Abstract
Background and aims
Recently, novel picosecond pulse duration lasers (ps-lasers) have been developed for the treatment of multicolored and recalcitrant tattoos, and safety and efficacy have been reported. We therefore hypothesized that ps-lasers could be an alternative treatment for dermal pigmented lesions. We performed a retrospective review to evaluate the efficacy and safety of the ps-laser for nevus of Ota.
Subjects and methods
A retrospective photographic review of 15 patients with nevus of Ota was performed (ages from 10 months to 65 yr). The patients were treated in the Ohshiro Clinic with a picosecond-domain 755 nm alexandrite laser (ps-Alex laser) from June 2015 to August 2017. Improvement was evaluated as the percentage of pigmentation clearance comparing the baseline findings with those at 3 months after the final treatment using a four category grading scale: Poor, 0–24%; Fair, 25–49%; Good, 50–74%; and Excellent 75–100% improvement. Adverse events were also assessed.
Results
All patients obtained clinical improvement ranging from fair to excellent. All 5 patients whose primary treatment was the ps-Alex laser obtained excellent in 2–3 treatment sessions (average 2.5 sessions), and the average total treatment span was 10.0 months. Treatment with the ps-Alex laser caused transient hyperpigmentation followed by improvement to complete resolution at 3 months of follow-up.
Conclusions
Our results suggest that 755 nm ps laser treatment is efficacious for the treatment of nevus of Ota with minimum adverse events.
Keywords: nevus of Ota, picosecond laser, Q-switched laser, post inflammatory pigmentation
Introduction
The introduction of selective pigment removal by pulsed lasers 1), so called selective photothermolysis 2), was considered a landmark in the laser treatment of cutaneous pigmented/vascular lesions by allowing for precise targeting of the abnormal pigment while sparing surrounding normal tissue, thus avoiding the risk of hyperpigmentation, hypopigmentation, and scarring associated with earlier treatment approaches such as continuous wave lasers, cryotherapy, dermabrasion and skin grafting.
The introduction of Q-switched lasers (lasers with pulse-widths in the nanosecond [ns] domain) to dermatological practice in the 1980s was viewed as a major break-through in the treatment of cutaneous pigmented lesions 3). Following Q-switched ns-domain laser treatment of dermal melanocytosis (dermal pigmented lesions) such as nevus of Ota, and Mongolian spots / ectopic Mongolian spots, the characteristic blue-gray color could be resolved completely with the Q-switched ruby, Q-switched alexandrite and Q-switched Nd:YAG lasers 4–11).
Recently, novel picosecond duration lasers (ps-lasers) have been developed for the treatment of unwanted tattoos. Since 2013, ps-lasers have become commercially available and subsequent clinical trials have reported safety and efficacy in treating multicolored and recalcitrant tattoos 12). It is considered that irradiation of targets with the ultra-short picosecond pulses can induce an almost instantaneous reaction in the chromophores in the skin with a combination of photomechanical and photothermal reactions. This achieves greater fragmentation of the targets in an almost nonlinear fashion, with even less damage to adjacent tissues than was achieved with the ns-domain lasers.
Application of the ps-laser for the treatment of unwanted tattoos started in the Ohshiro clinic from December 2013. From our experience of the great success achieved in tattoo removal with the ps-laser, we hypothesized that the ps-laser could be an alternative treatment for dermal pigmented lesions. In this study we performed a retrospective photographic review to evaluate the efficacy and safety in treating nevus of Ota using a ps-domain laser.
Subjects and methods
This retrospective study has been approved by the Ethics Committee of the Ohshiro Clinic (Approval Number: 036).
The present study was a retrospective photographic review of patients attending the Ohshiro Clinic, Tokyo, Japan, for the treatment of nevus of Ota from June 2015 to August 2017. Patients were screened for inclusion in the retrospective study. Exclusion criteria included any hyperphotosensitivity, active or systemic infections, taking any medication for which sunlight is a contraindication, history of immunosuppression. Pregnant woman and lactating woman were also excluded.
Patient medical information was extracted from the patient records, which included the age of patients at time of treatment, irradiation settings of each treatment, duration and number of treatment sessions, complications and clinical photographs. Clinical photographs were taken before, 1 week after, 1 month after, 2 month after, and 3 months after each treatment.
Fifteen patients met the inclusion criteria, 12 females, 3 males, ages ranging from 10 months to 65 years, mean 30.3 yr, who had dermal pigmented lesions. We divided them into two groups: namely those subjects who had no treatment before ps-Alex laser and those who had some previous treatment, such as the Q-switched ruby laser or cryotherapy. All patients were treated with the 755 nm alexandrite laser with a pulse width of 750 ps (ps-Alex laser) (Picosure®, Cynosure, Westfold, MA). The parameters used for each individual patient were 4.07–6.37 J/cm2 and a spot size of 2.2–2.5 mm in diameter. We decided the endpoint of irradiation was the appearance of the immediate slight-whitening phenomena (ISWP) over each target lesion.
The clinical outcome was evaluated by comparing the clinical photography at baseline and at 3 month after the final session. The clinical photography was assessed by two blinded independent plastic surgeons using a four-category grading scale based on the pigment clearance and treatment response according to the percentage of skin lightning with improvement scored as Poor 0–24%; Fair, 25–49%; Good, 50–74%; and Excellent, 75–100%. Adverse events, including the occurrence of crusting, blister formation, erythema, erosion, infection, hyperpigmentation and hypopigmentation were assessed every treatment session. Transient erythema (post inflammatory erythema: PIE) after the removal of crust and post inflammatory pigmentation (PIH) three month after treatment were assessed using a three-category grading scale (0, 1+, 2+) , and duration of PIE and PIH were also recorded.
Results
All fifteen patients obtained improvement with varying degrees of clearance (Table 1). The total treatment sessions were 38 (average 2.5). The results in 10 patients were scored as Excellent (66.7 %), 5 patients were scored as Good (33.3 %) and no patient was scored as Fair or Poor. The average of the interval between each session was 4.1 months and the average total treatment period was 11.6 months. Five patients who had no treatment before ps-Alex laser all obtained an Excellent score within 2–3 sessions and the average of the total treatment span was 10.0 months. There was no difference in improvement in the grading scale between the group which had no treatment before the ps-Alex laser and the one which had treatment, such as the Q-switched ruby laser.
Table 1: Clinical results with the ps-Alex laser for nevus of Ota.
| Total | ps-Alex only | Pre–treatment(+) | ||
|---|---|---|---|---|
| N=15 | N=5 | N=10 | ||
| Age (Ave.) | 30.3 yr | 27.4 yr | 31.8 yr | |
| Total No. of Treatment Sessions | 38 sessions | 13 sessions | 25 sessions | |
| Clinical Result : | Excellent (75–100 %) | 10 (66.7 %) | 4 (80.0 %) | 6 (60.0 %) |
| Good (50–74 %) | 5 (33.3 %) | 1 (20.0 %) | 4 (40.0 %) | |
| Fair (25–49 %) | 0 ( 0.0 %) | 0 ( 0.0 %) | 0 ( 0.0 %) | |
| Poor ( 0–24 %) | 0 ( 0.0 %) | 0 ( 0.0 %) | 0 ( 0.0 %) | |
| Total Treatment Period (Ave.) | 11.6 months | 10.0 months | 12.2 months | |
| Treatment Interval (Ave.) | 4.1 months | 3.8 months | 4.7 months | |
| No. of Treatment (Ave.) | 2.5 sessions | 2.5 sessions | 2.6 sessions | |
Anticipated acute complications were mild in severity and included swelling, pain and crust formation. All resolved completely within two weeks after treatment. PIE after separation of the microcrust was observed in 18 sessions (53.8 %), and disappeared at an average follow-up of 1.4 months. PIH was followed by improvement to complete resolution at an average follow-up of 2.7 months (Table 2). No complications, such as scarring, texture change or hypopigmentation, were recorded in the present study.
Table 2: Adverse events after ps-Alex laser treatment for nevus of Ota.
| Total | ps-Alex only | Pre–treatment(+) | |||
|---|---|---|---|---|---|
| N=15 | N=5 | N=10 | |||
| 38 sessions | 13 sessions | 25 sessions | |||
| Crust Formation : None | 15 (39.5 %) | 6 (46.2 %) | 8 (32.0 %) | ||
| Microcrust | 23 (60.5 %) | 7 (53.8 %) | 17 (68.0 %) | ||
| Crust | 0 ( 0.0 %) | 0 ( 0.0 %) | 0 ( 0.0 %) | ||
| Post Inflammatory Erythema: | 0 | 20 (52.6 %) | 6 (46.2 %) | 14 (56.0 %) | |
| 1+ | 14 (36.8 %) | 6 (46.2 %) | 8 (32.0 %) | ||
| 2+ | 4 (10.6 %) | 1 ( 7.6 %) | 3 (12.0 %) | ||
| Resolution Period of PIE (Ave.) | 1.4 months | 1.3 months | 1.4 months | ||
| PIH after 3 months: | 0 | 30 (78.9 %) | 10 (78.9 %) | 20 (80.0 %) | |
| 1+ | 8 (21.1 %) | 3 (21.1 %) | 5 (20.0 %) | ||
| 2+ | 0 ( 0.0 %) | 0 ( 0.0 %) | 0 ( 0.0 %) | ||
| Resolution Period of PIH (Ave.) | 2.7 months | 2.8 months | 2.7 months | ||
Representative results in two patients are shown for a 10 month old female infant treated with the ps-Alex laser in 3 sessions (Figure 1), and a 28 year old female also treated in 3 sessions (Figure 2). The independent grading in both patients was Excellent.
Figure 1:
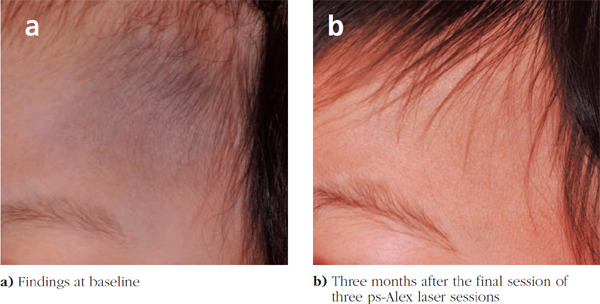
A 10-month-old female infant with previously untreated nevus of Ota
Figure 2:
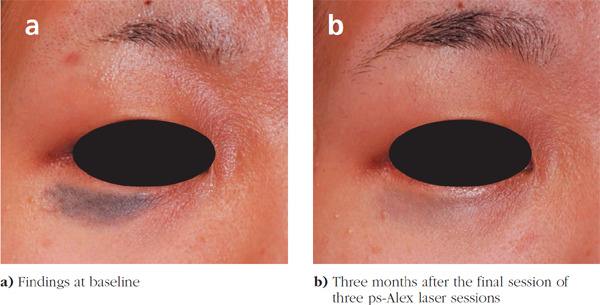
A 28-year-old female who had already undergone 2 sessions of Q-switched ruby laser
Discussion
Recently, treatment with the Q-switched ns-domain laser for nevus of Ota has been recognized as a standard approach, but complications such as hyperpigmentation, hypopigmentation, scar formation, and textural changes have reported after treatment 4–11) which sometimes seriously degraded the quality of life (QOL) of such affected patients. Ps-Alex laser treatment was scored Excellent by 66.7 % in our study subjects, with fewer sessions, a shorter erythema period, a shorter PIH period, and a shorter treatment period than we were historically used to with other treatment approaches, such as the Q-switched laser.
In our experience 13), we found some differences in crust formation, the length of the periods of erythema and secondary pigmentation when cases of nevus of Ota were treated with the Q-switched ruby laser compared with ps-Alex laser treatment. When the ISWP was used as the end-point in ps-Alex laser treatment for nevus of Ota, the microcrust formation followed on the irradiated area without blistering, which spontaneously separated around 10–14 days with slight erythema and pigment-clear skin. PIE lasted for 3–4 weeks and most of the PIH resolved in 3 months. On the other hand, patients treated with the Q-switched ruby laser got solid crusting, sometimes with blisters, on the treated skin which separated around 7–10 days with erythema and a bright blue-colored skin or pigment-clear skin. PIE was prolonged, lasting for 2–3 months, and during this period PIH appeared so that patients needed a 3–6 months' interval before the subsequent treatment to take care of the evolving skin conditions (Figure 3).
Figure 3:
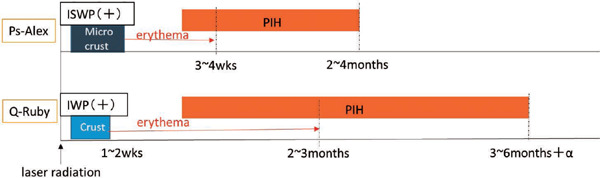
Comparison of crust formation, duration of post inflammatory erythema and post inflammatory pigmentation between the Q-switched ruby laser and ps-Alex laser.
When treating nevus of Ota with the Q-switched ruby lasers, more than 5–8 treatment sessions with a 3 to 6-month interval has usually been required to resolve the lesions clinically, normally accompanied by prolonged PIH. The total treatment period thus tended to be extended. Lu et al. mentioned the best treatment interval for nevus of Ota treated with the Q-switched Alex laser was 5 to 7 months, just as long as the Q-switched Ruby laser 14). Yu et al. reported in their meta-analysis that the treatment interval with the Q-switched Nd:YAG laser could be shorter than the Q-switched Alex laser because, theoretically, the longer Nd:YAG wavelength could avoid epidermal damage and enable deeper penetration. However, the longer wavelength of the Q-switched Nd:YAG laser could generate more collateral damage, and was associated with a higher complication rate than the Q-switched Alex laser 11). No matter what ns-domain laser wavelength was used, the inter-treatment interval had to be kept longer to avoid more serious complications.
In our study, following the ps-Alex laser treatments, little PIH was noted and it had resolved in 3 months in 78.9 % of all subjects. In addition, there was no complication with hypopigmentation, scar or texture change. Ps-domain laser irradiation can be almost instantaneously absorbed in epidermal and dermal chromophores in the skin with a combination of photomechanical and photothermal effects. This results in greater fragmentation of the pigment particles compared with the ns-domain laser, almost without collateral damage. We consider that, with treatment of nevus of Ota using the ps-Alex laser, we were able to achieve a similar level of clearance of skin as with the ns-domain laser. On the other hand, a shorter treatment interval and a shorter total treatment time could be expected with fewer complications. Moreover, ps-Alex laser treatment is associated with less damage to the epidermis, and can fragment deeper dermal melanin targets with its ultra-short pulse so that disturbing sequelae, such as heavy crust formation or bright blue darkening of the skin immediately after laser treatment, could be much less evident than in the case of treatment with the ns-domain laser. Patient post-treatment QOL is thus very much improved. Especially in Asians, PIE and PIH can occur in association with injury to the epidermis, particularly to the dermoepidermal junction, and repeated treatment sessions tend to result in untreatable hypopigmentation. A less-damaging treatment approach is therefore ideal and required. From this point of view, the ps-Alex laser might be a viable treatment option in treating nevus of Ota in the near future.
In our present study the number of cases is small and the follow-up period is comparatively short, so further randomized controlled trials involving larger patient populations and a long-term follow-up are required.
Conclusions
Based on our retrospective results, we propose that treatment of nevus of Ota with the ps-Alex laser is safe and effective. Moreover it appears more efficient than treatment with the Q-switched ruby laser from the point of decreased side effects such as PIE and PIH. We further suggest that both the inter-treatment interval and total treatment period could be shortened using the ps-Alex laser.
References
- 1: Oshiro T. Laser treatment for nevi. 1980, Medical Laser Research Co. Ltd. Tokyo; Pp17-52. [Google Scholar]
- 2: Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983; 220(4596):524-527 [DOI] [PubMed] [Google Scholar]
- 3: Anderson RR, Margolis GJ, Watanabe S, Flotte T, Hruza GJ, Dover JS. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd:YAG laser pulses at 1064, 532 and 355nm. J Invest Dermatol. 1989; 93: 28-32. [DOI] [PubMed] [Google Scholar]
- 4: Watanabe S, Takahashi H, Treatment of nevus of Ota with Q-switched ruby laser. N Engl J Med. 1994; 331: 1745-50 [DOI] [PubMed] [Google Scholar]
- 5: Kono T, Chan HL, Erçöçen A, Kikuchi Y, Uezono S, Iwasaka S, Isago T, Nozaki M. Use of Q-switched Ruby Laser in the Treatment of Nevus of Ota in Different Age Groups. Lasers in Surg Med. 2003; 32: 39-395 [DOI] [PubMed] [Google Scholar]
- 6: Choi CW, Kim HJ, Lee HJ, Kim YH, Kim WS. Treatment of nevus of Ota using low fluence Q-switched Nd:YAG laser. Inter J Derm. 2014; 53: 861-865 [DOI] [PubMed] [Google Scholar]
- 7: Shirakawa M, Ozawa T, Ohasi N, Ishii M, Harada T. Comparison of regional efficacy and complications in the treatment of aberrant Mongokian spots with the Q-switched ruby laser. J Cosme Laser Ther. 2010; 12: 138-142 [DOI] [PubMed] [Google Scholar]
- 8: Felton SJ, Niaimi FA, Ferguson JE, Mdan V. Our perspective of the treatment of neavus of Ota with 1,064-,755- and 532-nm wavelength lasers. Lasers Med Sci. 2014; 29: 1745-1749 [DOI] [PubMed] [Google Scholar]
- 9: Lam A.Y.-M., Wong D.S.-Y., Lam L.-K., Ho W.-S., Chan H.H.-L. A Retrospective Study on the Efficacy and complications of Q-switched Alexandrite laser in the treatment of Acquired Bilateral Nevus of Ota-like Macules. Dermatol Surg. 2001;27:11: 937-942. [DOI] [PubMed] [Google Scholar]
- 10: Kagami S, Asahina A, Watanabe R, Mimura Y, Shirai A, Hattori N, Watanabe T, Tamaki K. Treatment of 153 Japanese patients with Q-switched alexandrite laser. Lasers Med Sci. 2007; 22: 159-163 [DOI] [PubMed] [Google Scholar]
- 11: Yu P, Yu N, Diao W, Yang X, Feng Y, Qi Z. Comparison of clinical efficacy and complications between Q-switched alexandrite laser and Q-switched Nd:YAG laser on nevus of Ota: a systematic review and meta-analysis. Lasers Med Sci. 2016; 31:581-591 [DOI] [PubMed] [Google Scholar]
- 12: Bernstein EF, Schomacker KT, Basilavecchio LD, Plugis JM, Bhawalkar JD. A Novel Dual-Wavelength, Nd:YAG, picosecond-Domain Laser Safely and Effectively Removes Multicolor Tattoos. Lasers in Serg Med. 2015;47:52-548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13: Ohshiro T, Oshiro T, Sasaki K, Kishi K. Picosecond pulse duration laser treatment for dermal melanocytosis in Asians : A retrospective review. Laser Therapy. 2016; 25.2; 99-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14: Lu Z, Fang L, Jiao S. Treatment of nevus of Ota with the Q-switched Alexandrite laser. Chin Med J. 2003;116:226-230 [PubMed] [Google Scholar]


