐up rate: 24.9 (39,638 women) Mean rate change: 0.3 |
Mean baseline rate: 26.3 (34,735 women) Mean follow‐up rate: 24.7 (35,675 women) Mean rate change: ‐1.6 |
Mean difference in rate change: ‐1.9 (‐3.8 to ‐0.1) |
㊉㊉㊉㊉ HIGH |
| Caesarean section – elective | Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication results in little or no difference in elective caesarean section rate compared to routine maternity care | Mean baseline rate: 9.1 (39,175 women) Mean follow‐up rate: 9.0 (39,638 women) Mean rate change: ‐0.1 |
Mean baseline rate: 8.9 (34,735 women) Mean follow‐up rate: 9.1 (35,675 women) Mean rate change: 0.1 |
Mean difference in rate change: 0.2 (‐1.4 to 1.8) |
||
| Caesarean section – intrapartum | Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication slightly reduces intrapartum caesarean section compared to routine maternity care | Mean baseline rate: 15.4 (39,175 women) Mean follow‐up rate: 15.9 (39,638 women) Mean rate change: 0.4 |
Mean baseline rate: 17.4 (34,735 women) Mean follow‐up rate: 15.6 (35,675 women) Mean rate change: ‐1.8 |
Mean difference in rate change: ‐2.2 (‐4.3 to ‐0.1) |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality | Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication results in little or no difference in maternal mortality compared to routine maternity care | Mean baseline rate per 10,000 livebirths (39 175 women): 5.9 Mean follow‐up rate per 10,000 livebirths (39 638 women): 7.5 |
Mean baseline rate per 10,000 livebirths (34 735 women): 3.2 Mean follow‐up rate per 10,000 livebirths (35 675 women): 4.3 |
Mean difference in rate change: 0.66 (‐4.0 to 5.3) (re‐analysed) |
㊉㊉㊉㊉ HIGH |
|
| Maternal morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality | Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication results in little or no difference in neonatal mortality compared to routine maternity care | Mean baseline rate (39,175 women): 1.1 Mean follow‐up rate (39,638 women): 1.0 Mean rate change: ‐0.1 |
Mean baseline rate (34,735 women): 1.1 Mean follow‐up rate per 10,000 livebirths (35 675 women): 0.9 Mean rate change: ‐0.2 |
Mean difference in rate change (95% CI): ‐0.1 (‐0.4 to 0.3) |
㊉㊉㊉㊉ HIGH |
|
| Neonatal morbidity | Implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication results in little or no difference in Intrapartum foetal distress compared to routine maternity care | Mean baseline rate (39,175 women): 3.1 Mean follow‐up rate (39,638 women): 3.1 Mean rate change: 0.0 |
Mean baseline rate (34,735 women): 4.3 Mean follow‐up rate per 10,000 livebirths (35 675 women): 3.4 Mean rate change: ‐1.0 |
Mean difference in rate change (95% CI): –0·9 (–1·9 to –0·0) |
㊉㊉㊉㊉ HIGH |
|
|
Implementation of clinical practice guidelines combined with audit and feedback (Canada) (Chaillet 2015, cluster‐randomised trial) |
Caesarean section ‐ overall | Implementation of clinical practice guidelines combined with audit and feedback slightly reduces the overall caesarean section rate compared to routine maternity care | Baseline: 6671/28,698 (23.2%) Post‐intervention: 6767/28,781 (23.5%) |
Baseline: 5484/24,388 (22.5%) Post‐intervention: 5128/23,484 (21.8%) |
RD ‐1.8% (‐3.8 to ‐0.2) |
㊉㊉㊉㊉ HIGH |
| Caesarean section ‐ low risk group | Implementation of clinical practice guidelines combined with audit and feedback slightly reduces caesarean section rate compared to routine maternity care | Baseline: 1256/14,717 (8.5%) Post‐intervention: 1172/13,019 (9.0%) |
Baseline: 971/11,478 (8.5%) Post‐intervention: 763/10,067 (7.6%) |
RD ‐1.7% (‐3.0 to ‐0.3) | ||
| Elective repeat caesarean section | Implementation of clinical practice guidelines plus audit and feedback results in little or no difference in elective repeat caesarean section rate compared to routine maternity care groups | Baseline: 2404/28,698 (8.4%) Post‐intervention: 2598/28,781 (9.0%) |
Baseline: 1995/24,388 (8.2%) Post‐intervention: 1931/23,484 (8.2%) |
RD – 0.6% (‐0.07 to 1.28) | ||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Major maternal morbidity | Implementation of clinical practice guidelines combined with audit and feedback results in little or no difference in major maternal morbidity compared to routine maternity care | Baseline: 138/28,698 (0.48%) Post‐intervention: 141/28,781 (0.49%) |
Baseline: 161/24,388 (0.66%) Post‐intervention: 167/23,484 (0.71%) |
RD 0.03% (‐0.11 to 0.23) |
㊉㊉㊉㊉ HIGH |
|
| Minor maternal morbidity | Implementation of clinical practice guidelines combined with audit and feedback results in little or no difference in minor maternal morbidity compared to routine maternity care | Baseline: 3869/28,698 (13.5%) Post‐intervention: 4244/28,781 (14.7%) |
Baseline: 3293/24,388 (13.5%) Post‐intervention: 3576/23,484 (15.2%) |
RD 0.3% (‐1.2 to 1.8) |
||
| Major neonatal morbidity | Implementation of clinical practice guidelines combined with audit and feedback results in little or no difference in major neonatal morbidity compared to routine maternity care | Baseline: 1018/29,107 (3.5%) Post‐intervention: 1156/29,211 (4.0%) |
Baseline: 1172/24,823 (4.7%) Post‐intervention: 1070/23,902 (4.5%) |
RD ‐0.7% (‐1.3 to ‐0.1) |
||
| Minor neonatal morbidity | Implementation of clinical practice guidelines combined with audit and feedback results in little or no difference in minor neonatal morbidity compared to routine maternity care | Baseline: 3947/29,107 (13.6%) Post‐intervention: 5002/29,211 (17.1%) |
Baseline: 3936/25,823 (15.9%) Post‐intervention: 4261/23,902 (17.8%) |
RD ‐1.7% (‐2.6 to ‐0.9) |
||
| Intrapartum and neonatal deaths | Implementation of clinical practice guidelines combined with audit and feedback results in little or no difference in intrapartum and neonatal deaths compared to routine maternity care | Baseline: 14/29 107 (0.0%) Post‐intervention: 28/29,211 (0.0%) |
Baseline: 35/24 823 (0.1%) Post‐intervention: 20/23,902 (0.1%) |
RD ‐0.06% (‐0.08 to ‐0.03) |
||
|
Physician education by local opinion leader (obstetrician‐gynaecologist) Audit and feedback (Canada) (Lomas 1991, cluster‐randomised trial) |
Caesarean section – elective | Physician education by local opinion leader (obstetrician‐gynaecologist) reduced elective caesarean section compared to routine maternity care | Control: 66.8% (61.7 to 72.0) |
Opinion leader education: 53.7% (46.5 to 61.0) |
‐ |
㊉㊉㊉㊉ HIGH |
| Audit and feedback results in little or no difference in elective caesarean section compared to routine maternity care | Control: 66.8% (61.7 to 72.0) |
Audit and feedback: 69.7% (62.4 to 77.0) |
‐ | |||
| Caesarean section – unscheduled | There was no difference in unscheduled caesarean section between opinion leader education (obstetrician‐gynaecologist) and routine maternity care | Control: 18.7% (15.4 to 22.1) |
Opinion leader education: 21.4% (16.8 to 26.1) |
‐ | ||
| Audit and feedback results in little or no difference in unscheduled caesarean section rate compared to routine maternity care | Control: 18.7% (15.4 to 22.1) |
Audit and feedback: 18.6% (13.9 to 23.2) |
‐ | |||
| Spontaneous vaginal birth | Physician education by opinion leader (obstetrician‐gynaecologist) increases vaginal birth compared to routine maternity care | Control: 14.5% (10.3 to 18.7) |
Opinion leader education: 25.3% (19.3 to 31.2) |
‐ | ||
| Audit and feedback results in little or no difference in spontaneous vaginal birth rate compared to routine maternity care | Control: 14.5% (10.3 to 18.7) |
Audit and feedback: 11.8% (5.8 to 17.7) |
‐ | |||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal morbidity | Physician education by opinion leader (obstetrician‐gynaecologist) results in little or no difference in low Apgar score < 7 at 5 minutes compared to routine maternity care | Control: 1.2 (0.0 to 2.4) | Opinion leader education: 0.9 (0.0 to 2.6) | ‐ |
㊉㊉㊉㊉ HIGH |
|
| Rates of low Apgar score < 7 at 5 minutes were higher in audit and feedback group compared to routine maternity care | Control: 1.2 (0.0 to 2.4) | Audit and feedback: 5.9 (4.2 to 7.6) | ‐ | |||
|
Education of public health nurses on childbirth classes (Finland) (Hemminki 2008, cluster‐randomised trial) |
Caesarean section | Education of public health nurses on childbirth classes may lead to little or no difference in caesarean section rate compared to routine maternity care | 160 per 1000 | 198 per 1000 (159 to 242) |
OR 1.29 (0.99 to 1.67) |
㊉㊉㊀㊀ LOWa,b |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Peer review plus mandatory second opinion for caesarean section indication (Taiwan) (Liang 2004, interrupted time series study) |
Caesarean section | The effect of peer review plus mandatory second opinion for caesarean section indication on caesarean births is uncertain | Change in level of total caesarean deliveries at 12 monthsc: ‐2.4% (‐11.4 to 6.7); change in slopec: 1.34% (‐2.5 to 5.2). |
㊉㊀㊀㊀ VERY LOWd |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Audit and feedback using Robson classification (Chile) (Scarella 2011, interrupted time series study) |
Caesarean section | The effect of audit and feedback using Robson classification on caesarean section births is uncertain | Change in level of caesarean deliveries during interventionc: ‐11% (‐23.2 to 1.2), NS; change in slopec ‐1.1% (‐6.4 to 4.2), NS Change in level of caesarean deliveries in the immediate post‐intervention period compared with the intervention periodc: 8.6% (2.1 to 15.2), P = 0.022; change in slopec: ‐0.3% (‐1.6 to 0.9), NS |
㊉㊀㊀㊀ VERY LOWc |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Audit and feedback plus financial incentive (Iran) (Mohammadi 2012, controlled before‐after studies (reanalysed using interrupted time series methods)) |
Caesarean section | The effect of audit and feedback plus financial incentive on caesarean section births is uncertain | Change in level of caesarean deliveries during the interventionc: ‐14.6% (‐24.4 to ‐4.8), P = 0.02; change in slopec: ‐0.07% (‐1.5 to 1.3), NS |
㊉㊀㊀㊀ VERY LOWd |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Audit and feedback plus 24‐hour in‐house coverage by dedicated physician (USA) (Poma 1998, interrupted time series study) |
Caesarean section | The effect of audit and feedback plus 24‐hour in‐house coverage by a dedicated physician on caesarean section births is uncertain | Change in level of total caesarean deliveries (primary and repeat caesarean sections) at 24 monthsc: ‐6.6% (‐10.1 to ‐3.2); change in slopec: ‐0.11% (‐0.25 to 0.02) (data reanalysed) |
㊉㊀㊀㊀ VERY LOWd |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| ǂThe corresponding risk (absolute effect with intervention) (and its 95% confidence interval) is based on the assumed risk in the comparison group ((i.e. risk with control) and the relative effect of the intervention (and its 95% CI). About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as ‘quality of evidence’ or ‘confidence in the estimate’ †Substantially different = a large enough difference that it might affect a decision. CI: confidence interval; NR: not reported; NS: not significant; RD: risk difference; RR: risk ratio. | ||||||
|
aDowngraded one level for serious risk of bias (pilot study with no sample size calculation; unit of analysis error). bDowngraded one level for serious imprecision (confidence interval includes null effect) cTwo standardised effect sizes are obtained from ITS analysis: change in level (also called ‘step change’) and change in trend (also called ‘change in slope’) before and after the intervention. Change in level = difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; Change in trend = difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in caesarean section rate. dDowngraded one level for possible confounding (unclear whether the intervention occurred independently of other changes over time). | ||||||
Summary of findings 3. Interventions targeted at healthcare organisations or facilities.
| Intervention | Primary outcome measure | Plain language summary | Absolute effectǂ |
Relative effect (95% CI) |
Certainty (GRADE) | |
| with control |
with intervention (95% CI) |
|||||
| Financial interventions targeted at healthcare professionals | ||||||
|
Insurance reforms equalising physician fees for vaginal and caesarean section deliveries (USA) (Keeler 1996, interrupted time series study) |
Caesarean section | The effect of insurance reforms equalising physician fees for vaginal and caesarean section deliveries on caesarean births is uncertain | Caesarean section rates for non‐breech deliveries decreased by 1.2% (22.5% before reform versus 21.3% after reform) |
㊉㊀㊀㊀ VERY LOWa |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Insurance reforms equalising physician fees for vaginal and caesarean section deliveries (Taiwan) (Lo 2008, interrupted time series study) |
Caesarean section | The effect of insurance reforms equalising physician fees for vaginal and caesarean section deliveries on caesarean births is uncertain | The change in the level of total caesarean section rate following the rise in VBAC fees was ‐1.68 (95% CI ‐2.3 to ‐1.07); the change in slope was ‐0.004 (95% CI ‐0.05 to 0.04)b The change in the level of total caesarean section rate (for all indications and order of birth) following the rise in vaginal birth fees was 1.19 (95% CI ‐0.01 to 2.40) and the change in slope was ‐0.43 (95% CI ‐0.78 to ‐0.09)b |
㊉㊀㊀㊀ VERY LOWa |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Different staffing models of delivery care | ||||||
|
Collaborative midwifery‐labourist care (versus private model of care) (USA) (Rosenstein 2015, interrupted time series study) |
Primary caesarean section | Collaborative midwifery‐labourist care may reduce primary caesarean section compared to private model of care | Primary caesarean rate among privately insured women decreased from 31.7% to 25.0% (OR 0.56, 95% CI 0.39 to 0.81). Interrupted time series analysis estimated a 7% drop in the primary caesarean rate in the year after the intervention, and a decrease of 1.7% per year thereafter |
㊉㊉㊀㊀ LOWc |
||
| VBAC | Collaborative midwifery‐labourist care may increase VBAC compared to private model of care | VBAC rate increased from 13.3% before to 22.4% after the intervention (OR 2.03, 95% CI 1.08 to 3.80) | ||||
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
|
Labourist model of obstetric care (versus traditional model of obstetric care) (USA) (Srinivas 2016, controlled before‐after study) |
Caesarean section | Labourist model of obstetric care may lead to little or no difference in caesarean section rate compared to traditional model of obstetric care | Non‐labourist before: 28.5% (46,486 births) Non‐labourist after: 31.8% (42,348 births) |
Labourist before: 32.6% (47,206 births) Labourist after: 33.6% (35,210 births) |
OR 1.02 (0.97 to 1.1) |
㊉㊉㊀㊀ LOWc |
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal morbidity | Labourist model of obstetric care may lead to little or no difference in chorioamnionitis compared to traditional model of obstetric care | Non‐labourist before, % (N): 6.2 (10,018) Non‐labourist before, % (N): 4.8 (6339) |
Labourist before, % (N): 3.8 (5549) Labourist after, % (N): 3.5 (3814) |
OR 1.07 (0.88 to 1.30) |
㊉㊉㊀㊀ LOWc |
|
| Neonatal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal morbidity | Labourist model of obstetric care may lead to little or no difference in low Apgar (less than 7) at 5 minutes compared to traditional model of obstetric care | Non‐labourist before, % (N): 0.4 (557) Non‐labourist after, % (N): 0.4 (476) |
Labourist before, % (N): 0.2 (216) Labourist after, % (N): 0.2 (223) |
OR 1.09 (0.69 to 1.72) |
㊉㊉㊀㊀ LOWc |
|
| Labourist model of obstetric care may lead to little or no difference in birth asphyxia compared to traditional model of obstetric care | Non‐labourist before, % (N): 0.3 (398) Non‐labourist after, % (N): 0.2 (247) |
Labourist before, % (N): 0.2 (310) Labourist after, % (N): 0.2 (171) |
OR 0.75 (0.48 to 1.18) |
㊉㊉㊀㊀ LOWc |
||
| ǂThe corresponding risk (absolute effect with intervention) (and its 95% confidence interval) is based on the assumed risk in the comparison group ((i.e. risk with control) and the relative effect of the intervention (and its 95% CI). About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as ‘quality of evidence’ or ‘confidence in the estimate’ †Substantially different = a large enough difference that it might affect a decision. CI: confidence interval; NR: not reported; OR: odds ratio; RR: risk ratio; VBAC: vaginal birth after caesarean. | ||||||
|
aDowngraded one level for serious risk of bias (due to possible confounding of outcome; unclear whether the intervention occurred independently of other changes over time). bTwo standardised effect sizes are obtained from interrupted time series analysis: a change in level (also called ‘step change’) and a change in trend (also called ‘change in slope’) before and after the intervention. Change in level = difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; change in trend = difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in caesarean section rate. cObservational study which start at low certainty evidence according to GRADE (we did not downgrade or upgrade the certainty of evidence). | ||||||
Summary of findings 4. 'Cross‐cutting' interventionsa.
| Intervention | Primary outcome measure | Plain language summary | Absolute effectǂ | Relative effect (95% CI) |
Certainty (GRADE) |
|
| with control | with intervention | |||||
|
Multifaceted programme comprising education programme for hospital staff and women, audit of surgeon practices, public health campaign, monitoring rates of caesarean sections and neonatal outcomes (China) (Runmei 2012, controlled before‐after study) |
Caesarean section | The effect of multifaceted programme on caesarean section rate is uncertain | Change in level of caesarean deliveries during intervention: ‐13.4% (95% CI ‐19.6 to ‐7.1)b Change in slope of caesarean deliveries: ‐0.72% (95% CI ‐3 to 1.5)b |
㊉㊀㊀㊀ VERY LOWc |
||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Instrumental vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal morbidity | The effect of multifaceted programme on maternal morbidity is uncertain | "We found a significant increase in the incidence of all obstetric complications, with the exception of placental abruption, after 2004" |
㊉㊀㊀㊀ VERY LOWc |
|||
| Neonatal morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal morbidity | The effect of multifaceted programme on neonatal morbidity is uncertain | "The incidence of birth asphyxia did not increase after 2004 (P = 0.303)" |
㊉㊀㊀㊀ VERY LOWc |
|||
| Maternal or neonatal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
|
Multifaceted programme comprising transmission of information on caesarean section, training of health workers on best obstetric practices and inclusion of caesarean section rates as a criterion for hospital funding (Portugal) (Ayres‐De‐Campos 2015, interrupted time series study) |
Caesarean section | The effect of multifaceted programme on rates of caesarean section, VBAC and instrumental birth is uncertain | In the period between 2009 and 2014, representing the possible influence of the programme: rates of caesarean section in the study region decreased by 20.0% (from 36.0% to 28.8%, time trend P < 0.001)b; rates of instrumental vaginal delivery increased by 33.1% (from 13.7% to 18.2%, time trend P < 0.001)b; rates of VBAC increased by 99.8% (from 16.4% to 32.8%, time trend P < 0.001)b |
㊉㊀㊀㊀ VERY LOWc |
||
| VBAC | ||||||
| Instrumental vaginal birth | ||||||
| Spontaneous vaginal birth | NR | ‐ | ‐ | ‐ | ‐ | |
| Maternal mortality or morbidity | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal mortality | NR | ‐ | ‐ | ‐ | ‐ | |
| Neonatal morbidity | The effect of multifaceted programme on hypoxia‐related complications is uncertain | The incidence of hypoxia‐related complications decreased by 14.1% (from 0.71% to 0.61%, time trend P < 0.001)b | ㊉㊀㊀㊀ VERY LOWc |
|||
| ǂThe corresponding risk (absolute effect with intervention) (and its 95% confidence interval) is based on the assumed risk in the comparison group ((i.e. risk with control) and the relative effect of the intervention (and its 95% CI). About the certainty of the evidence (GRADE)* High: this research provides a very good indication of the likely effect; the likelihood that the effect will be substantially different† is low. Moderate: this research provides a good indication of the likely effect; the likelihood that the effect will be substantially different† is moderate. Low: this research provides some indication of the likely effect; however, the likelihood that it will be substantially different† is high. Very low: this research does not provide a reliable indication of the likely effect; the likelihood that the effect will be substantially different† is very high. *This is sometimes referred to as ‘quality of evidence’ or ‘confidence in the estimate’ †Substantially different = a large enough difference that it might affect a decision. CI: confidence interval; NR: not reported; VBAC: vaginal birth after caesarean. | ||||||
|
aMultifaceted interventions with components targeted at women, healthcare professionals or healthcare organisations. bTwo standardised effect sizes are obtained from interrupted time series analysis: a change in level (also called ‘step change’) and a change in trend (also called ‘change in slope’) before and after the intervention. Change in level = difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend; change in trend = difference between post‐ and pre‐intervention slopes. A negative change in level and slope indicates a reduction in caesarean section rate. cDowngraded one level for serious risk of bias (due to possible confounding of outcome, unclear whether the intervention occurred independently of other changes over time). | ||||||
1. Interventions targeted at women or families
See: Table 1
1.1 Education, birth preparation classes and support programmes
Data from three of the 15 studies included in this category, suggest that the following interventions may reduce caesarean section rates.
Childbirth training workshop (mothers alone versus control: risk ratio (RR) 0.55, 95% confidence interval (CI) 0.33 to 0.89; 60 participants, low‐certainty evidence); (couple versus control: RR 0.59, 95% CI 0.37 to 0.94; 60 participants, low‐certainty evidence; Valiani 2014, randomised trial).
Nurse‐led applied relaxation training programme (RR 0.22, 95% CI 0.11 to 0.43; 104 participants, low‐certainty evidence; Bastani 2006, randomised trial).
Psychosocial couple‐based prevention programme (RR 0.53, 95% CI 0.32 to 0.90, reanalysed; 147 participants, low‐certainty evidence; Feinberg 2015, randomised trial).
Data from two studies suggest that the following two interventions may increase rates of vaginal births.
Childbirth training workshop (mothers alone versus control: RR 2.25, 95% CI 1.16 to 4.36; 60 participants, low‐certainty evidence); (couple versus control: RR 2.13, 95% CI 1.09 to 4.16; 60 participants, low‐certainty evidence; Valiani 2014, randomised trial).
Psychoeducation (RR 1.33, 95% CI 1.11 to 1.61; 371 participants, low‐certainty evidence; Rouhe 2013, randomised trial).
Limited data were available on the effect of the four interventions on maternal and neonatal mortality or morbidity.
There was little or no difference in caesarean section rates between standard maternity care and the following seven interventions.
Antenatal education programme for physiologic childbirth (RR 1.03, 95% CI 0.72 to 1.49; 150 participants, moderate‐certainty evidence; Masoumi 2016, randomised trial).
Pelvic floor muscle training exercises with telephone follow‐up versus pelvic floor muscle training exercises without telephone follow‐up (RR 0.87, 95% CI 0.37 to 2.04; 90 participants, low‐certainty evidence; Wang 2014, randomised trial).
-
Antenatal education on natural childbirth preparation with training in breathing and relaxation techniques:
elective caesarean section: RR 0.95, 95% CI 0.58 to 1.56; 977 participants, moderate‐certainty evidence;
emergency caesarean section: RR 0.91, 95% CI 0.67 to 1.23; 977 participants, moderate‐certainty evidence (Bergstrom 2009, randomised trial).
Psychoeducation (RR 0.70, 95% CI 0.49 to 1.01; 371 participants, low‐certainty evidence; Rouhe 2013, randomised trial).
-
Computer‐based decision aids (information programme, decision analysis):
information group versus usual care group, elective caesarean section: RR 0.98, 95% CI 0.82 to 1.18, 478 participants, moderate‐certainty evidence;
information group versus usual care group, emergency caesarean section: RR 1.09, 95% CI 0.77 to 1.55, 478 participants, moderate‐certainty evidence;
decision analysis group versus usual care group, elective caesarean section: RR 0.83, 95% CI 0.68 to 1.02, 478 participants, moderate‐certainty evidence;
decision analysis group versus usual care group, emergency caesarean section: RR 1.05, 95% CI 0.74 to 1.50, 478 participants, moderate‐certainty evidence (Montgomery 2007, randomised trial).
Decision aid booklet (absolute change from baseline 26.2% versus control 22.6%; 227 participants, moderate‐certainty evidence; Shorten 2005, randomised trial).
Intensive group therapy (cognitive behavioural therapy and childbirth psychotherapy): RR 0.90, 95% CI 0.65 to 1.24; 176 participants, low‐certainty evidence (Saisto 2001, randomised trial).
The effect of psychoeducation sessions by telephone (Fenwick 2015, randomised trial), and prenatal education for husbands of pregnant women on caesarean section rates is uncertain (very low‐certainty evidence) (Sharifirad 2013, randomised trial).
Details of the effect estimates and GRADE certainty ratings are summarised in Table 9.
1.2 Different formats of educational interventions
Data from three studies assessing different formats of educational interventions showed little or no differences in rates of caesarean section or vaginal birth after caesarean between formats.
Role play versus standard education using lectures (caesarean section: RR 0.66, 95% CI 0.39 to 1.12; 67 participants, low‐certainty evidence; Navaee 2015, randomised trial).
Interactive decision aid versus educational brochures (vaginal birth after caesarean: 41% versus 37%; number of participants unclear, low‐certainty evidence; Eden 2014, randomised trial).
Individualised prenatal education and support programme versus written information in pamphlet (caesarean section: RR 0.92, 95% CI 0.82 to 1.03); (vaginal birth after caesarean, RR 1.08, 95% CI 0.97 to 1.21; 1275 participants, moderate‐certainty evidence; Fraser 1997, randomised trial).
Maternal and neonatal mortality or morbidity, where reported, were similar between study groups.
Details of the effect estimates and GRADE certainty ratings are summarised in Table 9.
2. Interventions targeted at healthcare professionals
See: Table 2
Among the eight interventions targeted at healthcare professionals, we found two that slightly reduced caesarean section rates (Althabe 2004; Chaillet 2015) and one that reduced caesarean section rate (Lomas 1991).
Implementation of clinical guidelines combined with mandatory second opinion for caesarean section indication versus routine maternity care (overall caesarean section, mean difference in rate change ‐1.9, 95% CI ‐3.8 to ‐0.1; high‐certainty evidence; Althabe 2004, cluster‐randomised trial).
Implementation of clinical guidelines combined with audit and feedback versus routine maternity care (overall caesarean section, risk difference (RD) ‐1.8%, 95% CI ‐3.8 to ‐0.2; high‐certainty evidence; Chaillet 2015, cluster‐randomised trial).
Physician education by local opinion leader versus routine maternity care (elective caesarean section, opinion leader education: 53.7%, 95% CI 46.5 to 61.0%; control: 66.8%, 95% CI 61.7 to 72.0%; high‐certainty evidence; Lomas 1991, cluster‐randomised trial).
There was little or no difference in maternal and neonatal mortality or morbidity between study groups, where reported, in the three studies (Table 11).
An economic evaluation of a multifaceted intervention implemented by Chaillet and colleagues showed that the intervention group experienced per‐patient reductions of 0.005 caesarean sections (95% CI ‐ 0.015 to 0.004, P = 0.09), which translated to CAD 180 (95% CI ‐277 to ‐83, P < 0.001; Chaillet 2015). The intervention was “dominant” (effective in reducing caesarean section rates and less costly than usual care) in 86.08% of simulations. It reduced costs in 99.99% of simulations. Cost reductions were driven by lower rates of neonatal complications in the intervention group (CAD ‐190, 95% CI ‐255 to ‐125, P < 0.001). The authors estimated that given 88,000 annual provincial births, a similar intervention could save CAD 15.8 million (range: 7.3 to 24.4 million) in Quebec annually (Johri 2017, economic evaluation of Chaillet 2015). Further prospective analysis to measure the budget impact of the multifaceted intervention showed that it led to savings of CAD 27 million in Quebec over four years, and that in the short to medium term, extending the intervention nationwide could lead to savings of CAD 150.5 million (Bermúdez‐Tamayo 2018, economic evaluation of Chaillet 2015).
There was little or no difference in caesarean section rates between the following two interventions and control.
Education of public health nurses on childbirth classes (odds ratio (OR) 1.29, 95% CI 0.99 to 1.67; 1568 participants, Low‐certainty evidence; Hemminki 2008, cluster‐randomised trial).
-
Audit and feedback and local opinion leader education:
elective caesarean section, audit and feedback: 69.7%, 95% CI 62.4 to 77.0;
unscheduled caesarean section, audit and feedback: 18.6%, 95% CI 13.9 to 23.2;
opinion leader education: 21.4%, 95% CI 16.8 to 26.1; control: 18.7%, 95% CI 15.4 to 22.1; high‐certainty evidence (Lomas 1991, cluster‐randomised trial).
The effect of the following interventions on caesarean section rates is uncertain (very low‐certainty evidence).
Peer review plus mandatory second opinion (Liang 2004, interrupted time series study).
Audit and feedback using the Robson classification (Scarella 2011, interrupted time series study).
Audit and feedback plus a financial incentive (Mohammadi 2012, controlled before‐after studies (reanalysed using interrupted time series methods)).
Audit and feedback plus 24‐hour in‐house coverage by a dedicated physician (Poma 1998, interrupted time series study).
Details of the effect estimates and GRADE certainty ratings are summarised in Table 11.
3. Interventions targeted at healthcare organisations or facilities
See: Table 3
3.1 Financial interventions targeted at healthcare professionals
Two studies involving insurance reforms equalising physician fees for vaginal births and caesarean sections were included in this category. The effect of these strategies on caesarean section rates is uncertain (very low‐certainty evidence) (Keeler 1996; Lo 2008, both interrupted time series studies). Maternal and neonatal mortality or morbidity were not reported.
Details of the effect estimates and GRADE certainty ratings are summarised in Table 13.
3.2 Different staffing models of delivery care
The collaborative midwifery‐labourist model of care (in which the obstetrician provides in‐house labour and delivery coverage, 24 hours a day, without competing clinical duties) may reduce caesarean section rates, and may increase rates of vaginal birth after caesarean section, compared to the private model of care (Rosenstein 2015, interrupted time series study).
The primary caesarean section rate among privately insured women decreased from 31.7% to 25.0% (OR 0.56, 95% CI 0.39 to 0.81). The interrupted time series analysis estimated a 7% drop in the primary caesarean rate in the year after the intervention, and a decrease of 1.7% per year thereafter (low‐certainty evidence).
The rate of vaginal births after caesarean section increased from 13.3% before to 22.4% after the intervention (OR 2.03, 95% CI 1.08 to 3.80; low‐certainty evidence).
Maternal and neonatal mortality or morbidity were not reported.
The labourist model of obstetric care, compared to routine delivery care, may lead to little or no difference in the following outcomes (Srinivas 2016, controlled before‐after study).
Caesarean section (OR 1.02, 95% CI 0.97 to 1.1; low‐certainty evidence).
Maternal morbidity (chorioamnionitis) (OR 1.07, 95% CI 0.88 to 1.30; low‐certainty evidence).
Neonatal morbidity (birth asphyxia) (OR 0.75, 95% CI 0.48 to 1.18; low‐certainty evidence).
Maternal and neonatal mortality were not reported.
Details of the effect estimates and GRADE certainty ratings are summarised in Table 13.
4. 'Cross‐cutting' interventions
See: Table 4
The effect of the following two multifaceted interventions on caesarean section rate and maternal and neonatal morbidity is uncertain (the certainty of available evidence is very low).
Programme comprising education for hospital staff and women, audit of surgeon practices, public health campaign, monitoring rates of caesarean sections and neonatal outcomes (Runmei 2012, controlled before‐after study).
Programme comprising transmission of information on caesarean section, training of healthcare workers on best obstetric practices and inclusion of caesarean section rates as a criterion for hospital funding (Ayres‐De‐Campos 2015, interrupted time series study).
Maternal or neonatal mortality were not reported in either studies. Details of effect estimates and GRADE certainty ratings are summarised in Table 15.
Discussion
Summary of main results
This review examined evidence from 29 studies assessing the effectiveness and safety of non‐clinical interventions intended to reduce caesarean section births. The studies assessed a range of interventions, targeting various stakeholders (women, families, healthcare professionals and healthcare organisations or facilities), mostly in high‐income countries. The summarised evidence is drawn from single studies assessing distinct interventions. Limited data were available on maternal and neonatal mortality and morbidity.
Overall, we found eight interventions to have a beneficial effect on at least one primary outcome measure with low‐, moderate‐ or high‐certainty evidence, and no moderate‐ or high‐certainty evidence of adverse effects: childbirth training workshop; nurse‐led applied relaxation training programme; psychosocial couple‐based prevention programme; psychoeducation; implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication; implementation of clinical practice guidelines combined with audit and feedback; physician education by local opinion leader (obstetrician‐gynaecologist); and collaborative midwifery–labourist model of care.
The review targeted settings with high rates of caesarean section rates, where large numbers of caesarean births are assumed to be unnecessary. However, the proportion of unnecessary caesarean sections was not reported in the included studies and it is unclear whether the observed changes in caesarean section rates occurred exclusively in those considered unnecessary. Given this uncertainty, caution should be exercised when interpreting the findings of this review.
Overall completeness and applicability of evidence
The summarised evidence is derived from a mixed population of pregnant women (nulliparous women, multiparous women, women with a fear of childbirth, women with high levels of anxiety, women having undergone a previous caesarean section, couples, husbands of pregnant women, and pregnant women with no particular health condition).
We did not identify any eligible studies that addressed five prespecified interventions: public dissemination of caesarean section rates; goal‐setting for caesarean section rates; policies that limit financial or legal liability in case of litigation of healthcare professionals or organisations; changing the physical or sensory environment of labour and delivery; and strategies to change organisational culture.
There were insufficient data to explore effects across important subgroups (e.g. whether effects of educational interventions varied by format, intensity or duration of birth preparation classes). The absence of evidence on the optimal education format is particularly concerning given that antenatal education is an established component of maternity care worldwide. Given that many women are in contact with the health system for care during pregnancy, interventions targeting women and families appear an appealing strategy with capacity to reach a large proportion of women, ensuring they are informed and that they receive the necessary support for informed decision‐making. More research is needed to understand women‐related determinants of birth choices so that the content and format of educational interventions can be tailored to relevant determinants of caesarean births.
Limited data were available on maternal and neonatal morbidity and mortality and healthcare resource utilisation. Reliable cost‐effectiveness data were available only for one intervention (implementation of clinical practice guidelines combined with audit and feedback) (Johri 2017). We did not find studies that assessed long‐term maternal and infant outcomes. Future studies should address this knowledge gap.
Most of the included studies were conducted in high‐income countries. The review findings are mostly generalisable to similar settings. However, differences in the determinants of caesarean births and healthcare systems may limit generalisability in some settings (e.g. the labourist model of obstetric care is largely limited to USA settings) (Rosenstein 2015; Srinivas 2016). None of the included studies were conducted in low‐income countries.
Certainty of the evidence
The review included 29 studies evaluating a wide range of interventions. We judged the certainty of evidence to be high in only three comparisons (implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication, implementation of clinical practice guidelines combined with audit and feedback, local opinion leader education). The certainty of evidence for the remaining interventions varied from very low (indicating considerable uncertainty in the effect estimates) to moderate (indicating that further research is likely to have an important impact in our confidence in the effect estimate and may change the estimate).
We downgraded the level of evidence for most outcomes, primarily because of study risk of bias (due to inadequate sequence generation and allocation concealment procedures) and imprecision of effect (due to small sample sizes and few numbers of events). Although we cannot entirely exclude the possibility of publication bias, we judged the likelihood of missing relevant studies as low given the comprehensive literature searches implemented.
Potential biases in the review process
The review has a number of limitations. We excluded many studies because of ineligible designs. It is possible that some of these studies contribute useful data that might complement evidence from the included studies. We were not able to reanalyse data from some studies because insufficient information was available. It is likely that we missed a number of relevant interventions because of lack of clear taxonomy in the classification of non‐clinical interventions to reduce caesarean births. In addition, a number of relevant interventions were identified during the peer review process; we will consider these in the next update of the review. We judged that the two studies currently awaiting classification do not have any impact on the review conclusions
Agreements and disagreements with other studies or reviews
We identified six related reviews published in the last 10 years (Boatin 2018; Catling‐Paull 2011a; Chaillet 2007; Long 2016; Lundgren 2015; Nilsson 2015).
The reviews addressed a range of strategies intended to reduce caesarean births or increase vaginal birth after caesarean. Similar to our review, most of the studies included in the reviews were from high‐income countries and limited data were available on maternal and neonatal mortality and morbidity and costs. There were differences between the reviews and our review regarding search strategies (e.g. search periods covered), study eligibility criteria (e.g. our review excluded cohort studies), and criteria for assessing the certainty of evidence (e.g. our review applied GRADE system). These differences explain some of the differences in the conclusions reached by the reviews. Relevant findings of the reviews are summarised in Table 16.
12. Related systematic reviews.
|
Boatin 2018 assessed the effect of audit and feedback using the Robson classification to reduce caesarean section rates. Studies (any design) that used the Robson classification within clinical audit cycles (including but not limited to strategies using audit and feedback) either alone or in multifaceted interventions to reduce caesarean section rate were eligible for inclusion. Six studies were included. All the studies used prospective uncontrolled before‐after designs and none accounted for confounding, blinding or intervention integrity (i.e. the degree to which the participants received the intervention, and consistency of the intervention). All six studies reported reductions in caesarean section rates. The authors noted that the results should be interpreted with caution because of limited methodological quality of the included studies. Catling‐Paull 2011a assessed the effect of non‐clinical interventions intended to increase the uptake or the success rates of VBAC, or both. Twenty‐seven studies were included in the review (five randomised trials, one prospective cohort study, nine retrospective cohort studies, one case–control study and 11 before‐after studies). The findings showed that national guidelines influence VBAC rates, but a greater effect is seen when institutions develop local guidelines, adopt a conservative approach to caesarean section, use opinion leaders, give individualised information to women, and give feedback to obstetricians about mode of birth rates. Chaillet 2007 assessed the effectiveness of interventions intended to reduce cesarean section rate. Ten studies were included in the review (three randomised trials, two cluster‐randomised trials and five interrupted time series studies). Audit and feedback, quality improvement, and multifaceted strategies were found to be effective for reducing the cesarean section rate. Long 2016 assessed the effect of OMBUs embedded within hospitals which provide comprehensive emergency obstetric and newborn care. Three randomised trials, one controlled before‐after study and six cohort studies were included in the review. Three cohort studies (one each from UK, China and Nepal) found more spontaneous vaginal deliveries, fewer caesarean sections and fewer episiotomies performed in OMBUs compared to standard obstetric units. There were no differences in these outcomes in randomised trials and the remaining cohorts. There were no or very few maternal and perinatal deaths in either OMBUs or standard obstetric units. One study reported higher satisfaction with midwife‐led birth care among women and midwives in the OMBUs. Lundgren 2015 assessed the effect of clinician‐centred interventions designed to increase the rate of VBAC. Three randomised trials were included in the review. The use of external peer review, audit and feedback had no effect on VBAC rates. An educational strategy delivered by an opinion leader increased VBAC rates. Nilsson 2015 assessed the effectiveness of women‐centred interventions during pregnancy and birth to increase rates of VBAC. Randomised trials or cluster randomised trials were eligible for inclusion. Three trials were included in the review. Two studies evaluated the effectiveness of decision aids for mode of birth and one evaluated the effectiveness of an antenatal education programme. The findings show that neither the use of decision aids nor information/education of women have a significant effect on VBAC rates. |
OMBU: onsite midwife‐led birth units; VBAC: vaginal birth after caesarean.
Authors' conclusions
Implications for practice.
We evaluated a wide range of non‐clinical interventions intended to reduce unnecessary caesarean section births, targeting various stakeholders (women or families, healthcare professionals, healthcare organisations or facilities). Across all categories, we found eight interventions to have a beneficial effect on at least one primary outcome measure with low‐, moderate‐ or high‐certainty evidence, and no moderate‐ or high‐certainty evidence of adverse effects: childbirth training workshop; nurse‐led applied relaxation training programme; psychosocial couple‐based prevention programme; psychoeducation; implementation of clinical practice guidelines combined with mandatory second opinion for caesarean section indication; implementation of clinical practice guidelines combined with audit and feedback; physician education by local opinion leader (obstetrician‐gynaecologist); and collaborative midwifery–labourist model of care.
Decisions to implement the interventions in other settings need to take into account: the extent to which routine settings resemble those in the included studies (e.g. determinants of caesarean births), presence of specific groups who might benefit from the intervention (e.g. women having undergone previous caesarean section), organisation of healthcare system (e.g. staffing models of care), baseline rates of caesarean births, financial burden of the interventions, and availability of routine data (Lavis 2009).
Implications for research.
We have identified knowledge gaps in primary research based on uncertainty in the available evidence (due to very low‐ or low‐certainty evidence, applicability of evidence or lack of studies, particularly around interventions targeted at women or families and healthcare organisations or facilities). We have also provided recommendations to improve aspects of study methodology and reporting. The research priorities are summarised in Table 17. We identified eight ongoing trials.
13. Recommendations for future research.
| Further research should focus on the following areas | |
| Population | Pregnant women who may be at risk of delivering by caesarean section without a medical indication or need
|
| Settings |
|
| Study designs |
|
| Interventions | Multifaceted (rather than single‐component) interventions tailored to local determinants (facilitators) of caesarean section practices are recommended The certainty of evidence for caesarean section rate was low to very low for the following interventions. Further studies are needed to address the uncertainty in the effect of these interventions Educational interventions targeted at women or families
Interventions targeted at healthcare professionals
Interventions targeted at healthcare organisations or facilities
Although not specifically designed to reduce caesarean births, the following interventions examined in related reviews showed benefits in reducing caesarean births and improving other birth outcomes (further studies are required to confirm observed benefits in areas with high caesarean section rates)
We did not identify any eligible studies on the following prespecified interventions (outlined in Table 1); studies evaluating the effects of these interventions are needed. Use of opinion leaders
Public dissemination of caesarean section rates
Financial strategies for healthcare professionals or organisations
Goal setting for caesarean section rates
Policies that limit financial/legal liability in case of litigation of healthcare professionals or organisations (tort reforms) Changing the physical or sensory environment of labour and delivery
Strategies to change the organisational culture
|
| Outcomes |
|
| Methodological considerations | Classification of caesarean section
Taxonomy of caesarean section interventions
Reporting interventions
|
What's new
| Date | Event | Description |
|---|---|---|
| 8 March 2018 | New citation required and conclusions have changed | We amended the conclusions to highlight the limitation of the evidence examined. |
| 8 March 2018 | New search has been performed | We updated the searches in August 2014, February 2017 and March 2018. We expanded the scope of the review and added 17 new studies in this update. We implemented GRADE and created 'Summary of findings' tables. We amended the author team. Two studies (Jang 2011; Vankan 2015) identified in the March 2018 searches are awaiting classification. |
History
Protocol first published: Issue 4, 2005 Review first published: Issue 6, 2011
| Date | Event | Description |
|---|---|---|
| 26 June 2009 | Amended | Converted to new review format. |
Acknowledgements
We would like to acknowledge the support of the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Effective Practice and Organisation of Care (EPOC) Group. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the NIHR.
We would like to thank the following individuals who provided prepublication comments for this update: EPOC and Cochrane Editors, Gillian Leng, Celeste Naude, Jemma Hudson, Toby Lasserson and Julia Worswick; and Paul Miller (EPOC Information Specialist). We would also like to thank Susan Bewley and the following members of the Cochrane Pregnancy and Childbirth International Consumer Panel: Gill Gyte, Alina Bishop, Rachel Plachcinski, Misty Pratt and Carol Sakala.
Appendices
Appendix 1. Search strategies (March 2018)
MEDLINE (OVID)
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily, Ovid MEDLINE and Versions(R) <1946 to 7 March 2018>
| No. | Search terms | Results |
| 1 | exp cesarean section/ | 40707 |
| 2 | ((caesarean or cesarean) adj2 (section? or birth? or deliver* or surgery)).ti,ab,kf. | 51101 |
| 3 | c‐section?.ti,ab,kf. | 1033 |
| 4 | natural childbirth/ | 2330 |
| 5 | (natural adj (birth or childbirth)).ti,ab,kf. | 599 |
| 6 | ((operative or surgical) adj (birth* or deliver*)).ti,ab,kf. | 1790 |
| 7 | (unnecessary cesarean* or unnecessary caesarean*).ti,ab,kf. | 136 |
| 8 | or/1‐7 | 67346 |
| 9 | patient education as topic/ | 78996 |
| 10 | decision making/ | 82374 |
| 11 | exp clinical audit/ | 21032 |
| 12 | exp education, professional/ | 273591 |
| 13 | ((caesarean or cesarean) adj5 rate?).ti,ab,kf. | 6689 |
| 14 | CS rate?.ti,ab,kf. | 405 |
| 15 | (decision adj2 (aid? or tool?)).ti,ab,kf. | 7433 |
| 16 | (audit? or feedback or fed back).ti,ab,kf. | 145940 |
| 17 | opinion leader?.ti,ab,kf. | 1182 |
| 18 | second opinion?.ti,ab,kf. | 1782 |
| 19 | ((midwife* or midwive*) adj2 (led or lead* or intervention* or manag*)).ti,ab,kf. | 848 |
| 20 | ((educat* or teach* or learn*) adj5 (pregnan* or women or woman or mother* or father* or husband* or parent* or physician* or midwife* or midwive* or nurs* or obstetric* or program* or intervention* or workshop*)).ti,ab,kf. | 175663 |
| 21 | ((antenatal or birth* or childbirth) adj (program* or lesson* or class* or educat*)).ti,ab,kf. | 1380 |
| 22 | psychoeducation.ti,ab,kf. | 2188 |
| 23 | or/9‐22 | 704026 |
| 24 | 8 and 23 | 8934 |
| 25 | randomized controlled trial.pt. | 455307 |
| 26 | controlled clinical trial.pt. | 92216 |
| 27 | multicenter study.pt. | 229741 |
| 28 | pragmatic clinical trial.pt. | 690 |
| 29 | (randomis* or randomiz* or randomly).ti,ab. | 758637 |
| 30 | groups.ab. | 1769815 |
| 31 | (trial or multicenter or multi center or multicentre or multi centre).ti. | 211228 |
| 32 | (intervention? or effect? or impact? or controlled or control group? or (before adj5 after) or (pre adj5 post) or ((pretest or pre test) and (posttest or post test)) or quasiexperiment* or quasi experiment* or pseudo experiment* or pseudoexperiment* or evaluat* or time series or time point? or repeated measur*).ti,ab. | 8329902 |
| 33 | non‐randomized controlled trials as topic/ | 293 |
| 34 | interrupted time series analysis/ | 388 |
| 35 | controlled before‐after studies/ | 305 |
| 36 | or/25‐35 | 9300000 |
| 37 | exp animals/ | 21359264 |
| 38 | humans/ | 16926842 |
| 39 | 37 not (37 and 38) | 4432422 |
| 40 | review.pt. | 2351394 |
| 41 | meta analysis.pt. | 85606 |
| 42 | news.pt. | 186291 |
| 43 | comment.pt. | 707682 |
| 44 | editorial.pt. | 452023 |
| 45 | cochrane database of systematic reviews.jn. | 13470 |
| 46 | comment on.cm. | 707679 |
| 47 | (systematic review or literature review).ti. | 107442 |
| 48 | or/39‐47 | 7827358 |
| 49 | 36 not 48 | 6500762 |
| 50 | 24 and 49 | 4681 |
| 51 | (2010* or 2011* or 2012* or 2013* or 2014* or 2015* or 2016* or 2017* or 2018*).dt,dp,ed,ep,yr. | 9397266 |
| 52 | 50 and 51 | 2247 |
Embase (OVID)
Embase <1974 to 2018 March 7>
| No. | Search terms | Results |
| 1 | exp *cesarean section/ | 27445 |
| 2 | ((caesarean or cesarean) adj2 (section? or birth? or deliver* or surgery)).ti,ab,kw. | 69574 |
| 3 | c‐section?.ti,ab,kw. | 2676 |
| 4 | *natural childbirth/ | 1481 |
| 5 | (natural adj (birth or childbirth)).ti,ab,kw. | 585 |
| 6 | (unnecessary cesarean* or unnecessary caesarean*).ti,ab,kw. | 171 |
| 7 | ((operative or surgical) adj (birth* or deliver*)).ti,ab,kw. | 2589 |
| 8 | or/1‐7 | 78200 |
| 9 | *patient education/ | 27239 |
| 10 | *shared decision making/ | 783 |
| 11 | *patient decision making/ | 1805 |
| 12 | exp *decision support system/ | 9529 |
| 13 | *clinical audit/ | 516 |
| 14 | *vocational education/ | 4615 |
| 15 | *continuing education/ | 8940 |
| 16 | *education program/ | 9465 |
| 17 | *in service training/ | 6606 |
| 18 | *medical education/ | 104893 |
| 19 | *childbirth education/ | 118 |
| 20 | ((caesarean or cesarean) adj5 rate?).ti,ab,kw. | 9705 |
| 21 | CS rate?.ti,ab,kw. | 806 |
| 22 | (decision adj2 (aid? or tool?)).ti,ab,kw. | 10568 |
| 23 | (audit? or feedback or fed back).ti,ab,kw. | 206003 |
| 24 | opinion leader?.ti,ab,kw. | 1605 |
| 25 | second opinion?.ti,ab,kw. | 2822 |
| 26 | ((midwife* or midwive*) adj2 (led or lead* or intervention* or manag*)).ti,ab,kw. | 1036 |
| 27 | ((educat* or teach* or learn*) adj5 (pregnan* or women or woman or mother* or father* or husband* or parent* or physician* or midwife* or midwive* or nurs* or obstetric* or program* or intervention* or workshop*)).ti,ab,kw. | 215925 |
| 28 | ((antenatal or birth* or childbirth) adj (program* or lesson* or class* or educat*)).ti,ab,kw. | 1334 |
| 29 | psychoeducation.ti,ab,kw. | 3573 |
| 30 | or/9‐29 | 580458 |
| 31 | 8 and 30 | 12104 |
| 32 | randomized controlled trial/ | 490387 |
| 33 | controlled clinical trial/ | 455867 |
| 34 | quasi experimental study/ | 4309 |
| 35 | pretest posttest control group design/ | 330 |
| 36 | time series analysis/ | 20321 |
| 37 | experimental design/ | 15194 |
| 38 | multicenter study/ | 177380 |
| 39 | (randomis* or randomiz* or randomly).ti,ab. | 1044802 |
| 40 | groups.ab. | 2397974 |
| 41 | (trial or multicentre or multicenter or multi centre or multi center).ti. | 293432 |
| 42 | (intervention? or effect? or impact? or controlled or control group? or (before adj5 after) or (pre adj5 post) or ((pretest or pre test) and (posttest or post test)) or quasiexperiment* or quasi experiment* or pseudo experiment* or pseudoexperiment* or evaluat* or time series or time point? or repeated measur*).ti,ab. | 10604676 |
| 43 | or/32‐42 | 11829255 |
| 44 | (systematic review or literature review).ti. | 126655 |
| 45 | "cochrane database of systematic reviews".jn. | 11656 |
| 46 | exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ | 25647687 |
| 47 | human/ or normal human/ or human cell/ | 19376788 |
| 48 | 46 not (46 and 47) | 6318930 |
| 49 | 44 or 45 or 48 | 6456024 |
| 50 | 43 not 49 | 9017948 |
| 51 | 31 and 50 | 7507 |
| 52 | limit 51 to yr="2014 ‐Current" | 2630 |
The Cochrane Library (Wiley)
| No. | Search terms | Results |
| #1 | [mh "cesarean section"] | 2950 |
| #2 | ((caesarean or cesarean) near/2 (section? or birth? or deliver* or surgery)):ti,ab | 3174 |
| #3 | c‐section?:ti,ab | 12 |
| #4 | [mh "natural childbirth"] | 34 |
| #5 | (natural next (birth or childbirth)):ti,ab | 23 |
| #6 | ((operative or surgical) next (birth* or deliver*)):ti,ab | 249 |
| #7 | (unnecessary next cesarean* or unnecessary next caesarean*):ti,ab | 12 |
| #8 | {or #1‐#7} | 5068 |
| #9 | [mh "patient education as topic"] | 8530 |
| #10 | [mh "decision making"] | 3940 |
| #11 | [mh "clinical audit"] | 356 |
| #12 | [mh "education, professional"] | 4356 |
| #13 | ((caesarean or cesarean) near/5 rate?):ti,ab | 397 |
| #14 | (CS next rate?):ti,ab | 19 |
| #15 | (decision near/2 (aid? or tool?)):ti,ab | 455 |
| #16 | (audit? or feedback or fed back):ti,ab | 8865 |
| #17 | (opinion next leader?):ti,ab | 125 |
| #18 | (second next opinion?):ti,ab | 11 |
| #19 | ((midwife* or midwive*) near/2 (led or lead* or intervention* or manag*)):ti,ab | 131 |
| #20 | ((educat* or teach* or learn*) near/5 (pregnan* or women or woman or mother* or father* or husband* or parent* or physician* or midwife* or midwive* or nurs* or obstetric* or program* or intervention* or workshop*)):ti,ab | 19774 |
| #21 | ((antenatal or birth* or childbirth) next (program* or lesson* or class* or educat*)):ti,ab | 133 |
| #22 | psychoeducation:ti,ab | 906 |
| #23 | {or #9‐#22} | 40779 |
| #24 | #8 and #23 | 420 |
| #25 | #8 and #23 Publication Year from 2014 to 2018 | 154 |
Cinahl (EBSCO)
| No. | Search terms | Results |
| S1 | (MH "Cesarean Section+") | 9,860 |
| S2 | ((caesarean or cesarean) N2 (section? or birth? or deliver* or surgery)) | 5,413 |
| S3 | c‐section | 334 |
| S4 | (natural N0 (birth or childbirth)) | 212 |
| S5 | ((operative or surgical) N0 (birth* or deliver*)) | 378 |
| S6 | (unnecessary cesarean* or unnecessary caesarean*) | 53 |
| S7 | (MH "Prepared Childbirth") | 631 |
| S8 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 | 12,977 |
| S9 | (MH "Patient Education") | 44,761 |
| S10 | (MH "Childbirth Education") | 1,934 |
| S11 | (MH "Childbirth Educators") | 420 |
| S12 | (MH "Decision Making") | 24,928 |
| S13 | (MH "Decision Making, Patient") | 11,466 |
| S14 | (MH "Decision Support Techniques") | 2,550 |
| S15 | (MH "Audit") | 10,726 |
| S16 | (MH "Psychoeducation") | 1,990 |
| S17 | (MH "Education, Clinical") | 9,012 |
| S18 | MH "Education, Continuing") | 7,685 |
| S19 | ((caesarean or cesarean) N5 rate?) | 1,090 |
| S20 | CS rate? | 97 |
| S21 | (decision N2 (aid? or tool?)) | 1,043 |
| S22 | (audit? or feedback or fed back) | 21,596 |
| S23 | (opinion leader?) | 343 |
| S24 | (second opinion?) | 141 |
| S25 | ((midwife* or midwive*) N2 (led or lead* or intervention* or manag*)) | 1,170 |
| S26 | ((educat* or teach* or learn*) N5 (pregnan* or women or woman or mother* or father* or husband* or parent* or physician* or midwife* or midwive* or nurs* or obstetric* or program* or intervention* or workshop*)) | 159,310 |
| S27 | ((antenatal or birth* or childbirth) N0 (program* or lesson* or class* or educat*)) | 2,897 |
| S28 | psychoeducation | 2,356 |
| S29 | S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 274,020 |
| S30 | S8 AND S29 | 2,191 |
| S31 | PT randomized controlled trial | 42,986 |
| S32 | PT clinical trial | 55,844 |
| S33 | PT research | 1,186,187 |
| S34 | (MH "Randomized Controlled Trials") | 40,140 |
| S35 | (MH "Clinical Trials") | 92,783 |
| S36 | (MH "Intervention Trials") | 6,880 |
| S37 | (MH "Nonrandomized Trials") | 253 |
| S38 | (MH "Experimental Studies") | 17,663 |
| S39 | (MH "Pretest‐Posttest Design+") | 30,750 |
| S40 | (MH "Quasi‐Experimental Studies+") | 10,272 |
| S41 | (MH "Multicenter Studies") | 34,631 |
| S42 | (MH "Health Services Research") | 8,010 |
| S43 | TI ( randomis* or randomiz* or randomly) OR AB ( randomis* or randomiz* or randomly) | 140,270 |
| S44 | TI (trial or effect* or impact* or intervention* or before N5 after or pre N5 post or ((pretest or "pre test") and (posttest or "post test")) or quasiexperiment* or quasi W0 experiment* or pseudo experiment* or pseudoexperiment* or evaluat* or "time series" or time W0 point* or repeated W0 measur*) OR AB (trial or effect* or impact* or intervention* or before N5 after or pre N5 post or ((pretest or "pre test") and (posttest or "post test")) or quasiexperiment* or quasi W0 experiment* or pseudo experiment* or pseudoexperiment* or evaluat* or "time series" or time W0 point* or repeated W0 measur*) | 961,623 |
| S45 | S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 | 1,568,152 |
| S46 | S30 AND S45 | 1,426 |
| S47 | S46 Limiters ‐ Exclude MEDLINE records | 418 |
| S48 | S47 Limiters ‐ Published Date: 20140101‐20181231 | 239 |
ClinicalTrials.gov
| Search terms | Results |
| “caesarean section” OR “caesarean birth” OR “caesarean delivery” OR “cesarean section” OR “cesarean birth” OR “cesarean delivery” Interventional Studies |
229 |
WHO International Clinical Trials Registry Platform (ICTRP)
| Search terms | Results |
| caesarean or cesarean | 1972 |
Appendix 2. Search strategies (August 2014)
MEDLINE (OVID) (In‐Process & Other Non‐Indexed Citations) (search date: 6 August 2014)
1 exp Cesarean Section/ (0) 2 ((caesarean or cesarean) adj2 (section? or birth? or deliver$)).ti,ab. (3115) 3 c‐section?.ti,ab. (60) 4 or/1‐3 (3151) 5 exp *education, continuing/ or *pamphlets/ or *advance directives/ or *reminder systems/ or *feedback/ (0) 6 (education$ adj2 (program$ or intervention? or meeting? or session? or strateg$ or workshop? or visit?)).tw. (3881) 7 (leaflet? or booklet? or poster?).tw. (2015) 8 ((written or printed or oral) adj information).tw. (103) 9 (information$ adj2 campaign).tw. (16) 10 (education$ adj1 (method? or material?)).tw. (406) 11 (outreach or facilitator? or "academic detailing" or "consensus conference?" or algorithm? feedback or marketing).tw. (3426) 12 ((opinion or education$ or influential) adj1 leader?).tw. (98) 13 ((reminder? or recall) adj2 system?).ti,ab. (61) 14 (prompter? or prompting).tw. (485) 15 (chart adj2 review$).ti,ab. (2255) 16 ((effect? or impact or record? or chart?) adj2 audit).tw. (79) 17 or/5‐16 (12411) 18 exp *reimbursement mechanisms/ or *capitation fee/ or *"deductibles and coinsurance"/ or *hospital charges/ or *Medicaid/ or *medicare/ (0) 19 fee for service.tw. (195) 20 cost shar$.tw. (88) 21 (copayment? or co payment?).tw. (104) 22 (prepay$ or prepaid or prospective payment?).tw. (91) 23 (formular? or fundhold? or "blue cross").tw. (305) 24 or/18‐23 (740) 25 *nurse clinicians/ or *nurse midwives/ or *nurse practitioners/ or *pharmacists/ or *patient care team/ or exp* patient care planning/ or exp *ambulatory care facilities/ or *ambulatory care/ (1) 26 (nurse adj (rehabilitator? or clinician? or practitioner? or midwi$)).tw. (671) 27 clinical pharmacist?.tw. (179) 28 paramedic?.tw. (226) 29 (team? adj2 (care or treatment or assessment or consultation)).tw. (905) 30 (care adj2 (coordinat$ or program$ or continuity)).tw. (1542) 31 (case adj management).tw. (453) 32 or/25‐31 (3802) 33 *home care services/ or *hospices/ or *nursing homes/ or *office visits/ or *house calls/ or *day care/ or *aftercare/ or *community health nursing/ or *medical records/ or *medical records systems, computerized/ or *peer review/ or *utilization review/ or exp *health services misuse/ (0) 34 (chang$ adj1 location?).tw. (45) 35 domiciliary.tw. (87) 36 (home adj1 treat$).tw. (86) 37 day surgery.tw. (97) 38 (information adj2 (management or system?)).tw. (2370) 39 or/33‐38 (2682) 40 *physician's practice patterns/ or *process assessment/ or *program evaluation/ or *length of stay/ or exp *"Referral and Consultation"/ or "consultation"/ or *drug therapy, computer assisted/ or *medical history taking/ or *telephone/ or *health maintenance organizations/ (0) 41 quality assurance.tw. (1140) 42 (early adj1 discharg$).tw. (140) 43 discharge planning.tw. (94) 44 offset.tw. (2484) 45 triage.tw. (831) 46 near patient testing.tw. (7) 47 (physician patient adj (interaction? or relationship?)).tw. (103) 48 managed care.tw. (325) 49 (hospital? adj1 merg$).tw. (7) 50 or/40‐49 (5108) 51 ((standard or usual or routine or regular or traditional or conventional or pattern) adj2 care).tw. (4458) 52 (program$ adj2 (reduc$ or increas$ or decreas$ or chang$ or improv$ or modify$ or monitor$ or care)).tw. (3703) 53 (computer$ adj2 (dosage or dosing or diagnosis or therapy or decision?)).tw. (266) 54 ((introduc$ or impact or effect? or implement$ or computer$) adj2 protocol?).tw. (428) 55 ((effect or impact or introduc$) adj2 (legislation or regulations or policy)).tw. (133) 56 or/51‐55 (8846) 57 17 or 24 or 32 or 39 or 50 (23890) 58 (intervention? or multiintervention? or multi‐intervention? or postintervention? or post‐intervention? or preintervention? or pre‐intervention?).ti,ab. (49536) 59 (change or changing or evaluation or IMPROVE or IMPROVES or improvement? or improving).ti. (42422) 60 ((chang$ or improv$ or quality or evaluat$) adj3 (care or healthcare or organi?ation$ or practitioner? or practice)).ab. (9504) 61 implement$.ti. (3663) 62 (multi‐facet$ or multifacet$).ti,ab. (1402) 63 ((guideline? or pathway? or protocol?) adj3 (adhere$ or concord$ or uptake or up‐take)).ti,ab. (702) 64 ((physician? or provider? or practitioner?) adj2 behavio$).ti,ab. (211) 65 (collaborat$ or teambased or team‐based or interdisciplinar$ or inter‐disciplinar$ or cross‐disciplin$).ti,ab. or team?.ti. (10943) 66 effectiveness.ti. or (effective adj2 practice).ti,ab. (4620) 67 Guideline adherence.hw. (2) 68 (financial or payment?).ti. (838) 69 evidence‐based.ti,hw. (2041) 70 or/58‐69 [INTERVENTION terms] (112958) 71 intervention?.ti. or (intervention? adj6 (clinician? or collaborat$ or community or complex or DESIGN$ or doctor? or educational or family doctor? or family physician? or family practitioner? or financial or GP or general practice? or hospital? or impact? or improv$ or individuali?e? or individuali?ing or interdisciplin$ or multicomponent or multi‐component or multidisciplin$ or multi‐disciplin$ or multifacet$ or multi‐facet$ or multimodal$ or multi‐modal$ or personali?e? or personali?ing or pharmacies or pharmacist? or pharmacy or physician? or practitioner? or prescrib$ or prescription? or primary care or professional$ or provider? or regulatory or regulatory or tailor$ or target$ or team$ or usual care)).ab. (16931) 72 (pre‐intervention? or preintervention? or "pre intervention?" or post‐intervention? or postintervention? or "post intervention?").ti,ab. [added 2.4] (1427) 73 (hospital$ or patient?).hw. and (study or studies or care or health$ or practitioner? or provider? or physician? or nurse? or nursing or doctor?).ti,hw. (2) 74 demonstration project?.ti,ab. (88) 75 (pre‐post or "pre test$" or pretest$ or posttest$ or "post test$" or (pre adj5 post)).ti,ab. (7453) 76 (pre‐workshop or post‐workshop or (before adj3 workshop) or (after adj3 workshop)).ti,ab. (78) 77 trial.ti. or ((study adj3 aim?) or "our study").ab. (66512) 78 (before adj10 (after or during)).ti,ab. (22446) 79 ("quasi‐experiment$" or quasiexperiment$ or "quasi random$" or quasirandom$ or "quasi control$" or quasicontrol$ or ((quasi$ or experimental) adj3 (method$ or study or trial or design$))).ti,ab,hw. (11324) 80 ("time series" adj2 interrupt$).ti,ab,hw. (121) 81 (time points adj3 (over or multiple or three or four or five or six or seven or eight or nine or ten or eleven or twelve or month$ or hour? or day? or "more than")).ab. (894) 82 pilot.ti. (4001) 83 Pilot projects/ (0) 84 (clinical trial or controlled clinical trial or multicenter study).pt. (489) 85 (multicentre or multicenter or multi‐centre or multi‐center).ti. (2155) 86 random$.ti,ab. or controlled.ti. (74207) 87 (control adj3 (area or cohort? or compare? or condition or design or group? or intervention? or participant? or study)).ab. not (controlled clinical trial or randomized controlled trial).pt. (38069) 88 (control year? or experimental year? or (control period? or experimental period?)).ti,ab. [Added May 30‐2013] (718) 89 evaluation studies as topic/ or prospective studies/ or retrospective studies/ [Added Jan 2013] (4) 90 (utili?ation or programme or programmes).ti. [Added Jan 2013] (3980) 91 (during adj5 period).ti,ab. [Added Jan 2013] (19076) 92 ((strategy or strategies) adj2 (improv$ or education$)).ti,ab. [Added Jan 2013] (2141) 93 (purpose adj3 study).ab. (19505) 94 "comment on".cm. or review.pt. or (review not "peer review$").ti. or randomized controlled trial.pt. [Changed Jan 2013] (83817) 95 (rat or rats or cow or cows or chicken? or horse or horses or mice or mouse or bovine or animal?).ti,hw. or veterinar$.ti, ab,hw. [Edited May 2013] (51956) 96 exp animals/ not humans.sh. (5) 97 (or/71‐93) not (or/94‐96) [EPOC Methods Filter 2.6‐added Evaluation Studies line forward‐‐Jan 20130 Medline] (204923) 98 (randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or placebo.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti. (49946) 99 exp animals/ not humans.sh. (5) 100 98 not 99 [Cochrane RCT Filter 6.4.d Sens/Precision Maximizing] (49946) 101 4 and (57 or 70) and 97 [EPOC Results before date limits] (195) 102 4 and (57 or 70) and 100 [RCT Results before date limits] (68) 103 (201008$ or 2011$ or 2012$ or 2013$ or 2014$).em,dp,yr. (1269997) 104 101 and 103 [EPOC 2010‐2014] (178) 105 102 and 103 [RCT 2010‐2014] (61)
Embase (OVID) (search date: 6 August 2014)
1 exp Cesarean Section/ (67446) 2 ((caesarean or cesarean) adj2 (section? or birth? or deliver$)).ti,ab. (56175) 3 c‐section?.ti,ab. (1525) 4 or/1‐3 (78835) 5 continuing education/ or professional development/ or reminder system/ or clinical education/ or in service training/ [EM] (56167) 6 (education$ adj2 (program$ or intervention? or meeting? or session? or strateg$ or workshop? or visit?)).tw. (58016) 7 (leaflet? or booklet? or poster?).tw. (36092) 8 ((written or printed or oral) adj information).tw. (2293) 9 (information$ adj2 campaign).tw. (484) 10 (education$ adj1 (method? or material?)).tw. (7609) 11 outreach.tw. (10141) 12 ((opinion or education$ or influential) adj1 leader?).tw. (1247) 13 facilitator?.tw. (15931) 14 academic detailing.tw. (443) 15 consensus conference?.tw. (5452) 16 ((reminder? or recall) adj2 system?).ti,ab. (1079) 17 (prompter? or prompting).tw. (6695) 18 algorithm?.tw. (155893) 19 feedback.tw. (101865) 20 (chart adj2 review$).ti,ab. (38759) 21 ((effect? or impact or record? or chart?) adj2 audit).tw. (1336) 22 marketing.tw. (22911) 23 or/5‐22 (501449) 24 *reimbursement/ or capitation fee/ or hospital charge/ or *"cost"/ or medicare/ or medicaid/ [EM] (95147) 25 fee for service.tw. (4223) 26 cost shar$.tw. (1425) 27 (copayment? or co payment?).tw. (1772) 28 (prepay$ or prepaid or prospective payment?).tw. (4843) 29 formular?.tw. (4781) 30 fundhold?.tw. (1) 31 blue cross.tw. (1403) 32 or/24‐31 (107608) 33 advanced practice nurse/ or clinical nurse specialist/ or nurse midwife/ or nurse practitioner/ or pharmacist/ or *patient care planning/ or *ambulatory care/ or *ambulatory monitoring/ [EM] (95763) 34 (nurse adj (rehabilitator? or clinician? or practitioner? or midwi$)).tw. (12691) 35 clinical pharmacist?.tw. (2904) 36 paramedic?.tw. (4518) 37 (team? adj2 (care or treatment or assessment or consultation)).tw. (14467) 38 (care adj2 (coordinat$ or program$ or continuity)).tw. (24786) 39 (case adj management).tw. (8860) 40 or/33‐39 (148821) 41 exp *home care/ or hospice/ or hospice care/ or *nursing home/ or aftercare/ or *community health nursing/ or medical record/ or *health care utilization/ or *"utilization review"/ [EM] (217481) 42 (chang$ adj1 location?).tw. (455) 43 domiciliary.tw. (3296) 44 (home adj1 treat$).tw. (2100) 45 day surgery.tw. (2940) 46 (information adj2 (management or system?)).tw. (32814) 47 or/41‐46 (254076) 48 *program development/ or *health care quality/ or *"length of stay"/ or patient referral/ or anamnesis/ or computer assisted drug therapy/ or health maintenance organization/ or *telemedicine/ or teleconsultation/ or telemonitoring/ [EM] (275665) 49 quality assurance.tw. (24832) 50 (early adj1 discharg$).tw. (3027) 51 discharge planning.tw. (2691) 52 offset.tw. (21988) 53 triage.tw. (13606) 54 near patient testing.tw. (253) 55 (physician patient adj (interaction? or relationship?)).tw. (2236) 56 managed care.tw. (18676) 57 (hospital? adj1 merg$).tw. (416) 58 or/48‐57 (352044) 59 ((standard or usual or routine or regular or traditional or conventional or pattern) adj2 care).tw. (56059) 60 (program$ adj2 (reduc$ or increas$ or decreas$ or chang$ or improv$ or modify$ or monitor$ or care)).tw. (52493) 61 (computer$ adj2 (dosage or dosing or diagnosis or therapy or decision?)).tw. (4815) 62 ((introduc$ or impact or effect? or implement$ or computer$) adj2 protocol?).tw. (3946) 63 ((effect or impact or introduc$) adj2 (legislation or regulations or policy)).tw. (2021) 64 or/59‐63 (117274) 65 23 or 32 or 40 or 47 or 58 or 64 (1328796) 66 4 and 65 (5198) 67 controlled clinical trial/ or controlled study/ or randomized controlled trial/ [EM] (4454983) 68 randomi?ed.ti. or ((random$ or control) adj3 (group? or cohort? or patient? or hospital$ or department?)).ab. or (controlled adj2 (study or trial)).ti. (727293) 69 (multicenter and (study or trial)).ti. (22099) 70 (random sampl$ or random digit$ or random effect$ or random survey or random regression).ti,ab. not randomized controlled trial/ [Per BMJ Clinical Evidence filter] (58004) 71 (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) and (human/ or normal human/ or human cell/) (15174084) 72 (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) not 71 (5874509) 73 (or/67‐69) not (or/70,72) [RCT Filter for EMBASE] (3041624) 74 intervention?.ti. or (intervention? adj6 (clinician? or collaborat$ or community or complex or DESIGN$ or doctor? or educational or family doctor? or family physician? or family practitioner? or financial or GP or general practice? or hospital? or impact? or improv$ or individuali?e? or individuali?ing or interdisciplin$ or multicomponent or multi‐component or multidisciplin$ or multi‐disciplin$ or multifacet$ or multi‐facet$ or multimodal$ or multi‐modal$ or personali?e? or personali?ing or pharmacies or pharmacist? or pharmacy or physician? or practitioner? or prescrib$ or prescription? or primary care or professional$ or provider? or regulatory or regulatory or tailor$ or target$ or team$ or usual care)).ab. (215196) 75 (pre‐intervention? or preintervention? or "pre intervention?" or post‐intervention? or postintervention? or "post intervention?").ti,ab. [added 2.4] (14286) 76 (hospital$ or patient?).hw. and (study or studies or care or health$ or practitioner? or provider? or physician? or nurse? or nursing or doctor?).ti,hw. (1771656) 77 demonstration project?.ti,ab. (2410) 78 (pre‐post or "pre test$" or pretest$ or posttest$ or "post test$" or (pre adj5 post)).ti,ab. (103001) 79 (pre‐workshop or post‐workshop or (before adj3 workshop) or (after adj3 workshop)).ti,ab. (910) 80 trial.ti. or ((study adj3 aim?) or "our study").ab. (905869) 81 (before adj10 (after or during)).ti,ab. (485407) 82 (time points adj3 (over or multiple or three or four or five or six or seven or eight or nine or ten or eleven or twelve or month$ or hour? or day? or "more than")).ab. (12888) 83 pilot.ti. or (pilot adj (project? or study or trial)).ab. (93525) 84 (multicentre or multicenter or multi‐centre or multi‐center).ti. (41370) 85 random$.ti,ab. or controlled.ti. (969384) 86 (control adj3 (area or cohort? or compare? or condition or design or group? or intervention? or participant? or study)).ab. (643628) 87 ((evaluation or prospective or retrospective) adj study).ti,ab. [Added Jan 2013] (244113) 88 (utili?ation or programme or programmes).ti. [Added Jan 2013] (73041) 89 (during adj5 period).ti,ab. [Added Jan 2013] (416162) 90 ((strategy or strategies) adj2 (improv$ or education$)).ti,ab. [Added Jan 2013] (23681) 91 *experimental design/ or *pilot study/ or quasi experimental study/ (8891) 92 ("quasi‐experiment$" or quasiexperiment$ or "quasi random$" or quasirandom$ or "quasi control$" or quasicontrol$ or ((quasi$ or experimental) adj3 (method$ or study or trial or design$))).ti,ab. (129669) 93 ("time series" adj2 interrupt$).ti,ab. (1214) 94 or/74‐93 (4719795) 95 (rat or rats or cow or cows or chicken? or horse or horses or mice or mouse or bovine or animal?).ti. (1629462) 96 (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) and (human/ or normal human/ or human cell/) (15174084) 97 (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) not 96 (5874509) 98 94 not (or/95,97) [EPOC Filter 2.5‐‐Added Lines Jan. 2013] (4071232) 99 66 and 73 [RCT] (1058) 100 66 and 98 [EPOC] (2773) 101 99 or 100 [ALL] (3024) 102 remove duplicates from 101 (2997) 103 limit 102 to yr="2010 ‐Current" (1343)
Cochrane Central Register of Controlled Trials (OVID) (search date: 6 August 2014)
1 (cesarean? or caeserean? or c‐section? or "abdominal birth$" or "abdominal deliver$").ti,hw,sh. (3610) 2 (reduc$ or decreas$ or lower$ or intervention?).ti. (49575) 3 (reduc$ or decreas$ or lower$ or intervention?).ab. (293801) 4 ((reduc$ or decreas$ or prevent$ or lower$ or intervention?) adj4 (cesarean$ or caesarean$ or c‐section$ or "abdominal deliver$")).ab. (595) 5 ((increas$ or escalat$ or growing or rising) adj4 (cesarean$ or caesarean$ or c‐section$ or "abdominal deliver$")).ab. (199) 6 1 and (or/2‐3) (1686) 7 or/4‐5 (753) 8 7 or 6 (1939) 9 limit 8 to yr="2010 ‐Current" (517) 10 8 and new.uf. (86) 11 limit 1 to yr="2010‐2014" (751) 12 1 and NEW.uf. (127) 13 or/9‐12 (771)
Cochrane Library; CDSR, DARE, (WILEY) (search date: 6 August 2014)
1. MeSH descriptor Cesarean Section explode all trees 2. (cesarean* or caeserean* or c‐section* or "abdominal birth*" or "abdominal deliver*"):ti,ab,kw. 3. (reduc* or decreas* or lower* or intervention*):ti OR (reduc* or decreas* or lower* or intervention*):ab 4. reduc* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab 5. decreas* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab 6. prevent* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab 7. lower* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab. 8. intervention* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab. 9. increas* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab. 10. escalat* near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab. 11. growing near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab. 12. rising near/4 (cesarean* or caesarean* or c‐section* or "abdominal deliver*"):ab. 13. ((#1 or #2) and #3) 14. (#4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12) 15. #13 or #14 16. #15, from 2010 to 2014
CINAHL (Ebsco) (search date: 6 August 2014)
Limits: 2010‐2014 (((((MW ( cesarean )) or (TI ( c section* OR cesarean OR caesarean OR "abdominal deliver*" )) or (AB ( c section* OR cesarean OR caesarean OR "abdominal deliver*" ))) AND ((( TI ( reduc* OR lower OR rising OR decreas* ) OR AB ( reduc* OR lower OR rising OR decreas* ) ))))) AND ((((TI ( interrupt* N2 series )) or (TI ( interrupt* N2 series )) or (AB ( interrupt* N2 series ))) OR ((TI ( randomized OR randomised OR control* OR trial* ))) OR ((MW ( clinical trials )) or (MW ( random assignment OR Chi square test OR pretest posttest design ))) OR ((MW ( quasi experiment* OR quasiexperiment* )) or (TI ( quasi experiment* OR quasiexperiment* )) or (AB ( quasi experiment* OR quasiexperiment* ))) OR ((TI ( intervention OR interventions )) or (AB ( intervention OR interventions )) or (MW ( intervention OR interventions ))))))
Appendix 3. Search strategies (February 2017)
Database: Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations and Ovid MEDLINE(R) <1946 to 17 February>
1 Health Facility Environment/ (4101) 2 environment?.ti,ab. (448054) 3 "Interior Design and Furnishings"/ (4251) 4 (Interior adj3 Design?).ti,ab. (194) 5 (furniture or furnishing$).ti,ab. (2830) 6 floor$.ti,ab. (35402) 7 Lighting/ (10904) 8 (light$ or lighting).ti,ab. (544050) 9 Music/ (12033) 10 Odorants/ (15526) 11 (scent or smell or odor).ti,ab. (19660) 12 Temperature/ (215850) 13 (room adj3 temperature).ti,ab. (56103) 14 ((hospital or unit or ward or clinic or department$ or organisat$ or organizat$) adj3 (goal$ or target$ or purpose or object$)).ti,ab. (8257) 15 Organizational culture/ (14966) 16 (organi?ation$ adj3 cultur$).ti,ab. (3222) 17 (corporate culture? or workplace culture? or work culture? or organ?ation$ ethos or organi?ation$ climate?).ti,ab. (1087) 18 or/1‐17 (1313524) 19 Cesarean Section/ (39364) 20 ((caesarean or cesarean) adj2 (section? or birth? or deliver$)).ti,ab. (47343) 21 c‐section?.ti,ab. (868) 22 or/19‐21 (61302) 23 18 and 22 (1295)
Database: Embase <1974 to 2017 17 February>
1 *health care facility/ (23887) 2 environment?.ti,ab. (535512) 3 1 and 2 (1435) 4 exp furniture/ (28200) 5 (Interior adj3 Design?).ti,ab. (221) 6 (furniture or furnishing$).ti,ab. (3749) 7 floor$.ti,ab. (48549) 8 Lighting/ (24299) 9 (light$ or lighting).ti,ab. (595293) 10 Music/ (16527) 11 odor/ (29465) 12 (scent or smell or odor).ti,ab. (25163)
13 room temperature/ or air temperature/ or environmental temperature/ (65969) 14 (room adj3 temperature).ti,ab. (59353) 15 ((hospital or unit or ward or clinic or department$ or organisat$ or organizat$) adj3 (goal$ or target$ or purpose or object$)).ti,ab. (15597) 16 (organi?ation$ adj3 cultur$).ti,ab. (3576) 17 (corporate culture? or workplace culture? or work culture? or organ?ation$ ethos or organi?ation$ climate?).ti,ab. (1242) 18 or/3‐17 (844128) 19 *cesarean section/ (27961) 20 ((caesarean or cesarean) adj2 (section? or birth? or deliver$)).ti,ab. (64076) 21 c‐section?.ti,ab. (2282) 22 or/19‐21 (69962) 23 18 and 22 (1500)
WHO International Clinical Trials Registry Platform (ICTRP) (searched April 2017)
Search terms: "caesarean section OR caesarean birth OR caesarean delivery"
ClinicalTrials.gov (searched April 2017)
Search terms: "caesarean section OR caesarean birth OR caesarean delivery"
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Althabe 2004.
| Methods | Cluster‐randomised trial | |
| Participants | 34 hospitals* (Argentina, Brazil, Cuba, Guatemala and Mexico) with 149,276 women Hospitals with similar baseline caesarean section rate of 15% or greater and more than 1000 deliveries per year | |
| Interventions | Intervention: implementation of evidence‐based guidelines with mandatory second opinion Control: routine care as per local guidelines |
|
| Outcomes | Caesarean section rate including elective and intrapartum, maternal length of hospital stay, maternal, perinatal and neonatal complications | |
| Notes | *36 hospitals were randomised but 2 hospitals were excluded due to one hospital closing after randomisation and therefore the matched hospital was also excluded. Baseline (control group) CS rate: 24.6% Date of study: October 1998 to June 2000 Funding: European Union; Pan American Health Organization (PAHO/WHO); UNDP/UNFPA/WHO/World Bank Special Programme of Research; Development and Research Training in Human Reproduction of WHO; Research Support Fund of São Paulo State, Brazil; Maternal and Infant Programme, Buenos Aires, Argentina; Population Council‐Regional Office for Latin America and the Caribbean; Epidemiological Research Center in Reproductive and Sexual Health, Guatemala; and Center of Studies in Maternal and Child Health of Campinas, Brazil Conflicts of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Paired units randomly assigned...randomisation was independently done in the statistical unit of the UNDP/UNFPA/WHO...with SAS statistical software" |
| Allocation concealment (selection bias) | Low risk | "Paired units randomly assigned...randomisation was independently done in the statistical unit of the UNDP/UNFPA/WHO...with SAS statistical software" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Impact of possible performance bias on main outcomes considered minimal |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcomes (modes of delivery) objective |
| Baseline characteristics similar? | Low risk | "6‐month period of baseline data collection...hospitals were matched by country, type of hospital and baseline caesarean section rate" |
| Baseline outcome measurements similar? | Low risk | "6‐month period of baseline data collection...hospitals were matched by country, type of hospital and baseline caesarean section rate" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Low risk | Group contamination considered unlikely (allocation by hospital) |
| Other bias | Low risk | No evidence of other bias |
Ayres‐De‐Campos 2015.
| Methods | Interrupted time series | |
| Participants | Portugal Births occurring in Portugal between 2000 and 2014 |
|
| Interventions | Concerted action on transmission of information and training of healthcare professionals, together with the inclusion of CS rates as a criterion for hospital funding | |
| Outcomes | CS rate, perinatal and maternal mortality, instrumental vaginal delivery, VBAC, hypoxia‐related complications and perineal lacerations | |
| Notes | Governmental sources were used to obtain data on national CS, perinatal and maternal mortality rates Baseline (control group) CS rate: 30.6% Date of study: 2000 and 2014 Funding: the authors stated that “No funding was received for the conduction of this study. The initial stages of the described concerted action were funded by the North Healthcare Regional Administration.” Conflicts of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | High risk | "Concern over rising CS rates has increased in Portugal over the last years and it is impossible to evaluate how much of the observed change was in effect due to the concerted action" |
| Shape of the intervention effect pre‐specified? | High risk | Not stated |
| Intervention unlikely to affect data collection? | Low risk | "Data for national indicators were retrieved from official sources, whereas those of state‐owned hospitals were obtained from a database used for benchmarking and hospital funding, so it is likely that individual hospitals put an effort into the quality of their data" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All relevant prespecified outcomes reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Bastani 2006.
| Methods | Randomised trial | |
| Participants | Iran 110 primigravida women with high levels of anxiety (initial state/trait anxiety scores over 30) recruited from 3 prenatal clinics in Iran Inclusion criteria: primigravida women with a wanted pregnancy, aged 18 to 30, between 14 and 28 weeks' gestation, high levels of anxiety, uncomplicated singleton pregnancies and no identified medical or obstetrical risk factors Exclusion criteria: any medical or obstetric complication during the 7 weeks of intervention and elective caesarean section |
|
| Interventions | Nurse‐led 7‐week applied relaxation training in groups Control: routine hospital‐based prenatal care | |
| Outcomes | Non‐vaginal deliveries (surgical or caesarean section and instrumental deliveries including forceps and vacuum extraction), preterm birth, low birth weight | |
| Notes | Baseline (control group) CS rate: 40% Date of study: October 2002 to February 2003 Funding: Not reported Conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned to 2 groups, using a block randomisation method". Unclear on the size of the blocks |
| Allocation concealment (selection bias) | Unclear risk | "Randomly assigned to 2 groups, using a block randomisation method". Unclear on the size of the blocks |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcomes (modes of delivery) objective |
| Baseline characteristics similar? | Low risk | "No differences in the demographic variables...or the dependent variables" |
| Baseline outcome measurements similar? | Low risk | "No significant differences in state/anxiety...and perceived stress between the groups before intervention" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes reported |
| Protected against contamination? | Unclear risk | Insufficient information available to assess likelihood of contamination |
| Other bias | Low risk | No evidence of other bias |
Bergstrom 2009.
| Methods | Randomised trial | |
| Participants | Sweden Inclusion criteria: Nulliparous, Swedish‐speaking and attending any of the participating clinics. No specific inclusion criteria were defined for the women's partners |
|
| Interventions | Intervention: antenatal education focusing on natural childbirth preparation with training in breathing and relaxation techniques (psychoprophylaxis) Control: standard antenatal education focusing on both childbirth and parenthood, without psychoprophylactic training Both groups: four 2‐hour sessions in groups of 12 participants during third trimester of pregnancy and one follow‐up after delivery |
|
| Outcomes | Mode of delivery, epidural analgesia, experience of childbirth, and parental stress in early parenthood | |
| Notes | Baseline (Control group) CS rate: 21% Date of study: October 2005 to February 2007 Funding: Swedish Research Council and Karolinska Institute Conflicts of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomisation was conducted by the computerised algorithm with two priorities: Stratification by (1) equal number of participants per model in all clinics taken together and (2) balancing the numbers of each model within the respective clinic." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information provided in the report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Main outcomes (modes of delivery) objective |
| Baseline characteristics similar? | Low risk | Baseline characteristics in study groups similar (Table 1 in the article) |
| Baseline outcome measurements similar? | Unclear risk | Baseline measures of main outcomes not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Numbers lost to follow‐up (Figure 1 in the article) unlikely to bias effect estimates |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes reported |
| Protected against contamination? | High risk | Some women in standard care also got psychoprophylaxis education at home |
| Other bias | High risk | Unit of analysis issues: “We have analysed data of individuals in spite of the fact that exposures was given to groups of individuals.” |
Chaillet 2015.
| Methods | Cluster‐randomised trial | |
| Participants | Canada Participants: 32 public hospitals with at least 300 deliveries in the year before initiation of study and a CS rate > 17% and at the time of recruitment, no recent or ongoing quality improvement programmes designed to reduce CS rate. All women who delivered at participating centres and whose newborns had a gestational age of at least 24 weeks and weighed at least 500g at delivery |
|
| Interventions | Implementation of evidence‐based guidelines (onsite training in evidence‐based clinical practice, facilitation by local opinion leader, supervision), audits of indications for caesarean delivery and provision of feedback to health professionals | |
| Outcomes | Caesarian section rate, vaginal delivery, pharmacologic induction of labour, artificial rupture of membranes, augmentation with oxytocin during labour, epidural analgesia, and episiotomy; composite risks of minor and major maternal complications; and composite risks of minor and major neonatal complications, excluding lethal congenital abnormalities |
|
| Notes | Baseline (control group) CS rate: 23.2% Date of study: April 2008 to October 2011 Funding: Canadian Institutes of Health Research Conflicts of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "To avoid imbalance in the size of the two groups, we used computer‐generated, blocked randomization within each stratum, with blocks consisting of four centers or, for strata with fewer than eight hospitals, two centers". Further details in trial protocol |
| Allocation concealment (selection bias) | Low risk | "To avoid imbalance in the size of the two groups, we used computer‐generated, blocked randomization within each stratum, with blocks consisting of four centers or, for strata with fewer than eight hospitals, two centers. Local investigators at each hospital were then immediately informed of the assignment status of their hospital." Further details in trial protocol |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Impact of possible performance bias on main outcomes considered minimal |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcomes of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | Table 1 in the article: baseline characteristics comparable |
| Baseline outcome measurements similar? | Low risk | Table 2 in the article: baseline outcome measures comparable |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of attrition bias |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Low risk | "By designating hospitals as the units of randomization, we ensured that all women within a given maternity unit were assigned to the same trial group, thereby reducing the risk of contamination of the intervention effect." |
| Other bias | Low risk | No evidence of other bias |
Eden 2014.
| Methods | Randomised trial | |
| Participants | USA Pregnant women who had one prior caesarean and were eligible for VBAC participated one time between 2005 and 2007 |
|
| Interventions | Intervention: evidence‐based, computerised decision aid Control: two evidence‐based educational brochures about caesarean delivery and VBAC |
|
| Outcomes | Change in decisional conflict around birth priorities, mode of delivery, birth priorities for women | |
| Notes | Baseline (control group) CS rate: not reported Date of study: 2005 to 2007 Funding: OHSU Foundation; NIH K12 grant (Building Interdisciplinary Research Careers in Women’s Health, 5K12HD043488‐04); grants 1 R03 HS013959 from the Agency for Healthcare Research and Quality and 1 K08 HS11338‐01 from the National Institute of Child Health & Human Development Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The research assistant logged into the secured, randomization database to obtain the decision tool assignment" |
| Allocation concealment (selection bias) | Low risk | "The research assistant logged into the secured, randomization database to obtain the decision tool assignment" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The women were unaware of their intervention assignment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | "The two groups of women (those who received the brochures and those who used the decision aid) were similar in all demographic, health insurance status, birth intention and obstetric history variables." |
| Baseline outcome measurements similar? | Unclear risk | Insufficient information provided in the report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "In cases of missing data for decisional conflict questions, a conservative approach was taken by assigning the missing response as unsure that was scored as a 2." |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in the results section |
| Protected against contamination? | Unclear risk | Insufficient information available to assess likelihood of contamination |
| Other bias | Low risk | No evidence of other bias |
Feinberg 2015.
| Methods | Randomised trial | |
| Participants | USA Pregnant women and their partner (couples were aged 18 and above, living together, and expecting a first child at recruitment) The analytic sample consisted of 147 mothers (71 from control, and 76 from the intervention group) who completed interviews when children were 6 months old (wave 2), interviewed from 2004 to 2006 |
|
| Interventions | Intervention: psychosocial couple‐based prevention programme Control: routine care (no educational classes) |
|
| Outcomes | Delivery mode, complications of pregnancy and delivery, mother and newborn length of hospital stay | |
| Notes | Baseline (control group) CS rate: 40% Date of study: “The analytic sample consisted of 147 mothers (71 from control, and 76 from the intervention group) who completed interviews when children were 6 months old (wave 2), interviewed from 2004 to 2006.” Funding: National Institute of Child Health and Development (K23 HD042575) and the National Institute of Mental Health (R21 MH064125‐01). Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information provided |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided |
| Baseline characteristics similar? | Low risk | In page 4 in the article: "To assess randomization, we performed attrition analysis and baseline equivalence testing by intervention condition. Results showed baseline equivalence across a wide array of pretest" |
| Baseline outcome measurements similar? | Unclear risk | Insufficient information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information provided |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in the results section |
| Protected against contamination? | Unclear risk | Insufficient information available to assess likelihood of contamination |
| Other bias | Low risk | No evidence of other bias |
Fenwick 2015.
| Methods | Randomised trial | |
| Participants | Australia Inclusion criteria: women between 12 to 24 weeks gestation, aged 16 years and older, able to read, write and understand English and with capacity to consent were invited to participate. (They should have had higher fear levels (WDEQ‐A ≥ 66)) Exclusion criteria: women who required an interpreter, or had a foetal diagnosis of major abnormality or incompatibility with life were excluded |
|
| Interventions | Intervention: psychoeducation by telephone Control: routine maternity care |
|
| Outcomes | Caesarean section, induction of labour (amniotomy, prostaglandin or syntocinon), epidural use in labour and neonatal admission to special care or intensive care nursery; Psychosocial outcomes: depressive symptoms, distressing flashbacks of the birth and parenting confidence Women’s satisfaction with their ultimate birth mode and feelings of fear |
|
| Notes | Baseline (control group) CS rate: 41.9% Date of study: May 2012 to June 2013 Funding: National Health & Medical Research Council, NHMRC grant number APP1025099 Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were allocated in blocks of ten and stratified by hospital site and parity using a centralised web‐based service to either intervention or control group" |
| Allocation concealment (selection bias) | Low risk | "A research assistant not involved in recruitment or provision of the intervention accessed the randomisation service following receipt of participant’s written consent and completed baseline measures." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likelihood of performance bias considered low given the nature of intervention (psychoeducation by telephone) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (delivery mode) objective |
| Baseline characteristics similar? | Low risk | Participant characteristics comparable |
| Baseline outcome measurements similar? | Unclear risk | Insufficient information provided in the report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There was no difference in the proportion of women in the intervention group and the control groups that dropped out of the study (46.5% and 45% respectively, P = 0.78)." |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Low risk | Likelihood of contamination considered low given the nature of intervention (psychoeducation by telephone) |
| Other bias | Low risk | No evidence of other bias |
Fraser 1997.
| Methods | Randomised trial | |
| Participants | 12 hospitals: 11 Canada and 1 USA
Pregnant women with single previous low caesarean birth with gestational age < 28 weeks Exclusion: women with previous VBAC, classic caesarean scar or known multiple pregnancies |
|
| Interventions | Prenatal education and support programme (first contact for provision of education and support at randomisation, second contact 8 weeks later) | |
| Outcomes | Attempt vaginal delivery, VBAC, caesarean section scheduled, unsuccessful or urgent, maternal morbidity, neonatal mortality and morbidity | |
| Notes | Baseline (control group) CS rate: 26.3% Date of study: April 1992 to November 1994 Funding: supported by operating grant No. MT 11430 from the Medical Research Council of Canada and by nominal awards (W.F. from the Medical Research Council of Canada, grant No DG‐401; E.M. from the National Health Research and Development Program, National Health Research Scholar, No. 6605‐2487‐47). Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Likely: "Randomization, which was performed through a centralized telephone answering service, was blocked and stratified by hospital and by the woman's motivation to attempt vaginal delivery." |
| Allocation concealment (selection bias) | Low risk | "Randomization, which was performed through a centralized telephone answering service, was blocked and stratified by hospital and by the woman's motivation to attempt vaginal delivery." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | The two groups of women (those who received the brochures and those who used the decision aid) were similar in all demographic, health insurance status, birth intention and obstetric history variables |
| Baseline outcome measurements similar? | Low risk | Stratified by women's motivation to attempt vaginal birth |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data on outcome measures |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Unclear risk | Insufficient information available to assess likelihood of contamination |
| Other bias | Low risk | No evidence of other bias |
Hemminki 2008.
| Methods | Cluster‐randomised trial | |
| Participants | Public health nurses in maternity health centres, Helsinki Finland | |
| Interventions | Training of public health nurses to focus more on mode of delivery in childbirth classes | |
| Outcomes | Mode of delivery, pain relief, labour induction, use of oxytocin, foetal electronic surveillance, Apgar score, care in neonatal or intensive care units and perinatal and infant deaths | |
| Notes | Pilot testing, no sample size calculation and cluster accommodation. Intervention did not succeed Baseline (control group) CS rate: 12% Date of study: 2002 to 2003 Funding: National Research and Development Centre for Welfare and Health (STAKES), Helsinki, Finland Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly allocated...on the throw of a dice" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information provided in the report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | "Measured by women's background characteristics, the cluster randomisation succeeded relatively well...with the exception of marital status, the pregnant women's background characteristics were very similar." There were no differences in distribution of the number of previous pregnancies |
| Baseline outcome measurements similar? | Unclear risk | Insufficient information provided in the report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High dropout in intervention group |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information provided in the report |
| Protected against contamination? | Low risk | Childbirth classes only provided to invited health workers |
| Other bias | High risk | No a priori sample size calculation |
Keeler 1996.
| Methods | Interrupted time series study | |
| Participants | USA 11,767 deliveries ‐ 5255 cases for the 12 months before and 6515 cases for the 12 months afterwards |
|
| Interventions | Equalising physician fees for vaginal and caesarean delivery | |
| Outcomes | Rate of caesarean deliveries, vaginal breech deliveries, caesarean deliveries due to breech | |
| Notes | Baseline (control group) CS rate: 25.3% Date of study: not reported (data set used – 12 months before and 12 months after May 1993) Funding: Agency for Health Care Policy and Research (AHCPR#282‐90‐0039) Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | No information provided in the report |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is point of intervention |
| Intervention unlikely to affect data collection? | Unclear risk | Insufficient information provided in the report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing outcome data not reported in the report |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes are reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | High risk | Insufficient data available for appropriate reanalysis |
Liang 2004.
| Methods | Interrupted time series analysis Comparisons of caesarean rates between 1993‐96 and 1997‐2000 |
|
| Participants | Taiwan Pregnant women in labour |
|
| Interventions | Peer review and mandatory second opinion | |
| Outcomes | Total, primary and repeat caesarean rates, Apgar scores | |
| Notes | Baseline (control group) CS rate: 37% Date of study: 1993 to 2000 Funding: not reported Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | No statement of another intervention occurring concurrently |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is point of intervention |
| Intervention unlikely to affect data collection? | Low risk | Data collection separate from intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unable to assess if all outcome data included |
| Selective reporting (reporting bias) | Low risk | Data on all relevant outcomes reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Lo 2008.
| Methods | Interrupted time series study | |
| Participants | Taiwan Pregnant women (2001 to 2005) |
|
| Interventions | Financial interventions: 1) Increase in vaginal birth after caesarean (VBAC) fee to the same level as caesarean section (April 2003); 2) Increase in vaginal birth fee to that of caesarean section (May 2005) | |
| Outcomes | Caesarean section and VBAC rates | |
| Notes | Baseline (control group) CS rate: 29% Date of study: 2001 to 2005 Funding: not stated Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | Insufficient information provided in the report |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is the point of intervention |
| Intervention unlikely to affect data collection? | Low risk | Considered unlikely to affect data collection |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No reference to missing data |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Lomas 1991.
| Methods | Cluster‐randomised trial | |
| Participants | Canada 76 physicians in 16 community hospitals |
|
| Interventions | Interventions: (1) audit and feedback + distribution of educational materials; (2) Local opinion leaders + distribution of educational materials Control: distribution of educational materials | |
| Outcomes | Trial of labour rates, vaginal births, maternal and neonatal morbidity | |
| Notes | Baseline (control group) CS rate: 20% Date of study: 1988 to 1989 Funding: National Health Research and Development Programme of Health and Welfare Canada Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified in the paper "randomly selected and assigned" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information provided in the report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | No significant differences between groups |
| Baseline outcome measurements similar? | Low risk | "Small difference in the overall caesarean section and VBAC rates prior to the study were not statistically significant" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear from the study report |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Low risk | Unlikely: unit of allocation is community hospital |
| Other bias | High risk | Unit of analysis errors |
Masoumi 2016.
| Methods | Randomised trial | |
| Participants | Iran Inclusion criteria: single foetus, no chronic disease such as diabetes, heart and lung chronic diseases, no infertility, no high risk pregnancy and no history of psychiatrist visit, do not use specific drugs, gestational age of 20 weeks Exclusion criteria: any problems or complications during pregnancy, failure to attend more than one session of training |
|
| Interventions | Intervention: antenatal education programme for physiologic childbirth in 8 two‐hour sessions Control: routine prenatal education |
|
| Outcomes | Fear of delivery, rates of physiologic, normal vaginal, CS deliveries | |
| Notes | Baseline (control group) CS rate: 40% Date of study: September 2012 to January 2013 Funding: Hamadan University of Medical Sciences. Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "160 people entered the study and were divided into two equal groups using the table of random numbers" |
| Allocation concealment (selection bias) | Low risk | "In inside of 160 envelopes, A and B letters were written. The eligible persons were given the envelopes respectively. After opening the envelope, the type of groups was found" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | "Baseline characteristics of women were similar in both groups" |
| Baseline outcome measurements similar? | Low risk | No important differences present |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Proportion of missing data unlikely to change main results |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in the results section |
| Protected against contamination? | Unclear risk | Allocation was by individual patients (cannot rule out contamination) |
| Other bias | Low risk | No evidence of other risk of bias |
Mohammadi 2012.
| Methods | Retrospective, before‐after study (reanalysed as an interrupted time series study) | |
| Participants | Iran 3494 pregnant women in General hospital, Tehran, Iran from May 2005 to December 2005 |
|
| Interventions | Clinical audit and feedback process; review of random sample of caesarean section patients for indication with financial incentive to practitioners who met the criteria | |
| Outcomes | Caesarean section rates | |
| Notes | Baseline (control group) CS rate: 40% Date of study: 2004 to 2005 Funding: Faculty of Medicine, Uppsala University Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | Insufficient information provided in the report |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is point of intervention |
| Intervention unlikely to affect data collection? | Low risk | Retrospective cohort study of all deliveries |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing data not reported |
| Selective reporting (reporting bias) | Low risk | All relevant data reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Montgomery 2007.
| Methods | Randomised trial | |
| Participants | UK 742 pregnant women from 4 maternity units with one previous lower segment caesarean section. Recruited by research midwife at antenatal clinic 10 to 20 weeks gestation |
|
| Interventions | Two patient decision‐aids: information programme providing information on the outcomes associated with planned vaginal delivery, elective caesarean section and emergency caesarean section; and a decision analysis containing information on descriptions of outcomes for mother and baby of each delivery method and women are asked to consider a value to these outcomes. This provides a recommended 'preferred option' based on maximised expected utility | |
| Outcomes | Primary: decisional conflict scale and actual mode of delivery Secondary: anxiety, knowledge of the decisional conflict scale and satisfaction | |
| Notes | Baseline (control group) CS rate: 24% Date of study: May 2004 to August 2006 Funding: BUPA Foundation; UK Department of Health National Coordinating Centre for Research Capacity Development Conflict of interest: the authors declare that they have no known conflict of interests |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "One member of the of the study team generated the randomisation sequence by computer..." |
| Allocation concealment (selection bias) | Low risk | "...another member of staff with no involvement in the trial performed the allocation" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Unclear risk | Insufficient information in the report |
| Baseline outcome measurements similar? | Low risk | Outcomes measured before intervention and no important differences reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Proportion of missing data similar for each group |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Low risk | Decision aids only provided to those women randomised to that arm |
| Other bias | Low risk | No evidence of other bias |
Navaee 2015.
| Methods | Randomised trial | |
| Participants | Iran Inclusion criteria: no experience of acute psychological emotions, delivery and childbirth fear score > 28, primiparous, single pregnancy, gestational age of 34–36 weeks, age of 18–35 years, no history of infertility, no indication for CS, and not having passed educational course for delivery methods |
|
| Interventions | Role play education versus standard education using lectures | |
| Outcomes | Fear of natural delivery, mode of delivery | |
| Notes | Baseline (control group) CS rate: 56.2% Date of study: not reported. Funding: Mashhad University of Medical Sciences, Iran Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided in the report |
| Allocation concealment (selection bias) | Unclear risk | The unit of allocation was health centre (however, no information was reported on allocation concealment) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (VBAC) objective |
| Baseline characteristics similar? | Low risk | There were no differences in baseline characteristics between study groups at baseline |
| Baseline outcome measurements similar? | Low risk | There were no differences in outcome measures at baseline (Table 1 in the article) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Unclear risk | Insufficient information provided to enable assessment of likelihood of group contamination |
| Other bias | Low risk | No evidence of other bias |
Poma 1998.
| Methods | Interrupted time series study | |
| Participants | USA Community hospital obstetric unit; women delivering over 6‐year period 1991 to 1996 |
|
| Interventions | Peer review and feedback regarding use of practice guidelines 24‐hour in‐house physician coverage | |
| Outcomes | Total, primary and repeat caesarean section rate, perinatal morbidity and mortality | |
| Notes | Baseline (control group) CS rate: 20.7% Date of study: January 1991 to December 1996 Funding: not stated Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | Insufficient information provided in the report |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is point of intervention |
| Intervention unlikely to affect data collection? | Unclear risk | No distinction between intervention and records collected |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No description of missing data |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Rosenstein 2015.
| Methods | Interrupted time series study | |
| Participants | USA Study period: 2005 and 2014: In 2011, privately insured women changed from a private practice model to one that included 24‐hour midwifery and labourist coverage. Primary caesarean delivery rates among nulliparous, term, singleton, vertex women and VBAC rates among women with prior caesarean delivery were compared before and after the change |
|
| Interventions | Expanded access to collaborative 24‐hour midwifery‐labourist care model | |
| Outcomes | Primary caesarean delivery and VBAC | |
| Notes | Baseline (control group) CS rate: 31.7% Date of study: 2005 to 2014 Funding: National Institute of Child Health and Human Development (Grant # HD01262); National Center for Advancing Translational Sciences (Grant # UCSF‐CTSI UL1 TR000004); and the non‐profit Prima Medical Foundation Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Low risk | "We cannot be certain whether other factors could have led to the decrease in rates, although there were no other official hospital policies that took effect during this time." |
| Shape of the intervention effect pre‐specified? | Low risk | "In our study, we graphically demonstrated the converse: primary caesarean rates were increasing slightly before the expansion and decreased afterward." |
| Intervention unlikely to affect data collection? | Low risk | Sources and methods of data collection were the same before and after the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not specified in the report |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in the results section |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Rouhe 2013.
| Methods | Randomised trial | |
| Participants | Finland Inclusion criteria: nulliparous women with severe fear of birth according to the Wijma Delivery Expectancy Questionnaire A (prenatal version) (W‐DEQ A) (REF 21) |
|
| Interventions | Intervention: psychoeducative group sessions led by a psychologist Women in the control group received a letter in which they were advised to discuss their fear of childbirth in their primary maternity healthcare unit. When needed, primary health care referred fearful women to a special maternity care unit |
|
| Outcomes | Mode of delivery, life satisfaction and general well‐being, costs, duration of labour and delivery, postpartum haemorrhage, usage of epidural or spinal analgesia, birthweight and umbilical arterial pH of the new born, Apgar scores, and interventions during the third stage of labour (suturing or surgical evacuation of placenta or membranes postpartum) | |
| Notes | Baseline (control group) CS rate: 32.5% Date of study: October 2007 to August 2009 Funding: Emil Aaltonen Foundation and the Signe and Ane Gyllenberg Foundation Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not reported (Women were randomised, by one of the researchers, to the intervention or control group in the proportion of 1:2 in balanced blocks of 18) |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes used |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcomes (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | Table 3 in the article: There were no significant differences between study groups in age, social status, education, previous pregnancies or marital status |
| Baseline outcome measurements similar? | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Protected against contamination? | Unclear risk | Insufficient information available to assess likelihood of contamination |
| Other bias | Low risk | No evidence of other bias |
Runmei 2012.
| Methods | Retrospective before‐after study Reanalysed as an interrupted time series study |
|
| Participants | China 25,280 pregnant women at a Regional referral centre, Yunnan, China from January 2005 to December 2011 |
|
| Interventions | Stage 1 (Jan 2005 to Dec 2006): educational programme for hospital staff Stage 2 (Jan to June 2007): monitoring of risk‐adjusted caesarean section rates Stage 3 (Jan 2005 to Dec 2011): monitoring of neonatal outcomes |
|
| Outcomes | Caesarean section rate, neonatal outcomes | |
| Notes | Only first two stages targeting caesarean sections were considered for analysis Baseline (control group) CS rate: 54.8% Date of study: 2001‐2011 Funding: Yunnan Science and Technology Committee, Yunnan Province Government (research grant 2009CA006) Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | Insufficient information provided in the report |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is point of intervention |
| Intervention unlikely to affect data collection? | Low risk | Retrospective cohort study of all deliveries |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Selective reporting (reporting bias) | Low risk | Data on all prespecified outcomes reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Saisto 2001.
| Methods | Randomised trial | |
| Participants | Finland
Physically healthy pregnant women with low obstetric risk and a diagnosis of fear of childbirth Exclusion criteria: contraindication to vaginal delivery (2 previous caesareans or vertical incision in previous caesarean) |
|
| Interventions | Intensive group therapy with trained obstetrician in cognitive behavioural therapy and childbirth psychology | |
| Outcomes | Requests for caesarean delivery at 38 weeks pregnancy Mode of delivery, duration of labour and pain relief Reporting level of anxiety, depression and concerns using multiple scales at 24 and 36 weeks | |
| Notes | Baseline (control group) CS rate: 15% Date of study: August 1996 to July 1999 Funding: Signe and Ane Gyllenberg Foundation, the Emil Aaltonen Foundation, Helsinki University Central Hospital, and the Academy of Finland Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided in the report |
| Allocation concealment (selection bias) | Low risk | "...randomly assigned to groups in balanced blocks of 20 by sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Baseline characteristics similar? | Low risk | Measured and no significant differences between groups found |
| Baseline outcome measurements similar? | Low risk | Measured and no significant differences between groups found |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Proportion of missing data similar in study groups |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Protected against contamination? | Low risk | No evidence of group contamination |
| Other bias | Low risk | No evidence of other bias |
Scarella 2011.
| Methods | Interrupted time series study | |
| Participants | Chile 4813 pregnant women at a regional health centre, admitted for spontaneous labour or pregnancy interruption Excluded deliveries with newborns < 500g, deliveries by private physicians |
|
| Interventions | Audit and feedback | |
| Outcomes | Caesarean section rate, neonatal outcomes | |
| Notes | Baseline (control group) CS rate: 36.8% Date of study: March 2007 to November 2008 Funding: not stated Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Intervention independent of other changes? | Unclear risk | Insufficient information provided in the report |
| Shape of the intervention effect pre‐specified? | Low risk | Point of analysis is point of intervention |
| Intervention unlikely to affect data collection? | Low risk | Insufficient information provided in the report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Selective reporting (reporting bias) | Low risk | Data on all relevant outcomes reported |
| Knowledge of the allocated interventions adequately prevented during the study? | Low risk | Main outcome of interest (mode of delivery) objective |
| Other bias | Low risk | No evidence of other bias |
Sharifirad 2013.
| Methods | Randomised trial | |
| Participants | Iran Inclusion criteria: primiparous pregnant women in 28‐32 pregnancy weeks who referred to private clinics and were willing to use caesarean section; lack of obvious barriers and medical diagnosis for vaginal delivery during sampling such as detectable medical causes; full consent and collaboration of pregnant women and their husbands in order to participate in the intervention |
|
| Interventions | Prenatal education for husbands of pregnant women | |
| Outcomes | Elective caesarian section rate; knowledge and attitudes | |
| Notes | Baseline (control group) CS rate: 50% Date of study: not stated Funding: none Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, but method of randomisation not mentioned |
| Allocation concealment (selection bias) | Unclear risk | No information provided in the report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Objective outcome measure (caesarean delivery) |
| Baseline characteristics similar? | Low risk | No significant difference between study groups |
| Baseline outcome measurements similar? | Low risk | No significant difference between study groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of attrition bias |
| Selective reporting (reporting bias) | Low risk | All prespecified outcome data reported |
| Protected against contamination? | Unclear risk | No clear steps to prevent contamination (could have been possible if there was communication between participants) |
| Other bias | Low risk | No evidence of other bias |
Shorten 2005.
| Methods | Randomised trial | |
| Participants | Australia Inclusion criteria: pregnant women with 1 previous caesarean section and medically eligible for a trial of vaginal birth Exclusion criteria: more than 1 previous caesarean section; classical or unknown uterine scar; history of uterine rupture or upper segment perforation; multiple pregnancy; and obstetric or medical contraindications to vaginal birth, or trial of vaginal birth or both in the current pregnancy |
|
| Interventions | Decision‐aid booklet describing risks and benefits of elective repeat caesarean section and trial of labour provided at 28 weeks gestation | |
| Outcomes | Mode of delivery, level of knowledge, decisional conflict score, preference for mode of delivery at 36 weeks and postnatal satisfaction | |
| Notes | Baseline (control group) CS rate: 30% Date of study: May 2001 to May 2003 Funding: MBF Research Grant, Sydney, The University of Wollongong New Researcher Grant Scheme, Wollongong, and NSW Midwives Association Research Scholarship, Sydney, New South Wales, Australia Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Opaque envelopes containing a random allocation for each participant code number were prepared by computer‐based randomized generation" |
| Allocation concealment (selection bias) | Low risk | "Opaque envelopes containing a random allocation for each participant code number were prepared by computer‐based randomized generation" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | "Socioeconomic and clinical baseline characteristics...were similar, except more intervention women reported experiencing problems after their previous caesarean section (infection, pain, breastfeeding problems) compared with the control group" |
| Baseline outcome measurements similar? | Low risk | Baseline outcome measures (pre‐scores) comparable |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Proportion of missing data is similar in both groups |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Protected against contamination? | Low risk | Decision‐aid was provided only to those in the intervention arm |
| Other bias | Low risk | No evidence of other bias |
Srinivas 2016.
| Methods | Controlled before‐after study | |
| Participants | USA Hospitals, matched 2:1 non‐labourist to labourist using the following variables.
|
|
| Interventions | Intervention: labourist model of obstetric care Control: standard care provided by the regular staff attending deliveries |
|
| Outcomes | Caesarean delivery, chorioamnionitis, induction of labour, preterm birth, maternal prolonged length of stay (> 2 days postpartum for vaginal delivery; > 4 days postpartum for caesarean delivery), Apgar at 5 minutes of < 7, birth asphyxia, injury, trauma, and neonatal death | |
| Notes | Baseline (control group) CS rate: 28.5% Date of study: 1998 to 2011 Funding: Maternal and Child Health Bureau R40 Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Controlled before‐after design |
| Allocation concealment (selection bias) | High risk | Controlled before‐after design |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Likelihood of performance bias considered minimal |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | "Hospital level characteristics were largely balanced post match with a few small non‐significant differences related to delivery volume and geography (Table 2 in the article)" |
| Baseline outcome measurements similar? | Low risk | Baseline outcomes between study groups comparable |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of attrition bias |
| Selective reporting (reporting bias) | Low risk | No evidence of selective outcome reporting |
| Protected against contamination? | Low risk | Likelihood of contamination considered minimal |
| Other bias | Low risk | No evidence of other bias |
Valiani 2014.
| Methods | Randomised trial | |
| Participants | Iran Inclusion criteria
|
|
| Interventions | Intervention: childbirth training workshop Control: conventional and routine education during maternal care by the midwives in healthcare centres, gynaecologists, and relatives |
|
| Outcomes | Knowledge, attitude, and delivery mode | |
| Notes | Baseline (control group) CS rate: 73.3% Date of study: not reported Funding: Isfahan University of Medical Sciences Conflict of interest: the authors declare that they have no known conflict of interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For random allocation of the subjects, the sequence of subjects’ allocation to either of the above mentioned groups was made by draw as mothers, couples, and control." |
| Allocation concealment (selection bias) | Unclear risk | Not specified in the report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not specified in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | No important difference were present |
| Baseline outcome measurements similar? | Low risk | No important difference were present |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in the results section |
| Protected against contamination? | Unclear risk | Allocation was by individual patients (cannot rule out contamination) |
| Other bias | Low risk | No evidence of other bias |
Wang 2014.
| Methods | Randomised trial | |
| Participants | China Inclusion criteria: 16‐32 weeks of gestation, normal cognitive function; no history of childbirth or abortion; diagnosis of singleton pregnancy by B‐ultrasound; no obvious risk factors according to prenatal and B‐ultrasound examination findings; and no history of urinary incontinence, pelvic surgery, pelvic organ prolapse, or vaginal wall prolapse |
|
| Interventions | Intervention: pelvic floor muscle training exercises with telephone follow‐up Control: pelvic floor muscle training without telephone follow‐up |
|
| Outcomes | Delivery mode, timing of each labour stage (first through third stages) (details of other outcomes available in paper) | |
| Notes | Baseline (control group) CS rate: 49.1% Date of study: December 2010 to March 2011 Funding: 2010 Youth Fund Project of Guangzhou Medical University (Project number: 2010A03) Conflict of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided in the report |
| Allocation concealment (selection bias) | Unclear risk | No information provided in the report |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided in the report |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Main outcome of interest (mode of delivery) objective |
| Baseline characteristics similar? | Low risk | No important difference present |
| Baseline outcome measurements similar? | Low risk | No important difference present |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information provided in the report |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes in the methods section are reported in the results section |
| Protected against contamination? | Low risk | Allocation was by practice and it is unlikely that the control group received the intervention |
| Other bias | Low risk | No evidence of other bias |
CS: caesarean section; VBAC: vaginal birth after caesarian
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Afshar 2015 | Ineligible design (prospective cohort study) |
| Arrieta 2011 | Intervention not aimed at reducing caesarean birth |
| Bailey 2010 | Intervention not aimed at reducing caesarean birth |
| Barber 2010 | Intervention not aimed at reducing caesarean birth |
| Bernitz 2011 | Intervention assessed addressed in a related Cochrane Review (Sandall 2016) |
| Bonfrer 2016 | National Health Insurance Scheme designed to increase access to maternal and infant healthcare services (including caesarean sections) |
| Calvo 2009 | Uncontrolled before‐after study |
| Chambliss 1992 | Intervention assessed addressed in a related Cochrane Review (Sandall 2016) |
| Chen 2014 | Uncontrolled before‐after study |
| Chittithavorn 2006 | ITS study with insufficient data points (only one data point before and after intervention) |
| Costa 2009 | Uncontrolled before‐after study |
| David 2001 | Not an intervention study |
| Dunn 2013 | Uncontrolled before‐after study |
| Fournier 2014 | Study assessed effect of fee exemption intended to increase access to caesarean deliveries |
| Ganji 2006 | Uncontrolled before‐after study |
| Gilbert 2012 | No control group |
| Gregory 1999 | ITS study with insufficient data points (fewer than 3 data points before intervention) |
| Gruber 1999 | The study was not an intervention study |
| Hemminki 2013 | Interventions in study were not specifically aimed at reducing caesarean section rate |
| Ho 2011 | Uncontrolled before‐after study |
| Howell 2004 | ITS study with insufficient data points (fewer than 3 data points before intervention) |
| Hutcheon 2015 | Not specifically designed to assess effect on primary outcome measures (primary outcome was a composite of adverse neonatal outcomes) |
| Iglesias 1991 | ITS study with insufficient data points (fewer than 3 data points before intervention) |
| Jenabi 2012 | Does not measure primary outcome of interest |
| Jiang 2015 | Major methodological flaws |
| Kasawara 2013 | Interventions in study were not aimed at reducing caesarean section rate |
| Kazandjian 1998 | Retrospective cohort, observation study |
| Kim 2005 | ITS study with insufficient data points (2 data points after the intervention) |
| Kiwankura 1993 | ITS study with insufficient data points (only 1 data point before and after intervention) |
| Kongnyuy 2008 | ITS study with insufficient data points |
| Koroukian 2001 | Not an intervention study |
| Kunthonkitidej 2001 | Insufficient number of sites to determine trend |
| Lagrew 1996 | ITS study with insufficient data points (fewer than 3 data points before intervention) |
| Law 1999 | Intervention assessed addressed in a related Cochrane Review (Sandall 2016) |
| Lee 2007 | Controlled ITS with insufficient data points after the intervention to determine trend |
| Leone 2016 | Study evaluates impact of user fee reform intended to increase access to maternal and child health services (including caesarean sections) |
| Main 1999 | CBA (data compared were not the same time and inappropriate control group) |
| Misra 2008 | ITS study with insufficient data points before and after the intervention |
| Morhason‐Bello 2009 | Intervention addressed in a related Cochrane Review (Bohren 2017) |
| Myers 1993 | ITS study with insufficient data points (only 1 data point before intervention) |
| Oleske 1992 | ITS study with insufficient data points (fewer than 3 data points before intervention) |
| Robson 1996 | ITS study with insufficient data points (fewer than 3 data points before intervention) |
| Saint 2003 | Caesarean section rate not measured |
| Sanavi 2014 | The study does not measure mode of delivery (reports behavioural intention change in women intending to have a caesarean section) |
| Santerre 1996 | Not an intervention study |
| Socol 1993 | ITS study with no defined intervention time point |
| Tussey 2015 | Clinical intervention |
| van Dillen 2008 | Uncontrolled before‐after study |
| Walker 2016 | Intervention not specifically designed to reduce caesarean section rate |
| Werner 2013 | Intervention not aimed at reducing caesarean section rate |
| Zanetta 1999 | ITS study with insufficient data points (only 1 data point before intervention) |
| Zhang 2016 | Intervention addressed in a related Cochrane Review (Sandall 2016) |
CBA: controlled before‐after; ITS: interrupted time series
Characteristics of studies awaiting assessment [ordered by study ID]
Jang 2011.
| Methods | Interrupted time series study Setting: South Korea Time‐series autoregressive integrated moving average (ARIMA) analysis was used to assess the effect of four repeated public releases (RPR) on caesarean section rates |
| Participants | Data sources: monthly data about institutional caesarean section rates and total deliveries from the Health Insurance Review & Assessment Service (HIRA) National Quality Improvement project database from 2003 through 2007 |
| Interventions | Repeated public releases on caesarean section rates |
| Outcomes | Caesarean section rates |
| Notes | Study will be considered for inclusion in the next update of the review |
Vankan 2015.
| Methods | Study design: not stated “Women pregnant after one previous CS without a contra‐indication for an intended VB were enrolled in six matched pairs of hospitals.” “The vaginal birth (VB) rate in the period before the study started was 48%. A difference of > 10 % was considered ‘inferior’ care. The sample size needed was 400 per study arm” |
| Participants | Women pregnant after one previous caesarean section without a contraindication for an intended vaginal birth |
| Interventions | Intervention (n = 479 women) Women in the intervention hospitals received a decision analysis, including both information on benefits and risks of intended vaginal birth or elective repeat caesarean delivery and a prediction model to calculate the individual vaginal birth probability Control (n = 441 women) Counselling in the control hospitals was performed according to usual care |
| Outcomes | Patient involvement, vaginal birth rate, elective and emergency caesarean section rate |
| Notes | Study will be considered for inclusion in the next update of the review |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12611000878976.
| Trial name or title | For pregnant women in the first half of their pregnancy with history of previous caesarean and eligible for vaginal birth after caesarean (VBAC), will using a decision aid increase their rate of VBAC compared to using a pamphlet? |
| Methods |
Country: New Zealand Study design: randomised trial |
| Participants | History of one previous caesarean less than 25 weeks gestation in current pregnancy |
| Interventions |
Intervention: the decision aid is a comprehensive 25 page booklet that first explains the risks and benefits of elective repeat caesarean and of VBAC, and then asks the woman to write down her own values and preferences about the two birth options. It will be administered at the time of the consultation in the Positive Birth After Caesarean Clinic. Control: the patient pamphlet is 6 pages and briefly lists risks and benefits of elective repeat caesarean and of VBAC. It is administered at the time of the consultation in Positive Birth After Caesarean Clinic |
| Outcomes |
Primary outcome: the rate of VBAC is determined using the perinatal database at the hospital Secondary outcomes
|
| Starting date | September 2014 |
| Contact information | Michelle Wise: m.wise@auckland.ac.nz |
| Notes | Trial registry number: ACTRN12611000878976 |
ACTRN12611001214921.
| Trial name or title | Does continuity of care impact decision making in the next birth after a caesarean section (VBAC)? A randomised controlled trial |
| Methods | Randomised trial |
| Participants | Pregnant women whose most recent birth was by caesarean section |
| Interventions | Midwifery continuity of care to women through pregnancy, labour, birth and early postnatal care Control: standard hospital care from different midwives through pregnancy, labour, birth and early postnatal care |
| Outcomes |
Primary outcome: proportion of women who attempt vaginal birth in their current pregnancy Secondary outcomes: proportion of vaginal births; neonatal health assessed at birth and at 28 days (Apgar scores, admission to special care nursery, length of stay in hospital, readmission to hospital); women's social and emotional outcomes examined using a survey at 36 weeks of pregnancy and at 6 weeks postpartum |
| Starting date | Not yet recruiting (anticipated 30/06/2012; as per trial registry record) |
| Contact information | caroline.homer@uts.edu.au |
| Notes | Trial registry number: ACTRN12611001214921; DOI: 10.1186/1471‐2393‐13‐140 |
ACTRN12613000161729.
| Trial name or title | Enhanced care and support in early labour (ECSEL): a randomised controlled trial to reduce caesarean sections for first‐time mothers |
| Methods |
Country: Australia Study design: randomised trial |
| Participants |
Inclusion criteria: women at normal risk of complication having their first baby booked at a participating hospital; live within 30 minutes drive of the hospital; English‐speaking Exclusion criteria: complications of pregnancy that would indicate early admission to hospital in labour (e.g. foetal growth restriction, antepartum haemorrhage, planned caesarean section) |
| Interventions |
Intervention: standard care in early labour is to telephone the midwife in the hospital birthsuite and seek advice on whether or not to come to hospital. The intervention here is that a known midwife will provide enhanced support (via telephone and/or home visiting) to assist women in the early or latent phases of labour to remain at home until labour is well established unless there is a reason to be admitted earlier. The support will include listening to the woman, taking a detailed history, assessing her current stage of labour and coping ability, advising whether or not to come to hospital, suggesting pain relief strategies and providing reassurance. This will be the midwife's main role, whereas midwives usually providing such guidance are concurrently providing care to women already admitted to hospital in labour. The study midwife will also visit the woman at home if this would be helpful (to be decided on an individual basis by the woman and the midwife). The duration of this additional support will vary according to individual needs between around 15 minutes and 3 hours. Control: women telephone midwives working in birthsuite/emergency department when they want advice readmission to hospital for the birth (standard care) |
| Outcomes |
Primary outcome: caesarean section for any indication Secondary outcomes
|
| Starting date | Anticipated: September 2014 |
| Contact information | Mary‐Ann Davey: m.davey@latrobe.edu.au |
| Notes | Trial registry number: ACTRN12613000161729 |
IRCT2013111010777N3.
| Trial name or title | The impact of a computerised decision aid on the mode of delivery, compared with conventional care |
| Methods |
Country: Iran Study design: randomised, parallel group trial |
| Participants |
Inclusion criteria: positive pregnancy test, being in good health, pregnancy above 28 weeks, and singleton pregnancy Exclusion criteria: unwanted pregnancy, inability to read and write and working with computer, experience of previous caesarean section |
| Interventions |
Intervention group: they will receive a computer‐based decision aid on mode of delivery Control group: they will receive the conventional care |
| Outcomes |
Primary outcome: decisional conflict, knowledge Secondary outcome: mode of delivery |
| Starting date | December 2013 |
| Contact information | Saeid Eslami: eslams@mums.ac.ir |
| Notes | IRCT registration number: IRCT2013111010777N3 |
ISRCTN10612254.
| Trial name or title | Improving the organisation of maternal health service delivery, and optimising childbirth, by increasing vaginal birth after caesarean section (VBAC) through enhanced women‐centred care |
| Methods |
Countries: Germany, Ireland and Italy Study design: multicentre cluster‐randomised trial |
| Participants |
Participant inclusion criteria
|
| Interventions |
Intervention: evidence‐based education of women and clinicians, introduction of communities of practice (women and clinicians sharing knowledge), opinion leaders, audit and peer review of caesarean sections in each hospital, and joint decision‐making by women and clinicians. The content and details of the intervention will be determined through systematic reviews and qualitative research Control: usual care |
| Outcomes |
Primary outcomes: change from baseline in each hospital in the proportion of women who have had one previous caesarean section who have a vaginal birth during the study Secondary outcomes
Health economic analyses will be done using data on clinical outcomes, direct costs (such as length of stay and antibiotic use) and indirect costs (such as productivity loss) during pregnancy and postnatal period. The study will also seek to assess adherence to guidelines and practice protocols, adherence to intervention quantity and quality, and midwife‐centred variables; to compare and contrast findings across the different hospitals. |
| Starting date | December 2013 |
| Contact information | Cecily Begley: cbegley@tcd.ie |
| Notes | Trial registry number: SRCTN10612254; DOI: 10.1186/ISRCTN10612254 |
ISRCTN48510263.
| Trial name or title | Appropriate decision for caesarean section in Burkina Faso |
| Methods |
Country: Burkina Faso Study design: cluster‐randomised trial |
| Participants |
Participant inclusion criteria For the hospitals:
For the patients: all women who deliver by caesarean section in selected hospitals during the study period For the health professionals: all health professionals involved in the decision‐making process for a caesarean section: obstetricians, general practitioners, nurses and midwives |
| Interventions |
Interventions The evidence‐based intervention will consist of three strategies to improve the competencies of maternity teams
To analyse the intervention process, a longitudinal qualitative study consisting of deliberative workshops and individual in‐depth interviews will be conducted. Control group: no external intervention is planned for this group |
| Outcomes |
Primary outcomes Change in the rate of non‐medically justified caesarean sections among all caesarean sections Secondary outcomes
|
| Starting date | March 2014 |
| Contact information | Charles Kabore: kaborewendyam@yahoo.fr |
| Notes | Trial registry number: ISRCTN48510263; DOI 10.1186/ISRCTN48510263 Protocol: http://www.ncbi.nlm.nih.gov/pubmed/27769190 |
ISRCTN50041378.
| Trial name or title | Reducing caesarean section rates in Ireland: a feasibility study and pilot randomised trial of an evidence‐based intervention designed to reduce unnecessary caesarean section |
| Methods |
Country: Ireland Study design: feasibility study and pilot cluster randomised trial Setting: hospitals Target number of participants: 2 clusters (400 participants in each cluster) |
| Participants |
Participant inclusion criteria
Participant exclusion criteria
|
| Interventions |
Intervention Intervention will likely consist of an appointment of an obstetric and midwife opinion leader who will facilitate women‐centred, evidence‐based antenatal classes (2 classes) and information session for clinicians, providing accurate information on the risks and benefits of both VBAC and repeat caesarean sections, second opinions for all caesarean sections (other than category 1), peer‐review of each caesarean section and feedback, reducing induction of labour rates, support of clinicians and women to choose normal options over medical intervention (e.g. mobility instead of oxytocin, water‐bath instead of pharmacological pain relief, reducing use of electronic foetal monitoring in low‐risk women) Control Usual care as per current hospital practice |
| Outcomes |
Primary outcome measures
Secondary outcome measures
|
| Starting date | September 2017 |
| Contact information | Cecily Begley: cbegley@tcd.ie |
| Notes | ISRCTN50041378 https://doi.org/10.1186/ISRCTN50041378 |
NCT02874443.
| Trial name or title | The REDUCED Trial: REDucing the Utilization of CEsarean Sections for Dystocia (REDUCED) |
| Methods |
Country: Canada Study design: cluster‐randomised trial |
| Participants | Inclusion criteria: centres in Alberta that provide intrapartum care, have facilities to perform caesarean section and deliver at least 70 primiparous women annually |
| Interventions |
Intervention: application of a knowledge translation strategy, of new clinical practice guidelines on labour management, to physicians and nurses caring for women in labour Control: no intervention |
| Outcomes |
Primary outcome: rate of caesarean section in primiparous women in labour Secondary outcomes
|
| Starting date | October 2016 |
| Contact information | Stephen Wood: slwood@ucalgary.ca |
| Notes | NCT Number: NCT02874443 |
NICU: Neonatal intensive care unit; VBAC: vaginal birth after caesarean
Differences between protocol and review
We updated the eligible study designs to align with current Cochrane EPOC criteria.
We amended study eligibility criteria as follows.
To avoid duplication and substantial overlap with related reviews, we excluded studies of other related interventions assessed in related reviews: midwife‐led continuity of care (Sandall 2016); continuous labour support (Bohren 2017); physical activity‐based interventions (i‐WIP 2017); alternative institutional birth environment (Hodnett 2012); and planned hospital birth versus planned home birth (Olsen 2012).
We only included non‐clinical interventions specifically designed to reduce caesarean section rates (interventions not specifically designed to reduce caesarean section rates are not included, even if they may incidentally reduce caesarean section rates; these interventions have been proposed for further research in areas with high caesarean section rates).
-
We expanded the scope of the review to include the following additional interventions.
Opinion leaders: dissemination of information or advocacy with support or campaigns from local or international opinion leader (role models, leadership persons, public celebrities).
Staffing models (e.g. different types of physician staffing models).
Goal‐setting for caesarean section rates (setting a specific predetermined goal for caesarean section rate).
Policies that limit financial/legal liability in case of litigation of healthcare professionals or organisations.
Strategies to change the organisational culture: strategies include various components of organisational culture (e.g. shared values, behaviours, norms, traditions, sense‐making) which may shape and/or contribute to the overall environment of an organisation).
We adopted a new system for classifying identified interventions drawing on updated EPOC taxonomy (Table 5; EPOC 2015). The new system also drew on the taxonomy drafted by the World Health Organization (WHO) expert panel on caesarean section guidelines.
Types of outcome measures (primary outcomes amended to include only modes of delivery: caesarean section, spontaneous vaginal birth, instrumental vaginal birth).
We implemented GRADE and created 'Summary of findings' tables.
New authors: Innie Chen, Newton Opiyo, Ana Pilar Betran, Sameh Mortazhejri, Jennifer Petkovic, Tamara Rader, Sugandha Agarwal, Monica Taljaard, Sharlini Yogasingam.
Contributions of authors
Original review
Protocol development (SK, PL, TL, RG)
All the authors contributed to the conduct of the review and approved the final version
For this update
Designing search strategies and undertaking searches (TR, IC, APB, NO)
Study selection (IC, EM, SM, APB, NO, SY, JP, SA, MT)
Data collection and study quality assessment (IC, ET, APB, NO, SM, JP, SA, MT)
Synthesis and writing of review (IC, APB, NO)
All authors commented on the draft review and approved the final version
Sources of support
Internal sources
-
Australian Satellite of the Cochrane EPOC Group, Monash University, Australia.
Tavender Emma
-
Bruyère Research Institute, University of Ottawa, Canada.
Jennifer Petkovic
-
Canadian Agency for Drugs and Technologies in Health (CADTH), Canada.
Tamara Rader
-
Review Production and Quality Unit, Cochrane, UK.
Newton Opiyo
-
Khon Kaen University, Thailand.
Malinee Laopaiboon
-
Lamphun Hospital, Thailand.
Suthit Khunpradit
-
Ottawa Hospital Research Institute, Canada.
Monica Taljaard, Sameh Mortazhejri, Sugandha Agarwal
-
Nanyang Technological University, Singapore.
Russell L Gruen
-
University of Melbourne, Australia.
Jason Wasiak
-
University of Ottawa, Canada.
Innie Chen
External sources
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Ana Pilar Betran (WHO employee, salary support)
Declarations of interest
Innie Chen: no known conflicts of interest Newton Opiyo is an editor with Cochrane EPOC and member of the WHO CS Guideline Technical Working Group Emma Tavender: no known conflicts of interest Sameh Mortazhejri: no known conflicts of interest Tamara Rader: no known conflicts of interest Jennifer Petkovic: no known conflicts of interest Sharlini Yogasingam: no known conflicts of interest Monica Taljaard: no known conflicts of interest Sugandha Agarwal: no known conflicts of interest Malinee Laopaiboon: no known conflicts of interest Jason Wasiak: no known conflicts of interest Suthit Khunpradit: no known conflicts of interest Pisake Lumbiganon: Member of the WHO CS Guideline Development Group (Co‐chair) Russell Gruen: no known conflicts of interest Ana Pilar Betran: Member of the WHO Steering Group who managed the CS guideline development process
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Althabe 2004 {published data only}
- Althabe F, Belizan JM, Villar J, Alexander S, Bergel E, Ramos S, et al. Mandatory second opinion to reduce rates of unnecessary caesarean sections in Latin America: a cluster randomised control trial. Lancet 2004;363(9425):1934‐40. [DOI] [PubMed] [Google Scholar]
Ayres‐De‐Campos 2015 {published data only}
- Ayres‐De‐Campos D, Cruz J, Medeiros‐Borges C, Costa‐Santos C, Vicente L. Lowered national cesarean section rates after a concerted action. Acta Obstetricia et Gynecologica Scandinavica 2015;94(4):391‐8. [DOI] [PubMed] [Google Scholar]
Bastani 2006 {published data only}
- Bastani F, Hidarnia A, Kazemnejad A, Vafaei M, Kashanian M. A randomized controlled trial of the effects of applied relaxation training on reducing anxiety and perceived stress in pregnant women. Journal of Midwifery & Women's Health 2005;50(4):e36‐e40. [DOI] [PubMed] [Google Scholar]
- Bastani F, Hidarnia A, Montgomery KS, Aguilar‐Vafaei ME, Kazemnejad A. Does relaxation education in anxious primigravid Iranian women influence adverse pregnancy outcomes? A randomised controlled trial. Journal of Perinatal & Neonatal Nursing 2006;20(2):138‐46. [DOI] [PubMed] [Google Scholar]
Bergstrom 2009 {published data only}
- Bergstrom M, Kieler H, Waldenstrom U. Psychoprophylaxis during labor: associations with labor‐related outcomes and experience of childbirth. Acta Obstetricia et Gynecologica Scandinavica 2010;89(6):794‐800. [DOI] [PubMed] [Google Scholar]
- Bergström M, Kieler H, Waldenström U. Effects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of child birth and parental stress in mothers and fathers. British Journal of Obstetrics and Gynaecology 2009;116(9):1167‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaillet 2015 {published data only}
- Chaillet N, Dumont A, Abrahamowicz M, Pasquier JC, Audibert F, Monnier P, et al. QUARISMA Trial Research Group. A cluster‐randomized trial to reduce cesarean delivery rates in Quebec. New England Journal of Medicine 2015;372(18):1710‐21. [DOI] [PubMed] [Google Scholar]
Eden 2014 {published data only}
- Eden KB, Perrin NA, Vesco KK, Guise JM. A randomized comparative trial of two decision tools for pregnant women with prior cesareans. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2014;43(5):568‐79. [DOI] [PubMed] [Google Scholar]
Feinberg 2015 {published data only}
- Feinberg ME, Roettger ME, Jones DE, Paul IM, Kan ML. Effects of a psychosocial couple‐based prevention program on adverse birth outcomes. Maternal and Child Health Journal 2015;19(1):102‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fenwick 2015 {published data only}
- Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. Effects of a midwife psycho‐education intervention to reduce childbirth fear on women's birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth 2015;15:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fraser 1997 {published data only}
- Fraser W, Maunsell E, Hodnett E, Moutquin J‐M. Randomized controlled trial of a prenatal vaginal birth after cesarean section education and support program. American Journal of Obstetrics and Gynecology 1997;176(2):419‐25. [DOI] [PubMed] [Google Scholar]
Hemminki 2008 {published data only}
- Hemminki E, Heikkila K, Sevon T, Koponen P. Special features of health services and register based trials ‐ experiences from a randomised trial of childbirth classes. BMC Health Services Research 2008;8:126‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keeler 1996 {published data only}
- Keeler EB, Fok T. Equalizing physician fees had little effect on cesarean rates. Medical Care Research and Review 1996;53(4):465‐71. [DOI] [PubMed] [Google Scholar]
Liang 2004 {published data only}
- Liang WH, Yuan CC, Hung JH, Yang ML, Yang MJ, Chen YJ. Effect of peer review and trial of labor on lowering cesarean section rates. Journal of the Chinese Medical Association 2004;67(6):281‐6. [PubMed] [Google Scholar]
Lo 2008 {published data only}
- Lo JC. Financial incentives do not always work ‐ an example of cesarean sections in Taiwan. Health Policy 2008;88(1):121‐9. [DOI] [PubMed] [Google Scholar]
Lomas 1991 {published data only}
- Lomas J, Enkin M, Anderson GM, Hannah WJ, Vayda E, Singer J. Opinion leaders vs adult and feedback to implement practice guidelines. Delivery after previous cesarean section. JAMA 1991;265(17):2202‐7. [PubMed] [Google Scholar]
Masoumi 2016 {published data only}
- Masoumi SZ, Kazemi F, Oshvandi K, Jalali M, Esmaeili‐Vardanjani A, Rafiei H. Effect of training preparation for childbirth on fear of normal vaginal delivery and choosing the type of delivery among pregnant women in Hamadan, Iran: A randomized controlled trial. Journal of Family and Reproductive Health 2016;10(3):115‐21. [PMC free article] [PubMed] [Google Scholar]
Mohammadi 2012 {published data only}
- Mohammadi S, Kallestal C, Essen B. A practical strategy for reducing cesarean section rates in a general hospital in Tehran, Iran. Journal of Reproductive Medicine 2012;57(1‐2):43‐8. [PubMed] [Google Scholar]
Montgomery 2007 {published data only}
- Montgomery AA, Emmett CL, Fahey T, Jones C, Ricketts I, Patel RR, Peters TJ, Murphy DJ, DiAMOND Study Group. Two decision aids for mode of delivery among women with previous caesarean section: randomised controlled trial. BMJ 2007;334(7607):1305‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery AA, DiAMOND Study Group. The DiAMOND trial protocol: a randomised controlled trial of two decision aids for mode of delivery among women with a previous caesarean section. BMC Pregnancy and Childbirth 2004;4(1):25‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Navaee 2015 {published data only}
- Navaee M, Abedian Z. Effect of role play education on primiparous women's fear of natural delivery and their decision on the mode of delivery. Iranian Journal of Nursing and Midwifery Research 2015;20(1):40‐6. [PMC free article] [PubMed] [Google Scholar]
Poma 1998 {published data only}
- Poma PA. Effect of departmental policies on cesarean delivery rates: a community hospital experience. Obstetrics and Gynecology 1998;91(6):1013‐8. [DOI] [PubMed] [Google Scholar]
Rosenstein 2015 {published data only}
- Rosenstein MG, Nijagal M, Nakagawa S, Gregorich SE, Kuppermann M. The association of expanded access to a collaborative midwifery and laborist model with cesarean delivery rates. Obstetrics and Gynecology 2015;126(4):716‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rouhe 2013 {published data only}
- Rouhe H, Salmela‐Aro K, Toivanen R, Tokola M, Halmesmäki E, Saisto T. Obstetric outcome after intervention for severe fear of childbirth in nulliparous women ‐ randomised trial. BJOG 2013;120(1):75‐84. [DOI] [PubMed] [Google Scholar]
Runmei 2012 {published data only}
- Runmei M, Lao Terence T, Yonghu S, Hong X, Yuqin T, Bailuan L, et al. Practice audits to reduce caesareans in a tertiary referral hospital in south‐western China. Bulletin of the World Health Organization 2012;90(7):488‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saisto 2001 {published data only}
- Saisto T, Salmela‐Aro K, Nurmi JE, Könönen T, Halmesmäki E. A randomized controlled trial of intervention in fear of childbirth. Obstetrics and Gynecology 2001;98(5):820‐6. [DOI] [PubMed] [Google Scholar]
Scarella 2011 {published data only}
- Scarella A, Chamy V, Sepulveda M, Belizan JM. Medical audit using the Ten Group Classification System and its impact on the cesarean section rate. European Journal of Obstetrics Gynecology and Reproductive Biology 2011;154(2):136‐40. [DOI] [PubMed] [Google Scholar]
Sharifirad 2013 {published data only}
- Sharifirad G, Rezaeian M, Soltani R, Javaheri S, Mazaheri MA. A survey on the effects of husbands' education of pregnant women on knowledge, attitude, and reducing elective cesarean section. Journal of Education and Health Promotion 2013;2:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shorten 2005 {published data only}
- Shorten A, Shorten B, Keogh J, West S, Morris J. Making choices for childbirth: a randomised controlled trial of a decision‐aid for informed birth after cesarean. Birth 2005;32(4):252‐61. [DOI] [PubMed] [Google Scholar]
Srinivas 2016 {published data only}
- Srinivas SK, Small DS, Macheras M, Hsu JY, Caldwell D, Lorch S. Evaluating the impact of the laborist model of obstetric care on maternal and neonatal outcomes. American Journal of Obstetrics and Gynecology 2016;215(6):770.e1‐.e9. [DOI] [PubMed] [Google Scholar]
Valiani 2014 {published data only}
- Valiani M, Haghighatdana Z, Ehsanpour S. Comparison of childbirth training workshop effects on knowledge, attitude, and delivery method between mothers and couples groups referring to Isfahan health centers in Iran. Iranian Journal of Nursing and Midwifery Research 2014;19(6):653‐8. [PMC free article] [PubMed] [Google Scholar]
Wang 2014 {published data only}
- Wang X, Li GY, Deng, ML. Pelvic floor muscle training as a persistent nursing intervention: Effect on delivery outcome and pelvic floor myodynamia. International Journal of Nursing Sciences 2014;1:48‐52. [Google Scholar]
References to studies excluded from this review
Afshar 2015 {published data only}
- Afshar Y, Mei J, Wong M, Gregory K, Kilpatrick S, Esakoff T. The role of the birth plan in obstetrical and neonatal outcomes and birth experience satisfaction. American Journal of Obstetrics and Gynecology 2015;212(1):S282. [Google Scholar]
Arrieta 2011 {published data only}
- Arrieta A. Health reform and cesarean sections in the private sector: The experience of Peru. Health Policy 2011;99(2):124‐30. [DOI] [PubMed] [Google Scholar]
Bailey 2010 {published data only}
- Bailey PE, Binh HT, Bang HT. Promoting accountability in obstetric care: use of criteria‐based audit in Viet Nam. Global Public Health 2010;5(1):62‐74. [DOI] [PubMed] [Google Scholar]
Barber 2010 {published data only}
- Barber SL. Mexico's conditional cash transfer programme increases cesarean section rates among the rural poor. European Journal of Public Health 2010;20(4):383‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bernitz 2011 {published data only}
- Bernitz S, Rolland R, Blix E, Jacobsen M, Sjøborg K, Øian P. Is the operative delivery rate in low‐risk women dependent on the level of birth care? A randomised controlled trial. BJOG 2011;118(11):1357‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonfrer 2016 {published data only}
- Bonfrer I, Breebaart L, Poel E. The effects of Ghana's National Health Insurance Scheme on maternal and infant health care utilization. PLoS One 2016;11(11):e0165623. [DOI] [PMC free article] [PubMed] [Google Scholar]
Calvo 2009 {published data only}
- Calvo A, Campillo C, Juan M, Roig C, Hermoso JC, Cabeza PD. Effectiveness of a multifaceted strategy to improve the appropriateness of cesarean sections. Acta Obstetricia et Gynecologica 2009;88(7):842‐5. [DOI] [PubMed] [Google Scholar]
Chambliss 1992 {published data only}
- Chambliss LR, Daly C, Medearis AL, Ames M, Kayne M, Paul R. The role of selection bias in comparing caesarean birth rates between physician and midwifery management. Obstetrics and Gynecology 1992;80:161‐5. [PubMed] [Google Scholar]
Chen 2014 {published data only}
- Chen CS, Liu TC, Chen B, Lin CL. The failure of financial incentive? The seemingly inexorable rise of cesarean section. Social Science & Medicine 2014;101:47‐51. [DOI] [PubMed] [Google Scholar]
Chittithavorn 2006 {published data only}
- Chittithavorn S, Pinjaroen S, Suwanrath C, Soonthornpun K. Clinical practice guideline for cesarean section due to cephalopelvic disproportion. Journal of the Medical Association of Thailand 2006;89(6):735‐40. [PubMed] [Google Scholar]
Costa 2009 {published data only}
- Costa ML, Cecatti JG, Milanez HM, Souza JP, Gulmezoglu M. Audit and feedback: effects on professional obstetrical practice and healthcare outcomes in a university hospital. Acta Obstetricia et Gynecologica 2009;88(7):793‐800. [DOI] [PubMed] [Google Scholar]
David 2001 {published data only}
- David S, Mamelle N, Riviere O. Estimation of an expected caesarean section rate taking into account the case mix of a maternity hospital. Analysis from the AUDIPOG Sentinelle Network (France). British Journal of Obstetrics and Gynaecology 2001;108(9):919‐26. [DOI] [PubMed] [Google Scholar]
Dunn 2013 {published data only}
- Dunn S, Sprague AE, Fell DB, Dy S, Harrold S, Lamontagne B, et al. The use of a quality indicator to reduce elective repeat caesarean section for low‐risk women before 39 Weeks’ gestation: The Eastern Ontario experience. Journal of Obstetrics and Gynaecology Canada 2013;35(4):306‐16. [DOI] [PubMed] [Google Scholar]
Fournier 2014 {published data only}
- Fournier P, Dumont A, Tourigny C, Philibert A, Coulibaly A, Traoré M. The free caesareans policy in low‐income settings: an interrupted time series analysis in Mali (2003‐2012). PLoS One 2014;9(8):e105130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ganji 2006 {published data only}
- Ganji F, Yusefi H, Baradaran A. Effect of a participatory intervention to reduce the number of unnecessary caesarean sections performed in Shahrekord of Iran. Journal of Medical Sciences 2006;6(4):690‐2. [Google Scholar]
Gilbert 2012 {published data only}
- Gilbert W, Bliss MC, Johnson A, Gregg L, Swanson C. Effect of education and provider transparency upon individual cesarean, episiotomy, antenatal steroid, and breastfeeding rates. American Journal of Obstetrics and Gynecology 2012;26(1):A1‐A38, S1‐S386. [Google Scholar]
Gregory 1999 {published data only}
- Gregory KD, Hackmeyer P, Gold L, Johnson AI, Platt LD. Using the continuous quality improvement process to safely lower the cesarean section rate. Joint Commission Journal on Quality Improvement 1999;25(12):619‐29. [DOI] [PubMed] [Google Scholar]
Gruber 1999 {published data only}
- Gruber J, Kim J, Mayzlin D. Physician fees and procedure intensity: the case of cesarean delivery. Journal of Health Economics 1999;18(4):473‐90. [DOI] [PubMed] [Google Scholar]
Hemminki 2013 {published data only}
- Hemminki E, Long Q, Zhang WH, Wu Z, Raven J, Tao F, et al. Impact of financial and educational interventions on maternity care: results of cluster randomized trials in rural China, CHIMACA. Maternal and Child Health Journal 2013;17:208‐21. [DOI] [PubMed] [Google Scholar]
Ho 2011 {published data only}
- Ho JJ, Japaraj RP, Che Anuar CY, Rostenberghe HA, Paeds SA, Chang ASM, et al. Influence of a targeted educational intervention on evidence‐based practice in two Malaysian maternity units: The sea ORCHID project in Malaysia. Medical Journal of Malaysia 2011;66(4):288‐95. [PubMed] [Google Scholar]
Howell 2004 {published data only}
- Howell EM, Dubay L, Kenney G, Sommers AS. The impact of Medicaid managed care on pregnant women in Ohio: a cohort analysis. Health Services Research 2004;39(4):825‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hutcheon 2015 {published data only}
- Hutcheon JA, Strumpf EC, Harper S, Giesbrecht E. Maternal and neonatal outcomes after implementation of a hospital policy to limit low‐risk planned caesarean deliveries before 39 weeks of gestation: an interrupted time‐series analysis. BJOG 2015;122(9):1200‐6. [DOI] [PubMed] [Google Scholar]
Iglesias 1991 {published data only}
- Iglesias S, Burn R, Saunders D. Reducing the cesarean section rate in a rural community hospital. Canadian Medical Association Journal 1991;146(10):1459‐64. [PMC free article] [PubMed] [Google Scholar]
Jenabi 2012 {published data only}
- Jenabi E, Hajiloo MM, Torkamani M. The effect of reflexology on relieving the labor pain. Iranian Journal of Obstetrics, Gynecology and Infertility 2012;14(8):34‐8. [Google Scholar]
Jiang 2015 {published data only}
- Jiang Y, Liu XW. Effect of new‐pattern obstetrical nursing in reducing cesarean delivery rate. Journal of Biological Regulators and Homeostatic Agents 2015;29(4):847‐51. [PubMed] [Google Scholar]
Kasawara 2013 {published data only}
- Kasawara KT, Burgos CS, Do Nascimento SL, Ferreira NO, Surita FG, Pinto E Silva JL. Maternal and perinatal outcomes of exercise in pregnant women with chronic hypertension and/or previous preeclampsia: A randomized controlled trial. ISRN Obstetrics and Gynecology 2013;857047:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kazandjian 1998 {published data only}
- Kazandjian VA, Lied TR. Cesarean section rates: effects of participation in a performance measurement project. Joint Commission Journal on Quality Improvement 1998;24(4):187‐96. [DOI] [PubMed] [Google Scholar]
Kim 2005 {published data only}
- Kim C‐Y, Ko S‐K, Kim K‐Y. Are league tables controlling epidemic of caesarean sections in South Korea?. BJOG: an International Journal of Obstetrics and Gynaecology 2005;112(5):607‐11. [DOI] [PubMed] [Google Scholar]
Kiwankura 1993 {published data only}
- Kiwankura AI, Moore WM. Influence of audit and feedback on the use of caesarean section in a geographically defined population. European Journal of Obstetrics, Gynecology and Reproductive Biology 1993;50(1):59‐64. [DOI] [PubMed] [Google Scholar]
Kongnyuy 2008 {published data only}
- Kongnyuy EJ, Leigh B, Broek N. Effect of audit and feedback on the availability, utilisation and quality of emergency obstetric care in three districts in Malawi. Women and Birth 2008;21(4):149‐55. [DOI] [PubMed] [Google Scholar]
Koroukian 2001 {published data only}
- Koroukian SM, Bush D, Rimm AA. Comparison of cesarean section rates in fee‐for‐service versus managed care patients in the Ohio Medicaid population, 1992‐1997. American Journal of Managed Care 2001;7(2):134‐42. [PubMed] [Google Scholar]
Kunthonkitidej 2001 {published data only}
- Kunthonkitidej K, Ngernset O. Self‐evaluation of obstetricians by delivery data to reduce cesarean section rate in Chai Nat Hospital. Journal of the Medical Association of Thailand 2001;84(11):1587‐93. [PubMed] [Google Scholar]
Lagrew 1996 {published data only}
- Lagrew DC Jr, Morgan MA. Decreasing the cesarean section rate in a private hospital: success without mandated clinical changes. American Journal of Obstetrics and Gynaecology 1996;174(1):184–91. [DOI] [PubMed] [Google Scholar]
Law 1999 {published data only}
- Law YY, Lam KY. A randomized controlled trial comparing midwife‐managed care and obstetrician‐managed care for women assessed to be at low risk in the initial intrapartum period. Journal of Obstetrics and Gynaecology Research 1999;25(2):107‐12. [DOI] [PubMed] [Google Scholar]
Lee 2007 {published data only}
- Lee K, Lee S. Effects of the DRG‐based prospective payment system operated by the voluntarily participating providers on the cesarean section rates in Korea. Health Policy 2007;81(2‐3):300‐8. [DOI] [PubMed] [Google Scholar]
Leone 2016 {published data only}
- Leone T, Cetorelli V, Neal S, Matthews Z. Financial accessibility and user fee reforms for maternal healthcare in five sub‐Saharan countries: a quasi‐experimental analysis. BMJ Open 2016;6(1):e009692. [DOI] [PMC free article] [PubMed] [Google Scholar]
Main 1999 {published data only}
- Main EK. Reducing cesarean birth rates with data‐driven quality improvement activities. Pediatrics 1999;103(1 Suppl E):374‐83. [PubMed] [Google Scholar]
Misra 2008 {published data only}
- Misra A. Impact of the HealthChoice Program on cesarean section and vaginal birth after C‐section deliveries: a retrospective analysis. Maternal Child Health Journal 2008;12(2):266‐74. [DOI] [PubMed] [Google Scholar]
Morhason‐Bello 2009 {published data only}
- Morhason‐Bello IO, Adedokun BO, Ojengbede OA, Olayemi O, Oladokun A, Fabamwo AO. Assessment of the effect of psychosocial support during childbirth in Ibadan, south‐west Nigeria: a randomised controlled trial. Australian and New Zealand Journal of Obstetrics and Gynaecology 2009;49(2):145‐50. [DOI] [PubMed] [Google Scholar]
Myers 1993 {published data only}
- Myers SA, Gleicher N. The Mount Sinai cesarean section reduction program: an update after 6 years. Social Science and Medicine 1993;37(10):1219‐22. [DOI] [PubMed] [Google Scholar]
Oleske 1992 {published data only}
- Oleske DM, Glandon GL, Tancredi DJ, Nassirpour M, Noak JR. Information dissemination and the cesarean birth rate. The Illinois experience. International Journal of Technology Assessment in Health Care 1992;8(4):708‐18. [DOI] [PubMed] [Google Scholar]
Robson 1996 {published data only}
- Robson MS, Scudamore IW, Walsh SM. Using the medical audit cycle to reduce cesarean section rates. American Journal of Obstetrics and Gynaecology 1996;174(1 Pt 1):199‐205. [DOI] [PubMed] [Google Scholar]
Saint 2003 {published data only}
- Saint S, Hofer TP, Rose JS, Kaufman SR, McMahon LF Jr. Use of critical pathways to improve efficiency: a cautionary tale. American Journal of Managed Care 2003;9(11):758‐65. [PubMed] [Google Scholar]
Sanavi 2014 {published data only}
- Sanavi FS, Ansari‐Moghaddam A, Shovey MF, Rakhshani F. Effective education to decrease elective caesarean section. Journal of the Pakistan Medical Association 2014;64(5):500‐5. [PubMed] [Google Scholar]
Santerre 1996 {published data only}
- Santerre RE. The effect of the ACOG guideline on vaginal births after cesarean. Medical Care Research and Review 1996;53(3):315‐29. [DOI] [PubMed] [Google Scholar]
Socol 1993 {published data only}
- Socol ML, Garcia PM, Peaceman AM, Dooley SL. Reducing cesarean births at a primarily private university hospital. American Journal of Obstetrics and Gynecology 1993;168(6 Pt 1):1748‐58. [DOI] [PubMed] [Google Scholar]
Tussey 2015 {published data only}
- Tussey CM, Botsios E, Gerkin RD, Kelly LA, Gamez J, Mensik J. Reducing length of labor and cesarean surgery rate using a peanut ball for women laboring with an epidural. Journal of Perinatal Education 2015;24(1):16‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Dillen 2008 {published data only}
- Dillen J, Lim F, Rijssel E. Introducing caesarean section audit in a regional teaching hospital in The Netherlands. European Journal of Obstetrics, Gynecology and Reproductive Biology 2008;139(2):151‐6. [DOI] [PubMed] [Google Scholar]
Walker 2016 {published data only}
- Walker DM, Cohen SR, Fritz J, Olvera‐García M, Zelek ST, Fahey JO, et al. Impact evaluation of PRONTO Mexico: a simulation‐based program in obstetric and neonatal emergencies and team training. Simulation in Healthcare 2016;11(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Werner 2013 {published data only}
- Werner A, Uldbjerg N, Zachariae R, Nohr EA. Effect of self‐hypnosis on duration of labor and maternal and neonatal outcomes: A randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica 2013;92(7):816‐23. [DOI] [PubMed] [Google Scholar]
Zanetta 1999 {published data only}
- Zanetta G, Tampieri A, Currado I, Regalia A, Nespoli A, Midwife T, et al. Changes in cesarean delivery in an Italian university hospital, 1982‐1996: a comparison with the national trend. Birth 1999;26(3):144‐8. [DOI] [PubMed] [Google Scholar]
Zhang 2016 {published data only}
- Zhang T, Liu C. Comparison between continuing midwifery care and standard maternity care in vaginal birth after cesarean. Pakistan Journal of Medical Sciences 2016;32(3):711‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Jang 2011 {published data only}
- Jang WM, Eun SJ, Lee CE, Kim Y. Effect of repeated public releases on cesarean section rates. Journal of Preventive Medicine and Public Health 2011;44(1):2‐8. [DOI] [PubMed] [Google Scholar]
Vankan 2015 {published data only}
- Vankan E, Schoorel E, Kuijk S, Aardenburg R, Delemarre F, Dirksen C, et al. Patient decision aid with individual risk estimation: An effective tool in choosing the mode of delivery after cesarean section. American Journal of Obstetrics and Gynecology 2015;212:S240‐1. [Google Scholar]
References to ongoing studies
ACTRN12611000878976 {published data only}
- ACTRN12611000878976. The effect of an antenatal decision aid booklet on rate of vaginal birth after caesarean (VBAC) in women with previous caesarean section [For pregnant women in the first half of their pregnancy with history of previous caesarean and eligible for vaginal birth after caesarean (VBAC), will using a decision aid increase their rate of VBAC compared to using a pamphlet?]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=343340 (first received 17 August 2011).
ACTRN12611001214921 {published data only}
- ACTRN12611001214921. A randomised controlled trial to determine whether continuity of care increases the rate of attempted vaginal birth after caesarean (VBAC) [A randomised controlled trial to determine whether midwifery continuity of care increases the rate of attempted vaginal birth for women with a previous caesarean section]. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=347744 (first received 24 November 2011).
ACTRN12613000161729 {published data only}
- ACTRN12613000161729. Enhanced care and support in early labour (ecsel) [Enhanced care and support in early labour (ecsel): a randomised controlled trial to reduce caesarean sections for first‐time mothers]. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=335208 (first received 07 February 2013).
IRCT2013111010777N3 {published data only}
- IRCT2013111010777N3. A computer based decision aids for mode of delivery (natural delivery or cesarean section) [The impact of a computerized decision aids on the mode of delivery, compared with conventional care]. who.int/trialsearch/Trial3.aspx?trialid=IRCT2013111010777N3 (first received 19 November 2013).
ISRCTN10612254 {published data only}
- ISRCTN10612254. Improving the organisation of maternal health service delivery, and optimising childbirth, by increasing vaginal birth after caesarean section (VBAC) through enhanced women‐centred care. isrctn.com/ISRCTN10612254 (first received 3 April 2013). [DOI] [PMC free article] [PubMed]
ISRCTN48510263 {published data only}
- ISRCTN48510263. Appropriate decision for caesarean section in Burkina Faso. isrctn.com/ISRCTN48510263 (first received 12 February 2014).
ISRCTN50041378 {unpublished data only}
- ISRCTN50041378. A feasibility study and pilot randomised trial of an intervention designed to reduce unnecessary caesarean section in Ireland. isrctn.com/ISRCTN50041378 (first received 12 February 2018).
NCT02874443 {published data only}
- NCT02874443. The REDUCED Trial: REDucing the Utilization of CEsarean Sections for Dystocia (REDUCED). clinicaltrials.gov/ct2/show/NCT02874443 (first received 22 August 2016).
Additional references
ACOG 2013
- The American College of Obstetricians and Gynecologists. Cesarean delivery on maternal request. Committee Opinion No. 559. Obstetrics and Gynecology 2013;121:904‐7. [DOI] [PubMed] [Google Scholar]
ACOG SMFM 2014
- Caughey AB, Cahill AG, Guise J‐M, Rouse DJ, American College of Obstetricians and Gynecologists, Society for Maternal‐Fetal Medicine. Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology 2014;210(3):179‐93. [DOI] [PubMed] [Google Scholar]
Bermúdez‐Tamayo 2018
- Bermúdez‐Tamayo C, Johri M, Chaillet N. Budget impact of a program for safely reducing caesarean sections in Canada. Midwifery 2018;60:20‐6. [DOI] [PubMed] [Google Scholar]
Bernal 2017
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. International Journal of Epidemiology 2017;46(1):348‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Betrán 2016a
- Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990‐2014. PLoS One 2016;11(2):e0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
Betrán 2016b
- Betrán AP, Torloni MR, Zhang J, Gülmezoglu AM, WHO Working Group on Caesarean Section. WHO Statement on caesarean section rates. BJOG 2016;123(5):667‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boatin 2018
- Boatin AA, Cullinane F, Torloni MR, Betrán AP. Audit and feedback using the Robson classification to reduce caesarean section rates: a systematic review. BJOG 2018;125(1):36‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohren 2017
- Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD003766.pub6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2013
- Brown HC, Paranjothy S, Dowswell T, Thomas J. Package of care for active management in labour for reducing caesarean section rates in low‐risk women. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD004907.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Catling‐Paull 2011a
- Catling‐Paull C, Johnston R, Ryan C, Foureur MJ, Homer CS. Non‐clinical interventions that increase the uptake and success of vaginal birth after caesarean section: a systematic review. Journal of Advanced Nursing 2011;67(8):1662‐76. [DOI] [PubMed] [Google Scholar]
Catling‐Paull 2011b
- Catling‐Paull C, Johnston R, Ryan C, Foureur MJ, Homer CS. Clinical interventions that increase the uptake and success of vaginal birth after caesarean section: a systematic review. Journal of Advanced Nursing 2011;67(8):1646‐61. [DOI] [PubMed] [Google Scholar]
Chaillet 2007
- Chaillet N, Dumont A. Evidence‐based strategies for reducing cesarean section rates: a meta‐analysis. Birth 2007;34(1):53‐64. [DOI] [PubMed] [Google Scholar]
Cook 2013
- Cook JR, Jarvis S, Knight M, Dhanjal MK. Multiple repeat caesarean section in the UK: incidence and consequences to mother and child. A national, prospective, cohort study. BJOG 2013;120(1):85‐91. [DOI] [PubMed] [Google Scholar]
Dweik 2014
- Dweik D, Girasek E, Mészáros G, Töreki A, Keresztúri A, Pál A. Non‐medical determinants of cesarean section in a medically dominated maternity system. Acta Obstetricia et Gynecologica Scandinavica 2014;93(10):1025‐33. [DOI] [PubMed] [Google Scholar]
EPOC 2015
- Cochrane Effective Practice, Organisation of Care (EPOC). EPOC Taxonomy, 2015. Available at epoc.cochrane.org/epoc‐taxonomy.
EPOC 2017
- Cochrane Effective Practice, Organisation of Care (EPOC). EPOC resources for review authors, 2017. Available at epoc.cochrane.org/epoc‐specific‐resources‐review‐authors.
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ, et al. Rating quality of evidence and strength of recommendations: What is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336(7651):995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hartmann 2012
- Hartmann KE, Andrews JC, Jerome RN, Lewis RM, Likis FE, McKoy JN, et al. Strategies to reduce cesarean birth in low‐risk women. Rockville (MD): Agency for Healthcare Research and Quality (US). AHRQ Comparative Effectiveness Review 2012; Vol. Report No.: 12(13)‐EHC128‐EF.
Hodnett 2012
- Hodnett ED, Downe S, Walsh D. Alternative versus conventional institutional settings for birth. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD000012.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoffmann 2014
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
Hoxha 2017
- Hoxha I, Syrogiannouli L, Luta X, Tal K, Goodman DC, Costa BR, et al. Caesarean sections and for‐profit status of hospitals: systematic review and meta‐analysis. BMJ Open 2017;7(2):e013670. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsu 2008
- Hsu KH, Liao PJ, Hwang CJ. Factors affecting Taiwanese women's choice of Cesarean section. Social Science and Medicine 2008;66(1):201‐9. [DOI] [PubMed] [Google Scholar]
i‐WIP 2017
- The International Weight Management in Pregnancy (i‐WIP) Collaborative Group. Effect of diet and physical activity based interventionsin pregnancy on gestational weight gain and pregnancy outcomes: meta‐analysis of individual participant data from randomised trials. BMJ 2017;358:j3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ji 2015
- Ji H, Jiang H, Yang L, Qian X, Tang S. Factors contributing to the rapid rise of caesarean section: a prospective study of primiparous Chinese women in Shanghai. BMJ Open 2015;5(11):e008994. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johri 2017
- Johri M, Ng ESW, Bermudez‐Tamayo C, Hoch JS, Ducruet T, Chaillet N. A cluster‐randomized trial to reduce caesarean delivery rates in Quebec: cost‐effectiveness analysis. BMC Medicine 2017;15(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kabir 2004
- Kabir AA, Steinmann WC, Myers L, Khan MM, Herrera EA, Yu S, et al. Unnecessary cesarean delivery in Louisiana: an analysis of birth certificate data. American Journal of Obstetrics and Gynecology 2004;190(1):10‐9; discussion 3A. [DOI] [PubMed] [Google Scholar]
Keag 2018
- Keag OE, Norman JE, Stock SJ. Long‐term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta‐analysis. PLoS Medicine 2018;15(1):e1002494. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koroukian 1998
- Koroukian SM, Trisel B, Rimm AA. Estimating the proportion of unnecessary cesarean sections in Ohio using birth certificate data. Journal of Clinical Epidemiology 1998;51(12):1327‐34. [DOI] [PubMed] [Google Scholar]
Lavis 2009
- Lavis JN, Oxman AD, Souza NM, Lewin S, Gruen RL, Fretheim A. SUPPORT Tools for evidence‐informed health Policymaking (STP) 9: Assessing the applicability of the findings of a systematic review. Health Research Policy and Systems 2009;7 Suppl 1:S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lin 2004
- Lin HC, Xirasagar S. Institutional factors in cesarean delivery rates: policy and research implications. Obstetrics and Gynecology 2004;103(1):128‐36. [DOI] [PubMed] [Google Scholar]
Lo 2003
- Lo JC. Patients' attitudes versus physician' determination: implications for cesarean sections. Social Science and Medicine 2003;57(1):91‐6. [DOI] [PubMed] [Google Scholar]
Long 2016
- Long Q, Allanson ER, Pontre J, Tunçalp Ö, Hofmeyr GJ, Gülmezoglu AM. Onsite midwife‐led birth units (OMBUs) for care around the time of childbirth: a systematic review. BMJ Global Health 2016;1(2):e000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lundgren 2015
- Lundgren I, Smith V, Nilsson C, Vehvilainen‐Julkunen K, Nicoletti J, Devane D, et al. Clinician‐centred interventions to increase vaginal birth after caesarean section (VBAC): a systematic review. BMC Pregnancy Childbirth 2015;15:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthy 2003
- Luthy DA, Malmgren JA, Zingheim RW, Leininger CJ. Physician contribution to a cesarean delivery risk model. American Journal of Obstetrics and Gynecology 2003;188(6):1579‐85. [DOI] [PubMed] [Google Scholar]
Marshall 2011
- Marshall NE, Fu R, Guise JM. Impact of multiple cesarean deliveries on maternal morbidity: a systematic review. American Journal of Obstetrics and Gynecology 2011;205(3):262.e1‐8. [DOI] [PubMed] [Google Scholar]
Mi 2014
- Mi J, Liu F. Rate of caesarean section is alarming in China. Lancet 2014;383(9927):1463‐4. [DOI] [PubMed] [Google Scholar]
NCC‐WCH 2011
- National Collaborating Centre for Women's and Children's Health. Caesarean Section. London: RCOG Press, 2011. [Google Scholar]
NICE 2013
- National Institute for Health and Clinical Excellence. Caesarean section: Evidence update March 2013. Evidence Update 2013; Vol. 35. [PubMed]
Nilsson 2015
- Nilsson C, Lundgren I, Smith V, Vehvilainen‐Julkunen K, Nicoletti J, Devane D, et al. Women‐centred interventions to increase vaginal birth after caesarean section (VBAC): A systematic review. Midwifery 2015;31(7):657‐63. [DOI] [PubMed] [Google Scholar]
O'Connor 1999
- O'Connor AM, Drake ER, Fiset V, Graham ID, Laupacis A, Tugwell P. The Ottawa patient decision aids. Effective Clinical Practice: ECP 1999;2(4):163‐70. [PubMed] [Google Scholar]
Olsen 2012
- Olsen O, Clausen JA. Planned hospital birth versus planned home birth. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD000352.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pang 2008
- Pang MW, Leung TN, Lau TK, Hang Chung TK. Impact of first childbirth on changes in women's preferences for mode of delivery: follow‐up of a longitudinal observational study. Birth 2008;35(2):121‐8. [DOI] [PubMed] [Google Scholar]
Robson 2001
- Robson MS. Classification of caesarean sections. Fetal and Maternal Medicine Review 2001;12:23‐39. [Google Scholar]
Sandall 2016
- Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife‐led continuity models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews 2016, Issue 4. [DOI: 10.1002/14651858.CD004667.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Scioscia 2008
- Scioscia M, Vimercati A, Cito L, Chironna E, Scatterella D, Selvaggi LE. Social determinants of the increasing caesarean section rate in Italy. Minerva Ginecologica 2008;60(2):115‐20. [PUBMED: 18487961] [PubMed] [Google Scholar]
Thomas 2001
- Thomas J, Paranjothy S, Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit. National Sentinel Caesarean Section Audit Report. www.rcog.org.uk/globalassets/documents/guidelines/research‐‐audit/nscs_audit.pdf 2001.
Timor‐Tritsch 2012
- Timor‐Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. American Journal of Obstetrics and Gynecology 2012;207(1):14‐29. [DOI] [PubMed] [Google Scholar]
WHO 1985
- World Health Organization. Appropriate technology for birth. Lancet 1985;2(8452):436‐7. [PubMed] [Google Scholar]
Ye 2015
- Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gülmezoglu AM, Betrán AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population‐based ecological study with longitudinal data. British Journal of Obstetrics and Gynaecology 2015;123(5):745‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zwecker 2011
- Zwecker P, Azoulay L, Abenhaim HA. Effect of fear of litigation on obstetric care: a nationwide analysis on obstetric practice. American Journal of Perinatology 2011;28(4):277‐84. [DOI] [PubMed] [Google Scholar]
Öst 1988
- Öst LG. Applied relaxation: Description of an effective coping technique. Scandinavian Journal of Behaviour Therapy 1988;17(2):83‐96. [Google Scholar]
References to other published versions of this review
Khunpradit 2005
- Khunpradit S, Lumbiganon P, Jaipukdee J, Laopaiboon M. Non‐clinical interventions for reducing unnecessary caesarean section. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD005528] [DOI] [PubMed] [Google Scholar]
Khunpradit 2011
- Khunpradit S, Tavender E, Lumbiganon P, Laopaiboon M, Wasiak J, Gruen RL. Non‐clinical interventions for reducing unnecessary caesarean section. Cochrane Database of Systematic Reviews 2011, Issue 6. [DOI: 10.1002/14651858.CD005528.pub2] [DOI] [PubMed] [Google Scholar]


